Professional Documents
Culture Documents
Manejo Anestésico de RN Com Hernia Diafragmática Direita
Uploaded by
FhomensCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Manejo Anestésico de RN Com Hernia Diafragmática Direita
Uploaded by
FhomensCopyright:
Available Formats
[Downloaded free from http://www.saudija.org on Tuesday, April 17, 2018, IP: 177.200.181.
146]
Letters to Editor
Page | 227
Fiberoptic endotracheal intubation through
a supraglottic conduit using an exchange catheter
Sir, Therefore, I believe that, intubation using a fiberoptic scope
and supraglottic device with the aid of exchange catheter is
I read with interest the original article in issue 1 a reliable, safe, and easy to teach method which should not
volume 9 entitled (a comparison of fiberoptical guided be replaced by a similar method which is not associated with
tracheal intubation via laryngeal mask and laryngeal tube). the use of an exchange catheter without strong evidence.
The authors have used laryngeal mask airway (LMA) or Ghazi Aldehayat
laryngeal tube as a conduit for intubating the trachea by Department of Anesthesia, King Hussein Medical Center,
5 mm internal diameter tube without an exchange catheter. Amman, Jordan
I have the following comments on their respected work: Address for correspondence:
Ghazi Aldehayat,
King Hussein Medical Center, P.O. Box 201, Tela Al Ali,
I use and supervise my trainee using a fiberoptic scope Amman 11953, Jordan.
and Aintree catheter as an exchange catheter through a E-mail: aldehayat@yahoo.co.uk
supraglottic airway (usually classical LMA) for difficult
intubation management, and I find this method is more REFERENCES
useful and practical than the method described by the
authors in this paper for the following reasons: 1. Berkow LC, Schwartz JM, Kan K, Corridore M, Heitmiller ES.
Use of the Laryngeal Mask Airway-Aintree Intubating
Catheter-fiberoptic bronchoscope technique for difficult
The endotracheal intubation using fibreoptic scope, intubation. J Clin Anesth 2011;23:534-9.
Aintree catheter and LMA technique is safe and efficient 2. Atherton DP, O’Sullivan E, Lowe D, Charters P. A ventilation-
for patients who are difficult to intubate after induction exchange bougie for fibreoptic intubations with the laryngeal
mask airway. Anesthesia 1996;51:1123-6.
of anesthesia.[1] Furthermore, using Aintree catheter 3. Asai T, Latto IP, Vaughan RS. The distance between the
(or equivalent exchange catheter) as a conduit is a quick grille of the laryngeal mask airway and the vocal cords. Is
procedure with no extra experience is needed.[2] In addition, conventional intubation through the laryngeal mask safe?
Anesthesia 1993;48:667-9.
using endotracheal tube without exchange catheter is
usually difficult and prone to dislodgment because of the
Access this article online
length of endotracheal tube, which is usually not long
Quick Response Code:
enough to pass through the LMA smoothly and needs more Website:
manipulation with extra device like a pusher.[3] Moreover, www.saudija.org
the authors have used an endotracheal tube with an internal
diameter of 5 mm to facilitate the insertion, however, an DOI:
endotracheal tube with this diameter is not suitable for adult 10.4103/1658-354X.152899
patient and may cause several adverse effects.
Right sided congenital diaphragmatic hernia: A rare
neonatal emergency
Sir, live births. Right sided lesions are rare (10-15%) compared
with left sided (85%) as liver plugs the opening. Right
Congenital diaphragmatic hernia (CDH) occurs in 1 in 5000 congenital diaphragmatic hernia carries disproportionately
Saudi Journal of Anesthesia Vol. 9, Issue 2, April-June 2015
[Downloaded free from http://www.saudija.org on Tuesday, April 17, 2018, IP: 177.200.181.146]
Letters to Editor
Page | 228
high mortality and morbidity. Presence of liver herniation worsens the right to left shunt. A right subcostal
is a predictive of poor outcome.[1] It results in caval incision was made. Liver and bowel loops were reduced
compression, reduced preload and impaired cardiac [Figure 2]. The defect in right hemidiaphragm was
output.[2] closed. Child remained stable throughout the surgery.
