Professional Documents
Culture Documents
Managing Acute Behavioural Disturbance
Uploaded by
StudentOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Managing Acute Behavioural Disturbance
Uploaded by
StudentCopyright:
Available Formats
Dr Diane Mullins, RCSI Tutor in Psychiatry, St Itas Hospital, Portrane
Management of an acutely aggressive patient / management of behaviourally
disturbed patient
****see algorithm page entitled management of acute behavioural disturbance and
include all of the information on that page****
Acute behavioural disturbance may occur secondary to
1. Substance misuse (both intoxication and withdrawal),
2. Physical illness (such as post head injury, hypoglycaemia)
3. Psychiatric conditions (including psychotic and personality disorders)
The aims of rapid tranquillisation
1. To reduce further suffering for the patient: psychological and physical (through
self-harm or accidents)
2. To reduce the risk of harm to others
3. To do no harm (by prescribing safe regimes and monitoring physical health)
Rapid tranquillisation preliminary steps
1. Endeavour to establish the underlying diagnosis behind the acute behavioural
disturbance before making any treatment decision
2. Allow a period of de-escalation see below
3. Only when de-escalation has failed to curb the disturbed behaviour should
medication be considered
De-escalation techniques
One staff member should assume control of a disturbed/violent situation
The staff member who has taken control should:
o Remove other patients from the area, enlist the help of colleagues
o Give clear, brief, assertive instructions to the patient and others in the vicinity
o Move towards a safe place and avoid being trapped in a corner
o Attempt to establish rapport and emphasise cooperation
o Ask open questions and inquire about the reason for the anger
o Show concern and attentiveness through non-verbal and verbal responses
o Listen carefully and show empathy, acknowledging any concerns
o Appear calm, self-controlled and confident
o Ask for any weapons to be placed in a neutral location rather than handed over
o Consider asking the patient to make use of the designated area or room
specifically for the purpose of reducing arousal and/or agitation to help them
calm down
Other items which should be done
Consult Senior Colleague
Review chart for any previous reactions to antipsychotics/sedatives
Ensure appropriate resuscitation equipment available
Review legal status (i.e. Mental Health Act or voluntary patient?)
Incident reporting and post-incident reviews
Any incident requiring rapid tranquillisation, physical intervention or seclusion
should be recorded
A post-incident review should take place as soon after the incident as possible, but
in any event within 72 hours of the incident ending
You might also like
- Psychological Profile of Jeffrey DahmerDocument3 pagesPsychological Profile of Jeffrey Dahmerautry31891% (11)
- Kernberg & Yeomans (2013)Document23 pagesKernberg & Yeomans (2013)Julián Alberto Muñoz FigueroaNo ratings yet
- Psychiatry Lecturio Summary2Document39 pagesPsychiatry Lecturio Summary2Raymond Lorenzo N. RacelaNo ratings yet
- Case Analysis Case Study HelgaDocument10 pagesCase Analysis Case Study Helgaapi-487413988No ratings yet
- Psychiatric Nursing HesiDocument6 pagesPsychiatric Nursing HesiKarla Lopez91% (11)
- Understanding Girls With ADHD: How They Feel and Why They Do What They Do - Kathleen NadeauDocument5 pagesUnderstanding Girls With ADHD: How They Feel and Why They Do What They Do - Kathleen NadeauryhyjutaNo ratings yet
- HESI Study Guide Psychiatric NursingDocument26 pagesHESI Study Guide Psychiatric NursingDean Winchester100% (4)
- Mental Health Triage Tool 2006Document1 pageMental Health Triage Tool 2006MelbourneFXNo ratings yet
- Schizophrenia Care Plan RNDocument8 pagesSchizophrenia Care Plan RNlisa75% (4)
- Hesi Psych Study GuideDocument16 pagesHesi Psych Study GuideR100% (17)
- Triage Assessment of Psychiatric Patient LectureDocument31 pagesTriage Assessment of Psychiatric Patient Lectureهشام عفانه100% (1)
