Professional Documents
Culture Documents
McGoldrick - Infection Control Ritual To Science - Based Practice
Uploaded by
UswaPutriemelelaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
McGoldrick - Infection Control Ritual To Science - Based Practice
Uploaded by
UswaPutriemelelaCopyright:
Available Formats
IMPROVING
INFECTION
CONTROL in
H O M E CA R E :
From Ritual to Science-Based Practice
While many home care
policies and procedures are developed with
the best of intentions, they frequently lack a scientific
basis and have been perpetuated over the years. This article
discusses infection control rituals in home care and hospice
and the importance of making patient care
practice decisions based on sound
scientific principles.
Home care and hospice nurses have always
adapted and applied infection prevention and
control strategies to the best of their abilities with
few, if any, external resources. Although home
care and hospice nurses are knowledgeable in the
basics of infection control, they often face a sig-
nificant challenge when adapting acute care prac-
tice to the home care setting. This adaptation has
resulted in a wide variation of practices and meth-
ods for patient care (e.g., cleaning and disinfect-
ing equipment, using clean versus sterile tech-
nique), as well as the development of many
ritualistic, arbitrary practices that have been cod-
ified in the home care and hospice organizations
policies and procedures.
MARY M. FRIEDMAN, MS, RN, CRNI, AND
EMILY RHINEHART, RN, MPH, CIC, CPHQ
vol. 18 no. 2 February 2000 http://www.nursingcenter.com Home Healthcare Nurse 99
2000 Lippincott Williams & Wilkins, Inc.
INFECTION CONTROL methods or definitions to measure the occur-
CHALLENGES IN HOME CARE rence of home care-acquired infections. The
The current body of infection control knowledge CDCs definitions for nosocomial infection (Gar-
and the development of guidelines and recom- ner et al., 1988) cannot be directly applied to
mendations for practice are based primarily on home care because they rely so heavily on labo-
acute care experience. Although there are many ratory data.
published guidelines for infection control practice The methods for surveillance of hospital infec-
related to handwashing and environmental con- tion are not suitable for home care either (Emori,
trol (Garner & Favero, 1986), isolation precau- 1991) because they recommend that a single indi-
tions (Garner, 1996), and control of multi-drug re- vidual (the infection control practitioner or ICP)
sistant microorganisms (Centers for Disease perform the surveillance by reviewing laboratory
Control, 1995) as well as other important issues, results, visiting clinical areas, interviewing staff,
they are specifically designed for the acute care reviewing medical records, and examining pa-
setting. Many of these recommended practices tients when appropriate. This approach is not lo-
may not be necessary or appropriate in the home gistically feasible in home care or hospice. The
care setting and, if they are, may require signifi- ICP in home care must rely on the professional
cant adaptation to make them feasible. The way nursing staff in the field to identify patients with
we do it in the hospital may not be practical or home care-acquired infections.
possible in the home care setting.
INFECTION CONTROL RITUALS
IN HOME CARE
Many recommended practices may not be necessary Although the concept of practicing infection con-
or appropriate in the home care setting and, if they trol in the home care setting is fundamental, it is
are, may require significant adaptation to make them the application of infection control principles that
feasible. The way we do it in the hospital may not is often a challenge for home care and hospice
be practical or possible in the home care setting. staff members and sometimes results in ritualistic
behavior. Some examples of these rituals follow.
For example, many of the items addressed in Ritual: Bag Technique
the Centers for Disease Controls (CDC) Guideline A prime example of a common ritualistic behavior
for Isolation Precautions in Hospitals (Garner, in home care is the handling of the nursing supply
1996) that refer to patient cohorting, restriction of bag. Many home care and hospice organizational
access and traffic flow, and placing patients in policies and procedures require the use of a bar-
rooms with negative air pressure obviously do rier (e.g., newspaper, chux, or wax paper) be-
not apply to the home care setting. In the home tween the nursing supply bag and the surface
setting, isolation precautions focus more on the upon which it is placed in the home.
protection of the home care staff member and It is also common for home care organizations
family, not other patients. to have a policy requiring that handwashing
In addition, there is minimal data on the inci- occur each time the staff member enters and
dence of home care-acquired infection (Danzig et reenters the nursing supply bag.
al., 1995; Kellerman et al., 1996; White & Ragland, An additional requirement may be to designate
1993) and there are currently no standardized a clean and dirty side of the bag. These poli-
cies and procedures were developed to address a
perceived risk (i.e., contamination of the nurs-
Mary M. Friedman, MS, RN, CRNI, is Principal and Home
ing bag and its contents).
Care Consultant, Home Health Systems, Inc., Marietta,
Georgia and a Home Care Nurse Surveyor, Joint Commis-
sion on Accreditation of Healthcare Organizations, Oak- Science
brook Terrace, Illinois. Address for correspondence: Mary There are no studies or scientific infection control
M. Friedman, 4857 Township Trace, Marietta, Georgia principles that would lead one to conclude that a
30066; e-mail: mmf@mindspring.com barrier placed under a nursing supply bag is nec-
Emily Rhinehart, RN, MPH, CIC, CPHQ, is Vice-President, essary or effective against preventing infections.
Quality Management, AIG Consultants, Inc., Healthcare Although microorganisms are a normal contami-
Management Division, Atlanta, Georgia. nant of walls, floors, and other surfaces, these en-
100 Home Healthcare Nurse http://www.nursingcenter.com vol. 18 no. 2 February 2000
vironmental surfaces are rarely associated with
transmission of infections to patient or person-
nel (Garner et al., 1986).
