Professional Documents
Culture Documents
PJ Nicholoff Steroid Protocol
Uploaded by
Yanna RizkiaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PJ Nicholoff Steroid Protocol
Uploaded by
Yanna RizkiaCopyright:
Available Formats
PJ Nicholoff Steroid Protocol
Background/Assessment
Normal basal secretion of cortisol from the adrenal gland is approximately 5-7
mg/m2/day or 8 -10 mg/day for adults. This amount increases during minor illnesses or
surgery to approximately 50 mg/day (5x normal physiologic secretion). These small
increases with uncomplicated surgery return to baseline in 24 hours. Procedures
producing greater surgical stress, have been shown to increase cortisol responses to
75-150 mg/day (10x normal physiologic secretion), which return to baseline in about 5
days.
Corticosteroids are prescribed for multiple diagnoses to a wide variety of patients. Long
term administration of corticosteroids may lead to suppression of the hypothalamic-
pituitary-adrenal (HPA) axis. Rapid reduction or abrupt withdrawal of corticosteroid
therapy that has been prolonged or at high doses can cause secondary adrenal
insufficiency (suppression of the HPA axis), and steroid withdrawal or deprivation
syndrome. Recovery from suppression of the HPA axis after discontinuing
corticosteroids can be prolonged (possibly 6 to 12 months) and may vary based on
doses, dosing schedules and duration of corticosteroid therapy. Since there is a great
deal of individual variability in susceptibility to suppression of the HPA axis after chronic
use of exogenous corticosteroids, it is not possible to predict with confidence which
patients will be affected. Current practice is to administer supplemental (stress) doses of
corticosteroids to patients with suspected suppression of the HPA axis in the
perioperative period and during acute illness to prevent acute adrenal insufficiency, or
adrenal crisis.
Defining HPA Suppressed Patients:
Recommendations differ slightly in defining a suppressed patient, but general
guidelines are below (Table 1):
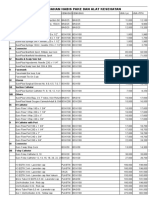
Table 1
Prednisone dose Prednisone Dose Suppression of HPA axis?
Equivalents/day - Adults Equivalents/Day - Pediatric
5mg/day or less 3 mg/m2/day or less Usually not suppressed.
Possibly suppressed. ACTH
5 20 mg/day 3-12 mg/m2/day stimulation test recommended or
give supplemental dose.
20 mg/day for >10 days or 12 mg/m2/day of prednisone Suppressed. Give supplemental
more for > 10 days or more dose.
Patients receiving disease appropriate corticosteroid doses (at least 10 times above the
physiologic cortisol dose) generally do not need stress doses if usual daily dose is
continued. Patients who are on maintenance physiologic dose of hydrocortisone for
primary disease of the HPA axis do require supplemental therapy.
Consultation with endocrinology is recommended for questions or concerns.
Recommendations for supplemental doses are generally divided by severity of stress
the patient may experience (medical or surgical). Supplemental steroid doses are then
based on degree of stress.
Corticosteroid Stress Doses:
Table 2
Medical/Surgical Stress Corticosteroid Dosage DOS* Postoperative Taper Regimen
Minor (local anesthesia, < 1 25mg or 30-50 mg/m2 po (if None
hour) able to take po) or IV Resume maintenance
(e.g. inguinal hernia, single tooth hydrocortisone (HC) or physiologic dose of
extraction, colonoscopy), mild equivalent hydrocortisone when illness,
febrile illness, mild, pain or fever subsides
nausea/vomiting, mild diarrhea)
Moderate 50mg or 50-75 mg/m2 IV 25 mg Q 8 or 50-75
(e.g. multiple teeth extraction, hydrocortisone or equivalent mg/m2/day q 6 hours X 24
fracture, pneumonia) hour. Taper to baseline over
1-2 days.
Major 100mg or 100 mg/m2/dose 50 mg IV Q 8 or 100
(e.g. Septic shock, multiple IV hydrocortisone or mg/m2/day q 6 hours X 24-
trauma/fractures or severe burns, equivalent 48hours. Taper to baseline
severe systemic infections, major over 1-3 days (continue stress
surgery, pancreatitis, orthopedic
dose if the physical stress
surgery including open
(fever or pain) continues).
reduction, spinal fusion, etc.)