- Substance Abuse Assessment, Diagnosis, and Initial Treatment Planning For Behavioral Health CliniciansDocument28 pagesSubstance Abuse Assessment, Diagnosis, and Initial Treatment Planning For Behavioral Health Clinicianseuronetit100% (1)
- Psychiatry Under Communist Dictatorship in RomaniaDocument418 pagesPsychiatry Under Communist Dictatorship in RomaniaargatuNo ratings yet
- Surgical Ho Guide PDFDocument76 pagesSurgical Ho Guide PDFMardiana KamalNo ratings yet
- Restraint Use and Patient Care: Nnual CompetencyDocument35 pagesRestraint Use and Patient Care: Nnual CompetencyrustiejadeNo ratings yet
- Rating ScalesDocument4 pagesRating Scalesnkivc100% (3)
- Anatomy VivaDocument126 pagesAnatomy VivaBayar A. AhmedNo ratings yet
- De-escalation and crisis intervention techniquesDocument5 pagesDe-escalation and crisis intervention techniquesJae DeeNo ratings yet
- Therapeutic ModalitiesDocument45 pagesTherapeutic ModalitiesShara Sampang100% (5)
- Psychiatric EmergenciesDocument10 pagesPsychiatric EmergenciesUdaya Sree100% (1)
- 4 - PsychoeducationDocument19 pages4 - PsychoeducationMuhammad AwaisNo ratings yet
- Andre Tan's Surgical NotesDocument163 pagesAndre Tan's Surgical NotesHani Nadiah75% (4)
- INTRODUCTION TO DIAGNOSTIC IMAGINGaDocument77 pagesINTRODUCTION TO DIAGNOSTIC IMAGINGaStudentNo ratings yet
- The Effectiveness of Psychodynamic Psychotherapies - An Update (2015) PDFDocument14 pagesThe Effectiveness of Psychodynamic Psychotherapies - An Update (2015) PDFmysticmdNo ratings yet
- HESI PsyDocument16 pagesHESI PsyKrista Howe100% (13)
- Rights of Mental Patients and Types of AdmissionDocument31 pagesRights of Mental Patients and Types of Admissioncasandra moranteNo ratings yet
- EMERGENCY NURSING CAREDocument110 pagesEMERGENCY NURSING CAREHarley Justiniani Dela CruzNo ratings yet
- Multiscale Dissociation Inventory (MDI)Document2 pagesMultiscale Dissociation Inventory (MDI)Gabriela Marc20% (5)
- Mental Health Nursing II NURS 2310: Unit 1 Basic Concepts of Mental Health and Mental IllnessDocument41 pagesMental Health Nursing II NURS 2310: Unit 1 Basic Concepts of Mental Health and Mental IllnessRocky Domingo LazaroNo ratings yet
- ABDOMINAL RADIOGRAPHS INTERPRETATION GUIDEDocument108 pagesABDOMINAL RADIOGRAPHS INTERPRETATION GUIDEStudent100% (1)
- Restraining Procedure: General Principles For Use of RestraintsDocument10 pagesRestraining Procedure: General Principles For Use of RestraintsHardeep KaurNo ratings yet
- Introduction to Hypnosis - The Powerful Support for Your Life: How Hypnosis Can Change your Life: Happiness, Health, Self-ConfidenceFrom EverandIntroduction to Hypnosis - The Powerful Support for Your Life: How Hypnosis Can Change your Life: Happiness, Health, Self-ConfidenceNo ratings yet
- What Happens During Drug Rehab? The Information You Need to Help Yourself or Someone You LoveFrom EverandWhat Happens During Drug Rehab? The Information You Need to Help Yourself or Someone You LoveNo ratings yet
- Restraints and Seclusion Copy-1Document47 pagesRestraints and Seclusion Copy-1غيداء الذويبيNo ratings yet
- Pyschiatric NursingDocument40 pagesPyschiatric Nursingtheglobalnursing100% (1)
- Mental Health Nursing II NURS 2310Document41 pagesMental Health Nursing II NURS 2310adni_wgNo ratings yet
- Psychiatric NoteDocument5 pagesPsychiatric Notemahmoudmustapha93No ratings yet
- Definitions of Mental Health: Psych NotesDocument5 pagesDefinitions of Mental Health: Psych NotesSharon TanveerNo ratings yet
- AgressionDocument35 pagesAgressionnamah odatNo ratings yet
- Milieutherapy 120106134352 Phpapp01Document16 pagesMilieutherapy 120106134352 Phpapp01Jocelle SalamilaoNo ratings yet
- Session 19 Psychiatric EmergenciesDocument59 pagesSession 19 Psychiatric EmergenciesMalakatete Mwaipojele-fNo ratings yet
- Mala EmergencyDocument9 pagesMala EmergencymalathiNo ratings yet
- A Basic Approach To A Patient With A Psychiatric Problem - Jullian Nasti FinalDocument3 pagesA Basic Approach To A Patient With A Psychiatric Problem - Jullian Nasti FinaltnsourceNo ratings yet
