Professional Documents
Culture Documents
SSC170001supp1 Prod
Uploaded by
Yohanes BongCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SSC170001supp1 Prod
Uploaded by
Yohanes BongCopyright:
Available Formats
Supplementary Online Content
Berros-Torres SI, Umscheid CA, Bratzler DW, et al; Healthcare Infection Control Practices Advisory
Committee. Centers for Disease Control and Prevention guideline for the prevention of surgical site
infection, 2017. JAMA Surg. Published online May 3, 2017. doi:10.1001/jamasurg.2017.0904
eAppendix 1. Centers for Disease Control and Prevention, Guideline for the Prevention of Surgical Site
Infection 2017 Background, Methods and Evidence Summaries
eAppendix 2. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site
Infection, 2017: Supplemental Tables
This supplementary material has been provided by the authors to give readers additional information
about their work.
2017 American Medical Association. All rights reserved. 1
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
eAppendix 1. Centers for Disease Control and Prevention, Guideline for the Prevention of Surgical Site Infection 2017: Background, Methods
and Evidence Summaries
TABLE OF CONTENTS
1. BACKGROUND ........................................................................................................................................................................................................................................................... 4
1.1. Prosthetic Joint Arthroplasty ................................................................................................................................................................................................................................. 4
2. SCOPE AND PURPOSE .............................................................................................................................................................................................................................................. 5
3. METHODS ................................................................................................................................................................................................................................................................... 5
3.1Guideline Questions ................................................................................................................................................................................................................................................ 5
3.1A. CORE SECTION GUIDELINE QUESTIONS.............................................................................................................................................................................................. 6
3.1B. PROSTHETIC JOINT ARTHROPLASTY SECTION GUIDELINE QUESTIONS .................................................................................................................................... 6
3.2. Literature Search ................................................................................................................................................................................................................................................... 7
3.3. Study Selection ...................................................................................................................................................................................................................................................... 8
3.4. Data Extraction and Synthesis ............................................................................................................................................................................................................................. 11
3.5. Formulating Recommendations ........................................................................................................................................................................................................................... 11
4. EVIDENCE REVIEW ................................................................................................................................................................................................................................................ 13
4.1. Core Section Evidence Review ........................................................................................................................................................................................................................... 13
4.1A. PARENTERAL ANTIMICROBIAL PROPHYLAXIS (AMP) .................................................................................................................................................................. 13
4.1B. NON-PARENTERAL ANTIMICROBIAL PROPHYLAXIS ..................................................................................................................................................................... 16
4.1C. GLYCEMIC CONTROL ............................................................................................................................................................................................................................. 20
4.1D. NORMOTHERMIA .................................................................................................................................................................................................................................... 21
4.1E. OXYGENATION ......................................................................................................................................................................................................................................... 22
4.1F. ANTISEPTIC PROPHYLAXIS ................................................................................................................................................................................................................... 25
4.2. Prosthetic Joint Arthroplasty Section Evidence Review ..................................................................................................................................................................................... 30
4.2A. BLOOD TRANSFUSION ........................................................................................................................................................................................................................... 30
4.2B. SYSTEMIC IMMUNOSUPPRESSIVE THERAPY ................................................................................................................................................................................... 32
4.2C. INTRA-ARTICULAR CORTICOSTEROID INJECTIONS ....................................................................................................................................................................... 34
4.2D. ANTICOAGULATION ............................................................................................................................................................................................................................... 36
4.2E. ORTHOPAEDIC SURGICAL SPACE SUIT .............................................................................................................................................................................................. 38
4.2F. POSTOPERATIVE AMP DURATION IN PROSTHETIC JOINT ARTHROPLASTY WITH THE USE OF A DRAIN ........................................................................ 39
4.2G. BIOFILM ..................................................................................................................................................................................................................................................... 39
5. RE-EMPHASIS OF SELECT 1999 CDC AND HICPAC RECOMMENDATIONS FOR PREVENTION OF SURGICAL SITE INFECTIONS ................................................. 41
5.1. Recommendations ............................................................................................................................................................................................................................................... 41
2017 American Medical Association. All rights reserved. 2
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
1. PREPARATION OF THE PATIENT ........................................................................................................................................................................................................... 41
2. HAND/FOREARM ANTISEPSIS FOR SURGICAL TEAM....................................................................................................................................................................... 41
3. OPERATING ROOM VENTILATION ........................................................................................................................................................................................................ 41
4. CLEANING AND DISINFECTION OF ENVIRONMENTAL SURFACES .............................................................................................................................................. 41
5. REPROCESSING OF SURGICAL INSTRUMENTS .................................................................................................................................................................................. 41
6. SURGICAL ATTIRE AND DRAPES .......................................................................................................................................................................................................... 41
7. STERILE AND SURGICAL TECHNIQUE ................................................................................................................................................................................................. 42
8. POST-OP INCISION CARE ......................................................................................................................................................................................................................... 42
6. REFERENCES ............................................................................................................................................................................................................................................................ 43
LIST OF FIGURES
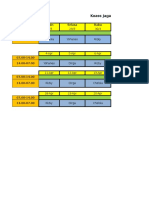
eFIGURE 1. Results of the Study Selection Process................................................................................................................................10
LIST OF TABLES
eTABLE A. Inclusion and Exclusion Criteria for Study Selection ............................................................................................................9
eTABLE B. CDC and HICPAC Categorization Scheme for Recommendations .....................................................................................12
2017 American Medical Association. All rights reserved. 3
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
1. BACKGROUND
In 2006, approximately 80 million surgical procedures were performed in the United States at inpatient hospitals (46 million)1 and
ambulatory hospital-affiliated or free-standing (32 million) settings.2 Between 2006 and 2009, surgical site infections (SSIs)
complicated approximately 1.9% of surgical procedures in the U.S.3 However, the number of SSIs is likely to be underestimated for
several reasons including poor case ascertainment after hospital discharge (given that approximately 50% of SSIs become evident after
discharge) and exclusion of some high-risk procedures from estimates (e.g., non-closed incisions).4National approaches to SSI
surveillance have produced varied estimates of risk in the scientific literature,5 which in combination with inconsistencies in coding and
a lack of standardization of post-discharge surveillance, has made it challenging to evaluate or compare interventions and track SSIs
over time.6
Multiple patient co-morbidities and risk factors, in addition to procedure-related risk factors, can impact the risk of SSI.6 SSIs result in
increased morbidity and mortality. Direct and indirect costs from SSIs include increased hospital length of stay, readmissions for
treatment including repeat surgical procedures, outpatient and emergency care visits, use of ancillary services, additional medications
(including prolonged antimicrobial therapy), lost productivity, and temporary or permanent disability.7 Actual attributable costs of SSIs
are difficult to determine. Cost estimates are commonly restricted to hospital charges and vary according to surgical procedure, depth of
infection, facility, region, country, publication year, study design, and accounting method.7-9 Estimated average attributable costs of
SSIs range from $10,443 to $25,546 per infection (2005 and 2002 dollars, respectively).10-13 Staphylococcus aureus and coagulase
negative staphylococci are the organisms most commonly associated with SSIs, but pathogens can vary by procedure.5 Costs can
exceed $90,000 per infection when the SSI involves a prosthetic joint implant14,15 or antimicrobial resistant organism.16 Approximately
55% of SSIs are deemed preventable by application of evidence-based strategies.13
In 2002, the Centers for Disease Control and Prevention (CDC) and Centers for Medicare & Medicaid Services (CMS) instituted the
Surgical Infection Prevention (SIP) project with the goal of reducing SSIs and developing effective prevention programs.17 In 2006,
SIP became the Surgical Care Improvement Program (SCIP) and expanded to include patient hair removal at the surgical site,
glycemic control, and normothermia process measures.18 With the Deficit Reduction Act of 2005, the U.S. Congress set forth a
mandate for hospital reporting of process, outcome, and other quality improvement measures, and for making this information
available to the public and CMS.19 This act required CMS to adjust payments downward for healthcare-associated infections that
could have been prevented through the application of evidence-based strategies. In 2009, the U.S. Department of Health and Human
Services' (HHS) National Action Plan to Prevent Health Care-Associated Infections: Road Map to Elimination set a 5-year target goal
of a 25% reduction in SSIs detected on admission and readmission, or a 0.75 Standardized Infection Ratio (SIR).20 Since January of
2012, CMSs Hospital Inpatient Quality Reporting Program has required facilities to report SSI outcome data through CDCs National
Healthcare Safety Network (NHSN).21 These data provide some national estimates of SSI prevention progress
(http://www.cdc.gov/hai/surveillance/progress-reports).22
1.1. Prosthetic Joint Arthroplasty
Prevention efforts should target all surgical procedures, but especially those in which both the human and financial burden is greatest.
In 2011, primary total knee arthroplasty (TKA) accounted for over half of the 1.2 million prosthetic joint arthroplasty procedures
(primary and revision) performed in the U.S., followed by total hip arthroplasty (THA), and hip hemi-arthroplasty.23 Primary shoulder,
elbow, and ankle arthroplasties are much less common. By 2030, prosthetic joint arthroplasties are projected to increase to 3.8 million
procedures per year.24-26
Infection is the most common indication for revision in TKA27 and the third most common indication in THA,28 following
instability/dislocation and mechanical loosening, S. aureus and coagulase negative staphylococci are the most common pathogens
associated with orthopaedic SSIs.5 Between 2001 and 2009, there was a significant increase in the risk of infection following hip and
knee arthroplasties (from 1.99% to 2.18% and from 2.05% to 2.18%, respectively).15 By 2030 the infection risk for hip and knee
arthroplasty is expected to increase to 6.5% and 6.8%, respectively.29 Owing to both increasing risk and the number of individuals
undergoing prosthetic joint arthroplasty procedures, by 2020 the total number of hip and knee prosthetic joint infection (PJI) cases is
projected to increase to 70,000 (from 25,000 in 2010) and up to 221,500 cases per year by 2030.15,29 Treatment of PJI commonly
involves a 2-stage procedure, with 4-to-8 weeks of parenteral antimicrobial therapy between stages. When eradication of the infection
is not possible, treatment can include arthrodesis or even amputation.30 In 2009, the average hospital cost for the revision of an infected
hip or knee arthroplasty was $93,600 and $24,200, respectively.15 Between 2001 and 2009, estimated total hospital costs for treating
PJI increased from $320 million to $566 million; costs reached $1 billion in 2014 and are projected to reach $1.62 billion by 2020.15
Any indwelling medical device or prosthetic implant has the potential to become colonized by organisms and embedded in biofilm.31,32
In the U.S., as many as 13 million people experience a biofilm-related infection every year.33 Biofilm is defined as a microbially
derived sessile community characterized by cells that are irreversibly attached to a substratum or interface or to each other, are
embedded in a matrix of extracellular polymeric substances that they have produced, and exhibit an altered phenotype with respect to
growth rate and gene transcription.32 Biofilm embedded organisms exhibit significant resistance to antimicrobial agents (10 to 1,000
times the minimum inhibitory concentration [MIC]) as compared with their free floating, planktonic counterparts.32 Between 7% and
39% of PJIs are culture negative,34,35 which is often attributed to previous antimicrobial therapy36 or the presence of difficult-to-culture
biofilm embedded organisms, making diagnosis, treatment, and the identification of prevention measures difficult to assess.
2017 American Medical Association. All rights reserved. 4
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Evidence-based guidelines have provided recommendations for the diagnosis of PJI using conventional testing techniques including
serologic and synovial fluid markers, tissue histopathology, traditional culture-based techniques, and imaging studies.37 Recently
published studies further support or add to these recommendations.35,36,38-40 Potential future strategies for the diagnosis of PJI include
the use of novel serologic41-45 and synovial fluid46 markers. In addition, novel strategies to improve the recovery of biofilm organisms
may enhance detection of organisms present in lower numbers or species present as a minority.31 Sonication of the explanted
prosthesis35,47-50 or cement spacer49 produces a diluent of released biofilm sonicate. Culture of sonicate effluent may have improved
culture sensitivity as compared with standard synovial fluid or tissue culture techniques. Different growth media35,51 and
microscopic35,51-55 techniques to better grow and characterize biofilm and the embedded organisms are also being explored. Adjunct
molecular techniques hold the potential to improve the sensitivity and specificity of traditional culture-based techniques.51-53,55-61
However, only culture-based techniques provide information on antimicrobial susceptibility, which drives PJI treatment. Therefore
exploring ways to enhance culturing techniques continues to be important.62 Multidisciplinary work to standardize the clinical diagnosis
of PJI is ongoing. 63
2. SCOPE AND PURPOSE
The Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infections, 2017 provides updated and
new recommendations for the prevention of surgical site infection (SSI). This Guideline does not provide comprehensive infection
control recommendations for prevention of SSIs; the exceptions are mentioned below. In 2014, the Healthcare Infection Control
Practices Advisory Committee (HICPAC), a federal advisory committee of the Centers for Disease Control and Prevention (CDC),
reviewed the strong recommendations found in the Guideline for Prevention of Surgical Site Infection, 1999.64 HICPAC determined
many of the 1999 recommendations to be accepted practices for the prevention of SSI. HICPAC recommended to CDC that these
recommendations be considered core surgical infection prevention practices. These recommendations are located in Section 5 of this
Guideline. The 1999 recommendations not updated in this Guideline are considered archived.
The specific areas of focus for the 2017 Guideline were informed by feedback received from clinical experts and input from HICPAC.
As in the Guideline for Prevention of Surgical Site Infection, 1999,64 the 2017 Guideline does not address SSI prevention issues unique
to: burns; trauma; surgical incisions allowed to heal by secondary intention; transplant procedures; transmission of bloodborne
pathogens from healthcare personnel to the patient; pediatric surgical practice; minimally invasive procedures; procedures performed
outside of the operating room (e.g., endoscopic procedures); non-surgical invasive procedures (e.g., cardiac catheterization,
interventional radiology); and other procedures or conditions not specifically mentioned.64 In general, SSI prevention measures deemed
effective in adults are also indicated in the pediatric surgical population, and those effective in the operating room can be adapted or
modified for other settings. In addition, this update does not address SSI surveillance or public reporting.65 Recommendations on
infection control in healthcare personnel,4,66 environmental infection control,67 and disinfection and sterilization of medical devices68 in
healthcare settings are addressed by other guidelines.
To evaluate the evidence on SSI prevention, questions addressing 13 intervention categories were examined. The Core Section of the
2017 Guideline encompasses literature across all surgical procedures and is comprised of 6 topics: parenteral antimicrobial prophylaxis,
non-parenteral antimicrobial prophylaxis, glycemic control, normothermia, oxygenation, and antiseptic prophylaxis. The literature for 7
topics related specifically to prosthetic joint arthroplasty procedures was evaluated in the Prosthetic Joint Arthroplasty section of the
Guideline. These 7 topics include: blood transfusions, systemic immunosuppressive therapy, intra-articular corticosteroid injections,
anticoagulation, orthopaedic surgical space suit, postoperative antimicrobial prophylaxis, and biofilm.
The 2017 Guideline is intended for use by surgeons; physician assistants; perioperative nurses and other allied perioperative assistive
personnel; anesthesia providers; postoperative inpatient and clinic nurses; infection prevention staff; healthcare epidemiologists;
healthcare administrators; other healthcare providers; and persons responsible for developing, implementing, delivering, and evaluating
infection prevention and control programs for surgical procedures performed in an operating room (inpatient or ambulatory setting).
The Guideline can also be used as a resource for professional societies or organizations that wish to develop more detailed
implementation guidance or to identify future research priorities where there are evidence gaps for the prevention of SSI.
3. METHODS
The 2017 Guideline was based on a targeted systematic review of the best available evidence on SSI prevention. An adapted approach
to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) was used to assess the quality of the
available evidence and the strength of the resulting recommendations, and to provide explicit links between them.69-72 The Guideline
development process has been previously described.73 Methods and details that were unique to this Guideline are included below.
3.1Guideline Questions
A preliminary list of questions was developed from a review of the 1999 CDC SSI Guideline.64 The current guideline does not re-
evaluate several strong recommendations (Section 5) offered by the 1999 CDC SSI guideline which are now considered to be accepted
2017 American Medical Association. All rights reserved. 5
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
practice for the prevention of SSI. Content experts were surveyed to provide feedback on the questions and to identify additional topics
of interest. Guideline questions were put in final form after they were vetted by the co-authors and HICPAC.
3.1A. Core Section Guideline Questions
Parenteral Antimicrobial Prophylaxis (AMP)
Q1. What are the most effective strategies for administering parenteral AMP to reduce the risk of SSI?
What is the optimal timing of preoperative AMP?
What is the optimal timing of AMP in cesarean section: prior to skin incision or at cord clamping?
How safe and effective is weight-adjusted AMP dosing?
How safe and effective is intraoperative redosing of AMP?
How safe and effective is postoperative AMP and what is the optimal duration?
Non-Parenteral Antimicrobial Prophylaxis
Q2. What are the most effective strategies for administering non-parenteral antimicrobial prophylaxis at the surgical incision to
reduce the risk of SSI?
A. How safe and effective is antimicrobial irrigation?
B. How safe and effective are antimicrobial agents applied to the surgical incision?
C. How safe and effective are antimicrobial-coated sutures; when and how should they be used?
D. How safe and effective are antimicrobial dressings applied to surgical incisions following primary closure in the
operating room?
Glycemic Control
Q3. How do perioperative blood glucose and hemoglobin A1c levels impact the risk of SSI, and what are their optimal
perioperative target levels in diabetic and non-diabetic patients?
Normothermia
Q4. How safe and effective is the maintenance of perioperative normothermia in reducing the risk of SSI?
Q5. What are the most effective strategies for achieving and maintaining perioperative normothermia?
Oxygenation
Q6. In patients with normal pulmonary function, how safe and effective is the perioperative use of increased fraction of inspired
oxygen (FiO2) in reducing the risk of SSI?
Q7. What is the optimal target FiO2 to reduce the risk of SSI; how and when should it be administered?
Antiseptic Prophylaxis
Q8. What are the most effective strategies for preparing the patients skin prior to surgery to reduce the risk of SSI?
A. How safe and effective is preoperative antiseptic bathing or showering?
B. How safe and effective are antiseptic skin preparation agents individually and in combination?
C. How safe and effective is the application of a microbial sealant immediately following skin preparation?
D. How safe and effective are plastic adhesive drapes?
Q9. How safe and effective is antiseptic irrigation prior to closing the surgical incision?
Q10. How safe and effective is repeat application of an antiseptic skin preparation agent to the surgical site immediately
prior to closing the surgical incision?
3.1B. Prosthetic Joint Arthroplasty Section Guideline Questions
Blood Transfusion
Q11. How do perioperative blood transfusions impact the risk of SSI in prosthetic joint arthroplasty patients?
A. Are specific blood products associated with a risk of SSI?
B. If the risk of SSI is increased, can this effect be isolated from the risk associated with more complex cases?
C. How does the volume of transfused blood product impact the risk of SSI?
D. How safe and effective is withholding blood transfusion to reduce the risk of SSI?
Systemic Immunosuppressive Therapy
Q12. How does systemic corticosteroid or other immunosuppressive therapy impact the risk of SSI in prosthetic joint arthroplasty
patients?
A. Does the type of agent impact the risk of SSI?
B. Does the preoperative duration of the therapy impact the risk of SSI?
C. Does the agent dose impact the risk of SSI?
Q13. What are the most effective strategies in managing systemic corticosteroid or other immunosuppressive therapy
perioperatively to reduce the risk of SSI in prosthetic joint arthroplasty patients?
2017 American Medical Association. All rights reserved. 6
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
A. How safe and effective is the discontinuation of these agents preoperatively, and when should they be resumed?
B. Should the agent dose be adjusted, and if so, for how long?
Q14. What is the optimal duration of postoperative AMP to reduce the risk of SSI in prosthetic joint arthroplasty patients who are
on systemic corticosteroid or other immunosuppressive therapy?
Intra-articular Corticosteroid Injections
Q15. How do preoperative intra-articular corticosteroid injections impact the risk of SSI in prosthetic joint arthroplasty patients?
Q16. What are the most effective strategies for managing the preoperative use of intra-articular corticosteroid injections to reduce
the risk of SSI in prosthetic joint arthroplasty patients?
A. Does the length of time between intra-articular corticosteroid injection and prosthetic joint arthroplasty impact the risk of
SSI?
B. Does the corticosteroid injection dose impact the risk of SSI?
Anticoagulation
Q17. What are the most effective strategies for managing perioperative venous thromboembolism (VTE) prophylaxis to reduce
the risk of SSI?
A. Does the risk of SSI differ by individual VTE prophylaxis agent?
B. What is the optimal timing and duration of perioperative VTE prophylaxis that also reduces the risk of SSI?
C. How safe and effective is modifying the dose of the perioperative VTE prophylaxis agent to reduce the risk of SSI?
Orthopaedic Space Suit
Q18. How safe and effective are orthopaedic space suits in reducing the risk of SSI in prosthetic joint arthroplasty patients, and
which healthcare personnel should wear them?
Antimicrobial Prophylaxis Duration with Drain Use
Q19. What is the optimal duration of postoperative AMP to reduce the risk of SSI in prosthetic joint arthroplasty in the presence
of a drain?
Biofilm
Q20. What are the most effective strategies to reduce the risk of biofilm formation and SSI in prosthetic joint arthroplasty
patients?
A. How effective are cement modifications (i.e., antimicrobial and nanoparticle loading)?
B. How effective are prosthesis surface modifications (i.e., antimicrobial coating, galvanic couples, printing technologies,
and nanotechnology)?
C. How effective are vaccines?
D. How effective are other biofilm control agents (e.g., biofilm dispersants, quorum-sensing inhibitors, novel antimicrobial
agents)?
3.2. Literature Search
Following the development of Guideline questions, search terms were developed for identifying literature most relevant to those
questions. For the purposes of quality assurance, these terms were compared to those used in relevant seminal studies and guidelines.
These search terms were then incorporated into search strategies for the relevant databases. Searches were performed in MEDLINE,
EMBASE, CINAHL, and the Cochrane Library. All databases were searched from 1998, when the previous guideline searches ended,
through April 2014 for the Core Section and December 2011 for the Prosthetic Joint Arthroplasty Section. Literature published since
these dates could affect one or more of the recommendations in this Guideline. References were imported into a reference manager
where duplicates were resolved. The detailed search strategy and results for the Core Section and the Prosthetic Joint Arthroplasty
Section can be found in eAppendix 2 of this Supplement.
Initial searches were designed to identify systematic reviews (SRs) and randomized controlled trials (RCTs). SRs that included non-
randomized trials and observational studies (OBS) were eligible for inclusion. Three factors influenced the decision to limit literature
searches to RCTs and SRs:
1. RCTs control for confounding more effectively than OBS and thus provide higher quality evidence on the efficacy of
therapies;
2. the broad scope of the Guideline; and
3. the value of providing updated recommendations in a timely manner.
When Guideline questions in the Prosthetic Joint Arthroplasty Section were not adequately addressed in the studies identified by the
initial searches, additional searches were performed. The additional searches used keywords that were more specific to each relevant
question and were not limited to SRs and RCTs.
2017 American Medical Association. All rights reserved. 7
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
3.3. Study Selection
Titles and abstracts were screened by one independent reviewer (S.I.B.T., D.B., R.R.K., or C.E.R.). A random sample of 10% of titles
and abstracts had a second independent review to ensure consistency in screening. Kappa scores, used to measure agreement between
the two independent reviewers beyond chance, ranged from 0.40.5, indicating moderate agreement between reviewers.74 Full text
articles were retrieved if they were:
1. relevant to one or more Guideline questions;
2. clinical practice guidelines, SRs, or primary study designs meeting the inclusion criteria (RCT for the Core and Prosthetic
Joint Arthroplasty sections and OBS for the Prosthetic Joint Arthroplasty section);
3. written in English; and
4. available as full text studies (meeting abstracts were excluded). Animal studies and in vitro basic science studies were
excluded from all topics except biofilm. Pediatric patient studies were included. Although the literature databases were
searched from 1998 to 2014, studies published earlier than 1998 were eligible for inclusion (e.g., studies suggested by the
expert panel, included in the 1999 guideline, or identified in published SRs).
Full-text articles were screened by two independent reviewers (S.I.B.T and R.R.K.; S.I.B.T. and C.E.R.; S.I.B.T and D.B., or D.B and
E.C.S.) and disagreements were resolved by discussion. Full-text articles were excluded if:
1. SSI was not reported as an outcome;
2. all patients included had dirty surgical procedures (except for Q2 addressing the use of aqueous iodophor irrigation);
3. the study only included oral or dental health procedures;
4. the surgical procedures did not include primary closure of the incision in the operating room (e.g., orthopedic pin sites,
thoracotomies, or percutaneous endoscopic gastrostomy [PEG] procedures, or wounds healing by secondary intention);
5. the study evaluated wound protectors used post-incision.
In the Core Section for Q1, parenteral antimicrobial prophylaxis studies comparing the efficacy of antimicrobial prophylaxis to no
prophylaxis (placebo-controlled studies) and studies comparing the efficacy of different prophylactic antimicrobial agents were
excluded. Also for Q2, non-parenteral antimicrobial prophylaxis, use of gentamicin collagen sponge studies were excluded because
they are not approved by the U.S. Food and Drug Administration (FDA). For Q8-10 antiseptic prophylaxis, studies evaluating vaginal
antisepsis in combination with abdominal antisepsis were excluded. In addition, studies using electrolyzed ionized solution (not
approved by the FDA for intraoperative irrigation of the surgical site) and dry povidone iodine powder spray studies were excluded.
For the Prosthetic Joint Arthroplasty section, studies were excluded if they did not specifically examine prosthetic joint arthroplasties.
Questions from 4 topics in the Prosthetic Joint Arthroplasty section were excluded from a targeted search when both:
1. the initial broad search identified very few or no RCTs or SRs that fit the inclusion criteria, and
2. the content experts excluded them as lower-priority topics for guideline questions (i.e., surgical attire [specifically gloves],
surgical techniques, anesthesia, and environmental factors).
Also, questions and related studies addressing diagnosis of periprosthetic joint infection (PJI) or biofilm were excluded because they
did not address SSI prevention. eTable 74 provides a list of inclusion and exclusion criteria used by reviewers.
2017 American Medical Association. All rights reserved. 8
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
eTABLE A. Inclusion and Exclusion Criteria for Study Selection
Section 1 Section 2
General Exclusion Criteria (all key (all key
questions) questions)
Not relevant to key questions
Not RCT or SR
Not in English
Not available as full text article
Surgical site infection not included as outcome
Oral medicine / dental health procedures
Not primary closure
Wound protector used post incision
Animal studies
Basic science studies
Not a prosthetic joint arthroplasty
Specific Exclusion Criteria Topic
Placebo-controlled studies Antimicrobial prophylaxis
Comparison of different antibiotics Antimicrobial prophylaxis
Vaginal antisepsis Skin Preparation
Epoeitin administration Blood transfusion
Specific Inclusion Criteria Topic
Dirty procedures Antimicrobial prophylaxis
Timing of AMP in high-risk Cesarean sections Antimicrobial prophylaxis
Non-AMP irrigation / topical application prior to wound closure
Antimicrobial prophylaxis
(povidone iodine, electrolyzed/ionized solutions)
Platelet gel prior to skin closure Skin preparation
A draft bibliography was shared with a panel of content experts, and the additional suggested references then progressed through title
and abstract screening and full text review as described above. Results of the entire study selection process are depicted in eFigure 1.
2017 American Medical Association. All rights reserved. 9
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
eFIGURE 1. Results of the Study Selection Process
5487 Potentially relevant studies 104 Studies suggested by content 168 Studies cited in 1999 CDC
identified in literature searches experts SSI guideline
5759 Titles and abstracts screened
4863 Studies excluded
896 Full text review
26 Clinical practice guidelines
719 Studies excluded
592 Not relevant to key questions
117 Study design
19 Additional clinical practice guidelines 6 Not available as full text article
identified by writing group
4 Not in English
17 Clinical practice
guidelines excluded
44 RCTs identified from excluded SRs
28 Clinical practice guidelines 25 Studies excluded, not
cited in present guideline relevant to key questions
170 Studies extracted into evidence
and GRADE tables
2017 American Medical Association. All rights reserved. 10
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
3.4. Data Extraction and Synthesis
For studies meeting the inclusion criteria, data on the study author, year, design, risk of bias, objective, population, setting, sample
size, interventions, and results of clinically relevant outcomes were extracted into standardized evidence tables. From these, evidence
tables were developed for each clinical topic represented by the questions. Studies were extracted into the most relevant evidence
table. Studies were organized by individual questions and subquestions. Data were extracted by a single author (S.I.B.T., E.C.S., B.L.,
or R.A.) and cross-checked by another author (S.I.B.T. or E.C.S.). Disagreements were resolved by the remaining authors. Data and
analyses were extracted as originally presented in the included studies. Meta-analyses were performed only where their use was
deemed critical to a recommendation and only in circumstances in which multiple studies with sufficiently homogenous populations,
interventions, and outcomes could be analyzed.
SRs were included if the individual studies fit the inclusion criteria. To avoid duplication of data, primary studies identified by the
search were excluded if they were also included in a SR captured in the search, unless:
1. the primary study also addressed a relevant question that was outside the scope of the included SRs, or
2. it was one of a select number of studies in the SR that fit the inclusion criteria and was used to perform a new meta-analysis.
SRs of primary studies that were fully captured in a more recent SR were excluded. The only exception was older SRs that
addressed a question relevant to the Guideline that was outside the scope of the newer SR.75
Statistical analyses were performed using Review Manager 5.1. For the purposes of this review, statistical significance was defined as
p0.05.
The risk of bias associated with each study was assessed using scales developed by the ECRI Institute Penn Medicine Center for
Evidence-based Practice, and scores were recorded in the evidence tables. eAppendix 2 of this Supplement includes the questions used
to assess the risk of bias of the included SRs, RCTs, and OBS. When the risk of bias was rated as High for >50% of studies making
up the evidence base for a given outcome, one point was deducted for Study Quality in the GRADE tables.
Heterogeneity was assessed using the I2 statistic and by evaluation of forest plots. When the I2 value exceeded 50%, and the source of
heterogeneity could not be explained by characteristics of the included studies, subgroup analysis, or examination of the forest plots,
one point was deducted for consistency in the GRADE tables.
Publication bias was evaluated for questions that addressed commercial products if there was a reasonable expectation that bias in the
publication of studies or the reporting of outcomes might be influenced by the sources of study funding. Additionally, funnel plots
were examined for patterns suggestive of publication bias. Disclosures of study authors reported conflicts of interest were also
reviewed, and relevant information is included in the evidence tables. When these analyses indicated the likely presence of publication
or reporting bias, 1 point was deducted for publication bias in the GRADE tables. All GRADE Tables, Evidence Tables, and Risk of
Bias Tables can be found in eAppendix 2 of the Supplement.
Evidence-based recommendations were cross-checked with those from other guidelines identified in an initial systematic search.
For all other methods, please refer to the Guideline Methods supplement.73
3.5. Formulating Recommendations
Recommendations were formulated based on current evidence that addressed Guideline questions at the time the literature searches
were conducted. Explicit associations between the evidence and recommendations are mentioned in the Evidence Review of the
Guideline (eAppendix 1 of the Supplement) as well as in the evidence tables and GRADE tables (eAppendix 2 of the Supplement).
Evidence-based recommendations were cross-checked with those from other guidelines identified in an initial systematic search.
Category I (levels A, B, and C) recommendations are ALL considered strong and should be equally implemented; only the quality of
the evidence underlying the recommendation(s) distinguishes levels A and B. Category IC recommendations are required by state or
federal regulation without regard to level of supporting evidence. Category II recommendations are considered weak
recommendations to be implemented at the discretion of individual institutions as supplementary procedures -- never in place of
Category I recommendations -- and are not intended to be systematically and routinely enforced. The categorization scheme used in
this Guideline is presented in eTable 2.
2017 American Medical Association. All rights reserved. 11
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
73,76
eTABLE B. CDC and HICPAC Categorization Scheme for Recommendations
Recommendation
Category Category Description
Category IA A strong recommendation supported by high-to-moderate quality evidence
suggesting net clinical benefits or harms.
Category IB A strong recommendation supported by low-quality evidence suggesting net
clinical benefits or harms, or an accepted practice (e.g., aseptic technique)
supported by low-to-very low-quality evidence.
Category IC A strong recommendation required by state or federal regulation.
Category II A weak recommendation supported by any quality evidence suggesting a tradeoff
between clinical benefits and harms.
No recommendation/ An unresolved issue for which there is either low-to-very low-quality evidence
unresolved issue with uncertain tradeoffs between benefits and harms or no published evidence on
outcomes deemed critical to weighing the risks and benefits of a given intervention.
The wording of each recommendation reflects the recommendation's strength. Active voice is used for Category I recommendations -
the strong recommendations. For example, phrases such as do or do not are used to convey certainty. Passive voice is used for
Category II recommendations - the weak recommendations. Words such as "consider or is not necessary are used to reflect lesser
certainty about an intervention. Additionally, some interventions described in this guideline may have clinical utility beyond the
prevention of SSIs, but these other uses were not evaluated and are outside the scope of this guideline. To recognize the possibility
that other uses may exist, these recommendations specified for the prevention of SSI.
Readers who wish to examine the evidence underlying the recommendations are referred to the Evidence Review in eAppendix 1 of
the Supplement and the evidence tables and GRADE tables in eAppendix 2 of the Supplement. The Evidence Review includes
narrative summaries of the data presented in the evidence tables and GRADE tables. The evidence tables include all study-level data
used in the Guideline, and the GRADE tables assess the overall quality of the evidence for each question and outcome examined.
2017 American Medical Association. All rights reserved. 12
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
4. EVIDENCE REVIEW
4.1. Core Section Evidence Review
4.1A. PARENTERAL ANTIMICROBIAL PROPHYLAXIS (AMP)
Q1. What are the most effective strategies for administering parenteral AMP to reduce the risk of SSI?
Q1A. What is the optimal timing of preoperative AMP?
The search did not identify RCTs or SRs that evaluated different timings of preoperative AMP administration and its impact on the
risk of SSI. The search only identified RCTs that evaluated timing of preoperative AMP administration in surgeries involving
tourniquets.
The available data on the optimal timing of antimicrobial prophylactic agent administration in surgeries involving tourniquets
examined AMP administered either before or after tourniquet inflation. For this comparison, deep SSI was the critical outcome in
decision-making. Length of stay and antimicrobial resistance were also evaluated. The evidence for this comparison consists of 2
RCTs.77,78 The findings of the evidence review and the grades for all important outcomes are shown in eAppendix 2 of the
Supplement: GRADE Table Q1 and Evidence Table Q1A.
Low-quality evidence suggested a benefit of AMP administration 1 minute after tourniquet inflation as compared with 5 minutes
before limb exsanguination and tourniquet inflation in elective lower limb musculoskeletal procedures. This was based on 1 small
RCT77 (N=106, high risk of bias) suggesting significantly fewer deep infections in the post-tourniquet inflation group. Patients had a
preoperative admission time of up to 5 days, and limbs were exsanguinated prior to tourniquet inflation. Tourniquet time was longer in
the pre-inflation AMP study group, but this difference was not significant.
Moderate-quality evidence suggested no difference in SSI rates based on AMP administration 10 minutes before tourniquet release vs.
10-30 minutes before tourniquet inflation, in total knee arthroplasties. This was based on no difference in deep SSI in 1 large, single-
institution RCT78 with 908 total knee arthroplasties and a moderate risk of bias. There were no differences in length of stay and
antimicrobial resistance between groups.
Other guidelines
The 1999 CDC Guideline for Prevention of Surgical Site Infection and other clinical practice guidelines, based on a review of the
evidence and expert opinion, recommend administering by the intravenous route a single dose of prophylactic antimicrobial agent only
when indicated. For most prophylactic agents, the 1999 CDC guideline recommended preoperative administration be timed such that a
bactericidal concentration of the drug is established in the serum and tissues when the incision is made, and other clinical practice
guidelines recommend that administration should be within 60 minutes prior to incision (vancomycin and fluoroquinolones within 60-
120 minutes prior to incision).17,64,79-85 This is considered accepted practice. None of the recommendations address whether it is
necessary to administer a complete or a partial infusion of the parenteral AMP dose prior to surgical incision.
Q1B. What is the optimal timing of AMP in cesarean section: prior to skin incision or at cord clamping?
The available data on optimal timing of antimicrobial prophylactic agent administration in cesarean section examined AMP
administered prior to skin incision versus at cord clamping.
For this comparison, post-partum endometritis was the critical outcome in decision-making. Other outcomes were also evaluated,
including incisional SSI, neonatal sepsis, neonatal sepsis workup, neonatal antimicrobial resistance, and neonate admission to higher
level of care. In general, endometritis was defined as fever > 100.4F (38C) on 2 occasions with uterine tenderness, purulent lochia,
tachycardia or leukocytosis. The findings of the evidence review and the grades for all important outcomes are shown in eAppendix 2
of the Supplement: GRADE Table Q1 and Evidence Table Q1B.
High-quality evidence suggested a benefit of AMP administration prior to skin incision as compared with administration immediately
after the umbilical cord is clamped in cesarean sections. This was based on a meta-analysis (N=2493) of 7 RCTs86-92 suggesting a 43%
reduction in the risk of developing post-partum endometritis and no difference in the odds of developing incisional SSI. High-quality
evidence from a meta-analysis (N=1080) of 3 RCTs86,87,92 showed no difference in neonatal sepsis. Moderate-quality evidence
consisting of 2 RCTs86,91 evaluating neonatal antimicrobial resistance in cases of sepsis found either no difference in neonatal
antimicrobial resistance between groups, or no cases of antimicrobial resistance, respectively. In addition, high-quality evidence from
a meta-analysis (N=1604) of 5 RCTs86-88,91,92 suggested no difference in neonatal sepsis workups. Lastly, high-quality evidence from a
meta-analysis (N=1694 neonates) of 5 studies86,87,89,91,92 suggested no difference in admissions to higher level of care. One of these
studies89 reported being funded by a pharmaceutical company.
Other guidelines
Clinical practice guidelines based on a review of the evidence and expert opinion recommend administration of a single preoperative
prophylactic antimicrobial agent by the intravenous route, based on the agent pharmacokinetics, commonly beginning within 60
2017 American Medical Association. All rights reserved. 13
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
minutes prior to skin incision in both elective and emergency cesarean section.79-81,83 Administration of AMP after cord clamping is no
longer recommended.64
Q1C. How safe and effective is weight-adjusted AMP dosing?
Searches of published studies did not identify RCTs or SRs that evaluated weight-adjusted AMP dosing and its impact on the risk of
SSI.
Other guidelines
Clinical practice guidelines based on a review of the evidence and expert opinion recommend increasing the single preoperative
prophylactic antimicrobial agent dose for select prophylactic antimicrobial agents in obese and morbidly obese patients.79-84 For
cefazolin, recommendations are to administer 2.0 g80-82,84 for patients weighing >60-80 kg and 3.0 g81,84 if >120 kg. For
aminoglycosides, dosing is calculated using the patients ideal body weight plus 40% of the difference between the actual and ideal
body weight.81,84,93 Vancomycin should be dosed at 15 mg/kg.80-82,84
Q1D. How safe and effective is intraoperative redosing of AMP?
The available data examining intraoperative redosing of AMP compared 1 preoperative dose versus 1 preoperative dose plus an
additional dose at 2 hours intraoperatively.
For this comparison, abdominal and perineal wound SSI and intra-abdominal abscess were the critical outcomes in decision-making.
Antimicrobial resistance was also evaluated as an outcome of interest. The evidence for this question consists of 1 RCT at moderate
risk of bias in elective colorectal surgery.94 The findings of the evidence review and the grades for all important outcomes are shown
in eAppendix 2 of the Supplement: GRADE Table Q1 and Evidence Table Q1D.
Moderate-quality evidence suggested no benefit of intraoperative AMP redosing. This was based on no difference in abdominal or
perineal wound infection, intra-abdominal abscess, or antimicrobial resistance in 1 elective colorectal surgery study from 1991.94
However, procedures with durations >3 hours had a significantly higher risk of SSI and 22% of patients with procedure durations 2
hours were not redosed. Fecal contamination almost doubled the SSI rate at every level of contamination (of note, patients underwent
mechanical bowel prep). Procedure duration and fecal contamination were not reported by study group. Limited power of the study
could result in a false negative finding.
Other guidelines
Clinical practice guidelines based on a review of the evidence and expert opinion recommend prophylactic antimicrobial agent
redosing in cases of prolonged procedures (when the procedure exceeds the half-life of the prophylactic antimicrobial agent or is
longer than 3-4 hours) and in patients with major blood loss (>1,500 ml) or extensive burns.80-84,95 Redosing should also be performed
at intervals of 1-2 times the prophylactic antimicrobial agent half-life, starting at the beginning of the preoperative dose.80-84,95 No
recommendations are provided for optimal prophylactic antimicrobial agent dosing in obese and morbidly obese patients when
redosing.
Q1E. How safe and effective is postoperative AMP and what is the optimal duration?
Administration of postoperative AMP was evaluated, both with all surgical procedures combined and by select surgical specialties.
Analysis focused on studies that used the same prophylactic antimicrobial agent in both arms. Studies that compared different
prophylactic antimicrobial agents or those administering only oral AMP were excluded. Postoperative AMP was defined as any
parenteral prophylactic antimicrobial agent administered after intraoperative closure of the surgical incision. Therefore, postoperative
AMP (in hours or days) does not include any AMP administered as a single preoperative dose and/or any intraoperative redosing.
The available data examined the following comparisons for different postoperative AMP durations:
1. All surgeriesNo post-op AMP vs. 24 hours
2. Cardiac
a. No post-op AMP vs. 24 hours
b. No post-op AMP vs. <96 hours
c. No post-op AMP vs. 7296 hours
d. 24 vs. 72 hours
3. ThoracicNo post-op AMP vs. 2 days
4. Vascular
a. No post-op AMP vs. 24 hours
b. <24 hours vs. 35 days
c. No post-op AMP vs. 5 days
5. Ear, nose, and throat - 24 hours vs. 35 days
6. Gynecologic
a. No post-op AMP vs. 24 hours
2017 American Medical Association. All rights reserved. 14
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
b. b. <24 hours vs. <2.5 days
7. Orthopaedic
a. FractureNo post-op AMP vs. 24 hours
b. Prosthetic Joint ArthroplastyNo post-op AMP vs. 24 hours
8. Colorectal: Bowel preparation with oral antimicrobials
a. No post-op AMP vs. 3 days
b. 24 hours vs. 5 days
9. Colorectal: Bowel preparation only
a. No post-op AMP vs. 24 hours
b. b. No post-op AMP vs. <2-3 days
10. Colorectal: Bowel preparation not reported
a. No post-op AMP vs. 24 hours
b. 24 hours vs. 23 days
11. Colorectal: No bowel preparation
a. No post-op AMP vs. 24 hours
b. No post-op AMP vs. <23 days
12. Appendectomy
a. No post-op AMP vs. 24 hours
b. No post-op AMP vs. 2 days
13. Rectal surgeryNo post-op AMP vs. 24 hours
14. Gastric surgery
a. No post-op AMP vs. 24 hours
b. No post-op AMP vs. 2 days
c. None vs. 4 days
15. Hepatectomy2 days vs. 5 days
For all comparisons, SSI (superficial, deep incisional, and organ/space) and trocar wound infection were the critical outcomes for
decision-making. Antimicrobial resistance, adverse events, length of stay, mortality, and other outcomes were also evaluated. The
evidence for this question consists of 45 RCTs in cardiac;96-100 thoracic;101 vascular; 102-104 ear, nose and throat;105,106 gynecologic;107-112
orthopaedic;113-118 and general surgical119-140 procedures. Twenty-eight (62%) studies were published between 1972 and 1998; 17
(38%) studies were published between 2003 and 2013. The findings of the evidence review and the grades for all important outcomes
are shown in eAppendix 2 of the Supplement: GRADE Table Q1 and Evidence Table Q1E.
Q1E.1. All surgeries - none vs. 24 hours
High-quality evidence suggested no benefit of continuing AMP after intraoperative closure of the surgical incisions. This was based
on no difference in SSI in 1 large meta-analysis (N=14,285) of 21 RCTs in cardiac; thoracic; vascular; ear, nose and throat;
gynecologic; orthopaedic; and general surgical procedures.99,102,108-120,122-124,128,133,137 Fourteen (67%) studies were published between
1984 and 1995; 7 were published between 2005 and 2013. Thirteen studies97,98,108,111,115,118,120-122,125,127-129 reported funding of the study
and/or receipt of study supplies from pharmaceutical companies.
Moderate-quality evidence suggested no benefit of continuing AMP after intraoperative closure of the surgical incision in cardiac
surgery. This is based on a meta-analysis (N=1746) of sternal organ/space infections in cardiac surgeries in 3 RCTs.97-99 Two
studies97,98 reported the authors received funding from pharmaceutical companies.
Results by select surgical specialties or procedures and individual comparators are available in eAppendix 2 of the Supplement:
GRADE Table Q1.
2017 American Medical Association. All rights reserved. 15
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Q1. Recommendations
1A. Administer preoperative antimicrobial agent(s) only when indicated, based on published clinical practice
guidelines and timed such that a bactericidal concentration of the agent(s) is established in the serum and
tissues when the incision is made. (Category IB strong recommendation; accepted practice) 64
(Guideline Question 1A)
1A1. No further refinement of timing can be made for preoperative antimicrobial agents based on clinical
outcomes. (No recommendation/unresolved issue) 77,78 (Guideline Question 1A)
1B. Administer the appropriate parenteral prophylactic antimicrobial agent(s) prior to skin incision in all cesarean
section procedures. (Category IA strong recommendation; high-quality evidence) 86-92 (Guideline
Question 1B)
1C. The search did not identify randomized controlled trials evaluating the harms and benefits of weight-adjusted
AMP dosing and its affect on the risk of SSI. Other organizations have made recommendations based on
observational and pharmacokinetic data and a summary of these recommendations can be found in the Other
guidelines section of the narrative summary for this question. (No recommendation/unresolved issue)
(Guideline Question 1C)
1D. The search did not identify sufficient randomized controlled trial evidence to evaluate the harms and benefits
of intraoperative redosing of parenteral prophylactic antimicrobial agents for the prevention of SSI. Other
organizations have made recommendations based on observational data and a summary of these
recommendations can be found in the Other guidelines section of the narrative summary for this question. (No
recommendation/unresolved issue) 94 (Guideline Question 1D)
1E. In clean and clean-contaminated procedures, do not administer additional prophylactic antimicrobial agent
doses after the surgical incision is closed in the operating room, even in the presence of a drain. (Category IA
strong recommendation; high-quality evidence) 96-140 (Guideline Question 1E)
4.1B. NON-PARENTERAL ANTIMICROBIAL PROPHYLAXIS
Q2. What are the most effective strategies for administering non-parenteral antimicrobial prophylaxis at the surgical incision
to reduce the risk of SSI?
Q2A. How safe and effective is antimicrobial irrigation?
The search identified 2 RCTs examining the impact of antimicrobial irrigation on SSI. For this comparison, SSI was the critical
outcome for decision-making. Product-related adverse events and antimicrobial resistance were also evaluated.
In elective colorectal surgeries, moderate-quality evidence suggests a reduction in SSI with intraperitoneal lavage using clindamycin-
gentamicin solution that is allowed to rest in the abdominal cavity for 3 minutes. This was based on 1 small RCT141 at low risk of bias
in 103 surgeries. In this study, both groups received preoperative AMP followed by an intraoperative bolus at 4 hours if the surgery
exceeded this time. Post-irrigation microbiologic samples were only taken from the group irrigated with clindamycin-gentamicin
solution. Post-irrigation cultures were positive in 2 patients (4%) in this group and both the Klebsiella spp. and Streptococcus
salivarius recovered were resistant to clindamycin and gentamicin. Product-related adverse events were not assessed.
In acute appendectomies, low-quality evidence suggested a reduction in SSI with wound irrigation using ampicillin solution when
compared with normal saline irrigation. This was based on 1 RCT142 (N=249) at moderate risk of bias in adult and pediatric patients
undergoing appendectomies for suspected acute appendicitis. Both groups received AMP, which was continued for 5 days
postoperatively if the appendix was found to be gangrenous or perforated. Almost all Streptococcus and Enterococcus isolates
cultured from intraoperative peritoneal and wound swabs were sensitive to ampicillin except for 30% of E. coli isolates. Postoperative
complications were infrequent and not associated with the intervention.
The search did not identify RCTs or SRs that evaluated the safety and effectiveness of soaking of surgical implants (e.g., meshes,
neurosurgical ventricular shunts) in antimicrobial solution prior to insertion (in combination with parenteral AMP) and its impact on
SSI.
Other guidelines
Two clinical practice guidelines, based on a review of the evidence, recommend against antimicrobial wound irrigation or intra-cavity
lavage to reduce the risk of SSI.85,95
2017 American Medical Association. All rights reserved. 16
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Q2B. How safe and effective are antimicrobial agents applied to the surgical incision?
The available data examined the following comparisons:
1. Ampicillin solution vs. no topical antimicrobial agent
2. Ampicillin powder vs. no topical antimicrobial agent
3. Chloramphenicol vs. no topical antimicrobial agent
4. Rifampin vs. no topical antimicrobial agent
5. Vancomycin powder in hemostatic paste vs. hemostatic paste
6. Autologous platelet-rich plasma (APRP) (spray or gel) vs. no APRP
For all comparisons, SSI was the critical outcome for decision-making. Wound dehiscence, wound closure, and product-related
adverse event outcomes were also evaluated. The evidence for the pharmacologic antimicrobial prophylactic agent comparators
consists of 6 RCTs,143-148 and for the APRP comparator the evidence consists of 4 RCTs.149-152 APRP provides a platelet concentrate
commonly used to enhance both wound hemostasis (formation of a fibrin clot) and wound healing (clot provides a matrix for the
migration of tissue-forming cells and endothelial cells involved in angiogenesis and thus the remodeling of the clot into repair
tissue).153,154 These characteristics have led to a significant increase in the use of APRP therapies for the treatment of chronic wounds
and multiple orthopaedic conditions including bone repair, tendon, and soft tissue injuries.155,156 In addition, in vitro studies have
demonstrated that APRP holds strong bactericidal activity and suggest its potential value as an adjunct topical antimicrobial
prophylactic agent for use at the time of surgical incision closure.157,158 In all studies, both groups received parenteral AMP. The
findings of the evidence review and grades for all important outcomes are shown in eAppendix 2 of the Supplement: GRADE Table
Q2 and Evidence Table Q2B.
Q2B.1. Ampicillin solution vs. no topical antimicrobial agent
In elective colorectal surgeries, low-quality evidence suggests no benefit to application of ampicillin solution to the subcutaneous and
subfascial layers when combined with bowel prep and AMP for 3 days postoperatively. This was based on 1 RCT145 (N=203) at
moderate risk of bias. This RCT included patients with previously known infections, including 1 patient with Fourniers Gangrene.
This study noted no adverse events associated with the intervention.
In acute appendectomies, moderate-quality evidence suggested a benefit to cleaning the subcutaneous tissues with ampicillin solution-
soaked gauze. This was based on 1 RCT146 (N=246) at moderate risk of bias. This reduction in SSI was not present in the simple, acute
appendicitis cases, but was significant in the perforated and gangrenous appendicitis cases. Both groups received preoperative
intramuscular AMP.
Q2B.2. Ampicillin powder vs. no topical antimicrobial agent
In elective colorectal surgeries, moderate-quality evidence suggested no benefit to ampicillin powder applied to the subfascial and
subcutaneous layers when compared with no topical antimicrobial. This is based on 1 RCT147 in (N=170) at moderate risk of bias.
AMP was administered preoperatively and was continued postoperatively for 2 doses over 12 hours for both groups.
Q2B.3. Chloramphenicol vs. no topical antimicrobial agent
Moderate-quality evidence suggested no benefit of topical chloramphenicol ointment in combination with parenteral AMP. This was
based on no difference in SSI in 1 small study at low risk of bias in 92 hemi-arthroplasty or dynamic hip screw fixation procedures for
hip fractures.143
Q2B.4. Rifampin vs. no topical antimicrobial agent
Low-quality evidence suggested a benefit of topical rifampin in combination with parenteral AMP. This was based on a reduced risk
of wound leakage, fewer local signs of inflammation, and reduced risk of wound dehiscence at the umbilical port site in 1 very small
(N=48) laparoscopic cholecystectomy study at moderate risk of bias.144 Umbilical port-site infection was defined as purulent wound
leakage. Based on results reported in a histogram, at 12 hours postoperatively, 71% of patients had purulent wound leakage including
almost half of the rifampin and all of the control groups. By 24 hours, the entire control group remained infected; a week later, only 2
infections remained. It is not clear if any of these were true infections.
Q2B.5. Vancomycin powder in hemostatic paste vs. hemostatic paste alone
Low-quality evidence suggested a benefit to applying vancomycin powder mixed with hemostatic paste to the cut sternal edges during
heart surgery. This was based on 1 RCT148 (N=416) at high risk of bias evaluating the effectiveness of vancomycin powder mixed
with hemostatic paste for the prevention of mediastinal/sternal SSI. This study showed a reduction in mediastinal/sternal SSI when
vancomycin powder was mixed with hemostatic paste and applied to cut sternal edges versus hemostatic paste alone applied to cut
sternal edges.
Other guidelines
Clinical practice guidelines based on a review of the evidence and expert opinion have recommendations both for82 and against95 the
use of non-parenteral antimicrobials in the prevention of SSI. There are also strong recommendations against the use of antimicrobial
2017 American Medical Association. All rights reserved. 17
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
ointments or creams on umbilical catheter insertion sites and other insertion sites, because of their potential to promote fungal
infections and antimicrobial resistance.159 These recommendations exclude dialysis catheters.
Q2B.6. Autologous platelet-rich plasma (spray or gel) vs. nothing
Moderate-quality evidence suggested no benefit of APRP spray or gel in combination with parenteral AMP. This was based on no
difference in SSI in a meta-analysis (N=452) of 4 small RCTs: 3 studies in cardiac procedures (low149, moderate151 and high152 risk of
bias) and 1 study in total knee arthroplasty (TKA) procedures150 (low risk of bias). Each individual study found no difference. The
cardiac studies applied APRP spray149,152 or gel151 (produced using the same type of commercial platelet concentrate system) to the
saphenous vein harvest site149,151 and/or the sternum.151,152 The TKA study150 applied APRP spray (produced using a different platelet
concentrate system than the cardiac studies) to the femoral and tibial cut bone surfaces and joint capsule followed by platelet poor
plasma sprayed on the subcutaneous tissue. Moderate-quality evidence from this latter study150 suggested significantly increased risk
of delayed total wound closure at 2 weeks postoperatively. Three of the 4 RCTs150-152 reported either industry support of the study or
receiving study supplies from the manufacturer.
Q2C. How safe and effective are antimicrobial-coated sutures, when and how should they be used?
The available data examined triclosan-coated sutures (absorbable) versus sutures without triclosan (absorbable) for the prevention of
SSI. The evidence for this question consists of 14 RCTs.160-173 For this comparison, overall SSI and deep SSI were the critical
outcomes for decision-making. Organ/space SSI, superficial SSI, ASEPSIS score174 (where points are given for Additional treatment,
the presence of Serous discharge, Erythema, Purulent exudate, Separation of the deep tissues, the Isolation of bacteria, and the
duration of inpatient Stay), antimicrobial resistance, wound dehiscence, and product-related adverse event outcomes were also
evaluated.
Moderate-quality evidence suggested tradeoffs in the use of triclosan-coated sutures to reduce overall SSI rates. A meta-analysis
(N=5388) of 14 RCTs160-173 in colorectal, abdominal, lower limb revascularization, cardiac, breast, cerebrospinal fluid shunt, and
mixed surgeries provided high-quality evidence for the reduction in the incidence of overall SSI with the use of triclosan-coated
sutures. However, a meta-analysis of 2 RCTs161,163 (N=1285) reporting on the outcome of deep SSI provided moderate-quality
evidence suggesting no benefit to using triclosan-coated sutures to prevent deep SSI. Given that all 14 RCTs utilized triclosan-coated
sutures in the deep and/or fascial layer, it was considered important to identify a benefit in the layer in which they are used.
Unfortunately, most of the 14 RCTs evaluating triclosan sutures only examined overall SSI and did not stratify analyses by SSI
type. Only the 2 aforementioned RCTs actually reported on deep SSI. The tradeoff between benefit in overall SSI and no benefit
in deep SSI (the layer most important to the evaluation of these deep antimicrobial sutures) results in a Category II recommendation
to consider their use, rather than a Category I recommendation to always use these sutures.
In addition, low-quality evidence based on a meta-analysis of 4 RCTs161,162,165,168 (N=1081) in appendectomies and coronary artery
bypass grafts (CABG), elective colorectal, and pediatric cerebrospinal fluid shunt surgeries, with heterogeneous patients and closure
types, suggested no difference in organ/space SSI rates when triclosan-coated sutures were used primarily in the deep layer. Moreover,
high-quality evidence suggested no benefit to using triclosan-coated sutures for the reduction of superficial SSI when this outcome
was specifically reported. This is based on a meta-analysis of 4 RCTs161,163,165,171 (N=1922) in appendectomies and CABG, open
abdominal, and breast cancer surgeries, where triclosan-coated sutures were used in deep closure in all 4 RCTs. Only 1 of the 4
RCTs171 with superficial SSI as an outcome utilized triclosan-coated sutures in cutaneous closure.
Moderate-quality evidence suggested no difference in SSI in colorectal surgeries where absorbable triclosan-coated sutures were used
to close the deep abdominal and fascial layers. This was based on a meta-analysis (N=1912) of 5 RCTs. 163,167-170,175 Administration of
bowel prep, length of postoperative AMP, suture type, length of follow-up, SSI definition, and method of closure were not uniform
across studies.
High-quality evidence suggested a benefit to using absorbable triclosan-coated sutures to close the abdominal and fascial layers in
abdominal surgeries, laparotomies and appendectomies (excluding colorectal surgeries). This was based on a meta-analysis (N=1208)
of 3 RCTs.161,163,167 Administration of postoperative AMP, suture type, length of follow up, SSI definition, and method of closure were
not uniform across studies.
High-quality evidence suggested a benefit to using absorbable triclosan-coated sutures in a subgroup of all surgery types excluding
colorectal and abdominal surgeries. This was based on a meta-analysis (N=2183) of 8 RCTs.160,162,164-166,171-173 Surgical populations
included CABG, lower limb revascularization, breast cancer surgery, pediatric cerebrospinal fluid shunt, and mixed pediatric and adult
surgeries. Length of postoperative AMP, suture type, length of follow up, SSI definition, and method of closure were not uniform
across studies.
In terms of harms, low-quality evidence suggested no difference between groups in antimicrobial resistance. Eight RCTs161,162,165,167-
169,172,173
reported no difference in cultured antimicrobial resistant bacteria between groups. However, none of the studies evaluated
triclosan resistance. This evaluation is limited by the absence of standardized methods for determining triclosan-resistance. Low-
quality evidence also suggested no difference in wound dehiscence between groups. This is based on a meta-analysis of 3
2017 American Medical Association. All rights reserved. 18
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
RCTs163,166,170 (N=1582) in elective colorectal, CABG, and open abdominal surgeries. Moreover, moderate-quality evidence consisting
of 2 RCTs166,171 suggested no difference in ASEPSIS scores in breast cancer surgeries and CABG open vein harvesting. Lastly, low-
quality evidence suggested no difference in product-related adverse events, based on 4 RCTs160-163 which reported no product-related
adverse events for either suture type. The authors of 5 of the 14 RCTs reported receiving funds from and/or being employed by the
manufacturer of triclosan-coated sutures.162,163,166,167,171
The findings of the evidence review, results by surgical procedures, and grades for all important outcomes are shown in eAppendix 2
of the Supplement: GRADE Table Q2 and Evidence Table Q2C.
Q2D. How safe and effective are antimicrobial dressings applied to surgical incisions following primary closure in the
operating room?
The available data examined silver-impregnated dressings versus standard dressing or standard gauze and tape for the prevention of
SSI. This data consisted of 2 RCTs. The evidence for this question consists of 1 RCT176 at moderate risk of bias and 1 RCT177 at low
risk of bias, both in elective colorectal surgeries. For this comparison, all SSI outcomes were critical outcomes for decision-making.
The duration of inpatient stay and product-related adverse event outcomes were also evaluated.
Moderate-quality evidence suggested no benefit to silver impregnated dressings. This was based on no difference in overall,
organ/space, deep, or superficial SSI in 1 small RCT177 (N=112). Dressings were removed on the seventh postoperative day in the
intervention group and as necessary in the control group. Patients received mechanical bowel prep in accordance with predefined
protocols. No adverse events related to the study were noted. An additional small RCT176 (N=109) suggested a reduction in superficial
SSI related to silver impregnated dressings; however, the SSI definition used in this study included antibiotic treatment for any
questionable infection. There was no difference in deep infections in this study. In both studies, authors reported receiving funds from
the dressing manufacturer.
The findings of the evidence review and the grades for all important outcomes are shown in eAppendix 2 of the Supplement: GRADE
Table Q2 and Evidence Table Q2D.
The search did not identify RCTs or SRs that evaluated the safety and effectiveness of other antimicrobial dressings (e.g., iodine or
other antimicrobial ointment-impregnated dressing) applied to surgical incisions closed primarily in the operating room (i.e., the skin
edges are re-approximated at the end of the procedure) and their impact on the risk of SSI.64 The search identified a SR of 16 RCTs
evaluating various non-antimicrobial dressings.178 This SR found no evidence to suggest that either covering the wound was effective
or that any one non-antimicrobial dressing was more effective than another in reducing the risk of SSI in surgical incisions that were
closed primarily in the operating room. This Guideline does not address prevention of SSI in trauma-related procedures, in surgical
incisions left open to heal by secondary intention (i.e., left open in the operating room to be closed later, left open to heal by
granulation, or which break open postoperatively), or burns.
2017 American Medical Association. All rights reserved. 19
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Q2. Recommendations
2A.1. Randomized controlled trial evidence suggests uncertain tradeoffs between the benefits and harms
regarding intraoperative antimicrobial irrigation (e.g., intra-abdominal, deep or subcutaneous tissues) for
the prevention of SSI. Other organizations have made recommendations based on the existing evidence
and a summary of these recommendations can be found in the Other Guideline section of the narrative
summary for this question. (No recommendation/unresolved issue) 141,142 (Guideline Question 2A)
2A.2. The search did not identify randomized controlled trials evaluating soaking prosthetic devices in
antimicrobial solutions prior to implantation for the prevention of SSI. (No
recommendation/unresolved issue) (Guideline Question 2A)
2B.1. Do not apply antimicrobial agents (i.e., ointments, solutions, or powders) to the surgical incision for the
prevention of SSI. (Category IB strong recommendation; low-quality evidence) 143-148 (Guideline
Question 2B)
2B.2. Application of autologous platelet-rich plasma is not necessary for the prevention of SSI. (Category II
weak recommendation; moderate-quality evidence suggesting a trade-off between clinical benefits
and harms) 149-152 (Guideline Question 2B)
2C. Consider the use of triclosan-coated sutures for the prevention of SSI. (Category II weak
recommendation; moderate-quality evidence suggesting a trade-off between clinical benefits and
harms) 160-173,175 (Guideline Question 2C)
2D. Randomized controlled trial evidence suggests uncertain tradeoffs between the benefits and harms
regarding antimicrobial dressings applied to surgical incisions following primary closure in the operating
room for the prevention of SSI. (No recommendation/unresolved issue)176,177 (Guideline Question 2D)
4.1C. GLYCEMIC CONTROL
Q3. How do perioperative blood glucose and hemoglobin A1c levels impact the risk of SSI, and what are their optimal
perioperative target levels in diabetic and non-diabetic patients?
To answer this question, analysis focused on:
A) Blood glucose
B) Hemoglobin A1c
C) Optimal perioperative target levels
D) Risk of SSI
Q3A. Blood glucose and optimal perioperative target levels
The available data examined strict versus standard blood glucose control in the prevention of SSI.
For this comparison, SSI and hypoglycemia were considered the critical outcomes for decision-making. Each study reported a primary
composite outcome variable that included SSI. Mortality, length of hospital stay, and surgical intensive care unit (SICU) stays were
also evaluated in weighing the risks and benefits of perioperative glycemic control. The evidence for this question consists of 2 RCTs
in cardiac surgery patients with glycemic control protocols (intravenous, intensive insulin therapy) instituted intraoperatively and
continued in the SICU for 24-36 hours.179,180 In both of these studies, 70-80% of patients were non-diabetics, highlighting the
importance of glycemic control in both diabetic and non-diabetic surgical populations. The findings of the evidence review and the
grades for all important outcomes are shown in eAppendix 2 of the Supplement: GRADE Table Q3 and Evidence Table Q3.
Moderate-quality evidence suggested no benefit of strict (80100 mg/dL180 or 80130 mg/dL179) as compared with standard blood
glucose target levels (<200 mg/dL180 or 160200 mg/dL179) in diabetic and non-diabetic cardiac patients. This was based on no
differences between groups for both the composite outcome variable and SSI in both studies. In Gandhi et al.180 (N=371), the
composite outcome variable included: death, sternal wound infections, prolonged pulmonary ventilation, cardiac arrhythmias, heart
block requiring pacemaker or cardiac arrest, stroke or acute renal failure within 30 days postoperatively. In Chan et al.179 (N=109), the
composite infection outcome included pneumonia, urinary tract infection, sepsis, septic shock, wound infection, bloodstream
infection, and catheter infection (did not specify if venous or urinary).
2017 American Medical Association. All rights reserved. 20
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
High-quality evidence suggested no increased risk of hypoglycemia with strict blood glucose target levels. This was based on no
differences between groups for the number of hypoglycemic episodes in the SICU180 or the ratio of hypoglycemic episodes per
number of glucose measurements.179 Hypoglycemia definitions differed among studies: <60 mg/dL in Gandhi and <50 mg/dL in
Chan. While there was no difference between groups for the number of hypoglycemic episodes in the SICU, in Chan et al., both
groups reported a higher proportion of hypoglycemia postoperatively as compared with intraoperatively, suggesting the importance of
continued close monitoring of glucose levels and the risk of hypoglycemic episodes in the postoperative period, even with standard
glycemic control. No clinical complications resulting from hypoglycemia were reported at 30 days of follow-up. In 1 study, authors
reported receiving funds from an insulin manufacturing company. 180
Other guidelines
While previous CDC guideline recommendations did not specify a perioperative blood glucose target level, they reported that in
diabetics increased glucose levels (>200 mg/dL) in the immediate postoperative period (48 hours) were associated with increased
risk of SSI.64 Blood glucose target level of <200 mg/dL became standard clinical practice. Both studies reviewed in this guideline
used <200 mg/dL as the upper blood glucose target level.179,180 Recently published professional society guidelines have recommended
a slightly lower absolute serum blood glucose target level of <180 mg/dL in diabetic84,181,182 and non-diabetic,84,181 non-critically ill
patients. In critically ill patients, blood glucose target levels <150180 mg/dL183 and 140200 mg/dL184 have been recommended. For
terminally ill patients, those with limited life expectancy, or those at high risk for hypoglycemia, a blood glucose target level of 200
mg/dL has been recommended.182 Intensive insulin therapy (blood glucose target levels of 80110 mg/dl) to normalize blood glucose
in the intensive care unit setting (surgical and medical) is not recommended in either diabetic or non-diabetic patients.84,184
Q3B. Perioperative hemoglobin A1C and optimal target levels
The search did not identify RCTs or SRs examining the association between hemoglobin A1c levels and risk of SSI.
Q3. Recommendations
3A.1. Implement perioperative glycemic control and use blood glucose target levels <200 mg/dL in diabetic and
non-diabetic patients. (Category IA strong recommendation; high to moderate-quality evidence)
179,180
(Guideline Question 3)
3A.2. The search did not identify randomized controlled trials evaluating lower (<200 mg/dL) or narrower blood
glucose target levels than recommended in this guideline, nor the optimal timing, duration, or delivery
method of perioperative glycemic control for the prevention of SSI. Other organizations have made
recommendations based on the existing evidence and a summary of these recommendations can be found
in the Other guidelines section of the narrative summary for this question. (No
recommendation/unresolved issue) (Guideline Question 3)
3B. The search did not identify randomized controlled trials evaluating the optimal hemoglobin A1c target
levels for the prevention of SSI in diabetic and non-diabetic patients. (No recommendation/unresolved
issue) (Guideline Question 3)
4.1D. NORMOTHERMIA
Q4. How safe and effective is the maintenance of perioperative normothermia in reducing the risk of SSI?
The available data examined the following comparisons:
1. Warming vs. no warming
2. Warming: perioperative vs. intraoperative only
For all comparisons, SSI was the critical outcome for decision-making. ASEPSIS score, mortality, blood loss, core temperature, length
of hospital stay, and duration of surgery outcomes were also evaluated. The evidence for this question consists of 3 RCTs.185-187 The
lower limit of normothermia has been inconsistently defined, ranging from a core temperature of 95.9F to 96.8F (35.5C-36C). The
findings of the evidence review and the grades for all important outcomes are shown in eAppendix 2 of the Supplement: GRADE
Table Q4-5 and Evidence Table Q4.
Q4A.1. Warming vs. no warming
High-quality evidence suggested a benefit of patient warming over no warming. This was based on a reduced risk of SSI in a meta-
analysis (N=616) of 2 RCTs with warming and maintenance of normothermia using various warming techniques in patients
undergoing elective hernia repair, varicose vein surgery, and breast surgery (preoperative warming)186 and elective colorectal surgery
(intraoperative warming).185 Normothermia was also associated with reduced risk of ASEPSIS scores >20, lower mean units of blood
transfused per patient, fewer patients transfused, and reduced hospital length of stay.185 No difference in mortality was observed.185
Both of these studies reported receiving funds from a warming equipment manufacturer.
2017 American Medical Association. All rights reserved. 21
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Q4A.2. Warming: perioperative vs. intraoperative only
Moderate-quality evidence suggested a benefit of perioperative warming. This was based on reduced incidence of SSI with
perioperative warming in 1 RCT of 103 patients undergoing elective major abdominal surgery.187
Q4. Recommendation
4. Maintain perioperative normothermia. (Category IA strong recommendation; high to moderate- quality
evidence) 185-187 (Guideline Question 4)
Q5. What are the most effective strategies for achieving and maintaining perioperative normothermia?
The search did not identify RCTs or SRs that evaluated the most effective strategies for achieving and maintaining perioperative
normothermia and their impact on the risk of SSI.
Other guidelines
Evidence-based clinical practice guidelines provide recommendations on perioperative management of normothermia including risk
factor assessment, temperature monitoring tools, and the safety and effectiveness of warming devices.188-191 Recently published
professional society guidelines have recommended a minimum temperature of 95.9F (35.5C) during the perioperative period.84
Q5. Recommendation
5. The search did not identify randomized controlled trials evaluating strategies to achieve and maintain
normothermia, the lower limit of normothermia, or the optimal timing and duration of normothermia for the
prevention of SSI. Other organizations have made recommendations based on observational data and a
summary of these recommendations can be found in the Other guidelines section of the narrative summary
for this question. (No recommendation/unresolved issue) (Guideline Question 5)
4.1E. OXYGENATION
Q6. In patients with normal pulmonary function, how safe and effective is the perioperative use of increased fraction of
inspired oxygen (FiO2) in reducing the risk of SSI?
To answer this question, 3 settings of oxygen delivery were analyzed:
A) General anesthesia: intraoperative endotracheal intubation and postoperative non-rebreathing mask;
B) Neuraxial anesthesia: intraoperative and postoperative non-rebreathing mask; and
C) Post-operative only: facemask and/or nasal cannula.
Q6A. General anesthesia: intra-operative only endotracheal intubation, 80% oxygen vs. 30% oxygen both without nitrous
oxide
For all comparisons, SSI was the critical outcome for decision-making. Adverse events were also evaluated.
Moderate-quality evidence suggested no benefit to supplemental 80% FiO2 compared with 30% FiO2 administered via endotracheal
intubation during the intraoperative period only. In 1 study192 at low risk of bias, 434 patients underwent general anesthesia for
abdominal, gynecologic and breast surgeries. Administration of FiO2 commenced after intubation and ended at extubation. In cases
where extubation was delayed beyond the end of the surgery, the FiO2 was maintained at the programmed level and oxygen was
administered during the postoperative period at the physicians discretion. There were significantly more protocol deviations in the
control group; the reasons for these deviations included desaturation and/or bradycardia. No difference was seen between groups in
adverse events, including nausea and vomiting, hypotension, and sternal pain. The authors of this study reported receiving study
funding from a medical oxygen supply company.
The findings of the evidence review and the grades for all important outcomes are shown in eAppendix 2 of the Supplement: GRADE
Table Q6-7 and Evidence Table Q6.
Q6B. General anesthesia: intra-operative endotracheal intubation and postoperative non-rebreathing mask
The available data examined the following comparisons:
1. 80% oxygen vs. 30% oxygenboth without nitrous oxide
2017 American Medical Association. All rights reserved. 22
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2. 80% oxygen/20% nitrous oxide vs. 35% oxygen/65% nitrous oxideboth with nitrous oxide started 30 minutes after surgical
incision
For all comparisons, SSI was the critical outcome for decision-making. ASEPSIS scores, mortality, respiratory failure, atelectasis,
tissue oxygenation, and length of stay were also evaluated. The evidence for this question consists of 7 RCTs.193-199 One study198
represents a subanalysis of a larger study;196 therefore results in the GRADE table reflect solely those of the larger study. The findings
of the evidence review and the grades for all important outcomes are shown in eAppendix 2 of the Supplement: GRADE Table Q6-7
and Evidence Table Q6. The authors of 1 of these studies193 reported receiving study funding from a medical oxygen supply company.
Q6B.1. 80% oxygen vs. 30% oxygenboth without nitrous oxide
Moderate-quality evidence suggested a benefit of supplemental 80% FiO2 administered via endotracheal intubation intraoperatively
and non-rebreathing mask for 26 hours postoperatively in patients under general anesthesia. This was based on a meta-analysis
(N=2622) of 5 RCTs193-196,198,199 at low risk of bias (2 in 791 elective colorectal surgeries,193,195 1 in 235 open reduction and internal
fixation procedures,199 1 in 210 elective open appendectomy194 procedures, and in 1 multicenter, mixed surgical population196,198).
There was no significant difference in adverse events.196,198
The 3 studies reporting a significant SSI reduction all optimized perioperative tissue oxygen delivery by maintaining normothermia
and avoiding hypo or hypervolemia.193-195 Greif et al.,195 the larger colorectal study (N=500), confirmed optimized tissue oxygen
delivery, measuring significantly higher intraoperative and postoperative subcutaneous tissue oxygen tension and higher muscle
oxygen tension using 80% oxygen.
Meyhoff et al., 196,198 the large (N=1386), multicenter, mixed population study of emergency or elective laparotomy for a variety of
general and gynecologic surgical conditions, found no difference in overall, organ/space, deep, or superficial SSI. However, due to a
number of factors, the study failed to optimize tissue oxygen delivery. While the target core temperatures were 96.8F to 98.6F (36C
-37C), the minimum reported temperatures were 95.0F and 95.2F (35.0C and 35.1C) in each group, respectively. More
importantly, fluid replacement was intentionally restricted, limiting postoperative weight gain to less than 1 kg. Mortality at 1430
days was rare, there was no difference between groups, and it was not associated with use of increased oxygenation.193,195 In a recent
follow-up study (median 2.3 years, range 1.33.4), administration of 80% oxygen was associated with significantly increased long-
term mortality only in patients undergoing cancer surgery. The only gynecologic patients included in this study were those with
ovarian cancer.200 It is not clear what other cancer patients were included. One study199 of elective open reduction and internal
fixations of 235 tibial fractures in 217 patients also showed no difference. Optimized tissue oxygen delivery, normothermia, and
normovolemia were not described. This study identified no treatment-associated adverse events.
Q6B.2. 80% oxygen/20% nitrous oxide vs. 35% oxygen/65% nitrous oxideboth groups started nitrous oxide 30 minutes after
incision
Moderate-quality evidence suggested no benefit of supplemental 80% FiO2 (20% nitrous oxide added 30 minutes after incision)
administered via endotracheal intubation intraoperatively and non-rebreathing mask for 26 hours postoperatively in patients under
general anesthesia. This was based on increased risk of SSI (all combined) in 1 small (N=160), mixed surgical population study.197
Several factors may account for the increased incidence of total SSIs in the intervention group. Patients in the 80% FiO2 group had
significantly increased body mass index (BMI), higher blood loss, and were more crystalloid infused. On multivariate logistic
regression analysis, 80% oxygen and remaining intubated postoperatively remained predictive of SSI. Mortality was rare in either
group and unrelated to increased supplemental oxygenation.
Q6C. Neuraxial anesthesia: Intraoperative and postoperative non-rebreathing mask
The available data on the impact of different levels of supplemental increased FiO2 on SSI in patients under regional anesthesia
examined 80% oxygen versus 30% oxygen.
For this comparison, SSI was the critical outcome for decision-making. Length of stay was also evaluated. The evidence for this
question consists of 3 RCTs.201-203 The findings of the evidence review and the grades for all important outcomes are shown in
eAppendix 2 of the Supplement: GRADE Table Q6-7 and Evidence Table Q6.
Moderate-quality evidence suggested no benefit of supplemental 80% FiO2 administered via non-rebreathing mask intra and
postoperatively in patients under neuraxial anesthesia. This was based on no difference in risk of SSI in a meta-analysis of 3 studies201-
203
(N=1559) in cesarean sections. Two studies201,203 (N=728) did not note any protocol used during the study to optimize tissue
oxygenation. The largest study202 (N=831) ensured adequate volume replacement and normothermia.
Q6D. Postoperative only: Facemask and/or nasal cannula
The data available on the impact of different levels of supplemental increased FiO2used in the postoperative period only examined 28
30% oxygen versus room air.
2017 American Medical Association. All rights reserved. 23
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
For this comparison, SSI was the critical outcome for decision-making. SSI type (organ/space, superficial and deep SSI), ASEPSIS
scores, mortality, adverse events, tissue oxygenation, and length of stay were also evaluated. The evidence for this question consists of
2 RCTs.204,205 The findings of the evidence review and the grades for all important outcomes are shown in eAppendix 2 of the
Supplement: GRADE Table Q6-7 and Evidence Table Q6.
Moderate-quality evidence suggested no benefit of supplemental 2830% FiO2 administered via facemask and/or nasal cannula solely
in the postoperative period. This was based on no difference in SSIs from 2 studies.204,205 Turtiainen et al., 204 a lower limb vascular
surgery study (N=274) at low risk of bias, used 30% oxygen via facemask in the recovery room and on the first postoperative day on
the ward, followed by constant oxygen flow of 5 L/min via nasal cannula during the second postoperative day. A significant reduction
in SSI was seen only in isolated groin incisions. Subcutaneous tissue oxygen tension (measured hourly for the first 4 hours, then at 18
and 36 hours) was significantly higher in the supplemental oxygenation group. Whitney et al.,205 a second, smaller study at high risk of
bias in 24 cervical spine procedures reported no wound complications in either group (supplemental 28% oxygen administered at
2L/min via nasal cannula for 36 hours after discharge from the post-anesthesia care unit as compared with room air). Mortality204 and
adverse events204,205 were rare, did not differ between groups, and were unrelated to use of supplemental oxygenation.