DOS - Day of surgery
Patients using high dose twice-weekly corticosteroid-dosing schedule:
If patients using a twice-weekly dosing schedule are unable to take
corticosteroids by mouth during a time when they should be taking
corticosteroids (due to nausea, vomiting, diarrhea, etc.), patients should take
stress doses intravenously as indicated above.
If patients using a twice weekly dosing schedule are undergoing/experiencing a
moderate or major medical/surgical stressor in their life, cortisol level should be
drawn and it is recommended that they follow the stress dosing
recommendations in the above table.
No literature exists for these recommendations. The recommendations are
based on expert opinion and practice.
Recommendation for Corticosteroid Therapy Withdraw:
Below is one recommendation for tapering chronic corticosteroids (generally
managed in an outpatient setting):
Start on a Monday, giving 20-25% lower corticosteroid dose for 2 weeks (or
longer)
If multiple doses are taken, start first to reduce multiple daily doses to a single
morning dose
o Cut the dose 20-25% again for 2 weeks (or longer); continue this
schedule
o Continue until dose is near physiologic dose (3mg/m2/day of prednisone
or 3.6mg/m2/day of Deflazacort)
When near physiologic dose, substitute corticosteroids with short acting form of
corticosteroid or hydrocortisone (12 mg/m2/day of hydrocortisone)
This will also enable the patient to have a supply of hydrocortisone to be used
for stress doses if needed in times of stress after coming off steroids
o Continue to taper off by 20-25% each week (or longer)
o Give every other day for 2 weeks (or longer)
o Stop
o WATCH VERY CAREFULLY FOR SIGNS OF ADRENAL CRISIS (see below)
Alert parents to signs/symptoms of adrenal crisis
If patients have symptoms of adrenal insufficiency during the taper, the steroid
dose prior to the taper should be maintained for longer
IF THE PATIENT HAS A SERIOUS ILLNESS/INJURY DURING THE TAPER, THEY
MAY NEED A STRESS DOSE OF CORTICOSTEROIDS:
Encourage parents to continue to report any serious events until 1 year post-
taper
o The stress doses of hydrocortisone is 30-50 mg/m2/day, or higher, for
major stress (see Table 2)
o Patients need to go to the emergency room if having signs or symptoms
of adrenal crisis. Serum electrolytes with blood glucose and cortisol level
should be obtained.
o Patients should see a pediatric endocrinologist for evaluation of HPA axis
during the process of corticosteroid therapy withdrawal.
Patients using high dose twice-weekly corticosteroid-dosing schedule:
It is recommended that patients electing to discontinue the use of twice weekly
corticosteroids, do so under the guidance of a neuromuscular provider and/or
endocrinologist.
No literature exists for these recommendations. The recommendations are
based on expert opinion and practice
Testing HPA axis:
After reaching half the physiological dose (5-6 mg/m2/day of hydrocortisone or
1-1.5 mg/m2/day of prednisone), morning serum cortisol and ACTH should be
assayed monthly (may do less frequently), until they reach normal levels.
When baseline morning serum ACTH and cortisol are normal, discontinue the
corticosteroid and carry out the rapid ACTH stimulation test monthly until post-
stimulation cortisol response is normal (post-stimulus level > 20 mcg/dL). When
this point is reached, it can be considered that the HPA axis has recovered
Modification of above protocol:
Omit monthly AM cortisol and ACTH and perform an ACTH stimulation test in 3
months after discontinuation of corticosteroids
During this time (3 months before getting ACTH stimulation test), patients will
need to take stress dose at the time of stress
If ACTH stimulation test result is abnormal (peak cortisol <20), patients will need
to continue taking stress doses of hydrocortisone at the time of stress. (Patients
Repeat ACTH stimulation test again in 1-2 months later and families would need
to have teaching on this with an endocrine nurse.)
