Professional Documents
Culture Documents
Clinics in Surgery: Fecopneumothorax Surgery by Thoracoabdominal Incision After Mckeown Esophagectomy
Uploaded by
saraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinics in Surgery: Fecopneumothorax Surgery by Thoracoabdominal Incision After Mckeown Esophagectomy
Uploaded by
saraCopyright:
Available Formats
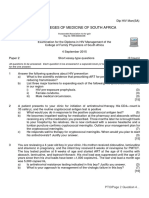
Clinics in Surgery Case Report
Published: 12 Oct, 2018
Fecopneumothorax Surgery by Thoracoabdominal Incision
after McKeown Esophagectomy
Julio Sesma1 and Mong-Wei Lin2*
1
Department of Thoracic Surgery, Hospital General Universitario Alicante, Alicante, Spain
2
Department of Surgery, National Taiwan University Hospital and National Taiwan University College of Medicine,
Taipei, Taiwan
Abstract
Fecopneumothorax is an unusual but life-threatening condition. Fecopneumothorax after
esophagectomy is extremely rare, with only two reported cases; it is managed with a two-
staged surgical approach: Laparotomy followed by thoracotomy. We report the first case, to our
knowledge, of fecopneumothorax due to colonic intrathoracic perforation after minimally invasive
esophagectomy managed by a left thoracoabdominal incision and barrel-loop colostomy. As the
surgical field was already known to be contaminated, loop colostomy was considered to avoid
anastomotic site leakage and related complications. The thoracoabdominal incision is a safe and
feasible approach that allows one-step surgery for the thoracic and abdominal field.
Introduction
Fecopneumothorax is an unusual but life-threatening condition that is usually associated with
intrathoracic colon perforation due to a strangulated diaphragmatic hernia [1-4]. The most frequent
causes are congenital [3] and traumatic conditions [4] but it can also occur as an extremely rare
complication after esophagectomy [1,2]. In global literature, only two cases of fecopneumothorax
after esophagectomy [1,2] have been reported that were treated by a two-stage surgery: Laparotomy
for hernia reduction and colectomy in the first stage and lateral thoracotomy or video-assisted
thoracic surgery (VATS) for decortication in the second stage. We present the first case in the world
literature for fecopneumothorax due to colonic intrathoracic perforation after minimally invasive
esophagectomy managed by a left thoracoabdominal incision.
OPEN ACCESS Case Presentation
*Correspondence: A 59-year-old man who had undergone a minimally invasive McKeown esophagectomy
Mong-Wei Lin, Department of Surgery, with VATS and laparoscopic approach as well as gastric tube reconstruction due to middle third
National Taiwan University Hospital and esophageal squamous cell carcinoma was referred to our department 12 months after surgery.
National Taiwan University College of The first follow-up computed tomography (CT) shows no diaphragmatic hernia 6 months after
Medicine, Taipei, Taiwan, Tel: 886-2- minimally invasive McKeown esophagectomy. He complained about intermittent cramping
2312-3456 (ext. 65085);
epigastric pain and dyspnea 7 days before this admission. Physical examination revealed tachycardia
(122/min) and tachypnea (22/min) with decreased breathing sounds on the left side. Laboratory data
E-mail: mwlin@ntu.edu.tw
showed a white blood cell count of 11930/µL with left shift change (Seg 86.0%), elevated C-reactive
Received Date: 10 Sep 2018
protein (> 40 mg/dL), elevated blood urea nitrogen (BUN)/creatinine (77.1/3.6 mg/dL) and elevated
Accepted Date: 10 Oct 2018
lactate level (2.88 mmol/L). Blood gas analysis showed severe acidosis (pH 7.141, pCO2 45.3 mmHg,
Published Date: 12 Oct 2018
HCO3 15.3 mmol/L, base excess -13.9 mmol/L). A chest radiograph revealed left basal and lateral
Citation: pneumothorax, with pleural effusion and lower lung collapse. The left, upper-chest field showed one
Sesma J, Lin M-W. Fecopneumothorax huge bullous lesion. The CT scan showed a diaphragmatic hernia, intrathoracic perforation of the
Surgery by Thoracoabdominal Incision transverse colon, and pleural effusion. The diagnosis was confirmed as colon perforation-related
after McKeown Esophagectomy. Clin fecopneumothorax with septic shock and acute renal failure.
