Professional Documents
Culture Documents
Word DR Sofi
Uploaded by
Muhammad Ferhat E.S.0 ratings0% found this document useful (0 votes)
7 views23 pagesword
Original Title
Word Dr Sofi
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentword
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
7 views23 pagesWord DR Sofi
Uploaded by
Muhammad Ferhat E.S.word
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 23
ABSTRACT
Postmenopausal bleeding (PMB) can be the rst sign of endometrial
cancer. In case of thickened endometrium, endometrial sampling is
often used in these women. In this systematic review, we studied the
accuracy of endometrial sampling for the diagnoses of endometrial
cancer, atypical hyperplasia and endometrial disease (endometrial
pathology, including benign polyps).
We systematically searched the literature for studies
comparing the results of endometrial sampling in women with
postmenopausal bleeding with two different reference standards:
blind dilatation and curettage (D&C) and hysteroscopy with
histology. We assessed the quality of the detected studies by the
QUADAS-2 tool. For each included study, we calculated the fraction of
women in whom endometrial sampling failed. Furthermore, we
extracted numbers of cases of endometrial cancer, atypical
hyperplasia and endometrial disease that were identied or missed by
endometrial sampling.
We detected 12 studies reporting on 1029 women with
postmenopausal bleeding: ve studies with dilatation and curettage
(D&C) and seven studies with hysteroscopy as a reference test. The
weighted sensitivity of endometrial sampling with D&C as a reference for
the diagnosis of endometrial cancer was 100% (range 100100%) and
92% (71100) for the diagnosis of atypical hyperplasia. Only one
study reported sensitivity for endometrial disease, which was 76%.
When hysteroscopy was used as a reference, weighted sensitivities of
endometrial sampling were 90% (range 50100), 82% (range 5694) and
39% (2169) for the diagnosis of endometrial cancer, atypical
hyperplasia and endometrial disease, respectively. For all diagnosis
studied and the reference test used, specicity was 98100%. The
weighted failure rate of endometrial sampling was 11% (range 153%),
while insufcient samples were found in 31% (range 776%). In these
women with insufcient or failed samples, an endometrial (pre) cancer
was found in 7% (range 018%).
In women with postmenopausal bleeding, the sensitivity of
endometrial sampling to detect endometrial cancer and especially
atypical hyperplasia and endometrial disease, including endometrial
polyps, is lower than previously thought. Therefore, further diagnostic
work-up for focal pathology is warranted, after a benign result of
endometrial sampling.
Introduction
Postmenopausal bleeding (PMB) is one of the most frequent
complaints with which women present in the outpatient gynecology clinic.
As PMB might be the rst sign of endometrial cancer, accurate diagnostic
work up is necessary in these women. Despite many studies on the
different diagnostic measures in women with PMB, there is no consensus
on the best diagnostic pathway [14].
In many guidelines the measurement of endometrial thickness by
transvaginal sonography (TVS) is used as a rst step in the diagnostic
pathway to distinguish women with a low and a high risk of having
endometrial cancer. Clark et al. found that a strategy with TVS as the
initial test with a cut-off of 4 mm followed by endometrial sampling was
the most cost-effective [5]. In situations where ultrasound is not directly
available, endometrial sampling can be used as the rst step [6].
The meta-analysis by Dijkhuizen et al. was the rst meta-
analysis on the diagnostic accuracy of endometrial sampling in women
with postmenopausal bleeding [7]. Several years after that, two other
meta-analyses were published [8,9]. These meta- analyses found that
sensitivity, which is crucial to rule out endometrial cancer, was
around 99%. However, in these studies (blind) dilatation and curettage
(D&C) had been used as reference standard. Nowadays, D&C is almost
completely replaced by hysteroscopy as a reference standard [10].
Also, only a small proportion of women in these meta-analyses was
postmenopausal.
In view of this, we decided to conduct a systematic review and
meta-analysis to study the diagnostic accuracy of endometrial sampling
in women with PMB regarding the diagnoses of endometrial cancer and
atypical hyperplasia compared to two different reference standards:
blind D&C and the current reference standard: hysteroscopy with
histology or hysterectomy [10].
Methods
Identication of studies
In April 2015, we performed a computerized search in MEDLINE,
EMBASE and Science Direct1 to identify all studies on the diagnostic
accuracy of endometrial sampling published between January 1965 and
March 2015. The search was limited to studies in humans; language
restrictions were not applied. We used all known synonyms for the
following keywords: postmen- opausal bleeding AND endometrial
sampling. We included observational studies on the evaluation of the
diagnostic accuracy of endometrial sampling in women with PMB.
References cited in the selected articles were checked for further relevant
articles not identied by the electronic searches. The search strategy can
be found in the Appendix.
Selection criteria
This review focused on diagnostic studies in which the
histology results of endometrial sampling were compared with the
results of a reference standard. The articles had to study women with
postmenopausal uterine bleeding, the diagnostic test of interest was
endometrial sampling (histology), the reference standard had to be
endometrial histological ndings from (blind) D&C, diagnostic
hysteroscopy with histology by targeted biopsy or D&C or hysterectomy.