Duration of surgery was 2 h. Intraoperative blood
A 4-day-old baby weighing 2.3 kg born by vaginal and fluid loss were replaced with Isolyte P. Child was
delivery at 36 weeks. He was diagnosed antenatally as electively ventilated postoperatively. IV morphine
a case of CDH. In view of respiratory distress he was infusion was started for sedation. Muscle relaxants were
intubated. Ventilation was instituted by keeping peak avoided, and spontaneous respiration was encouraged.
inspiratory pressure (PIP) of 20 cm H2O, FiO2 of 0.6 Child was extubated on POD 5, but could not tolerate
and respiratory rate of 60/min. Circulatory support extubation and was reintubated on the same day. On
was started in the form of dopamine infusion and POD 8 again trial for extubation was given which he
intravenous fluid. His echo revealed moderate pulmonary tolerated well.
hypertension. Chest X-ray showed multiple intestinal
loops with liver herniation in right sided hemithorax The goal of preoperative stabilization includes blood
and severe mediastinal shift in the left side [Figure 1]. pressure normal for gestational age, preductal SpO2 of
His ABG revealed pH-7.25, PCO2-44 mmHg, PO2-88 85-95%, lactate <3 mmol/L, urine output >2 ml/kg.[3]
mmHg HCO3-18 mEq/L and lactates-1.5 ummol/L. His This was achieved in our case. Ventilation strategy
preductual and postductal SpO2 differed by 5%. Hb was first described by Wung et al. was used in this case.[4]
15 g% and the rest of the investigations were normal. It aims at achieving adequate tissue oxygenation with
After 3 days of stabilization child was posted for surgical minimal barotrauma. It consists of limiting PIP <25 cm
repair of the hernia. H2O, permissive hypercapnia (PaCO2 between 45 and
60 mmHg). This strategy has shown to increase in
Inside operation theater routine monitors survival and decreased use in extracorporeal membrane
(electrocardiogram, noninvasive blood pressure, oxygenation. Continuous nasogastric suctioning should
SpO 2, EtCO 2, temperature) were attached. Neonatal be done to prevent bowel distension and further lung
resuscitation trolley was kept ready. Baseline parameters compression.
of heart rate 144/min and BP-66/40 mmHg were
noted. His preductal SpO 2 was 95% and posductal Until date, there are no uniform guidelines for the
saturation was 90%. Continuous nasogastric suctioning management of CDH. Many centers lack advanced
was done. Intravenous (IV) fentanyl 5 ug and IV neonatal care facilities affecting the prognosis. However,
atracurium was given. Pressure controlled ventilation still conventional technique have shown good outcome.[5]
was started with PIP of 20 cm H2O, respiratory rate of
50/min with FiO 2 of 0.7. Anesthesia was maintained Leena Harshad Parate,
with oxygen, air and sevoflurane. The anaesthetic goal Chamanahalli Rajappa Geetha, Saurabh Vig
was to avoid hypoxia, hypotension and hypothermia, Department of Anesthesia, M.S. Ramaiah Medical Collage,
which increases pulmonary vascular resistance and Bengaluru, Karnataka, India
Figure 2: Right congenital diaphragmatic hernia with reduced contents
Figure 1: Chest X-ray showing intestinal loops and liver herniation (liver and intestine)
Vol. 9, Issue 2, April-June 2015 Saudi Journal of Anesthesia
[Downloaded free from http://www.saudija.org on Tuesday, April 17, 2018, IP: 177.200.181.146]
Letters to Editor
Page | 229
Address for correspondence: 2010;98:354-64.
Dr. Leena Harshad Parate, 4. Wung JT, Sahni R, Moffitt ST, Lipsitz E, Stolar CJ.
Department of Anaesthesia, M.S. Ramaiah Medical Collage, Congenital diaphragmatic hernia: Survival treated with very
Bengaluru, Karnataka, India. delayed surgery, spontaneous respiration, and no chest tube.
E-mail: dr_leenag@yahoo.co.in J Pediatr Surg 1995;30:406-9.
5. Kaparti L, Padmaja R. Anaesthetic management of a neonate
with right sided congenital diaphragmatic hernia. J Clin Diagn
REFERENCES Res 2013;7:3002-3.
1. Bösenberg AT, Brown RA. Management of congenital
Access this article online
diaphragmatic hernia. Curr Opin Anaesthesiol 2008;21:323-31.
2. Zankl A, Osterheld MC, Vial Y, Beurret N, Meuli R, Quick Response Code:
Website:
Meagher-Villemure K, et al. Right-sided diaphragmatic
eventration: A rare cause of non-immune hydrops fetalis. www.saudija.org
Neonatology 2007;92:14-8.
