Professional Documents
Culture Documents
Who
Uploaded by
Lian Tolombot LambeyCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Who
Uploaded by
Lian Tolombot LambeyCopyright:
Available Formats
Research
Research
Peri-operative pulse oximetry in low-income countries: a cost
effectiveness analysis
SamanthaLBurn,a PeterJChilton,a AtulAGawandeb & RichardJLilfordc
Objective To evaluate the costeffectiveness of pulse oximetry compared with no peri-operative monitoring during surgery in low-
income countries.
Methods We considered the use of tabletop and portable, hand-held pulse oximeters among patients of any age undergoing major surgery
in low-income countries. From earlier studies we obtained baseline mortality and the effectiveness of pulse oximeters to reduce mortality.
We considered the direct costs of purchasing and maintaining pulse oximeters as well as the cost of supplementary oxygen used to treat
hypoxic episodes identified by oximetry. Health benefits were measured in disability-adjusted life-years (DALYs) averted and benefits and
costs were both discounted at 3% per year. We used recommended costeffectiveness thresholds both absolute and relative to gross
domestic product (GDP) per capita to assess if pulse oximetry is a costeffective health intervention. To test the robustness of our results
we performed sensitivity analyses.
Findings In 2013 prices, tabletop and hand-held oximeters were found to have annual costs of 310 and 95 United States dollars (US$),
respectively. Assuming the two types of oximeter have identical effectiveness, a single oximeter used for 22 procedures per week averted
0.83 DALYs per annum. The tabletop and hand-held oximeters cost US$374 and US$115 per DALY averted, respectively. For any country
with a GDP per capita above US$677 the hand-held oximeter was found to be costeffective if it prevented just 1.7% of anaesthetic-related
deaths or 0.3% of peri-operative mortality.
Conclusion Pulse oximetry is a costeffective intervention for low-income settings.
based on a synthesis of data from previously published studies
Introduction from a large number of different countries. While the group of
The pulse oximeter is a non-invasive medical device that moni- low-income countries is heterogeneous, the analysis presented
tors oxygen saturation and pulsation. When used continu- here is readily adaptable to specific national contexts.
ously during surgery, it can provide early warning of hypoxia,
hypovolaemia and impending cardiac arrest. Since oximetry
can warn of problems such as misplaced endotracheal tubes
Methods
which can readily be rectified the World Federation of We investigated the equivalent annual costs of purchasing and
Societies of Anaesthesiologists recommends its routine use maintaining pulse oximeters, as well as the costs of increased
for every patient undergoing anaesthesia in the world.1,2 The oxygen flow used to treat any hypoxic episodes identified by
World Health Organization (WHO) includes pulse oximetry as oximetry. We took a health services perspective. In quantifying
a component of its Surgical Safety Checklist, which is recom- the health benefits of peri-operative oximetry, we considered
mended for use in every operating theatre.1 However, it has the number of disability-adjusted life-years (DALYs) averted
recently been estimated that pulse oximetry is unavailable in by using pulse oximetry to reduce the incidence of fatal intra-
5170% of operating theatres in low-income countries,3 partly operative hypoxic episodes. We ignored non-fatal cases of
because of the high purchase cost of a standard commercial hypoxic brain injury. Base case analysis was conducted using
tabletop pulse oximeter approximately 1000 United States version 3.0.1 of the R software package (R Foundation for
dollars (US$).4 The Lifebox oximetry project, which cur- Statistical Computing, Vienna, Austria) and Microsoft Excel
rently operates alongside the WHO Safe Surgery Saves Lives 2010 (Microsoft, Redmond, USA) and sensitivity analysis us-
initiative, provides a hand-held pulse oximeter for low- and ing the TreeAge Pro 2013 software package (TreeAge Software
middle-income countries that costs US$250.4 However, even Inc., Boston, USA).
this smaller sum is a considerable investment for resource-
Costs
constrained settings. Furthermore, because no evidence of
the costeffectiveness of pulse oximetry for peri-operative We only considered oximeters that met the IEC606011,
monitoring in low-income countries has yet been published, ISO9919:2005 or ISO80601261:2011 international stan-
it is not clear how oximetry should be prioritized among the dards for safety and performance. There are two main types
many costeffective interventions available. 5 In this paper, of stand-alone pulse oximeter designed for peri-operative
we conducted a costeffectiveness analysis of pulse oximetry use: the standard commercial tabletop oximeter and a less
compared with no peri-operative monitoring for patients expensive hand-held device with similar functionality but a
undergoing surgery in low-income countries. This study is more portable and durable design and a rechargeable battery.6
a
School of Health and Population Sciences, University of Birmingham, Edgbaston, Birmingham B15 2TT, England.
b
Ariadne Labs at Brigham and Womens Hospital and the Harvard School of Public Health, Boston, United States of America.
c
Warwick Medical School, University of Warwick, Coventry, England.
Correspondence to Samantha L Burn (email: samantha.burn@new.oxon.org).
(Submitted: 12 February 2014 Revised version received: 13 July 2014 Accepted: 20 July 2014 Published online: 24 September 2014)
858 Bull World Health Organ 2014;92:858867 | doi: http://dx.doi.org/10.2471/BLT.14.137315
Research
SamanthaL Burn et al. Costeffectiveness of pulse oximetry
could also provide an early warning
Box1. Search strategy for key parameters published in systematic reviews
of a deterioration in the patients un-
Baseline anaesthetic-related mortality derlying condition that was unrelated
1. Surgery[Mesh] OR surg* OR operat* OR perioperat* OR peri-operat* OR intraoperat* OR to anaesthesia. Also, as oximetry may
intra-operat* OR in theatre have been used in one or more of the
2. Anesthesia[Mesh] OR anesth* OR anaesth* OR peri-anesth* OR perianesth* OR post-anesth* studies investigated by Bainbridge et al.,
OR post-anaesth* 467 deaths per million procedures may
3. Death OR mortalit* OR morbidit* OR survival* represent an underestimate of mortality
4. (#1 OR #2) AND #3 in the absence of oximetry.