Identied articles were merged into a common le, duplicates were
deleted, and results were divided between two reviewers (NvH and
MMP) who independently examined the assigned articles and
classied each as exclude, include, or unsure. Initial screening
began with a title screen. Subsequently, abstracts were retrieved and
screened to determine eligibility. Finally, full text articles were retrieved
and screened for inclusion. A third reviewer (MB) settled discrepancies.
For articles, which included both pre- and postmenopausal women, but
did not report separately on the postmenopausal group, we sent an
email to the corresponding author to ask for the data on
postmenopausal women. For articles which were published before
1997 and therefor no of the corresponding author was mentioned,
we searched the internet (Google, PubMed) for an to contact the
corresponding author. We calculated the agreement on the
selection of studies between the reviewers.
Quality assessment
Two reviewers (NvH and MMP) independently assessed the
methodological quality of each selected paper using the QUADAS-2 tool for
diagnostic studies, modied to conform to this review [11]. Disagreements
were resolved via consensus and if necessary via consensus of a third
reviewer (MB).
We decided a priori the criteria of each study for low risk of bias in each
of the four main domains of the Quadas-2 tool: patient selection,
index test, reference standard, and ow and timing [11]. For patient
selection, the in- and exclusion criteria had to be clearly stated, and the
patient sample had to be consecutive. For the index test, the independent
assessment of the pathologist for endometrial sampling without knowledge
of the results of the reference test had to be clearly stated, and the histology-
results had to be pre-specied. For the reference standard (D&C or
hysteroscopy) it had to be clearly stated that results were interpreted
without knowledge of the result of endometrial sampling. For patient
ow and timing, the time between endometrial sampling and reference
test, if all patients received the same reference test and if all patients were
included in the analysis, had to be clearly stated. Applicability was based
on patients with PMB, endometrial sampling as the index test, D&C or
diagnostic hysteroscopy with histology as reference test.
For all articles, each domain was assessed in terms of risk and bias,
and the rst three domains were also assessed in terms of applicability
for this review. Each item was labeled low, high, or unclear. Studies,
which scored high bias on more than one of four items, were excluded. And
only studies, which scored low on all three items of concerns on
applicability, were included in this review. We included all applicable
studies on this subject, regardless of the number of postmenopausal women
included and regardless if data were collected prospectively or
retrospectively.
Data extraction
For studies, which included pre- and postmenopausal women, we
used only those calculations and conclusions concerning the latter. From
each article we extracted (if available): the reference standard that was
used, the number of women who underwent endometrial sampling, the
number of women in whom endome- trial sampling was not possible,
failed or showed insufcient material for a pathologic diagnosis, the
number of women who underwent both endometrial sampling and the
reference standard, the number of cases with endometrial cancer, atypical
hyperplasia or endometrial disease. Hyperplasia without atypia was
consid- ered a benign result.
Endometrial disease was dened as benign endometrial polyps in
one study, and as polyps, hyperplasia and cancer together in most other
studies. For this meta-analysis we decided to dene endometrial disease
as endometrial cancer, atypical hyperplasia and benign endometria
polyps together as endometrial disease.
Data analysis
For each study, we calculated the percentage of women in
whom endometrial sampling failed to provide a diagnosis, either due to
the possibility to obtain tissue (for example because of cervical
stenosis) or due to the fact that the sample which was obtained was
insufcient for the pathologist to establish a diagnosis. We described
the number of endometrial cancers in women with a failed endometrial
sampling.
For studies that had numbers available, we constructed 2 2
tables and calculated sensitivity and specicity for the diagnosis of
endometrial cancer, atypical hyperplasia or endometrial disease.
Sensitivity, specicity and negative and positive likelihood ratios (LR
and LR+) were calculated for the cases in which both endometrial
sampling as well as the reference test was successful. We calculated the
weighted sensitivity, specicity and likelihood ratios, taking into account
the size of each study, compared to the two different reference strategies.
When a 2x2 table could be constructed, we plotted the sensitivity against
the 1- specicity in a receiver-operating curve (ROC).
Results
Study selection
Our systematic search identied 499 titles. After exclusion of
studies, which did not exist online anymore and exclusion of
duplicates, we identied 377 articles, of which 65 articles were found to
be relevant (Fig. 1). After reading these 65 articles in full text, we could
include 11 studies that reported on postmenopausal women only, 2
articles that described data on postmenopausal women separately in a
total population of perimenopausal women and 17 articles that compared
the results of endometrial sampling with histology ndings from (blind)
D&C or diagnostic hysteros- copy in a combined population of pre-
and postmenopausal women.
In none of the 17 studies that reported on a combination of pre- and
postmenopausal women, we were able to contact the corresponding
author. In 10 studies these authors did not respond, while contact details
were not available for the other 7 studies. Therefore, we had to exclude
these 17 studies from the meta- analysis [1228]. The initial agreement
of the two reviewers (NvH and MMP) regarding eligibility was 94%
(weighted kappa 0.88 (95% CI 0.760.99)).
