Professional Documents
Culture Documents
Tschanz Et Al Mmna and Nps-Final - Landscape
Uploaded by
api-362872552Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tschanz Et Al Mmna and Nps-Final - Landscape
Uploaded by
api-362872552Copyright:
Available Formats
Indicators of Nutritional Status Predict Neuropsychiatric Symptoms in Dementia
The Cache County Dementia Progression Study
J Tschanz1, C Sanders1, H Wengreen1, S Schwartz1, S Behrens, C Corcoran1, C Lyketsos2 and The Cache County Investigators
1Utah State University, Logan, UT; 2The Johns Hopkins University, Baltimore, MD
Measures: MMNA Predicts Neuropsychiatric Symptoms and Symptom Clusters:
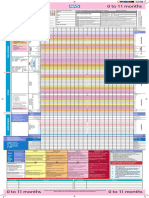
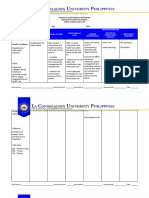
Abstract Nutritional status Figure 1 - Neuropsychiatric Symptoms
30" 30"
Background. Neuropsychiatric
symptoms
(NPS)
are
common
in
demen6a
and
are
associated
Modified Mini Nutritional Assessment (mMNA) was adapted from the Mini Malnourished"
Malnourished"
At"Risk"for"Malnutri:on"
At"Risk"for"Malnutri:on"
with
worse
pa6ent
outcomes
and
caregiver
stress.
Persons
with
demen6a
are
also
at
greater
risk
Nutritional Assessment8 (MNA), a well-established assessment of nutritional 25"
25"
Well"Nourished"
Well"Nourished"
for
malnutri6on.
Using
a
popula6on-based
sample,
we
examined
the
associa6on
between
status in older adults.
NPI Total Score
20"
indicators of nutri6onal status and course of NPS in demen6a. Figure 1 shows the association
Methods. 257 individuals with demen6a (72% Alzheimers disease, 54% female) were followed mMNA excluded items associated with severity of dementia (presence of 20"
severe dementia), neuropsychiatric status (e.g., depression) and subjective 15" between nutritional status and NPS for
annually
for
up
to
6.5
years.
Mean(SD)
age
was
86(5.35).
Nutri6onal
status
was
assessed
using
a
those who are well-nourished, at risk
modied
Mini-Nutri6onal
Assessment
(mMNA)
and
NPS
via
the
12-domain
Neuropsychiatric
report of nutritional status. New threshold values (22 pt max): 15"
<12.5=malnourished, 13-17.5= risk for malnutrition, 17.5=well-nourished.
10" for malnutrition and malnourished.
Inventory (NPI-12). Cluster scores were calculated by summing domains for depression, anxiety
10"
and irritability (Aec6ve) and hallucina6ons and delusions (Psychosis); Agita6on and Apathy were Neuropsychiatric status 5"
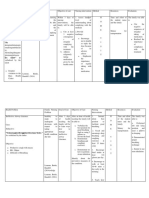
Figures 2a and 2b display a similar
single domains. Linear mixed models tested the associa6on between nutri6onal status (mMNA
Neuropsychiatric inventory (NPI) assessed hallucinations, delusions, anxiety, 5" association for specific NPS symptom
total score or clinical groups of malnourished, risk for malnutri6on, and well-nourished, 13%, 37% 0"
and
50%
at
baseline,
respec6vely),
and
total
NPI-12
score
and
the
four
symptom
clusters.
Also
depression, apathy, agitation/aggression, irritability, aberrant motor behavior, 0" 1" 2" 3" 4" 5" 6" clusters for selected mMNA scores.
Years
from
Baseline
examined
were
mMNA
component
scores
as
predictors
of
total
NPI.
Covariates
tested
included
disinhibition, euphoria, sleep and appetite. Max total = 144 pts. 0"
0" 1" 2" 3" 4" 5" 6"
demographics,
place
of
residence,
demen6a
type,
age
of
demen6a
onset
and
dura6on,
caregiver
Figure
2a
-
Psychosis
35" Figure
2b
-
Apathy
co-residency
and
APOE
genotype.
