Professional Documents
Culture Documents
An Analytical Study of Childhood Malnutrition of Boys From Urban Schools of Haryana
Uploaded by
Anonymous CwJeBCAXpOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
An Analytical Study of Childhood Malnutrition of Boys From Urban Schools of Haryana
Uploaded by
Anonymous CwJeBCAXpCopyright:
Available Formats
Scholarly Research Journal for Humanity Science & English Language,
Online ISSN 2348-3083, SJ IMPACT FACTOR 2016 = 4.44, www.srjis.com
UGC Approved Sr. No.48612, FEB-MAR 2018, VOL- 6/26
https://doi.org/10.21922/srjhsel.v6i26.11684
AN ANALYTICAL STUDY OF CHILDHOOD MALNUTRITION OF BOYS FROM
URBAN SCHOOLS OF HARYANA
Ajay Kumar1 & Sanjay Trama2
1
Assistant Professor, S.A. Jain College, Ambala city
2
Assistant professor, S.A. Jain College, Ambala city
Abstract
The purpose of the study was to explore prevalence of malnutrition in school going boys of urban
school of Haryana the study was done on 70 school boys of 10-12 years from urban areas of Haryana
and the study shows that 51.42% boys are under nourished and fall in underweight category where as
25.71% of total boys deal with the problem of malnutrition. The sample subject had been delimited to
school boys of 10-12 year from urban areas. Digital weight machine and stadiometer were used
examine the BMI of the subjects. Very low percentage of boys was found overweight and obese from
urban school. Perhaps high demand of knowledge regarding nutritional values and health education
is required in the society. Health services and health supervision must be given timely to children to
avoid problems like malnutrition.
Keywords- BMI, WHO, Obesity, malnutrition
R4Z Scholarly Research Journal's is licensed Based on a work at www.srjis.com
Introduction
Malnutrition- It is a condition that results eating a diet in which nutrients are either not
enough or are too much such that the diet causes health problems. It may involve calories,
protein, carbohydrates, vitamins or minerals. Not enough nutrients are called under nutrition
or undernourishment while too much is called over nutrition. Malnutrition is often used to
specifically refer to under nutrition where an individual is not getting enough calories, protein
or micronutrients. Extreme undernourishment, known as starvation, may have symptoms that
include a short height, thin body, very poor energy levels. There are two main types of under
nutrition; protein energy malnutrition and dietary deficiencies. Protein energy malnutrition
has two severe forms: marasmus (a lack of protein and calories) and kwashiorkor (a lack of
just protein).
Protein- energy malnutrition (PEM) under nutrition is sometimes used as a synonym of
protein energy malnutrition. Kwashiorkor: It is mainly caused by inadequate protein intake
resulting in a low concentration of amino acids. It is identified by swelling of the extremities
and belly, which is deceiving of actual nutritional status. Marasmus: It is mainly caused by an
Copyright © 2017, Scholarly Research Journal for Interdisciplinary Studies
Ajay Kumar & Sanjay Trama
7590
(Pg. 7589-7592)
inadequate intake of protein and energy. It can result from a sustained diet of inadequate
energy and protein and the metabolism adapts to prolong survival.
Malnutrition in children
Here understood as under nutrition is common globally and result in both and long term
eversible negative health outcomes in duding stunted growth which may also link cognitive
development deficits, underweight and wasting. The WHO estimates that malnutrition
accounts for 54% of child mortality worldwide. Another estimate also by WHO states that
childhood underweight is the cause for about 35% of all deaths of children under the age of
five years worldwide. The main causes are unsafe water, inadequate sanitation or insufficient
hygiene.
Method and methodology
The sampling was done by random selection which includes boys of 10 to 12 years of age
from urban schools of Haryana. Anthropometric measurements were taken to calculate BMI
of the subjects. Weight was measured in the upright position to the nearest 0.1 kg using
calibrated electronic balance. Height was measured without shoes to the nearest 0.1 cm using
calibrated stadiometer. The instruments required in the study are as follows:
1. A digital weighing machine.
2. Height measuring scale..
BMI classification – It is to assess how much an individual’s body weight departs from what
is normal or desirable for a person of his or her height. BMI = Weight (Kg.) / Height2 (m).
