Professional Documents
Culture Documents
DIC Algorithm PDF
Uploaded by
Rico NovyantoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
DIC Algorithm PDF
Uploaded by
Rico NovyantoCopyright:
Available Formats
Disseminated Intravascular Coagulation Algorithm
Please review definition and pathophysiology when using the algorithm
Assess for the presence of risk factors, both major and minor or contributing:
Septicemia
Severe trauma
solid tumors and hematologic malignancies
Obstetric emergency
large aortic aneurysms or giant hemangiomas
Severe toxic or immunologic reactions (eg, transfusion reactions) or severe inflammation (eg, acute pancreatitis).
Source: http://emedicine.medscape.com/article/199627-overview#ClinicalCauses
YES NO
Are Risk
Factors
Present?
Initiate client education for Health Seeking
Behaviors:
Teach risk factors to help client identify
rationale for early medical evaluation of
Monitor for presence of signs/ symptoms: health problems to prevent the
Life-threatening hemorrhage complication of DIC
Diffuse thrombosis o Promote safety in young adult
Occult bleeding client at greatest risk for trauma
Hemodynamic instability secondary to increased risk taking
Change in mentation behavior
NO
S/s of ARDS o Encourage pregnant women to
Oliguria seek prenatal care.
Petechiae & purpura o Follow ACS recommendations to
prevent cancer
Teach s/s to report.
Are positive
findings present? Initiate the plan of care for a Risk for Ineffective
Therapeutic Regimen management:
Explain course and progression of disease to client and
family.
Discuss that DIC can be acute or chronic. And is
Potentially
frequently experienced by clients with sepsis, obstetric
unstable? Stable? emergencies and malignanc y.
Acute DIC is a medical emergency that requires critical
care intervention while chronic DIC can be managed as
an outpatient.
Follow collaborative plan of care PC:
DIC is diagnosed by evaluating the DIC score of a
Hemorrhagic shock
coagulopathy panel that includes platelets, fibrinogen,
FDP, PT/PTT, CBC, Fibrinogen
See plan of care for acute arterial thrombosis,
Acute DIC is managed through treatment of the
critical limb ischemia, acute renal failure,
underlying cause and supportive care, anticoagulants,
cardiac tamponade, intracranial hemorrhage
antithrombotics, activated protein C (APC), and
antifibrinolytics while chronic DIC is managed with
antiplatelets.
Teach client complications of disorder
Susan McCabe revised 10/1/08
Collaborative Problem
OUTCOMES/BENCHMARKS:
A & O X 3, RR 12-20, eupneic, pulse oximetry > 90-95%, lungs clear
HR: 60-100 no dysrhythmia, chest pain fee, 100 <SBP < 140, no s/s of frank or occult bleeding,
platelets > 100, PT/PTT WNL, urine output > 30 ml/hr
Potential Complication: Hemorrhagic shock/MODS secondary to DIC
ASSESS s/s of DIC: Monitor for presence of the disorder
Life-threatening hemorrhage
Diffuse thrombosis/gangrenous digits Initiate ACLS monitoring; monitor for tachypnea,
Occult bleeding hypotension, and tachycardia
Hemodynamic instability Monitor Pulse oximetry to identify desaturation, & if present
evaluate ABGs for acidosis
Change in mentation
Initiate cardiac monitoring to identify compensatory
S/s of ARDS tachycardia and dysrhythmia
Oliguria Initiate neurochecks to indentify ICH
Petechiae & purpura Mon results of coagulopathy study: Platelets < 50-100,
increased FDP, prolonged PT/PTT and decreased
Assess for high risk populations fibrinogen
Septicemia Monitor CBC for decreased Hg & HCT
Severe trauma Monitor LFTs for hepatic dysfunction
solid tumors and hematologic malignancies Monitor results of chest x-ray and echocardiography to
Obstetric emergency evaluate for ARDS, cardiac tamponade, hemothorax
large aortic aneurysms or giant Monitor CT head for hemorrhagic stroke
hemangiomas Monitor BMP for elevations in serum creatinine and
Severe toxic or immunologic reactions (eg, calculate GFR
transfusion reactions) or severe Monitor urine output >30 ml/hr
inflammation (eg, acute pancreatitis). Monitor ultrasound in obstetric client
Potential Complication: Hemorrhagic shock/MODS secondary to DIC
DO CALL
Initiate actions to promote hemostasis and prevent
thrombosis Evaluate for the presence of refractory hypoxemia,
Initiate oxygen therapy and titrate to maintain pulse oliguria, hepatic failure, worsening chest pain, neuro
oximetry >90-95% deficits, hemorrhage, hemodynamic instability and
Prepare to intubate of client develops impaired signs of MODS
consciousness and hypoxemia Initiate ACLS protocol and shock management, call the
Establish IV access & initiate fluid resuscitation ready response team and MD
Administer anticoagulation therapy according to hospital
protocol in cases with obvious thromboembolic
disease or where fibrin deposition predominates
Administer Antithrombin III IV as ordered
Administer antifibrinolytics such as amicar if ordered
Administer IV fluids and vasoactive agents as prescribed
according to results of hemodynamic monitoring
Administer PRBS & blood products as ordered & monitor
for reaction
Apply sequential TEDS as ordered
Treat the underlying cause
Antibiotics for sepsis and Drotrecogin alfa-activated
(Xigris) in severe sepsis, surgical intervention for trauma,
etcHematology consult
Performs nursing actions to minimize complications
of an exacerbation of the disorder
Initiate bleeding precautions
Implement ventilator bundle if intubated
Complications of immobility
Susan McCabe revised 10/1/08
DIC score:
Source: http://emedicine.medscape.com/article/779097-diagnosis
Does the patient have an underlying disorder (eg, sepsis, trauma, obstetric emergency)
Risk assessment
compatible with DIC?
