Professional Documents
Culture Documents
Uti Aimj
Uploaded by
Roberto López MataOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Uti Aimj
Uploaded by
Roberto López MataCopyright:
Available Formats
Annals of Internal Medicine
In the Clinic
Urinary Tract
Infection Screening and Prevention
U
rinary tract infections (UTIs) are common
in both inpatient and outpatient settings.
This article provides an evidence-based,
Diagnosis and Evaluation
clinically relevant overview of management of
UTIs, including screening, diagnosis, treatment,
and prevention. Conditions covered include
acute cystitis (both uncomplicated and compli- Treatment and Management
cated), catheter-associated UTI, and asymptom-
atic bacteriuria in both women and men.
Practice Improvement
CME/MOC activity available at Annals.org.
Physician Writer doi:10.7326/AITC201710030
Kalpana Gupta, MD, MPH
Larissa Grigoryan, MD, PhD CME Objective: To review current evidence for screening, prevention, diagnosis, evaluation,
Barbara Trautner, MD, PhD treatment, management, and practice improvement of urinary tract infection.
From VA Boston Healthcare Funding Source: American College of Physicians.
System and Boston University
School of Medicine, Boston, Disclosures: Dr. Gupta, ACP Contributing Author, reports personal fees from Paratek
Massachusetts; Center for Pharmaceuticals, Iterum Therapeutics, Tetraphase Pharmaceuticals, Ocean Spray, UpToDate,
Innovations in Quality, and Melinta Therapeutics outside the submitted work and chairs the Infectious Diseases
Effectiveness, and Safety at Society of America guidelines on urinary tract infection. Dr. Grigoryan, ACP Contributing
the Michael E. DeBakey Author, reports a grant from Zambon Pharmaceuticals outside the submitted work. Dr.
Veterans Affairs Medical Trautner, ACP Contributing Author, reports grants from the National Institutes of Health, the
Center and Baylor College of U.S. Department of Veterans Affairs Health Services Research and Development Service, and
Medicine, Houston, Texas; Zambon Pharmaceuticals and other support from Zambon Pharmaceuticals outside the
and Houston VA Health submitted work. Disclosures can also be viewed at www.acponline.org/authors/icmje
Services Research and /ConictOfInterestForms.do?msNum=M17-1676.
Development Center of With the assistance of additional physician writers, the editors of Annals of Internal
Excellence, and Baylor College Medicine develop In the Clinic using MKSAP and other resources of the American
of Medicine, Houston, Texas. College of Physicians.
In the Clinic does not necessarily represent ofcial ACP clinical policy. For ACP clinical
guidelines, please go to https://www.acponline.org/clinical_information/guidelines/.
2017 American College of Physicians
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
Urinary tract infections (UTIs) are long-term (30 days) indwelling
common in both outpatient and catheters. As men age, acquired
inpatient settings. Clinical entities abnormalities of the urinary tract
encompassed by the term UTI impair normal bladder emptying,
include asymptomatic bacteriuria which narrows the sex-based dif-
(ASB), acute uncomplicated cysti- ference in UTI rates (2).
tis, recurrent cystitis, catheter-
associated ASB, catheter- The strongest risk factors in pre-
associated UTI (CAUTI), prostatitis, menopausal women include sex-
and pyelonephritis. These catego- ual intercourse, use of spermi-
ries are further distinguished by cides, and previous UTI. A history
the presence or absence of symp- of maternal UTI and age at rst UTI
1. Hooton TM, Scholes D, toms referable to the urinary tract are also important risk factors in
Hughes JP, Winter C,
Roberts PL, Stapleton AE, and the patient's sex, comorbid this group, suggesting a genetic
et al. A prospective study
conditions, and genitourinary his- component to susceptibility (3).
of risk factors for symp-
tomatic urinary tract infec- tory, including the presence of Pregnant women are also at in-
tion in young women.
stones, stents, or catheters. Be- creased risk. Changes in vaginal
N Engl J Med. 1996;335:
468-74. [PMID: 8672152] cause acute cystitis is the most microbial ora in perimenopausal
2. Schaeffer AJ, Nicolle LE.
Urinary tract infections in common manifestation of UTI and women may increase risk for UTI.
older men [Letter]. N Engl
is most prevalent in women, most In contrast to the predominant role
J Med. 2016;374:2192.
[PMID: 27248641] clinical research on UTI has been of behavioral risk factors in pre-
3. Scholes D, Hooton TM,
done in women. Clinicians must menopausal women, mechanical
Roberts PL, Stapleton AE,
Gupta K, Stamm WE. Risk consider whether recommenda- and physiologic factors that affect
factors for recurrent uri-
nary tract infection in tions derived from this evidence bladder emptying are important in
young women. J Infect
base are applicable to their patient postmenopausal women (4). Dia-
Dis. 2000;182:1177-82.
[PMID: 10979915] populations. betes increases risk for all urinary
4. Hooton TM. Recurrent infectious disorders, from ASB to
urinary tract infection in
women. Int J Antimicrob In the absence of known abnor- perirenal abscess and emphyse-
Agents. 2001;17:259-68.
[PMID: 11295405]
malities of the urinary tract, women matous pyelonephritis (5). In men,
5. Hooton TM. Pathogenesis are at higher risk for UTIs than risk for UTI is primarily related to
of urinary tract infections:
an update. J Antimicrob men. Premenopausal women are prostatic hypertrophy that occurs
Chemother. 2000;46 at especially high risk for acute with advancing age. Temporary
Suppl 1:1-7. [PMID:
11051617] cystitisincidence is 0.5 0.7 case urinary catheterization is the major
6. Nicolle LE, Bradley S,
Colgan R, Rice JC, Schaef-
per person-year among sexually medical intervention that increases
fer A, Hooton TM; Infec- active women (1). Other popula- risk for UTI. Other comorbid condi-
tious Diseases Society of
America. Infectious Dis- tions at risk for UTI include patients tions that increase risk in both
eases Society of America with voiding abnormalities related sexes include the presence of
guidelines for the diagno-
sis and treatment of to diabetes; neurogenic bladder; stones or foreign bodies (such as
asymptomatic bacteriuria
in adults. Clin Infect Dis.
spinal cord injury; pregnancy; ureteral stents) in the urinary sys-
2005;40:643-54. [PMID: prostatic hypertrophy; or urinary tem and diseases associated with
15714408]
7. Abrutyn E, Mossey J, Ber- tract instrumentation, including neurogenic bladder.
lin JA, Boscia J, Levison M,
Pitsakis P, et al. Does
asymptomatic bacteriuria
predict mortality and does
antimicrobial treatment
Screening and Prevention
reduce mortality in elderly
ambulatory women? Ann
Is there a role for screening for does not decrease this risk (8).
Intern Med. 1994;120: UTI or ASB? ASB is a marker for poor overall
827-33. [PMID: 7818631]
8. Hooton TM, Scholes D, In men and nonpregnant women, health status in diabetic patients,
Stapleton AE, Roberts PL,
screening for ASB is generally noncatheterized women in retire-
Winter C, Gupta K, et al.
A prospective study of not recommended because ment homes, and catheterized
asymptomatic bacteriuria inpatients but is not an indepen-
in sexually active young treatment does not improve clini-
women. N Engl J Med. dent risk factor for death.
2000;343:992-7. [PMID: cal outcomes (6). ASB does not
11018165] lead to hypertension, chronic kid-
9. Wing DA, Fassett MJ,
ASB during pregnancy (4%7% of
Getahun D. Acute pyelo- ney disease, or decreased dura- pregnant women) is associated
nephritis in pregnancy: an
18-year retrospective anal- tion of survival (7). Women with with progression to symptomatic
ysis. Am J Obstet Gynecol.
2014;210:219.e1-6.
ASB are at increased risk for UTI, including pyelonephritis (9).
[PMID: 24100227] symptomatic UTI, but treatment Acute pyelonephritis occurs in up
2017 American College of Physicians ITC50 In the Clinic Annals of Internal Medicine 3 October 2017
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
to 2% of pregnancies in the ter placement and cystoscopy
United States and is the most without biopsy do not warrant
common nonobstetric cause of screening for ASB.
hospitalization during pregnancy
(9). ASB during pregnancy is also Renal transplant recipients who
associated with low birthweight have ASB are at higher risk for pye-
and preterm labor, although a lonephritis, but whether pyelone-
causative relationship has not phritis affects graft function is con-
been established. troversial (12, 13). The relationship
of ASB to UTI and sepsis in pa-
The most recent Cochrane review (10) on this tients with neutropenia has not
topic found that antibiotic treatment of ASB was been well-studied. Bacteriuria di-
associated with signicantly decreased risk for py- agnosed in neutropenic patients
elonephritis, premature birth, and low birth- as part of a fever work-up is by
weight compared with no treatment. However, denition symptomatic.
the 14 included studies were done between
1960 and 1987, and the risk of bias was judged How can UTI be prevented?
to be high. The quality of the evidence was Prevention of symptomatic UTI in
judged to be very low (pyelonephritis) and low patients with ASB is recom-
(prematurity and low birthweight). mended only in pregnant women
A cohort study of 4283 healthy pregnant or before an invasive urologic pro-
women in the Netherlands who had very low cedure. Urine culture should be
risk for preterm delivery found much lower done and infection should be
rates of pyelonephritis than previous studies treated with directed antimicrobial
(11). The proportion of pregnant women with therapy based on culture results.
untreated ASB who developed pyelonephritis
was 5 of 208 (2.4%) compared with 24 of Symptomatic UTI in women with
4034 (0.6%) without ASB (odds ratio [OR], 3.9 recurrent episodes can be pre-
[95% CI, 1.4 11.4]). Women with untreated vented with antimicrobial prophy-
ASB were also more likely than those without laxis. This decision should be indi-
ASB to have subsequent UTI treated with anti- vidualized. Given increasing 10. Smaill FM, Vazquez JC.
biotics during pregnancy (OR, 2.9 [CI, 2.0 antimicrobial resistance, regular Antibiotics for asymp-
4.2]) and recurrent UTI treated with antibiotics tomatic bacteriuria in
use of antimicrobials to prevent pregnancy. Cochrane
during pregnancy (OR, 3.5 [CI, 1.8 6.7]). Database Syst Rev. 2015:
UTI may not be appealing, and CD000490. [PMID:
Screening for and treatment of approaches other than antimicro- 26252501]
11. Kazemier BM, Koning-
ASB are also recommended be- bial prophylaxis, such as patient- stein FN, Schneeberger
C, Ott A, Bossuyt PM, de
fore transurethral resection of the initiated therapy or nonantimicro- Miranda E, et al. Mater-
prostate (TURP) or other urinary bial prevention, may be preferred nal and neonatal conse-
quences of treated and
tract instrumentation resulting in even if they are less effective in untreated asymptomatic
reducing symptomatic events. If bacteriuria in pregnancy:
mucosal bleeding. Studies have a prospective cohort
shown that TURP in bacteriuric antibiotics are used to prevent re- study with an embedded
randomised controlled
men can precipitate bacteremia current UTI, they may be pre- trial. Lancet Infect Dis.
with associated sepsis and that scribed postcoitally or continu- 2015;15:1324-33.
