Professional Documents
Culture Documents
Listeriosis Outbreak Situation Report - 22april 2018 - Fordistribution
Uploaded by
eNCA.comOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Listeriosis Outbreak Situation Report - 22april 2018 - Fordistribution
Uploaded by
eNCA.comCopyright:
Available Formats
Situational Report
Outbreak Name Listeriosis Country affected South Africa
Date & Time of report 20 April 2018 Investigation start date August 2017
Prepared by National Listeria Incident Management Team (IMT)
Figure 1 (left). Electron micrograph showing
two Listeria monocytogenes bacteria,
illustrating the single ‘flagellum’ that makes
the organism motile (courtesy Dr Monica
Birkhead, NICD)
1. HIGHLIGHTS
A multisectorial incident management team (IMT) has been formed by the National Department of Health (NDoH) to
strengthen co-ordination of outbreak response and strengthen health systems to prevent future outbreaks. Funding is
being sourced.
The number of cases of laboratory-confirmed listeriosis reported per week has decreased since the implicated
products were recalled on 04 March 2018, with eight additional cases reported this week. Of the eight cases reported
this week, one case occurred in October 2017 and was retrospectively reported.
Since the recall, a total of 50 cases have been reported
a. Twenty-four (48%) were among neonates ≤28 days old
b. Three (6%) were among children age 1 month to 14 years old
As of 17 April 2018, a total of 1 019 laboratory-confirmed listeriosis cases have been reported to NICD since 01 January
2017.
2. BACKGROUND
Listeriosis was not notifiable until 15 December 2017. Prior to 2017, an average of 60 to 80 laboratory-confirmed listeriosis
cases per year (approximately 1 per week), were reported in South Africa. In July 2017, an increase in laboratory-confirmed
cases of listeriosis was reported to National Institute for Communicable Diseases (NICD) which was followed by
investigations into the reported increase. On 05 December 2017, the listeriosis outbreak was declared by the Minister of
Health, Dr. Aaron Motsoaledi. The source of the outbreak was identified as ready-to-eat processed meat products
manufactured at Enterprise Foods’ Polokwane production facility. A recall of affected products was initiated on 05 March
2018.
3. EMERGENCY MANAGEMENT APPROACH
Emergency response activities that have been conducted by various stakeholders are continuing and intensifying, including
surveillance (detection and investigation of cases), risk communication activities, and food safety legislative review and
reform. To inform and support these activities, additional activities will be implemented in a phased approach as follows:
Phase 1: Identification of at-risk food processing plants, development of material and training of staff to support
inspections of facilities
Phase 2: Inspection of at-risk food processing plant and strengthening of district environmental health
practitioners
Phase 3: Reporting and consolidation of health system strengthening activities, and after action review.
4. PUBLIC HEALTH ACTION/RESPONSE INTERVENTIONS
1. CO-ORDINATION
A multi-sectoral incident management team (IMT) has been strengthened under the leadership of the Department of
Health. This development builds on the initial EOC activation in December, and draws upon appropriate experts from
key stakeholders, essential to the control of this emergency and with the skills to strengthen the system for future
outbreaks of this nature.
Listeriosis outbreak situation report - 22/04/2018 1
An updated Listeriosis Emergency Response Plan (ERP, April 2018) has been developed and approved by the DG
NDoH. The aim of the ERP is to intensify response activities to control and end the current listeriosis outbreak and
strengthen health systems to prevent future outbreaks. Response activities are being directed by the designated
Incident Manager according to the plan which includes a robust monitoring framework for tracking the progress.
A two-day combined meeting of provincial and national stakeholders including health promotion and
communications staff, Communicable Disease Co-ordinators and environmental health practitioners, along with NICD
and WHO technical experts will be held on 24/25 April to communicate details of the ERP.
A WHO Listeriosis Technical Meeting is taking place in Johannesburg on from 19-21 April 2018 attended by delegates
from 16 countries from the SADC region and beyond. The aim of the meeting is to share experiences from South
Africa, increase awareness of listeriosis and guide countries to start preparing contingency plans to respond and
control listeriosis.
2. SURVEILLANCE
Descriptive epidemiology
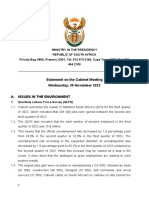
1 019 cases reported from 01 January 2017 to 17 April 2018. The number of reported cases has decreased
since the implicated products were recalled on 04 March 2018 (Figure 1).
