Professional Documents
Culture Documents
Basilar Artery Duplication
Uploaded by
ChavdarCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Basilar Artery Duplication
Uploaded by
ChavdarCopyright:
Available Formats
289
Case Report
I
Percutaneous Transhepatic Recanalization and
Thrombolysis of the Superior Mesenteric Vein
J. Robert Yankes,1 John P. Uglietta,1 John Grant,2 and Simon D. Braun1’3
Thrombolysis has been described in a variety of settings branch of the right portal vein was punctured in a single pass with a
and is well established in the treatment of peripheral arterial, 22-gauge Chiba needle (Medi-Tech, Watertown, MA). A 0.01 8-in.
dialysis shunt, and coronary arterial thrombosis. We report (0.046-cm) mandril guidewire was advanced into the portal vein. A
our experience in applying this technique in a patient who had coaxial 4/6 French Braun dilator (Cook, Bloomington, IN) was used
to dilate the tract with exchange to a 6.5-French Kumpe catheter
thrombosis of the superior mesenteric vein.
(Cook). Vigorous hand injection showed a contour bulge at the orifice
of the superior mesenteric vein. A 0.038-in. (0.097-cm) straight guide-
wire was used to probe the orifice and was advanced through the
Case Report
thrombus. The wire was advanced more peripherally into the superior
A 58-year-old woman presented with a 10-month history of pro- mesentenc vein, and the Kumpe catheter was advanced through the
gressive epigastric and back pain and recent onset of jaundice and thrombus. As the catheter was slowly withdrawn through most of
acholic stools. An abdominal CT was performed at another hospital, the length of the thrombus, urokinase was injected by hand at a
and a mass was identified in the head of the pancreas. Subsequent concentration ofS000 units/mlfor a total of2O,000 units. The catheter
percutaneous biopsy revealed pancreatic carcinoma. She was trans- was left with its tip embedded in the most central portion of the
ferred to Duke University Medical Center and underwent a pancrea- thrombus, and urokinase was infused at a rate of 4000 units/mm for
ticoduodenectomy. During this procedure, the superior mesenteric a total of 4 hr, with periodic hand injections of contrast material to
vein was mobilized and freed of adherent tumor, leading to a rent in adjust the catheter position more peripherally and to follow the
the vein, which was closed with a 6.0 suture. Her postoperative progression of thrombolysis. After demonstration of a narrow but
course was complicated by sepsis, pneumonia, and respiratory dis- patent lumen, a 0.038-in. (0.097-cm) guidewire was once again
tress requiring prolonged intubation. She developed massive ascites advanced into the peripheral superior mesenteric vein, and an 8-mm
and had hypoactive-to-absent bowel sounds. Plain abdominal radio- occlusion balloon was introduced. This was swept repeatedly through
graphs suggested the presence of bowel wall edema. A CT scan the central region of the superior mesenteric vein in order to clear
suggested thrombus in the superior mesenteric vein (Fig. 1A). She residual thrombus. At the location of previous thrombosis, significant
was started on total parenteral nutrition. Three weeks later, because resistance and balloon deformation indicated a structural stenosis.
her condition had not improved, the patient was referred for mesen- An 8-mm-diameter angioplasty balloon was introduced, and the vein
teric angiography, which revealed severe peripheral splanchnic vaso- was dilated with three separate 60-sec inflations. Reinjection of the
constriction, bowel wall thickening, and occlusion of the proximal peripheral superior mesenteric vein through the angioplasty balloon
superior mesenteric vein (Fig. 1B). Selective splenic arteriography lumen showed patency (Fig. i C). The catheter was slowly withdrawn
showed patency of the portal vein. Because of the patient’s poor through the portal vein until hand injection of contrast material mdi-
overall physical condition, she was considered a poor candidate for cated that its tip lay in the liver parenchyma. Two tandemly placed 3-
surgical thrombectomy and was referred for percutaneous recanali- mm Gianturco coils were deposited within the tract, and a single large
zation of the superior mesenteric vein. plug of Gelfoam was placed peripherally near the liver surface. The
Because the splanchnic venous flow was being shunted away from patient was then given heparin.