[PMID: 26255208]
antimicrobial treatment of the ously. Postcoital antibiotic 12. Fiorante S, Fernandez-
Ruiz M, Lopez-Medrano
bacteriuria can prevent these prophylaxis has been shown to be F, Lizasoain M, Lalueza A,
complications. The level of risk highly effective in preventing Morales JM, et al. Acute
graft pyelonephritis in
associated with specic invasive symptomatic recurrences in renal transplant recipi-
urologic procedures other than women with 3 4 UTIs per year, ents: incidence, risk
factors and long-term
TURP in patients with preexisting particularly if these are temporally outcome. Nephrol Dial
Transplant. 2011;26:
bacteriuria is not well-dened. associated with coitus. 1065-73. [PMID:
However, the Infectious Diseases 20805254]
A randomized, double-blind, placebo- 13. Fiorante S, Lopez-
Society of America (IDSA) recom- Medrano F, Lizasoain M,
controlled trial found that among women with Lalueza A, Juan RS, An-
mends that procedures antici- at least 2 culture-documented UTIs in the previ- dres A, et al. Systematic
pated to cause mucosal bleeding ous year, postcoital use of a single dose of trim- screening and treatment
of asymptomatic bacteri-
warrant screening by urine cul- ethoprimsulfamethoxazole (TMPSMX) (40 mg uria in renal transplant
ture and treatment of ASB before recipients. Kidney Int.
plus 200 mg) resulted in an infection rate of 0.3 2010;78:774-81. [PMID:
the procedure (6). Simple cathe- per patient per year compared with 3.6 per pa- 20720526]
3 October 2017 Annals of Internal Medicine In the Clinic ITC51 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
tient per year in the control group (14). Adverse A randomized trial found a potentially protec-
effects were infrequent and minor. In women tive effect on recurrent UTI with cranberry prod-
who are intolerant of or resistant to TMPSMX, an ucts compared with placebo; however, the
14. Stapleton A, Latham RH,
alternative agent (such as nitrofurantoin macro- study was underpowered (18). Another ran-
Johnson C, Stamm WE. crystals or a uoroquinolone) may be as effective domized controlled trial of twice-daily cran-
Postcoital antimicrobial
prophylaxis for recurrent
as TMPSMX for postcoital prophylaxis, although berry juice consumption versus placebo found
urinary tract infection. A clinical evidence specically related to postcoital no between-group difference in the rate of
randomized, double- use is not available for these agents.
blind, placebo-controlled UTI recurrence (19). In a recent randomized
trial. JAMA. 1990;264: double-blind trial of women in nursing homes,
703-6. [PMID: 2197450] For women with more frequent
15. Albert X, Huertas I, no signicant difference was observed for any
Pereiro II, Sanfelix J, recurrences, more frequent co-
of the clinical or microbiologic outcomes (20).
Gosalbes V, Perrota C. itus, or recurrences temporally In another trial that included premenopausal
Antibiotics for preventing
recurrent urinary tract unrelated to coitus, continuous women with complicated and uncomplicated
infection in non- (daily, thrice-weekly, or weekly)
pregnant women. recurrent UTI, TMPSMX was more effective at
Cochrane Database Syst prophylaxis may be preferable, preventing recurrent UTI than cranberry cap-
Rev. 2004:CD001209.
[PMID: 15266443] with dosing frequency tailored to sules, but at the expense of promoting antibi-
16. Schwenger EM, Tejani the individual patient's response. otic resistance (21). Daily consumption of a
AM, Loewen PS. Probiot-
ics for preventing urinary However, rates decrease only cranberry beverage decreased the number of
tract infections in adults during the active prophylaxis pe-
and children. Cochrane
clinical UTIs in a randomized, double-blind,
Database Syst Rev. 2015: riod and in many cases return to placebo-controlled, multicenter study that in-
CD008772. [PMID:
26695595] baseline levels after antimicrobial cluded women with a recent UTI (22). The
17. Mike LA, Smith SN, Sum- therapy is discontinued. Because number of antibiotic courses for symptomatic
ner CA, Eaton KA, Mob-
ley HL. Siderophore some women may not wish to UTIs also was reduced in the cranberry group
vaccine conjugates pro- take prophylactic antibiotics reg- compared with the placebo group.
tect against uropatho-
genic Escherichia coli ularly, patient-initiated therapy A Cochrane review and meta-analysis concluded
urinary tract infection.
Proc Natl Acad Sci U S A. may have greater appeal. that cranberry juice cannot be recommended for
2016;113:13468-
13473. [PMID: In a meta-analysis of 19 trials of prophylactic prevention of UTI (23). However, in another meta-
27821778]
antibiotics for acute cystitis, 17 of which tested analysis, cranberry-containing products were as-
18. Stapleton AE, Dziura J,
Hooton TM, Cox ME, daily antibiotic use, the range of having 1 clin- sociated with a protective effect against UTIs (24).
Yarova-Yarovaya Y, Chen
ical recurrence was 0 0.27 person-years in the A protective effect of cranberry products was also
S, et al. Recurrent urinary
tract infection and uri- antibiotic group and 1.123.6 person-years in found in a recent meta-analysis, although the pa-
nary Escherichia coli in
the placebo group (15). tient populations in the studies that provided the
women ingesting cran-
berry juice daily: a ran- summarized data were heterogeneous, compris-
domized controlled trial. Increased awareness of the role ing children, men with prostate cancer, and
Mayo Clin Proc. 2012;
87:143-50. [PMID: of the microbiome in overall women with recurrent UTI. The cranberry prod-
22305026]
19. Barbosa-Cesnik C, Brown
health, concern for selection for ucts studied were also heterogeneous (25).
MB, Buxton M, Zhang L, antibiotic-resistant bacteria, and
DeBusscher J, Foxman B.
the difculty of treating resistant In postmenopausal women, daily
Cranberry juice fails to
prevent recurrent urinary urinary pathogens have led to topical application of intravaginal
tract infection: results
exploration of nonantimicrobial estriol cream may help reduce
from a randomized
placebo-controlled trial. approaches to UTI prevention. the frequency of symptomatic
Clin Infect Dis. 2011;52:
23-30. [PMID: These include probiotics (typi- episodes.
21148516]
cally lactobacilli), cranberry prod-
20. Juthani-Mehta M, Van Two studies in a 2008 Cochrane systematic re-
Ness PH, Bianco L, Rink ucts, D-mannose, and vaccines. A view (26) compared vaginal estrogens with
A, Rubeck S, Ginter S,
et al. Effect of cranberry Cochrane meta-analysis of trials placebo and concluded that vaginal estrogens
capsules on bacteriuria
plus pyuria among older
of lactobacilli concluded that reduced the number of UTIs in postmeno-
women in nursing probiotics did not signicantly pausal women. Oral estrogens did not reduce
homes: a randomized
clinical trial. JAMA.
reduce risk for UTI compared UTI compared with placebo. Use of vaginal es-
2016;316:1879-1887. with placebo or antibiotics (16). trogens can result in vaginal itching, burning,
[PMID: 27787564]
21. Beerepoot MA, ter Riet Currently, no vaccines are ap- discharge, and metrorrhagia (26). Clinical
G, Nys S, van der Wal
WM, de Borgie CA, de
proved for use in UTI prevention practice guidelines developed by the Society
Reijke TM, et al. Cranber- in the United States, although of Gynecologic Surgeons Systematic Review
ries vs antibiotics to Group (27) recommend vaginal estrogens for
prevent urinary tract
preclinical testing has identied
infections: a randomized promising candidates (17). postmenopausal women with recurrent UTI.
double-blind noninferior-
ity trial in premeno-
Data on the risk for cancer in women using
pausal women. Arch Debate is ongoing about the ef- vaginal estrogens are limited (27). A discus-
Intern Med. 2011;171: fectiveness of cranberry products
1270-8. [PMID:
sion of possible cancer risk should be individ-
21788542] in the prevention of UTI. ualized for each patient.
2017 American College of Physicians ITC52 In the Clinic Annals of Internal Medicine 3 October 2017
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
Screening and Prevention... Inappropriate screening for ASB can lead
to unnecessary antibiotic use. Screening for and treatment of ASB are
recommended only in pregnant women and patients about to have an
invasive urologic procedure. Postcoital antibiotic prophylaxis should be
considered for women with 2 or more UTIs per year, particularly if these
are temporally associated with coitus. Otherwise, daily or thrice-weekly
antibiotic prophylaxis can be used to prevent UTI. Clinicians should
consider topical intravaginal estrogen therapy to prevent symptomatic
UTIs for postmenopausal women with recurrent UTIs. Evidence on the
usefulness of cranberry products for UTI prevention is inconclusive.