Effectiveness of pulse oximetry in reducing hypoxic episodes and/or peri-operative mortality For robustness, we replicated the
1. Surgery[Mesh] OR surg* OR operat* OR perioperat* OR peri-operat* OR intraoperat* OR search procedure used by Bainbridge
intra-operat* OR in theatre et al.14 to identify any recent studies of
2. Oximet* OR oxymet* relevance that had been published on
3. Death OR mortalit* OR morbidit* OR survival* or before 30 December 2012. We found
no new studies relating to low-income
4. Anoxia[Mesh] OR anox* OR hypox*
countries. We also examined the six
5. (#1 AND #2) AND (#3 OR #4)
studies that were excluded by Bainbridge
et al. because of small sample size16,17 or
The oximeter distributed by the Lifebox lated and total peri-operative mortal- because they pertained exclusively to
charity is of the second type. ity including studies from low-income one clinical area.1821 Two of these stud-
Costs are given in 2013 prices countries published between 1Janu- ies contained estimates of anaesthetic-
and discounted at 3% per year as ary 1990 and 31December 2012. The related avoidable mortality for a general
recommended in version two of the search terms used included variants of population, which were 1985 and 7500
Disease Control Priorities in Developing anaesthetic, surgery, operation, intra- deaths per million procedures. In our
Countries5 and the WHO-CHOICE7,8 operative, peri-operative, peri-surgical, sensitivity analysis, we therefore con-
guidelines for evaluation of the costef- death, mortality and survival (Box1). sidered values of anaesthetic-related
fectiveness of health interventions in We searched the following databases: avoidable mortality that varied from 253
developing countries. Domestic taxes MEDLINE via OvidSP, EMBASE via deaths per million procedures i.e. the
were excluded. We assumed that no OvidSP, Scopus, the Cochrane Database lowest estimate from the studies inves-
extra operations would be carried out of Systematic Reviews, the Database tigated by Bainbridge et al.14 to 7500
as a result of introducing oximetry and of Abstracts of Reviews of Effects, the deaths per million procedures.
that no extra clinical staff time would be Health Technology Assessment Data-
Effectiveness in reducing mortality
required. We included supplementary base and the International Prospective
oxygen9 resulting from an increase in the Register of Systematic Reviews. We The available data on the effectiveness
incidence of detected hypoxia10 when used the Centre for Reviews and Dis- of pulse oximetry come from obser-
oximetry is used. semination filter (strategy2.1) to iden- vational studies e.g. before-and-after
tify systematic reviews.13 No language studies or critical incident reports and
Health benefits
restrictions were applied. randomized controlled trials. In this
Most of the published data on the per- Two systematic reviews of anaes- context, such studies and trials are im-
formance of oximeters relate to tabletop thetic-related and total peri-operative perfect. Since peri-operative deaths are
oximeters. However, the low-cost hand- mortality that included studies from extremely rare, none of the relevant ran-
held oximeter distributed by Lifebox has low-income countries were identi- domized controlled trials is adequately
recently been found to perform as well as fied.14,15 Since it was the more recent of powered to detect the effects of oximetry
tabletop oximeters that have been pro- the two reviews and included a formal on the probability of such deaths.10,22 The
duced by major manufacturers, made meta-analysis, we used the study by relevant observational studies do not al-
commercially available in the United Bainbridge et al.14 to parameterize our low causeeffect statements to be made
States of America.11 For our analysis, we costeffectiveness estimates. This study with confidence since such studies are
therefore assumed that the effectiveness found that total peri-operative mortality confounded by temporal changes that
of the hand-held devices in averting in low-income countries i.e. countries are unrelated to oximetry.23,24
peri-operative death was identical to with a human development index be- We did a systematic search to iden-
that of the tabletop devices. low 0.8 was 2445 deaths per million tify systematic reviews of the effective-
Lifebox has found that the oxim- procedures.14 They also found that, in ness of oximetry in preventing hypoxia
eters it distributes can be used for 2530 low-income countries, problems in the and peri-operative death published be-
surgeries per week.12 For our analysis, we administration of anaesthesia e.g. tween 1January 1990 and 31December
assumed that each of the oximeters we oesophageal intubation or kinking of 2012 (Box1). We searched the same set
investigated was used at about 80% of the endotracheal tube were the sole of databases as for baseline anaesthetic-
these frequencies8 i.e. in 22 procedures or contributing cause of 467 deaths per related mortality. We identified one sys-
per week. million procedures. We took 467 deaths tematic review of randomized controlled
per million procedures as our baseline trials of the effectiveness of pulse oxim-
Baseline mortality
for deaths that were potentially prevent- etry, in which the authors concluded that
We did a systematic search to identify able by oximetry. However, this may be pulse oximetry reduces the incidence
systematic reviews of anaesthetic-re- a conservative estimate, since oximetry of hypoxaemia by 3367% but appears
Bull World Health Organ 2014;92:858867| doi: http://dx.doi.org/10.2471/BLT.14.137315 859
Research
Costeffectiveness of pulse oximetry SamanthaL Burn et al.
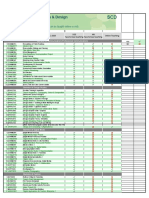
Table 1. Costs of purchasing, maintaining and repairing pulse oximeters
Parameter Point estimate (range)a Data source(s) and assumptionsa
Commercial tabletop Hand-held device
device
Cost of purchase, shipping 1065 (6003000) 250 (250280) Lifebox product information4
and internal transport, US$
Life-span, years 6 (48) 8 (610) Expert opinion
Annuitized maintenance 34 (1785) 18 (1531) Probes for tabletop device replaced every 2 (13) years at
costs, including those for a cost of US$100.40,c Probes for hand-held device replaced
replacement probes and every 2 (13) years at a cost of US$254 and batteries for
batteries, US$b hand-held device replaced every year at a cost of US$104
Annuitized repair costs, US$ 45 (3060) 6 (213) 15% (1020%) chance of breakage of a tabletop device each
year, at a total cost per year of US$355 including shipping.40,c
5% (110%) chance of breakage of hand-held device
each year, at a total cost per year of US$65 during the first
2years when the device is under warranty and US$138
thereafter4
Annual cost of treating 35 (1752) 35 (1752) Incidence of hypoxia is 7.9% with pulse oximetry and
additional hypoxic episodes 0.4% without oximetry.10 If hypoxia is detected, oxygen
identified by pulse flow increased by 8 litres/min for 10 minutes,c at a cost of
oximetry, US$ US$0.40 per additional hypoxic episode detected9
Total equivalent annual 310 95 Authors calculations. Uncertainty explored in sensitivity
cost, US$ analysis
US$: United States dollars.
a
All costs are shown adjusted to 2013 values, assuming 3% inflation per year.
b
Excludes share of general overhead costs attributable to use of pulse oximetry i.e. costs of cleaning and electricity.
c
Value partly or entirely based on expert opinion.