Platelet count
Laboratory coagulation D-dimer and FDPs
tests Fibrinogen
PT and aPTT
Platelet count: >100 = 0 points, <100 = 1 point, <50 = 2 points
Elevated fibrin marker: No elevation = 0 points, moderate increase = 2 points, strong
Scoring increase = 3 points
Prolonged PT: <3 sec = 0 points, >3 <6 = 1 point, >6 = 2 points
Fibrinogen level: >1 g/L = 0 points, <1 = 1 point
Greater than or equal to 5 = compatible with overt DIC, repeat scoring daily
Calculate score
Less than 5 suggestive of non-overt DIC
Susan McCabe revised 10/1/08
You might also like
- Assessment of bleeding Shock in a Politraumatized PatientFrom EverandAssessment of bleeding Shock in a Politraumatized PatientNo ratings yet
- The Multi-Organ Donor: A Guide to Selection, Preservation and ProcurementFrom EverandThe Multi-Organ Donor: A Guide to Selection, Preservation and ProcurementRating: 5 out of 5 stars5/5 (1)
- Oncological Emergencies-2018Document8 pagesOncological Emergencies-2018CamiloRada100% (1)
- The Nurse in The Emergency Department Is Caring For A Patient With A PartialDocument13 pagesThe Nurse in The Emergency Department Is Caring For A Patient With A Partialhasan ahmdNo ratings yet
- Rds NRP 2021Document33 pagesRds NRP 2021Aiwi Goddard MurilloNo ratings yet
- Uncovering an Uncommon Cause of PsychosisDocument2 pagesUncovering an Uncommon Cause of PsychosissavinaumarNo ratings yet
- Intraoperative Fluid ManagementDocument23 pagesIntraoperative Fluid ManagementMirela Marina BlajNo ratings yet
- Pain Management in Critically Ill Patient: Prof. Dr. Andi Husni Tanra, PHD, SP - An-Kic-KmnDocument42 pagesPain Management in Critically Ill Patient: Prof. Dr. Andi Husni Tanra, PHD, SP - An-Kic-KmnReza Prakosa Sedyatama100% (1)
- Presentation SWINE FLUDocument40 pagesPresentation SWINE FLUdr_hammadNo ratings yet
- Breast Cancer Medical Surgical NursingDocument5 pagesBreast Cancer Medical Surgical NursingKath RubioNo ratings yet
- Chapter 6 Cancer PrepU QuestionsDocument7 pagesChapter 6 Cancer PrepU QuestionsKevin ClarkNo ratings yet
- Neonatal ResuscitationDocument7 pagesNeonatal ResuscitationJavier López García100% (1)
- Lip Cancer-Ablative and Reconstructive Surgery: ChapDocument52 pagesLip Cancer-Ablative and Reconstructive Surgery: ChapYang Lin Chen100% (1)
- Dhanusthamba/Dhanurvata/Tetanus: Dr. Mahesh C KundagolDocument19 pagesDhanusthamba/Dhanurvata/Tetanus: Dr. Mahesh C KundagolkundagolNo ratings yet
- Early Emergency Care ProceduresDocument53 pagesEarly Emergency Care ProceduresDwi ayu oktaveni100% (1)
- Guide to the Intercollegiate MRCS ExaminationDocument55 pagesGuide to the Intercollegiate MRCS ExaminationjuweriyNo ratings yet
- Job Description of A Nurse AnesthetistDocument3 pagesJob Description of A Nurse AnesthetistlhalamNo ratings yet
- Surgery 2012Document28 pagesSurgery 2012max_21ruNo ratings yet
- Emergency NursingDocument5 pagesEmergency Nursingchelljynxie100% (2)
- Introduction To PALLIATIVE CAREDocument73 pagesIntroduction To PALLIATIVE CARERajesh T Eapen100% (1)
- Pediatric Assessment Physical ExamDocument9 pagesPediatric Assessment Physical ExamBea SamonteNo ratings yet
- Trauma McqsDocument12 pagesTrauma Mcqschanaish6100% (1)
- Initial Assessment and Management of Multiply Injured PatientsDocument30 pagesInitial Assessment and Management of Multiply Injured PatientsSikaNo ratings yet
