Professional Documents
Culture Documents
Jurnal Mata 4
Uploaded by
randy_27995Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jurnal Mata 4
Uploaded by
randy_27995Copyright:
Available Formats
PERSPECTIVE
Avoidance, Recognition, and Management of
LASIK Complications
STEVEN C. SCHALLHORN, MD, ERIC C. AMESBURY, MD, AND DAVID J. TANZER, MD
PURPOSE: To provide important concepts of the latest LASIK complications, the prompt recognition of complica-
developments in laser in situ keratomileusis (LASIK) tions when they occur, and their management will be
complication avoidance, recognition, and management. discussed in four categories as shown in the Table.
DESIGN: A perspective.
METHODS: A comprehensive literature search and re- KERATOME AND FLAP COMPLICATIONS: A mechani-
view of a total of 816 publications that discussed LASIK cal keratome or femtosecond laser can be used to create the
complications from 1992 to 2005 was conducted. LASIK flap. Although femtosecond laser use for LASIK flaps
RESULTS: The risk of visually threatening complica- is a newer technology, it is known that miscreated flaps, flap
tions is inherent in any ophthalmologic surgical proce- striae, interface inflammation, traumatic flap tears with initial
dure. Not only does LASIK require the use of several flap lift, loss of suction, and epithelial defects are some
complex medical devices, but there can be significant possible complications. Recent reports suggest that creating a
human variation in response to this surgical intervention. flap with a femtosecond laser, with careful surgical technique
As a result, many potential complications can occur after to avoid trauma during flap lift, may offer advantages such as
LASIK. The risk of many complications can be mitigated comparable attained spheric equivalent and acuity, with less
by appropriate patient selection and preoperative, surgi- induced astigmatism and better flap thickness predictability
cal, and postoperative care. Unforeseen complications when compared with mechanical keratomes.1 Further inves-
will occur, despite meticulous planning, and must be tigation is needed to understand the complications that are
managed. Important current developments in the avoid- specific to the femtosecond flaps that could be expected
ance, recognition, and management of LASIK complica- commonly and the effective management strategies.
tions are reviewed.
CONCLUSIONS: Complications as a result of LASIK INTRAOPERATIVE COMPLICATIONS: Complications
can threaten vision and may cause debilitating symptoms during LASIK that are specific to the mechanical keratome
in an otherwise healthy eye. Advancing our understand- include free flaps, thin flaps, incomplete flaps, flap button-
ing of the prevention and management of the complica- holes, flap decentration, and epithelial defects. The total
tions of LASIK is an endeavor that must be continued as incidence of all intraoperative LASIK flap complications that
long as refractive surgery is performed. (Am J Oph- have been published in studies of 1000 eyes ranges from
thalmol 2006;141:733739. 2006 by Elsevier Inc. All 0.3% to 5.7%. A learning curve exists for the beginning
rights reserved.) LASIK surgeon, and experience decreases the incidence of
keratome-related complications.2 The surgical team must
B
ECAUSE LASER IN SITU KERATOMILEUSIS (LASIK) RE- have thorough knowledge of the specific operating procedures
quires the use of several complex medical devices and for the keratome that is being used. Careful examination and
there can be significant human variation in response testing of all equipment before commencing surgery are
to surgical intervention, many potential complications can essential to avoid an intraoperative surprise. The surgeon
occur. The most current concepts in avoidance of common should evaluate the flap immediately after cutting and before
laser ablation to ensure a consistent thickness, an intact
Accepted for publication Nov 21, 2005. hinge, good centration, and adequate diameter and should
From the Department of Ophthalmology, Naval Medical Center, San
Diego, California (S.C.S., D.J.T.); Department of Ophthalmology, Naval identify any epithelial defects or other potential issues that
Hospital, Great Lakes, Illinois (E.C.A.). may affect healing.
Inquiries to Steven C. Schallhorn, MD, Captain, Medical Corps, USN, A flap that lacks a hinge that attaches it to the cornea is
Department of Ophthalmology, Naval Medical Center, San Diego, 34800
Bob Wilson Dr, San Diego, CA 92134; e-mail: SCSchallhorn@nmcsd. known as a free flap or cap. Loss of suction during the
med.navy.mil keratome pass can cause shallow engagement of the keratome
0002-9394/06/$32.00 2006 BY ELSEVIER INC. ALL RIGHTS RESERVED. 733
doi:10.1016/j.ajo.2005.11.036
tive steep corneal curvature appears to be a factor that
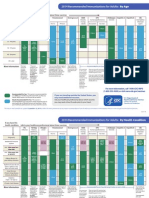
TABLE. LASIK Complications and Management contributes to flap buttonholes. General guidance to avoid
flap buttonholes includes the use of a small diameter kera-
Keratome and flap complications tome ring and deeper cutting plate when operating on
Intraoperative complications corneas with keratometry readings of 46. Extremely steep
Ectasia
corneas also must be scrutinized clinically and with topogra-
Flap striae
phy and pachymetry to rule out keratoconus.
Flap dislocation
The causes of flap decentration include improper align-
Laser complications
Misinformation/improper ablation
ment of the suction ring or drift after suction engagement. A
Decentered or improperly registered ablation significantly decentered flap whose edge lies within the
Reduced quality of vision ablation optical zone can induce astigmatism and visually
Complications of healing/infection/inflammation disabling higher order aberrations. This should be avoided by
Recurrent corneal erosions the attention of the surgeon to anatomic landmarks during
Infectious keratitis the application of suction.
