Professional Documents
Culture Documents
VBAC Score
Uploaded by
praburastraCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
VBAC Score
Uploaded by
praburastraCopyright:
Available Formats
LETTERS OBG
MANAGEMENT
Term Breech Trial It should be noted, however, that none of
conclusions challenged the breech deliveries were counted in the sig-
nificant perinatal morbidity and mortality
I read with great
interest The term
breech: vaginal or
cases for that year, unless other obstetric cir-
cumstances were present. Could this indicate
that it is better to wait and see how a patients
cesarean delivery? labor patterns develop before deciding to per-
[January], by Alex form a cesarean? Our impression is that peri-
Vidaeff, MD, Edward natal mortality and morbidity have more to do
Yeomans, MD, Ellen with the way a labor is conducted than the
Mozurkewich, MD, mode of delivery. We propose that further
and Martin Gimovsky, research is needed to establish a safe and stan-
MD, regarding the dard way of supervising a breech labor, and to
Term Breech Trial solve such debatable issues as the use of aug-
(TBT) conducted by Mary E. Hannah. The mentation, epidural analgesia, or premature
studys remarkable scientific design, along interference with the fetus during delivery.
with the work of all those involved, undoubt- GABRIEL BANCEANU, PHD
edly gave significant weight to the conclusion B U C H A R E S T, R O M A N I A
that elective cesarean should be the preferred
mode of delivery for term breech fetuses. Drs. Vidaeff and Yeomans respond:
Our teaching hospital in Romania had the It appears as though Dr. Banceanu feelsas
honor of participating in the TBT. In this we dothat further research on term breech
country, term breech pregnancies with no deliveries is still needed. Selection of appro-
other complications are allowed to undertake priate candidates for vaginal breech delivery
is the first step in the process, and undeni-
ably a very important one. However, as Dr.
Perinatal mortality and morbidity have
Banceanu points out, the management of
more to do with the way a labor is labor and delivery is often critical in deter-
mining outcomes. Unfortunately, this ele-
conducted than the mode of delivery.
ment could not be controlled or adequately
accounted for in the TBT.
a well-supervised trial of labor, and approxi- A recent challenge to the American Col-
mately 60% of these fetuses are delivered vagi- lege of Obstetricians and Gynecologists
nally. But in reviewing the TBT results from (ACOG) endorsement of planned cesarean
our institution, we observed that even in study delivery for breech presentation at term indi-
conditions, only 60% of the patients random- cates to us that obstetricians can still agree to
ized to planned vaginal birth actually deliv- disagree on this subject.1
ered vaginally; the others delivered via cesare-
an due to complications during laborfind- Dr. Mozurkewich responds:
ings consistent with the overall results report- I appreciate Dr. Banceanus comments. It is
ed by the TBT. interesting to note that at his hospital, a trial
C O N T I N U E D
16 OBG MANAGEMENT October 2002
LETTERS C O N T I N U E D
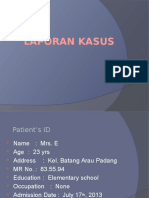
TA B L E 1 trial conditions, the investigators reported
VBAC risk scoring system*, increases in perinatal morbidity and mor-
tality in the planned vaginal birth group.2
SCORE 2 FOR SCORE 1 FOR SCORE 0 FOR
EACH ITEM EACH ITEM EACH ITEM
In addition, the authors performed a sub-
analysis in which subjects were excluded if
Past:
they experienced vaginal breech delivery
1 cesarean 2 cesareans More than 2 cesareans
after prolonged labor, induction or augmen-
2-layer closure 2-layer closure, with 1-layer closure
postoperative fever tation of labor, footling or uncertain breech
Cesarean more than Cesarean 1-2 Cesarean less than presentation at delivery, or if the clinician at
2 years ago years ago 1 year ago delivery was not skilled or experienced. De-
Cesarean not due Cesarean performed Cesarean performed
spite these exclusions, planned cesarean sec-
to CPD due to dystocia due to CPD
Term vaginal birth Premature vaginal No vaginal birth
tion prevailed. For these reasons, I feel the
birth overall conclusions and recommendations
Present: of the TBT are quite robust.