CLINICAL BOTTOM LINE 22. Maki KC, Kaspar KL,
Khoo C, Derrig LH, Schild
AL, Gupta K. Consump-
tion of a cranberry juice
beverage lowered the
Diagnosis and Evaluation number of clinical uri-
nary tract infection epi-
sodes in women with a
What signs and symptoms curacy of cystitis self-diagnosis in recent history of urinary
should raise suspicion of UTI? emergency department settings tract infection. Am J Clin
Nutr. 2016;103:1434-
The most common symptoms of (30, 31). Many women in these 42. [PMID: 27251185]
studies had multiple sex partners 23. Jepson RG, Williams G,
UTI in noncatheterized persons Craig JC. Cranberries for
include dysuria, urinary fre- or vaginal discharge and thus did preventing urinary tract
infections. Cochrane
quency, and urgency. not meet criteria for patient- Database Syst Rev. 2012;
initiated therapy. Thus, this ap- 10:CD001321. [PMID:
23076891]
A meta-analysis of the accuracy of history and proach should be used only in 24. Wang CH, Fang CC,
physical examination for diagnosing acute un- settings with an established pa- Chen NC, Liu SS, Yu PH,
complicated UTI in ambulatory women found Wu TY, et al. Cranberry-
tientprovider relationship and containing products for
that the probability of UTI was approximately prevention of urinary
50% in those who presented with 1 or more low risk for sexually transmitted tract infections in suscep-
symptoms. Specic combinations of symp- disease (STD). tible populations: a sys-
tematic review and meta-
toms increased the probability to more than analysis of randomized
90%. Symptoms that increased the probability In catheterized patients, signs controlled trials. Arch
Intern Med. 2012;172:
were dysuria, hematuria, and costovertebral an- and symptoms suggestive of 988-96. [PMID:
gle tenderness. A history of vaginal discharge or CAUTI include new onset or 22777630]
25. Lus A, Domingues F,
irritation decreased the probability of UTI (28). worsening of fever, rigors, al- Pereira L. Can cranberries
contribute to reduce the
tered mental status, malaise or incidence of urinary tract
A prospective trial enrolled women who had at
lethargy with no other identied infections? A systematic
least 2 episodes of cystitis in the prior 12 review with meta-
cause, ank pain, costovertebral analysis and trial sequen-
months from a university-based primary care
clinic (29). The participants were given urine angle tenderness, acute hematu- tial analysis of clinical
trials. J Urol. 2017.
collection materials and a course of uoroquin- ria, or pelvic discomfort. In pa- [PMID: 28288837]
26. Perrotta C, Aznar M,
olone antibiotics, both to be used if they devel- tients whose catheters have been Mejia R, Albert X, Ng
oped symptoms of UTI. Overall, 88 of 172 removed within the past 48 CW. Oestrogens for pre-
venting recurrent urinary
women self-diagnosed a total of 172 UTIs. Lab- hours, dysuria, urgent or fre- tract infection in post-
oratory evaluation showed a uropathogen in quent urination, or suprapubic menopausal women.
Cochrane Database Syst
144 cases (84%), sterile pyuria in 19 cases pain or tenderness are also sug- Rev. 2008:CD005131.
(11%), and no pyuria or bacteriuria in 9 cases gestive of CAUTI (32). Guidelines [PMID: 18425910]
27. Rahn DD, Carberry C,
(5%). Clinical and microbiological cures oc- also specify that 103 or more Sanses TV, Mamik MM,
curred in 92% and 96%, respectively, of Ward RM, Meriwether
colony-forming units per milliliter KV, et al; Society of Gy-
culture-conrmed episodes. necologic Surgeons
of urine is sufcient for diagnosis Systematic Review
In other populations, such as of CAUTI. By denition, CAUTI Group. Vaginal estrogen
for genitourinary syn-
women visiting emergency de- can occur with indwelling ure- drome of menopause: a
partments, self-diagnosis of UTI thral (Foley) catheters, suprapu- systematic review. Obstet
Gynecol. 2014;124:
has been found to be less accu- bic catheters, or condom cathe- 1147-56. [PMID:
25415166]
rate. Low agreement between ters. Because many of these 28. Bent S, Nallamothu BK,
patients and clinicians and a dening symptoms are nonspe- Simel DL, Fihn SD, Saint
S. Does this woman have
higher rate (17%21%) of chla- cic, other infections and poten- an acute uncomplicated
mydia diagnoses have been re- tial causes should be considered urinary tract infection?
JAMA. 2002;287:2701-
ported in studies evaluating ac- before attributing the symptoms 10. [PMID: 12020306]
3 October 2017 Annals of Internal Medicine In the Clinic ITC53 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
Table 1. Differential Diagnosis of Acute Cystitis in Women
Condition Pathogens History Symptoms
Vaginitis Candida, Trichomonas Possibly new sex partner or Vaginal discharge, odor, or itching;
vaginalis, Bacteroides unprotected sexual activity; external dysuria (from urine coming
species, Gardnerella history of vaginitis into contact with inamed and irritated
vaginalis vulvar epithelial surfaces)
Urethritis Chlamydia trachomatis, New sex partner, unprotected Gradual onset of symptoms (Chlamydia)
Neisseria sexual activity, history of sexually vaginal discharge; urinary frequency
gonorrhoeae, or transmitted disease or recurrent or urgency
herpes simplex virus genital herpes simplex virus
Irritation None No unusual sexual exposure; Vaginal itching or discharge; usually a
possible chemical or allergen diagnosis of exclusion, unless withdrawal
exposures (e.g., douches, bath of a suspected offending substance
products, feminine hygiene leads to resolution of symptoms
products, spermicides)
Pyelonephritis Same as acute cystitis Previous urinary tract infection Constitutional symptoms (fever, malaise,
(pyelonephritis or cystitis) sweats, headache), gastrointestinal
symptoms (anorexia, nausea, vomiting,
abdominal pain), local renal symptoms
(back, ank, or loin pain), voiding
symptoms (as in cystitis)
to catheter-associated bacteri- phritis is longer than for cystitis;
uria. Distinguishing between treatment of incipient pyelone-
CAUTI and catheter-associated phritis with a short-course regi-
ASB is challenging. men for cystitis could predispose
the patient to relapse. Pyelone-
What other disorders should be
phritis may or may not be associ-
considered?
29. Gupta K, Hooton TM, ated with symptoms of cystitis,
Roberts PL, Stamm WE. Alternative diagnoses to consider
Patient-initiated treat- which in some patients may over-
ment of uncomplicated include sexually transmitted ure-
shadow the renal or systemic
recurrent urinary tract thritis or vaginitis, noninfectious
infections in young manifestations. In patients pre-
women. Ann Intern Med. urethritis, and early pyelonephri-
2001;135:9-16. [PMID: senting with symptoms of acute
11434727] tis (Table 1). Symptoms of STDs
cystitis, clinicians should conrm
30. Wilbanks MD, Galbraith may be subtle and thus should
JW, Geisler WM. Dysuria the absence of fever, nausea,
in the emergency depart- always be considered in the dif-
ment: missed diagnosis vomiting, rigors, and ank pain.
ferential diagnosis. A history of
of Chlamydia trachoma- In men with urinary symptoms
tis. West J Emerg Med. vaginal discharge or irritation
2014;15:227-30. [PMID: and fever, both acute infectious
24672617] decreases the probability of UTI
prostatitis and pyelonephritis
31. Donofrio JC, Weiner SG. and warrants a work-up for STDs
Female patient self- should be considered in the
diagnosis compared with and other vaginal conditions,
emergency physician
such as candidiasis (28). differential diagnosis.
diagnosis of urinary tract
infection. J Emerg Med. What tests should be done?
2013;45:969-73. [PMID: A cross-sectional study screened 296 sexually
24063877]
active females aged 14 22 years who were vis- Women presenting with classic
32. Hooton TM, Bradley SF,
Cardenas DD, Colgan R, iting a teen health center for both UTI (by urine symptoms of cystitis (dysuria or
Geerlings SE, Rice JC,
et al; Infectious Diseases
culture) and STD (by vaginal swab and nucleic urinary frequency) without symp-
Society of America. Diag- acid amplication testing). In this population, toms suggesting alternative diag-
nosis, prevention, and
treatment of catheter-
the prevalence of UTI and STD were 17% and noses or underlying complica-
associated urinary tract 33%, respectively; 4% had both. The presence tions may be treated for UTI
infection in adults: 2009
International Clinical
or absence of urinary symptoms did not pre- without further testing. For such
Practice Guidelines from dict STD, indicating that telephone manage- women, self-initiated therapy or
the Infectious Diseases
ment may not be appropriate for adolescent
Society of America. Clin telephone clinic provider-
Infect Dis. 2010;50:625- females with urinary symptoms (33).
63. [PMID: 20175247] guided presumptive therapy may
33. Huppert JS, Biro F, Lan
D, Mortensen JE, Reed J,
Clinicians should also consider be appropriate (34). In women
Slap GB. Urinary symp- pyelonephritis (or prostatitis in presenting with symptoms of
toms in adolescent fe-
males: STI or UTI? J Ado- men) before initiating therapy for acute cystitis, a positive urine
lesc Health. 2007;40: acute cystitis. The recommended dipstick result can help to con-
418-24. [PMID:
17448399] duration of therapy for pyelone- rm the diagnosis, but a negative
2017 American College of Physicians ITC54 In the Clinic Annals of Internal Medicine 3 October 2017
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
result cannot rule out the diagno- rms the diagnosis of UTI, and to
sis in women with a high pretest provide specic information about
probability (28, 35). Thus, a dip- the organism and its antimicrobial
stick test is not necessary if the susceptibility. Performing a culture
history is clearly diagnostic of UTI (with susceptibility testing) on a
(particularly in women with symp- pretreatment urine sample is ap-
toms akin to previous episodes). propriate for women with sus-
pected cystitis if the diagnosis is
In women with acute dysuria, not clear, if an unusual or
pyuria is a highly sensitive indica- antimicrobial-resistant organism is
tor of bacteriuria and can be used suspected, if the episode repre-
as a surrogate for urine culture sents a suspected relapse or treat-
(35). If the diagnosis is not clear- ment failure, or if the patient's ther-
cut or additional complicating fac- apeutic options are limited by
tors or alternative diagnoses are medication intolerance.