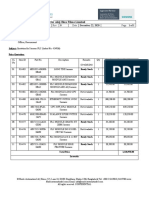
Table 2. Effectiveness and costeffectiveness of pulse oximeters
Parameter Point estimate (range) Data source(s) and assumption
Commercial tabletop Hand-held device
device
Baseline anaesthetic- 467 (2537500) 467 (2537500) Systematic review of anaesthetic-related mortality14
related mortality, deaths
per million operations
requiring general
anaesthesia
Anaesthetic-related deaths 10 (350) 10 (350) Authors estimates based on intermediate outcomes
averted by oximetry, % from systematic review of randomized control trials22 and
observational data14,28,29
Discounted DALYs per 15.5 (1030) 15.5 (1030) Authors calculation based on approximation of age
death avoideda distribution of patients undergoing surgery36 and health-
adjusted life expectancy by age35
Number of times each 22 (2030) 22 (2030) Assumed 80% utilization8 of maximum capacity of 2530
oximeter used per week operations per week12
Discounted DALYs averted 0.83 0.83 Authors calculation
per year of oximeter use
Equivalent annual cost of 310 95 See Table1
oximeter, US$b
Cost per DALY averted, 374 115 Authors calculation
US$c
DALY: disability-adjusted life-year; US$: United States dollars. b
From Table1, in 2013 values.
a
Based on region-specific life-tables. c
In 2013 values.
to have no statistically significant effect attributable decline in hypoxaemia to standards, including pulse oximetry,
on mortality.22 To check the robustness that observed in the included studies. have been widely implemented.14,28,29
of this result, we reviewed the studies Other observational data indicate that While much of the evidence assem-
that were excluded because they were anaesthetic-related mortality in high- bled relates to high-income countries,
not randomized.22 These excluded stud- income countries has declined by 64% the results of a before-and-after study
ies2527 that indicated a similar oximetry- since the 1980s, as various monitoring conducted in the Republic of Moldova
860 Bull World Health Organ 2014;92:858867| doi: http://dx.doi.org/10.2471/BLT.14.137315
Research
SamanthaL Burn et al. Costeffectiveness of pulse oximetry
indicated that the introduction of pulse of pulse oximetry were too small to alter respectively. 7 For the group of low-
oximetry along with the entire WHO overall national life expectancies. income countries as a whole, US$677
Surgical Safety Checklist reduced and US$2031 are one and three times
Costeffectiveness thresholds
the number of hypoxaemic episodes the 2013 GDP per capita, respectively.39
lasting at least twominutes by 44%.30 We used two common types of costef-
Another before-and-after study found fectiveness thresholds for health inter-
that introduction of the checklist led to ventions in low-income countries:37 the
Results
a 60% reduction in total peri-operative absolute thresholds used by the World Our cost and costeffectiveness esti-
mortality over four study sites in low- Bank in the World development report mates are summarized in Table1 and
income countries.31 However, the check- 1993 38 and the thresholds defined Table2, respectively. In the base case
list contains several other items known relative to the corresponding gross do- comparing each type of oximeter
to be associated with improved safety mestic product (GDP) per capita used with no monitoring of oxygen satura-
outcomes, so these reductions are prob- by WHO-CHOICE.7 According to the tion and assuming both the tabletop
ably not attributable to oximetry alone. World development report 1993, inter- and hand-held pulse oximeters reduce
We selected 50% as the upper plau- ventions that, in 1993, cost no more than anaesthetic-related mortality by 10%
sible limit for effectiveness of oximetry US$25 and US$150 per DALY averted the costs per DALY averted were
in reducing anaesthetic-related deaths, could be considered highly attractive US$374 for the tabletop pulse oximeter
since this is the figure obtained us- and attractive, respectively. Assuming and US$115 for the hand-held oximeter.
ing the surrogate outcome of hypoxic 3% inflation per year, the corresponding Since we assume in this analysis that the
episodes in the randomized control thresholds for the year 2013 would be effectiveness of the two types of oximeter
trials described above.10,22 This a highly US$45 and US$271. WHO-CHOICE is identical and the hand-held oximeter
optimistic value, since surrogate out- considered interventions that, per DALY is less costly, the hand-held oximeter
comes are notorious for overestimating averted, cost no more than one and three dominates the tabletop oximeter. The
clinical benefit.3234 We therefore used times the relevant GDP per capita to be costeffectiveness of the hand-held
50% as an upper bound for effective- very costeffective and costeffective, oximeter fell below the very costeffec-
ness. For a lower bound we selected a
2% improvement in anaesthetic-related
mortality, to represent a very pessimistic Fig. 1. Costeffectiveness of pulse oximetry as a function of the proportion of
estimate given the randomized control anaesthetic-related deaths averted
trials and observational evidence cited
above. For the base case we used effec-
tiveness of 10%, founded on the nature
50 000
of the available evidence and based on
Upper bound
Lower bound
Base case
discussion with our advisors. Since there
is considerable uncertainty surrounding 20 000
these values, we conducted extensive
10 000
sensitivity analysis.
Disability-adjusted life-years averted 5 000
Cost per DALY averted (US$)
Health benefits were measured in Threshold for costeffective intervention
2 000
DALYs averted, with uniform age-
weighting and discounting at 3% per 1 000
Threshold for very costeffective intervention
annum. DALYs were calculated using
actual life expectancy rather than life 500
expectancy for a hypothetical reference Threshold for attractive intervention
group.5 Using pooled health-adjusted 200
life expectancy tables for the Eastern
Sub-Sahara Global Burden of Disease re- 100
gion35 and a probability density function Threshold for highly attractive intervention
50
of the ages of patients undergoing major
surgery in Mozambique, Uganda and
the United Republic of Tanzania,36 we 20
calculated that 15.5 DALYs are averted 0 10 20 30 40 50 60
per anaesthetic-related death avoided. % of anaesthetic-related deaths averted by pulse oximetry
We assumed that the sex distribu-
tion of patients was the same as that of DALY: disability-adjusted life-year; GDP: gross domestic product; US$: United States dollars.
the relevant national population. We Note: The costeffective thresholds were for the year 2013. Attractive interventions were based on the
World development report 1993.38 Costeffective interventions were based on World Health Organization
also assumed that, in all cases of averted guidelines, with very costeffective and costeffective interventions below one (US$677) and three
death, a patients health-adjusted life ex- (US$2031) times the GDP per capita for the group of low-income countries, respectively7,39
pectancy did not differ from that of the The base case, lower bound and upper bound are our own estimates of the proportions of anaesthetic-
general population and that the benefits related deaths that could be averted by the routine use of pulse oximetry.