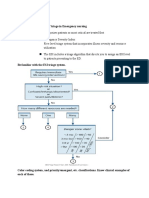
Bag Technique Procedure
Although there may be items inside the nurs-
1. Place the supply bag on a clean, dry surface in the
ing bag that must be maintained as clean or
patients home.
sterile, the outside of the bag generally does
not pose a risk for transmission of infection. If 2. Wash the hands with soap and running water before
an item truly is soiled and cannot be cleaned direct contact with the patient. If the patient is in-
or disinfected in the home, it should be placed fected or colonized with multidrug-resistant bacteria
in a separate container for transport back to
(e.g., M.R.S.A or V.R.E), wash the hands with antibac-
the office and cleaned. Therefore, a dirty
side of the bag is not necessary. terial soap and running water. If running water is not
It is also not necessary for the hands to be available, cleanse the hands with a waterless hand-
washed multiple times to retrieve items from washing product.
the nursing supply bag during the course of
3. Remove the needed supplies from the supply bag
care. Care should be taken not to reenter the
bag while wearing soiled gloves. However, en- and place on a clean, dry surface.
tering the nursing supply bag with clean hands 4. Perform patient care.
to retrieve patient care items does not require
repeated handwashing. 5. If an oral thermometer (semicritical equipment) was
used, clean and disinfect the thermometer with a
1. Most items in the bag are clean, noncritical 70% isopropyl alcohol prep pad and return to the
items (e.g., stethoscope, blood pressure cuff, supply bag.
measuring tape). Clean items may be returned
to the nursing supply bag after use provided 6. If noncritical equipment (i.e., blood pressure cuff,
there is no visible soiling. stethoscope, scale, etc.) was used, clean the supplies
2. Items that must be sterile for use (e.g., lancets, if soiled and return to the supply bag. If not soiled, re-
needles, and syringes) are protected by wrap- turn to the supply bag. If the patient is infected or col-
pers. Sterile items are usually discarded after use.
onized with multidrug-resistant bacteria, and equip-
Figure 1 contains an example of a basic nursing ment has not been designated for the patients
bag technique procedure that may be followed in individual use, clean and disinfect the equipment with
the home. a disinfectant of the home care or hospice organiza-
tions choice prior to replacing the noncritical equip-
Ritual: Routine Foley Catheter Change ment in the supply bag.
Another patient care practice that has become stan-
dard, but is contrary to published data and guide- 7. Remove personal protective equipment (gown and
lines, is the routine changing of foley catheters gloves), if worn.
every 30 days in the absence of complications. 8. Wash the hands with soap and running water. If the
patient is infected or colonized with multidrug-resis-
Science
tant bacteria (e.g., M.R.S.A or V.R.E), wash the
The CDC Guideline for Prevention of Catheter-As-
sociated Urinary Tract Infections (Wong, 1983) hands with antibacterial soap and running water. If
specifically states that indwelling catheters running water is not available, cleanse the hands
should not be changed at arbitrary fixed intervals again with a waterless handwashing product and
in the absence of leaking, malfunctioning, or pal- wash the hands with soap and running water as
pable concretions in the catheter lumen. soon as possible.
The Health Care Finance Administration
(HCFA) provides reimbursement for these skilled
Figure 1. Bag Technique Procedure. Source: Friedman,
nursing services and reimbursement guidelines M. (1998). Surveillance, Prevention, and Control of Infec-
state that absent any complications, foley tion. Home Care Policy and Procedure Manual. Home
catheters generally require skilled care once ap- Health Systems, Inc., Marietta, GA. Used with permission.
vol. 18 no. 2 February 2000 http://www.nursingcenter.com Home Healthcare Nurse 101
proximately every 30 days and silicone catheters APPLYING BASIC PRINCIPLES
generally require skilled care once every 6090 OF INFECTION PREVENTION
days (HCFA, 1996). As a result, many Medicare- AND CONTROL
certified home health agencies routinely change Decisions for infection prevention and control
catheters and drainage sets every 30 days. measures should always be based on scientific
Reconsideration should be given to this prac- principles and/or data, if available. To avoid ritu-
tice as data demonstrates that this routine patient alistic infection-control behaviors when practic-
care practice is not necessary. ing in the home care setting, understanding the
basic principles of infection prevention and con-
trol is essential. These principles are found in two
WHY LACK OF KNOWLEDGE rudimentary models: the epidemiologic triangle
PERPETUATES RITUALS (Figure 2) and the chain of infection (Figure 3).
Infection control rituals in home care and hospice
occur for several reasons: Epidemiologic Triangle
1. The initial risk assessment for infection may be The epidemiologic triangle represents the three
invalid. Risk is commonly overestimated and essential elements necessary for infectionthe
perceived to be greater than it actually is; such host, agent, and environment.
is the case with nursing bag technique.
Host. The host factors are critical in determining
2. The interventions to reduce the perceived risk
whether an infection is likely to occur. The
may be inappropriate, resulting in practices
patients risk is dependent upon many variables
that are unnecessary and waste limited re-
including their age, immune status, nutritional
sources. For example, some home care and
status, integrity of the skin and mucus
hospice organizations place all soiled dressing
membranes, and presence of indwelling devices.
supplies in a red bag and dispose of it as
In many cases, a home care patient may be
medical waste versus household waste (when
immune to a specific microorganism due to active
the items may be considered household waste
immunity from a previous infection (e.g.,
per state regulations).
chickenpox) or immunization (e.g., hepatitis B). If
3. Staff members dispose of all waste generated
a patient is not immune, he or she may be
throughout the course of obtaining a blood
considered a susceptible host.
sample (i.e. both sharps and non-sharp items
such as sterile wrappers, etc.) in a sharps con-
tainer when only sharps items need to be HOST
placed in the sharps container.
These medical waste-management practices
not only are beyond the requirements of the Oc-
cupational Safety and Health Administrations re-
quirements in the Bloodborne Pathogen Rule, but
add to the organizations costs for additional
sharp containers and disposal of medical waste.