possible, a more thorough and
broad-based diagnostic evaluation Escherichia coli is isolated in
should be done. more than 90% of patients with
uncomplicated cystitis and pyelo-
Blood tests (including cultures) nephritis. Other coliforms, includ-
are not indicated in women with ing Klebsiella and Proteus, are
suspected cystitis unless they are less common. Staphylococcus
needed to screen for alternative saprophyticus causes uncompli-
diagnoses or to assess the status cated cystitis and pyelonephritis
of a known underlying medical in a small proportion (5%10%) of
condition (such as diabetes melli- otherwise healthy women. E coli
tus). Up to 30% of women with is a predominant pathogen in
acute pyelonephritis may have complicated UTI, but other coli-
secondary bacteremia, and iden- forms and enterococci are also
tication of the organism by common. CAUTI in patients with
blood culture can be helpful in short-term catheters can be
caused by E coli as well as by a 34. Saint S, Scholes D, Fihn
cases where antibiotics are SD, Farrell RG, Stamm
started in advance of the urine spectrum of typical hospital- WE. The effectiveness of
a clinical practice guide-
culture. Diabetic women and re- acquired pathogens, including line for the management
nal transplant recipients have a Klebsiella, Citrobacter, Enterobac- of presumed uncompli-
cated urinary tract infec-
higher incidence of secondary ter, Pseudomonas, coagulase- tion in women. Am J
Med. 1999;106:636-41.
bacteremia with UTI, so blood negative staphylococci, entero- [PMID: 10378621]
cultures should be done if these cocci, and Candida. Patients with 35. Lachs MS, Nachamkin I,
Edelstein PH, Goldman
patients have systemic signs of long-term catheters typically have J, Feinstein AR, Schwartz
infection (36, 37). polymicrobial infections; in addi- JS. Spectrum bias in the
evaluation of diagnostic
tion to the aforementioned patho- tests: lessons from the
Pretreatment urine culture is also gens, Proteus, Morganella, and rapid dipstick test for
urinary tract infection.
considered standard of care if the Providencia are common (38). Ann Intern Med. 1992;
patient is pregnant or male. In 117:135-40. [PMID:
1605428]
women, urine culture is generally Interpretation of urine culture 36. Geerlings SE. Urinary
not required in suspected acute results depends on the clinical tract infections in pa-
tients with diabetes
uncomplicated cystitis because the context and the urinalysis nd- mellitus: epidemiology,
pathogenesis and treat-
spectrum of causative organisms is ings; the threshold of bacteriuria ment. Int J Antimicrob
predictable and urine culture re- required for the diagnosis of Agents. 2008;31 Suppl
1:S54-7. [PMID:
sults often are not available until acute cystitis is not absolute. 18054467]
after completion of short-course Even a low concentration (102 37. Mercon M, Regua-
Mangia AH, Teixeira LM,
empirical treatments. colony-forming units per millili- Irino K, Tuboi SH, Gon-
calves RT, et al. Urinary
ter) of coliform bacteria in a urine tract infections in renal
The role of urine culture is to pro- sample from a woman with acute transplant recipients:
virulence traits of uro-
vide retrospective conrmation of dysuria and pyuria often repre- pathogenic Escherichia
the presence of bacteriuria, which sents true (that is, from within the coli. Transplant Proc.
2010;42:483-5. [PMID:
in the correct clinical setting con- urinary tract) bacteriuria. Such 20304171]
3 October 2017 Annals of Internal Medicine In the Clinic ITC55 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
organisms should not be dis- ture protocol able to isolate fastidi-
missed as contaminants in a ous organisms provided a more
clinical setting suggestive of cys- complete description of clinically
titis. On the other hand, even relevant uropathogens (40). Com-
high concentrations (>105 pared with enhanced quantitative
colony-forming units per millili- urine culture, standard urine cul-
ter) of nonpathogens may not ture missed 67% of uropathogens
reect true bacteriuria if the urine overall and missed uropathogens
specimen was not collected in 50% of participants with severe
properly or was allowed to stand urinary symptoms (40).
at room temperature before pro-
cessing. Organisms other than Is there a role for diagnostic
coliform bacilli, S saprophyticus, imaging?
and Enterococcus (for example, For uncomplicated bladder infec-
lactobacilli, -streptococci, and tions, imaging studies (abdomi-
coagulase-negative staphylococci nal radiography, ultrasonogra-
other than S saprophyticus) are phy, computed tomography, and
usually considered contaminants excretory urography) add little or
in urine cultures from women with no benet but increase cost and
uncomplicated cystitis, whereas in cause delays and sometimes dis-
complicated UTI almost any organ- comfort or complications for the
ism can be causative and must be patient. Such studies should be
seriously considered if the patient done only if pretest suspicion is
is symptomatic. high for an alternative diagnosis
or an anatomical problem (such
Limitations of urine sampling are
as a bladder obstruction or
now better recognized. In a study
stone) that requires intervention.
comparing paired specimens of
A recent study presented a clini-
midstream urine and urine col-
cal prediction rule consisting of a
38. Nicolle LE. Catheter- lected by means of a urethral
related urinary tract in- history of urolithiasis, a urine pH
fection. Drugs Aging. catheter obtained from women
of 7.0 or greater, and/or renal
2005;22:627-39. [PMID: with acute cystitis, the presence of
16060714]
E coli in midstream urine was insufciency (estimated glomeru-
39. Hooton TM, Roberts PL,
Cox ME, Stapleton AE.
highly predictive of bladder bacte- lar ltration rate 40 mL/min/
Voided midstream urine
culture and acute cystitis riuria, even at very low counts (39). 1.73 m2) to be used at emer-
in premenopausal
In contrast, both enterococci and gency departments for selective
women. N Engl J Med.
2013;369:1883-91. group B streptococci were isolated use of radiologic imaging in
[PMID: 24224622] adults presenting with febrile UTI
40. Price TK, Dune T, Hilt EE, frequently from midstream urine
Thomas-White KJ,
but rarely from paired specimens (41). This rule may lead to a 40%
Kliethermes S, Brincat C,
et al. The clinical urine of urine sampled from the bladder reduction in the number of imag-
culture: enhanced tech-
through catheterization (39). Misin- ing studies without missing clini-
niques improve detec-
tion of clinically relevant terpretation of such cultures may cally relevant outcomes, such as
microorganisms. J Clin
Microbiol. 2016;54: result in undertreatment of low- infection of the kidneys' collect-
1216-22. [PMID:
quantity E coli infections or inap- ing system and renal abscess
26962083]
41. van Nieuwkoop C, propriate treatment of infection (41). Although men with acute
Hoppe BP, Bonten TN, cystitis should be considered for
Van't Wout JW, Aarts NJ, with enterococci or group B strep-
Mertens BJ, et al. Pre- tococci identied in midstream further evaluation for urologic
dicting the need for
radiologic imaging in urine. Thus, in women with symp- abnormalities, imaging studies
adults with febrile uri-
toms of acute cystitis, a low con- for acute cystitis in men younger
nary tract infection. Clin
Infect Dis. 2010;51: centration of E coli (alone or in than 45 years or in older men
1266-72. [PMID:
21034195] conjunction with other bacteria) in without symptoms of voiding dif-
42. Ulleryd P, Zackrisson B, a midstream urine specimen culties or hematuria may not be
Aus G, Bergdahl S, Hu-
gosson J, Sandberg T. should not be considered a con- useful. The evidence base for
Selective urological eval-
uation in men with fe-
taminant. In another study, a cul- male cystitis is limited (42).
brile urinary tract infec-
tion. BJU Int. 2001;88:
15-20. [PMID:
11446838]
2017 American College of Physicians ITC56 In the Clinic Annals of Internal Medicine 3 October 2017
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
Diagnosis and Evaluation... In ambulatory adult women, patient history
has a high predictive value for presence or absence of cystitis. Clinicians
should consider a diagnosis of pyelonephritis (or prostatitis in men) before
starting therapy for acute cystitis. Complicating factors that would affect the
appropriate diagnostic work-up and course of therapy should also be con-
sidered. Urinalysis should be used to conrm the diagnosis in women with
suspected UTI when the history alone is not diagnostic. Clinicians should
always perform urine culture in patients with pyelonephritis, complicated
UTI, or a history of failure of initial therapy or multidrug resistance. Empiri-
cal therapy should be initiated and then adjusted on the basis of the results
of the urine culture (if it is done).
CLINICAL BOTTOM LINE
Treatment and Management
What are the preferred known urologic abnormalities or
treatments of UTI? comorbid conditions (44). Rec-
ommendations for treatment that
Treatment of UTI depends on
take into account current resis-
host factors (such as sex, com-
tance rates and other popula-
promised immune system, or
tions have been published more
urologic abnormalities), severity
recently (45, 46).
of illness, and risk for multidrug
resistance. The prevalence of re- Management of UTI is affected
sistance in community popula- by the increasing prevalence of
tions has increased and must be resistant organisms and the po- 43. Linsenmeyer K, Strymish
J, Gupta K. Two simple
considered, even in outpatients. tential for propagation of resis- rules for improving the
accuracy of empiric treat-
In women with symptoms of cys- tance among normal host ora ment of multidrug-
resistant urinary tract
titis without fever or signs of sys- with the use of broad-spectrum infections. Antimicrob
temic infection, outpatient oral antibiotics. Four agents are rec- Agents Chemother.