Bull World Health Organ 2014;92:858867| doi: http://dx.doi.org/10.2471/BLT.14.137315 861
Research
Costeffectiveness of pulse oximetry SamanthaL Burn et al.
tive threshold of one times the GDP per low baseline mortality and effectiveness. cate that pulse oximetry is costeffec-
capita for low-income countries. The corresponding costeffectiveness tive. Obtaining parameter estimates for
The purchase of a hand-held ox- acceptability curve (Fig.3) indicates that a decision model is often difficult. In
imeter for each of the 77000 operating hand-held pulse oximeters are likely to this case, the problem was compounded
theatres globally that currently do not be considered costeffective compared by a paucity of evidence relating to use
have pulse oximeters3 would cost about with no oximetry with all but the most of oximetry in low-income settings and
US$19.3 million. Using the parameters stringent costeffectiveness threshold. the very low frequency of the outcome
in this paper, we estimate that equipping Pulse oximetry fell under the WHO of interest. To estimate the effectiveness
all of these operating theatres with pulse very costeffective threshold in 83% of of oximetry in averting peri-operative
oximeters would reduce the global bur- the simulations and under the attractive death, it was necessary to extrapolate
den of disease by 63800 DALYs per year. costeffectiveness threshold from the from surrogate outcomes and from
World development report 1993 in 62% observational studies in high income
Sensitivity analyses
of the simulations. The results of the countries. Another possibility would
Given the paucity of trial data and the probabilistic sensitivity analysis should have been to estimate this parameter
uncertainty surrounding the effective- be interpreted with caution because of by means of a Bayesian elicitation, but
ness of pulse oximetry in averting an- our uncertainty about the relationship the estimate would still have been an
aesthetic-related mortality, we explored between identified hypoxic episodes informed guess. Our approach instead
the sensitivity of our results to variation and mortality. was to carry out extensive sensitivity
in the key parameters. analysis. In our base case, the hand-
Fig.1 shows the cost per DALY held pulse oximeter appeared to be
averted as a function of the percentage
Discussion very costeffective for low-income
of anaesthetic-related mortality pre- Although this study is not entirely countries if it prevented just 1.7% of
vented by pulse oximetry. The hand-held based on hard evidence from random- anaesthetic-related deaths or 0.3% of
pulse oximeter falls below the attractive ized controlled trials, our results indi- total peri-operative deaths. It is worth
threshold for 2013 from the World de-
velopment report 1993, if it prevents 4%
Fig. 2. Costeffectiveness of pulse oximetry as a function of baseline anaesthetic-
of anaesthetic-related mortality. It falls related mortality
below the GDP per capita of the group
of low-income countries if it prevents
1.7% of anaesthetic-related mortality
Lower bound
Base case
Upper bound
(0.3% of total peri-operative mortal-
ity). The wide variation seen in levels 10 000
of anaesthetic-related and total peri-
operative mortality between settings 5 000
has an impact on the costeffectiveness Threshold for costeffective intervention
of pulse oximetry.14,16,17,41 Fig.2 shows
the cost of a hand-held pulse oximeter,
per DALY averted, as a function of 1 000
Cost per DALY averted (US$)
Threshold for very costeffective intervention
baseline anaesthetic-related mortality, 500
assuming that pulse oximetry prevents Threshold for attractive intervention
10% of anaesthetic-related deaths. With
baseline anaesthetic-related mortalities
of 25341 and 750017 deaths per million 100
operations requiring general anaesthe-
sia, a hand-held pulse oximeter would 50 Threshold for highly attractive intervention
have cost US$211 and US$7 per DALY
averted, respectively.
We conducted a basic probabilis-
tic sensitivity analysis by carrying out 10
1000 iterations using the parameter
distributions given in Table3. The ef- 0
fectiveness of oximetry in averting 2 000 4 000 6 000 8 000
death was assumed to be independent Baseline anaesthetic-related mortality
of baseline anaesthetic-related mortal- (deaths per million operations requiring general anaesthesia)
ity. Although the median incremental DALY: disability-adjusted life-year; GDP: gross domestic product; US$: United States dollars.
costeffectiveness was US$154 per Note: The costeffective thresholds were for the year 2013. Attractive interventions were based on the
DALY averted, the corresponding mean World development report 1993.38 Costeffective interventions were based on World Health Organization
costeffectiveness was much higher guidelines, with very costeffective and costeffective interventions below one (US$677) and three
(US$2031) times the GDP per capita for the group of low-income countries, respectively7,39
US$628 largely because of the small The base case,14 lower bound14 and upper bound17 report levels of the baseline anaesthetic-related
number of simulations with extremely mortality that occurs or might occur in the absence of pulse oximetry.
862 Bull World Health Organ 2014;92:858867| doi: http://dx.doi.org/10.2471/BLT.14.137315
Research
SamanthaL Burn et al. Costeffectiveness of pulse oximetry
Table 3. Parameters included in probabilistic sensitivity analysis
Parameter Point Distribution Distributional Data source(s)
estimate parameters
Anaesthetic-related mortality, deaths 467 Lognormal =6.0; =0.56 Systematic review, with variance
per million operations requiring increased to take into account higher
general anaesthesia mortality for excluded studies14
Proportion of anaesthetic-related 0.1 Beta =1; =9 Authors estimates based on
deaths averted by pulse oximetry intermediate outcomes from review
of randomized control trials22 and
observational data14,28,29
Annual equivalent cost of purchasing 83 Lognormal =4.4; =0.81 Authors calculation
and maintaining a hand-held pulse
oximeter, US$ per 1000 operations
requiring general anaesthesia
US$: United States dollars.
cess to oximetry may be willing to use
Fig. 3. Costeffectiveness acceptability curve for pulse oximetry
alternatives to general anaesthesia that
may be safer in some situations e.g.
100 spinal blocks in obstetrics. Third, there
Iterations in which pulse oximetry appears costeffective (%)
attractive intervention
is a role for oximetry outside the operat-
Threshold for highly
90 Threshold for costeffective
ing theatre e.g. in monitoring patients
80 in the recovery room and mothers and
costeffective intervention
neonates during vaginal delivery, and
70 reducing oxygen use in patients with
pneumonia who are tachypnoeic but
Threshold for very
60
intervention
well saturated.42,43
Threshold for attractive
Our analysis considered only
50
stand-alone tabletop and hand-held
40 oximeters. A third type of oximeter, the
intervention
fingertip oximeter, is even cheaper than
30 the hand-held devices with a purchase
cost of US$3044 but is designed only
20
for spot-checks in primary care and
10 probably has limited usefulness in op-
erating theatres, since it lacks an audible
0 tone that changes with oxygen satura-
500 1 000 1 500 2 000 2 500 tion, an alarm to indicate desaturation
Costeffectiveness threshold (US$ per DALY averted) and a plethysmograph display. As well
DALY: disability-adjusted life-year; GDP: gross domestic product; US$: United States dollars. as stand-alone pulse oximeters, pulse
Note: The costeffective thresholds were for the year 2013. Attractive interventions were based on the oximetry may be built into other devices
World development report 1993.38 Costeffective interventions were based on World Health Organization e.g. anaesthesia machines or sphyg-
guidelines, with very costeffective and costeffective interventions below one (US$677) and three
(US$2031) times the GDP per capita for the group of low-income countries, respectively7,39
momanometers or combined with
electrocardiography or capnography in
a multivariable monitor.45 In practice
noting that to detect an improvement of In this paper, we only considered the choice of which type of oximeter to
this magnitude in total peri-operative deaths averted by oximetry. Our esti- purchase is likely to depend on a variety
mortality in a randomized controlled mates of the costeffectiveness of pulse of setting-specific considerations. For
trial would require a sample size of oximetry would probably have increased example, in a setting with only inter-
almost 1.5 billion patients and such a if we had also considered non-fatal mittent electricity supply, a standard
trial will never be conducted. The aim brain damage. Discussions with doc- tabletop oximeter would be unsuitable
of the WHO Global Pulse Oximetry tors working in low-income countries because of its inability to function for
Project is to make pulse oximetry more highlighted several additional points. long periods without mains electricity.