Q6. Recommendations
6A. Randomized controlled trial evidence suggests uncertain tradeoffs between the benefits and harms regarding
the administration of increased fraction of inspired oxygen (FiO2) via endotracheal intubation during only the
intraoperative period in patients with normal pulmonary function undergoing general anesthesia for the
prevention of SSI. (No recommendation/unresolved issue) 192 (Guideline Question 6)
6B. For patients with normal pulmonary function undergoing general anesthesia with endotracheal intubation,
administer increased FiO2 intraoperatively and post-extubation in the immediate postoperative period. To
optimize tissue oxygen delivery, maintain perioperative normothermia and adequate volume replacement.
(Category IA strong recommendation; moderate quality evidence) 193-199 (Guideline Question 6)
6C. Randomized controlled trial evidence suggests uncertain tradeoffs between the benefits and harms regarding
the administration of increased FiO2 via facemask during the perioperative period in patients with normal
pulmonary function undergoing general anesthesia without endotracheal intubation or neuraxial anesthesia
(i.e., spinal, epidural, or local nerve blocks) for the prevention of SSI. (No recommendation/unresolved
issue) 201-203 (Guideline Question 6)
6D. Randomized controlled trial evidence suggests uncertain tradeoffs between the benefits and harms regarding
the administration of increased FiO2 via facemask or nasal cannula during only the postoperative period in
patients with normal pulmonary function for the prevention of SSI. (No recommendation/unresolved issue)
204,205
(Guideline Question 6)
Q7. What is the optimal target FiO2 to reduce the risk of SSI; how and when should it be administered?
The search did not identify RCTs or SRs that evaluated both the optimal FiO2 and how and when it should be administered, and
included SSI as an outcome. All studies evaluating the use of supplemental increased oxygenation both intraoperatively and
postoperatively used 80% FiO2 as the target level.
Other guidelines
Evidence-based clinical practice guidelines recommend maintaining patient homeostasis by optimizing oxygenation during major
surgery and in the recovery period (maintaining a >95% hemoglobin saturation) in concert with maintaining both patient temperature
to avoid hypothermia, and adequate perfusion during surgery.84,95
Q7. Recommendation
7. The search did not identify randomized controlled trials evaluating the optimal target level, duration, and
delivery method of FiO2 for the prevention of SSI. Other organizations have made recommendations based
on observational data and a summary of these recommendations can be found in the Other guidelines
section of the narrative summary for this question. (No recommendation/ unresolved issue) ( Question 7)
2017 American Medical Association. All rights reserved. 24
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
4.1F. ANTISEPTIC PROPHYLAXIS
Q8. What are the most effective strategies for preparing the patients skin prior to surgery to reduce the risk of SSI?
To answer this question, 4 subquestions were asked:
A) How safe and effective is preoperative antiseptic bathing or showering?
B) How safe and effective are antiseptic skin preparation agents individually and in combination?
C) How safe and effective is the application of a microbial sealant immediately following intraoperative skin preparation?
D) How safe and effective are plastic adhesive drapes? It should be noted that while the recommendations in this section apply
to patients known to be colonized with S. aureus, they do not separately address the different antiseptic skin preparations that
may be suggested for these patients.
Q8A. How safe and effective is preoperative antiseptic bathing or showering?
The available data examined the following comparisons:
1. Chlorhexidine gluconate (CHG) solution vs. placebo solution
2. CHG solution vs. un-medicated bar soap
3. CHG solution vs. no wash
4. CHG whole body wash vs. partial body wash
5. Aqueous iodophor solution vs. control (routine personal hygiene)
6. CHG washcloth vs. un-medicated bar soap
For all comparisons, SSI was the critical outcome for decision-making. Product-related adverse reactions were also evaluated. The
evidence for this question consists of 1 SR206 (7 RCTs207-213) evaluating CHG solution and 1 RCT214 evaluating povidone iodine
solution. The RCTs span a 26-year period, with 6 published between 1983 and 1992, and 2 between 2008214 and 2009.212 The search
did not identify RCTs or SRs that evaluated optimal preoperative timing, number of showers/baths, or number of product applications
at each shower/bathing episode, and their impact on the risk of SSI. The findings of the evidence review and grades for all important
outcomes are shown in eAppendix 2 of the Supplement: GRADE Table Q8-10 and Evidence Table Q8A.
Q8A.1. CHG solution vs. placebo solution
High-quality evidence suggested no benefit of preoperative bathing or showering with 4% CHG solution as compared with placebo.
This was based on no difference in SSI in both a meta-analysis (N=7791) of 4 RCTs206,207,209,211,212 and a meta-analysis (N=6302)
restricted to only the 2 higher-quality studies.206,207,211 Each individual trial found no difference. Five months into 1 large study, the
placebo solution was found to have antimicrobial properties and was changed; however, the study did not stratify by or exclude that
data.209 Procedures included in the studies were elective or potentially contaminated surgery,207 elective inpatient surgery,209 elective
clean surgical procedures including thyroidectomy, inguinal herniorrhaphy, hip and knee surgery, laminectomy, mastectomy, vascular
surgery,211 and elective plastic surgery of the trunk.212 Number of preoperative showers/baths, amount of antiseptic used per bath,
bathing instructions to each group, intraoperative antiseptic skin preparation agent, use of AMP, and follow-up varied among studies.
Three studies instructed patients to shower207,211,212 and 1 instructed them to shower or bathe.209 Product-related adverse reactions
(irritation, itching, reddening of the skin) were rare and did not differ between groups.206,207,211,212
Q8A.2. CHG solution vs. un-medicated bar soap
High-quality evidence suggested no benefit of preoperative bathing or showering with 4% CHG solution as compared with un-
medicated bar soap. This was based on no difference in SSI in a meta-analysis (N=1443) of 3 RCTs.206,208-210 Heterogeneity for this
comparison was high. Only the largest study (N=1315) reported a reduction in SSI with 4% CHG; however, no special
showering/bathing instructions were given to the un-medicated bar soap group, whereas great care was taken to ensure that the
patients using [CHG]complied with the instructions.209 Of the 2 smaller, lesser-quality studies, one208 suggested a higher rate of
SSI with CHG, while the other210 suggested no difference. Number of preoperative baths, bathing instructions, intraoperative
antiseptic skin preparation agent, AMP use, procedures, and follow up varied among studies. One study instructed patients to bathe,208
1 to shower,210 and 1 to shower or bathe.209
Q8A.3. CHG solution vs. no wash
Moderate-quality evidence suggested no benefit of preoperative showering with 4% CHG solution as compared with no wash. This
was based on no difference in a meta-analysis (N=1142) of 3 RCTs.206,210,212,213 Despite instructions not to shower, it is unclear
whether the no wash groups showered. The largest study213 favored 4% CHG, while the other 2210,212 suggested no difference.
Heterogeneity for this comparison was significant. Studies included outpatient and inpatient procedures, patients undergoing
vasectomy,210 plastic surgery of the trunk,212 and elective, clean biliary tract, inguinal hernia, or breast cancer213 procedures. There
were also differences in SSI definitions among studies.
Q8A.4. CHG whole body vs. partial body wash
Moderate-quality evidence suggested a benefit of a CHG shower (i.e., a whole body wash including the scalp) as compared with a
partial body wash (restricted to the proposed surgical site). This was based on reduced risk of SSI with whole body washing (1 time, 2
2017 American Medical Association. All rights reserved. 25
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
applications on the afternoon before surgery) in 1 large RCT (N=1093) of elective clean biliary tract, inguinal hernia, and breast
cancer procedures.206,213
Q8A.5. Aqueous iodophor solution vs. control (routine personal hygiene)
Very low-quality evidence suggested no benefit of preoperative shower with 10% aqueous iodophor solution as compared with routine
personal hygiene. This was based on no infections reported in either group in 1 small RCT (N=114) in elective, clean plastic surgical
procedures (thorax or abdomen) designed to evaluate the products efficacy in reducing skin contamination, not SSI.214
Q8A.6. CHG washcloth vs. un-medicated bar soap
Moderate-quality evidence suggested no benefit of 2 full body wipes with 2% chlorhexidine washcloths the night before and morning
of surgery as compared with a shower with un-medicated bar soap the morning of surgery. This was based on no infections reported in
either group in 1 small RCT215 (N=100) in elective, shoulder surgeries designed to evaluate the products efficacy in reducing skin
contamination, not SSI. In this study, authors reported receiving funds from the CHG washcloth manufacturer.
Other guidelines
Clinical practice guidelines recommend that patients shower or bathe with an antiseptic agent or soap on at least the night before
surgery.64,85,95 This is considered accepted practice. They do not favor the use of one antiseptic agent over another. There may be
contraindications for specific antiseptic-agent use in some patients or surgical procedures.
Q8B. How safe and effective are antiseptic skin preparation agents individually and in combination?
The available data examined the following comparisons:
1. Aqueous iodophor: 1-step vs. 2-step
2. Aqueous iodophor (1- or 2-step) vs. iodophor in alcohol (1-step with or without adhesive drape)
3. CHG-alcohol (1- or 2-step) vs. aqueous iodophor (1- or 2-step)
4. CHG-alcohol (1- or 2-step) vs. iodophor-alcohol (1- or 2-step)
a. CHG-alcohol (2-step) vs. iodophor-alcohol (2-step)
b. CHG-alcohol (1-step) vs. iodophor-alcohol (1-step)
For all comparisons, SSI was the critical outcome for decision-making. Product-related adverse event outcomes were also evaluated.
The evidence for this question consists of 14 RCTs.216-229 The findings of the evidence review and the grades for all important
outcomes are shown in eAppendix 2 of the Supplement: GRADE Table Q8-10 and Evidence Table Q8B.
Q8B.1. Aqueous iodophor: 1-step vs. 2-step
High-quality evidence suggested no benefit of using 2-step as compared with 1-step aqueous iodophor for skin preparation of the
surgical site. This was based on no difference in SSI in 2 RCTs at moderate risk of bias.220,227 One study in 234 clean (30%) and clean-
contaminated (70%) oncologic, non-laparoscopic abdominal procedures compared povidone iodine paint (1% iodine) to a 5-minute
povidone iodine scrub (0.75% iodine) followed by povidone iodine paint (1% iodine).220 Another study in 108 CABG procedures did
not report the product concentration or scrub duration.227 In the latter study, patients were also instructed to take antimicrobial showers
(unspecified product) the evening before and the morning of surgery.
Q8B.2. Aqueous iodophor (1- or 2-step) vs. iodophor in alcohol (1-step with or without adhesive drape)
Low-quality evidence suggested no benefit of iodophor in alcohol as compared with aqueous iodophor. This was based on no
difference in SSI in a meta-analysis (N=626) of 5 RCTs including 4 RCTs at moderate risk221,222,226,227 and 1 at low risk225 of bias.
Only 1 study at moderate risk of bias in CABG procedures showed a reduced risk of sternal SSI with iodophor in alcohol (with or
without plastic adhesive drape).227 A second study (low risk of bias) in CABG procedures using iodophor impregnated plastic
adhesive drape at the sternal site showed no difference between groups.225 The remaining studies, at moderate risk of bias, reported no
infections in THA and TKA,221 shoulder,226 and foot and ankle222 procedures. However, each was designed to evaluate the products
efficacy in reducing skin contamination, not SSI.
Q8B.3. CHG-alcohol (1- or 2-step) vs. aqueous iodophor (1- or 2-step)
High-quality evidence suggested a benefit of CHG-alcohol as compared with aqueous iodophor. This was based on a reduced risk of
SSI in a meta-analysis (N=1976) of 5 RCTs (2 low risk,219,228 1 moderate risk,226 and 2 high risk217,224 of bias) and no difference in
product-related adverse events. Only 1 large study showed a reduced risk of SSI in multiple mixed clean-contaminated abdominal and
non-abdominal (thoracic, gynecologic, and urologic) procedures.219 CHG-alcohol was specifically associated with reduced risk of
superficial and deep incisional SSI, but not organ/space SSI or sepsis. The study in clean hernia repairs (herniotomy, herniorrhaphy, or
hernioplasty) showed no difference between groups.228 In both of these studies, authors reported receiving funds from and/or being
employed by the manufacturer of the CHG-alcohol product. Of the 3 studies at moderate or high risk of bias, 1 in clean, clean-
contaminated or contaminated general surgery224 procedures showed no difference, and the studies in clean elective shoulder226 and
foot and ankle217 procedures reported no infections; however, each was designed to evaluate the products efficacy in reducing skin
contamination, not SSI.
2017 American Medical Association. All rights reserved. 26
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
High-quality evidence from 2 studies suggested no difference in product-related adverse events, including skin irritation or pruritus or
erythema around the wound.219,224
Q8B.4. CHG-alcohol (1- or 2-step) vs. iodophor-alcohol (1- or 2-step)
High-quality evidence suggested no benefit of CHG-alcohol (1- or 2-step) as compared with iodophor alcohol (1-or 2-step). This was
based on no difference in SSI in a meta-analysis (N=1323) of 6 RCTs.216,218,223,226,229,230 Three studies (1 at low risk,216 1 at moderate
risk,218 and 1 at high risk229 of bias) compared 2-step application, and 3 studies223,226,230 at moderate risk of bias compared 1-step
product application. There was no difference in SSI in individual meta-analyses of 2-step or 1-step product application. Details
are available under the individual comparators below.
Q8B.4.a. CHG-alcohol (2-step) vs. iodophor-alcohol (2-step)
High-quality evidence suggested no benefit of 2-step CHG-alcohol as compared with 2-step iodophor-alcohol. This was based on no
difference in SSI in 3 studies that compared 0.5% chlorhexidine gluconate and alcohol with 10% povidone-iodine (1% available
iodine) and 23% isopropyl alcohol.216,218,229 No preoperative antiseptic shower protocol was reported in the studies. The large,
moderate risk of bias study in a mixed general surgery population reported no difference.216 CHG-alcohol was associated with a
significant reduction in SSI in biliary and other clean procedures. One study (at high risk of bias) in elective, clean, plastic surgery
breast procedures reported no difference between groups.229 The smallest study (at moderate risk of bias) in foot procedures reported
no infections in either group.218 However, the study was designed to evaluate the products efficacy in reducing skin contamination,
not SSI.
Q8B.4.b. CHG-alcohol (1-step) vs. iodophor-alcohol (1-step)
High-quality evidence suggested no benefit of 1-step CHG-alcohol as compared with 1-step iodophor-alcohol. This was based on no
difference in SSI in 3 studies at moderate risk of bias that compared 2% chlorhexidine gluconate with 70% alcohol (water insoluble
film) to 0.7% iodine with 74% alcohol (water insoluble film).223,226,230 One study in shoulder procedures (96 arthroscopies and 4
arthroplasties) reported no infections in either group.226 Patients were instructed to shower the evening prior to surgery (product not
reported). Iodophor-impregnated plastic adhesive drapes were applied to the shoulder arthroplasties operative site. The second study
reported only 1 wound infection following 80 foot and ankle procedures.223 Patients were not instructed to take an antiseptic shower
prior to surgery. The third study230 of 100 patients undergoing elective lumbar spine surgery reported no deep or superficial SSI in
either group at 6 months follow-up. Patients were instructed to adhere to routine bathing practices. All 3 studies were designed to
evaluate the products efficacy in reducing skin contamination, not SSI, and all received funding by one or both product
manufacturers.
Other guidelines
Clinical practice guidelines recommend skin preparation with an antiseptic agent, but do not favor one antiseptic agent over
another.64,95,231 Recently published professional society guidelines have recommended skin preparation with alcohol-containing
preoperative skin preparatory agents.84 There may be contraindications to the use of specific antiseptic skin preparation agents for
specific patients.
Q8C. How safe and effective is the application of a microbial sealant immediately following intraoperative skin preparation?
The available data examined the application of a cyanoacrylate-based microbial skin sealant immediately after skin preparation as
compared to no sealant.
For this comparison considered SSI was the critical outcome for decision-making. Product-related adverse events were also evaluated.
The evidence for this question consists of 4 RCTs.232-235 The findings of the evidence review and the grades for all important outcomes
are shown in eAppendix 2 of the Supplement: GRADE Table Q8-10 and Evidence Table Q8C.
Low-quality evidence suggested no benefit of cyanoacrylate-based microbial skin sealant applied immediately following skin
preparation. This was based on no difference in SSI in a meta-analysis (N=609) of 4 RCTs evaluating surgical site skin preparation
with povidone iodine alcohol232,234,235 or aqueous povidone iodine 233,234 solution followed by application of cyanoacrylate-based skin
sealant before skin incision (1 CABG sternal and/or venous harvest site,234 1 CABG leg saphenous vein harvest site,232 1 open inguinal
hernia repair233, and 1 pediatric scoliosis correction235). The 2 CABG studies also followed skin sealant application with plastic
adhesive drape application. One study at moderate risk of bias235 and 2 studies at low risk of bias232,233 suggested no difference
between groups. However, due to the low number of events in the latter study, superiority could not be established and study
enrollment ceased once the cyanoacrylate sealant was granted regulatory approval by the FDA (based on porcine data on skin
contamination).233 All studies were funded by and/or authors had a financial relationship with the skin sealant manufacturer. Only 1
small study232 (low risk of bias) suggested a reduced risk of SSI; however, the authors acknowledged that the apparent increased risk
of SSI in the control legs could be explained by their use of a grading system236 whose stringent criteria included minimal erythema or
discharge as SSI. High-quality evidence suggested no significant product-related sensitivity or other adverse events.232-234 In the
inguinal hernia repair study, surgeons reported difficulty incising through the clear film (4/166 patients) and 1 reported visible
flaking of the film at the time of procedure (no report of plastic adhesive drape use).233
2017 American Medical Association. All rights reserved. 27
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Q8D. How safe and effective are plastic adhesive drapes?
The available data examined the following comparisons:
1. Non-iodophor impregnated adhesive drape vs. no drape
2. Iodophor-impregnated adhesive drape vs. no drape
For all comparisons, SSI was the critical outcome for decision-making. The evidence for this question consists of 6 RCTs.227,237-241
The findings of the evidence review and the grades for all important outcomes are shown in eAppendix 2 of the Supplement: GRADE
Table Q8-10 and Evidence Table Q8D.
Q8D.1. Non-iodophor impregnated drape vs. no drape
Moderate-quality evidence suggested no benefit of non-iodophor impregnated plastic adhesive drapes in addition to skin preparation
as compared with skin preparation alone. This was based on no difference in SSI in a meta-analysis (N=1742) of 4 RCTs spanning a
30-year period (19712001), each reporting no difference.237,239-241 The 2 most recent studies237,241 used polyurethane adhesive drapes;
drape material information was not reported in the older239,240 studies. The surgical skin preparation agent applied prior to the
application of the adhesive drapes varied among studies and may have impacted drape adhesion. Studies included general
surgery,239,240 cesarean section,241 and hip fracture237 surgery.
Q8D.2. Iodophor-impregnated drape vs. no drape
High-quality evidence suggested no benefit of iodophor-impregnated plastic adhesive drapes in addition to skin preparation as
compared with skin preparation alone. This was based on no difference in SSI in a meta-analysis (N=1113) of 2 RCTs spanning a 15-
year period (1987-2002), each reporting no difference.227,238 Both studies used povidone iodine alcohol skin preparation (2-step
application in the study at low risk of bias in abdominal procedures238 and 1-step application in the study at moderate risk of bias in
CABG227 procedures).
Other guidelines
Other evidence-based clinical practice guidelines recommend against the routine use of non-iodophor impregnated plastic adhesive
drapes and recommend that if a plastic adhesive drape is required, then an iodophor-impregnated one should be used (unless the
patient has an iodine allergy).84,95,242
Q8. Recommendations
8A. Advise patients to shower or bathe (full body) with soap (antimicrobial or non-antimicrobial) or an
antiseptic agent on at least the night before the operative day. (Category IB strong recommendation;
accepted practice) 206-214 (Guideline Question 8A)
8A.1. Randomized controlled trial evidence suggests uncertain tradeoffs between the benefits and harms
regarding the optimal timing of the preoperative shower or bath, the total number of soap or antiseptic
agent applications, or the use of chlorhexidine gluconate washcloths for the prevention of SSI. (No
recommendation/unresolved issue) 215 (Guideline Question 8A.1)
8B. Perform intraoperative skin preparation with an alcohol-based antiseptic agent, unless contraindicated.
(Category IA strong recommendation; high-quality evidence) 216-230 (Guideline Question 8B)
8C. Application of a microbial sealant immediately following intraoperative skin preparation is not necessary
for the prevention of SSI. (Category II weak recommendation; low-quality evidence suggesting a
trade-off between clinical benefits and harms) 232-235 (Guideline Question 8C)
8D. The use of plastic adhesive drapes with or without antimicrobial properties, is not necessary for the
prevention of SSI. (Category II weak recommendation; high to moderate-quality evidence
suggesting a trade-off between clinical benefits and harms) 227,237-241 (Guideline Question 8D)
Q9. How safe and effective is antiseptic irrigation prior to closing the surgical incision?
The available data examined aqueous iodophor irrigation versus normal saline for the prevention of SSI.
For this comparison, superficial and deep SSIs and organ/space abscess were the critical outcomes for decision-making. Product-
related adverse events including wound healing and iodine toxicity outcomes were also evaluated. The evidence for this question
consists of 7 RCTs.243-249 In all studies, both groups received parenteral AMP, but the specific protocol was not necessarily described.
2017 American Medical Association. All rights reserved. 28
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
The findings of the evidence review and the grades for all important outcomes are shown in eAppendix 2 of the Supplement: GRADE
Table Q8-10 and Evidence Table Q9.
Moderate-quality evidence suggested no benefit of aqueous iodophor peritoneal lavage in contaminated and dirty general surgical
abdominal cases. This was based on no difference in organ/space abscess formation in meta-analysis (N=268) of 3 RCTs.246,247,249
Aqueous iodophor solution amount, concentration, application, and perioperative AMP regimen varied among studies.
Moderate-quality evidence suggested a benefit of intraoperative aqueous iodophor irrigation of the deep incision, in combination with
parenteral AMP, for clean spine procedures. This was based on moderate-quality evidence from a meta-analysis (N=660) of 2 RCTs
suggesting a reduced risk of deep SSI when the deep tissues were irrigated and allowed to soak for 3 minutes with 0.35% povidone
iodine solution, then irrigated with an additional 2 L of normal saline prior to bone grafting and spinal instrumentation.243,244 All
procedures in both studies were performed by the same surgeon. Perioperative AMP included preoperative parenteral dose,
postoperative parenteral dosing for 2 days followed by oral prophylaxis for an additional 3 days. Over 80% of the SSIs were caused by
Methicillin-resistant Staphylococcus aureus (MRSA).
High-quality evidence suggested a benefit of aqueous iodophor irrigation of the subcutaneous tissue in combination with parenteral
AMP for clean-contaminated, contaminated, and dirty open abdominal procedures. This was based on reduced risk of superficial SSI
on meta-analysis (N=329) of 2 RCTS that performed 60 seconds of subcutaneous tissue irrigation with 10% aqueous iodophor
solution prior to wound closure.245,248 The larger 248 study administered parenteral AMP preoperatively and for 48 hours
postoperatively, while the smaller245 study only reported administering perioperative parenteral AMP. Individual meta-analyses of
clean-contaminated (N=149) and dirty (N=90) procedures both showed reduced risk of superficial SSI.
High-quality evidence from 3 studies suggested no increased risk of product-related adverse events244,245,247 or iodine toxicity.245-247
Moderate-quality evidence from 2 studies suggested no wound healing problems.243,245
The search did not identify RCTs or SRs that evaluated the safety and effectiveness of soaking surgical implants (e.g., meshes,
neurosurgical ventricular shunts) in antiseptic solution prior to insertion (in combination with parenteral AMP) and its impact on SSI.
Q9. Recommendation
9A. Consider intraoperative irrigation of deep or subcutaneous tissues with aqueous iodophor solution for the
prevention of SSI. Intra-peritoneal lavage with aqueous iodophor solution in contaminated or dirty
abdominal procedures is not necessary. (Category II weak recommendation; moderate-quality
evidence suggesting a trade-off between clinical benefits and harms) 243-249 (Guideline Question 9)
9B. The search did not identify randomized controlled trials evaluating the soaking of prosthetic devices in
antiseptic solutions prior to implantation for the prevention of SSI. (No recommendation/unresolved
issue) (Guideline Question 9)
Q10. How safe and effective is repeat application of an antiseptic skin preparation agent to the surgical site immediately prior
to closing the surgical incision?
The available data examined the repeat application of aqueous iodophor solution to the patients skin immediately prior to closing the
surgical incision versus no additional application of topical antiseptic agent for the prevention of SSI. For this comparison, SSI was
considered the critical outcome for decision-making.
Low-quality evidence suggested no benefit of repeat application of aqueous iodophor solution to the patients skin immediately prior
to closing the surgical incision, in combination with parenteral AMP. This was based on no difference in SSI (combined or individual
incisional or organ/space SSI) in a small study at high risk of bias, in 107 gastric and colorectal procedures.250
The search did not identify RCTs or SRs that evaluated repeat application of chlorhexidine, chlorhexidine-alcohol, iodophor alcohol
or topical antiseptic agents other than aqueous iodophor solution. The findings of the evidence review and the grades for all important
outcomes are shown in eAppendix 2 of the Supplement: GRADE Table Q8-10 and Evidence Table Q10.
2017 American Medical Association. All rights reserved. 29
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Q10. Recommendation
10. RCT evidence is insufficient to evaluate the tradeoffs between the benefits and harms of repeat application
of antiseptic agents to the patients skin immediately prior to closing the surgical incision for the prevention
of SSI. (No recommendation/unresolved issue) 250 (Guideline Question 10)
4.2. Prosthetic Joint Arthroplasty Section Evidence Review
4.2A. BLOOD TRANSFUSION
Q11. How do perioperative blood transfusions impact the risk of SSI in prosthetic joint arthroplasty patients?
For the general question of risk of any blood transfusion on SSI, SSI was the critical outcome for decision-making. The evidence for
this question consists of 2 RCTs251,252 and 4 OBS.253-256 All of the studies reflect European transfusion practices between 1999 and
2007. Studies were published between 2001 and 2008; however, only 2 report the study periods (19982000).255,256 All studies were at
low risk of bias.
When reported, hemoglobin thresholds for blood transfusion ranged between 8 and 11g/dL. The findings of the evidence review and
the grades for all important outcomes are shown in eAppendix 2 of the Supplement: GRADE Table Q11 and Evidence Table Q11.
High-quality evidence suggested blood transfusions increased the risk of SSI. This was based on increased risk of SSI in a meta-
analysis (N=8493) of 6 studies, 2 RCTs251,252 and 4 OBS,253-256 and a separate meta-analysis (N=7484) of the 4 OBS. Analysis
combined allogeneic, autologous, and autologous plus allogeneic blood transfusion data. Data in both of these meta-analyses may be
driven by 2 OBS with a large number of patients who received allogeneic-only blood transfusion and the possibility of selection bias
inherent in OBS.254,256 In contrast, meta-analysis of the 2 RCTs (N=1009) does not suggest an increased risk of SSI with autologous
and autologous plus additional allogeneic blood transfusions.
Q11A. Are specific blood products associated with a risk of SSI?
The available data examined the following comparisons:
1. Allogeneic blood (any) vs. no transfusion
a. Allogeneic not WBC depleted vs. no transfusion
b. Allogeneic WBC depleted vs. no transfusion
c. Allogeneic buffy coat depleted vs. no transfusion
d. Allogeneic WBC filtered vs. no transfusion
e. Allogeneic lower WBC content vs. allogeneic higher WBC content
2. Autologous blood (any) vs. no transfusion
a. Autologous WBC filtration vs. no transfusion
b. Autologous whole blood vs. no transfusion
c. Autologous not WBC depleted vs. no transfusion
d. Autologous buffy coat depleted vs. no transfusion
e. Autologous lower WBC content vs. autologous higher WBC content
f. Post-operative salvage only vs. autologous donated blood
3. Allogeneic blood (any) vs. autologous blood (any)
a. Allogeneic WBC WBC depleted vs. autologous not WBC depleted
b. Allogeneic WBC filtered vs. autologous buffy coat depleted.
4. Combined autologous and allogeneic (any) vs. no transfusion
a. Combined autologous and allogeneic vs. autologous only
For all comparisons, SSI, PJI, or reoperation due to wound infection were the critical outcomes for decision-making. Wound
disturbance was also evaluated. The evidence for this question consists of 2 RCTs251,252 and 7 OBS253-259 studies. There were
differences among studies, including: surgical procedures; definition of SSI; blood product white blood cell (WBC) content; length of
blood product storage; hemoglobin transfusion trigger levels and other criteria for transfusion; as well as follow-up. In several studies,
missing data resulted in discrepancies in the numbers. The findings of the evidence review and the grades for all important outcomes
are shown in eAppendix 2 of the Supplement: GRADE Table Q11 and Evidence Table 11A.
Q11A.1. Allogeneic blood (any) vs. no transfusion
Low-quality evidence suggested that allogeneic blood transfusions increased the risk of SSI. This was based on increased risk of SSI
in a meta-analysis (N=5737) of 4 OBS253-256 studies in primary and revision THA and TKA and no difference in reoperation due to
wound infection in another OBS.259 See individual comparators in eAppendix 2 of the Supplement: GRADE Table 11 for specific
study findings.
2017 American Medical Association. All rights reserved. 30
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Q11A.2 Autologous blood (any) vs. no transfusion
Moderate-quality evidence suggested that autologous blood transfusions did not increase the risk of SSI. This was based on no
difference in a meta-analysis (N=970) of 2 RCTs.251,252 One large RCT in THA suggested no difference at 90 days of follow-up.251
The second small RCT in THA reported no infections in either group; however, this study was designed to evaluate transfusion
induced immunomodulation, not SSI, and follow-up was limited to 7 days.252 In contrast, 1 large254 (N=912) prospective OBS in
primary and revision THA and TKA suggested reduced risk of SSI and a smaller253 study in primary THA and TKA reported only 1
infection in the transfused group. One RCT reported receiving study supplies from a blood bag manufacturer.251 See individual
comparators in eAppendix 2 of the Supplement: GRADE Table 11 for specific study findings.
Q11A.3. Allogeneic blood (any) vs. autologous blood (any)
Moderate-quality evidence suggested that allogeneic blood transfusions increased the risk of SSI when compared with autologous
transfusions. This was based on a greater than 4-fold increase in risk in a meta-analysis (N=2592) of 3 OBS.253,254,258 Allogeneic blood
products included whole blood, WBC depleted, WBC filtered and not filtered; autologous products included whole blood, buffy coat
depleted, and perioperative cell salvage-washed blood. See individual comparators in eAppendix 2 of the Supplement: GRADE Table
Q11 for specific study findings.
Q11A.4. Combined autologous and allogeneic blood (any) vs. no transfusion
Moderate-quality evidence suggested that combined autologous and additional allogeneic blood transfusions did not increase the risk
of SSI. This was based on no difference in subanalysis in 1 RCT251 (N=470) and 2 OBS253,254 (N=1632). In each study, patients
received allogeneic blood transfusion only after all (23 units) of the autologous donated blood (with or without additional salvage
blood) had been transfused. Autologous blood products included autologous whole blood, packed red blood cells, salvage blood,254
buffy coat depleted,253 or WBC filtered.251 Allogeneic blood products included WBC depleted or not depleted254 or WBC
filtered (WBCF).253,256 Transfusion triggers included: hemoglobin levels of 8-9 g/dL,251,254 <11g/dL for autologous transfusions and
<6 g/dL for allogeneic transfusions or <10 g/dL in patients with cardiovascular or cerebrovascular disease, or symptomatic anemia in
another257 study. See individual comparators in eAppendix 2 of the Supplement: GRADE Table Q11 for specific study findings.
Other guidelines
Recent blood transfusion practice guidelines recommend more restrictive transfusion strategies than those used in these studies.260 In
hemodynamically stable postoperative surgical patients, transfusion is recommended for hemoglobin levels of 8 g/dL or less for those
with symptoms (e.g., chest pain, orthostatic hypotension or tachycardia unresponsive to fluid resuscitation, or congestive heart
failure). In adult and pediatric intensive care unit patients, the recommended hemoglobin level for transfusion is 7 g/dL or less.
Q11B. If the risk of SSI is increased, can this effect be isolated from the risk associated with more complex cases?
The search did not identify data that directly evaluated the association between increasing blood transfusion requirements, more
complex cases, and the risk of SSI in prosthetic joint arthroplasty patients. However, data from 3 OBS254,256,257 stratified blood
transfusion requirements and 1 OBS254 reported blood loss, both by procedure type. See individual comparators in eAppendix 2 of the
Supplement: GRADE Table Q11 for specific study findings.
Q11C. How does the volume of transfused blood product impact the risk of SSI?
The search did not identify data that evaluated differences in the volume of transfused blood product and their impact on the risk of
SSI in prosthetic joint arthroplasty patients.
Q11D. How safe and effective is withholding blood transfusions to reduce the risk of SSI?
The search did not identify data that both evaluated the safety and effectiveness of withholding blood transfusions and its impact on
the risk of SSI in prosthetic joint arthroplasty patients.
Other guidelines
Clinical practice guidelines recommend against withholding transfusion of necessary blood products from surgical patients as a means
to prevent SSI.64 This is considered accepted practice.
2017 American Medical Association. All rights reserved. 31
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Q11. Recommendation
11A. Available evidence suggests uncertain tradeoffs between the benefits and harms of blood transfusions on
the risk of SSI in prosthetic joint arthroplasty. Other organizations have made recommendations on this
topic and a summary of these recommendations can be found in the Other guidelines section of the
narrative summary for this question. (No recommendation/unresolved issue) 251-259 (Guideline Question
11A-C)
11B. Do not withhold transfusion of necessary blood products from surgical patients as a means to prevent SSI.
(Category IB strong recommendation; accepted practice) 64 (Guideline Question 11D)
4.2B. SYSTEMIC IMMUNOSUPPRESSIVE THERAPY
Q12. How does systemic corticosteroid or other immunosuppressive therapy impact the risk of SSI in prosthetic joint
arthroplasty patients?
Immunosuppressive therapies used to treat rheumatoid arthritis (RA) are divided into disease-modifying antirheumatic drugs
(DMARDs) and biologic agents. The most common DMARD is methotrexate, but these drugs can also include hydroxychloriquine,
leflunomide, minocycline, sulfasazaline, azathioprine, cyclosporine and gold. DMARD combination therapy includes 2 or 3 drugs,
most of which are methotrexate-based. Biologic agents are commonly divided into non-tumor necrosis factor (TNF) agents (e.g.,
anakinra, abatacept, rituximab, and tocilizumab) and anti-TNF agents (e.g., adalimumab, etanercept, infliximab, certolizumab pegol,
and golimumab). Systemic corticosteroids most commonly refer to oral prednisone use.
To answer this question, the following subquestions were asked:
A) Does the type of agent impact the risk of SSI?
B) Does the preoperative duration of therapy impact the risk of SSI? and
C) Does the agent dose impact the risk of SSI?
Q12A. Does the type of agent impact the risk of SSI?
The available data examined the following comparisons:
1. Biologic agents (non-TNF and anti-TNF) vs. DMARDs
2. DMARDs: methotrexate vs. no DMARD therapy
For all comparisons, SSI, PJI, superficial SSI, deep wound abscess, and infected hematoma were the critical outcomes for decision-
making. Drug-related adverse events, as well as the adverse events of a surgical wound necrotic eschar, and serous drainage were also
evaluated. Adverse events of surgical wound was a composite variable that included: wound dehiscence (not completely healed 14
days after surgery or needs secondary closure), continued discharge, and culture-positive infection. The evidence for this question
consists of 4 OBS in RA patients.261-264 All studies were at low risk of bias. The authors in 2 of these studies reported receiving funds
from pharmaceutical companies.261,262 The findings of the evidence review and the grades for all important outcomes are shown in
eAppendix 2 of the Supplement: GRADE Table Q12-16 and Evidence Table Q12-16.
Q12.A.1. Biologic agents (non-TNF and anti-TNF) vs. DMARDs
Very low-quality evidence suggested biologic agent therapy (non-TNF and anti-TNF) increased the risk of SSI. This was based on
greater than 5-fold increase in risk of SSI and superficial SSI, but no difference in PJI in 3 separate meta-analyses (N=528) of 2
OBS.261,262 Multivariate logistic regression analyses in both studies identified biologic agents as a significant risk factor for infection,
and in 1 study261 they were also a risk factor for deep venous thrombosis (DVT). Very-low quality evidence also suggested no
difference in other adverse events of the surgical wound.263 For superficial SSI, the large262 study in primary or revision THA or TKA
RA patients (superficial SSI rate 18.8%) reported a significantly increased risk with biologic agents, while the smaller261 study
(superficial SSI rate of 7.4%) reported no difference. The large and small studies each reported no difference in PJI; however, the
number of events in both groups (n=3 and 1, respectively) and the number of arthroplasty procedures in the smaller study (N=108)
limited the power of the analyses.
Biologic agents included anti-TNFs (etanercept, infliximab, adalimumab) and non-TNFs (anakinra, abatacept and rituximab). In each
study, patients had established RA (on average > 10 years). All patients on biologic agent therapy also received prednisone 3-5
mg/day, and the majority also received methotrexate (88%261 to 92%263) and/or another DMARD261 (13%). DMARD patients in all 3
studies were on single or multiple DMARD therapy in addition to daily prednisone (average, 3 mg/day). The most common DMARD
was methotrexate, but none of the studies reported average weekly doses, and only 1 reported the DMARD perioperative
administration protocol (it was administered continuously).262
2017 American Medical Association. All rights reserved. 32
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Q12.A.2. DMARDs: methotrexate vs. no DMARD therapy
Very low-quality evidence suggested methotrexate therapy did not increase the risk of SSI. This was based on no difference in PJI,
deep wound abscess, infected hematoma, necrotic eschar, or serous drainage at 6 months of follow-up in 1 OBS.264 For each outcome,
both the study size and the total number of events were limited. This 1991 study utilized data collected between 1978 and 1987 with
patients on a mean weekly methotrexate dose of 8.7 mg (range: 7.512.5 mg) and could be considered sub-therapeutic in current
clinical practice.265 The methotrexate group included both patients who had continued and patients who had stopped methotrexate
within 4 weeks of surgery. While patients in the no therapy group had never taken methotrexate, some were on daily prednisone (the
study does not report how many).
Q12B. Does the preoperative duration of the therapy impact the risk of SSI?
The search did not identify data that directly evaluated the length of time that immunosuppressive therapy was used preoperatively
and the impact this therapy had on the risk of SSI in prosthetic joint arthroplasty patients. Thus, disease duration was evaluated as a
proxy. SSI was the critical outcome for decision-making. The evidence for this question consists of 2 OBS.261,262 The search did not
reveal data that evaluated patients with early RA (<6 months). The findings of the evidence review and the grades for all important
outcomes are shown in eAppendix 2 of the Supplement: GRADE Table 12-16 and Evidence Table Q12.
Low-quality evidence suggested that in patients with established RA (>6 months), years of disease duration was a risk factor for SSI.
This was based on increased risk in 2 OBS that performed multivariate logistic regression analyses comparing infected to non-infected
patients on biologic (anti-TNF) agents and DMARDs.261,262
Q12C. Does the agent dose impact the risk of SSI?
The search did not identify data that directly evaluated different doses of biologic agents or DMARDs and their impact on the risk of
SSI in arthroplasty patients. The available data examined doses of prednisone and risk of SSI in patients on biologic agents (anti-TNF)
as compared with those on DMARDs.
For this comparison, SSI was the critical outcome for decision-making. The evidence for this question consists of 2 OBS in RA
patients.261,262 The findings of the evidence review and the grades for all important outcomes are shown in eAppendix 2 of the
Supplement: GRADE Table Q12-16 and Evidence Table Q12.
Very low-quality evidence suggested higher prednisone dose increased the risk of SSI. This was based on increased risk of SSI on
multivariate logistic regression analyses comparing infected and non-infected patients in 2 OBS.261,262 The small study, with the
majority of patients on combination biologic/DMARD or dual DMARD therapy, suggested that increasing prednisone dose was a risk
factor for SSI.261 Patients in the biologic agent group were on significantly higher daily prednisone doses (5 mg/day; range 27) than
those in the DMARD group (3 mg/day; range 05). The larger study, where none of the patients were on combination biologic and
DMARD therapy, suggested prednisone dose was not a risk factor for SSI. Patients in both groups were on an average prednisone
dose of 3 mg/day (range, 05).262 Results were not stratified by immunosuppressive therapy agent.
Q13. What are the most effective strategies in managing systemic corticosteroids or other immunosuppressive therapy
perioperatively to reduce the risk of SSI in prosthetic joint arthroplasty patients?
Q13A. How safe and effective is the discontinuation of these agents preoperatively and when should they be resumed?
The available data examined the following comparisons:
1. DMARDs: methotrexate stopped vs. continued perioperatively
2. Biologic agents: anti-TNF stopped vs. continued perioperatively
The evidence for this question consists of 4 OBS examining DMARDs264,266-268 and 1 OBS examining biologic agents266 in RA
patients. All studies were at low risk of bias. For all comparisons PJI was the critical outcome for decision-making. RA flares, infected
hematomas, necrotic eschar, and non-communicating serous drainage outcomes were also evaluated. The findings of the evidence
review and the grades for all important outcomes are shown in eAppendix 2 of the Supplement: GRADE Table Q12-16 and Evidence
Table Q12-13.
Q13A.1. DMARDs: methotrexate stopped vs. continued perioperatively
Low-quality evidence suggested no increased risk of PJI with methotrexate continued throughout the perioperative period. This was
based on no difference in PJI in a meta-analysis of 3 small OBS264,267,268 and a separate OBS266 . In the meta-analysis, both the number
of procedures (N=180) and events (n=7) were small. The studies were performed between 1991 and 1996, and the methotrexate doses
could be considered subtherapeutic in current practice.265 Procedures followed, and length of time during which therapy was stopped
varied. In a larger study, stopping DMARD therapy at the time of surgery (not defined) reduced the incidence of subsequent PJI.266
The authors of this larger study reported receiving funds from multiple pharmaceutical companies.
2017 American Medical Association. All rights reserved. 33
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Q13A.2. Biologic agents: anti-TNF stopped vs. continued perioperatively
Very low-quality evidence suggested no difference in risk of PJI with continuation of biologic (anti-TNF) therapy perioperatively.
This was based on no difference in risk of PJI in a small subanalysis in 1 OBS in THA and TKA patients. 266 Both the number of
patients (N=50) and events (n=3), all in the group continuing biologic agent therapy perioperatively, were very small.
Q13B. Should the agent dose be adjusted, and if so, for how long?
The search did not identify data that evaluated perioperative immunosuppressive therapy dose adjustment and its impact on the risk of
SSI in prosthetic joint arthroplasty patients.
Other guidelines
Clinical practice guidelines provide conflicting recommendations regarding the perioperative management of immunosuppressive
therapy. In 2008, the American College of Rheumatology (ACR) provided no recommendation for the perioperative management of
DMARDs due to the absence of consistent evidence.269 The following year, a multinational guideline suggested that methotrexate
could be safely continued in the perioperative period in RA patients undergoing elective orthopaedic surgery.265 Their
recommendation was based on studies with low methotrexate dosing (413 mg/week). For biologic agents, the British Society for
Rheumatology recommended in 2005 that treatment with anti-TNF agents be withheld for 24 weeks prior to major surgical
procedures and restarted postoperatively if there was no evidence of infection and wound healing was satisfactory.270
Recommendations were based solely on information provided by pharmaceutical companies. In 2008, ACR recommended that
biologic agents not be used for at least 1 week prior to and 1 week following surgery (based on the pharmacokinetic properties of a
given agent).269 The 2012 ACR update does not address perioperative management of immunosuppressive therapy.271
Q12 and Q13. Recommendation
12 and 13. Available evidence suggests uncertain tradeoffs between the benefits and harms of systemic
corticosteroid or other immunosuppressive therapy on the risk of SSI in prosthetic joint arthroplasty.
Other organizations have made recommendations based on the existing evidence and a summary of
these recommendations can be found in the Other guidelines section of the narrative summary for
this question. (No recommendation/unresolved issue) 261-264,266-268 (Guideline Questions 12 and 13)
Q14. What is the optimal duration of postoperative AMP to reduce the risk of SSI in prosthetic joint arthroplasty patients who
are on systemic corticosteroid or other immunosuppressive therapy?
The search did not identify data that specifically evaluated differences in duration of postoperative AMP in prosthetic joint
arthroplasty patients who were on systemic corticosteroids or other immunosuppressive agents and its impact on the risk of SSI.
However, multiple procedures examined in the Core Section, Q1.E: Postoperative AMP duration that included patients on
immunosuppressive therapy showed no benefit of continuing AMP after closing the surgical incision in the operating room. Therefore,
the broader recommendation for duration of postoperative AMP should be applied to prosthetic joint arthroplasty procedures
irrespective of use of systemic corticosteroid or other immunosuppressive therapies.
Q14. Recommendation
14. For prosthetic joint arthroplasty patients on systemic corticosteroid or other immunosuppressive therapy,
Recommendation 1E applies: In clean and clean-contaminated procedures, do not administer additional
prophylactic antimicrobial agent doses after the surgical incision is closed in the operating room, even in
the presence of a drain. (Category IA strong recommendation; high- quality evidence) 96-140
(Guideline Question 14)
4.2C. INTRA-ARTICULAR CORTICOSTEROID INJECTIONS
Q15. How do preoperative intra-articular corticosteroid injections impact the risk of SSI in prosthetic joint arthroplasty
patients?
The available data examined the following comparisons:
1. History of corticosteroid injection vs. no injection
a. TKA: injection vs. no injection
b. THA: injection vs. no injection
2017 American Medical Association. All rights reserved. 34
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
For all comparisons, any SSI, PJI, and superficial SSI were the critical outcomes for decision-making. The evidence for this question
consists of 2 OBS in TKA272,273 and 3 OBS in THA274-276 patients. All studies were at low risk of bias. The findings of the evidence
review and the grades for all important outcomes are shown in eAppendix 2 of the Supplement: GRADE Table Q12-16 and Evidence
Table Q15.
Low-quality evidence suggested that preoperative intra-articular corticosteroid injection did not increase the risk of SSI following total
joint arthroplasty. This was based on no difference in a meta-analysis (N=1146) of 5 OBS in TKA272,273 and THA.274-276 See individual
comparators below and in eAppendix 2 of the Supplement: GRADE Table Q12-16 for individual TKA and THA findings.
Q15.1.a. TKA: injection vs. no injection
Very low-quality evidence suggested that preoperative intra-articular corticosteroid injection did not increase the risk of SSI following
TKA. This was based on no difference in SSI, PJI, or superficial SSI in meta-analyses (N=414) of 2 OBS.272,273 Both the total number
of patients and events were small. One study in 144 patients273 suggested that a history of preoperative intra-articular injection was
significantly associated with PJI after TKA (3 infections, all in the injection group) while another study in 270 TKAs272 reported no
PJIs in either group. Both studies had 1 year of follow-up. The majority of infections were superficial SSIs, and no difference was
reported at 30 days of follow-up. In the smaller study, patients received injections in the orthopaedic clinic, rheumatology clinic, or
general practice setting, while those in the larger study all received their injections in the operating room using strict aseptic technique.
Patients had been injected within 11273 and 12272 months of surgery.
Q15.1.b. THA: injection vs. no Injection
Very low-quality evidence suggested that a preoperative intra-articular corticosteroid injection did not increase the risk of infection
following THA. This was based on no difference in SSI, PJI, or superficial SSI on separate meta-analyses of 3 OBS.274-276 No
difference in PJI or superficial SSI was reported in each individual study. In 2 studies, both the number of patients and events was
small.274,276 Corticosteroid doses and follow-up periods varied. In each study, corticosteroid injection was administered in a radiology
suite using standard protocols for aseptic technique, and 1 study also indicated that the radiologists wore sterile masks and gowns.274
Q16. What are the most effective strategies for managing the preoperative use of intra-articular corticosteroid injections to
reduce the risk of SSI in prosthetic joint arthroplasty patients?
The search did not identify data that evaluated different intra-articular corticosteroid injection agents and their impact on risk of SSI.
To answer this question, 2 subquestions were asked:
A) Does the length of time between corticosteroid injection and prosthetic joint arthroplasty impact the risk of SSI?
B) Does the corticosteroid injection dose impact the risk of SSI?
Q16A. Does the length of time between intra-articular corticosteroid injection and prosthetic joint arthroplasty impact the
risk of SSI?
The available data evaluated different lengths of time between preoperative intra-articular corticosteroid injection and prosthetic joint
arthroplasty and the impact on the risk of SSI in THA only, not TKA.
For all comparisons, SSI was the critical outcome for decision-making. The evidence for this question consists of 2 OBS.274,275 The
findings of the evidence review and the grades for all important outcomes are shown in eAppendix 2 of the Supplement: GRADE
Table Q12-16 and Evidence Table Q16.
Low-quality evidence suggested no association between the length of time between intra-articular corticosteroid injection and THA
and the development of SSI. This was based on no difference in the length of time between injection and surgery and the development
of SSI in 2 OBS.274,275 The smaller, underpowered study also reported no association between the number of injections and SSI.274 In
the larger study, while there was no difference in PJI or superficial SSI (mean time between injection and THA was 112 days), the
mean time from injection to surgery for those diagnosed with PJI was less than half as long as those diagnosed with superficial SSI
(44 vs. 112 days).275
Q16B. Does the corticosteroid injection dose impact the risk of SSI?
The search did not identify data that evaluated different doses of preoperative intra-articular corticosteroid injections and their impact
on the risk of SSI.
Other guidelines
While clinical practice guidelines include intra-articular corticosteroid injections among their pharmacologic recommendations for the
initial management of knee and hip osteoarthritis, they do not provide recommendations on management strategies with regard to SSI
prevention.277 Safe injection practices apply to the administration of intra-articular corticosteroid injections.278
2017 American Medical Association. All rights reserved. 35
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Q15 and Q16. Recommendation
15 & 16. Available evidence suggests uncertain tradeoffs between the benefits and harms of preoperative intra-
articular corticosteroid injection on the incidence of SSI in prosthetic joint arthroplasty. Other
organizations have made recommendations based on observational data and a summary of these
recommendations can be found in the Other guidelines section of the narrative summary for this
question. (No recommendation/unresolved issue)272-276 (Guideline Questions 15 and 16)
4.2D. ANTICOAGULATION
Q17. What are the most effective strategies for managing perioperative venous thromboembolism (VTE) prophylaxis to
reduce the risk of SSI in prosthetic joint arthroplasty patients?
To answer this question 3 subquestions were asked:
A) Does the risk of SSI differ by individual VTE prophylaxis agent?
B) What is the optimal timing and duration of perioperative VTE prophylaxis for the reduction of SSI in prosthetic joint
arthroplasty patients?
C) How safe and effective is modifying the dose of the perioperative VTE prophylaxis agent to reduce the risk of SSI?
Q17A. Does the risk of SSI differ by individual VTE prophylaxis agent?
The available data examined the following comparisons between different anticoagulation agents:
1. Enoxaparin vs. fondaparinux
2. Enoxaparin vs. rivaroxaban
3. Enoxaparin vs. aspirin (acetylsalicylic acid [ASA]) and mechanical prophylaxis
4. Enoxaparin vs. bemiparin vs. fraxiparin vs. fondaparinux
5. Low molecular weight heparin (LMWHs) or fondaparinux vs. ASA
6. Warfarin vs. no pharmacologic or mechanical prophylaxis
7. Warfarin vs. ASA mechanical prophylaxis
8. Higher vs. lower mean International Normalized Ratio (INR)
For all comparisons, SSI and PJI were the critical outcomes in decision-making. Hemorrhagic wound complications, time until wound
was dry or persistent wound drainage, drug-related adverse events, and wound hematoma outcomes were also evaluated. The evidence
for this question consists of 1 SR,279 4 RCTs,280-283 and 5 OBS28,284-287 in primary and revision, unilateral, THA, TKA, and hip fracture
procedures. Injectable agents included LMWHs (Factor Xa and some thrombin inhibition), most commonly enoxaparin or the indirect
Factor Xa inhibitor fondaparinux. Oral agents included rivaroxaban (direct Factor Xa inhibitor), warfarin (Vitamin K antagonist,
Factors II, VII, IX, X inhibitors), and ASA (cyclooxygenase inhibitor). No reversing agents currently exist for fondaparinux or
rivaroxaban. The search did not identify studies that evaluated warfarin as compared to enoxaparin or the impact of unfractionated
heparin or clopidogrel on the risk of SSI. The findings of the evidence review and the grades for all important outcomes are shown in
eAppendix 2 of the Supplement: GRADE Table Q17 and Evidence Table Q17A-B.
Q17A.1. Enoxaparin vs. fondaparinux
Low-quality evidence suggested no difference between perioperative injectable VTE prophylaxis with enoxaparin or fondaparinux and
risk of SSI. This was based on no difference in SSI and no drug-related adverse events at the end of VTE prophylaxis (11 days) in a
large meta-analysis (N=7237) of 4 RCTs (in primary and revision THA, TKA, and hip fracture procedures (osteosynthesis and hemi-
arthroplasties).279,288-291 The studies were large, international, multi-center studies evaluating the safety and effectiveness of these
agents in reducing the risk of postoperative VTE, not SSI. While fondaparinux administration was standardized (2.5 mg once a day
starting postoperatively, except in hip fractures where it was started preoperatively if the case was delayed for >24 hours), enoxaparin
dose and timing of administration varied among studies (30 mg twice a day starting postoperatively288,291 or 40 mg once a day starting
preoperatively289,290). In all 4 studies, prophylaxis was scheduled to last 5-9 days postoperatively. SSI was a secondary outcome and
follow-up was limited (up to 11 days postoperatively). The 4 individual RCTs and the SR meta-analysis were all sponsored by the
manufacturer of fondaparinux and authored by the same investigators, in which the lead, senior, and multiple co-authors reported
serving as scientific consultants to the manufacturers of both agents evaluated in the studies. Turpie et al., indicated that the sponsor
was responsible for data collection and final statistical analysis.291
Q17A.2. Enoxaparin vs. rivaroxaban
High-quality evidence suggested no difference between injectable enoxaparin and oral rivaroxaban and risk of SSI. This was based on
no difference in SSI in a large meta-analysis (N=12,383) of 4 RCTs in elective primary or revision THA or TKA, and no difference in
hemorrhagic wound complications or drug-related adverse events.280-283 These studies were large, international, multi-center studies at
2017 American Medical Association. All rights reserved. 36
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
low risk of bias, evaluating the safety and effectiveness of once daily dosing with enoxaparin or rivaroxaban in reducing the risk of
postoperative VTE, not SSI. Eriksson et al.,280 and Kakkar et al.,282 compared enoxaparin 40 mg once-a-day started preoperatively to
rivaroxaban 10 mg once-a-day started postoperatively in elective unilateral primary (95%) or revision THA. Rivaroxaban was
administered for 35 days in both studies; enoxaparin was administered for 35 days in one280 and 10-14 days in the other.282 Follow up
was approximately 2 months. Two other studies evaluated these agents in elective unilateral primary (97%) or revision TKA,
administered over 10-14 days.281,283 While rivaroxaban administration was standardized (10 mg once-a-day, started preoperatively),
enoxaparin dose and timing varied among studies (40 mg once-a-day, started preoperatively283 or 30 mg twice a day started
postoperatively). SSI was a secondary outcome, and follow-up was approximately 6 weeks. All studies were sponsored by the
manufacturer of rivaroxaban and authored by investigators who were employees of the manufacturer or who served as scientific
consultants to the manufacturers of both agents evaluated in the studies.
Q17A.3 Enoxaparin vs. ASA and mechanical prophylaxis
Very low-quality evidence suggested no difference between injectable enoxaparin and combined oral ASA and mechanical
prophylaxis and risk of SSI. This was based on no increased risk of SSI on logistic regression analysis in 1 large study in primary
THA or TKA.286 Enoxaparin was associated with a longer time until wound was dry in THA, but not TKA. Enoxaparin was started
12-24 hours postoperatively. ASA 325 mg along with pneumatic compression devices was started on the morning after surgery.
Analysis was limited to patients with a closed suction drain and normal coagulation profile. Duration of VTE prophylaxis and follow-
up period were not reported.
Q17A.4. Enoxaparin vs. bemiparin vs. fraxiparin vs. fondaparinux
Very low-quality evidence suggested no difference between perioperative injectable LMWHs, ultra LMWH and fondaparinux, and
risk of SSI. This was based on no difference in PJI at 6 months of follow-up in a small, nested, case-control study within a larger
European multicenter prospective study investigating the independent effects of VTE prophylaxis timing on the risk of PJI in TKA
(low risk of bias).284 Of note, logistic regression analysis suggested that hematoma formation increased the risk of PJI 4-fold.
Q17A.5. Enoxaparin, dalterparin, tinzaparin or fondaparinux vs. ASA mechanical prophylaxis
Very low-quality evidence suggested no difference between perioperative injectable LMWH, fondaparinux, and combined oral ASA
(with or without mechanical VTE prophylaxis), and risk of SSI. This was based on no difference in SSI in a subanalysis (n=41,917) of
a very large retrospective OBS (low risk of bias) using administrative data from a national sample of primary TKAs.28 Data were
collected from 307 facilities over a 2-year period and compared the risk of VTE, bleeding, SSI, and mortality in primary TKA
patients, 4,719 (5.0%) of whom were on ASA, 51,923 (55.3%) on oral warfarin, and 37,198 (39.6%) on injectable agents (LMWHs
and fondaparinux were combined in the analysis). Pneumatic compression devices were used on the day of surgery or on the first
postoperative day in 1,795 (38%), 28,757 (55%), and 17,756 (48%) of the populations, respectively. Patients on ASA had fewer
baseline comorbidities, lower baseline risk of VTE, and received care in hospitals with shorter average length of stay that more
commonly discharged to the patients home after surgery. The study included SSIs detected at the time of admission or upon
readmission to the hospital within 30 days of the index procedure using International Classification of Diseases, Ninth Revision,
Clinical Modification (ICD-9-CM) wound infection codes. Authors indicated that subtherapeutic dosing and/or inappropriate dose
timing of the LMWHs or synthetic Factor Xa inhibitor may have impacted the results.
Q17A.6. Warfarin vs. no pharmacologic or mechanical prophylaxis
Very low-quality evidence suggested no difference between oral warfarin VTE prophylaxis and no pharmacologic or mechanical
prophylaxis, and risk of SSI. This was based on no difference in SSI (deep or superficial) in 1 large retrospective OBS in primary
unilateral TKA at 3 months of follow-up (low risk of bias).287 History of anticoagulation prophylaxis for cardiac (arrhythmia or
prosthetic valve) or thromboembolic event was not associated with increased risk of SSI or gastrointestinal bleed in patients on 6
weeks of postoperative warfarin VTE prophylaxis. INR levels (target INR: 1.62.2) were monitored and medication adjusted twice
weekly. Standardized postoperative protocols in both groups included continuous passive motion, physical therapy, weight bearing,
and similar pain and nausea medications.
Q17A.7. Warfarin vs. ASA mechanical prophylaxis
Low-quality evidence suggested no difference between perioperative oral warfarin and ASA (with or without mechanical VTE
prophylaxis), and risk of SSI. This was based on no difference in SSI in 2 large retrospective studies at low risk of bias.28,286 In 1 large
single institution study, logistic regression analysis suggested that in THA and TKA, warfarin (target INR=2) started on the day of
surgery was not associated with an increased risk of SSI or longer time until wound was dry, as compared with ASA 325 mg with
pneumatic compression devices started on the morning after surgery.286 Duration of VTE prophylaxis and follow-up period were not
reported. Analysis was limited to patients with a closed suction drain and normal coagulation profile. A second, large study using
administrative data collected from 307 facilities over a 2-year period, suggested no difference in SSI in primary TKAs.28 Target INR
was not reported. Pneumatic compression devices were used on the day of surgery or on the first postoperative day in 55% of patients
on warfarin and 38% of patients on ASA. SSIs were detected on admission or readmission to the hospital within 30 days of the index
procedure using ICD-9-CM wound infection codes. Authors indicated that subtherapeutic dosing or inappropriate timing may have
impacted results.
Q17A.8. Higher vs. lower INR
Very low-quality evidence suggested no difference between higher and lower oral warfarin INRs and risk of SSI. This was based on
no difference in PJI in a small (N=154) 1:2 case control study in primary and revision THA and TKAs (low risk of bias).285 Low dose
2017 American Medical Association. All rights reserved. 37
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
warfarin (target INR=1.5) was administered on the day of surgery and continued for 6 weeks. Thirteen patients on anticoagulation
therapy preoperatively for a chronic condition were heparinized postoperatively until fully anticoagulated on warfarin with a higher
target INR=23. All of these patients were in the infected cohort. The INR was also significantly higher in patients with wound-related
problems who later developed infection. In addition, infected patients and those with wound complications were more likely to have
INR > 1.5 at the time of hospital discharge. Infected patients also had a significantly higher incidence of wound hematomas. On
multivariate logistic regression analysis, wound hematomas and persistent wound drainage were significant risk factors for PJI. Nine
(69%) of the heparinized patients developed wound complications, including: hematomas, persistent wound drainage, or delayed
wound healing.
Q17B. What is the optimal timing and duration of perioperative VTE prophylaxis that also reduces the risk of SSI?
The available data examined VTE prophylaxis started preoperatively as compared with postoperatively in patients receiving injectable
LMWHs (enoxaparin, bemiparin, or fraxiparin) or fondaparinux.
For this comparison, PJI was the critical outcome in decision-making. The evidence for this question consists of 1 OBS in TKA, at
low risk of bias.284 The search did not identify data that evaluated optimal timing in THA or in patients taking oral agents. The search
did not identify data that evaluated optimal duration of perioperative anticoagulation prophylaxis and its impact on SSI. The findings
of the evidence review and the grades for all important outcomes are shown in eAppendix 2 of the Supplement: GRADE Table Q17
and Evidence Table Q17A-B.
Very low-quality evidence suggested that close perioperative administration of injectable LMWHs or fondaparinux VTE prophylaxis
agents did not increase the risk of PJI. This was based on no difference in PJI at 6 months of follow-up, in a small, nested, multicenter,
case control study in TKAs.284
Other guidelines
Clinical practice guidelines on prevention of VTE in patients undergoing THA, TKA, or hip fracture procedures provide
recommendations on choice, timing, and duration of VTE prophylaxis.292,293
Q17C. How safe and effective is modifying the dose of perioperative VTE prophylaxis agent to reduce the risk of SSI?
The search did not identify data that evaluated the safety and effectiveness of modifying the dose of perioperative VTE prophylaxis
agent and its impact on the risk of SSI.
Q17. Recommendation
17. Available evidence suggests uncertain tradeoffs between the benefits and harms of venous
thromboembolism prophylaxis on the incidence of SSI in prosthetic joint arthroplasty. Other organizations
have made recommendations based on the existing evidence and these references can be found in the Other
guidelines section of the narrative summary for this question. (No recommendation/unresolved
issue)28,279-288,290,291 (Guideline Question 17)
4.2E. ORTHOPAEDIC SURGICAL SPACE SUIT
Q18. How safe and effective are orthopaedic surgical space suits in reducing the risk of SSI in prosthetic joint arthroplasty
patients, and which healthcare personnel should wear them?
The available data evaluated the use of a space suit as compared with no space suit.
For this comparison, deep SSI requiring reoperation, deep SSI requiring revision, and deep SSI were the critical outcomes in decision-
making. Superficial SSI outcome was also evaluated. The evidence for this question consists of 3 OBS at low risk of bias.294-296 The
findings of the evidence review and the grades for all important outcomes are shown in eAppendix 2 of the Supplement: GRADE
Table Q18 and Evidence Table Q18.
Very-low quality evidence suggested no benefit to using an orthopaedic space suit to reduce the risk of SSI. This was based on no
difference in deep SSI requiring reoperation,295 deep SSI requiring revision surgery,294 or deep or superficial SSI296 in 3 OBS. The
number of events for each of these studies was low. The largest national joint registry study with multiple subgroup analyses
suggested that use of a space suit was associated with an increased number of deep SSIs requiring revision surgery within 6 months of
THA or TKA, but this evidence was limited in size.294 Results did not differ based on the presence or absence of laminar flow. A large
multicenter study using administrative data from patients undergoing TKA suggested no difference in deep SSIs requiring reoperation
within 90 days.295 Reoperations included incision and drainage and implant removal. The definition of deep SSI in this study may
have included PJI. Space suit and laminar flow use varied between groups. A third small study in THA and hip hemiarthroplasties
reported only 1 deep SSI in the space suit group and 1 superficial SSI in each group at 24 months of follow-up.296 High-efficiency
particulate air (HEPA)/mixed turbulent filtration was used in both groups.
2017 American Medical Association. All rights reserved. 38
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
The search did not identify data that quantified potential complications associated with the use of space suits. In 1 large national joint
registry study (N=88,311), comments by surgeons completing a questionnaire (n=35) included limited spatial awareness and ease of
contamination due to an apparent false sense of security with the use of a space suit.294 The efficacy of the space suit as personal
protective equipment was not evaluated.
Also, the search did not identify data that evaluated the association between specific health care personnel wearing a space suit and
SSI. One retrospective controlled study included a surgeon questionnaire reporting that the surgeon, assistant, and scrub nurse were
the team members wearing a full space suit.294 One prospective controlled study reported those same team members wearing the space
suit in the intervention group.296
Q18. Recommendation
18. Available evidence suggests uncertain tradeoffs between the benefits and harms of orthopaedic surgical
space suits or the health care personnel who should wear them for the prevention of SSI in prosthetic joint
arthroplasty. (No recommendation/unresolved issue) 294-296 (Guideline Question 18)
4.2F. POSTOPERATIVE AMP DURATION IN PROSTHETIC JOINT ARTHROPLASTY WITH THE USE OF A DRAIN
Q19. What is the optimal duration of postoperative AMP to reduce the risk of SSI in prosthetic joint arthroplasty in the
presence of a drain?
The search did not identify data that directly evaluated optimal postoperative AMP duration in the presence of a drain and its impact
on the risk of SSI in prosthetic joint arthroplasty patients. However, multiple procedures examined in the Core Section, Q1.E:
Postoperative AMP duration that included use of a drain (including prosthetic joint arthroplasty procedures) showed no benefit of
continuing AMP after closing the incision in the operating room. Therefore, the broader recommendation for postoperative AMP
duration should be applied to prosthetic joint arthroplasty procedures irrespective of drain use.
Q19. Recommendation
19. In prosthetic joint arthroplasty, Recommendation 1E applies: In clean and clean-contaminated procedures,
do not administer additional prophylactic antimicrobial agent doses after the surgical incision is closed in
the operating room, even in the presence of a drain. (Category IA - strong recommendation; high-
quality evidence) 96-140 (Guideline Question 19)
4.2G. BIOFILM
Q20. What are the most effective strategies to reduce the risk of biofilm formation and SSI in prosthetic joint arthroplasty
patients?
To answer this question 4 subquestions were asked:
A) How effective are cement modifications (i.e., antimicrobial and nanoparticle loading)?
B) How effective are prosthesis modifications (i.e., antimicrobial coating, galvanic couples, printing technologies, and
nanotechnology)?
C) How effective are vaccines?
D) How effective are other biofilm control agents (e.g., biofilm dispersants, quorum-sensing inhibitors, novel antimicrobial
agents)?
Q20A. How effective are cement modifications (i.e., antimicrobial and nanoparticle loading)?
The search did not identify data that evaluated the safety and effectiveness of cement modifications in THA and the risk of SSI. In
vitro studies and studies that evaluated antimicrobial loaded cement in the absence of perioperative parenteral AMP were excluded
from the analysis. The available data examined cefuroxime loaded cement vs. plain cement in primary TKA patient receiving
perioperative AMP.
For this comparison, deep SSI was the critical outcome in decision-making. In these studies, deep SSI likely refers to or includes PJI.
The evidence for this question consists of 2 RCTs.297,298 The findings of the evidence review and the grades for all important outcomes
are shown in eAppendix 2 of the Supplement: GRADE Table Q20 and Evidence Table Q20.
Moderate-quality evidence suggested a benefit of cefuroxime loaded cement. This was based on a reduced risk of deep SSI in a meta-
analysis (N=428) of 2 RCTs: 1 large study in non-diabetic297 patients and 1 small study (N=78) in diabetic 298 patients. Both studies
were at moderate risk of bias. There were no deep SSIs in the cefuroxime loaded cement groups at an average 49 months of follow-up.
A single surgeon performed all TKAs in an operating room without ultraviolet lights, laminar flow, or use of an orthopaedic surgical
space suit. Only the tibial and patellar components were cemented. Cefuroxime 2 g in 40 g polymethyl methacrylate cement was used
2017 American Medical Association. All rights reserved. 39
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
in the study groups. AMP included parenteral cefazolin and gentamicin preoperatively then every 6 and 12 hours, respectively,
postoperatively for 36 hours followed by cefazolin orally for 7 more days. Data on organisms isolated from the SSIs and antimicrobial
resistance were not reported.
Q20B. How effective are prosthesis surface modifications (i.e., antimicrobial coating, galvanic couples, printing technologies,
and nanotechnology)?
The search did not identify in vivo studies that evaluated the safety and effectiveness of prosthesis modifications and their impact on
biofilm formation and the risk of SSI.
Q20C. How effective are vaccines?
The search did not identify in vivo studies that evaluated the safety and effectiveness of vaccines and their impact on biofilm
formation and the risk of SSI.
Q20D. How effective are other biofilm control agents (e.g., biofilm dispersants, quorum-sensing inhibitors, novel antimicrobial
agents)?
The search did not identify in vivo studies that evaluated the safety and effectiveness of other biofilm control agents and their impact
on biofilm formation and the risk of SSI
Q20. Recommendations
20A. Available evidence suggests uncertain tradeoffs between the benefits and harms regarding cement
modifications and the prevention of biofilm formation or SSI in prosthetic joint arthroplasty. (No
recommendation/unresolved issue) 297,298 (Guideline Question 20A)
20B. The search did not identify studies evaluating prosthesis modifications for the prevention of biofilm
formation or SSI in prosthetic joint arthroplasty. (No recommendation/unresolved issue) (Guideline
Question 20B)
20C. The search did not identify studies evaluating vaccines for the prevention of biofilm formation or SSI in
prosthetic joint arthroplasty. (No recommendation/unresolved issue) (Guideline Question 20C)
20D. The search did not identify studies evaluating biofilm control agents such as biofilm dispersants, quorum-
sensing inhibitors, or novel antimicrobial agents for the prevention of biofilm formation or SSI in prosthetic
joint arthroplasty. (No recommendation/unresolved issue) (Guideline Question 20D)
2017 American Medical Association. All rights reserved. 40
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
5. RE-EMPHASIS OF SELECT 1999 CDC AND HICPAC RECOMMENDATIONS FOR
PREVENTION OF SURGICAL SITE INFECTIONS
The Centers for Disease control and Prevention (CDC), Guideline for Prevention of Surgical Site Infection 2017 addresses new and
updated strategies for the prevention of Surgical Site Infections (SSIs) in healthcare settings. The 2017 Guideline focuses on a few
select areas, and not all of the recommendations that were made in 1999 were reviewed as a part of the guideline development process.
However, CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC) recognized that many of the
recommendations remain important and have become infection control standards for surgical infection prevention.
In 2014, HICPAC reviewed the 1999 strong recommendations for which the evidence was not re-assessed as part of the development
of the 2017 Guideline. This was to reaffirm them as accepted practices (e.g., standard of care). At the July 2014 HICPAC meeting,
HICPAC reviewed and recommended to CDC that many of the 1999 strong recommendations should be re-emphasized as accepted
practice for preventing surgical site infections.299 CDC and HICPAC recommend that facilities should continue to follow the
recommendations outlined below.
5.1. Recommendations
1. PREPARATION OF THE PATIENT
a. Whenever possible, identify and treat all infections remote to the surgical site before elective operations and
postpone elective operations on patients with remote site infections until the infection has resolved.
b. Do not remove hair preoperatively unless the hair at or around the incision site will interfere with the operation. If
hair removal is necessary, remove immediately before the operation, with clippers.
c. Encourage tobacco cessation for a minimum of at least 30 days before elective operations.
d. Ensure skin around the incision site is free of gross contamination before performing antiseptic skin preparation.
2. HAND/FOREARM ANTISEPSIS FOR SURGICAL TEAM
a. Perform preoperative surgical hand/forearm antisepsis according to manufacturers recommendations for the product
being used.
b. See 2002 Guidelines for Hand Hygiene in Healthcare Settings for additional surgical hand antisepsis
recommendations.300
3. OPERATING ROOM VENTILATION
a. Maintain positive pressure ventilation in the operating room and adjoining spaces. Maintain the number of air
exchanges, airflow patterns, temperature, humidity, location of vents, and use of filters in accordance with
recommendations from the most recent version of the Facilities Guidelines Institute Guidelines for Design and
Construction of Hospitals and Outpatient Facilities (current version 2014).301
4. CLEANING AND DISINFECTION OF ENVIRONMENTAL SURFACES
a. Do not perform special cleaning or closing of operating rooms after contaminated or dirty operations.
5. REPROCESSING OF SURGICAL INSTRUMENTS
a. Sterilize all surgical instruments according to published guidelines and manufacturers recommendations.
b. Immediate-use steam sterilization should never be used for reasons of convenience, as an alternative to purchasing
additional instrument sets, or to save time. This practice should be reserved only for patient care items that will be
used immediately in emergency situations when no other options are available.
c. Refer to CDC and HICPAC Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008 for additional
recommendations.68
6. SURGICAL ATTIRE AND DRAPES
a. Wear a surgical mask that fully covers the mouth and nose when entering the operating room if an operation is about
to begin or already under way, or if sterile instruments are exposed. Wear the mask throughout the operation.
b. Wear a new, disposable, or hospital laundered head covering for each case, when entering the operating room.
Ensure it fully covers all hair on the head and all facial hair not covered by the surgical mask.
c. Wear sterile gloves if serving as a member of the scrubbed surgical team. Put on sterile gloves after donning a sterile
gown.
d. Use surgical gowns and drapes that are effective barriers when wet (i.e., materials that resist liquid penetration).
e. Change scrub suits that are visibly soiled, contaminated, and/or penetrated by blood or other potentially infectious
materials.
2017 American Medical Association. All rights reserved. 41
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
7. STERILE AND SURGICAL TECHNIQUE
a. Adhere to principles of sterile technique when performing all invasive surgical procedures.
b. If drainage is necessary, use a closed suction drain. Place a drain through a separate incision distant from the
operative incision. Remove the drain as soon as possible.
8. POST-OP INCISION CARE
a. Protect primarily closed incisions with a sterile dressing for 24-48 hours postoperatively.
2017 American Medical Association. All rights reserved. 42
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
6. REFERENCES
1. DeFrances CJ, Lucas CA, Buie VC, Golosinskiy A. 2006 National Hospital Discharge Survey. National health
statistics reports; no 5. 2008; Available at: http://www.cdc.gov/nchs/data/nhsr/nhsr005.pdf. Accessed January 25,
2017.
2. Cullen KA, Hall MJ, Golosinskiy A. Ambulatory Surgery in the United States, 2006. National health statistics
reports; no 11. Revised. 2009; Available at: http://www.cdc.gov/nchs/data/nhsr/nhsr011.pdf. Accessed January 25,
2017.
3. Mu Y, Edwards JR, Horan TC, Berrios-Torres SI, Fridkin SK. Improving risk-adjusted measures of surgical site
infection for the National Healthcare Safety Network. Infect Control Hosp Epidemiol. 2011;32(10):970-986.
4. McKibben L, Horan T, Tokars JI, et al. Guidance on public reporting of healthcare-associated infections:
recommendations of the Healthcare Infection Control Practices Advisory Committee. Am J Infect Control.
2005;33(4):217-226.
5. Sievert DM, Ricks P, Edwards JR, et al. Antimicrobial-resistant pathogens associated with healthcare-associated
infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control
and Prevention, 2009-2010. Infect Control Hosp Epidemiol. 2013;34(1):1-14.
6. Fry DE. Fifty ways to cause surgical site infections. Surg Infect (Larchmt). 2011;12(6):497-500.
7. Urban JA. Cost analysis of surgical site infections. Surg Infect (Larchmt). 2006;7 Suppl 1:S19-22.
8. Fry DE. The economic costs of surgical site infection. Surg Infect (Larchmt). 2002;3 Suppl 1:S37-43.
9. Yasunaga H, Ide H, Imamura T, Ohe K. Accuracy of economic studies on surgical site infection. J Hosp Infect.
2007;65(2):102-107.
10. Anderson DJ, Kirkland KB, Kaye KS, et al. Underresourced hospital infection control and prevention programs:
penny wise, pound foolish? Infect Control Hosp Epidemiol. 2007;28(7):767-773.
11. Centers for Disease Control and Prevention. The Direct Medical Costs of Healthcare-Associated Infections in U.S.
Hospitals and the Benefits of Prevention. 2009; Available at: http://www.cdc.gov/hai/pdfs/hai/scott_costpaper.pdf
Accessed January 25, 2017.
12. Stone PW, Braccia D, Larson E. Systematic review of economic analyses of health care-associated infections. Am J
Infect Control. 2005;33(9):501-509.
13. Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, Brennan PJ. Estimating the proportion of
healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control
Hosp Epidemiol. 2011;32(2):101-114.
14. Bozic KJ, Ries MD. The impact of infection after total hip arthroplasty on hospital and surgeon resource utilization.
J Bone Joint Surg Am. 2005;87(8):1746-1751.
15. Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United
States. J Arthroplasty. 2012;27(8 Suppl):61-65 e61.
16. Engemann JJ, Carmeli Y, Cosgrove SE, et al. Adverse clinical and economic outcomes attributable to methicillin
resistance among patients with Staphylococcus aureus surgical site infection. Clin Infect Dis. 2003;36(5):592-598.
17. Bratzler DW, Houck PM, for the Surgical Infection Prevention Guidelines Writers Workgroup. Antimicrobial
prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Clin Infect
Dis. 2004;38(12):1706-1715.
18. Bratzler DW, Hunt DR. The surgical infection prevention and surgical care improvement projects: national
initiatives to improve outcomes for patients having surgery. Clin Infect Dis. 2006;43(3):322-330.
19. U.S. Government Printing Office. The Deficit Reduction Act of 2005. 2006; Available at:
http://www.gpo.gov/fdsys/pkg/BILLS-109s1932enr/pdf/BILLS-109s1932enr.pdf Accessed January 25, 2017.
20. U.S. Department of Health and Human Services. HHS Action Plan to Prevent Healthcare Associated Infections.
2013; Available at: https://health.gov/hcq/prevent-hai-action-plan.asp. Accessed January 25, 2017.
21. U.S. Department of Health and Human Services, Centers for Medicare & Medicaid Services. 42 CFR Parts 412,
413, 415, et al. Medicare Program; Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and
2017 American Medical Association. All rights reserved. 43
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
the Long-term Care Hospital Prospective Payment System Changes and FY2011 Rates; Provider Agreements and
Supplier Approvals; and Hospital Conditions of Participation for Rehabilitation and Respiratory Care Services;
Medicaid Program: Accreditation for Providers of Inpatient Psychiatric Services; Final Rule. 2010; Available at:
https://www.gpo.gov/fdsys/pkg/FR-2010-08-16/pdf/2010-19092.pdf. Accessed January 25, 2017.
22. Malpiedi PJ, Peterson KD, Soe MM, et al. 2011 National and State Healthcare-Associated Infection Standardized
Infection Ratio Report. Published February 11, 2013. 2013; Available at: http://www.cdc.gov/hai/pdfs/SIR/SIR-
Report_02_07_2013.pdf. Accessed January 25, 2017.
23. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project net (HCUPnet). 2011
Nationwide Inpatient Sample (NIS). 2011; Available at: http://hcupnet.ahrq.gov/. Accessed January 25, 2017.
24. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the
United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780-785.
25. Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J. Infection burden for hip and knee arthroplasty in the
United States. J Arthroplasty. 2008;23(7):984-991.
26. Kurtz SM, Ong KL, Schmier J, Zhao K, Mowat F, Lau E. Primary and revision arthroplasty surgery caseloads in the
United States from 1990 to 2004. J Arthroplasty. 2009;24(2):195-203.
27. Bozic KJ, Kurtz SM, Lau E, et al. The epidemiology of revision total knee arthroplasty in the United States. Clin
Orthop Relat Res. 2010;468(1):45-51.
28. Bozic KJ, Vail TP, Pekow PS, Maselli JH, Lindenauer PK, Auerbach AD. Does aspirin have a role in venous
thromboembolism prophylaxis in total knee arthroplasty patients? J Arthroplasty. 2010;25(7):1053-1060.
29. Kurtz SM, Ong KL, Schmier J, et al. Future clinical and economic impact of revision total hip and knee arthroplasty.
J Bone Joint Surg Am. 2007;89 Suppl 3:144-151.
30. Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004;351(16):1645-1654.
31. Donlan RM. New approaches for the characterization of prosthetic joint biofilms. Clin Orthop Relat Res.
2005(437):12-19.
32. Donlan RM, Costerton JW. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol
Rev. 2002;15(2):167-193.
33. Wolcott RD, Rhoads DD, Bennett ME, et al. Chronic wounds and the medical biofilm paradigm. J Wound Care.
2010;19(2):45-46, 48-50, 52-43.
34. Berbari EF, Marculescu C, Sia I, et al. Culture-negative prosthetic joint infection. Clin Infect Dis. 2007;45(9):1113-
1119.
35. Trampuz A, Piper KE, Jacobson MJ, et al. Sonication of removed hip and knee prostheses for diagnosis of infection.
N Engl J Med. 2007;357(7):654-663.
36. Malekzadeh D, Osmon DR, Lahr BD, Hanssen AD, Berbari EF. Prior use of antimicrobial therapy is a risk factor for
culture-negative prosthetic joint infection. Clin Orthop Relat Res. 2010;468(8):2039-2045.
37. American Academy of Orthopaedic Surgeons. AAOS Guideline on the Diagnosis of Periprosthetic Joint Infections
of the Hip and Knee. 2010; Available at: http://www.aaos.org/research/guidelines/PJIguideline.pdf. Accessed
January 25, 2017.
38. Bedair H, Ting N, Jacovides C, et al. The Mark Coventry Award. Diagnosis of early postoperative TKA infection
using synovial fluid analysis. Clin Orthop Relat Res. 2011;469(1):34-40.
39. Bori G, Munoz-Mahamud E, Garcia S, et al. Interface membrane is the best sample for histological study to
diagnose prosthetic joint infection. Mod Pathol. 2011;24(4):579-584.
40. Morgan PM, Sharkey P, Ghanem E, et al. The value of intraoperative gram stain in revision total knee arthroplasty.
J Bone Joint Surg Am. 2009;91A(9):2124-2129.
41. Bottner F, Wegner A, Winkelmann W, Becker K, Erren M, Gotze C. Interleukin-6, procalcitonin and TNF-alpha:
markers of peri-prosthetic infection following total joint replacement. J Bone Joint Surg Br. 2007;89(1):94-99.
42. Buttaro MA, Tanoira I, Comba F, Piccaluga F. Combining C-reactive protein and interleukin-6 may be useful to
detect periprosthetic hip infection. Clin Orthop Relat Res. 2010;468(12):3263-3267.
2017 American Medical Association. All rights reserved. 44
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
43. Di Cesare PE, Chang E, Preston CF, Liu CJ. Serum interleukin-6 as a marker of periprosthetic infection following
total hip and knee arthroplasty. J Bone Joint Surg Am. 2005;87(9):1921-1927.
44. Drago L, Vassena C, Dozio E, et al. Procalcitonin, C-reactive protein, interleukin-6, and soluble intercellular
adhesion molecule-1 as markers of postoperative orthopaedic joint prosthesis infections. Int J Immunopathol
Pharmacol. 2011;24(2):433-440.
45. Worthington T, Dunlop D, Casey A, Lambert P, Luscombe J, Elliott T. Serum procalcitonin, interleukin-6, soluble
intercellular adhesin molecule-1 and IgG to short-chain exocellular lipoteichoic acid as predictors of infection in
total joint prosthesis revision. Br J Biomed Sci. 2010;67(2):71-76.
46. Nilsdotter-Augustinsson A, Briheim G, Herder A, Ljunghusen O, Wahlstrom O, Ohman L. Inflammatory response
in 85 patients with loosened hip prostheses - A prospective study comparing inflammatory markers in patients with
aseptic and septic prosthetic loosening. Acta Orthop. 2007;78(5):629-639.
47. Holinka J, Bauer L, Hirschl AM, Graninger W, Windhager R, Presterl E. Sonication cultures of explanted
components as an add-on test to routinely conducted microbiological diagnostics improve pathogen detection. J
Orthop Res. 2011;29(4):617-622.
48. Nguyen LL, Nelson CL, Saccente M, Smeltzer MS, Wassell DL, McLaren SG. Detecting bacterial colonization of
implanted orthopaedic devices by ultrasonication. Clin Orthop Relat Res. 2002(403):29-37.
49. Sorli L, Puig L, Torres-Claramunt R, et al. The relationship between microbiology results in the second of a two-
stage exchange procedure using cement spacers and the outcome after revision total joint replacement for infection.
The use of sonication to aid bacteriological analysis. J Bone Joint Surg Br. 2012;94B(2):249-253.
50. Vergidis P, Greenwood-Quaintance KE, Sanchez-Sotelo J, et al. Implant sonication for the diagnosis of prosthetic
elbow infection. J Shoulder Elbow Surg. 2011;20(8):1275-1281.
51. Koskela A, Nilsdotter-Augustinsson A, Persson L, Soderquist B. Prevalence of the ica operon and insertion
sequence IS256 among Staphylococcus epidermidis prosthetic joint infection isolates. Eur J Clin Microbiol Infect
Dis. 2009;28(6):655-660.
52. Arciola CR, Campoccia D, Baldassarri L, et al. Detection of biofilm formation in Staphylococcus epidermidis from
implant infections. Comparison of a PCR-method that recognizes the presence of ica genes with two classic
phenotypic methods. J Biomed Mater Res. 2006;76(2):425-430.
53. Holmberg A, Lood R, Morgelin M, et al. Biofilm formation by Propionibacterium acnes is a characteristic of
invasive isolates. Clin Microbiol Infect. 2009;15(8):787-795.
54. Neut D, van Horn JR, van Kooten TG, van der Mei HC, Busscher HJ. Detection of biomaterial-associated infections
in orthopaedic joint implants. Clin Orthop Relat Res. 2003(413):261-268.
55. Stoodley P, Kathju S, Hu FZ, et al. Molecular and imaging techniques for bacterial biofilms in joint arthroplasty
infections. Clin Orthop Relat Res. 2005(437):31-40.
56. Dubouix-Bourandy A, de Ladoucette A, Pietri V, et al. Direct detection of Staphylococcus osteoarticular infections
by use of Xpert MRSA/SA SSTI real-time PCR. J Clin Microbiol. 2011;49(12):4225-4230.
57. Kobayashi N, Inaba Y, Choe H, et al. Simultaneous intraoperative detection of methicillin-resistant Staphylococcus
and pan-bacterial infection during revision surgery. Use of simple DNA release by ultrasonication and real-time
polymerase chain reaction. J Bone Joint Surg Am. 2009;91A(12):2896-2902.
58. Krimmer V, Merkert H, von Eiff C, et al. Detection of Staphylococcus aureus and Staphylococcus epidermidis in
clinical samples by 16S rRNA-directed in situ hybridization. J Clin Microbiol. 1999;37(8):2667-2673.
59. Montanaro L, Arciola CR, Baldassarri L, Borsetti E. Presence and expression of collagen adhesin gene (cna) and
slime production in Staphylococcus aureus strains from orthopaedic prosthesis infections. Biomaterials.
1999;20(20):1945-1949.
60. Riggio MP, Dempsey KE, Lennon A, Allan D, Ramage G, Bagg J. Molecular detection of transcriptionally active
bacteria from failed prosthetic hip joints removed during revision arthroplasty. Eur J Clin Microbiol Infect Dis.
2010;29(7):823-834.
61. Rohde H, Burandt EC, Siemssen N, et al. Polysaccharide intercellular adhesin or protein factors in biofilm
accumulation of Staphylococcus epidermidis and Staphylococcus aureus isolated from prosthetic hip and knee joint
infections. Biomaterials. 2007;28(9):1711-1720.
2017 American Medical Association. All rights reserved. 45
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
62. Larsen LH, Lange J, Xu Y, Schonheyder HC. Optimizing culture methods for diagnosis of prosthetic joint
infections: a summary of modifications and improvements reported since 1995. J Med Microbiol. 2012;61(Pt
3):309-316.
63. Workgroup Convened by the Musculoskeletal Infection Society. New definition for periprosthetic joint infection. J
Arthroplasty. 2011;26(8):1136-1138.
64. Mangram AJ, Horan TC, Pearson ML, et al. Guideline for Prevention of Surgical Site Infection, 1999. Am J Infect
Control. 1999;27(2):97-132; quiz 133-134; discussion 196.
65. Centers for Disease Control and Prevention. National Healthcare Safety Network. Surgical Site Infection (SSI)
Event. 2017; Available at: http://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf. Accessed January 25, 2017.
66. Centers for Disease Control and Prevention, Healthcare Infection Control Practices Advisory Committee, Bolyard
EA, et al. Guideline for Infection Control in Health Care Personnel, 1998. 1998; Available at:
http://www.cdc.gov/hicpac/pdf/InfectControl98.pdf. Accessed January 25, 2017.
67. Centers for Disease Control and Prevention. Guidelines for Environmental Infection Control in Health-Care
Facilities: Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee
(HICPAC) MMWR 2003;52(No. RR-10):148.
68. Centers for Disease Control and Prevention, Healthcare Infection Control Practices Advisory Committee, Rutala
WA, Weber DJ. Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008. 2008; Available at:
http://www.cdc.gov/hicpac/pdf/guidelines/Disinfection_Nov_2008.pdf. Accessed January 25, 2017.
69. Guyatt GH, Oxman AD, Kunz R, et al. Going from evidence to recommendations. BMJ. 2008;336(7652):1049-
1051.
70. Guyatt GH, Oxman AD, Kunz R, et al. What is "quality of evidence" and why is it important to clinicians? BMJ.
2008;336(7651):995-998.
71. Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength
of recommendations. BMJ. 2008;336(7650):924-926.
72. Schunemann HJ, Oxman AD, Brozek J, et al. Grading quality of evidence and strength of recommendations for
diagnostic tests and strategies. BMJ. 2008;336(7653):1106-1110.
73. Umscheid CA, Agarwal RK, Brennan PJ, Healthcare Infection Control Practices Advisory Committee. Updating the
guideline development methodology of the Healthcare Infection Control Practices Advisory Committee (HICPAC).
Am J Infect Control. 2010;38(4):264-273.
74. McGinn T, Wyer PC, Newman TB, et al. Tips for learners of evidence-based medicine: 3. Measures of observer
variability (kappa statistic). Can Med Assoc J. 2004;171(11):1369-1373.
75. Whitlock EP, Lin JS, Chou R, Shekelle P, Robinson KA. Using existing systematic reviews in complex systematic
reviews. Ann Intern Med. 2008;148(10):776-782.
76. Centers for Disease Control and Prevention, Healthcare Infection Control Practices Advisory Committee, Umscheid
CA, Agarwal RK, Brennan PJ. Updating the Guideline Methodology of the Healthcare Infection Control Practices
Advisory Committee (HICPAC). 2010; Available at: http://www.cdc.gov/hicpac/pdf/guidelines/2009-10-
29HICPAC_GuidelineMethodsFINAL.pdf. Accessed January 25, 2017.
77. Akinyoola AL, Adegbehingbe OO, Odunsi A. Timing of antibiotic prophylaxis in tourniquet surgery. J Foot Ankle
Surg. 2011;50(4):374-376.
78. Soriano A, Bori G, Garcia-Ramiro S, et al. Timing of antibiotic prophylaxis for primary total knee arthroplasty
performed during ischemia. Clin Infect Dis. 2008;46(7):1009-1014.
79. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 120: Use of prophylactic
antibiotics in labor and delivery. Obstet Gynecol. 2011;117(6):1472-1483.
80. Anonymous. Antimicrobial prophylaxis for surgery. Treat Guidel Med Lett. 2012;10(122):73-78; quiz 79-80.
81. Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery.
Am J Health Syst Pharm. 2013;70(3):195-283.
82. Engelman R, Shahian D, Shemin R, et al. The Society of Thoracic Surgeons practice guideline series: Antibiotic
prophylaxis in cardiac surgery, part II: Antibiotic choice. Ann Thorac Surg. 2007;83(4):1569-1576.
2017 American Medical Association. All rights reserved. 46
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
83. van Schalkwyk J, Van Eyk N, Society of Obstetricians Gynaecologists of Canada Infectious Diseases Committee.
Antibiotic prophylaxis in obstetric procedures. J Obstet Gynaecol Can. 2010;32(9):878-892.
84. Anderson DJ, Podgorny K, Berrios-Torres SI, et al. Strategies to prevent surgical site infections in acute care
hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35 Suppl 2:S66-88.
85. WHO Organization. Global guidelines on the prevention of surgical site infection. 2016;
http://apps.who.int/iris/bitstream/10665/250680/1/9789241549882-eng.pdf?ua=1. Accessed February 6, 2017.
86. Sullivan SA, Smith T, Chang E, Hulsey T, Vandorsten JP, Soper D. Administration of cefazolin prior to skin
incision is superior to cefazolin at cord clamping in preventing postcesarean infectious morbidity: a randomized,
controlled trial. Am J Obstet Gynecol. 2007;196(5):455 e451-455.
87. Thigpen BD, Hood WA, Chauhan S, et al. Timing of prophylactic antibiotic administration in the uninfected
laboring gravida: a randomized clinical trial. Am J Obstet Gynecol. 2005;192(6):1864-1868; discussion 1868-1871.
88. Wax JR, Hersey K, Philput C, et al. Single dose cefazolin prophylaxis for postcesarean infections: before vs. after
cord clamping. J Matern Fetal Med. 1997;6(1):61-65.
89. Osman B, Abbas A, Ahmed MA, Abubaker MS, Adam I. Prophylactic ceftizoxime for elective cesarean delivery at
Soba Hospital, Sudan. BMC Res Notes. 2013;6:57.
90. Witt A, Doner M, Petricevic L, et al. Antibiotic prophylaxis before surgery vs after cord clamping in elective
cesarean delivery: a double-blind, prospective, randomized, placebo-controlled trial. Arch Surg. 2011;146(12):1404-
1409.
91. Macones GA, Cleary KL, Parry S, et al. The timing of antibiotics at cesarean: a randomized controlled trial. Am J
Perinatol. 2012;29(4):273-276.
92. Yildirim G, Gungorduk K, Guven HZ, et al. When should we perform prophylactic antibiotics in elective cesarean
cases? Arch Gynecol Obstet. 2009;280(1):13-18.
93. Bauer LA, Edwards WA, Dellinger EP, Simonowitz DA. Influence of weight on aminoglycoside pharmacokinetics
in normal weight and morbidly obese patients. Eur J Clin Pharmacol. 1983;24(5):643-647.
94. Cuthbertson AM, McLeish AR, Penfold JC, Ross H. A comparison between single and double dose intravenous
timentin for the prophylaxis of wound infection in elective colorectal surgery. Dis Colon Rectum. 1991;34(2):151-
155.
95. National Institute for Health and Clinical Excellence (NICE). Surgical Site Infection: Prevention and Treatment of
Surgical Site Infection (NICE Clinical Guideline 74). 2008; https://www.nice.org.uk/guidance/cg74. Accessed
January 25, 2017.
96. Austin TW, Coles JC, Burnett R, Goldbach M. Aortocoronary bypass procedures and sternotomy infections: a study
of antistaphylococcal prophylaxis. Can J Surg. 1980;23(5):483-485.
97. Conte JE, Jr., Cohen SN, Roe BB, Elashoff RM. Antibiotic prophylaxis and cardiac surgery. A prospective double-
blind comparison of single-dose versus multiple-dose regimens. Ann Intern Med. 1972;76(6):943-949.
98. Nooyen SM, Overbeek BP, Brutel de la Riviere A, Storm AJ, Langemeyer JJ. Prospective randomised comparison
of single-dose versus multiple-dose cefuroxime for prophylaxis in coronary artery bypass grafting. Eur J Clin
Microbiol Infect Dis. 1994;13(12):1033-1037.
99. Tamayo E, Gualis J, Florez S, Castrodeza J, Eiros Bouza JM, Alvarez FJ. Comparative study of single-dose and 24-
hour multiple-dose antibiotic prophylaxis for cardiac surgery. J Thorac Cardiovasc Surg. 2008;136(6):1522-1527.
100. Lin MH, Pan SC, Wang JL, et al. Prospective randomized study of efficacy of 1-day versus 3-day antibiotic
prophylaxis for preventing surgical site infection after coronary artery bypass graft. J Formos Med Assoc.
2011;110(10):619-626.
101. Bernard A, Pillet M, Goudet P, Viard H. Antibiotic-prophylaxis in pulmonary surgery - a prospective randomized
double-blind trial of flash cefuroxime versus 48-hour cefuroxime. J Thorac Cardiovasc Surg. 1994;107(3):896-900.
102. Oostvogel HJ, van Vroonhoven TJ, van der Werken C, Lenderink AW. Single-dose vs. short-term antibiotic therapy
for prevention of wound infection in general surgery. A prospective, randomized double-blind trial. Acta Chir
Scand. 1987;153(10):571-575.
103. Hall JC, Christiansen KJ, Goodman M, et al. Duration of antimicrobial prophylaxis in vascular surgery. Am J Surg.
1998;175(2):87-90.
2017 American Medical Association. All rights reserved. 47
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
104. Hasselgren PO, Ivarsson L, Risberg B, Seeman T. Effects of prophylactic antibiotics in vascular surgery. A
prospective, randomized, double-blind study. Ann Surg. 1984;200(1):86-92.
105. Carroll WR, Rosenstiel D, Fix JR, et al. Three-dose vs extended-course clindamycin prophylaxis for free-flap
reconstruction of the head and neck. Arch Otolaryngol Head Neck Surg. 2003;129(7):771-774.
106. Liu SA, Tung KC, Shiao JY, Chiu YT. Preliminary report of associated factors in wound infection after major head
and neck neoplasm operations--does the duration of prophylactic antibiotic matter? J Laryngol Otol.
2008;122(4):403-408.
107. Chang WC, Hung YC, Li TC, Yang TC, Chen HY, Lin CC. Short course of prophylactic antibiotics in
laparoscopically assisted vaginal hysterectomy. J Reprod Med. 2005;50(7):524-528.
108. Hemsell DL, Heard ML, Nobles BJ, Hemsell PG. Single-dose cefoxitin prophylaxis for premenopausal women
undergoing vaginal hysterectomy. Obstet Gynecol. 1984;63(3):285-290.
109. Mayer HO, Petru E, Haas J, Heydarfadai M. Perioperative antibiotic prophylaxis in patients undergoing radical
surgery for gynecologic cancer: single dose versus multiple dose administration. Eur J Gynaecol Oncol.
1993;14(3):177-181.
110. Su HY, Ding DC, Chen DC, Lu MF, Liu JY, Chang FY. Prospective randomized comparison of single-dose versus
1-day cefazolin for prophylaxis in gynecologic surgery. Acta Obstet Gynecol Scand. 2005;84(4):384-389.
111. Turano A. New clinical data on the prophylaxis of infections in abdominal, gynecologic, and urologic surgery.
Multicenter Study Group. Am J Surg. 1992;164(4A Suppl):16S-20S.
112. Lyimo FM, Massinde AN, Kidenya BR, Konje ET, Mshana SE. Single dose of gentamicin in combination with
metronidazole versus multiple doses for prevention of post-caesarean infection at Bugando Medical Centre in
Mwanza, Tanzania: a randomized, equivalence, controlled trial. BMC Pregnancy Childbirth. 2013;13:123.
113. Ali M, Raza A. Role of single dose antibiotic prophylaxis in clean orthopedic surgery. J Coll Physicians Surg Pak.
2006;16(1):45-48.
114. Buckley R, Hughes GNF, Snodgrass T, Huchcroft SA. Perioperative cefazolin prophylaxis in hip fracture surgery.
Can J Surg. 1990;33(2):122-127.
115. Garotta F, Pamparana F. Antimicrobial prophylaxis with ceftizoxime versus cefuroxime in orthopedic surgery.
Ceftizoxime Orthopedic Surgery Italian Study Group. J Chemother. 1991;3 Suppl 2:34-35.
116. Gatell JM, Garcia S, Lozano L, Soriano E, Ramon R, SanMiguel JG. Perioperative cefamandole prophylaxis against
infections. J Bone Joint Surg Am. 1987;69(8):1189-1193.
117. Ritter MA, Campbell E, Keating EM, Faris PM. Comparison of intraoperative versus 24 hour antibiotic prophylaxis
in total joint replacement. A controlled prospective study. Orthop Rev. 1989;18(6):694-696.
118. Wymenga AB, Hekster YA, Theeuwes A, Muytjens HL, van Horn JR, Slooff TJ. Antibiotic use after cefuroxime
prophylaxis in hip and knee joint replacement. Clin Pharmacol Ther. 1991;50(2):215-220.
119. Aberg C, Thore M. Single versus triple dose antimicrobial prophylaxis in elective abdominal surgery and the impact
on bacterial ecology. J Hosp Infect. 1991;18(2):149-154.
120. Bates T, Roberts JV, Smith K, German KA. A randomized trial of one versus three doses of augmentin as wound
prophylaxis in at-risk abdominal surgery. Postgrad Med J. 1992;68(804):811-816.
121. Becker JM, Alexander DP. Colectomy, mucosal proctectomy, and ileal pouch-anal anastomosis. A prospective trial
of optimal antibiotic management. Ann Surg. 1991;213(3):242-247.
122. Carr ND, Hobbiss J, Cade D, Schofield PF. Metronidazole in the prevention of wound sepsis after elective colorectal
surgery. J R Coll Surg Edinb. 1984;29(3):139-142.
123. Fujita S, Saito N, Yamada T, et al. Randomized, multicenter trial of antibiotic prophylaxis in elective colorectal
surgery: single dose vs 3 doses of a second-generation cephalosporin without metronidazole and oral antibiotics.
Arch Surg. 2007;142(7):657-661.
124. Grundmann R, Burkardt F, Scholl H, Koelschbach D. One versus three doses of metronidazole/mezlocillin for
antibiotic prophylaxis in colon surgery. Chemioterapia. 1987;6(2 Suppl):604-605.
125. Hall JC, Watts JM, Press L, O'Brien P, Turnidge J, McDonald P. Single-dose antibiotic prophylaxis in contaminated
abdominal surgery. Arch Surg. 1989;124(2):244-247.
2017 American Medical Association. All rights reserved. 48
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
126. Juul P, Klaaborg KE, Kronborg O. Single or multiple doses of metronidazole and ampicillin in elective colorectal
surgery. A randomized trial. Dis Colon Rectum. 1987;30(7):526-528.
127. Karran SJ, Sutton G, Gartell P, Karran SE, Finnis D, Blenkinsop J. Imipenem prophylaxis in elective colorectal
surgery. Br J Surg. 1993;80(9):1196-1198.
128. Kow L, Toouli J, Brookman J, McDonald PJ. Comparison of cefotaxime plus metronidazole versus cefoxitin for
prevention of wound infection after abdominal surgery. World J Surg. 1995;19(5):680-686; discussion 686.
129. McArdle CS, Morran CG, Pettit L, Gemmell CG, Sleigh JD, Tillotson GS. Value of oral antibiotic prophylaxis in
colorectal surgery. Br J Surg. 1995;82(8):1046-1048.
130. Mendel V, Jung D, Heymann H. Single-shot antibiotic prophylaxis in colon surgery. Chemioterapia. 1987;6(2
Suppl):597-600.
131. Moesgaard F, Lykkegaard-Nielsen M. Preoperative cell-mediated immunity and duration of antibiotic prophylaxis
in relation to postopertive infectious complications. A controlled trial in biliary, gastroduodenal and colorectal
surgery. Acta Chir Scand. 1989;155(4-5):281-286.
132. Mohri Y, Tonouchi H, Kobayashi M, Nakai K, Kusunoki M, Group MSIR. Randomized clinical trial of single-
versus multiple-dose antimicrobial prophylaxis in gastric cancer surgery. Br J Surg. 2007;94(6):683-688.
133. Mui LM, Ng CS, Wong SK, et al. Optimum duration of prophylactic antibiotics in acute non-perforated
appendicitis. ANZ Journal of Surg. 2005;75(6):425-428.
134. Suzuki T, Sadahiro S, Maeda Y, Tanaka A, Okada K, Kamijo A. Optimal duration of prophylactic antibiotic
administration for elective colon cancer surgery: A randomized, clinical trial. Surgery. 2011;149(2):171-178.
135. Togo S, Tanaka K, Matsuo K, et al. Duration of antimicrobial prophylaxis in patients undergoing hepatectomy: a
prospective randomized controlled trial using flomoxef. J Antimicrob Chemother. 2007;59(5):964-970.
136. Wenzel M, Heinrich M, Schmidt C. Peri-operative infection prophylaxis with ornidazole and gentamicin in elective
colonic surgery. Pharmatherapeutica. 1985;4(6):351-355.
137. Hussain MI, Alam MK, Al-Qahatani HH, Al-Akeely MH. Role of postoperative antibiotics after appendectomy in
non-perforated appendicitis. J Coll Physicians Surg Pak. 2012;22(12):756-759.
138. Haga N, Ishida H, Ishiguro T, et al. A prospective randomized study to assess the optimal duration of intravenous
antimicrobial prophylaxis in elective gastric cancer surgery. Int Surg. 2012;97(2):169-176.
139. Imamura H, Kurokawa Y, Tsujinaka T, et al. Intraoperative versus extended antimicrobial prophylaxis after gastric
cancer surgery: a phase 3, open-label, randomised controlled, non-inferiority trial. Lancet Infect Dis.
2012;12(5):381-387.
140. Hirokawa F, Hayashi M, Miyamoto Y, et al. Evaluation of postoperative antibiotic prophylaxis after liver resection:
a randomized controlled trial. Am J Surg. 2013;206(1):8-15.
141. Ruiz-Tovar J, Santos J, Arroyo A, et al. Effect of peritoneal lavage with clindamycin-gentamicin solution on
infections after elective colorectal cancer surgery. J Am Coll Surg. 2012;214(2):202-207.
142. Al-Shehri MY, Saif S, Ibrahim A, et al. Topical ampicillin for prophylaxis against wound infection in acute
appendicitis. Ann Saudi Med. 1994;14(3):233-236.
143. Kamath S, Sinha S, Shaari E, Young D, Campbell AC. Role of topical antibiotics in hip surgeries - A prospective
randomised study. Injury. 2005;36(6):783-787.
144. Neri V, Fersini A, Ambrosi A, Tartaglia N, Valentino TP. Umbilical port-site complications in laparoscopic
cholecystectomy: role of topical antibiotic therapy. JSLS. 2008;12(2):126-132.
145. Juul P, Merrild U, Kronborg O. Topical ampicillin in addition to a systemic antibiotic prophylaxis in elective
colorectal surgery. A prospective randomized study. Dis Colon Rectum. 1985;28(11):804-806.
146. Seco JL, Ojeda E, Reguilon C, et al. Combined topical and systemic antibiotic prophylaxis in acute appendicitis. Am
J Surg. 1990;159(2):226-230.
147. Raahave D, Hesselfeldt P, Pedersen T, Zachariassen A, Kann D, Hansen OH. No effect of topical ampicillin
prophylaxis in elective operations of the colon or rectum. Surg Gynecol Obstet. 1989;168(2):112-114.
148. Vander Salm TJ, Okike ON, Pasque MK, et al. Reduction of sternal infection by application of topical vancomycin.
J Thorac Cardiovasc Surg. 1989;98(4):618-622.
2017 American Medical Association. All rights reserved. 49
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
149. Almdahl SM, Veel T, Halvorsen P, Vold MB, Molstad P. Randomized prospective trial of saphenous vein harvest
site infection after wound closure with and without topical application of autologous platelet-rich plasma. Eur J
Cardiothorac Surg. 2011;39(1):44-48.
150. Peerbooms JC, de Wolf GS, Colaris JW, Bruijn DJ, Verhaar JAN. No positive effect of autologous platelet gel after
total knee arthroplasty A double-blind randomized controlled trial: 102 patients with a 3-month follow-up. Acta
Orthop. 2009;80(5):557-562.
151. Litmathe J, Philipp C, Kurt M, Boeken U, Gams E, Feindt P. The use of autologous platelet gel (APG) for high-risk
patients in cardiac surgery - is it beneficial? Perfusion. 2009;24(6):381-387.
152. Dorge H, Sellin C, Bury MC, et al. Incidence of deep sternal wound infection is not reduced with autologous platelet
rich plasma in high-risk cardiac surgery patients. Thorac Cardiovasc Surg. 2013;61(3):180-184.
153. Arnoczky SP, Shebani-Rad S. The Basic Science of Platelet-rich Plasma (PRP): What Clinicians Need to Know.
Sports Med Arthrosc. 2013;21(4):180-185.
154. Marlovits S, Mousavi M, Gabler C, Erdos J, Vecsei V. A new simplified technique for producing platelet-rich
plasma: a short technical note. Eur Spine J. 2004;13 Suppl 1:S102-106.
155. Hsu WK, Mishra A, Rodeo SR, et al. Platelet-rich plasma in orthopaedic applications: evidence-based
recommendations for treatment. J Am Acad Orthop Surg. 2013;21(12):739-748.
156. Martinez-Zapata MJ, Marti-Carvajal AJ, Sola I, et al. Autologous platelet-rich plasma for treating chronic wounds.
Cochrane Database Syst Rev. 2012;10:CD006899.
157. Bielecki TM, Gazdzik TS, Arendt J, Szczepanski T, Krol W, Wielkoszynski T. Antibacterial effect of autologous
platelet gel enriched with growth factors and other active substances: an in vitro study. J Bone Joint Surg Br.
2007;89(3):417-420.
158. Moojen DJ, Everts PA, Schure RM, et al. Antimicrobial activity of platelet-leukocyte gel against Staphylococcus
aureus. J Orthop Res. 2008;26(3):404-410.
159. O'Grady NP, Alexander M, Burns LA, et al. Guidelines for the Prevention of Intravascular Catheter-related
Infections. Am J Infect Control. 2011;39(4 Suppl 1):S1-34.
160. Ford HR, Jones P, Gaines B, Reblock K, Simpkins DL. Intraoperative handling and wound healing: controlled
clinical trial comparing coated VICRYL plus antibacterial suture (coated polyglactin 910 suture with triclosan) with
coated VICRYL suture (coated polyglactin 910 suture). Surg Infect (Larchmt). 2005;6(3):313-321.
161. Mingmalairak C, Ungbhakorn P, Paocharoen V. Efficacy of antimicrobial coating suture coated polyglactin 910
with tricosan (Vicryl plus) compared with polyglactin 910 (Vicryl) in reduced surgical site infection of appendicitis,
double blind randomized control trial, preliminary safety report. J Med Assoc Thai. 2009;92(6):770-775.
162. Rozzelle CJ, Leonardo J, Li V. Antimicrobial suture wound closure for cerebrospinal fluid shunt surgery: a
prospective, double-blinded, randomized controlled trial. J Neurosurg. 2008;2(2):111-117.
163. Diener MK, Knebel P, Kieser M, et al. Effectiveness of triclosan-coated PDS Plus versus uncoated PDS II sutures
for prevention of surgical site infection after abdominal wall closure: the randomised controlled PROUD trial.
Lancet. 2014;384(9938):142-152.
164. Galal I, El-Hindawy K. Impact of using triclosan-antibacterial sutures on incidence of surgical site infection. Am J
Surg. 2011;202(2):133-138.
165. Isik I, Selimen D, Senay S, Alhan C. Efficiency of antibacterial suture material in cardiac surgery: a double-blind
randomized prospective study. Heart Surg Forum. 2012;15(1):E40-45.
166. Thimour-Bergstrom L, Roman-Emanuel C, Schersten H, Friberg O, Gudbjartsson T, Jeppsson A. Triclosan-coated
sutures reduce surgical site infection after open vein harvesting in coronary artery bypass grafting patients: a
randomized controlled trial. Eur J Cardiothorac Surg. 2013;44(5):931-938.
167. Justinger C, Slotta JE, Ningel S, Graber S, Kollmar O, Schilling MK. Surgical-site infection after abdominal wall
closure with triclosan-impregnated polydioxanone sutures: results of a randomized clinical pathway facilitated trial
(NCT00998907). Surgery. 2013;154(3):589-595.
168. Nakamura T, Kashimura N, Noji T, et al. Triclosan-coated sutures reduce the incidence of wound infections and the
costs after colorectal surgery: a randomized controlled trial. Surgery. 2013;153(4):576-583.
2017 American Medical Association. All rights reserved. 50
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
169. Baracs J, Huszar O, Sajjadi SG, Horvath OP. Surgical site infections after abdominal closure in colorectal surgery
using triclosan-coated absorbable suture (PDS Plus) vs. uncoated sutures (PDS II): a randomized multicenter study.
Surg Infect (Larchmt). 2011;12(6):483-489.
170. Rasic Z, Schwarz D, Adam VN, et al. Efficacy of antimicrobial triclosan-coated polyglactin 910 (Vicryl* Plus)
suture for closure of the abdominal wall after colorectal surgery. Coll Antropol. 2011;35(2):439-443.
171. Williams N, Sweetland H, Goyal S, Ivins N, Leaper DJ. Randomized trial of antimicrobial-coated sutures to prevent
surgical site infection after breast cancer surgery. Surg Infect (Larchmt). 2011;12(6):469-474.
172. Turtiainen J, Saimanen EI, Makinen KT, et al. Effect of triclosan-coated sutures on the incidence of surgical wound
infection after lower limb revascularization surgery: a randomized controlled trial. World J Surg. 2012;36(10):2528-
2534.
173. Seim BE, Tonnessen T, Woldbaek PR. Triclosan-coated sutures do not reduce leg wound infections after coronary
artery bypass grafting. Interact Cardiovasc Thorac Surg. 2012;15(3):411-415.
174. Wilson AP, Treasure T, Sturridge MF, Gruneberg RN. A scoring method (ASEPSIS) for postoperative wound
infections for use in clinical trials of antibiotic prophylaxis. Lancet. 1986;1(8476):311-313.
175. Diener MK, Knebel P, Kieser M, Probst P, Buchler MW. Antibiotic sutures against surgical site infections--Authors'
reply. Lancet. 2014;384(9952):1425-1426.
176. Krieger BR, Davis DM, Sanchez JE, et al. The use of silver nylon in preventing surgical site infections following
colon and rectal surgery. Dis Colon Rectum. 2011;54(8):1014-1019.
177. Biffi R, Fattori L, Bertani E, et al. Surgical site infections following colorectal cancer surgery: a randomized
prospective trial comparing common and advanced antimicrobial dressing containing ionic silver. World J Surg
Oncol. 2012;10:94.
178. Dumville JC, Walter CJ, Sharp CA, Page T. Dressings for the prevention of surgical site infection. Cochrane
Database Syst Rev. 2011(7):CD003091.
179. Chan RP, Galas FR, Hajjar LA, Bello CN, Piccioni MA, Auler JO, Jr. Intensive perioperative glucose control does
not improve outcomes of patients submitted to open-heart surgery: a randomized controlled trial. Clinics.
2009;64(1):51-60.
180. Gandhi GY, Nuttall GA, Abel MD, et al. Intensive intraoperative insulin therapy versus conventional glucose
management during cardiac surgery: a randomized trial. Ann Intern Med. 2007;146(4):233-243.
181. Lazar HL, McDonnell M, Chipkin SR, et al. The Society of Thoracic Surgeons practice guideline series: Blood
glucose management during adult cardiac surgery. Ann Thorac Surg. 2009;87(2):663-669.
182. Umpierrez GE, Hellman R, Korytkowski MT, et al. Management of hyperglycemia in hospitalized patients in non-
critical care setting: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(1):16-38.
183. Jacobi J, Bircher N, Krinsley J, et al. Guidelines for the use of an insulin infusion for the management of
hyperglycemia in critically ill patients. Crit Care Med. 2012;40(12):3251-3276.
184. Qaseem A, Humphrey LL, Chou R, Snow V, Shekelle P, Physicians CGCotACo. Use of intensive insulin therapy
for the management of glycemic control in hospitalized patients: a clinical practice guideline from the American
College of Physicians. Ann Intern Med. 2011;154(4):260-267.
185. Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection
and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334(19):1209-
1215.
186. Melling AC, Ali B, Scott EM, Leaper DJ. Effects of preoperative warming on the incidence of wound infection after
clean surgery: a randomised controlled trial. Lancet. 2001;358(9285):876-880.
187. Wong PF, Kumar S, Bohra A, Whetter D, Leaper DJ. Randomized clinical trial of perioperative systemic warming
in major elective abdominal surgery. Br J Surg. 2007;94(4):421-426.
188. National Institute for Clincial Excellence (NICE). Management of Inadvertent Perioperative Hypothermia in Adults
(NICE Clinical Guideline 65). 2008; http://www.nice.org.uk/Guidance/CG65. Accessed January 25, 2017.
189. Forbes SS, Eskicioglu C, Nathens AB, et al. Evidence-based guidelines for prevention of perioperative hypothermia.
J Am Coll Surg. 2009;209(4):492-503 e491.
2017 American Medical Association. All rights reserved. 51
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
190. Hooper VD, Chard R, Clifford T, et al. ASPAN's evidence-based clinical practice guideline for the promotion of
perioperative normothermia: second edition. J Perianesth Nurs. 2010;25(6):346-365.
191. Burlingame B, Denholm B, Link T, et al. Guideline for Prevention of Unplanned Patient Hypothermia. In: Connor
R, ed. AORN Guidelines for Perioperative Practice. Denver, CO: Association of periOperative Registered, Nurses;
2016.
192. Thibon P, Borgey F, Boutreux S, Hanouz JL, Le Coutour X, Parienti JJ. Effect of perioperative oxygen
supplementation on 30-day surgical site infection rate in abdominal, gynecologic, and breast surgery: the ISO2
randomized controlled trial. Anesthesiology. 2012;117(3):504-511.
193. Belda FJ, Aguilera L, Garcia de la Asuncion J, et al. Supplemental perioperative oxygen and the risk of surgical
wound infection: a randomized controlled trial. JAMA. 2005;294(16):2035-2042.
194. Bickel A, Gurevits M, Vamos R, Ivry S, Eitan A. Perioperative hyperoxygenation and wound site infection
following surgery for acute appendicitis: a randomized, prospective, controlled trial. Arch Surg. 2011;146(4):464-
470.
195. Greif R, Akca O, Horn EP, Kurz A, Sessler DI, Group OR. Supplemental perioperative oxygen to reduce the
incidence of surgical-wound infection. N Engl J Med. 2000;342(3):161-167.
196. Meyhoff CS, Wetterslev J, Jorgensen LN, et al. Effect of high perioperative oxygen fraction on surgical site
infection and pulmonary complications after abdominal surgery The PROXI randomized clinical trial. JAMA.
2009;302(14):1543-1550.
197. Pryor KO, Fahey TJ, 3rd, Lien CA, Goldstein PA. Surgical site infection and the routine use of perioperative
hyperoxia in a general surgical population: a randomized controlled trial. J Am Med Assoc. 2004;291(1):79-87.
198. Staehr AK, Meyhoff CS, Rasmussen LS, Group PT. Inspiratory oxygen fraction and postoperative complications in
obese patients: a subgroup analysis of the PROXI trial. Anesthesiology. 2011;114(6):1313-1319.
199. Stall A, Paryavi E, Gupta R, Zadnik M, Hui E, O'Toole RV. Perioperative supplemental oxygen to reduce surgical
site infection after open fixation of high-risk fractures: a randomized controlled pilot trial. J Trauma Acute Care
Surg. 2013;75(4):657-663.
200. Meyhoff CS, Jorgensen LN, Wetterslev J, Christensen KB, Rasmussen LS, Group PT. Increased long-term mortality
after a high perioperative inspiratory oxygen fraction during abdominal surgery: follow-up of a randomized clinical
trial. Anesth Analg. 2012;115(4):849-854.
201. Gardella C, Goltra LB, Laschansky E, et al. High-concentration supplemental perioperative oxygen to reduce the
incidence of postcesarean surgical site infection: a randomized controlled trial. Obstet Gynecol. 2008;112(3):545-
552.
202. Duggal N, Poddatoori V, Noroozkhani S, Siddik-Ahmad RI, Caughey AB. Perioperative oxygen supplementation
and surgical site infection after cesarean delivery: a randomized trial. Obstet Gynecol. 2013;122(1):79-84.
203. Scifres CM, Leighton BL, Fogertey PJ, Macones GA, Stamilio DM. Supplemental oxygen for the prevention of
postcesarean infectious morbidity: a randomized controlled trial. Am J Obstet Gynecol. 2011;205(3):267 e261-269.
204. Turtiainen J, Saimanen EI, Partio TJ, et al. Supplemental postoperative oxygen in the prevention of surgical wound
infection after lower limb vascular surgery: a randomized controlled trial. World J Surg. 2011;35(6):1387-1395.
205. Whitney JD, Heiner S, Mygrant BI, Wood C. Tissue and wound healing effects of short duration postoperative
oxygen therapy. Biol Res Nurs. 2001;2(3):206-215.
206. Webster J, Osborne S. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection.
Cochrane Database Syst Rev. 2012;9(9):CD004985.
207. Byrne DJ, Napier A, Cuschieri A. The value of whole body disinfection in the prevention of postoperative wound
infection in clean and potentially contaminated surgery. A prospective, randomised, double-blind placebo-controlled
clinical trial. Surg Res Commun. 1992;12(1):43-52.
208. Earnshaw JJ, Berridge DC, Slack RC, Makin GS, Hopkinson BR. Do preoperative chlorhexidine baths reduce the
risk of infection after vascular reconstruction? Eur J Vasc Surg. 1989;3(4):323-326.
209. Hayek LJ, Emerson JM, Gardner AM. A placebo-controlled trial of the effect of two preoperative baths or showers
with chlorhexidine detergent on postoperative wound infection rates. J Hosp Infect. 1987;10(2):165-172.
210. Randall PE, Ganguli L, Marcuson RW. Wound infection following vasectomy. Br J Urol. 1983;55(5):564-567.
2017 American Medical Association. All rights reserved. 52
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
211. Rotter ML, Larsen SO, Cooke EM, et al. A comparison of the effects of preoperative whole-body bathing with
detergent alone and with detergent containing chlorhexidine gluconate on the frequency of wound infections after
clean surgery. J Hosp Infect. 1988;11(4):310-320.
212. Veiga DF, Damasceno CA, Veiga-Filho J, et al. Randomized controlled trial of the effectiveness of chlorhexidine
showers before elective plastic surgical procedures. Infect Control Hosp Epidemiol. 2009;30(1):77-79.
213. Wihlborg O. The effect of washing with chlorhexidine soap on wound infection rate in general surgery. A controlled
clinical study. Ann Chir Gynaecol. 1987;76(5):263-265.
214. Veiga DF, Damasceno CA, Veiga Filho J, et al. Influence of povidone-iodine preoperative showers on skin
colonization in elective plastic surgery procedures. Plast Reconstr Surg. 2008;121(1):115-118; discussion 119-120.
215. Murray MR, Saltzman MD, Gryzlo SM, Terry MA, Woodward CC, Nuber GW. Efficacy of preoperative home use
of 2% chlorhexidine gluconate cloth before shoulder surgery. J Shoulder Elbow Surg. 2011;20(6):928-933.
216. Berry AR, Watt B, Goldacre MJ, Thomson JW, McNair TJ. A comparison of the use of povidone-iodine and
chlorhexidine in the prophylaxis of postoperative wound infection. J Hosp Infect. 1982;3(1):55-63.
217. Bibbo C, Patel DV, Gehrmann RM, Lin SS. Chlorhexidine provides superior skin decontamination in foot and ankle
surgery: a prospective randomized study. Clin Orthop Relat Res. 2005;438:204-208.
218. Cheng K, Robertson H, St Mart JP, Leanord A, McLeod I. Quantitative analysis of bacteria in forefoot surgery: a
comparison of skin preparation techniques. Foot Ankle Int. 2009;30(10):992-997.
219. Darouiche RO, Wall MJ, Jr., Itani KM, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site
antisepsis. N Engl J Med. 2010;362(1):18-26.
220. Ellenhorn JD, Smith DD, Schwarz RE, et al. Paint-only is equivalent to scrub-and-paint in preoperative preparation
of abdominal surgery sites. J Am Coll Surg. 2005;201(5):737-741.
221. Gilliam DL, Nelson CL. Comparison of a one-step iodophor skin preparation versus traditional preparation in total
joint surgery. Clin Orthop Relat Res. 1990(250):258-260.
222. Hort KR, DeOrio JK. Residual bacterial contamination after surgical preparation of the foot or ankle with or without
alcohol. Foot Ankle Int. 2002;23(10):946-948.
223. Ostrander RV, Botte MJ, Brage ME. Efficacy of surgical preparation solutions in foot and ankle surgery. J Bone
Joint Surg Am. 2005;87(5):980-985.
224. Paocharoen V, Mingmalairak C, Apisarnthanarak A. Comparison of surgical wound infection after preoperative skin
preparation with 4% chlorhexidine [correction of chlohexidine] and povidone iodine: a prospective randomized trial.
J Med Assoc Thai. 2009;92(7):898-902.
225. Roberts A, Wilcox K, Devineni R, Harris R, Osevala M. Skin preparation in CABG surgery: a prospective
randomized trial. Complication Surg. 1995;14(6):724, 741-724, 747.
226. Saltzman MD, Nuber GW, Gryzlo SM, Marecek GS, Koh JL. Efficacy of surgical preparation solutions in shoulder
surgery. J Bone Joint Surg Am. 2009;91(8):1949-1953.
227. Segal CG, Anderson JJ. Preoperative skin preparation of cardiac patients. AORN J. 2002;76(5):821-828.
228. Sistla SC, Prabhu G, Sistla S, Sadasivan J. Minimizing wound contamination in a 'clean' surgery: comparison of
chlorhexidine-ethanol and povidone-iodine. Chemotherapy. 2010;56(4):261-267.
229. Veiga DF, Damasceno CAV, Veiga J, et al. Povidone iodine versus chlorhexidine in skin antisepsis before elective
plastic surgery procedures: a randomized controlled trial. Plast Reconstr Surg. 2008;122(5):170e-171e.
230. Savage JW, Weatherford BM, Sugrue PA, et al. Efficacy of surgical preparation solutions in lumbar spine surgery. J
Bone Joint Surg Am. 2012;94(6):490-494.
231. Burlingame B, Denholm B, Link T, et al. Guideline for Preoperative Patient Skin Antisepsis. In: Connor R, ed.
AORN Guidelines for Perioperative Practice. Denver, CO: Association of periOperative Registered, Nurses; 2016.
232. Iyer A, Gilfillan I, Thakur S, Sharma S. Reduction of surgical site infection using a microbial sealant: a randomized
trial. J Thorac Cardiovasc Surg. 2011;142(2):438-442.
233. Towfigh S, Cheadle WG, Lowry SF, Malangoni MA, Wilson SE. Significant reduction in incidence of wound
contamination by skin flora through use of microbial sealant. Arch Surg. 2008;143(9):885-891; discussion 891.
2017 American Medical Association. All rights reserved. 53
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
234. von Eckardstein AS, Lim CH, Dohmen PM, et al. A randomized trial of a skin sealant to reduce the risk of incision
contamination in cardiac surgery. Ann Thorac Surg. 2011;92(2):632-637.
235. Dromzee E, Tribot-Laspiere Q, Bachy M, Zakine S, Mary P, Vialle R. Efficacy of integuseal for surgical skin
preparation in children and adolescents undergoing scoliosis correction. Spine (Phila Pa 1976). 2012;37(21):E1331-
1335.
236. Bailey IS, Karran SE, Toyn K, Brough P, Ranaboldo C, Karran SJ. Community surveillance of complications after
hernia surgery. BMJ. 1992;304(6825):469-471.
237. Chiu KY, Lau SK, Fung B, Ng KH, Chow SP. Plastic adhesive drapes and wound infection after hip fracture
surgery. Aust N Z J Surg. 1993;63(10):798-801.
238. Dewan PA, Van Rij AM, Robinson RG, Skeggs GB, Fergus M. The use of an iodophor-impregnated plastic incise
drape in abdominal surgery--a controlled clinical trial. Aust N Z J Surg. 1987;57(11):859-863.
239. Jackson DW, Pollock AV, Tindal DS. The value of a plastic adhesive drape in the prevention of wound infection. A
controlled trial. Br J Surg. 1971;58(5):340-342.
240. Psaila JV, Wheeler MH, Crosby DL. The role of plastic wound drapes in the prevention of wound infection
following abdominal surgery. Br J Surg. 1977;64(10):729-732.
241. Ward HRG, Jennings OGN, Potgieter P, Lombard CJ. Do plastic adhesive drapes prevent post caesarean wound
infection? J Hosp Infect. 2001;47(3):230-234.
242. Burlingame B, Denholm B, Link T, et al. Guideline for Sterile Technique. In: Connor R, ed. AORN Guidelines for
Perioperative Practice. Denver, CO: AORN; 2016.
243. Chang FY, Chang MC, Wang ST, Yu WK, Liu CL, Chen TH. Can povidone-iodine solution be used safely in a
spinal surgery? Eur Spine J. 2006;15(6):1005-1014.
244. Cheng MT, Chang MC, Wang ST, Yu WK, Liu CL, Chen TH. Efficacy of dilute betadine solution irrigation in the
prevention of postoperative infection of spinal surgery. Spine (Phila Pa 1976). 2005;30(15):1689-1693.
245. Rogers DM, Blouin GS, O'Leary JP. Povidone-iodine wound irrigation and wound sepsis. Surg Gynecol Obstet.
1983;157(5):426-430.
246. Sindelar WF, Brower ST, Merkel AB, Takesue EI. Randomised trial of intraperitoneal irrigation with low molecular
weight povidone-iodine solution to reduce intra-abdominal infectious complications. J Hosp Infect. 1985;6 Suppl
A:103-114.
247. Sindelar WF, Mason GR. Intraperitoneal irrigation with povidone-iodine solution for the prevention of intra-
abdominal abscesses in the bacterially contaminated abdomen. Surg Gynecol Obstet. 1979;148(3):409-411.
248. Sindelar WF, Mason GR. Irrigation of subcutaneous tissue with povidone-iodine solution for prevention of surgical
wound infections. Surg Gynecol Obstet. 1979;148(2):227-231.
249. Vallance S, Waldron R. Antiseptic vs. saline lavage in purulent and faecal peritonitis. J Hosp Infect. 1985;6 Suppl
A:87-91.
250. Harihara Y, Konishi T, Kobayashi H, et al. Effects of applying povidone-iodine just before skin closure.
Dermatology. 2006;212:53-57.
251. Frietsch T, Karger R, Scholer M, et al. Leukodepletion of autologous whole blood has no impact on perioperative
infection rate and length of hospital stay. Transfusion. 2008;48(10):2133-2142.
252. Frietsch T, Krombholz K, Tolksdorf B, Nebe T, Segiet W, Lorentz A. Cellular immune response to autologous
blood transfusion in hip arthroplasty: whole blood versus buffy coat-poor packed red cells and fresh-frozen plasma.
Vox Sang. 2001;81(3):187-193.
253. Innerhofer P, Klingler A, Klimmer C, Fries D, Nussbaumer W. Risk for postoperative infection after transfusion of
white blood cell-filtered allogeneic or autologous blood components in orthopedic patients undergoing primary
arthroplasty. Transfusion. 2005;45(1):103-110.
254. Rosencher N, Kerkkamp HEM, Macheras G, et al. Orthopedic Surgery Transfusion Hemoglobin European
Overview (OSTHEO) study: blood management in elective knee and hip arthroplasty in Europe. Transfusion.
2003;43(4):459-469.
2017 American Medical Association. All rights reserved. 54
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
255. Weber EW, Slappendel R, Prins MH, van der Schaaf DB, Durieux ME, Strumper D. Perioperative blood
transfusions and delayed wound healing after hip replacement surgery: effects on duration of hospitalization. Anesth
Analg. 2005;100(5):1416-1421, table of contents.
256. Llewelyn CA, Taylor RS, Todd AAM, et al. The effect of universal leukoreduction on postoperative infections and
length of hospital stay in elective orthopedic and cardiac surgery. Transfusion. 2004;44(4):489-500.
257. Borghi B, Casati A, Rizzoli Study Group on Orthopaedic Anaesthesia. Incidence and risk factors for allogenic blood
transfusion during major joint replacement using an integrated autotransfusion regimen. Eur J Anaesthesiol.
2000;17(7):411-417.
258. del Trujillo MM, Carrero A, Munoz M. The utility of the perioperative autologous transfusion system OrthoPAT (R)
in total hip replacement surgery: a prospective study. Arch Orthop Trauma Surg. 2008;128(10):1031-1038.
259. Pedersen AB, Mehnert F, Overgaard S, Johnsen SP. Allogeneic blood transfusion and prognosis following total hip
replacement: a population-based follow up study. BMC Musculoskelet Disord. 2009;10:167.
260. Carson JL, Grossman BJ, Kleinman S, et al. Red blood cell transfusion: a clinical practice guideline from the
AABB*. Ann Intern Med. 2012;157(1):49-58.
261. Kawakami K, Ikari K, Kawamura K, et al. Complications and features after joint surgery in rheumatoid arthritis
patients treated with tumour necrosis factor-alpha blockers: perioperative interruption of tumour necrosis factor-
alpha blockers decreases complications? Rheumatology (Oxford). 2010;49(2):341-347.
262. Momohara S, Kawakami K, Iwamoto T, et al. Prosthetic joint infection after total hip or knee arthroplasty in
rheumatoid arthritis patients treated with nonbiologic and biologic disease-modifying antirheumatic drugs. Mod
Rheumatol. 2011;21(5):469-475.
263. Hirano Y, Kojima T, Kanayama Y, et al. Influences of anti-tumour necrosis factor agents on postoperative recovery
in patients with rheumatoid arthritis. Clin Rheumatol. 2010;29(5):495-500.
264. Perhala RS, Wilke WS, Clough JD, Segal AM. Local infectious complications following large joint replacement in
rheumatoid arthritis patients treated with methotrexate versus those not treated with methotrexate. Arthritis Rheum.
1991;34(2):146-152.
265. Visser K, Katchamart W, Loza E, et al. Multinational evidence-based recommendations for the use of methotrexate
in rheumatic disorders with a focus on rheumatoid arthritis: integrating systematic literature research and expert
opinion of a broad international panel of rheumatologists in the 3E Initiative. Ann Rheum Dis. 2009;68(7):1086-
1093.
266. Bongartz T, Halligan CS, Osmon DR, et al. Incidence and risk factors of prosthetic joint infection after total hip or
knee replacement in patients with rheumatoid arthritis. Arthritis Rheum. 2008;59(12):1713-1720.
267. Bridges SL, Jr., Lopez-Mendez A, Han KH, Tracy IC, Alarcon GS. Should methotrexate be discontinued before
elective orthopedic surgery in patients with rheumatoid arthritis? J Rheumatol. 1991;18(7):984-988.
268. Carpenter MT, West SG, Vogelgesang SA, Casey Jones DE. Postoperative joint infections in rheumatoid arthritis
patients on methotrexate therapy. Orthopedics. 1996;19(3):207-210.
269. Saag KG, Teng GG, Patkar NM, et al. American College of Rheumatology 2008 recommendations for the use of
nonbiologic and biologic disease-modifying antirheumatic drugs in rheumatoid arthritis. Arthritis Rheum.
2008;59(6):762-784.
270. Ledingham J, Deighton C, British Society for Rheumatology Standards, Guidelines and Audit Working Group.
Update on the British Society for Rheumatology guidelines for prescribing TNFalpha blockers in adults with
rheumatoid arthritis (update of previous guidelines of April 2001). Rheumatology (Oxford). 2005;44(2):157-163.
271. Singh JA, Furst DE, Bharat A, et al. 2012 update of the 2008 American College of Rheumatology recommendations
for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of rheumatoid arthritis.
Arthritis Care Res. 2012;64(5):625-639.
272. Desai A, Ramankutty S, Board T, Raut V. Does intraarticular steroid infiltration increase the rate of infection in
subsequent total knee replacements? Knee. 2009;16(4):262-264.
273. Papavasiliou AV, Isaac DL, Marimuthu R, Skyrme A, Armitage A. Infection in knee replacements after previous
injection of intra-articular steroid. J Bone Joint Surg Br. 2006;88B(3):321-323.
2017 American Medical Association. All rights reserved. 55
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
274. Kaspar S, de Beer JD. Infection in hip arthroplasty after previous injection of steroid. J Bone Joint Surg Br.
2005;87B(4):454-457.
275. McIntosh AL, Hanssen AD, Wenger DE, Osmon DR. Recent intraarticular steroid injection may increase infection
rates in primary THA. Clin Orthop Relat Res. 2006;451:50-54.
276. Sreekumar R, Venkiteswaran R, Raut V. Infection in primary hip arthroplasty after previous steroid infiltration. Int
Orthop. 2007;31(1):125-128.
277. Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use
of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res.
2012;64(4):465-474.
278. Centers for Disease Control and Prevention, Siegel JD, Rhinehart E, Jackson M, Chiarello L, Healthcare Infection
Control Practices Advisory Committee. 2007 Guideline for Isolation Precautions: Preventing Transmission of
Infectious Agents in Healthcare Settings 2007; Available at:
http://www.cdc.gov/hicpac/2007IP/2007isolationPrecautions.html. Accessed January 25, 2017.
279. Turpie AGG, Bauer KA, Eriksson BL, Lassen MR, Steering Committees of the Pentasaccharide Orthopedic
Prophylaxis Studies. Fondaparinux vs enoxaparin for the prevention of venous thromboembolism in major
orthopedic surgery - A meta-analysis of 4 randomized double-blind studies. Arch Intern Med. 2002;162(16):1833-
1840.
280. Eriksson BI, Borris LC, Friedman RJ, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after hip
arthroplasty. N Engl J Med. 2008;358(26):2765-2775.
281. Turpie AG, Lassen MR, Davidson BL, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee
arthroplasty (RECORD4): a randomised trial. Lancet. 2009;373(9676):1673-1680.
282. Kakkar AK, Brenner B, Dahl OE, et al. Extended duration rivaroxaban versus short-term enoxaparin for the
prevention of venous thromboembolism after total hip arthroplasty: a double-blind, randomised controlled trial.
Lancet. 2008;372(9632):31-39.
283. Lassen MR, Ageno W, Borris LC, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee
arthroplasty. N Engl J Med. 2008;358(26):2776-2786.
284. Asensio A, Antolin FJ, Sanchez-Garcia JM, et al. Timing of DVT prophylaxis and risk of postoperative knee
prosthesis infection. Orthopedics. 2010;33(11):800.
285. Parvizi J, Ghanem E, Joshi A, Sharkey PF, Hozack WJ, Rothman RH. Does "excessive" anticoagulation predispose
to periprosthetic infection? J Arthroplasty. 2007;22(6):24-28.
286. Patel VP, Walsh M, Sehgal B, Preston C, Dewal H, Di Cesare PE. Factors associated with prolonged wound
drainage after primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89A(1):33-38.
287. Sachs RA, Smith JH, Kuney M, Paxton L. Does anticoagulation do more harm than good? A comparison of patients
treated without prophylaxis and patients treated with low-dose warfarin after total knee arthroplasty. J Arthroplasty.
2003;18(4):389-395.
288. Bauer KA, Eriksson BI, Lassen MR, Turpie AG, Steering Committee of the Pentasaccharide in Major Knee Surgery
Study. Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after elective major
knee surgery. N Engl J Med. 2001;345(18):1305-1310.
289. Eriksson BI, Bauer KA, Lassen MR, Turpie AG, Steering Committee of the Pentasaccharide in Hip-Fracture
Surgery Study. Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after hip-
fracture surgery. N Engl J Med. 2001;345(18):1298-1304.
290. Lassen MR, Bauer KA, Eriksson BI, Turpie AG, European Pentasaccharide Elective Surgery Study Steering
Committee. Postoperative fondaparinux versus preoperative enoxaparin for prevention of venous thromboembolism
in elective hip-replacement surgery: a randomised double-blind comparison. Lancet. 2002;359(9319):1715-1720.
291. Turpie AG, Bauer KA, Eriksson BI, Lassen MR, Pentathalon Study Steering Committee. Postoperative
fondaparinux versus postoperative enoxaparin for prevention of venous thromboembolism after elective hip-
replacement surgery: a randomised double-blind trial. Lancet. 2002;359(9319):1721-1726.
292. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic
therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical
Practice Guidelines. Chest. 2012;141(2 Suppl):e278S-325S.
2017 American Medical Association. All rights reserved. 56
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
293. Jacobs JJ, Mont MA, Bozic KJ, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on:
preventing venous thromboembolic disease in patients undergoing elective hip and knee arthroplasty. J Bone Joint
Surg Am. 2012;94(8):746-747.
294. Hooper GJ, Rothwell AG, Frampton C, Wyatt MC. Does the use of laminar flow and space suits reduce early deep
infection after total hip and knee replacement? The ten-year results of the New Zealand Joint Registry. J Bone Joint
Surg Br. 2011;93B(1):85-90.
295. Miner AL, Losina E, Katz JN, Fossel AH, Platt R. Deep infection after total knee replacement: impact of laminar
airflow systems and body exhaust suits in the modern operating room. Infect Control Hosp Epidemiol.
2007;28(2):222-226.
296. Pasquarella C, Pitzurra O, Herren T, Poletti L, Savino A. Lack of influence of body exhaust gowns on aerobic
bacterial surface counts in a mixed-ventilation operating theatre. A study of 62 hip arthroplasties. J Hosp Infect.
2003;54(1):2-9.
297. Chiu FY, Chen CM, Lin CF, Lo WH. Cefuroxime-impregnated cement in primary total knee arthroplasty: a
prospective, randomized study of three hundred and forty knees. J Bone Joint Surg Am. 2002;84-A(5):759-762.
298. Chiu FY, Lin CF, Chen CM, Lo WH, Chaung TY. Cefuroxime-impregnated cement at primary total knee
arthroplasty in diabetes mellitus. A prospective, randomised study. J Bone Joint Surg Br. 2001;83(5):691-695.
299. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. Meeting Minutes:
Healthcare Infection Control Practices Advisory Committee (HICPAC), July 2014. 2014;
http://www.cdc.gov/hicpac/pdf/mm/HICPAC_July2014_Summary_With_Liaison_ReportsFINAL.pdf. Accessed
January 25, 2017.
300. Centers for Disease Control and Prevention, Healthcare Infection Control Practices Advisory Committee. Guideline
for Hand Hygiene in Health-Care Settings: Recommendations of the Healthcare Infection Control Practices
Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. MMWR. 2002;51(RR-16):1-
56.
301. Facilities Guidelines Institute, American Society for Healthcare Engineering. Guidelines for design and construction
of hospitals and outpatient facilities. Chicago, IL: American Hospital Association; 2014.
2017 American Medical Association. All rights reserved. 57
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
eAppendix 2. Centers for Disease Control and Prevention, Guideline for the Prevention of Surgical Site Infection 2017: Supplemental Tables
TABLE OF CONTENTS
1. GUIDELINE SEARCH STRATEGIES ..................................................................................................................................................................................................................... 61
1.1. Core Section Search Strategies ........................................................................................................................................................................................................................... 62
1.1A. CORE SECTION GENERAL SEARCHES ................................................................................................................................................................................................ 62
1.2. Prosthetic Joint Arthroplasty Section Search Strategies ..................................................................................................................................................................................... 64
1.2A. PROSTHETIC JOINT ARTHROPLASTY SECTION GENERAL SEARCHES ...................................................................................................................................... 64
1.2B. PROSTHETIC JOINT ARTHROPLASTY SECTION TARGETED SEARCHES: TRANSFUSION ...................................................................................................... 66
1.2C. PROSTHETIC JOINT ARTHROPLASTY SECTION TARGETED SEARCHES: IMMUNOSUPPRESSIVE THERAPY .................................................................... 71
1.2D. PROSTHETIC JOINT ARTHROPLASTY SECTION TARGETED SEARCHES: ANTICOAGULATION ........................................................................................... 76
1.2E. PROSTHETIC JOINT ARTHROPLASTY SECTION TARGETED SEARCHES: ORTHOPAEDIC SPACE SUIT ............................................................................... 81
1.2F. PROSTHETIC JOINT ARTHROPLASTY SECTION TARGETED SEARCH: ANTIMICROBIAL PROPHYLAXIS WITH A DRAIN .............................................. 87
1.2G. PROSTHETIC JOINT ARTHROPLASTY SECTION TARGETED SEARCH: BIOFILM ...................................................................................................................... 92
2. EVIDENCE, GRADE and RISK OF BIAS ASSESSMENT TABLES...................................................................................................................................................................... 96
2.1. Core Section GRADE, Evidence, and Risk of Bias Assessment Tables ............................................................................................................................................................. 96
2.1A. Q1 PARENTERAL ANTIMICROBIAL PROPHYLAXIS (AMP) ............................................................................................................................................................ 96
2.1B. Q2 NON-PARENTERAL AMP ................................................................................................................................................................................................................ 226
2.1C. Q3 GLYCEMIC CONTROL ..................................................................................................................................................................................................................... 310
2.1D. Q4-5 NORMOTHERMIA ......................................................................................................................................................................................................................... 315
2.1E. Q6-7 OXYGENATION ............................................................................................................................................................................................................................. 328
2.1F. Q8-10 ANTISEPTIC PROPHYLAXIS ..................................................................................................................................................................................................... 371
2.2. Prosthetic Joint Arthroplasty Section GRADE, Evidence, and Risk of Bias Assessment Tables ..................................................................................................................... 446
2.2A. Q11 BLOOD TRANSFUSION ................................................................................................................................................................................................................. 446
2.2B. Q12-16 SYSTEMIC IMMUNOSUPPRESSIVE THERAPY.................................................................................................................................................................... 496
2.2C. Q17 ANTICOAGULATION ..................................................................................................................................................................................................................... 531
2.2D. Q18 ORTHOPAEDIC SPACE SUIT ........................................................................................................................................................................................................ 566
2.2E. Q20 BIOFILM ........................................................................................................................................................................................................................................... 578
3. EVALUATION OF THE RISK OF BIAS OF AN INDIVIDUAL STUDY ............................................................................................................................................................ 586
3.1. Instructions ........................................................................................................................................................................................................................................................ 586
3.2. Checklist for Systematic Reviews ..................................................................................................................................................................................................................... 586
2017 American Medical Association. All rights reserved. 58
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
3.3. Checklist for Randomized Controlled Trials..................................................................................................................................................................................................... 586
3.4. Checklist for Observational Studies .................................................................................................................................................................................................................. 586
3.5. Translating Risk of Bias into GRADE Tables .................................................................................................................................................................................................. 587
4. EVIDENCE TABLE EXTRACTION TEMPLATES .............................................................................................................................................................................................. 588
5. STUDY TYPE DETERMINATION ........................................................................................................................................................................................................................ 590
6. REFERENCES ......................................................................................................................................................................................................................................................... 591
LIST OF FIGURES
eFIGURE A. STUDY TYPE DETERMINATION ALGORITHM (Adapted from: Hartling et. al. 2010) .................................................................................................................. 590
LIST OF TABLES
eTABLE 1. MEDLINE Search: Core Section ................................................................................................................................................................................................................ 62
eTABLE 2. EMBASE Search: Core Section .................................................................................................................................................................................................................. 62
eTABLE 3. MEDLINE Search: Ortho Section ............................................................................................................................................................................................................... 64
eTABLE 4. EMBASE Search: Ortho Section................................................................................................................................................................................................................. 65
eTABLE 5. MEDLINE Targeted Search: Transfusion ................................................................................................................................................................................................... 66
eTABLE 6. EMBASE Targeted Search: Transfusion ..................................................................................................................................................................................................... 68
eTABLE 7. Cochrane Database of Systematic Reviews Targeted Search: Transfusion ................................................................................................................................................. 70
eTABLE 8. MEDLINE Targeted Search: Immunosuppressive Therapy........................................................................................................................................................................ 71
eTABLE 9. EMBASE Targeted Search: Immunosuppressive Therapy ......................................................................................................................................................................... 74
eTABLE 10. Cochrane Database of Systematic Reviews Targeted Search: Immunosuppressive Therapy.................................................................................................................... 75
eTABLE 11. MEDLINE Targeted Search: Anticoagulation .......................................................................................................................................................................................... 76
eTABLE 12. EMBASE Targeted Search: Anticoagulation ............................................................................................................................................................................................ 78
eTABLE 13. Cochrane Database of Systematic Reviews Targeted Search: Anticoagulation ........................................................................................................................................ 80
eTABLE 14. MEDLINE Targeted Search: Orthopaedic Space Suit .............................................................................................................................................................................. 81
eTABLE 15. EMBASE Targeted Search: Orthopaedic Space Suit ................................................................................................................................................................................ 83
eTABLE 16. Cochrane Database of Systematic Reviews Targeted Search: Orthopaedic Space Suit ............................................................................................................................ 85
eTABLE 17. CINAHL Targeted Search: Orthopaedic Space Suit ................................................................................................................................................................................. 85
eTABLE 18. MEDLINE Targeted Search: Antimicrobial Prophylaxis with a Drain ..................................................................................................................................................... 87
eTABLE 19. EMBASE Targeted Search: Antimicrobial Prophylaxis with a Drain....................................................................................................................................................... 89
eTABLE 20. Cochrane Database of Systematic Reviews Targeted Search: Antimicrobial Prophylaxis with a Drain................................................................................................... 91
eTABLE 21. MEDLINE Targeted Search: Biofilm........................................................................................................................................................................................................ 92
2017 American Medical Association. All rights reserved. 59
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
eTABLE 22. EMBASE Targeted Search: Biofilm ......................................................................................................................................................................................................... 94
eTABLE 23. Cochrane Database of Systematic Reviews Targeted Search: Biofilm ..................................................................................................................................................... 95
eTABLE 24. GRADE Table for Q1 Parenteral AMP ..................................................................................................................................................................................................... 96
eTABLE 25. Evidence Table for Q1A. What is the optimal timing of preoperative AMP in surgeries involving tourniquet inflation? ..................................................................... 119
eTABLE 26. Evidence Table for Q1B. What is the optimal timing of AMP in cesarean section: prior to skin incision or at cord clamping? ............................................................ 123
eTABLE 27. Evidence Table for Q1D. How safe and effective is intraoperative redosing of AMP? .......................................................................................................................... 142
eTABLE 28. Evidence Table for Q1E. How safe and effective is postoperative AMP and what is the optimal duration? .......................................................................................... 144
eTABLE 29. Risk of Bias Assessments of Randomized Controlled Trials for Q1 Parenteral AMP ............................................................................................................................ 223
eTABLE 30. GRADE Table for Q2 Non-Parenteral AMP ........................................................................................................................................................................................... 226
eTABLE 31. Evidence Table for Q2A. How safe and effective is antimicrobial irrigation? ........................................................................................................................................ 242
eTABLE 32. Evidence Table for Q2B. How safe and effective are antimicrobial agents applied to the surgical incision?......................................................................................... 246
eTABLE 33. Evidence Table for Q2C. How safe and effective are antimicrobial-coated sutures; when and how should they be used? .................................................................... 267
eTABLE 34. Evidence Table for Q2D. How safe and effective are antimicrobial dressings applied to surgical incisions following primary closure in the operating room? .......... 304
eTABLE 35. Risk of Bias Assessments of Randomized Controlled Trials for Q2 Non-Parenteral AMP .................................................................................................................... 308
eTABLE 36. GRADE Table for Q3 Glycemic Control ................................................................................................................................................................................................ 310
eTABLE 37. Evidence Table for Q3. How do perioperative blood glucose and hemoglobin A1C levels impact the risk of SSI and what are their optimal perioperative target levels
in diabetic and non-diabetic patients? ........................................................................................................................................................................................................................... 312
eTABLE 38. Risk of Bias Assessments of Randomized Controlled Trials for Q3 Glycemic Control ......................................................................................................................... 314
eTABLE 39. GRADE Table for Q4-5 Normothermia .................................................................................................................................................................................................. 315
eTABLE 40. Evidence Table for Q4. How safe and effective is the maintenance of perioperative normothermia in reducing the risk of SSI? ......................................................... 318
eTABLE 41. Risk of Bias Assessments of Randomized Controlled Trials for Q4-5 Normothermia ........................................................................................................................... 327
eTABLE 42. GRADE Table for Q6-7 Oxygenation ..................................................................................................................................................................................................... 328
eTABLE 43. Evidence Table for Q6. In patients with normal pulmonary function, how safe and effective is the perioperative use of increased fraction of inspired oxygen (FiO2) in
reducing the risk of SSI? ............................................................................................................................................................................................................................................... 337
eTABLE 44. Risk of Bias Assessments of Randomized Controlled Trials for Q6-7 Oxygenation .............................................................................................................................. 370
eTABLE 45. GRADE Table for Q8-10 Antiseptic Prophylaxis ................................................................................................................................................................................... 371
eTABLE 46. Evidence Table for Q8A. How safe and effective is preoperative antiseptic bathing or showering? ...................................................................................................... 381
eTABLE 47. Evidence Table for Q8B. How safe and effective are antiseptic skin preparation agents individually and in combination? .................................................................. 384
eTABLE 48. Evidence Table for Q8C. How safe and effective is the application of a microbial sealant immediately following skin preparation? .................................................. 412
eTABLE 49. Evidence Table for Q8D. How safe and effective are plastic adhesive drapes? ...................................................................................................................................... 424
2017 American Medical Association. All rights reserved. 60
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
eTABLE 50. Evidence Table for Q9. How safe and effective is antiseptic irrigation prior to closing the surgical incision? ...................................................................................... 430
eTABLE 51. Evidence Table for Q10. How safe and effective is repeat application of an antiseptic skin preparation agent to the surgical site immediately prior to closing the
surgical incision? .......................................................................................................................................................................................................................................................... 439
eTABLE 52. Risk of Bias Assessments of Systematic Reviews for Q8-10 Antiseptic Prophylaxis ............................................................................................................................ 443
eTABLE 53. Risk of Bias Assessments of Randomized Controlled Trials for Q8-10 Antiseptic Prophylaxis ............................................................................................................ 443
eTABLE 54. GRADE Table for Q11 Blood Transfusion ............................................................................................................................................................................................. 446
eTABLE 55. Evidence Table for Q11. How do perioperative blood transfusions impact the risk of SSI in prosthetic joint arthroplasty patients? .................................................... 458
eTABLE 56. Risk of Bias Assessments of Randomized Controlled Trials for Q11 Blood Transfusion ...................................................................................................................... 495
eTABLE 57. Risk of Bias Assessments of Other Controlled Studies for Q11 Blood Transfusion ............................................................................................................................... 495
eTABLE 58. GRADE Table for Q12-16 Systemic Immunosuppressive Therapy........................................................................................................................................................ 496
eTABLE 59. Evidence Table for Q12-13 Systemic Immunosuppressive Therapy ...................................................................................................................................................... 505
eTABLE 60.Evidence Table for Q15. How does preoperative intra-articular corticosteroid injection impact the risk of SSI in prosthetic joint arthroplasty patients?..................... 519
eTABLE 61. Risk of Bias Assessments of Other Controlled Studies for Q12-16 Systemic Immunosuppressive Therapy ......................................................................................... 530
eTABLE 62. GRADE Table for Q17 Anticoagulation ................................................................................................................................................................................................. 531
eTABLE 63. Evidence Table for Q17. What are the most effective strategies for managing perioperative venous thromboembolism (VTE) prophylaxis to reduce the risk of SSI?
