Professional Documents
Culture Documents
Nutrition 5
Uploaded by
Faith Dianasas Requina0 ratings0% found this document useful (0 votes)
6 views2 pagesnutrition notes for NLE
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentnutrition notes for NLE
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views2 pagesNutrition 5
Uploaded by
Faith Dianasas Requinanutrition notes for NLE
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 2
Provide bed rest • Kidneys: acute tubular necrosis
• Provide high-calorie diet • Hemorrhage, DIC
• Monitor for signs of GI bleeding • Pancreatic abscess
• Monitor mental status: lethargy, • Pancreatic pseudocysts
somnolence, personality changes • Pancreas insufficiency
• Limit visitors / isolation procedures if ASSESSMENT
infectious • Nausea
MEDICATIONS: • Severe abdominal pain around umbilicus
• Antiemetics • Abdominal rigidity
• Antibiotics ( to decrease ammonia • Signs of shock
production by intestinal bacteria) • Dark urine, clay-colored stools if due to
• Vitamin K bile duct obstruction (stones)
CLIENT EDUCATION LAB:
• HAV: Good hand washing practice • Elevate amylase, lipase
• HBV: Avoid unprotected sexual • If serum calcium low> poorer prognosis
intercourse Avoid sharing of needles ANALYSIS:
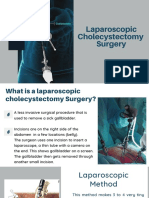
GALLBLADDER • Fluid and electrolyte balance?
cholelithiasis = presence of gallstones in the • Adequate nutrition?
gallbladder IMPLEMENTATION
CHOLELITHIASIS • Keep client NPO
• Usually asymptomatic (70%) • Assist with nasogastric tube
• May cause biliary colic (20%) • Monitor vital signs
• May cause cholecystitis (10%) • Monitor input/output
BILIARY COLIC • Assess for respiratory difficulties and base
• Steady, cramplike pain in epigastrium of lungs.
• Murphy’s sign (inspiratory arrest during CLIENT EDUCATION
palpation of liver margin) • Strict avoidance of alcohol
• Pain does not subside spontaneously MALDIGESTION
ANALYSIS Dysfunction of pancreas
• Dehydration due to nausea and vomiting? • Chronic pancreatitis
• Risk of acute pancreatitis if stone • Cystic fibrosis
obstructs duct Lack of specific enzymes
IMPLEMENTATION • Lactase deficiency
• No oral food during acute cholecystitis Lack of bile salts
DIAGNOSIS: • Biliary cirrhosis
• X-ray, ultrasound, scan to visualize stones • Resected terminal ileum
• ERCP to visualize ducts • Bacterial overgrowth
MEDICATIONS: MALABSORPTION
• Analgesics Dysfunction of small bowel
• Antibiotics • Short bowel syndrome
• Ursodiol: (resolves small cholesterol • Bacterial overgrowth
stones, but does not help in acute attack) • Celiac disease
POSTOPERATIVE: • Tropical sprue
• Monitor T-tube drainage (up to 500ml in Note: Diarrhea often leads to transients
first 24h is normal) lactase deficiency: Teach client to avoid milk
CLIENT EDUCATION: when having diarrhea of any cause.