3. Reiss I, Schaible T, van den Hout L, Capolupo I, Allegaert K,
DOI:
van Heijst A, et al. Standardized postnatal management of
infants with congenital diaphragmatic hernia in Europe: 10.4103/1658-354X.152900
The CDH EURO Consortium consensus. Neonatology
Low oxygen saturation: Really a hypoxia?
Sir, Pulse oximeter system consists of a peripheral probe together
with a microprocessor unit displaying a plethysmographic
A 50-year-old male patient with severe mitral stenosis waveform, the SpO2 and the pulse rate. The probe is placed
was scheduled for mitral valve replacement. Before on the fingertip, earlobe or nose. Probe has two LEDs
anesthesia induction, pulse oximetry probe was applied emitting red spectrum (660 nm) and the infrared spectrum
on left index finger and right radial artery was cannulated (940 nm). Photodetector on the other side of the probe
for blood pressure monitoring. Patient’s saturation was senses the light passed through the tissue. Oxygenation of
99% on pulse oximetry at room air. Surgery was done hemoglobin influences the amount of light absorption at each
after going on cardiopulmonary bypass (CPB). During frequency.[1] Pulse oximeter calculates the ratio of pulsatile
CPB, saturation was not displayed on pulse oximetry due to nonpulsatile absorbance and derive the SpO2. Adequate
to nonpulsatile perfusion flow. Saturation monitoring arterial pulsations are essential to distinguish the light
was done by in line arterial blood gas analysis, which was absorbed by arterial blood from that absorbed by venous
consistently above 95%. As the weaning from bypass blood. Inaccurate reading may be displayed in the presence of
was started, pulsatile arterial waveform appeared with poor peripheral pulsations, low cardiac output, hypovolemia,
pressure of 153/50 mmHg. However, pulse oximetry peripheral vascular disease, improper positioning,
showed saturation of 65% with good plethysmographic hypotension, hypothermia, CPB, low cardiac output.[1]
waveform correlating with heart rate [Figure 1]. Another
pulse oximetry probe was attached to ear lobule, which
showed oxygen saturation (SpO2) of 99%. Arterial blood
gas analysis revealed saturation of 98.9% with PaO2
of 178 mmHg on FiO2 of 0.5. Pulse oximetry probe
on the finger was examined, it was not misplaced, but
dusky discoloration was observed on the left hand below
forearm probably because of prolonged compression
by leaning over by surgeon while operating. As the
compressive effect was removed, SpO2 on the same
finger probe showed saturation of 98% in a short period Figure 1: Monitor display showing low saturation with good
of time. plethysmographic waveform
Saudi Journal of Anesthesia Vol. 9, Issue 2, April-June 2015
You might also like
- Toccata and Fugue in D Minor - GuitarsDocument12 pagesToccata and Fugue in D Minor - GuitarsFhomensNo ratings yet
- 0995 02 AllemandeDocument2 pages0995 02 AllemandeFhomensNo ratings yet
- Symphony Number 2 Second Movement D Major Score and PartsDocument15 pagesSymphony Number 2 Second Movement D Major Score and PartsFhomensNo ratings yet
- (Free Scores - Com) - Joplin Scott Entertainer 18457Document6 pages(Free Scores - Com) - Joplin Scott Entertainer 18457FhomensNo ratings yet
- CH Trio Violin PDFDocument7 pagesCH Trio Violin PDFFhomensNo ratings yet
- Robert de Visee': Sarabande Transcription Arto Wikla 1990 The Bass '7' Is in High F Sharp, It Can Be Replaced by B On 7th CourseDocument1 pageRobert de Visee': Sarabande Transcription Arto Wikla 1990 The Bass '7' Is in High F Sharp, It Can Be Replaced by B On 7th CourseFhomensNo ratings yet