Legitimately, home care nurses have had mini-
mal data and little guidance to support patient
care practice. Therefore, when unsure how to
handle a specific patient care situation, the staff
member will frequently err on the side of caution
to avoid doing the wrong thing. This practice is
common in the use of personal protective equip-
ment. In home care and hospice organizations,
staff have been observed wearing gloves, mask,
and gown and using sterile technique (when the AGENT ENVIRONMENT
physicians order or agency policy did not require
it) to clean and dress a noninfected pressure ulcer
on a patients heel. Figure 2. The Epidemiologic Triangle.
102 Home Healthcare Nurse http://www.nursingcenter.com vol. 18 no. 2 February 2000
Agent. The agent of infection is the microorganism
that causes an infection. The agent may be a
bacterium, virus, yeast, fungi, or some other Causative agent
microorganism that can cause human infection.
The mere presence of microorganisms is not
necessarily a risk to the patient. Many bacteria are
normal flora found in various anatomic sites, such
susceptible host Reservoir
as the normal colonization of the intestinal tract
with E. coli and other bowel flora.
Mode of Transmission. The mode of transmission
is the transfer of the infectious agent from its
environment or reservoir to a susceptible host.
Portal of entry Portal of exit
There are five modes of transmission:
1. Contact (direct and indirect),
2. Droplet, Mode of transmission
3. Airborne,
4. Vector-borne (disease spread by insects, such
as malaria), and
5. Vehicle (disease spread by a common source
Figure 3. The Chain of Infection.
such as contaminated water or seafood).
Infection control strategies related to patient not susceptible to the infection. For example, a
care, including isolation precautions, focus on home care staff member may, through a needle
contact transmission, droplet transmission, and stick, be exposed to a patient infected with he-
airborne transmission. patitis B. However, if the home care staff member
has received the hepatitis B vaccine and is im-
Chain of Infection mune, no infection will occur. Thus, all of these
All three elements within the epidemiologic trian- factors must be considered when evaluating the
gle must be present for a patient to become in- risk of infection and determining the appropriate
fected; however, an infection will not always procedures to decrease risk.
occur in the presence of all three elements. Infec-
tion depends on the characteristics of the agent ASSESSING THE RISK OF
and host, as well as the potential for transmission. INFECTION FROM HOME CARE
All of the variables in the chain of infection must EQUIPMENT
be considered in the assessment of infection risk. Assessing the risk of person-to-person transmis-
First, although there is a reservoir or source of sion is frequently more straightforward than as-
infection, there must be a portal of exit. For ex- sessing the risk and determining the appropriate
ample, an individual may be infected with hepati- control measures when inanimate objects or home
tis B, but they will not transmit the virus unless care equipment are involved. In home care, only a
there is bleeding, excretion of bloody body fluids, few select items are reused from one patient to an-
or sexual contact. In addition, the susceptible pa- other (e.g., stethoscope, sphygmomanometer,
tient must be exposed through a portal of entry. thermometer, scale). When determining the po-
Touching the intact skin of a person with any tential risk related to reusing equipment on more
bloodborne disease does not cause exposure or than one patient, the scheme developed by E. H.
transmission. Spaulding is most useful (Spaulding, 1968).
A portal of entry for transmission of hepatitis B Spaulding divided all medical devices into
might be a needlestick or sharps injury, exposure three categories (i.e., noncritical, semicritical,
to blood via nonintact skin, or a splash to mucous and critical) and provided guidance for the level
membrane. However, even if there is a reservoir of cleaning and disinfecting that is necessary after
of infection and a portal of exit and entry, there use based on the risk of infection transmission
still may not be a risk for infection if the patient is from the object.
vol. 18 no. 2 February 2000 http://www.nursingcenter.com Home Healthcare Nurse 103
SPALDINGS CATEGORIES
FOR CLEANING AND example, the question regarding the
DISINFECTING OBJECTS appropriate time frame for use of irri-
gating solutions is frequently posed.
Noncritical Devices are those that only touch intact skin. These Should solutions be discarded every
items are considered low risk and only require cleaning or low-level 24 hours, 48 hours, or once a week?
disinfection when visibly soiled. Examples of noncritical devices Because there is no data on the
used in the home setting include blood pressure cuffs, scales, and ideal or necessary time frame for use,
stethoscopes. an attempt should be made to select a
reasonable quantity (e.g., 150 ml. ver-
Semicritical Items are those that come into contact with nonintact sus 500 ml.) that will be used within a
skin and mucus membrane. These items require intermediate level reasonable period of time (e.g., one or
disinfection before being used on another patient. Examples of semi- two visits or days). To add to the mar-
critical devices used in the home setting include respiratory therapy gin of safety, the solution should be
stored in a manner that will minimize
equipment and oral thermometers.
potential for contamination (Rhine-
Critical Items are those that contact sterile body spaces, such as the hart & Friedman, 1999).
urinary bladder or the venous system, and should be sterile for use Another area of uncertainty is the
and discarded. Examples of critical devices used in the home setting use of sterile versus clean technique.
Some patient care practices requiring
include indwelling urethral catheters and intravenous catheters.
aseptic technique in the hospital can
be provided safely in the home using
clean technique, although there may
A common example of ritualistic behavior re- be no reference or data for this practice. For ex-
lated to patient equipment is the routine disinfec- ample, experience and anecdotal evidence shows
tion of noncritical medical devices such as stetho- that intermittent urinary catheterization can be
scopes and blood pressure cuffs in between home safely accomplished as a clean procedure in the
visits and patient use. Items that do not ordinarily home. Tracheostomy care and suctioning are also
touch the patient (e.g., the nursing supply bag) or frequently performed using clean technique in the
touch only intact skin (e.g., a scale) are generally home but always performed using aseptic tech-
not involved in disease transmission and do not nique in a hospital or other institutional setting.
require cleaning or disinfection between every
use on different patients. In most cases, these MOVING FORWARD:
items need only be cleaned when they are visibly BASING HOME CARE
soiled. However, the presence of multi-drug resis- PRACTICE ON SCIENCE
tant microorganisms is an exception. Unfortunately, some unnecessary infection control
If a patient is infected or colonized with van- practices have been reinforced during home care
comycin-resistant enterocci (VRE) or other mul- surveys conducted by state, federal, and/or volun-
tidrug-resistant microorganism (e.g., Methicillin tary accrediting bodies. When the surveyor re-
Resistant Staph aureus), the noncritical item views the care being provided in the home by the
should be cleaned with a low-level disinfectant or home care or hospice staff members, he or she will
the item should be assigned to the colonized or observe for breaches in applicable state or federal
infected patient exclusively (CDC, 1995). This rec- laws and regulations. The surveyor will also note
ommendation is based upon surveillance data whether the staff follow the home care or hospices
and evidence of transmission of multidrug-resis- own policies and procedures without necessarily
tant microorganisms in the acute care setting. examining the appropriateness of the practice.