Epithelial ingrowth An epithelial defect during LASIK is one of the most
Diffuse lamellar keratitis (DLK) common intraoperative complications and is associated
Post-LASIK dry eye
with pain and delayed visual recovery. Other complications
Other complications of LASIK
can result, including diffuse lamellar keratitis (DLK), epithe-
Intraocular pressure measurement after LASIK
lial ingrowth, and microbial keratitis. Epithelial defects usu-
Optic neuropathy and glaucoma
ally occur as a result of trauma from the keratome pass but
may be indicative of underlying epithelial basement mem-
on the corneal surface, which allows the blade to skim across brane disease (EBMD). A bandage contact lens usually is
the top of the cornea and produce a cap, a thin flap, or an applied and left in place until the epithelium heals. Preven-
incomplete flap. After suction is engaged, to avoid free caps tion of epithelial defects involves the avoidance of preop-
and other problems associated with inadequate suction, the erative eye medications, the restriction of the application
surgeon should complete four checks before cutting the flap: of anesthetic drops to immediately before surgery, and
(1) Ensure sufficient intraocular pressure with a tonometer, copious irrigation during the keratome pass.
(2) confirm that the patients vision has dimmed, (3) palpate
the cornea for firmness, and (4) ensure the suction ring has a ECTASIA: Ectasia of the cornea is a progressive anterior
firm grasp of the eye. Another suction problem that can affect shift of the cornea that is associated with central steepening
flap creation is occlusion of the suction port other than at the and thinning, myopic shift, and visual symptoms. Ectasia after
globe, sometimes referred to as pseudosuction; this problem LASIK is vision-threatening and is one of the more difficult
should be ruled out before the flap is cut by gentle traction on complications to manage, requiring a penetrating keratoplasty
the globe with suction on. A flat keratometry reading on the in severe cases. Because of this, avoidance is crucial.
preoperative cornea should be factored into preoperative Pre-existing keratoconus and a thin residual bed are two
planning, because flatter corneas are associated with free flaps identified risk factors that can be avoided in most cases by
and thin flaps. If a free flap is cut, the surgeon can still proceed proper preoperative evaluation and include corneal topog-
with LASIK, as long as the cap is found and the bed diameter raphy and pachymetry. A computation of the estimated
allows adequate space to ablate the cornea safely. The cap is residual bed should be performed in all LASIK cases. The
replaced after ablation, usually without sutures. Each cornea estimated flap thickness and ablation depth is subtracted
should be marked before flap creation (for example, with a from the preoperative central pachymetry. A better esti-
radial keratotomy corneal marking device) so that, if a free mate is to perform intraoperative pachymetry after the flap
flap is created, it can be replaced in the proper meridian; is lifted and subtract the estimated ablation depth to
otherwise, an irregular astigmatism is likely to be created, and account for keratome variability in flap thickness. A
other aberrations invite epithelial ingrowth because of mis- generally accepted minimum is 250 m. However, there
matched flap edges. If a thin or incomplete flap occurs, the have been reports of postoperative ectasia after a residual
keratome should be stopped; ablation should be aborted, and bed thickness over 250 m is confirmed.3 Rigid gas
the flap should be replaced and allowed to heal for 3 to 6 permeable (RGP) contact lenses and penetrating kerato-
months before another procedure is attempted. plasty are treatment modalities that are available for
LASIK flap buttonholes are ring-shaped flaps with a cen- visually debilitating keratectasia after LASIK. The use of
tral hole or thin area. Flap buttonholes can result in the loss intrastromal corneal rings such as Intacs (Addition Tech-
of best-corrected visual acuity (BCVA) or other visual dis- nology, Inc, Fremont, California, USA) is being investi-
turbances such as glare, starburst, or diplopia. Blade imper- gated for viability as an alternative to penetrating
fections, power decrease in the keratome motor, and loss of keratoplasty for post-LASIK corneal ectasia. Given the
suction during the aforementioned procedure can cause but- encouraging results of intrastromal corneal ring therapy for
tonholes. Barring keratome or suction difficulties, preopera- keratoconus, patients with post-LASIK corneal ectasia
734 AMERICAN JOURNAL OF OPHTHALMOLOGY APRIL 2006
have also been treated with Intacs with good results.4,5 system with a software interface. Laser ablation can result
Most treated eyes had improvement in BCVA and uncor- in complications from a variety of sources.
rected visual acuity, and delay of penetrating keratoplasty
was achieved. MISINFORMATION/IMPROPER ABLATION: One of the
most common, most feared, and most easily avoided compli-
FLAP STRIAE: Flap striae (wrinkles or folds in the LASIK cation is unintentional ablation, which is caused by the entry
flap) can be seen as a complication immediately after the flap of incorrect patient treatment information into the excimer
is replaced or thereafter. The incidence of flap striae has been laser system. An error (such as entering the wrong sign or a
reported as high as 10% in the early stages of the surgeons misplaced decimal) can result in a dramatic under or over-
experience, which suggests that surgical skill plays a role in correction and may induce astigmatism.
the cause.6 Careful examination after the replacement of the Real-time chart review and a verbal confirmation from
flap intraoperatively and a postoperative examination can the patient before the start of treatment will lessen the
help identify folds early and expedite management if needed. opportunity for error. Advanced systems that can autorec-
Microstriae are defined as folds in the epithelium on post- ognize the patient (for example, iris detail) may reduce the
LASIK examination. Pooling of fluorescein can be used to likelihood of this type of error dramatically. A nomogram
distinguish microstriae from full-thickness folds. If there is no adjustment is applied commonly to the preoperative man-
pooling, then the flap folds are considered microstriae. Mi- ifest refraction to increase the predictability of the out-
crostriae usually are not visually significant and do not have come that is based on the results of previous patient
deleterious long-term consequences, and surgical interven- treatments. However, a nomogram that is miscalculated,
tion usually is not indicated. misinterpreted, or improperly applied can result in over- or
Full-thickness folds, or macrostriae, involve the stroma undercorrection.