- Managing Diphtheria Cases and OutbreaksDocument11 pagesManaging Diphtheria Cases and Outbreaksbrigde_xNo ratings yet
- Dr. Anad's Guide to Urosepsis: Causes, Symptoms and TreatmentDocument23 pagesDr. Anad's Guide to Urosepsis: Causes, Symptoms and TreatmentJihad Anad100% (1)
- Seizures in Children JULIO 2020Document29 pagesSeizures in Children JULIO 2020Elizabeth HendersonNo ratings yet
- Emergence Delirium in Pediatric Patients: Recognition, Prevention and TreatmentDocument34 pagesEmergence Delirium in Pediatric Patients: Recognition, Prevention and TreatmentMorad SatariNo ratings yet
- Hepatobiliary DiseaseDocument52 pagesHepatobiliary DiseaseMelissa Laurenshia ThenataNo ratings yet
- Emergency Document For UHDocument16 pagesEmergency Document For UHShahidul Islam ChowdhuryNo ratings yet
- Normal Laboratory Values With Nursing Consideration - UsnganDocument8 pagesNormal Laboratory Values With Nursing Consideration - UsnganPrincess Nasima M. UsnganNo ratings yet
- Critical Care Nursing Responsibilities and SkillsDocument47 pagesCritical Care Nursing Responsibilities and SkillsAamirNo ratings yet
- Trauma Protocol Manual Final 2012 WordDocument250 pagesTrauma Protocol Manual Final 2012 WordelaNo ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document24 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)hendra2darmawanNo ratings yet
- JWC Convatec Wound-Hygiene-28pp 14-Feb CA Web-LicDocument28 pagesJWC Convatec Wound-Hygiene-28pp 14-Feb CA Web-LicAjeng Kania100% (1)
- Thyroid Function Tests ExplainedDocument25 pagesThyroid Function Tests ExplainedEva SinghNo ratings yet
- Surgical Principles From MbbsBasicDocument47 pagesSurgical Principles From MbbsBasicbasic100% (5)
- PICU Common ProblemDocument49 pagesPICU Common ProblemRawabi rawabi1997No ratings yet
- Haramaya University College of Health and Medical Sciences School of Nursing and Midwifery MSC in Nursing (Major in Adult Health Nursing)Document54 pagesHaramaya University College of Health and Medical Sciences School of Nursing and Midwifery MSC in Nursing (Major in Adult Health Nursing)Beyene Feleke100% (1)
- Csbpr7 Acute Stroke Management Module Final Eng 2022Document161 pagesCsbpr7 Acute Stroke Management Module Final Eng 2022Vigneshwara NagarajanNo ratings yet
- Prioritizing patients in the emergency departmentDocument27 pagesPrioritizing patients in the emergency departmentSoleh RamlyNo ratings yet
- Neck Trauma LecDocument49 pagesNeck Trauma Lecapi-3743483100% (2)
- Wound International Best Practice Guidelines Non ComplexDocument27 pagesWound International Best Practice Guidelines Non ComplexEdu WilliamNo ratings yet
- 1 Perspectives of Pediatric NursingDocument57 pages1 Perspectives of Pediatric NursingBluebloodboyNo ratings yet
- DiphtheriaDocument49 pagesDiphtheriasultanNo ratings yet
- Nsg241 Study Guide Exam 5Document76 pagesNsg241 Study Guide Exam 5NatalieAndersonNo ratings yet
- Nasopharyngeal CarcinomaDocument44 pagesNasopharyngeal CarcinomapopoyingNo ratings yet
- Hospital ICU Organization and TypesDocument82 pagesHospital ICU Organization and TypesPaul Shan GoNo ratings yet
- JBI - Wound ManagementDocument4 pagesJBI - Wound ManagementBethanyNo ratings yet
- Head Trauma: Will/Grundy EMS 2009 2 Trimester May CMEDocument100 pagesHead Trauma: Will/Grundy EMS 2009 2 Trimester May CMESytrose Morales100% (1)