NPS cluster scores: Affective (sum of depression, anxiety and irritability for max
4.5" 8" mMNA"="5"
Results. Total
NPI-12
scores
increased
over
6me
(1.3
points/year).
In
mul6variable
models,
higher
36 pts); Psychosis (sum of hallucinations and delusions for max 24 pts); Agitation 4"
30"
mMNA"="12"
7" mMNA"="5"
mMNA
score
was
associated
with
lower
total
NPI-12
score
(B=-1.2;
SE=.15).
Malnourished
persons
(max 12 pts), and Apathy (max 12 pts). 3.5"
25"
mMNA"="20"
mMNA"="12"
6"
NPI Cluster Score
(B=8.10; SE=1.37) and those at risk for malnutri6on (B=3.09; SE=0.91) had worse NPS-12 scores Statistical Modeling:
3" 20"
5"
mMNA"="20"
compared
to
well-nourished
par6cipants.
Higher
mMNA
scores
were
associated
with
lower
2.5"
15"
"mMNA"="5""
4"
Aec6ve
(B=-.09;
SE=.05),
Psychosis
(B=-.09;
SE=0.04),
and
Apathy
(B=-.19;
SE=0.05)
cluster
scores.
Linear mixed models (random intercepts and slopes) tested the following: 2" "mMNA"="12""
3"
1.5" 10" mMNA"="20"
MMNA
components
associated
with
greater
NPS
were
a
decline
in
food
intake
(B=2.35;
SE=.51),
Total mMNA score or clinical groups of malnourished, risk for malnutrition, 1" 2"
some
weight
loss
(B=7.36;
SE=1.24),
being
bed/chair
bound
(B=6.64;
SE=1.59),
limited
mobility
5"
and well-nourished and total NPI-12 score. 0.5" 1"
(B=2.68;
SE=.99)
and
lower
dairy
intake
(B=2.63;
SE=1.65),
though
over
6me,
higher
dairy
intake
0" 0"
0"
was
associated
with
increasing
NPS
(B=1.82;
SE=.89).
mMNA component scores and total NPI-12 score. 0" 1" 2" 3" 4" 5" 6" 0"
0"
1"
1"
2"
2"
3"
3"
4"
4"
5"
5" 6"
6"
Conclusions. Nutri6onal
status
is
associated
with
NPS
in
demen6a.
A
decline
in
food
intake,
Years
from
Baseline
weight
loss
and
limited
mobility
are
risk
factors
and
may
signal
the
need
for
interven6on.
Covariates: demographics, place of residence, dementia type, age of
Addressing
nutri6onal
deciencies
may
reduce
the
occurrence
and
severity
of
NPS.
dementia onset and duration, caregiver co-residence, and APOE genotype. Conclusions
Results We extend prior work demonstrating the association of nutritional status in the
Introduction Sample Characteristics: progression of cognitive and functional impairment in dementia, but now in
predicting more severe NPS and affective, psychotic and apathy symptom
Malnutrition is characterized by poor appetite, insufficient caloric intake, 257 persons with dementia (72% AD) with mean (sd) age of 86.0 (5.4), clusters; results were robust to controlling for dementia onset, duration, caregiver
weight loss and low muscle mass and is a recognized problem among older education of 13.3 (3.0) yrs. Baseline characteristics are below. co-residence and APOE genotype.
! Males!(118)! Females!(139)! Total!(257)!
adults and in persons with dementia1. Decline in food intake, weight loss and mobility should be monitored over the
Dementia!Duration!(M,!SD)! 2.97!(1.52)! 3.87!(2.09)**! 3.46!(1.90)!
Nutritional status declines over the course of dementia1 and poorer nutritional mMNA!Total!Score!(M,!SD)! 17.29!(2.69)! 15.90!(3.04**! 16.54!(2.96)! course of dementia and may signal the need for intervention.
mMNA!Groups!(N,!%)! ! ! !
status is associated with cognitive2,3 and functional decline3,4, and the !!!!!Malnourished! 11!(9)! 23!(17)**! 34!(13)! The results identify a potentially important modifiable factor that may reduce
occurrence of neuropsychiatric symptoms (NPS)3,5. !!!!!AtIrisk!for!Malnutrition! 31!(26)! 63!(45)**! 94!(37)! the occurrence and severity of NPS.