Quality assessment
Table 2 presents quality assessment of the included studies [29
41]. Quality assessment showed in four studies (25%) a low risk of bias on
all four items, three studies showed a high risk of bias on one of the
items, while eight studies had an unclear risk of bias on the description of
methods on patient selection, the index or reference test. All studies,
except for one scored low on the three items of applicability [2940].
Based on a high concern of applicability of the index test and reference
standard described in OConnell et al., we decided to exclude this study
[41]. After study selection and quality assessment, we included 12
articles in this systematic review, reporting on 1029 women with
postmeno- pausal bleeding (Tables 1 and 2, Fig. 2).
Diagnostic accuracy of endometrial sampling in women with PMB
Tables 1 and 3 show the ndings of the 12 included studies [2940].
The Pipelle device was used in eight studies [29,30,3234,3739], while
the other studies reported on the use of Accurette [40], Endorette [35],
and Novak endometrial sampler [31]. One study reported on two
different sampling methods: Accurette and Vabra [36].
Blind D&C was used as the reference standard in ve
studies [3438] while hysteroscopy with histology (by biopsy and/or
curettage) was the reference standard in seven studies [29
33,39,40]. In three studies the diagnosis of endometrial cancer detected
by endometrial sampling was conrmed by hysterectomy and not by
hysteroscopy or D&C [29,30,38].
All 12 studies reported on the fraction of women in whom
endometrial sampling failed, mostly due to cervical stenosis. The
failure rates of endometrial sampling varied between 1% and 53%,
with a weighted failure rate of 11%. Eight studies reported on the
fraction of women in whom insufcient material was found at
histology, which varied between 7% and 76%, with a weighted
insufcient rate of 31% [31,3338,40]. In the article by Batool et al. the
rate of insufcient samples was much higher than in the other studies
(42/55). In 37 of these women with an insufcient sample, material was
also insuf- cient for diagnosis by D&C, which might explain the
high insufent-rate [37].
The weighted percentage of women with endometrial (pre) cancer
among those who had failed or insufcient sampling is 7% (range 018%
in seven studies). Goldberg et al. described a percentage of 18%
endometrial cancer in women with insufcient or failed samples. This
article from 1982, lacked detail on the small number of women (n = 12)
included [36].
Fig. 1. Study selection owchart. * The reference list for excluded
studies is available from the corresponding author.
Diagnosis of endometrial cancer
From all 12 articles we could extract data on the sensitivity, and
specicity and likelihood ratios regarding the diagnosis endome- trial
cancer (Table 4). The sensitivity of endometrial sampling was 100% in all
ve studies using blind D&C (LR of 0), but varied between 50 and
100% in the seven studies using hysteroscopy with histology as a reference
standard, with a weighted sensitivity of 90% and a LR of 0.10. Specicity
was 99100% regardless of the reference standard that was used. Fig. 3A
shows an ROC plot of the performance of the 12 studies that allowed the
calculation of both sensitivity and specicity.
Diagnosis of (pre)malignancy of the endometrium
With respect to the diagnosis of endometrial (pre-) cancer, i.e.
atypical hyperplasia or endometrial cancer we could calculate
sensitivity, and specicity and likelihood ratios from the data in all ve
studies using D&C as a reference and in four studies using hysteroscopy
as a reference (Table 4). The weighted sensitivity in studies using D&C
was 92% (range 71100%) with a LR of 0.08, whereas the weighted
sensitivity in studies using hysteroscopy as a reference standard was 82%
(range 5694%), with a LR of 0.18. Specicity was 99100% in all studies.
Fig. 3B shows an ROC plot of the performance of the twelve studies that
allowed the calculation of both sensitivity and specicity.
Diagnosis of endometrial disease
As in most studies diagnostic accuracy regarding benign
pathology was not described separately, we decided to extract data on
the accuracy regarding the diagnosis of endometrial disease, i.e.
endometrial cancer, hyperplasia and endometrial polyps together
(Table 4). The sensitivity of endometrial sampling was 29% in one study
using blind D&C and the weighted sensitivity was 39% (range 2169%),
with a LR of 0.61 in ve studies using hysteroscopy with histology as a
reference standard. Specicity was again high, 98100% regardless of the
reference standard used.
Fig. 2. Overall risk of bias and applicability using a modied Quadas-
2 tool [11].
Fig. 3C shows an ROC plot of the performance of the twelve studies that
allowed the calculation of both sensitivity and specicity.
Discussion
In this meta-analysis we assessed the diagnostic accuracy of
endometrial sampling regarding the diagnoses of endometrial cancer,
endometrial (pre) cancer and endometrial disease (includ- ing
endometrial polyps) in women with PMB, compared to two different
reference strategies: D&C and hysteroscopy. Specicity of endometrial
sampling is very high, irrespective of the type of disease or the
reference test that was used. Sensitivities, on the other hand, are lower
than anticipated based on existing meta- analyses, for all types of
disease, but especially for atypical hyperplasia and endometrial
disease, which includes endometrial polyps. Therefore we can conclude
that a positive test result of endometrial sapling is very accurate in
diagnosing endometrial (pre)cancer or endometrial disease. However,
endometrial sam- pling is not very accurate in ruling out endometrial
(pre)cancer and endometrial disease and therefore further diagnostic
work-up for focal pathology is warranted, after a benign result of
endometrial sampling.