...................................................................................................................................................................................................................................................................................... 536
eTABLE 64. Risk of Bias Assessment of Systematic Reviews for Q17 Anticoagulation ............................................................................................................................................ 564
eTABLE 65. Risk of Bias Assessments of Randomized Controlled Trials for Q17 Anticoagulation .......................................................................................................................... 564
eTABLE 66. Risk of Bias Assessments of Other Controlled Studies for Q17 Anticoagulation ................................................................................................................................... 564
eTABLE 67. GRADE Table for Q18 Orthopaedic Space Suit ..................................................................................................................................................................................... 566
eTABLE 68. Evidence Table for Q18. How safe and effective are orthopaedic space suits in reducing the risk of SSI in prosthetic joint arthroplasty patients and then which
healthcare personnel should wear them?....................................................................................................................................................................................................................... 568
eTABLE 69. Risk of Bias Assessments of Other Controlled Studies for Q18 Orthopaedic Space Suit ....................................................................................................................... 577
eTABLE 70. GRADE Table for Q20 Biofilm .............................................................................................................................................................................................................. 578
eTABLE 71. Evidence Table for Q20A. How effective are cement modifications (i.e., antimicrobial and nanoparticle loading)? ............................................................................ 580
eTABLE 72. Risk of Bias Assessments of Randomized Controlled Trials for Q20 Biofilm........................................................................................................................................ 585
eTABLE 73. Systematic Review (SR) Extraction Template ........................................................................................................................................................................................ 588
eTABLE 74. Randomized Controlled Trial (RCT) Extraction Template ..................................................................................................................................................................... 588
eTABLE 75. Other Observational Studies (OBS) Extraction Template ....................................................................................................................................................................... 589
1. GUIDELINE SEARCH STRATEGIES
2017 American Medical Association. All rights reserved. 61
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
1.1. Core Section Search Strategies
1.1A. CORE SECTION GENERAL SEARCHES
eTABLE 1. MEDLINE Search: Core Section
# Search History Results
1 exp Surgical Wound Infection/ 25,893
2 "surgical site infection*".af. 2,130
3 1 or 2 26,382
4 limit 3 to English language 19,318
5 limit 4 to yr="1998 -Current" 8,709
6 limit 5 to guideline 19
7 limit 5 to systematic reviews 429
8 limit 5 to practice guideline 27
9 limit 5 to meta analysis 161
10 limit 5 to "reviews (maximizes specificity)" 262
11 6 or 7 or 8 or 9 or 10 469
12 limit 5 to randomized controlled trial 715
13 11 or 12 1,170
eTABLE 2. EMBASE Search: Core Section
# Search History Results
1 'surgical infection'/exp or 'surgical site infection' or 'surgical wound infection' 19,658
2 limit 1 to English language 13,666
3 limit 2 to 'randomized controlled trial'/de 749
4 limit 3 [1998-2012]/py 566
5 limit 2 to [review] 1,580
6 limit 2 to ('meta analysis'/de OR 'practice guideline'/de) 639
7 'systematic review'/exp 43,081
8 5 and 7 82
2017 American Medical Association. All rights reserved. 62
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
9 6 or 8 679
10 limit 9 to [1998-2012]/py 654
11 4 or 10 1,220
2017 American Medical Association. All rights reserved. 63
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
1.2. Prosthetic Joint Arthroplasty Section Search Strategies
1.2A. PROSTHETIC JOINT ARTHROPLASTY SECTION GENERAL SEARCHES
eTABLE 3. MEDLINE Search: Ortho Section
# Search History Results
1 (arthroplast* or replac* or replant* or joint* or implant* or reconstruct* or prosthe*).af. 1,052,637
2 exp Arthroplasty, Replacement/ or exp Arthroplasty/ 29,697
3 exp Orthopedic Procedures/ 176,717
4 exp Joints/su [Surgery] 42,769
5 1 or 2 or 3 or 4 1,135,596
6 exp Wound Infection/ 34,108
7 "surgical site infection*".af. 2,130
8 exp Prosthesis-Related Infections/ 6,283
9 exp Bone Diseases, Infectious/ 29,730
10 exp Soft Tissue Infections/ 1,876
11 exp Skin Diseases, Infectious/ 90,359
12 6 or 7 or 8 or 9 or 10 or 11 158,415
13 5 and 12 24,509
14 exp Surgical Procedures, Operative/ 2,113,349
15 (surgical* or surgery* or operati*).af. 2,629,634
16 14 or 15 3,467,669
17 (arthro* or orthop*).af. 316,829
18 16 and 17 206,698
19 12 and 18 9,513
20 13 or 19 26,888
21 limit 20 to (english language and yr="1998 - Current") 11,604
22 limit 21 to systematic reviews 262
23 limit 21 to meta analysis 50
2017 American Medical Association. All rights reserved. 64
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
24 limit 21 to guideline 14
25 limit 21 to practice guideline 22
26 limit 21 to "reviews (maximizes specificity)" 137
27 limit 21 to randomized controlled trial 294
28 22 or 23 or 24 or 25 or 26 or 27 595
eTABLE 4. EMBASE Search: Ortho Section
# Search History Results
'wound infection'/exp or 'surgical infection'/exp or 'prosthesis infection'/exp or 'bone infection'/exp or 'soft tissue infection'/exp or
1 'skin infection'/exp or 'surgical site infection'; limit to English language, EMBASE, and [1998-2012]/py 69,175
'arthroplasty'/exp or 'arthroplasty replacement'/exp or 'orthopedic surgery'/exp or ('joint'/exp and surg*) or arthroplast* or replac* or
replant* or (joint* and' surgery'/exp) or implant* or reconstruct* or prosthe* or (('surgery'/exp or surgical* or operativ* and (arthro* or
2 orthop*)) and [1998-2012]/py 856,609
3 1 and 2 14,117
4 meta-analysis/exp 57,212
5 3 and 4 121
6 limit 3 to systematic review/de 234
7 limit 3 to practice guideline /de 383
8 limit 3 to randomized controlled trial/de 430
9 5 or 6 or 7 or 8 1,059
2017 American Medical Association. All rights reserved. 65
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
1.2B. PROSTHETIC JOINT ARTHROPLASTY SECTION TARGETED SEARCHES: TRANSFUSION
eTABLE 5. MEDLINE Targeted Search: Transfusion
# Search History Results
1 (exp "prostheses and implants"/ or prosthe*.af. or implant*.af. or orthoped*.af. or orthopaed*.af.) and (exp joints/ or joint*.af.) 101,924
2 exp Joints/su [Surgery] 44,456
3 exp Arthroplasty, Replacement/ or exp Arthroplasty/ 32,010
4 arthroplast*.af. 42,928
5 exp "Orthopedic Procedures"/ and exp "Joints"/ 39,956
6 or/1-5 141,563
7 exp Infection/ or infection*.af. or infecting.af. or infected.af. or exp "Prosthesis-Related Infections"/ 1,533,905
8 exp Blood Transfusion/ or (blood and transfus*).af. 114,443
9 exp Blood Platelets/ or platelet*.af. or "blood product*".af. 195,879
10 8 or 9 292,467
11 exp Random Allocation/ 73,596
12 exp Randomized Controlled Trials as Topic/ or exp Randomized Controlled Trial/ 394,924
13 exp Double-Blind Method/ 113,512
14 exp Single-Blind Method/ 15,853
15 exp Clinical Trial/ 667,767
16 exp Clinical Trials as Topic/ 251,205
17 clinical trial.pt. 467,170
18 clinical trial, phase i.pt. 11,868
(clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or
19 multicenter study or clinical trial).pt. 665,448
20 or/11-19 895,443
21 (clinical adj trial$).tw. 164,609
22 ((singl$ or doubl$ or treb$ or tripl$) adj (blind$3 or mask$3)).tw. 111,059
23 placebo$.tw. 133,778
24 randomly allocated.tw. 13,342
2017 American Medical Association. All rights reserved. 66
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
25 (allocated adj2 random$).tw. 15,627
26 exp Placebos/ 30,626
27 or/20-26 996,307
28 case report.tw. 164,158
29 letter/ 735,581
30 historical article/ 280,723
31 exp Editorial/ 291,753
32 or/28-31 1,454,788
33 27 not 32 956,341
34 exp "Sensitivity and Specificity"/ 350,527
35 (sensitivity or specificity).tw. 590,136
36 ((pre-test or pretest) adj probability).tw. 980
37 post-test probability.tw. 268
38 predictive value$.tw. 54,259
39 likelihood ratio$.tw. 6,512
40 exp "Predictive Value of Tests"/ 117,980
41 or/33-40 1,740,790
42 exp Meta-Analysis as Topic/ 11,873
43 (meta analy$ or metaanaly$).tw. or exp Meta-analysis/ 48,899
44 (systematic adj (review$1 or overview$1)).tw. 29,904
45 exp Review Literature as Topic/ 6,079
46 or/41-45 1,784,999
47 (embase or cochrane or psyclit* or psychlit* or psycinfo or psychinfo).tw. 27,796
48 (cinahl or cinhal).ab. 5,997
49 (science citation index or bids or cancerlit).ab. 2,135
50 or/46-49 1,792,516
2017 American Medical Association. All rights reserved. 67
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
51 (reference list$ or bibliograph$ or hand-search$ or relevant journals or manual search$).ab. 18,484
52 (selection criteria or data extraction).ab. 20,349
53 exp Review/ 1,675,847
54 52 and 53 14,038
55 50 or 51 or 54 1,800,552
56 exp Comment/ or exp Editorial/ or exp Letter/ 1,108,385
57 55 not 56 1,770,101
exp Epidemiologic studies/ or exp case control studies/ or exp cohort studies/ or Case control.tw. or (cohort adj (study or
studies)).tw. or cohort analy$.tw. or (Follow up adj (study or studies)).tw. or (observational adj (study or studies)).tw. or
58 Longitudinal.tw. or Retrospective.tw. or Cross sectional.tw. or exp Cross-sectional studies/ 1,553,551
59 57 or 58 2,972,690
60 6 and 7 and 10 and 59 150
61 limit 60 to english language 136
62 limit 61 to yr="1998 -Current" 103
eTABLE 6. EMBASE Targeted Search: Transfusion
# Search History Results
blood transfusion/exp or (blood/exp and (transfusion/exp or transfused)) or thrombocyte/exp or blood/exp or platelet* or blood
1 product/exp or blood products and [english]/lim and [embse]/lim and [1998-2012]/py 627,207
2 prostheses and orthoses/exp or prosthe$ or implant$ or orthoped$ or orthopaed$ 399,873
joint/exp or joint$ or joint surgery/exp or arthroplasty/exp or arthroplasty or arthroplasties or arthroplasty replacement or
3 (orthopedic surgery/exp and joint/exp) 603,883
4 2 and 3 69,054
5 infection/exp 2,328,600
6 infection$ or infecting or infected 2,654,665
7 prosthesis related and infections 95
8 prosthesis-related infections/exp 2,328,600
9 5 or 6 or 7 or 8 2,660,483
2017 American Medical Association. All rights reserved. 68
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
10 1 and 4 and 9 353
11 clinical study/exp or case control study/exp or family study/exp or longitudinal study/exp or retrospective study/exp 5,942,135
12 prospective study/exp 189,505
13 randomized controlled trial/exp 307,692
14 12 not 13 165,671
cohort analysis/exp or (cohort and adj and (study or studies)) or (case and control and adj and (study or studies)) or (follow and
up and adj and (study or studies)) or (observational and adj and (study or studies)) or (epidemiologic$ and adj and (study or
15 studies)) or (cross and sectional and adj and (study or studies)) 115,089
16 11 or 12 or 14 or 15 5,986,679
17 meta analysis/exp or (meta and adj and analy$) or metaanaly$ or (systematic and adj and (review$ or overview$)) 61,427
18 cancerlit or cochrane or embase/exp or psychlit/exp or psyclit/ or science citation index/exp or bids or scopus 44,494
reference lists or bibliograph$ or hand search$ or manual search$ or relevant journals or data extraction/exp or selection
19 criteria 28,035
20 review.pt. 4
21 review/exp 1,831,423
22 20 or 21 1,831,427
23 19 and 22 15,584
24 letter.pt. or editorial.pt. 3
25 letter/exp or editorial/exp 1,179,933
26 24 or 25 1,179,934
27 17 or 18 or 23 98,049
28 27 not 26 93,355
sensitivity and specificity/exp or sensitivity or specificity or (pre test or pretest and adj and probability/exp) or post-test
probability or predictive and value$ or likelihood and ratio$ or predictive value/exp or diagnostic accuracy /exp and [english]/lim
29 and [embase]/lim and [1998-2012]/py 144,775
clinical trial/exp or randomized controlled trial/exp or randomization/exp or single blind procedure/exp or double blind
procedure/exp or crossover procedure/exp or placebo/exp or randomi?ed and controlled and trial$ or rct$ or random allocation
or randomly allocated or allocated randomly or allocated and adj2 and random$ or single and blind$ or double and blind$ or
30 (treble or triple and adj and blind$) or placebo$ or prospective study/exp 541,923
2017 American Medical Association. All rights reserved. 69
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
case study/exp or case study or case report/exp or case report or abstract report/exp or abstract report or letter/exp or letter
31 and [1998-2012]/py 1,237,206
32 30 not 31 529,538
33 16 or 28 or 29 or 32 6,160,948
34 10 and 33 232
eTABLE 7. Cochrane Database of Systematic Reviews Targeted Search: Transfusion
# Search History Results
(transfus* or platelet* or "blood product*") and (surgery or surgical* or operat*) and (joint* or arthroplast* or prosthe* or implant*) in
1 Title, Abstract or Keywords 6
2017 American Medical Association. All rights reserved. 70
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
1.2C. PROSTHETIC JOINT ARTHROPLASTY SECTION TARGETED SEARCHES: IMMUNOSUPPRESSIVE THERAPY
eTABLE 8. MEDLINE Targeted Search: Immunosuppressive Therapy
# Search History Results
1 (exp "prostheses and implants"/ or prosthe*.af. or implant*.af. or orthoped*.af. or orthopaed*.af.) and (exp joints/ or joint*.af.) 102,099
2 exp Joints/su [Surgery] 44,522
3 exp Arthroplasty, Replacement/ or exp Arthroplasty/ 32,116
4 arthroplasty*.af. 43,040
5 exp Orthopedic Procedures/and exp Joints/ 40,017
6 or/1-5 141,821
7 exp Infection/ or infection*.af. or infecting.af. or infected.af. or exp "Prosthesis-Related Infections"/ 1,540,242
8 exp Random Allocation/ 73,745
9 exp Randomized Controlled Trials as Topic/ or exp Randomized Controlled Trial/ 397,784
10 exp Double-Blind Method/ 113,903
11 exp Single-Blind Method/ 15,934
12 exp Clinical Trial/ 670,938
13 exp Clinical Trials as Topic/ 253,167
14 clinical trial.pt. 467,996
15 clinical trial, phase i.pt. 11,949
16 (clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or
668,584
multicenter study or clinical trial).pt.
17 or/8-16 900,674
18 (clinical adj trial$).tw. 165,764
19 ((singl$ or doubl$ or treb$ or tripl$) adj (blind$3 or mask$3)).tw. 111,446
20 placebo$.tw. 134,478
21 randomly allocated.tw. 13,417
22 (allocated adj2 random$).tw. 15,704
23 exp Placebos/ 30,699
24 or/17-23 1,002,057
2017 American Medical Association. All rights reserved. 71
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
25 case report.tw. 164,536
26 letter/ 742,239
27 historical article/ 281,301
28 exp Editorial/ 295,205
29 or/25-28 1,465,799
30 24 not 29 961,541
31 exp Sensitivity and Specificity/ 351,908
32 (sensitivity or specificity).tw. 592,438
33 ((pre-test or pretest) adj probability).tw. 988
34 post-test probability.tw. 272
35 predictive value$.tw. 54,458
36 likelihood ratio$.tw. 6,573
37 exp "Predictive Value of Tests"/ 118,435
38 or/30-37 1,748,938
39 exp Meta-Analysis as Topic/ 12,009
40 (meta analy$ or metaanaly$).tw. or exp Meta-analysis/ 49,740
41 (systematic adj (review$1 or overview$1)).tw. 30,487
42 exp Review Literature as Topic/ 6,208
43 or/38-42 1,793,694
44 (embase or cochrane or psyclit* or psychlit* or psycinfo or psychinfo).tw. 28,506
45 (cinahl or cinhal).ab. 6,190
46 (science citation index or bids or cancerlit).ab. 2,196
47 or/43-46 1,801,291
48 (reference list$ or bibliograph$ or hand-search$ or relevant journals or manual search$).ab. 18,852
49 (selection criteria or data extraction).ab. 20,813
50 exp Review/ 1,682,836
2017 American Medical Association. All rights reserved. 72
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
51 49 and 50 14,472
52 47 or 48 or 51 1,809,350
53 exp Comment/ or exp Editorial/ or exp Letter/ 1,119,204
54 52 not 53 1,778,639
55 exp Epidemiologic studies/ or exp case control studies/ or exp cohort studies/ or Case control.tw. or (cohort adj (study or
studies)).tw. or cohort analy$.tw. or (Follow up adj (study or studies)).tw. or (observational adj (study or studies)).tw. or 1,560,697
Longitudinal.tw. or Retrospective.tw. or Cross sectional.tw. or exp Cross-sectional studies/
56 54 or 55 2,986,243
57 exp Immunosuppressive Agents/ 229,191
58 exp Immunosuppression/ 46,654
59 "immunosuppressive therapy".af. 10,624
60 immune*.af. 408,428
61 immunolog*.af. 56
62 exp Adrenal Cortex Hormones/ 315,501
63 exp Steroids/ 657,932
64 exp methotrexate/ or exp cyclophosphamide/ 67,761
65 exp Tumor Necrosis Factor-alpha/ 83,932
66 "systemic corticosteroids".af. 2,228
67 steroid*.af. 244,914
68 tumor necrosis factor*.af. 116,734
69 (cyclophosphamide or cytoxan or methotrexate).af. 83,530
70 tnf.af. 90,322
71 exp Injections, Intra-articular/ or intra-articular*.af. 11,059
72 or/57-71 1,544,611
73 6 and 7 and 56 and 72 360
74 limit 73 to english language 312
75 limit 74 to yr="1998 -Current" 250
2017 American Medical Association. All rights reserved. 73
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
eTABLE 9. EMBASE Targeted Search: Immunosuppressive Therapy
# Search History Results
1 prostheses and orthoses/exp or prosthe$ or implant$ or orthoped$ or orthopaed$ 399,873
2 joint/exp or joint$ or joint surgery/exp or arthroplasty/exp or arthroplasty or arthroplasties or arthroplasty replacement or
603,893
(orthopedic surgery/exp and joint/exp)
3 1 and 2 69,054
4 infection/exp 2,328,600
5 infection$ or infecting or infected 2,654,665
6 prosthesis related and infections 95
7 prosthesis-related infections/exp 2,328,600
8 4 or 5 or 6 or 7 2,660,483
9 clinical study/exp or case control study/exp or family study/exp or longitudinal study/exp or retrospective study/exp 5,942,135
10 prospective study/exp 188,505
11 randomized controlled trial/exp 307,692
12 10 not 11 165,671
13 cohort analysis/exp or (cohort and adj and (study or studies)) or (case and control and adj and (study or studies)) or (follow and
up and adj and (study or studies)) or (observational and adj and (study or studies)) or (epidemiologic$ and adj and (study or 115,089
studies)) or (cross and sectional and adj and (study or studies))
14 9 or 10 or 12 or 13 5,986,679
15 meta analysis/exp or (meta and adj and analy$) or metaanaly$ or (systematic and adj and (review$ or overview$)) 61,427
16 cancerlit or cochrane or embase/exp or psychlit/exp or psyclit/ or science citation index/exp or bids or scopus 44,495
17 reference lists or bibliograph$ or hand search$ or manual search$ or relevant journals or data extraction/exp or selection
28,035
criteria
18 review.pt. 4
19 review/exp 1,831,423
20 18 or 19 1,831,427
21 17 and 20 15,584
22 letter.pt. or editorial.pt. 3
2017 American Medical Association. All rights reserved. 74
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
23 letter/exp or editorial/exp 1,179,933
24 22 or 23 1,179,934
25 15 or 16 or 21 98,049
26 25 not 24 93,355
27 sensitivity and specificity/exp or sensitivity or specificity or (pre test or pretest and adj and probability/exp) or post-test
probability or predictive and value$ or likelihood and ratio$ or predictive value/exp or diagnostic accuracy /exp and [english]/lim 144,775
and [embase]/lim and [1998-2012]/py
28 clinical trial/exp or randomized controlled trial/exp or randomization/exp or single blind procedure/exp or double blind
procedure/exp or crossover procedure/exp or placebo/exp or randomi?ed and controlled and trial$ or rct$ or random allocation
539,487
or randomly allocated or allocated randomly or allocated and adj2 and random$ or single and blind$ or double and blind$ or
(treble or triple and adj and blind$) or placebo$ or prospective study/exp
29 case study/exp or case study or case report/exp or case report or abstract report/exp or abstract report or letter/exp or letter
1,237,206
and [1998-2012]/py
30 28 not 29 529,538
31 14 or 26 or 27 or 30 6,160,948
32 immunosuppressive agent/exp or immunosuppressive treatment/exp or immunosuppressive therapy or immunosuppressive
agents or immunolog* or methotrexate or cyclophosphamide or adrenal cortex hormones or systemic corticosteroids or tumor
1,749,571
necrosis factor or cytoxan or tnf or intra articular or tumor necrosis factor/exp or intraarticular drug administration/exp or
steroid/exp or corticosteroid/exp or methotrexate/exp or cyclophosphamide/exp and [1998-2012]/py
33 3 and 8 and 32 697
34 31 and 33 398
eTABLE 10. Cochrane Database of Systematic Reviews Targeted Search: Immunosuppressive Therapy
# Search History Results
1 "(immuno* or immunolog* or steroid* or corticosteroid* or "adrenal cortex hormone*" or methotrexate or cyclophosphamide or
cytoxan or tnf or "tumor necrosis factor*" or (intra-articular" and inject*)) and (surgery or surgical* or operat*) and (joint* or 21
arthroplast* or prosthe* or implant*) in Title, Abstract or Keywords
2017 American Medical Association. All rights reserved. 75
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
1.2D. PROSTHETIC JOINT ARTHROPLASTY SECTION TARGETED SEARCHES: ANTICOAGULATION
eTABLE 11. MEDLINE Targeted Search: Anticoagulation
# Search History Results
1 (exp "prostheses and implants"/ or prosthe*.af. or implant*.af. or orthoped*.af. or orthopaed*.af.) and (exp joints/ or joint*.af.) 101,924
2 exp Joints/su [Surgery] 44,456
3 exp Arthroplasty, Replacement/ or exp Arthroplasty/ 32,010
4 arthroplasty*.af. 42,928
5 exp Orthopedic Procedures/and exp Joints/ 39,956
6 or/1-5 141,563
7 exp Infection/ or infection*.af. or infecting.af. or infected.af. or exp "Prosthesis-Related Infections"/ 1,533,905
8 exp Random Allocation/ 73,596
9 exp Randomized Controlled Trials as Topic/ or exp Randomized Controlled Trial/ 394,924
10 exp Double-Blind Method/ 113,512
11 exp Single-Blind Method/ 15,853
12 exp Clinical Trial/ 667,767
13 exp Clinical Trials as Topic/ 251,205
14 clinical trial.pt. 467,170
15 clinical trial, phase i.pt. 11,868
(clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or
16 multicenter study or clinical trial).pt. 665,448
17 or/8-16 895,443
18 (clinical adj trial$).tw. 164,609
19 ((singl$ or doubl$ or treb$ or tripl$) adj (blind$3 or mask$3)).tw. 111,059
20 placebo$.tw. 133,778
21 randomly allocated.tw. 13,342
22 (allocated adj2 random$).tw. 15,627
23 exp Placebos/ 30,626
24 or/17-23 996,307
2017 American Medical Association. All rights reserved. 76
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
25 case report.tw. 164,158
26 letter/ 735,581
27 historical article/ 280,723
28 exp Editorial/ 291,753
29 or/25-28 1,454,788
30 24 not 29 956,341
31 exp Sensitivity and Specificity/ 350,527
32 (sensitivity or specificity).tw. 590,136
33 ((pre-test or pretest) adj probability).tw. 980
34 post-test probability.tw. 268
35 predictive value$.tw. 54,259
36 likelihood ratio$.tw. 6,512
37 exp "Predictive Value of Tests"/ 117,980
38 or/30-37 1,740,790
39 exp Meta-Analysis as Topic/ 11,873
40 (meta analy$ or metaanaly$).tw. or exp Meta-analysis/ 48,899
41 (systematic adj (review$1 or overview$1)).tw. 29,904
42 exp Review Literature as Topic/ 6,079
43 or/38-42 1,784,999
44 (embase or cochrane or psyclit* or psychlit* or psycinfo or psychinfo).tw. 27,796
45 (cinahl or cinhal).ab. 5,997
46 (science citation index or bids or cancerlit).ab. 2,135
47 or/43-46 1,792,516
48 (reference list$ or bibliograph$ or hand-search$ or relevant journals or manual search$).ab. 18,484
49 (selection criteria or data extraction).ab. 20,349
50 exp Review/ 1,675,847
2017 American Medical Association. All rights reserved. 77
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
51 49 and 50 14,038
52 47 or 48 or 51 1,800,552
53 exp Comment/ or exp Editorial/ or exp Letter/ 1,108,385
54 52 not 53 1,770,101
exp Epidemiologic studies/ or exp case control studies/ or exp cohort studies/ or Case control.tw. or (cohort adj (study or
studies)).tw. or cohort analy$.tw. or (Follow up adj (study or studies)).tw. or (observational adj (study or studies)).tw. or
55 Longitudinal.tw. or Retrospective.tw. or Cross sectional.tw. or exp Cross-sectional studies/ 1,553,551
56 54 or 55 2,972,690
57 exp Heparin/ 53,476
58 exp warfarin/ 12,695
59 exp aspirin/ 35,444
60 exp Anticoagulants/ or anticoagul*.af. 191,442
61 "low-dose unfractionated".af. 111
62 (clopidogrel or plavix).af. 6,385
63 (warfarin* or aspirin* or heparin*).af. 136,516
64 exp Platelet Aggregation Inhibitors/ 84,124
65 anti-platelet*.af. 2,453
66 or/57-65 299,002
67 6 and 7 and 56 and 66 52
68 limit 67 to english language 45
69 limit 68 to yr-1998-Current 28
eTABLE 12. EMBASE Targeted Search: Anticoagulation
# Search History Results
1 infection/exp 2,328,600
2 Infection$ or infecting or infected 2,654,665
3 prosthesis related and infections 95
2017 American Medical Association. All rights reserved. 78
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
4 prosthesis-related infections/exp 2,328,600
5 1 or 2 or 3 or 4 2,660,483
6 prostheses and orthoses/exp or prosthe$ or implant$ or orthoped$ or orthopaed$ 399,873
joint/exp or joint$ or joint surgery/exp or arthroplasty/exp or arthroplasty or arthroplasties or arthroplasty replacement or
7 (orthopedic surgery/exp and joint/exp) 603,883
8 6 and 7 69,054
heparin/exp or warfarin/exp or acetylsalicylic acid/exp or anticoagulant agent/exp or antithrombotic agent/exp or anticoagul*
9 or low-dose unfractionated or clopidogrel or plavix or warfarin* or heparin* or aspirin or anti platelet 481,497
10 5 and 8 and 9 374
11 meta analysis/exp or (meta and adj and analy$) or metaanaly$ or (systematic and adj and (review$ or overview$)) 61,427
12 cancerlit or cochrane or embase/exp or psychlit/exp or psyclit/ or science citation index/exp or bids or scopus 44,495
reference lists or bibliograph$ or hand search$ or manual search$ or relevant journals or data extraction/exp or selection
13 criteria 28,035
14 review.pt. 4
15 review/exp 1,831,423
16 14 or 15 1,831,427
17 13 and 16 15,584
18 letter.pt. or editorial.pt. 3
19 letter/exp or editorial/exp 1,179,933
20 18 or 19 1,174,934
21 11 or 12 or 17 98,049
22 21 not 20 93,355
clinical trial/exp or randomized controlled trial/exp or randomization/exp or single blind procedure/exp or double blind
procedure/exp or crossover procedure/exp or placebo/exp or randomi?ed and controlled and trial$ or rct$ or random allocation
or randomly allocated or allocated randomly or allocated and adj2 and random$ or single and blind$ or double and blind$ or
23 (treble or triple and adj and blind$) or placebo$ or prospective study/exp 541,923
case study/exp or case study or case report/exp or case report or abstract report/exp or abstract report or letter/exp or letter
24 and [1998-2012]/py 1,237,206
25 23 not 24 529,538
2017 American Medical Association. All rights reserved. 79
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
26 clinical study/exp or case control study/exp or family study/exp or longitudinal study/exp or retrospective study/exp 5,942,135
27 prospective study/exp 189,505
28 randomized controlled trial/exp 307,692
29 27 not 28 165,671
cohort analysis/exp or (cohort and adj and (study or studies)) or (case and control and adj and (study or studies)) or (follow and
up and adj and (study or studies)) or (observational and adj and (study or studies)) or (epidemiologic$ and adj and (study or
30 studies)) or (cross and sectional and adj and (study or studies)) 115,089
31 26 or 27 or 29 or 30 5,986,679
sensitivity and specificity/exp or sensitivity or specificity or (pre test or pretest and adj and probability/exp) or post-test
probability or predictive and value$ or likelihood and ratio$ or predictive value/exp or diagnostic accuracy /exp and english]/lim
32 and [embase]/lim and [1998-2012]/py 144,775
33 22 or 25 or 31 or 32 6,160,948
34 10 and 33 and [english]/lim and [embase]/lim and [1998-2012]/py 221
eTABLE 13. Cochrane Database of Systematic Reviews Targeted Search: Anticoagulation
# Search History Results
("low molecular weight" or "low-molecular-weight" or anticoag* or heparin or warfarin or aspirin or clopidogrel or plavix or "Platelet
Aggregation Inhibit*" or anti platelet* ) and ( surgery or surgical* or operat* ) and (joint* or arthroplast* or prosthe* or implant* ) in
1 Title, Abstract or Keywords 8
2017 American Medical Association. All rights reserved. 80
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
1.2E. PROSTHETIC JOINT ARTHROPLASTY SECTION TARGETED SEARCHES: ORTHOPAEDIC SPACE SUIT
eTABLE 14. MEDLINE Targeted Search: Orthopaedic Space Suit
# Search History Results
1 (exp prostheses and implants/ or prosthe*.af. or implant*.af. or orthoped*.af. or orthpaed*.af.) and (exp joints/ or joint*.af.) 102,254
2 exp Joints/su [Surgery] 44,595
3 exp Arthroplasty, Replacement/ or exp Arthroplasty/ 32,203
4 arthroplasty*.af. 43,132
5 exp Orthopedic Procedures/ and exp Joints/ 40,095
6 or/ 1-5 142,045
7 exp Infection/ or infection*.af. or infecting.af. or infected.af. or exp Prosthesis-Related Infections/ 1,541,705
8 exp Random Allocation/ 73,817
9 exp Randomized Controlled Trials as Topic/ or exp Randomized Controlled Trial/ 398,286
10 exp Double-Blind Method/ 114,004
11 exp Single-Blind Method/ 15,965
12 exp Clinical Trial/ 671,638
13 exp Clinical Trials as Topic/ 253,375
14 clinical trial.pt. 468,127
15 clinical trial, phase i.pt. 11,960
(clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or
16 multicenter study or clinical trial).pt. 669,278
17 or /8-16 901,656
18 (clinical adj trial$).tw. 166,027
19 ((singl$ or doubl$ or treb$ or tripl$) adj (blind$3 or mask$3)).tw. 111,543
20 placebo$.tw. 134,617
21 randomly allocated.tw. 13,439
22 (allocated adj2 random$).tw. 15,726
23 exp Placebos/ 30,724
24 or/17-23 1,003,206
2017 American Medical Association. All rights reserved. 81
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
25 case report.tw. 164,737
26 letter/ 742,890
27 historical article/ 281,494
28 exp Editorial/ 295,617
29 or/25-28 1,467,233
30 24 not 29 962,656
31 exp Sensitivity and Specifity/ 352,539
32 (sensitivity or specifity).tw. 593,131
33 ((pre-test or pretest) adj probability).tw. 988
34 post-test probability.tw. 273
35 predictive value$.tw. 54,533
36 likelihood ratio$.tw. 6,584
37 exp Predictive Value of Tests/ 118,653
38 or/30-27 1,751,101
39 exp Meta-Analysis as Topic/ 12,014
40 (meta analy$ or metaanaly$).tw. or exp Meta-analysis/ 49,880
41 (systematic adj (review$1 or overview$1)).tw. 30,599
42 exp Review Literature as Topic/ 6,214
43 or/38-42 1,795,992
44 (embase or Cochrane or psyclit* or psychlit* or psycinfo or psychinfo).tw. 28,587
45 (cinahl or cinhal).ab. 6,206
46 (science citation index or bids or cancerlit).ab. 2,197
47 or/43-46 1,803,599
48 (reference list$ or bibliograph$ or hand-search$ or relevant journals or manual search$).ab. 18,879
49 (selection criteria or data extraction).ab. 20,833
50 exp Review/ 1,684,812
2017 American Medical Association. All rights reserved. 82
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
51 49 and 50 14,483
52 47 or 48 or 51 1,811,665
53 exp Comment/ or exp Editorial/ or exp Letter/ 1,120,430
54 52 not 53 1,780,921
exp Epidemiologic studies/ or exp case control studies/ or exp cohort studies/ or Case control.tw. or (cohort adj (study or
studies)).tw. or cohort analy$.tw. or (Follow up adj (study or studies)).tw. or (observational adj (study or studies)).tw. or
55 Longitudinal.tw. or Retrospective.tw. or Cross sectional.tw. or exp Cross-sectional studies/ 1,563,211
56 54 or 55 2,990,436
57 exp Protective Clothing/ or exp Space Suits/ 9,233
58 (exhaust* or exhaust suit*).af. 27,803
59 (body exhaust suit* or body-exhaust suit* or space suit*).af. 254
60 57 or 58 or 59 36,996
61 6 and 7 and 56 and 60 37
62 limit 61 to english language 35
63 limit 62 to yr=1998-Current 21
eTABLE 15. EMBASE Targeted Search: Orthopaedic Space Suit
# Search History Results
1 meta analysis/exp or (meta and adj and analy$) or metaanaly$ or (systematic and adj and (review$ or overview$)) 61,427
2 cancerlit or cochrane or embase/exp or psychlit/exp or psyclit/ or science citation index/exp or bids or scopus 44,494
reference lists or bibliograph$ or hand search$ or manual search$ or relevant journals or data extraction/exp or selection
3 criteria 28,035
4 review.pt. 4
5 review/exp 1,831,422
6 4 or 5 1,831,427
7 3 and 6 15,584
8 letter.pt. or editorial.pt. 3
9 letter/exp or editorial/exp 1,179,933
2017 American Medical Association. All rights reserved. 83
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
10 8 or 9 1,179,934
11 1 or 2 or 7 98,049
12 11 not 10 93,355
clinical trial/exp or randomized controlled trial/exp or randomization/exp or single blind procedure/exp or double blind
procedure/exp or crossover procedure/exp or placebo/exp or randomi?ed and controlled and trial$ or rct$ or random allocation
or randomly allocated or allocated randomly or allocated and adj2 and random$ or single and blind$ or double and blind$ or
13 (treble or triple and adj and blind$) or placebo$ or prospective study/exp 541,923
case study/exp or case study or case report/exp or case report or abstract report/exp or abstract report or letter/exp or letter
14 and [1998-2012]/py 1,237,206
15 13 not 14 529,538
16 clinical study/exp or case control study/exp or family study/exp or longitudinal study/exp or retrospective study/exp 5,942,135
17 prospective study/exp 189,505
18 randomized controlled trial/exp 307,692
19 17 not 18 165,671
cohort analysis/exp or (cohort and adj and (study or studies)) or (case and control and adj and (study or studies)) or (follow and
up and adj and (study or studies)) or (observational and adj and (study or studies)) or (epidemiologic$ and adj and (study or
20 studies)) or (cross and sectional and adj and (study or studies)) 115,089
21 16 or 19 or 20 5,986,679
sensitivity and specificity/exp or sensitivity or specificity or (pre test or pretest and adj and probability/exp) or post-test
probability or predictive and value$ or likelihood and ratio$ or predictive value/exp or diagnostic accuracy /exp and english]/lim
22 and [embase]/lim and [1998-2012]/py 144,775
23 12 or 15 or 21 or 22 6,160,948
24 infection/exp 2,328,600
25 Infection$ or infecting or infected 2,654,665
26 prosthesis related and infections 95
27 prosthesis-related infections/exp 2,328,600
28 24 or 25 or 26 or 27 2,660,483
29 prostheses and orthoses/exp or prosthe$ or implant$ or orthoped$ or orthopaed$ 399,873
joint/exp or joint$ or joint surgery/exp or arthroplasty/exp or arthroplasty or arthroplasties or arthroplasty replacement or
30 (orthopedic surgery/exp and joint/exp) 603,883
2017 American Medical Association. All rights reserved. 84
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
31 29 and 30 69,054
surgical attire/exp or surgical attire or protective clothing/exp or space suit or exhaust suit or body exhaust suit or body-
32 exhaust suit 12,127
33 23 and 28 and 31 and 32 and [english]/lim and [embase]/lim and [1998-2012]/py 7
eTABLE 16. Cochrane Database of Systematic Reviews Targeted Search: Orthopaedic Space Suit
# Search History Results
(suit* or clothing) and (surgery or surgical* or operat*) and (joint* or arthroplast* or prosthe* or implant*) in Title, Abstract or
1 Keywords 8
eTABLE 17. CINAHL Targeted Search: Orthopaedic Space Suit
# Search History Results
1 (MH Protective Clothing+) 3,434
2 exhaust suit* 4
3 space suit* 3
4 1 or 2 or 3 3,438
5 (MH Arthoplasty+) or (MH Arthroplasty, Replacement+) 10,000
6 (MH Prostheses and Implants+) 34,039
7 (MH Joints/SU) 111
8 (MH Surgery, Operative+) 197,035
9 (MH Surgery, Operative+) and orthopedic* or orthopaedic* or joint* 20,595
10 ((prosthe* or implant* or orthopaed* or orthoped*)) and MW joints 196
11 arthroplasty or arthroplasties 10,691
12 5 or 6 or 7 or 10 or 11 62,799
13 11 and 12 22
14 13 and 4 21
15 (MH Infection+) 62,911
2017 American Medical Association. All rights reserved. 85
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
16 (MH Prosthesis-Related Infections) 610
17 infection* or infected or infecting 129,848
18 15 or 16 or 17 129,848
19 14 and 18 14
20 (MH Operating Rooms) 4,940
21 operating room* 8,369
22 20 or 21 8,369
23 19 and 22 7
2017 American Medical Association. All rights reserved. 86
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
1.2F. PROSTHETIC JOINT ARTHROPLASTY SECTION TARGETED SEARCH: ANTIMICROBIAL PROPHYLAXIS WITH A DRAIN
eTABLE 18. MEDLINE Targeted Search: Antimicrobial Prophylaxis with a Drain
# Search History Results
1 exp Anti-Infective Agents/ 1,155,786
2 exp Antibiotic Prophylaxis/ 7,457
3 (antimicrobial or ("anti-infective" and agents) or anti-infective agents).af. 139,832
4 1 or 2 or 3 1,181,549
5 exp Time/ or exp Time Factors/ or timing.af. or time.af. or timed.af. or duration.af. 2,675,015
6 exp Drainage/ 41,403
7 drain*.af. 93,852
8 6 or 7 102,200
9 4 and 5 and 8 1,930
10 (exp "prostheses and implants"/ or prosthe*.af. or implant*.af. or orthoped*.af. or orthopaed*.af.) and (exp joints/ or joint*.af.) 102,254
11 exp Joints/su [Surgery] 44,595
12 exp Arthroplasty, Replacement/ or exp Arthroplasty/ 32,203
13 arthroplasty*.af. 43,132
14 exp Orthopedic Procedures/and exp Joints/ 40,095
15 or/10-14 142,045
16 exp Infection/ or infection*.af. or infecting.af. or infected.af. or exp "Prosthesis-Related Infections"/ 1,541,705
17 exp Random Allocation/ 73,817
18 exp Randomized Controlled Trials as Topic/ or exp Randomized Controlled Trial/ 398,286
19 exp Double-Blind Method/ 114,001
20 exp Single-Blind Method/ 15,965
21 exp Clinical Trial/ 671,638
22 exp Clinical Trials as Topic/ 253,375
23 clinical trial.pt. 468,127
24 clinical trial, phase i.pt. 11,960
25 (clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or 669,278
2017 American Medical Association. All rights reserved. 87
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
multicenter study or clinical trial).pt.
26 or/17-25 901,656
27 (clinical adj trial$).tw. 166,027
28 ((singl$ or doubl$ or treb$ or tripl$) adj (blind$3 or mask$3)).tw. 111,543
29 placebo$.tw. 134,617
30 randomly allocated.tw. 13,439
31 (allocated adj2 random$).tw. 15,726
32 exp Placebos/ 30,724
33 or/26-32 1,003,206
34 case report.tw. 164,737
35 letter/ 742,890
36 historical article/ 281,494
37 exp Editorial/ 295,617
38 or/34-37 1,467,233
39 33 not 38 962,656
40 exp Sensitivity and Specificity/ 352,539
41 (sensitivity or specificity).tw. 593,131
42 ((pre-test or pretest) adj probability).tw. 988
43 post-test probability.tw. 273
44 predictive value$.tw. 54,533
45 likelihood ratio$.tw. 6,584
46 exp "Predictive Value of Tests"/ 118,653
47 or/39-46 1,751,101
48 exp Meta-Analysis as Topic/ 12,014
49 (meta analy$ or metaanaly$).tw. or exp Meta-analysis/ 49,880
50 (systematic adj (review$1 or overview$1)).tw. 30,599
2017 American Medical Association. All rights reserved. 88
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
51 exp Review Literature as Topic/ 6,214
52 or/47-51 1,795,992
53 (embase or cochrane or psyclit* or psychlit* or psycinfo or psychinfo).tw. 28,587
54 (cinahl or cinhal).ab. 6,206
55 (science citation index or bids or cancerlit).ab. 2,197
56 or/52-55 1,803,599
57 (reference list$ or bibliograph$ or hand-search$ or relevant journals or manual search$).ab. 18,879
58 (selection criteria or data extraction).ab. 20,833
59 exp Review/ 1,684,812
60 58 and 59 14,483
61 56 or 57 or 60 1,811,665
62 exp Comment/ or exp Editorial/ or exp Letter/ 1,120,430
63 61 not 62 1,780,921
exp Epidemiologic studies/ or exp case control studies/ or exp cohort studies/ or Case control.tw. or (cohort adj (study or
studies)).tw. or cohort analy$.tw. or (Follow up adj (study or studies)).tw. or (observational adj (study or studies)).tw. or
64 Longitudinal.tw. or Retrospective.tw. or Cross sectional.tw. or exp Cross-sectional studies/ 1,563,211
65 63 or 64 2,990,436
66 9 and 15 and 16 79
67 65 and 66 46
68 limit 67 to english language 38
69 limit 68 to yr=1998-Current 24
eTABLE 19. EMBASE Targeted Search: Antimicrobial Prophylaxis with a Drain
# Search History Results
antiinfective agent/exp or antibiotic prophylaxis/exp or antimicrobial/exp or anti infective or anti-infective agents/exp and
1 [english]/lim and [embase]/lim and [1998-2012]/py 909,070
2 meta analysis/exp or (meta and adj and analy$) or metaanaly$ or (systematic and adj and (review$ or overview$)) 61,427
3 cancerlit or cochrane or embase/exp or psychlit/exp or psyclit/ or science citation index/exp or bids or scopus 44,494
2017 American Medical Association. All rights reserved. 89
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
reference lists or bibliograph$ or hand search$ or manual search$ or relevant journals or data extraction/exp or selection
4 criteria 28,035
5 review.pt. 4
6 review/exp 1,831,423
7 5 or 6 1,831,427
8 4 and 7 15,584
9 letter.pt. or editorial.pt. 3
10 letter/exp or editorial/exp 1,179,933
11 9 or 10 1,179,934
12 2 or 3 or 8 98,049
13 12 not 11 93,355
clinical trial/exp or randomized controlled trial/exp or randomization/exp or single blind procedure/exp or double blind
procedure/exp or crossover procedure/exp or placebo/exp or randomi?ed and controlled and trial$ or rct$ or random allocation
or randomly allocated or allocated randomly or allocated and adj2 and random$ or single and blind$ or double and blind$ or
14 (treble or triple and adj and blind$) or placebo$ or prospective study/exp 541,923
case study/exp or case study or case report/exp or case report or abstract report/exp or abstract report or letter/exp or letter
15 and [1998-2012]/py 1,237,206
16 14 not 15 529,538
17 clinical study/exp or case control study/exp or family study/exp or longitudinal study/exp or retrospective study/exp 5,942,135
18 prospective study/exp 189,505
19 randomized controlled trial/exp 307,692
20 18 not 19 165,671
cohort analysis/exp or (cohort and adj and (study or studies)) or (case and control and adj and (study or studies)) or (follow and
up and adj and (study or studies)) or (observational and adj and (study or studies)) or (epidemiologic$ and adj and (study or
21 studies)) or (cross and sectional and adj and (study or studies)) 115,089
22 17 or 20 or 21 5,987,932
sensitivity and specificity/exp or sensitivity or specificity or (pre test or pretest and adj and probability/exp) or post-test
probability or predictive and value$ or likelihood and ratio$ or predictive value/exp or diagnostic accuracy /exp and english]/lim
23 and [embase]/lim and [1998-2012]/py 144,775
24 13 or 16 or 22 or 23 6,162,421
2017 American Medical Association. All rights reserved. 90
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
25 infection/exp 2,328,600
26 Infection$ or infecting or infected 2,654,665
27 prosthesis related and infections 95
28 prosthesis-related infections/exp 2,328,600
29 25 or 26 or 27 or 28 2,660,841
30 prostheses and orthoses/exp or prosthe$ or implant$ or orthoped$ or orthopaed$ 399,873
joint/exp or joint$ or joint surgery/exp or arthroplasty/exp or arthroplasty or arthroplasties or arthroplasty replacement or
31 (orthopedic surgery/exp and joint/exp) 603,883
32 30 and 31 69,062
33 1 and 24 and 29 and 32 and [english]/lim and [embase]/lim and [1998-2012]/lim 1,364
34 drain/exp or drain* 138,118
35 33 and 34 115
eTABLE 20. Cochrane Database of Systematic Reviews Targeted Search: Antimicrobial Prophylaxis with a Drain
# Search History Results
(antisept* or antibiotic* or antimicrobial* or anti-infect*) and (surgery or surgical* or operat*) and (joint* or arthroplast* or prosthe* or
1 implant*) in Title, Abstract or Keywords 12
2017 American Medical Association. All rights reserved. 91
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
1.2G. PROSTHETIC JOINT ARTHROPLASTY SECTION TARGETED SEARCH: BIOFILM
eTABLE 21. MEDLINE Targeted Search: Biofilm
# Search History Results
1 (exp "prostheses and implants"/ or prosthe*.af. or implant*.af. or orthoped*.af. or orthopaed*.af.) and (exp joints/ or joint*.af.) 100,195
2 exp Joints/su [Surgery] 43,624
3 exp Arthroplasty, Replacement/ or exp Arthroplasty/ 30,982
4 arthroplast*.af. 41,886
5 exp "Orthopedic Procedures"/ and exp "Joints"/ 39,075
6 or/1-5 139,184
7 exp Infection/ or infection*.af. or infecting.af. or infected.af. or exp "Prosthesis-Related Infections"/ 1,511,311
8 (adhesin* or biofilm*).af. 22,728
9 exp Adhesins, Bacterial/ 5,227
10 "adhesin, staphylococcus aureus".af. 93
("bacterial adhesin receptor" or "polysaccharide intercellular adhesin" or "adhesin, Pseudomonas" or "Bap protein, Staphylococcus
11 aureus").af. 322
12 exp Biofilms/ 11,763
13 exp Staphylococcus aureus/ 42,676
14 or/8-13 64,215
15 6 and 7 and 14 515
16 limit 15 to english language 472
17 limit 16 to yr="1998 -Current" 382
18 exp Random Allocation/ 72,622
19 exp Randomized Controlled Trials as Topic/ or exp Randomized Controlled Trial/ 386,853
20 exp Double-Blind Method/ 111,942
21 exp Single-Blind Method/ 15,496
22 exp Clinical Trial/ 656,004
23 exp Clinical Trials as Topic/ 247,358
24 clinical trial.pt. 464,810
2017 American Medical Association. All rights reserved. 92
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
25 clinical trial, phase i.pt. 11,518
(clinical trial, phase ii or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or randomized controlled trial or
26 multicenter study or clinical trial).pt. 653,827
27 or/18-26 878,988
28 (clinical adj trial$).tw. 160,316
29 ((singl$ or doubl$ or treb$ or tripl$) adj (blind$3 or mask$3)).tw. 109,518
30 placebo$.tw. 131,568
31 randomly allocated.tw. 13,041
32 (allocated adj2 random$).tw. 15,306
33 exp Placebos/ 30,269
34 or/28-33 977,370
35 case report.tw. 161,905
36 letter/ 726,601
37 historical article/ 278,462
38 exp Editorial/ 285,735
39 or/35-38 1,435,636
40 34 not 39 937,867
41 exp "Sensitivity and Specificity"/ 342,804
42 (sensitivity or specificity).tw. 578,788
43 ((pre-test or pretest) adj probability).tw. 953
44 post-test probability.tw. 260
45 predictive value$.tw. 53,070
46 likelihood ratio$.tw. 6,322
47 exp "Predictive Value of Tests"/ 114,791
48 or/41-47 833,451
49 exp Meta-Analysis as Topic/ 11,663
50 (meta analy$ or metaanaly$).tw. or exp Meta-analysis/ 46,882
2017 American Medical Association. All rights reserved. 93
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
51 (systematic adj (review$1 or overview$1)).tw. 28,388
52 exp Review Literature as Topic/ 5,925
53 or/49-52 74,728
54 (embase or cochrane or psyclit* or psychlit* or psycinfo or psychinfo).tw. 26,489
55 (cinahl or cinhal).ab. 5,754
56 (science citation index or bids or cancerlit).ab. 2,076
57 or/54-56 28,166
58 (reference list$ or bibliograph$ or hand-search$ or relevant journals or manual search$).ab. 18,009
59 (selection criteria or data extraction).ab. 19,848
60 exp Review/ 1,647,360
61 59 and 60 13,695
62 53 or 57 or 58 or 61 96,348
63 exp Comment/ or exp Editorial/ or exp Letter/ 1,090,861
64 62 not 63 90,596
exp Epidemiologic studies/ or exp case control studies/ or exp cohort studies/ or Case control.tw. or (cohort adj (study or
studies)).tw. or cohort analy$.tw. or (Follow up adj (study or studies)).tw. or (observational adj (study or studies)).tw. or
65 Longitudinal.tw. or Retrospective.tw. or Cross sectional.tw. or exp Cross-sectional studies/ 1,518,084
66 17 and 40 14
67 17 and 48 23
68 17 and 64 2
69 17 and 65 88
70 66 or 67 or 68 or 69 107
eTABLE 22. EMBASE Targeted Search: Biofilm
# Search History Results
1 biofilm/exp or adhesin/exp or biofilm* or adhesion* and [english]/lim and [1998-2012]/py 23,287
2 arthroplasty/exp and [english]/lim and [1998-2012]/py 37,286
2017 American Medical Association. All rights reserved. 94
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
# Search History Results
3 1 and 2 104
3 and (case control study/de or clinical protocol/de or clinical study/de or clinical trial/de or consensus development/de or
controlled clinical trial/de or controlled study/de or culture technique/de or human/de or in vitro study/de or major clinical
4 study/de or practice guideline/ de or prospective study/de) 94
5 infection/exp and [english]/lim and [1998-2012]/py 1,005,608
6 4 and 5 82
7 4 and [embase]/lim and [1998-2012]/py 83
eTABLE 23. Cochrane Database of Systematic Reviews Targeted Search: Biofilm
# Search History Results
1 (biofilm* or adhesin*) in Title, Abstract or Keywords 8
2017 American Medical Association. All rights reserved. 95
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2. EVIDENCE, GRADE and RISK OF BIAS ASSESSMENT TABLES
2.1. Core Section GRADE, Evidence, and Risk of Bias Assessment Tables
2.1A. Q1 PARENTERAL ANTIMICROBIAL PROPHYLAXIS (AMP)
2.1A1. GRADE TABLE: Q1 PARENTERAL AMP
eTABLE 24. GRADE Table for Q1 Parenteral AMP
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
Q1. What are the most effective strategies for administering parenteral AMP to reduce the risk of SSI?
Q1A. What is the optimal timing of preoperative AMP?
Elective Lower Limb Musculoskeletal Procedures (majority fracture repairs with some soft tissue surgeries)
In 1 RCT (N=106) of a mixture of implant
AMP 1
surgeries with soft tissue operations, where
minute
limbs were exsanguinated prior to tourniquet
after vs. 5
Deep 1 inflation, Patients in the group who received
minutes 1 RCT High -1 0 0 -1 0 0 0 0 Low Low
SSI* intravenous antibiotics after tourniquet
prior to
inflation had significantly fewer deep
tourniquet
infections: 2/52 (3.9%) vs. 8/54 (14.8%);
inflation
p=0.03, at 12 month follow up.
Primary Total Knee Arthroplasty
In 1 RCT (N=908) of primary knee
arthroplasties, patients who received
AMP 10 Deep 2 intravenous antibiotics after tourniquet inflation
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
minutes SSI* had fewer deep SSI at 12 months follow up:
before 12/466 (2.6%) vs. 16/442 (3.6%); p=0.44 but
tourniquet this difference was not significant.
release vs.
There was no difference in the mean length of Moderate
10-30 Length of 2
1 RCT stay between groups: 6.41.6 vs. 6.52.1 High 0 0 0 -1 0 0 0 0 Moderate
minutes Stay
days; p=0.58
before
tourniquet Antimicr- 19/ 31 organisms isolated from 28 SSI were
inflation obial 2 Staphylococcus.
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Resista- MRSA: 1/12 (8.3%) vs. 1/16 (6.25%)
nce Methicillin Resistant-Coagulase Negative
2017 American Medical Association. All rights reserved. 96
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
Staphylococcus aureus: 4/12 (25.0%) vs. 2/16
(12.5%)
Q1B. What is the optimal timing of AMP in cesarean section: prior to skin incision or at cord clamping?
N=2493 Mothers from 7 RCTs all undergoing
SSI- Cesarean section overall OR: 0.57 (0.34-
3-9 2
Endome- 7 RCTs 0.94); p=0.03; I =0 indicating a reduction in High 0 0 0 0 0 0 0 0 High
tritis* the odds of developing endometritis with
administration of AMP prior to skin incision
N=2493 Mothers from 7 RCTs all undergoing
SSI 3-9
7 RCTs cesarean section, overall OR: 0.82 (0.52 High 0 0 0 0 0 0 0 0 High
Incisional 2
1.31); p=0.41; I =0; indicating no difference
N=1080 Neonates from 3 RCTs all delivered
Cesarean by Cesarean section, administration of AMP to
section the mother prior to skin incision did not
AMP Neonatal 6-8 significantly affect proven neonatal sepsis-
3 RCTs 2 High 0 0 0 0 0 0 0 0 High
timing: Sepsis OR: 0.81 (0.45 1.44); p=0.47; I =0
1 RCT stated that there was no significant
5
Prior to High
skin difference in the rate of neonatal sepsis
incision vs. between groups but data was not shown.
at cord N=1604 Neonates delivered by cesarean
clamping section from 5 RCTs, administration of AMP to
Neonatal
5 RCTs the mother prior to skin incision did not
Sepsis 4,6-9 High 0 0 0 0 0 0 0 0 High
significantly affect suspected sepsis that
Workup
required workup: OR: 0.92 (0.68 1.24);
2
p=0.58; I =0
In 1 RCT , 13 cases of sepsis among 357
8
Neonatal
neonates did not show increased antimicrobial
Antimicr-
4,8 resistance 2/6 vs. 3/7
obial 2 RCTs High 0 0 0 -1 0 0 0 0 Moderate
In 1 RCT , with 38 cases of suspected sepsis
4
Resista-
there were no cases of antibiotic resistance in
nce
the neonates
2017 American Medical Association. All rights reserved. 97
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
Neonate N=1694 Neonates from 5 RCTs all delivered
Admissi- by Cesarean section, administration to the
on to 5 RCTs mother prior to skin incision did not
3,4,6-8 High 0 0 0 0 0 0 0 0 High
Higher significantly affect admission of neonate to an
Level increased infant care unit. OR: 0.92 (0.64
2
Care 1.32); p=0.64; I =0
Q1C. How safe and effective is weight-adjusted AMP dosing? Our search did not identify RCTs or SRs that evaluated weight-adjusted AMP dosing and its impact
on the risk of SSI.
Q1D. How safe and effective is intraoperative redosing of AMP?
In 1 RCT (N=278) in elective colorectal
surgery, 271 patients completed 30 day follow
up. No difference: 10/143 (7%) vs. 7/128
(5%); p>0.05
Patients with procedure duration >3h had a
significantly higher probability of infection
(5/37 (14%)) as compared to those with 2-3hr
1
(5/127 (4%)) or <2h duration 7/107 (7%);
Preoperati-
p<0.05. Of note, 36/164 (22%) of patients with
ve dose
SSI* procedure durations 2h were not redosed
vs. 10
(Abdomi- 1 RCT intraoperatively (antimicrobial half-life was 68 High 0 0 0 -1 0 0 0 0 Moderate
1
nal) min). Study does not report these infections
preoperati-
by single dose versus redosed. Moderate
ve dose
plus Increasing fecal contamination almost
doubled the infection rate at every level from
additional
2/67 (3%) in those with no contamination, to
dose at 2h
intraoperat- 10/162 (6%) in those with moderate, and 5/38
ively (13%) in those with gross contamination,
p<0.05 (contamination unknown in 4). Study
does not report these infections by single
dose versus redosed.
Intra-
Abdomi- 10
1 RCT No difference: 8/146 (5%) vs. 10/132 (8%) High 0 0 0 -1 0 0 0 0 Moderate
nal
Abscess*
2017 American Medical Association. All rights reserved. 98
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
Perineal
10
Wound 1 RCT No difference: 4/9 vs. 4/9 High 0 0 0 -1 0 0 0 0 Moderate
Infection*
Antimicr-
No difference: 1 minor SSI in each group
obial 10
1 RCT culture positive for MRSA as the sole High 0 0 0 -1 0 0 0 0 Moderate
resistan-
organism
ce
Q1E. How safe and effective is postoperative AMP and what is the optimal duration?
All Surgeries
In a meta-analysis of 21 RCTs, (N=14,285) no
None 11-
21 RCT benefit of continuing AMP after the wound is
vs. SSI* 31 High 0 0 0 0 0 0 0 0 High High
closed in the operating room: OR: 1.19 (0.94
<24h 2
1.50); p=0.15; I =25%
Cardiac Surgery
In a meta-analysis of 3 RCTs
12,32,33
Organ- (N=1746),
None
Space 3 RCT there was no benefit of continuing AMP after
vs. 12,32,33 High 0 0 0 -1 0 0 0 0 Moderate Moderate
Sternal the wound was closed in the operating room:
96h 2
SSI* OR: 1.84 (0.82 4.14); p= 0.14; I =0
24h AMP duration reduced the risk of SSI at
12 month follow up in 1 large RCT with N=838
patients undergoing CABG with or without
valve replacement: 30 /419 (7.2%) vs. 15/419
(3.6%); p=0.02. Overall rate of SSI was 5.9%.
Patients received their first dose of AMP 20-
None
30 min after induction of anesthesia, and
vs. 12
SSI* 1 RCT those whose procedures lasted >3h were High 0 0 0 -1 0 0 0 0 Moderate Moderate
24h
redosed intraoperatively.
The no postoperative AMP group also had
statistically higher proportion of patients on
intraaortic balloon pump postoperatively
(0.03) and received more blood transfusions
(0.01).Patients who presented with both
osteomyelitis and mediastinitis were reported
2017 American Medical Association. All rights reserved. 99
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
as both an organ/space and a deep incisional
SSI. Between 1 and 3 of 5 deep SSI patients
in the no postoperative AMP group may
have had both. Since the study did not stratify
those results, deep SSI data were excluded
from this analysis.
No S. aureus decolonization was performed.
No difference: 14/419 (3.3%) vs. 8/419
Organ/
(1.9%); p=0.19 at 12 month follow up.
Space 12
1 RCT No statistically significant differences between High 0 0 0 -1 0 0 0 0 Moderate
Sternal
groups for osteomyelitis, mediastinitis, or
SSI
endocarditis individually.
24 AMP reduced the risk of superficial
Superfic- 12 incisional SSI:16 (3.8%) vs. 7 (1.7%); p=0.04
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
ial SSI However, it is not clear if incisional SSIs
included both sternal and donor site wounds.
12 No difference at 30d, 90d and 365d (P=0.12,
Mortality 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
0.18, and 0.34, respectively)
No differences: (14.7515.8 vs. 12.214.2);
p=0.25.
Length of 12 Of note, patients in both groups were
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Stay hospitalized for approximately 10 days before
surgery and had long mean ICU stays:
10.310.9 vs. 9.18.7; p=0.09.
The most frequently isolated organisms were
Antimicr- Staphylococcus epidermis and
obial 12 Staphylococcus aureus (p0.05) and the
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Resista- majority of SSIs were polymicrobial: 57.1% vs.
nce 60.0%.
MRSA: 4/35 (11.4%) vs. 9/15 (60%); p<0.01
2017 American Medical Association. All rights reserved. 100
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
Organ/
Space 2 RCT No difference in meta-analysis (N=908) of 2
32,33 2 High 0 0 0 -1 0 0 0 0 Moderate
SSI* RCTs, OR: 4.28 (0.47 39.24); p=0.20; I =0
Sternal
Superfic-
32-
ial 3 RCT No difference in meta-analysis (N=993) of 3
34 2 High 0 0 0 -1 0 0 0 0
Sternal RCTs: OR: 1.23 (0.44 3.45); p=0.69; I =0 Moderate
SSI*`
No difference in 1 large RCT where 766
SSI* Leg
(91%) of 844 CABG patients underwent leg
Graft 33
1 RCT vein harvest. 23/377 (6.1%) vs. 20/389 High 0 0 0 -1 0 0 0 0 Moderate
Donor
(5.1%); 7 day follow up. Overall donor site SSI
Site
rate 5.6% (43/766)
Leg Graft
No difference: 18 reports of wound
None Donor
dehiscence in each group (7-day follow up).
vs. Site 33 Moderate
1 RCT The authors included donor site wound High 0 0 0 -1 0 0 0 0 Moderate
72-96h Wound
dehiscence in their calculation of the overall
Dehisce-
infection rate.
nce
Superfic-
ial Leg
33 No difference: 5/377 (1.3%) vs. 2/389 (0.5%);
Graft 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
p=0.26 (7 day follow up)
Donor
Site SSI*
Significantly shorter length of stay with
Length of 34 postoperative AMP in one small (N=85) RCT
1 RCT High -1 0 0 -1 0 0 0 0 Low
Stay with data collected 35 years ago: 12.034.2
versus 14.67.5 days; P<0.05
Antimicr-
One study both incisional SSIs were
34
obial 2 RCT
32,34 Staphylococcus aureus High -1 0 0 -1 0 0 0 0 Low
Resista-
One study incisional SSI: The no
32
nce
2017 American Medical Association. All rights reserved. 101
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
postoperative AMP group had 1
Staphylococcus aureus and 1 Staphylococcus
epidermis infection as compared to 1 Serratia
marcescens and 1 Enterococcus infection in
those with postoperative AMP. The one case
of endocarditis in the group with no
postoperative AMP was a Staphylococcus
epidermis.
Sternal 35 No difference in 30 day SSI (N=231) 13/120
1 RCT High -1 0 0 -1 0 0 0 0 Low
SSI* (10.8%) vs. 9/111 (8.1%); p=0.48
Deep
35 No difference in deep sternal SSI (N=231)
Sternal 1 RCT High -1 0 0 -1 0 0 0 0 Low
3/120 (2.5%) vs. 1/111 (0.9%); p=0.62
SSI*
Superfic-
No difference in superficial sternal SSI
ial 35
1 RCT (N=231) 3/120 (2.5%) vs. 2/111 (1.8%); High -1 0 0 -1 0 0 0 0 Low
Sternal
24h SSI*
p=1.00
vs. Low
72h No difference in harvest site SSI (N=231) at
Harvest 35
1 RCT 30 days 73/120 (5.8%) vs. 6/111 (5.4%); High -1 0 0 -1 0 0 0 0 Low
Site SSI*
p=0.89
Total
35 No difference in length of stay: 15.15.2 days
Length of 1 RCT High -1 0 0 -1 0 0 0 0 Low
versus 16.79.1 days; p=0.10
Stay
No difference in rates of MSSA: 3/120 (2.5%)
Antimicr-
vs. 3/111 (2.7%); p=1.00; or MRSA: 2/120
obial 35
1 RCT (1.7%) vs. 3/111 (2.7%); p=0.67 High -1 0 0 -1 0 0 0 0 Low
Resista-
Although not significant, nasal swab screen
nce
results prior to surgery were higher in 1-day
2017 American Medical Association. All rights reserved. 102
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
group for both MSSA: 8/120 (7.3%) vs. 16/111
(15.5%); p=0.06; and MRSA: 6/120 (5.5%) vs.
4/111 (3.9%); p=0.75.
Thoracic Surgery
No difference in 1 RCT (N=203) of patients
undergoing thoracic surgery (thoracotomy
36
SSI* 1 RCT with lung resection): 7/102 (7%) vs. 2/101 High 0 0 0 -1 0 0 0 0 Moderate
(2%); p=0.11.
Overall SSI rate was 4.4%.
Significantly more empyema in group without
Organ/
postoperative AMP: 6/102 (6%) vs. 1/101
Space
36 (1%); p=0.03.
SSI 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Both groups received AMP at induction of
(empye-
anesthesia and were redosed intraoperatively
ma)
(2h).
None
vs. Incisional 36 No difference: 1/102 (1%) vs. 1/101 (1%); Moderate
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
2 days SSI p=0.9.
36 4 (2%) postoperative deaths; none related to
Mortality 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
AMP or SSI.
Length of 36 No differences: 151.6 days versus 131
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Stay days.
Adverse 36 No side effects of the antimicrobial
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Events prophylaxis were noted.
Vascular Surgery
2017 American Medical Association. All rights reserved. 103
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
No difference in 1 RCT subanalysis (N=169)
None of clean, clean-contaminated, and
16
vs. SSI* 1 RCT contaminated elective and emergency High 0 0 0 -1 0 0 0 0 Moderate Moderate
<24 hours vascular surgery procedures: 2/89 (3.8%) vs.
3/80 (2.3%), p>0.05 (1 month follow up).
No difference in 1 RCT, of patients
<24h undergoing acute femoral embolectomy or
vs. SSI* 37 thrombectomy, subanalysis (N=121): 2/52 High 0 0 0 -1 0 0 0 0 Moderate Moderate
1 RCT
3 days (3.8%) vs. (3/69) 4.3%; p=0.89 (30 day follow
up).
Reduced risk of SSI with postoperative AMP
in 1 RCT of emergency and elective open
arterial reconstructions (N=302): 28/153
(18%) vs. 15/149 (10%); OR: 2.00 (1.02
3.92); p=0.04 (42 day follow up).
38 Overall SSI rate: 14.2% (43/302).
SSI* 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
None Patients received first dose of AMP (over 30
vs. minutes) after induction of anesthesia. Moderate
5 days Patients tended to be elderly and debilitated,
with a higher proportion of those in the no
postoperative AMP being current smokers
and insulin dependent diabetics.
Organ/
38
Space 1 RCT No difference: 1 graft infection in each group. High 0 0 0 -1 0 0 0 0 Moderate
SSI
Ear, nose, and throat (ENT) procedures
No difference on meta-analysis of 2 small
RCTs (N=127): OR: 1.54 (0.59 4.05);
24h
2
p=0.38 ; I =0
2 RCT
1 RCT of 53 patients undergoing head and
39
vs. SSI* 39,40 High 0 0 0 -1 0 0 0 0 Moderate Moderate
3-5 days neck procedures including myocutaneous flap
reconstruction reported an overall wound
infection rate of 24.5% (13/53) at 30 day
2017 American Medical Association. All rights reserved. 104
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
follow up and no difference between groups:
8/26 (30.7%) vs. 5/27 (18.5%); p=0.47.
1 RCT in 74 patients undergoing head and
40
neck procedures including immediate flap
reconstruction reported an overall wound
infection rate of 10.8% (8/74) at 7 day follow
up and no difference between groups 4/35
(11%) vs. 4/39 (10%); p=0.99
Length of 39 No difference: 2518 vs. 2215 days;
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Stay p=0.627.
Pharyng- No difference: 3/35 (9%) vs. 3/39 (8%) (7 day
ocutane- 40 follow up).
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
ous Overall pharyngocutaneous fistula rate: 6/74
Fistula (8%).
Gynecologic Procedures
No difference in SSI in a meta-analysis
(N=1917) of 5 RCTs: OR: 0.92 (0.51 1.65);
2
p=0.77; I =0
In 1 RCT (N=531) of patients undergoing
13
laparoscopic-assisted vaginal hysterectomy
(LAVH) or ovarian cystectomy (LAOC), total
abdominal or vaginal hysterectomies (TAH or
None TVH), 1 trocar site infection was reported in
5 RCT
vs. SSI* 13,27-30 each group at 90 day follow up: 1/267 vs. High -1 0 0 -1 0 0 0 0 Low Low
24h 1/264.
In 1 RCT (N=66) of patients undergoing
27
radical gynecologic pelvic surgery for
malignancy, 1 abdominal wound infection was
reported in each group at 8 day follow up:
1/37 vs. 1/29.
In 1 RCT with a subpopulation of 608
29
patients undergoing unspecified gynecologic
2017 American Medical Association. All rights reserved. 105
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
procedures, no difference in SSI at minimum
7 day follow up: 12/385 vs.4/223; p=0.53
28
In 1 RCT of 112 patients undergoing
vaginal hysterectomy, no difference in SSI at
3-6 week follow up: 1/58 vs. 2/54
30
In 1 RCT of 500 women undergoing
cesarean section, No difference in SSI at 30
day follow-up: 12/250 (4.8%) vs. 16/250
(6.4%).
In 1 RCT (N=531) among the 478 who had
laparoscopic-assisted vaginal hysterectomy
(LAVH), total abdominal or vaginal
Organ/
13 hysterectomies (TAH or TVH), only 1 vaginal
space 1 RCT High -1 0 0 -1 0 0 0 0 Low
cuff infection with pelvic abscess was reported
SSI
in a patient who underwent LAVH in the 24
hour group: 0/237 vs. 1/241 (0.41%) at 90 day
follow up.
In 1 RCT (N=531), among the 455 (86%)
patients who had a laparoscopic-assisted
vaginal hysterectomy (LAVH) or ovarian
Trocar
13 cystectomy (LAOC), only 1 trocar wound
Wound 1 RCT High -1 0 0 -1 0 0 0 0 Low
infection was reported in a patient who
Infection
underwent LAOC in the no postoperative AMP
group: 1/226 (0.44%) vs. 0/229. (90 day follow
up).
13
One RCT no difference: 4.02 1.51 vs.
3.971.27.
27
Length of 3 RCT One RCT no difference: 18 days (range 12-
13,27,28 High -1 0 0 0 0 0 0 0 Moderate
Stay 23) vs. 19 days (range, 12-23 days).
28
One RCT no difference : days SD: 4.41.1
vs. 4.71.2 days.
2017 American Medical Association. All rights reserved. 106
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
No difference: 1 RCT (N=156) in patients
undergoing a laparoscopic-assisted vaginal
41
SSI* 1 RCT hysterectomy (LAVH) no difference: 2/74 High 0 0 0 -1 0 0 0 0 Moderate
(2.7%) vs. 3/82 (3.6%) (7 day follow up)
Overall SSI rate: 3.2% (5/156)
<24h
vs. Organ/ Moderate
<2.5 days 41 No difference 1 vaginal cuff abscess in each
Space 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
group. (7 day follow up).
SSI
Trocar
41 No difference: 1/74 (1.4%) vs. 3/82 (3.7%);
wound 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
p=0.38. (7 day follow up)
infection
Orthopaedic Surgery Fracture Surgery
No difference on meta-analysis of 4 RCTs
(N=1722): OR: 1.87 (0.70 4.94); p=0.21 ;
2
I =44%
3 RCTs
14, 17, 19
reported no difference
between groups for all SSIs combined.
One RCT (N=191) in hip fracture patients
14
reported a total of 4 (2.1%) infections and no
difference between groups at 6w follow up:
2/83 (2.4%) vs. 2/108 (1.9%); p=0.79. Both
None
were superficial SSI. Postop dosing group
vs. SSI* 4 RCT High -1 0 0 -1 0 0 0 0 Low Low
received AMP for another 24h.
24h
14,17-19
1 RCT (N=200) in a mix of clean
17
orthopaedic fracture surgeries reported a total
of 14(7%) infections, and no difference
between groups at 28day follow up: 8% vs.
6%; p=0.27 Postop dosing group received
AMP for another 24h.
1 RCT (N=614) in orthopaedic fracture
19
fixation and arthroplasty patients, no
difference: 2/301 (0.66%) vs. 3/313 (1.27%);
2017 American Medical Association. All rights reserved. 107
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
p=0.45 (10 day follow up); overall SSI rate
0.98%.
18
1 RCT (N=717) in a mix of orthopaedic
fracture surgeries, reported a total of 23
(3.2%) infections (follow up period not
reported) with a significantly higher risk of SSI
among the no postoperative AMP group :
20/382 (5.3%) vs. 3/335 (0.89%); p<0.01 This
significance was seen for both
hemiarthroplasties: 5/76 (6.5%) vs. 0/74 (0%);
p=0.03 and all other procedures combined:
15/306 (5%) vs. 3/261 (1%); p<0.01.
Postoperative dosing group received AMP for
another 20h postop. Patients in both groups
were hospitalized for approximately 5 days
before surgery.
No difference on meta-analysis of 2 RCTs
(N=391): OR: 0.33 (0.03 3.19); p=0.34.
14
One RCT (N=191) in hip fracture patients
reported no deep infections in either group
2 RCT
Deep 14,17 (0/83 vs. 0/108) at 6 week follow up.
High -1 0 0 -1 0 0 0 0 Low
17
SSI 1 RCT (N=200) in a mix of clean orthopedic
fracture surgeries reported a total of 4 (2%)
deep infections and no difference between
groups at 28 day follow up: 1% vs. 3%;
p=0.34.
No difference in meta-analysis of 2 RCT
(N=391), no difference between groups OR:
2
1.99 (0.64 6.17); p=0.24; I =0%.
14
Superfic- 2 RCT 1 RCT (N=191) in hip fracture patients
14,17 High -1 0 0 0 0 0 0 0 Moderate
ial SSI reported a total of 4 (2.1%) infections and no
difference: 2/83 (2.4%) vs. 2/108 (1.9%);
p=0.79 (6 week follow up).
17
1 RCT (N=200) in a mix of clean
2017 American Medical Association. All rights reserved. 108
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
orthopaedic fracture surgeries reported a total
of 10 (5%) superficial SSIs and no difference:
7% vs. 3%; p=0.21 (28 days follow up).
In 1 RCT (N=191), there were 7 (3.4%)
14
deaths. There were no significant differences
in mortality between groups 3/121 (2.4%) vs.
Mortality 2 RCT 4/83 (4.81%) and no deaths resulted from
14,18 High 0 0 0 0 0 0 0 0 High
infections.
In 1 RCT (N=717) there were 30 deaths
18
(4%); 1 patient had an uncontrolled wound
infection but the cause of death was a stroke.
In 1 RCT (N=191), there were no anaphylactic
Adverse 14
1 RCT reactions, allergies, or renal toxicity related to High 0 0 0 -1 0 0 0 0 Moderate
Events
antimicrobial prophylaxis administration.
In 1 RCT (N=191), Staphylococcus aureus
14
isolated from all SSIs. No gram negative
organisms isolated. No mention of
antimicrobial resistance.
In 1 RCT (N=200) Staphylococcus aureus
17
was the commonest organism isolated,
followed by E. coli. Eight of the 14 SSIs had a
Antimicr-
negative wound culture (7 superficial, 1 deep).
obial 3 RCT
14,17,18 No mention of resistance. High 0 0 0 0 0 0 0 0 High
Resista-
18
nce In 1 RCT (N=717) 31 organisms isolated
from 23 wound infections: 9 Staphylococcus
aureus, 4 S. epidermis, and 4 E. coli all
sensitive to the AMP. In addition, 4
Pseudomonas aeruginosa, and 3
Streptococcus faecalis all resistant to the
AMP and 7 strains of other gram negative
bacilli, 2 of them resistant to the AMP.
Orthopaedic Surgery - Prosthetic Joint Arthroplasty
2017 American Medical Association. All rights reserved. 109
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
No difference in a meta-analysis of 2 RCT,
(N=2,847) no difference between groups OR:
1.84 (0.68 4.98); p=0.23.
In the larger RCT (N=2651) in THA, TKA,
20
and hemiarthroplasty patients, no difference in
None 2 RCT PJI between groups at 13 month follow up:
20,21
vs. SSI* 11/1327 (0.83%) vs. 6/1324 (0.45%); p=0.17; High 0 0 0 0 0 0 0 0 High High
24h RR: 1.83, (0.68-4.93).
In the second smaller study (N=196), in
21
unilateral or bilateral THA or TKA patients no
infections (including deep wound infections)
were reported in either group at 12 month
follow up.
Colorectal Surgery
BOWEL PREPARATION INCLUDED ORAL ANTIMICROBIALS PREOPERATIVELY
No difference in 1 RCT (N=360) in patients
SSI* 42 undergoing elective laparotomy for colorectal
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Incisional malignancy: 15/179 (8.4%) vs. 13/181 (7.2%);
p=0.67 (30 day follow up).
SSI* No difference: 1/179 (0.6%) vs. 2/181 (1.1%);
42
Organ/ 1 RCT p=0.58 (30 day follow up). High 0 0 0 -1 0 0 0 0 Moderate
Space All 3 caused by anastomotic leak.
None
vs. Culture isolates available for 23/28 patients Moderate
3 days with incisional SSI: Pseudomonas aeruginosa
Antimicr-
most commonly isolated in both groups
obial 42
1 RCT followed by Enterococcus faecalis. MRSA High 0 0 0 -1 0 0 0 0 Moderate
resistan-
isolated from 3 patients all in the groups
ce
without postoperative administration of AMP
(in 2 as part of polymicrobial SSI).
Adverse
No Clostridium difficile in either group.
42
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
events
2017 American Medical Association. All rights reserved. 110
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
1 RCT (N=40) in patients with chronic
ulcerative colitis, familial polyposis, or
Gardners syndrome undergoing colectomy,
43
SSI* 1 RCT mucosal proctectomy with ileal pouch-anal High 0 0 0 -2 0 0 0 0 Low
24h anastomosis reported no wound or intra-
vs. abdominal infections in either group at 1yr Low
5 days follow up: 0/22 vs. 0/18.
Length of 43 No difference: (meanSD) 8.70.4 days vs.
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
stay 8.40.2 days.
BOWEL PREPARATION ONLY
No difference in a meta-analysis of 4 RCTs
(N=894), no difference between groups OR:
2
1.58 (0.76 3.28); p=0.22; I =57%.
1 RCT (N=377) in elective open and
15
laparoscopic colorectal procedures for colon
cancer postoperative AMP was associated
with reduced risk of SSI at 30 day follow up:
27/190(14.2%) vs. 8/187(4.3%); p<0.01. On
multivariate analysis antimicrobial dose was
None the only significant factor associated with
4 RCT
vs. SSI* 15,22-24 incisional SSI (p<0.01). High -1 -1 0 0 0 0 0 0 Low Low
1 RCT 1 subgroup analysis 1 (N=138) in
22
<24h
patients undergoing elective colorectal
procedures suggests no difference: 12/138
(8.7%); 5/71 (7.0%) vs. 7/67 (10.4%); p =0.48
(28-41 day follow up).
1 RCT subgroup analysis 2 (N=135) in
22
patients undergoing elective colorectal
procedures suggests no difference: 16/135
(11.9%); 8/65 (12.3%) vs. 8/70 (11.4%);
p=0.87 (28-41 day follow up).
2017 American Medical Association. All rights reserved. 111
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
1 RCT (N=154) in elective colorectal
24
procedures suggests no difference: 40/77
(5.2%) vs. 40/77 (5.2%); Follow up NR.
1 RCT (N= 90) in elective colorectal
23
procedures, excluding inflammatory bowel
disease, suggests no difference for abdominal
wounds: 18/90 (20%): 7/22 (31%) vs. 11/68
(16%); p=0.12; or perineal wounds: 1/3
(33.3%) vs. 7/13 (53.8%); p=0.53. (6 week
follow up).
No difference in a meta-analysis (N=531) of 2
2
RCTs OR: 0.73 (0.30 1.77); p=0.49; I =0%.
1 RCT no difference: 5/190 (2.6%) vs.
15
Organ/
2 RCT 9/187 (4.8%); p=0.26. (30 day follow up).
space 15,24 High -1 0 0 0 0 0 0 0 Moderate
1 RCT no difference for intra-abdominal
24
SSI
abscess 2/77 (2.6%) vs. 1/77 (1.3%); p=0.57
or peritonitis 2/77 (2.6%) vs. 2/77 (2.6%);
Follow up NR.
No difference in a meta-analysis of 3 RCTs:
2
OR 1.35 (0.70 2.61); p=0.37; I =0%.
1 RCT with subanalysis in elective colorectal
44
procedures (n=207) suggests no difference
between groups at 35 day follow up:
11/102(10.7%) vs. 6/105 (5.6%); p=0.19.
1 RCT (N=443) in elective colorectal
45
None
44-
vs. 3 RCT procedures for cancer, inflammatory bowel
All SSI* 46 High 0 0 0 0 0 0 0 0 High Moderate
<2 3 disease (10%), and other (10%), suggests no
days difference between groups for deep wound
infections: 17/294 (5.8%); 9/149 (6%) vs.
8/145 (6%) or for intra-abdominal abscess:
3/294 (1.0%); 1/149 (1%) vs. 2/145 (1%) at 30
day follow up.
1 RCT (N=100) in elective colorectal
46
procedures for cancer or diverticulitis
2017 American Medical Association. All rights reserved. 112
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
suggests no difference between groups: 3/100
(3.0%); 2/54 (3.7%) vs. 1/46 (2.1%); p=0.66
(Follow up NR).
