Professional Documents
Culture Documents
2.02 Lab - Acid Fast Staining
Uploaded by
Miguel CuevasCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2.02 Lab - Acid Fast Staining
Uploaded by
Miguel CuevasCopyright:
Available Formats
Second Shifting 2014
Microbiology Faculty
ACID FAST STAINING
2.02L
Topic Outline:
I. Overview
A. Brief History
B. Mycolic Acid
C. AFB Smear
D. Acid Fast Organisms
II. Methodology
III. Ziehl-Neelsen Method
IV. Kinyoun Modification of ZN Method
V. Diagnosis of TB Disease
A. Specimen Collection
B. Sputum Collection
C. Specimen Processing
D. Extrapulmonary TB
E. AFB Smear Classification Figure 1. Mycbacterium tuberculosis
Nocardia, Rhodococcus, Legionella
OVERVIEW Isospora, Cryptosporidium
A. BRIEF HISTORY METHODOLOGY
1882: Robert Koch reported discovery of tubercle bacillus and MATERIALS
described appearance of the bacilli resulting from a complex o Sputum smear
staining procedure o Acid fast stain:
1890s: acid fast staining is also known as Ziehl-Neelsen method: Carbol fuchsin
o Frank Ziehl: first to use carbolic acid (phenol) as mordant Acid alcohol
o Friedrich Neelsen: kept Ziehls mordant, but changed the Loefflers methylene blue
primary stain to basic fuchsin (first used by Ehrlich in 1882) o Microscope (OIO)
o Ziehl-Neelsen method uses heat to help primary stain o Alcohol lamp
penetrate the cell wall - hot staining method
1915: Kinyoun published cold staining method PROCEDURE
B. MYCOLIC ACID
Responsible for pathogenicity by inhibiting phagocytosis by
immune cells
With high lipid content; renders the cell wall waxy and
impermeable to gram staining
To view cells in samples, staining requires higher concentrations
of dye solution and/or a heating period
However, once the cell wall is stained with the primary stain,
they resist decolorization with acid alcohol (hence, acid fast)
C. AFB SMEAR
Important role in the early diagnosis of mycobacterial infections
Microscopy: oldest, easiest, most rapid and inexpensive
procedure that can be performed in laboratory to detect
presence of AFB
However, AFB smear should not be used in place of culture
o AF smear requires 105 acid fast bacilli per ml of sputum for
recognition by direct microscopy
o Culture detects as few as 10-100 CFU/ml of sputum
Purpose:
1. Provides presumptive diagnosis of mycobacterial disease
2. Smear positive patients are rapidly identified and are the
most infectious cases
3. It is used to follow the success of chemotherapy of
tuberculous patients
4. It is of vital importance to the patients discharge from the Figure 2. Acid fast Staining Procedure
hospital, or return to gainful employment
5. It can confirm that cultures growing on media are indeed ZIEHL-NEELSEN METHOD
acid-fast Also known as the hot staining method
Heat is applied during the primary stain to increase the stain
D. ACID FAST ORGANISMS penetration and help drive the stain into the mycobacterial cell
Mycobacteria: wall
o Grow at a relatively slow rate Once stained, acid fast organisms resist decolorization with acid
o Gram ghost or gram neutral (fail to take up both primary and alcohol (hydrochloric acid-ethanol)
counterstain on Gram staining)
o Contain mycolic acid in cell wall
Transcribers: Bautista, de Castillo, Gamboa, Wong Page 1 of 2
2.02 Acid Fast Staining
o Coughing
o Induced sputum
o Bronchoscopy
o Gastric aspiration
B. SPUTUM COLLECTION
