Professional Documents
Culture Documents
Reviewer On Immunization (KMBM)
Uploaded by
Kathleen Grace Maniago0 ratings0% found this document useful (0 votes)
35 views8 pagesreviewer immunization
Original Title
Reviewer on Immunization (Kmbm)
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentreviewer immunization
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
35 views8 pagesReviewer On Immunization (KMBM)
Uploaded by
Kathleen Grace Maniagoreviewer immunization
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 8
IMMUNIZATION o Live attenuated microorganism
The process of inducing immunity against a specific Measles, mumps, rubella,
disease varicella, rotavirus, and live
Passive through administration of antibody- attenuated influenza vaccines
containing preparations o Toxoids
Active by administering a vaccine or toxoid to Modified bacterial toxin made
stimulate the immune system to produce a non-toxic but still able to induce
prolonged humoral and/or cellular immune an active immune response
response Tetanus and diphtheria
Passive Active Most B-lymphocyte response re quire the assistance of
Administration of Injection of an antigen CD4 helper T lymphocytes. These T-lymphocyte-
preformed Ab dependent responses tend to induce high levels of
Can be induced naturally Protection produced by functional antibody with high avidity, mature over time
through transplacental the persons own from primarily an IgM response to a long-term persistent
transfer of Ab during immune system IgG response and induce immunologic memory that
gestation leads to enhanced responses upon boosting.
Protection may persist Usually permanent T-lymphocyte-dependent vaccines
for months to as long as o Include protein moieties
a year after birth o Induce good immune responses even in
young infants
T-lymphocyte-independent vaccines
PASSIVE IMMUNIZATION
o Polysaccharide antigens induce B-
Major indication - to provide protection to:
lymphocyte responses in the absence
Immunodeficient children with B-
of T-lymphocyte help
lymphocyte defects who have difficulties
o Associated with poor immunity, and
making Ab
absence of an enhanced or booster
Persons exposed to infectious diseases or
response on repeat exposure to the
at imminent risk of exposure where there is not
antigen
adequate time to develop an active immune
o To overcome this, polysaccharides
response to a vaccine
have been conjugated, or covalently
Persons with an infectious disease as part of
linked, to protein carriers, converting
specific therapy for that disease
the vaccine to a T-lymphocyte-
dependent vaccine
ACTIVE IMMUNIZATION
Live Attenuated Vaccines
VACCINES
Tend to induce long-term responses
Defined as whole or parts of microorganisms
They replicate, often similarly to natural
administered to prevent an infectious disease
infections, until an immune response shuts
Can induce immunity through stimulation of
down reproduction
antibody formation, cellular immunity, or both
Mostly administered as single-dose schedules
Protection is thought to be mediated primarily
Repeat dose, like MMR, is to induce an initial
by B-lymphocytes, which produce antibody
immune response in persons who failed to
Can consist of:
respond to the first dose
o Whole inactivated microorganisms
IPV, Hepatitis A
Inactivated Vaccines
o Parts of microorganism
Tend to require multiple doses to induce an
Acellular pertussis, HPV,
adequate immune response
Hepatitis B
More likely to need boosters to maintain
o Polysaccharide capsules
immunity
Pneumococcal and
Some inactivated vaccines, however, appear
meningococcal polysaccharide
to induce long-term immunity, perhaps life-long,
vaccines
after a primary series
o Polysaccharide capsules conjugated to
o e.g. Hep B vaccine, IPV
protein carrier
Hib, pneumococcal, and
meningococcal conjugate
vaccines
ROUTE OF ADMINISTRATION A rapid plunge of the needle through the
Injectable vaccines should be administered in skin without aspirating and rapid injection
areas unlikely to cause local neural, vascular, or may decrease discomfort
tissue injury. Rubbing or stroking the skin near the
o Upper, outer quadrant of the buttocks injection site with moderate intensity before
should not be used because the gluteal and during vaccination also may reduce the
region consists mostly of fat in young sensation of pain
children and because of potential injury Psychological Techniques for Minimizing