Surg. 2018; 3: 2155.
We performed an emergent left-thoracoabdominal incision to explore and repair the colonic
Copyright © 2018 Mong-Wei Lin. This and diaphragmatic injuries at the same stage of surgery. The surgery started within 6 hrs after
is an open access article distributed patient arrival at our emergency department. We identified the site of the diaphragmatic hernia and
under the Creative Commons Attribution perforated colon in the left hemithorax, with a total of 700 cc of fecaloid effusion surrounding the
License, which permits unrestricted area. Diffuse pleural thickening was noted (Figure 2B). Suction of the thoracic fecaloid effusion and
use, distribution, and reproduction in VATS decortication was performed to allow adequate lung expansion. The transverse colon was
any medium, provided the original work firmly incarcerated in the hiatal defect of the diaphragm. Therefore, the peritoneal cavity was not
is properly cited. contaminated with fecaloid effusion. Ischemic compromise and transverse colon perforation were
Remedy Publications LLC., | http://clinicsinsurgery.com/ 1 2018 | Volume 3 | Article 2155
Mong-Wei Lin, et al., Clinics in Surgery - Thoracic Surgery
found, so we performed a transverse colon necrotic portion resection repair as the first stage of surgery may lead to contamination of the
at the level of the incarcerated site. Due to poor bowel preparation, we peritoneal cavity. We suggest that the thoracoabdominal approach
did not perform direct colon anastomosis. A double-barrel colostomy allows better exposure of both cavities, thereby helping to perform
involving the proximal and distal end of the colon was performed. meticulous decortication with subsequent diaphragmatic repair. In
The diaphragmatic defect was repaired by primary suture. Thoracic addition, colon replacement can be better performed via 2 cavities for
and abdominal cavities were irrigated with warm saline fluid. visual control, to identify any thoracic or abdominal inconvenience
during the repositioning maneuvers.
The patient’s clinical condition improved after surgery. The
inotropic agent was discontinued on the second postoperative day. In the 2 reported cases, no loop colostomy was performed. As in
Renal function recovered to the normal range. He was transferred our case, fecopneumothorax due to intrathoracic colonic perforation
to the general ward on the third postoperative day. His condition can lead to quick clinical worsening, severe septic shock, and
was complicated with limited surgical wound infection to the lower multiple organ failure. Therefore, in this context, with poor colonic
part of the wound. Wound culture revealed Bacteroides fragilis preparation and the presence of an already contaminated surgical
and Enterococcus avium. The wound condition improved after field, loop colostomy and anastomosis in a second-stage operation
wound care and antibiotic therapy. The patient was discharged on could be a good strategy to avoid anastomotic site leakage and related
postoperative day 33 and readmitted for colostomy closure 2 months complications. The colostomy closure may be scheduled 1-2 months
postoperatively. No other complications occurred and the follow-up after the first episode of sepsis recovery.
was uneventful.
Although fecopneumothorax due to colonic perforation is an
Comment extremely rare presentation after esophagectomy, it can lead to
life-threatening conditions. Thoracoabdominal incision is a safe
Fecopneumothorax due to colonic perforation is an extremely
and feasible approach that allows one-step surgery for thoracic
rare presentation after esophagectomy [1,2]. To our knowledge,
and abdominal fields, helping colonic replacement maneuvers,
this is the third case of fecopneumothorax after esophagectomy;
decortication, and diaphragmatic repair. As the surgical field is already
the first one was managed through a thoracoabdominal approach.
known to be contaminated, loop colostomy should be considered to
Fecopneumothorax may occur from 2 months to 10 years after the first
avoid anastomotic site leakage and related complications.
esophageal surgery. The first case underwent a left hemicolectomy,
pleural cavity lavage, and primary transverse/sigmoid colon Acknowledgement
anastomosis [2]. The second case underwent colectomy for resection
The authors declare no conflicts of interest. This study was
of the necrotic portion and primary anastomosis, thoracic irrigation,
supported by the Ministry of Science and Technology, Taiwan
and debridement [1]. The surgical procedures of the previous two
(MOST105-2628-B002-011-MY2) and National Taiwan University
cases were both performed as two-stage surgeries: Laparotomy at the
Hospital, Taipei, Taiwan (NTUH107-N004038).
first stage and then thoracotomy at the second stage. Besides, the 2
previous cases underwent primary anastomosis despite poor colon References
preparation. By contrast, this case underwent a left thoracoabdominal 1. Kim KW, Lee JI, Kim JS, Park KY, Park CH, Jeon YB. Fecopneumothorax:
approach with a double-barrel colostomy. The colostomy closure was a rare case of delayed colon diaphragmatic herniation following
performed 2 months after the first surgery. esophagectomy. Indian J Surg. 2015;77:117-9.