The WHO classification of BMI are valid when applied to adults, and do not predict health.
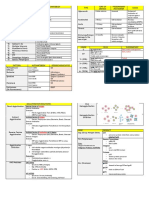
Category BMI range Kg/m2
Malnutrition < 16
Underweight 16 – 18.5
Normal 18.5 – 25
Overweight 25 – 30
Obese 30 – 40
Result and discussion
In the present study total 70 subjects were taken from urban school of Haryana in the age
group 10-12 years
Copyright © 2017, Scholarly Research Journal for Interdisciplinary Studies
Ajay Kumar & Sanjay Trama
7591
(Pg. 7589-7592)
Table no 1- Urban subjects were arranged according to WHO criteria based on BMI
value
Group BMI Urban n-70 %
starvation <16 18 25.71%
under nourished 16-18.5 18 25.71%
normal 18.5-25 30 42.85%
Overweight 25-30 4 5.71%
obese 30-40 0 0%
starvation under weight normal over weight obese
5.71 0
25.71
42.85
25.71
In urban students study 25.71% subjects fall in starvation category and 25.71% subjects fall
in under nourished. 42.85% subjects fall in normal category and 5.71% subjects are
overweight. Out of 70 subjects 51.42% are under nourished and starvation which is
significantly very high where as obese/over weight is significantly very low. 42.85% normal
category students show that children are aware about their health and health programmed are
helping students to maintain their nutritional status.
Conclusion
In the present study we found the prevalence of malnutrition is high in urban students as more
than 50% students are starvation and under nourished. The study also suggests that normal
weight rates remain high in urban students and overweight/obese rates remain low in urban
students. The study shows the risk of mental and physical growth this can be due to lack of
hygiene, unsafe water, and lack of nutrition diet and unawareness of health issues
(malnutrition) in urban students. In some cases total body fat % is much below the prescribed
limit. Social attention has to be given for their overall nutrition.
Reference:
Styne DM. Childhood and Adolescent Obesity. PCNA 2001; 48: 823-847.
Must A, PF Jacques, GE Dallal, CJ Bajema, WH Dietz. Long-term morbidity and mortality of
overweight adolescents. A follow-up of the Harvard Growth Study of 19 1922 to 1935. N Engl
J Med 1992; 327: 1350-1355.
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. Geneva,
World Health Organisation 2000 (WHO Technical Report Series, No.894).
Kissebah AH, Freedman DS, Peiris AN. Health risks of obesity. Med Clin North Am 1989; 73: 111-
38.
Copyright © 2017, Scholarly Research Journal for Interdisciplinary Studies
Ajay Kumar & Sanjay Trama
7592
(Pg. 7589-7592)
Baron RB. Obesity in chapter on nutrition, edited by Tierney Jr. LM, McPhee SJ, Papadakis MA,
Current Medical Diagnosis and Treatment 2003, 42nd Ed, New Delhi, Lange Medical
Books/McGraw–Hill, 2003; 1224-7.
Després JP, Lemieux I. Prud’homme D. Treatment of obesity: need to focus on high risk abdominally
obese patients. Br Med J 2001; 322: 716-20.
Keys A, Fidanza F, Karvonen MJ et al. Indices of relative weight and obesity. J Chronic Dis 1972;
25: 329-43.
Pouliot MC, Despre’s JP, Nadeau A et al. Visceral obesity in men. Associations with glucose
tolerance, plasma insulin and lipoprotein levels. Diabetes 1992; 41: 826-34.
Hakim AS. Medical complications of obesity, SB Gupta (ed), Medicine Update Associations of
Physicians of India, Mumbai, 2002; 12: 480-2.
Colditz GA, Willett WC, Stampfer MJ et al. Weight as a risk factor for clinical diabetes in women. Am
J Epidemiol 1990; 132: 501- 13.
Klesges RC, Coates TJ, Brown G. Parental influences on childrens’ eating behavior and relative
weight. J Appl Behav Anal 1986; 16: 371-378.