An important strength of this meta-analysis is that we
performed a thorough search for articles on the diagnostic accuracy
in women with PMB. By searching with all synonyms for PMB and
endometrial sampling, we think we selected all articles on this subject.
We also selected articles, which described only a subgroup of
postmenopausal women and tried to contact the authors of these
articles. Unfortunately, none of them responded. We included all
eligible articles, regardless of the language used.
This article also has several limitations. Publication bias and the risk
of missing potentially relevant articles are concerns with any
systematic review. We attempted to mitigate this issue by using a robust
search strategy, by checking cross-references and by consulting with a
clinical librarian. Also, observer agreement regarding study selection
was high. However, by performing this rigorous systematic search, we
could only identify four more studies compared to the three existing
meta-analyses on this subject [79].
Another weakness is that, because only a small number of
studies is available and most studies are based on small samples, we had
to draw conclusions based on a limited number of patients. Apart from the
limited power, the relatively small number of studies and variability in
methods also did not allow for more standard statistical analyses
recommended for diagnostic test accuracy reviews, such as pooling
sensitivity and specicity using the bivariate model or estimating
summary ROCs.
The three existing meta-analyses focused on the diagnostic
accuracy of endometrial sampling in a mixed population of pre- and
postmenopausal women [79]. As the diagnostic accuracy of a test is
strongly dependent on the prevalence (or pre-test probability) of a
diagnosis, and the prevalence of endometrial cancer and atypical
hyperplasia is much lower in pre-versus postmenopausal women, we
think it is important to study this subject in a selected population of
women with PMB. Therefore, we searched specically for articles on the
diagnostic accuracy of endometrial sampling in women with PMB and
included only these studies, which reported data on postmenopausal
bleeding separately.
Fig. 3. A1 tm 3C2. Receiver operating curve (ROC) plots demonstrating
the accuracy of endometrial sampling in diagnosing endometrial
cancer, endometrial (pre) cancer or endometrial disease with D&C or
hysteroscopy as a reference standard.
Endometrial sampling fails in 42% of cases (either technical failure
or insufent material) and in 7% of these cases a (pre)malignancy is
found. This nding is in accordance with ndings in other studies,
which describe a failure or inconclusive rate of 1650% and in 520% of
these cases signicant endometrial pathology is found [4244].
Therefore, a case of a failed or inconclusive sample, should lead to
further diagnostic work up. Also, a benign result of endometrial
sampling is not completely reassuring, as sensitivities and LR are
lower than anticipated based on previous literature. In the three existing
meta-analyses (blind) D&C has been used as a reference standard,
which is worrisome as D&C is known to miss 5085% of focal
intracavitary pathology [45,46]. As D&C could miss focal pathology, it
could also possibly miss endometrial (pre) cancer in an endometrial
polyp. Therefore, nowadays, D&C is almost completely replaced by
hysteroscopy as a reference standard, both in clinical as well as in research
settings [10]. It suggests that endometrial sampling, which is
performed as a mini-curettage, as well misses a signicant number of focal
pathologies and therefore possibly also focal (pre) cancers. Because
atypical hyperplasia is regarded as endometrial (pre) cancer, (in 17
52% an underlying cancer is found at hysterectomy [47]), it is
important to diagnose not only endometrial cancer but also atypical
hyperplasia. Given the above
ndings, further diagnostic work up for focal intracavitary
pathology in women with a failed, insufcient or benign result of
endometrial sampling seems warranted.
The results of this systematic review suggest that the sensitivity of
endometrial sampling is lower than was thought before for all types of
disease, but especially for the diagnosis of atypical hyperplasia and
endometrial disease in general. The question is if we can reassure
patients without an endometrial polyp and a benign result of
endometrial sampling. Is sensitivity of endome- trial sampling
especially low in women with an endometrial polyp? Unfortunately we
cannot answer these questions based on available literature. Therefore,
more research on this subject is needed, using larger samples, given the
prevalence of endometrial cancer and atypical hyperplasia (510%).
Future research should therefore aim to gather information about
large (prospective) cohorts of patients with PMB, to study the (cost)
effectiveness and diagnostic accuracy of the endometrial biopsy and
hysteroscopy in the diagnostic pathway in women with PMB and a
thickened endometrium on TVS.
Funding
This research received no specic grant from any funding
agency in the public, commercial or not-for-prot sectors.
References
[1] Dutch Society of Obstetrics and Gynecology (NVOG). Diagnostics
in abnormal vaginal blood loss in the postmenopausal period; 2003.
[2] American College of Obstetricians and Gynecologists. ACOG
Committee Opinion No. 426: the role of transvaginal
ultrasonography in the evaluation of postmenopausal bleeding.
Obstet Gynecol 2009;113(Febru- ary):4624.