Fecopneumothorax can lead to life-threatening conditions. 2. Markogiannakis H, Theodorou D, Tzertzemelis D, Dardamanis D,
Therefore, early surgical intervention with an appropriate approach is Toutouzas KG, Misthos P, et al. Fecopneumothorax: a rare complication
a key to achieve successful treatment. Instead of two-step surgeries with of esophagectomy. Ann Thorac Surg. 2007;84(2):651-2.
independent approaches, we propose a thoracoabdominal approach 3. Chai Y, Zhang G, Shen G. Adult Bochdalek hernia complicated with a
to allow full cleaning of the chest cavity and complete decortication, perforated colon. J Thorac Cardiovasc Surg. 2005;130(6):1729-30.
diaphragm repair, and colonic replacement and resection in a one- 4. Seelig MH, Klingler PJ, Schönleben K. Tension fecopneumothorax due to
step surgery. As the surgical field is already contaminated in the colonic perforation in a diaphragmatic hernia. Chest. 1999;115:288-91.
thoracic area, a laparotomy for the perforated colon reduction and
Remedy Publications LLC., | http://clinicsinsurgery.com/ 2 2018 | Volume 3 | Article 2155
You might also like
- McKeown EsophagectomyDocument9 pagesMcKeown EsophagectomyDa JunNo ratings yet
- 1 s2.0 S2210261223004741 MainDocument5 pages1 s2.0 S2210261223004741 MainDevita SanangkaNo ratings yet
- Spontaneous Perforation of A Malignified Corrosive Stricture of The Esophagus and Subsequent Perforation of A Giant Duodenal Stress UlcusDocument4 pagesSpontaneous Perforation of A Malignified Corrosive Stricture of The Esophagus and Subsequent Perforation of A Giant Duodenal Stress UlcusTeodorNo ratings yet
- Massive Right Hemothorax As The Source of Hemorrhagic Shock After Laparoscopic Cholecystectomy - Case Report of A Rare Intraoperative ComplicationDocument3 pagesMassive Right Hemothorax As The Source of Hemorrhagic Shock After Laparoscopic Cholecystectomy - Case Report of A Rare Intraoperative ComplicationDaniel LesmanaNo ratings yet
- Duodenal Perforation Following Blunt Abdominal Trauma - ProQuest PDFDocument5 pagesDuodenal Perforation Following Blunt Abdominal Trauma - ProQuest PDFWilliam WiryawanNo ratings yet
- Bile Duct Injuries in Difficult Laparoscopic CholecystectomyDocument7 pagesBile Duct Injuries in Difficult Laparoscopic CholecystectomyAna MariaNo ratings yet
- R HemicolectomyDocument15 pagesR Hemicolectomyrwilah100% (1)
- An Unusual Cause of Acute Abdominal Pain in Oncology: Jejunostomy Tube Placement ComplicationDocument4 pagesAn Unusual Cause of Acute Abdominal Pain in Oncology: Jejunostomy Tube Placement ComplicationIJAR JOURNALNo ratings yet
- Pi Is 2213576614000049Document3 pagesPi Is 2213576614000049Ditha FadhilaNo ratings yet
- Surgical Endoscopy Oct.1997Document87 pagesSurgical Endoscopy Oct.1997Saibo BoldsaikhanNo ratings yet
- Fonc 12 803221Document4 pagesFonc 12 803221Haekal HafizhNo ratings yet
- Perineal hernia mesh repair techniqueDocument15 pagesPerineal hernia mesh repair techniqueValean DanNo ratings yet
- Laparoscopic Cholecystectomy After Conservative Su - 2024 - International JournaDocument4 pagesLaparoscopic Cholecystectomy After Conservative Su - 2024 - International JournaRonald QuezadaNo ratings yet
- Nasser2015Document5 pagesNasser2015hengkileonardNo ratings yet
- Surgery Open Digestive Advance: G. Pasinato, J.-M RegimbeauDocument7 pagesSurgery Open Digestive Advance: G. Pasinato, J.-M RegimbeauRashmeeta ThadhaniNo ratings yet
