Professional Documents
Culture Documents
Article WJPR 1423131099
Uploaded by
Jasleen KaurOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Article WJPR 1423131099
Uploaded by
Jasleen KaurCopyright:
Available Formats
World Journal of Pharmaceutical Research
Kiran et al. World Journal of Pharmaceutical Research
SJIF Impact Factor 5.045
Volume 4, Issue 2, 1435-1441. Research Article ISSN 2277– 7105
ANTIBIOTIC PROPHYLAXIS AND SURGICAL SITE INFECTIONS IN
HERNIA PATIENTS – AN OBSERVATIONAL STUDY IN A PRIVATE
AND GOVERNMENT TERTIARY CARE HOSPITALS
1
Dr.Kiran Lakkol Jambulingappa*, 2Dr.Umakant Nagashetty Patil,
3
Dr.Shivashankaramurthy K G, 4Mr.Chetan Kumar and 5Dr.Apoorva B M
1,3
Associate Professor of Pharmacology, SSIMSRC, Davanagere-577005.
2
Professor & Head of Pharmacology, SSIMSRC, Davanagere-577005.
4
Research co-ordinator, SSIMSRC, Davanagere-577005.
5
Postgraduate student of Pharmacology, SSIMSRC, Davanagere-577005.
ABSTRACT
Article Received on
13 Dec 2014, Background: Surgical site infections are one of the most common
Revised on 07 Jan 2015, causes of nosocomial globally resulting in high morbidity and
Accepted on 01 Feb 2015
mortality. The irrational prescription of antibiotics is responsible for
the development of resistance to micro organisms along with
*Correspondence for
economical burden to the patients. Aim: To evaluate the incidence of
Author
Dr. Kiran Lakkol postoperative wound infections of patients undergoing hernia surgeries
Jambulingappa and to study the prescription pattern of prophylactic antibiotics in
Associate Professor of private and government tertiary care hospitals. Materials and
Pharmacology,
methods: An observational study where patients undergoing hernia
SSIMSRC, Davanagere-
surgeries admitted in the surgical wards of private and government
577005.
tertiary care hospital by selecting 30 patients from each hospitals. Data
was analyzed using Microsoft Office Excel 2007 and values were presented descriptively.
Results: The overall prevalence of surgical site infections in this study was 21.66%. Mean
age in both the hospitals was 42(±14.23) and 49.6(±16.79) respectively and sex was 09:01and
12:01 respectively. Cephalosporins (71.73%) and Aminoglycosides (13.04%) were the most
commonly prescribed class of antibiotics. The mean average duration of prescription was
2.43(±0.95) to 06 days and follow-up was 3.62(±10.1) to 09 days. Conclusion: Urgent steps
like specific guidelines, training and monitoring the use of prophylactic antibiotics are needed
to correct some irrational approaches to prevent the causing burden to the patients.
www.wjpr.net Vol 4, Issue 2, 2015. 1435
Kiran et al. World Journal of Pharmaceutical Research
KEYWORDS: Antibiotic prophylaxis, surgical site infections, hernia repair.
INTRODUCTION
Surgical wound infection is one of the most commonly occurring surgical complications.
Infection of a wound may result from a number of factors both intrinsic and extrinsic to the
patients. Although many of the intrinsic factors cannot be modified, the external ones can
certainly be influenced. In particular those related to aseptic conditions, surgical technique
and peri-operative care. However even under the most scrupulous aseptic conditions and with
a careful technique, post-operative wound infection still presents a very serious problem.
Surgical site infection (SSI) accounts for 20% of all healthcare associated infections.[1]
Approximately 5% of patients undergoing surgery develop SSI.[2] SSI results in failure of
wound healing with subsequent increased treatment cost, a greater likelihood of admission to
the intensive care unit, prolonged hospital stay and higher post-operative mortality.[3,4] In
particular, studies have demonstrated an extra 7-10 days inpatient stays in those with SSI.[4-6]
The use of antibiotic prophylaxis to avoid infectious complications of surgery is very
common in surgical practice. However, indiscriminate use of antibiotics can lead to problems
including an increase in costs and the emergence of resistant micro-organisms. The benefits
of antibiotic prophylaxis either in clean-contaminated, contaminated and dirty surgery are
universally accepted but in case of clean surgery it is generally accepted in when the
placement of prosthetic materials, or the presence of infection poses a significant risk to the
patient. Nonetheless, controversy remains about the use of antibiotics in some types of clean
surgery.