to the sciatic nerve Injection Pain
Intramuscular (IM) injections for infants and Parent-led or physician-led age-
young children appropriate distraction can reduce
o Anterolateral thigh muscle pain-related distress at the time of
preferred because of its muscle injection
mass relative to other sites Pharmacologic Techniques for Minimizing
o Needle length Injection Pain
58 in. for newborn infants Topically applied agents may reduce
1 in. for infants 2-12 mo./o the pain of injection
1 to 1 14 in for older children o Currently available topical
IM injections for adolescents and adults anesthetics require 30-60
o Deltoid muscle of the arm minutes to provide adequate
o Needle length: 1 1 12 in anesthesia so planning ahead is
Subcutaneous inoculations also usually necessary
should be given in the thigh of infants and the
deltoid area of older children Simultaneous Administration of Multiple Vaccines
Intradermal vaccines generally should be Most vaccines can be given simultaneously
administered on the volar aspect of the forearm without impairment of effectiveness or safety
Data indicate possible impaired immune
Most inactivated vaccines, including DTaP, Hep responses when 2 or more parenterally
A, Hep B, Hib, inactivated influenza vaccine, administered live-virus vaccines are not given
PCV13, MCV4, and Tdap, are administered simultaneously but rather within 28 days of each
intramuscularly (IM). other
Commonly used live attenuated vaccines, MMR
and varicella, should be dispensed
subcutaneously (SC)
IPV and PPS23 (pneumococcal polysaccharide
vaccine) can be given IM or SC
RV vaccine and OPV are the only US-licensed
vaccines for children that are administered by
the oral route
Managing Injection Pain
Truthful & empathetic preparation for injections
is beneficial, using the words that are
explanatory without evoking anxiety
pressure, squeezing and poking rather
than pain, hurt and shot
Parents and medical care providers should not VACCINE CONTRAINDICATIONS AND
tell children that it wont hurt because this type PRECAUTIONS
of statement has been show to ineffective in Contraindication
reducing pain at the time of injection o A condition in a patient that increases
Physical Techniques for Minimizing Injection the risk of a serious adverse reaction
and for whom this increased risk of an
Pain
adverse reaction outweighs the benefit
Breastfeeding
of the vaccine
Children should be held on the lap of a
parent or other caregiver
Older children may be more comfortable
sitting on the examination table edge &
hugging their parent chest to chest
Precaution Family history of sudden unexpected death
o A condition in a recipient that might Family history of an adverse event following
increase the risk or seriousness of an immunization
adverse reaction or complicate making Breastfeeding or pregnancy in a household
another diagnosis because of a contact
possible vaccine-related reaction
Established, generic contraindications are: Lapsed Immunizations
o moderate or severe illness A lapse in the immunization schedule does not
o a previous anaphylactic reaction to the require reinitiating the entire series or addition of
specific vaccine, and doses to the series for any vaccine in the
o a severe hypersensitivity reaction, such recommended schedule
as anaphylaxis, to a vaccine constituent Subsequent immunizations should be given at
The decision to defer immunization in a febrile the next visit as if the usual interval had elapsed
child should be based on the physicians o For RV vaccine, the doses to be
assessment of the severity of the illness rather administered are age limited, so catch-
than the degree of fever up may not be possible
o Children with minor illness and low-
grade fever generally should be Unknown or Uncertain Immunization Status
vaccinated, especially if a child is A person with unknown or uncertain
unlikely to return promptly for the immunization status should be considered
deferred immunization disease-susceptible, and recommended
Administration of live virus vaccines such as immunizations should be initiated without delay
MMRV generally is contraindicated in patients on a schedule commensurate with the persons
with altered immunity current age
o Morbidity & mortality rates of measles Serologic testing is an alternative to vaccination
and lack of complication from for certain antigens (e.g. measles, rubella,