widely available is based on best prac- First, pulse oximetry may actually The presence of combined capnography
tice from high-income countries and reduce overall oxygen use, since flow or other functionality in an expensive
the results of informal analysis1 rather rate can be reduced where saturation unit that can be used for oximetry is
than on an explicit calculation of what is adequate. Second, the availability of only valuable if the requisite expertise
oximetry would have to achieve to be oximetry may change clinical practice. is present.46
costeffective. For example, only practitioners with ac-
Bull World Health Organ 2014;92:858867| doi: http://dx.doi.org/10.2471/BLT.14.137315 863
Research
Costeffectiveness of pulse oximetry SamanthaL Burn et al.
There is a large body of literature fectiveness of health interventions and neering and Physical Sciences Research
relating to costeffectiveness of health the literature on technical specifications Council Multidisciplinary Assessment
interventions in low-income coun- for devices, allowing decision-makers of Technology Centre for Healthcare
tries.5,7 Much of this literature relates to to proceed beyond the prioritization of programme (grant GR/S29874/01). The
evaluations of complex interventions complex interventions to the selection National Institute for Health Research
that are of little value in specific device- of specific devices for different clinical (NIHR) Collaborations for Leadership
procurement decisions. There is also an settings.46 in Applied Health Research and Care
emerging interest in frugal innovation for Birmingham and the Black Coun-
i.e. the adaptation of existing medi- Acknowledgements try, and the NIHR Senior Investigator
cal technologies to make them more We thank Iain Wilson, Alan Merry, Award granted to RJL also contributed
affordable and more suitable for use in Tracy Roberts, Amanda Chapman, resources.
low-resource settings.6,40,47 We hope that Karin, Jane Kabutu Gatumbu, Isabeau
analysis of the type presented here in Walker, John Crowe, Philippa Lilford, Competing interests: AAG is the Chair of
which the types and grades of device Jonathan Pon and Derek Barrett. the Lifebox Foundation Board. The other
available for a particular purpose are authors declare no competing interests.
made explicit could help bridge the Funding: This study was supported pri-
gap between the literature on costef- marily by the United Kingdoms Engi-
:
- .
- 2013
.
. 95 310
0.83 22
. .
. 115 374
.
. 677
%1.7
%3 %0.3
- . .
-
. .
:
2013 ,
310 95
, 22
, 0.83 DALY
DALY 374 115
, 677
, 1.7%
0.3%
(DALY) , ,
3% (
(GDP) )
864 Bull World Health Organ 2014;92:858867| doi: http://dx.doi.org/10.2471/BLT.14.137315
Research
SamanthaL Burn et al. Costeffectiveness of pulse oximetry
Rsum
Oxymtrie de pouls priopratoire dans les pays revenu faible: une analyse de la rentabilit
Objectif valuer la rentabilit de loxymtrie de pouls par rapport brut (PIB) par habitant afin dvaluer si loxymtrie de pouls tait une
labsence de surveillance priopratoire lors dune chirurgie dans les intervention de sant rentable. Pour tester la solidit de nos rsultats,
pays revenu faible. nous avons effectu des analyses de sensibilit.
Mthodes Nous avons considr lutilisation doxymtres de pouls Rsultats Avec les prix de 2013, les oxymtres poser et les oxymtres
poser et doxymtres de pouls portatifs chez des patients de tous ges portatifs prsentaient des cots annuels de 310et 95dollars,
ayant subi une opration chirurgicale importante dans des pays revenu respectivement. En supposant que les deux types doxymtre ont une
faible. partir dtudes antrieures, nous avons obtenu la mortalit de efficacit identique, un seul oxymtre utilis pour 22interventions par
rfrence et lefficacit des oxymtres de pouls pour rduire la mortalit. semaine permettait dviter 0,83EVCI par an. Les oxymtres poser
Nous avons considr les cots directs de lachat et de lentretien des et les oxymtres portatifs cotaient 374$ et 115$ par EVCI vite,
oxymtres de pouls, ainsi que le cot de loxygne supplmentaire respectivement. Pour tous les pays avec un PIB par habitant suprieur
utilis pour traiter les pisodes hypoxiques identifis par oxymtrie. Les 677$, loxymtre portatif sest avr rentable sil vitait seulement
avantages pour la sant ont t mesurs en esprance de vie corrige de 1,7% des dcs lis lanesthsie ou 0,3% de mortalit priopratoire.
lincapacit (EVCI) vite, et les avantages et les cots ont t actualiss Conclusion Loxymtrie de pouls est une intervention rentable pour
3% par an. Nous avons utilis les seuils de rentabilit recommands les pays faible revenu.
la fois de manire absolue et relative par rapport au produit intrieur
()
,
.
. , .
, , 2013
, , 310 95 .
. ,
, , 22
. , 0,83 DALY .
DALY 374 115
, .
, , 677
. ,
, 1,7% 0,3%
( DALY), .
3% .
- .
, ,
Resumen
La oximetra de pulso perioperatoria en los pases de ingresos bajos: un anlisis de la rentabilidad
Objetivo Evaluar la rentabilidad de la oximetra de pulso en comparacin interno bruto (PIB) per cpita para evaluar si la oximetra de pulso es
con la ausencia de vigilancia perioperatoria durante la ciruga en pases una intervencin de salud rentable. Por ltimo, se realiz un anlisis de
de ingresos bajos. sensibilidad para poner a prueba la solidez de los resultados.