For example, if the policies and procedures
PRACTICE WITHOUT DATA state that staff must use barriers under the nurs-
With a lack of recommendations for patient care ing supply bag and this procedure is not followed,
practice specifically addressing home care and lit- a deficiency or recommendation may be cited. It
tle or no data on the incidence of home care-ac- does not necessarily mean that the policy was
quired infection, home care nurses must apply sci- reasonable in its requirements for infection pre-
entific principles along with common sense to vention and control. When infection control pro-
address these issues and protect their patients. For cedures are followed in a particular manner with-
104 Home Healthcare Nurse http://www.nursingcenter.com vol. 18 no. 2 February 2000
out comment from the surveyor, the home care or share their results through meetings and publica-
hospice organizations staff often conclude that tions. This will allow home care and hospice or-
they must be following proper procedures be- ganizations to move their patient care practice
cause the surveyor said nothing. from ritual to a sound, scientific basis.
Based on anecdotal reports, many home care
and hospice organizations continue ritualistic or REFERENCES
unnecessary practices because the surveyor told Centers for Disease Control and Prevention. (1995). Rec-
the organizations staff that that was the way a ommendations for preventing the spread of van-
certain technique should be performed. Under- comycin resistance: Recommendations of the hospi-
standably, a home care staff member may hesitate tal infection control practices advisory committee
(HICPAC). American Journal of Infection Control, 23
to challenge a surveyors recommendation at that
(2), 8794.
time and the surveyor may fail to provide a refer-
Danzig, L., Short, L., Collins, K., Mahoney, M., Sepe, S.,
ence or a scientific basis for his or her comment. Bland, L., & Jarvis, W. (1995). Bloodstream infections
Some home care and hospice organizations are associated with a needleless intravenous infusion
hesitant to abandon the ritualistic practice of nurs- system in patients receiving home infusion therapy.
ing bag technique because in certain states their Journal of the American Medical Association, 273(23),
surveyor wants to see them use barriers. For a 18621864.
surveyor to make a valid citation to a home care or Emori, G., Culver, D., & Horan, T. (1991). National noso-
hospice organization for breaches in infection con- comial infections surveillance system (NNIS): De-
trol practice, the finding(s) must be based on stan- scription of surveillance methods. American Journal
dards of practice or scientific data. If surveyors of Infection Control, 19, 259267.
Garner, J. S. (1996). Guideline for isolation precautions
in hospitals. Infection Control and Hospital Epidemiol-
With a lack of recommendations for patient care ogy, 17(1), 5380.
practice specifically addressing home care and little Garner, J., & Favero, M. (1986). CDC Guideline for hand-
or no data on the incidence of home care-acquired washing and hospital environmental control, 1985.
infection, home care nurses must apply scientific American Journal of Infection Control, 14(3), 110129.
Garner, J., Jarvis, W., Emori, T., Horan, T., & Hughes, J.
principles along with common sense to address these
(1988). CDC definitions for nosocomial infection.
issues and protect their patients.
American Journal of Infection Control, 16, 2840.
Garner, J., & Favero, M. (1986). CDC Guideline for hand-
give any direction for infection control practice washing and hospital environmental control, 1985.
that does not appear sound, the home care or hos- American Journal of Infection Control, 14(3), 110129.
Health Care Finance Administration. (1996, April).
pice organization should request more specific in-
Medicare Home Health Agency Manual. Revised Mate-
formation and rationale for the recommendation
rial. Transmittal No. 277.
in an open, nonconfrontational manner. Kellerman, S., Shay. D., Howard, J., Goes, C., Feusner, J.,
Ritualistic practices should be carefully exam- Rosenberg, J., Vugia, D., & Jarvis, W. (1996). Blood-
ined to determine their validity based upon a sci- stream infections in home infusion patients: The in-
entific model (i.e., epidemiologic triangle and fluence of race and needleless intravascular access
chain of infection). Practices that are determined devices. Journal of Pediatrics, 129(5), 711717.
to be unnecessary and do not contribute to re- Rhinehart, E., & Friedman, M. (1999). Infection Control in
ducing infection risk should be eliminated. Home Care. Gaithersburg, MD: Aspen.
Home care and hospice organizations will be un- Soule, B. (Ed.). (1983). The APIC Curriculum for Infection Con-
able to base their practice on outcome data until fur- trol Practice. Dubuque, IA: Kendall/Hunt Publishing Co.