and are associated with a loss of visual acuity. To help Significant accommodation during refraction or acquisi-
differentiate from microstriae, fluorescein pooling and an tion of wavefront measurements can result in overcorrection
asymmetric gutter will be seen with macrostriae. The when myopia is treated and undercorrection when hyperopia
treatment includes irrigation underneath and replacement of is treated. A cycloplegic refraction is essential when accom-
the flap and putting the flap on tension to eliminate the folds, modation is suspected, especially in young patients.
either with instruments specifically designed to smooth the It is important to develop and standardize a surgical
flap or by the placement of sutures. Removal of the epithe- technique with regard to timing and hydration to produce
lium of a flap with chronic stromal folds may increase consistent results and lessen the likelihood of over- or
success in flattening macrostriae. undercorrection.13 A stromal bed that has pooled moisture
or is very dry can affect results, as can flap-to-treatment
FLAP DISLOCATION: Both early and late flap dislocation time, duration of ablation, and flap replacement technique.
has been reported as complications of LASIK. Studies of Most of these issues can be factored into a nomogram, but
1000 eyes after LASIK have reported up to 2.0% incidence only if the surgical technique is consistent.
of spontaneous flap dislocation, mostly within the first 24
hours after surgery. Careful and consistent techniques are DECENTERED OR IMPROPERLY REGISTERED ABLA-
needed when positioning the flap during surgery and at TION: A decentered ablation occurs when the correct laser
examination of the flap in the first hour and first day after treatment is displaced peripherally relative to the visual axis.
LASIK. Immediate replacement of partially or completely Decentration is assessed by postoperative corneal topography
dislocated flaps in the early postoperative period, as with or by a difference map between the postoperative and
full-thickness folds, usually results in the maintenance of preoperative topography. A displacement of 1 mm gener-
preoperative BCVA. Typically, the flap is repositioned by ally is considered significant and can result in debilitating
simple irrigation and reapproximation of the flap, and pro- visual symptoms such as monocular diplopia, glare, halos,
phylactic antibiotic and corticosteroid drops are used. The and starburst phenomena.7 However, even a subclinical
longer a flap is dislocated, the greater the chance of other decentration of 0.5 mm potentially can impact the visual
complications such as striae, epithelial ingrowth, or DLK and outcome.8 This would be most apparent when a smaller
possible loss of visual acuity. If epithelium has grown under optical zone treatment diameter is used, such as is used
the flap during displacement, it should be removed before commonly to treat hyperopia.
replacement, with or without the use of sutures to hold the We recommend five current techniques to avoid decentra-
flap in place. Late traumatic flap dislocation is a rare but tion: First, the full attention of the surgeon is needed to
well-known complication that requires intensive therapy and confirm that the automated eye tracker has engaged properly
may lead to further complications such as a loss of BCVA and and remains active throughout treatment. Second, the laser
loss of the flap. manufacturers calibration methods must be performed rou-
tinely to ensure that the eye tracker remains properly aligned.
LASER-RELATED COMPLICATIONS: The excimer laser Third, it is imperative to position each patient under the laser
uses a sophisticated, computer-controlled beam delivery carefully and in a manner conducive to fine adjustment
VOL. 141, NO. 4 LASIK COMPLICATIONS 735
before and during treatment; if a patients head is placed at many clinical studies, such as glare, starburst, and halos.1315
the edge of the bed or joystick limits, the surgeon will be Newly developed aberrometers have demonstrated that
unable to compensate for slight changes in patient move- LASIK can induce optical aberrations that can impair high-
ment. Fourth, despite eye tracker technology, if a patients quality vision.17 Pupil size has been correlated to symptoms in
gaze drifts during ablation, the lateral displacement between the early postoperative time period, presumably because the
the limbus or the pupil and the treated cornea can result in an mesopic pupil would allow light from the untreated cornea to
ablation that is decentered. This complication can be pre- create a halo effect around the viewed image.17 However, no
vented if the surgeon actively confirms that the patient long-term relationship between the size of the low light pupil
continues to fixate on the proper visual target throughout and quality of vision symptoms has been observed after
the procedure. Fifth, it is generally recognized that the LASIK.18 WFG LASIK appears to result in better quality of
ablation should be centered on the line of sight to obtain vision than conventional LASIK.19 This is based on changes
the best visual outcome.9 Centering the treatment on the in BCVA, contrast sensitivity, and patient questionnaires.
visual axis (the corneal apex) instead of the line of sight There is less induction of higher-order aberration with WFG
can result in decentration. LASIK, especially spheric aberration.