Coughing: most commonly used method
o Health care worker should wear personal protective
equipment and should coach and directly supervise patient
when sputum is collected
o Patient should be informed that sputum is the material
brought up from the lungs, and that mucus from the nose or
throat and saliva are not good specimens
o Patient should perform deep cough, and then cough up the
Figure 3. Ziehl-Neelsen Method specimen into a sterile container
o Container must be properly sealed, labelled and examined
KINYOUN MODIFICATION OF ZN METHOD immediately
Also known as the cold staining method Specimens with too many squamous epithelial cells and/or few
Kinyoun modification removed the heating step and instead PMNs are not suitable for culture
used a higher concentration of the carbol fuchsin primary stain BARTLETTS CLASSIFICATION:
This method is preferred when the AFB to be examined is in a 1. <10 epithelial cells/LPF (Prioritized criterion; if >10 epithelial
tissue sample cells, saliva was collected, not sputum)
2. >25 PMN/LPF
C. SPECIMEN PROCESSING
At least three (3) consecutive sputum specimens are needed
o Collected in 8- to 24-hour intervals
o At least one (1) being an early morning specimen
If possible, specimens should be obtained in an airborne
infection isolation (AII) room or other isolated, well-ventilated
area (e.g., outdoors)
D. EXTRAPULMONARY TB
TB disease can occur in almost any anatomical site; thus, a
variety of clinical specimens other than sputum may be
Figure 4. Kinyoun Modification of ZN Method submitted for examination:
o Urine
Table 1. Ziehl-Neelsen Hot Method vs. Kinyoun Cold Method o CSF
o Pleural fluid
o Pus
o Biopsy specimens (ex. lung tissue)
E. AB SMEAR CLASSIFICATION
Table 2. AFB Smear Classification Reporting of Results
DIAGNOSIS OF TB
A complete medical evaluation for TB disease includes:
o Medical history
o Physical examination
o Test for M. tuberculosis infection Culture remains the gold standard for laboratory confirmation
o Chest radiograph of TB disease, and growing bacteria are required to perform
o Bacteriologic examination of clinical specimens: drug-susceptibility testing and genotyping
Specimen collection, processing and review Positive cultures for M. tuberculosis confirm the diagnosis of TB
AFB smear classification and results disease; however, in the absence of a positive culture, TB
Direct detection of M. tuberculosis in clinical specimen using disease may also be diagnosed on the basis of clinical signs and
nucleic acid amplification (NAA) symptoms alone
Specimen culturing and identification Culture examinations should be done on all diagnostic
Drug susceptibility and testing specimens, regardless of AFB smear or Nucleic Acid Amplification
(NAA) results
A. SPECIMEN COLLECTION ***
There are four (4) collection methods for pulmonary TB disease:
Transcribers: Bautista, de Castillo, Gamboa, Wong Page 2 of 2
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hedgehog Welfare Society: African Hedgehog Care SheetDocument4 pagesHedgehog Welfare Society: African Hedgehog Care SheetMiguel CuevasNo ratings yet
- Neisseria Chlamydia MycoplasmaDocument6 pagesNeisseria Chlamydia MycoplasmaMiguel CuevasNo ratings yet
- Flavivirus Family and DiseasesDocument6 pagesFlavivirus Family and DiseasesMiguel CuevasNo ratings yet
- 3.9 CoronavirusDocument3 pages3.9 CoronavirusMiguel CuevasNo ratings yet