[3] Epstein E. Management of postmenopausal bleeding in Sweden: a
need for increased use of hydrosonography and hysteroscopy. Acta
Obstet Gynecol Scand 2004;83(January (1)):8995.
[4] Goldstein RB, Bree RL, Benson CB, et al. Evaluation of the
woman with postmenopausal bleeding: Society of Radiologists in
Ultrasound-Sponsored Consensus Conference statement. J
Ultrasound Med 2001;20(October (10)): 102536.
[5] Clark TJ, Barton PM, Coomarasamy A, Gupta JK, Khan KS.
Investigating post- menopausal bleeding for endometrial cancer:
cost-effectiveness of initial diagnostic strategies. BJOG
2006;113(May (5)):50210.
[6] van Hanegem N, Breijer MC, Khan KS, et al. Diagnostic
evaluation of the endometrium in postmenopausal bleeding: an
evidence-based approach. Maturitas 2011;68(February (2)):15564.
[7] Dijkhuizen FP, Mol BW, Brolmann HA, Heintz AP. The accuracy of
endometrial sampling in the diagnosis of patients with endometrial
carcinoma and hyper- plasia: a meta-analysis. Cancer
2000;89(October (8)):176572.
[8] Clark TJ, Mann CH, Shah N, Khan KS, Song F, Gupta JK. Accuracy of
outpatient endometrial biopsy in the diagnosis of endometrial
cancer: a systematic quantitative review. BJOG 2002;109(March
(3)):31321.
[9] Clark TJ, Mann CH, Shah N, Khan KS, Song F, Gupta JK. Accuracy of
outpatient endometrial biopsy in the diagnosis of endometrial
hyperplasia. Acta Obstet Gynecol Scand 2001;80(September
(9)):78493.
[10] Clark TJ. Accuracy of hysteroscopy in the diagnosis of
endometrial cancer and hyperplasia: a systematic quantitative
review. J Am Med Assoc2002;288(13):161021.
[11] Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a
revised tool for the quality assessment of diagnostic accuracy
studies. Ann Intern Med 2011;155(October (8)):52936.
[12] Antoni J, Folch E, Costa J, et al. Comparison of cytospat and
pipelle endometrial biopsy instruments. Eur J Obstet Gynecol Reprod
Biol 1997;72(1):5761.
[13] Bibbo M, Reale FR, Reale JC, et al. Assessment of three sampling
techniques to detect endometrial cancer and its precursors. A
preliminary report. Acta Cytol 1979;23(SeptemberOctober (5)):353
9.
[14] Ferry J, Farnsworth A, Webster M, Wren B. The efcacy of the
pipelle endo- metrial biopsy in detecting endometrial carcinoma. Aust
N Z J Obstet Gynaecol
[15] Goldchmit R, Katz Z, Blickstein I, Caspi B, Dgani R. The accuracy of
endometrial Pipelle sampling with and without sonographic
measurement of endometrial thickness. Obstet Gynecol
1993;82(November (5)):72730.
[16] Greenwood SM, Wright DJ. Evaluation of the ofce endometrial
biopsy in the detection of endometrial carcinoma and atypical
hyperplasia. Cancer 1979;43(April (4)):14748.
[17] Guido RS, Kanbour-Shakir A, Rulin MC, Christopherson WA.
Pipelle endome- trial sampling. Sensitivity in the detection of
endometrial cancer. J Reprod Med 1995;40(August (8)):5535.
[18] Huang GS, Gebb JS, Einstein MH, Shahabi S, Novetsky AP,
Goldberg GL. Accuracy of preoperative endometrial sampling for
the detection of high- grade endometrial tumors. Am J Obstet
Gynecol 2007;196(March (3)):243.e1.e5.
[19] Kavak Z, Ceyhan N, Pekin S. Combination of vaginal
ultrasonography and pipelle sampling in the diagnosis of
endometrial disease. Aust N Z J Obstet Gynaecol 1996;36(February
(1)):636.
[20] Larson DM, Krawisz BR, Johnson KK, Broste SK. Comparison of
the Z-sampler and Novak endometrial biopsy instruments for in-
ofce diagnosis of endome- trial cancer. Gynecol Oncol 1994;54(July
(1)):647.
[21] Machado F, Moreno J, Carazo M, Leon J, Fiol G, Serna R. Accuracy of
endometrial biopsy with the Cornier pipelle for diagnosis of
endometrial cancer and atypical hyperplasia. Eur J Gynaecol Oncol
2003;24(34):27981.
[22] Polena V, Mergui JL, Zerat L, Sananes S. The role of Pipelle Mark II
sampling in endometrial disease diagnosis. Eur J Obstet Gynecol
Reprod Biol 2007;134(Oc- tober (2)):2337.
[23] Salet-Lizee D, Gadonneix P, Van Den Akker M, Villet R. The
reliability of study methods of the endometrium. A comparative
study of 178 patients. J Gynecol Obstet Biol Reprod (Paris)
1993;22(6):5939.
[24] Stovall TG, Photopulos GJ, Poston WM, Ling FW, Sandles LG.