- Ear, Nose, and Throat EmergenciesDocument23 pagesEar, Nose, and Throat EmergenciesRajesh SharmaNo ratings yet
- Peadiatric Brain Tumour: Wong Ann Cheng MD (Ukm) MRCPCH (Uk)Document48 pagesPeadiatric Brain Tumour: Wong Ann Cheng MD (Ukm) MRCPCH (Uk)An Zheng100% (4)
- MRCPCH q15Document30 pagesMRCPCH q15Galaleldin AliNo ratings yet
- Special Circumstances GuidelinesDocument19 pagesSpecial Circumstances GuidelinesRayNo ratings yet
- Initial Assessment and Management: Presented by Fayez Abillama, MDDocument53 pagesInitial Assessment and Management: Presented by Fayez Abillama, MDDaniel GhosseinNo ratings yet
- Renal System Examination OSCE GuideDocument23 pagesRenal System Examination OSCE GuideBasem Fuad MohammadNo ratings yet
- Causes and Symptoms of PeritonitisDocument33 pagesCauses and Symptoms of PeritonitisnurulamaliahnutNo ratings yet
- Tumours of The Central Nervous System: FM Brett MD., FrcpathDocument57 pagesTumours of The Central Nervous System: FM Brett MD., FrcpathDrGasnasNo ratings yet
- Pathophysiology of Varicose Vein - Chronic Venous InsufficiencyDocument31 pagesPathophysiology of Varicose Vein - Chronic Venous InsufficiencyDavid Christian100% (1)
- Hypertension Annals of Internal Medicine 2014Document16 pagesHypertension Annals of Internal Medicine 2014jhazpeitiaNo ratings yet
- Cad Fullguideline 510127Document8 pagesCad Fullguideline 510127Ana MariaNo ratings yet
- Tendon Gliding Exercises HandDocument1 pageTendon Gliding Exercises HandRico NovyantoNo ratings yet
- DR Sarah Hearnshaw - Early Management of The Patient With Acute GI BleedingDocument38 pagesDR Sarah Hearnshaw - Early Management of The Patient With Acute GI BleedingRico NovyantoNo ratings yet
- 1957 6954 1 PBDocument9 pages1957 6954 1 PBsega prirahmadanNo ratings yet
- PremetrexedDocument12 pagesPremetrexedRico NovyantoNo ratings yet
- Sirkulasi A - H - ADocument31 pagesSirkulasi A - H - ARico NovyantoNo ratings yet
- Blood-Pressure Chart PDFDocument1 pageBlood-Pressure Chart PDFayaskantkNo ratings yet
- Sirkulasi A - H - ADocument31 pagesSirkulasi A - H - ARico NovyantoNo ratings yet
- 1957 6954 1 PBDocument9 pages1957 6954 1 PBsega prirahmadanNo ratings yet
- Diagnostic Study Appraisal Worksheet PDFDocument3 pagesDiagnostic Study Appraisal Worksheet PDFdian_c87No ratings yet
- Blood-Pressure Chart PDFDocument1 pageBlood-Pressure Chart PDFayaskantkNo ratings yet
- ApacheIII RiskScoreCard AZDocument1 pageApacheIII RiskScoreCard AZRico NovyantoNo ratings yet
- ApacheIII RiskScoreCard AZDocument1 pageApacheIII RiskScoreCard AZRico NovyantoNo ratings yet
- ApacheIII RiskScoreCard AZDocument1 pageApacheIII RiskScoreCard AZRico NovyantoNo ratings yet
- ApacheIII RiskScoreCard AZDocument1 pageApacheIII RiskScoreCard AZRico NovyantoNo ratings yet
- ApacheIII RiskScoreCard AZDocument1 pageApacheIII RiskScoreCard AZRico NovyantoNo ratings yet
- Jamaica's Unemployment Aims, Causes and SolutionsDocument23 pagesJamaica's Unemployment Aims, Causes and Solutionsnetzii300067% (3)
- Hi Tracy: Total Due Here's Your Bill For JanuaryDocument6 pagesHi Tracy: Total Due Here's Your Bill For JanuaryalexNo ratings yet
- Redminote5 Invoice PDFDocument1 pageRedminote5 Invoice PDFvelmurug_balaNo ratings yet
- Concepts of Cavity Prep PDFDocument92 pagesConcepts of Cavity Prep PDFChaithra Shree0% (1)