the occlusion by collateral vessels and because an arterial approach Bowel sounds gradually returned during the week after the pro-
would preclude passing a guidewire through the occluded segment cedure. A follow-up sonogram of the portal and mesenteric veins
to create a channel for the flow of thrombolytic agents, a portal indicated antegrade flow of blood from the superior mesenteric vein
venous approach was chosen. In order to limit the number of needle into the portal vein, and CT performed 16 days later confirmed
passes and thus reduce the risk of hemorrhage, sonographic guid- patency of the superior mesenteric and portal veins. Ascites gradually
ance was used to choose an entry point for transhepatic catheteri- resolved, and the patient was started on nasojejunal tube feedings.
zation of the portal vein. With the patient under local anesthesia, a Two weeks later, clinical deterioration led to exploratory laparotomy,
Received January 4, 1988; accepted after revision February 21 , 1988.
I Department of Radiology, P.O. Box 3808, Duke University Medical Center, Durham, NC 27710. Address reprint requests to J. R. Yankes.
2 Department of Surgery, Duke University Medical Center, Durham, NC 27710.
3 Present address: Department of Radiology, Memorial Mission Hospital, Asheville, NC 28801.
AJR 151:289-290, August 1988 0361-803X/88/1 51 2-0289 © American Roentgen Ray Society
Fig. 1.-58-year-old woman who had thrombosis of the superior mesenteric vein.
A, CT scan shows thrombus within superior mesenterlc veIn (arrow).
B, Venous phase of superior mesenteric arteriogram shows occlusion of superior mesenteric vein.
C, Postangloplasty Injection of superior mesenteric veIn (arrow) shows patency. Note peripheral splanchnic venous channel (arrowhead).
at which time a short segment of ischemic small bowel was resented. urokinase would minimize any risks associated with potential
The superior mesenteric vein was found to be patent. Progressive embolization of fragments of clot. We employed standard
recovery followed, and the patient was discharged from the hospital techniques of percutaneous transhepatic portography [7] to
in good condition.
gain access to the portal system and adapted the technique
of high-dose urokinase infusion, as previously described for
use in the peripheral arterial system [8]. The use of sono-
Discussion graphic guidance allowed entry into the portal system in a
single pass with a small-gauge Chiba needle; embolization of
Thrombosis of the superior mesenteric vein is a relatively
the access tract at the conclusion of the procedure provided
uncommon cause of intestinal vascular compromise; several hemostasis, thus improving the margin of safety. No data
studies have shown frequencies of 5-23% [i -3]. Thrombosis exist regarding the safety of splanchnic venous angioplasty
may develop in association with portal hypertension, focal or in the postoperative period. It was thought that the thrombotic
generalized abdominal inflammation, or hypercoagulable occlusion was almost certainly the result of the surgically
states; after trauma; or in the perioperative period. It also may induced stenosis and that the likelihood of long-term patency
occur as a primary event [4]. Clinically, it may be acute or would be low if this were not corrected. As the alternative to
subacute. Abdominal pain is usually present and may be of successful percutaneous treatment would have been reex-
either sudden or gradual onset. Physical examination and ploration and venous bypass, the potential benefit of the
laboratory evaluation reveal inconstant and nonspecific find-
procedure was thought to outweigh the risk. Our results
ings such as fever, evidence of volume depletion, ascites, suggest that in the subset of patients with thrombosis of the
leukocytosis, systemic acidosis, and blood in the stools. superior mesenteric vein and nongangrenous bowel, throm-
Plain abdominal radiography may show ileus or ascites.
bolysis via the percutaneous transhepatic approach may be
Bowel wall thickening and mucosal irregularity, when present,
a useful initial approach to treatment.