!!!!!WellInourished! 76!(65)! 53!(38)**! 129!(50)!
The majority of studies to date have examined nutritional status and dementia
progression in clinical samples with limited follow-up times.
Clinical!Dementia!Rating1!(M,!SD)!
MiniIMental!State!Exam!(M,!SD)!
1.21!(0.52)!
21.35!(5.99)!
1.42!(0.66)*!
19.76!(7.41)!
1.32!(0.61)!
20.50!(6.82)!
Citations
1. Cortex et al., 2008 Alz & Dem 2008 4:22-9.
NPI!Total!Score!(M,!SD)! 10.48!(11.47)! 12.92!(10.85)! 11.77!(11.19)!
We examined the association between indicators of nutritional status and NPI!Cluster!Scores!(M,!SD)! ! ! !
2. Vellas, B., Lauque, S., Gillette-Guyonnet, S., Andrieu, S., Cortes, F., Nourhashmi, F., Grandjean H. (2005). Impact
of nutritional status on the evolution of Alzheimer's disease and on response to acetylcholinesterase inhibitor
neuropsychiatric symptoms in a population based sample of persons with !!!!!Psychosis!(max!pts!=!24)! 1.04!(2.84)! 1.56!(3.04)! 1.33!(2.96)! treatment. J Nutr Health Aging, 9(2), 75-80.
dementia. !!!!!Affective!(max!pts!=!36)! 2.72!(3.75)! 3.78!(4.19)*! 3.30!(4.02)! 3. Guerin, O., Soto, M.E., Brocker, P., Robert, P.H., Benoit, M., & Vellas, B. Nutritional status assessment during
!!!!!Agitation/Aggr!(max!pts!=!12)! 0.69!(1.87)! 0.83!(1.76)! 0.77!(1.81)! Alzheimer's disease: results after one year (the REAL French Study Group). (2005). J Nutr Health Aging, 9(2), 81-4.
4. Saragat, B., Buffa, R., Mereu, E., Succa, V., Cabras, S., Mereu, R.M., Marini, E.. (2012). Nutritional and psycho-
Methods !!!!!Apathy!(max!pts!=!12)!
!
2.03!(3.27)! 2.31!(3.34)! 2.18!(3.31)!
functional status in elderly patients with Alzheimer's disease. J Nutr Health Aging, 16(3), 231-6.
Higher mMNA was associated with lower total NPI-12 (B=-1.2; SE = .15). The Mal- 5. Spaccavento, S., Del Prete, M., Craca, A., & Fiore, P. (2009). Influence of nutritional status on cognitive, functional
Participants: and neuropsychiatric deficits in Alzheimer's disease. Arch Gerontol Geriatr, 48(3), 356-60. doi:10.1016/j.archger.
nourished (B=8.10; SE=1.37) and those at risk for malnutrition (B=3.09; SE = 0.91) had 2008.03.002.
Persons with incident dementia diagnosed in the Cache County Memory worse NPS versus the well-nourished. There was no effect on rate of change in NPS. 6. Breitner, J.C., Wyse, B.W., Anthony, J.C., et al. APOE-epsilon4 count predicts age when prevalence of AD
increases, then declines: the Cache County Study. Neurology, 1999; 53: 321-331.
Study6 were enrolled in the Dementia Progression Study7 (DPS), a population- 7. Tschanz, J.T., Corcoran, C., Schwartz, S., et al. Progression in Cognition, Function and Neuropsychiatric Symptoms
Higher mMNA scores were associated with lower Affective (B=-.09; SE = .05),
based study of the course of dementia and modifying factors. in a Population Cohort with Alzheimers Dementia. The Cache County Dementia Progression Study. Am J Geriat
Psychosis (B=-.-9; SE = 0.04) and Apathy (B=-.19; SE = .05) scores. There was no Psychiatry, 2011;19:532-42.