Organ/ 45 No difference: 1/149 (1%) vs. 2/145 (1%).
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Space* Overall Organ/Space SSI rate: 3/294 (1.0%).
Antimicr-
obial 2 RCT No difference in bacterial isolates and no
45,46 High -1 0 0 -1 0 0 0 0 Low
Resista- report of antimicrobial resistance.
nce
BOWEL PREPARATION NOT REPORTED
No difference for colorectal cases in 1 RCT
None
25 (N=224) in at-risk abdominal surgery: 40/224
vs. SSI* 1 RCT High 0 0 0 -1 0 0 0 0 Moderate Moderate
(17.9%); 23/113(20.4%) vs. 17/111 (15.3%);
24h
p>0.2 (30 day follow up).
No difference in a meta-analysis of 4 RCTs,
(N=802) no difference between groups OR:
2
1.13; (0.75 1.70); p=0.57; I =12%.
1 RCT (N=87) colorectal surgery suggests
47
no difference: 20/87 (23.0%); 13/45 (28.9%)
vs. 7/42 (16.7%); p=0.18 (28 day follow up).
1 RCT with subanalysis (n=428) in high-risk
48
colorectal procedures suggests no difference:
24h 47-
4 RCT 45/428 (11%); 22/209 (11%) vs. 23/219
vs. SSI* 50 High 0 0 0 0 0 0 0 0 High High
(11%); p=0.99 (30 day follow up).
2-3 days
1 RCT (N=60) in elective colon surgery no
49
difference: 6/30 (20%) vs. 10/30 (33.3%);
p=0.25.
1 RCT in elective colorectal surgery
50
subanalysis (n=227) no difference in
abdominal wound: 23/113 (19.5%) vs. 22/114
(19.3); p=0.84; perineal wound: 7/113 (6.2%)
vs. 3/114 (2.6%);p=0.20.
2017 American Medical Association. All rights reserved. 113
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
No difference in a meta-analysis (N=715) of 3
2
RCTs: OR: 0.77 (0.37 1.63); p=0.50; I =0%.
1RCT Intra-abdominal abscess. No
48
difference: 14/428 (3%) total; 6/209 (3%) vs.
8/219 (4%); p=0.65 (30 day follow up).
1RCT Intra-abdominal abscess no
49
Organ/ 48-
3 RCTs difference: 2/30 (7%) vs. 2/30 (7%); Peritonitis
Space 50 High 0 0 0 0 0 0 0 0 High
no difference: 1/30 (3%) vs. 3/30 (10%);
p=0.32 (follow up NR).
1 RCT Intrapelvic abscess no difference:
50
2/113 (1.8%) vs. 2/114 (1.8%); Intra-
abdominal abscess no difference: 2/113
(1.8%) vs. 1/114 (0.9%); p=0.56; Peritonitis no
difference: 0/113 vs. 1/114 (0.9%).
Adverse events possibly related to
antimicrobial agent included 2 patients with
Adverse 50 phlebitis in the group receiving <24 AMP and
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Events in the group receiving longer AMP, 2 cases of
hypotension, 1 phlebitis, 1 erythema, and 1
rash.
NO BOWEL PREPARATION
No difference in 1 RCT subpopulation (n=46)
None
22 of emergency colorectal procedures: 6/46
vs. SSI* 1 RCT High 0 0 0 -1 0 0 0 0 Moderate Moderate
(13.0%); 4/21 (19.0%) vs. 2/25 (8.0%); p=0.28
24h
(28-42 day follow up).
None No difference in 1 RCT subpopulation (n=38)
vs. 44 of emergency colorectal procedures: 1/17
SSI* 1 RCT High 0 0 0 -1 0 0 0 0 Moderate Moderate
<2 3 (5.8%) vs. 4/21 (20.0%); p=0.26 (35 day
days follow up).
General Surgery - OTHER
Appendectomy
2017 American Medical Association. All rights reserved. 114
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
No difference in a meta-analysis of 4 RCTs
(N=1039), OR: 0.85 (0.52 1.41); p=0.54;
2
I =0.
1 RCT of emergency non-perforated open
11
appendectomies reported no difference in
incisional wound infections between groups:
6/92 (6.5%) vs. 6/94 (6.4%) at 30 day follow.
None No deep incisional or organ/space infections
4 RCT
vs. SSI* 11,22,25,31 were reported in either group. High 0 0 0 0 0 0 0 0 High High
24h 1 RCT (N=377) of emergency open
31
appendectomies suggested no difference:
9/195 (4.6%) vs. 8/182 (4.3%); p=0.92.
1 RCT with subpopulation of
25
appendectomies (n=247): 11/114 (9.6%) vs.
21/133 (15.8%); p=0.16.
Drug regimen 1 : n=112: 4/54 vs. 4/58.
22
Drug regimen 2 : n=117 2/63 vs. 0/54.
22
Increased risk of SSI with 2 days
None
44 postoperative AMP: 1 RCT subpopulation of
vs. SSI* 1 RCT High 0 0 0 -1 0 0 0 0 Moderate Moderate
appendectomies (n=246): 3/127 (2.3%) vs.
2 days
10/119 (8.4%); p<0.05.
Rectal surgery
No difference in 1 RCT subanalysis of 48
None
26 elective rectal surgery patients: 2/19 (10.5%)
vs. SSI* 1 RCT High 0 0 0 -1 0 0 0 0 Moderate Moderate
vs. 1/29 (3.4%); p=0.35. (1 month follow up).
24h
Number of events is small.
Gastric Surgery
No difference in 1 RCT with subanalysis
gastric procedures (n=64) including
None
Organ/ 26 gastrectomy (n=8), gastric banding (n=35)
vs. 1 RCT High 0 0 0 -1 0 0 0 0 Moderate Moderate
space* and other gastric (n=21) reported deep
24h
surgical sepsis: 1/24 (4%) vs. 4/40 (10%);
p=0.41.
2017 American Medical Association. All rights reserved. 115
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
No difference in meta-analysis of 2 RCTs
(N=683) of elective gastric cancer surgeries
both with 30 day follow up and intraoperative
AMP bolus administered every 3 hours of
surgery. OR: 0.87 (0.28 2.65); p=0.80;
2
I =71%
2 RCT
1 RCT (N=325) 15/164 (9.1%) vs. 10/161
52
SSI* 51,52 High -1 -2 0 0 0 0 0 0 Very Low
(6.2%); there was a higher incidence of
transfusion in the multiple dose group.
1 RCT (N=355) suggested no difference
51
8/176 (5%) vs. 16/179 (9%); p=0.138; there
was a higher incidence of transfusion in the
multiple dose group: 0/176 vs. 4/176 (2.2%).
No difference in metaanalysis of two RCTs.
(N=683); OR: 1.08 (0.37 3.17); P=0.89;
2
I =75%.
None
In 1 RCT (N=325) there were fewer SSI in
52
vs. Very Low
the multiple dose group but this difference
2 days Organ/
2 RCT was not significant: 11/164 (6.7%) vs. 6/164
Space 51,52 High -1 -2 0 0 0 0 0 0 Very Low
(3.7%); p=NS (Note: 9/164 (5.5%) vs. 3/161
SSI
(0.9%) patients manifested both organ/space
and incisional infections).
1 RCT (N=355) suggested fewer SSI in the
51
single dose group but this was not significant
7/176 (4%) vs. 11/179 (6%); p=0.47.
No difference in metaanalysis of two RCTs.
2
(N=683); 0.79 (0.08 7.87); 0.84; I =75%.
In 1 RCT (N=325) there were fewer SSI in
52
the multiple dose group but this difference
Incisional 2 RCT
51,52 was not significant: 14/164 (8.5%) vs. 7/164 High -1 -2 0 0 0 0 0 0 Very low
SSI
(4.3%) (Note: 9/164 (5.5%) vs. 3/161 (19%)
patients manifested both organ/space and
incisional infections).
1 RCT (N=355) suggested higher SSI in the
51
2017 American Medical Association. All rights reserved. 116
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
multiple dose group but this difference was
not significant: 1/176 (<1%) vs. 5/179 (3%);
p=0.215.
Antimicr-
obial 52 No difference in antimicrobial resistance
1 RCT High -1 0 0 -1 0 0 0 0 Low
Resista- between groups: 2/15 vs. 0/10.
nce
No difference in 1 RCT of elective gastric
surgery for gastric cancer (excluded colorectal
53
SSI* 1 RCT surgery): 23/243 (9.5%) vs. 21/243 (8.6%) High 0 0 0 -1 0 0 0 0 Moderate
p=NS. (30 day follow up)
Overall SSI rate of 9.1% (44/486)
Organ/
53 No difference: 12/243(4.9%). Vs.
None Space 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
10/243(4.1%) p=NS
vs. SSI Moderate
4 days
Incisional 53 No difference: 14/243 (5.8%) vs. 11/243
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
SSI (4.5%); p=NS
Antimicr-
obial 53
1 RCT No difference in isolate resistance patterns. High 0 0 0 -1 0 0 0 0 Moderate
Resista-
nce
Hepatectomy
No difference in 1 RCT (N=188) in
54 hepatectomies: 7/94 (7.5%) vs. 13/94
SSI* 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
(13.8%); 14 day follow up; p=0.24.
None vs. Overall SSI rate: 10.6% (20/188). Moderate
3 days
Organ/
54 No difference: 4/94 (4.3%) vs. 11/91 (11.7%);
Space 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
p=0.10
SSI
2017 American Medical Association. All rights reserved. 117
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
GRADE
Large Magnitude
Overall
Publication Bias
of
Dose-response
Quantity GRADE
Study Quality
Comparis- Outcom- Starting Evidenc
Confounders
Consistency
and Type of Findings of
Directness
on e GRADE e for
Evidence Evidenc-
Precision
Outcom-
e Base
e
Incisional 54 No difference: 3/94 (3.2%) vs. 3/94 (3.2%);
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
SSI p=1.00
There was a significantly longer length of stay
Length of 54
1 RCT in the multiple dose group: 12 (4-91) days vs. High 0 0 0 -1 0 0 0 0 Moderate
Stay
14 (5-265) days; p=0.03
No difference in 1 RCT (N=180) in
55 hepatectomies: 4/89 (4.5%) vs. 4/91 (4.4%);
SSI* 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
14 day follow up
Overall SSI rate: 4.4% (8/180)
Organ/
2 days vs. 55 No difference: 2/89 (2.2%) vs. 3/91 (3.3%); Moderate
5 days Space 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
p=0.67
SSI
Incisional 55 No difference: 2/89 (2.2%) vs. 1/91 (1.1%);
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
SSI p=0.56
*Critical outcome; OR: Odds Ratio; RR: Risk Ratio; CI: Confidence Interval
2017 American Medical Association. All rights reserved. 118
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.1A2. EVIDENCE TABLES: Q1 PARENTERAL AMP
Q1. What are the most effective strategies for administering parenteral AMP to reduce the risk of SSI?
Q1A. What is the optimal timing of preoperative AMP? Our search did not identify RCTs or SRs that evaluated different timings of preoperative AMP
administration and its impact on the risk of SSI.
eTABLE 25. Evidence Table Q1A. Q1A. What is the optimal timing of preoperative AMP in surgeries involving tourniquet
inflation?
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Akinyoo- RCT To compare Number of patients: Intervention group: n=52 SSI Definitions:
la 1, 2 the clinical N=106 Intravenous cefuroxime at Postoperative wound Wound infections:
1
2011 outcomes in Patient a dose appropriate to infection spontaneous
(ES) patients Characteristics the patients age and Intervention: 2/52 (3.9%) drainage of pus
administered Age, y: meanSD body weight was Control: 8/54 (14.8%) after suture
prophylactic Intervention: 25.62 administered 1 minute P=0.031 removal or in
antibiotics 5 SD (17.5) after tourniquet inflation association with
minutes Control: 31.22 SD followed by 3 doses at Other infections: NR overt wound
before (20.6) 8 hour intervals during Topic-specific outcomes dehiscence. If a
exsanguinatio p=0.687 the initial postoperative Interval to wound healing, wound infection
n and inflation Gender: 76/106 period. weeks: meanSD was identified in
of the (71.7%) were male Timing of intervention: Intervention: 3.00.5 the
tourniquet but not reported intraoperative Control: 4.0 2.3 postoperative
(Intervention) which group Duration of intervention: P=0.002 period, a swab
and those Obesity: NR NA Reoperations: NR specimen of
administered Comorbidities: NR Device/agent: cefuroxime Length of stay: NR exudate was
prophylactic Monitoring intervention: Mortality: NR sent for
antibiotics 1 Procedures: NA Adverse events: NR microscopy,
minute after Open reduction internal Control group: n=54 culture and
inflation of the fixation 76/106 Intravenous cefuroxime at sensitivity testing
tourniquet (71.7%)) a dose appropriate to to guide
(control) in Intervention: 40/52 the patients age and subsequent
elective lower (74.1%) body weight was antibiotic
limb Control: 36/54 (69.2%) administered 5 minutes therapy.
orthopedic Soft tissue release: before tourniquet Wound healing: a
operations. 23/106 (21.7%) inflation followed by 3 well coated non-
Intervention: 11/52 doses at 8 hour tender wound
(20.4%) intervals during the with a linear scar
Control: 12/54 (23.1%) initial postoperative and no sign of
Triple arthrodesis 5/106 period. infection.
(4.7%) Perioperative care
Intervention: 2/52 Standard preventive Anesthesia: all
(3.7%) measures: patients
2017 American Medical Association. All rights reserved. 119
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Control: 3/54 (5.8%) All operations were underwent
Kellers operation 2/106 performed within 5 days general
(1.7%) of admission anesthesia
Intervention: 1/52 Tourniquet time (min) except for 2 who
(1.9%) meanSD had spinal
Control: 1/54 (1.9%) Intervention: 69.832.8 anesthesia
Indications: Control: 75.3 30.8 Eparch bandage
Tibial fracture 54/106 P=0.396 was used for
(50.9%) exsanguination
Intervention: 26/52 and the
(50%) tourniquet was
Control: 28/54 (51.9%) applied to the
Ankle fracture/ thigh in all cases
dislocation 22/106 Other notes:
(20.8%) Underpowered to
Intervention: 10/52 measure
(19.2%) infection rates
Control: 12/54 Follow-up: 12
(22.2%) months postop
Hallux valgus 2/106 Funding Source
(1.9%)) Conflicts:
Intervention: 1/52 Authors: NR
(1.9%) Institution: NR
Control: 1/54 (1.9%) Study: NR
Clubfoot 28/106 Supplies: NR
(26.4%)
Intervention: 15/52
(28.9%)
Control: 13/54 (24.1%)
Setting: 1 university
hospital
Location: Nigeria
Dates: February 2005
January 2006
Inclusion Criteria:
Patients who
underwent clean,
elective orthopedic
2017 American Medical Association. All rights reserved. 120
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
operations on the
lower limbs with the
use of a tourniquet
hemostasis.
Exclusion Criteria: NR
Soriano RCT To evaluate Number of patients: Intervention group: SSI Definitions:
2
2008 1, 3, 4, the N=908 n=466 NOTE: when an infection Deep tissue
(ES) 5, 10 importance of Patient Placebo administered 10- was suspected, the infection rate:
a tourniquet- Characteristics: no 30 minutes before patient underwent open CDC SSI
release dose, differences in inflation of the debridement Guideline
with a characteristics tourniquet and 1.5g of Total Deep SSI at 3 Criteria
randomized, between groups cefuroxime was months = 24/908 Perioperative
double-blind Age, y: meanSD administered 10 min (2.64%) care:
study of Intervention: 70.97.2 before release of the Intervention: 9/466 Anesthesia: spinal
primary total Control: 71.27.6 tourniquet. A (1.9%) Other notes:
knee Gender: female% postoperative dose of Control: 15/442 (3.4%) Sample size
arthroplasty Intervention: 73.6% 1.5g cefuroxime P=0.21 calculated from
performed Control: 76.5% administered at 6h after a previous deep
during Obesity: the end of the Total cumulative Deep SSI tissue infection
ischemia. Intervention: 37.8% procedure. at 12 months = 28/908 rate (4%) in the
Control: 35.5% (3.08%) institution.
Comorbidities Timing of intervention: Intervention: 12/466 Follow-up: 12
Diabetes mellitus intraoperative (2.6%) months post
Intervention: 14.6% Duration of intervention: Control: 16/442 (3.6%) discharge
Control: 18.3% NR P=0.44 Funding Source
Device/agent: 1.5g Conflicts:
Procedures: Total cefuroxime Other infections: NR Authors: None
knee arthroplasty Monitoring intervention Topic-specific Institution: NR
Indications: Control group: n=442 outcomes: Study: NR
Arthritis 1.5g cefuroxime MSSA SSI at 3 months = Supplies: NR
Intervention: 98.8% administered 10-30 9/24 (37.5%)
Control: 98.7% minutes before inflation Intervention: 3/9 (33.3%)
Rheumatoid arthritis of the tourniquet and Control: 6/15 (40%)
Intervention: 1.2% placebo was MSSA SSI between 4-12
Control: 1.3% administered 10 min months = 4/4 (100%)
before release of the Intervention: 3/3 (100%)
Setting: Single center tourniquet. A Control: 1/1 (100%)
Location: Spain postoperative dose of
2017 American Medical Association. All rights reserved. 121
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Dates: September 1.5g cefuroxime MRSA SSI at 3 months =
2004 December administered at 6h after 6/24 (25%)
2005. the end of the Intervention: 1/9 (11.1%)
Inclusion Criteria: procedure. Control: 1/15 (6.67%)
Patients undergoing MSSA SSI between 4-12
a primary total knee Standard preventive months = 0/4
arthroplasty who measures: Intervention: 0/3
signed the informed Laminar Air Flow: not used Control: 0/1
consent. Skin Prep: leg washed
Exclusion Criteria: with soap then with COPD with/without deep
Patients allergic to 10% povidone iodine tissue infection at 12
penicillin solution. months
Cement All prostheses Uninfected (n=880): 9.5%
cemented and none Infected (n=28): 21.4%
used antimicrobial P=0.05
impregnated cement.
Drains: 1 profound and 1 ASA Score 3-4 at 12
superficial drain tube months
left after closing the Uninfected (n=880): 129
wound were removed (14.8%)
within the first 48 hours Infected (n=28): 12
after the surgical (42.9%)
procedures P<0.001
Transfusion: during the
th
surgical procedure and Low 4 day hematocrit
the first 6h after the infection rate at 12
procedure, an RBC months
transfusion was given Uninfected (n=880):
when the hemoglobin 28.33.8
level was <9g/dL. After Infected (n=28): 26.54.1
this period, the P=0.02
threshold for RBC
transfusion was <8g/dL Reoperations: NR
Mean no of transfusions All deep prosthetic joint
SD infections included an
Intervention: 0.91.3 open debridement and
Control: 0.81.3 3 deep cultures of
Duration of ischemia: synovial fluid samples
(meanSD, min) and periprosthetic
2017 American Medical Association. All rights reserved. 122
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Intervention: 54.117.9 tissue samples from
Control: 53.918.3 different sites.
Length of stay, days:
meanSD
Intervention: 6.41.6
Control: 6.52.1
Mortality: NR
Adverse events: NR
eTABLE 26. Evidence Table for Q1B. What is the optimal timing of AMP in cesarean section: prior to skin incision or at cord
clamping?
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Osman RCT To investigate Number of patients: Intervention group: n=90 SSI: Definitions:
3
2013 1, 2, 3, the timing of N=180 Patients who received a Endometritis Post-operative
(ES) 4, 10 prophylactic Patient single intravenous Intervention: 0/90 febrile morbidity:
ceftizoxime for Characteristics injection of 1g Control: 0/90 an oral
elective Age, y, mean (SD) ceftizoxime 40 minutes Superficial wound temperature of
38 C on two
o
cesarean Intervention: 30.5 (7.4) pre-incision infection:
delivery at the Control: 32.2 (5.2) Timing of intervention: Intervention: 8/90 (6.7%) occasions at
study hospital. P=0.08 preoperative Control: 3/90 (3.3%) least 4 hours
Gender: all female Duration of intervention: P=0.2 (all incidences apart, excluding
Obesity: BMI, mean NA occurred post- the first 24h.
Calculated by Device/agent: 1g discharge) Postoperative
extractor from mean ceftizoxime infection
height & mean Monitoring intervention: Other infections: NR Endometritis: fever,
weight in study NA Topic-specific uterine
Intervention: 30.9 Control group: n=90 outcomes: tenderness, and
Control: 31.2 Patients who received a Neonatal outcomes abnormal lochia
P=0.1 single intravenous Admission to the nursery: Wound infection:
Comorbidities: NR injection of 1g Intervention: 15/90 fever, cellulitis &
2017 American Medical Association. All rights reserved. 123
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Gestational age, ceftizoxime post cord (16.7%) exudates
weeks: mean (SD) clamping Control: 15/90 (16.7%) Peritonitis: elevated
Intervention: 38.2 (1.1) Standard preventive P=0.1 temperature,
Control: 38.3 (0.9) measures : NR Jaundice tachycardia,
P=0.7 Intervention: 5/90 (5.5%) abdominal
Gravidity: mean (SD) Control: 4/90 (4.4%) distension and
Intervention: 3.5 (1.6) P=1.0 pain with
Control: 36.9 (0.4) Reoperations: NR guarding and
P=0.5 Length of stay: NR rigidity
Procedures: elective Mortality: NR aggravated by
cesarean section Adverse events: moving and
Indications: Skin rash breathing with
Repeated cesarean Intervention: 0/90 (0) absent bowel
delivery: Control: 1/90 (1.1%) sounds at the
Intervention: 55/90 P=1.0 onset of paralytic
(61.1%) ileus.
Control: 61/90 (67.8%) Perioperative
P=0.1 care: NR
Breech presentation: Other notes: study
Intervention: 10/90 was
(11.1%) underpowered
Control: 8/90 (8.9%) Follow-up: 6
P=0.6 weeks post op at
Hypertensive disorder clinic visit.
Intervention: 2/90 Funding Source
(2.2%) Conflicts:
Control: 1/90 (1.1%) Authors: None
P=0.5 Institution: NR
Bad obstetrics events Study: Industry
Intervention: 7/90 Supplies: NR
(7.8%)
Control: 11/90 (12.2%)
P=0.3
Others
Intervention: 16/90
(17.8%)
Control: 9/90 (10%)
P=0.1
2017 American Medical Association. All rights reserved. 124
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Setting: 1 university
hospital
Location: Sudan
Dates: May 2011
August 2011
Inclusion Criteria:
Patients who were
planned for elective
cesarean delivery
(e.g. repeated scars,
breech and low lying
placenta)
Exclusion Criteria:
Severe anemia,
twins, diabetes
mellitus, impaired
glucose test,
received antibiotics
within 2 weeks prior
to the operation, if
they had any visible
infection at any site
or elevated
temperature at the
time of the
operation; if they
were allergic to drug
used; or refusal to
participate in study
2017 American Medical Association. All rights reserved. 125
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Witt RCT To compare Number of patients: Intervention group: SSI: Definitions:
5
2011 1, 2, 3, the N=741 n=370 Local Wound Infection Wound infection:
(ES) 4, 5, 6, effectiveness Patient 2g of cefazolin mixed with (LWI), purulent
7, 8, 9 of cefazolin, a Characteristics 100mL saline Intervention: 9/370 discharge or
first- Age, y: mean (SD) administered 20-30 (2.4%) erythema (>1cm
generation Intervention: 31.3 (6.3) minutes before skin Control: 9/371 (2.4%) in diameter) and
cephalosporin, Control: 32.2 (5.8) incision Risk difference: 1.1%, induration of the
administered Gender: all female Timing of intervention: 95%CI (-1.8%-4.0%); incision site.
2
before skin Obesity: BMI (kg/m ), preoperative P=0.60 Urinary tract
incision vs. mean (SD) Duration of intervention: infection: if there
after umbilical Intervention: 28.3 (5.4) NA LWI during hospital stay were clinical
cord clamping Control: 28.3 (5.4) Device/agent: 2g Intervention: 6/370 symptoms (i.e.
vs. placebo in Comorbidities: cefazolin in 100mL (1.6%) polyuria and
a 3-arm Gestational diabetes saline Control: 8/371 (2.2%) dysuria) and a
randomized mellitus, Monitoring intervention: LWI at 3 weeks positive urine
trial of women Intervention: 39/370 NA postpartum dipstick nitrite
undergoing (10.5%) Control group: n=371 Intervention: 3/370 test result.
elective Control: 33/371 (8.9%) 2g cefazolin in 100mL (0.8%) Perioperative
cesarean History of allergy saline administered at Control: 1/371 (0.3%) care: delivery
delivery. Intervention: 27/370 cord clamping performed by
(17.3%) Standard preventive Endometritis: resident under
Control: 30/371 (8.1%) measures: NR Intervention: 1/370 the supervision
Immunosuppression, (0.3%) of fully trained
Intervention: 4/370 Control: 1/371 (0.3%) attending
(1.1%) Endometritis during physicians using
Control: 2/371 (0.5%) hospital stay a modified
Anticoagulation: Intervention: 0/370 Misgav Ladach
Intervention: 9/370 Control: 1/371 (0.3%) technique.
(2.4%) Endometritis at 3 weeks Other notes:
Control: 12/371 (3.2%) postpartum power
Intervention: 1/370 calculation
Procedures: elective (0.3%) demonstrated a
cesarean delivery. Control: 0/371 sample size of
Indications: NR 360 per arm for
Setting: 1 university Other infections: a power of 90%
hospital Urinary tract infection to detect an
Location: Austria (UTI), absolute
Dates: March 1, 2004 Intervention: 8/370 reduction of 5%
January 31, 2010 (2.2%) in primary
2017 American Medical Association. All rights reserved. 126
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Inclusion Criteria: Control: 4/371 (1.1%) outcome at
women undergoing UTI during hospital stay =0.05
cesarean delivery Intervention: 5/370 Follow-up: 30
with a gestational (1.4%) days postop via
age of at least 37 Control: 4/371 (1.1%) telephone
weeks and UTI at 3 weeks postpartum survey. If
reassuring fetal Intervention: 3/370 patients reported
heart traces. Women (0.8%) any of the signs
who experienced Control: 0/371 & symptoms of
rupture of an outcome
membranes and Topic-specific measure, they
labor contractions outcomes: were asked to
were also included Pelvic Abscesses report to the
Exclusion Criteria: Intervention: 1/370 clinic for
o
fever >38 C, (0.3%) confirmation
cephalosporin Control: 1/371 (0.3%) Funding Source
allergy, age <18 Conflicts:
years, and exposure Neonatal Outcomes: Authors: NR
to any antibiotic showed no statistically Institution: NR
agent within 1 week significant difference Study: NR
before delivery. between groups (data Supplies: NR
not shown)
Reoperations: NR
Length of stay days:
mean (SD),
Intervention: 5.5 (1.6)
Control: 5.5 (1.9)
Mortality: NR
Adverse events: NR
Macones RCT To compare Number of patients: Intervention group: NOTE: study reported Definitions:
4
2011 1, 2, 3, maternal and N=434 n=217 percentages only. Maternal infectious
(ES) 4, 5, 6, neonatal Patient 1 g Cefazolin given <30 Numerators were morbidities: (1)
9 outcomes in Characteristics: minutes prior to skin calculated by postoperative
women who both groups were incision. extractor: fever (defined as
o
receive similar with respect Timing of intervention: oral temp >38 C
prophylactic to baseline preop SSI: on two separate
antibiotics demographics Duration of intervention: Wound infection: occasions more
2017 American Medical Association. All rights reserved. 127
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
prior to skin Age, y: mean NA Intervention: 0.5% than 6h apart,
incision with Intervention: 28.9 Device/agent: 1 g (1/217) after the initial
those who Control: 28.3 cefazolin Control: 1.4% (3/217) 24h postop
receive P=0.27 Monitoring intervention: RR: 2.8 (0.7-4.2), P=0.37 period); (2)
antibiotics at Gender: all females NA wound infection
cord clamping Obesity: Control group: n=217 Endometritis (defined as
Not reported but cited 1g Cefazolin given at cord Intervention: 2.8% purulent
as similar at baseline clamping (6/217) discharge from
Comorbidities: NR Standard preventive Control: 2.8% (6/217) the incision); (3)
African American race: measures: RR: 1.0 (0.7-1.3), P=1.00 endomyometritis
Intervention: 65.3% Antimicrobial prophylaxis: (defined as
(142/217) patients received 1g fundal
Control: 64.7 cefazolin. If allergic to Other infections: tenderness and
(140/217) penicillin, they received Urinary Tract Infection: fever); (4)
P=0.99 900mg clindamycin. Intervention: 0.9% urinary tract
Gravidity: mean Cefazolin: (2/217) infection
Intervention: 3.5 Intervention: 90.2% Control: 0.9% (2/217) (defined as
Control: 3.3 (196/217) RR: 1.0 (0.3-4.0), P=1.00 fever, positive
P=0.17 Control: 92.1% (200/217) urine culture).
Gestational Age, P=0.71 Topic-specific
weeks: mean outcomes: Perioperative
Intervention: 38.7 Fever: care:
Control: 38.9 Intervention: 2.3% Patients were
P=0.70 (5/217) managed in the
Control: 3.7% (8/217) postpartum
Procedures: RR: 1.6 (0.8-2.2), P=0.42 period at the
Scheduled cesarean discretion of
Intervention: 73.4% Neonatal outcomes: treating
(159/217) NICU Admission physicians.
Control: 71.4% Intervention: 3.5% Regional
(155/217) (8/217) Anesthesia
P=0.62 Control: 4.0% (9/217) Intervention:
Low transverse RR: 1.1 (0.7-1.8) 92.1% (200/217)
cesarean Suspected sepsis Control: 90.6%
Intervention: 95.4% Intervention: 8.9% (197/217)
(207/217) (19/217) P=0.88
Control: 95.4% Control: 8.9% (19/217)
(207/217) RR: 1.0 (0.7-1.3) Other notes: 217
P=1.00 subjects per arm
2017 American Medical Association. All rights reserved. 128
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
was calculated
Indications Reoperations: NR to see a
Setting: 2 university Length of stay: NR decrease in the
hospitals Mortality: NR composite
Location: USA Adverse events: NR maternal
Dates: NR infectious
Inclusion Criteria: morbidity rate of
those undergoing 10% in the cord
nonemergency clamp group
cesarean surgery at (based on pilot
36 weeks gestation data), with type I
or greater. error of 0.05,
(Pregnancies were type II error of
dated by best 0.20.
obstetric estimate
using standard Follow-up: in the
criteria.) hospital and
Exclusion Criteria: postpartum stay.
known fetal Funding Source
anomaly, exposure Conflicts:
to antibiotics within 7 Authors: NR
days of admission Institution: NR
(including Study: NR
intrapartum Group B Supplies: NR
Streptococcus
prophylaxis), need
for emergency
cesarean delivery
(i.e. for category III
electronic fetal
monitoring, maternal
distress, obstetric
hemorrhage),
rupture of
membranes >18h,
and overt maternal
intrapartum infection
requiring antibiotics.
2017 American Medical Association. All rights reserved. 129
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Yildirim RCT The aim was Number of patients: Intervention group: SSI: Definitions :
6
2009 1, 7, 8, to determine N=389 n=194 Wound infection: Elective cesarean
(ES) 9 whether the Patient Characteristics: 1g cefazolin sodium Intervention: 6/194 section:
timing of no significant administered 10-45min (3.1%) Cesarean
prophylactic differences in prior to skin incision. Control: 8 (4.1%) section
antibiotics at demographics Timing of intervention: P = 0.59 performed
cesarean between groups preop RR: 1.34, 95%CI (0.45- before the
delivery Age, y: mean SD Duration of intervention: 3.93) presence of
influences Intervention: NA Endometritis: labor
maternal and 28.254.87 Device/agent: 1g Intervention: 5/194 Wound infection:
neonatal Control: 27.535.02 cefazolin sodium (2.6%) signs of
infectious P=0.15 Monitoring intervention: Control: 7/195 (3.6%) erythema,
morbidity. Gender: all female NA P = 0.56 swelling,
2
Obesity: BMI (kg/m ): Control group: n=195 RR: 1.40, 95%CI (0.43- discharge or
mean SD 1g cefazolin sodium was 4.51) tenderness
Intervention: administered after Urinary tract
31.982.89 clamping of the Other infections: infection: clinical
Control: 31.962.29 umbilical cord. Urinary Tract Infections: signs were
P=0.93 Intervention: 3/194 checked and a
Comorbidities Standard preventive (1.5%) urinalysis was
Gravidity: meanSD measures Control: 5/195 (2.6%) performed.
Intervention: Antibiotic prophylaxis: 1 g P = 0.47 Neonatal sepsis:
2.571.05 of cefazolin sodium was RR: 1.67, 95%CI (0.39- suspected if
Control: 2.451.05 used for antibiotic 7.11) tachycardia
P=0.25 prophylaxis. No other and/or
Parity: meanSD antimicrobial Topic-specific tachypnea as
Intervention: prophylaxis was outcomes: well as an
1.140.67 administered unless a Postoperative hematocrit increased white
Control: 1.110.68 postoperative infection level, %: meanSD, count with bands
P=0.59 was diagnosed. Intervention: 30.170.97 was present and
Gestational Age at Catheter: a foley catheter Control: 30.040.92 was confirmed
delivery: meanSD, was inserted pre- P=0.18 by positive
weeks cesarean section and Postoperative hemoglobin culture.
Intervention: removed postop. level, (g/l): meanSD Perioperative
38.320.94 Skin prep the abdomen Intervention: 9.910.50 care: NR
Control: 38.240.69 was cleaned with a Control: 9.780.59 Other notes:
P=0.31 povidone iodine P=0.02 Prior to this study,
solution. Estimated blood loss, (ml): the institution
Procedures: elective Incision: Pfannistiel meanSD had a 20%
2017 American Medical Association. All rights reserved. 130
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
cesarean section incisions were done on Intervention: postcesarean
Indications: indications all patients, followed by 656.29190.54 endometritis
for cesarean section transverse lower uterine Control: 668.92203.57 rate.
were similar when segment incision and P=0.52 Study power. A
the two groups were delivery of the fetus and Operative time, (min): sample size of
compared placenta. meanSD 197 was
Previous cesarean, Closure: suturing of the Intervention: 36.632.66 calculated to
Intervention: 168 uterine incision was Control: 37.123.89 provide 80%
(86.6%) performed without P=0.14 power to detect
Control: 173 (88.7%) exteriorization of the a 50% difference
Multiple pregnancy uterus. The abdominal Neonatal outcomes: in postoperative
Intervention: 5 (2.6%) wall was closed in two Intervention: n=201 infections, with
Control: 5 (2.6%) layers then skin Control: n=198 =0.05
Fetal macrosomia incisions were closed. Birth weight, (g): Follow-up: 6
(>4500g) meanSD weeks postop
Intervention: 8 (4.1%) Intervention: Funding Source
Control: 6 (3.1%) 3263.75505.86 Conflicts:
Breech and Control: 3232.92500.26 Authors: None
malpresentation, P=0.53 Institution: None
Intervention: 13 5-minute Apgar score: Study: None
(6.7%) meanSD Supplies: None
Control: 10 (5.1%) Intervention: 9.080.71
Placenta previa Control: 9.060.78
Intervention: 0 P=0.79
Control: 1 (0.5%) Neonatal Sepsis:
Intervention: 9/201
Setting: 1 tertiary care (4.4%)
hospital Control: 13/198 (6.3%)
Location: Turkey P = 0.38
Dates: June 2007 RR: 1.47 (0.61-3.53)
December 2007 NICU Admission
Inclusion Criteria: Intervention: 4/201 (2%)
Women undergoing Control: 7/198 (3.4%)
elective cesarean P = 0.35
section at the RR: 1.77 (0.51-6.16)
hospital without Sepsis workup:
exclusion criteria Intervention: 23/201
Exclusion Criteria: (11.2%)
use of antibiotics Control: 30/198 (14.6%)
2017 American Medical Association. All rights reserved. 131
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
during the last 24h, P = 0.30
pathology that RR: 1.35 (0.75-2.42)
should be treated NICU Length of Stay,
with antibiotics, pre- days: meanSD
existing maternal Intervention: 8.252.62
diseases (such as Control: 5.662.58
diabetes, collagen P=0.16
vascular disease,
immune system Reoperations: NR
problems), Length of stay, days:
chorioamnionitis, meanSD
fever on admission, Intervention: 2.301.09
need of transfusion Control: 2.391.18
before or during the p=0.46
cesarean section,
ruptured Mortality: NR
membranes, Adverse events:
emergency cesarean There were no serious
section, and pre- side effects related to
term cesarean the use of cefazolin.
section.
Sullivan RCT To conduct a Number of patients: Intervention group: SSI: (Follow up 6 weeks) Definitions:
8
2007 1, 2, 3, prospective, N=357 n=175 Wound Infections Endomyometritis:
(ES) 4, 5, 6, double-blind, Patient Received 1gm cefazolin Intervention: 5/175 (3%) maternal fever
7, 8, 9, randomized Characteristics: No mixed with 50 cc Control: 10/182 (5%) greater than
o
10 clinical trial to significant normal saline 15-60 Relative Risk (95% CI) 100.4 F on 2
determine differences found minutes prior to 0.52 (0.18-1.5) separate
whether between groups. incision. Placebo (50 cc P>0.05 occasions along
antibiotic Age, y: mean normal saline) Adjusted OR (95% CI) with uterine
prophylaxis Intervention: administered at cord 0.4 (0.1-1.3) fundal
administered 28.36.1 clamp Endomyometritis tenderness,
preoperatively Control: 28.36.0 Timing of intervention: Intervention: 2/175 (1%) tachycardia or
is more Gender: All Female Pre and Intraoperative Control: 10/182 (5%) leukocytosis.
effective in Obesity (Maternal Duration of intervention: Relative Risk (95% CI) Wound Infection:
preventing Weight) mean SD preoperative 0.2 (0.2-0.94) purulent
infectious Intervention: (Intervention) and P<0.05 discharge,
morbidity 225.3144.5 Intraoperative (Control) Adjusted Odds Ratio erythema, and
following Control: 228.1152.9 Device/agent: Cefazolin (95% CI) induration of the
cesarean Comorbidities: Monitoring intervention: 0.22 (0.05-0.9) incision site.
2017 American Medical Association. All rights reserved. 132
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
delivery than Diabetes NR Total Infectious Morbidity Hematomas,
administration Intervention: 17/175 Control group: n=182 Intervention: 8/175 seromas, or
following cord (10%) Received placebo (50 cc (4.5%) wound
clamp. Control: 29/182 normal saline) 15-60 Control: 21/182 (11.5%) breakdowns: in
(16%) min prior to incision. Relative Risk (95% CI) the absence of
Preeclampsia 1gm cefazolin mixed 0.4 (0.18-0.87) previously
Intervention: 18/175 with 50 cc normal saline Statistically significant discussed signs
(10.3%) administered at the time Adjusted OR (95% CI) were not
Control: 25/182 of cord clamping. 0.35 (0.14-0.82) considered
(13.7%) Standard preventive wound
Operative Time, min: measures: NR Other infections: infections.
mean SD Pyelonephritis: 1 case in Neonatal Sepsis:
Intervention: intervention group. diagnosed by a
43.513.6 Pneumonia: 1 case in positive blood
Control: 4814.9 control group culture.
Parity: mean Topic-specific Perioperative
Intervention: 1.4 outcomes: care: NR
Control: 1.2 Neonatal outcomes Other notes:
Premature delivery Sepsis Weakness of
(<37wks): Intervention: 6/185 (3%) this study is the
Intervention: 30/175 Control: 7/194 (3.6%) high-risk nature
(17%) Suspected sepsis of the study
Control: 46/182 Intervention: 35/185 population. They
(25%) (19%) were more
Procedures: Cesarean Control: 36/194 (18.5%) obese, more
Section Delivery; No difference in causative likely to have
Performed by organisms or increased diabetes,
resident physicians incidence of antibiotic preterm delivery,
as primary surgeons resistant organisms. multiple
which resulted in NICU Admission gestation and be
increased average Intervention: 25/175 of minority
surgery time (14.3%) ethnicity than
Control: 33/182 (18.3%) the general
Indications: P=0.40 population. The
Arrest disorders NICU Days: meanSD location of the
Intervention: 50/175 Intervention: 14.215.8 trial was in a
(28.6%) Control: 19.724.9 tertiary care
Control: 53/182 P=0.01 center.
(29.1%) No statistical difference in Follow-up:
2017 American Medical Association. All rights reserved. 133
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Non-reassuring fetal terms of birth weight, Through their
status gestational age, septic hospital course
Intervention: 36/175 workup, intermediate and up to the 6-
(20.6%) admission, NICU week
Control: 39/182 admission, length of postpartum visit.
(21.4%) stay or pH<7.1 Funding Source
Not laboring Reoperations: NA Conflicts:
Intervention: 51/175 Length of stay: NR Authors: None
(29.1%) (NICU, see above) Institution: None
Control: 44/182 Mortality: NR Study: None
(23.8%) Adverse events: No Supplies: None
Other cases of maternal
Intervention: 38/175 anaphylaxis or other
(21.7%) adverse events related
Control: 45/182 to cefazolin use
(24.7%) reported during the trial.
Setting: 1 Tertiary Hematomas & Seromas
Care Hospital that did not meet
Location: USA criteria for wound
Dates: NR (26 months infections: 7 cases total
total)
Inclusion Criteria:
Women whose
pregnancies were
older than 24 weeks
estimated
gestational age and
required cesarean
delivery
Exclusion Criteria:
cephalosporin
allergy, gestational
age less than 18
weeks, exposure to
any antibiotic agent
within 1 week of
delivery, or the need
for emergent
cesarean delivery.
2017 American Medical Association. All rights reserved. 134
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Thigpen RCT To determine Number of patients: Intervention group: SSI: (follow up 6 weeks) Definitions:
7
2005 1, 2, 3, if the N=302 n=153. Received 2g Wound Infection: Endometritis:
(ES) 4, 5, 6, administration Patient cefazolin in fluid just Intervention: 6/153 Maternal
7, 8, 9 of prophylactic Characteristics: No before skin incision and (3.9%) temperature
100.4 F on 2
o
antibiotics for significant statistical placebo at cord Control: 8/149 (5.4%)
cesarean difference existed in clamping RR (95% CI): 0.84 (0.45- separate
section at the baseline Timing of intervention: 1.55) occasions 6
time of cord characteristics pre and intraoperatively Not statistically hours apart
clamping, as between groups Duration of intervention: significant exclusive of the
opposed to Age, y: meanSD preoperative Endometritis first 12 hours
immediately Intervention: 23.55.7 (intervention) and Intervention: 12/153 following
before the skin Control: 24.35.9 intraoperative (at (7.8%) surgery,
incision, Gender: 100% Female clamping) Control: 22/149 (14.8%) accompanied by
influences the Obesity: NR Device/agent: Cefazolin RR (95% CI): 0.67 (0.42- uterine
incidence of Comorbidities: NR Monitoring intervention: 1.07) tenderness and/
maternal Time after ruptured NR Not statistically or purulent or
infectious membranes, h: Control group: n=149 significant foul smelling
morbidity and/ meanSD Received placebo just lochia.
or negatively Intervention: 7.25.8 before skin incision and ITT Analysis Wound infection:
impacts upon Control: 8.66.4 2g cefazolin in fluid at Maternal infection: with or without
the neonatal P=0.045 cord clamping RR (95% CI): 0.81 (0.52- an elevated
course. Gestational age at Standard preventive 1.40) maternal
delivery, nulliparity measures: temperature,
and history of ABX: Other infections: No accompanied by
previous cesarean Group B Streptococcal cases of maternal tenderness with
delivery, need for ABX Pneumonia or wound
cervical ripening, Intervention: 27/153 Pyelonephritis. dehiscence,
induction, cervical (17.6%) Topic-specific breakdown of
exam on admission, Control: 40/ 149 (26.8%) outcomes: the surgical
cervical dilatation RR (95% CI): 0.74 (0.55- Neonatal morbidity edges, and/ or
was similar. 1.03) No statistically significant purulent
Procedures: Cesarean No other antibiotics were difference between the drainage
section delivery given unless a two groups (birth Urinary tract
Indications: postoperative infection weight, Apgars, UaPh, infection:
Arrest disorder was diagnosed. NICU admissions, Maternal
Intervention: 86/153 sepsis or sepsis temperature
100.4 F on 2
o
(56.2%) workup, or maternal
Control: 91/149 comorbidities or separate
(61.1%) contributing factors. occasions 6
2017 American Medical Association. All rights reserved. 135
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Fetal Distress Infection: hours apart
Intervention: 17/153 Intervention: 20/153 exclusive of the
(11.1%) (13.1%) first 12 hours
Control: 18/149 Control: 21/149 (14.1%) following
(12.1%) RR (95% CI): 0.96 (0.68- surgery, with a
Other 1.34) positive urine
Intervention: 50/153 Sepsis culture,
(32.7%) Intervention: 7/153 abnormal
Control: 40/149 (4.6%) urinalysis, and
(26.8%) Control: 7/149 (4.7%) flank pain.
P=.541 RR (95% CI): 0.96 (0.58- Pneumonia:
1.69) hyperpyrexia, as
Setting: 1 Regional Suspected sepsis well as x-ray and
Medical center Intervention: 11/153 physical
Location: USA (7.2%) examination
Dates: NR (30 month Control: 14/149 (9.4%) findings
period) RR (95% CI): 0.76 (0.47- consistent with
Inclusion Criteria: 1.22) lung
Singleton Pneumonia consolidation.
pregnancies if the Intervention: 1/153 Neonatal Sepsis:
patient had labored (0.7%) Suspected if
and required Viral Syndrome tachycardia and/
cesarean surgery. Intervention: 1/153 or tachypnea, as
Group B Strep (0.7%) well as an
prophylaxis Pyelonephritis: none increased white
(aqueous penicillin) NICU Admission count with
was allowed. Intervention: 14/153 bands, was
Exclusion Criteria: (9.2%) present and was
Multiple Control: 8/149 (5.4%) confirmed by
pregnancies, acute RR: 1.28, 95%CI (0.91- positive blood
chorioamnionitis, 1.79) cultures.
allergy to penicillin or Reoperations: NA Perioperative
cephalosporins, Length of stay: NR care: Most
cesarean section women had
without labor, or the Mortality: NR regional
administration of Adverse events: NR anesthesia.
systemic antibiotics General Anesthesia
within the past 2 Intervention:
weeks. 16/153 (10.5%)
2017 American Medical Association. All rights reserved. 136
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Control: 17/ 149
(11.4%)
RR (95% CI):
0.95 (0.66-1.38)
Other notes:
Prospective
power analysis
performed for
risk of
endometritis and
wound infection
determined that
270 women in
each arm were
sufficient (power
0.80) to detect
10% difference.
(Based on
projected 10%
risk of infection
in post-cesarean
population). An
interim analysis
was planned for
the power
analysis
because the
investigation
was not
concluded near
the completion
(4 months) of the
fellowship of the
senior author.
The interim
power analysis
indicated that
with the rate of
infection being
2017 American Medical Association. All rights reserved. 137
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
50% more than
expected for the
2 groups, there
was an 80%
power to detect
a difference with
a total of 300
randomized
women.
Follow-up: For 6
weeks
postpartum.
Funding Source
Conflicts:
Authors: NR
Institution: NR
Study: NR
Supplies: NR
Wax RCT To test the Number of patients: Intervention group: n=49 SSI (follow up 2 & 6 Definitions:
9
1997 1, 2, 3, hypothesis N=90 1g cefazolin in 50 ml 0.9% weeks) Endometritis: Fever
o
(ES) 4, 5, 6, that a single 1 Patient saline administered Wound infection: to 100.4 F on 2
7, 8, 9, g dose of Characteristics: within 5 min of deciding Intervention: 1/49 (2%) occasions at
10 cefazolin Patients were similar to proceed with Control: 2/41 (4.9%) least 6h apart or
administered between groups with cesarean delivery. The P=0.35 a single fever
101 F outside
o
preoperatively regards to: placebo of 50 ml 0.9% Endometritis:
is no more Maternal Age, y: saline was administered Intervention: 1/49 (2%) the first 24h
effective than meanSD over 5 minutes at cord Control: 1/41 (2.4%) following
one Intervention: 24.74.5 clamping 1 subject in Intervention delivery
administered Control: 25.24.8 Timing of intervention: group experienced both associated with
after cord Gender: 100% Female Pre and intraoperatively endometritis and wound uterine or
clamping in Obesity: Duration of intervention: infection. parametrial
preventing Weight: meanSD Intra and Other infections: No tenderness,
post-cesarean Intervention: 19126 postoperatively secondary infections malodorous or
infections lb. Device/agent: Cefazolin were seen in either purulent lochia,
Control: 18932 lb. Monitoring intervention: group or leukocytosis
Comorbidities: NR NR Topic-specific Wound infection:
Duration of labor Control group: n=41 outcomes: Incisional
meanSD 50 ml 0.9% saline was Neonatal Morbidity: erythema,
Intervention: 13.07.2 administered within 5 Pneumonia: tenderness,
2017 American Medical Association. All rights reserved. 138
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
h minutes of deciding to Intervention: 2/49 (4.1%) warmth, with or
Control: 9.97.3 h proceed with cesarean Control: 0/41 without purulent
P=0.03 delivery. The 1.g of Febrile illness drainage.
Duration of internal cephazolin in 50 ml readmissions Intra-abdominal
monitors meanSD 0.9% saline was Intervention: 2/49 (4.1%) abscesses,
Intervention: 11.14.2 administered over 5 Control: 0/41 septic pelvic
h minutes at cord No source of infection thrombophlebitis
Control: 9.34.7 h clamping. was identified in either , or symptomatic
P=0.04 Standard preventive neonate Treatment: urinary tract
Newborn 1 and 5 measures: Both discharged after infection: ND
minute Apgar AMP: Time from first receiving 72h of Neonatal
scores<7, umbilical infusion to incision antibiotics and no Outcomes:
arterial cord (min) mean SD further sequelae Sepsis screen,
pH<7.20 and NICU Intervention: 3531 Suspected Sepsis workup: sepsis,
admissions similar Control: 3626 Intervention: 6/49 pneumonia
between two groups (12.2%) (based on
Procedures: (not Skin prep: All patients Control: 2/41 (4.9%) clinical and
statistically received identical skin P=0.28 radiographic
significant between prep of iodophor and Workup was negative in findings), and
groups) isopropyl alcohol. all meningitis: ND
Primary: 61/90 (67.8%) Surgical Drape: Occlusive Meningitis: none Perioperative
Primary w/ tubal adhesive surgical Delayed onset or partially care:
ligation: 5/90 (5.6%) drapes were used for treated infections Indwelling catheter:
Repeat: 18/90 (20%) each case. 2weeks: 84 infants : placed
Repeat with tubal Nonstandard preventive none preoperatively
ligation: 6/90 (6.7%) measures: 6 weeks: 76 infants: for bladder
All procedures were Technique: Intraoperative none drainage.
performed by surgical technique was Other notes: None
residents under the determined by surgeon Reoperations: NA Follow-up:
supervision of attending Length of stay: NR Mothers were
physicians. Mortality: NR counseled
Indications: Adverse events: None verbally and
Arrest of dilation or reported for mothers or given written
descent: infants. instructions
Intervention: 30/49 describing signs
(61.2%) of infection
Control: 20/41 before leaving
(48.8%) the hospital and
Fetal Distress scheduling
2017 American Medical Association. All rights reserved. 139
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Intervention: 3/49 follow-up.
(6.1%) Mothers were
Control: 9/41 (22.0%) contacted by
P=0.03 phone or seen in
Malpresentation clinic at 2weeks
Intervention: 4/49 (n=83/90; 11 by
(8.2%) phone and 72 in
Control: 6/41 (14.6%) clinic) and 6
Repeat in labor weeks (n=76/90;
Intervention: 4/49 5 by phone and
(8.2%) 71 in clinic_ after
Control: 5/41 (12.2%) delivery.
Other Infants were
Intervention: 8/49 examined by a
(16.3%) pediatrician 2
Control: 1/41 (2.4%) weeks post-
P=0.03 partum. Mothers
Setting: 1 Military were interviewed
Hospital and infant charts
Location: USA reviewed at 6
Dates: NR (12 month weeks of life.
period) Funding Source
Inclusion Criteria: Conflicts:
Singleton subjects Authors: None
undergoing Institution: None
cesarean delivery at Study: None
37 week gestation. Supplies: None
Exclusion Criteria:
Penicillin or
cephalosporin
allergy, antibiotic use
within 2 weeks of
delivery,
temperature 37.8 C
o
in labor,
administration of
group B
streptococcal or sub-
acute bacterial
2017 American Medical Association. All rights reserved. 140
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
endocarditis
prophylaxis during
labor, insulin-
dependent diabetes
mellitus, human
immunodeficiency
virus infection,
chronic
glucocorticoid use,
or multiple gestation.
Q1C. How safe and effective is weight-adjusted AMP dosing? Our search did not identify RCTs or SRs that evaluated weight-adjusted AMP dosing
and its impact on the risk of SSI.
2017 American Medical Association. All rights reserved. 141
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
eTABLE 27. Evidence Table for Q1D. How safe and effective is intraoperative redosing of AMP?
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Cuthbert- RCT To determine Number of patients Intervention group: SSI: Definitions:
son 1, 2, 4, whether a N=278 n=132 Intra-abdominal Wound infection: if
10
1991 7 double dose of Patient Patients who received 2 abscess: there was a
(ES) intravenous Characteristics: doses of 3.1g of 2doses: 10/132(8%) purulent
Timentin there were no timentin. 1 1dose: 8/146 (5%) vs. discharge from
provides statistically intravenously just Perineal wound the suture line or
superior significant before incision the infection: if there was a
prophylaxis differences between other, 2 hours after the 2doses: 4/9 non-purulent
with respect to groups. beginning of the 1dose: 4/9 discharge that
postoperative Age: NR operation. Antimicrobial contained
wound Gender: NR Timing of intervention: Resistance: pathogenic
infection Obesity: NR pre and intra/post op No difference: 1 minor SSI bacteria.
compared with Comorbidities: NR Duration of intervention: in each group culture
a single dose, Procedures: 2h after the beginning positive for MRSA as Perioperative
they Abdominal of the operation. the sole organism care: NR
performed a operations where the Device/agent: Timentin Other notes: None
controlled bowel was opened. 3.1g Follow-up: 30
clinical trial in Setting: 11 hospitals Control group: n=146 days
patients Location: Australia Patients received a single Funding Source
undergoing Dates: NR dose of timentin of 3.1g Conflicts:
elective Inclusion Criteria: intravenously just Authors: NR
colorectal patients undergoing before incision. Institution: NR
surgery. elective abdominal Standard preventive Study: NR
operations in which measures: The bowel Supplies: NR
the bowel was was mechanically
opened. cleansed preoperatively
Exclusion Criteria: and no oral
Patients known to be antimicrobials were
allergic to penicillin administered.
or who had received
antimicrobials in the
72 hours before their
planned operation.
Patients were
excluded if the large
bowel was not
opened at operation,
2017 American Medical Association. All rights reserved. 142
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
if intra-abdominal
pus was found at
operation, if a stoma
or mucous fistula
was brought out
through the main
abdominal wound
and/or if the main
abdominal wound
was not closed
primarily.
2017 American Medical Association. All rights reserved. 143
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
eTABLE 28. Evidence Table for Q1E. How safe and effective is postoperative AMP and what is the optimal duration?
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Hirokawa RCT To evaluate Number of patients: Intervention group: n=94 SSI: Definitions:
54
2013 1, 2, 6, the necessity N=190 Flomoxef sodium (FMOX) SSI: Combined SSI and
(ES) 7, 8, 9, of Patient 1.0g was given 30 Intervention: 7/94 (7.5%) remote infection.
10 postoperative Characteristics: the minutes before the Control: 13/94 (13.8%) SS (secondary
antibiotic two groups were operation and every 3 P=0.24 outcome): a
prophylaxis matched for hours during the Superficial/deep incisional condition in
after liver characteristics operation. Intervention: 3/94 (3.2%) which purulent
resection Age, y: median (range) Timing of intervention: Control: 3/94 (3.2%) discharge was
without Intervention: 68 (35- Preoperative P=1.000 observed from
reconstruction 82) Duration of intervention: Organ/space any incision or
of the intestine Control: 68 (22-88) NA Intervention: 4/94 (4.3%) space that was
or biliary tract. Gender: m:f Device/agent: 1.0g Control: 11/94 (11.7%) manipulated
Intervention: 64:30 flomoxef sodium P=0.10 during operation
Control: 30:34 administered <30 days after
Obesity intravenously Other infections surgery with or
Comorbidities: Monitoring intervention: Remote site infections without
Virus infection: NA Intervention: 2/94 (2.1%) microbiologic
Intervention: 42/94 Control group: n=94 Control: 8/94 (8.5%) evidence, per
(44.7%) Flomoxef sodium (FMOX) P=0.10 the guidelines
Control: 29/94 (30.9%) 1.0g was given 30 Topic-specific issued by the
minutes before the outcomes: NA CDC.
Procedures: Liver operation and every 3 Reoperations: NR Remote site
resection hours during the Length of stay: infection: a
Primary hepatectomy: operation then every 12 Postoperative hospital condition in
Intervention: 9/94 hours for 3 days after stay, days: median which fever and
(9.6%) the operation. (range) leukocytosis
Control: 17/94 (22.1%) Standard preventive Intervention: 12 (4-91 were present
P-0.14 measures: Control: 14 (5-265) with bacteria in
Hemiheptaectomy: Surgery: performed P=0.034 sputum, urine,
Intervention: 28/94 according to standard catheter tip,
(29.8%) techniques: Mortality: blood, or bile
Control: 24/94 (25.5%) Cavity Irrigation: Intervention: 1/94 (1.1%) juice or
Segmentectomy: abdominal cavity was Control: 1/94 (1.1%) according to the
Intervention: 27/94 irrigated 4L of warm physicians
(28.7%) saline. Adverse events: NR judgment
Control: 22/94 (23.4%) Drains: not inserted regardless of
Limited resection: Blood transfusion: carried microbiologic
Intervention: 39/94 out when surgical evidence.
2017 American Medical Association. All rights reserved. 144
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
(41.5%) bleeding >1000m and Signs of infection
Control: 48/94 (51.1%) hemoglobin level (Primary
decreased to <8.0 g/dL Outcome):
Indications: postoperative
Hepatocellular status with 1 of
Carcinoma: the following
Intervention: 44/94 inflammatory
(46.8%) findings after
Control: 44/94 (46.8%) postoperative
Cholangiocellular day (POD) 4: (1)
carcinoma: body
Intervention: 3/94 temperature
38 C; (2) white
o
(3.2%)
Control: 4/94 (4.3%) blood cell count
12,000/mm ;
3
Colorectal metastasis:
Intervention: 42/94 and (3)
(44.7%) additional
Control: 37/94 (39.4%) increase (>20%
Living-donor liver increase from
transplantation: the previous
Intervention: 1/94 value) in white
(1.2%) blood cell count
Control: 4/94 (4.3%) and/or C-
reactive protein.
Setting: 1 University Perioperative
Medical Hospital care: NR
Location: Japan Other notes: None
Dates: April 2008 Follow-up: NR
June 2011 Funding Source
Inclusion Criteria: Conflicts:
patients from 18-90 Authors: None
years and adequate Institution: None
organ functional Study: None
reserve of important Supplies: None
organ systems
(heart, lungs,
kidneys, and liver
[Child-Pugh class A
or B])
2017 American Medical Association. All rights reserved. 145
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Exclusion Criteria: (1)
severe
comorbidities, such
as preoperative
infection,
hemodialysis,
myocardial
infarction, or
respiratory disorders
requiring oxygen
inhalation; (2)
concomitant
operations on other
organs, including
biliary or digestive
tract anastomosis;
(3) proven mental
illness; and (4)
absences of
informed consent.
Lyimo RCT To determine Number of patients: Intervention group: SSI: Definitions:
30
2013 1, 4, 7, the N=500 n=250 Total Surgical Site Infection: presence
(ES) 8, 9, 10 equivalence of Patient Patients received a single Infection: of fever (temp
o
intravenous Characteristics: intravenous dose of Intervention: 12/250 >38 C at least 4
single dose of patients in both gentamicin(3mg/Kg) (4.8%) [95%CI 2.2-7.4] hours apart on
gentamicin groups were similar plus metronidazole Control: 16/250 (6.4%) two or more
(3mg/kg) plus at baseline. (500mg) 30 60 Absolute difference occasions,
metronidazole Age minutes before (95%CI): 1.6% (-2.4- excluding the
(500mg) given 20 y: operation 5.6%) [95%CI 3.4-9.4] first 24h post
30 60 min Intervention: 38/250 Timing of intervention: Incidence rates of post cesarean.)and
before incision (15.2%) preoperative cesarean infections signs and
and multiple Control: 42/250 Duration of intervention: Intervention: 1.7/ 1000 symptoms of
doses of (16.8%) NA person days abdominal
gentamicin 21-30 y: Device/agent: Gentamicin Control: 2.3 / 1000 wound infection
(3mg/kg) and Intervention: 146/250 (3mg/Kg) plus person days or endometritis
metronidazole (28.4%) metronidazole (500mg): Incidence rate ratio = Abdominal wound
(500mg) given Control: 135/250 Monitoring intervention: 0.74 995%CI 0.32- infection: partial
both 30-60 (54.0%) NA 1.65), p=0.2146 or total
min before >30 y: Control group: n=250 Other infections: NR dehiscence,
2017 American Medical Association. All rights reserved. 146
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
incision and Intervention: 66/250 3 doses - Patients Topic-specific presences of
followed by (26.4%) received a dose of outcomes: NR purulent or
gentamicin Control: 73/250 gentamicin (3mg/Kg) Reoperations: NR serous
(3mg/kg) once (29.3%) plus metronidazole Length of stay: NR discharge form
a day and Gender: 100% female (500mg) 30 60 Mortality: NR the wound with
metronidazole Obesity: minutes before Adverse events: NR indurations,
(500mg) every Intervention: 83/250 operation followed by warmth and
8 hours for 24 (33.2%) gentamicin (3mg/Kg) tenderness.
hours after Control: 63/250 once a day and Endometritis: the
emergency (25.2%) metronidazole (500mg) presence of
o
cesarean Comorbidities every 8 hours for 24h fever (38 C or
surgery Gravidity: postoperatively above) in
Multigravida: Standard preventive association with
Intervention: 173/250 measures: one or more of
(69.2%) Wound dressing: wound the following:
Control: 167/250 was left open. uterine
(66.8%) tenderness or
Presence of cesarean foul smelling
scar, yes lochia.
Intervention: 98/250 Perioperative
(39.2%) care:
Control: 87/250 Bladder catheter
(34.8%) was removed
Ruptured amniotic after 48h
membrane Other notes:
Intervention: 129/250 Sample size was
(51.6%) calculated to be
Control: 158/250 490 based on
(63.2%) alpha = 0.05 and
P=0.01 beta = 0.20
Duration of operation Follow-up: 30
(>60 min) days postop.
Intervention: 99/250 Patients who
(39.6%) could not attend
Control: 110/250 their follow up
(44.0%) appointments
Procedures: were contacted
emergency cesarean via phone or by
section communicating
2017 American Medical Association. All rights reserved. 147
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Indications: NR with a ten cell
Setting: Single leader via
teaching hospital physical
Location: Tanzania address.
Dates: October 2011 Funding Source
May 2012 Conflicts:
Inclusion Criteria: Authors: None
pregnant women Institution: None
admitted to the Study: None
institutions labor Supplies: None
ward that needed or
had indication for
emergency cesarean
section (under spinal
anesthesia) during
the study dates that
had consented to the
study.
Exclusion Criteria:
Pregnant women
with fever (temp
38 C), prolonged
o
obstructed labor,
and prolonged and
premature rupture of
membranes (rupture
of membrane >12
hours). Pregnant
women presenting
with features of
chorioamnionitis
(i.e., foul smelling
lochia, uterine
tenderness
associated with
fever) allergies to the
antibiotic used in the
study, or those who
had used the
2017 American Medical Association. All rights reserved. 148
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
antibiotics in the 24
hours preceding the
operation or
unconscious patients
who could not
provide consent.
Haga RCT To confirm the Number of patients: Intervention group: SSI: Definitions:
52
2012 1, 6 validity of N=325 n=164 Overall SSI: SSI Incision site
(ES) single-dose Patient A single dose of 1g Intervention: 15/164 infection and
antimicrobial Characteristics cefazolin administered (9.1%) organ/space
prophylaxis for Age, y: mean (range) intravenously. An Control: 10/161 (6.2%) infection were
the prevention Intervention: 68 (33- additional dose Difference (95%CI): -2.9% CDC SSI
of SSI and 90) administered when (-5.9-0.00) Guideline
examined Control: 68 (39-91) surgery duration >3h. definitions
independent Gender: male:female Timing of intervention: Superficial/ Incisional Anastomotic
risk factors Intervention: 118:46 preop Infections dehiscence:
influencing the Control: 117:44 Duration of intervention: Intervention: 14/164 confirmed by
development Obesity: preop (8.5%) clinical and/or x-
of surgical site BMI mean (range), Device/agent: 1g Control: 7/161 (4.3%) ray examination
2
infections kg/m cefazolin Difference (95%CI): -4.2 (- Remote infection:
following Intervention: 21.7 Monitoring intervention: 6.9- -1.5) an infection
elective (15.2-31.6) NA occurring at a
gastric cancer Control: 21.9 (15.4- Control group: n=161 Organ/space infections site other than
surgery. 31.6) 6 doses - 1g cefazolin Intervention: 11/164 the surgical site,
Comorbidities: administered (6.7%) such as
Diabetes mellitus: intravenously. An Control: 6/161 (3.7%) pneumonia,
Intervention: 38/164 additional dose Difference (95%CI): -3.0 (- urinary tract
(23.2%) administered when 5.5- -0.6) infection,
Control: 36/161 surgery duration >3h. Organ/space infections enteritis, or
(22.4%) An additional 5 doses related to anastomic bloodstream
were given every 12h dehiscence or (catheter-
Procedures: elective postop pancreatic fistula related)
gastric surgery Standard preventive Intervention: 10/164 infection.
Total gastrectomy: measures: (6.1%) Perioperative
proximal/distal Wound covering: surgical Control: 6/161 (3.7%) care:
gastrectomy: towels for conventional Other notes:
Intervention: 66:98 gastrectomy, wound Both Superficial & power
Control: 66:95 protectors for Organ/Space calculation
Combined resection: laparoscopic or Intervention: 9/164 based on
2017 American Medical Association. All rights reserved. 149
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Intervention: 37/164 laparoscopic-assisted (5.5%) detecting an 8%
Control: 36/161 surgeries. Control: 3/161 (1.9%) difference in the
Gallbladder: Anastomoses = stapled. incidence of
Intervention: 15/164 Rinsing abdominal cavity- SSIs with a CI of
Control: 13/161 copiously rinsing with 2- Other infections: 95% and a
Spleen: 3L saline before closure All remote infections: power of 80%
Intervention: 23/164 Closure approximated by Intervention: 6/164 resulted in
Control: 20/161 staples (3.7%) sample size of
Pancreas: Drains closed suction Control: 5/161 (3.1%) 159 in each arm.
Intervention: 3/164 drains were placed sub- P=0.78 Follow-up: 30
Control: 2/161 hepatically and/or Pneumonia: days postop via
Liver: subphrenically Intervention: 3/164 inspection at
Intervention: 2/164 according to the type of (1.8%) outpatient clinic.
Control: 2/161 gastrectomy, brought Control: 2/161 (1.2%) Funding Source
Small intestine: out through separate Enterocolitis: Conflicts:
Intervention: 0/164 stab wounds. Drains Intervention: 1/164 Authors: NR
Control: 1/161 were removed after 7 (0.6%) Institution: NR
days. Control: 2/161 (1.2%) Study: NR
Indications: gastric Dressing sterile dressing Urinary Tract Infection: Supplies: NR
cancer was removed within Intervention: 1/164
Pathologic stage: 48h (0.6%)
1/II:III/IV Blood Transfusion: Control: 0/161
Intervention: 54:110 Intervention: 10/164 Bloodstream infection:
Control: 65:96 (6.1%) Intervention: 1/164
P=0.16 Control: 21/161 (13.0%) (0.6%)
P=0.03 Control: 1/161 (0.6%)
Setting: one university
medical center Topic-specific
Location: Japan outcomes:
Dates: February 2007 Multivariate regression
November 2010 analysis
Inclusion Criteria: Blood Loss (every 100mL)
Patients undergoing OR (95%CI): 1.13 (1.05-
elective surgery for 1.23), p<0.01
BMI (25 kg/m ):
2
gastric cancer
Exclusion Criteria: OR (95%CI): 2.76 (1.10-
Patients <20 years 6.90), P=0.03
old, those with a Age (every 10 years
known allergy to increment:
2017 American Medical Association. All rights reserved. 150
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
cephalosporins, OR (95%CI): 1.65 (1.01-
those with any 2.70), P=0.046
infection within the Reoperations: NR
prior 2 weeks, those Length of stay:
with synchronous Mortality: NR
cancer at any sites Adverse events: NR
other than the
stomach, and those
needing colon
resection because of
tumor involvement.
Hussain RCT To determine Number of patients: Intervention group: SSI Definitions :
31
2012 1, 6, 7, the role of N=377 n=195 Surgical site infection SSI: pus discharge
(ES) 8, 10 postoperative Patient A single preoperative dose Intervention: 9/195 from wound that
antibiotics in Characteristics: of cefuroxime sodium (4.6%) necessitated
reducing the statistically there and metronidazole half Control: 8/182 (4.3%) wound opening
surgical site was no difference an hour before surgery. and drainage.
infections between group Timing of intervention: Other infections: NR Intra-abdominal
(SSIs) and characteristics. Preoperative Topic-specific collection: fluid
intra- Age, y: meanSD, Duration of intervention: outcomes: collection inside
abdominal Intervention: NA No Intraabdominal the peritoneal
abscess 32.7810.62 Device/agent: cefuroxime collection of fluid cavity confirmed
formation after Control: 31.709.96 sodium reported by ultrasound or
open Gender: ratio of m:f Monitoring intervention: Reoperations: NR computed
appendectomy Intervention: 1.15:1 NA Length of stay, days: tomography and
in patients Control: 1.16:1 Control group: n=182 Intervention: 2.290.82 requiring
with non- Obesity: NR A preoperative dose of Control: 2.350.48 drainage.
perforated Comorbidities: NR cefuroxime sodium and Perioperative
appendicitis Exclusionary criteria metronidazole half an Mortality: no perioperative care: NR
(NPA), and to Procedures: hour before surgery mortality Other notes: NR
define the emergency open plus an additional dose Adverse events: NR Follow-up: 30
uniform appendectomy of cefuroxime sodium days
guidelines in Indications: acute and metronidazole at Funding Source
the appendicitis 8h postop Conflicts:
management Setting: 1 tertiary care Standard preventive Authors: NR
of these hospital measures Institution: NR
patients in our Location: Saudi Arabia Technique: performed Study: NR
institution. Dates: January 2010 through right lower Supplies: NR
July 2011 quadrant incision.
2017 American Medical Association. All rights reserved. 151
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Inclusion Criteria: Wound closure: primarily
Patients admitted in all patients following
with the clinical washing with normal
diagnosis of acute saline.
appendicitis
undergoing
emergency open
appendectomy.
Exclusion Criteria:
Patients who had
received antibiotics
within 72 hours of
admission or who
were diabetics,
immunocompromise
d, or pregnant. Also,
those who were
found to have
complicated
appendicitis
(gangrenous,
perforated,
appendicular mass
or abscess) or
normal appendix
per-operatively were
excluded as well.
Imamura RCT To assess Number of patients: Intervention group: SSI Definitions:
51
2012 1, 2, 4, non-inferiority N=355 n=176 Total: Superficial, Deep
(ES) 10 of the Patient 1g Cefazolin 30 min after Intervention: 8/176 (5%) incisional &
omission of Characteristics: anesthesia and before Control: 16/179 (9%) organ/space
postoperative patient the surgical incision RR (95%CI) 0.51 (0.22- infections were
antimicrobial characteristics were plus every 3h 1.16) diagnosed by
prophylaxis in balanced between intraoperatively. P=0.138 CDC NNIS
patients with groups. Timing of intervention: OR for SSI with infection
gastric cancer Age: y, median (range) preoperative intraoperative antimicrobial definitions.
Intervention: 66 (36- Duration of intervention: prophylaxis: Perioperative
84) NA Patients with BMI<25 care: NR
Control: 65 (35-84) Device/agent: 1g 0.31 (0.099-0.998), Other notes:
2017 American Medical Association. All rights reserved. 152
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Gender; Male: female cefazolin p=0.050 power
Intervention: 115:61 Monitoring intervention: Patients who with BMI25 calculation was
Control: 120:59 NA 1.09 (0.25-4.72), P=0.91 conducted for
2
Obesity: BMI (kg/m ) Control group: n=179 All 24 SSI in patients who composite SSI.
Intervention: 22.3 1 g cefazolin before the underwent distal Follow-up: 30
(16.3-33.0) surgical incision, every gastrectomy without days postop
Control: 22.5 (12.4- 3h intraoperatively plus protocol violation. Funding Source
32.9) 1g cefazolin on Superficial incisional: Conflicts:
Comorbidities: postoperative day 0 (at Intervention: 1/176 (<1%) Authors: None
Blood loss, median night) and every 12h Control: 45/179 (3%) Institution: None
(range) mL until postoperative day P=0.215 Study: None
Intervention: 200 (1- 2 (2g/ day for 2 Deep Incisional: Supplies: None
880) postoperative days) Intervention: 0/176
Control: 210 (1-1700) Standard preventive Control: 0/179
measures: Organ/space
Procedures: distal Drainage Tube: Intervention: 7/176 (4%)
gastrectomies and Intervention: 157/176 Control: 11/179 (6%)
lymphadenectomies. (89.2%) P=0.469
Two patients underwent Control: 153/179 (85.5%) O/S With anastomotic
a total gastrectomy Transfusion: leakage
because they had a Intervention: 0/176 Intervention: 1/176
positive resection Control: 4/175 (2.3%) (0.6%)
margin, and one had Care before and after Control: 4/179 (2.3%)
palliative bypass surgery and wound O/S without anastomotic
surgery with management were leakage
gastrointestinal done according to Intervention: 6/176
anastomosis. respective institutional Control: 7/179 (2.3%)
Indications: gastric standards.
cancer Other infections:
Setting: Seven Remote site infections:
hospitals (4 tertiary Overall:
care & 3 university Intervention: 5% (CI 2-
hospitals) 10)
Location: Japan Control: 3% (CI 1-7)
Dates: June 2, 2005
December 6, 2007 Pneumonia or bronchitis:2
Inclusion Criteria: patients (unclear which
patients who had group)
histologically proven UTI
2017 American Medical Association. All rights reserved. 153
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
gastric Intervention: 10/176
adenocarcinoma that (0.6%)
was deemed curable Control: 1/179 (0.6%)
with a distal
gastrectomy. Topic-specific
Patients with an ASA outcomes: NR
score of 1 or 2 Reoperations : NR
Exclusion Criteria: If Length of stay:
patients had an Intervention: 12 (7-114)
active or Control: 12 (7-87)
uncontrolled P=0.742
infection, received Mortality: NR
neoadjuvant Adverse events: no
chemotherapy, or severe reaction to
had been given antimicrobial
steroids. prophylaxis occurred in
either group.
Lin RCT To elucidate Number of patients: Intervention group: SSI (30 days): Definitions:
35
2011 1 the effect of N=231 n=120 Sternal Wound infection SSI CDC 1999
(ES) the duration of Patient Patients received 1g of Intervention: 13/120 Guideline
prophylactic Characteristics: cefazolin within 1 hour (10.8%) Definitions
antibiotics, a baseline prior to incision, and an Control: 9/111 (8.0%) Perioperative
prospective, characteristics were additional dose was P=0.48 care: NR
randomized similar in each allowed if it was a Deep infections Other notes: None
control study group. prolonged operation (1 Intervention: 3/120 Follow-up: 1
was Age, y: meanSD additional dose for (2.5%) month postop
conducted to Intervention: 64.49.6 every 3-4 hours of Control: 1/111 (0.9%) Funding Source
compare the Control: 65.511.5 surgery). Then 1g P=0.62 Conflicts:
effectiveness P=0.45 cefazolin every 8 hours Superficial Authors: NR
of preventing Gender: male, for 3 doses after the Intervention: 3/120 Institution: NR
SSI after Intervention: 94/120 operation. (2.5%) Study: NR
Coronary (78.3%) Timing of intervention: Control: 2/111 (1.8%) Supplies: NR
Artery Bypass Control: 90/111 pre and postoperatively P=1.00
Graft (CABG) (81.1%) Duration of intervention; Harvest Site Infection
using1-day or P=0.60 Na Intervention: 7/120
m2
3-day Obesity: BMI (kg/ ), Device/agent: Cefazolin (5.8%)
antibiotic meanSD Monitoring intervention: Control: 6/111 (5.4%)
prophylaxis. Intervention: 25.02.8 NA P=0.89
Control: 25.12.9 Control group: n=111
2017 American Medical Association. All rights reserved. 154
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
P=0.84 Patients received 1g of Other infections: NR
Comorbidities cefazolin within 1 hour Topic-specific
Hypertension: prior to incision, and an outcomes:
Intervention: 80/120 additional dose was Time to SSI, d:
(66.7%) allowed if it was a Intervention: 12.83.3
Control: 75/111 prolonged operation (1 Control: 18.95.3
(67.6%) additional dose for P=0.004
P=0.88 every 3-4 hours of
Diabetes Mellitus surgery). Then 1g Reoperations: NR
Intervention: 52/120 cefazolin every 8 hours Length of stay:
(43.3%) for 9 doses after the Postop ICU Stay, d
Control: 43/111 operation. meanSD
(38.7%) Standard preventive Intervention: 2.20.9
P=0.48 measures: Control: 2.61.6
Smoking MRSA Swab screening P=0.05
Intervention: 46/120 for MRSA carriage was Postop LOS, d meanSD
(38.3%) conducted 1 day preop. Intervention: 12.13.6
Control: 34/111 No decolonizing agents Control: 16.79.1
(30.6%) were used. P=0.10
P=0.22
COPD Mortality:
Intervention: 3/120 3 patients died
(2.5%) immediately after
Control: 0/111 surgery but were
P=0.60 excluded.
Adverse events: NR
Nasal Swab Screening
S. aureus positive
Intervention: 14/120
(12.7%)
Control: 20/111
(19.4%)
P=0.18
MSSA carrier
Intervention: 8/120
(7.3%)
Control: 16/111
(15.5%)
P=0.06
2017 American Medical Association. All rights reserved. 155
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
MRSA carrier
Intervention: 6/120
(5.5%)
Control: 4/111 (3.9%)
P=0.75
Procedures: Coronary
Artery Bypass Graft
(CABG)
Emergency
Intervention: 26/120
(21.7%)
Control: 30/111
(27.0%)
P=0.34
Indications
Setting: 1 university
hospital
Location: Taiwan
Dates: June 2002
April 2004
Inclusion Criteria:
Patients who
underwent non-
emergency CABG
surgery and were
18 years old.