vaccination of children infected with HIV hepatitis A, and tetanus)
have led to recommendations that No evidence suggests that administration of
these children, unless significantly vaccines to already immune recipients is
immunocompromised, receive the harmful
MMR vaccine
Because of a theoretical risk to the developing Interchangeability of Vaccine Products
fetus, administration of live virus vaccines in When possible, effort should be made to
most cases is not recommended for pregnant complete a series with vaccine made by the
women same manufacturer
Although data documenting the effects of
MISCONCEPTIONS interchangeability are limited, most experts
Common conditions that should not delay vaccination have considered vaccines interchangeable
but often are considered mistakenly to be when administered according to their
contraindications include: recommended indications
Diarrhea Licensed vaccines that may be used
Minor upper respiratory tract illnesses (including interchangeably during a vaccine series
otitis media) with or without fever include:
Mild to moderate local reactions to a previous o Diphtheria & tetanus toxoid
dose of vaccine vaccines
Exposure to an infectious disease o Hepatitis A vaccines
Current antimicrobial therapy o Hepatitis B vaccines
Being in the convalescent phase of an acute o Rabies vaccines
illness o RV vaccines
Allergy to duck meat or duck feathers as long as recommendations
Allergy to an antibiotic (except anaphylactic concerning conversion from a 2-
reaction to neomycin, gentamicin, dose regimen to a 3-dose
or streptomycin, if any of these are in the regimen are followed
vaccine to be administered) o Hib conjugate vaccines
History of non-anaphylactic allergy to egg as long as recommendations for a
Personal or family history of seizures total of 3 doses in the first year of
life are followed
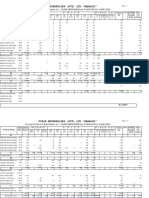
The National Immunization Program (NIP) o Measles-Mumps-Rubella (MMR)
Previously known as the Expanded Program on vaccine given at 12 months of age
Immunization (EPI) A school based immunization program to
Consists of the following antigens: provide catch-up doses for school children and
o BCG vaccine, single dose given at birth adolescents has been established
o Monovalent Hepatitis B vaccine given at o Measles-Rubella (MR) and Tetanus-
birth Diphtheria (Td) vaccines are
o DPT-Hib-Hep B vaccine, 3 doses given administered to Grade 1 and Grade 7
at 6-10-14 weeks of age students enrolled in public schools
o Oral Polio vaccine (OPV), 3 doses given o Human Papillomavirus (HPV) shall be
at 6-10-14 weeks of age, a single dose given to female children 9-10 years old
of Inactivated Polio vaccine (IPV) is at health facilities in priority provinces
given with the 3rd dose of OPV at 14 Quadrivalent HPV 2 doses are
weeks given at 0, 6 months
o Pneumococcal conjugate vaccine
(PCV), 3 doses given at 6-10-14 weeks Other recommended vaccines not part of the NIP
of age o Japanese Encephalitis vaccine
o Rotavirus vaccine given at a minimum o Influenza vaccine (Trivalent/Quadrivalent)
age of 6 weeks with a minimum interval o Hepatitis A vaccine
of 4 weeks between doses. The last
dose should be administered not later Interim recommendation for use
than 32 weeks of age. o Dengue tetravalent vaccine
o Measles-containing vaccine (either
monovalent measles vaccine or MMR)
given at 9 months of age
BACILLE CALMETE-GURIN (BCG) VACCINE Special Indications
Live attenuated strain derived from o For pre-term infants
Mycobacterium bovis Born to HBsAg (-) mothers &
Used primarily in young infants in an attempt to medically stable give 1 dose
st
prevent disseminated and other life-threatening at 30 days chronological age
manifestations of M. tuberculosis disease regardless of weight and this can
o However, does not prevent infection with be counted as part of the 3-dose
M. tuberculosis primary series
Given on the right upper deltoid, intradermally, at Another dose of HBV is needed
birth or at earliest possible age after birth, for those < 2 kg whose 1 dose
st
preferably within the first 2 months was received at birth
Dose: o For term infants
o 0.05 mL children less than 12 months Born to HBsAg (+) mothers -
o 0.1 mL children more than 12 months give HBV and HBIg (0.5 mL)
Contraindications: within 12 hours of life. HBIg
o Burns, skin infections, certain primary or should be administered not later