Singleton Twins (both cephalic) Twins (only
first cephalic) REFERENCES
Cephalic Breech Other presentations 1. Hauth JC, Cunningham FG. Vaginal breech delivery is still justified. Obstet
Gynecol. 2002;99:1115-1116.
Fetal weight less Fetal weight Fetal weight
2. Hannah ME, Hannah WJ, Hewson SA, Hodnett ED, Saigal S, Willan AR.
than 3,500 g 3,500-4,500 g above 4,500 g
Planned cesarean section versus planned vaginal birth for breech presentation at
Expect spontaneous Expect labor will Expect labor will term: A randomized multicenter trial. Lancet. 2000;356:1375-1383.
labor need augmentation need to be induced 3. Hannah WJ, Allardice J, Amankwah K, et al. The Canadian consensus on
breech management at term. J SOGC. 1994;16:1839-1858.
Maternal weight Maternal weight Maternal weight
less than 170 lbs 171-250 lbs above 250 lbs
CPD = cephalopelvic disproportion; VBAC = vaginal birth after cesarean
*Low risk: 16-20 points; medium risk: 6-15 points; high risk: 0-5 points Scoring patients for VBAC
Score 0 for each item you cannot document from history.
n VBAC: Safer
of labor did not result in any perinatal deaths
or cases of serious perinatal morbidity among
I than you think
[August], Ellen Mozurkewich,
TBT participants. He suggests that optimal MD, recommends carefully
management of the properly selected breech selecting patients for vaginal
presentation at term may be to allow a trial of delivery after cesarean
labor and to assign mode of delivery based on (VBAC). However, she does
intrapartum progress. However, the planned not offer clear guidelines for
vaginal birth group in the TBT essentially such a selection process. Here
received the same management protocol that at Elmhurst Hospital Center-
Dr. Banceanu describes.2 The guidelines that Mt. Sinai affiliation, we utilize
formed the TBTs protocol for intrapartum a scoring system to identify candidates at low, medi-
management stemmed from a Canadian con- um, and high risk for VBAC (Table 1). While patients
sensus conference on breech presentation at who score from 16 to 20 points are considered low-risk
term and established clear conditions neces- and, therefore, good candidates for VBAC, patients
sary for the continuation of labor trials.3 But who score 0 to 5 points are considered high-risk and
even despite these relatively optimal should never be offered a trial of labor. Medium-risk
C O N T I N U E D
18 OBG MANAGEMENT October 2002
LETTERS C O N T I N U E D
patients, scoring from 6 to 15 points, require
individualized consideration with extensive
counseling.
E. HAKIM-ELAHI, MD
C H I E F O F W O M E N S H E A LT H S E RV I C E S
E L M H U R S T H O S P I TA L C E N T E R
E L M H U R S T, N Y
Dr. Mozurkewich responds:
Thank you, Dr. Hakim-Elahi, for your
comments. To my knowledge, none of the
scoring systems designed to predict failed trial
of labor have proven reliable.
In an assessment of several models,
Macones and colleagues reported a best-
model sensitivity for prediction of failed trial of
labor of 77%, with a specificity of 65%.1 This
means that 35% of women discouraged from
undergoing a trial of labor under this system
would have achieved vaginal delivery. Other
investigators have reported on scoring systems
with similar test characteristics.2,3 In a decision
analysis, Macones suggested that an ideal
system should have both sensitivity and
specificity in excess of 75% in order to obtain
a reasonable trade-off between reduction in
morbidity and the total rate of cesarean
sections.4 In the absence of a validated
scoring system meeting these requirements,
our institution continues to select and counsel
candidates for trial of labor according to
published ACOG guidelines.5
REFERENCES
1. Macones GA, Hausman N, Edelstein R, Stamilio DM, Marder SJ. Predicting out-
comes of trials of labor in women attempting vaginal birth after cesarean delivery:
A comparison of multivariate methods with neural networks. Am J Obstet Gynecol.