8. Guigoz, Y., Vellas, B., & Garry, P.J. (1994). Mini Nutritional Assessment: A Practical Assessment Tool for Grading the
Procedures: effect on rate of change in NPS clusters. Nutritional State of Elderly Patients. In B. J. Vellas, Y. Guigoz, P. J. Garry & J. L. Albarede (Eds.), Facts and Research
in Gerontology (15-59). U.S.A.: Springer Publishing Company.
DPS researchers visited participants and caregivers approximately every 6 Decline in food intake (B=2.35; SE = .51), weight loss (B=7.36; SE = 1.24), bed/chair 9. Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). Mini-mental state: A practical method for grading the
months, collecting information on neuropsychiatric symptoms (NPS), and bound (B=6.64; SE = 1.59), limited mobility (B=-2.68; SE = .99) and lower dairy intake cognitive state of patients for the clinician. Journal Of Psychiatric Research, 12(3), 189-198. doi:
10.1016/0022-3956(75)90026-6
cognitive and functional status. Nutritional status was assessed annually and (B=2.63, SE = .1.65) were associated with higher NPS. 10. Hughes CP, Berg L, Danziger WL, Coben L, Martin R. (1982). A new clinical scale for the staging of dementia. The
data from these visits were used for up to 7 years from baseline. British journal of psychiatry. 1982;140:566572.
Over time, higher dairy intake (B=1.82; SE=.89) was associated with worse NPS. ***Supported by NIA grants R01AG21136 & R01AG11380***
You might also like
- LCUP Family Nursing Care Plan AsthmaDocument3 pagesLCUP Family Nursing Care Plan AsthmaKia MadineNo ratings yet
- FNCPDocument4 pagesFNCPVincent GuillanoNo ratings yet
- Adverse Events and Their Contributors Among Older Adults During Skilled Nursing Stays For Rehabilitation: A Scoping ReviewDocument16 pagesAdverse Events and Their Contributors Among Older Adults During Skilled Nursing Stays For Rehabilitation: A Scoping Reviewfebbywahyunitaa kasimNo ratings yet
- CHN LandscapeDocument17 pagesCHN LandscapenicanicsraakinNo ratings yet
- Effects of Peer-Led Interventions For Patients With Cancer: A Meta-AnalysisDocument23 pagesEffects of Peer-Led Interventions For Patients With Cancer: A Meta-AnalysisMuthya GhitaNo ratings yet
- Novilyn C. Pataray BSN - Ii Aids: St. Paul College of Ilocos SurDocument1 pageNovilyn C. Pataray BSN - Ii Aids: St. Paul College of Ilocos SurCharina AubreyNo ratings yet
- Effects of Risperidone On Social and Memory Deficits in An Animal Model of Autism.Document1 pageEffects of Risperidone On Social and Memory Deficits in An Animal Model of Autism.Mara HabashNo ratings yet
- Evidence Based Therapies For Mood DisordersDocument34 pagesEvidence Based Therapies For Mood DisordersNaisargi SoniNo ratings yet
- LCUP Family Nursing Care Plan Format 2023Document2 pagesLCUP Family Nursing Care Plan Format 2023Kia MadineNo ratings yet
- Computation and FNCPDocument3 pagesComputation and FNCPWinnie AriolaNo ratings yet
- A Guide To Sudoscan NewDocument7 pagesA Guide To Sudoscan NewLaura B. BautistaNo ratings yet
- Mini-Mental State Examination (MMSE) - MedWorks MediaDocument4 pagesMini-Mental State Examination (MMSE) - MedWorks MediaemergencyNo ratings yet
- Evidence Based PracticeDocument6 pagesEvidence Based PracticeNazir AhmedNo ratings yet
- FNCP TemplateDocument8 pagesFNCP TemplateMary Ann Sambo OgoyNo ratings yet
- The Selfmedication Hypothesis of Addictive Disorders Focus On He 1985Document6 pagesThe Selfmedication Hypothesis of Addictive Disorders Focus On He 1985BrujoucmNo ratings yet