The treatment of a visually significant decentered ablation Assessment of quality of vision symptoms after LASIK
is difficult at best. It is normally not amenable to a simple includes a complete examination that pays attention to the
spherocylindric treatment. Correction can be achieved by the tear film, flap integrity, corneal clarity, crystalline lens, and
placement of a second ablation at 180 degrees opposite the retina. An evaluation of uncorrected visual acuity, BCVA,
original decentered treatment. However, it is difficult to and manifest refraction is needed. Topography is useful in the
determine the size and shape of the treatment and to properly assessment of the regularity of the central cornea and ablation
place the ablation on the cornea; significant flattening of the centration. If the preoperative topography is available, a
cornea can result in a hyperopic shift in refraction. Topo- difference map can be used. The usefulness of aberrometry to
graphic data can be used selectively to create an ablation determine the extent of higher-order aberrations must be
profile by the combination of multiple spherocylindric cor- balanced against the potential difficulty in interpreting the
rections of various diameters and offset on the cornea to results, because there are no well-established standards for
create a more regular corneal shape.10 Studies that used this these aberrations that can be used for comparison; the pupil
technique have shown a reduction of refractive cylinder, size used in the aberration analysis can effect the amount and
improvement in best-corrected and uncorrected visual acuity, type of aberrations dramatically, and it is not established how
and improved corneal regularity. More recently, an aberrom- these aberrations affect the quality of vision.
eter has been used to compute directly an ablation profile that Many of these symptoms abate with time as healing and
takes into account not only the residual refractive error but cortical adaptation occur. In lieu of a significant refractive
also higher order aberrations, especially coma. Wavefront- error, observation is often the appropriate management.
guided (WFG) retreatment for decentered ablation has re- Spectacles may be useful in guiding a possible retreatment.
sulted in improvements in best-corrected and uncorrected Slightly over-minused spectacles for suspected night myopia
acuity.11 may help abate symptoms. Pharmacologic pupillary constric-
Another important aspect of proper centering of the tion can be effective in the reduction of symptoms for
ablation deals with accurate registration of the ablation on patients with both small and large mesopic pupils. Rigid gas
the cornea for the treatment of astigmatism and/or higher permeable (RGP) contact lens can be both diagnostic and
order aberrations (WFG LASIK). Unintentional cyclotorsion therapeutic in symptomatic patients. For example, an RGP
can occur when a patient lies underneath the excimer laser trial lens can rule in an early cataract as the cause of
and can result in a reduction in the efficacy of astigmatic symptoms. A well-tolerated, well-fitting lens may also be
correction or an induction of astigmatism. For WFG treat- therapeutic. WFG retreatment holds great promise to address
ments, the ablation pattern is determined during the wave- symptoms that are caused by higher-order aberrations.20
front capture with the patient seated. Even subtle
cyclotorsional misalignment between the wavefront treat- COMPLICATIONS OF HEALING/INFECTION/INFLAM-
ment pattern and the eye under the laser can result in MATION: The postoperative complications that are perhaps
induced higher-order aberrations. Proper registration of the the most perplexing are those that are related to the human
ablation has been performed typically by the alignment of the healing process. Even with proven equipment, standardized
treatment to limbal marks placed before surgery. Newer and proper surgical techniques, and adequate postoperative
techniques show great promise to improve registration, in care, the ocular response to surgery can result in an unwanted
particular iris or scleral recognition. Iris or scleral details that outcome. In these cases, complications must be recognized
are captured during the wavefront capture are aligned to and managed appropriately.
recognition of the same details under the excimer laser.
RECURRENT CORNEAL EROSIONS: LASIK has been
REDUCED QUALITY OF VISION: Symptoms related to reported to induce or precipitate recurrent corneal erosions
decreased quality of vision after LASIK have been reported in (RCE). Symptoms that are suggestive of RCE include sharp
736 AMERICAN JOURNAL OF OPHTHALMOLOGY APRIL 2006
eye pains, the sensation of the eyelid sticking, and soreness of antibiotics may be required for those cases that do not
the eyelid to touch. Triggers for RCE after LASIK include respond clinically to topical treatment. Removal of the flap,
epithelial trauma at the time of the LASIK procedure and especially in mycobacterial infections, may be required if
previously undiagnosed EBMD. Patients with diabetes melli- antibiotic treatment fails to halt the progression of the
tus who undergo LASIK are at a significantly higher risk of disease. When diagnosed and treated appropriately, most
the development of postoperative epithelial complications. sight-threatening microbial keratitis after LASIK heals with
This can lead to poorer refractive results when compared with minimal scarring and best spectacle-corrected visual acuity of
treated eyes of nondiabetic patients. Corneal erosions after 20/40.25
LASIK have been associated with a significant increase in Endophthalmitis, though rare after LASIK, can occur
DLK, even after re-epithelialization has been completed.21 and requires prompt evaluation and treatment to avoid a
Prevention of epithelial trauma at the time of surgery is the permanent visual sequela. Prompt treatment with intrave-
key to the reduction of the incidence of RCE after LASIK. nous, intravitreal, and topical antibiotics can result in
This includes minimization of preoperative eye medications successful resolution, although BCVA, and corneal clarity
(particularly anesthetic drops), copious irrigation during the may be reduced.
keratome pass, and minimization of epithelial desiccation.
RCE usually responds to treatment with ocular lubricants, EPITHELIAL INGROWTH: Epithelial ingrowth describes a
and a bandage contact lens can be considered to speed population of aberrant epithelial cells within the flap inter-
reepithelialization time and reduce discomfort and irritation. face after LASIK. Epithelial ingrowth occurs either by con-
Cases in which loose epithelium is noted after LASIK should tiguous migration of cells from the edge of the flap or by direct
be identified as potential RCE cases and followed appropri- implantation of cells in the interface during the LASIK
ately, especially if subsequent enhancement procedures are procedure. Defining clinically significant epithelial growth as
being considered. DLK, if present, should be treated appro- that which required surgical removal, the incidence is approx-
priately with topical corticosteroids. For RCE after LASIK imately 1%. Risk factors for epithelial ingrowth include poor
that does not respond to conventional therapy, anterior flap adhesion because of a perioperative epithelial defect,
stromal puncture has been reported to be useful and EBMD, DLK after surgery, and possibly thin flaps and diabe-
effective.22 tes mellitus. Avoidance of epithelial defects after surgery is
the most important preventive measure to reduce the occur-
INFECTIOUS KERATITIS: Infectious keratitis is a well- rence of epithelial ingrowth. Meticulous attention to proper
known, but rare, complication of LASIK. A survey was realignment of the flap edges is also an important factor.