Since week 9 (5 March 2018), cases per week have dropped to fewer than 15/week, with 8 cases reported in
week 14. At the height of the outbreak, 30 or more cases were reported weekly.
Neonates ≤28 days of age are the most affected age group (on account of increased vulnerability of
pregnant women), followed by adults aged 15 – 49 years of age (Figure 2). Most cases have been reported
from Gauteng Province (59%,579/1 019), followed by Western Cape (13%, 127/1 019) and KwaZulu-Natal
(7%, 73/1 019) provinces (Table 1).
45
RECALL 45
40 40
35 35
Number of cases
30 30
25 25
20 20
15 15
10 10
5 5
0 0
1 3 5 7 9 11 13 15 17 19 21 23 25 27 29 31 33 35 37 39 41 43 45 47 49 51 1 3 5 7 9 11 13 15 17
2017 2018
Epidemiological weeks
Figure 2: Epidemic curve of laboratory-confirmed listeriosis cases by epidemiological week (numbered weeks of the
year, starting with week 1 in January) and date of sample collection, South Africa, 01 January 2017 to 17 April 2018
(n=1 019)
500
400
300
Nunber of cases
200 OUTCOME PENDING
100 DISCHARGED
0 DIED
≤28 days 1Month - 15 - 49 50 - 64 ≥65 years Age
14 years years years Unknown
Age group
Figure 3: Age distribution and outcome of laboratory-confirmed listeriosis cases, South Africa, 01 January 2017 to 17
April 2018 (n=1 019)
Listeriosis outbreak situation report - 22/04/2018 2
Table 1. Number of laboratory-confirmed listeriosis cases and deaths by province, where outcome data is available:
Outcome available (% of total Number of deaths (% of those Total cases (% of cases
Province
cases in RSA) with outcome available) in all provinces)
Gauteng 370 (62.0) 105 (28.4) 597 (58.6)
Western Cape 113 (89.0) 29 (25.7) 127 (12.5)
KwaZulu-Natal 47 (64.4) 18 (38.3) 73 (7.2)
Mpumalanga 45 (95.7) 11 (24.4) 47 (4.6)
Limpopo 33 (63.5) 7 (21.2) 52 (5.1)
Eastern Cape 30 (56.6) 11 (36.7) 53 (5.2)
Free State 30 (85.7) 8 (26.7) 35 (3.4)
North West 25 (86.2) 7 (28.0) 29 (2.8)
Northern Cape 5 (83.3) 3 (60.0) 6 (0.6)
Total 698 (68.5) 199 (28.5) 1 019 (100)
Following a recall of implicated products, the number of cases are going down. However, it is anticipated that cases
could still be reported for the following reasons:
a. The incubation period of listeriosis can be up to 70 days
b. The implicated products have a long shelf life and it is possibly that despite the recall some products have
not been removed from retail or consumer’s homes
c. Cross-contamination at retail and in the home can occur
Analysis by exposure
a. Before recall
106 interviews done before the recall
90/106 (84%) of people interviewed reported consuming ready-to-eat processed meat
products
88/90 (97%) of people who consumed ready-to-eat processed meat products had consumed
polony
o Post recall
23 interviews done post recall.
15/23 (65%) of ill people or their proxy reported consuming or handling polony prior to their
illness onset
Monitoring for additional cases will continue, and any new cases reported will be interviewed.
3. LABORATORY
NICD:
a. Of the 1 019 laboratory-confirmed cases, whole genome sequencing of 442 isolates has been completed to
date, with 92% (406/442) identified as Sequence Type 6 (ST6), 8% (36/442) representing 11 other Sequence
Types (ST1, ST101, ST2, ST204, ST219, ST224, ST3, ST5, ST54, ST8, and ST876).
b. Whole genome sequencing has also been conducted on 411 isolates from food and environmental samples
to date. Thirty-eight isolates (9%) have been identified as ST6, and 19 Sequence Types account for the
remainder.
c. All clinical isolates received at NICD will undergo whole genome sequencing.
NHLS Public Health Laboratory:
a. In addition to standard food microbiology, enumerative microbiology for Listeria, aligned with the ISO
11290 methodology, has been introduced in the NHLS Public Health Laboratory at Wits Medical School.
b. Additional staffing and equipment requests have been submitted. Both staffing and equipment are required
to ensure an adequate laboratory response to this outbreak.
c. Training programs have been developed to ensure that food specimens are collected and transported
correctly and in accordance with legislative requirements.
d. All Listeria monocytogenes isolates from food samples are submitted to the NICD for whole genome
sequencing.