Pipelle endome- trial sampling in patients with known endometrial
carcinoma. Obstet Gynecol 1991;77(June (6)):9546.
[25] Stovall TG, Solomon SK, Ling FW. Endometrial sampling prior to
hysterectomy. Obstet Gynecol 1989;73(March (3 Pt 1)):4059.
[26] Tahir MM, Bigrigg MA, Browning JJ, Brookes ST, Smith PA. A
randomised controlled trial comparing transvaginal ultrasound,
outpatient hysteroscopy and endometrial biopsy with inpatient
hysteroscopy and curettage. Br J Obstet Gynaecol
1999;106(December (12)):125964.
[27] Tay SK, Tan SA, Chua KM, Lim-Tan SK. The diagnostic value
and patient acceptability of outpatient endometrial sampling with
Gynoscann. Aust N Z J Obstet Gynaecol 1992;32(February (1)):736.
[28] Zorlu CG, Cobanoglu O, Isik AZ, Kutluay L, Kuscu E. Accuracy
of pipelle endometrial sampling in endometrial carcinoma.
Gynecol Obstet Invest 1994;38(4):2725.
[29] Van den Bosch T, Vandendael A, Van Schoubroeck D, Wranz PA,
Lombard CJ. Combining vaginal ultrasonography and ofce
endometrial sampling in the diagnosis of endometrial disease in
postmenopausal women. Obstet Gynecol 1995;85(March (3)):349
52.
[30] Van den Bosch T, Vandendael A, Wranz PA, Lombard CJ.
Endopap-versus Pipelle-sampling in the diagnosis of
postmenopausal endometrial disease. Eur J Obstet Gynecol Reprod
Biol 1996;64(January (1)):914.
[31] Giusa-Chiferi MG, Goncalves WJ, Baracat EC, de Albuquerque
Neto LC, Borto- letto CC, de Lima GR. Transvaginal ultrasound,
uterine biopsy and hysteros- copy for postmenopausal bleeding. Int
J Gynaecol Obstet 1996;55(October (1)):3944.
[32] Gupta JK, Wilson S, Desai P, Hau C. How should we investigate
women with postmenopausal bleeding? Acta Obstet Gynecol Scand
1996;75(May (5)):4759.
[33] De Silva BY, Stewart K, Steven JD, Sathanandan M. Transvaginal
ultrasound measurement of endometrial thickness and endometrial
pipelle sampling as an alternative diagnostic procedure to
hysteroscopy and dilatation and curet- tage in the management of
post-menopausal bleeding. J Obstet Gynaecol 1997;17(June
(4)):399402.
[34] Bunyavejchevin S, Triratanachat S, Kankeow K, Limpaphayom
KK. Pipelle versus fractional curettage for the endometrial sampling
in postmenopausal women. J Med Assoc Thail 2001;84(June (Suppl.
1)):S32630.
[35] Epstein E, Skoog L, Valentin L. Comparison of Endorette and
dilatation and curettage for sampling of the endometrium in women
with postmenopausal bleeding. Acta Obstet Gynecol Scand
2001;80(October (10)):95964.
[36] Goldberg GL, Tsalacopoulos G, Davey DA. A comparison of
endometrial sam- pling with the Accurette and Vabra aspirator and
uterine curettage. S Afr Med J 1982;61(January (4)):1146.
[37] Batool T, Reginald PW, Hughes JH. Outpatient pipelle endometrial
biopsy in the investigation of postmenopausal bleeding. Br J Obstet
Gynaecol 1994;101(June (6)):5456.
[38] Ben-Baruch G, Seidman DS, Schiff E, Moran O, Menczer J.
Outpatient endometrial sampling with the Pipelle curette. Gynecol
Obstet Invest 1994;37(4):2602.
[39] Mortakis AE, Mavrelos K. Transvaginal ultrasonography and
hysteroscopy in the diagnosis of endometrial abnormalities. J Am
Assoc Gynecol Laparosc 1997;4(August (4)):44952.
[40] Spicer JM, Siebert I, Kruger TF. Postmenopausal bleeding: a
diagnostic ap- proach for both private and public sectors. Gynecol
Obstet Invest 2006;61(3): 1748.
[41] OConnell LP, Fries MH, Zeringue E, Brehm W. Triage of
abnormal postmeno- pausal bleeding: a comparison of endometrial
biopsy and transvaginal sono- hysterography versus fractional
curettage with hysteroscopy. Am J Obstet Gynecol 1998;178(May
(5)):95661.
[42] Farrell T, Jones N, Owen P, Baird A. The signicance of an
insufcient Pipelle sample in the investigation of post-menopausal
bleeding. Acta Obstet Gynecol Scand 1999;78(October (9)):8102.
[43] Visser NC, Breijer MC, Herman MC, et al. Factors attributing to
the failure of endometrial sampling in women with postmenopausal
bleeding. Acta Obstet Gynecol Scand 2013;92(October (10)):1216
22.
[44] van Doorn HC, Opmeer BC, Burger CW, et al. Inadequate ofce
endometrial sample requires further evaluation in women with
postmenopausal bleeding and abnormal ultrasound results. Int J
Gynaecol Obstet 2007;99(November (2)):1004.