are suggestive of intestinal ischemia. Specific diagnosis of
mesenteric venous thrombosis requires angiography or dem-
onstration of an intraluminal filling defect on CT. REFERENCES
Nonsurgical treatment of portal vein occlusion has been 1 . Muniaguma S. Mesenteric vascular
AJ, Allender disease: clinical features
described. Paquet et al. [5] used IV streptokinase in the and review of the literature. Med Ann DC 1974;43(6):295-305
fibrinolytic therapy of portal vein thrombosis and described a 2. Sigh AP, Shah AC, Lee ST. Acute mesenteric vascular occlusion: a
review of thirty-two patients. Surgery 1975;78(5):617-618
favorable outcome in five patients. Uflacker et al. [6] described
3. Ver Steeg KR, Broders CW. Gangrene of the bowel. Surg Clin North Am
the treatment of portal vein occlusion by percutaneous (trans- 1979;59(5):869-876
hepatic) angioplasty. 4. Grendell JH, Ockner AK. Mesenteric venous thrombosis. Gastroenterology
However, to our knowledge, neither the percutaneous re- 1982;82:358-372
canalization of the superior mesenteric vein nor the direct 5. Paquet KJ, Raschke E, Popov S, BUcheler E. The fibrinolytic therapy of
thrombosed portal veins and shunts in liver cirrhosis with portal hyperten-
infusion of fibrinolytic agents into the mesenteric-portal sys-
sion and in prehepatic block. J Cardiovasc Surg 1971;12(2): 147-1 51
tern has been described. This approach allowed direct guide- 6. Uflacker A, Alves M, Cantisani GG, Souza HP, Wagner J, Mordes LF.
wire recanalization of the occluded segment, instillation of Treatment of portal vein obstruction by percutaneous transhepatic angie-
high concentrations of urokinase directly into the thrombus, piasty. Gastroenterology 1985;88: 176-180
7. Okuda K, Kimura K, Takayasu K. Percutaneous transhepatic portography
and mechanical clearance of residual thrombus with an occlu-
and sclerotherapy. Scm Liver Dis 1982;2(1): 57-66
sion balloon, all of which were judged likely to minimize 8. McNamara TO, Fisher JR. Thrombolysis of peripheral arterial and graft
procedure time and thus reduce the risks of systemic fibri- occlusions: improved results using high-dose urokinase. AIR
nolysis. We thought that the high concentration of infused 1985;1 44: 769-775
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Tu of The OrbitDocument12 pagesTu of The OrbitChavdarNo ratings yet
- Simultaneous Giant Cavity Pulmonary Lesion and Pneumothorax Following COVID-19 PneumoniaDocument3 pagesSimultaneous Giant Cavity Pulmonary Lesion and Pneumothorax Following COVID-19 PneumoniaChavdarNo ratings yet
- CT Chest ScoringDocument10 pagesCT Chest ScoringChavdarNo ratings yet
- Maximum CT ScoreDocument11 pagesMaximum CT ScoreChavdarNo ratings yet
- Study To Assess Aetiology, Clinical and Imaging Characteristics of Post Covid 19 Pulmonary CavitationDocument5 pagesStudy To Assess Aetiology, Clinical and Imaging Characteristics of Post Covid 19 Pulmonary CavitationChavdarNo ratings yet
- Pulmonary Cavitation An Under-RecognizedDocument8 pagesPulmonary Cavitation An Under-RecognizedChavdarNo ratings yet
- Lung Cavitation As A Consequence ofDocument6 pagesLung Cavitation As A Consequence ofChavdarNo ratings yet
- Orbital Peripheral Nerve SheathDocument15 pagesOrbital Peripheral Nerve SheathChavdarNo ratings yet