secondary immunodeficiencies (including than 7 days of age, if not
HIV infection), persons receiving immediately available
immunosuppressive medications o For infants born to mothers w/
(including high-dose corticosteroids) unknown HBsAg status
Adverse Reactions BW 2 kg
o Uncommon (1-2%) Administer HBV within
Subcutaneous abscess 12 hours of birth and
Regional (axillary) determine mothers
lymphadenopathy HBsAg ASAP. If HBsAg
o Rare (0.1 to 1 case per million) (+), administer HBIg not
Osteitis affecting the epiphysis of later than 7 days of age
long bones BW < 2 kg
Disseminated fatal infection Administer HBIg in
addition to HBV within
Usual Accelerated 12 hours of life
Reactions Reactions Contraindications
Induration 2-4 weeks 2-3 days o History of anaphylaxis to a previous dose
Pustule formation 5-7 weeks 5-7 days of vaccine
Scar formation 2-3 months 2-3 weeks Adverse Reactions
o Soreness at injection site
o Possible association with GBS following
HEPATITIS B VACCINE
first dose of plasma-derived vaccine; no
HBV infection is a leading cause of acute hepatitis
evidence of association with recombinant
Incidence is especially high in many Asian and
vaccine
African countries
Given intramuscularly, in the anterolateral thigh or
DIPHTHERIA AND TETANUS TOXOID AND PERTUSSIS
deltoid area (depending on the age and size of the
(DTP) VACCINE
recipient)
Diphtheria and Tetanus component are toxoids
o Only single-antigen hepatitis B vaccine
while Pertussis component can either be whole-
can be used for doses given to infants
cell (DTP) or acellular (DTaP)
between birth and 6 weeks of age
o Incidence of local and systemic reactions
o Single-antigen or combination vaccine
are more associated with whole-cell
may be used to complete the series; four
pertussis vaccine
doses of vaccine may be administered if a
Given intramuscularly
birth dose is given and a combination
vaccine is used to complete the series Given at a minimum age of 6 weeks with a
Schedule: Birth-6-10-14 weeks (minimum interval minimum interval of 4 weeks
o Recommended interval between 3rd and
of 4 weeks)
Dose: 0.5 mL 4th dose is 6 months but a minimum of 4
months is valid
o 5th dose may not be given if the 4th dose
was administered at age 4 years or older
Contraindications Adverse Reactions
o Immediate anaphylactic reaction o Hib vaccines are well-tolerated
subsequent immunization with any of the o Local reactions occur in approximately
three components should be avoided 25% of recipients but typically are mild
o Encephalopathy and last less than 24 hours
Defined as a severe, acute, CNS
disorder unexplained by another POLIOMYELITIS VACCINE
cause and may be manifested by Two forms:
major alterations in o OPV (Sabin strain)
consciousness or by generalized Elimination of poliovirus infection
or focal seizures that persist for has been achieved primarily
more than a few hours without through the use of OPV
recovery within 24 hours Induced optimal intestinal
Occurring within 7 days after immunity, painless and
administration of a previous dose secondarily immunized some
of DTP/DTaP/Tdap not contacts by fecal-oral spread of
attributable to another the vaccine virus
identifiable cause o IPV (Salk strain)
Should not receive additional To eliminate the risk for vaccine-
doses of a vaccine that contains associated paralytic polio
pertussis Since 2000, outbreaks of paralytic poliomyelitis
Adverse Reactions caused by neurovirulent polioviruses that are
o Whole-cell pertussis vaccine derived from Sabin OPV vaccine strain have
Local & febrile reactions more occurred among underimmunized children living in
common; develop within the first certain economically deprived regions
24 hours and brief in duration o Low immunization rates permitted these
More serious uncommon, vaccine-derived polioviruses (VDPV) to
usually occurs within the first 48 circulate for long periods of time and by
hours of receiving vaccination, continuous mutation, acquire biologic
resolves spontaneously without properties that are indistinguishable from
sequelae: naturally occurring wild polioviruses
Prolonged crying for 3 OPV given per orem; IPV given intramuscularly
hours or longer Contraindications
occurring o History of anaphylactic reaction after
Temperature of 40.5OC receiving a previous dose of IPV or an
or greater anaphylactic reaction to one of the
Hypotonic- antibiotics in the vaccine preparation (i.e.