Mtodos Se tuvieron en cuenta oxmetros de pulso manuales, tanto de Resultados En 2013, se hall que los precios de los oxmetros de
mesa como porttiles, entre los pacientes de todas las edades sometidos mesa y porttiles suponan unos costes anuales de 310 y 95 dlares
a una intervencin quirrgica importante en pases de ingresos bajos. estadounidenses (US$), respectivamente. En el supuesto de que
A partir de los estudios anteriores se obtuvo la mortalidad inicial y ambos tipos de oxmetro tengan la misma eficacia, el uso de un nico
la eficacia de los oxmetros de pulso para reducir la mortalidad. Se oxmetro para 22 procedimientos por semana evit 0,83 AVAD por
consideraron los costes directos de la adquisicin y del mantenimiento ao. Los oxmetros de mesa y manuales cuestan 374 US$ y 115 US$
de los oxmetros de pulso, as como el coste del oxgeno complementario por AVAD evitado, respectivamente. Para cualquier pas con un PIB per
que se utiliza para tratar los episodios de hipoxia identificados mediante cpita superior a 677 US$ el oxmetro manual result ser rentable con
la oximetra. Se midieron los beneficios para la salud en aos de vida con tan solo impedir un 1,7% de las muertes relacionadas con la anestesia
discapacidad (AVAD) evitados, mientras que los beneficios y los costes o el 0,3% de la mortalidad perioperatoria.
se descontaron al 3% por ao. Utilizamos los umbrales de rentabilidad Conclusin La oximetra de pulso es una intervencin rentable para
recomendados, tanto absolutos como relativos, respecto al producto entornos de ingresos bajos.
Bull World Health Organ 2014;92:858867| doi: http://dx.doi.org/10.2471/BLT.14.137315 865
Research
Costeffectiveness of pulse oximetry SamanthaL Burn et al.
References
1. Merry AF, Eichhorn JH, Wilson IH. Extending the WHO Safe Surgery Saves 21. Zoumenou E, Gbenou S, Assouto P, Ouro Bangna Maman AF, Lokossou
Lives project through global oximetry. Anaesthesia. 2009;64(10):10458. T, Hounnou G, et al. Pediatric anesthesia in developing countries:
doi: http://dx.doi.org/10.1111/j.1365-2044.2009.06104.x PMID: 19735392 experience in the two main university hospitals of Benin in West Africa.
2. Enright A, Merry A. The WFSA and patient safety in the perioperative setting. Paediatr Anaesth. 2010;20(8):7417. doi: http://dx.doi.org/10.1111/j.1460-
Can J Anaesth. 2009;56(1):813. doi: http://dx.doi.org/10.1007/s12630-008- 9592.2010.03348.x PMID: 20670238
9001-x PMID: 19247772 22. Pedersen T, Nicholson A, Hovhannisyan K, Mller AM, Smith AF, Lewis SR.
3. Funk LM, Weiser TG, Berry WR, Lipsitz SR, Merry AF, Enright AC, et al. Global Pulse oximetry for perioperative monitoring. Cochrane Database Syst Rev.
operating theatre distribution and pulse oximetry supply: an estimation 2014;3:CD002013. PMID: 24638894
from reported data. Lancet. 2010;376(9746):105561. doi: http://dx.doi. 23. Sacks H, Chalmers TC, Smith H Jr. Randomized versus historical controls
org/10.1016/S0140-6736(10)60392-3 PMID: 20598365 for clinical trials. Am J Med. 1982;72(2):23340. doi: http://dx.doi.
4. Our product. Lifebox: saving lives through safer surgery [Internet]. London: org/10.1016/0002-9343(82)90815-4 PMID: 7058834
Lifebox Foundation; 2013. Available from: http://www.lifebox.org/about- 24. Kunz R, Oxman AD. The unpredictability paradox: review of empirical
lifebox/our-product/ [cited 2013 Jul 17]. comparisons of randomised and non-randomised clinical trials. BMJ.
5. Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, et al. 1998;317(7167):118590. doi: http://dx.doi.org/10.1136/bmj.317.7167.1185
Disease control priorities in developing countries. Washington: World Bank; 2006. PMID: 9794851
6. Pulse oximeter: technology opportunity assessment. Seattle: Program for 25. Mateer JR, Olson DW, Stueven HA, Aufderheide TP. Continuous pulse
Appropriate Technology in Health; 2013. Available from: http://sites.path. oximetry during emergency endotracheal intubation. Ann Emerg Med.
org/mnhtech/files/2013/06/Proofed-Pulse-oximeter_FINAL_27June2013. 1993;22(4):6759. doi: http://dx.doi.org/10.1016/S0196-0644(05)81846-3
pdf [cited 2014 Aug 18]. PMID: 8457094
7. Edejer TT-T, Baltussen R, Adam T, Hutubessy R, Acharya A, Evans DB, et al. 26. Cot CJ, Goldstein EA, Cot MA, Hoaglin DC, Ryan JF. A single-blind study
Making choices in health: WHO guide to cost effectiveness analysis. Geneva: of pulse oximetry in children. Anesthesiology. 1988;68(2):1848. doi: http://
World Health Organization; 2003. dx.doi.org/10.1097/00000542-198802000-00002 PMID: 3277484
8. Hutubessy R, Chisholm D, Edejer TT-T. Generalized costeffectiveness 27. Cot CJ, Rolf N, Liu LMP, Goudsouzian NG, Ryan JF, Zaslavsky A, et al. A
analysis for national-level priority-setting in the health sector. Cost Eff single-blind study of combined pulse oximetry and capnography in
Resour Alloc. 2003;1(1):8. doi: http://dx.doi.org/10.1186/1478-7547-1-8 children. Anesthesiology. 1991;74(6):9807. PMID 1904206.
PMID: 14687420 28. Gibbs N, Rodoreda P. Anaesthetic mortality rates in Western Australia
9. Howie SR, Hill S, Ebonyi A, Krishnan G, Njie O, Sanneh M, et al. Meeting 19802002. Anaesth Intensive Care. 2005;33(5):61622. PMID: 16235480
oxygen needs in Africa: an options analysis from the Gambia. Bull World 29. Eichhorn JH. Prevention of intraoperative anesthesia accidents and related
Health Organ. 2009;87(10):76371. doi: http://dx.doi.org/10.2471/ severe injury through safety monitoring. Anesthesiology. 1989;70(4):5727.
BLT.08.058370 PMID: 19876543 doi: http://dx.doi.org/10.1097/00000542-198904000-00002 PMID: 2929993
10. Moller JT, Johannessen NW, Espersen K, Ravlo O, Pedersen BD, Jensen 30. Kwok AC, Funk LM, Baltaga R, Lipsitz SR, Merry AF, Dziekan G, et al.