• Reduce dietary fat and cholesterol intake DIARRHEA
PANCREATITIS SECRETORY
ACUTE PANCREATITIS • Large volume watery stools
Causes – Alcohol abuse, cholelithiasis • Persists with fasting
Features – Elevate lipase, amylase (cholera, dysentery)
Mortality rate – 10% OSMOTIC
CHRONIC PANCREATITIS • Bulky, greasy stools
Causes – Alcohol abuse, rarely due to • Improves with fasting
cholelithiasis (lactase deficiency, pancreatic insufficiency,
Features – pancreatic calcifications short bowel syndrome)
COMPLICATIONS OF ACUTE PANCREATIS INFLAMMATORY
• Peritoneum: fat necrosis • Frequent but small stools
• Lungs: respiratory distress syndrome • Blood and/or pus
(inflammatory bowel disease, irradiation,
shigella, amebiasis)
DYSMOTILITY
• Diarrhea alternating with constipation
(irritable bowel syndrome, diabetes
mellitus)
LOWER ABDOMINAL PAIN
Appendicitis
• Vague periumbilical pain, nausea
• Later localizes to lower right quadrant
• Perforation: high fever and leukocytosis
Diverticulitis
• Elderly patients
• Steady pain
• Localized to lower left quadrant
• Left sided appendicitis
Inflammatory bowel disease
• Chronic, cramping pain
• Diarrhea, blood and pus in stool
Intestinal obstruction
• Hyperactive bowel sounds
Intestinal infraction
• Absent bowel sounds
• Gross or occult blood in stool
APPENDICITIS
ASSESSMENT
• Nausea, anorexia
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Professional Guide To Signs and Symptoms 6th Edition PDFDocument822 pagesProfessional Guide To Signs and Symptoms 6th Edition PDF1102sn83% (6)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- PLE 2019 Surgery Questions and AnswersDocument30 pagesPLE 2019 Surgery Questions and Answersdickson78% (9)
- Essentials of Abdomino-Pelvic Sonography PDFDocument293 pagesEssentials of Abdomino-Pelvic Sonography PDFEliza Crăciun100% (4)
- Nursing Practice III: Total Laryngectomy CareDocument7 pagesNursing Practice III: Total Laryngectomy CareMichelle GambolNo ratings yet
- List of Simplified Medical VocabularyDocument72 pagesList of Simplified Medical VocabularyJinnaNo ratings yet
- 2018 Ultrasound A Core Review PDFDocument617 pages2018 Ultrasound A Core Review PDFsun sealNo ratings yet
- Wash 4Document6 pagesWash 4Faith Dianasas RequinaNo ratings yet
- Wash 4Document6 pagesWash 4Faith Dianasas RequinaNo ratings yet
- Hand Hygiene and HandwashingDocument8 pagesHand Hygiene and HandwashingFaith Dianasas RequinaNo ratings yet
- Wash 1Document6 pagesWash 1Faith Dianasas RequinaNo ratings yet
- Wash 2Document6 pagesWash 2Faith Dianasas RequinaNo ratings yet
- Wash 4Document6 pagesWash 4Faith Dianasas RequinaNo ratings yet
- Wash 3Document6 pagesWash 3Faith Dianasas RequinaNo ratings yet
- Hand Hygiene and Handwashing: InfectionDocument7 pagesHand Hygiene and Handwashing: InfectionFaith Dianasas RequinaNo ratings yet
- Inventory of Medicines: July 9, 2021Document1 pageInventory of Medicines: July 9, 2021Faith Dianasas RequinaNo ratings yet
- Hand Hygiene and HandwashingDocument7 pagesHand Hygiene and HandwashingFaith Dianasas RequinaNo ratings yet
- Terms: InfectionDocument7 pagesTerms: InfectionFaith Dianasas RequinaNo ratings yet
- Inventory of Medicines: July 9, 2021Document1 pageInventory of Medicines: July 9, 2021Faith Dianasas RequinaNo ratings yet
- Hand Hygiene and HandwashingDocument8 pagesHand Hygiene and HandwashingFaith Dianasas RequinaNo ratings yet
- Hand Hygiene and HandwashingDocument7 pagesHand Hygiene and HandwashingFaith Dianasas RequinaNo ratings yet
- Hand Hygiene and HandwashingDocument8 pagesHand Hygiene and HandwashingFaith Dianasas RequinaNo ratings yet
- BMIapril 2021Document2 pagesBMIapril 2021Faith Dianasas RequinaNo ratings yet
- 1Document1 page1Faith Dianasas RequinaNo ratings yet
- Inventory of Medicines: July 9, 2021Document1 pageInventory of Medicines: July 9, 2021Faith Dianasas RequinaNo ratings yet
- BMIapril 2021Document2 pagesBMIapril 2021Faith Dianasas RequinaNo ratings yet
- Inventory of Medicines: July 9, 2021Document1 pageInventory of Medicines: July 9, 2021Faith Dianasas RequinaNo ratings yet
- Inventorymeds 2021Document1 pageInventorymeds 2021Faith Dianasas RequinaNo ratings yet