Spaulding, E. H. (1968). Chemical disinfection of medical
ther progress in the surveillance of home care-ac-
and surgical materials. In C. A. Lawrence, & S. S.
quired infection is made. This will be difficult until
Block (Eds.), Disinfection, Sterilization, and Preserva-
specific definitions for home care-acquired infec- tion (pp. 517531). Philadelphia: Lea & Febiger.
tions and methods for surveillance are developed White, M., & Ragland, K., (1993). Surveillance of intra-
and standardized. Without standardized definitions venous catheter-related infections among home care
and methods it will be difficult to determine the ac- clients. American Journal of Infection Control, 21,
tual risks for home care-acquired infections and the 231235.
effectiveness of specific infection control measures. Wong, E. S. (1983). Guideline for prevention of catheter-
It is imperative that home care organizations associated urinary tract infections. American Journal
begin to collect data in an organized fashion and of Infection Control, 11, 2831.
vol. 18 no. 2 February 2000 http://www.nursingcenter.com Home Healthcare Nurse 105
www.homehealthcarenurse.com
Continuing Education Test To earn continuing education (CE) credit, follow these instructions:
1. Read the article on page 99. Complete sections A, B, and C* on the Wilkins is accredited as a provider of CE in nursing by the
enrollment coupon. Each question has only one correct answer. American Nurses Credentialing Centers Commission on
2. Send the coupon with your $11.25 registration fee to: Continuing Accreditation. Lippincott Williams & Wilkins is also an approved
Education Department, Lippincott Williams & Wilkins, 345 Hud- provider of nursing CE in Alabama, California, Florida, and Iowa
son Street, New York, NY 10014. and holds the following provider numbers: AL #ABNP0114; CA
#CEP11749; FL #27F0002; IA #75. All of its home study offerings are
1.5 hours Within 6 weeks youll be notified of your test results. A passing classified for Texas nursing CE requirements as Type I.
score for this test is 15 correct answers. If you pass, you will *In accordance with the Iowa Board of Nursing Administrative rules governing
receive a certificate of completion. If you fail, you have the option grievances, a copy of your evaluation of the CE offering (section C) may be submitted
of taking the test again at no additional cost. Lippincott Williams & directly to the Iowa Board of Nursing.
CE Test: Improving Infection Control in Home Care: From Ritual to Science-Based Practice
Mary M. Friedman, MS, RN, CRNI, and Emily Rhinehart, RN, MPH, CIC, CPHQ
General Purpose 5. According to the Centers for Disease Control, how 13. Infection control strategies related to patient care
To introduce the registered professional nurse to the sci- often should Foley catheters be changed? usually relate to all of the following except
entific basis of infection control in the home. a. every 30 days a. contact transmission. c. airborne transmission.
b. every 60 days b. droplet transmission. d. vehicle transmission.
Objectives c. at fixed intervals upon the request of the client
14. According to E. H. Spaulding, a semicritical device is
After reading this article and taking the following test d. when complications occur
you will be able to: one that
1. Identify current infection control practices in home 6. Improper disposal of non-sharp items in a sharps a. touches only intact skin.
care and hospice. container can lead to all of the following except b. contacts mucous membranes.
2. Discuss the effectiveness of current practices. a. increased agency costs for disposal of items. c. requires low-level disinfection.
3. Defend infection control practices that vary from tra- b. fines to agency for incorrect disposal techniques. d. should be sterile for use.
ditional practice. c. waste of agency resources.
15. Noncritical medical devices should be assigned for
d. complaints from contracted medical waste disposal
use to one patient exclusively when the client
Questions companies.
a. is infected with a multi-drug resistant microorganism.
1. In general, infection control and prevention strate- 7. A new nurse at your agency asks you about blood b. is on intravenous antibiotics.
gies in home care have been borne pathogen rules. Because you are late for a c. has a history of hepatitis.
a. developed after careful scientific research. meeting you refer her to the d. tests positive for HIV.
b. identified as rigid and unvaried. a. Health Care Financing Administration (HCFA).
16. Which of these statements regarding the storage of
c. reproduced from acute care experiences. b. Office of Inspector General (OIG).
solutions in the home is correct?
d. constructed with the assistance of numerous external c. Occupational Safety and Health Administration (OSHA).
a. Solutions are to be discarded after 24 hours.
resources. d. Department of Health Services (DHS).
b. Solutions are to be discarded after 48 hours.
2. Surveillance of home care infections differs from that 8. Elements of the epidemiologic triangle include c. Length of time solutions may be kept is OSHA regulated.
of the hospital in which of the following ways? which three interrelated components? d. Length varies based on agency policy.
a. review of laboratory data a. host-agent-environment
17. A home procedure in which sterility must be main-
b. visiting clinical areas b. host-agent-host
tained is
c. reviewing medical records c. host-genetic core-environment
A. tracheostomy care.
d. reliance on professional nursing staff d. social environment-host-agent
B. intravenous therapy.
3. During orientation a home care nurse learns about 9. A factor that is not a link in the chain of infection is C. intermittent urinary catheterization.
bag technique. Which of the following statements a. portal of exit. D. enteral feedings.
regarding this technique is true? b. nonsusceptible host.
18. During surveys, it is most critical to
a. Never set the bag directly on the floor. c. reservoir.
a. perform procedures as taught by your preceptor.
b. You must wash your hands each and every time you d. mode of transmission.
b. follow agency policy and procedures.
enter the nursing bag. 10. A susceptible host c. discard soiled dressings in biohazard bags.
c. Research supports the designation of a clean and a. displays active immunity. d. adapt the procedure to the surveyors specifications.
dirty side of the bag. b. causes an infection.
d. There is no scientific basis for placing a barrier under 19. According to the author, home care infection control
c. receives an immunization.
the nursing bag. practices are based on
d. is not immune.
a. reliable external resources. c. scientific data.
4. Scientific infection control principles indicate that a 11. E. coli is normally found within which system? b. rituals. d. past outcomes of care.
soiled item that cannot be disinfected in the home a. Gastrointestinal c. Cardiovascular
a. can be placed directly inside the nursing bag. 20. In order for a surveyor to cite a home care organiza-
b. Respiratory d. Endocrine
b. can be placed in a separate container for transport to tion for breaches in infection control, the finding
the office. 12. Transmission of an infection by a mosquito is known as must be based on
c. can be left out and hand-carried to the office for cleaning. a. vector-borne. c. contact. a. standards of practice.
d. can be rinsed off immediately in the patients home, b. droplet. d. vehicle. b. surveyors practice experiences.
then transported to the office. c. theoretical data.
d. nonspecific information.