Exclusion Criteria:
Patients with existing
preoperative
infections; those
undergoing
treatment with
antibiotics;
hypersensitivity to
cefazolin; renal
dysfunction (serum
creatinine level
2017 American Medical Association. All rights reserved. 156
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
>2mg/dL or
creatinine clearance
<35mL/min, or under
hemodialysis
treatment); left
ventricular ejection
fraction <30%;
obesity (body mass
2
index >31kg/m );
chronic obstructive
pulmonary disease
(COPD); undergoing
combined surgery
other than CABG;
neutropenia
(leukocyte count
3
<1000/cm );
pregnancy or
undertaking
breastfeeding; or
refusal of consent
Suzuki RCT To establish Number of patients: Intervention group: SSI: (follow up 4 weeks) Definitions:
42
2011 1, 2, 7, the optimal N=360 n=179 Incisional SSI Postoperative
(ES) 8, 9 duration of Patient A single dose of Intervention: 15/179 infection: an
perioperative Characteristics: No oxacephem (1g) (8.4%) infection
antimicrobial significant difference antimicrobial 11/15: No fever and occurring within
administration was observed in prophylaxis was were improved by 30 days after
of an baseline patient administered removal of some surgery.
oxacephem characteristics intravenously before sutures and abscess SSI: diagnosed by
antimicrobial between groups. surgery. The drainage 2 physicians
in patients Age, y, meanSD antimicrobial was given 2/15: Developed fever Incisional SSI:
undergoing Intervention 6511 from 1 hour before the and were treated by macroscopic
elective colon Control: 669. incision was made. antimicrobials & abscess or
cancer Gender m/f When the operative abscess drainage purulent
surgery, by Intervention: 101/84 time exceeded 3 hours, Control: 13/181 (7.2%) discharge
determining Control: 101/84 an addition al gram of 13/13: No fever and observed on the
the incidence Obesity: NR antimicrobial was were improved by operative wound
of SSIs with Comorbidities: administered removal of some Organ/ space SSI:
the use of Diabetes Timing of intervention: sutures and abscess An infection in
2017 American Medical Association. All rights reserved. 157
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
mechanical Intervention: 17/185 Pre and intraoperatively drainage the organ
preparation (9.2%) (based on procedure P=0.0008 (=0.10) subjected to
and chemical Control: 14/185 duration) Duration of Organ/ space SSI surgery.
preparation (7.6%) intervention: Pre and Intervention: 1/179 Remote infection:
together with Procedures: Elective intraoperatively (vs. up (0.6%) Evaluated by
oral laparotomy for colon to 4 days in controls) Control: 2/181 (1.1%) chest plain films,
antimicrobial cancer Device/agent: oxacephem P<0.001 (=0.10) sputum, urine,
administration. Indications: colon 1g IV antimicrobial 3/3: anastomic blood, or
cancer Monitoring intervention: leakage catheter culture
T Category NR (Cultures of after surgery.
Tis, T1/ T2-T4 drainage or purulence Other infections: Perioperative
Intervention: 21/164 were made) Remote Infection care: NR
Control: 29/156 Control group: n=181 Intervention: 8/179 (4.5%) Other notes: Non-
TNM Classification: not Oxacephem (1g) 6/8: Catheter infection inferiority margin
significant; antimicrobial was Detected Post-OP day is 10% (=0.10).
Setting: 1 university administered 3 or later & resolved Based on this,
hospital intravenously twice with catheternremoval there were no
Location: Japan daily for 4 days from the & antimicrobial differences in
Dates: August 2002- day of surgery until administration incidence of
October 2007 post-op day 3. The 1/8: Jugular vein SSIs,
Inclusion Criteria: antimicrobial was given phlebitis organ/space or
Patients undergoing from 1 hour before the 1/8: Pneumonia remote
elective laparotomy incision was made. Control: 6/181 (3.3 %) infections
for colon cancer When the operative 4/6: Catheter infection between groups
Exclusion Criteria: time exceeded 3 hours, Detected Post-OP n (single dose vs.
Patients with stoma, an addition al gram of day 5 or later & postop dosing X
those who could not antimicrobial resolved with catheter up to 4 days)
undergo the normal prophylaxis was removal & abx Follow-up: 4
mechanical administered 1/6: Urinary Tract weeks post-
preparation owing to Standard preventive Infection discharge at a
stenosis or measures: 1/6: Pneumonia hospital visit.
obstruction, and Bowel Prep: All patients P<0.0001 (=0.10) Funding Source
those with a underwent mechanical C. difficile Colitis Conflicts:
preoperative and chemical Intervention: 0/179 Authors: NR
diagnosis of stage IV preparation of the Control: 0/181 Institution: NR
and American bowel. Study: NR
Society of 1. Mechanical: 10 ml Topic-specific Supplies: NR
Anesthesiologists of sodium outcomes: NA
score of 3. picosulfate was Reoperations:
2017 American Medical Association. All rights reserved. 158
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
orally 3/3 Organ/ space SSI
administered 2 developed fever and
days before required reoperation
surgery and 2,000 Length of stay:
ml of polyethylene Mean Length of stay for
glycol-electrolyte patients with colon
sodium was orally cancer: 154 days
administered in (facility data)
the morning of the Mortality: NR
day before surgery Adverse events:
2. Chemical: 0.5g of Small Bowel Obstruction
kanamycin sulfate Intervention: 5/179
and 0.5g of (2.8%)
metronidazole Control: 8/181 (4.4 %)
were orally P<0.0001 (=0.10)
administered at 1, Other
2 and 11pm on the Intervention: 2/179
day before the (1.1%)
operation. 1/2: Venous
thrombosis of the lower
extremities
1/2: Duodenal
Stenosis
Control: 2/181 (1.1 %)
1/2: Postoperative
hemorrhage
1/2: Duodenal
Stenosis
Tamayo RCT To test the Number of patients: Intervention group: SSI: (Follow up at least 1 Definitions:
12
2008 1, 2, 4, hypothesis N=838 n=419 year) CDC definitions
(ES) 7, 8, 9 that single Patient A single dose of 2g Total SSIs: 50/838 (5.9%) were used
doses of Characteristics: cefazolin was Intervention: 30/419 throughout.
cefazolin are Both groups were administered (8.3%) Superficial SSI
as effective as homogeneous and intravenously between Control: 15/419 (3.6%) The infection
a 24-hour comparable in as far 20-30 minutes after the P=0.004 covers the skin
regimen of as their demographic induction of anesthesia. Total Incisional SSI and
cefazolin in profiles and clinical . For all procedures Intervention: 21 (5.0%) subcutaneous
preventing characteristics were lasting more than 3 Control: 7 (1.7%) cellular tissue
SSIs in adults concerned except for hours, a new dose of 1g P=0.007 and is
2017 American Medical Association. All rights reserved. 159
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
undergoing transfusions (below). of cefazolin was Superficial Incisional SSI accompanied by
cardiac Age, y: meanSD administered Intervention: 16 (3.8%) one of the
procedures Intervention: intraoperatively. Control: 7 (1.7%) following:
67.510.5 Timing of intervention: P=0.04 purulent
Control: 68.210.5 Single dose Deep Incisional SSI drainage
Gender: m/f preoperatively (re- Intervention: 5 (1.2%) through the
Intervention: 272/147 dosed intraoperatively Control: 0 incision, positive
Control: 247/172 depending on P=0.03 results of the
P=0.07 procedure Organ/Space SSI incisional
Obesity: NR duration)Duration of Intervention: 14 (3.3%) culture, and
Comorbidities intervention: Pre and Mediastinitis and classic
Diabetes: intraop vs. extended endocarditis were inflammatory
Intervention: 111/419 dosing X 24hrs postop documented signs that allow
(26.5%) in controls simultaneously in 2 the wound to be
Control: 125/419 Device/agent: Cefazolin patients opened by the
(29.8%) 2g IV Control: 8 (1.9%) surgeon except
Peripheral Vascular Monitoring intervention: P=0.19 in cases in which
Disease Wound cultures Osteomyelitis the incisional
Intervention: 25/419 Control group: n=419 Intervention: 3 (0.7%) culture was
(5.9%) Administered 2g of Control: 2 (0.5%) negative.
Control: 38/419 (9%) cefazolin intravenously P=0.5 Deep incisional SSI
P=0.08 between 20-30 minutes Mediastinitis Infection
Intraoperative values after the induction of Intervention: 8 (1.9%) involves the
not statistically anesthesia, followed by Control: 5 (1.2%) deep soft tissues
significant except for 1g every 8 hours. For P=0.28 of the incision
Intraoperative values: all procedures lasting Endocarditis with at least 1 of
Hematocrit after CPB, more than 3 hours, a Intervention: 5 (1.2%) the following:
meanSD: new dose of 1g of Control: 1 (0.2%) purulent
cefazolin was P=0.10 drainage, a deep
Interventions:27.07 administered Other infections: incision that
4.20 intraoperatively. Sepsis spontaneously
Control: 26.484.07 Standard preventive Intervention: 17 (4.0%) dehisced or was
P=0.05 measures: NR Control: 18 (4.2%) deliberately
Postoperative values P=0.50 opened by the
Intra-aortic balloon Topic-specific surgeon when
pump outcomes: patient had a
Intervention: 5/419 Antimicrobial resistance: fever (temp
38 C), or
o
(1.1%) Pathogens isolated
Control: 14/419 were similar distribution localized pain or
2017 American Medical Association. All rights reserved. 160
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
(3.3%) in both groups tenderness
P=0.03 (P0.05). 43/50 (86%) (unless the
Red cell transfusion of SSIs were gram results of an
patients positive cocci (S. incisional culture
Intervention: 261/419 epidermis (SE) most were negative),
(62.3%) common, followed by S. or evidence of
Control: 216/419 aureus (SA). deep incision
(51.5%) SE-MRSE infection found
P=0.01 Intervention: 12/20 SE in a direct
Procedures: Elective and 12/35 (34.3%) SSI examination or
Coronary artery Control: 5/9 SE and 5/15 second
bypass grafting (33%) SSI operation
(CABG) or valve SE-MSSE Mediastinitis
operations or both Intervention: 8/20 SE and Organ/space
Indications: NR 8/35 (22.8%) SSI SSI
Setting: 1 tertiary-level Control: 4/9 se and 4/15 characterized by
hospital (26.6%) SSI 1 of the
Location: Spain following:
Dates: September SA-MRSA positive results
2003 January Intervention : 4/11 SA of a culture
2007 and 4/35 (11.4)% SSI obtained from
Inclusion Criteria: Control: 1/5 SA and 1/15 mediastinal
Adult patients (>18 SSI (6.6%) tissue or fluid
years of age) SA-MSSA: during a surgical
undergoing elective Intervention 7/11 SA and operation,
coronary artery 7/35 (20.0%) SSI patient fever
(temp 38 C),
o
bypass grafting Control: 4/5 SA and 4/15
(CABG), valve (26.6%) SSI sternal pain or
operations or both instability,
by means of Gram negative bacilli in mediastinal
sternotomy. 12/50 (24%) ; involvement
Exclusion Criteria: polymicrobial SSI rates suggested by a
Presence of active similar between groups computed
infection, the Reoperations: NR tomographic
administration of Length of stay: scan, or
antimicrobial therapy Preoperative organisms
in the 48 hours hospitalization d, cultured form the
before surgical meanSD mediastinal area
intervention, Intervention: 9.77.9 Sternal
2017 American Medical Association. All rights reserved. 161
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
emergency surgical Control: 10.810.3 osteomyelitis
intervention, or P=0.11 An organ/space
allergy to Mean ICU Stay d, SSI indicated by
betalactams. Also, meanSD persistent
patients with Intervention: 10.310.9 purulent
transplants or who Control: 9.18.7 drainage from
did not wish to P=0.09 the sternotomy &
participate in the Duration of hospitalization confirmed by
study. after operation d, microbiologic
meanSD and
Intervention: 14.7515.8 histopathologic
Control: 12.214.2 findings.
P=0.25 Endocarditis
Organ/space
Mortality: SSI
30 day: characterized by
Intervention: 22 (5.2%) Dukes criteria
Control: 31 (7.4%) (Durack 1994)
P=0.12 Perioperative
90 day: care: NR
Intervention: 29 (6.9%) Other notes:
Control: 37 (8.8%) SSI Risk
P=0.18 Stratification:
365 day NNIS
Intervention: 43 (10.3%) Statistical Analysis:
Control: 48 (11.5%) Study powered
P=0.34 to detect
reduction in SSI
Adverse events: rate of <5% with
Intra-aortic balloon pump a=0.20 and
Intervention: 5 (1.1%) =0.05 (n=419
Control: 14 (3.3%) in each arm)
P=0.03 Follow-up:
Red cell transfusion Patients were
patients examined daily
Intervention: 261 while in the
(62.3%) hospital. Cardiac
Control: 216 (51.5%) surgeons
P=0.01 personally
2017 American Medical Association. All rights reserved. 162
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Arterial Fibrillation followed up with
Intervention: 17 (4.0%) patients in the
Control: 21 (5.0%) cardiac
P=0.30 outpatient clinic
Respiratory Failure for at least 1
Intervention: 28 (6.6%) year after
Control: 23 (5.4%) discharge from
P=0.28 the hospital
Acute Renal Failure Funding Source
Intervention: 21 (5.0%) Conflicts:
Control: 27 (6.4%) Authors: NR
P=0.22 Institution: NR
Renal replacement Study: NR
treatment Supplies: NR
Intervention: 12 (2.8%)
Control: 13 (3.1%)
P=0.50
Liu RCT To investigate Number of patients: Intervention group: n=27 SSI: (follow up 30 days) Definitions:
39
2008 1, 2, 3, the impact of n=53 Received one dose of Surgical wound infection: Surgical wound
(ES) 4, 6, 7, the duration of Patient preoperative Total: 13 (24.5%) infection:
8, 10 prophylactic Characteristics: prophylactic Intervention: 5 (18.5%) Purulent
antimicrobials There were no antimicrobial Control: 8 (30.7%) discharge either
on post- significant (intravascular P=0.473 spontaneously
operative differences between clindamycin 300mg) Bivariate analysis of or by incision
wound groups according to one hour before incision population based on and drainage
infection in basic data and and then at 6 hour infections within 30 days
patients laboratory studies. intervals over a period Bivariate analysis of after the
undergoing Age, y: meanSD of 72 hours. population based on operation.
major head Timing of intervention: infections Perioperative
and neck Intervention:56.412 Pre and postoperatively Infected n=14 / Uninfected care: NR
neoplasm .3 Duration of intervention: n=40 Other notes:
operations Control: 56.511.1 1 hour before incision to Tumor size, cm: meanSD Operative
and to Gender: m/f 24 or 72 hours after Infected: 3.21.3 procedures were
determine Intervention: 23/4 surgery Uninfected: 2.21.1 all performed by
associated Control:21/5 Device/agent: P=0.005 one surgeon and
2
factors in post- Obesity: BMI, kg/m , clindamycin Tracheostomy all post-
operative average Monitoring intervention: Infected: 13 (100%) operative wound
wound Intervention: 23.6 NR Uninfected: 14 (50%) conditions were
infection. Control: 23.6 Control group: n=26 P<0.001 evaluated by
2017 American Medical Association. All rights reserved. 163
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Comorbidities Received one dose of Duration of antimicrobials another doctor
Previous radiotherapy: preoperative 24 hours (Control) (Statistical
Intervention: 2/27 prophylactic Infected: 8 (61.5%) analysis: sample
(14.8%) antimicrobial Uninfected: 18 (45%) size not large
Control: 8/26 (30.8%) (intravascular P<0.001 enough and
Perioperative data: clindamycin 300mg) 72 hours (Intervention) statistic power
Surgical reconstruction one hour before incision Infected: 5 (38.5%) unsatisfied
Intervention: 4/27 and then at 6 hour Uninfected: 22 (55%) Follow-up: 30
(14.8%) intervals over a period P<0.001 days
Control: 10/26 (38.5%) of 24 hours. Previous radiotherapy postoperatively
Perioperative blood Infected: 8 (61.5%) Funding Source
loss Standard preventive Uninfected: 4 (10.0%) Conflicts:
Intervention: 239110 measures: NR P<0.001 Authors: None
Control: 262136 Previous chemotherapy Institution: None
Perioperative blood Infected: 9 (69.2%) Study: None
transfusion: YES Uninfected: 4 (10.0%) Supplies: None
Intervention: 4/27 P<0.001
(14.8%) Surgical reconstruction
Control: 7/26 (26.9%) Infected: 10 (76.9%)
Uninfected: 4 (10%)
Procedures: Head and P<0.001
neck surgical Serum Albumin: g/dlSD
procedures Infected: 3.50.7
Reconstruction with Uninfected: 4.10.4
free flaps or P=0.013
pectoralis major Hemoglobin: g/dlSD
myocutaneous flaps: Infected: 10.81.9
14/53 (26.4%) Uninfected: 13.41.8
Intervention: 4/27 P<0.001
(14.8%) Perioperative blood loss:
Control: 10/26 mlSD
(38.5%) Infected: 380113
Laryngectomies Uninfected: 208 93
accounted for small P<0.001
portion of cases Perioperative blood
Indications: Tumor transfusion
Sites Infected: 7 (53.8%)
Oral cavity/Oropharynx/ Uninfected: 4 (10.0%)
Larynx/ P<0.001
2017 American Medical Association. All rights reserved. 164
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Hypopharynx/ Logistic regression
Others identified preop
Intervention: hemoglobin 10.5g/dL
18/2/1/2/4 (p=0.025) and surgical
Control: reconstruction (P=0.036)
1/7/2/13/3 as independent risk factors
Setting: 1 Veterans Other infections: NR
Hospital Topic-specific
Location: Taiwan outcomes:
Dates: January 2004- Antimicrobial Resistance:
December 2004 NR
Inclusion Criteria: 13/53 (24.5%) total SSIs
Patients scheduled 6/13 (46.1%) polymicrobial
to receive head and P. aeruginosa (9/13,
neck surgical 69.2%)
procedures that E. faecalis (4/13, 30.0%)
would enter the K. pneumonia (4/13,
upper aerodigestive 30.8%)
tract. C. koseri (1/13, 7.7%)
Exclusion Criteria: A. baumannii (1/13, 7.7%)
Those under Reoperations: NR
antimicrobial Length of stay, d:
treatment, allergic to Intervention: 2215
clindamycin, with Control: 2518
diabetes mellitus, or P=0.627
reluctant to join this Mortality: NR
protocol. Adverse events: One
patient developed an
allergic reaction after
treatment and was
forced to drop out.
2017 American Medical Association. All rights reserved. 165
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Fujita RCT To determine Number of patients: Intervention group: SSI: (follow up NR) Definitions: ND
15
2007 1, 2, 7, the efficacy of N=377 n=190 Total SSI Perioperative
(ES) 8, 9, 10 a single-dose Patient Single Dose Group Intervention: 32/190 care: To ensure
regimen of Characteristics: Received 1 g cefmetazole (16.8%) High infection that the trial
second- Although patient age just before skin incision. rate results were
generation was significantly Though additional Control: 17/187 (9.1%) applicable
cephalosporin higher in the control doses are generally,
cefmetazole group, other patient recommended every 3- Incisional SSI specific
without characteristics were 4 hours during Intervention: 27/190 instructions on
metronidazole identical. extended surgery, none (14.2%) surgical
and oral Age, y: meanSD were given Control: 8/187 (4.3%) techniques and
antimicrobials Intervention: Timing of intervention: P=0.009 on postoperative
with regards to 59.411.1 Preoperatively care were not
reduction in Control: 62.19.8 Duration of intervention: Organ or Space SSI included
incidences of P=0.01 Preoperatively or Intervention: 5 (2.6%) Other notes:
surgical site Gender: m/f preoperatively and up Control: 9 (4.8%) Trial was designed
infections and Intervention: 126/64 to 16 hours P=0.26 as non-inferiority
all other Control: 107/80 postoperatively in test to detect 5%
infectious Obesity: NR controls. Because only incidence of difference in
complications Comorbidities: NR Device/agent: incisional SSIs differed incidence of
following Procedures: cefmetazole 1g significantly between incisional SSI
elective Colorectal Surgery Monitoring intervention: groups, subset analysis with CI 95%,
colorectal Conventional: NA performed: Multivariate power 90%
surgery. Intervention: 129/190 Control group: n=187 analysis revealed assuming
(67.9%) 3-Dose Group antimicrobial dose was the incidence of
Control: 133/187 Received 1 g cefmetazole only significant factor infection of 5%.
(71.1%) just before skin incision associated with incisional Sample size of
Colectomy/ anterior plus 2 postoperative 1g SSI (P=0.002). This result 238 required in
resection/ doses at 8 and 16 is confusing unless they both arm. After
abdominoperineal hours after the first meant to say antimicrobial 1yr interim
resection administration. Though duration. analysis
Intervention: 73/56/0 additional doses are revealed
Control: 77/53/3 recommended every 3- The incidence of incisional significant
Laparoscopic: 4 hours during SSI in the control was difference
Intervention: 61/190 extended surgery, none lower even in patients between groups
(32.1%) were given whose surgery lasted 3hrs and enrollment
Control: 54/187 or less than in the was stopped.
(28.9%) Standard preventive intervention group. Significance at
Colectomy/ Anterior measures: <0.05
2017 American Medical Association. All rights reserved. 166
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
resection Bowel Prep: Patients The incidence of incisional Follow-up:
Intervention: 49/12 underwent mechanical SSI associated with Wounds were
Control: 42/12 bowel prep with 2L laparoscopic surgery was checked daily
No gastric or hepatic polyethylene glycol- lower than in conventional until discharge
resections included) electrolyte solution 1 although not statistically and at the first
Indications: day before surgery. No significant postoperative
Colon cancer: 241/377 oral AMP was Other infections: Urinary hospital visit
(63.9%) Rectal administered as part of tract infections, (when? NR)
cancer: 136/377 the bowel prep pneumonia, septicemia, Funding Source
(36.1%) infective diarrhea and Conflicts:
Setting: 7 major line sepsis. Authors: None
hospitals Other Institution: None
Location: Japan Intervention: 12/190 Study: None
Dates: May 6, 2004 (6.3%) Supplies: None
April 25, 2005 Control: 9/187 (4.8%)
Inclusion Criteria: P=0.52
Patients aged 20-80 Total Infections: (SSI plus
years scheduled to other)
undergo elective Intervention: 44/190
colorectal surgery. (23.1%)
Exclusion Criteria: Control: 26/187 (13.9%)
Emergency P=0.03
operations, C. difficile Colitis:
obstruction of the Intervention: 0
small bowel, stomal Control: 2/187 (1.1%)
surgery or bypass Topic-specific
surgery, outcomes: NR
preoperative Reoperations: NR
infectious diseases, Length of stay, d:
penicillin or meanSD
cephalosporin Intervention: 12.57.4
allergy, antimicrobial Control: 12.25.6
administration before P=0.66
hospitalization, With incisional SSI: n=35
inflammatory bowel 14.69.3
diseases, angina or Without incisional SSI:
myocardial n=342
infarction, mild or 12.16.2
severe renal P=0.03
2017 American Medical Association. All rights reserved. 167
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
dysfunction, mild or Mortality: NR
severe diabetes Adverse events:
mellitus, and steroid Postoperative
administration before Complications [Mainly
surgery Small Bowel
Obstruction]
Intervention: 18/190
(9.5%)
Control: 18/187 (9.6%)
P= 0.96
Mohri RCT To compare Number of patients: Intervention group: SSI: (follow up 6 weeks) Definitions: CDC:
53
2007 1, 4, 6, the efficacy of N= 486 n=243 Overall: 44 (9.1%) Incisional SSI:
(ES) 7, 8, 9 single- and Patient Single does prophylaxis Intervention: 23 (9.5%) Infection
multiple-dose Characteristics: Cefazolin 1 g IV: n=122 Control: 21 (8.6%) occurring within
antimicrobial Baseline (50.2%) Difference %: 0.9 (-4.3, 30 days after
prophylaxis for characteristics were Ampicillin-Sulbactam 1.5g: 5.9) operation and
the prevention similar between n=121 (49.8%) 3 patients in the involving skin,
of surgical-site groups. 30 minutes prior to intervention group had subcutaneous
infection in Age, y: mean (range) surgery, patients an infection that tissue or deep
patients Intervention: 68 (22- received either 1g involved both the soft tissue (e.g.
undergoing 91) cefazolin or 1.5 g incisional and deep or fascial and
elective Control: 68 (23-90) ampicillin-sulbactam by organ/space sites muscle layers) of
gastric cancer Gender: no male (%) slow intravenous Incisional the incision site,
surgery. Intervention: 174 infusion over 15 Intervention: 14 (5.8%) and at least one
(71.6%) minutes. An additional Control: 11 (4.5%) of the following
Control: 164 (67.5%) dose was administered Difference %: 1.3 (-2.7, Purulent
2
Obesity, BMI, kg/m , if the operation was 5.2) drainage, with or
Mean(range) prolonged beyond 3h. Organ/Space without laboratory
Intervention: 21.6 Timing of intervention: Intervention: 12 (4.9%) confirmation, from
(13.4-31.6) Preop and intraop if Control: 10 (4.1%) the incision
Control: 21.4 (13.6- procedure lasted >3hrs Difference %: 0.8 (-2.9, Organisms
34.0) Duration of intervention: 4.5) isolated from an
Comorbidities Preop and intraop if Other infections: NR aseptically
Diabetes Mellitus (no procedure lasted >3hrs Topic-specific obtained culture of
Intervention: 17/243 vs. perioperative in outcomes: fluid or soft tissue
(7.0%) controls for total 7 AMP Antimicrobial Resistance: from the incision
Control: 19/243 doses ( at 12hr intervals 33/47 (70.2%) SSIs had At least one of
(7.8%) ) purulent discharge and the following signs
Gastric Cancer: T1/ T2- Device/agent: cefazolin were cultured. or symptoms of
2017 American Medical Association. All rights reserved. 168
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
4 1g IV or ampicillin- 13/33 (39.3%) were infection: pain or
Intervention: 94/149 sulbactam 1.5g (V culture positive tenderness,
Control: 108/135 Monitoring intervention: S. aureus: 3 Intervention; localized swelling,
Operative details: Control group: n=243 2 control redness, heat or
o
Blood loss: mean Multiple dose prophylaxis MRSA: 2 intervention 2 fever (38 C)
(range) Cefazolin: n=121 (49.8%) control Spontaneous
Intervention: 338 (10- Ampicillin-sulbactam: E. faecium 1 control wound dehiscence
2811) n=122(50.2%) Streptococcus spp. 1 Abscess or other
Control: 405.7 (10- 30 minutes prior to control evidence of
2917) surgery, patients E. coli 1 intervention infection involving
P=0.028 received either 1g S. marcescens 1 the fascia or
cefazolin or 1.5 g intervention muscle layer found
Extent of Lymph node ampicillin-sulbactam by Enterobacter spp 1 on direct
resection slow intravenous intervention examination,
D0 or D1 infusion over 15 There were no appreciable during reoperation,
Intervention: 92/243 minutes. An additional differences between or by
(37.9%) dose was administered groups in the resistance histopathological
Control: 112/243 if the operation was pattern of isolates. or radiological
(46.1%) prolonged beyond 3h. examination.
D2 The same dose of Reoperations: NR Organ/space SSI:
Intervention 151/243 antibiotics was given at Length of stay: NR Infection occurring
(62.1%) 12 hour intervals Mortality: NR within 30 days
Control: 131/243 postoperatively to Adverse events: AMP after operation and
(53.9%) achieve a total of 7 was not associated with involving the intra-
antibiotic doses. any major side effects abdominal cavity
Procedures: Elective Standard preventive and at least one of
gastric cancer measures: the following:
surgery Hair removal: Hair was Purulent
Total or proximal shaved using electric discharge from a
gastrectomy/ distal clippers after induction drain placed
gastrectomy/ wedge of general anesthesia through a stab
resection/ Skin prep: surgical site wound into the
gastrojejunostomy was wiped with 10% intra-abdominal
Intervention: povidone-iodine cavity
78/147/2/16 solution before surgery Organisms
Control: 94/141/1/7 and draped with a isolated form an
Indications: gastric disposable towel. aseptically
cancer Closure: Absorbable obtained culture of
Setting: 10 centers synthetic sutures were fluid or tissue in
2017 American Medical Association. All rights reserved. 169
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Location: Japan used for closure of the the intra-
Dates: May 2001 fascia and peritoneum. abdominal cavity
December 2004 Skin was closed using Abscess or other
Inclusion Criteria: stainless steel staples evidence of
Patients undergoing and the wound then infection involving
elective gastric wiped with normal the intra-
cancer surgery in saline. Staples were abdominal cavity
one of ten centers. removed after 7 days. found on direct
Exclusion Criteria: Drains: Intra-abdominal examination,
Aged<20 years, drainage tubes were during reoperation,
pregnant, allergic to passed through a stab or by
penicillins or incision separate from histopathological
cephalosporins, had the wound. They were or radiographic
received removed within 48h of examination.
antimicrobial surgery Perioperative
treatment in the past Local antimicrobial care: See
2 weeks, had an Irrigation: None standard
infection at the time Adhesive dressing: site preventive
of surgery, had kept covered with an measures
malignant disease of adhesive dressing until Other notes: None
another organ, or removal of the staples. Follow-up:
had colorectal Non-standard preventive Patients
resection at the time measures: assessed daily
of surgery. Also, Antimicrobial prophylaxis until discharge
moderate or severe choice: choice of cefazolin with
liver disease or ampicillin-sulbactam postoperative
(alkaline was left to the operating follow-up at 6
phosphatase, surgeon who was blinded weeks by an
alanine to treatment schedule. independent
aminotransferase, investigator at
aspartate each institution.
aminotransferase or Funding Source
total bilirubin more Conflicts:
than 5 times the Authors: NR
upper limit of Institution: NR
normal) and sever Study: NR
renal impairment Supplies: NR
(serum creatinine
level above 2.0
2017 American Medical Association. All rights reserved. 170
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
mg/dl.)
Togo RCT To investigate Number of patients: Intervention group: n= SSI: (follow up 30 days) Definitions:
55
2007 1, 2, 6, two different N=180 89 Total SSI SSI: CDC
(ES) 7, 8, 9, postoperative Patient 1g fluorometholone was Intervention: 4/89 (4.5%) Guideline
10 durations of Characteristics: administered 30 Control: 4/91 (4.4%) definitions for
antimicrobial There were no minutes before surgery, P=0.033 Prevention of
prophylaxis significant followed by 1g every 3 Intra-abdominal infection Surgical Site
administration differences in any hours during surgery, (infection at cut surface Infection were
(fluorometholo category between 1g 2 hours after of liver= Organ/Space) used.
ne) after groups. completion of surgery, Intervention: 2/89 (2.2%) Inflammatory
elective Age, y: mean SD and then 1g every 12 Control: 3/91 (3.3%) findings (fever
hepatectomy Intervention: hours)for 2 days Wound infection and flare,
and their 62.811.2 postoperatively (Incisional) drainage of pus
respective Control: 61.610.7 Timing of intervention: Intervention: 2/89 (2.2%) from incision, or
impact on the Gender: m/f Pre-, intra-, and Control: 1/91 (1.1%) drain, detection
incidence of Intervention: 55/34 postoperatively Statistically Significant of a pathogen by
SSI and Control: 61/30 Duration of intervention: Postoperative infection culture of fluid
Systemic Obesity: NR Beginning 30 minutes Risk Factors or tissue sample
inflammatory Comorbidities before surgery and Infected n=13 and fluid
response Diabetes Mellitus (-//+) continued for 2 days vs. Non-infected: n=167 retention on
syndrome Intervention: 70/5/14 5 days in controls Duration of operation, min: imaging
(SIRS). Control: 68/5/18 Device/agent: meanSD indicating
Specifically, 2- Operative findings: fluorometholone 1g IV Infected: 494106 presence of pus
day versus 5- No significant Monitoring intervention: Non-infected: 352107 in a deep region.
day difference between Hematological and P<0.001 Cases judged as
postoperative groups in terms of biochemical tests were Bile Fistula (+/-) SSI by physician
regimens. resection rates, number performed before Infected: 4/9 included even if
of liver segments surgery, immediately Non-infected: 4/163 pus drainage
resected, prognostic after surgery, and P<0.001 and culture
score, operation time, additional tests were negative.
2017 American Medical Association. All rights reserved. 171
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
blood loss or blood performed as needed. Other infections: Systemic
transfusion Control group: n=91 Remote Infections Inflammatory
Procedures: Elective 1g fluorometholone was Intervention: 3/89 (3.4%) Response
Hepatectomy without administered 30 Control: 2/91 (2.2%) Syndrome
the reconstruction of minutes before surgery, P=0.242 (SIRS): the
the biliary or followed by 1g every 3 Catheter Infection consensus
intestinal tract hours during surgery, Intervention: 2/89 (2.2%) criteria
Indications: 1g 2 hours after Control: 2/91 (2.2%) established by
Hepatocellular completion of surgery, Pneumonia the American
carcinoma/ liver and then 1g every 12 Intervention: 1/89 (1.1%) Thoracic Society
metastasis/ donor/ hours for 5 days Control: 0/91 and the Society
other postoperatively Postoperative infections of Critical Care
Intervention: 33/43/4/9 Standard preventive total (SSI + RI) Medicine were
Control: 33/45/5/8 measures: Intervention: 7/89 (7.9%) used. When 2/ 4
Setting: 1 University ABX prophylaxis: No Control: 6/91 (6.6%) of the following
Hospital patient received pre- P=0.049 criteria were
Location: Japan operative administration SIRS Positive Rate present:
Dates: April 2003 of oral antimicrobial At Postop day 2 Body
March 2006 agents. Intervention: 26/89 temperature of
36 C and 38 C
o o
Inclusion Criteria: (31.7%)
Patients who Control: 12/91 (14.1%) A pulse rate of
underwent elective P=0.007 90/min
liver resection for At Postop day 3 A respiratory rate
hepatic lesions. Intervention: 12/89 of 20/min or
Exclusion Criteria: (14.6%) PaCO2> 32 torr
Patients who were Control: 4/91 (4.7%) White blood cell
concomitantly P=0.029 counts of
treated with the After Postop day 3 12,000/mm and
3
resection of other Intervention: 6/89 (7.3%) 4,000/mm or
3
organs resection Control: 5/91 (5.9%) 10% immature
and anastomosis of P=0.709 cells
the bile duct; SIRS Duration all (mean) Biliary
drainage and Intervention: 1.34 days Complications:
resection and Control: 0.95 days Drainage of bile
anastomosis of the P=0.065 from the
digestive tract and abdominal wound
patients In whom Topic-specific and drain, showing
apparent infection outcomes: a total bilirubin
was noted at the Treatment: when post- level of >5mg/mL
2017 American Medical Association. All rights reserved. 172
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
time of surgery. operative infection was or 3 times the
Also, patients with a diagnosed during the serum level in the
past medical history study, the treatment discharge fluid.
of allergic reaction to was changed to An intra-
-lactams, a pre- therapeutic abdominal
operative serum antimicrobial agents. accumulation of
creatinine level of Diarrhea: bile confirmed by
1.5 mg/dL, diabetes Intervention: 2/89 (2.2%) percutaneous
mellitus under insulin Control: 0/91 drainage
control, treatment
with antimicrobials P=0.150 Cholangiographic
within 1 week before No cases of C. difficile evidence of bile
surgery, judged detected. leakage.
ineligible by the Post-operative
attending physician, Reoperations: NR complications:
and non-consent to Length of stay: conditions in which
the study. Intervention: 15.246.84 the admission
days period after
Control: 15.116.07 surgery exceeded
days 22 das
P=0.896 (meanSD),
Perioperative
Mortality: None during the care: NR
admission period in Other notes:
either group None
Adverse events: Follow-up: 30
No severe complications days after
observed. surgery
Funding Source
Conflicts:
Authors: None
Institution: None
Study: None
Supplies: None
Ali RCT To compare Number of patients: Intervention group: SSI Definitions:
17
2006 4, 5 the proportion N=200 n=100 All SSI Wound evaluation:
(ES) of early Patient 1dose: 1 dose of 2g 1dose: 8/100 (8%) done using the
postoperative Characteristics:Age, ceftazidime Multi: 6/100 (6%) prescribed
infection y: NR intravenously 30 proforma for
2017 American Medical Association. All rights reserved. 173
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
cases in clean Gender: NR minutes before the Deep SSI postoperative
orthopedic Obesity: NR initial operative incision Total: 4/200 (2%) fever developing
surgery after a Comorbidities: NR and 2 placebo doses 1 dose: 1% or persisting
single dose of Procedures: mix of after 12h each. Multi: 3%; 48hours after
prophylactic clean orthopedic Timing of intervention: p=0.34 the surgery,
antimicrobial fracture surgeries pre and postop. discharge from
and multiple Setting: 1 public Duration of intervention: Superficial SSI the wound, and
doses of hospital preop up to 24h postop. Total of 10 (5%) superficial overlying skin
prophylactic Location: Pakistan Device/agent: SSIs and no difference:: inflammation.
antimicrobial Dates: April 2004 ceftazidime. 1dose: 7% Wound infection
March 2005 Control group: n=100 Multi: 3%; was noted to be
Inclusion Criteria: Any 3dose: 1 dose of 2g p=0.21 superficial or
age and either ceftazidime deep.
gender undergoing intravenously 30 Antimicrobial resistance: Other notes: None
clean orthopedic minutes before the Staphylococcus aureus Follow-up: 28
surgery and initial operative incision was the commonest days
available for and 2 doses after 12h organism isolated, Funding Source
complete follow-up. each. followed by E. coli. Conflicts:
Exclusion Criteria: Eight of the 14 SSIs Authors: NR
Patients with any Standard preventive had a negative wound Institution: NR
generalized measures: culture (7 superficial, 1 Study: NR
debilitating disease, Weight adjusted dosing: in deep). No mention of Supplies: NR
diabetes mellitus, patients under 12y, the resistance
any infective focus in antimicrobial
the body, poor prophylaxis dose
quality of the skin at adjusted for weight.
the incision site,
allergy to
cephalosporin, open
fracture, revision
surgery within last 6
weeks, use of
antimicrobials within
the last 7 days and
duration of surgery
>3h.
2017 American Medical Association. All rights reserved. 174
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Mui RCT To investigate Number of patients: Intervention1 group: n= SSI: (follow up 30 days) Definitions:
11
2005 1, 6, 7, the infective N=269 92 Intravenous Wound infections Wound infection:
(ES) 8, 9 complications Patient cefuroxime (1.5g) and Intervention1: 6/92 discharge of pus
rate after open Characteristics: All metronidazole (500mg) (6.5%) that required
appendectomy baseline were given at induction Odds Ratio (95% CI): surgical
for non- characteristics were of general anesthesia. 1 drainage before
perforated comparable Intervention2 group: n= Intervention2: 6/94 discharge
appendicitis Age, y: mean (SD) 94 Intravenous (6.4%) Intra-abdominal
(NPA)receivin Intervention1: 36.3 cefuroxime (1.5g) and Odds Ratio (95% CI): collection or
g different (15.6) metronidazole (500mg) 1.01 (0.34-3.26) abscess: a fluid
durations of Intervention2: 32.1 were given at induction Control: 3/83 (3.6%) collection
prophylactic (13.2) of general anesthesia Odds Ratio (95% CI): diagnosed at
antimicrobials Control: 35.1 (13.4) followed by two more 0.89 (0.46-7.79) ultrasound or
cefuroxime P=0.12 doses of IV P I1&I2=0.97 computed
and Gender: m/f antimicrobials. P I1orI2 & C= 0.5 tomography
metronidazole Intervention1: 65/27 Timing of intervention: which required
perioperative Intervention2: 66/28 Pre operatively All required local wound drainage
regimens: Control: 54/29 Duration of intervention: exploration with daily C. difficile
1) single dose P=0.68 Single dose at induction dressing enterocolitis-
preoperative, Obesity: NR of anesthesia vs. up to All infected wounds healed diagnosed by
2) 1 preop and Comorbidities: NR 5 days postoperatively by 30-days positive fecal
2 postop Procedures: for controls postoperative follow up. clostridium toxin
(three-dose/1- Emergency open Device/agent: Intra-abdominal Perioperative
day) and appendectomy Intravenous cefuroxime Infections/abscesses care:
3) preop and through right lower 1.5g, and No patients developed Discharge: when
5-days postop quadrant incision metronidazole 500mg. intra-abdominal fully mobilized,
using muscle Monitoring intervention: collection or abscesses. could tolerate a
splitting approach NR Other infections: NR normal oral diet
and appendices Control group: n= 83 Topic-specific with evidence of
were removed in the Intravenous cefuroxime outcomes: bowel activity
standard fashion (1.5g) and The incidence of AMP- (normal bowel
Indications: acute non- metronidazole (500mg) related complications sounds and
perforated given at induction of was significantly higher passing flatus or
appendicitis general anesthesia in the control group (5d) stool), apyrexial
o
Setting: 1 university followed by a 5-day as compared with for 12h (<37 C
hospital course of Intervention 1 (single tympanic), and
Location: China antimicrobials. IV dose): had adequate
Dates: July 1995 Antimicrobials were OR, (95% CI) pain control on
December 2000 administered until 1.05(1.001-1.1); oral analgesics.
2017 American Medical Association. All rights reserved. 175
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Inclusion Criteria: patients could tolerate a P=0.048 Other notes: Study
Patients aged 15-70 semi-solid or solid diet C. difficile enterocolitis is underpowered
with the clinical when IV antimicrobials Intervention1 (single Patients were
diagnosis of acute, were substituted by oral dose): 0/92 randomized after
non-perforated formula: 250mg Odds Ratio (95% CI): open
appendicitis cefuroxime 2x/day and 1 appendectomy
undergoing 400mg metronidazole Intervention2 (3d): 1/94 determined NPA
emergency open 3X/day (1.1%) Follow-up: After
appendectomy Standard preventive Odds Ratio (95% CI): discharge all
Exclusion Criteria: measures: 1.01 (0.99-1.03) patients were
Patients who had a Closure: The peritoneum, Control (5d): 4/83 (4.8%) followed up at
history of oblique muscles and Odds Ratio I1 vs. C 10 days
preadmission the Scarpas fascia (95% CI): 1.05 (1.001- postoperatively
antimicrobials, closed with 3/O 1.1) for wound
diabetes mellitus, polyglycolic sutures and P I1&I2=1.0 assessment and
steroid therapy, the skin was closed P I1 & C= 0.048 via stitches removal
known drug allergy with interrupted vertical Fishers exact test and the second
to the study mattress with 3/O All cases of C. diff follow up was
antimicrobials, monofilament sutures in enterocolitis recovered conducted for
ruptured appendicitis a standardized manner. uneventfully after 7d wound problems
and appendicular Peritoneal lavage: none course of oral occurring at 30
mass or abscess Wound Lavage: none vancomycin days
formation. Also, Local antimicrobials: Reoperations: postoperatively
pregnant women none By definition (see next Funding Source
and patients who column) all wound Conflicts:
refused consent. infections (15/15) Authors: NR
required surgical Institution: NR
drainage Study: NR
All infections were treated Supplies: NR
by laying open the
wound site, and
packing with normal
saline ribbon gauze
twice per day to allow
healing by secondary
intention.
All infected wounds were
healed at 30d f/u
Length of stay, d: mean
2017 American Medical Association. All rights reserved. 176
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
(SD)
Intervention1: 4.3 (1.3)
Intervention2: 4.6 (1.2)
Control: 4.8 (2.3)
P=0.13
Mortality: No
perioperative mortality
Adverse events: See
topic specific events for
AMP adverse events
Chang RCT To investigate Number of patients: Intervention group: n=74 SSI: (follow up within 7 Definitions:
41
2005 (pilot whether a N=156 Intravenous push stat of days of discharge) Operative site
(ES) study) short course Patient 2g cephalothin followed Operative Site Infection infection:
1, 2, 9, of Characteristics: No by a 1g injection every Intervention: 2/74 (2.7%) includes pelvic
10 antimicrobials differences in patient 6 hours. Gentamycin 1/2: Trocar site wound cellulitis, vaginal
(<24 hours or operative began with an 80mg IV infection cuff abscess,
between the characteristics drip followed by a 60- 1/2: 1 cuff abscess pelvic abscess,
first and final between groups. 80mg injection every 8 Control: 3/82 (3.6%) and wound
doses) is as Age, y: mean SD hours. The first dose 1/3: infection infection
efficacious as Intervention: 41.15.8 was administered within 1/3: cellulitis (Sharpiro 1982)
longer courses Control: 42.37.1 1 hour prior to the 1/3: trocar site wound Urinary tract
(30-60 hours) Gender: 100% Female incision and continued infection during infection (UTI):
in Obesity: NR for <24 hours hospitalization (instead diagnosed from
laparoscopical Comorbidities: NR Timing of intervention: of within 7 days of patients
ly assisted Pre and postoperatively discharge) symptoms and
vaginal Procedures: Duration of intervention: P=0.735 signs and to
hysterectomy Laparoscopically From 1 hour prior to whether there
(LAVH). assisted vaginal incision to either <24 Other infections: Urinary was a positive
hysterectomy hours or 30-60hours Tract Infection: urinalysis
(LAVH) Device/agent: Intervention: 2 (2.7%) Perioperative
Indications: Cephalothin 2g IV and 1/2: during care: NR
Myoma uterus: 70 gentamycin 80mg IV hospitalization Other notes: Pilot
Intervention: 37 Monitoring intervention: 1/2: w/in 7 days of study with low
Adenomyosis: 53 NR discharge power to
Intervention: 28 Control group: n=82 Control: 2 (2.4%) determine
Cervical carcinoma in Intravenous push stat of 2/2: w/in 7 days of statistically
situ: 17 2g cephalothin followed discharge significant
Intervention:10 by a 1g every 6 hours. P=0.917 differences in
Cervical carcinoma Ia1: Gentamycin began with the rate of
2017 American Medical Association. All rights reserved. 177
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
9 an 80mg IV drip Topic-specific operation site
Intervention:3 followed by a 60-80mg outcomes: NA infection and UTI
Other: 7 injection every 8 hours. Reoperations: NR between the 2
Setting: 1 medical The first dose was Length of stay, groups. To
center injected within 1 hour d:meanSD achieve power
Location: Taiwan prior to the incision and Intervention: 4.31.1 of 0.80, 3,800-
Dates: June 2001-July continued for 24 hours Control: 4.21.3 5,200 cases in
2002 P=0.89 both groups
Inclusion Criteria: Standard preventive Mortality: NR would be
Patients undergoing measures: Adverse events: NR necessary
LAVH. Preop serum NR Follow-up: Within
hemoglobin 7 days of
level>9g/dL and discharge
normal renal function collected from
tests (serum patients charts
BUN/Creatinine) Funding Source
Exclusion Criteria: Conflicts:
LAVH cases with Authors: None
complications and Institution: None
those patients who Study: None
required therapeutic Supplies: None
antimicrobials and
other associated
surgical procedures
were excluded from
the study
Su RCT To compare Number of patients: Intervention group: n= SSI: (follow up 90 days) Definitions:
13
2005 1, 2 the efficacy of N=531 267 Serious infectious Infectious
(ES) a single-dose Patient One dose of 1g cefazolin morbidity morbidity:
versus a 1-day Characteristics: intravenously before Intervention: 1/267 If body temperature
course of (N=548 before 17 surgery upon induction (0.37%) was greater than
o
prophylactic patients excluded of anesthesia by the 1/1: Trocar wound 38.5 C, the
antimicrobials due to loss to f/u) anesthesiologist within infection at postop day patient was
for There were no 30 minutes before 27 from LAOC surgery assessed for
postoperative differences between surgery. If the surgery Control: 1/264 (0.37%) signs and
wound groups regarding duration was greater 1/1: vaginal cuff symptoms of
infection general status than 4h, and additional infection with pelvic infection
outcomes and Age, y: meanSD dose of 1.g cefazolin abscess at postop day including one or
cost- Intervention: administered 7 from LAVH surgery more of the
2017 American Medical Association. All rights reserved. 178
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
effectiveness 45.779.74 intravenously. following:
in gynecologic Control:45.189.31 Timing of intervention: Other infections: An abdominal
o
operations. Gender: 100% Female Pre, intra and Fever (>38.5 C on two wound infection or
2
Obesity: BMI, kg/m , postoperatively occasions 4 or more trocar wound
meanSD Duration of intervention: hours apart excluding infection (including
Intervention: Either preoperatively, or the night of surgery) wound discharge
23.211.13 Preoperatively through Intervention: 112 or abscess)
Control:23.321.05 24 hours /267(41.9%) Pelvic Abscess or
Comorbidities: NR postoperatively. 67/112 had blood tubo-ovarian
Wound classification: Device/agent: Cefazolin drawn for cultures but abscess
Clean: LAOC 1g IV none had septicemia Vaginal cuff
Clean contaminated: Monitoring intervention: Control: 120/264 abscess
TVH, TAH, LAVH NR (45.4%) Postoperative
Operative Control group: n= 264 74/112 had blood septicemia
characteristics: One dose of 1g cefazolin drawn for cultures but
Duration of surgery, intravenously before none had septicemia Perioperative
min: surgery upon induction Topic-specific care:
meanSD of anesthesia by the outcomes: Anesthesia
Intervention: anesthesiologist within Timing of AMP before Genera/spinal
98.1435.54 30 minutes before incision, min: meanSD Intervention
Control: 98.8735.48 surgery followed by Intervention: 21.079.96 n=273: 257/16
Procedures: Total another three doses of Control:22.7013.22 Control
vaginal 1g cefazolin every 6hr n=275:260/15
hysterectomy (TVH) after surgery X1 day. If Antimicrobial resistance:
Total abdominal the surgery duration none reported. Other notes: NNIS
hysterectomy (TAH) was greater than 4h, Intervention trocar wound SSI risk
Laparoscopic-assisted and additional dose of culture: P. aeruginosa stratification.
vaginal 1.g cefazolin was Control vaginal cuff Follow-up:
hysterectomy administered cultures: E coli, B. During
(LAVH) intravenously. fragilis hospitalization,
Laparoscopic assisted Standard preventive Reoperations: abdominal and
ovarian cystectomy measures: There were Intervention: Infection perineal exams
(LAOC) no differences between required debridement of were performed
LAOC/LAVH/TAH/TVH groups regarding trocar wound and daily by
Intervention: preoperative drainage with pen-rose gynecological
36/190/27/20 examination and drain. Readmission stay staff to assess
Control:34/195/25/21 preparation, skin was 8 days for infection. If
Indications: NR disinfection, Control: Infection & signs/symptoms
Setting: 1 hospital postoperative abscess required developed,
2017 American Medical Association. All rights reserved. 179
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Location: Taiwan intravenous fluid drainage with pen-rose examiner
Dates: June 1, 2001 therapy (for 36h only), drain and readmission collected
January 31, 2003 and indwelling urethral stay was 4 days. samples from
Inclusion Criteria: catheterization (for 24h Length of stay, days, pelvic cavity and
Women 18 years only). meanSD wound site for
old scheduled to Skin Prep: The surgical Intervention: 3.971.27 culture before
undergo elective site was prepared by Control:4.021.51 initiating
vaginal or abdominal swabbing with antimicrobial
hysterectomy (total povidone-iodine or Mortality: NR therapy.
vaginal alcoholiodine for Adverse events: NR After discharge: 90
hysterectomy (TVH) about 5 min and days
and total abdominal Hair removal-trimming/ postoperatively
hysterectomy (TAH), shaving of the surgical at the first,
laparoscopic- area according to the second and third
assisted vaginal standard practice in months after
hysterectomy or our hospital (did not surgery, vital
ovarian cystectomy specify how many in signs, physical
(LAVH or LAOC) for each). examination,
nonmalignant and pelvic
disease. sonography
Exclusion Criteria: were performed
Women who had when patient
major surgery in the returned to the
month before clinic for
elective gynecologic evaluation.
surgery, had known Funding Source
or suspected Conflicts:
hypersensitivity or Authors: None
intolerance to Institution: None
cephalosporin, or Study: None
had any coexisting Supplies: None
disease that would
require antimicrobial
therapy during the
study. Also, patients
who had taken
antimicrobials the
week before surgery
2017 American Medical Association. All rights reserved. 180
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Carroll RCT To clearly Number of patients: Intervention group: n= SSI: (follow up: Definitions:
40
2003 1, 4, 8, address the N=74 35 discharge or 7days Head and neck
(ES) 9, 10 duration of Patient Short course (1 day): postop) wound and
antimicrobial Characteristics: No 900mg Clindamycin Wound infection donor site
prophylaxis statistically intravenously initiated Intervention: 4/35 (11%) evaluated for:
(either 3 significant difference immediately Control: 4/39 (10%) Wound color
doses [1 day] existed between preoperatively to total 3 P=0.99 1: normal
or 15 doses [3 study groups or doses every 8 hours. 2: pink
days]) in between patients Timing of intervention: Other infections: 3: red or swollen
patients with with and without Pre and postoperatively Women were more likely Drainage
head and neck complications (data Duration of intervention: than men to develop 1: none
cancer listed below is for From preoperatively to Remote Infections 2: serious
requiring free- entire population (N). 16-56 hours (specifically UTI) 25% 3: purulent
flap Age, y: postoperatively. vs. 2%; P=0.004 Wound infection
reconstruction meanSD61.612.5 Device/agent: Other/ remote infections A wound was
of cancer range 21-88 years Clindamycin (including UTI & considered
defects. Gender (m/f): 46/28 Monitoring intervention: enterocolitis) infected when
Obesity: NR NR Intervention: 4/35 (11%) the color
Comorbidities: NR Control group: n= 39 Control: 4/39 (10%) became red or
Previous radiotherapy: Long Course (3 days) P=0.99 the wound was
24/74 (32%) 900mg Clindamycin swollen. A pink
Flap Type: intravenously initiated Topic-specific wound that
Fibula/jejunum/radial preoperatively to total outcomes: developed
forearm/rectus: 15 doses every 8 hours. purulent
9/19/31/15 C. difficile enterocolitis: drainage was
Tumor site: Buccal/floor Standard preventive 1/74 (1%) they dont also considered
of measures: NR specify in which group infected.
mouth/hypopharynx/ Reoperations: NR
larynx/maxilla/ Length of stay: NR Perioperative
oropharynx/roof of Mortality: care: NR
mouth/ tongue: Intervention: 1/35 (3%) Other notes:
5/15/14/7/11/8/10/4 Control: 1/39 (3%) Accrual of
Procedures: Surgical P=0.99 patients for the
ablation of head and study was
neck malignancies Adverse events: stopped when
with immediate free- Pharyngocutaneous annual review of
flap reconstruction Fistula the data
including: radial Intervention: 3/35 (9%) disclosed that
forearm, jejunum, Control: 3/39 (8%) differences
2017 American Medical Association. All rights reserved. 181
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
rectus and fibula by P=0.99 between the
descending order of Postoperative fistula was study groups
frequency. more common in men were much lower
Indications: (n) but P=0.08 than those
Stage II/III/IV: 7/21/46 Flap Necrosis projected in
(91% stage III or IV) Intervention: 0/35 initial sample
Setting: 1 center Control: 1/39 (3%) size
Location: USA P=0.99 determinations.
Dates: January 1, Vascular Compromise of A difference of
1998- April 30, 2001 flap 1%, recalculated
Inclusion Criteria: Intervention: 2/35 (6%) estimate of
Patients scheduled Control: 1/39 (3%) sample size for 2
to undergo surgical P=0.99 sided
ablation of head and significance level
neck malignancies of 0,005 with
with immediate free- 80% power
flap reconstruction would require
Exclusion Criteria: more than
Patients undergoing 10,000 subjects
secondary in each
reconstruction and treatment arm.
those whose tumor Follow-up:
did not involve the Wounds were
mucous membranes evaluated daily
of the upper for 7 days
aerodigestive tract postoperatively
(or until
discharge) by a
blinded faculty
head and neck
surgeon.
Funding Source
Conflicts:
Authors: None
Institution: None
Study: None
Supplies: None
2017 American Medical Association. All rights reserved. 182
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Hall RCT To compare Number of patients: Intervention group: n= SSI: (follow up 42 days Definitions:
38
1998 1, 2, 6, the incidence N=302 153 postop) Wound infections:
(ES) 7, 8, 9 of wound Patient Single Dose Overall rate of wound discharge of pus
infection after Characteristics: 3g ticarcillin/ 0.1g morbidity: (wound + minor or a serous
emergency Both groups were clavulanate by slow wound): 101/302 (34%) discharge that
elective comparable with intravenous infusion contains
vascular respect to putative (over 30 minutes) Wound infection: 43/302 pathogenic
surgery risk factors for a immediately after the (14%) organisms
following the wound infection at induction of anesthesia. Intervention: 28/153 Graft infection: an
administration baseline and during Patients received an (18%) overt clinical event
of the same the perioperative additional dose if the Control: 15/149 (10%) characterized by
agent as period. surgery was prolonged P=0.041 the need for
either short- Age, y: median (range) beyond 3 hours. Relative risk estimate aggressive
term Intervention: 70 (64- Timing of intervention: (95%CI) interventions and
prophylaxis or 75) Pre, intra and = 2.00 (-1.02-3.92) confirmed by
a multiple Control: 69 (64-76) postoperatively Median time to microbiology.
dose regimen. Gender: m/f Duration of intervention: presentation of wound Minor wound
Intervention: 116/37 From immediately after infection: 13 days infections: Local
Control: 103/46 the induction of (range: 2-43 days) abscess or
2
Obesity, BMI, kg/m , anesthesia to vs. five Minor wound infections: serous
mean (range) days in controls. 58/302 (19%) discharge not
Intervention: 25 (22- Device/agent: 3g Intervention: 35/153 meeting their
27) ticarcillin/ 0.1g (23%) established
Control: 24 (22-27) clavulanate Control: 23/149 (15%) criteria for
Comorbidities Monitoring intervention: Graft infection: 2/302 wound infection
IDDM: NR (<1%)
Intervention: 3/153 Control group: n= 149 Intervention: 1/153 Vascular surgery:
(2%) Multiple Dose (<1%) All open arterial
Control: 3/149 (2%) 3g ticarcillin/ 0.1g Control: 1/149 (<1%) procedures.
NIDDM: clavulanate by slow Patients undergoing lower Shock: (Dellinger
Intervention: 31/153 intravenous infusion limb surgery had 1985)
(20%) (over 30 minutes) greatest risk of wound clinical signs of
Control: 16/149 (11%) immediately after the infection (24/95 or 25%) reduced
Current Smoker induction of anesthesia. Other infections: NR peripheral
Intervention: 53/153 Patients received an Topic-specific perfusion plus
(35%) additional dose if the outcomes: any two of the
Control: 39/149 (26%) surgery was prolonged No major side effects following:
Previous myocardial beyond 3 hours. After associated with the Systolic blood
infarction the initial dose, patients parenteral pressure (BP) <80
2017 American Medical Association. All rights reserved. 183
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Intervention: 38/153 received 3g ticarcillin/ administration of AMP mm HG for 1 hour
(25%) 0.1g clavulanate Pulse rate
Control: 37/149 (25%) intravenously at 6 Diarrhea with C. difficile >120bmp (sinus
Previous stroke hourly intervals for a Intervention: 2/153 minute rhythmia)
Intervention: 20/153 maximum total of 20 (1.3%) for more than 1
(13%) doses (i.e., until the Control: 1/149 (0.7%) hour
Control: 16/149 (11%) lines are removed Urine output less
Previous ischemic but<5 days) Antimicrobial resistance: than 80ml for any
attack Authors state that they 4 hour period
Intervention: 15 Standard preventive did not detect any Use of pressors
(10%) measures: appreciable difference to maintain the
Control: 9 (6%) Skin prep: preoperative in the resistance blood pressure for
Previous cardiovascular chlorhexidine skin patterns of the isolates at least 1 hour.
surgery wash. between groups Obesity: Body
Intervention: 62/153 Wound closure & Drains: (statistical significance mass index (BMI)
(41%) there was uniform not tested) Among weight/ the square
Control: 65/149 (44%) wound closure and several isolates from 25 of the height.
Comparable with drain tubes did not exit patients are the Insulin dependent
regards to operation through wounds. following: diabetes mellitus
type, duration, ABX irrigation: No local S. aureus (IDDM): an
intraoperative shock, irrigation of tissues with Intervention: 5/15 (33%) episode of
wound closure antibiotic solutions. Control: 4/10 (40%) ketoacidosis or
technique, total Diarrhea: Patients with MRSA dependence on
length of wounds postop diarrhea had Intervention: 1/5 SA (20%) insulin
and duration of stools evaluated for or 1/15 isolates (7%) Non-Insulin
drainage in days. enteropathogens. Control: 2/4 SA (50%) or dependent
Intervention vs. Control 2/10 isolates (20%) diabetes mellitus
Use of Cell saver: S epidermis (SE) (NIDDM):
47 (31%) vs. 51(34%) Intervention: 1/15 (7%) indicated by a
Peri-op blood Control: 3/15 (20%) requirement for
transfusion Resistance not reported oral hypoglycemic
32 (21%) vs. 40 (27%) for SE medication
Number of wounds per Length of stay =
patient: Reoperations: number of
1: 86 (56%) vs. 83 Intervention: 16 (10%) postoperative days
(56%) 8/16 Amputation/ in hospital
2: 34 (22%) vs. 41 debridement of tissue Perioperative
(28%) 5/16 Revision of graft care:
3: 31 (20%) vs. 22 2/16 Hemostasis Nosocomial
2017 American Medical Association. All rights reserved. 184
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
(15%) 0/16 CABG infections were
4: 2 (1%) vs. 3 (2%) 1/16 Intestinal managed in
Procedures: Adhesions accordance with
Emergency or Control: 17 (11%) the institutional
Elective: 7/17 Amputation/ antimicrobial
Abdominal aortic debridement of tissue guidelines.
aneurysm: 86/ 302 3/17 Revision of graft Other notes: As
(28.5%) 4/17 Hemostasis might be
Groin-distal bypass: 2/17 CABG expected, the
73/302 (24.2%) 1/17 Intestinal patients tended
Aorto-groin bypass: Adhesions to be elderly and
49/302 (16.2%) Length of stay: median debilitated.
Carotid (range) More intervention
endarterectomy: Intervention: 9/153 (6-13 patients were
37/302 (12.3%) Control: 9/149 (7-13%) smokers,
Miscellaneous lower 86% of patients admitted NIDDM and had
limb: 28/302 (9.3%) to ICU were discharged severe cardiac
Groin procedures: w/in 48 hours. disease.
22/302 (7.3%) Mortality: Follow-up: 42
Other: 7/302 (2.3%) Intervention: 8/153 (5%) days after
Indications: NR Control: 5/149 (3%) surgery
Setting: 1 hospital No patient died as a result Funding Source
Location: Australia of a wound or graft Conflicts:
Dates: January 1993 infection. Authors: NR
October 1995 Adverse events: Institution: NR
Inclusion Criteria: All Administration of Study: Industry
adults undergoing antimicrobials Supplies: NR
Vascular surgery (all Intervention: 37/153
open arterial (24%)
procedures.) Control: 27/149 (18%)
Exclusion Criteria: Requirement of wound
Patients undergoing dressing
endovascular Intervention: 23/153
procedures, (15%)
administration of Control: 22/149 (15%)
antimicrobial agents
within 48 hours of
surgery, a history of
hypersensitivity to
2017 American Medical Association. All rights reserved. 185
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
penicillin, and
profound
comorbidity.
Kow RCT To evaluate Number of patients: Intervention group: SSI Definitions:
22
1995 1, 2, 6 the efficacy of N=1010 n=516 All procedures Wound infection:
(ES) one dose of Patient 1dose CFX: n=252: 2g Total: 58/1010 (5.7%) the presence of
antimicrobial Characteristics cefoxitin intravenously 1dose: 31/516 (6.0%) purulent
vs. 3 doses There was an even on induction of 3dose: 27/494 (5.5%) discharge from
covering the distribution of anesthesia P>0.19 the wound or a
24h patients for each 1dose CTX+M: n=264: 1g serous
postoperative antimicrobial cefotaxime + 500mg 1dose CFX: 17/252 (6.7%) discharge with
period using a regimen. metronidazole on 3dose CFX: 17/254 (6.7%) positive culture
new Procedures: Elective induction of anesthesia of pathogenic
antimicrobial and emergency Timing of intervention: 1dose CTX+M: 14/264 organisms.
prophylaxis intra-abdominal pre and postop (5.3%) Perioperative
consisting of surgeries. Duration of intervention: 3dose CTX+M: 10/240 care: NR
cefotaxime Setting: 2 hospitals. preop and up to 12h (4.2%) Other notes: Study
plus Location: Australia postop was not
metronidazole Dates: September Device/agent: cefoxitin or sufficiently
or cefoxitin 1989 - January 1992 cefotaxime plus powered for
Inclusion Criteria: metronidazole Elective colorectal smaller sub
Patients 16 years Control group: n= procedures analyses.
and older, admitted 3dose CFX: n=254: 2g CTX+M: suggests no Follow-up: 28-41
to the two hospitals cefoxitin intravenously difference day follow-up.
for all types of intra- on induction of Total: 12/138 (8.7%); Funding Source
abdominal surgery anesthesia followed by 1dose: 5/71(7.0%) Conflicts:
(elective and another 2g at 6 & 12h 7/67(10.4%); p =0.48 (28- Authors: NR
emergency) postop 41 day follow up) Institution: NR
Exclusion Criteria: if 3dose CTX+M: n=240: 1g Study: Industry
there was a history cefotaxime + 500mg CFX: suggests no Supplies: NR
of allergy to metronidazole on difference:
cephalosporins, induction of anesthesia Total: 16/135 (11.9%);
penicillin, or followed by 1g of 1dose: 8/65(12.3%)
metronidazole, had cefotaxime at 6 & 12h 3dose: 8/70(11.4%);
received postop. p=0.87
antimicrobials. Also Standard preventive
if operative findings measures: Emergency colorectal
indicated the need Skin prep: PI Solution procedures:
for prolonged Plastic wound protectors: Total: 6/46 (13.0%);
2017 American Medical Association. All rights reserved. 186
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
antimicrobials, or the not allowed. 1dose: 4/21 (19.0%) vs.
need for delayed Bowel Prep: all patients 3dose: 2/25 (8.0%);
primary wound undergoing elective p=0.28
closure were colorectal surgery were
excluded. Also if a given mechanical (non- Appendectomy:
patient died in the 14 antimicrobial) bowel Drug regimen 1: n=112:
days after the prep of up to 3 L of a 1doseCFX: 4/54 (7.4%)
operation with no colonic lavage solution 3dose CFX: 4/58 (6.9%)
evidence of prior to operation. Drug regimen 2: n=117
infection, they were 1doseCTX+M: 2/63
excluded from the (3.2%)
analysis. 3dose CTX+M: 0/54
Esophageal, gastric, and
small bowel surgery
Drug regimen 1: n=82:
1doseCFX: 1/42 (2.4%)
3dose CFX: 3/40 (7.5%)
Drug regimen 2: n=81
1doseCTX+M: 1/41
(2.4%)
3dose CTX+M: 1/41
(2.4%)
Biliary Surgery:
Drug regimen 1: n=158:
1doseCFX: 2/83 (2.4%)
3dose CFX: 2/75 (2.7%)
Drug regimen 2: n=140
1doseCTX+M: 3/76
(3.9%)
3dose CTX+M: 0/64
2017 American Medical Association. All rights reserved. 187
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
McArdle RCT To compare Number of patients Intervention group: n=45 SSI Definitions:
47
1995 1, 7, 8 an oral N=87 Patients administered Total: 20/87 (23.0%) Wound sepsis: the
(ES) ciprofloxacin/ Patient gentamicin 120mg and Single day: 13/45(28.9%) presence of pus
parenteral Characteristics: the metronidazole 500mg 3day: 7/42(16.7%); either
metronidazole groups were intravenously at p=0.18 discharging
regimen with a comparable in in induction of anesthesia spontaneously
parenteral terms of followed by gentamicin or requiring
aminoglycosid characteristics. 80mg and drainage.
e/metronidazol Procedures: colorectal metronidazole 500mg Major wound
e combination surgery at 8h & 16h post-op sepsis: the
commonly Setting: 1 university (3doses total) discharge of pus
used for hospital Timing of intervention: with
prophylaxis in Location: United pre and postop constitutional
colorectal Kingdom Duration of intervention: disturbance
surgery, and Dates: NR 1 shot or 3 days postop Minor wound
the value of Inclusion Criteria: Device/agent: gentamicin infections:
1day versus 3 patients undergoing 120mg or 80mg and patients with
days of colorectal surgery. metronidazole 500mg cellulitis and a
antimicrobial Exclusion Criteria: NR Control group: n=42 positive wound
cover. Patients administered culture.
gentamicin 120mg and Perioperative
metronidazole 500mg care: NR
intravenously at Other notes: NR
induction of anesthesia Follow-up: 4
followed by 80mg weeks post
gentamicin and discharge
metronidazole 500mg Funding Source
3times/ day for 3 days Conflicts:
postop. Authors: NR
Standard preventive Institution: NR
measures: NR Study: Industry
Supplies: NR
2017 American Medical Association. All rights reserved. 188
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Nooyen RCT To compare a Number of patients: Intervention group: SSI: (7 day follow up) Definitions:
33
1994 1, 2, 4, single dose of N=844 n=419 Overall (sternal + leg Wound infection:
(ES) 7, 8 cefuroxime Patient After placement of a wounds): 54/844 diagnosed if all
with their Characteristics: peripheral line in the (6.3%) Note: authors of the following
currently Risk factors and operating room, report it as 5.3% using criteria were
recommended patient patients received N=1016 even though met:
3-day course characteristics were 20mg/kg cefuroxime they excluded 172 Redness
of cefuroxime similar between intravenously at patient from all other Purulent
with regard to groups. induction of anesthesia. final analysis ( see discharge
effectiveness Age range Timing of intervention: NOTE at bottom of Positive culture
in preventing Intervention: 34-86 Pre, intra and results) (if pathogenic
postoperative Control: 33-86 postoperatively Sternal Site organisms were
wound Age>70 years Duration of intervention: Total complications of isolated)
infection. Intervention: 79/419 From induction of healing Infection of the
(18.9%) anesthesia to 3 days Intervention: 58/419 sternum was
Control: 86/425 postop (13.8%) differentiated into
(20.2%) Device/agent: Cefuroxime Control: 56/425 (13.2%) superficial
Gender: m/f Monitoring intervention: P=0.35 infection or
Intervention: 329/90 NR Mediastinitis mediastinitis
Control: 353/72 Control group: n=425 Intervention: 2/419 Mediastinitis:
Obesity: NR After placement of a (0.5%) fever>38C, chest
Comorbidities peripheral line in the Control: 0/425 pain or sternal
Diabetes Mellitus operating room, No cases of late onset instability and a
Intervention: 34/419 patients received mediastinitis were purulent
(8.1%) 20mg/kg cefuroxime reported after discharge discharge from
Control: 41/425 intravenously at from hospital.(but they the mediastinal
(9.6%) induction of anesthesia dont indicate how long area from which
COPD then continued postop) pathogenic
Intervention: 14/419 cefuroxime three times Wound infection microorganisms
(3.3%) a day intravenously for Intervention: 5/419 could be isolated.
Control: 11/425 3 consecutive days. (1.2%) Respiratory Tract
(2.6%) Control: 4/425 (0.9%) infection: If
History of smoking Standard preventive Minor Complication patients were
Intervention: 354/419 measures: Intervention: 51/419 febrile, Gram
(84.5%) SA Decolonization: (12.2%) stain of sputum
Control: 363/425 Starting two days prior Control: 52/425 (12.2%) demonstrated
(82.4%) to surgery, all patients Donor site leg many
Use of corticosteroids undergoing Intervention: n=377 polymorphonucl
Intervention: 10/419 cardiopulmonary Control: n=389 ear leukocytes
2017 American Medical Association. All rights reserved. 189
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
(2.4%) surgery are treated Total complications of and a
Control: 10/425 intra-nasally with a healing predominant
(2.4%)Operative: cream consisting of Intervention: 118/377 organism, and
Primary/ re-operation 0.1% chlorhexidine and (31.3%) the chest X-ray
Intervention: 398/21 0.5% neomycin to Control: 130/389 showed a new
Control: 398/27 eliminate possible (33.4%) pulmonary
Emergency/ elective Staphylococcus aureus. P=0.41 infiltration
Intervention: 411/8 Closure: All skin wounds Wound infection Urinary Tract
Control: 407/18 were closed with intra- Intervention: 5/377 Infection (UTI): if
(18 vs. 8, P<0.08) cutaneous re- (1.3%) the urine culture
though the rate of absorbable sutures Control: 2/389 (0.5%) was positive
(10 cfu/ml) in
5
infection was not Jugular Vein Catheter Minor complications
higher among Removal: catheter was Intervention: 95/377 the presence of
emergency removed after 48 hours (25.2%) fever for which
procedures. in all cases Control: 110/389 no other cause
Donor vessels (28.3%) could be found.
Leg veins only// Left Wound dehiscence Perioperative
internal mammary Intervention: 18/377 care:
artery +/- leg veins// (4.8%) Graft: The internal
Both internal Control: 18/389 (4.6%) mammary artery
mammary arteries Other infections: graft, when
+/- leg veins UTI used, was
Intervention: Intervention: 4/377 harvested on a
94//223//102 (1.0%) pedicle of soft
Control: 118//212//95 Control: 1/389 (0.2%) tissue equal in
Respiratory tract infection width to that of
Procedures: Coronary Intervention: 5/377 both mammary
Artery Bypass (1.3%) veins. Leg veins
Grafting (CABG) Control: 3/389 (0.7%) were obtained
Indications: NR by standard
Setting: 1 hospital Topic-specific measures
Location: The outcomes: NR Postoperative
Netherlands. Reoperations: NR-See samples of
Dates: October 1989 - NOTE below sputum and
December 1990 Length of stay: NR urine and if
Inclusion Criteria: All Mortality: none- See necessary
patients undergoing NOTE below wound exudates
coronary artery Adverse events: NR- see were collected
bypass grafting NOTE below on first and
2017 American Medical Association. All rights reserved. 190
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
(CABG) including following days.
elective and NOTE: Of 1016 patients Other notes: See
emergency surgery, included in the study, results for
primary and 172 were excluded reasons for
reoperation. from final analysis for exclusion from
Exclusion Criteria: the following reasons final analysis
Exclusion from (in some more than one
randomization: reason was present): Follow-up: On the
Refusal of consent, Reason: Intervention seventh day
administration of (n)/control (n) postop, the
systemic Chest open>6h: 42/27 sternotomy and
antimicrobial Repeat thoracotomy within donor site
treatment within the 7 days: 22/30 wounds were
previous 48 h, Intra-aortic balloon pump: examined for
hypersensitivity to 8/6 healing,
cefuroxime or the Artificial ventilation >24h: redness,
presence of 7/10 discharge of
prosthetic valves or Death within 7d (non- fluid without
a vascular infectious): 1/8 ( all died signs of
prosthesis. in OR or did not come infection, or
off IABP) infection by a
Additional antimicrobials: blinded
15/3 physician
Other operative procedure: Funding Source
0/5 Conflicts:
No wound inspection: 1/1 Authors: Industry
They report that neither Institution: NR
wound infection nor Study: Industry
mediastinitis occurred Supplies: NR
in any of these patients
Bernard RCT To determine Number of patients: Intervention group: n= SSI: (follow up 8 days) Definitions: Deep
36
1994 1, 2, 3, whether a N=203 101 Total deep infections: Infections:
(ES) 4, 5, 7, longer Patient 48 hour cefuroxime Intervention: 47/101 46% Wound
8, 9 antimicrobial Characteristics: All A 1.5g dose of cefuroxime Control: 66/102 (65%) infections +
prophylaxis characteristics were was delivered P=0.005 Pneumonia +
regimen for 48 balanced except intravenously at the Difference in infection severe
hours after those with a P-value moment of induction of rates (19%11%) bronchopneumo
pulmonary below anesthesia. A second remained significant (p=- nia +empyema+
operation Age, y: mean (range) dose was .01) after adjusting for fistula)
2017 American Medical Association. All rights reserved. 191
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
decreases the Intervention: 56 (19- systematically delivered multiple variables) Pneumonia:
rate of deep 78) 2 hours later to obtain Wound infection defined on the
infections in Control: 61 (17-81) high seric Intervention: 1/101 (1%) basis of the x-
pleura, P=0.02 concentrations until the Control: 1/102 (1%) ray film with
bronchi and Gender: m/f end of the procedure. P=0.9 specific
parenchyma. Intervention: 91/10 1.5g cefuroxime was Empyema parenchymal
Control: 85/17 given every 6 hours Intervention: 1/101 (1%) features
Obesity: NR after the operation for Control: 6/102 (6%) associated with
Comorbidities 48 hours. The first P=0.03 temperatures
o
Tobacco packs/year: postoperative infusion Pneumonia between 37.5
o
mean (range) was given exactly 6 Intervention: 17/101 38 C.
Intervention: 33 (0- hours after the second (17%) X-ray appearance
120) infusion. Control: 31/102 (30%) Class 1: normal
Control: 33 (0-120) Timing of intervention: P=0.01 Class 2: moderate
Quit Smoking more Pre, intra and Severe infiltrate
than 1 month postoperatively Bronchopneumonia Class 3: important
Intervention: 18/101 Duration of intervention: Intervention: 25/101 infiltrate/atelecta
(18%) From induction of (25%) sis
Control: 15/102 (15%) anesthesia until 48 Control: 25/102 (25%) Severe
P(not significant) hours after the second P=0.9 Bronchopneumo
o
Alcohol: (L/day), mean dose during surgery Fever (>38 C) nia an
(range) Device/agent: Cefuroxime Intervention: 5/101 (5%) association of
Intervention: 0.4 (0-3) Monitoring intervention: Control: 10/102 (10%) purulent
Control: 0.5 (0-5) NR P=0.09 expectorations
Chronic bronchitis: Control group: n=102 and atelectasis
Intervention: 30/101 Flash cefuroxime. Other infections: on the plain
(29.7%) A 1.5g dose of cefuroxime Fistulas chest x-ray film
Control: 36/102 was delivered Intervention: 2/101 (2%) associated with
(35.3%) intravenously at the Control: 7/102 (7%) a temperature
Diabetes moment of induction of P=0.045 higher than
o
Intervention: 5/101 anesthesia. A second 38 C.
(5.0%) dose was Topic-specific Empyemas and
Control: 4/102 systematically delivered outcomes: septicemias:
(3.92%) 2 hours later to obtain Antimicrobial resistance: when associated
Cardiac insufficiency high seric Pathogens cultured with a
Intervention: 5/101 concentrations until the from pleura, bronchi, temperature
(5.0%) end of the procedure. A drains and blood were higher than
o
Control: 6/102 (5.9%) placebo was similar in the two 38 C. As soon
Previous administered every 6 groups. Did not specify as a septic
2017 American Medical Association. All rights reserved. 192
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Chemotherapy hours after the antimicrobial condition,
Intervention: 16/101 operation for 48 hours. resistance. bacteriologic
(15.8%) Standard preventive Reoperations: NR samples were
Control: 8/102 (7.8%) measures: Length of stay, days: obtained from
P=0.07 Skin prep: local cutaneous meanSD expectorations,
Previous Radiotherapy disinfection with Intervention: 131 pleura, drains,
Intervention: 5/101 povidone-iodine at 12 Control: 151.6 and blood.
(5.0%) and 1 hour pre-op. Mortality: 4/203 (2%) Perioperative
Control: 3/102 (2.9%) Analgesic: all patients Intervention: 3/101 (3%) care:
Transfusion, units: were given the same Control: 1/102 (1%) Respiratory
mean(range) analgesia: Morphinic 1/4: Pulmonary recovery:
Intervention: 0.32(0-8) antalgic drugs were embolism aerosols were
Control: 0.5 (0-12) infused intravenously 1/4: Cerebral given to each
Procedures: every 4 hours. hemorrhage patient on a
Lobectomy: 108/203 1/4: Mesenteric regular basis
(53.2%) infarction and a respiratory
Pneumonectomy: 1/4: Respiratory failure program of
71/203 (35.0%) with acute physiotherapy
Wedge resection: bronchopneumonia followed.