- Dwnload Full Fundamentals of Human Neuropsychology 7th Edition Kolb Test Bank PDFDocument12 pagesDwnload Full Fundamentals of Human Neuropsychology 7th Edition Kolb Test Bank PDFprindivillemaloriefx100% (12)
- People V Gona Phil 54 Phil 605Document1 pagePeople V Gona Phil 54 Phil 605Carly GraceNo ratings yet
- A Business Development PlanDocument90 pagesA Business Development PlanRishabh Sarawagi100% (1)
- Soal Ulangan Harian Smester 1 Kelas 8 SMP BAHASA INGGRISDocument59 pagesSoal Ulangan Harian Smester 1 Kelas 8 SMP BAHASA INGGRISsdn6waykhilauNo ratings yet
- The Experience of God Being Consciousness BlissDocument376 pagesThe Experience of God Being Consciousness BlissVivian Hyppolito100% (6)
- Lauritzen 1964Document10 pagesLauritzen 1964Priyanka GandhiNo ratings yet
- Residential Water Piping Installation GuideDocument28 pagesResidential Water Piping Installation GuideMunir RasheedNo ratings yet
- Kasapreko PLC Prospectus November 2023Document189 pagesKasapreko PLC Prospectus November 2023kofiatisu0000No ratings yet
- Safe Handling of Solid Ammonium Nitrate: Recommendations For The Environmental Management of Commercial ExplosivesDocument48 pagesSafe Handling of Solid Ammonium Nitrate: Recommendations For The Environmental Management of Commercial ExplosivesCuesta AndresNo ratings yet
- TarotDocument21 pagesTarotKrystal Jacquot100% (2)
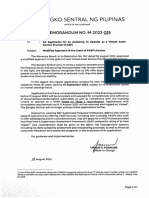
- BSP Memorandum No. M-2022-035Document1 pageBSP Memorandum No. M-2022-035Gleim Brean EranNo ratings yet
- Biochemical Aspect of DiarrheaDocument17 pagesBiochemical Aspect of DiarrheaLiz Espinosa0% (1)
- Madagascar's Unique Wildlife in DangerDocument2 pagesMadagascar's Unique Wildlife in DangerfranciscogarridoNo ratings yet
- Dislocating The Sign: Toward A Translocal Feminist Politics of TranslationDocument8 pagesDislocating The Sign: Toward A Translocal Feminist Politics of TranslationArlene RicoldiNo ratings yet
- 6 Holly Fashion Case StudyDocument3 pages6 Holly Fashion Case StudyCaramalau Mirela-Georgiana0% (1)
- Orbit BioscientificDocument2 pagesOrbit BioscientificSales Nandi PrintsNo ratings yet
- American Buffalo - DAVID MAMETDocument100 pagesAmerican Buffalo - DAVID MAMETRodrigo Garcia Sanchez100% (10)
- Factors of Cloud ComputingDocument19 pagesFactors of Cloud ComputingAdarsh TiwariNo ratings yet
- Review For Development of Hydraulic Excavator Attachment: YANG Cheng Huang Kui LI Yinwu WANG Jingchun ZHOU MengDocument5 pagesReview For Development of Hydraulic Excavator Attachment: YANG Cheng Huang Kui LI Yinwu WANG Jingchun ZHOU MengZuhaib ShaikhNo ratings yet
- Method Statement For Wall Panels InstallationDocument11 pagesMethod Statement For Wall Panels InstallationChristos LoutrakisNo ratings yet
- Promotion From Associate Professor To ProfessorDocument21 pagesPromotion From Associate Professor To ProfessorKamal KishoreNo ratings yet
- ExpressionismDocument16 pagesExpressionismRubab ChaudharyNo ratings yet
- Ass. No.1 in P.E.Document8 pagesAss. No.1 in P.E.Jessa GNo ratings yet
- Geller (LonginusRhetoric'sCure)Document27 pagesGeller (LonginusRhetoric'sCure)Miguel AntónioNo ratings yet
- Text Detection and Recognition in Raw Image Dataset of Seven Segment Digital Energy Meter DisplayDocument11 pagesText Detection and Recognition in Raw Image Dataset of Seven Segment Digital Energy Meter DisplaykkarthiksNo ratings yet
- Assessment: Bipolar DisorderDocument2 pagesAssessment: Bipolar DisorderMirjana StevanovicNo ratings yet