Robinson TN. Reducing children’s television viewing to prevent obesity. A randomized controlled
trial. JAMA 1999; 282; 1561- 1567.
Avula Laxmaiah, Balakrishna N, Kamasamudram V Mohanan N. Factors Affecting Prevalence of
Overweight Among 12- to 17- years-old Urban Adolescents in Hydrabad, India. Obesity
15:1384-1390 (2007).
Centers for Disease Control and Prevention: Overweight children and adolescents 6–19 years of age,
according to sex, age, race, and Hispanic origin: United States, selected years 1963–65
through1999–2000
Ogden CL, Flegal KM, Carroll MD, Johnson CL: Prevalence and trends in overweight among US
children and adolescents, 1999– 2000. JAMA 288:1728–1732, 2002.
Sung RYT, Tong PCY, Yu CW, Lau PWC, Mok GTF, Yam M-C, Lam PKW, Chan JCN: High
prevalence of insulin resistance and metabolic syndrome in overweight/obese preadolescent
Hong Kong Chinese children aged 9–12 years. Diabetes Care 26:250– 251, 2003.
Booth ML, Wake M, Armstrong T, Chey T, Hesketh K, Mathur S: The epidemiology of overweight and
obesity among Australian children and adolescents, 1995–97. Aust N Z J Public Health
25:162–169, 2001.
Booth ML, Chey T, Wake M, Norton K, Hesketh K, Dollman J, Robertson I: Change in the prevalence
of overweight and obesity among young Australians, 1969–1997. Am J Clin Nutr 77:29–36,
2003.
McCarthy HD, Ellis SM, Cole TJ: Central overweight and obesity in British youth aged 11 16 years:
cross sectional surveys of waist circumference. BMJ 326:624–627, 2003.
Steinberger J, Daniels SR: Obesity, insulin resistance, diabetes, and cardiovascular risk in children:
an American Heart Association scientific statement from the Atherosclerosis, Hypertension,
and Obesity in the Young Committee (Council on Cardiovascular Disease in the Young) and
the Diabetes Committee (Council on Nutrition, Physical Activity, and Metabolism).
Circulation 107:1448–1453, 2003.
Steinberger J, Moran A, Hong CP, Jacobs DR Jr, Sinaiko AR: Adiposity in childhood predicts obesity
and insulin resistance in young adulthood. J Pediatr 138:469–473, 2001.
Reddy KS, Prabhakaran D, Shah P, Shah D. Differences in body mass index and waist: hip ratios in
north Indian rural and urban population. Obes Rev 2002; 3: 197-202.
Chadha SL, Gopinath N, Shekhawar S. Urban rural
Copyright © 2017, Scholarly Research Journal for Interdisciplinary Studies
You might also like
- Homesh RaniDocument7 pagesHomesh RaniAnonymous CwJeBCAXpNo ratings yet
- The Need of Remote Voting Machine in Indian Voting SystemDocument7 pagesThe Need of Remote Voting Machine in Indian Voting SystemAnonymous CwJeBCAXpNo ratings yet
- 29.yuvraj SutarDocument4 pages29.yuvraj SutarAnonymous CwJeBCAXpNo ratings yet
- 25.suresh ChenuDocument9 pages25.suresh ChenuAnonymous CwJeBCAXpNo ratings yet
- The Use of English Language During PandemicDocument7 pagesThe Use of English Language During PandemicAnonymous CwJeBCAXpNo ratings yet
- A Study of Effect of Age and Gender On Stress of AdolescentsDocument5 pagesA Study of Effect of Age and Gender On Stress of AdolescentsAnonymous CwJeBCAXpNo ratings yet
- 4.Dr Gagandeep KaurDocument13 pages4.Dr Gagandeep KaurAnonymous CwJeBCAXpNo ratings yet
- 19.Dr Ibrahim Aliyu ShehuDocument29 pages19.Dr Ibrahim Aliyu ShehuAnonymous CwJeBCAXpNo ratings yet