- Mouton Charles Prague Ms II KK 80Document148 pagesMouton Charles Prague Ms II KK 80Fhomens100% (2)
- Villa-Lobos Canto Do Serto Arr. For Guitar Quartet by Charles EagerDocument8 pagesVilla-Lobos Canto Do Serto Arr. For Guitar Quartet by Charles EagerFhomensNo ratings yet
- JS Bach - Little Fugue in G Minor For Guitar EnsembleDocument11 pagesJS Bach - Little Fugue in G Minor For Guitar EnsembleFhomensNo ratings yet
- Menuett 2 Anna M ArchDocument1 pageMenuett 2 Anna M ArchFhomensNo ratings yet
- Sonata Prima: Dario CastelloDocument2 pagesSonata Prima: Dario CastelloFhomensNo ratings yet
- 4822797-Rujero y Paradetas From The Spanish Suite For Viola GuitarDocument19 pages4822797-Rujero y Paradetas From The Spanish Suite For Viola GuitarFhomensNo ratings yet
- Mouton ForewordDocument2 pagesMouton ForewordFhomensNo ratings yet
- Ricercars Over Genevan Psalm Tunes: For Renaissance LuteDocument8 pagesRicercars Over Genevan Psalm Tunes: For Renaissance LuteFhomensNo ratings yet
- Prelude PDFDocument1 pagePrelude PDFFhomensNo ratings yet
- J.S. Bach's Sarabande in B flat majorDocument1 pageJ.S. Bach's Sarabande in B flat majorFhomensNo ratings yet
- Anaesthetic Management of A Neonate With Right Sided Congenital Diaphragmatic HerniaDocument2 pagesAnaesthetic Management of A Neonate With Right Sided Congenital Diaphragmatic HerniaFhomensNo ratings yet
- 4822797-Rujero y Paradetas From The Spanish Suite For Viola Guitar PDFDocument1 page4822797-Rujero y Paradetas From The Spanish Suite For Viola Guitar PDFFhomensNo ratings yet
- IMSLP299865-PMLP485606-Farnaby, Giles - Pearce Did Dance With Petronella PDFDocument3 pagesIMSLP299865-PMLP485606-Farnaby, Giles - Pearce Did Dance With Petronella PDFFhomensNo ratings yet
- Safety and Efficacy of Postoperative Epidural Analgesia PDFDocument15 pagesSafety and Efficacy of Postoperative Epidural Analgesia PDFFhomensNo ratings yet
- Cui - Farniente For Piano Trio From A Argenteau Op40 No2 Cello PDFDocument1 pageCui - Farniente For Piano Trio From A Argenteau Op40 No2 Cello PDFFhomensNo ratings yet
- IMSLP299763-PMLP485437-Farnaby, Giles - Among The DaffadilliesDocument4 pagesIMSLP299763-PMLP485437-Farnaby, Giles - Among The DaffadilliesFhomensNo ratings yet
- German Headstart - Module X PDFDocument15 pagesGerman Headstart - Module X PDFFhomensNo ratings yet
- Surgical Management of The Retained Epidural Catheter Fragment Complicated by Postoperative PhlegmonDocument3 pagesSurgical Management of The Retained Epidural Catheter Fragment Complicated by Postoperative PhlegmonFhomensNo ratings yet
- Anesthetic Management of A Case of Congenital Diaphragmatic Hernia Delayed DiagnosisDocument3 pagesAnesthetic Management of A Case of Congenital Diaphragmatic Hernia Delayed DiagnosisFhomensNo ratings yet
- Manejo Anestésico de RN Com Hernia Diafragmática DireitaDocument3 pagesManejo Anestésico de RN Com Hernia Diafragmática DireitaFhomensNo ratings yet
- Anaesthetic Management of A Neonate With Right Sided Congenital Diaphragmatic HerniaDocument2 pagesAnaesthetic Management of A Neonate With Right Sided Congenital Diaphragmatic HerniaFhomensNo ratings yet
- Anesthetic Management of A Case of Congenital Diaphragmatic Hernia Delayed DiagnosisDocument3 pagesAnesthetic Management of A Case of Congenital Diaphragmatic Hernia Delayed DiagnosisFhomensNo ratings yet
- Abdominal Compartiment SyndromeDocument10 pagesAbdominal Compartiment SyndromeFhomensNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Torture-Definition Quiroga JaransonDocument6 pagesTorture-Definition Quiroga JaransonAlfred KassarNo ratings yet