hyporesponsive episode streptomycin, polymyxin B or neomycin)
described as collapse or o Pregnant women
shock-like state Adverse Reactions
Seizure within 3 days of o OPV can cause vaccine-associated
vaccination brief, self- paralytic polio
limited, and generalized
and occur in association PNEUMOCOCCAL VACCINE
with fever S. pneumoniae is the most common cause of otitis
o Acellular pertussis vaccine media, occult bacteremia, and bacterial
Local & febrile reactions as well pneumonia requiring hospitalization
as more serious reactions rarely Given intramuscularly, for 3 doses, at a minimum
occur age of 6 weeks with an interval of at least 4 weeks
between doses plus a booster dose given 6
HAEMOPHILUS INFLUENZAE TYPE B (Hib) VACCINE months after the 3rd dose
Before the introduction of routine infant and Adverse Reactions
childhood vaccination against Hib, this pathogen o PCV appears to be safe
was the major cause of invasive bacterial o Most commonly reported reactions are
infections in young children (meningitis and local reactions at the injection site
epiglottitis) Contraindications
Given intramuscularly o In persons who have had a severe
Given as a 3-dose primary series with a minimum reaction, such as anaphylaxis or a
age of 6 weeks and a minimum interval of 4 weeks; localized, severe hypersensitivity
booster dose is given between 12-15 months of response, revaccination should be
age with an interval of 6 months from the 3rd dose avoided
ROTAVIRUS VACCINE Contraindications
RV is a major cause of AGE o Immunocompromised patients
Given per orem (malignancy, primary or secondary
o Monovalent human RV vaccine (RV1) is immunodeficiency states) EXCEPT
given as a 2-dose series asymptomatic HIV-infected patients
Provided as a lyophilized powder After cessation of chemotherapy,
that is reconstituted with a patients should not receive
supplied diluent measles vaccine for at least 3
o Pentavalent human bovine RV vaccine months
(RV5) is given as a 3-dose series o Persons who have received systemic
Provided in a squeezable plastic corticosteroids in doses of 2mkday or 20
dosing tube with a twist-off cap mg daily or on alternate days for an
Given at a minimum age of 6 weeks with a interval of 14 days or longer should avoid
minimum interval of 4 weeks between doses; the receiving MMR vaccine for at least 1
last dose should be administered not later than 32 month after cessation of CS therapy
weeks of age
Contraindications MEASLES-MUMPS-RUBELLA (MMR) VACCINE
o Severe hypersensitivity to any component Given subcutaneously, for 2 doses, at a minimum
of the vaccine age of 12 months with a minimum interval of at
RV1 oral applicator contains latex least 4 weeks
o Severe combined immunodeficiency o 2nd dose is usually given from 4-6 years of
(SCID) age but may be given earlier
o History of intussusception Adverse Reactions
o RV vaccine should not be administered to o Parotitis and fever mumps component
infants with acute, moderate to severe o Fever, lymphadenopathy, or rash rubella
gastroenteritis until the condition component
improves Contraindications
Adverse Reactions o Pregnancy
o Intussusception o Sever febrile illness
Associated with a tetravalent o Known history of anaphylactic reaction to
rhesus-based RV vaccine; rubella vaccine, gelatin or neomycin
withdrawn from the market o Immunodeficiency states
Data from phase III efficacy trials
of RV5 did not suggest an VARICELLA VACCINE
increased risk for development of Given subcutaneously, for 2 doses, at a minimum