- 1 s2.0 S2211568414002538 MainDocument11 pages1 s2.0 S2211568414002538 MainChavdarNo ratings yet
- Pulmonary Cavitations As An Atypical CT Finding in COVID-19 PatientsDocument2 pagesPulmonary Cavitations As An Atypical CT Finding in COVID-19 PatientsChavdarNo ratings yet
- COVID 19 Pneumonia Imaging Follow Up: When and How? A Proposition From ESTI and ESRDocument11 pagesCOVID 19 Pneumonia Imaging Follow Up: When and How? A Proposition From ESTI and ESRChavdarNo ratings yet
- Severe Post-Tonsillectomy Haemorrhage TreatedDocument3 pagesSevere Post-Tonsillectomy Haemorrhage TreatedChavdarNo ratings yet
- Lung Cavitation Due To COVID-19 PneumoniaDocument2 pagesLung Cavitation Due To COVID-19 PneumoniaChavdarNo ratings yet
- One-Year Follow-Up of Chest CT Findings inDocument11 pagesOne-Year Follow-Up of Chest CT Findings inChavdarNo ratings yet
- Annals of Clinical Medicine and Research: Pulmonary Cavitation Post-COVID-19 Pneumonia: A CaseDocument3 pagesAnnals of Clinical Medicine and Research: Pulmonary Cavitation Post-COVID-19 Pneumonia: A CaseChavdarNo ratings yet
- Radiologic Aspects of COVID-19 Pneumonia Outcomes and Thoracic ComplicationsDocument15 pagesRadiologic Aspects of COVID-19 Pneumonia Outcomes and Thoracic ComplicationsChavdarNo ratings yet
- Clavicle and Sternoclavicular JointDocument14 pagesClavicle and Sternoclavicular JointChavdarNo ratings yet
- Radiological Management and Follow-Up ofDocument12 pagesRadiological Management and Follow-Up ofChavdarNo ratings yet
- Ann Clin Transl Neurol - 2019 - Campbell - Hearing Impairment After Subarachnoid HemorrhageDocument11 pagesAnn Clin Transl Neurol - 2019 - Campbell - Hearing Impairment After Subarachnoid HemorrhageChavdarNo ratings yet
- FMRI After SAHDocument13 pagesFMRI After SAHChavdarNo ratings yet
- Clinical Significance of Azygos VeinDocument6 pagesClinical Significance of Azygos VeinChavdarNo ratings yet
- CT Evaluation of Congenital and AcquiredDocument14 pagesCT Evaluation of Congenital and AcquiredChavdarNo ratings yet
- Gas in The SternoclavicularJoints ofDocument3 pagesGas in The SternoclavicularJoints ofChavdarNo ratings yet
- Imaging of Palatal LumpsDocument11 pagesImaging of Palatal LumpsChavdarNo ratings yet
- Complications of COVID-19 in The Maxillo-Facial Region Clinical Case and Review of The LiteratureDocument6 pagesComplications of COVID-19 in The Maxillo-Facial Region Clinical Case and Review of The LiteratureChavdarNo ratings yet
- Hard Palate CovidDocument7 pagesHard Palate CovidChavdarNo ratings yet
- Endovasc Jug BulbDocument7 pagesEndovasc Jug BulbChavdarNo ratings yet
- Focus: Jugular Bulb and Skull Base Pathologies: Proposal For ADocument8 pagesFocus: Jugular Bulb and Skull Base Pathologies: Proposal For AZeptalanNo ratings yet
- Dehiscent High-Riding Jugular Bulb Presenting AsDocument3 pagesDehiscent High-Riding Jugular Bulb Presenting AsChavdarNo ratings yet
- Urgent Carotid Endarterectomy in A COVID-19 PatientDocument8 pagesUrgent Carotid Endarterectomy in A COVID-19 PatientChavdarNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Camptodactyly: Amalia Irsha Adhari (1506668510) Eldesta Nisa Nabila (1406642233)Document38 pagesCamptodactyly: Amalia Irsha Adhari (1506668510) Eldesta Nisa Nabila (1406642233)Amalia IrshaNo ratings yet