2015;59:7593-6. [PMID:
antibiotic therapy is recom- ommended for rst-line therapy: 26416859]
mended. Clinicians should ask nitrofurantoin, TMPSMX, pivme- 44. Gupta K, Hooton TM,
Naber KG, Wullt B, Col-
about factors that may inuence cillinam, and fosfomycin trometa- gan R, Miller LG, et al;
Infectious Diseases Soci-
the choice of antimicrobial agent, mol (44). Alternative agents ety of America. Interna-
including pregnancy and breast- include -lactams and uoro- tional clinical practice
guidelines for the treat-
feeding, use of other medica- quinolones. Two important modi- ment of acute uncompli-
cated cystitis and pyelo-
tions, drug allergy history, recent cations to previous recommen- nephritis in women: a
antibiotic therapy, other recent dations should be noted. First, 2010 update by the
Infectious Diseases Soci-
infections or positive culture re- TMPSMX should be used with ety of America and the
sults, and recent travel. Previous caution as a rst-line empirical European Society for
Microbiology and Infec-
microbiology should also be re- agent because resistance is wide- tious Diseases. Clin Infect
Dis. 2011;52:e103-20.
viewed because it can be useful spread. Clinicians should con- [PMID: 21292654]
in predicting multidrug resis- sider use in the setting of known 45. Walker E, Lyman A,
Gupta K, Mahoney MV,
tance of the current pathogen susceptibility based on previous Snyder GM, Hirsch EB.
microbiology or practice in a low- Clinical management of
(43). Also, complicating factors an increasing threat:
should be considered because resistance prevalence area. Sec- outpatient urinary tract
infections due to
management of uncomplicated ond, uoroquinolones have been multidrug-resistant uro-
cystitis differs from that of pyelo- moved to the last class of agents pathogens. Clin Infect
Dis. 2016;63:960-5.
nephritis and complicated UTI. (after -lactams) and should be [PMID: 27313263]
46. Grigoryan L, Trautner
The IDSA has published guide- used only when no other oral op- BW, Gupta K. Diagnosis
lines for treatment of uncompli- tions are available because of a and management of
urinary tract infections in
cated cystitis and pyelonephritis, warning from the U.S. Food and the outpatient setting: a
specically in premenopausal, Drug Administration (FDA) that review. JAMA. 2014;
312:1677-84. [PMID:
nonpregnant women with no risk for serious harms outweighs 25335150]
3 October 2017 Annals of Internal Medicine In the Clinic ITC57 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
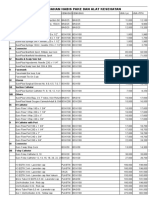
Table 2. Treatment Regimens for Acute Uncomplicated Cystitis
Drug Dose and Duration Common Adverse Effects Comments*
Recommended agents
Nitrofurantoin 100 mg twice daily Nausea, headache Resistance rare to date; may be useful for multidrug-
monohydrate/ for 5 d resistant pathogens; cost varies; usually
macrocrystals well-tolerated; FDA pregnancy category B
Trimethoprim 160/800 mg (1 DS Rash, urticaria, nausea, Excellent efcacy if local resistance <20%;
sulfamethoxazole tablet) twice daily vomiting, resistance prevalence is increasing; use
for 3 d hematologic signs with caution unless known susceptibility;
inexpensive; extensive clinical experience; avoid
during pregnancy, particularly rst and third
trimesters; FDA pregnancy category C
Fosfomycin 3-g single-dose Diarrhea, nausea, May be useful for multidrug-resistant pathogens;
trometamol sachet headache may be less effective than other agents; FDA
pregnancy category B
Alternative agents
-Lactams Dose varies by agent; Diarrhea, nausea, Resistance varies by agent; increased adverse
5- to 7-d regimen vomiting, rash, effects compared with other choices; FDA
urticaria pregnancy category B
Fluoroquinolones Dose varies by agent; Nausea, vomiting, Risk may outweigh benet for treatment of
3-d regimen diarrhea, headache, outpatient uncomplicated cystitis (FDA
drowsiness, warning). Resistance prevalence increasing; cost
insomnia, tendon varies; excellent efcacy; high collateral
rupture, neuropathy damage; better reserved for more serious
conditions; avoid during pregnancy; FDA
pregnancy category C
DS = double-strength; FDA = U.S. Food and Drug Administration.
* FDA pregnancy category B: Animal reproduction studies have failed to demonstrate a risk to the fetus and there are no
adequate and well-controlled studies in pregnant women. FDA pregnancy category C: Animal reproduction studies have shown
an adverse effect on the fetus and there are no adequate and well-controlled studies in humans, but potential benets may
warrant use of the drug in pregnant women despite potential risks (www.drugs.com/pregnancy-categories.html).
benets. Treatment regimens Each agent comes with caveats.
for cystitis and pyelonephritis Nitrofurantoin concentrates in
are listed in Tables 2 and 3, re- urine but has little tissue penetra-
spectively. tion and should be avoided if
Table 3. Oral Treatment Regimens for Acute Uncomplicated Pyelonephritis*
Drug Dose and Duration Comments Other
Fluoroquinolones
Ciprooxacin 500 mg twice daily for If local resistance Consider adding an initial 1-time intravenous
Ciprooxacin XR 57 d prevalence is <10% dose of a long-acting parenteral anti-
Levooxacin 1000 mg once daily for microbial (such as 1 g of ceftriaxone, 1 g of
57 d ertapenem, or a single 24-h dose of an
750 mg once daily for aminoglycoside) if there is concern that the
57 d organism might be resistant, if the patient
might not tolerate oral therapy, or if oral
therapy could be delayed
Trimethoprim 160/800 mg (1 DS tablet) If pathogen known to be Same as above
sulfamethoxazole twice daily for 1014 d susceptible; otherwise,
give an initial
intravenous agent
-Lactams Dose varies by agent; Oral -lactams are less Give an initial intravenous dose of a long-
10- to 14-d regimen effective and should be acting parenteral antimicrobial when using
used with caution only oral -lactams
when other agents
cannot be used
DS = double-strength; XR = extended-release.
* For pyelonephritis, a urine culture and susceptibility testing should always be performed, and the initial empirical therapy
should be tailored appropriately on the basis of the infecting uropathogen. Uncomplicated pyelonephritis indicates absence of
pregnancy, nephrolithiasis, or urinary tract obstruction. The choice between these agents should be based on local resistance
data, and the regimen should be tailored on the basis of susceptibility results.
2017 American College of Physicians ITC58 In the Clinic Annals of Internal Medicine 3 October 2017
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
there is a possibility of pyelone- cated cystitis. Whether patients
phritis. A 5-day course of nitrofu- with diabetes need longer treat-
rantoin was as effective as a ment has not been robustly stud-
3-day course of TMPSMX in ied. In a retrospective observa-
terms of both clinical and micro- tional cohort study, duration of
biological cure in a randomized therapy for women with diabetes
trial (47). The main limitation of and UTI was longer, but without
use of TMPSMX is the increasing improved outcomes compared
rate of resistance among uro- with women without diabetes,
pathogens and evidence that in suggesting that the duration of 47. Gupta K, Hooton TM,
Roberts PL, Stamm WE.
vitro resistance correlates with UTI therapy in women with dia- Short-course nitrofuran-
bacterial and clinical failure in at betes should be the same as in toin for the treatment of
acute uncomplicated
least 50% of women. Fosfomycin those without (51). In men with cystitis in women. Arch
Intern Med. 2007;167:
is available in the United States UTI, data on the optimal duration 2207-12. [PMID:
but is used infrequently. The rec- are limited; however, an observa- 17998493]
48. Falagas ME, Kastoris AC,
ommended 3-g single dose may tional study of 14 versus 7 days Kapaskelis AM, Karageor-
found no benet and higher gopoulos DE. Fosfomycin
not be as efcacious as other rec- for the treatment of
ommended agents, and it should rates of Clostridium difcile infec- multidrug-resistant,
including extended-
not be used if pyelonephritis is tion in the longer-treatment spectrum beta-lactamase
suspected. Susceptibility data are group (52). producing, Enterobacteri-
aceae infections: a sys-
not routinely reported for this tematic review. Lancet
Pyelonephritis is a tissue-invasive Infect Dis. 2010;10:43-
drug, but surveys show that it disease, and the initial empirical 50. [PMID: 20129148]
49. Linsenmeyer K, Strymish
retains activity against multidrug- regimen should be broad enough J, Weir S, Berg G,
resistant uropathogens, such as to ensure in vitro activity against
Brecher S, Gupta K. Activ-
ity of fosfomycin against
extended-spectrum -lactamase the likely uropathogen. Performing extended-spectrum--
producing gram-negative organ- urine culture and susceptibility
lactamase-producing
uropathogens in patients
isms (48 50). Pivmecillinam, testing before starting therapy is in the community and
hospitalized patients.
which is currently unavailable in essential so that therapy can be Antimicrob Agents Che-
the United States, is an extended- tailored. Clinicians should rule out
mother. 2016;60:
1134-6. [PMID:
spectrum penicillin that is active complicated infection (pregnancy, 26596940]
50. Sastry S, Clarke LG, Al-
against gram-negative organisms nephrolithiasis, or obstruction), rowais H, Querry AM,
but is used only for treatment of determine whether the patient can Shutt KA, Doi Y. Clinical
appraisal of fosfomycin
UTI. Although efcacy rates are take oral antibiotics and whether in the era of antimicro-
lower than for other recom- they require hospitalization, and
bial resistance. Antimi-
crob Agents Chemother.
mended agents, its low resis- decide whether there is high risk 2015;59:7355-61.
[PMID: 26369978]
tance rates have made it a popu- for uoroquinolone or extended- 51. Grigoryan L, Zoorob R,
lar rst-line choice in some spectrum -lactamase resistance Wang H, Horseld M,
Gupta K, Trautner BW.
European countries. -Lactams (53). Less workup, longer
generally have inferior efcacy treatment, but no clinical
benet observed in
and greater rates of adverse ef- If oral therapy is feasible, a 7-day women with diabetes
regimen of oral ciprooxacin is and acute cystitis. Diabe-
fects and thus are considered tes Res Clin Pract. 2017;
alternative agents. The uoro- preferred if local resistance rates 129:197-202. [PMID:
28544925]
quinolones ooxacin, ciprooxa- to uoroquinolones do not exceed 52. Drekonja DM, Rector TS,
cin, and levooxacin are highly 10% (a threshold that is increas- Cutting A, Johnson JR.