intussusception relative to age of 12 months (12-15 mos) and 2 dose given
nd
placebo at 4-6 years of age
o 2-dose regimen is recommended to
MEASLES VACCINE prevent breakthrough varicella
Given subcutaneously, at age 9 months but may (chickenpox occurring in a previously
be given as early as 6 months of age in cases of vaccinated person) due to waning
outbreaks as declared by public health authorities antibody titers
Adverse Reactions Adverse Reactions
o Immunization produces a mild or o Local reactions
inapparent, non-communicable infection o Varicella-like rash at site of injection
o Vaccine-associated symptoms (fever Occur within 2 weeks, usually
higher than 39.4OC occurring 5-10 days maculopapular rather than
after immunization or transient rash) vesicular
develop in 5-18% of recipients Contraindications similar to MMR vaccine
o Thrombocytopenia
Usually not clinically apparent MEASLES-MUMPS-RUBELLA-VARICELLA (MMRV)
but thrombocytopenic purpura VACCINE
occurring after vaccination has Can be given as an alternative to separately
been reported administered MMR and varicella vaccine
o CNS disease (encephalitis or
encephalopathy) reported at a rate of
less than 1 case/1 million doses of
vaccine administered
o SSPE risk is extremely low (0.7 SSPE
cases per million vaccine doses)
o To date, no convincing evidence
establishes that any vaccine causes
autism or autism spectrum disorder
INFLUENZA VACCINE HEPATITIS A VACCINE
2 forms Given intramuscularly, as a 2-dose series, at a
o Trivalent vaccine given either minimum age of 12 months where the 2nd dose is
intramuscularly or subcutaneously given at least 6 months from the 1st dose
o Quadrivalent vaccine given
intramuscularly HUMAN PAPILLOMAVIRUS VACCINE (HPV)
Dose: Genital HPV infection is thought to be the most
o 6 months to 35 months 0.25 mL common sexually transmitted viral infection
o 36 months to 18 years 0.5 mL Infection with HPV causes virtually all cases of
Given at a minimum age of 6 months cervical cancer
o Children 6 months to 8 years receiving Given intramuscularly, as a 3-dose series, with a
influenza vaccine for the first time 2 minimum age of 9 years
doses, 4 weeks apart 2 types and schedule of doses
o Children 9 to 18 years 1 dose annually o Bivalent HPV (HPV2) given at 0, 1 and 6
Schedule: Annual vaccination should begin in months
February but may be given throughout the year o Quadrivalent HPV (HPV4) given at 0, 2 and
Contraindications 6 months
o Trivalent inactivated influenza vaccine The only HPV vaccine
(TIV) recommended for routine
Infants younger than 6 months immunization of males at 11 or 12
Children who have a moderate to years of age
severe febrile illness Minimum interval between the 1st and 2nd dose is
o Live attenuated influenza vaccine (LAIV) at least 1 month and the minimum interval between
Pregnancy the 2nd and 3rd dose is at least 3 months.
Children younger than 2 years o 2-dose schedule is an option for girls 9 to
Moderate to severe febrile illness 14 years of age for both HPV2 and HPV4,
Receiving aspirin or salicylates doses given at least 6 months apart
Immunosuppressed states
Chronic, underlying medical
condition (metabolic disorders, SOURCES:
DM, pulmonary, cardiac, renal
disorders or Chapter 172, Nelson Textbook of Pediatrics, 20th edition
hemoglobinopathies) Chapter 244, Feigin & Cherrys Textbook of Pediatric
Children aged 2-4 years old with Infectious Diseases, 7th edition
a history of recurrent wheezing or Red Book 30th edition, American Academy of Pediatrics
a medically attended wheezing Preventive Pediatric Health Care Handbook 2016,