- Actea SpicataDocument4 pagesActea SpicataRaveendra MungaraNo ratings yet
- PNSS Drug StudyDocument2 pagesPNSS Drug Studyrain peregrinoNo ratings yet
- Fisa de Disciplina - ENG - Reumatologie - 2019 - 2020Document4 pagesFisa de Disciplina - ENG - Reumatologie - 2019 - 2020flo108No ratings yet
- Triads in Surgery ListDocument2 pagesTriads in Surgery ListTalha AnwarNo ratings yet
- Group 1 Parkinsons Pre TestDocument4 pagesGroup 1 Parkinsons Pre TestAyman NabilNo ratings yet
- ECMO For COVID 19 Updated 2021 Guidelines From.98326Document42 pagesECMO For COVID 19 Updated 2021 Guidelines From.98326risanataliasiburianNo ratings yet
- Post-Op OliguriaDocument13 pagesPost-Op OliguriaNigel SparksNo ratings yet
- Obg MCQSDocument11 pagesObg MCQSShriyansh ChaharNo ratings yet
- Safety in Sports: Made By: Shrreya Swaarnim Class: XD Roll No.: 40Document5 pagesSafety in Sports: Made By: Shrreya Swaarnim Class: XD Roll No.: 40Shrreya SwaarnimNo ratings yet
- Tle 10Document49 pagesTle 10peepee poopooNo ratings yet
- NitrofurantoinDocument3 pagesNitrofurantoinapi-3797941No ratings yet
- Sept 4, 2015Document8 pagesSept 4, 2015Deity CelleNo ratings yet
- 2-Physiotherapy For FracturesDocument17 pages2-Physiotherapy For FracturesJuanitoCabatañaLimIIINo ratings yet
- Butamirate CitrateDocument2 pagesButamirate CitratenisircNo ratings yet
- Sti Villains Project InstructionsDocument2 pagesSti Villains Project Instructionsapi-544556482No ratings yet
- Perioral DermatitisDocument6 pagesPerioral DermatitisYeni OktaviaNo ratings yet
- 3 MBBS Part I Routine (Theory) Department of Pediatrics Total: 20 Duration: 1hrDocument12 pages3 MBBS Part I Routine (Theory) Department of Pediatrics Total: 20 Duration: 1hrGaurav BatniNo ratings yet
- Nursing Care Plan for Postpartum PainDocument2 pagesNursing Care Plan for Postpartum PainJoseph Nawen Sindiong100% (1)
- Nursing Care Plan for Hiatal Hernia ReliefDocument3 pagesNursing Care Plan for Hiatal Hernia ReliefLalaine Nadulpit100% (2)
- Psychiatrics McqsDocument20 pagesPsychiatrics McqsHirwaNo ratings yet
- Globemed FormDocument4 pagesGlobemed Formangeloriondo1217No ratings yet
- Bernabe Ncm109 LabDocument4 pagesBernabe Ncm109 LabKarl LintanNo ratings yet
- Breast - Calcifications Differential Diagnosis: Anatomy Diagnostic ApproachDocument22 pagesBreast - Calcifications Differential Diagnosis: Anatomy Diagnostic ApproachDokdem AjaNo ratings yet
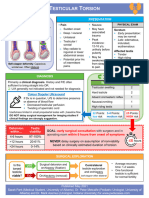
- Testicular Torsion, Peds Cases NotesDocument1 pageTesticular Torsion, Peds Cases NotesdzalhcNo ratings yet
- 17 Protective Measures OKDocument69 pages17 Protective Measures OKMary Rose LatorreNo ratings yet
- Mosbys Child Health Nursing 1Document62 pagesMosbys Child Health Nursing 1Darren VargasNo ratings yet
- Zollinger-Ellison Syndrome (Gastrinoma)Document15 pagesZollinger-Ellison Syndrome (Gastrinoma)Huy QuangNo ratings yet
- Grave's Ophthalmopathy: Susy Fatmariyanti Delfitri Lutfi, Hendrian D. SoebagjoDocument12 pagesGrave's Ophthalmopathy: Susy Fatmariyanti Delfitri Lutfi, Hendrian D. SoebagjoriskhapangestikaNo ratings yet
- Knee PainDocument2 pagesKnee PainKKNo ratings yet