A Lippincott Williams & Wilkins CE Home Study Enrollment Course B
Test Responses: Darken one for
your answer to each question.
Improving Infection Control in Home Care: From Ritual to Science-Based Practice
1. a b c d 11. a b c d
CE Credit: 1.5 Contact Hours Fee: $11.25 Registration Deadline: February 28, 2002
2. a b c d 12. a b c d
Please check all that apply: LPN RN CNS NP CRNA CNM Other ______________________
SS# __________________________________ Are you certified? Yes No 3. a b c d 13. a b c d
Certified by__________________________________________________________Telephone # _______________________ 4. a b c d 14. a b c d
Last Name ______________________________________________ First Name ___________________________ MI______ 5. a b c d 15. a b c d
Address ___________________________________________________ City ______________ State _____ Zip___________ 6. a b c d 16. a b c d
State of Licensure #1 _______ License No. #1 _____________ State of Licensure #2 _______ License No. #2 ____________
7. a b c d 17. a b c d
Position Title _____________________________________ Area of Specialty _____________________________________
8. a b c d 18. a b c d
C 1. Did this CE activitys learning objectives relate to its general purpose? Y N 9. a b c d 19. a b c d
2. Was the journal home study format an effective way to present the material? Y N 10. a b c d 20. a b c d
3. Was the content current to nursing practice? Y N
4. How long did it take you to complete this CE activity? _______ hours
5. Suggestions for future topics _____________________________________________________________________
106 Home Healthcare Nurse http://www.nursingcenter.com vol. 18 no. 2 February 2000
You might also like
- Community Health Nursing Advocacy For Population Health 5th Edition PDFDocument2 pagesCommunity Health Nursing Advocacy For Population Health 5th Edition PDFDebra20% (5)
- Nursing Theories and Nursing Practice Third Edition PDFDocument539 pagesNursing Theories and Nursing Practice Third Edition PDFTUTIK SISWATI100% (1)
- Wound Care Giudeline NHS Bolton HospitalDocument44 pagesWound Care Giudeline NHS Bolton HospitalJumatun Mona WarahNo ratings yet
- Lippincott ProceduresDocument3 pagesLippincott ProceduresYmon TuallaNo ratings yet
- BSN Learning Plan Senior CapstoneDocument3 pagesBSN Learning Plan Senior Capstoneapi-258684779100% (1)
- Algorithm-Acls Lvad 200808Document1 pageAlgorithm-Acls Lvad 200808Hyunsoo EllisNo ratings yet
- The New Doctor 09Document52 pagesThe New Doctor 09Almas JanjuaNo ratings yet
- Team Nursing ConferenceDocument9 pagesTeam Nursing ConferenceShesly Philomina100% (5)
- AWMA 2011 Standards For Wound Management v2Document36 pagesAWMA 2011 Standards For Wound Management v2Agung Ginanjar100% (1)
- Api Q0315Document68 pagesApi Q0315Abidi HichemNo ratings yet
- 2011 Advanced Cardiovascular Life Support (Acls) Classroom Course & Materials Frequently Asked Questions (Faqs)Document5 pages2011 Advanced Cardiovascular Life Support (Acls) Classroom Course & Materials Frequently Asked Questions (Faqs)Edogawa RakhmanNo ratings yet
- TOEFL BrochureDocument2 pagesTOEFL BrochureknowledgeIconNo ratings yet
- PMVDocument28 pagesPMVRajesh VermaNo ratings yet
- Chap 10Document29 pagesChap 10Koby100% (5)
- HH Monograph PDFDocument234 pagesHH Monograph PDFAnonymous WmArPQl3BNo ratings yet
- Infection Control Guidelines - Health Canada PDFDocument66 pagesInfection Control Guidelines - Health Canada PDFkimeligioNo ratings yet
- GCOE Provision 4-6Document29 pagesGCOE Provision 4-6Justine May GervacioNo ratings yet
- Updated 10-16-14 Quick Reference Guide Digital Npuap Epuap Pppia 16oct2014Document75 pagesUpdated 10-16-14 Quick Reference Guide Digital Npuap Epuap Pppia 16oct2014Anonymous kZQet6QA100% (1)
- Practical Guidelines Infection Control PDFDocument110 pagesPractical Guidelines Infection Control PDFRao Rizwan Shakoor100% (1)
- ASPEN Critical Care - Susan BrantleyDocument44 pagesASPEN Critical Care - Susan BrantleyVitoria SilvaNo ratings yet
- Patient Safety and Quality Care MovementDocument9 pagesPatient Safety and Quality Care Movementapi-300362983No ratings yet
- Infection Prevention: JhpiegoDocument419 pagesInfection Prevention: JhpiegosimplyrosalynNo ratings yet
- PEARS Handout 2016Document8 pagesPEARS Handout 2016Carrie DAndreaNo ratings yet
- Protocol Final 2014 Last PDFDocument222 pagesProtocol Final 2014 Last PDFAbdelrahman MamdouhNo ratings yet
- Wound CareDocument36 pagesWound CareZulfadli SallehNo ratings yet
- Needle Stick Injyry PolicyDocument16 pagesNeedle Stick Injyry PolicyJery JsNo ratings yet
- Adult Bradycardia Algorithm: Identify and Treat Underlying CauseDocument1 pageAdult Bradycardia Algorithm: Identify and Treat Underlying CausenebrasNo ratings yet
- Medical Surgical BulletDocument9 pagesMedical Surgical Bulletensermu kebebewNo ratings yet