- Drug Study BipolarDocument13 pagesDrug Study BipolarrahimsyusophNo ratings yet
- Eating Disorders Hope Despite Mortal RiskDocument3 pagesEating Disorders Hope Despite Mortal RiskElizabet BravoNo ratings yet
- Gender and DevelopmentDocument68 pagesGender and Developmentyan deeNo ratings yet
- Plans Section 4 - Google DriveDocument1 pagePlans Section 4 - Google Driveroofyosama2030No ratings yet
- Atypical Depression Current PerspectivesDocument10 pagesAtypical Depression Current PerspectivesIgnacioJoséCalderónPérezNo ratings yet
- Life Chart Methodology For Bipolar Disorder: ManiaDocument1 pageLife Chart Methodology For Bipolar Disorder: ManiaAmaury RoblesNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Planning Intervention EvaluationDocument10 pagesNursing Care Plan: Assessment Diagnosis Planning Intervention EvaluationJalene AdanNo ratings yet
- Pankepp - Affective Neuroscientific Approaches To Depression and AddictionDocument9 pagesPankepp - Affective Neuroscientific Approaches To Depression and AddictionPsiquiatria Clinica ProyectarteNo ratings yet
- St. Paul University Philippines: School of Nursing and Allied Health Sciences College of NursingDocument4 pagesSt. Paul University Philippines: School of Nursing and Allied Health Sciences College of NursingChristian UmosoNo ratings yet
- Nursing Care Plan: Objective: Admission DiagnosisDocument4 pagesNursing Care Plan: Objective: Admission DiagnosisJe ZalNo ratings yet
- Unintended Pregnancy and DepressionDocument8 pagesUnintended Pregnancy and DepressionMeera Al AliNo ratings yet
- LCUP Family Nursing Care Plan (Hypertension)Document4 pagesLCUP Family Nursing Care Plan (Hypertension)Kia MadineNo ratings yet
- Family Nursing Care Plan (Hypertension)Document4 pagesFamily Nursing Care Plan (Hypertension)KANT JAMES D. MAHANNo ratings yet
- Resources-Assessment Tools 0Document10 pagesResources-Assessment Tools 0ib pkNo ratings yet
- Fuente 1Document8 pagesFuente 1Jaque RANo ratings yet
- Pews Observation and Escalation Chart 0 11 Months UpdatedDocument1 pagePews Observation and Escalation Chart 0 11 Months Updatedanitn2020No ratings yet
- Intervention Plan Fernandez, Marvel Jazzreal Bauzon, Dianne Health Problem Cues Family Nursing Problems Goal of Care Objectives Interven Tion PlanDocument4 pagesIntervention Plan Fernandez, Marvel Jazzreal Bauzon, Dianne Health Problem Cues Family Nursing Problems Goal of Care Objectives Interven Tion PlanMarvel JazzrealNo ratings yet
- Texas Health Steps Periodicity ScheduleDocument2 pagesTexas Health Steps Periodicity ScheduleLujain Al OmariNo ratings yet
- Psychological Distress Amongst Health Workers and The General Public During The COVID-19 Pandemic in Saudi Arabia (Kuesioner CPDI)Document10 pagesPsychological Distress Amongst Health Workers and The General Public During The COVID-19 Pandemic in Saudi Arabia (Kuesioner CPDI)Febri YolandaNo ratings yet
- Books and Other Media Livres Et Autres DocumentsDocument1 pageBooks and Other Media Livres Et Autres DocumentsElena ElenaaNo ratings yet
- Spector, Hebditch, Stoner & Gibbor 2016Document10 pagesSpector, Hebditch, Stoner & Gibbor 2016CLNo ratings yet
- NCPDocument5 pagesNCPLouise GumilaNo ratings yet
- 433 Psychiatry Team Child PsychiatryDocument10 pages433 Psychiatry Team Child PsychiatrySherlina Rintik Tirta AyuNo ratings yet