23/203 (11.3%) Other notes:
Indications: Adverse events: No side Statistical
Lung cancer: 160/203 effects of the treatment & errors fixed at
(78.8%) were noted. 5% level.
Lung metastasis: Duration of chest Infection
17/203 (8.4%) drainage: estimated risk
Benign tumor: 20/203 Intervention: 5.50.8 was 30% with
(9.9%) days aim to reduce
Chronic pulmonary Control: 5.71 days risk to 10% (20%
emphysema with reduction).
blebs: 6/203 (3.0%) Needed to
Setting: 1 hospital include 200
Location: France patients (total or
Dates: January 1, each arm?)
1991- June 30, 1992 Five patients
Inclusion Criteria: All included in the
patients undergoing analysis (2
thoracotomy with intervention, 5
lung resection for controls were
lung cancer, lung not given full
2017 American Medical Association. All rights reserved. 193
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
metastasis or treatment
chronic pulmonary because of
emphysema with missing
blebs. prescriptions)
Exclusion Criteria: Follow-up
o
Temperature > 38 C, Abnormal
purulent pulmonary
expectoration, features on plain
curative x-ray,
antimicrobial therapy expectorations
that had been and temperature
stopped less than 8 were recorded
days prior, infected daily from
tumor, purulent postoperative
pleurisy, lung day 3 up to 8
abscess, days) No
bronchiectasis, specific about
exploratory wound follow up.
thoracotomy, Funding Source
mediastinal tumor, Conflicts:
chronic renal Authors: NR
insufficiency, or - Institution: NR
lactamase allergy. Study: NR
Supplies: NR
Karran RCT To investigate Number of patients: Intervention group: SSI Definitions:
50
1993 1, 7, 8 the use of the N=227 n=113 All SSI (some patients Surgical Infection: if
(ES) antimicrobial Patient 2dose: patients received suffered more than 1 a purulent
imipenem for Characteristics intravenously imipenem infection) discharge
perioperative Patients were well 1g at induction of 2dose: 34/113 (30.1%) occurred from
prophylaxis in matched for anesthesia with a single 4dose: 29/114 (25.4%); the wound, a
elective demographic and further dose of positive
colorectal surgical data imipenem 1g at 3h Intra-pelvic abscess: bacteriological
surgery at collected. postop. 2dose: 2/113 (1.8%) culture was
both single Age, y: NR Timing of intervention: 4dose: 2/114 (1.8%); obtained, or a
dose and Gender: NR pre and postop deep abscess
multiple dose Obesity: NR Duration of intervention: Intra-abdominal abscess developed at the
regimens. Comorbidities: NR up to 16h postop 2dose: 2/113 (1.8%) site of operation.
Procedures: elective Device/agent: imipenem 4dose: 1/114 (0.9%);
2017 American Medical Association. All rights reserved. 194
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
colorectal Control group: n=114 p=0.56; Perioperative
Setting: 1 University 4dose: patients received care: NR
hospital imipenem 1g Peritonitis Other notes: None
Location: UK intravenously at 2dose: 0/113 Follow-up: 6-8
Dates: NR induction of anesthesia 4dose: 1/114 (0.9%) weeks postop
Inclusion Criteria: with further doses and Funding Source
Patients over 18 of imipenem: 1g at 3h Abdominal wound: Conflicts:
years of age postop and 500mg at 2dose: 23/113 (19.5%) Authors: NR
undergoing elective 8h and 16h postop 4dose: 22/114 (19.3); Institution: NR
colorectal surgery. p=0.84 Study: Industry
Exclusion Criteria: Standard preventive Supplies: NR
Pregnancy, known measures: skin prep: Perineal wound:
allergy to any study use of antiseptic lavage 2dose: 7/113 (6.2%)
drug, concomitant was left to the 4dose: 3/114 (2.6%);
infection, serious discretion of the p=0.20
comorbidity or operating surgeon. Adverse events
inflammatory bowel Adverse events possibly
disease. Also, related to antimicrobial
patients who had agent included 2
been treated with patients with phlebitis in
antimicrobials in the the group receiving <24
preceding 72h or AMP and in the group
who had received receiving longer AMP 2
steroids, cases of hypotension, 1
antineoplastic phlebitis, 1 erythema,
agents or and 1 rash
radiotherapy before
surgery.
Mayer RCT To perform a Number of patients: Intervention group: n=37 SSI Definitions: NR
27
1993 1, 7 prospective n=66 1dose: 4g piperacillin and 1 abdominal wound Perioperative
(ES) randomized Patient 800mg tinidazole infection was reported care: NR
study Characteristics intravenously 30 min in each group Other notes: none
comparing Groups were not before surgery 1dose: 1/37 (3.0%) Follow-up: 8 days
single dose significantly different. Timing of intervention: 3dose: 1/29 (3.5%) postop
antimicrobials Age, y: NR pre and postop Funding Source
prophylaxis Gender: NR Duration of intervention: Conflicts:
with multiple- Obesity: NR 1 dose or 3 does. (up to Length of stay: Authors: NR
dose regimen Comorbidities: NR 16h postop) No differences: Institution: NR
2017 American Medical Association. All rights reserved. 195
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
in patients Procedures: Radical Device/agent: piperacillin 1dose: 18 days (range 12- Study: NR
undergoing surgery for a and tinidazole 23) Supplies: NR
radical surgery gynecological Control group: n=29 3dose: 19 days (range, 12-
for malignancy patients who received 23 days)
gynecologic Setting: 1 university 4g piperacillin and 800
malignancy hospital mg tinidazole 30 min
Location: Austria before surgery and at 8
Dates: June 1987 & 16h postop.
September 1988 Standard preventive
Inclusion Criteria: measures: NR
Patients undergoing
radical surgery for a
gynecological
malignancy.
Exclusion Criteria:
Patients who had
infections within the
last two weeks,
received
antimicrobials or had
a history of allergic
reaction to either
study antimicrobial.
Also if radical
surgery was not
possible or
indicated.
Bates RCT To study a Number of patients: Intervention group: SSI Definitions:
25
1992 1, 2, 4, large number N=900 n=449 All procedures: Wound sepsis:
(ES) 7, 8 of patients in Patient One dose of antimicrobials None: 48/449 Major minor or
two hospitals Characteristics: given on induction of 24h: 49/451 late
within the patients were anesthesia Perioperative
same health matched between Timing of intervention: Colorectal Sub-Population: care: NR
district to groups except for: Pre and post op (N=224) in at-risk Other notes: None
determine if Age: age>80y Duration of intervention: abdominal surgery Follow-up: 1
there is a 1 dose: 57/446 1 pre op dose or 16h 1 dose: 23/113(20.4%) month
significant (12.8%) postop. 3 doses: 17/111(15.3%) Funding Source
difference 3 dose: 46/550 (8.4%) Device/agent: augmentin P>0.2 Conflicts:
between Gender: NR (1:10 combination of Appendectomy Sub- Authors: NR
2017 American Medical Association. All rights reserved. 196
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
single and Obesity: NR amoxicillin and Population: (n=247): Institution: NR
multiple dose Comorbidities: NR clavulanic acid.) 1 dose: 11/114 (9.6%) Study: NR
regimes of Indications: Control group: N = 551 3 dose: 21/133(15.8%) Supplies: Industry
amoxicillin Inflamed appendix Three doses of p=0.16
250mg/ 1 dose: 71/114 (62%) antimicrobials with the
clavulanic acid 3 dose: 101/133 first given on induction
125mg for (76%) of anesthesia and two
prophylaxis in Dose violation additional injections at 8
at-risk 1 dose: 3/446 (0.7%) & 16h later.
surgery. 3 dose: 13/550 (2.4%)
Procedures: Standard preventive
Appendectomies measures: NR
and all open gastric,
esophageal, colonic
or biliary surgery. All
patients coming to
laparotomy for
intestinal obstruction
including that due to
strangulated hernia
were entered into
the study as well as
patients with intra-
abdominal
malignancy
Setting: 2 General
Hospitals
Location: United
Kingdom
Dates: May 1986
June 1988
Inclusion Criteria: All
patients aged 16 or
over admitted under
2 surgical firms at 2
adjacent district
general hospitals for
at-risk abdominal
surgery with
2017 American Medical Association. All rights reserved. 197
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
potential opening of
a viscus.
Exclusion Criteria: All
patients known to be
allergic to penicillin.
If patients had
received
antimicrobials within
the previous 48h or if
the surgeon
considered that pre-
operative
antimicrobial
administration were
essential, they were
also excluded. Also,
declination of
consent was
excluded although
all received
prophylactic
antimicrobials.
Patients found to
have purulent (fecal)
peritonitis were
withdrawn from the
study
Turano RCT To compare Number of patients: Intervention group: SSI Definitions:
29
1992 1 the efficacy N=608 n=385 All Surgeries Wound infection:
(ES) and safety of Patient 1dose: 1g cefotaxime 1dose: 28/1802 (1.6%) discharge of
two schedules Characteristics intravenously 30 min 3dose: 39/1765 (2.2%) serous or
of prophylactic Recorded, not reported before incision and seropurulent
cefotaxime in Age, y: NR might be repeated in 6h subpopulation of 608 material from the
abdominal Gender: NR if the surgery lasted patients undergoing wound within 7
gynecologic Obesity: NR more than 3h. unspecified gynecologic days of
and urologic Comorbidities: NR Timing of intervention: procedures, operation.
surgery Procedures: pre and postop 1dose: 12/385 (3.1%) Perioperative care
unspecified Duration of intervention: 3dose: 4/223 (1.8%) : NR
gynecologic preop or p=0.53 Other notes: None
2017 American Medical Association. All rights reserved. 198
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
procedures. Device/agent: cefotaxime Follow-up:
Indications: NR Control group: n=223 minimum 7 day
Setting: 226 Surgical 3dose: 1g cefotaxime follow-up (or
units intravenously 30 min until discharge).
Location: Italy before incision and 1.g Funding Source
Dates: January 1, 1990 doses at 6 and 12h Conflicts:
June 30, 1991 postop. (3doses total). Authors: NR
Inclusion Criteria: Institution: NR
patients of any age Standard preventive Study: Industry
undergoing measures: NR Supplies: NR
gynecologic
procedures
(abdominal and
vaginal
hysterectomy and
myomectomy.)
Exclusion Criteria:
known or suspected
-lactam sensitivity,
treatment with any
antimicrobial in the 7
days preceding
surgery, requirement
for combination
antimicrobial
treatment resulting
from the nature of
the patients
condition or type of
surgical procedures
(e.g.
immunosuppression
or colorectal
surgery) or terminal
illness.
2017 American Medical Association. All rights reserved. 199
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Wymenga RCT To establish Number of patients: Intervention group: SSI (13 months) Definitions:
20
1992 1, 2, 7, the efficacy of N=2651 n=1327 Confirmed joint
(ES) 8 a single Patient 1dose: 1500mg 1dose: 11/1327 (0.83%) sepsis: a
perioperative Characteristics cefuroxime given 3dose: 6/1324 (0.45%); positive
antimicrobial The two trial arms were intravenously upon p=0.17; bacteriologic
dose for well matched with induction of anesthesia RR: 1.83, 95%CI (0.68- culture at
infection respect to the 30min before the 4.93). reoperation or a
prophylaxis in general and operation draining sinus
joint orthopedic Timing of intervention: Strong evidence of
replacement diagnoses, risk pre and postop sepsis: four or
with a factors and Duration of intervention: more possible
randomized, medications. preop and up to 16h signs of
controlled, Age, y: NR postop infection:
multicenter Gender: NR Device/agent: cefuroxime Category I: in
study. Obesity: NR Control group: n=1327 patients who
Comorbidities: NR 3dose: 1500mg only showed two
cefuroxime given or three possible
Procedures: THA, TKA intravenously upon signs of sepsis;
and hemiarthroplasty induction of anesthesia Category II: a
procedures 30min before the definite
Indications: NR operation then 750mg diagnosis could
Setting: 27 hospitals given at 8 & 16h not be made;
Location: The postop. Category III:
Netherlands were not
Dates: July 1, 1986 Standard preventive suspected of
July 1, 1988 measures: having joint
Inclusion Criteria: AMP Skin prep: in 3 sepsis.
Patients undergoing centers, the wound was Wound infection in
total hip rinsed with a fluid postop period:
replacement, containing an erythema more
hemiarthroplasty of antimicrobial, whereas than 1cm from
the hip or total knee 2 centers used PI to the incision.
arthroplasty rinse the wound. Perioperative
Exclusion Criteria: care: NR
allergy to Other notes: Study
cephalosporin, was sufficiently
penicillin powered.
anaphylaxis, the use Follow-up: 13
of antimicrobials less months
2017 American Medical Association. All rights reserved. 200
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
than 48h before the Funding Source
operation, use of Conflicts:
perioperative Authors: NR
antimicrobial Institution: NR
administration other Study: Industry
than cefuroxime, Supplies: Industry
malignancy, former
or current sepsis in
the joint and the use
of gentamicin-
impregnated bone
cement for prosthetic
fixation.
Aberg RCT To compare Number of patients: Intervention group: n= SSI: Definitions:
26
1991 1, 7, 8 the triple N=415 patients; 200 All Procedures: Deep surgical
(ES) versus single 428 operations 1 dose of cefuroxime (with 1dose: 8/207 (3.9%) sepsis:
dose of Patient the addition of 3dose:15/221 (6.8%) peritonitis, intra-
cefuroxime Characteristics metronidazole for abdominal
(with the Patients were well surgery of the jejunum, subanalysis of 48 elective abscess, or
addition of matched between ileum, colon, and rectal surgery patients: septicemia.
metronidazole groups. rectum-anus. 1dose: 2/19 (10.5%) Perioperative
for the Age, y: NR Timing of intervention 3dose: 1/29 (3.4%); care: NR
surgeries of Gender: NR Duration of intervention p=0.35 Other notes: None
the jejunum, Obesity: NR Device/agent: cefuroxime Follow-up: within 1
ileum, colon Comorbidities: NR (with metronidazole for subanalysis gastric month
and rectum- Procedures: rectal surgeries) procedures (n=64) Funding Source
anus). laparotomy, Control group: n=215 including gastrectomy Conflicts:
Concomitantly vagotomy, 3 doses of cefuroxime (n=8), gastric banding Authors: None
to introduce a gastrectomy, gastric (with the addition of (n=35) and other gastric Institution: None
system for banding, other metronidazole for (n=21) Study: None
continuous gastric, surgery of the jejunum, deep surgical sepsis: Supplies: None
surveillance of cholecystectomy, ileum, colon, and 1dose: 1/24 (4%)
postoperative choledochal surgery, rectum-anus. 3dose: 4/40 (10%);
wound pancreatectomy, Standard preventive p=0.41
infections. surgery of jejunum, measures: NR
ileum, or colon,
rectal anterior
resection, rectal
amputation.
2017 American Medical Association. All rights reserved. 201
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Indications: NR
Setting: 1 county
hospital
Location: Sweden
Dates: February 1988
May 1990
Inclusion Criteria:
Consecutive patients
16 years or older
scheduled for
elective abdominal
surgery during the
study dates.
Exclusion Criteria:
due to unscheduled
perioperative
antimicrobial therapy
Becker RCT To study in a Number of patients: Intervention group: n=18 SSI Definitions:
43
1991 1, 3, 4, prospective, n=40 After 12h postop, patients no wound or intra- Wound was
(ES) 5, 6, 7, double-blind Patient received 1g cefoxitin abdominal infections in considered
8, 9 randomized, Characteristics: intravenously every 6h either group at 1yr uninfected if it
fashion, the Patient for 5 days beginning 6h follow up: was healing
efficacy of a characteristics were after fixed postop dose 5 day: 0/22 vs. without evidence
short similar between Timing of intervention: 12h: 0/18 of erythema or
perioperative groups except: postop Length of stay: discharge.
course versus Entry into bowel Duration of intervention: No difference, days: Infected: if purulent
an extended lumen: 5 days (meanSD) drainage was
postoperative 5day: 9/18 (50%) Device/agent: 1g cefoxitin 5 day: 8.70.4 present,
course of 12h: 6/22 (27%) but intravenously. 12h: 8.40.2. regardless of
intravenous major contamination Control group: n=22 culture results or
antimicrobials was not statistically After 12h postop, patients if nonpu8rulent
in patients significantly different. received placebo material
undergoing Age, y: NR (dextrose in water) contained
colectomy, Gender: NR intravenously every 6h pathogenic
mucosal Obesity: NR for 5 days beginning 6h bacteria.
protectomy Comorbidities: NR after fixed postop dose Deep infection if
and ileal Procedures: Standard preventive infection
pouch-anal Colectomy, mucosal measures: extended below
anastomosis. protectomy, and ileal 1) clear liquid diet for 4 fascia
2017 American Medical Association. All rights reserved. 202
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
pouch-anal days before surgery; 2) Moderate when
anastomosis. mechanical bowel prep subcutaneous
Indications: chronic consisting of 300ml of tissues were
ulcerative colitis, oral magnesium citrate involved.
familial polyposis, or and 2 tap water Possibly infected
Gardners syndrome enemas administered evidence of
Setting: 1 university on preop day 2 and induration and
hospital 300ml of oral inflammatory
Location: USA magnesium citrate and changes of the
Dates: NR (9months) tap water enemas until skin but without
Inclusion Criteria: clear administered on purulent
Patients with chronic preop day 1; 3) oral discharge
ulcerative colitis, antimicrobial Perioperative
familial polyposis or preparation consisting Care: NR
Gardners syndrome of 1g neomycin and 1g Other notes: None
who required erythromycin base by Follow-up: 8
colectomy and who mouth at 1:00pm, weeks post
were candidates for 2:00pm,. And 11:00pm discharge when
mucosal protectomy on preop day 1; 4) 2g loop ileostomy
with ileal pouch-anal cefoxitin administered was closed.
anastomosis. intravenously during a Patients were
Exclusion Criteria: 20 min period then followed for
Allergy to penicillin immediately before 12 months after
or cephalosporin; surgery with additional closure.
antimicrobial use 2g iv doses of cefoxitin Funding Source
within 1 week before given at 6h and 12h Conflicts:
operation, after the initial dose. Authors: NR
mechanical bowel Also, rectum was irrigated Institution: NR
obstruction or any with PI solution via Study: Industry
other functional or transanal rectal Supplies: NR
anatomic reason catheter.
precluding
mechanical bowel
prep; or the
presence of an
existing ileostomy or
colostomy.
2017 American Medical Association. All rights reserved. 203
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Garotta RCT To evaluate Number of patients: Intervention group: SSI: Definitions :
19
1991 1, 2 the relative N=614 n=301 1dose: 2/301 (0.66%) Wound infection:
(ES) effectiveness Patient 1dose: given 2g Multi: 3/313 (0.96%) purulent
of two Characteristics: ceftizoxime exudation with
cephalosporin both arms were intravenously 30 positive
antimicrobials, homogeneous for minutes before the microbiologic
ceftizoxime vs. several operation culture.
cefuroxime, in characteristics such Timing of intervention:
preventing the as patients age, pre and postop Perioperative
development sex, length and type Duration of intervention: care: NR
of of operation and preop and up to 12h Other notes: none
complicating postop procedures. after operation Follow-up: 1 year
infections in Age, y: NR Device/agent: ceftizoxime Funding Source
patients Gender: NR Control group: n=313 Conflicts:
submitted to Obesity: NR 2dose: given 2g Authors: Industry
elective Comorbidities: NR ceftizoxime Institution: NR
surgery in Procedures: Hip or intravenously 30 Study: NR
orthopedic knee replacement or minutes before the Supplies: NR
departments. fracture fixation operation and 12h
Indications: NR postop.
Setting: 30 hospitals Standard preventive
Location: Italy measures: NR
Dates: NR
Inclusion Criteria:
Patients >18 years,
undergoing
orthopedic surgeries
such as hip or knee
replacement and
fractures fixed by
foreign bodies.
Exclusion Criteria:
Evidence of acute
infection;
antimicrobial
treatment within 48
hours prior to
operation or use of
local antimicrobials;
2017 American Medical Association. All rights reserved. 204
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
and open fractures
Buckley RCT To determine Number of patients: Intervention1 group: n= SSI: (Follow up 6 weeks) Definitions:
14
1990 1, 3, 4, whether or not N=312 108 Wound infection Definite Wound
(ES) 5 cefazolin Patient AMP Four doses: 2g Intervention1+2: 4/191 infection: if there
decreased Characteristics: All Cefazolin administered (2.0%) was a purulent
early groups similar in age intravenously when Control: 4/121 (3.7%) discharge,
postoperative (P=0.75) and sex anesthesia was P=0.46 whether or not
wound distribution (P=0.86) induced, then 1g When not combined organisms were
infection rates, Age, y: meanSD cefazolin every 6 hours Intervention1: 2/108 cultured.
and whether (range) intravenously for three (1.6%) Possible wound
single-dose Intervention1: doses making a total of Intervention2: 2/83 infection:
cefazolin was 76.314.9 (18-100) four doses of cefazolin (2.4%) inflammation
as effective as Intervention2: Intervention2 group: n= Control: 4/121 (3.7%) without
multiple dose 77.112.1 (33-94) 83 All superficial except for 1 discharge and
(4 doses) Control: 76.113.4 AMP single dose: 2g control group deep wounds that
cefazolin in (29-96) Cefazolin administered infection in a 96-year- drained culture-
preventing Gender m/f intravenously when old woman which was positive serous
early Intervention1: 32/89 anesthesia was implicated in her death fluid. The patient
postoperative Intervention2: 22/61 induced, then saline at 14 days postop. was followed up
wound Control: 3/75 every 6 hours All other infected patients until the wound
infections Obesity NR intravenously for three were discharged from healed or
resulting from Comorbidities NR doses. the study after 6 weeks drained pus.
hip surgery. Procedures: Timing of intervention: with healed wounds. Perioperative
They also Prosthetic Hip: Pre, intra and Wound infection by care: NR
compared Intervention1: 56/108 postoperatively Operation Type Other notes: Due
single and 3 (51.9%) Duration of intervention: Prosthetic Hip: to low infection
doses to no Intervention2: 32/83 From induction of Intervention1+2: 2/191 rates, groups
AMP. (38.6%) anesthesia to 24 hours (1.0%) Intervention1 &
Control: 33121 postop. Control: 2/121 (1.9%) Intervention2
(27.3%) Device/agent: Cefazolin Pins + Compression were combined
Multiple Pins: (21 Total) Monitoring intervention: Screws to increase the
Intervention1: 8/108 Blood cefazolin levels Intervention1+2: 2/191 power.
(7.4%) were examined (1.0%) Statistics:
Intervention2: 5/83 intraoperatively for the Control: 2/121 (1.9%) Sample size of 120
(6.0%) first 14 patients and P=0.72 per arm selected
Control: 8121 (6.6%) found to be 10 times Average age of infected to detect
Compression Screw: the minimal inhibitory patients: 84.2 years (8 difference in
2017 American Medical Association. All rights reserved. 205
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
(170 Total) concentration years older than non- infection rate of
Intervention1: 57/108 Control group: n= 121 infected patients though 9% with
(52.8%) No AMP: Saline not statistically probability of
Intervention2: 46/83 administered significant (p=0.11) type a error of
(55.4%) intravenously for four <0.10 and type
Control: 67/121 doses. Other infections: NR error of <0.20.
(55.4%) Standard preventive Topic-specific Follow-up:
Type of surgery was measures: NR outcomes: NR Complete follow-
not evenly Non-standard preventive Antimicrobial resistance: up at 6 weeks
distributed between measures All infections were S. post-op.
groups: (P=0.05) but Surgery: Fractured hip aureus sensitive to Funding Source
this variable did not was treated with either hip cephalothin. No gram Conflicts:
turn out to be a pinning (with compression negatives were Authors: NR
confounder screw or multiple pins) or a isolated. Institution: NR
Drain Used (179 Total hip prosthesis implant. Reoperations: NR Study: NR
Intervention1: 67/108 Drain: At surgeons Length of stay: NR, but Supplies: NR
(62.0%) discretion, a drain was no patients length of
Intervention2: 49/83 placed for subcutaneous stay was lengthened by
(59.0%) tissue drainage. a drug-related
Control: 63/121 complication
(52.1%) Mortality:
P=0.85, = 5.95, df =
2
Total: 15 deaths (4.8%)
2 Intervention1: 3/108
Indications: Fractured (2.8%)
hip (interochanteric Intervention2: 4/83
or subcapital) (4.8%)
Setting: 1 hospital Control: 8/121 (6.6%)
Location: Canada Cause of all deaths was
Dates: December 1, cardiopulmonary except
1985 December1 , for the patient
1988 described above who
Inclusion Criteria: All died of multi-organ
adults with an system failure (the deep
interochanteric or wound infection
subcapital hip possibly contributed)
fracture. All patients who died were
Exclusion Criteria: in their ninth or tenth
Cephalosporin decade of life.
allergy, pathologic Adverse events: No
2017 American Medical Association. All rights reserved. 206
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
fracture due to anaphylactic reactions,
tumor, previous allergies or renal
surgery on the toxicity related to
fractured hip, cefazolin
treatment with an administration. Also, no
antimicrobial other cefazolin cross-
than cefazolin, or a reactions with patients
preoperative course who claimed a history
in hospital longer of penicillin rashes
than 7 days.
Hall RCT To evaluate Number of patients: Intervention group: SSI Definitions:
44
1989 1, 2, 7, the efficacy of N=1027 n=519 patients given 1 Total colorectal: Wound Infection:
(ES) 8 moxalactam Patient 1g moxalactam Total: 22/245 (9.0%) purulent wound
given as a Characteristics: NR intravenously at Single: 12/119(10.1%) discharge or a
single dose or Age, y: NR induction of anesthesia 48h: 10/126(7.9%); serous wound
as a 48-hour Gender: NR Timing of intervention: p=0.56 discharge with
regimen for a Obesity: NR pre and post-operative Elective colorectal culture of
range of Comorbidities: NR Duration of intervention: procedures (n=207) pathogenic
potentially Procedures: 1 dose or 48h postop. Single: 11/102(10.7%) organisms.
contaminated Appendectomy, Device/agent: 1g 48h: 6/105(5.6%); Major wound
abdominal cholecystectomy, moxalactam p=0.19 infection: if it
operations. bile duct surgery, intravenously resulted in an
elective colorectal, Control group: n=508 Emergency Colorectal extension of the
emergency patients who received (no bowel prep in hospital stay or
colorectal, 1g of moxalactam emergency cases): required
gastroduodenal, and intravenously at Single: 1/17(5.8%) dressings at
small-bowel surgery. induction of anesthesia 48h: 4/21(20.0%); home for more
Setting: 2 centers followed by 1g of p=0.26 than 7 days
(both general moxalactam Minor wound
hospitals) intravenously every 6h infection: if
Location: Australia for a further 7 doses. neither of these
Dates: NR Equaling a total of 8g in features
Inclusion Criteria: 48h/ occurred.
consecutive patients Standard preventive Peritoneal infection:
>14 years of age measures: Patients if pus or
who were were given 10mg of peritoneal fluid
undergoing Vitamin K containing
potentially intramuscularly prior to pathogenic
contaminated operation due to reports organisms were
2017 American Medical Association. All rights reserved. 207
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
abdominal surgery at of coagulopathy found at the
one of 2 hospitals. associated with operations, if
Exclusion Criteria: moxalactam. there was
Postop antimicrobial Skin prep Povidone spontaneous
for residual infection; Iodine & no local discharge or
antimicrobial antimicrobial or needle
administration within antiseptic prep aspiration of pus
48h prior to Drain tubes were from the
operation; viscus not passed through a peritoneal cavity
opened at operation; separate incision. or if there was a
failure to give Bowel prep all patients collection of pus
informed consent received a two-day present at
failure to give initial mechanical bowel prep autopsy.
dose of moxalactam (no oral antimicrobials Other notes: Study
history of were administered) was sufficiently
cephalosporin powered to
sensitivity or detect a
penicillin difference in
anaphylaxis; wound infection
established renal or rates.
th
liver failure; reaction Follow-up: 5
to initial dose of postoperative
moxalactam. week.
Ritter RCT To identify the Number of patients: Intervention group: n=98 SSI Definitions: NR
21
1989 1, 7, 8 relationship N=196 2dose: Two intraoperative In the second smaller Perioperative
(ES) between the Patient doses of cefuroxime study (N=196), in care: NR
duration of Characteristics (1500mg & 750mg) unilateral or bilateral Other notes: None
prophylaxis Reported but not Timing of intervention: THA or TKA patients no Follow-up:
and the significant intergroup intra and postop infections (including 12month follow
incidence of differences. Duration of intervention: deep wound infections) up
latent wound Procedures: primary intraop up to 24h were reported in either Funding Source
infection- unilateral or bilateral postop group Conflicts:
TKA or THA Device/agent: cefuroxime 2dose: 0/98 Authors: NR
Indications: NR Control group: n=98 5dose: 0/98 Institution: NR
Setting: 1 university 5dose: Two intraoperative Study: NR
Hospital doses of cefuroxime Supplies: NR
Location: USA (1500mg & 750mg)
Dates: NR followed by 24h of
Inclusion Criteria: postop cefuroxime
2017 American Medical Association. All rights reserved. 208
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Patients undergoing (750mg every 8 hours)
primary unilateral or
bilateral THA or TKA Standard preventive
Exclusion Criteria: NR measures: NR
Moesgaa- RCT To investigate Number of patients: Intervention group: SSI Definitions:
rd 1, 2, 7, the N=428 n=209 Total: 45/428 (11%); Wound infection:
48
1989 8 relationship Patient Short-term prophylaxis: 6hr: 22/209 (11%) presence of pus,
(ES) between Characteristics: gentamicin 80mg iv + 2day: 23/219 (11%) either
preoperative groups were well metronidazole 500mg iv p=0.99 discharging
cell-mediated matched and equally at the start of the spontaneously
immunity distributed. operation followed by Intra-abdominal abscess: or requiring
(CMI) and Age, y: NR repetition of these Total: 14/428 (3%) drainage.
postoperative Gender: NR doses 6 hours later. 6hr: 6/209 (3%) Intra-abdominal
infection and Obesity: NR Timing of intervention: 2day: 8/219 (4%) abscess: verified
whether Comorbidities: NR pre and postop p=0.65 by surgical
patients with Procedures: elective Duration of intervention: drainage or
impaired CMI colorectal surgery 6h or 2 days ultrasound
would benefit Indications: NR Device/agent: gentamicin guided
from Setting: 1 university 80mg iv + aspiration of
prolonged hospital metronidazole 500mg iv pus.
antimicrobial Location: Denmark Control group: n=219 Perioperative
prophylaxis. Dates: 1982-1986 Long term prophylaxis: Care: NR
Inclusion Criteria: all gentamicin 80mg iv + Other notes: none
patients undergoing metronidazole 500mg iv Follow-up: 30
elective colorectal at the start of the days
surgery. operation followed by Funding Source
Exclusion Criteria: repetition of these Conflicts:
Those admitted for doses every 8hours for Authors: NR
rectal amputation, 2 days. Institution: NR
known allergy to the Standard preventive Study: NR
antimicrobials used, measures: Bowel prep Supplies: NR
pregnancy, age<15 NR
years, and any
antimicrobial therapy
5 days prior to
surgery.
2017 American Medical Association. All rights reserved. 209
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Grundm- RCT To define Number of patients: Intervention group: n=25 SSI Definitions: NR
ann 1 whether a N=154 Patients who received a SSI: Perioperative
24
1987 single Patient single dose of 1dose: 4/77 (5.2%) care: NR
(ES) preoperative Characteristics: metronidazole and 3dose: 4/77 (5.2%) Other notes: None
dose of While statistical mezlocillin (5g/0.5g) Follow-up: NR
mezlocillin/ significance is not prior to the operation Intra-abdominal abscess Funding Source
metronidazole indicated, the 1 dose Timing of intervention: 1dose: 2/77 (2.6%) Conflicts:
is sufficient in group had a higher pre and postoperative. 2doses: 1/77 (1.3%); Authors: NR
colon surgery percentage of high Duration of intervention: p=0.57 Institution: NR
or whether risk patients up to 6h postop Study: NR
under certain including patients Device/agent: Peritonitis Supplies: NR
circumstances with age>58 years, metronidazole and 1dose: 2/77 (2.6%)
(long operation time mezlocillin (5g/0.5g) 3doses: 2/77 (2.6%);
operation >2.5h, Body Monitoring intervention:
time, weight>69kg, pre, intra and postop.
insufficient insufficient bowel Control group: n=28
bowel prep, lavage and blood Patients received 5g
high blood transfusions. metronidazole/ 0.5g
loss) a Age, y: NR mezlocillin prior to the
multiple Gender: NR operation, a second
administration Obesity: NR dose 90 minutes post-
of Comorbidities: NR skin incision and 6
antimicrobials Procedures: elective hours after the second
is more colorectal surgery dose.
justified. Indications: NR Standard preventive
Setting: 1 university measures:
hospital Bowel Prep: Orthograde
Location: Germany bowel prep with no
Dates: NR antimicrobial
Inclusion Criteria: ingredients. And no
patients undergoing preop oral antimicrobial
colon surgery. for the purpose of
Exclusion Criteria: NR bowel prep.
2017 American Medical Association. All rights reserved. 210
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Juul RCT To evaluate Number of patients: Intervention group: SSI Definitions :
45
1987 1, 2, 7, the N=294 Patients received 1.5g Deep wound infections: Deep wound
(ES) 8 prophylactic Patient metronidazole and 3g Total: 17/294 (5.8%); infection:
effect of a Characteristics: No ampicillin intravenously Single Dose: 9/149 (6%) accumulation of
single dose significant at induction of Multiple: 8/145 (6%) pus either with
versus differences between anesthesia spontaneous
multiple doses groups. Timing of intervention: Intra-abdominal abscess: discharge or
of systemic Age, y: NR Pre and postoperative Total: 3/294 (1.0%) requiring
ampicillin and Gender: NR Duration of intervention: Single: 1/149 (1%) surgical
metronidazole Obesity: NR 1 dose or 3 postop days Multiple 2/145 (1%) drainage.
in elective Comorbidities: NR Device/agent: Wound dehiscence:
colorectal Procedures: Elective metronidazole & Topic Specific subcutaneous
surgery. colorectal surgery ampicillin outcomes: and fascial
Indications: NR Control group: No difference in bacterial breakdown, but
Setting: 1 university Patients received 1.5g isolates and no report without pus
hospital metronidazole and 3g of antimicrobial accumulation.
Location: Denmark ampicillin intravenously resistance Intra-Abdominal
Dates: October 1983- at induction of Abscess-
April 1986 anesthesia followed by intraperitoneal or
Inclusion Criteria: Metronidazole 0.5g and pelvic collection
Patients 18y or ampicillin 1g each 3 of pus with
older, undergoing times during the second spontaneous
elective colorectal and third postoperative discharge or
surgery during the days. which required
study dates. Standard preventive surgical
Exclusion Criteria: measures : drainage.
Patients receiving Bowel prep: bowel was
antimicrobials in the emptied either Perioperative
preoperative period conventionally or by care: NR
or those with a whole gut irrigation. Other notes: None
history of Follow-up : 30
hypersensitivity to days
ampicillin or Funding Source
metronidazole. Also, Conflicts:
patients not Authors: NR
receiving full does or Institution: NR
the bowel note being Study: NR
opened during Supplies: NR
surgery.
2017 American Medical Association. All rights reserved. 211
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Mendel RCT To assess the Number of patients: Intervention group: n=54 SSI Definitions: NR
46
1987 1 prophylactic N=100 Patients receiving a single Perioperative
(ES) value of a Patient shot of 5g mezlocillin Total: 3/100 (3.0%); care: NR
one-shot Characteristics: NR and 500mg Single dose: 2/54 (3.7%) Other notes: none
regimen of Age, y: NR metronidazole 3day: 1/46 (2.1%); Follow-up: NR
antimicrobials. Gender: NR Timing of intervention: p=0.66 Funding Source
Obesity: NR pre and postop Conflicts:
Comorbidities: NR Duration of intervention: Authors: NR
1dose or 3 days postop Institution: NR
Procedures: elective Device/agent: Study: NR
excision of colorectal mezlocillin5g and Supplies: NR
carcinoma or metronidazole 500mg
diverticulitis. Control group: n=46
Indications: NR patients receiving 9
Setting: 1 Hospital doses of 5g mezlocillin
Location: Germany and 500mg
Dates: NR metronidazole (a 3 day
Inclusion Criteria: regimen)
Patients requiring Standard preventive
excision of colorectal measures:
carcinoma or Bowel prep: all patients
diverticulitis underwent standard
Exclusion Criteria: preop bowel prep (from
Patients with a 4 days preop!)
colostomy or who
had received other
antimicrobials within
72h of operation.
Gatell RCT To compare Number of patients: Intervention group: SSI Definitions:
18
1987 1, 3, 4, the use of five N=717 n=382 1dose: 20/382 (5.2%) Wound infection:
(ES) 5, 7, 8, doses of Patient 1dose: 1 preoperative 5dose: 3/335 (0.9%) diagnosed when
10 cefamandole Characteristics: intravenous dose of p=0.004 the wound
with a single Characteristics were cefamandole (2g) given drained pus
preoperative similar between hour before starting Hemiarthroplasties: spontaneously
dose for groups. the operation. This was 1dose: 5/76 (6.5%) or was inflamed
preventing Age, y: NR followed by 4 doses of 5dose: 0/74 (0%); to the point that
wound Gender: NR placebo following the p=0.03 it had to be
infection s Obesity: NR control drug schedule opened by the
after so-called Comorbidities: NR Timing of intervention All other procedures surgeon and
2017 American Medical Association. All rights reserved. 212
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
clean Duration of intervention combined: then drained
orthopedic Procedures: Clean Device/agent: 1dose: 15/306 (5%) purulent
operations in orthopedic cefamandole 5dose: 3/261(1%); material. A
which there operations in which 5dose: patients receiving p=0.006. hematoma or
was there was a metal a 2g cefamandole dose wound draining
implantation of device implanted. intravenously 30 min Antimicrobial Resistance serous material
a metal Indications: NR preop and 2g 31 organisms isolated was considered
device. Setting: 1 university intravenously at 2h after from 23 wound to be infected
hospital the start of surgery. This infections: 9 only when it
Location: Spain was followed by 1 gram Staphylococcus aureus, cultured positive.
Dates: NR intravenously or 4 S. epidermis and 4 E.
Inclusion Criteria: All intramuscularly at 8, 14, & coli all sensitive to the Perioperative
adults scheduled for 24 hours thereafter. AMP. In addition, 4 care: NR
an orthopedic Control group: n=335 Pseudomonas Other notes: None
surgical procedures Standard preventive aeruginosa, and 3 Follow-up:
that required measures: Streptococcus faecalis Minimum
insertion of a metal Skin prep: skin was all resistant to the AMP 12months
device for fixation of shaved with disposable and 7 strains of other (range 12-24
bone. razor & cleaned with gram negative bacilli, 2 months) or if
Exclusion Criteria: antiseptic soap just of them resistant to the patients had an
total joint before entering OR. AMP. infection, until
replacement, a Alcoholic PI was metal device
known allergy to applied to the operative Mortality was removed.
penicillin or site and allowed to There were 30 deaths Funding Source
cephalosporins, and remain for 2min. (4%); 1 patient had an Conflicts:
those who had Patients in both groups uncontrolled wound Authors: None
immunosuppressive were hospitalized for infection but the cause Institution: None
treatment, those who approximately 5 days of death was a stroke. Study: None
had an open fracture before surgery. Supplies: None
or a previous
infection of the
operative field, and
those receiving any
antimicrobials.
2017 American Medical Association. All rights reserved. 213
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Oostvog- RCT To compare a Number of patients Intervention group: n=80 SSI Definitions:
el 1, 2, 3, short term N=169 (1dose) Vascular surgery Wound infection:
16
1987 5, 6, 7 antimicrobial Patient Received 2 million U Single Dose: 3/80 (2.3%) presence of pus
(ES) regimen (1 Characteristics: the benzylpenicillin i.v. + 3 Dose: 2/89 (3.8%) discharging
preop & 2 two groups did not 120mg tobramycin i.m. p>0.5 spontaneously
postop doses) differ significantly. 1hr preop or requiring
with a single- Age, y: NR Timing of intervention: drainage
dose regimen Gender: NR pre and postop Perioperative
of intravenous Obesity: NR Duration of intervention: care: NR
antimicrobials. Comorbidities: NR 1 dose or 12h postop. Other notes: None
Procedures: vascular Device/agent: Follow-up: 1
surgery benzylpenicillin + month
Indications: NR tobramycin Funding Source
Setting: 1 general Control group: n=89 Conflicts:
hospital (3dose) Authors: NR
Location: the Received 2 million U Institution: NR
Netherlands benzylpenicillin i.v. + Study: NR
Dates: November 1983 120mg tobramycin i.m. Supplies: NR
January 1985 1hr preop plus 1million
Inclusion Criteria: All U benzylpenicillin i.v. +
patients admitted for 80mg tobramycin i.m. at
emergency or 6h & 12h postop.
elective surgery
during the study Standard preventive
dates if the operation measures: NR
was classified as
clean-
contaminated or
contaminated
according to the
NRC criteria; or
when a vascular
operation was
planned (Clean
operation)
Exclusion Criteria:
patients with multiple
trauma or
mechanical intestinal
2017 American Medical Association. All rights reserved. 214
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
obstruction or who
were already
receiving
antimicrobials for
reasons other than
prevention of wound
infections, or who
had severely
impaired renal
function or known
hypersensitivity to
one of the study
antimicrobials. Also
excluded were all
patients found at
operation to have
bacterial peritonitis.
Also perineal
wounds.
Wenzel RCT To investigate Number of patients: Intervention group: n=30 SSI Definitions:
49
1985 1, 2, 7, and compare N=60 1dose: 1 dose of 100mg Total SSI Wound infection:
(ES) 8, 9 the extent of Patient ornidazole and 80mg 1dose: 6/30 (20%) edematous
the reduction Characteristics gentamicin 48hDose: 10/30 (33.3%) and/or red
in post- No significant administered p=0.25 wound with a
operative differences in patient intravenously 45min Intra-abdominal abscess: purulent
infection risk parameters. before operation with No difference: secretion.
in patients Age, y: NR pre-medication. 1dose: 2/30 (7%) Perioperative
undergoing Gender: NR Timing of intervention: 48hdose: 2/30 (7%); care: NR
elective Obesity: NR pre and postop Other notes:
colonic Comorbidities: NR Duration of intervention: Peritonitis :no difference: Complication
surgery using Procedures: Surgery up to 48h postop 1dose: 1/30 (3%) rates were high
two of the colon and Device/agent: ornidazole 48hdose: 3/30 (10%); for both groups.
prophylaxis rectum and gentamicin p=0.32 Follow-up: NR
regimens. 1) A Indications: NR Control group n=30 Funding Source
one shot Setting: 1 hospital. 48h: 1 dose of 100mg Superficial SSI: Conflicts:
method versus Location: Germany ornidazole and 80mg 1dose: 3/30 (10%) Authors: NR
2) pre-op Dates: NR gentamicin 48h Dose: 5/30 (16.7%) Institution: NR
combined with Inclusion Criteria: administered Study: NR
postop Patients who had to intravenously 45min Supplies: NR
2017 American Medical Association. All rights reserved. 215
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
antimicrobial undergo abdominal before operation with
infusions for surgery involving pre-medication.
up to 48h. opening of the colon. Followed by 3 further
Exclusion Criteria: doses of 500mg
Patients who were to ornidazole at 12h
have intervals and 3 doses of
appendectomies, 80mg gentamicin at 8h
those known intervals.
hypersensitivity to Standard preventive
ornidazole or measures: patients
aminoglycosides, with non-stenosing
those who received tumors were fed a full
antimicrobial calorie diet and were
treatment less than fed orally or enterally up
5d before the to the day preceding
operation and those the operation. Patients
with pre-operative with stenosing tumors
fecal contamination. were given parenteral
feeding additionally or
exclusively.
Bowel Prep: NR
Carr RCT To establish Number of patients: Intervention group: n=22 SSI: Definitions:
all durations 24h
23
1984 1, 3 whether N=90 Patients receiving only a Infected wound:
(ES) additional Patient pre-operative bolus of combined suggest no one from which
doses of Characteristics: the 500ml intravenous difference between there was a
intravenous four groups of metronidazole. groups for purulent
metronidazole patients were well Timing of intervention: Total Wounds discharge from
for up to 24h matched. pre and postop 1 dose: 8/25 (32%) the main suture
after elective Age, y: NR Duration of intervention: 2-4doses: 18/81 (22.2%) line even if
colorectal Gender: NR up to 24h culture was
surgery would Obesity: NR Device/agent: Abdominal wounds: negative.
reduce the Comorbidities: NR metronidazole Total 18/90 (20%): Perioperative
wound Procedures: Intestinal Control group: n=68 1dose: 7/22 (31%) care: NR
infection rate anastomoses. Patients receiving 2-4doses: 11/68 (16%) Other notes: None
further. Indications: NR postoperative p=0.12 Follow-up: 6
Setting: 1 teaching intravenous 500mg weeks post op.
hospital injections of Perineal wounds: Funding Source
Location: United metronidazole every 8h 1/3 (33.3%) vs. Conflicts:
Kingdom up to 24h postop. 7/13 (53.8%); Authors: NR
2017 American Medical Association. All rights reserved. 216
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Dates: April 1980 Standard preventive p=0.53, at 6 week follow Institution: NR
February 1982 measures: up. Study: NR
Inclusion Criteria: Bowel prep consisted of Supplies: Industry
Patients who magnesium sulphate 2g
underwent elective TDS for 3 days before
colorectal surgery the operation and a
during the study standard mechanical
dates. method of bowel prep
Exclusion Criteria: containing no
Patients who antimicrobials.
received
antimicrobials in the
preceding 2 weeks
and patients with
inflammatory bowel
disease who had
abscesses, fistulas
or toxic dilatation of
the colon.
Hasselg- RCT To evaluate Number of patients: Intervention group: SSI Definitions:
ren 1, 3, 4, the effects of a N=121 1day: patients Wound infection:
37
1984 5, 6, 7, 1 day versus a Patient administered 3 doses of 1day: 2/52 (3.8%) accumulation of
(ES) 8 3-day course Characteristics: cefuroxime 1.5g 3day: 3/69 (4.3%) pus that drained
of cefuroxime relative distribution intravenously beginning p=0.89 spontaneously
on infection of risk factors did not 1 hour before surgery or after
rates in differ significantly and then every 8 hours debridement.
peripheral between the study ( up to 16h postop) Graft infection:
vascular groups. Timing of intervention: defined as any
surgery. Age, y: NR pre and postop persistent
Gender: NR Duration of intervention: wound infection
Obesity: NR 1 or 3 days postop communicating
Comorbidities: NR Device/agent: 1.5g with graft
Procedures: vascular cefuroxime iv material.
surgery Control group:
Indications: NR 3day: patients Perioperative
Setting: 1 university administered 9 doses of care: NR
hospital cefuroxime 1.5g Other notes: NR
Location: Sweden intravenously beginning Follow-up: 30 day
Dates: January 1981 1 hour before surgery follow up
2017 American Medical Association. All rights reserved. 217
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
June 1983 and then every 8 hours Funding Source
Inclusion Criteria: ( up to 64h postop) Conflicts:
Patients scheduled Standard preventive Authors: NR
for vascular measures: Institution: NR
reconstructive Skin prep: wash with Study: NR
surgery of the lower chlorhexidine soap 3 Supplies: NR
limbs and patients times on day prior to
undergoing acute surgery.
femoral Hair removal: shaving
embolectomy or immediately prior to
thrombectomy. surgery.
Exclusion Criteria:
Patients scheduled
for an aortic
bifurcation graft;
patients having
received
antimicrobials within
1 week prior to
surgery; patients
with cellulitis or wet
gangrene on lower
extremities; and
patients with a
history or penicillin
or cephalosporin
allergy.
Hemsell RCT To compare a Number of patients: Intervention group: n=58 SSI Definitions:
28
1984 1, 2, 4, preoperative N=112 1 dose: patients received 1 Minor postop
(ES) 5, 6, 7, dose with Patient preoperative dose of 2g 1dose: 1/58 (1.7%) infection: cystitis
8 three Characteristics cefoxitin i.m. when 3dose: 2/54 (3.7%) when a
perioperative Clinical and surgical called into the operating woman had
doses of variables were room. Cefoxitin was lower urinary
cefoxitin given statistically similar diluted with 0.5% Length of stay: tract irritative
to between groups. lidocaine without No difference, days: mean symptoms and
5
premenopaus Age, y: NR epinephrine in the hip SD: 10 or more
al women Gender: NR Timing of intervention: 1dose: 4.41.1 colonies of a
scheduled for Obesity: NR preop or postop 3dose: 4.71.2 days single
vaginal Comorbidities: NR Duration of intervention: uropathogen per
2017 American Medical Association. All rights reserved. 218
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
hysterectomy. Procedures: vaginal up to 12h postop milliliter of urine.
hysterectomy Device/agent: cefoxitin Major postop
Indications: NR Control group: n=54 infection: pelvic
Setting: 1 university 3dose: patients received 1 cellulitis an
hospital preoperative dose of 2g extra-peritoneal
Location: USA cefoxitin i.m. when infection
Dates: February called into the operating involving
December 1982 room. Cefoxitin was primarily the
Inclusion Criteria: diluted with 0.5% parametrial
premenopausal lidocaine without tissues. This
women undergoing epinephrine in the hip; involved
vaginal this was followed by complaints of
hysterectomy intravenous infusion of increasing lower
Exclusion Criteria: 2g cefoxitin dose at 6 & abdominal
known allergy to 12h postop. and/or pelvic
cephalosporins, pain, tenderness
cephamycins, or Standard preventive to the gentle
lidocaine; history of measures: deep palpation
immediate Povidone-iodine douche of the
hypersensitivity was taken the night inferolateral
reaction to penicillin; before the surgery abdominal wall,
history of and an elevated
antimicrobial therapy temperature.
within the 48h before Tenderness was
surgery; temperature always
of greater than or asymmetrical.
o
equal to 38 C during Perioperative
the 24h before care: NR
surgery, concomitant Other notes: none
infection or any other Follow-up: 3-6
condition that might weeks post-
preclude accurate surgery.
evaluation of Funding Source
response to therapy. Conflicts:
Authors: NR
Institution: NR
Study: Industry
Supplies: NR
2017 American Medical Association. All rights reserved. 219
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Austin RCT To examine Number of patients: Intervention group: n=38 SSI Definitions:
34
1980 1 the effect the n=85 2dose: Patients who Superficial sternal SSI Infections:
(ES) need for Patient received cephalothin 2g 2dose: 1/38 (2.6%) diagnosed
chemoprophyl Characteristics intravenously 3days: 1/47 (2.1%) clinically and
axis beyond Findings of the two immediately before f/u NR supported by
the immediate groups were similar cardiac bypass was total and
operative Age, y: NR begun and 2g at the Antimicrobial resistance: differential
period in Gender: NR end of the operation. Both incisional SSIs were leukocyte
Aortocoronary Obesity: NR Timing of intervention: Staphylococcus aureus counts, by local
Bypass Comorbidities: NR pre and postop. cultures and by
procedures. Procedures: Duration of intervention: Length of stay, days blood cultures
aortocoronary either for the surgery or Significantly shorter length and
bypass up to 3days postop. of stay with roentgenograms
Indications: NR Device/agent: cephalothin postoperative AMP in where indicated.
Setting: 1 university Control group: n=47 one small (N=85) RCT Duration of
hospital 3days: Patients who with data collected 35 hospitalization:
Location: Canada received cephalothin 2g years ago: defined as the
Dates: Sept 1, 1977 intravenously 2dose: 12.034.2 number of days
June 30, 1978 immediately before 3day: 14.67.5 form operation
Inclusion Criteria: All cardiac bypass was P<0.05 until discharge.
patients who begun and 2g at the Perioperative
underwent end of the operation. care: NR
aortocoronary This was then followed Other notes: None
bypass operation at by 1g cephalothin q6h Follow-up: NR
the study hospital for 3 days. Funding Source
during the study Conflicts:
dates. Standard preventive Authors: NR
Exclusion Criteria: IF measures: Institution: NR
patients had a Skin prep: surgical field Study: NR
history of an was sprayed with a Supplies: NR
accelerated allergic combination of
reaction to penicillin polymyxin and
or allergy to bacitracin.
cephalosporins, or if
they refused to give
consent.
2017 American Medical Association. All rights reserved. 220
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Conte RCT To evaluate Number of patients: Intervention group: n=30 SSI Definitions:
32
1972 1, 3, 4, single-dose N=64 1dose 1g cephalothin Organ/Space Sternal SSI Major infection: a
(ES) 5, 6, 7 versus Patient intravenously during 1dose: 1/30 (3.3%) wound infection
multiple dose Characteristics surgery. 20dose: 1/34 (2.9%) with purulent
regimens of The groups were Timing of intervention: drainage and
cephalothin in randomly distributed pre, intra and postop Superficial Sternal SSI positive cultures
patients and did not differ Duration of intervention: 1 dose: 2/30 (6.7%) with our without
undergoing significantly. intraop or from the night 20 dose: 2/34 (5.9%) bacteremia that
th
cardiac Age, y: NR before surgery until 4 required surgical
surgery. Gender: NR day postop Antimicrobial resistance: drainage and
Obesity: NR Device/agent: cephalothin Incisional SSI: The no prolonged the
Comorbidities: NR Control group: n=34 postoperative AMP postoperative
Procedures: cardiac 20dose: received 1g group course.
surgery cephalothin before, 1dose: had 1 Minor infection was
Indications: NR during and after surgery Staphylococcus aureus defined as
Setting: 1 university at 6 hour intervals from and 1 Staphylococcus wound infection
hospital 6pm the night before epidermis infection as with little or no
Location: USA the surgery until noon compared to purulent
th
Dates: 1969 of the 4 postop day. 20dose: 1 Serratia drainage, a
December 1970 Standard preventive marcescens and 1 positive culture,
Inclusion Criteria: measures : NR Enterococcus infection minimal edge
patients scheduled Organ/Space Sternal SSI: separation, and
for cardiac surgery 1dose: The one case of a rapid response
with endocarditis was a to local care.
cardiopulmonary Staphylococcus Perioperative
bypass. epidermis care: NR
Exclusion Criteria: Other notes: None
unwilling to Follow-up:
participate, if there 6months - 2
was a language years
barrier, or if there Funding Source
was difficulty in Conflicts:
comprehension to Authors: Industry
prevent performed Institution: NR
consent. If they were Study: Industry
under 21 years of Supplies: Industry
age, if the case was
an emergency, if
they had received
2017 American Medical Association. All rights reserved. 221
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
penicillin in doses
greater than 400,000
units/day or any
other antimicrobials
during the 2 weeks
prior to surgery, or if
they had a history of
allergic reaction to
the protocol drug.
Also, death from a
noninfectious cause
within 24h after
surgery, significant
deviations from the
protocol or apparent
allergy to the
protocol drug.
2017 American Medical Association. All rights reserved. 222
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.1A3. RISK OF BIAS ASSESSMENTS: Q1 PARENTERAL AMP STUDIES
eTABLE 29. Risk of Bias Assessments of Randomized Controlled Trials for Q1 Parenteral AMP
Funding
Randomiza- Outco- Attrition source(s)
Describ- tion Describ- me smaller than Attrition disclosed and
ed as appropriat- ed as asses- Study Investiga- Attrition 10-15% of appropriat- no obvious Overa-
Author randomi- ely double- sor participa- tor describ- assigned ely conflict of ll Risk
Year Q zed performed blind blinded nt blinded blinded ed patients analyzed interest of Bias
Question 1: Parenteral Antimicrobial Prophylaxis (AMP)
Aberg Mode-
26 1
1991 rate
Akinyoola
1 1 High
2011
Ali
17 1 High
2006
Austin
34 1 High
1980
Bates Mode-
25 1
1992 rate
Becker
43 1 Low
1991
Bernard
36 1 Low
1994
Buckley Mode-
14 1
1990 rate
Carr
23 1 High
1984
Carroll Mode-
40 1
2003 rate
Chang Mode-
41 1
2005 rate
Conte
32 1 Low
1972
Cuthbertson Mode-
10 1
1991 rate
Fujita
15 1 Low
2007
Garotta
19 1 High
1991
Gatell
18 1 Low
1987
Grundmann
24 1 High
1987
2017 American Medical Association. All rights reserved. 223
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Funding
Randomiza- Outco- Attrition source(s)
Describ- tion Describ- me smaller than Attrition disclosed and
ed as appropriat- ed as asses- Study Investiga- Attrition 10-15% of appropriat- no obvious Overa-
Author randomi- ely double- sor participa- tor describ- assigned ely conflict of ll Risk
Year Q zed performed blind blinded nt blinded blinded ed patients analyzed interest of Bias
Haga
52 1 High
2012
Hall
38 1 Low
1998
Hall Mode-
44 1
1989 rate
Hasselgren
37 1 Low
1984
Hemsell
28 1 Low
1984
Hirokawa
54 1 Low
2013
Hussain Mode-
31 1
2012 rate
Imamura Mode-
51 1
2012 rate
Juul Mode-
45 1
1987 rate
Karran Mode-
50 1
1993 rate
Kow Mode-
22 1
1995 rate
Lin
35 1 High
2011
Liu
39 1 Low
2008
30
Lyimo Mode-
1
2013 rate
Macones
4 1 Low
2011
Mayer
27 1 High
1993
McArdle Mode-
47 1
1995 rate
Mendel
46 1 High
1987
Moesgaard 1 Mode-
2017 American Medical Association. All rights reserved. 224
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Funding
Randomiza- Outco- Attrition source(s)
Describ- tion Describ- me smaller than Attrition disclosed and
ed as appropriat- ed as asses- Study Investiga- Attrition 10-15% of appropriat- no obvious Overa-
Author randomi- ely double- sor participa- tor describ- assigned ely conflict of ll Risk
Year Q zed performed blind blinded nt blinded blinded ed patients analyzed interest of Bias
48
1989 rate
Mohri
53 1 Low
2007
Mui Mode-
11 1
2005 rate
Nooyen Mode-
33 1
1994 rate
Oostvogel
16 1 Low
1987
Osman Mode-
3 1
2013 rate
Ritter Mode-
21 1
1989 rate
Soriano Mode-
2 1
2008 rate
Su
13 1 High
2005
Sullivan
8 1 Low
2011
Suzuki Mode-
42 1
2011 rate
Tamayo
12 1 Low
2008
Thigpen
7 1 Low
2005
Togo
55 1 Low
2007
Turano
29 1 High
1992
Wax
9 1 Low
1997
Wenzel Mode-
49 1
1985 rate
Witt
5 1 Low
2011
Wymenga Mode-
20 1
1992 rate
2017 American Medical Association. All rights reserved. 225
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Funding
Randomiza- Outco- Attrition source(s)
Describ- tion Describ- me smaller than Attrition disclosed and
ed as appropriat- ed as asses- Study Investiga- Attrition 10-15% of appropriat- no obvious Overa-
Author randomi- ely double- sor participa- tor describ- assigned ely conflict of ll Risk
Year Q zed performed blind blinded nt blinded blinded ed patients analyzed interest of Bias
Yildirim Mode-
6 1
2009 rate
2.1B. Q2 NON-PARENTERAL AMP
2.1B1. GRADE TABLE Q2: NON-PARENTERAL AMP
eTABLE 30. GRADE Table for Q2 Non-Parenteral AMP
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
Q2. What are the most effective strategies for administering non-parenteral AMP at the surgical incision to reduce the risk of SSI?
Q2A. How safe and effective is antimicrobial irrigation?
Colorectal Surgeries
In one small RCT (N=103), in elective
colorectal cancer surgeries, use of
clindamycin-gentamicin was associated
with a reduction in SSI: 4% vs. 14%;
56 p<0.01. OR: 4.94 (1.27-19.19)
SSI* 1 RCT High 0 0 0 -1 0 0 0 0 Moderate Moderate
Antimicrobial solution was allowed to rest
in the abdominal cavity for 3 minutes.
Clindamycin-
Both groups received preoperative AMP
Gentamicin
with an intraoperative bolus after 4 hours,
Solution vs.
with no mechanical bowel prep
normal saline
Post- irrigation samples were taken only in
the intervention group (post antimicrobial
Antimicrob- irrigation). These cultures were positive in
56
ial 1 RCT 2 patients (4%). Detected microorganisms High 0 0 0 -2 0 0 0 0 Low Low
resistance were Klebsiella spp and Streptococcus
salivarius. Both of these organisms were
resistant to clindamycin and gentamicin.
2017 American Medical Association. All rights reserved. 226
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
Acute Appendectomies
In one RCT (N=246), in acute
appendectomies, irrigation with ampicillin
solution was associated with an overall
57 reduction in SSI: 1/117 (0.9%) vs. 7/132
SSI* 1 RCT High 0 0 0 -2 0 0 0 0 Low
(5.3%); p<0.05
A reduction was specifically seen in SSI
for acute appendicitis cases: 0/88 vs.
6/102 (5.9%); P<0.05
Ampicillin
Product
Solution vs. Low
Related 57 One patient in each group noted some
Normal saline 1 RCT High 0 0 0 -2 0 0 0 0 Low
Adverse redness in the wound
Events
Almost all Streptococci and Enterococci
were sensitive to Ampicillin and 30% of E.
Antimicrob-
57 coli isolates were sensitive to ampicillin in
ial 1 RCT High 0 0 0 -2 0 0 0 0 Low
samples cultured from intraoperative
resistance
peritoneal and wound swabs. E. coli
results were not reported by group.
Q2B. How safe and effective are topical antimicrobial agents applied to the surgical incision?
Topical Ampicillin - Solution
Colorectal Surgeries
In 1 RCT (N=203) in elective colorectal
surgeries, use of topical ampicillin was
associated with no difference in SSI:
5/105 (4.8%) vs. 5/98 (5.1%), (95%CI: -
Ampicillin
5.6-6.2), p=NS
solution vs. 58 Low
SSI* 1 RCT Both groups received preoperative AMP High 0 0 0 -2 0 0 0 0 Low
no topical
of ampicillin and metronidazole which was
antimicrobial
continued 3 times daily for 3 days
postoperatively, and standard or whole-
gut bowel prep
These surgeries included some patients
2017 American Medical Association. All rights reserved. 227
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
with known infections including one with
Fourniers Gangrene (not indicated which
group)
Product
Related 58 No product related hypersensitivity or any
1 RCT High 0 0 0 -2 0 0 0 0 Low
Adverse other adverse events were observed
Events
Acute Appendectomies
In 1 RCT (N=246) of emergency acute
appendectomies, cleaning the
subcutaneous tissues with ampicillin
solution soaked gauze reduced surgical
Ampicillin site infections: 5/126 (4%) vs. 15/120
solution vs. (13%); p<0.02.
59
No topical SSI* 1 RCT Differences were not significant in the High 0 0 0 -1 0 0 0 0 Moderate Moderate
antimicrobial simple appendicitis cases, but were
agent significant in the gangrenous and
perforated cases (advanced) 5/58 (9%)
vs. 14/52 (27%); p<0.02
Both groups received intramuscular
antimicrobial prophylaxis.
Topical Ampicillin - Powder
In 1 RCT (N=170) in elective colorectal
surgeries, ampicillin powder applied to the
subfascial and subcutaneous layers of the
Ampicillin
wound before closure was not associated
powder vs.
60 with a reduction in SSI: 5/81 (6.2%) vs.
No topical SSI* 1 RCT High 0 0 0 -1 0 0 0 0 Moderate Moderate
6/89 (6.7%); p>0.05
antimicrobial
Both groups received parenteral
agent
antimicrobial prophylaxis preoperatively
and 2 additional doses up to 12h postop.
Follow up was not reported
Topical Chloramphenicol
2017 American Medical Association. All rights reserved. 228
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
In a study of 92 hip fracture repairs, no
difference between groups: 12 (13.0%),
Chloramphenic-
4/47 (8.5%) vs. 8/45 (17.8%); p=0.20.
ol vs.
61 Both groups received parenteral
No topical SSI* 1 RCT High 0 0 0 -1 0 0 0 0 Moderate Moderate
antimicrobial prophylaxis
antimicrobial
agent Chloramphenicol ointment was applied to
the surgical site at the end of the
procedure and on postoperative day 3
Topical Rifampin
In a small (N=48), lower-quality study of
patients after video laparoscopic
cholecystectomy, use of rifampin
associated with reduced risk of umbilical
port site infection (defined as purulent
wound leakage: (p<0.005) and fewer local
signs of inflammation (p<0.001)
According to results reported in a
histogram, at 12 hours postoperatively,
purulent wound leakage was present
62 among 34/48 (70.8%) of the study
Rifampin vs. SSI* 1 RCT High -1 0 0 -1 0 0 0 0 Low
population: 10/24 (41.7%) vs. 24/24
No topical
(100%). At 24 hours: 0/24 vs. 24/24 and Low
antimicrobial
by postoperative day seven: 0/24 vs. 2/24
agent
of the normal saline group. Unclear if any
of these were truly infections.
Both groups received parenteral AMP
Sterile rifampin (250mg) applied to the
umbilicus (formulation not specified)
preoperatively, intraoperatively, and
postoperatively (every 12 hours for 72
hours)
Wound
62 Rifampin associated with reduced risk for
Dehiscen- 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
dehiscence (p<0.01)
ce
2017 American Medical Association. All rights reserved. 229
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
Vancomycin Paste
In one RCT at high risk of bias, in 416
heart operations performed via median
Vancomycin
sternotomy there was a reduction in
powder mixed
SSI* sternal / mediastinal SSI with vancomycin
with hemostatic 63
Mediastinal 1 RCT powder mixed with a hemostatic paste High -1 0 0 -1 0 0 0 0 Low Low
paste vs.
/sternal made from absorbable gelatin and topical
Hemostatic
thrombin and applied to the cut sternal
paste
edges vs. hemostatic paste alone: 1/223
(0.45%) vs. 7/193 (3.6%); p=0.02
Autologous Platelet Rich Plasma
In a meta-analysis (N=452) of 4 small
RCTs in cardiac surgery and total knee
arthroplasty, use of autologous platelet
64-
4 RCT rich plasma was not associated with a
Autologous SSI* 67 High 0 0 0 -1 0 0 0 0 Moderate
difference in SSI OR: 1.14 (0.56-2.31);
Platelet rich 2
p=0.72; I =0
plasma-APRP Moderate
Each individual study did not find a
(gel or spray) vs.
difference
No APRP
At two weeks after surgery, use of a spray
Total
65 was associated with decreased likelihood
wound 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
of total wound closure: 11% vs. 35%;
closure
p=0.02
Q2C. How safe and effective are antimicrobial-coated sutures; when and how should they be used?
Antimicrobial- In a meta-analysis (N=5388) of 14 RCTs
coated suture that included heterogeneous surgeries
(absorbable) vs. and patients, sutures, closure levels, and
Non- 14 RCT closure types in both intervention and
68-81 Moderate
antimicrobial- SSI* comparator arms across studies, there High 0 0 0 0 0 0 0 0 High
coated suture was a reduction in SSI: OR: 0.69 (0.55
2
(absorbable and 0.86); p<0.01; I =28%. All studies used
non-absorbable) triclosan-coated suture as the
antimicrobial-coated suture.
2017 American Medical Association. All rights reserved. 230
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
In a meta-analysis (N=1081) of 4 RCTs
that included heterogeneous surgeries
and patients, no difference in organ/space
SSI rates was observed: OR: 0.49 (0.07
2
3.43); p=0.47; I =71%. All studies used
triclosan-coated suture as the
antimicrobial-coated suture.
1 RCT abdominal wound was closed
74
with interrupted sutures using either
triclosan coated vs. uncoated 910 braided
polyglactin. Skin was closed with staples
Organ/ 4 RCT
1 RCT abdominal sheath was closed
78
74,78-80 High 0 -1 0 -1 0 0 0 0 Low
Space SSI
using either triclosan coated vs. uncoated
910 braided polyglactin. Skin closure was
not reported
1 RCT wound was closed using either
79
triclosan coated vs. uncoated 910 braided
polyglactin. Skin closure was not reported
1 RCT galea and fascia were closed
80
with using either triclosan coated vs.
uncoated 910 braided polyglactin. Skin
closure was with absorbable
monofilament sutures
In a meta-analysis (N=1285) of 2 RCTs
that included colorectal and abdominal
surgeries, no difference in deep SSI rates
was observed: OR: 0.86 (0.49 1.54);
2
p=0.62; I =0.
1 RCT fascia closure occurred via
77
2 RCT
Deep SSI* 77,78 High 0 0 0 -1 0 0 0 0 Moderate
continuous mass closure using triclosan
coated or uncoated polydioxanone
sutures. Skin was closed using staples
1 RCT abdominal sheath was closed
78
using either triclosan coated vs. uncoated
910 braided polyglactin. Skin closure was
2017 American Medical Association. All rights reserved. 231
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
not reported.
In a meta-analysis (N=1922) of 4 RCTs
that included heterogeneous surgeries, no
difference in superficial SSI rates was
observed: OR: 1.06 (0.76 1.48); p=0.72;
2
I =0.
1 RCT fascia closure occurred via
77
continuous mass closure using triclosan
coated or uncoated polydioxanone
sutures. Skin was closed using staples
1 RCT abdominal sheath was closed
78
using either triclosan coated vs. uncoated
910 braided polyglactin. Skin closure was
not reported
Superficial 4 RCT
1 RCT wound was closed using either
79
72,77-79 High 0 0 0 0 0 0 0 0 High
SSI
triclosan coated vs. uncoated 910 braided
polyglactin. Skin closure was not reported
1 RCT the subcutaneous and
72
subcuticular layers were closed with
triclosan coated or uncoated braided 910
polyglactin or with triclosan coated or
uncoated poliglecaprone 25 at the
surgeons discretion. Wounds were
dressed with butterfly stitches, sterile
adhesive dressing and either transparent
adhesive wound covering or non-
transparent adhesive wound covering or
wound covering alone
In 1 RCT mean ASEPSIS score was
73
lower in the triclosan coated suture group
ASEPSIS 2 RCT
72,73 at all times measured (day 4, 30, 60) but High 0 0 0 -1 0 0 0 0 Moderate
score
never reached statistical significance at all
specified endpoints
2017 American Medical Association. All rights reserved. 232
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
In 1 RCT mean ASEPSIS score was
72
lower in the triclosan-coated suture group
at two weeks postop but this did not reach
statistical significance. There was no
difference at 6 weeks postop.
No studies reported specific testing for
triclosan resistance.
In 3 RCT
68,69,71
wounds were cultured and
no antibiotic resistant strains were
reported at 30 days follow up.
In 1 RCT wounds were cultured and no
78
antibiotic resistant strains were found at 1
year follow up.
In 1 RCT wounds were cultured and no
79
MRSA was recovered from wounds in
either group at 30 days follow up.
In 1 RCT preoperatively screened
75
Antimicrob- 8 RCT patients at risk for MRSA or with previous
68,69,71,74,
ial MRSA incidence and decontamination High 0 0 0 -2 0 0 0 0 Low
75,78-80
resistance had wounds cultured 2 weeks post op with
no resistant bacteria reported.
In 1 RCT in pediatric cerebrospinal fluid
80
shunt implants and revisions, wounds
were cultured: MRSA: 1/2 (50%) vs. 1/8
(12.5%) for antimicrobial suture vs.
standard, both in revision surgeries at up
to 6 months follow up.
In 1 RCT in elective colorectal surgeries,
74
wounds were cultured and suggested no
difference in the incidence of MRSA: 0/9
vs. 1/19 (5.3%); missing data: 2/9 (22.2%)
vs. 6/19 (31.6%) at 30 days follow up.
Wound
3 RCT Meta-analysis of 3 RCTs (N=1582): OR:
Dehiscen- 70,73,77 2 High 0 -1 0 -1 0 0 0 0 Low
0.89 (0.31 2.58); p=0.83; I =76%
ce
2017 American Medical Association. All rights reserved. 233
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
1 RCT of 374 CABG leg harvesting sites
73
suggested no difference in non-infectious
leg wound dehiscence within 60 days:
11/161 (6.8%) vs. 13/152 (8.5%); p=NS
1 RCT (N=1185) in mixed open
77
abdominal surgeries suggested no
difference in non-infectious wound
dehiscence: 66/587 (13.4%) vs. 81/598
(16.3%), OR: 0.80 (0.56-1.14); p=0.21;
however the study suggested a decrease
in reoperation for burst abdomen with
triclosan-coated sutures as compared to
controls: 9/587 (1.9%) vs. 22/598 (4.5%);
OR: 0.80 (0.18-0.88); p=0.02.
1 RCT suggested a reduction in
70
dehiscence with triclosan coated sutures:
1/91 (1.1%) vs. 7/93 (7.7%); p=0.03.
Adverse
4 RCT
77,78,80,81
events- 4 RCT no serious adverse events
77,78,80,81 High 0 0 0 -2 0 0 0 0 Low
product reported for either suture type.
related
Colorectal Surgery
In a meta-analysis (N=1912) of 5 RCTs in
colorectal surgery, no difference in SSI:
2
OR: 0.71; (0.47 1.08); p=0.11; I =48%.
Antimicrobial-
2 RCTs suggested a reduction in SSI: 1
coated suture 74
large RCT (N=410) at 30 day follow up
(absorbable) vs.
5 RCT where abdominal wounds were closed
Non- 70,71,74,75,
SSI* with interrupted sutures using either High 0 0 0 -1 0 0 0 0 Moderate Moderate
antimicrobial- 77,82
triclosan coated vs. uncoated 910 braided
coated suture
polyglactin and skin was closed with
(absorbable and 70
staples. 1 small RCT (N=182), with
non-absorbable)
follow up not reported, the abdominal wall
was closed with single-layer mass
technique (peritoneum, muscle & fascia)
2017 American Medical Association. All rights reserved. 234
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
using triclosan coated or uncoated
braided size 0 polyglactin 910. Skin was
closed with non-absorbable monofilament
polyamide. Both suggested a reduction in
SSI 9/206 (4.3%) vs. 19/204 (9.3%);
p=0.05; and 4/91 (4.3%) vs. 12/91
(13/2%); p=0.04 respectively.
Preoperative AMP was followed by an
intraoperative bolus delivered at 3h and
antibiotics were continued for 48h postop
in the larger study. AMP was delivered at
induction of anesthesia in the smaller
study and wound infection was not
defined.
1 subanalysis of 243 colorectal surgeries
75
in a study of abdominal surgeries where
abdominal fascia was closed with coated
or uncoated 2-0 monofilament
polydioxanone loop; no subcutaneous
sutures were used; skin was closed with
staples; suggested a reduction in SSI
though not significant: 17/143 (12%) vs.
19/100 (19%). This study was conducted
as a part of a clinical care pathway.
1 subanalysis of a large, multicenter
77,82 71
RCT (N=690) and 1 RCT (N=385)
suggested no difference in SSI at 30
77,82
days.1 Subanalysis of 690 colorectal
surgeries suggested no difference: 62/344
(18.0%) vs. 60/346 (17.3%); p=0.81.
Continuous mass closure with triclosan-
coated or uncoated polydioxanone
sutures were used for the fascia, skin
closure was achieved with staples and
antimicrobial prophylaxis was given prior
2017 American Medical Association. All rights reserved. 235
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
71
to skin incision, 1 RCT (N=385)
suggested no difference: 23/188 (12.2%)
vs. 24/197 (12.2%); Preoperative AMP
was delivered 30 minutes before incision.
Triclosan coated sutures were used in
skin closure for both intervention and
control groups.
Abdominal Surgeries, Laparotomies & Appendectomies (excluding colorectal)
In a meta-analysis (N=1208) of 3 RCTs,
antimicrobial sutures reduced SSI: OR:
2
0.63; 95% CI: 0.42 0.95; p=0.03; I =0.
1 subanalysis of 612 abdominal
75
surgeries suggested a reduction in SSI:
14/341 (4.1%) vs. 23/271 (8.5%). This
study was conducted as a part of a clinical
care pathway where abdominal fascia was
closed with coated or uncoated 2-0
monofilament polydioxanone loop; no
Antimicrobial-
subcutaneous sutures were used; and
coated suture
skin was closed with staples.
(absorbable) vs.
77
Non- 3 RCT 1 subanalysis of 495 mixed abdominal
SSI* 75,77,78 surgeries where fascia closure occurred High 0 0 0 0 0 0 0 0 High High
antimicrobial-
via continuous mass closure using
coated suture
triclosan coated or uncoated
(absorbable and
polydioxanone sutures and skin was
non-absorbable)
closed using staples at 30 day follow up:
no difference in SSI: 25/243 (10.3%) vs.
36/252 (14.3%); Preop AMP was
administered 30-60 minute before incision
in both studies.
1 small (N=100) RCT in
78
appendectomies, where the abdominal
sheath was closed using either triclosan
coated vs. uncoated 910 braided
polyglactin and skin closure was not
2017 American Medical Association. All rights reserved. 236
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
reported, suggested no difference at 1
year follow up: 5/50 (10%) vs. 4/50(8%);
p=0.73; all were superficial SSIs except
for 1 deep SSI in the control group
All Surgeries except Colorectal and Abdominal Surgeries, Laparotomies & Appendectomies
Antimicrobial-
coated suture
In a meta-analysis (N=2183) of 8 RCTs in
(absorbable) vs.
8 RCT heterogeneous surgeries and patient
Non- 68,69,72,73,
SSI* populations, antimicrobial sutures reduced High 0 0 0 0 0 0 0 0 High High
antimicrobial- 76,79-81
SSI OR: 0.68 (0.49 0.95); p=0.02;
coated suture 2
I =24%.
(absorbable and
non-absorbable)
Cardiac Surgery
One RCT (N=510) suggested no
79
difference in sternal infections at 30 day
follow up: 4/170 (2.4%) vs. 12/340 (3.5%);
Sternal 79 OR: 0.66 (0.21-2.07); p=0.48. Triclosan
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
SSI* coated or uncoated polyglactin 910
sutures were used, but the level of closure
was not specified, AMP and skin prep
Antimicrobial-
were not reported.
coated suture
In a meta-analysis (N=1099) of 3 RCTs in
(absorbable)
cardiac surgeries, there was a suggestion
versus non-
that antimicrobial sutures reduced SSI Moderate
antimicrobial- 2
(OR: 0.72 (0.48 1.09); p=0.12; I =0.
coated suture
2 RCT (N=510 and N=328 ) suggested
79 69
(absorbable and
Donor Site no difference in donor site SSI at 1 month
non-absorbable) 3 RCT
Superficial 69,73, 79 follow up: 5/142 (3.5%) vs. 10/260 (3.8%); High 0 0 0 0 -1 0 0 0 Moderate
SSI* p=1.00; and 16/160 (10%) vs. 17/163
(10.4%) respectively. The larger of the two
did not report AMP or standard preventive
measures and wounds were closed with
either triclosan coated or uncoated
polyglactin 910 (level of closure not
2017 American Medical Association. All rights reserved. 237
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
specified). The smaller RCT utilized
triclosan coated or uncoated polyglactin
910 (level of closure was not specified),
alcohol CHG skin prep and preoperative
AMP, an intraoperative bolus at 3h with
antibiotics administered up to 24h postop.
1 RCT (N=374) suggested a decrease
73
in donor site SSI at 60 days follow up:
23/184 (12.5%) vs. 38/190 (20.0%);
p=0.05. Patients were administered AMP
30 minutes prior to incision, an
intraoperative bolus at 2h and were given
2 additional antibiotic doses up to 24h
postop. Normothermia was maintained.