episode in the previous 12 Philippine Pediatric Society
months
Children taking influenza antiviral
medications should not receive kmbm 2016
LAIV until 48 hours after stopping
therapy
JAPANESE ENCEPHALITIS VIRUS VACCINE
JE virus is the most important cause of epidemic
arboviral encephalitis in Asia
o JE is endemic in the Philippines
Given subcutaneously
o Children 9 months to 17 years should
receive one primary dose followed by a
booster dose 12-24 months after the
primary dose
o Individuals 18 years and older should
receive a single dose only
Contraindications
o Previous severe allergic reaction after a
previous dose of JE-VC is a
contraindication to administration of
subsequent doses
Contains protamine sulfate
Adverse Reactions
o Local or mild systemic reactions
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Intern Pocket Card Surviving GraysDocument2 pagesThe Intern Pocket Card Surviving GraysKathleen Grace ManiagoNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Immunization LectureDocument32 pagesImmunization LectureMekdes ZewdeNo ratings yet
- Immunization Review GPDocument46 pagesImmunization Review GPKishore ChandkiNo ratings yet
- Anes Drugs TableDocument20 pagesAnes Drugs TableKathleen Grace ManiagoNo ratings yet
- Vaccination: Yunus Ariyanto FKM - Univ. JemberDocument11 pagesVaccination: Yunus Ariyanto FKM - Univ. JemberDian WidyaningtyasNo ratings yet
- Obstetrics and Gynecology Mock Simulation OutputDocument4 pagesObstetrics and Gynecology Mock Simulation OutputKathleen Grace ManiagoNo ratings yet
- Learn Basic Knot TyingDocument10 pagesLearn Basic Knot TyingKathleen Grace Maniago100% (1)
- IM Typed HeheDocument12 pagesIM Typed HeheKathleen Grace ManiagoNo ratings yet
- Personal Protective Equipment (PPE) Alex P. Bello MDDocument8 pagesPersonal Protective Equipment (PPE) Alex P. Bello MDKathleen Grace ManiagoNo ratings yet
- Thyroid PhysiologyDocument25 pagesThyroid PhysiologyKathleen Grace ManiagoNo ratings yet
- ARMY ScienceDocument3 pagesARMY ScienceKathleen Grace ManiagoNo ratings yet
- When Your Anxiety Is Getting The Best of YouDocument1 pageWhen Your Anxiety Is Getting The Best of YouKathleen Grace ManiagoNo ratings yet
- Ultrasound RotationDocument4 pagesUltrasound RotationKathleen Grace ManiagoNo ratings yet
- New Doc NewDocument1 pageNew Doc NewKathleen Grace ManiagoNo ratings yet
- With Notesent 1Document8 pagesWith Notesent 1Kathleen Grace ManiagoNo ratings yet
- ...Document1 page...Kathleen Grace ManiagoNo ratings yet
- Commed SummaryDocument19 pagesCommed SummaryKathleen Grace ManiagoNo ratings yet
- Ent 3Document3 pagesEnt 3Kathleen Grace ManiagoNo ratings yet
- Q 1 - P, Then The Probability Distribution of A Binomial Random Variable X, The Number ofDocument3 pagesQ 1 - P, Then The Probability Distribution of A Binomial Random Variable X, The Number ofKathleen Grace ManiagoNo ratings yet
- Chap2 OutoutlinelineDocument7 pagesChap2 OutoutlinelineKathleen Grace ManiagoNo ratings yet
- Famtree RizalDocument2 pagesFamtree RizalKathleen Grace ManiagoNo ratings yet
- A Part in Everything We Are in Our Heart... "Document2 pagesA Part in Everything We Are in Our Heart... "Kathleen Grace ManiagoNo ratings yet
- Musiiiic UploadsDocument1 pageMusiiiic UploadsKathleen Grace ManiagoNo ratings yet
- Prayer To St. Joseph of CupertinDocument1 pagePrayer To St. Joseph of CupertinKathleen Grace ManiagoNo ratings yet
- PrintDocument1 pagePrintKathleen Grace ManiagoNo ratings yet
- Neonatal Nursing Crash CourseDocument13 pagesNeonatal Nursing Crash CourseOmprakash SainiNo ratings yet