Alternatively, when laboratory tests cannot be carried out:
Patients who have used corticosteroids for prolonged periods can be considered
as having suppression of the HPA axis up to 1 year after discontinuation of
corticosteroid therapy and therefore need hydrocortisone stress dose coverage
during the time of stress
Risk factors for adrenal crisis include:
Dehydration
Infection and other physical stress
Injury to the adrenal or pituitary gland
Stopping treatment too suddenly with glucocorticoid medications such as
prednisone hydrocortisone
Surgery
Trauma
Symptoms of adrenal crisis can include any of the following:
Abdominal pain
Shock
Confusion or coma
Dehydration
Dizziness or light-headedness
Fatigue
Flank pain
Headache
High fever
Loss of appetite
Loss of consciousness
Low blood pressure
Nausea
Profound weakness
Rapid heart rate
Rapid respiratory rate (see tachypnea)
Slow, sluggish movement
Unusual and excessive sweating on face or palms
Vomiting
Exams and Tests
Tests that may be ordered to help diagnose acute adrenal crisis include:
ACTH (cosyntropin) stimulation test
Cortisol level
Blood sugar
Serum potassium
Serum sodium
Serum pH
Corticosteroid Conversion Table
Table 3
Medication Equivalent doses
Cortisone 25 mg
Hydrocortisone 20 mg
Deflazacort 6 mg
Prednisone 5 mg
Methyl prednisone 4 mg
Triamcinolone 4 mg
Betamethasone 0.75 mg
Dexamethasone 0.75 mg
References
1. Hallman MR, Head DE, Coursin DB, Joffe AM. (2013) When and why should
perioperative glucocorticoid replacement be administered? Evidence-Based
Practice of Anesthesiology. Philadelphia, PA. Elsevier.
2. Marik PE, Varon J. Requirement of perioperative stress doses of corticosteroids.
Arch Surg. 2008;143(12):1222-1226.
3. Kohl BA, Schwartz S. Surgery in the patient with endocrine dysfunction. Med
Clin N Am. 2009;93:1031-1047.
4. Jaffer AK, Grant PJ. Perioperative Medicine: Medical Consultation and
Comanagement. Hoboken, NJ: John Wiley & Sons Inc.;2012
5. 5.Hamrahian AH, Roman S, Milan S. The surgical patient taking
glucocorticoids.In: UpToDate, Martin KA, Collins KA(Ed), UpToDate, Waltham,
MA, 2014.
6. Stewart PM. The adrenal cortex. In: Larsen PR, Kronenberg HM, Melmed S,
Polonsky KS, eds. Williams Textbook of Endocrinology. 10th ed. Philadelphia,
PA: Saunders; 2003:491551
7. Patient/Parent information: Acute adrenal crisis.
http://www.nlm.nih.gov/medlineplus/ency/article/000357.htm
Acknowledgements
St. Vincents Hospital, Indianapolis, IN
Dr. Philip Zeitler, Childrens Hospital Colorado, Aurora, CO
Dr. Sasigarn Bowden, Nationwide Childrens Hospital, Columbus, OH
Dr. Doug Biggar, Holland Bloorview Kids Rehab, Toronto, ON
Dr. Jerry Mendell, Nationwide Childrens Hospital, Columbus, OH
Dr. Anne M. Connolly, St. Louis Childrens Hospital, St. Louis, MO
In honor of the late Philip James PJ Nicholoff, for his contribution to the global
Duchenne community.