PF, et al. Randomized evaluation of pulse oximetry in 20,802 patients: II. Implementation of the World Health Organization surgical safety
Perioperative events and postoperative complications. Anesthesiology. checklist, including introduction of pulse oximetry, in a resource-limited
1993;78(3):44553. doi: http://dx.doi.org/10.1097/00000542-199303000- setting. Ann Surg. 2013;257(4):6339. doi: http://dx.doi.org/10.1097/
00007 PMID: 8457045 SLA.0b013e3182777fa4 PMID: 23207242
11. Dubowitz G, Breyer K, Lipnick M, Sall JW, Feiner J, Ikeda K, et al. Accuracy 31. Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP, et
of the Lifebox pulse oximeter during hypoxia in healthy volunteers. al.; Safe Surgery Saves Lives Study Group. A surgical safety checklist to
Anaesthesia. 2013;68(12):12203. doi: http://dx.doi.org/10.1111/ reduce morbidity and mortality in a global population. N Engl J Med.
anae.12382 PMID: 23992483 2009;360(5):4919. doi: http://dx.doi.org/10.1056/NEJMsa0810119 PMID:
12. Lifebox annual review. London: Lifebox Foundation; 2011. Available from: 19144931
http://www.lifebox.org/wp-content/uploads/Lifebox-annual-review-2011. 32. Ciani O, Buyse M, Garside R, Pavey T, Stein K, Sterne JA, et al. Comparison of
pdf [cited 2014 July 25]. treatment effect sizes associated with surrogate and final patient relevant
13. Lee E, Dobbins M, Decorby K, McRae L, Tirilis D, Husson H. An optimal outcomes in randomised controlled trials: meta-epidemiological study. BMJ.
search filter for retrieving systematic reviews and meta-analyses. BMC Med 2013;346:f457. doi: http://dx.doi.org/10.1136/bmj.f457 PMID: 23360719
Res Methodol. 2012;12(1):51. doi: http://dx.doi.org/10.1186/1471-2288-12- 33. Moynihan R. Surrogates under scrutiny: fallible correlations, fatal
51 PMID: 22512835 consequences. BMJ. 2011;343:d5160. doi: http://dx.doi.org/10.1136/bmj.
14. Bainbridge D, Martin J, Arango M, Cheng D; Evidence-based Peri-operative d5160 PMID: 21844159
Clinical Outcomes Research (EPiCOR) Group. Perioperative and anaesthetic- 34. Yudkin JS, Lipska KJ, Montori VM. The idolatry of the surrogate. BMJ.
related mortality in developed and developing countries: a systematic 2011;343:d7995. doi: http://dx.doi.org/10.1136/bmj.d7995 PMID: 22205706
review and meta-analysis. Lancet. 2012;380(9847):107581. doi: http:// 35. Salomon JA, Wang H, Freeman MK, Vos T, Flaxman AD, Lopez AD, et al.
dx.doi.org/10.1016/S0140-6736(12)60990-8 PMID: 22998717 Healthy life expectancy for 187 countries, 19902010: a systematic analysis
15. Braz LG, Braz DG, da Cruz DS, Fernandes LA, Mdolo NSP, Braz JRC. Mortality for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2144
in anesthesia: a systematic review. Clinics (Sao Paulo). 2009;64(10):9991006. 62. doi: http://dx.doi.org/10.1016/S0140-6736(12)61690-0 PMID: 23245606
16. Hansen D, Gausi SC, Merikebu M. Anaesthesia in Malawi: complications and 36. Galukande M, von Schreeb J, Wladis A, Mbembati N, de Miranda H, Kruk
deaths. Trop Doct. 2000;30(3):1469. PMID: 10902471 ME, et al. Essential surgery at the district hospital: a retrospective descriptive
17. Ouro-Bangna Maman AF, Tomta K, Ahouangbvi S, Chobli M. Deaths analysis in three African countries. PLoS Med. 2010;7(3):e1000243. doi:
associated with anaesthesia in Togo, West Africa. Trop Doct. 2005;35(4):220 http://dx.doi.org/10.1371/journal.pmed.1000243 PMID: 20231871
2. doi: http://dx.doi.org/10.1258/004947505774938666 PMID: 16354475 37. Shillcutt SD, Walker DG, Goodman CA, Mills AJ. Cost effectiveness in
18. Fenton PM, Whitty CJM, Reynolds F. Caesarean section in Malawi: low- and middle-income countries: a review of the debates surrounding
prospective study of early maternal and perinatal mortality. BMJ. decision rules. Pharmacoeconomics. 2009;27(11):90317. doi: http://dx.doi.
2003;327(7415):587. doi: http://dx.doi.org/10.1136/bmj.327.7415.587 PMID: org/10.2165/10899580-000000000-00000 PMID: 19888791
12969922 38. World development report 1993: investing in health [Internet]. Washington:
19. Enohumah KO, Imarengiaye CO. Factors associated with anaesthesia-related Oxford University Press; 1993. Available from: http://books.google.co.uk/
maternal mortality in a tertiary hospital in Nigeria. Acta Anaesthesiol Scand. books?id=vuGyAAAAIAAJ [cited 2014 Jul 25].
2006;50(2):20610. doi: http://dx.doi.org/10.1111/j.1399-6576.2006.00945.x 39. World development indicators. Washington: World Bank; 2014.
PMID: 16430543 40. Reardon S. Frugal science gets DIY diagnostics to worlds poorest. New Sci.
20. Walker IA, Obua AD, Mouton F, Ttendo S, Wilson IH. Paediatric surgery 2013;219(2933):201. doi: http://dx.doi.org/10.1016/S0262-4079(13)62184-3
and anaesthesia in south-western Uganda: a cross-sectional survey. Bull 41. McKenzie AG. Mortality associated with anaesthesia at Zimbabwean
World Health Organ. 2010;88(12):897906. doi: http://dx.doi.org/10.2471/ teaching hospitals. S Afr Med J. 1996;86(4):33842. PMID: 8693367
BLT.10.076703 PMID: 21124714
866 Bull World Health Organ 2014;92:858867| doi: http://dx.doi.org/10.2471/BLT.14.137315
Research
SamanthaL Burn et al. Costeffectiveness of pulse oximetry
42. Duke T, Wandi F, Jonathan M, Matai S, Kaupa M, Saavu M, et al. Improved 45. Core medical equipment. Geneva: World Health Organization; 2011.
oxygen systems for childhood pneumonia: a multihospital effectiveness Available from: http://whqlibdoc.who.int/hq/2011/WHO_HSS_EHT_
study in Papua New Guinea. Lancet. 2008;372(9646):132833. doi: http:// DIM_11.03_eng.pdf [cited 2014 Jul 25].
dx.doi.org/10.1016/S0140-6736(08)61164-2 PMID: 18708248 46. Medical devices: managing the mismatch. An outcome of the priority
43. Matai S, Peel D, Wandi F, Jonathan M, Subhi R, Duke T. Implementing an medical devices project. Geneva: World Health Organization; 2010. Available
oxygen programme in hospitals in Papua New Guinea. Ann Trop Paediatr. from: http://whqlibdoc.who.int/publications/2010/9789241564045_eng.