Urinary tract infection in
efcacious in 3-day regimens but ingly being exceeded, even in male veterans: treatment
patterns and outcomes.
are recommended as alternative community-based pyelonephritis JAMA Intern Med. 2013;
agents because of the aforemen- [53]). Giving the extended-release 173:62-8. [PMID:
23212273]
tioned FDA warning. Increasing formulation of ciprooxacin or a 53. Talan DA, Takhar SS,
rates of uoroquinolone resis- once-daily dose of levooxacin for Krishnadasan A, Abraha-
mian FM, Mower WR,
tance and concerns about safety 57 days is acceptable, but evi- Moran GJ; EMERGEncy
ID Net Study Group.
reinforce the importance of re- dence is limited (44). TMPSMX is Fluoroquinolone-
serving these agents for condi- also effective if the pathogen is resistant and extended-
spectrum -lactamase-
tions other than acute cystitis. susceptible, but a course of 10 14 producing Escherichia
coli infections in patients
days is recommended. If suscepti- with pyelonephritis,
Most data on treatment duration bility of the uropathogen is not United States(1). Emerg
Infect Dis. 2016;22.
are from women with uncompli- known, an initial 1-time intrave- [PMID: 27532362]
3 October 2017 Annals of Internal Medicine In the Clinic ITC59 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
nous dose of ceftriaxone or ertap- quinolones were as effective as
54. Chenoweth CE, Gould enem, or a long-acting aminogly- traditional intravenous regimens
CV, Saint S. Diagnosis,
management, and pre-
coside is recommended before and at least as effective as oral
vention of catheter- outpatient oral therapy. In a study TMPSMX or TMP (particularly for
associated urinary tract
infections. Infect Dis Clin comparing ciprooxacin versus organisms resistant to TMP
North Am. 2014;28:105-
19. [PMID: 24484578]
TMPSMX, an initial dose of intra- SMX). However, resistance to
55. Talan DA, Stamm WE, venous ceftriaxone resulted in im- uoroquinolones among uro-
Hooton TM, Moran GJ,
Burke T, Iravani A, et al. proved outcomes in women re- pathogens is increasing world-
Comparison of cipro-
oxacin (7 days) and
ceiving TMPSMX who had a wide. If the local prevalence of
trimethoprim- resistant uropathogen. Oral uoroquinolone resistance ex-
sulfamethoxazole (14
days) for acute uncompli- -lactam agents are not recom- ceeds 10%, another broad-
cated pyelonephritis
pyelonephritis in wom-
mended because of inferior ef- spectrum antimicrobial should
en: a randomized trial. cacy rates. be considered, including an
JAMA. 2000;283:1583-
90. [PMID: 10735395] extended-spectrum cephalospo-
56. Hicks LA, Bartoces MG, In patients admitted for intrave- rin with or without an aminogly-
Roberts RM, Suda KJ,
Hunkler RJ, Taylor TH Jr,
nous therapy, a broad-spectrum coside or a carbapenem. Combi-
et al. US outpatient anti- agent should be given until sus- nations of a -lactam and a
biotic prescribing varia-
tion according to geogra- ceptibilities are known. A carba- -lactamase inhibitor (for exam-
phy, patient population,
and provider specialty in
penem agent, an extended- ple, ampicillinsulbactam, ticar-
2011. Clin Infect Dis. spectrum -lactam with or without cillin clavulanate, or piperacillin
2015;60:1308-16.
[PMID: 25747410] an aminoglycoside, or another tazobactam) or imipenem
57. Fleming-Dutra KE, Hersh
AL, Shapiro DJ, Bartoces
regimen chosen on the basis of cilastatin could also be
M, Enns EA, File TM Jr, local resistance patterns is appro- considered (32). For CAUTI, the
et al. Prevalence of inap-
propriate antibiotic pre- priate. Patients with risk factors for recommended duration of anti-
scriptions among US
ambulatory care visits,
Pseudomonas or multidrug resis- microbial treatment is 7 days for
2010 2011. JAMA. tance who are severely ill should patients who have prompt reso-
2016;315:1864-73.
[PMID: 27139059] receive initial therapy with a car- lution of symptoms and 10 14
58. Grigoryan L, Zoorob R,
Wang H, Trautner BW. bapenem (imipenem cilastatin, days for those with a delayed re-
Low concordance with ertapenem, meropenem, or dorip- sponse. For those with CAUTI
guidelines for treatment
of acute cystitis in pri- enem). This can be tailored once who are not severely ill, a 5-day
mary care. Open Forum
Infect Dis. 2015;2: susceptibility is known. Two re- regimen of levooxacin may be
ofv159. [PMID: cently approved agents (ceftazi- considered (32, 54). In patients
26753168]
59. May L, Mullins P, Pines dimeavibactam and ceftolozane with CAUTI who have had a cath-
J. Demographic and
treatment patterns for tazobactam) should be considered eter in place for 2 weeks or lon-
infections in ambulatory in cases of anticipated carbap- ger, the catheter should be re-
settings in the United
States, 2006 2010. Acad enem resistance or extremely re- moved or replaced (32).
Emerg Med. 2014;21:
17-24. [PMID: sistant Pseudomonas, typically in
24552520] consultation with an infectious dis- In pregnant women with symp-
60. Shapiro DJ, Hicks LA,
Pavia AT, Hersh AL. Anti- ease specialist. tomatic UTI, urine culture and
biotic prescribing for
adults in ambulatory care
susceptibility testing should be
in the USA, 200709. Patients with underlying comor- performed. Empirical therapy
J Antimicrob Chemother. bidities and substantial prior
2014;69:234-40. [PMID: with an oral antimicrobial agent
23887867] health care exposure are more that is safe for use in pregnant
61. Kobayashi M, Shapiro
DJ, Hersh AL, Sanchez likely to have a drug-resistant or- women should be given for 37
GV, Hicks LA. Outpatient ganism, respond poorly to anti-
antibiotic prescribing days, depending on which drug
practices for uncompli- microbial therapy even when the is used. Antibiotic therapy should
cated urinary tract infec-
tion in women in the organism is susceptible, and de- be adjusted on the basis of cul-
United States, 2002 velop complications if initial ther-
2011. Open Forum Infect ture results.
Dis. 2016;3:ofw159. apy is suboptimal. Broader-
[PMID: 27704014]
62. Kahan NR, Chinitz DP, spectrum empirical therapy with Is there a role for nonpharma-
Kahan E. Physician ad- agents to which resistance is cologic therapies, including
herence to recommenda-
tions for duration of least common and longer treat- alternative therapies?
empiric antibiotic treat-
ment for uncomplicated ment durations are intended to There is no dened role for non-
urinary tract infection in blunt the negative effects of host drug therapy in managing acute
women: a national drug
utilization analysis. Phar- compromise on treatment out- cystitis. Clinicians should advise
macoepidemiol Drug comes. In clinical trials of therapy patients that use of ibuprofen
Saf. 2004;13:239-42.
[PMID: 15255090] for complicated UTI, oral uoro- and nondrug approaches, such
2017 American College of Physicians ITC60 In the Clinic Annals of Internal Medicine 3 October 2017
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
as increased uid intake, con- longed duration of symptoms How should patients be
sumption of cranberry juice, and before presentation (>3 days), followed?
acupuncture, have no known and recent travel to an area with In uncomplicated cystitis, no
benet. Patients should be coun- a high prevalence of antibiotic- follow-up is needed if symptoms
seled that relying on nondrug resistant uropathogens all in- resolve. In pregnant women,
therapies to treat acute cystitis is crease the risk for resistant infec- urine culture should be done
essentially the same as treating tion. Urologic complications that after treatment to conrm eradi-
the condition with a placebo. increase risk for treatment failure cation of bacteriuria, and re-
include urinary tract stones, void- peated urinalyses or urine cul-
When should patients be
ing disorders, indwelling cathe- tures should be done at intervals
hospitalized? ters, stents, urinary obstruction, to conrm sterility of the urine
Complicated cystitis or pyelone- duplicated collecting system or through the time of delivery. Preg-
phritis may require inpatient other anatomical abnormalities, nant women who have already
management. Factors that may or vesicoureteral reux. The com- had bacteriuria during their preg-
warrant hospitalization include bination of obstruction and infec- nancy are at increased risk for re-
serious comorbid conditions and tion puts the patient at increased currence and need closer moni-
pregnancy. Patients with high risk for upper UTI (pyelonephri- toring than those who had sterile
fever, dehydration, high leuko- tis), sepsis, and perinephric or urine at initial screening. How-
cyte count, or other evidence of intrarenal abscess. In particular, ever, more evidence is needed to
sepsis may require inpatient su- patients with CAUTI who do not dene the appropriate frequency
pervision, as do those who are respond promptly to appropriate of follow-up cultures and retreat-
vomiting and thus unable to take antibiotic therapy may have ob- ment strategies (10).
oral therapy. Another consider- struction or stones in the upper
ation is whether the patient has urinary tract. Effective urine Because complicated UTI is
an upper urinary tract condition drainage reduces intraluminal highly heterogeneous, the ap-
that requires drainage or surgical pressure and restores the ow of proach to monitoring during
intervention. On rare occasions, a antibiotic-containing urine. and after therapy must be indi-
patient may have a multidrug- vidualized. Patients with compli-
resistant organism in the urine When should clinicians consult cated UTI should be followed
that is susceptible only to paren- a specialist? clinically for resolution of symp-
terally administered antimicrobial Consultation with an infectious toms and be reevaluated if
agents or is intolerant of agents disease specialist is recom- symptoms worsen or do not im-
that can be given orally. Treat- mended for complicated UTI, prove within 24 48 hours. In
ment trials have shown efcacy of particularly in patients with in- CAUTI, it is important to monitor
oral therapy with a uoroquino- dwelling bladder catheters, in response to therapy by the pa-
lone for mild, acute pyelonephri- those hospitalized because of tient's symptoms rather than by
tis in women, and thus many upper tract disease, in men with repeated urine cultures, given
women with pyelonephritis can UTI, or when the organisms iso- that recurrent bacteriuria is the
be managed successfully at lated in the urine are resistant to norm in patients whose indwell-
home (55). Clinical judgment is standard antibiotics. ing catheter remains in place.
required to determine which pa- What is the correct approach
Consultation with an infectious
tients are appropriate for outpa- to secondary prevention in
disease specialist or a urologist is
tient management, and a period patients with a history of UTI?
warranted for patients with possi-
of observation in the emergency Recurrent UTI is estimated to
ble upper urinary tract involve-
department may be warranted. occur in up to 50% of women
ment who do not respond to ap-
What are common reasons for propriate antibiotic therapy within 1 year of an initial UTI (4).
failure of therapy? within 72 hours. A surgically cor- Other than the antimicrobial
Underlying medical conditions rectable lesion may be present in prophylaxis recommended in
that increase risk for delayed or men who report voiding difcul- the Screening and Prevention
incomplete response to therapy, ties or acute urine retention or section, there are few measures
relapse, or infection include who have early recurrent UTI or that women can take to prevent
pregnancy, diabetes mellitus, persistent microscopic hematu- recurrent UTI. A large case con-
and immunosuppression. Ad- ria. Stones, strictures, and occult trol study in premenopausal
vanced age, recent UTI, recent cancer are among the differential women found no associations
antibiotic use, previous infection diagnoses for men with these between risk for recurrent UTI and
with a resistant organism, pro- symptoms. precoital and postcoital voiding,
3 October 2017 Annals of Internal Medicine In the Clinic ITC61 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
frequency of urination, wiping pat- frequent use of pantyhose or tights,
terns, douching, use of hot tubs, or daily uid consumption (3).