- Wound Forum 14Document12 pagesWound Forum 14Lia Mar'atush SholihahNo ratings yet
- Student Handbook Emergency Medical Technician - BasicDocument47 pagesStudent Handbook Emergency Medical Technician - BasicFolkert WunderlichNo ratings yet
- Ielts WritingDocument16 pagesIelts WritingHiềnAnhNo ratings yet
- Algorithm-ACLS CA in Pregnancy In-Hospital 200612Document1 pageAlgorithm-ACLS CA in Pregnancy In-Hospital 200612Hyunsoo EllisNo ratings yet
- National Clinical Guideline No. 5 Clinical Handover Nov2014Document306 pagesNational Clinical Guideline No. 5 Clinical Handover Nov2014Ahmad JuliadiNo ratings yet
- 5 Storyboard (Contoh 1)Document1 page5 Storyboard (Contoh 1)RaniCianTarNo ratings yet
- 11 Infection Prevention and ControlDocument24 pages11 Infection Prevention and ControlKristian Dave DivaNo ratings yet
- Wound International Best Practice Guidelines Non ComplexDocument27 pagesWound International Best Practice Guidelines Non ComplexEdu WilliamNo ratings yet
- Patient Safety PPT PDFDocument39 pagesPatient Safety PPT PDFGraha KhitanNo ratings yet
- 5 Emergency Action Principles - PPTX JuleslectureDocument55 pages5 Emergency Action Principles - PPTX JuleslectureBessy Ramos100% (1)
- Appetizer For Toefl (PBT)Document77 pagesAppetizer For Toefl (PBT)cocote161No ratings yet
- Wound Infection Best PracticeDocument12 pagesWound Infection Best PracticeAnonymous 1nMTZWmzNo ratings yet
- Safe Injection Practices and Handling of SharpsDocument26 pagesSafe Injection Practices and Handling of SharpsbrightyNo ratings yet
- Infection Control Nurses AssociationDocument43 pagesInfection Control Nurses Associationlelgeorge100% (2)
- Technologies Designed To Help Improve Patients OutcomeDocument53 pagesTechnologies Designed To Help Improve Patients OutcomeHarby Ongbay AbellanosaNo ratings yet
- Mask19Document8 pagesMask19steven saputraNo ratings yet
- Kozier and Erb's Fundamentals of Nursing (3rd Australian Edition)Document24 pagesKozier and Erb's Fundamentals of Nursing (3rd Australian Edition)Christian Paul Capablanca Garcia0% (1)
- British Journal of Nursing Volume 14 Issue 10 2005 (Doi 10.12968/bjon.2005.14.10.18102) Preston, Rosemary M - Aseptic Technique - Evidence-Based Approach For Patient SafetyDocument6 pagesBritish Journal of Nursing Volume 14 Issue 10 2005 (Doi 10.12968/bjon.2005.14.10.18102) Preston, Rosemary M - Aseptic Technique - Evidence-Based Approach For Patient SafetyPriscilla CarmiolNo ratings yet
- CDC ManualDocument764 pagesCDC ManualBryan Astorga Guerrero100% (2)
- Vital Signs and Early Warning ScoresDocument47 pagesVital Signs and Early Warning Scoresdr_nadheem100% (1)
- Introduction To Nursing Research Part 1Document22 pagesIntroduction To Nursing Research Part 1Ciedelle Honey Lou DimaligNo ratings yet
- ENA Leadership Conference 2013 ProgramDocument17 pagesENA Leadership Conference 2013 ProgramEmergency Nurses AssociationNo ratings yet
- Wound ManagementDocument4 pagesWound ManagementnrhmhealthNo ratings yet
- Errors in NursingDocument59 pagesErrors in NursingCzerwin JualesNo ratings yet
- Mark Sta Maria RESUME3Document3 pagesMark Sta Maria RESUME3mak_stamaiaNo ratings yet
- Crash Cart: Marcha M Phillips Hondros College School of NursingDocument5 pagesCrash Cart: Marcha M Phillips Hondros College School of Nursingjenn1722No ratings yet
- Registration and Billing System &CSSDDocument4 pagesRegistration and Billing System &CSSDSthitapragyan senapatiNo ratings yet
- Infection Control and ProphylaxisDocument19 pagesInfection Control and ProphylaxisRechie RechNo ratings yet
- 05 Figure2 1 Environmental Tour FormDocument8 pages05 Figure2 1 Environmental Tour FormErna WahyuningtyasNo ratings yet
- Nsg241 Study Guide Exam 5Document76 pagesNsg241 Study Guide Exam 5NatalieAndersonNo ratings yet
- Golden Ielts - 275 Nguyen Trai, Thanh Xuan, Hanoi: April 21, 2017Document2 pagesGolden Ielts - 275 Nguyen Trai, Thanh Xuan, Hanoi: April 21, 2017Kim Chi VuNo ratings yet
- NURSING THE CHILDBEARING FAMILY: Passbooks Study GuideFrom EverandNURSING THE CHILDBEARING FAMILY: Passbooks Study GuideNo ratings yet
- NURSING CARE OF ADULTS II: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNo ratings yet
- NCLEX-RN Exam Prep 2024-2025: 500 NCLEX-RN Test Prep Questions and Answers with ExplanationsFrom EverandNCLEX-RN Exam Prep 2024-2025: 500 NCLEX-RN Test Prep Questions and Answers with ExplanationsNo ratings yet
- PrintVersion PDFDocument28 pagesPrintVersion PDFUswaPutriemelelaNo ratings yet
- Perceived Stress Scale: Reliability and Validity Study in GreeceDocument12 pagesPerceived Stress Scale: Reliability and Validity Study in Greecegastro fkikunibNo ratings yet
- TYM1 Poster 5 Insulin PDFDocument1 pageTYM1 Poster 5 Insulin PDFUswaPutriemelelaNo ratings yet
- Professional Role Development: Ns. Eliyana, S.Kep., MNSDocument51 pagesProfessional Role Development: Ns. Eliyana, S.Kep., MNSUswaPutriemelelaNo ratings yet