- JAK Inhibitors For Alopecia Areata: A Systematic Review and Meta-AnalysisDocument7 pagesJAK Inhibitors For Alopecia Areata: A Systematic Review and Meta-AnalysisMasithaNo ratings yet
- NCP (GDM)Document16 pagesNCP (GDM)Jay Jay Jayyi100% (1)
- NCP ZabalaDocument1 pageNCP Zabalabryan.zabala.mnlNo ratings yet
- Nursing Care Plan: Precipitating FactorDocument5 pagesNursing Care Plan: Precipitating FactorJe ZalNo ratings yet
- Nursing Care Plan Cues Nursing Diagnosis Goal Nursing Intervention Rationale EvaluationDocument5 pagesNursing Care Plan Cues Nursing Diagnosis Goal Nursing Intervention Rationale EvaluationRuss ElizondoNo ratings yet
- Malnutrition FNCPDocument3 pagesMalnutrition FNCPMaribel ValenzuelaNo ratings yet
- 0022 3956 - 2875 - 2990026 620160913 28497 Y2c5d5 With Cover Page v2Document11 pages0022 3956 - 2875 - 2990026 620160913 28497 Y2c5d5 With Cover Page v2Ivan VazquezNo ratings yet
- NURSING CARE PLANS EditedDocument13 pagesNURSING CARE PLANS Editedalijeslia lyricsNo ratings yet
- LCUP Family Nursing Care Plan (Hypertension)Document4 pagesLCUP Family Nursing Care Plan (Hypertension)Kia MadineNo ratings yet
- Finals AssignemntDocument3 pagesFinals Assignemnteliza luisNo ratings yet
- Poor Compliance With Treatment As Health Threat CuesDocument11 pagesPoor Compliance With Treatment As Health Threat CuesAsniah Hadjiadatu AbdullahNo ratings yet
- Sample FNCP For InfectionDocument3 pagesSample FNCP For InfectionAnonymous gHwJrRnmNo ratings yet
- HealthcareDocument11 pagesHealthcareali veliNo ratings yet
- Navarro, General Trias City, Cavite: Senior High School DepartmentDocument5 pagesNavarro, General Trias City, Cavite: Senior High School DepartmentVan TracilynNo ratings yet
- 11 - NCPsDocument6 pages11 - NCPsellian3leiNo ratings yet
- Comparing The 3rd and 4th Generation HIV Algorithms in A High-Risk PopulationDocument1 pageComparing The 3rd and 4th Generation HIV Algorithms in A High-Risk PopulationAniketNo ratings yet
- Actual 1 CPDocument4 pagesActual 1 CPjangomanaloNo ratings yet
- Pharmacotherapy For Irritability and Aggression in Children With ASDDocument56 pagesPharmacotherapy For Irritability and Aggression in Children With ASDSam JacksonNo ratings yet
- Hamilton 1959Document6 pagesHamilton 1959Areta Nabiel SiamsirajNo ratings yet
- 1 Halker Singh Evaluation of Headaches MC Clinical Reviews 2024 CA R SecureDocument62 pages1 Halker Singh Evaluation of Headaches MC Clinical Reviews 2024 CA R Securecadena.astridNo ratings yet
- Literature Review TemplateDocument1 pageLiterature Review TemplateLa MorochaNo ratings yet
- Behrens Et Al Taut-Gsa FinalDocument1 pageBehrens Et Al Taut-Gsa Finalapi-362872552No ratings yet
- Behrens Et Al Agitation-5Document1 pageBehrens Et Al Agitation-5api-362872552No ratings yet
- Sanders Et Al Mmna Final-RevisedDocument1 pageSanders Et Al Mmna Final-Revisedapi-362872552No ratings yet
- Sanders Et Al Ins2017-Jt-Cls-FinalDocument1 pageSanders Et Al Ins2017-Jt-Cls-Finalapi-362872552No ratings yet
- Ins Poster-Jt 1-28-17jmmsbkv-FinalDocument1 pageIns Poster-Jt 1-28-17jmmsbkv-Finalapi-362872552No ratings yet
- Affective Temperaments and SH in Adolescents - PortugalDocument8 pagesAffective Temperaments and SH in Adolescents - Portugalsoliveira_149796No ratings yet
- Intro Child PsychiatryDocument122 pagesIntro Child PsychiatryayunisallehNo ratings yet