Listeriosis outbreak situation report - 22/04/2018 3
3. ENVIRONMENTAL HEALTH and FOOD SAFETY
a. A team of environmental health practitioners (EHPs) have been seconded from national, provincial and district
authorities and from the South African Medical Health Services (SAMHS) to work full-time in the IMT.
b. A risk evaluation framework has been drawn up to assist with identification of food processing plants for
inspection. Lists of food processing plants have been requested from district municipalities.
c. A checklist and inspection manual to facilitate inspections of high-risk facilities using the current legislative policy
framework for food safety is being drawn up.
4. RECALL PROCESS
a. The National Consumer Commission (NCC) has provided the International Network of Food Safety Authorities
(INFOSAN) with required details regarding lists of recalled products and their export destinations.
b. The Department of Environmental Affairs (DEA) is collating certificates of destruction for recalled products. The
volumes of recalled and destroyed product is being calculated.
5. TRAINING/CAPACITY BUILDING
a. A top-up skills training programme for environmental health offices and risk communication specialists has been
developed for roll-out to all the provinces. The first training is scheduled for 03-04 May 2018 in Gauteng
Province.
b. A situational analysis of NHLS public health laboratories has been conducted. For the current Listeria outbreak
response, the NHLS Public Health Laboratory in Prince Street, Durban has been identified as a second site for
Listeria testing. Other NHLS public health laboratories across the country will be capacitated in due course.
6. RISK COMMUNICATION, COMMUNITY ENGAGEMENT & SOCIAL MOBILISATION
a. Information and education material is being reviewed. The five keys to safer food messages have been translated
and reviewed, prior to printing and distribution. A Five Keys to Safer Food poster has been shared with provinces
to check the relevance and correctness of the language used.
b. Over 145 health awareness campaigns and education programs have been conducted on listeriosis in the nine
Provinces. The target audience includes members of the community, food handlers and various institutions
(crèches, clinics, old age homes school learners, schools, hospitals, soup kitchens, restaurants, retail, butcheries,
fisherman’s accommodation establishments, supermarkets, pension pay points, informal traders, bakeries, tuck
shops & taverns) including employees within the various organs of state).
c. IEC Materials were reprinted in municipalities and uploading on their websites and internal communications
systems.
7. POLICY GUIDANCE and LEGISLATION
Training materials that outline the current food safety legislative framework including regulations governing the rights
and duties of inspectors are being developed to support inspection teams. A technical Sub-Committee has been
established to review and propose amendments to RSA food safety and outbreak response legislation.
5. CHALLENGES/GAPS
Initial funding to support the ERP has been obtained and authorised through the NDoH. Additional funding has been
requested.
6. RECOMMENDATIONS & PRIORITY FOLLOW UP ACTIONS
Clinicians are requested to notify cases through the notifiable medical conditions (NMC) surveillance channels. NHLS and
private clinical laboratories are requested to continue to send all Listeria spp. isolates to NICD to facilitate case monitoring
and whole genome sequencing. All “ready to eat” food processing factories are advised to review their processes, to
ensure that their package products are safe for distribution and consumption by the public.
7. CONCLUSIONS
The formation of a multisectoral incident management team, and development of a listeria emergency response plan will
strengthen the response to the listeria outbreak, and contribute to health system strengthening to prevent future outbreaks.