Surgery of inguinal hernia is one of the most common techniques performed in a general
surgical service making up approximately a third of total interventions.[7] This type of surgery
is considered clean and it has been estimated that the rate of post-operative infection should
not be greater than 2%.[8-11]
Currently, the use of antibiotic prophylaxis is recommended for elective open mesh inguinal
hernia repair.[8,9 &11] However this treatment is not universally accepted. For hernia repair not
involving prosthetic material, the antibiotic prophylaxis is not recommended in the absence
of risk factors, but the controversy arises when wound infection rates exceed the expected
figures.[12-14] Therefore, there is interest in SSI and its prevention amongst surgeons and
www.wjpr.net Vol 4, Issue 2, 2015. 1436
Kiran et al. World Journal of Pharmaceutical Research
amongst many other healthcare professionals, because of the increase patient morbidity and
the associated financial burden. This study will depict a clear picture of use of prophylactic
antibodies and the rate of SSIs in hernia patients in two tertiary care hospitals.
MATERIALS AND METHODS
Study design and data collection
An observational study was conducted in 60 patients undergoing hernia surgeries admitted in
the surgical wards of Government and Private hospitals, Davangere with 30 patients from
each hospital.
Postoperative surgical wound infection was considered by the presence of at least one of the
following criteria:
1. Purulent drainage from the surgical site with or without laboratory confirmation.
2. At least one of the following signs or symptoms of infection like pain or tenderness, local
swelling, redness or heat and a superficial incision deliberately opened by surgeon, unless
the incision in culture-negative.
3. An abscess or other evidence of infection is found on a direct examination, during
reoperation, or by the histopathology or radiology examination.
4. Diagnosis of surgical site infection by the surgeon or attending physician.
Inclusion criteria
All patients of either sex of any age undergoing hernia surgeries admitted to the surgical
wards of Government and Private Hospitals, Davangere, Karnataka.
Exclusion criteria
Patients with diabetes, tuberculosis and obesity are excluded from the study.
Demographic details like patient’s age, sex and data related to prescription pattern, average
number of drugs used per patient, duration of treatment was collected in standard case study
forms.
Collected data was analyzed by frequency, percentage, mean and standard deviation.
Statistical software used was Graph Pad.
RESULTS AND DISCUSSION
Out of 60 patients, 26 (86.66%) were male and 4 (13.33%) were female in private hospital
and 28 (93.33%) were male and 2 (6.66%) were female in government hospital. The mean
www.wjpr.net Vol 4, Issue 2, 2015. 1437
Kiran et al. World Journal of Pharmaceutical Research
age and sex of patients was 49.6 (SD=16.79) and 12:01 in private and in government hospital
42 (SD=14.23) and 09:01 respectively. The distributions of age and sex groups are shown in
figure 1 and 2.
Figure 1: Bar Chart showing age distribution in two different hospitals
Figure 2: Bar Chart showing sex wise distribution in two different hospitals
In private hospital, out of 30 patients, 16 were diagnosed for inguinal hernia surgery, 14 were
diagnosed as other types of hernia surgery and in government hospital, 23 were diagnosed for
inguinal surgery and 7 were diagnosed as other types of hernia surgery.
All the 60 patients received the prophylactic antibiotics preoperatively and post operatively.