conducted by the American Society of Cataract and Refrac- Other preventative measures may include the irrigation
tive Surgery in 2003 and, based on 116 infections that were and the wiping of the stromal interface with sponges, the
reported by LASIK surgeons who had performed an estimated aspiration of irrigation fluid and debris with a suctioning
338,550 procedures, determined the incidence of post-LASIK lid speculum, and the use of a bandage contact lens for the
microbial keratitis to be 0.03%.23 Symptoms of pain, dis- first day after surgery.26
charge, epithelial defects, and anterior chamber reactions The decision to treat usually depends on the progression of
within 1 week of surgery are more likely to be associated with the epithelial ingrowth and the potential to affect vision.
Gram-positive infection. Atypical organisms (which include Initial treatment consists of the lifting of the flap and manual
mycobacteria, fungus, and acanthamoeba) have a more de- removal of the growth of epithelial cells from the stromal
layed onset and result in a prolonged disease course. Flap surface and the back side of the lifted flap. Replacement of the
elevation and culture should be performed when post-LASIK flap in proper position is important in the reduction of the
infectious keratitis is suspected. Rapid intervention is corre- likelihood of primary or recurrent epithelial ingrowth. Clin-
lated with improved visual outcome. Microbial keratitis can ically significant epithelial ingrowth recurs in approximately
mimic DLK in the immediate postoperative time period. 25% of eyes after the initial surgical removal.27 The suturing
Both have inflammation of the flap interface. A discrete of the flap into position or fibrin glue (Tisseel; Baxter, Baxter
infiltrate cells or several focal infiltrates in the anterior Corp, Mississauga, Ontario, Canada) at the flap edge has been
chamber, perilimbal injection, and severe eye pain are all used to prevent recurrent epithelial ingrowth after LASIK
indicative of a microbial process. Delayed-onset mycobacte- and epithelial ingrowth removal.28
rial keratitis after LASIK has been reported up to twenty-four
weeks after surgery. A reported outbreak of Mycobacterium DLK: DLK, also called the Sands of the Sahara syn-
chelonae infection after LASIK required the removal of the drome, is a post-LASIK inflammatory condition in the
flap in seven of 10 eyes that were involved because of the interface that appears as a multifocal and/or diffuse inflam-
failure of all conservative measures.24 mation that is confined to the interface and is associated with
Management of microbial keratitis after LASIK includes pain, photophobia, redness, and/or tearing. Inflammation
topical fortified antibiotic therapy, irrigation of stromal bed usually appears between two and six days after surgery but
with antibiotic solution after lifting the flap, and sending the may present six months after surgery. Most surgeons use a
scraping of the infiltrate for microbiologic evaluation. Oral threefold strategy of identification, staging, and intervention
VOL. 141, NO. 4 LASIK COMPLICATIONS 737
for rapid diagnosis and appropriate treatment of DLK. Al- measurement with GAT and also noncontact tonometry.
though epithelial defects are associated strongly with DLK Studies that have examined the relationship between central
formation, not all cases of epithelial defects result in the corneal thickness and GAT have reported varying results;
appearance of inflammatory cells in the flap interface. some studies concluded a linear relationship exists allowing a
With appropriate diagnosis and treatment, DLK should simple corrective formula, and others did not. Some clini-
resolve without sequelae and yield visual outcomes that are cians use these corrective formulae to adjust post-LASIK
comparable with cases with uneventful postoperative cours- GAT readings.34,35 Reported underestimation of intraocular
es.29 Corticosteroids are the mainstay of the treatment of pressure after hyperopic LASIK suggests that other post-
DLK because it is primarily an inflammatory condition. Flap LASIK changes (such as reduced rigidity, altered corneal
lift and irrigation may be required in cases that are refractory microstructure, and changes in corneal curvature) also influ-
to initial topical medication. Phototherapeutic keratectomy ence the accuracy of GAT. Contact pneumatonometry may
(PTK) has also been reported to be effective in the treatment be a more accurate method of intraocular pressure measure-
of DLK that is recalcitrant to conservative measures. In cases ment in post-LASIK eyes.36 Another device, the Pascal
of known atopy, patients can be treated with antihistamines dynamic contour tonometer (Swiss Microtechnology AG,
before surgery to control the disease and to reduce the risk of Port, Switzerland) may also be less affected than GAT by
DLK and the potential for vision loss. It is essential to corneal changes after LASIK.37 The drawbacks to the use of
measure intraocular pressure in all cases of suspected DLK to alternate devices include added cost and a need for more data
rule out pressure-induced post-LASIK interface keratitis be- to support their use. Currently, given that GAT is inaccurate
cause topical corticosteroids are ineffective in this condition when used to measure intraocular pressure after LASIK, the
and may worsen the process.30 clinician must use a corrective factor or an alternate method
of tonometry (such as contact pneumatonometry or dynamic
POST-LASIK DRY EYE: Up to 48% of patients complain of
contour tonometer) until larger, prospective studies verify the
dryness symptoms during the first six months after surgery; accuracy of these methods and provide further guidance.