- Tumors of The Head and NeckDocument5 pagesTumors of The Head and NeckMiguel CuevasNo ratings yet
- RetinaDocument6 pagesRetinaMiguel CuevasNo ratings yet
- Hypertension and Cardiovascular DiseaseDocument99 pagesHypertension and Cardiovascular DiseaseMiguel CuevasNo ratings yet
- Hedgehog Care GuideDocument2 pagesHedgehog Care GuideMiguel CuevasNo ratings yet
- 3 NonVolatile and Local Anes (Bautista)Document11 pages3 NonVolatile and Local Anes (Bautista)Miguel CuevasNo ratings yet
- JURIS - Code of Ethics of The Medical Profession and Its Implementing Guidelines PDFDocument8 pagesJURIS - Code of Ethics of The Medical Profession and Its Implementing Guidelines PDFKate Sarah GabasaNo ratings yet
- CFM Module 2Document11 pagesCFM Module 2Miguel CuevasNo ratings yet
- Muscular Insertion: Medial Rectus 5.5mm Away From Sclera (Nearest) Superior Rectus 8mm Away From Sclera (Farthest)Document7 pagesMuscular Insertion: Medial Rectus 5.5mm Away From Sclera (Nearest) Superior Rectus 8mm Away From Sclera (Farthest)Miguel CuevasNo ratings yet
- Pathophysiology of Gout: German VersionDocument7 pagesPathophysiology of Gout: German VersionMiguel CuevasNo ratings yet
- Surg Diseases of The StomachDocument8 pagesSurg Diseases of The StomachMiguel CuevasNo ratings yet
- Code of Ethics With Irr 2Document53 pagesCode of Ethics With Irr 2Kate Sarah GabasaNo ratings yet
- Obstetric Case HistoryDocument2 pagesObstetric Case HistoryMiguel CuevasNo ratings yet
- 3 AnxietyDocument151 pages3 AnxietyMiguel CuevasNo ratings yet
- EnterobacteriaceaeDocument7 pagesEnterobacteriaceaeMiguel CuevasNo ratings yet
- 2 Thyroid, Parathyroid - BartolomeDocument10 pages2 Thyroid, Parathyroid - BartolomeMiguel CuevasNo ratings yet
- 1 DSM VDocument75 pages1 DSM VMiguel CuevasNo ratings yet
- RA 2382 The Medical Act of 1959Document18 pagesRA 2382 The Medical Act of 1959Simon James SemillaNo ratings yet
- Muscular Insertion: Medial Rectus 5.5mm Away From Sclera (Nearest) Superior Rectus 8mm Away From Sclera (Farthest)Document7 pagesMuscular Insertion: Medial Rectus 5.5mm Away From Sclera (Nearest) Superior Rectus 8mm Away From Sclera (Farthest)Miguel CuevasNo ratings yet
- Muscle & Spinal CordDocument9 pagesMuscle & Spinal CordMiguel CuevasNo ratings yet
- Head & Neck Masses 2013Document46 pagesHead & Neck Masses 2013Miguel CuevasNo ratings yet
- Embryo Excretory SystemDocument6 pagesEmbryo Excretory SystemMiguel CuevasNo ratings yet
- Muscular Insertion: Medial Rectus 5.5mm Away From Sclera (Nearest) Superior Rectus 8mm Away From Sclera (Farthest)Document7 pagesMuscular Insertion: Medial Rectus 5.5mm Away From Sclera (Nearest) Superior Rectus 8mm Away From Sclera (Farthest)Miguel CuevasNo ratings yet
- Development of Placenta - Doc BartolomeDocument4 pagesDevelopment of Placenta - Doc BartolomeMiguel CuevasNo ratings yet
- viral hepatitis (1) 肝炎Document64 pagesviral hepatitis (1) 肝炎Umesh BabuNo ratings yet
- Hepatitis GDocument1 pageHepatitis GMiguel CuevasNo ratings yet
- OSCE SkillsDocument9 pagesOSCE SkillsgoodbyethereNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Manage High-Risk PregnanciesDocument33 pagesManage High-Risk PregnanciesDakshayini MbNo ratings yet
- Cleaning Allergen Polyurethane 1Document128 pagesCleaning Allergen Polyurethane 1Yudhi AdiNo ratings yet