You might also like
- Perioperative Steroid GuidelineDocument3 pagesPerioperative Steroid Guidelinebellahunter92No ratings yet
- Guide to Using Steroids in Palliative CareDocument6 pagesGuide to Using Steroids in Palliative CareMariskaNo ratings yet
- TyphoidDocument2 pagesTyphoidFatma HasanNo ratings yet
- 01 - 007 Corticosteroids in DentistryDocument3 pages01 - 007 Corticosteroids in DentistryplsssssNo ratings yet
- Perioperative Corticosteroid Administration: Adel M. Bassily-Marcus, MD - Andrew B. Leibowitz, MDDocument6 pagesPerioperative Corticosteroid Administration: Adel M. Bassily-Marcus, MD - Andrew B. Leibowitz, MDEka NovitasariNo ratings yet
- Methylprenisolone (Medrol)Document15 pagesMethylprenisolone (Medrol)ddandan_2No ratings yet
- Perioperative Medicine:: Management of Chronic SteroidsDocument20 pagesPerioperative Medicine:: Management of Chronic SteroidsGus LionsNo ratings yet
- ADocument1 pageASukmawatiNo ratings yet
- Revision 1Document21 pagesRevision 1NaifmxNo ratings yet
- Steroid Guidelines Summary 2008Document2 pagesSteroid Guidelines Summary 2008Iniya RajendranNo ratings yet
- Glucocorticoid Withdrawal PDFDocument9 pagesGlucocorticoid Withdrawal PDFSérgio HenriqueNo ratings yet
- Management of Gout in AdultsDocument3 pagesManagement of Gout in AdultsZubair Mahmood KamalNo ratings yet
- Aida Protocol For Apl: InductionDocument4 pagesAida Protocol For Apl: InductionGabrielNo ratings yet
- Oral Surgery & Pain Managment 13-14Document175 pagesOral Surgery & Pain Managment 13-14Priya SargunanNo ratings yet
- Nursing ResponsibilitiesDocument4 pagesNursing ResponsibilitiesMaureen Joy Cascayan EspirituNo ratings yet
- Clinical guidelines for corticosteroid use in palliative careDocument5 pagesClinical guidelines for corticosteroid use in palliative careAdia MasooraNo ratings yet
- SteroidDocument26 pagesSteroidzhakaNo ratings yet
- Prescribing Opioids in Renal PatientsDocument5 pagesPrescribing Opioids in Renal PatientsAnonymous 9dVZCnTXSNo ratings yet
- 1.13 Hyper-CVAD-MA Version 2.1Document5 pages1.13 Hyper-CVAD-MA Version 2.1Alina CrissNo ratings yet
- Prescribing Info for Dostinex TabletsDocument9 pagesPrescribing Info for Dostinex TabletsasdwasdNo ratings yet
- Deep Vein ThrombosisDocument22 pagesDeep Vein ThrombosisEznal MahidinNo ratings yet
- Hyper Cvad NHLhiDocument6 pagesHyper Cvad NHLhisevag002816No ratings yet
- Systemic Anti-Infl Ammatory AgentsDocument5 pagesSystemic Anti-Infl Ammatory Agentsbebek sakitNo ratings yet
- Lanoxin (Digoxin)Document3 pagesLanoxin (Digoxin)E100% (5)
- Antiemetic Guidelines For ChemotherapyDocument11 pagesAntiemetic Guidelines For ChemotherapyAaron AntonioNo ratings yet
- L 51 R Hypercvad R MaDocument7 pagesL 51 R Hypercvad R MaMohamed MahmoudNo ratings yet
- Xtampza ER Dosage GuideDocument6 pagesXtampza ER Dosage GuideKolade YousuffNo ratings yet
- Docetaxel - 40mg/ml Injection: InstructionDocument11 pagesDocetaxel - 40mg/ml Injection: InstructionywNo ratings yet
- AIIMS Issues New Guidelines For Treatment of CovidDocument7 pagesAIIMS Issues New Guidelines For Treatment of Covidsenthil kumarNo ratings yet
- 4 SharedDocument11 pages4 Sharedpkgarg_iitkgpNo ratings yet
- PREDNISONEDocument4 pagesPREDNISONECay SevillaNo ratings yet
- Endo PDFDocument16 pagesEndo PDFDanekka TanNo ratings yet
- Discussion 2Document14 pagesDiscussion 2Issa HudencialNo ratings yet