- Psychiatric Emergencies 2Document27 pagesPsychiatric Emergencies 2Lulano MbasuNo ratings yet
- Psychological Considerations in General Health CareDocument2 pagesPsychological Considerations in General Health CaremiNo ratings yet
- Dokumen - Tips - Psychiatric Emergencies 1Document108 pagesDokumen - Tips - Psychiatric Emergencies 1RahelAdmasuNo ratings yet
- Acute Behavioural Disturbance (ABD) in ED: Mohammed Aneez SPR Ed Wexham Park HospitalDocument23 pagesAcute Behavioural Disturbance (ABD) in ED: Mohammed Aneez SPR Ed Wexham Park HospitalAneez MohamedNo ratings yet
- Case PresentationDocument19 pagesCase PresentationforraalNo ratings yet
- S E L F - P E R C E P T I O N - S E L F - C O N C E P T P A T T E R A. 1Document4 pagesS E L F - P E R C E P T I O N - S E L F - C O N C E P T P A T T E R A. 1Diana TardecillaNo ratings yet
- Unit 7 Therapies Used in PsychiatryDocument26 pagesUnit 7 Therapies Used in PsychiatryIsha BhusalNo ratings yet
- Module 2 Mental HealthDocument8 pagesModule 2 Mental HealthViolet CrimsonNo ratings yet
- Characteristics of a Good First AiderDocument6 pagesCharacteristics of a Good First Aiderlennahfe19No ratings yet
- 35 Protocol Pharmacologikal Treatment PDFDocument35 pages35 Protocol Pharmacologikal Treatment PDFdragutinpetric100% (1)
- MH - CBT and Anxiety May05Document8 pagesMH - CBT and Anxiety May05sylvan_williamsNo ratings yet
- Laporan Pendahuluan Pada Pasien HalusinasiDocument9 pagesLaporan Pendahuluan Pada Pasien HalusinasiAemaTz Fsa HusbandnuashafaselamanyaNo ratings yet
- Classical ConditioningDocument7 pagesClassical ConditioningCHIOMA AGUHNo ratings yet
- Aggressive Behaviors - ExtendedDocument7 pagesAggressive Behaviors - ExtendedTeresa SilvaNo ratings yet
- Psych Lec Rle 20230216Document4 pagesPsych Lec Rle 20230216Aly ArlosNo ratings yet
- Ethics in ResuscitationDocument26 pagesEthics in ResuscitationSuresh NaiduNo ratings yet
- Social Pharmacy Notes - 1Document5 pagesSocial Pharmacy Notes - 1Gerald Limo Arap ChebiiNo ratings yet
- Psychological First Aid GuideDocument44 pagesPsychological First Aid GuideIvygrace Ampodia-SanicoNo ratings yet
- Psyche NotesDocument41 pagesPsyche Notesjadagayle 825No ratings yet
- Lesson 7 Crs3Document20 pagesLesson 7 Crs3Francis Kyle SalesNo ratings yet
- Ethical Issues in Psychological Research and TreatmentDocument3 pagesEthical Issues in Psychological Research and Treatmentquality assuranceNo ratings yet
- Ati Funds ReviewDocument11 pagesAti Funds Reviewmrsfelic08No ratings yet
- Basic First Aid Techniques DOC From ISKCONDocument27 pagesBasic First Aid Techniques DOC From ISKCONKrishna DasNo ratings yet
- KPJ Presentation (Psychiatry Training)Document20 pagesKPJ Presentation (Psychiatry Training)Dr Puteri Nur Sabrina Binti Mohd HanapiNo ratings yet
- DNR or End of Life Care DecisionsDocument20 pagesDNR or End of Life Care DecisionsAllessandria Daphne Sac BagacinaNo ratings yet
- Psychiatric EmergenciesDocument10 pagesPsychiatric EmergenciesPoonam RanaNo ratings yet
- Psychiatric Health Law and EthicsDocument38 pagesPsychiatric Health Law and EthicsMichael S. PetryNo ratings yet
- Management of AgitationDocument8 pagesManagement of AgitationMahmoud Ahmed MahmoudNo ratings yet
- Adjustment Disorder (Including Acute Stress Reaction) : Presenting ComplaintsDocument4 pagesAdjustment Disorder (Including Acute Stress Reaction) : Presenting ComplaintsAprilihardini LaksmiNo ratings yet
- Seclusion and Physical Restraint: GeneralDocument6 pagesSeclusion and Physical Restraint: GeneralMegan ClearyNo ratings yet
- Tardive DyskinesiaDocument2 pagesTardive DyskinesiaStudentNo ratings yet
- Tricyclic Antidepressants: Indications, Side Effects & CautionsDocument1 pageTricyclic Antidepressants: Indications, Side Effects & CautionsStudentNo ratings yet
- Assessment of DSH & Suicide RiskDocument2 pagesAssessment of DSH & Suicide RiskStudentNo ratings yet
- Suicide Rate Trends by Gender: Irish National Suicide Mortality DataDocument1 pageSuicide Rate Trends by Gender: Irish National Suicide Mortality DataStudentNo ratings yet
- AutismDocument3 pagesAutismkylieverNo ratings yet