2001;184:409-413.
2. Flamm B, Geiger A. Vaginal birth after cesarean delivery: An admission scoring
system. Obstet Gynecol. 1997;90:907-910.
3. Weinstein D, Benshushan A, Tanos V, Zilberstein R. Predictive score for vaginal
birth after cesarean section. Am J Obstet Gynecol. 1996;174:192-198.
4. Macones GA. The utility of clinical tests of eligibility for a trial of labor following
cesarean section: A decision analysis. BJOG. 1999;106:642-646.
5. American College of Obstetricians and Gynecologists. Vaginal birth after previous
cesarean delivery. Practice bulletin #5. Washington, DC: ACOG;1999.
October 2002 OBG MANAGEMENT 21
You might also like
- Maternal and Fetal Outcomes in Patients With Previous Caesarean Section Undergoing Trial of Vaginal BirthDocument14 pagesMaternal and Fetal Outcomes in Patients With Previous Caesarean Section Undergoing Trial of Vaginal BirthIJAR JOURNALNo ratings yet
- VBACDocument8 pagesVBACKukuh PrasetyoNo ratings yet
- Epidural Analgesia in Mothers Undergoing Trial of Vaginal Birth After Previous Cesarean Section: A Prospective StudyDocument7 pagesEpidural Analgesia in Mothers Undergoing Trial of Vaginal Birth After Previous Cesarean Section: A Prospective StudySANo ratings yet
- Mode of Delivery of Twins: Andrew Breeze, Gordon SmithDocument5 pagesMode of Delivery of Twins: Andrew Breeze, Gordon SmithHarvey alvin HartonoNo ratings yet
- SOGC Clinical Practice Guideline on Vaginal Delivery of Breech PresentationDocument10 pagesSOGC Clinical Practice Guideline on Vaginal Delivery of Breech PresentationVanessa MacarioNo ratings yet
- Client Initials: Medical Diagnosis: Cephalopelvic Disproportion Eu DEFINITION: The RelationshipDocument2 pagesClient Initials: Medical Diagnosis: Cephalopelvic Disproportion Eu DEFINITION: The RelationshipLyssa Monique67% (3)
- Infant Outcome After Complete Uterine RuptureDocument8 pagesInfant Outcome After Complete Uterine RuptureHeiddy Ch SumampouwNo ratings yet
- Vaginal Birth After Caeserean Section: BY Seun ODocument24 pagesVaginal Birth After Caeserean Section: BY Seun OOlaiya OluwaseunNo ratings yet
- Iams 2011Document6 pagesIams 20118jxfv2gc5tNo ratings yet
- Views of maternity staff on promoting vaginal birth after caesareanDocument57 pagesViews of maternity staff on promoting vaginal birth after caesareanBagusHibridaNo ratings yet
- E002803 FullDocument7 pagesE002803 FullAzrul MDNo ratings yet
- Educational Topic 32: Obstetric Procedures: U 2: O S C: PDocument4 pagesEducational Topic 32: Obstetric Procedures: U 2: O S C: PStetho LoveNo ratings yet
- Gestational Diabetes Induction of LaborDocument13 pagesGestational Diabetes Induction of LaborRalph AlbertoNo ratings yet
- Optimal Timing for Cesarean Delivery in Women with Multiple CesareansDocument10 pagesOptimal Timing for Cesarean Delivery in Women with Multiple CesareansNica Joy DesquitadoNo ratings yet
- MALPRESENTATIONDocument13 pagesMALPRESENTATIONLady Jane CaguladaNo ratings yet
- Term Breech TrialDocument9 pagesTerm Breech TrialAndy Tan Wei KeatNo ratings yet
- Embarazo Prolongado PDFDocument5 pagesEmbarazo Prolongado PDFGLORIA ANDREA ORJUELA FLOREZNo ratings yet