[45] Epstein E, Ramirez A, Skoog L, Valentin L. Dilatation and
curettage fails to detect most focal lesions in the uterine cavity in
women with postmeno- pausal bleeding. Acta Obstet Gynecol
Scand 2001;80(December (12)):11316.
[46] Gebauer G, Hafner A, Siebzehnrubl E, Lang N. Role of hysteroscopy
in detection and extraction of endometrial polyps: results of a
prospective study. Am J Obstet Gynecol 2001;184(January (2)):59
63.
[47] Trimble CL, Kauderer J, Zaino R, et al. Concurrent endometrial
carcinoma in women with a biopsy diagnosis of atypical
endometrial hyperplasia: a Gynecologic Oncology Group study.
Cancer 2006;106(February (4)): 8129.
You might also like
- Gambaran Usg PDFDocument5 pagesGambaran Usg PDFMahend AuliaNo ratings yet
- Gynecology Outpatient Clinic April 13th 2020Document3 pagesGynecology Outpatient Clinic April 13th 2020Muhammad Ferhat E.S.No ratings yet
- Duty Report 7 November 2017 PirngadiDocument22 pagesDuty Report 7 November 2017 PirngadiMuhammad Ferhat E.S.No ratings yet
- Realease ObstructionDocument4 pagesRealease ObstructionMuhammad Ferhat E.S.No ratings yet
- Tabel Induk BlastocystDocument3 pagesTabel Induk BlastocystMuhammad Ferhat E.S.No ratings yet
- Duty Report Wednesday, October 18Th 2017 Supervisor: Dr. Hilma P. Lubis, Mked (Og), SpogDocument3 pagesDuty Report Wednesday, October 18Th 2017 Supervisor: Dr. Hilma P. Lubis, Mked (Og), SpogMuhammad Ferhat E.S.No ratings yet
- Group Cycles Culture To D5 Blastocyst Embryo % P-Value (MII) P-Value (Age) Age MIIDocument1 pageGroup Cycles Culture To D5 Blastocyst Embryo % P-Value (MII) P-Value (Age) Age MIIMuhammad Ferhat E.S.No ratings yet
- Gynecology Outpatient Clinic April 16th 2020Document3 pagesGynecology Outpatient Clinic April 16th 2020Muhammad Ferhat E.S.No ratings yet
- Tabel Blastocyst 2 EditDocument1 pageTabel Blastocyst 2 EditMuhammad Ferhat E.S.No ratings yet
- Proposal MenopauseDocument5 pagesProposal MenopauseMuhammad Ferhat E.S.No ratings yet
- Background 2Document14 pagesBackground 2Muhammad Ferhat E.S.No ratings yet
- Realease ObstructionDocument4 pagesRealease ObstructionMuhammad Ferhat E.S.No ratings yet
- Frequency Table DR MarissaDocument4 pagesFrequency Table DR MarissaMuhammad Ferhat E.S.No ratings yet
- Data SpssDocument26 pagesData SpssMuhammad Ferhat E.S.No ratings yet
- Duty Report Sept 14th 2017 HamDocument31 pagesDuty Report Sept 14th 2017 HamMuhammad Ferhat E.S.No ratings yet
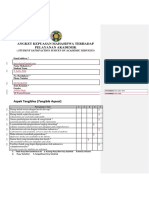
- Angket Kepuasan Mahasiswa Terhadap Pelayanan Akademik: (Student Satisfaction Survey On Academic Services)Document4 pagesAngket Kepuasan Mahasiswa Terhadap Pelayanan Akademik: (Student Satisfaction Survey On Academic Services)Muhammad Ferhat E.S.No ratings yet
- Mapping Ruangan 24 September 2017Document6 pagesMapping Ruangan 24 September 2017Muhammad Ferhat E.S.No ratings yet
- Angket Kepuasan Mahasiswa Terhadap Pelayanan Akademik: (Student Satisfaction Survey On Academic Services)Document4 pagesAngket Kepuasan Mahasiswa Terhadap Pelayanan Akademik: (Student Satisfaction Survey On Academic Services)Muhammad Ferhat E.S.No ratings yet
- Manuscript DR AdrianDocument12 pagesManuscript DR AdrianMuhammad Ferhat E.S.No ratings yet
- Mapping Obgyn 27 September 2017Document8 pagesMapping Obgyn 27 September 2017Muhammad Ferhat E.S.No ratings yet
- Follow Up PasienDocument20 pagesFollow Up PasienMuhammad Ferhat E.S.No ratings yet
- Mapping Obgyn 2 Oktober 2017Document7 pagesMapping Obgyn 2 Oktober 2017Muhammad Ferhat E.S.No ratings yet
- Pasien MaisarahDocument10 pagesPasien MaisarahMuhammad Ferhat E.S.No ratings yet
- Mapping Ruangan 24 September 2017Document6 pagesMapping Ruangan 24 September 2017Muhammad Ferhat E.S.No ratings yet
- Pasien MasdalipahDocument11 pagesPasien MasdalipahMuhammad Ferhat E.S.No ratings yet