- On Line Lecture - Risk Assessment in PsychiatryDocument52 pagesOn Line Lecture - Risk Assessment in PsychiatryStudentNo ratings yet
- Breaking Patient ConfidentialityDocument1 pageBreaking Patient ConfidentialityStudentNo ratings yet
- Ect NotesDocument3 pagesEct NotesStudentNo ratings yet
- Capacity To ConsentDocument1 pageCapacity To ConsentStudentNo ratings yet
- Diagnosis of DementiaDocument3 pagesDiagnosis of DementiaStudentNo ratings yet
- CBTDocument2 pagesCBTStudentNo ratings yet
- ClozapineDocument2 pagesClozapineStudentNo ratings yet
- Drugs Psychosis - ReviewDocument16 pagesDrugs Psychosis - ReviewStudentNo ratings yet
- Malaysian Guidelines in Treatment of STIDocument105 pagesMalaysian Guidelines in Treatment of STIMrchip Muhammad Faiz NasirNo ratings yet
- Why Does My Child Needs HPV Vaccination?Document2 pagesWhy Does My Child Needs HPV Vaccination?StudentNo ratings yet
- Final Surgical Long Case Collection by Classof2016 PMCDocument32 pagesFinal Surgical Long Case Collection by Classof2016 PMCStudentNo ratings yet
- Safe and Unsafe TouchDocument26 pagesSafe and Unsafe TouchStudentNo ratings yet
- Neuro PacesDocument138 pagesNeuro PacesStudentNo ratings yet
- References: Scientific Background (Part 1)Document2 pagesReferences: Scientific Background (Part 1)StudentNo ratings yet
- Management of Hypertension: Clinical Practice GuidelinesDocument96 pagesManagement of Hypertension: Clinical Practice GuidelinesamirunNo ratings yet
- Occipital NeuralgiaDocument12 pagesOccipital NeuralgiaStudentNo ratings yet
- Case On Cutaneous WoundDocument4 pagesCase On Cutaneous WoundStudentNo ratings yet
- Shsortho Essentials1Document9 pagesShsortho Essentials1kristinNo ratings yet
- PHQ 9 en FRDocument3 pagesPHQ 9 en FRZICONo ratings yet
- KADS-11 Scale for Assessing Adolescent DepressionDocument3 pagesKADS-11 Scale for Assessing Adolescent DepressionNelly Q. NisaNo ratings yet
- 7718 (08) Review of Cases - Somatoform DisordersDocument48 pages7718 (08) Review of Cases - Somatoform DisordersnewazNo ratings yet
- Behavioral Disorders in Children...Document3 pagesBehavioral Disorders in Children...Abhishek1789No ratings yet
- Psychological Dynamics of Self-Injury Actors StudyDocument10 pagesPsychological Dynamics of Self-Injury Actors StudyRini DewiNo ratings yet
- Psych QuizDocument3 pagesPsych QuizRoderick AgbuyaNo ratings yet
- Understanding Psychotic DisordersDocument41 pagesUnderstanding Psychotic DisordersFan Eli100% (1)
- Personality Disorders: 4 Core Defining FeaturesDocument2 pagesPersonality Disorders: 4 Core Defining FeaturesYet ConcepcionNo ratings yet
- Link Between Salvador Dali's Artistic Creativity and PsychopathologyDocument10 pagesLink Between Salvador Dali's Artistic Creativity and PsychopathologyOmme Hani Alizadeh Sahraei100% (1)
- Types of Stress: The Counseling Team InternationalDocument1 pageTypes of Stress: The Counseling Team InternationalashokNo ratings yet
- Schizoaffective With Bipolar DisordersDocument14 pagesSchizoaffective With Bipolar DisordersNaomi MasudaNo ratings yet
- Case Vignette Assignment 3Document2 pagesCase Vignette Assignment 3mysteryvan19810% (1)
- Running Head: CASE STUDY 1Document18 pagesRunning Head: CASE STUDY 1Jhobz Salmorin MamengNo ratings yet
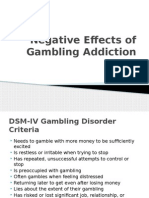
- Gambling Addiction PowerpointDocument11 pagesGambling Addiction PowerpointEK200620No ratings yet
- Relationship Between Anxiety and Addiction To A Depressant DrugDocument7 pagesRelationship Between Anxiety and Addiction To A Depressant DrugRian YupitaNo ratings yet
- Adjustment DisorderDocument7 pagesAdjustment DisorderRif'aNo ratings yet
- Bipolar Brochure English FINAL 150109 PDFDocument9 pagesBipolar Brochure English FINAL 150109 PDFIka M. HendrajayaNo ratings yet
- Girl Interrupted Book ReviewDocument7 pagesGirl Interrupted Book Reviewapi-348337992No ratings yet
- Concept PaperDocument11 pagesConcept PaperSun ShineNo ratings yet
- Gambling Addiction Among Adolescents 2375 4494 1000e121Document2 pagesGambling Addiction Among Adolescents 2375 4494 1000e121merin sunilNo ratings yet