Professional Documents
Culture Documents
10 - Chapter 1 PDF
Uploaded by
AnjnaKandariOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10 - Chapter 1 PDF
Uploaded by
AnjnaKandariCopyright:
Available Formats
1
1. Introduction
A Medication Use Evaluation (MUE), or Drug Use Evaluation (DUE) program
is a planned, criteria-based systematic process for monitoring, evaluating, and
continually improving medication use, with the ultimate aim of improving
medication-related outcomes for a group of patients or consumers [1]
MUE is called by different terms namely drug utilization review, drug usage
review, drug use review, drug use evaluation, and drug utilization evaluation.
It is an important component of health care organizations quality
improvement program. The goal of MUE is to provide all patients with the
most rational, safe, and effective drug therapy through the assessment and
improvement of specific medication use processes. MUE may focus on a
specific medication, a class of medications; medications used in the
management of a specific disease state or clinical setting, medications related
to a clinical event, a specific component of the medication use process, or can
be based on specific outcomes [2].
The demand for and hence the cost of health care are increasing in all
countries as the improvement and sophistication of health technologies
increase. Medicines form a small but significant proportion of total health care
costs and one that has been growing consistently as new medicines are
marketed. Many governments are focusing their activities on promoting the
effective and economic use of resources allocated to health care [3].
Pharmacoeconomics can be defined as the measurement of both the costs
and consequences of therapeutics decision making. Pharmacoeconomics can
assist in the planning process and help assign priorities where, for example,
medicines with a worse outcome and lower cost can be compared with
medicines with higher cost and better outcomes [3]. There are number of
methods available for pharmaco-economic assessment like Cost-
effectiveness analysis, Cost of illness, each of which will be used depending
on the outcomes desired and interventions targeted.
2
1.1 Diabetes Mellitus
Diabetes is a metabolic disorder characterized by hyperglycemia, which is
associated with abnormalities in carbohydrate, fat and protein metabolism,
and results in chronic complications including microvascular, macrovascular
and neuropathic disorders. As a result of an aging population, changes in
lifestyle and higher levels of obesity, diabetes affects an increasing number of
patients, and the number is expected to reach more than double, world wide,
by the year 2030 [4].
Pharmacological therapy for diabetic patients is aimed at controlling
hyperglycaemia to prevent or impede complications of diabetes. The results of
the Diabetes Control and Complications Trial (DCCT) and United Kingdom
Prospective Diabetes Study (UKPDS) have showed that intensive DM
management can reduce risk of complications. Therefore aggressive drug
therapy is necessary for diabetic patients to achieve adequate glycemic
control. Oral hypoglycemics can be used alone or in combination with other
oral antidaibetic drugs (OADs) or insulin. Until 1994, oral antidaibetic drugs
available for the treatment of type 2 diabetes mellitus was limited to some
sulphonylureas and biguanides. In the last few years, four new classes were
available for the treatment. The newer agents include an alpha-glucosidase
inhibitor, the newest sulphonylurea glimepiride (1999), meglitinides (2002),
glitazones (2000) and gliptines is released in 2008 [5-7].
Hypertension affects about 60% of patients with type 2 diabetes. Serious
cardiovascular events are more than twice as likely in patients with diabetes
and hypertension as either disease alone. Hypertension and lipid disorders in
type 2 diabetes also contribute to increased coronary risk. It may be 2.3 times
higher in men and 2.9 times higher in women with type 2 diabetes mellitus
compared to nondiabetic subjects. Type 2 diabetes mellitus commonly
associated with elevated BP and with athergenic lipid abnormalities and this
combination represents a major cause of elevated coronary risk. This has
been explicitly recognized in clinical guidelines for the management of
hypertension or hypercholesterolaemia [8].
3
Appropriate use of antihypertensive agents may improve BP control and
reduce complications in patients with diabetes. Evidence also supports the
need for using multiple antihypertensive agents rather than monotherapy to
achieve target BP control and greater renoprotection. In addition, more recent
data from the antihypertensive and lipid lowering treatment to prevent heart
attack trial (ALLHAT) highlight the frequent need to use multidrug regimens to
treat BP to target levels, especially in type 2 diabetes [9].