- Class Indications: GentamicinDocument3 pagesClass Indications: GentamicinBer Anne Jaropojop TahilNo ratings yet
- Top 5 Corticosteroids For Use in Emergency SettingsDocument4 pagesTop 5 Corticosteroids For Use in Emergency SettingsIulian Cătălin GrămadăNo ratings yet
- Protocol-010Document12 pagesProtocol-010hatem newishyNo ratings yet
- AIIMS issues new guidelines for treatment of Covid-19 casesDocument7 pagesAIIMS issues new guidelines for treatment of Covid-19 casessenthil kumarNo ratings yet
- Doxorubicin: Mechanism of ActionDocument3 pagesDoxorubicin: Mechanism of ActionGeorge FogNo ratings yet
- Diazepam, Lanoxin, Hemostan, NaprexDocument6 pagesDiazepam, Lanoxin, Hemostan, NaprexRene John Francisco100% (1)
- Cyclosporine PDFDocument6 pagesCyclosporine PDFFazdrah AssyuaraNo ratings yet
- Glucocorticoid Withdrawal - UpToDateDocument7 pagesGlucocorticoid Withdrawal - UpToDateGiancarlos GuzmanNo ratings yet
- Management of Reactions in Leprosy: How Should Lepra Reactions Be Managed?Document2 pagesManagement of Reactions in Leprosy: How Should Lepra Reactions Be Managed?Echa AdityaNo ratings yet
- Stress Steroid Management For Children With Primary or Secondary Adrenal FailureDocument5 pagesStress Steroid Management For Children With Primary or Secondary Adrenal FailureGhada ElhassanNo ratings yet
- Ketamine Infusion For CRPS or Opioid Weaning GuidelineDocument14 pagesKetamine Infusion For CRPS or Opioid Weaning GuidelineAlia SandoQaNo ratings yet
- Dosing of Ivermectin & Other TherapeuticsDocument7 pagesDosing of Ivermectin & Other TherapeuticsTom100% (2)
- Azacitidine V2 4.14Document3 pagesAzacitidine V2 4.14GabrielNo ratings yet
- Management of Status Epilepticus 2022Document8 pagesManagement of Status Epilepticus 2022albert siraitNo ratings yet
- Florinef (Fludrocortisone)Document3 pagesFlorinef (Fludrocortisone)E100% (1)
- What Steroid Supplementation Is Required For A Patient With Primary Adrenal Insufficiency Undergoing A Dental Procedure?Document6 pagesWhat Steroid Supplementation Is Required For A Patient With Primary Adrenal Insufficiency Undergoing A Dental Procedure?AnthonyNo ratings yet
- Ketorolac (Systemic) - Drug Information - UpToDateDocument42 pagesKetorolac (Systemic) - Drug Information - UpToDateJosué Pablo Chicaiza AbadNo ratings yet
- Pediatric Dosage CalculationsDocument5 pagesPediatric Dosage CalculationsLovely Anjenell MacalingaNo ratings yet
- Lanoxin and Digitoxin Drug GuideDocument5 pagesLanoxin and Digitoxin Drug GuideCarson BirthNo ratings yet
- GoutDocument47 pagesGoutsyifasqaNo ratings yet
- Standard Treatment Guidelines - HysterectomyDocument3 pagesStandard Treatment Guidelines - Hysterectomydr_rajatjainNo ratings yet
- Prednisone TabDocument10 pagesPrednisone TabrantiadrianiNo ratings yet
- MEDICAL WARD PHARMACY ASSESSMENTDocument5 pagesMEDICAL WARD PHARMACY ASSESSMENTadilah fazliNo ratings yet
- FACTS: There Is No Cure & Complete: Sustained Remissions Are Rare. Principles of TherapyDocument12 pagesFACTS: There Is No Cure & Complete: Sustained Remissions Are Rare. Principles of TherapyAzizan HannyNo ratings yet
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingFrom EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingNo ratings yet
- A Statistical Inquiry Into the Nature and Treatment of EpilepsyFrom EverandA Statistical Inquiry Into the Nature and Treatment of EpilepsyNo ratings yet