- Sindroma Dalam Psikiatri: Yuliana Ratna WatiDocument23 pagesSindroma Dalam Psikiatri: Yuliana Ratna WatiAyi Abdul BasithNo ratings yet
- Saadat Hasan Manto, Partition, and Mental Illness Through The Lens of Toba Tek SinghDocument6 pagesSaadat Hasan Manto, Partition, and Mental Illness Through The Lens of Toba Tek SinghIrfan BalochNo ratings yet
- Conners 3 Parent Assessment ReportDocument19 pagesConners 3 Parent Assessment ReportEspíritu Ciudadano100% (2)
- Psychosocial Assessment: NameDocument2 pagesPsychosocial Assessment: NameZyra DIOKNONo ratings yet
- My MMPIDocument11 pagesMy MMPIchris7121992100% (1)
- Adolescent Screening and Assessment Instrument Compendium: For Substance Abuse and Mental Health DisordersDocument21 pagesAdolescent Screening and Assessment Instrument Compendium: For Substance Abuse and Mental Health DisordersIván Rosario VillafañeNo ratings yet
- Behavioral Activation For Anxiety Disorders: Derek R. Hopko, Sarah M. C. Robertson and C. W. LejuezDocument21 pagesBehavioral Activation For Anxiety Disorders: Derek R. Hopko, Sarah M. C. Robertson and C. W. LejuezJuan Alberto GonzálezNo ratings yet
- The Truman Show DelusionDocument19 pagesThe Truman Show DelusionKenNo ratings yet
- New York City SchizophreniaDocument4 pagesNew York City SchizophreniaMocanu MihaiNo ratings yet
- Introduction To DSM-IVDocument3 pagesIntroduction To DSM-IVRoci ArceNo ratings yet
- Obsessive Compulsive Disorder Questionnaire PackDocument4 pagesObsessive Compulsive Disorder Questionnaire PackNathaly BerríoNo ratings yet
- Personality DisordersDocument16 pagesPersonality Disorderssomebody_ma100% (1)
- Psych Care PlanDocument3 pagesPsych Care Plancwarrington0967% (3)
- Q-Asc: Section A - PlayDocument6 pagesQ-Asc: Section A - PlayGemaAspergerAsturiasNo ratings yet
- Conners 3rd EditionDocument6 pagesConners 3rd EditionCristina0% (3)
- Hoarding and How To Approach It Guidance For Environmental Health Officers and OthersDocument20 pagesHoarding and How To Approach It Guidance For Environmental Health Officers and OthersKemaing francois lewisNo ratings yet
- Handout For The Course Emotional DisturbanceDocument54 pagesHandout For The Course Emotional DisturbanceMohammed Demssie MohammedNo ratings yet
- Rehabilitation For DementiaDocument14 pagesRehabilitation For DementiaKlinik Malalayang MedikaNo ratings yet
- MP 2016 Companion Guide PDFDocument307 pagesMP 2016 Companion Guide PDFMercuria Nim100% (1)
- Icd 11Document22 pagesIcd 11Shubhangi Vats100% (1)
- NSTP 2 Module 2 AssignmentDocument3 pagesNSTP 2 Module 2 Assignmentmikomikomik0% (1)
- Relapse PreventionDocument1 pageRelapse PreventionAnonymous nYp4sSNo ratings yet
- Mental Health Case StudyDocument14 pagesMental Health Case Studyapi-607930687No ratings yet
- Diagnostic Criteria For 298Document1 pageDiagnostic Criteria For 298Pradeep KumarNo ratings yet
- Report Regarding DepressionDocument18 pagesReport Regarding Depressiontech masterNo ratings yet
- Multiple Personality Disorder Presentation SlideDocument17 pagesMultiple Personality Disorder Presentation Slideestefania sofea zahara67% (3)
- ANALYTICAL EXPOSITION TEXT, TITLE Dissociative Identity DisorderDocument2 pagesANALYTICAL EXPOSITION TEXT, TITLE Dissociative Identity Disordernina arianyNo ratings yet
- MCQS:: A) Imipramine 1 C) Nortriptyline 2 D) Duxepine 3 E) AmitryptalineDocument7 pagesMCQS:: A) Imipramine 1 C) Nortriptyline 2 D) Duxepine 3 E) AmitryptalineEyob MizanNo ratings yet