- Ultrasound Evaluation of Uterine Scar After Cesarean Section and Next BirthDocument4 pagesUltrasound Evaluation of Uterine Scar After Cesarean Section and Next BirthSyifarNo ratings yet
- Ectopic Pregnancy: A ReviewDocument13 pagesEctopic Pregnancy: A ReviewDinorah MarcelaNo ratings yet
- (Augmentation) Medical and SurgicalDocument17 pages(Augmentation) Medical and SurgicalNadiya RashidNo ratings yet
- To Vbac or Not To Vbac: PerspectiveDocument3 pagesTo Vbac or Not To Vbac: Perspectiveharani roimaNo ratings yet
- Intrauterine Fetal TransfusionsDocument10 pagesIntrauterine Fetal TransfusionsSaddam FuadNo ratings yet
- Factors Associated With Successful Vaginal Birth After Cesarean Section and Outcomes in Rural Area of AnatoliaDocument5 pagesFactors Associated With Successful Vaginal Birth After Cesarean Section and Outcomes in Rural Area of AnatoliaVindee VictoryNo ratings yet
- Beyond The Breech Trial. Maggie BanksDocument4 pagesBeyond The Breech Trial. Maggie Bankspurpleanvil100% (2)
- Emergency Delivery and Peripartum EmergenciesDocument20 pagesEmergency Delivery and Peripartum EmergenciesRocky PangerapanNo ratings yet
- The Role of Labor Induction in Modern ObstetricsDocument7 pagesThe Role of Labor Induction in Modern ObstetricsKevin Stanley HalimNo ratings yet
- Can Pre Eclampsia Explain Higher Cesarean Rates in The Different Groups of Robson's Classification?Document6 pagesCan Pre Eclampsia Explain Higher Cesarean Rates in The Different Groups of Robson's Classification?Mariana HernandezNo ratings yet
- Laasch and PuschekDocument4 pagesLaasch and PuschekShobhit SwarankarNo ratings yet
- 0714 Obg Manuck PDFDocument9 pages0714 Obg Manuck PDFKeeranmayeeishraNo ratings yet
- 2008 Sagittal Suture Overlap in Cephalopelvic DisproportionDocument7 pages2008 Sagittal Suture Overlap in Cephalopelvic DisproportionayupurnamasariiNo ratings yet
- Mode of Delivery of Twin Gestation With Very Low Birthweight: Is Vaginal Delivery SafeDocument8 pagesMode of Delivery of Twin Gestation With Very Low Birthweight: Is Vaginal Delivery SafeaetpbgNo ratings yet
- 10 Recommendation SC-SibaiDocument5 pages10 Recommendation SC-SibaiHervi LaksariNo ratings yet
- Forgotten Transvaginal Cervical Cerclage Stitch in First Pregnancy Benefits Reaped Till The Second PregnancyDocument2 pagesForgotten Transvaginal Cervical Cerclage Stitch in First Pregnancy Benefits Reaped Till The Second PregnancyAna AdamNo ratings yet
- Latent Phase of LaborDocument8 pagesLatent Phase of LaborKevin SNo ratings yet
- POGS PB Dystocia Sept 2022Document6 pagesPOGS PB Dystocia Sept 2022John Piox Badiang100% (1)
- Aogs 14255Document6 pagesAogs 14255Christian YzaguirreNo ratings yet
- persistent occiput posteriorDocument15 pagespersistent occiput posteriorm8wyb2f6ngNo ratings yet
- Induccion Del Parto Basado en La EvidenciaDocument11 pagesInduccion Del Parto Basado en La EvidenciaFredy Dante Zegarra VásquezNo ratings yet
- Breech Presentation - CGDocument13 pagesBreech Presentation - CGJun MingNo ratings yet
- Rupture of The Cervix During Pregnancy After Cervical Pessary Insertion For Preventing Preterm BirthDocument4 pagesRupture of The Cervix During Pregnancy After Cervical Pessary Insertion For Preventing Preterm BirthNuril AzizahNo ratings yet