- Vikor Enterprises (PVT) LTD "Karachi"Document2 pagesVikor Enterprises (PVT) LTD "Karachi"aliNo ratings yet
- Prueba de Certificación de Nivel Avanzado de Inglés Cuadernillo de PreguntasDocument3 pagesPrueba de Certificación de Nivel Avanzado de Inglés Cuadernillo de PreguntasJonathan Baricot HernandezNo ratings yet
- Vaccines!!!Document6 pagesVaccines!!!Stephanie OngNo ratings yet
- Narrative Report: Polio Outbreak Response Immunization Bopv Round 2Document4 pagesNarrative Report: Polio Outbreak Response Immunization Bopv Round 2Cristina MelloriaNo ratings yet
- Covid 19 Daily Reporting DasDocument6 pagesCovid 19 Daily Reporting DasRuhayati88gmail.com EyeshieldNo ratings yet
- Using Antimicrobial Foam DressingsDocument1 pageUsing Antimicrobial Foam DressingsRicardo BalauNo ratings yet
- Pediatric Health Maintenance in The 21st Century: A View From The TrenchesDocument6 pagesPediatric Health Maintenance in The 21st Century: A View From The Trenchesmarc_garciabNo ratings yet
- Off-Label Drug Use in Pediatric PatientsDocument7 pagesOff-Label Drug Use in Pediatric PatientsFika Setra RikantaraNo ratings yet
- BHS-Crossing: Individual Treatment RecordDocument2 pagesBHS-Crossing: Individual Treatment Recordjohnmorts2014No ratings yet
- Common Side Effects of Immunization and Their Nursing InterventionsDocument4 pagesCommon Side Effects of Immunization and Their Nursing InterventionsPatricia G ChiuNo ratings yet
- Symphonic 2023Document6 pagesSymphonic 2023Muthya Aulina FahriyanNo ratings yet
- DNB Pediatrics - MCQ DNB Pediatics - December 2015Document7 pagesDNB Pediatrics - MCQ DNB Pediatics - December 2015Manju Manjunath100% (1)
- Covid19 Vaccination Report Personnel LearnerDocument39 pagesCovid19 Vaccination Report Personnel LearnerAnalyn SamillanoNo ratings yet
- Daftar Kedatangan Isolasi Mandiri 25 Desember 2021Document3 pagesDaftar Kedatangan Isolasi Mandiri 25 Desember 2021Tirta BudiawanNo ratings yet
- Communicating The Benefits and Risks of VaccinesDocument8 pagesCommunicating The Benefits and Risks of VaccinesBrandeice BarrettNo ratings yet
- Bora Institute of Allied Health SciencesDocument2 pagesBora Institute of Allied Health Sciencesshubham vermaNo ratings yet
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary DetailsAman SinghNo ratings yet
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary DetailsDipak GuptaNo ratings yet
- Aakash Vaccine CertificateDocument1 pageAakash Vaccine CertificateB 87 VISHWAKARMA AAKASH ACHCHHELALNo ratings yet
- WA 2009 Certificate of ExemptionDocument1 pageWA 2009 Certificate of ExemptionDonnaNo ratings yet
- Flyer PICUNICU 2023Document2 pagesFlyer PICUNICU 2023nurdin aji iskandarNo ratings yet
- Tingkat Stres Ibu Menyusui Dan Pemberian Asi Pada Bulan Pertama Stress Levels of Breastfeeding Mothers and Breast Milk in The First MonthDocument14 pagesTingkat Stres Ibu Menyusui Dan Pemberian Asi Pada Bulan Pertama Stress Levels of Breastfeeding Mothers and Breast Milk in The First MonthNadia Rahima RahmahNo ratings yet
- National Immunization ScheduleDocument3 pagesNational Immunization SchedulescribdscribdtestNo ratings yet
- Vaccination Chart India 2018Document4 pagesVaccination Chart India 2018Dayanand ShettyNo ratings yet
- GHIZAI: Jurnal Gizi Dan KeluargaDocument7 pagesGHIZAI: Jurnal Gizi Dan Keluargaapriyandi akNo ratings yet
- Breastfeeding Benefits for Baby's Brain Development and HealthDocument5 pagesBreastfeeding Benefits for Baby's Brain Development and HealthTaylor SwiftNo ratings yet