- BMIapril 2021Document2 pagesBMIapril 2021Faith Dianasas RequinaNo ratings yet
- Body Mass Index (BMI) : Name HT (CM) WT (KG) Age BMI Remarks Orange HouseDocument2 pagesBody Mass Index (BMI) : Name HT (CM) WT (KG) Age BMI Remarks Orange HouseFaith Dianasas RequinaNo ratings yet
- Medicines 2021Document1 pageMedicines 2021Faith Dianasas RequinaNo ratings yet
- Body Mass Index (Bmi) : Name H (CM) W (KG) Age BMI Remarks Orange HouseDocument2 pagesBody Mass Index (Bmi) : Name H (CM) W (KG) Age BMI Remarks Orange HouseFaith Dianasas RequinaNo ratings yet
- Body Mass Index (BMI) : Name HT (CM) WT (KG) Age BMI Remarks Orange HouseDocument2 pagesBody Mass Index (BMI) : Name HT (CM) WT (KG) Age BMI Remarks Orange HouseFaith Dianasas RequinaNo ratings yet
- Inventory of Medicines: July 9, 2021Document1 pageInventory of Medicines: July 9, 2021Faith Dianasas RequinaNo ratings yet
- Body Mass Index (BMI) : Name HT (CM) WT (KG) Age BMI Remarks Orange HouseDocument2 pagesBody Mass Index (BMI) : Name HT (CM) WT (KG) Age BMI Remarks Orange HouseFaith Dianasas RequinaNo ratings yet
- Body Mass Index (BMI) : Name HT (CM) WT (KG) Age BMI Remarks Orange HouseDocument2 pagesBody Mass Index (BMI) : Name HT (CM) WT (KG) Age BMI Remarks Orange HouseFaith Dianasas RequinaNo ratings yet
- Body Mass Index (BMI) : Name HT (CM) WT (KG) Age BMI Remarks Orange HouseDocument2 pagesBody Mass Index (BMI) : Name HT (CM) WT (KG) Age BMI Remarks Orange HouseFaith Dianasas RequinaNo ratings yet
- Case Presentation About Calculous CholecyctitisDocument23 pagesCase Presentation About Calculous CholecyctitiskarenNo ratings yet
- Gastroenterology - GallbladderDocument2 pagesGastroenterology - GallbladderEugen MNo ratings yet
- IIIDocument13 pagesIIIapi-3828211No ratings yet
- Abdominal Examination Guide for Medical StudentsDocument9 pagesAbdominal Examination Guide for Medical StudentsAnonymous 278KLXQgI3No ratings yet
- Meshoma A Rare Complication of Abdomen and HerniaDocument3 pagesMeshoma A Rare Complication of Abdomen and HernialeartaNo ratings yet
- Disease of Biliary SystemDocument88 pagesDisease of Biliary SystemProsanta Kr BhattacharjeeNo ratings yet
- اسئله جراحه مدققهDocument59 pagesاسئله جراحه مدققهNour AhmededNo ratings yet
- MCQ Block 13Document15 pagesMCQ Block 13Liliana Surya Fatimah0% (1)
- Abdomen in Acute-Critical Care MedicineDocument50 pagesAbdomen in Acute-Critical Care MedicineBejinaruOanaSiCristiNo ratings yet
- CholecystitisDocument10 pagesCholecystitisCris Pin BumatangNo ratings yet
- Intraoperative CholangiogramDocument3 pagesIntraoperative CholangiogramPauline Jimenea100% (2)
- CHOLELITHIASISDocument12 pagesCHOLELITHIASISShenbagam MahalingamNo ratings yet
- Repair of Common Bile Duct InjuriesDocument12 pagesRepair of Common Bile Duct InjuriesDragoș PopaNo ratings yet
- CH 59 Care of Patients With Problems of The Biliary System and PancreasDocument28 pagesCH 59 Care of Patients With Problems of The Biliary System and Pancreasjrflores1284No ratings yet
- Cholecystitis PresentationDocument12 pagesCholecystitis PresentationShivangi KulbhaskarNo ratings yet
- 5 Obstructive Jaundice EditedDocument33 pages5 Obstructive Jaundice EditedNadhirah ZulkifliNo ratings yet
- PIR Abril 2010Document72 pagesPIR Abril 2010parasilviaNo ratings yet
- General Surgery: (Gallbladder Disease)Document1 pageGeneral Surgery: (Gallbladder Disease)Matt100% (1)
- KolelitiasisDocument20 pagesKolelitiasisonjieeNo ratings yet
- Interventional Approaches Gallbladder DiseaseDocument9 pagesInterventional Approaches Gallbladder DiseaseAntônio GoulartNo ratings yet
- Laparoscopic Cholecystectomy SurgeryDocument22 pagesLaparoscopic Cholecystectomy SurgeryKn VelasquezNo ratings yet
- 08-DISEASES LIVER Q - 5836757647Document12 pages08-DISEASES LIVER Q - 5836757647azizNo ratings yet
- Therapeutic Guidelines Antimicrobial Prophylaxis SurgeryDocument86 pagesTherapeutic Guidelines Antimicrobial Prophylaxis SurgeryhendryfransiskusNo ratings yet
- Liver & Gall Bladder: Presented by DR - Sujaya NairDocument102 pagesLiver & Gall Bladder: Presented by DR - Sujaya Nairjoy rajNo ratings yet