soreness of the eye to touch has been reported in 6.7% of
LASIK patients, and sharp pains have been reported in 8.0% OPTIC NEUROPATHY AND GLAUCOMA: There have
of LASIK patients.31 The risk of refractive regression after been reports of ischemic optic neuropathy after LASIK that is
LASIK appears to increase in patients with chronic dry eye. presumed to be caused by transient ischemia or barotrauma
Tear secretion and tear film stability are reduced during the from keratome suction.38 Corticosteroid-induced glaucoma
early postoperative time period after LASIK.32 This may be has been reported after LASIK and may be difficult to identify
the result of a loss of trophic influence from severed corneal because of interface fluid or other mechanism.39 Such reports
nerve bundles after the creation of the flap with the keratome underscore the importance of evaluation before surgery to
and may be influenced by hinge position and width. Fortu- identify pre-existing glaucoma or optic neuropathy and to
nately, dry eye complaints typically resolve approximately six monitor for the development of these conditions after surgery.
to twelve months after surgery. The use of artificial tears or
punctal plugs in the early postoperative period may help to
prevent unwanted symptoms and ocular surface damage.33
Preoperative screening of patients with mild-to-moderate dry SUMMARY
eyes is important for counseling and postsurgical planning.
Patients with severe dry eye are generally not good surgical OUR PATIENTS BENEFIT BY AN ONGOING EVALUATION OF
candidates for LASIK. the surgical complications and events that pose a threat to
vision, both in quantity and quality. This is a never-ending
OTHER COMPLICATIONS OF LASIK: In addition to the pursuit. The advancement of our understanding of the pre-
myriad of potential complications from the flap, instru- vention and treatment of complications is an endeavor that
mentation, and normal healing processes, there are a must be continued as long as refractive surgery is
number of other issues that are associated with LASIK. performed.12,16
INTRAOCULAR PRESSURE MEASUREMENTS AFTER
LASIK: Accurate measurement of intraocular pressure is
essential for monitoring patients who are being treated for REFERENCES
glaucoma or who are at risk for the development of glaucoma,
1. Durrie DS, Kezirian GM. Femtosecond laser versus mechan-
including corticosteroid-induced glaucoma. Goldmann appla- ical keratome flaps in wavefront-guided laser in situ kerato-
nation tonometry (GAT), which is still considered the mileusis: prospective contralateral eye study. J Cataract
current gold standard for intraocular pressure measurement, Refract Surg 2005;31:120 126.
assumes a normal central corneal thickness of 520 m. A thin 2. Farah SG, Azar DT, Gurdal C, Wong J. Laser in situ keratom-
central corneal thickness, as is often the case after myopic ileusis: literature review of a developing technique. J Cataract
ablation, will result in a falsely low intraocular pressure Refract Surg 1998;24:989 1006.
738 AMERICAN JOURNAL OF OPHTHALMOLOGY APRIL 2006
3. Miyata K, Tokunaga T, Nakahara M, et al. Residual bed 21. Asano-Kato N, Toda I, Tsubota K. Severe late-onset recur-
thickness and corneal forward shift after laser in situ kerato- rent epithelial erosion with diffuse lamellar keratitis after
mileusis. J Cataract Refract Surg 2004;30:10671072. laser in situ keratomileusis. J Cataract Refract Surg 2003;29:
4. Pokroy R, Levinger S, Hirsh A. Single intacs segment for 2019 2021.
post-laser in situ keratomileusis keratectasia. J Cataract 22. Malecha MA. Anterior stromal puncture for recurrent cor-
Refract Surg 2004;30:16851695. neal erosion after laser in situ keratomileusis. J Cataract
5. Kymionis GD, Siganos CS, Kounis G, Astyrakakis N, Kaly- Refract Surg 2004;30:496 498.
vianaki MI, Pallikaris IG. Management of post-LASIK cor- 23. Solomon R, Donnenfeld ED, Azar DT, et al. Infectious
neal ectasia with intacs inserts. Arch Ophthalmol 2003;121: keratitis after laser in situ keratomileusis: results of an
322326. ASCRS survey. J Cataract Refract Surg 2003;29:20012006.
6. Gimbel HV, Basti S, Kaye GB, Ferensowicz M. Experience 24. Freitas D, Alvarenga L, Sampaio J, et al. An outbreak of
during the learning curve of laser in situ keratomileusis. J mycobacterium chelonae infection after LASIK. Ophthal-
Cataract Refract Surg 1996;22:542550. mology 2003;110:276 285.
7. Mulhern MG, Foley-Nolan A, OKeefe M, Condon PI. Topo- 25. Pushker N, Dada T, Sony P, et al. Microbial keratitis after
graphical analysis of ablation centration after excimer laser laser in situ keratomileusis. J Refract Surg 2002;18:280 286.
photorefractive keratectomy and laser in situ keratomileusis for 26. Walker MB, Wilson SE. Incidence and prevention of epi-
high myopia. J Cataract Refract Surg 1997;23:488 494. thelial ingrowth within the interface after laser in situ
8. Mihashi T. Higher-order wavefront aberrations induced by keratomileusis. Cornea 2000;19:170 173.
small ablation area and sub-clinical decentration in simu- 27. Wang MY, Maloney RK. Epithelial ingrowth after laser in
lated corneal refractive surgery using a perturbed schematic situ keratomileusis. Am J Ophthalmol 2000;129:746 751.
eye model. Semin Ophthalmol 2003;18:41 47. 28. Anderson NJ, Hardten DR. Fibrin glue for the prevention of
9. Uozato H, Guyton DL. Centering corneal surgical proce- epithelial ingrowth after laser in situ keratomileusis. J Cata-
dures. Am J Ophthalmol 1987;103:264 275. ract Refract Surg 2003;29:14251429.