- Satuan Acara Penyuluhan KBDocument7 pagesSatuan Acara Penyuluhan KBUswaPutriemelelaNo ratings yet
- Professional Role Development: Ns. Eliyana, S.Kep., MNSDocument51 pagesProfessional Role Development: Ns. Eliyana, S.Kep., MNSUswaPutriemelelaNo ratings yet
- DR Ganaraja B 2011Document5 pagesDR Ganaraja B 2011UswaPutriemelelaNo ratings yet
- 1 s2.0 S2352013216300436 Main PDFDocument10 pages1 s2.0 S2352013216300436 Main PDFUswaPutriemelelaNo ratings yet
- Satuan Acara Penyuluhan KBDocument7 pagesSatuan Acara Penyuluhan KBUswaPutriemelelaNo ratings yet
- 2-14-1409399244-1.Applied-Relations Among Loneliness, Depression, Anxiety - Jayashree PanickerDocument10 pages2-14-1409399244-1.Applied-Relations Among Loneliness, Depression, Anxiety - Jayashree PanickerUswaPutriemelelaNo ratings yet
- DR Ganaraja B 2011Document5 pagesDR Ganaraja B 2011UswaPutriemelelaNo ratings yet
- Meeting 2.3.latihan Menyusun Abstrak-1Document3 pagesMeeting 2.3.latihan Menyusun Abstrak-1UswaPutriemelelaNo ratings yet
- Aristawati, DKKDocument8 pagesAristawati, DKKUswaPutriemelelaNo ratings yet
- Global Health PDFDocument32 pagesGlobal Health PDFYhan-yhan Rodriguez KhouNo ratings yet
- Laila Ely Vol 8 Juli 2012Document7 pagesLaila Ely Vol 8 Juli 2012UswaPutriemelelaNo ratings yet
- E83105Document19 pagesE83105UswaPutriemelelaNo ratings yet
- 1 SMDocument7 pages1 SMwirajatiNo ratings yet
- 1 SMDocument7 pages1 SMwirajatiNo ratings yet
- Curriculum, Planning and DevelopmentDocument3 pagesCurriculum, Planning and DevelopmentMIbrahimNo ratings yet
- Challenges of Being A Critical Care NurseDocument14 pagesChallenges of Being A Critical Care NurseKatie PurryNo ratings yet
- Establishment of Nursing SchoolDocument82 pagesEstablishment of Nursing SchoolRadhaNo ratings yet
- Nursing BulletsDocument88 pagesNursing BulletsEunice Lorraine Reyes MarasiganNo ratings yet
- ScriptDocument7 pagesScriptD A M N E R ANo ratings yet
- Near DrowningDocument15 pagesNear DrowningshenysusantisinaNo ratings yet
- MDCCCDocument2 pagesMDCCCMaria DianeNo ratings yet
- Example Physical Assessment PDF FormatDocument2 pagesExample Physical Assessment PDF FormatJasonNo ratings yet
- TheCompassionCompetenceScale StudentNursesDocument10 pagesTheCompassionCompetenceScale StudentNursesvirieguiaNo ratings yet
- Foreword I II General Overview 4Document54 pagesForeword I II General Overview 4Becca SalvadorNo ratings yet
- Past Student BiosDocument3 pagesPast Student BiosGary PierceyNo ratings yet
- Nursing Care Plan-1 Age: 50Y Medical Diagnoses: Leukemia Assessment Nursing Diagnosis Planning Intervention Scientific Rationale EvaluationDocument1 pageNursing Care Plan-1 Age: 50Y Medical Diagnoses: Leukemia Assessment Nursing Diagnosis Planning Intervention Scientific Rationale EvaluationBheru LalNo ratings yet
- Module 5: Family Nursing Process: Family Nursing Care PlanDocument2 pagesModule 5: Family Nursing Process: Family Nursing Care PlanTanya Alyssa Untalan AquinoNo ratings yet
- Home Health Services VisitsDocument29 pagesHome Health Services Visitsmery eka yaya fujiantiNo ratings yet
- Family Health AssessmentDocument47 pagesFamily Health Assessmentangeleigh viernesNo ratings yet
- Module 12 13Document6 pagesModule 12 13Noisy KenNo ratings yet
- Who Ecsa FrameworkDocument5 pagesWho Ecsa FrameworkJPNo ratings yet
- n82 - Procedure For Aural ToiletDocument2 pagesn82 - Procedure For Aural ToiletDaniel Tanri Rannu100% (1)
- WHO Global Strategyworkforce2030 PDFDocument48 pagesWHO Global Strategyworkforce2030 PDFgmantzaNo ratings yet
- Chapter 20 - Postoperative Nursing ManagementDocument17 pagesChapter 20 - Postoperative Nursing ManagementTeemara KingNo ratings yet
- Konsep Proses KeperawatanDocument20 pagesKonsep Proses KeperawatanriskaNo ratings yet
- Health Delegate - Primary Health Care Nurse (20464)Document1 pageHealth Delegate - Primary Health Care Nurse (20464)Enrique Salvador Padial RamosNo ratings yet
- What Makes Team Communication Effective: A Qualitative Analysis of Interprofessional Primary Care Team Members' PerspectivesDocument4 pagesWhat Makes Team Communication Effective: A Qualitative Analysis of Interprofessional Primary Care Team Members' PerspectivesjovanaNo ratings yet
- Modern Concept of Child CareDocument209 pagesModern Concept of Child CareSadhu PriyankaNo ratings yet
- Jonathan Onigama n362 Cover Letter Resume 11 6 2015 RevisedDocument3 pagesJonathan Onigama n362 Cover Letter Resume 11 6 2015 Revisedapi-302664277No ratings yet
- Test Bank For Maternal Child Nursing 5th Edition by Mckinney For 29 99Document24 pagesTest Bank For Maternal Child Nursing 5th Edition by Mckinney For 29 99GabriellaMartinwfon100% (50)
- PS - Reduction of Patient Restraint and Seclusion in Health Care SettingsDocument15 pagesPS - Reduction of Patient Restraint and Seclusion in Health Care SettingsEndang Sri PurwantiNo ratings yet