Some patients are received more than one antibiotic. Total 15 numbers of antibiotics were
www.wjpr.net Vol 4, Issue 2, 2015. 1438
Kiran et al. World Journal of Pharmaceutical Research
prescribed, consists classes of Cephalosporins, Aminoglycosides, Fluoroquinolones,
Tetracycline, Pencillin, Macrolide and few Fixed Dose Combinations. Most common used
antibiotics were Cefotaxim (in 36 cases) and followed by Ceftriaxome (in 14 cases) and least
administered antibiotics were Ceftazidime, Cefdinir, Ciprofloxacin, Doxycyclin, Ampicillin,
respectively. Drug prescription pattern and average duration of antibiotics prescription is
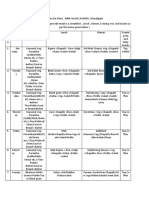
mentioned in the table 1.
Table 1: Drug prescription pattern and average duration of prescription
Total No. No. of Cases Average Duration of Rx
Prescribed Antibiotics
of Cases Private Government Private Government
CEPHALOSPORINS
Cefotaxim 36 13 23 2.43±0.95 2.43±0.95
Ceftriaxone 14 08 06 3.75+1.83 2.5±0.5
Cefixime 08 06 02 03 03
Cefuroxime 06 05 01 4+1.66 03
Ceftazidime 01 01 0 5 --
Cefdinir 01 01 0 5 --
AMINOGLYCOSIDES
Amaikacin 12 09 03 4+1.66 03
FLUOROQUINOLONES
Ciprofloxacin 01 01 00 05 --
TETRACYCLINE
Doxycycline 01 01 00 06 --
PENCILLIN
Amoxicillin 03 00 03 -- 3.67+0.94
Ampicillin 01 01 00 03 --
MACROLIDE
Azithromycin 03 03 00 3.67+1.15 --
F DC
Amoxycillin+Clavulinic acid 04 04 00 2.75±1.7 --
Cefixime+Cloxacillin 01 01 00 10 --
The mean duration of follow-up days was 6.13 (SD=2.33) in private and 3.62 (SD=1.01) in
government hospital. Total 13 numbers of patients developed surgical site infections in both
private and government hospitals.
DISCUSSIONS
In this study it clearly shows the slight increase in rate of postoperative surgical site
infections in clean surgeries also even after the administration of prophylactic antibiotics. In
the private hospital, drug prescription pattern shows the usage of higher antibiotics which are
of much higher price and this will increase the emergence of antimicrobial resistance, super-
infection, and the risks of toxic and adverse drug reactions along with the increase of cost of
www.wjpr.net Vol 4, Issue 2, 2015. 1439
Kiran et al. World Journal of Pharmaceutical Research
therapy. Prophylaxis with the broad spectrum antibodies like Fluroquinolones or fourth or
third generation Cephalosporins should not be prescribed. For surgical prophylaxis it is
important to select an antibiotic with narrowest antibacterial spectrum to reduce the
emergence of resistance and also because broad spectrum antibiotics may be required later if
patient develops serious sepsis. First generation Cephalosporins like Cefazolin is the best
agent for surgical prophylaxis. But in this study, 71.73% patients received broad sepectrum
Cephalosporins like Cefotaxim, Ceftriaxone, Cefixime. This simply reflects the non-
adherence to the recommendations or either the less availability or less aware to the
recommended guidelines.
Also study results shows the only usage of prophylactic antibiotics will not reduce the
surgical site infections but also preoperative assessment to optimize underlying disease such
as diabetes mellitus, aseptic techniques in the operating theatre also contribute in developing
surgical site infections. So preoperative, intraoperative and postoperative management can
modify the risk for developing surgical site infections.
CONCLUSION
Excessive and inappropriate use of antibiotics in health care facilities and the communities
contributes to development of antibiotic resistance. Multiple antibiotics are available and
information or a standard guideline about antibiotic use pattern is necessary to formulate a
constructive approach to the problem of inappropriate drug use. Additional study is needed to
answer questions such as what constitutes a real risk factor, selective use of antibiotics
according to patient risk factors, the cost effectiveness of prophylactic antibiotics and late
onset infection, among other questions. This approach might finally reduce the burden to the
patients.
REFERENCES
1. De Lissovoy G, Fraeman K, Hutchins V et al. Surgical site infection: incidence and
impact on hospital utilization and treatment costs. Am J Infect Control, 2009; 37: 387-97.