- 13.nasir RasheedDocument9 pages13.nasir RasheedAnonymous CwJeBCAXpNo ratings yet
- Historical Development of Play Schools in IndiaDocument11 pagesHistorical Development of Play Schools in IndiaAnonymous CwJeBCAXpNo ratings yet
- Customers' Consciousness About Financial Cyber Frauds in Electronic Banking: An Indian Perspective With Special Reference To Mumbai CityDocument13 pagesCustomers' Consciousness About Financial Cyber Frauds in Electronic Banking: An Indian Perspective With Special Reference To Mumbai CityAnonymous CwJeBCAXpNo ratings yet
- Women Empowerment and Religion's Role in Gender Relations in KargilDocument10 pagesWomen Empowerment and Religion's Role in Gender Relations in KargilAnonymous CwJeBCAXpNo ratings yet
- 1.prof. Ajay Kumar AttriDocument8 pages1.prof. Ajay Kumar AttriAnonymous CwJeBCAXpNo ratings yet
- Technostress, Computer Self-Efficacy and Perceived Organizational Support Among Secondary School Teachers: Difference in Type of School, Gender and AgeDocument13 pagesTechnostress, Computer Self-Efficacy and Perceived Organizational Support Among Secondary School Teachers: Difference in Type of School, Gender and AgeAnonymous CwJeBCAXpNo ratings yet
- Effect of Life Skill Training On Mental Health Among B.ed. Interns in Relation To Their Impulsive BehaviourDocument9 pagesEffect of Life Skill Training On Mental Health Among B.ed. Interns in Relation To Their Impulsive BehaviourAnonymous CwJeBCAXpNo ratings yet
- Aggression Among Senior Secondary School Students in Relation To Their Residential BackgroundDocument8 pagesAggression Among Senior Secondary School Students in Relation To Their Residential BackgroundAnonymous CwJeBCAXpNo ratings yet
- 28 Shailaja KanwarDocument12 pages28 Shailaja KanwarAnonymous CwJeBCAXpNo ratings yet
- A Lookout at Traditional Games Played by Tribes in IndiaDocument4 pagesA Lookout at Traditional Games Played by Tribes in IndiaAnonymous CwJeBCAXpNo ratings yet
- 25 AshaDocument5 pages25 AshaAnonymous CwJeBCAXpNo ratings yet
- 26 Dr. Reni Francis Mr. Rajendra DeshmukhDocument5 pages26 Dr. Reni Francis Mr. Rajendra DeshmukhAnonymous CwJeBCAXpNo ratings yet
- 30 Trishala BhaskarDocument7 pages30 Trishala BhaskarAnonymous CwJeBCAXpNo ratings yet
- 31 Dr. Suman Kumari, Prof. Sudarshana Rana & Ms. Anita VermaDocument9 pages31 Dr. Suman Kumari, Prof. Sudarshana Rana & Ms. Anita VermaAnonymous CwJeBCAXpNo ratings yet
- 29 Balwinder SinghDocument8 pages29 Balwinder SinghAnonymous CwJeBCAXpNo ratings yet
- 24 Adv Raj KumarDocument5 pages24 Adv Raj KumarAnonymous CwJeBCAXpNo ratings yet
- 22 Pavithra.g ArticleDocument8 pages22 Pavithra.g ArticleAnonymous CwJeBCAXpNo ratings yet
- 23 JayalakshmiDocument9 pages23 JayalakshmiAnonymous CwJeBCAXpNo ratings yet
- 21 DR ReniDocument6 pages21 DR ReniAnonymous CwJeBCAXpNo ratings yet
- Payal BhatiDocument10 pagesPayal BhatiAnonymous CwJeBCAXpNo ratings yet
- Deepa AnwarDocument17 pagesDeepa AnwarAnonymous CwJeBCAXpNo ratings yet
- Suyambukani VDocument6 pagesSuyambukani VAnonymous CwJeBCAXpNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 5as Powerpoint PresentationDocument50 pages5as Powerpoint PresentationkahtrshNo ratings yet
- HPLC Method Development and Validation of Combined Dosage Form of Atenolol and Indapamide in TabletsDocument22 pagesHPLC Method Development and Validation of Combined Dosage Form of Atenolol and Indapamide in TabletsRam VijayNo ratings yet