Listeriosis outbreak situation report - 22/04/2018 4
You might also like
- Power Alert 1 - 05 January 2023Document1 pagePower Alert 1 - 05 January 2023eNCA.comNo ratings yet
- Letter To DG TshanganaDocument1 pageLetter To DG TshanganaeNCA.comNo ratings yet
- DCS To Terminate Concession Contract at Mangaung Correctional CentreDocument1 pageDCS To Terminate Concession Contract at Mangaung Correctional CentreeNCA.comNo ratings yet
- Media Statement - Dsac On The Passing of Aka 11 February 2023 - 230211 - 082746Document2 pagesMedia Statement - Dsac On The Passing of Aka 11 February 2023 - 230211 - 082746eNCA.comNo ratings yet
- Media Statement - Arrest of GuptasDocument1 pageMedia Statement - Arrest of GuptaseNCA.comNo ratings yet
- Media Statement - Moretele Municipality Manager Arrest Welcome 18 July 2022Document3 pagesMedia Statement - Moretele Municipality Manager Arrest Welcome 18 July 2022eNCA.comNo ratings yet
- Anc GP Notice.Document1 pageAnc GP Notice.eNCA.comNo ratings yet
- Gauteng Premier Saddened by Rising Death Toll Following The Boksburg Truck ExplosionDocument2 pagesGauteng Premier Saddened by Rising Death Toll Following The Boksburg Truck ExplosioneNCA.comNo ratings yet
- Cabinet Statement Final830Document18 pagesCabinet Statement Final830eNCA.comNo ratings yet
- Order GP0522Document10 pagesOrder GP0522eNCA.comNo ratings yet
- Media Statement - Fuel Prices Adjustment For October 2022Document3 pagesMedia Statement - Fuel Prices Adjustment For October 2022eNCA.comNo ratings yet
- Media Statement - Fuel Prices For Jun 2022Document4 pagesMedia Statement - Fuel Prices For Jun 2022eNCA.comNo ratings yet
- Premier David Makhura To Handover His Resignation Letter To The Speaker of The Provincial LegislatureDocument3 pagesPremier David Makhura To Handover His Resignation Letter To The Speaker of The Provincial LegislatureeNCA.comNo ratings yet
- Gauteng Provincial Government Places Senior Health Officials On Precautionary Suspension As The Siu Begins An Investigation Into Procurement at Tembisa HospitalDocument2 pagesGauteng Provincial Government Places Senior Health Officials On Precautionary Suspension As The Siu Begins An Investigation Into Procurement at Tembisa HospitaleNCA.comNo ratings yet
- Government Gazette Staatskoerant: Republic of South Africa Republiek Van Suid AfrikaDocument4 pagesGovernment Gazette Staatskoerant: Republic of South Africa Republiek Van Suid AfrikaeNCA.com100% (3)
- Power Alert 1 - 22 June 2022Document1 pagePower Alert 1 - 22 June 2022eNCA.comNo ratings yet
- Second Booster Dose For J&J VaccineDocument2 pagesSecond Booster Dose For J&J VaccineeNCA.comNo ratings yet
- MFMA2020-21 Media-Release 15 June Final ApprovedDocument14 pagesMFMA2020-21 Media-Release 15 June Final ApprovedeNCA.comNo ratings yet
- Temporary Closure of Tembisa Hospital After Fatal Incident 20220209Document1 pageTemporary Closure of Tembisa Hospital After Fatal Incident 20220209eNCA.comNo ratings yet
- CEF Press Release 25 Feb 2022Document4 pagesCEF Press Release 25 Feb 2022eNCA.com100% (1)
- 13-4 CoOperativeGovernanceDocument8 pages13-4 CoOperativeGovernanceeNCA.comNo ratings yet
- Joint Statement-Extension of The Temporary Reduction in The General Fuel LevyDocument2 pagesJoint Statement-Extension of The Temporary Reduction in The General Fuel LevyeNCA.comNo ratings yet
- Statement DLCA XtensionDocument9 pagesStatement DLCA XtensioneNCA.comNo ratings yet
- Letter To Phathiswa Magopeni 28 Jan 2022Document2 pagesLetter To Phathiswa Magopeni 28 Jan 2022eNews Channel AfricaNo ratings yet
- Fire Safety Observations Parliamentary Complex 2 January 2022Document22 pagesFire Safety Observations Parliamentary Complex 2 January 2022eNCA.comNo ratings yet
- Pule Mlambo Progrmme (A)Document1 pagePule Mlambo Progrmme (A)eNCA.comNo ratings yet
- Statement On Passing of Emalahleni Executive MayorDocument2 pagesStatement On Passing of Emalahleni Executive MayoreNCA.comNo ratings yet