2. Gottrup F. Prevention of surgical-wound infections. N Eng J Med, 2000; 342: 202-4.
3. Bowler PG, Duerden BI, Armstrong DG. Wound microbiology and associated
approached to wound management. Clin Microbiol Rev, 2001; 14: 244-69.
4. Kirkland KB, Briggs JP, Trivette SL et al. The impact of surgical-site infections in the
1990s: attribute mortality, excess length of hospitalization, and extra costs. Infect Control
Hosp Epidemiol, 1999; 20: 725-30.
www.wjpr.net Vol 4, Issue 2, 2015. 1440
Kiran et al. World Journal of Pharmaceutical Research
5. Johnson JT, Yu VL. Role of anaerobic bacteria in postoperative wound infections
following oncologic surgery of the head and neck. Ann Otol Rhino Laryngol Suppl, 1991;
154: 46-8.
6. Zoutman D, McDonald S, Vethanayagan D. Total and attributable costs of surgical-
wound infections at a Canadian tertiary-care center. Infect Control Hosp Epidemiol,
1998; 19: 254-9.
7. Cainzos M, Lazano F, Balibrea JL, Davila D, Potel J, Gomez Alonso A et al.
Postoperative infection: multicentric, prospective and controlled study. Cir Esp, 1990;
48(5): 481-90.
8. Condon RE, Wittmann DH. The use of antibiotics in general surgery. Curr Robl Surg,
1991; 28(12): 803-907.
9. Page CP, Bohen JMA, Fletcher JR, MacManus AT, Solomkin JS, Wittmann DH.
Antimicrobial prophylaxis for surgical wounds. Guidelines of clinical care. Arch Surg,
1993; 128: 79-88.
10. Dellinger EP, Gross PA, Barrett TL, Krause PJ, Martone WJ, McGowan JE, et al. Quality
standard for antimicrobial prophylaxis in surgical procedures. Clin Infect Dis, 1994; 18:
422-7.
11. Woods RK, Dellinger EP. Current guidelines for antibiotic prophylaxis of surgical
wounds. Am Fam Physician, 1998; 58(11): 2731-40.
12. Bailey IS, Karran SE, Toyn K, Brough P, Ranaboldo C, Karran SJ. Community
surveillance of complications after hernia surgery. BMJ, 1992; 304(6825): 469-71.
13. Ranaboldo CJ, Karran SE, Bailey S, Karran SJ. Antimicrobial prophylaxis in clean
surgery: hernia repair. J Antimicrob chemother, 1993; 31: 35-41.
14. Homes J, Readman R. A study of wound infections following inguinal hernia repair. J
Hosp Infect, 1994; 28: 153-6.
www.wjpr.net Vol 4, Issue 2, 2015. 1441
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- 41 How To Cure DiseaseDocument60 pages41 How To Cure DiseaseEdie M Murgia0% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Chemotherapeutic Agents or Anti-MicrobialsDocument36 pagesChemotherapeutic Agents or Anti-MicrobialsPROF DR SHAHMURADNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Wound Care Basics: Types, Staging, Assessment & TreatmentDocument26 pagesWound Care Basics: Types, Staging, Assessment & TreatmentIntan Purnamasari100% (1)
- Surgical Site InfectionDocument14 pagesSurgical Site InfectionSri AsmawatiNo ratings yet
- Antimicrobial AgentsDocument3 pagesAntimicrobial AgentsErnie G. Bautista II, RN, MD100% (2)
- Preparation of Fortified Eye Drops: DR Sushmita G ShahDocument16 pagesPreparation of Fortified Eye Drops: DR Sushmita G Shahพานาที ลลันลาNo ratings yet
- Veterinary Drug Formulary GuideDocument245 pagesVeterinary Drug Formulary GuideAhmad Raza100% (4)
- Meropenem Drug StudyDocument2 pagesMeropenem Drug StudyPhoebe Guevarra100% (8)
- Infectious Disease GuideDocument33 pagesInfectious Disease GuideSilvia KesegNo ratings yet