10. Lin DY, Manche EE. Custom-contoured ablation pattern 29. Stulting RD, Randleman JB, Couser JM, Thompson KP. The
method for the treatment of decentered laser ablations. epidemiology of diffuse lamellar keratitis. Cornea 2004;23:
J Cataract Refract Surg 2004;30:16751684. 680 688.
11. Mrochen M, Krueger RR, Bueler M, Seiler T. Aberration- 30. Nordlund ML, Grimm S, Lane S, Holland EJ. Pressure-
sensing and wavefront-guided laser in situ keratomileusis: induced interface keratitis: a late complication following
management of decentered ablation. J Refract Surg 2002;18: LASIK. Cornea 2004;23:225234.
418 429. 31. Hovanesian JA, Shah SS, Maloney RK. Symptoms of dry eye
12. Ailo JL, Arola A, Rodriguez-Mier FA. Selective zonal ablations and recurrent erosion syndrome after refractive surgery.
with excimer laser for correction of irregular astigmatism in- J Cataract Refract Surg 2001;27:577584.
duced by refractive surgery. Ophthalmology 2000;107:662 673. 32. Yu EY, Leung A, Rao S, Lam DS. Effect of laser in situ
13. Pop M, Payette Y. Photorefractive keratectomy versus laser keratomileusis on tear stability. Ophthalmology 2000;107:
in situ keratomileusis: a control-matched study. Ophthalmol- 21312135.
ogy 2000;107:251257. 33. Toda I, Asano-Kato N, Komai-Hori Y, Tsubota K. Dry eye
14. Hersh PS, Steinert RF, Brint SF. Photorefractive keratec- after laser in situ keratomileusis. Am J Ophthalmol 2001;
tomy versus laser in situ keratomileusis: comparison of 132:17.
optical side effects: Summit PRK-LASIK study group. Oph- 34. Chihara E, Takahashi H, Okazaki K, et al. The preoperative
thalmology 2000;107:925933. intraocular pressure level predicts the amount of underesti-
15. Brunette I, Gresset J, Boivin JF, et al. Functional outcome and mated intraocular pressure after LASIK for myopia. Br J
satisfaction after photorefractive keratectomy: part 2, survey of Ophthalmol 2005;89:160 164.
690 patients. Ophthalmology 2000;107:1790 1796. 35. Cheng AC, Fan D, Tang E, Lam DS. Effect of corneal
16. Oshika T, Miyata K, Tokunaga T, et al. Higher order curvature and corneal thickness on the assessment of intraoc-
wavefront aberrations of cornea and magnitude of refractive ular pressure using noncontact tonometry in patients after
correction in laser in situ keratomileusis. Ophthalmology myopic LAKIK surgery. Cornea 2006;25:26 28.
2002;109:1154 1158. 36. Duch S, Serra A, Castanera J, Abos R, Quintana M.
17. Helgesen A, Hjortdal J, Ehlers N. Pupil size and night vision Tonometry after laser in situ keratomileusis treatment.
disturbances after LASIK for myopia. Acta Ophthalmol J Glaucoma 2001;10:261265.
Scand 2004;82:454 460. 37. Siganos SS, Papastergiou GI, Moedas C. Assessment of the
18. Schallhorn SC, Kaupp SE, Tanzer DJ, et al. Pupil size and Pascal dynamic contour tonometer in monitoring intraocular
quality of vision after LASIK. Ophthalmology 2003;110: pressure in unoperated eyes and eyes after LASIK. J Cataract
1606 1614. Refract Surg 2004;30:746 751.
19. Kaiserman I, Hazabassanov R, Varssano D, Grinbaum A. 38. Lee AG, Kohnen T, Ebner R, et al. Optic neuropathy
Contrast sensitivity after wavefront-guided LASIK. Ophthal- associated with laser in situ keratomileusis. J Cataract Refract
mology 2004;111:454 457. Surg 2000;26:15811584.
20. Salz JJ. Wavefront-guided treatment for previous laser in situ 39. Hamilton DR, Manche EE, Rich LF, Maloney RK. Steroid-
keratomileusis and photorefractive keratectomy: case reports. induced glaucoma after laser in situ keratomileusis associated
J Refract Surg 2003;19:S697S702. with interface fluid. Ophthalmology 2002;109:659 665.
VOL. 141, NO. 4 LASIK COMPLICATIONS 739
Biosketch
Steven C. Schallhorn, MD, is currently the director of the Navy Refractive Surgery Center at the Naval Medical Center
in San Diego (NMCSD), California. He has led Navy research on the safety and efficacy of refractive surgery including
a comprehensive program for Naval aviation. Many of his studies involve the effects of laser vision correction on the
quality of vision.