- Obstructed Left Colon One Stage Surgery in A Developing CountryDocument2 pagesObstructed Left Colon One Stage Surgery in A Developing CountrysolysanNo ratings yet
- Reconstruction of A Traumatic Duodenal Transection With A Pedicled Ileal Loop: A Case ReportDocument6 pagesReconstruction of A Traumatic Duodenal Transection With A Pedicled Ileal Loop: A Case ReportHanny RusliNo ratings yet
- Diagnosing Gastric Volvulus in Chest X-Ray: Report of Three CasesDocument4 pagesDiagnosing Gastric Volvulus in Chest X-Ray: Report of Three CasesSuraj KurmiNo ratings yet
- Baldoni 2011Document10 pagesBaldoni 2011naili nsnNo ratings yet
- Laparoscopic Repair of Vesicovaginal FistulaDocument4 pagesLaparoscopic Repair of Vesicovaginal FistulaGloria AteNo ratings yet
- Evaluating Esophagectomy Complications Using International Consensus DefinitionsDocument7 pagesEvaluating Esophagectomy Complications Using International Consensus DefinitionsPaulo RoseroNo ratings yet
- Laparoscopy Improves Outcomes for Peritoneal Dialysis CathetersDocument9 pagesLaparoscopy Improves Outcomes for Peritoneal Dialysis CathetersdharmaNo ratings yet
- Oesophagocoloplasty Outcomes for Corrosive StricturesDocument12 pagesOesophagocoloplasty Outcomes for Corrosive StricturesSpandan KadamNo ratings yet
- Vascular High Ligation and Embryological Dissection in Laparoscopic Restorative Proctocolectomy For Ulcerative ColitisDocument3 pagesVascular High Ligation and Embryological Dissection in Laparoscopic Restorative Proctocolectomy For Ulcerative ColitisYacine Tarik AizelNo ratings yet
- Sotelo Et Al, Laparoscopic Rectovesical Fistula RepairDocument5 pagesSotelo Et Al, Laparoscopic Rectovesical Fistula RepairjordynixnNo ratings yet
- Adenocarcinoma Arising in A Colonic Interposition After Esophagectomy For Benign Stricture and Review of The LiteratureDocument3 pagesAdenocarcinoma Arising in A Colonic Interposition After Esophagectomy For Benign Stricture and Review of The LiteratureMaghfirah MahmuddinNo ratings yet
- 19Document3 pages19Elizabeth ToapantaNo ratings yet
- Jurding 1Document7 pagesJurding 1Yuda DanangNo ratings yet
- Chevallay 2020Document17 pagesChevallay 2020Maria PalNo ratings yet
- Pub+Enterite+Necrozante+Iasi UnlockedDocument5 pagesPub+Enterite+Necrozante+Iasi UnlockedlPiNGUSlNo ratings yet
- Lap Chole Case StudyDocument3 pagesLap Chole Case StudyKinshuki Jain100% (1)
- Williams2013 Article LaparoscopicManagementOfHighTrDocument3 pagesWilliams2013 Article LaparoscopicManagementOfHighTrVishnu priya kokkulaNo ratings yet
- Trauma Abdomen 3Document3 pagesTrauma Abdomen 3Miftah MiftahNo ratings yet
- Management of Enterocutaneous FistulaDocument11 pagesManagement of Enterocutaneous FistulaSyed Nusrath100% (1)
- Portal Vein Injury in A Patient Undergoing Video-Assisted Cholecystectomy: Case Report and Review of LiteratureDocument4 pagesPortal Vein Injury in A Patient Undergoing Video-Assisted Cholecystectomy: Case Report and Review of LiteratureYacine Tarik AizelNo ratings yet
- Abdomen FungusDocument7 pagesAbdomen FungusHAMMADNo ratings yet
- A Case of Primary Actinomycosis and Secondary Eumycetoma in Anterior Abdomen Wall - A Case ReportDocument7 pagesA Case of Primary Actinomycosis and Secondary Eumycetoma in Anterior Abdomen Wall - A Case ReportHAMMADNo ratings yet
- San Pablo Colleges Medical Center case presentation on cholelithiasisDocument43 pagesSan Pablo Colleges Medical Center case presentation on cholelithiasisMary Rose LinatocNo ratings yet