- Stewardship Booklet Practical Guide To Antimicrobial Stewardship in HospitalsDocument23 pagesStewardship Booklet Practical Guide To Antimicrobial Stewardship in HospitalsZunisa Rizki100% (4)
- Mechanical Ventilation: Patient EducationDocument2 pagesMechanical Ventilation: Patient EducationAnis AidNo ratings yet
- From VAP To VAE: Establishing New Definitions For Ventilator-Associated Events in AdultsDocument22 pagesFrom VAP To VAE: Establishing New Definitions For Ventilator-Associated Events in AdultsJasleen KaurNo ratings yet
- Menu For MessDocument2 pagesMenu For MessJasleen KaurNo ratings yet
- Copd IntroDocument2 pagesCopd IntroSamuel JayNo ratings yet
- NowDocument1 pageNowJasleen KaurNo ratings yet
- ExercisesDocument4 pagesExercisesJasleen KaurNo ratings yet
- Ham A PDFDocument2 pagesHam A PDFHanum Maftukha100% (1)
- TABLE 11-1 - Compensatory Responses To Antihypertensive DrugsDocument1 pageTABLE 11-1 - Compensatory Responses To Antihypertensive DrugsJasleen KaurNo ratings yet
- Needs Assessment Questionnaire For CaregiversDocument4 pagesNeeds Assessment Questionnaire For CaregiversJasleen KaurNo ratings yet
- Total Knee Replacement Manual and Therapy/Rehab Protocol: Dr. Edward Kelly, MD, MBADocument12 pagesTotal Knee Replacement Manual and Therapy/Rehab Protocol: Dr. Edward Kelly, MD, MBAJasleen KaurNo ratings yet
- Blood Products and Their IndicationsDocument33 pagesBlood Products and Their IndicationsJasleen KaurNo ratings yet
- Role of Nurses in Triage and Disaster Preparedness: Workshop OnDocument2 pagesRole of Nurses in Triage and Disaster Preparedness: Workshop OnJasleen KaurNo ratings yet
- Table Common MedsDocument5 pagesTable Common Medsdanielc503No ratings yet
- Pulmonary Embolism: Amina Adel Al-QaysiDocument37 pagesPulmonary Embolism: Amina Adel Al-QaysiJasleen Kaur100% (2)
- Chest: Postgraduate Education CornerDocument8 pagesChest: Postgraduate Education CornerJasleen KaurNo ratings yet
- Measurement of CENTRAL VENOUS PRESSURE Via A TransducerDocument22 pagesMeasurement of CENTRAL VENOUS PRESSURE Via A TransducerJasleen KaurNo ratings yet
- 05 N044 42092Document18 pages05 N044 42092Jasleen KaurNo ratings yet
- Neocon 2017Document71 pagesNeocon 2017Jasleen KaurNo ratings yet
- 7ASTHMAPDocument10 pages7ASTHMAPErwin BawonoNo ratings yet
- Positive ETA culture and purulent secretions indicate probable VAPDocument1 pagePositive ETA culture and purulent secretions indicate probable VAPJasleen KaurNo ratings yet
- Dr. Clare Fenwick, 2010Document35 pagesDr. Clare Fenwick, 2010Jasleen KaurNo ratings yet
- CwsDocument25 pagesCwsJasleen KaurNo ratings yet
- 231Document9 pages231Jasleen KaurNo ratings yet
- The Gastrointestinal Tract and Ventilator-Associated PneumoniaDocument14 pagesThe Gastrointestinal Tract and Ventilator-Associated PneumoniaJasleen KaurNo ratings yet
- Pulmonary Embolism Is A Common and Potentially Lethal ConditionDocument13 pagesPulmonary Embolism Is A Common and Potentially Lethal ConditionJasleen KaurNo ratings yet
- YearbookDocument52 pagesYearbookJasleen KaurNo ratings yet
- Measuring Functional Progress after Hip ReplacementDocument7 pagesMeasuring Functional Progress after Hip ReplacementJasleen KaurNo ratings yet