Treatment and Management... The IDSA has standard-of-care guide-
lines for treatment of acute uncomplicated cystitis, acute uncomplicated
pyelonephritis, and CAUTI. Fluoroquinolones should not be the rst
choice for uncomplicated cystitis given high levels of resistance and risk
for serious adverse effects. Nonpharmacologic therapies for cystitis
have no proven benets and can lead to adverse outcomes. Posttreat-
ment follow-up should include monitoring of the clinical response to
therapy. Repeated urine cultures are needed only for pregnant women.
63. Drug Safety Communica- CLINICAL BOTTOM LINE
tion. FDA advises restrict-
ing uoroquinolone
antibiotic use for certain
uncomplicated infec-
tions. Accessed at www
.fda.gov/newsevents
/newsroom/press
announcements Practice Improvement
/ucm513183.htm on
30 August 2017. What measures do U.S. quinolones should be avoided in
64. Requirements for the stakeholders use to evaluate uncomplicated UTIs (provided
Catheter-Associated Uri-
nary Tract Infections the quality of care? that alternative treatment options
(CAUTI) National Patient
Safety Goal for Hospitals. Antibiotic stewardship has an are available) because the risk for
Accessed at www.joint
essential role in slowing the rise serious adverse effects generally
commission.org/assets/1
/6/R3_Cauti_HAP.pdf on of multidrug-resistant bacterial outweighs the benets.
30 August 2017.
65. Hospital Compare. Medi- pathogens. In 2011, 262 million The Joint Commission has added
care.gov. Accessed at
www.medicare.gov
prescriptions were given for out- measuring and monitoring of
/hospitalcompare/About patient antibiotics in the United CAUTI prevention practices and
/What-Is-HOS.html on
30 August 2017. States (56). Data from cross- outcomes to its requirements for
66. Saint S, Meddings JA,
Calfee D, Kowalski CP,
sectional outpatient surveys sug- acute care hospitals (64), and
Krein SL. Catheter- gest that 30% of outpatient anti- consumers can compare CAUTI
associated urinary tract
infection and the Medi- biotic prescriptions may be rates across hospitals by using
care rule changes. Ann inappropriate (57). The principle Hospital Compare at Medicare
Intern Med. 2009;150:
877-84. [PMID: of antibiotic stewardship es- .gov (65). The increased focus on
1952856784]
67. Mody L, Greene MT,
poused by the Centers for Dis- prevention of CAUTI, particularly
Meddings J, Krein SL, ease Control and Prevention in through decreasing unnecessary
McNamara SE, Trautner
BW, et al. A national its Get Smart About Antibiotics use of urinary catheters, has likely
implementation project campaign that is relevant to treat-
to prevent catheter- benetted patients (66). For ex-
associated urinary tract ment of UTI is to prescribe the ample, the Agency for Healthcare
infection in nursing
home residents. JAMA right drug in the right dose for Research and Quality funded na-
Intern Med. 2017;177: the right duration. Despite this, tional campaigns in both acute
1154-1162. [PMID:
28525923] uoroquinolones are the most and long-term care facilities that
68. Saint S, Greene MT,
Krein SL, Rogers MA,
commonly used antibiotic for un- led to decreased use of urinary
Ratz D, Fowler KE, et al. complicated acute cystitis (58 catheters and fewer CAUTIs (67,
A program to prevent
catheter-associated uri- 61). Prescribing antibiotics for an 68).
nary tract infection in excessively long duration to treat
acute care. N Engl J
Med. 2016;374:2111-9. acute cystitis is also a common What do professional organiza-
[PMID: 27248619] tions recommend with regard
69. Gould CV, Umscheid CA, practice (58, 62). Antibiotic stew-
Agarwal RK, Kuntz G, ardship programs for outpatient to care?
Pegues DA; Healthcare
Infection Control Prac- management of UTI must ad- Professional organizations in the
tices Advisory Commit-
tee. Guideline for pre-
dress both the type and duration United States and abroad have
vention of catheter- of antimicrobial therapy. The ur- released practice guidelines on
associated urinary tract
infections 2009. Infect gency of addressing these issues UTI that address 3 categories:
Control Hosp Epidemiol. was reinforced by an FDA warn- acute cystitis, CAUTI, and ASB.
2010;31:319-26. [PMID:
20156062] ing in July 2016 (63) that uoro- Guidelines for management and
2017 American College of Physicians ITC62 In the Clinic Annals of Internal Medicine 3 October 2017
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
prevention of CAUTI have been in 2005, were endorsed by the 70. Yokoe DS, Anderson DJ,
Berenholtz SM, Calfee
released by the Healthcare Infec- U.S. Preventive Services Task DP, Dubberke ER, Elling-
son KD, et al; Society for
tion Control Practices Advisory Force in 2008, and are currently Healthcare Epidemiology
Committee of the Centers for being updated. The Choosing of America (SHEA). A
compendium of strate-
Disease Control and Prevention Wisely campaign (72) of the Amer- gies to prevent
(69), the Association for Profes- ican Board of Internal Medicine healthcare-associated
infections in acute care
sionals in Infection Control and discourages urine culture in pa- hospitals: 2014 updates.
Infect Control Hosp Epi-
Epidemiology in its Compen- tients without symptoms local- demiol. 2014;35:967-
dium of Strategies to Prevent ized to the urinary tract (that is, 77. [PMID: 25026611]
71. European Association of
screening for ASB), recom-
Healthcare-Associated Infections Urology 2015 Guidelines
mends against treating bacteri- on Urologic Infections.
in Acute Care Hospitals (70), the Accessed at https:
uria in adults without specic //uroweb.org/wp-content
IDSA (32), and the European Asso- /uploads/19-Urological
urinary symptoms, and encour-
ciation of Urology (71). ASB guide- ages removing or not placing
-infections_LR2.pdf on
30 August 2017.
lines were published by the IDSA unnecessary urinary catheters. 72. ABIM Foundation.
AMDA Urine cultures
without clear signs and
symptoms. 4 September
2013. Accessed at www
.choosingwisely.org
/clinician-lists/amda
-urine-cultures on 17
August 2017.
In the Clinic Clinical Guidelines
IntheClinic
www.idsociety.org/Guidelines/Patient_Care/IDSA
Tool Kit
_Practice_Guidelines/Infections_by_Organ_System
/Genitourinary/Uncomplicated_Cystitis_and
_Pyelonephritis_(UTI)
Guidelines from the Infectious Diseases Society of
America.
www.nice.org.uk/guidance/qs90
Guidelines for treatment of adults with UTI from the
Urinary Tract National Institute for Health and Care Excellence.
Infection Patient Information
www.acponline.org/system/les/documents/practice
-resources/patient-resources/urinary-tract-infection
Printable information for patients from the American
College of Physicians.
https://medlineplus.gov/urinarytractinfections.html
Printable handouts for patients on various aspects of UTI.
3 October 2017 Annals of Internal Medicine ITC63 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
WHAT YOU SHOULD In the Clinic
Annals of Internal Medicine
KNOW ABOUT URINARY
TRACT INFECTION
What Is a Urinary Tract Infection?
A urinary tract infection (UTI) is a common infec-
tion of the urethra (the tube that takes urine out
of the body), bladder, or kidney. Bacteria can
get into the urethra and travel to the bladder,
causing an infection. The infection can also
travel to the kidneys. You may have higher risk
for UTIs if you:
Men can also get UTIs, but they are more
common in women.
Are sexually active.
Are pregnant.
Use certain types of birth control, such as a
spermicide.
Have a blocked ow of urine, for example
from a kidney stone.
Use a urinary catheter.
Have diabetes.
Have bladder or spinal cord injuries.
Have an enlarged prostate.
Have had a previous UTI.
What Are the Warning Signs?
Pain or burning when urinating
Urgent or frequent need to urinate
Blood in the urine
Pain in the lower back or pelvic area
Fever
Patient Information
How Is It Diagnosed?
Your doctor will ask about your symptoms. In
some cases, you may need to give a urine sam-
ple, which will help your doctor conrm UTI and this is a good option because resistance to anti-
decide which treatment is best. biotics is increasing.
How Is It Treated? Questions for My Doctor
Medicines called antibiotics are used to treat How can I prevent future UTIs?
UTIs. When will my symptoms go away?
Some people get frequent UTIs. Talk with your Do I need medicine? How should I take it?
doctor about treatment options if this is the If I don't take antibiotics, will the infection go
case. away on its own?
What should I do if I don't feel better after
How Can It Be Prevented? taking the antibiotics?
If you have frequent UTIs, your doctor may sug- Does drinking cranberry juice help?
gest patient-initiated therapy when you have Do over-the-counter medicines treat the
typical symptoms or may prescribe an antibiotic infection?
to take after sex, although it is unclear whether Should I stop having sex when I have a UTI?