- Diversity of Avenue PlantingDocument38 pagesDiversity of Avenue Plantingjoseph Lalremruata100% (1)
- Polycystic Ovary SyndromeDocument11 pagesPolycystic Ovary SyndromeABC11No ratings yet
- AUTOIMMUNE DISEASES AND ASSOCIATED AUTOANTIBODIESDocument8 pagesAUTOIMMUNE DISEASES AND ASSOCIATED AUTOANTIBODIESLynx EemanNo ratings yet
- Final Report KopinskiDocument11 pagesFinal Report Kopinskiapi-439568635No ratings yet
- Ocular Manifestations of HIV: A ReviewDocument33 pagesOcular Manifestations of HIV: A Reviewhenok birukNo ratings yet
- Chirurgie Pediatrica Engleza 125 Teste 2019 08.02.2019Document25 pagesChirurgie Pediatrica Engleza 125 Teste 2019 08.02.2019gm hashNo ratings yet
- Hand Hygiene GuideDocument151 pagesHand Hygiene GuideEmmanuel CuevasNo ratings yet
- Hypnotism MesmerismDocument32 pagesHypnotism MesmerismMuthu KumarNo ratings yet
- Guidelines For Preventive Activities in General PracticeDocument382 pagesGuidelines For Preventive Activities in General PracticeDr. Serin KuriakoseNo ratings yet
- Physical Assessment - General Survey GuideDocument2 pagesPhysical Assessment - General Survey GuideDanielle TorresNo ratings yet
- Bee Stings: The British Beekeepers AssociationDocument3 pagesBee Stings: The British Beekeepers AssociationantonioforteseNo ratings yet
- PESCI Recalls PDFDocument9 pagesPESCI Recalls PDFDanishNo ratings yet
- Neuro Degenerat yDocument33 pagesNeuro Degenerat yJoel Torres VillenaNo ratings yet
- Applied Part of Kulliyat With Reference To Venesection (Fasd) : A ReviewDocument4 pagesApplied Part of Kulliyat With Reference To Venesection (Fasd) : A ReviewDebby Adhila ShanahanNo ratings yet
- Hancock County Comprehensive Health AssessmentDocument169 pagesHancock County Comprehensive Health AssessmentGenna FreedNo ratings yet
- Chronic Kidney Disease Case PresDocument32 pagesChronic Kidney Disease Case Presnnaesor_1091No ratings yet
- Wellness Worksheet 010Document2 pagesWellness Worksheet 010Abiud UrbinaNo ratings yet
- Assessment Exam in Cc2and3Document7 pagesAssessment Exam in Cc2and3mika de guzmanNo ratings yet
- Typhoid Fever and Cure Well VersedDocument1 pageTyphoid Fever and Cure Well Versedscope 3901No ratings yet
- FitnessAssessment 2015 16 PDFDocument16 pagesFitnessAssessment 2015 16 PDFlaxave8817No ratings yet
- Assessment Questions (Assessment Criteria)Document2 pagesAssessment Questions (Assessment Criteria)sujanaNo ratings yet
- Bedah Anak Lanjut Pilihan GandaDocument1 pageBedah Anak Lanjut Pilihan GandaGilberto ChafrinaNo ratings yet
- Nursing Health History Format (Used For Client Care Plan)Document2 pagesNursing Health History Format (Used For Client Care Plan)Hamid Colangcag AmborNo ratings yet
- The Future of Health and Wellbeing in The WorkplaceDocument15 pagesThe Future of Health and Wellbeing in The WorkplaceSalim MuftahNo ratings yet
- Detoxification and Toxicology PDFDocument26 pagesDetoxification and Toxicology PDFMetcher Maa AkhiNo ratings yet
- Magnesium and Type 2 Diabetes: Mario Barbagallo, Ligia J DominguezDocument7 pagesMagnesium and Type 2 Diabetes: Mario Barbagallo, Ligia J DominguezbayuwinotoNo ratings yet
- Bacterial Keratitis PritiDocument58 pagesBacterial Keratitis Pritipriti08988% (8)