- Subhepatic Appendix: An Ectopic Topography Not To Be Disregarded: A Case ReportDocument4 pagesSubhepatic Appendix: An Ectopic Topography Not To Be Disregarded: A Case ReportPawan MishraNo ratings yet
- Transanal Minimally Invasive Surgical Approach To Total Pelvic ExenterationDocument7 pagesTransanal Minimally Invasive Surgical Approach To Total Pelvic ExenterationWarren SeowNo ratings yet
- Successful Emergency Resection of A Massive Intra-Abdominal Hemophilic PseudotumorDocument5 pagesSuccessful Emergency Resection of A Massive Intra-Abdominal Hemophilic Pseudotumoryudhi kurniawanNo ratings yet
- perbaikan anastomosisDocument6 pagesperbaikan anastomosisReagen DeNo ratings yet
- 1 s2.0 S0065341116000038 MainDocument12 pages1 s2.0 S0065341116000038 MainFlorin AchimNo ratings yet
- Anesthetic Management of Esophageal Atresia Correction in a NewbornDocument4 pagesAnesthetic Management of Esophageal Atresia Correction in a NewbornRicardo HernandezNo ratings yet
- KJR 18 299Document10 pagesKJR 18 299Willian HolandaNo ratings yet
- 4 PDFDocument3 pages4 PDFSamiaNazNo ratings yet
- Clinical Outcomes After Restorative Proctocolectomy With IPAA Using Ultrasonically Activated Scalpel For Ulcerative Colitis (2012)Document9 pagesClinical Outcomes After Restorative Proctocolectomy With IPAA Using Ultrasonically Activated Scalpel For Ulcerative Colitis (2012)陳玉芝No ratings yet
- Short esophagus surgery relieves symptomsDocument4 pagesShort esophagus surgery relieves symptomsayuNo ratings yet
- Management of Incidental Bochdalek Hernia in An Asymptomatic Adult: A Case ReportDocument4 pagesManagement of Incidental Bochdalek Hernia in An Asymptomatic Adult: A Case ReportBhushan D ThombareNo ratings yet
- Submental Intubation in Patients With Complex Maxillofacial InjuriesDocument4 pagesSubmental Intubation in Patients With Complex Maxillofacial InjuriesMudassar SattarNo ratings yet
- An Unusual Source of Tension - ChestDocument5 pagesAn Unusual Source of Tension - ChestKaran KalraNo ratings yet
- Jurnal Bedah 2Document5 pagesJurnal Bedah 2nafamaulidinaNo ratings yet
- Post Polypectomy Electrocoagulation Syndrome A Rare Cause of Acute Abdominal PainDocument5 pagesPost Polypectomy Electrocoagulation Syndrome A Rare Cause of Acute Abdominal PainCom DigfulNo ratings yet
- Ms AJCRS 99757Document6 pagesMs AJCRS 99757Cesar DominguezNo ratings yet
- Delayed Diaphragmatic Hernia DiagnosisDocument3 pagesDelayed Diaphragmatic Hernia DiagnosisNining Rhyanie TampubolonNo ratings yet
- Lap Chole DictationDocument2 pagesLap Chole DictationAshish DongreNo ratings yet
- 4 Series CPTDocument13 pages4 Series CPTPraviiNo ratings yet
- Open Versus Laparoscopic Mesh Repair of Ventral Hernias: A Prospective StudyDocument3 pagesOpen Versus Laparoscopic Mesh Repair of Ventral Hernias: A Prospective Study'Adil MuhammadNo ratings yet
- The Ileoanal Pouch: A Practical Guide for Surgery, Management and TroubleshootingFrom EverandThe Ileoanal Pouch: A Practical Guide for Surgery, Management and TroubleshootingJanindra WarusavitarneNo ratings yet
- Hawaii Medical PediatricsDocument10 pagesHawaii Medical PediatricstinkictijoNo ratings yet
- Check Your English Vocabulary For MedicineDocument65 pagesCheck Your English Vocabulary For MedicineOlga Poleszak100% (1)
- Change Management in Health Care: Robert James Campbell, EddDocument17 pagesChange Management in Health Care: Robert James Campbell, EddeossNo ratings yet