- Media Statement 21 December 2021Document2 pagesMedia Statement 21 December 2021eNCA.comNo ratings yet
- MEDIA RELEASE Janssen Vaccine BoosterDocument2 pagesMEDIA RELEASE Janssen Vaccine BoostereNCA.comNo ratings yet
- Zuma ParoleDocument34 pagesZuma ParoleTimesLIVE100% (1)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Instrumentation Positioner PresentationDocument43 pagesInstrumentation Positioner PresentationSangram Patnaik100% (1)
- Nursing Care Management of a Client with Multiple Medical ConditionsDocument25 pagesNursing Care Management of a Client with Multiple Medical ConditionsDeannNo ratings yet
- S5-42 DatasheetDocument2 pagesS5-42 Datasheetchillin_in_bots100% (1)
- Unit-1: Introduction: Question BankDocument12 pagesUnit-1: Introduction: Question BankAmit BharadwajNo ratings yet
- 08 Sepam - Understand Sepam Control LogicDocument20 pages08 Sepam - Understand Sepam Control LogicThức Võ100% (1)
- Sysmex Xs-800i1000i Instructions For Use User's ManualDocument210 pagesSysmex Xs-800i1000i Instructions For Use User's ManualSean Chen67% (6)
- IGCSE Chemistry Section 5 Lesson 3Document43 pagesIGCSE Chemistry Section 5 Lesson 3Bhawana SinghNo ratings yet
- Motor Master 20000 SeriesDocument56 pagesMotor Master 20000 SeriesArnulfo Lavares100% (1)
- To Introduce BgjgjgmyselfDocument2 pagesTo Introduce Bgjgjgmyselflikith333No ratings yet
- Water Jet CuttingDocument15 pagesWater Jet CuttingDevendar YadavNo ratings yet
- TheEconomist 2023 04 01Document297 pagesTheEconomist 2023 04 01Sh FNo ratings yet
- Cushman Wakefield - PDS India Capability Profile.Document37 pagesCushman Wakefield - PDS India Capability Profile.nafis haiderNo ratings yet
- UAPPDocument91 pagesUAPPMassimiliano de StellaNo ratings yet
- Evaluating MYP Rubrics in WORDDocument11 pagesEvaluating MYP Rubrics in WORDJoseph VEGANo ratings yet
- Wi FiDocument22 pagesWi FiDaljeet Singh MottonNo ratings yet
- Borello-Bolted Steel Slip-Critical Connections With Fillers I. PerformanceDocument10 pagesBorello-Bolted Steel Slip-Critical Connections With Fillers I. PerformanceaykutNo ratings yet
- JurnalDocument9 pagesJurnalClarisa Noveria Erika PutriNo ratings yet
- C6 RS6 Engine Wiring DiagramsDocument30 pagesC6 RS6 Engine Wiring DiagramsArtur Arturowski100% (3)
- AFNOR IPTDS BrochureDocument1 pageAFNOR IPTDS Brochurebdiaconu20048672No ratings yet
- Non Circumvention Non Disclosure Agreement (TERENCE) SGDocument7 pagesNon Circumvention Non Disclosure Agreement (TERENCE) SGLin ChrisNo ratings yet
- Biagioli Did Galileo Copy The TelescopeDocument28 pagesBiagioli Did Galileo Copy The TelescopeGregory HooNo ratings yet
- Iq TestDocument9 pagesIq TestAbu-Abdullah SameerNo ratings yet
- Federal Complaint of Molotov Cocktail Construction at Austin ProtestDocument8 pagesFederal Complaint of Molotov Cocktail Construction at Austin ProtestAnonymous Pb39klJNo ratings yet
- "Behind The Times: A Look at America's Favorite Crossword," by Helene HovanecDocument5 pages"Behind The Times: A Look at America's Favorite Crossword," by Helene HovanecpspuzzlesNo ratings yet
- Towards A Human Resource Development Ontology Combining Competence Management and Technology-Enhanced Workplace LearningDocument21 pagesTowards A Human Resource Development Ontology Combining Competence Management and Technology-Enhanced Workplace LearningTommy SiddiqNo ratings yet
- QuickTransit SSLI Release Notes 1.1Document12 pagesQuickTransit SSLI Release Notes 1.1subhrajitm47No ratings yet
- Google Dorks For PentestingDocument11 pagesGoogle Dorks For PentestingClara Elizabeth Ochoa VicenteNo ratings yet
- Malware Reverse Engineering Part 1 Static AnalysisDocument27 pagesMalware Reverse Engineering Part 1 Static AnalysisBik AshNo ratings yet
- Passenger E-Ticket: Booking DetailsDocument1 pagePassenger E-Ticket: Booking Detailsvarun.agarwalNo ratings yet
- En dx300lc 5 Brochure PDFDocument24 pagesEn dx300lc 5 Brochure PDFsaroniNo ratings yet