- Pasien Poli GinekologiDocument1 pagePasien Poli GinekologiMuhammad Ferhat E.S.No ratings yet
- Manuscript DR AdrianDocument12 pagesManuscript DR AdrianMuhammad Ferhat E.S.No ratings yet
- Ginek Ward 14 AgustussDocument51 pagesGinek Ward 14 AgustussMuhammad Ferhat E.S.No ratings yet
- Ginek Ward 19 AgustusDocument22 pagesGinek Ward 19 AgustusMuhammad Ferhat E.S.No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Paradigms of ManagementDocument2 pagesParadigms of ManagementLaura TicoiuNo ratings yet
- Simba s7d Long Hole Drill RigDocument2 pagesSimba s7d Long Hole Drill RigJaime Asis LopezNo ratings yet
- LEARNING ACTIVITY Sheet Math 7 q3 M 1Document4 pagesLEARNING ACTIVITY Sheet Math 7 q3 M 1Mariel PastoleroNo ratings yet
- Kalley Ltdn40k221twam Chassis msd6308 SM PDFDocument49 pagesKalley Ltdn40k221twam Chassis msd6308 SM PDFjulio cesar calveteNo ratings yet
- Managerial EconomicsDocument3 pagesManagerial EconomicsGuruKPONo ratings yet
- Oxgen Sensor Cat WEBDocument184 pagesOxgen Sensor Cat WEBBuddy Davis100% (2)
- Easa Management System Assessment ToolDocument40 pagesEasa Management System Assessment ToolAdam Tudor-danielNo ratings yet
- Lab StoryDocument21 pagesLab StoryAbdul QadirNo ratings yet
- Beauty ProductDocument12 pagesBeauty ProductSrishti SoniNo ratings yet
- Allan S. Cu v. Small Business Guarantee and FinanceDocument2 pagesAllan S. Cu v. Small Business Guarantee and FinanceFrancis Coronel Jr.No ratings yet
- Cell Organelles ColoringDocument2 pagesCell Organelles ColoringThomas Neace-FranklinNo ratings yet
- PHY210 Mechanism Ii and Thermal Physics Lab Report: Faculty of Applied Sciences Uitm Pahang (Jengka Campus)Document13 pagesPHY210 Mechanism Ii and Thermal Physics Lab Report: Faculty of Applied Sciences Uitm Pahang (Jengka Campus)Arissa SyaminaNo ratings yet
- Done - NSTP 2 SyllabusDocument9 pagesDone - NSTP 2 SyllabusJoseph MazoNo ratings yet
- Chromate Free CoatingsDocument16 pagesChromate Free CoatingsbaanaadiNo ratings yet
- Pipeline Welding SpecificationDocument15 pagesPipeline Welding Specificationaslam.ambNo ratings yet
- Production of Sodium Chlorite PDFDocument13 pagesProduction of Sodium Chlorite PDFangelofgloryNo ratings yet
- 2018 NAMCYA CHILDREN'S RONDALLA ENSEMBLE GuidelinesDocument3 pages2018 NAMCYA CHILDREN'S RONDALLA ENSEMBLE GuidelinesJohn Cedrick JagapeNo ratings yet
- Dermatology Study Guide 2023-IvDocument7 pagesDermatology Study Guide 2023-IvUnknown ManNo ratings yet
- Form Active Structure TypesDocument5 pagesForm Active Structure TypesShivanshu singh100% (1)
- SEC QPP Coop TrainingDocument62 pagesSEC QPP Coop TrainingAbdalelah BagajateNo ratings yet
- SiloDocument7 pagesSiloMayr - GeroldingerNo ratings yet
- Bula Defense M14 Operator's ManualDocument32 pagesBula Defense M14 Operator's ManualmeNo ratings yet
- Stroboscopy For Benign Laryngeal Pathology in Evidence Based Health CareDocument5 pagesStroboscopy For Benign Laryngeal Pathology in Evidence Based Health CareDoina RusuNo ratings yet
- Ball Valves Pentair Valves and ControlsDocument16 pagesBall Valves Pentair Valves and ControlsABDUL KADHARNo ratings yet
- N4 Electrotechnics August 2021 MemorandumDocument8 pagesN4 Electrotechnics August 2021 MemorandumPetro Susan BarnardNo ratings yet
- Gabinete STS Activity1Document2 pagesGabinete STS Activity1Anthony GabineteNo ratings yet
- Oxygen Cost and Energy Expenditure of RunningDocument7 pagesOxygen Cost and Energy Expenditure of Runningnb22714No ratings yet
- Developing the cycle of maslahah based performance management system implementationDocument27 pagesDeveloping the cycle of maslahah based performance management system implementationM Audito AlfansyahNo ratings yet
- Manual WinMASW EngDocument357 pagesManual WinMASW EngRolanditto QuuisppeNo ratings yet
- HSSC English Model PaperDocument32 pagesHSSC English Model PaperMaryam Abdus SalamNo ratings yet