- Nutritional Therapy in Major BurnsDocument6 pagesNutritional Therapy in Major BurnsRuth Danielle GasconNo ratings yet
- Circadian Patterns of ST Elevation Myocardial Infarction in The New MillenniumDocument7 pagesCircadian Patterns of ST Elevation Myocardial Infarction in The New MillenniumYanna RizkiaNo ratings yet
- 10 1001@jama 2017 0059Document2 pages10 1001@jama 2017 0059Fernando GeldresNo ratings yet
- vhrm0204 371Document8 pagesvhrm0204 371Yanna RizkiaNo ratings yet
- HTN PamphletDocument20 pagesHTN PamphletMaria Ivy MendozaNo ratings yet
- sr11 252Document48 pagessr11 252arulrajiv1No ratings yet
- HTN PamphletDocument20 pagesHTN PamphletMaria Ivy MendozaNo ratings yet
- WHO HTM TB 2016.06 EngDocument16 pagesWHO HTM TB 2016.06 EngTammy Utami DewiNo ratings yet
- Tuberculosis Surveillance Monitoring Europe 2018 Rev1 PDFDocument206 pagesTuberculosis Surveillance Monitoring Europe 2018 Rev1 PDFYanna RizkiaNo ratings yet
- Contemporary Diagnosis and Management of Preterm LaborDocument4 pagesContemporary Diagnosis and Management of Preterm LaborYanna RizkiaNo ratings yet
- JNC 8Document14 pagesJNC 8amiwahyuniNo ratings yet
- APA - DSM5 - Level 2 Anxiety Adult PDFDocument3 pagesAPA - DSM5 - Level 2 Anxiety Adult PDFDiana TodeaNo ratings yet
- Routine Newborn Assessment PDFDocument17 pagesRoutine Newborn Assessment PDFYanna RizkiaNo ratings yet
- Hiv WhoDocument480 pagesHiv Whoأبو أويس شرف الدينNo ratings yet
- Tyg AcylDocument30 pagesTyg AcylYanna RizkiaNo ratings yet
- EGDT in Pediatric Septic ShockDocument11 pagesEGDT in Pediatric Septic ShockYanna RizkiaNo ratings yet
- 149 Ipp Jan March 2017 9Document9 pages149 Ipp Jan March 2017 9Yanna RizkiaNo ratings yet
- Srep 45870Document11 pagesSrep 45870Yanna RizkiaNo ratings yet
- Anes CH 32Document12 pagesAnes CH 32Yanna RizkiaNo ratings yet
- Annular Lesions in Dermatology PDFDocument6 pagesAnnular Lesions in Dermatology PDFYanna RizkiaNo ratings yet
- Differences Between Adult and Pediatric Septic ShockDocument7 pagesDifferences Between Adult and Pediatric Septic ShockYanna RizkiaNo ratings yet
- Overview SepsisDocument13 pagesOverview SepsisYanna RizkiaNo ratings yet
- ACC16 ProgramPDF PATH AcuteCoronaryDocument23 pagesACC16 ProgramPDF PATH AcuteCoronaryIsrael de la CruzNo ratings yet
- Understanding the Pathophysiology and Management of SepsisDocument20 pagesUnderstanding the Pathophysiology and Management of Sepsiskartini ciatawiNo ratings yet
- BMJ c4416 FullDocument8 pagesBMJ c4416 FullLukman Al-HafizNo ratings yet
- Biomarkers For Pediatrics Sepsis and Pediatric ShockDocument15 pagesBiomarkers For Pediatrics Sepsis and Pediatric ShockYanna RizkiaNo ratings yet
- Important Considerations For Diagnosing and Managing Sever Pediatric SepsisDocument12 pagesImportant Considerations For Diagnosing and Managing Sever Pediatric SepsisYanna RizkiaNo ratings yet
- Procalcitnonin and CRP in SIRS and SepsisDocument9 pagesProcalcitnonin and CRP in SIRS and SepsisYanna RizkiaNo ratings yet
- Management of Criticalli Ill Child SepsisDocument4 pagesManagement of Criticalli Ill Child SepsisYanna RizkiaNo ratings yet
- Daftar PustakaDocument4 pagesDaftar PustakajhnaidillaNo ratings yet
- College Nursing Exam ReviewDocument8 pagesCollege Nursing Exam ReviewKenneth NovenoNo ratings yet