The results of the United Kingdom Prospective Diabetes Study published in
1998 demonstrated the importance of good control of BP in reducing the
onset and progression of microvascular and macrovascular complications of
the condition. In this study, the ACE inhibitors, captopril and the beta blocker,
atenolol appeared to be of equal efficacy in the management of hypertension
in diabetes patients, but other evidence suggests that ACE inhibitors or
angiotensin receptor antagonists might reduce proteinuria or delay the onset
of nephropathy in subjects with type 2 diabetic patients [10].
The results of the HOPE study suggested that the prescription of an ACE
inhibitor (Ramipril) prevents complications of diabetes mellitus and had wider
benefits in reducing the incidence of myocardial infarction, stroke, overt
nephropathy as well as cardiovascular and all-cause mortality [11].
There is also increasing evidence of the benefits from cholesterol-lowering
therapy using statin drugs in the primary and secondary prevention of
coronary heart disease in subjects with diabetes mellitus. In the Heart
Protection Study, treatment of diabetes subjects with simvastatin led to a
reduction of about a quarter in new coronary events, revascularization and
strokes even in subjects who did not have elevated baseline cholesterol
concentrations [12].
1.2 Need for the study
There are various guidelines available for the management of type 2 diabetes
mellitus with hypertension and with raised cholesterol etc. Clinical practice
may depart from recommended standards based on the results of clinical
4
trials/ experience. Surveillance of variations in clinical practice may raise
questions concerning current patterns of practice and thus help to refine
policies or inform interventions to promote change [8].
In the management of diabetes, pattern of prescription may be driven by
patient factors (e.g.: body weight, motivation to improve), physician specific
variables (eg; usual practice patterns) and /or nonclinical issues (eg; patient
out-of-pocket expense). Evidencebased guidelines for prescribing
antidiabetic drug, typically, rely on objectively measurable criteria such as
HbA1C level and weight [13].
Guidelines for the treatment of type 2 diabetes have increasingly favored
tighter glycemic control, necessitating the use of more aggressive
pharmacological therapy. However the process by which physicians choose
glucose-lowering medicines is poorly documented. There is a need for
systematic study of how the drugs are being used together, whether
monotherapy, combination therapy or insulin in combination with oral therapy
among patients with type 2 diabetes [14].
The impact of diabetes on health care expenditures has been increasingly
recognized. Number of cost of illness studies have shown a threefold
increase in the direct costs of diabetic patients compared with non-diabetic
patients in the setting of different health care systems. Recent studies have
consistently shown that people with diabetes are more likely to develop many
complications, both acute and long term. Type 2 diabetes therefore, has
increasingly become the main cause of growing costs in hospitalization and
drugs. The excess costs were largely due to an increased number of hospital
days, expensive outpatients treatments, higher costs for nursing home care
and increased drug consumption. Diabetes is closely related to other cost-
intensive chronic conditions, especially cardiovascular disease and risk
factors (e.g. hypertension, lipid disorders) [15,16].
In a study at Canada on the cost of management of diabetes, it has been
reported that cardiovascular disease was the major contributor to the direct
5
costs of diabetes. Therefore it has been suggested that the prevention of
cardiovascular disease in the patient with diabetes should become an
imperative [17]. To formulate an effective health planning and resource
allocation, it is important to determine economic burden with or without the
absence of chronic complications.
1.3 Objectives
General objective:
To evaluate the prescription patterns and cost of illness of type 2 diabetic
patients.
Specific objectives:
1. To determine the trends in drug use patterns among patients with type
2 diabetes.
2. To evaluate the prescription pattern of antihypertensive medications in
type 2 diabetic patients.
3. To evaluate the pattern of lipid lowering therapy in type 2 diabetic
patients.