739.e1 AMERICAN JOURNAL OF OPHTHALMOLOGY APRIL 2006
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Contoh CV Untuk Nursing MalaysiaDocument4 pagesContoh CV Untuk Nursing MalaysiaWahyudin Aziz100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Nanotube Transistors Replace SiliconDocument1 pageNanotube Transistors Replace Siliconrandy_27995No ratings yet
- Jurding Mata 2Document8 pagesJurding Mata 2randy_27995No ratings yet
- What Is A Z Score PDFDocument2 pagesWhat Is A Z Score PDFrandy_27995No ratings yet
- IV Paracetamol and Pda Closure in Preterm InfantsDocument6 pagesIV Paracetamol and Pda Closure in Preterm Infantsrandy_27995No ratings yet
- Jurding MataDocument7 pagesJurding Matarandy_27995No ratings yet
- Nutrients: Protein Nutrition and Malnutrition in CKD and ESRDDocument19 pagesNutrients: Protein Nutrition and Malnutrition in CKD and ESRDrandy_27995No ratings yet
- Jurding Mata 3Document35 pagesJurding Mata 3randy_27995No ratings yet
- Fulltext SMDJ v2 1005Document5 pagesFulltext SMDJ v2 1005randy_27995No ratings yet
- ProQuestDocuments 2015-07-07Document16 pagesProQuestDocuments 2015-07-07randy_27995No ratings yet
- Jurnal GERDDocument8 pagesJurnal GERDrandy_27995No ratings yet
- TB Paru AnakDocument36 pagesTB Paru Anakrandy_27995No ratings yet
- Adult Schedule Easy ReadDocument2 pagesAdult Schedule Easy Readtummalapalli venkateswara raoNo ratings yet
- GODocument6 pagesGOrandy_27995No ratings yet
- Tugas B.inggris (Computer Technology)Document3 pagesTugas B.inggris (Computer Technology)randy_27995No ratings yet
- 02 Becoming A First Aider, Assessing A CasualtyDocument15 pages02 Becoming A First Aider, Assessing A CasualtyEric OngNo ratings yet
- BAG TECHNIQUE FOR EFFECTIVE PUBLIC HEALTH NURSING CAREDocument40 pagesBAG TECHNIQUE FOR EFFECTIVE PUBLIC HEALTH NURSING CAREhapices100% (1)
- HW 1 PathoDocument4 pagesHW 1 PathoBryan RallomaNo ratings yet
- Pomr 1Document7 pagesPomr 1Afifa Prima GittaNo ratings yet
- Oxygen-Induced Hypercapnia in COPD PDFDocument4 pagesOxygen-Induced Hypercapnia in COPD PDFsatyagraha84No ratings yet
- HR 1701 - Commending Medical and Nursing Board TopnotchersDocument2 pagesHR 1701 - Commending Medical and Nursing Board TopnotchersBayan Muna Party-listNo ratings yet
- Vitapex. A Case Report PDFDocument4 pagesVitapex. A Case Report PDFPamela GuzmánNo ratings yet
- Topic 1 What Is Patient Safety?Document14 pagesTopic 1 What Is Patient Safety?Lilik WijayatiNo ratings yet
- Department of SurgeryDocument8 pagesDepartment of SurgeryDeusah EzrahNo ratings yet
- Advance Trauma Life SupportDocument67 pagesAdvance Trauma Life SupportraffellaNo ratings yet
- Comparison of Icd 10 and DSM 5: BY Anitha J I Mphil Clinical PsychologyDocument102 pagesComparison of Icd 10 and DSM 5: BY Anitha J I Mphil Clinical Psychologyanitha1118No ratings yet
- Dr. Sherif Eladawy Dr. Amr Bassiouny Dr. Yehia Hussein: Presented byDocument8 pagesDr. Sherif Eladawy Dr. Amr Bassiouny Dr. Yehia Hussein: Presented byYahya Hassan Hussein El-tamalyNo ratings yet
- PROCTOSIGMOIDOSDocument5 pagesPROCTOSIGMOIDOSJopet Llanita0% (1)
- HemodyalisisDocument148 pagesHemodyalisisRatnaSuryatiNo ratings yet
- Nursing Ethics DilemmasDocument3 pagesNursing Ethics DilemmasDeng Navarro PasionNo ratings yet
- Schizophrenia and HomeopathyDocument5 pagesSchizophrenia and HomeopathyAlokojjal Banerjee100% (1)
- Direct Immunofluorescence and Histopathology in Chronic Discoid Lupus ErythematosusDocument4 pagesDirect Immunofluorescence and Histopathology in Chronic Discoid Lupus ErythematosusdesiNo ratings yet
- Persona Knee Surgical TechniqueDocument72 pagesPersona Knee Surgical TechniquedrorthokingNo ratings yet
- 20 Jaundice#e856Document87 pages20 Jaundice#e856Alina CazanNo ratings yet
- BIOPSY Oral SurgeryDocument34 pagesBIOPSY Oral SurgeryNisha ChoudharyNo ratings yet
- Ultrasound in Critical CareDocument4 pagesUltrasound in Critical CareFranz MiguelNo ratings yet
- A Comparison Between 2 Absorbable Hemostatic AgentDocument5 pagesA Comparison Between 2 Absorbable Hemostatic AgentadhityasdewiNo ratings yet
- Stigma in PsihozaDocument22 pagesStigma in PsihozaBurca LarisaNo ratings yet
- Critical Care Testing - Quality AssuranceDocument120 pagesCritical Care Testing - Quality AssuranceAbhijit Mokashi100% (1)
- Angle 2007 Vol. 77, No. 2, Pp. 376-381Document6 pagesAngle 2007 Vol. 77, No. 2, Pp. 376-381André MéndezNo ratings yet
- Beltran, Justin KyleDocument4 pagesBeltran, Justin KyleKYLENo ratings yet
- Asthma PhenotypesDocument55 pagesAsthma PhenotypesAnonymous so6ZnlKywNo ratings yet
- Bab I.First Aid: PPSDM MigasDocument31 pagesBab I.First Aid: PPSDM MigasacidafdolaNo ratings yet
- 50 Item Medical-Surgical Nursing Test DrillDocument17 pages50 Item Medical-Surgical Nursing Test DrillFilipino Nurses CentralNo ratings yet