- Self Information Form Selkirk Mental Health CentreDocument11 pagesSelf Information Form Selkirk Mental Health Centredenden007No ratings yet
- Progressive Muscle RelaxationDocument16 pagesProgressive Muscle RelaxationFaith DawnNo ratings yet
- Enoxaparin (Lovenox)Document1 pageEnoxaparin (Lovenox)ENo ratings yet
- Ws Viii Dyspepsia - Dr. Ignatia Sinta Murti, SP - Pd-KgehDocument79 pagesWs Viii Dyspepsia - Dr. Ignatia Sinta Murti, SP - Pd-KgehSriHandaryatiNo ratings yet
- Long-Term Evaluation of Periodontal TherapyDocument16 pagesLong-Term Evaluation of Periodontal TherapyRanuch TakNo ratings yet
- Compilation of Notes If Marijuana Will Be Legalized in The PhilippinesDocument42 pagesCompilation of Notes If Marijuana Will Be Legalized in The PhilippinesLajilaNo ratings yet
- Roxonin LeafletDocument2 pagesRoxonin LeafletmohammedfirasatNo ratings yet
- Negative PracticeDocument9 pagesNegative PracticeEzequiel OcampoNo ratings yet
- Ce Booklet Fall 14Document28 pagesCe Booklet Fall 14api-279863771No ratings yet
- RAD: Reactive Attachment Disorder ResourcesDocument8 pagesRAD: Reactive Attachment Disorder ResourcesveronicaNo ratings yet
- Aigen 2005 - Being in Music Foundations of NRMT - Livro CompletoDocument79 pagesAigen 2005 - Being in Music Foundations of NRMT - Livro CompletoJuan CruzNo ratings yet
- Magneto Therapy NotesDocument5 pagesMagneto Therapy NotesMadan Kumar100% (2)
- Jurnal Enzim AmilaseDocument6 pagesJurnal Enzim AmilaseTriRatnaFauziahNo ratings yet
- Leczenie Endodontyczne Czy Implantologiczne? Endodontic Treatment or Dental Implant Treatment?Document5 pagesLeczenie Endodontyczne Czy Implantologiczne? Endodontic Treatment or Dental Implant Treatment?Izabella Tomera-NiekowalNo ratings yet
- Proc, SWB PDFDocument152 pagesProc, SWB PDFNovi AriantiNo ratings yet
- Maura Sills: Karuna InstituteDocument1 pageMaura Sills: Karuna Instituteapi-266696024No ratings yet
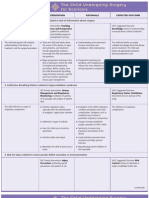
- NURSING CARE PLAN The Child Undergoing Surgery For ScoliosisDocument3 pagesNURSING CARE PLAN The Child Undergoing Surgery For ScoliosisscrewdriverNo ratings yet
- Vestibular Reha PDFDocument657 pagesVestibular Reha PDFRetnoNo ratings yet
- Revised PADS As of Nov 9 2018Document79 pagesRevised PADS As of Nov 9 2018Angela Buid InongNo ratings yet
- Maguire - Barden - FINAL AFFIDAVIT PDF (Nuance) W-HighlightsDocument34 pagesMaguire - Barden - FINAL AFFIDAVIT PDF (Nuance) W-HighlightsSyndicated NewsNo ratings yet
- Relationship Between The Five Element Points and Some Major Physiological SystemsDocument4 pagesRelationship Between The Five Element Points and Some Major Physiological SystemsNilton Benfatti100% (1)
- Dosis Oseltamivir CDCDocument3 pagesDosis Oseltamivir CDCivonne marinNo ratings yet
- TopicalpaincontrolmedicationDocument47 pagesTopicalpaincontrolmedicationJ C Torres FormalabNo ratings yet
- Alternative Modalities of Care: By: Firoz Qureshi Dept. Psychiatric NursingDocument68 pagesAlternative Modalities of Care: By: Firoz Qureshi Dept. Psychiatric NursingsanthiyasandyNo ratings yet
- Purac BF P - 41Document2 pagesPurac BF P - 41FiraFfirehsNo ratings yet
- Dailymed - Nlm.nih - Gov METRONIDAZOLEDocument16 pagesDailymed - Nlm.nih - Gov METRONIDAZOLELip StickNo ratings yet
- Web BrochureDocument12 pagesWeb BrochureZoe Brigden-SmallwoodNo ratings yet
- Licensing Requirements for Psychiatric Care FacilitiesDocument3 pagesLicensing Requirements for Psychiatric Care FacilitiesAgnes Cheverloo CastilloNo ratings yet
- Self AttuneDocument6 pagesSelf AttuneBodibodi100% (2)