4. To determine the cost of illness (COI) for diabetic inpatients.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Push Pull Legs RoutineDocument4 pagesThe Push Pull Legs RoutineSparkbuggy57% (7)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Piaggio MP3 300 Ibrido LT MY 2010 (En)Document412 pagesPiaggio MP3 300 Ibrido LT MY 2010 (En)Manualles100% (3)
- Introduction of MaintenanceDocument35 pagesIntroduction of Maintenanceekhwan82100% (1)
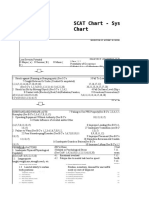
- SCAT Chart - Systematic Cause Analysis Technique - SCAT ChartDocument6 pagesSCAT Chart - Systematic Cause Analysis Technique - SCAT ChartSalman Alfarisi100% (1)
- Electrical Interview Questions & Answers - Hydro Power PlantDocument2 pagesElectrical Interview Questions & Answers - Hydro Power PlantLaxman Naidu NNo ratings yet
- JPK-056-07-L-1754 - Rev 0Document245 pagesJPK-056-07-L-1754 - Rev 0aibek100% (1)
- Egg Pasteurization Manual 1969Document54 pagesEgg Pasteurization Manual 1969Tomas MuzzioNo ratings yet
- Bes 124 AssignmentDocument9 pagesBes 124 AssignmentAnjnaKandariNo ratings yet
- Bes 121 AssignmentDocument10 pagesBes 121 AssignmentAnjnaKandariNo ratings yet
- Bes 123 AssignmentDocument10 pagesBes 123 AssignmentAnjnaKandariNo ratings yet
- MS 612Document11 pagesMS 612AnjnaKandariNo ratings yet
- MS 94Document9 pagesMS 94AnjnaKandariNo ratings yet
- Bes 122 AssignmnentDocument10 pagesBes 122 AssignmnentAnjnaKandariNo ratings yet
- MS 97Document12 pagesMS 97AnjnaKandariNo ratings yet
- MS 96Document7 pagesMS 96AnjnaKandariNo ratings yet
- MS 27Document9 pagesMS 27AnjnaKandariNo ratings yet
- Ms 91Document8 pagesMs 91AnjnaKandariNo ratings yet
- MS 55Document10 pagesMS 55AnjnaKandariNo ratings yet
- Assignment Course Code: MS - 56 Course Title: Materials Management Assignment Code: MS-56 /TMA/SEM - II/2020 Coverage: All BlocksDocument6 pagesAssignment Course Code: MS - 56 Course Title: Materials Management Assignment Code: MS-56 /TMA/SEM - II/2020 Coverage: All BlocksAnjnaKandariNo ratings yet
- MS 29Document10 pagesMS 29AnjnaKandariNo ratings yet
- MS 95Document8 pagesMS 95AnjnaKandariNo ratings yet
- MS 25Document10 pagesMS 25AnjnaKandariNo ratings yet
- MS 57Document9 pagesMS 57AnjnaKandariNo ratings yet
- MS 04Document9 pagesMS 04AnjnaKandariNo ratings yet
- MS-03Document16 pagesMS-03AnjnaKandariNo ratings yet
- MS 10Document10 pagesMS 10AnjnaKandariNo ratings yet
- Ms 11Document8 pagesMs 11AnjnaKandariNo ratings yet
- MS 09Document12 pagesMS 09AnjnaKandariNo ratings yet
- MS 02Document10 pagesMS 02AnjnaKandariNo ratings yet
- MS 44Document9 pagesMS 44AnjnaKandariNo ratings yet
- MS 07Document8 pagesMS 07AnjnaKandariNo ratings yet
- MS 46Document8 pagesMS 46AnjnaKandariNo ratings yet
- MS 28Document9 pagesMS 28AnjnaKandariNo ratings yet
- MS 45Document8 pagesMS 45AnjnaKandariNo ratings yet
- Assignment Reference Material (2020-21) I.B.O.-03 India's Foreign TradeDocument8 pagesAssignment Reference Material (2020-21) I.B.O.-03 India's Foreign TradeAnjnaKandariNo ratings yet