- 7ASTHMAPDocument10 pages7ASTHMAPErwin BawonoNo ratings yet
- Ham A PDFDocument2 pagesHam A PDFHanum Maftukha100% (1)
- Augmentin in JDocument15 pagesAugmentin in JChutharat SucharitNo ratings yet
- Multiple Species: Section 2.1Document10 pagesMultiple Species: Section 2.1WormInchNo ratings yet
- DR Retno Budiarti, DR., M.Kes Microbiology Department FK UhtDocument45 pagesDR Retno Budiarti, DR., M.Kes Microbiology Department FK UhtalyaNo ratings yet
- Recommended Antibiotic Therapy in Severe Sepsis or Septic ShockDocument4 pagesRecommended Antibiotic Therapy in Severe Sepsis or Septic ShockBoy ReynaldiNo ratings yet
- NCLEX REVIEW AntibioticsDocument7 pagesNCLEX REVIEW Antibioticsneonstar100% (1)
- Antibacterial Activity of Aloe Vera Gel Against Multidrug Resistant Staphylococcus Aureus and Pseudomonas AeruginosaDocument7 pagesAntibacterial Activity of Aloe Vera Gel Against Multidrug Resistant Staphylococcus Aureus and Pseudomonas AeruginosaUMYU Journal of Microbiology Research (UJMR)100% (1)
- Careplan Week2Document2 pagesCareplan Week2api-302138606No ratings yet
- Phytoalexins PhytoanticipinsDocument3 pagesPhytoalexins PhytoanticipinsSébastien BellowNo ratings yet
- IDSA Guidelines for Managing Complicated Intra-abdominal InfectionsDocument32 pagesIDSA Guidelines for Managing Complicated Intra-abdominal InfectionsSylvain ColluraNo ratings yet
- Microbial Keratitis Royal College of OphthalmologistDocument2 pagesMicrobial Keratitis Royal College of OphthalmologistmahadianNo ratings yet
- Nama Prinsipal Kode Produk Nama Produk Unit Stok HnappnDocument4 pagesNama Prinsipal Kode Produk Nama Produk Unit Stok HnappnNoperitaNo ratings yet
- Opportunity, Challenge and Scope of Natural Products in Medicinal ChemistryDocument434 pagesOpportunity, Challenge and Scope of Natural Products in Medicinal ChemistryCamilla Karen Fernandes Carneiro100% (1)
- Antimicrobial Susceptibility Trends Among Gram-Negative Bacilli Causing Bloodstream Infections Results From The China Antimicrobial Resistance Surveillance Trial (CARST) Program, 2011-2020Document13 pagesAntimicrobial Susceptibility Trends Among Gram-Negative Bacilli Causing Bloodstream Infections Results From The China Antimicrobial Resistance Surveillance Trial (CARST) Program, 2011-2020Mrcom HvqyNo ratings yet
- Drug Information Bulletin 39 05Document4 pagesDrug Information Bulletin 39 05amritaryaaligarghNo ratings yet
- Mcqs 6Document19 pagesMcqs 6Muhammad JavedNo ratings yet
- 01.Guideline Idsa การรักษา Esbl, Cre, Mdr-psa (2021)Document44 pages01.Guideline Idsa การรักษา Esbl, Cre, Mdr-psa (2021)Nattawat TeerawattanapongNo ratings yet
- Panchagavya (Uses Benefits and Preparation)Document16 pagesPanchagavya (Uses Benefits and Preparation)Shreya VermaNo ratings yet
- MC Great Lakes SlidesDocument26 pagesMC Great Lakes Slidesapi-666654042No ratings yet
- Ous Microstrep Plus: Answers For LifeDocument2 pagesOus Microstrep Plus: Answers For LifeJimboreanu György PaulaNo ratings yet
- Cephalosporins: A Brief Overview of Their Chemistry, Mechanism of Action, and ClassificationDocument34 pagesCephalosporins: A Brief Overview of Their Chemistry, Mechanism of Action, and ClassificationTasnim sarairehNo ratings yet
- Antibiotics 1038832656Document20 pagesAntibiotics 1038832656Achilles Ok OkNo ratings yet