- Ectopic PregnancyDocument39 pagesEctopic PregnancyMuhammad SherazNo ratings yet
- Dip HIV Man (SA) Past Papers - 2015 2nd Semester 24-1-2017Document2 pagesDip HIV Man (SA) Past Papers - 2015 2nd Semester 24-1-2017matentenNo ratings yet
- Medical CertificateDocument126 pagesMedical CertificateAnonymous mummYD0% (1)
- Know Your Magnetic FieldDocument75 pagesKnow Your Magnetic FieldAtma Jnani100% (5)
- PTA 210 PTA Technique: Vital SignsDocument64 pagesPTA 210 PTA Technique: Vital SignsChristelle Brookshiel Demayo MarbaNo ratings yet
- Chapter 69 Nursing Management EmergencyDocument6 pagesChapter 69 Nursing Management EmergencyMeganNo ratings yet
- Differential Diagnosis of Scalp Hair FolliculitisDocument8 pagesDifferential Diagnosis of Scalp Hair FolliculitisandreinaviconNo ratings yet
- Chin 2001Document13 pagesChin 2001zaheerbdsNo ratings yet
- Vital Signs GuideDocument4 pagesVital Signs GuideellithNo ratings yet
- Ncp-Ineffective Tissue Perfusion (Aortic Stenosis)Document2 pagesNcp-Ineffective Tissue Perfusion (Aortic Stenosis)Daniel Vergara Arce67% (3)
- SM REF 0020, Ethox Infu SurgPressureInfusion Rev1Document1 pageSM REF 0020, Ethox Infu SurgPressureInfusion Rev1icuNo ratings yet
- Report - For MaamDocument7 pagesReport - For MaamSherchen Antonio-CortesNo ratings yet
- Counselling of PatientsDocument38 pagesCounselling of Patientsamir masaud100% (1)
- Surgical Pathology of The Gastrointestinal System Bacterial, Fungal, Viral, and Parasitic Infections PDFDocument234 pagesSurgical Pathology of The Gastrointestinal System Bacterial, Fungal, Viral, and Parasitic Infections PDFBogdan CarabasNo ratings yet
- NSVD Patient Sleep IssuesDocument3 pagesNSVD Patient Sleep IssuesAlma Gobaleza100% (1)
- AsphyxiaDocument35 pagesAsphyxiaAna Cristina Montillano100% (1)
- Qip PesentationDocument14 pagesQip Pesentationapi-340409341No ratings yet
- Osce EmergenciesjDocument31 pagesOsce EmergenciesjTess WilliamsNo ratings yet
- United States Complaint in Intervention in False Claims Act Lawsuits Accusing Insys Therapeutics of Paying Kickbacks and Engaging in Other Unlawful Practices to Promote Subsys, A Powerful Opioid PainkillerDocument37 pagesUnited States Complaint in Intervention in False Claims Act Lawsuits Accusing Insys Therapeutics of Paying Kickbacks and Engaging in Other Unlawful Practices to Promote Subsys, A Powerful Opioid PainkillerBeverly Tran100% (1)
- Intravenous Nutrient TherapyDocument15 pagesIntravenous Nutrient TherapySuresh IndiaNo ratings yet
- Annotated BibliographyDocument4 pagesAnnotated Bibliographyapi-317390500No ratings yet
- Analysis of The Galactose-1-Phosphate Uridyltransferase Gene in Specimens Identified Through Newborn ScreeningDocument1 pageAnalysis of The Galactose-1-Phosphate Uridyltransferase Gene in Specimens Identified Through Newborn ScreeningboyzbanjarboyzNo ratings yet
- Placement - BrochureDocument2 pagesPlacement - Brochureapi-266528333No ratings yet
- Pancreatic Pseudocyst Laparoscopic Drainage Case ReportDocument17 pagesPancreatic Pseudocyst Laparoscopic Drainage Case ReportrazvanccNo ratings yet
- Inpatient Department OverviewDocument25 pagesInpatient Department OverviewRachana VishwajeetNo ratings yet
- 9 Tips On How To Make A Good SOAPIEDocument7 pages9 Tips On How To Make A Good SOAPIEMagbanua Airene MarielNo ratings yet
- Programme BroshureDocument2 pagesProgramme BroshureMagilas S. SalvacionNo ratings yet