2008;28(1):718. doi: http://dx.doi.org/10.1179/146532808X270716 PMID: pdf [cited 2014 Jul 25].
18318953 47. Compendium of innovative health technologies for low-resource settings
44. Savage A. Why are the chosen pulse oximeters so expensive? BMJ. 20112013. Geneva: World Health Organization; 2014. Available from:
2012;344:e210, discussion e219. doi: http://dx.doi.org/10.1136/bmj.e210 http://apps.who.int/iris/bitstream/10665/108781/1/9789241564731_eng.
PMID: 22252691 pdf?ua=1 [cited 2014 Jul 25].
Bull World Health Organ 2014;92:858867| doi: http://dx.doi.org/10.2471/BLT.14.137315 867
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Otitis MediaDocument7 pagesOtitis MediaLian Tolombot LambeyNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- 1 SM PDFDocument16 pages1 SM PDFRaNo ratings yet
- Jurnal 1Document5 pagesJurnal 1Lian Tolombot LambeyNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- PDFDocument10 pagesPDFLian Tolombot LambeyNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Manuskrip Titin BaruDocument11 pagesManuskrip Titin BaruLian Tolombot LambeyNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- PDFDocument10 pagesPDFLian Tolombot LambeyNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Fullpapers Ijchn6fbc22c576full PDFDocument10 pagesFullpapers Ijchn6fbc22c576full PDFLian Tolombot LambeyNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Eng PDFDocument252 pagesEng PDFLian Tolombot LambeyNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- 17 010417Document2 pages17 010417Lian Tolombot LambeyNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- 17 010417Document2 pages17 010417Lian Tolombot LambeyNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Fullpapers Ijchn6fbc22c576full PDFDocument10 pagesFullpapers Ijchn6fbc22c576full PDFLian Tolombot LambeyNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hard DiskDocument9 pagesHard DiskAmarnath SahNo ratings yet
- CL Honours Report NamanDocument11 pagesCL Honours Report NamanNaman VermaNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- SCD Course List in Sem 2.2020 (FTF or Online) (Updated 02 July 2020)Document2 pagesSCD Course List in Sem 2.2020 (FTF or Online) (Updated 02 July 2020)Nguyễn Hồng AnhNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Names of Planner(s) : Style of Experience: (Whole Class, Small Group, Etc.) Lab: KindergartenDocument4 pagesNames of Planner(s) : Style of Experience: (Whole Class, Small Group, Etc.) Lab: Kindergartenapi-428128701No ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- LC For Akij Biax Films Limited: CO2012102 0 December 22, 2020Document2 pagesLC For Akij Biax Films Limited: CO2012102 0 December 22, 2020Mahadi Hassan ShemulNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- CE EVALUATION EXAM No. 4 - MGT, Fluid Properties, Hydrostatic Force (Answer Key)Document6 pagesCE EVALUATION EXAM No. 4 - MGT, Fluid Properties, Hydrostatic Force (Answer Key)Angelice Alliah De la CruzNo ratings yet
- Bridge Over BrahmaputraDocument38 pagesBridge Over BrahmaputraRahul DevNo ratings yet
- Approvals Management Responsibilities and Setups in AME.B PDFDocument20 pagesApprovals Management Responsibilities and Setups in AME.B PDFAli LoganNo ratings yet
- HRM Practices in NepalDocument22 pagesHRM Practices in NepalBodhiNo ratings yet
- EPW, Vol.58, Issue No.44, 04 Nov 2023Document66 pagesEPW, Vol.58, Issue No.44, 04 Nov 2023akashupscmadeeaseNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Determinant of Nurses' Response Time in Emergency Department When Taking Care of A PatientDocument9 pagesDeterminant of Nurses' Response Time in Emergency Department When Taking Care of A PatientRuly AryaNo ratings yet
- Abilash - Subramanian CV - 003 PDFDocument4 pagesAbilash - Subramanian CV - 003 PDFAbilash SubramanianNo ratings yet
- Cash Flow July 2021Document25 pagesCash Flow July 2021pratima jadhavNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- OTP User Manual For English) v1,0Document15 pagesOTP User Manual For English) v1,0auyinNo ratings yet
- Stress Management HandoutsDocument3 pagesStress Management HandoutsUsha SharmaNo ratings yet
- Third Party Risk Management Solution - WebDocument16 pagesThird Party Risk Management Solution - Webpreenk8No ratings yet
- Sabian Aspect OrbsDocument8 pagesSabian Aspect Orbsellaella13100% (2)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Section 1 Company Overview StandardsDocument34 pagesSection 1 Company Overview StandardsChris MedeirosNo ratings yet
- Ce-Series - TK60981-ML-18 IM - Rev - 0 - 05-13Document96 pagesCe-Series - TK60981-ML-18 IM - Rev - 0 - 05-13VERDADE MUNDIAL GUERRANo ratings yet
- Quality Standards For ECCE INDIA PDFDocument41 pagesQuality Standards For ECCE INDIA PDFMaryam Ben100% (4)
- ME-6501Computer Aided Design (CAD) WITH QB - BY Civildatas - Com 1Document85 pagesME-6501Computer Aided Design (CAD) WITH QB - BY Civildatas - Com 1Nathar ShaNo ratings yet
- Jurnal Job DescriptionDocument13 pagesJurnal Job DescriptionAji Mulia PrasNo ratings yet
- Documentation Report On School's Direction SettingDocument24 pagesDocumentation Report On School's Direction SettingSheila May FielNo ratings yet
- AMS ANALITICA-AIRFLOW TSP-HVS BrochureDocument1 pageAMS ANALITICA-AIRFLOW TSP-HVS BrochureShady HellaNo ratings yet
- Strategic Management SlidesDocument150 pagesStrategic Management SlidesIqra BilalNo ratings yet
- Building Material Supplier in GurgaonDocument12 pagesBuilding Material Supplier in GurgaonRodidustNo ratings yet
- Installation 59TP6A 08SIDocument92 pagesInstallation 59TP6A 08SIHenry SmithNo ratings yet
- Darkle Slideshow by SlidesgoDocument53 pagesDarkle Slideshow by SlidesgoADITI GUPTANo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Anker Soundcore Mini, Super-Portable Bluetooth SpeakerDocument4 pagesAnker Soundcore Mini, Super-Portable Bluetooth SpeakerM.SaadNo ratings yet
- L 11Document3 pagesL 11trangNo ratings yet