- Care After Delivery: Postpartum Care: SBA - Presentation 5 (C)Document31 pagesCare After Delivery: Postpartum Care: SBA - Presentation 5 (C)Siva SaranNo ratings yet
- QUIZDocument14 pagesQUIZhahaha0% (1)
- A) Long-Term Follow-Up of Patients With Migrainous Infarction - Accepted and Final Publication From Elsevier1-s2.0-S030384671730344X-mainDocument3 pagesA) Long-Term Follow-Up of Patients With Migrainous Infarction - Accepted and Final Publication From Elsevier1-s2.0-S030384671730344X-mainRodrigo Uribe PachecoNo ratings yet
- IU Vaccine LawsuitDocument55 pagesIU Vaccine LawsuitJoe Hopkins100% (2)
- Pathology Integumentary SystemDocument4 pagesPathology Integumentary SystemMaui GamutanNo ratings yet
- Resume Atiyeh KaboudvandDocument2 pagesResume Atiyeh Kaboudvandarian tejaratNo ratings yet
- Types and Causes of Phobias ExplainedDocument24 pagesTypes and Causes of Phobias ExplainedDebjyoti BanerjeeNo ratings yet
- Li vs Soliman: Informed Consent in Chemotherapy TreatmentDocument7 pagesLi vs Soliman: Informed Consent in Chemotherapy TreatmentLulu VedNo ratings yet
- Lesson 3 BloodDocument50 pagesLesson 3 BloodJulius Memeg PanayoNo ratings yet
- Post Test 19Document4 pagesPost Test 19Naomi VirtudazoNo ratings yet
- Pramipexole Effect on Depressive Symptoms in Parkinson's DiseaseDocument6 pagesPramipexole Effect on Depressive Symptoms in Parkinson's DiseaseCarmen CiursaşNo ratings yet
- Wa0008.Document2 pagesWa0008.Mmangaliso KhumaloNo ratings yet
- Case Study CKD DM Type 2Document7 pagesCase Study CKD DM Type 2Brian Cornel0% (3)
- ComprehensiveDocument4 pagesComprehensiveDeekshitha Turaka0% (1)
- Vascular Diseases: Idar Mappangara Department of Cardiology Hasanuddin UniversityDocument31 pagesVascular Diseases: Idar Mappangara Department of Cardiology Hasanuddin UniversityriniNo ratings yet
- GHC Gut Health Course Syllabus - MKTGDocument23 pagesGHC Gut Health Course Syllabus - MKTGKat HerreraNo ratings yet
- Primary Progressive Aphasia: Neurological ProgressDocument8 pagesPrimary Progressive Aphasia: Neurological ProgressDranmar AhmedNo ratings yet
- Case Pre Ovarian CystDocument56 pagesCase Pre Ovarian Cystthesa1201No ratings yet
- Proteinuria and Chronic Kidney DiseaseDocument34 pagesProteinuria and Chronic Kidney DiseaseВалерий ГаврилуцаNo ratings yet
- Daftar Pustaka BCB BMK BBLC Ikterus NeonatorumDocument3 pagesDaftar Pustaka BCB BMK BBLC Ikterus NeonatorumFitri Nur DiniNo ratings yet
- Triage Process Prioritizes PatientsDocument5 pagesTriage Process Prioritizes PatientsWyen Cabatbat50% (2)
- Nursing Care Plan For "Herniated Nucleus Pulposus Ruptured Inter Vertebral Disc"Document9 pagesNursing Care Plan For "Herniated Nucleus Pulposus Ruptured Inter Vertebral Disc"jhonroks100% (7)
- Price List PT - Thirza 2019Document8 pagesPrice List PT - Thirza 2019Permana JuliansyahNo ratings yet
- Total Abdominal Hysterectomy Bilateral Salpingo OophorectomyDocument3 pagesTotal Abdominal Hysterectomy Bilateral Salpingo OophorectomyLouise BravoNo ratings yet
- RespiratoryDocument18 pagesRespiratoryReneé Camille50% (2)
- Cushing's Disease PathophysiologyDocument3 pagesCushing's Disease PathophysiologyAj MacotoNo ratings yet
- Peppermint: (Mentha Piperita)Document12 pagesPeppermint: (Mentha Piperita)MarjoryStewartBaxter100% (2)
- Schizophrenia Presentation by Dr. MORAHDocument39 pagesSchizophrenia Presentation by Dr. MORAHChikezie OnwukweNo ratings yet