- 0091-2182 2885 2990126-0 PDFDocument1 page0091-2182 2885 2990126-0 PDFParahmitaNo ratings yet
- Second-Stage Labor: How Long Is Too Long?: ObstetricsDocument6 pagesSecond-Stage Labor: How Long Is Too Long?: ObstetricsKhoti JahNo ratings yet
- Defining Failed Induction of LaborDocument10 pagesDefining Failed Induction of LaborOktaviani Dewi RatihNo ratings yet
- Term Alive Intra Abdominal Ectopic Pregnancy: Case ReportDocument3 pagesTerm Alive Intra Abdominal Ectopic Pregnancy: Case ReportLeannarys Mendoza DelgadoNo ratings yet
- Factors Associated With Successful Vaginal Birth After Cesarean Section and Outcomes in Rural Area of AnatoliaDocument8 pagesFactors Associated With Successful Vaginal Birth After Cesarean Section and Outcomes in Rural Area of AnatoliaIllona SaharaNo ratings yet
- Ajog 2Document6 pagesAjog 2Coc OfclansNo ratings yet
- Clinical Evaluation of Labor: An Evidence-Based ApproachDocument13 pagesClinical Evaluation of Labor: An Evidence-Based ApproachAlejandro Abarca VargasNo ratings yet
- Case 29a: Placenta PreviaDocument12 pagesCase 29a: Placenta PreviaLuis PadillaNo ratings yet
- Nclex Pregnancy ComplicationsDocument6 pagesNclex Pregnancy Complicationsvienny kayeNo ratings yet
- Normal Vaginal Delivery at Term After Expectant Management of Heterotopic Caesarean Scar Pregnancy: A Case ReportDocument3 pagesNormal Vaginal Delivery at Term After Expectant Management of Heterotopic Caesarean Scar Pregnancy: A Case Reportdiaaabdallah209No ratings yet
- NCP Alterations in Normal LaborDocument9 pagesNCP Alterations in Normal LaborCameron De GuzmanNo ratings yet
- Double Foley Catheter For Labor Induction - An Alternative MethodDocument9 pagesDouble Foley Catheter For Labor Induction - An Alternative Methodgrace liwantoNo ratings yet
- 3195 12163 1 PBDocument5 pages3195 12163 1 PBTiAs TiAriyahNo ratings yet
- Caesarean Scar Pregnancy. Diagnosis, Natural History and Treatment (Curr Opin Obstet Gynecol - Oct 2022)Document8 pagesCaesarean Scar Pregnancy. Diagnosis, Natural History and Treatment (Curr Opin Obstet Gynecol - Oct 2022)garomeros5366No ratings yet
- Diminished Ovarian Reserve and Assisted Reproductive Technologies: Current Research and Clinical ManagementFrom EverandDiminished Ovarian Reserve and Assisted Reproductive Technologies: Current Research and Clinical ManagementOrhan BukulmezNo ratings yet
- Absolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationFrom EverandAbsolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationNo ratings yet
- Pregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsFrom EverandPregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsNo ratings yet
- On Autumn's Wing, A Story of Birth Trauma, Brain Injury and Miracles.From EverandOn Autumn's Wing, A Story of Birth Trauma, Brain Injury and Miracles.No ratings yet
- Labor MechanismDocument33 pagesLabor MechanismPratama IkoNo ratings yet
- ALODocument30 pagesALOpraburastraNo ratings yet
- ObgynDocument36 pagesObgynpraburastraNo ratings yet
- Bekas SCDocument16 pagesBekas SCpraburastraNo ratings yet
- Bekas SC 3xDocument22 pagesBekas SC 3xpraburastraNo ratings yet
- PRMDocument22 pagesPRMpraburastraNo ratings yet