- Bipolar and Related Disorder: Recio, Kate M. Far Eastern University - Cavite PSY1831-ADocument20 pagesBipolar and Related Disorder: Recio, Kate M. Far Eastern University - Cavite PSY1831-AKate RecioNo ratings yet
- Chapter 1-Assessment A. Nursing Health History Demographic DataDocument11 pagesChapter 1-Assessment A. Nursing Health History Demographic DataxxkaceNo ratings yet
- PASSIVE MOVEMENT TECHNIQUESDocument58 pagesPASSIVE MOVEMENT TECHNIQUESabdulahNo ratings yet
- Laporan Diet Pasca BedahDocument13 pagesLaporan Diet Pasca BedahYuliza RosalinaNo ratings yet
- 2018 01 Early Pregnancy Loss LightDocument41 pages2018 01 Early Pregnancy Loss LightMishal FatimaNo ratings yet
- Pharmaceutical Assasination (Partial)Document14 pagesPharmaceutical Assasination (Partial)jamie_clark_2100% (2)
- Cervical Spondylopathy and Menstrual Disorder TreatmentDocument17 pagesCervical Spondylopathy and Menstrual Disorder TreatmentManoel LuizNo ratings yet
- Diasys Katalog 2019 190506 ScreenDocument104 pagesDiasys Katalog 2019 190506 Screendr-abdullah husseinNo ratings yet
- Advances and Challenges in Stroke RehabilitationDocument13 pagesAdvances and Challenges in Stroke Rehabilitationarif 2006No ratings yet
- Fetal Blood Sampling: 1. PurposeDocument7 pagesFetal Blood Sampling: 1. PurposeMuathNo ratings yet
- Peyronies DiseaseDocument6 pagesPeyronies Diseaseapi-255601700No ratings yet
- Study On Emergence of MDR Pathogen and Its Microbiological StudyDocument9 pagesStudy On Emergence of MDR Pathogen and Its Microbiological StudyIJAR JOURNALNo ratings yet
- Case Study 2Document8 pagesCase Study 2api-547174770No ratings yet
- USA V Snap Diagnostics, LLC, Gil Raviv and Stephen Burton (1:15-cv-06204)Document54 pagesUSA V Snap Diagnostics, LLC, Gil Raviv and Stephen Burton (1:15-cv-06204)Jonah Meadows100% (1)
- Talk WslidesDocument43 pagesTalk WslidesraydonalNo ratings yet
- Prospect Frisium in EnglezaDocument4 pagesProspect Frisium in EnglezaTanasa AdrianNo ratings yet
- Diagnostic Accuracy StudiesDocument4 pagesDiagnostic Accuracy StudiesoktarinanurfazrianianjasNo ratings yet
- ThesisDocument5 pagesThesisVictoria ManeboNo ratings yet
- Cyanotic Congenital Heart DiseaseDocument6 pagesCyanotic Congenital Heart DiseaseSimran JosanNo ratings yet
- Njala University: Bo Campus-Kowama LocationDocument32 pagesNjala University: Bo Campus-Kowama LocationALLIEU FB SACCOHNo ratings yet
- Propofol Infusion SyndromeDocument7 pagesPropofol Infusion SyndromewadejackNo ratings yet
- Misoprostol For Treatment of Early Pregnancy LossDocument2 pagesMisoprostol For Treatment of Early Pregnancy LossJuan KipronoNo ratings yet
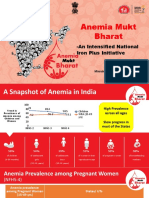
- Anemia Mukt Bharat: - An Intensified National Iron Plus InitiativeDocument23 pagesAnemia Mukt Bharat: - An Intensified National Iron Plus InitiativeAnggun100% (1)
- Physiotherapy of Avian RespiratoryDocument3 pagesPhysiotherapy of Avian RespiratoryMichael MekhaNo ratings yet
- Plant Disease ResistanceDocument35 pagesPlant Disease ResistanceAnuraj DaheriyaNo ratings yet
- Classifications of Pharmaceutical Drugs1Document24 pagesClassifications of Pharmaceutical Drugs1RPh Krishna Chandra JagritNo ratings yet
- Fournier's Gangrene: Yang Lu MS3 AUC School of MedicineDocument15 pagesFournier's Gangrene: Yang Lu MS3 AUC School of MedicineYang JunNo ratings yet
- Adel Elkady Sba PDFDocument290 pagesAdel Elkady Sba PDFAsh Ame100% (2)