For More Information
MedlinePlus
https://medlineplus.gov/urinarytractinfections.html
National Institutes of Health
www.niddk.nih.gov/health-information/urologic-diseases/bladder
-infection-uti-in-adults
Downloaded From: https://annals.org/ by a Dalhousie University-Dal-11762 User on 10/03/2017
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Test Bank For Medical Terminology 2nd Edition by BostwickDocument7 pagesTest Bank For Medical Terminology 2nd Edition by Bostwicka596727542No ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Digestive System Test Questions and AnswersDocument4 pagesDigestive System Test Questions and Answersflorin100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Rehabilitation of Muscle Dysfunction in HemophiliaDocument14 pagesRehabilitation of Muscle Dysfunction in HemophiliadavidcorzoNo ratings yet
- Nursing Care Plan For "Herniated Nucleus Pulposus Ruptured Inter Vertebral Disc"Document9 pagesNursing Care Plan For "Herniated Nucleus Pulposus Ruptured Inter Vertebral Disc"jhonroks100% (7)
- DENGUE CS NCP 1Document8 pagesDENGUE CS NCP 1Karyl SaavedraNo ratings yet
- Doctors Tell All-And It's Bad - Meghan O'Rourke - The AtlanticDocument7 pagesDoctors Tell All-And It's Bad - Meghan O'Rourke - The AtlanticAlexNo ratings yet
- Pathophysiology of Septic ShockDocument19 pagesPathophysiology of Septic ShockRoberto López MataNo ratings yet
- AnalgesicDocument56 pagesAnalgesicMuhammad hilmiNo ratings yet
- Prometric Exam Ophthalmology 28-3-2013Document10 pagesPrometric Exam Ophthalmology 28-3-2013Hasan Dahamsheh100% (4)
- Hyperglycemic CrisisDocument9 pagesHyperglycemic CrisisRoberto López MataNo ratings yet
- 2017 ACC Expert Consensus Decision Pathway For Optimization of Heart Failure TreatmentDocument30 pages2017 ACC Expert Consensus Decision Pathway For Optimization of Heart Failure TreatmentRoberto López MataNo ratings yet
- Top 10 Myths Regarding The Diagnosis and Treatment of CellulitisDocument8 pagesTop 10 Myths Regarding The Diagnosis and Treatment of CellulitisRoberto López MataNo ratings yet
- Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Synopsis of The 2017 American College of Cardiology:American Heart Association Hypertension GuidelineDocument10 pagesPrevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Synopsis of The 2017 American College of Cardiology:American Heart Association Hypertension GuidelineRoberto López MataNo ratings yet
- HTN Emergencies and UrgenciesDocument14 pagesHTN Emergencies and UrgenciesRoberto López MataNo ratings yet
- Update On The Management of Venous ThromboembolismDocument8 pagesUpdate On The Management of Venous ThromboembolismRoberto López MataNo ratings yet
- Necrotizing Soft-Tissue InfectionsDocument13 pagesNecrotizing Soft-Tissue InfectionsRoberto López MataNo ratings yet
- Best Clinical Practice: AnaphylaxisDocument6 pagesBest Clinical Practice: AnaphylaxisputriNo ratings yet
- Fluid Therapy Options and Rational SelectionDocument13 pagesFluid Therapy Options and Rational SelectionRoberto López MataNo ratings yet
- ADA 2018 Diabetes CareDocument150 pagesADA 2018 Diabetes CareRoberto López Mata100% (1)
- Diagnosis and Treatment of HyperkalemiaDocument9 pagesDiagnosis and Treatment of HyperkalemiaRoberto López MataNo ratings yet
- Uric Acid Is A Strong Risk Marker For Developing Hypertension From PrehypertensionDocument16 pagesUric Acid Is A Strong Risk Marker For Developing Hypertension From PrehypertensionRoberto López MataNo ratings yet
- Sudden Cardiac Arrest During Participation in Competitive SportsDocument11 pagesSudden Cardiac Arrest During Participation in Competitive SportsRoberto López MataNo ratings yet
- Hepatitis B Vaccination, Screening, and Linkage To Care - Best Practice Advice From The American College of Physicians and The Centers For Disease Control and PreventionDocument12 pagesHepatitis B Vaccination, Screening, and Linkage To Care - Best Practice Advice From The American College of Physicians and The Centers For Disease Control and PreventionRoberto López MataNo ratings yet
- Atrial Fibrillation and HypertensionDocument17 pagesAtrial Fibrillation and HypertensionRoberto López MataNo ratings yet
- Effects on the Incidence of Cardiovascular Events of the Addition of Pioglitazone Versus Sulfonylureas in Patients With Type 2 Diabetes Inadequately Controlled With Metformin (TOSCA.it)- A Randomised, Multicentre TrialDocument11 pagesEffects on the Incidence of Cardiovascular Events of the Addition of Pioglitazone Versus Sulfonylureas in Patients With Type 2 Diabetes Inadequately Controlled With Metformin (TOSCA.it)- A Randomised, Multicentre TrialRoberto López MataNo ratings yet
- The Use of Cephalosporins in Penicillin-Allergic Patients - A Literature ReviewDocument9 pagesThe Use of Cephalosporins in Penicillin-Allergic Patients - A Literature ReviewRoberto López MataNo ratings yet
- The Role of Nitroglycerin and Other Nitrogen Oxides in Cardiovascular TherapeuticsDocument18 pagesThe Role of Nitroglycerin and Other Nitrogen Oxides in Cardiovascular TherapeuticsRoberto López MataNo ratings yet
- The Dark Sides of Fuid Administration in The Critically Ill PatientDocument3 pagesThe Dark Sides of Fuid Administration in The Critically Ill PatientRoberto López MataNo ratings yet
- Diuretic Treatment in Heart FailureDocument12 pagesDiuretic Treatment in Heart FailureRoberto López Mata100% (1)
- Effects of Acarbose On Cardiovascular and Diabetes Outcomes in Patients With Coronary Heart Disease and Impaired Glucose Tolerance (ACE) - A Randomised, Double-Blind, Placebo-Controlled TrialDocument10 pagesEffects of Acarbose On Cardiovascular and Diabetes Outcomes in Patients With Coronary Heart Disease and Impaired Glucose Tolerance (ACE) - A Randomised, Double-Blind, Placebo-Controlled TrialRoberto López MataNo ratings yet
- Synopsis of The 2017 U.S. Department of Veterans Affairs: Management of Type 2 Diabetes MellitusDocument10 pagesSynopsis of The 2017 U.S. Department of Veterans Affairs: Management of Type 2 Diabetes MellitusRoberto López MataNo ratings yet
- A Test in Context - D-DimerDocument10 pagesA Test in Context - D-DimerRoberto López MataNo ratings yet
- Rivaroxaban Vs Warfarin Sodium in The Ultra-Early Period After Atrial Fibrillation-Related Mild Ischemic StrokeDocument10 pagesRivaroxaban Vs Warfarin Sodium in The Ultra-Early Period After Atrial Fibrillation-Related Mild Ischemic StrokeRoberto López MataNo ratings yet
- 2015 ESC Guidelines For The Diagnosis and Management of Pericardial DiseasesDocument44 pages2015 ESC Guidelines For The Diagnosis and Management of Pericardial DiseasesRoberto López MataNo ratings yet
- Acute Monocular Vision LossDocument9 pagesAcute Monocular Vision LossRoberto López MataNo ratings yet
- Dual Antithrombotic Therapy With Dabigatran After PCI in Atrial FibrillationDocument12 pagesDual Antithrombotic Therapy With Dabigatran After PCI in Atrial FibrillationRoberto López MataNo ratings yet
- Evaluation and Management of Lower-Extremity UlcersDocument9 pagesEvaluation and Management of Lower-Extremity UlcersRoberto López MataNo ratings yet
- Aquatic Exercise - Lung Function and Weight LossDocument48 pagesAquatic Exercise - Lung Function and Weight LossDr Vaishali MathapatiNo ratings yet
- Price List PT - Thirza 2019Document8 pagesPrice List PT - Thirza 2019Permana JuliansyahNo ratings yet
- Volunteer Report FinalDocument11 pagesVolunteer Report FinalBeenish JehangirNo ratings yet
- GHC Gut Health Course Syllabus - MKTGDocument23 pagesGHC Gut Health Course Syllabus - MKTGKat HerreraNo ratings yet
- Use of Oral Rehydration Therapy in The Treatment of Childhood Diarrhoea in Douala, CameroonDocument5 pagesUse of Oral Rehydration Therapy in The Treatment of Childhood Diarrhoea in Douala, CameroonKiti AstutiNo ratings yet
- Scribd 020922 Case Study-Oncology A&kDocument2 pagesScribd 020922 Case Study-Oncology A&kKellie DNo ratings yet
- Surgery Chapter 1 SkinDocument6 pagesSurgery Chapter 1 Skinnandoooo86No ratings yet
- Atom Electrosurgical SystemDocument40 pagesAtom Electrosurgical SystemOgut AjaNo ratings yet
- GallstonesDocument17 pagesGallstonesع ب و دNo ratings yet
- Pulmonary Edema and Hemorrhagination Causes in Salt Water Drowning (39Document9 pagesPulmonary Edema and Hemorrhagination Causes in Salt Water Drowning (39Akash AkashNo ratings yet
- Caring Adoption Associates: Medical Examination Report of Prospective Adoptive ParentDocument1 pageCaring Adoption Associates: Medical Examination Report of Prospective Adoptive ParentaniketsethiNo ratings yet
- Title: Congenital Hypothyroidism: A Ran Sacker Escaping Under The Nose AbstractDocument6 pagesTitle: Congenital Hypothyroidism: A Ran Sacker Escaping Under The Nose AbstractKavita KhannaNo ratings yet
- 10 1016@j Joen 2019 10 009Document8 pages10 1016@j Joen 2019 10 009fatimahNo ratings yet
- Lesson 3 BloodDocument50 pagesLesson 3 BloodJulius Memeg PanayoNo ratings yet
- IU Vaccine LawsuitDocument55 pagesIU Vaccine LawsuitJoe Hopkins100% (2)
- College Nursing Exam ReviewDocument8 pagesCollege Nursing Exam ReviewKenneth NovenoNo ratings yet
- Phylum Class Order Genera: Apicomplexa Haematozoa Haemosporida Plasmodium Piroplasmida Coccidia EimeriidaDocument39 pagesPhylum Class Order Genera: Apicomplexa Haematozoa Haemosporida Plasmodium Piroplasmida Coccidia EimeriidaMegbaruNo ratings yet
- Resume Atiyeh KaboudvandDocument2 pagesResume Atiyeh Kaboudvandarian tejaratNo ratings yet
- Annotated Bibliography On Internet AddictionDocument4 pagesAnnotated Bibliography On Internet AddictionJanet Martel100% (3)
- Allen Part Pedia CaseDocument3 pagesAllen Part Pedia CasePaul Michael Baguhin0% (1)
- Indian List-Of-HospitalsDocument564 pagesIndian List-Of-HospitalsPinder BaiNo ratings yet
- The Role of Drotaverine in IbsDocument5 pagesThe Role of Drotaverine in IbsAli Abd AlrezaqNo ratings yet