- Ekstirpasi Myoma Geburt + Kuretase HP GynDocument22 pagesEkstirpasi Myoma Geburt + Kuretase HP GynpraburastraNo ratings yet
- 2012 Karshaniya YavaguDocument4 pages2012 Karshaniya YavaguRANJEET SAWANTNo ratings yet
- Prostaglandins: An Overview of Structure and FunctionDocument33 pagesProstaglandins: An Overview of Structure and FunctionMuhammad JamalNo ratings yet
- PrimaquineDocument3 pagesPrimaquineVijayakumar NsNo ratings yet
- History of HIVDocument4 pagesHistory of HIVHyrum KamandeNo ratings yet
- UAS Genap Semester II Kebidanan STIKES HafshawatyDocument3 pagesUAS Genap Semester II Kebidanan STIKES HafshawatyHanna HannaNo ratings yet
- Theory and Practice of Pure Tone Audiometry - PTADocument12 pagesTheory and Practice of Pure Tone Audiometry - PTAsolhazNo ratings yet
- CNA Chapter 1 & 2 TermsDocument1 pageCNA Chapter 1 & 2 TermsMarina ChakarNo ratings yet
- Past PapaersDocument515 pagesPast PapaersShariq ShaNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakaNurfauziyahNo ratings yet
- Medication To Manage Abortion and MiscarriageDocument8 pagesMedication To Manage Abortion and MiscarriageNisaNo ratings yet
- Diet PlanDocument6 pagesDiet Plantrical27 tricalNo ratings yet
- Elevated BilirubinDocument5 pagesElevated BilirubinNovita ApramadhaNo ratings yet
- Resume - Viroja Sweta For PortfolioDocument1 pageResume - Viroja Sweta For Portfolioapi-608195339No ratings yet
- Review of Literature on Rabies Prevention and ControlDocument24 pagesReview of Literature on Rabies Prevention and ControlBeah Claudette AbundoNo ratings yet
- FESS ComplicationsDocument17 pagesFESS ComplicationsJoe NumberNo ratings yet
- Fetal risks of macrosomia in diabetic pregnanciesDocument27 pagesFetal risks of macrosomia in diabetic pregnanciesIful SaifullahNo ratings yet
- Drug Study - Nifedipine PODocument1 pageDrug Study - Nifedipine POJet BautistaNo ratings yet
- FormsDocument15 pagesFormsBiswajit DasNo ratings yet
- Medical Assessment Form Blank-1Document4 pagesMedical Assessment Form Blank-1Zakiya HassanNo ratings yet
- Safe SexDocument11 pagesSafe SexnathanNo ratings yet
- Volume 43, Number 12, March 23, 2012Document56 pagesVolume 43, Number 12, March 23, 2012BladeNo ratings yet
- Clinical Biochemistry ReviewDocument10 pagesClinical Biochemistry Reviewyaykatai100% (2)
- Feline Asthma: Laura A. Nafe, DVM, MS, Dacvim (Saim)Document5 pagesFeline Asthma: Laura A. Nafe, DVM, MS, Dacvim (Saim)Miruna ChiriacNo ratings yet
- 6 5 Nerves Hormones and HomeostasisDocument19 pages6 5 Nerves Hormones and Homeostasisapi-235355872No ratings yet
- Aula 1Document14 pagesAula 1Brigida Cirqueira GuimaraesNo ratings yet
- Evaluation of Fetal HeartDocument59 pagesEvaluation of Fetal Heartاد ريما البدر100% (3)
- Urinary System Disorders Practice Quiz #1 (50 Questions)Document26 pagesUrinary System Disorders Practice Quiz #1 (50 Questions)Emy TandinganNo ratings yet
- Mgi Presentation - ReyDocument65 pagesMgi Presentation - ReyCharlot Jade Paderes67% (3)
- Remote Area Nursing Emergency GuidelinesDocument325 pagesRemote Area Nursing Emergency Guidelineslavinia_dobrescu_1No ratings yet
- Conscious Sedation PaediatricsDocument44 pagesConscious Sedation PaediatricsReeta TaxakNo ratings yet