- MS 05Document6 pagesMS 05AnjnaKandariNo ratings yet
- Assignment Reference Material (2020-21) I.B.O.-02 Internationl Marketing ManagementDocument8 pagesAssignment Reference Material (2020-21) I.B.O.-02 Internationl Marketing ManagementAnjnaKandariNo ratings yet
- RCF's Market Analysis of Dealer NetworkDocument70 pagesRCF's Market Analysis of Dealer NetworkAshok KushwahaNo ratings yet
- Kidde Ads Fm200 Design Maintenance Manual Sept 2004Document142 pagesKidde Ads Fm200 Design Maintenance Manual Sept 2004José AravenaNo ratings yet
- Group 17-Solid State NMR - Questions-AnswersDocument5 pagesGroup 17-Solid State NMR - Questions-AnswersOmkar AkulwarNo ratings yet
- Specialized Connective TissueDocument15 pagesSpecialized Connective TissueSebNo ratings yet
- Rainer M. Holm-Hadulla, Alina Bertolino: Use of Drugs by Jazz MusiciansDocument3 pagesRainer M. Holm-Hadulla, Alina Bertolino: Use of Drugs by Jazz MusiciansTitikshaNo ratings yet
- H1 Revision Notes DNA and GenomicsDocument6 pagesH1 Revision Notes DNA and GenomicsJiaLi XieNo ratings yet
- Berman Et Al-2019-Nature Human BehaviourDocument5 pagesBerman Et Al-2019-Nature Human BehaviourMira mNo ratings yet
- Olpers MilkDocument4 pagesOlpers MilkARAAJ YOUSUFNo ratings yet
- CanteenDocument8 pagesCanteenmahesh4uNo ratings yet
- Module 4 q2 Smaw-9-10Document15 pagesModule 4 q2 Smaw-9-10Louvre Ferris Salabao TangbawanNo ratings yet
- NMC Confirmation FormDocument3 pagesNMC Confirmation FormGianina AvasiloaieNo ratings yet
- 2VV-33C-R4-V5 Product SpecificationsDocument5 pages2VV-33C-R4-V5 Product Specificationsnhan sieuNo ratings yet
- Experiment 4 (Group 1)Document4 pagesExperiment 4 (Group 1)Webster Kevin John Dela CruzNo ratings yet
- 3.SAFA AOCS 4th Ed Ce 2-66 1994Document6 pages3.SAFA AOCS 4th Ed Ce 2-66 1994Rofiyanti WibowoNo ratings yet
- Experiment Report Basic Physics "Total Internal Reflection"Document10 pagesExperiment Report Basic Physics "Total Internal Reflection"dita wulanNo ratings yet
- GDCR Final PDFDocument311 pagesGDCR Final PDFHrushikesh PatelNo ratings yet
- Somali Guideline of InvestorsDocument9 pagesSomali Guideline of InvestorsABDULLAHI HAGAR FARAH HERSI STUDENTNo ratings yet
- Persuasive Essay Eng 101nDocument6 pagesPersuasive Essay Eng 101napi-341545248No ratings yet
- Lab 9-Measurement of Filtrate Loss and Mud Cake Thickness of Drilling Mud Sample Using Dead Weight Hydraulic Filter Press Considering API Standard.Document17 pagesLab 9-Measurement of Filtrate Loss and Mud Cake Thickness of Drilling Mud Sample Using Dead Weight Hydraulic Filter Press Considering API Standard.Sunny BbaNo ratings yet
- Rise School of Accountancy Test 08Document5 pagesRise School of Accountancy Test 08iamneonkingNo ratings yet
- Jee Main Sample Paper 5Document19 pagesJee Main Sample Paper 5DavidNo ratings yet
- Deadline Anchors BrochureDocument3 pagesDeadline Anchors Brochurejlmunozv100% (2)
- Homework 5 - 2020 - 01 - v3 - YH (v3) - ALV (v2)Document5 pagesHomework 5 - 2020 - 01 - v3 - YH (v3) - ALV (v2)CARLOS DIDIER GÓMEZ ARCOSNo ratings yet