This study utilized antimicrobial sutures in
both the subcutaneous and cutaneous
layers in the intervention arm.
Breast Cancer Surgery
1 RCT in mixed breast cancer surgeries
72
Antimicrobial- (N=146) suggested no difference at 6
coated suture weeks follow up: 10/66 (15.2%) vs. 14/61
(absorbable) vs. (22.9%); p=NS. Triclosan coated sutures
Non- 72 were used in both subcutaneous and
SSI* 1 RCT High 0 0 0 -1 0 0 0 0 Moderate Moderate
antimicrobial- subcuticular closure in the intervention
coated suture arm. 8/146 patients were administered
(absorbable and preoperative AMP and 0/8 developed SSI.
non-absorbable) Not reported which group these 8
belonged.
Mixed Surgeries
Antimicrobial- A meta-analysis (N=597) of 2 RCTs of
coated suture mixed surgical populations, suggested no
(absorbable) vs. 2 RCT difference SSI OR: 0.76 (0.13-4.46);
SSI* 76,81 2 High 0 0 0 -1 0 0 0 0 Moderate Moderate
Non- p=0.76; I =45%.
1 RCT in mixed surgeries (N=450)
76
antimicrobial-
coated suture suggested a decrease in SSI at 60 days
2017 American Medical Association. All rights reserved. 238
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
(absorbable and follow up: 17/230 (7%) vs. 33/220 (15%);
non-absorbable) p=0.01.
Triclosan coated or uncoated polyglactin
910 sutures were used in all surgical
steps, except in some cases
polypropylene sutures were used for
laparotomy closure and vascular sutures.
Poliglecaprone 25 was used for skin
closure for the entire uncoated suture
group. In the triclosan coated suture
group, skin closure was not uniform
across surgical specialties. Standard of
care was not uniform and not in line with
current standards in some instances. It is
not reported which group these patients
belonged to.
1 RCT (N=147) in mixed pediatric
81
general surgery patients used coated or
uncoated polyglactin 910 for unspecified
levels of closure and suggested an
increase in SSI with triclosan coated
sutures 80 days follow up, however this
difference was not significant: 3/98 (3.1%)
vs. 0/49; p=0.22. AMP was not reported
Lower Limb Revascularization
1 RCT in lower limb revascularization
Antimicrobial- surgeries (N=276) where triclosan coated
coated suture or uncoated polyglactin was used for
(absorbable) vs. subcutaneous closure, and triclosan
Non- 68 coated or uncoated poliglecaprone
SSI* 1 RCT High 0 0 0 -1 0 0 0 0 Moderate Moderate
antimicrobial- sutures were used for intracutaneous
coated suture closure; suggested no difference in SSI at
(absorbable and 30 days follow up: 31/139 (22.3%) vs.
non-absorbable) 30/137 (21.9%); OR: 1.02 (0.58-1.81);
p=0.94. Although AMP was not
2017 American Medical Association. All rights reserved. 239
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
standardized across hospitals, differences
were evenly distributed across groups.
Triclosan coated sutures were used in
both subcutaneous and intracutaneous
closure in the intervention arm.
Pediatric Cerebrospinal Fluid Shunt Surgeries
1 RCT in pediatric cerebrospinal shunt
fluid surgeries (N=61) where galea and
fascia were closed with triclosan coated
Antimicrobial- or uncoated polyglactin 910 and skin was
coated suture closed with absorbable poliglecaprone 25
(absorbable) vs. sutures, suggested a reduction in SSI at
Non- 80 6 month follow up: 2/46 (4.3%) vs. 8/38
SSI* 1 RCT High 0 0 0 -1 0 0 0 0 Moderate Moderate
antimicrobial- (21%); OR: 0.17 (0.03-0.86); p=0.03.
coated suture Skin prep with CHG & PI; Pre-op AMP;
(absorbable and iodine-impregnated adhesive drapes;
non-absorbable) antibiotic wound irrigation prior to
closure. Silicone shunt components were
soaked in antibiotic solution before
implantation
Q2D. How safe and effective are antimicrobial dressings applied to surgical incisions following primary closure in the operating room?
One small RCT (N=112) in elective
83
colorectal cancer surgeries suggested no
difference in SSI rates when comparing a
moisture retentive dressing containing
Silver
1.2% ionic silver with standard dressing:
impregnated
9/58 (15.5%) vs. 11/54 (20.4%); p=0.62
dressing vs. 2 RCT
One small RCT (N=109) in elective
84
SSI* 83,84 High 0 -1 0 0 0 0 0 0 Moderate Moderate
standard
colorectal surgeries suggested a reduction
dressing or
in SSI using silver nylon dressing vs.
gauze
standard gauze and tape: 7/ 55 (13%) vs.
18/54 (33%); p=0.01. Any questionable
SSI treated with antibiotics was included
in SSI definition
2017 American Medical Association. All rights reserved. 240
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
One small RCT (N=112) in elective
83
colorectal cancer surgeries suggested no
Organ/ 83 difference in organ/space SSI rates when
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Space SSI* comparing a moisture retentive dressing
containing 1.2% ionic silver with standard
dressing: 1/58 (1.7%) vs. 1/54 (1.9%)
One small RCT (N=112) in elective
83
colorectal cancer surgeries suggested no
difference in deep SSI rates when
comparing a moisture retentive dressing
containing 1.2% ionic silver with standard
dressing: 3/58 (5.2%) vs. 2/54 (3.7%).
2 RCT
One small RCT (N=109) in elective
84
Deep SSI* 83,84 High 0 0 0 -1 0 0 0 0 Moderate
colorectal surgeries suggested no
difference in deep SSI using silver nylon
dressing vs. standard gauze and tape: 2/
55 (4%) vs. 4/54 (7%); p=0.4. Any
questionable SSI treated with antibiotics
was included in SSI definition.
One small RCT (N=112) in elective
83
colorectal cancer surgeries suggested no
difference in superficial SSI rates when
comparing a moisture retentive dressing
containing 1.2% ionic silver with standard
dressing: 5/58 (8.6%) vs. 8/54 (14.8%);
Superficial 2 RCT p=0.80
83,84 High 0 0 0 -1 0 0 0 0 Moderate
One small RCT (N=109) in elective
84
SSI*
colorectal surgeries suggested a reduction
in superficial SSI using silver nylon
dressing vs. standard gauze and tape: 5/
55 (9%) vs. 14/54 (26%); p=0.02. Any
questionable SSI treated with antibiotics
was included in SSI definition.
2017 American Medical Association. All rights reserved. 241
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE GRADE
Publication Bias
Overall
Dose-response
Quantity Starti- of
Study Quality
Confounders
Consistency
GRADE
Directness
Magnitude
Precision
and Type ng Eviden-
Comparison Outcome Findings of
Large
of GRAD- ce for
Eviden-
Evidence E Outco-
ce Base
me
No difference in median length of stay
Length of 83
1 RCT between groups: 6 (3-21) vs. 6.5 (2-17) High 0 0 0 -1 0 0 0 0 Moderate
Stay
days
Adverse 83 No adverse events were noted relating to
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
events the study intervention
*Critical outcome; OR: Odds Ratio; RR: Risk Ratio; CI: Confidence Interval
2.1B2. EVIDENCE TABLES: Q2 NON-PARENTERAL AMP
Q2. What are the most effective strategies for administering non-parenteral antimicrobial prophylaxis at the surgical incision to reduce the risk of SSI?
eTABLE 31. Evidence Table for Q2A. How safe and effective is antimicrobial irrigation?
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Ruiz- RCT To evaluate Number of patients: Intervention group: n= SSI: (30 days) Definitions:
Tovar 1, 2, 4, the effects of N= 108 52 Wound infection: Wound infection:
56
2012 5, 7, 8, peritoneal Patient Irrigation of the entire Intervention:4% (2/54) presence of a
(ES) 9, 10 lavage with Characteristics: Age, abdominal cavity was Control:14% (7/51) purulent
normal saline y: (meanSD) performed with 500mL P=0.009 discharge from
or an antibiotic Intervention: normal saline followed OR: 4.94 (1.27-19.19) the surgical
solution 69.911.5 by a second lavage with wound and
(clindamycin- Control: 68.510.2 a 500mL gentamicin- Intraabdominal abscess: confirmed with
gentamicin) on Gender: female/male clindamycin solution Intervention: 0/54 microbiologic
intra- Intervention: 60/40 (gentamicin 240mg Control: 6% (3/51) culture.
abdominal Control: 62/38 Clindamycin 600mg) P=0.014 Intra-abdominal
abscesses Obesity: NR During this lavage; the OR: 2.14 (1.13-3.57) abscess: the
and wound Comorbidities: solution was allowed to All abscesses were presence of fluid
infection, and Diabetes Mellitus sit in the abdominal smaller than 4cm and collection at CT
to determine Intervention: 32% cavity for 3 minutes. were managed without scan in a
the Control: 29% Timing of intervention: requiring percutaneous symptomatic
microbiologic Procedures: Intraoperatively drainage. patient,
impact of both Sigmoidectomy, right Duration of intervention: Other infections: NR presenting with
irrigations on colectomy, upper Intraoperatively Topic-specific fever, abdominal
2017 American Medical Association. All rights reserved. 242
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
peritoneal anterior resection of Device/agent: 500mL outcomes: NR pain, prolonged
contamination. rectum, Hartmann gentamicin-clindamycin Reoperations: NR postoperative
procedure, Miles solution (gentamicin Length of stay: NR ileus, or septic
procedure, Lower 240mg Clindamycin Mortality: NR status.
anterior resection of 600mg) Adverse events: NR Anastomotic leak:
rectum, left Monitoring intervention: evidence of
colectomy, total NA Antimicrobial rectal contrast
colectomy, palliative Control group: n=51 Resistance: extravasation at
colostomy, palliative Irrigation of the entire Post- irrigation samples CT scan.
ileostomy. No abdominal cavity was were taken only in the Perioperative
significant difference performed with 500mL intervention group (post care: NR
between groups in normal saline followed antimicrobial irrigation). Other notes: NR
surgery distribution. by aspiration of the Cultures were positive in 2 Follow-up: 30
Indications: Tumor liquid and abdominal patients (4%) Detected days post
stage wall closure. microorganisms were discharge
I Standard preventive Klebsiella spp and Funding Source
Intervention: 26% measures: Streptococcus salivarius. Conflicts:
Control: 22% Antimicrobial Prophylaxis: Both of these organisms Authors: None
II ciproflaxin 400mg and were resistant to Institution: None
Intervention: 50% metronidazole 1,500 gentamicin and Study: None
Control: 54% mg. Single dose clindamycin. Supplies: None
III preoperatively, within
Intervention: 20% 30 minutes of incision
Control: 24% and redosed after 4
Setting: 1 hospital hours when surgery is
Location: Spain prolonged.
Dates: January 2010 Mechanical bowel prep:
December 2010 none.
Inclusion Criteria: Surgical Approach: open
Diagnosis of Bowel clamping:
colorectal performed by all
neoplasms and surgeons
elective colorectal Closure: abdominal wall
surgery. was closed using
Exclusion Criteria: continuous sutures of
Preoperative absorbable
diagnosis of chronic monofilament
renal failure (due to polydioxanone (size no
risk of nephrotoxicity 2). Skin was closed with
2017 American Medical Association. All rights reserved. 243
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
associated with staples.
intraperitoneal
gentamicin
absorption) or
anastomotic leak in
the postoperative
course which would
represent a bias in
the diagnosis of
intra-abdominal
infection.
Al-Shehri RCT To investigate Number of patients: Intervention group: SSI: (1 month) Definitions:
57
1994 1, 6, 7, the efficacy of N= 249 n=117 Total Wound infection:
(ES) 8, the addition of Patient Wounds were irrigated Intervention: 1/117 purulent
topical Characteristics: with 1g ampicillin in 100 (0.9%) discharge in the
ampicillin to groups were ml sterile normal saline Control: 7/132 (5.3%) wound
systemic comparable by at closure P<0.05 regardless of the
antimicrobials characteristics listed Timing of intervention: Acute appendicitis: culture results or
in reducing below intraoperatively Intervention: 0/88 occurrence of
post Age, y: mean (range) Duration of intervention: Control: 6/102 (5.9%) serous
appendectomy Intervention: 24 (4-66) NA P<0.05 discharge with a
wound Control: 21 (5-80) Device/agent: 1 g positive growth
infection rate Gender: male ampicillin on 100ml Other infections: NR on culture.
in a properly Intervention: 77/117 sterile normal saline Perioperative
controlled (65.8%) Monitoring intervention: Topic-specific care: NR
randomized Control: 90/132 NA outcomes: Other notes:
prospective (68.2%) Control group: n=132 Intraabdominal pelvic Follow-up: one
trial Obesity: NR Wounds were irrigated abscesses: none in month
Comorbidities: NR with 100 ml sterile either group Funding Source
Procedures: normal saline at Postoperative ileus Conflicts:
appendectomy closure. Intervention: 1/117 Authors: NR
through gridiron Standard preventive (0.9%) Institution: NR
incision measures: Control: 2/132 (1.5%) Study: NR
Indications: Mechanical bowel prep: Fever (attributed to Supplies: NR
Normal Appendix: AMP: intravenous atelectasis and treated
Intervention: 26/117 metronidazole (500mg with chest physiotherapy
(22.2%) for adults and and early ambulation)
Control: 27/132 15mg/kg/body weight Intervention: 3/117
(20.5%) for children) and (2.6%)
2017 American Medical Association. All rights reserved. 244
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Acute Appendix: gentamicin (75mg for Control: 2/132 (1.5%)
Intervention: 88/117 adults and
(75.2%) 1.5mg/kg/body weight Length of stay:
Control: 102/132 for children) one hour Intervention: 77/117
(77.3%) before surgery. If (65.8%)
Advanced appendicitis appendix was found to Control: 90/132 (68.2%)
(histologically proven be gangrenous or
gangrenous or perforated antibiotics Mortality:
perforated appendix) were continued for 5 Adverse events:
Intervention: 3/117 days postoperatively. Redness in wound
(2.6%) Intervention: 1/117
Control: 3/132 (2.3%) (0.9%)
Setting: 1 University Control: 1/132 (0.8%)
Hospital Antimicrobial
Location: Saudi Arabia Resistance:
Dates: Almost all streptococci and
Inclusion Criteria: enterococci were
patients undergoing sensitive to ampicillin
appendectomy besides 30% of the E.
through gridiron coli isolates. (overall
incision for clinically numbers not reported)
suspected acute
appendicitis
Exclusion Criteria:
Allergy to ampicillin
and other systemic
diseases requiring
systemic antibiotic
administration
2017 American Medical Association. All rights reserved. 245
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
eTABLE 32. Evidence Table for Q2B. How safe and effective are antimicrobial agents applied to the surgical incision?
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Dorge RCT To investigate Number of patients: Intervention group: n= SSI: (at 30 days) Definitions:
67
2013 1 whether the N=196 97 Deep sternal wound Deep sternal
(ES) topical Patient PRP and thrombin were infection: wound infection
application of Characteristics: injected simultaneously Intervention: 6/97 (6.2%) requiring
autologous There were no between the sternal Control: 3/99 (3.0%) revision surgery:
PRP (platelet differences with edges after the sternal P=0.293 CDC definition
rich plasma) respect to age, sex, wires had been placed Other infections: NR and clinical
reduces the type of operation, and to the presternal Topic-specific evidence of
incidence of and operative data tissue using the outcomes: NR mediastinitis
deep sternal between groups. recommended dual Reoperations: all DSWI seen at revision
wound Risk factors were spray applicator required reoperation. surgery.
infections in distributed equally immediately prior to Length of stay: NR Perioperative
patients at between groups sternal closure. Mortality: NR care:
high risk Age, y: meanSD Timing of intervention: Adverse events: NR Other notes:
undergoing Intervention: 68 (8.6) intraoperative Follow-up: 30
cardiac Control: 67 (9.5) Duration of intervention: days
surgery with Gender male intraoperative Funding Source
full Intervention: 76/97 Device/agent: blood was Conflicts:
sternotomy. (78.4%) drawn just prior to Authors: NR
Control: 66/99 surgery and mixed with Institution: NR
(66.6%) 6 and 1.2mL Study: Industry
Obesity: BMI >30 anticoagulant calcium Supplies: NR
2
kg/m citrate 5.5%
Intervention: 29/97 respectively. The
(29.9%) anticoagulated blood
Control: 37/99 was then processed
(37.4%) using a platelet
Comorbidities separation system to
Diabetes mellitus yield 12mL autologous
Intervention: 43/97 PRP and 8mL thrombin.
(44.3%) Monitoring intervention:
Control: 32/99 NA
(32.3%) Control group: n=99
Renal failure: Thrombin injected only
Intervention: 0/97 during closure.
Control: 3/99 (3.0%) Standard preventive
Procedures: elective measures:
cardiac surgery with Preop Skin prep: shower
2017 American Medical Association. All rights reserved. 246
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
full sternotomy on morning prior to surgery
cardiopulmonary Hair Removal: patients
bypass and were shaved the
cardioplegic cardiac morning prior to the
arrest. operation.
Indications: NR AMP: intravenous
Setting: 1 university antibiotic prophylaxis
hospital with 3 x 2g cefazolin.
Location: Germany Skin prep: operative field
Dates: 9 months NR was wiped with
when. povidone-iodine
Inclusion Criteria: at alcohol.
least one risk factor Drapes: patients were
for deep sternal draped in standard
wound infection fashion & operative field
(DSWI)including was covered in an
diabetes mellitus adhesive transparent
(oral anti-diabetic drape.
medication or insulin
dependent), chronic
obstructive lung
disease (inhalative
steroids), renal
insufficiency (chronic
dialysis), obesity
2
(BMI>30kg/m ),
reduced left
ventricular function
(*ejection fraction
<35), old age (>80
years) use of double
IMA, and chronic
use of systemic
corticosteroids.
Exclusion Criteria:
emergency
operation (operation
within 24 hours of
admission) and
2017 American Medical Association. All rights reserved. 247
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
acute infection.
Patients were
excluded
postoperatively if the
thorax had to be left
open with a
secondary closure,
or if they had to
undergo
rethoracotomy of
any cause except
DSWI.
Almdahl RCT To explore the Number of patients: Intervention group: n= SSI: (Day 3 and 6 w Definitions:
64
2011 1, 2, 7, potential of N=139 69 postop) SSI: ASEPSIS
(ES) 8, 9 Platelet-rich Patient PRP was sprayed on the Harvest Site Infection (6 Score (day 3);
plasma (PRP) Characteristics: wound immediately weeks): CDC definitions
spray Relevant baseline before closure. Platelet Overall: 17/139 (12%) (6w postop).
treatment to variables were well pure plasma (PPP) was Intervention: 9/69 (13%) Perioperative
prevent leg matched between applied after wound Control: 8/70 (11%) care: Same
wound groups except the closure. P=0.80 (95%CI: -13% to between groups.
infections from lesser preoperative Timing of intervention: 9%) Other notes: The
open use of statins in the Intraoperatively There was no correlation confounding
saphenous control group (see Duration of intervention: between early (day 3) effect of statins
vein below) Intraoperatively secretion and is explained to
harvesting for Age, y: meanSD Device/agent: Platelet- development of wound have minor
Coronary Intervention: 64.88.6 rich plasma spray infection (p=0.64) importance and
Artery Bypass Control: 66.08.8 (made using autologous Positive cultures it doesnt affect
Graft (CABG) Gender, male: thrombin). A measure Intervention: 6 the conclusions.
Intervention: 84.1% of 55cc whole blood Control: 4 They had expected
Control: 84.3% was collected giving All contained S. aureus an SSI rate of
2
Obesity: BMI kg/m about 7ccof PRP and except in one with B. 20% with goal of
meanSD about 30cc of platelet fragilis and one 15% reduction to
Intervention: 27.23.9 pure plasma (PPP). betahemolytic 5% with PRP
Control: 27.73.8 Monitoring intervention: Streptococcus treatment (not
Comorbidities NR Other infections: NR achieved).
Current smoker Control group: n= 70 Topic-specific Follow-up:
Intervention: 21.7% Standard surgical outcomes: Wounds were
Control: 14.3% technique with no Cosmetics (Self scored: 1- inspected at day
Previous smoker additional wound 10) 3 (ASEPSIS
2017 American Medical Association. All rights reserved. 248
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Intervention: 31.9% spraying or Intervention: mean 8.7 Score). 6 weeks
Control: 47.1% applications. (range 2-10, median 9) postoperatively,
Diabetes Standard preventive Control: mean 8.6 (range the patients
Intervention: 23.2% measures: 5-10, median 9) were called and
Control: 18.6% Vein harvesting: P=0.34 assessment of
Statin undertaken by the full Top Score (10) wound infection
Intervention: 94.2% open technique. Intervention: 29 (42.0%) occurrence was
Control: 78.6% Closure: harvest wound Control: 18 (25.7%) made according
P=0.01 was closed with P=0.50 to a specific form
Procedures: CABG- intracutaneous ASEPIS Score (Day 3) (CDC criteria).
related open poliglecaprone Intervention: 13 patients Follow-up was
saphenectomy according to local & total scores 33 100%.
Indications: NR routine. Control: 14 patients and Funding Source
Setting: I hospital Antimicrobial prophylaxis: total scores 34 Conflicts:
Location: Norway 2g intravenous P=0.51 Authors: NR
Dates: January cephalothin 5 times Reoperations: NR Institution: NR
October 2008 until the first Length of stay: NR Study: NR
Inclusion Criteria: postoperative day. Mortality: All patients Supplies: Industry
Patients undergoing survived
first-time CABG Adverse events: No
using treatment related
cardiopulmonary adverse events were
bypass and cold observed.
crystalloid Note: 3 intervention and 4
cardioplegic arrest control patients who
Exclusion Criteria: fulfilled SSI criteria
Patients with received antimicrobial
bleeding disorders treatment without prior
and those on microbiological
immunosuppressive specimen.
medication
(including
cyclooxygenase
(COX)-II inhibitors).
Litmathe RCT To answer Number of patients: Intervention group: n= SSI: (follow up 40 days) Definitions: NR
66
2009 1, 3, 4, whether the N=44 22 No statistically significant Perioperative
(ES) 5 application of Patient Autologous platelet gel differences in healing care:
autologous Characteristics: (APG) was applied to between groups. Surgical
platelet gel Age, y:meanSD the surgical wounds. Major sternal bone and techniques:
2017 American Medical Association. All rights reserved. 249
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
(APG) will Intervention: 65.88.1 This included the soft tissue complication CABG was
lead to a Control: 669.1 sternal bone, the leading to surgical performed using
reduction in Gender: m:f presternal soft tissue, revision (with the standard
sternal wound Intervention:14:8 and the vein-harvesting satisfactory results after approach of a
and vessel Control: 17:5 site. secondary surgery): median
2
harvest site Obesity, BMI; kg/m , Timing of intervention: Total: 4/44 (9%) sternotomy
infections and meanSD Intraoperatively Intervention: 1/22 (4.5%) using the
a reduction in Intervention: 32.44.3 Duration of intervention: Control: 3/22 (13.6%) extracorporeal
postoperative Control:34.212.3 Application time circulation (ECC)
blood loss in Comorbidities Device/agent: Autologous Major healing and warm blood
high-risk Diabetes Mellitus: platelet gel (APG) complications at vein cardioplegia
patients 44/44 patients prepared using a max harvest site according to
undergoing IDDM: 10/22 (45.5%) in of 16ml whole blood (successfully treated Calafiore.
cardiac each group collected through an with vacuum assisted Combined
surgery. existing line and closure therapy) procedures were
Procedures: Elective anticoagulated with Total: 4/44 (9%) carried out using
Coronary artery citrate dextrose Intervention: 2/22 (9%) cold crystalloid
bypass grafting solution. Per patient a Control: 2/22 (9%) cardioplegic
(CABG) or combined maximum of 9-30ml of solution
coronary surgery platelet-rich plasma Other infections: NR Other notes:
and valve was produced. Topic-specific Wound healing
replacement without Monitoring intervention: outcomes: The need of data was
redo. NR transfusion was lower in presented in bar
Indications: NR Control group: n= 22 the intervention group graphs.
Setting: 1 hospital The sternal wound and but not statistically Follow-up: at 4, 15
Location: Germany vein harvesting site significant. and 40 days.
Dates: NR received conventional Cumulative ventilation time Funding Source
Inclusion Criteria: All treatment only Intervention: 11.78.4h Conflicts:
patients at risk for Control: 1412.2h Authors: NR
the development of Standard preventive P=0.5 Institution: NR
surgical wound measures: Drainage blood loss at 6, Study: NR
infections who Anti-platelet drug 12h and before removal Supplies: NR
required cardiac medication: (at least of chest tube was
surgery including aspirin) 7 days prior to slightly higher for
those with diabetes surgery. intervention group but
mellitus, obesity not statistically
2
(BMI>25kg/m , significant
active smoker, Total ~1000ml vs. 800ml;
peripheral vascular P=0.14
2017 American Medical Association. All rights reserved. 250
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
disease and heart Reoperations:
failure according to Surgical revision:
NYHA III-IV. Intervention: 1/22 (4.5%)
Exclusion Criteria: Control: 3/22 (13.6%)
Emergency Calculated and
operations, active microbiologically
endocarditis, lung specific antimicrobial
infections or drug therapy was
pneumonia, i.v. drug applied in all 4 cases.
abuse, HIV or Vacuum assisted closure
thrombopenia. therapy was utilized to
heal vein harvesting
site was used in 2
patients in each group
(9.1%)
Length of stay:
ICU stay slightly shorter in
intervention group:
48.644.4 h vs. 51.3
53.3h; p=0.67
Mortality: NR
Adverse events:
One patient in each group
(4.5%) underwent re-
intubation due to
cardiopulmonary failure.
NOTE: Lowest rectal
temperature showed
hypothermia in both
groups but they do not
specify when this was
recorded or if it was
corrected
34.2 C1.4 vs.
34.4 C1.4; p=0.5
2017 American Medical Association. All rights reserved. 251
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Peerbo- RCT To investigate Number of patients: Intervention group: n=32 SSI: (follow up 3 Definitions:
oms 1, 3, 4, whether the N=102 but complete The wound was dried and months) SSI: a wound score
65
2009 5, 6, 7, application of data were recorded subcutaneous tissues Superficial wound infection form was used for
(ES) 8, 9 a platelet for 73 patients. were sprayed with at 2 weeks scoring wound
concentrate Denominators in approximately 6mL of Intervention: 1/32 healing: where 0 =
(in spray form) results vary. Platelet-Rich Plasma (2.8%) dry wound with no
might improve Patient (PRP) at a distance of Control: 1/41 (2.2%) signs of infection
the repair of Characteristics: 10-15 cm with the knee Both were successfully and 100=wound
wounds after Baseline patient flexed at 90 degrees treated with antibiotics. leakage with signs
primary characteristics were which exposes the knee of infection. Wound
unilateral total similar between cavity. After closure of Total wound closure scoring was
knee groups. the joint capsule, with Third day postop conducted by a
arthroplasty Both groups had the platelet poor plasma Intervention: 7/32 blinded trained
(TKA) with a normal wound (PPP) fraction (approx. (21.8%) orthopedics
primary focus healing. Missing 10mL) and the skin was Control: 6/41 (14.6%) resident
on wound data was analyzed closed with staples. 95% CI: 7% (-11% to Wound Closure:
healing and a to compare per Timing of intervention: 25%) P=0.5 wound score 0:
secondary protocol and ITT Intraoperatively Fourth day postop no leakage or
focus on knee populations and no Duration of intervention: Intervention: 7/32 signs of infection
function, use differences were Intraoperatively (21.8%) Wound leakage:
of analgesics, found (duration of spray time). Control: 13/41 (31.7%) scores>0
and Age, y: mean(SD) Device/agent: Autologous 95% CI: -9% (-30% to WOMAC Score
hemoglobin Intervention: 77 (4.4) platelet gel (APG) 10%) P=0.4 utilized to
values. Control: 78 (5.1) prepared using a max Two weeks postop determine pain,
Gender: male of 16ml whole blood Intervention: 4/36 stiffness and
Intervention: 13 collected through an (11.1%) physical function
(26%) existing line and anti- Control: 16/46 (34.9%) Perioperative
Control: 11 (21%) coagulated with citrate 95% CI: -24% (-41% to care:
Obesity (exclusion dextrose solution. Per 17%) P=0.02 Knee incision was
criteria) patient a maximum of dressed
Height, cm: mean(SD) 9-30ml of platelet-rich Other infections: NR postoperatively
Intervention: 168 (9.1) plasma was produced. Topic-specific wit compression
Control: 168 (8.1) outcomes: Using bandages and
Weight, kg: mean(SD) Monitoring intervention: N=102, Drop in rehabilitation
Intervention: 83 (16) NR hemoglobin, pain at was started on
Control: 79 (12) Control group: n-41 rest, pain during the day after
Comorbidities: NR Received no spraying with walking, use of pain surgery using
(exclusion criteria) PRP or PPP medication, WOMAC crutches
Procedures: Primary Standard preventive score, and Range of according to the
2017 American Medical Association. All rights reserved. 252
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
unilateral total knee measures: motion were not Joint Care
arthroplasty. (TKA) Surgical procedure: all statistically significantly Program
Indications: procedures took place different between (created by the
Osteoarthritis of the in a training hospital control and intervention. medical
knee. using the same surgical Reoperations: NR instrumentation
Setting: 1 training procedure performed by Length of stay: NR company who
hospital an orthopedic Mortality: NR sponsored this
Location: The consultant or a Adverse events: NR study).
Netherlands supervised senior Other notes: Due
Dates: June 2005 orthopedic resident. to a partial
March 2007 Surgical Approach: The reorganization of
Inclusion Criteria: No medial parapatellar the ward, no or
age limit for inclusion approach was used, partial
but the criteria for averting the patella measurements
participation laterally. were recorded
included pain and Tourniquet: was used and for a number of
radiographic knee after implantation, the the study
osteoarthritis. tourniquet was deflated patients. Missing
Exclusion Criteria: and primary hemostasis data were
Platelet count was achieved. attributed to the
150x10 /L,
9
Prosthesis: A cemented last known
hemoglobin level posterior cruciate result carried
6.5mmol/L, retaining prosthesis forward
BMI>33kg/m2, and was used in all cases. principle. This
systemic disorders Irrigation: before closure of resulted in a loss
such as diabetes, the wound layers, the of power for the
rheumatoid arthritis, soft tissues and knee study.
and hepatitis. joint were rinsed with Follow-up: Wound
saline solution to and function
remove all debris scores were
Drains: Deep or measured at
subcutaneous drains days 3-5, and at
were not used. regular control
Analgesic: paracetamol every 2 weeks.
(3g daily) and Functional
diclofenac (50mg 3 scores were also
times daily) with measured at 6
pantaprazol (40mg and 12 weeks
daily) for protection postoperatively.
2017 American Medical Association. All rights reserved. 253
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
against ulcers. Funding Source
Anticoagulant: Conflicts:
subcutaneous injection Authors: NR
of 0.3mL low-molecular- Institution: NR
weight-heparin daily Study: Industry
before the operation Supplies: NR
and continued until a
sufficient effect of oral
anticoagulants
(acenocoumarol) was
achieved.
Non-standard preventive
measures:
Anticoagulant: oral
anticoagulants were
used up to 12 weeks
postoperatively.
Neri RCT To evaluate Number of patients: Intervention group: n=24 All data presented in bar Definitions: NR
62
2008 1, 7, 8, the use of N=48 12 hr. Preop: graph rather than Parameters
(ES) 9 topical Patient Disinfection of the numerical form. evaluated:
prophylactic Characteristics: umbilical and SSI: (follow up 60 days) Umbilical region
antimicrobial Age, y: mean (range): periumbilical skin with Topical administration of pain (pain scale 0-
(i.e., rifamycin) 38 (21-64) iodopovidone rifamycin reduced the 5)
for prevention Gender m:f: 418:30 Application of a sterile incidence of omphalitis Analgesic drug
of post- video Obesity: NR medication with 3ml of (statistically significant) administration for
laparoscopic Comorbidities: NR rifamycin (250mg) on the Mean values of local signs localized umbilical
cholecystecto Procedures: Video- umbilicus of inflammation was region pain
my (VLC) at laparoscopic Intraop: statistically significantly Signs of
the umbilical cholecystectomy Suture of the umbilical higher in the control inflammation
port-site. (VLC) access: muscular fascia versus the intervention (rubor, calor,
Indications: and of the skin wound group (P<0.001) tumor) of the
uncomplicated with polyglycolic sutures Occurrence of umbilical umbilical wound
cholelithiasis Disinfection of the wound leakage was (on a scale of 1-5)
Setting: 1 university umbilical wound and peri- statistically significantly including wound
hospital. umbilical skin with lower at 12, 24, 36, and warmness,
Location: USA iodopovidone first then 48, and day 3, 4, 5, 6 hyperemia,
Dates: September with 0.9% saline solution. and 7 in the intervention umbilical wound
2006 April 2007 Application of a sterile versus control group swelling and
Inclusion Criteria: medication with 3mL of (p<0.005) redness
2017 American Medical Association. All rights reserved. 254
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Patients with rifamycin (250mg) on the Dehiscence of umbilical Purulent leakage
uncomplicated umbilical wound. wound sutures occurred through the
cholelithiasis Postoperative. in fewer patients in the umbilical wound.
undergoing At 12, 24, 36, 48 & 72 h intervention versus Dehiscence of the
uncomplicated post-VLC, rifamycin was control groups at 12, umbilical skin
video-laparoscopic applied in a sterile fashion 24, 36, and 48, and day sutures.
cholecystectomy to the umbilical wound of 3, 4, 5, 6 and 7 Incisional hernia
(VLC) all the patients. (p<0.001) in umbilical region
Exclusion Criteria: at postoperative
Acute cholecystitis Timing of intervention: Other infections: NR day #60
with localized Pre, intra and Topic-specific
peritonitis; umbilical postoperative outcomes: Perioperative
hernia; Duration of intervention: Pain- postoperative care: NR
immunodepressed from 12hours prior to observation of pain Other notes: none
patients; VLC to 72 hours localized in umbilical Follow-up: Clinical
uncompensated postoperatively. region in patients in data were
diabetes; perforation Device/agent: Topical both groups statistically registered at 12,
of the gallbladder in rifamycin less in intervention 24, 36 and 48h
the peritoneal cavity Monitoring intervention: group (P<0.001) after VLC and
during VLC; and rd th
NR on the 3 , 4 ,
perforation of the Number of patients th th
Control group: n=24 6 , and 7 post-
gallbladder during 12 hr. Preop: requiring additional VLC day. For
removal through the Disinfection of the analgesics (yes/no) patients
umbilicus with bile umbilical and presented in bar graph dismissed before
leakage. form but shows fewer rd
periumbilical skin with 3 postoperative
iodopovidone patients in intervention day, there was
Intraop: than control requiring an ambulatory
Suture of the umbilical additional analgesics at outpatient
access: muscular fascia hour 12, 24, 36, and 48, control on the
and day 3, 4, 5,and 6 th
and of the skin wound 60 day post-
with polyglycolic sutures P<0.005 VLC, the
Disinfection of the Reoperations: NR possible
umbilical wound and peri- Length of stay: Mean presence of
umbilical skin with (range) incisional hernia
iodopovidone first then Intervention: 3 (1-8) days in the umbilical
with 0.9% saline solution. Control: 4 (3-8) days. region was
Mortality: NR registered.
Standard preventive Adverse events: Funding Source
measures: Conflicts:
2017 American Medical Association. All rights reserved. 255
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Laparoscopic technique: Authors: NR
Hasson open technique Institution: NR
AMP: IV administration of Study: NR
2g ceftriaxone, followed Supplies: NR
by a second
intraoperative dose and
a final dose after 24
hours.
Kamath RCT To study the Number of patients: Intervention group: n= SSI: (follow up 30 days) Definitions:
61
2005 1, 4, 6, role of the N=92 47 Superficial Infection: Surgical site
(ES) 7, 8, 9 topical Patient Topical chloramphenicol Intervention: 4/47 (8.5%) surveillance was
antimicrobial Characteristics: ointment was applied to Control: 8/45 (17.8%) based on the
chloramphenic Age, y: mean 78.6 (44- the surgical site at the Positive wound swabs in 5 guidelines
ol in reducing 101) end of procedure and of 8 in control group: 1 issued by the
rd
the incidence Gender: m:f = 28:72 3 day postoperatively Pseudomonas, 2 Scottish Centre
of superficial Obesity NR and wound dressed MRSA, and 2 MSSA. for Infection and
surgical site Comorbidities: with low adherence None in the intervention Environmental
infection Rheumatoid arthritis:4 dressing (rayon group had positive Health (SCIEH)
following Diabetes: 9 absorbent pad with wound swabs. Superficial SSI
surgery for hip Cardiac, respiratory, adhesive border) 1. infection occurs
fractures. renal or other Timing of intervention: Univariate estimated w/in 30 days
systemic pathology: Intra and relative risk (95% CI) of after operation
91 postoperatively infection 2. and involves only
Smoking history Duration of intervention: Smoking (no infected (%)) skin and
(current or past): intra and Current: 8/31 (25.8%) subcutaneous
100% postoperatively Former/never: 4/61 tissue of incision
Preop hospitalization: Device/agent: (6.6%) 3. Patient has at
average 1.7 days (1- Chloramphenicol RR: 4.957 (1.359-18.084) least one of the
8) Monitoring intervention: Gender (no infected (%)) following
Procedures: NR Male: 5/25 (20%) purulent discharge
Hemiarthroplasty Control group: n=45 Female: 7/67 (10.4%) form the
(uncemented No antimicrobial ointment RR: 2.143 (0.611-7.512) superficial
prosthesis) 54/92 administered. Wound Age (no infected (%)) incision
(58.7%) dressed with low >71 years: 10/70 organisms isolated
Internal fixation of the adherence dressing (14.3%) form an
fracture with (rayon absorbent pad >70 years: 2/22 (9.1%) aseptically
dynamic hip screw: with adhesive border) RR: 1.667(0.335-8.259) obtained culture
2017 American Medical Association. All rights reserved. 256
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
46/92 (23.9%) Standard preventive Treatment (no infected of fluid or tissue
Indications: fracture of measures: (%)) form the
the neck of femur AMP: intravenous Intervention: 4/47 (8.5%) superficial
Intracapsular fracture: cefuroxime Control: 8/45 (17.8%) incision
54/92 (58.7%) Anticoagulant: RR: 0.430 (0.120-1.544) at least one of the
Extra capsular fracture: postoperative following signs
46/92 (23.9%) subcutaneous injection Multivariate estimated or symptoms of
Setting: 1 hospital of enoxaparin for DVT relative risk (95% CI) of infection: pain or
Location: Scotland prophylaxis infection tenderness,
Dates: April 2002 Non-standard preventive Current Smoker: localized
March 2003 measures: ARR: 7.29 (1.62-32.67); swelling,
Inclusion Criteria: Closure: P=0.009 redness or heat
Patients who could Clips: 97/100 (97%) Male Gender and superficial
give informed (removed 12 days ARR: 0.92 (0.19-4.31); incision, is
consent and who postop) P=0.912 deliberately
were admitted with Subcuticular stitches: Age<70 years opened by
fracture neck of 2/100 (2%) ARR: 0.30 (0.05-1.96) surgeon unless
femur. Interrupted nylon: 1/100 P=0.209 incision is
Exclusion Criteria: (1%) IC Fracture: culture negative.
Pathological Grade of surgeon: ARR: 0. 52 (0.06-1.13); Diagnosis of SSI
fractures and Middle grades: 82/100 P=0.072 by physician.
undisplaced (82%) Treatment: Intervention: The following are
intracapsular neck of Senior house officers ARR: 0.36 (0.08-1.56); NOT SSI
femur fractures under senior P=0.172 1. Stitch abscess
needing internal supervision: 10/100 (minimal
fixation. (10%) Other infections: inflammation and
Consultant: 8/100 (8%) Chest infections: 7/92 discharge
(7.6%) confined to the
1/7: intervention and points of suture
also had wound penetration)
infection 2. Infected burn
1/7: control and also wound
had wound infection 3. incisional SSI
UTI: 5/92 (5.4%) that extends into
1/5: control and also had the fascial and
wound infection muscle layers
Topic-specific (Deep incisional
outcomes: SSI)
9 patients in the study had Perioperative
2017 American Medical Association. All rights reserved. 257
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
no associated illness care:
and none of these had Mobilization:
wound infections. according to
Reoperations: NR standard
Length of stay: average protocol.
inpatient stay: 18.5 (10- Other notes: None
90) days either in an Follow-up: The
orthopedic ward or wound was
rehabilitation ward checked on the
rd th th
following which patients 3 , 6 , 12 and
th
were either sent back to 30 day postop
their own home or care Funding Source
home as appropriate. Conflicts:
Mortality: 7 patients died Authors: NR
because of unrelated Institution: NR
causes during follow Study: NR
up. Supplies: NR
1/7 hemiarthroplasty had
malignancy confirmed
on histology &
excluded.
Adverse events:
1 Intervention and 2
control patients
wounds continued to
discharge through
sinuses for up to 3
months but all
eventually settled down
with oral antimicrobials
and dressings.
Seco RCT To compare Number of patients: Intervention group: SSI: (4-6 weeks by mail) Definitions:
59
1990 1, 2, 5, the results of N= 246 n=126 Total: Wound infection:
(ES) 6, 7, 8, systematic Patient Patients were treated with Intervention: 5/126 (4%) patients in whom
9 clindamycin , Characteristics: the 1g Ampicillin in 20ml Control: 15/120 (13%) pus appeared or
with our median age and sex Saline as topical P<0.02 if there was
without topical ratio were similar solution. Gauze was (only one infection serious
ampicillin to between groups impregnated with occurred post- discharge and a
determine if Age y: median (range) ampicillin solution. The discharge) positive culture
2017 American Medical Association. All rights reserved. 258
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
the Intervention: 29 (12- subcutaneous tissues Simple: Perioperative
combination of 93) were cleaned with this Intervention: 0/68 care:
the antibiotics Control: 29 (12-79) gauze and the Control: 1/68 (1%) Approach: 96%
is more Gender: male remaining solution was P=NS through a grid-
effective than Intervention: 83/126 allowed to rest in the Advanced: iron incision
the (66%) wound. Intervention: 5/58 (9%) Other notes:
clindamycin Control: 82/120 (68%) Timing of intervention: Control: 14/52 (27%) Follow-up: 7-10
alone is Obesity: NR intraoperatively P<0.02 days postop in
sufficient Comorbidities: NR Duration of intervention: Appendicitis with person. 4-6
NA Peritonitis with or weeks via mail.
Procedures: Device/agent: 1g abscess (only Funding Source
emergency ampicillin in 20mL percentages given. Conflicts:
appendectomy for saline Numerator and Authors: NR
acute appendicitis Monitoring intervention: denominator not Institution: NR
Indications: acute NA reported) Study: NR
appendicitis: Control group: n=120 Intervention: 13% Supplies: NR
Simple: Patients did not receive Control: 35%
Intervention: 68/126 topical ampicillin Other infections: NR
(54%) Standard preventive Topic-specific
Control: 68/120 (57%) measures: outcomes:
Gangrenous: AMP: 600mg clindamycin Intervention: 83/126
Intervention: 32/126 intramuscularly. (66%)
(25%) Skin prep: with povidone- Control: 82/120 (68%)
Control: 29/120 (24%) iodine. Reoperations:
Perforated: Retroperitoneal abscess
Intervention: 26/126 as cause (E. coli was
(21%) isolated)
Control: 23/120 (19%) Intervention: 0/126
Control: 1/120 (1%)
Setting: 1 Tertiary Length of stay: Median
hospital (range), days
Location: Spain Intervention: 7 (3-18)
Dates: 1 year, when Control: 7 (3-40)
NR. Mortality: NR
Inclusion Criteria: Adverse events:
Patients undergoing Fever
emergency Intervention: 3/126 (1%)
appendectomies for Control: 1/120 (1%)
acute appendicitis. Wound hematoma
2017 American Medical Association. All rights reserved. 259
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Exclusion Criteria: Intervention: 1/126 (1%)
Patients <12 years Control: 1/120 (1%)
old, those who Postoperative ileus
underwent elective Intervention: 0/126
surgeries, and those Control: 2/120 (1%)
who had previously Pulmonary embolism:
been treated with Intervention: 0/126
antibiotics Control: 1/120 (1%)
Acute respiratory
insufficient
Intervention: 1/126 (1%)
Control: 0/120
Unspecific diarrhea
Intervention: 1/126 (1%)
Control: 0/120
Raahave RCT To conduct a Number of patients: Intervention group: n= SSI: (follow up NR) Definitions:
60
1989 1, 5, 7, randomized N= 170 81 Intervention: 5/81 (6.2%) Wound infection: a
(ES) 8 controlled trial Patient Patients had 2g ampicillin Control: 6/89 (6.7%) collection of pus,
to investigate Characteristics: powder applied in the P>0.05 draining either
the effect of Age, y: median (range) wound subfacially and Other infections: NR spontaneously
ampicillin Intervention: 72 (32- subcutaneously during or at the site of
applied locally 90) closure. Topic-specific incision.
in combination Control: 69 (28-90) Timing of intervention: outcomes: Wound rupture
with a 12 hour Gender: male intraoperatively Wound dehiscence: recorded
parenteral Intervention: 39/81 Duration of intervention: Intervention: 2/81 (2.5%) separately
antibiotic (48.1%) NA Control: 1/89 (1.1%) Evidence of
regimen with Control: 46/89 Device/agent: Monitoring P>0.05 anastomotic
cefotaxime. (51.7%) intervention: NA Intra-abdominal abscess leakage: air or
Obesity: NR Control group: n= 89 Intervention: 3/81 (3.7%) feces or both
Comorbidities: NR Not described Control: 2/89 (2.2%) delivered by the
Standard preventive P>0.05 drains.
Procedures: Elective measures: Patients with anastomoses Perioperative
colorectal surgeries: Mechanical bowel prep: Intervention: 66 care: NR
Right transverse three day liquid diet Control: 71 Other notes: None
colonic resection: plus 250ml of a Anastomotic leakage Follow-up: NR
Intervention: 22/81 complete nutrient Intervention: 3/66 (4.5%) Funding Source
(27.8%) powder in 500ml of Control: 6/71 (8.5%) Conflicts:
Control: 22/89 water twice per day; P>0.05 Authors: NR
(24.7%) 30ml of 50% Reoperations: NR Institution: NR
2017 American Medical Association. All rights reserved. 260
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Left colonic & sigmoid magnesium sulfate Length of stay: NR Study: NR
resection: twice/ day Mortality: NR Supplies: NR
Intervention: 21/81 Anastomoses: done in two Adverse events: Patients
(25.9%) layers through and showed no allergic
Control: 23/89 through polyglycolic reactions to or other
(25.8%) acid and seroserous side effects from the
Low anterior resection: silk sutures. antibiotics used.
Intervention: 20/81 Low anterior resections:
(24.7%) stapling instrument was
Control: 21/89 often used instead of
(23.6%) sutures and an
Abdominoperineal extraperitoneal drain
excision: was inserted.
Intervention: 6/81 Closure: all abdominal
(7.4%) wounds were closed
Control: 12/89 with PGA sutures in the
(13.5%) peritoneum, fascia and
Laparotomy with subcutis; nylon sutures
colostomy: were used in the skin
Intervention: 4/81 AMP: 2g cefotaxime
(4.9%) intravenously at
Control: 5/89 (5.6%) induction of anesthesia.
Other: Dose was repeated at
Intervention: 4/81 6h and 12h postop.
(4.9%)
Control: 2/89 (2.2%)
Indications:
Adenocarcinoma:
Intervention: 70/81
(86.4%)
Control: 72/89
(80.9%)
Benign neoplasms:
Intervention: 4/81
(4.9%)
Control: 2/89 (2.2%)
Diverticulitis:
Intervention: 4/81
(4.9%)
2017 American Medical Association. All rights reserved. 261
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Control: 8/89 (9.0%)
Other:
Intervention: 3/81
(3.7%)
Control: 7/89 (7.9%)
Setting: 1 University
Hospital
Location: Denmark
Dates: NR
Inclusion Criteria:
Consecutive patients
scheduled for
elective colorectal
surgery.
Exclusion Criteria:
Patients who were
allergic to the
antibiotics used
patients under
antibiotic treatment
during the last three
preoperative days,
patients who did not
adhere to the
planned antibiotic
regimen and patients
whose colon was not
opened.
Vander RCT To test the Number of patients: Intervention group: n= SSI: (at 1 month) Definitions:
Salm 1 hypothesis N=417 223 Sternal/ mediastinal SSI not defined:
63
1989 that topical Patient Hemostatic paste mixed infection Sternal &
(ES) vancomycin Characteristics: with 250g powdered Intervention: 1/223 mediastinal
(to which S. Characteristics of vancomycin was (0.45%) necessitated a
non-aureus is patients were applied to sternum: At Control: 7/193 (3.6%) major
almost always indistinguishable end of operation before P=0.02 reoperation and
sensitive) between groups sternum closure, a both were
applied to the except for repeat hemostatic paste Other infections: NR counted as
cut sternal operations containing 1gm Topic-specific sternal
edges will Age, y: mean powdered absorbable outcomes: NR infections.
2017 American Medical Association. All rights reserved. 262
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
reduce the Intervention: 62.5 gelatin, and topical Superficial
incidence of Control: 62.0 thrombin was applied to S. aureus infections infections were
these Gender, male the cut edges of the Intervention: 1/223 counted as no
infections. Intervention: 154/223 sternum. (0.4%) sternal
(69%) Timing of intervention: Control: 2/193 (1.0%) infections
Control: 129/193 intraoperative Perioperative
(67%) Duration of intervention: S. non-aureus infections care: NR
Obesity: NR intraoperative Intervention: 0/223 Other notes: NR
Comorbidities Device/agent: hemostatic Control: 5/193 (2.6%) Follow-up: 1
Diabetes mellitus paste containing month
Intervention: 47/223 vancomycin powder Reoperations: Funding Source
(21%) Monitoring intervention: Length of stay: NR Conflicts:
Control: 37/193 (19%) NA Mortality: Authors: NR
Repeat operations Control group: n=193 Intervention: 15/223 Institution: NR
Intervention: 29/223 Hemostatic paste alone (6.7%) Study: NR
(13%) was applied to sternum: Control: 9/193 (4.6%) Supplies: NR
Control: 11/193 At end of operation P=NS
(5.7%) before sternum closure,
P=0.008 a hemostatic paste Adverse events:
Procedures: heart containing 1gm No complication resulted
operations powdered absorbable from the topical
performed via gelatin, and topical vancomycin
median sternotomy. thrombin was applied to
Indications: NR the cut edges of the
Setting: 1 university sternum.
medical center Standard preventive
Location: USA measures:
Dates: May 1986 July Hair removal: with an
1986 electric razor the day
Inclusion Criteria: all before the operation for
patients of 3 scheduled operations
surgeons who had AMP: cefazolin or
heart operations vancomycin in case of
performed via a penicillin allergy.
median sternotomy Preoperatively and for
during the study 36h postop.
dates (including
emergency
operations)
2017 American Medical Association. All rights reserved. 263
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Exclusion Criteria: NR
Juul RCT To evaluate Number of patients: Intervention group: SSI: (days) Definitions:
58
1985 1, 2, 3, the role of N= 203 n=105 Deep wound infection Deep Wound
(ES) 4, 5, 7, topical Patient Received subcutaneous Intervention: 5/105 infection:
8 ampicillin Characteristics: the and subfascial (4.8%) accumulation of
when systemic two groups were application of 1g of Control: 5/98 (5.1%) pus requiring
perioperative considered similar ampicillin in 10ml of P=NS surgical
antibiotic according to gender saline in each of the Other infections: NR drainage.
prophylaxis age, efficiency of surgical wounds. Topic-specific Wound dehiscence:
with ampicillin preoperative bowel Timing of intervention: outcomes: included
and prep, and type of intraoperatively Dehiscence subcutaneous
metronidazole surgery. Duration of intervention: Intervention: 7/105 as well as fascial
is used. Age, y: mean (range) NA (6.7%) breakdown but
Intervention: 69 (21- Device/agent: 1g Control: 4/98 (4.1%) not pus
96) ampicillin in 10ml saline P=NS accumulation.
Control: 69 (26-91) Monitoring intervention: Hernia Perioperative
Gender: male NA Intervention: 10/105 care:
Intervention: 56/105 Control group: n=98 (10.8%) Other notes:
(53.3%) Received no further Control: 3/98 (3.3%) Follow-up:
Control: 61/98 (62.2%) prophylactic antibiotic P=NS observed daily
Obesity: NR treatment. Unclear if until the
Comorbidities: NR wounds were irrigated Reoperations: cutaneous
Procedures: with saline. - 7 patients with sutures were
Abdominoperineal Standard preventive dehiscence were re- removed.
resection measures: operated upon because Funding Source
Intervention: 11/105 Mechanical bowel prep: of rupture of the fascia. Conflicts:
(10.5%) Either conventional or Not reported which Authors: NR
Control: 12/98 (12.3%) whole-gut irrigation group. Institution: NR
Low anterior resection Blind evaluation of - 6 patients had temporary Study: NR
Intervention: 21/105 bowel prep efficiency transverse colostomies Supplies: NR
2017 American Medical Association. All rights reserved. 264
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
(20%) was conducted during because of anastomotic
Control: 19/98 (19.4%) surgery breakdown after low
Colonic resection AMP: all received anterior resection. Not
Intervention: 44/105 ampicillin 1g 3x/day and reported which group.
(41.9%) metronidazole 0.5g Length of stay:
Control: 47/98 (48.0%) 3x/day intravenously Mortality:
Colostomy n1 from induction of 2 patients died from
Intervention: 15/105 anesthesia to 3 days cardiopulmonary
(14.3%) postoperatively. complications in the first
Control: 7/98 (7.1%) Closure: abdominal and postoperative week.
Closure of colostomy perineal wounds were Not reported which
n1 closed primarily with group.
Intervention: 11/105 absorbable sutures in Adverse events:
(10.5%) peritoneum and fascia, No hypersensitivity
Control: 7/98 (7.1%) Drains: retroperitoneal reactions or other side
Other drainage was used after effects were
Intervention: 3/105 low anterior resection encountered from
(2.9%) and abdominoperineal treatment with
Control: 6/98 (6.1%) excision of the rectum. antibiotics.
Indications:
Colorectal cancer
Intervention: 80/105
(76.2%)
Control: 89/98 (90.8%)
Diverticulitis
Intervention: 11/105
(10.5%)
Control: 8/98 (8.2%)
Inflammatory bowel
disease
Intervention: 7/105
(6.7%)
Control: 2/98 (2.0%)
Other
Intervention: 7/105
(6.7%)
Control: 3/98 (3.1%)
**NOTE other
includes previously
2017 American Medical Association. All rights reserved. 265
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
known infections
including one case
of Fourniers
gangrene which
resulted in a deep
wound infection.
Setting: 1 University
Hospital
Location: Denmark
Dates: April 1982
September 1983
Inclusion Criteria:
Patients undergoing
elective colonic and
rectal surgery.
Exclusion Criteria:
Patients receiving
antibiotics in the
preoperative period
or those with a
history of
hypersensitivity to
ampicillin or
metronidazole
2017 American Medical Association. All rights reserved. 266
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
eTABLE 33. Evidence Table for Q2C. How safe and effective are antimicrobial-coated sutures; when and how should they be
used?
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Diener RCT To yield Number of patients: Intervention group: SSI: Definitions:
77,82
2014 1, 2, 4, reliable data N=1185 n=587 Composite SSI within 30 Superficial & deep
(ES) 5, 6, 7, for the Patient Closure of the abdominal days SSI: CDC:
8, 9 effectiveness Characteristics: the fascia after midline Intervention: 87/587 Superficial SSI:
of triclosan study was balanced laparotomy with (14.8%) within 30 days
coated in terms of patient triclosan-coated Control: 96/598 (16.1%) postop and
polydioxanone and operation polydioxanone sutures. OR: 0.91 (0.66-1.25) involved only
sutures for characteristics Timing of intervention: P=0.64 skin or
abdominal Age, y: mean (SD) intraoperative Multiple imputations of the subcutaneous
fascia closure Intervention: 64.7 Duration of intervention: missing data yielded in tissue around
in the (11.8) closure until absorption a similar result (p=0.62) the incision plus
prevention of Control: 65.0 (12.1) Device/agent: triclosan- Superficial at least one of
surgical site Gender: female, coated or uncoated Intervention: 53/587 the following:
infections, Intervention: 226/587 polydioxanone sutures. (9.2%) purulent
compared with (38.5%) Monitoring intervention: Control: 56/598 (9.4%) drainage from
non-coated Control: 230/598 assessed in person and Deep the incision site;
polydioxanone (38.5%) validated via Intervention: 22/587 organisms
2
sutures. The Obesity, BMI (mg/kg ): assessment of (3.7%) isolated by
null mean (SD) photographs of Control: 25/598 (4.2%) culture from the
hypothesis to Intervention: 26.1 (4.3) abdominal wound by an Missing incision; pain or
be tested Control: 26.1 (4.6) independent primary Intervention: 12/587 tenderness,
states that the Comorbidities: outcome validation (2.0%) localized
rate of Diabetes mellitus: committee consisting of Control: 15/598 (2.5%) swelling,
superficial and Intervention: 81/587 3 board-certified redness, or heat
deep (13.8%) surgeons who reviewed SSI By Surgery and the incision
incisional Control: 96/598 all photographs blinded Colorectal: N=690 is opened
surgical site (16.1%) to group. Intervention: 62/344 deliberately by a
infections COPD Control group: n=598 (18.0%) surgeon unless
within 30 days Intervention: 38/587 Closure of the abdominal Control: 60/346 (17.3%) the culture is
after midline (6.5%) fascia after midline P=0.81 negative; or
incision is Control: 51/598 (8.5%) laparotomy with Hepatiopancreato-biliary: diagnosis of
equal in both Malignant disease uncoated N=74 superficial
treatment Intervention: 407/587 polydioxanone sutures. Intervention: 4/34 surgical site
groups. (69.3%) (11.8%) infection by a
Control: 442/598 Standard preventive Control: 3/40 (7.5%) surgeon or
(73.9%) measures: P=0.53 attending
Anemia Closure: achieved by Upper-gastrointestinal physician.
2017 American Medical Association. All rights reserved. 267
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Intervention: 167/587 continuous mass tract: N=140 Deep SSI: occurred
(28.4%) closure with use of two Intervention: 5/67 (7.5%) within 30 days
Control: 166/598 loops one from the Control: 15/73 (20.5%) postop, were
(27.8%) cranial and the caudal P=0.03 related to the
Chronic Renal end of the incision in a procedure, and
insufficiency continuous suture involved deep
Intervention: 23/587 technique Factors associated with soft tissues,
(3.9%) Skin closure staples. SSI within 30 days OR such as the
Control: 20/598 (3.3%) Drains no drains (95%CI); p fascia, and
allowed. BMI: 1.09 (1.05-1.14); muscles, plus at
Surgeon Experience: Antibiotic prophylaxis P<0.0001 least one of the
No certificate patients had to receive following:
Intervention: 58/587 antibiotic prophylaxis Chronic renal insufficiency: purulent
(9.9%) before the incision. 2.96 (13.6-6.46); p=0.0064 drainage form
Control: 75/598 the incision but
(12.5%) Anemia: 1.73 (1.16-2.59); not from the
p=0.0071 organ or space
Wound Status of the surgical
Clean No Antibiotic prophylaxis site; dehiscence
Intervention: 144/587 5.19 (1.56-17.1); 0.0074 of a deep
(24.5%) incision or a
Control: 138/598 Malignant disease: deep incision is
(23.1%) 0.060 (0.38-0.93); 0.0236 opened by a
Clean-contaminated surgeon
Intervention: 430/587 Combination of target because of pain,
(73.3%) organ (vs. other) fever or
Control: 450/598 colon, rectum, liver, tenderness;
(75.3%) pancreas, & stomach. abscess or other
Contaminated 6.37 (2.71-14.98), 0.0193 evidence of
Intervention: 11/587 infection at the
(1.9%) Surgeons expertise incision site or
Control: 9/598 (1.5%) 1.73 (1.02-2.93); p=0.0405 diagnosis of
Dirty deep surgical
Intervention: 2/587 Other infections: NR site infection by
(0.3%) Topic-specific a surgeon or
Control: 1/598 (0.2%) outcomes: attending
Wound dehiscence physician.
Duration of surgery, Intervention: 66 (13.4%)
min (SD) Control: 81 (16.3%) Perioperative
2017 American Medical Association. All rights reserved. 268
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Intervention: 179.3 OR: 0.80 (0.56-1.14) care: NR
(87.1) P=0.21 Other notes:
Control: 185 (90.9) Missing Wounds were
Intervention: 96 (13.4%) inspected at
Blood loss ml, Control: 81 (16.3%) postop days 10
mean(SD) & 30
Intervention: 478.9 Burst abdomen Follow-up:
(639.6) Intervention: 9/587 30 days postop
Control: 503.0 (666.7) (1.9%) Funding Source
Control: 22/598 (4.5%) Conflicts:
Antibiotic Prophylaxis OR: 0.40 (0.18-0.88) Authors: NR
Intervention: 578/587 P=0.0194 Institution: NR
(98.5%) Missing Study: Industry
Control: 586/598 Intervention: 104/587 Supplies: NR
(98.0%) (17.6%)
Antibiotic Therapy Control: 109/598
Intervention: 126/587 (18.2%)
(21.5%)
Control: 112/598 Reoperations: NR
(18.7%) Length of stay:
Postop hospital stay, days,
Procedures: mean (SD)
Abdominal midline Intervention: 13.0 (7.4)
laparotomy. Control: 12.5 (6.3)
Resection & MD: 0.47 (-0.32-1.25)
anastomosis P=0.99
Intervention: 422/587
(71.9%) ICU Stay, days, mean
Control: 442/598 (SD)
(73.9%) Intervention: 2.3 (3.8)
Resection & resection + Control: 2.3 (3.6)
exploration MD: 0.01 (-0.41 0.43)
Intervention: 72/587 P=0.54
(12.3%)
Control: 63/598 Mortality:
(10.5%) Intervention: 9/587
Exploration (1.5%)
Intervention: 12/587 Control: 20/598 (3.3%)
(2.0%) OR: 0.46 (0.21-1.01)
2017 American Medical Association. All rights reserved. 269
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Control: 14/598 (2.3%) P=0.48
Resection or All deaths classified as
anastomosis & other unrelated to
Intervention: 5/587 intervention and most
(0.9%) were due to septic
Control: 3/598 (0.5%) shock, multiple organ
Resection & other failure or cardiac and
Intervention: 0/587 pulmonary
Control: 3/598 (0.5%) decompensation.
Exploration & other Adverse events:
Intervention: 2/587 Wound dehiscence
(0.3%) Intervention: 66/587
Control: 2/598 (0.3%) (13.4%)
Resection & resection Control: 81/598 (16.3%)
or anastomosis OR: 0.80 (0.56-1.14)
Intervention: 0/587 P=0.21
Control: 1/598 (0.2%) Missing
Intervention: 96/587
Indications: (13.4%)
Target Organ for Control: 81/598 (16.3%)
surgery
Colon Burst abdomen
Intervention: 189/587 Intervention: 9/587
(32.2%) (1.9%)
Control: 214/598 Control: 22/598 (4.5%)
(35.8%) OR: 0.40 (0.18-0.88)
Rectum P=0.0194
Intervention: 145/587 Missing
(24.7%) Intervention: 104/587
Control: 117/598 (17.6%)
(19.6%) Control: 109/598
Stomach (18.2%)
Intervention: 67/587 Serious Adverse Events
(11.4%) Unrelated to intervention:
Control: 73/598 130/146 (86.1%) vs.
(12.2%) 137/138 (87.3%)
Pancreas Possibly related to
Intervention: 32/587 intervention:
(5.5%) 21/146 (13/9%) vs. 17/138
2017 American Medical Association. All rights reserved. 270
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Control: 37/598 (6.2%) (87.3%)
Liver Probably related to
Intervention: 2/587 intervention:
(0.3%) 0/146 vs. 2/138 (1.3%)
Control: 3/598 (0.5%) Not Assessable:
Combination of the 0/146 vs. 1/138 (0.6%)
above Missing: 0/146 vs. 1/138
Intervention: 33/587 (0.6%)
(5.6%) Surgical site infection: 7
Control: 37/598 (6.2%) (46%) vs. 10 (63%)
Other Burst abdomen 8 (53%)
Intervention: 119/587 vs. 10 (63%)
(20.3%) Anastomotic insufficiency:
Control: 117/598 39 (258%) vs. 34
(19.6%) (215%)
Intra-abdominal fluid
Setting: Multi-center collection or abscess:
(24 secondary and 14 (93%) vs. 7 (44%)
tertiary care centers) Bleeding: 12 (79%) vs. 14
Location: Germany (89%)
Dates: April 7, 2010 (as Cardiovascular: 9 (60%)
single center trial) vs. 14 (89%)
and Jan 24, 2011 as Pulmonary: 15 (99%) vs.
multicenter trial. 13 (82%)
Both ended October Renal 7 (46%) vs. 8
19, 2012 (51%)
Inclusion Criteria: Other gastrointestinal
Adults (18 years) problems: 21 (139%)
who underwent vs. 24 (152%)
midline abdominal Other: 15 (99%) vs. 21
laparotomy for any (133%)
reason. Not assessable: 4 (26%)
Exclusion Criteria: vs. 3 (19%)
Impaired mental
state or language
problems or if they
were participating in
another intervention
trial that interfered
2017 American Medical Association. All rights reserved. 271
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
with the intervention
or outcome of this
trial.
Thimour- RCT To test the Number of patients: Intervention group: n= SSI: Definitions:
Bergstr- 1, 2, 3, hypothesis N=374 184 CDC Criteria SSI: CDC
om 4, 5, 6, that wound Patient Wound closed Intervention: 23/184 Superficial SSI
73
2013 7, 8 closure with Characteristics: subcutaneously with (12.5%) must have at
(ES) sutures coated baseline patient triclosan coated Control: 38/190 (20.0%) least one of the
with triclosan characteristics not monofilament P=0.0516 (by Fishers following
would reduce significantly different polyglactin suture and exact test) features: (i)
P=0.497 (by test)
2
SSI after open between groups intracutaneously with a purulent
vein Age, y: mean SD 4.0 triclosan coated RR: 0.63 (0.39-1.00) drainage; (ii)
harvesting. Intervention: 67.68.3 monofilament Culture Proven positive culture,
Control: 66.98.1 polyglecaprone suture. Intervention: 14/184 (iii) pain,
P=0.45 Timing of intervention: (7.6%) tenderness,
Gender: Female intraoperative Control: 23/190 (12.1%) swelling,
Intervention: 39/184 Duration of intervention: P=0.15 redness and
(21.1%) closure until absorption Antibiotic Treated deliberately
Control: 31/190 Device/agent: triclosan Intervention: 20/184 opened incision
(16.3%) coated or conventional (10.9%) by surgeon and
P=0.23 monofilament Control: 35/190 (18.4%) culture proven or
P=0.039 (by test)
2 2
Obesity: BMI, kg/m : polyglactin suture and not cultured, and
MeanSD 4.0 triclosan coated or P=0.042 (by Fishers (iv) infection
Intervention: 27.64.1 conventional exact test) diagnosis by
Control: 27.64.1 monofilament physician.
P=0.67 polyglecaprone suture. Leg SSI and Deep SSI: had to
Comorbidities: Monitoring intervention: Demographics involve fascia or
Diabetes: trained nurse BMI muscle layers
Insulin treatment: Control group: n=190 SSI: 28.34.3 Secondary
Intervention: 22/184 Wound closed No SSI: 27.43.8 endpoints:
(11.9%) subcutaneously with P=0.081 (i) purulent
Control: 21/190 conventional Diabetes Insulin drainage;
2017 American Medical Association. All rights reserved. 272
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
(11.1%) monofilament treatment (ii) antibiotic-treated
P=0.78 polyglactin suture and Intervention: 12/61 SSI according to
Oral Treatment: intracutaneously with a (19.7%) CDCs definition
Intervention: 20/184 4.0 conventional Control: 31/313 (9.9%) within 60 days
(10.8%) monofilament P=0.029 postop.
Control: 22/190 polyglecaprone suture. (iii) ASEPSIS score
(11.6%) Operative Characteristics at Days 30 & 60
P=0.83 Standard preventive and Infections postop
Dietary Treatment measures: Number of bypasses (iv) non-infectious
Intervention: 4/184 Surgical technique: all SSI: 3.41.0 leg-wound
(2.2%) patients were No SSI: 3.11.0 dehiscence
Control: 7/190 (3.7%) performed P=0.014 within 60 days
P=0.38 Cardiopulmonary postop
Smoking bypass Other infections: NR Perioperative
On-going Normothermia: was Topic-specific care: NR
o
Intervention: 29/184 maintained (35-36 C) outcomes: Other notes:
(15.8%) Transfusion: cold Noninfectious dehiscence Study power:
Control: 31/190 intermittent blood Intervention: 11/161 Based on a 20%
(16.3%) cardioplegia. (6.8%) infection rate
P=0.88 Antibiotic prophylaxis: all Control: 13/152 (8.5%) found by a pilot
Number of bypasses patients received 4 P=0.57 study, an 80%
Intervention: 3.00.9 parenteral doses of ASEPSIS score, day 4 power and a p-
Control: 3.21.0 cloxacillin 2g. First Mean and SD value of 0.05
P=0.008 administered 20min Intervention: 0.41.2 showed 180
prior to skin incision, Control: 0.30.8 patients were
Procedures: second 2h after first P=0.44 needed in each
CABG does and following Median and range group to show a
Intervention: 164/184 doses 6h & 24h later. Intervention: 0 (0-12) 50% reduction in
(89.1%) Patients with allergy to Control: 0 (0-5) SSI
Control: 167/190 cloxacillin received P=0.78 Wounds inspected
(87.9%) clindamycin. ASEPSIS score, day 30 at postop days 4
P=0.71 Closure: leg incision Mean and SD & 30 by trained
CABG+ AVR closed with one Intervention: 3.07.6 research nurse
Intervention: 17/184 subcutaneous Control: 4.79.4 and at 60 days
(9.2%) continuous suture and P=0.070 postop, patients
Control: 22/190 one continuous Median and range interviewed by
(11.6%) intracutaneous suture. Intervention: 0 (0-45) telephone.
P=0.46 Covered with drape, Control: 0 (0-43) Follow-up:
CABG+mitral repair compresses and elastic P=0.20 60 days postop
2017 American Medical Association. All rights reserved. 273
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Intervention: 3/184 bandages. Drape ASEPSIS score, day 60 Funding Source
(1.6%) removed on Postop Mean and SD Conflicts:
Control: 1/190 (0.5%) Day 4. Intervention: 3.78.7 Authors: None
P=0.30 Control: 5.410.0 Institution: NR
Indications: NR P=0.097 Study: Industry
Setting: 1 university Median and range Supplies: NR
hospital Intervention: 0 (0-45)
Location: Sweden Control: 0 (0-43)
Dates: March 2009 P=0.46
February 2012
Inclusion Criteria: Operation Time, min: Leg
Patients planned for vein harvesting
Coronary Artery Intervention: 6132
Bypass Graft, Control: 4819
CABG+Aortic Valve P<0.001 (This
replacement (AVR) significance remained
or CABG+mitral after adjusting for
valve repair or operating surgeon level
replacement of experience
Exclusion Criteria: Cultures taken: No
ongoing sepsis or resistant bacteria
septicemia, ongoing reported Staphyloccous
bacterial infections aureus:
or antibiotic Intervention: 7/23 (44)
treatment, Control: 15/38 (52)
participation in other p=0.61
clinical studies, or Reoperations: NR
other severe disease Length of stay: NR
that might influence Mortality: considered lost
wound healing, to follow up
emergency surgery Intervention: 1/184 (0.5%)
or known allergy to Control: 1/190 (0.5%)
triclosan. Adverse events:
Postoperative bleeding
(ml/12h)
Intervention: 470 (95-
1950)
Control: 482 (110-4550)
P=0.94
2017 American Medical Association. All rights reserved. 274
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Postoperative Bleeding
SSI: 430 (95-1485)
No SSI: : 500 (140-4550)
P=0.050
Justinger RCT To investigate Number of patients: Intervention group: SSI Definitions:
75
2013 1, 3, 4, the effect of N=856 n=485 Total: SSI- CDC NHSN
(ES) 5, 6, 7, impregnating, Patient Abdominal fascia closed Intervention: 31/485 definitions used:
8 with triclosan, Characteristics with triclosan-impregnated (6.4%) Wound infection
polydioxanone Age, y: meanSD, polydioxanone loop. Control: 42/371 (11.3%) was identified by
sutures used Intervention: 6313 OR: 0.501 (0.3-0.9) the presence of
for abdominal Control: 6313 Timing of intervention: P<0.05 erythema,
wall closure P=0.923 intraoperative induration, pain
on the rate of Gender: M:F Duration of intervention: SSI by Wound and discharge of
SSI Intervention:301:184 closure until absorption Classification: P<0.05 serous or
Control: 224:147 Device/agent: Clean: contaminated
Obesity: BMI>30 polydioxanone sutures Intervention: 14/286 fluid.
Intervention: 76/485 either conventional or (4.8%) Perioperative
(16.4%) triclosan coated. Control: 22/245 (8.9%) care: A
Control: 54/371 Monitoring intervention: Clean-Contaminated: standardized
(15.8%) postop wounds were Intervention: 14/162 clinical pathway
P=0.713 assessed daily by 2 (8.6%) was used
Comorbidities blinded observers. Control: 16/97 (16.5%) Other notes:
Diabetes mellitus Control group: n=371 Contaminated: Sample size: An
Intervention: 49/485 Abdominal fascia closed Intervention: 3/37 (8.1%) assumed SSI
(10.1%) with conventional Control: 4/25 (16%) reduction from
Control: 35/371 (9.4%) polydioxanone loop. Septic 12% to 6%
P=0.4.19 Standard preventive Intervention: 0/0 resulted in a
measures: Control: 0/4 calculated
Procedures: MRSA- patients with sample size of
Wound classification: previous methicillin- 350 patients for
p<.05 resistant SSI by Surgery each arm to
Clean: Staphylococcus aureus Upper GI Tract achieve a power
Intervention: 286/485 contamination of Intervention: 3/59 (5%) of 1-b=0.08 for
the one-sided
2
(59%) patients at risk for Control: 2/41 (5%)
Control: 245/371 MRSA contamination Hepatopancreatobiliary test at a level
(66%) were screened Intervention: 9/201 (4%) a=0.025 and a
Clean contaminated preoperatively and Control: 14/173 (8%) low dropout rate
Intervention: 162/485 decontaminated, if Small Intestine of 5%
(33.4%) elective Intervention: 1/19 (5%) Study used groups
2017 American Medical Association. All rights reserved. 275
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Control: 97/371 Bowel Prep- all patients Control: 3/14 (21%) of 50 100
(26.1%) undergoing colorectal Vascular Surgery consecutive
Contaminated resections had preop Intervention: 0/26 patients either to
Intervention: 37/485 bowel prep with 3L of Control: 0/24 control or the
(7.6%) prepacol Other triclosan
Control: 25/371 (6.7%) Preop shower all Intervention: 1/27 (4%) treatment group
Septic patients had a regular Control: 4/19 (21%) Follow-up: within 2
Intervention: 0/485 shower without iodine Colorectal weeks post-
Control: 4/371 (1.1%) within 24h preop Intervention: 17/143 discharge
Indications: NR Hair removal: abdominal (12%) Funding Source
Setting: One University wall hair removed but Control: 19/100 (19%) Conflicts:
Hospital when and how was not Total SSI Colorectal Authors: NR
Location: Switzerland described. Procedures: Institution: NR
Dates: September Antibiotic prophylaxis: all SSI/Colo Procedures = Study: Industry
2009 - September patients received 36/243 (14.8%) Supplies: NR
2011 metronidazole and OR: 3.3 (1.9-5.7)
Inclusion Criteria: all ceftriaxone; P<0.05
patients scheduled metronidazole and
to undergo open clindamycin in case of BMI >30 and SSI
abdominal allergy) within 60 14/130 (10.8%)
exploration and minutes prior to OR: 1.68 (*0.8-3.2)
surgery and closure incision. Additional P=0.12
of the incision in a doses were
standard fashion administered in Other infections: NR
(laparotomy) who surgeries >4h Topic-specific
gave consent. Skin prep: Alcohol-based outcomes:
Exclusion Criteria: povidone-iodine Wound culture results
Refusal of surgery, Drape: skin drape used (reported in %)
minimally invasive and wound edges were Staphylococci
procedures or protected with surgical Intervention: 23.1%
nonsurgical swaps. Swabs were Control: 23.1%
therapies, burst soaked in povidone Enterococci
abdomen, planned iodine solution for Intervention: 23.1%
revision within 30 patients with a Control: 30.1%
days, or an on- contaminated Streptococci
demand re- abdominal cavity. Intervention: 5.1%
laparotomy for Normothermia: Control: 5.1%
organ/space temperature was kept Pseudomonas spp.
o
infections. Mortality >35 C in patients with a Intervention: 0
2017 American Medical Association. All rights reserved. 276
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
in the follow up warming device. Control: 2.5%
period and abdomen Found organ/space Enterobacteriacae
not closed during the infection: patients with Intervention: 15.4%
initial procedure. an organ/space Control: 23.1%
infection upon Others
laparotomy underwent Intervention: 15.4%
an abdominal lavage Control: 23.1%
with Ringers lactate MDRO not reported
solution of at least 5L
Closure: abdominal wall Reoperations: NR
closed with continuous
suture & peritoneum Length of stay:
was not closed In hospital stay: meanSD
separately. Skin closed (range), days
with staples. Intervention: 1513 (2-
Wound rinsing: post- 134)
closure, wound rinsed Control: 1118 (2-209)
with Ringers solution. P=0.300
Oxygenation: in patients
with a history of Mortality: Exclusionary
Cardiovascular disease, 10 patients died. Cause of
oxygen was supplied death an d study arm
via nasal tube to not reported
maintain oxygen Adverse events: NR
saturation of >95%
postop.
Glycemic control: patients
requiring intensive care
treatment had a tight
postoperative glucose
control and correction
of hyperglycemic states
by continuous or
intermittent insulin
administration.
2017 American Medical Association. All rights reserved. 277
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Nakamur- RCT To evaluate Number of patients: Intervention group: SSI: Definitions:
a 1, 4, 5, whether the N=410 n=206 Total: 28/410 (6.8%) Wound infection:
74
2013 7, 8, 9 incidence of Patient Wounds closed with Wound Infection CDC 1999
(ES) wound Characteristics: no triclosan-coated Intervention: 9/206 Guideline.
infections can significant difference polyglactin 910 (4.3%) Perioperative care
be reduced existed between antimicrobial sutures Control: 19/204 (9.3%) Other notes: The
when groups Timing of intervention: P=0.047 assumed
triclosan- Age, y: meanSD intraoperative expected wound
coated sutures Intervention: Duration of intervention: Organ/space infection rates of
are used for 69.411.3 closure until absorption Intervention: 5/206 4% to 5% for the
abdominal Control: 70.211.1 Device/agent: polyglactin (4.3%) study group and
wound P=0.44 910 sutures either Control: 4/204 (9.3%) 10% to 11% for
closures and Gender M:F conventional or P=0.74 the control
to evaluate the Intervention: 130:76 triclosan coated group. With a 2-
impact on Control: 112:92 Monitoring intervention: Wound infection by sided
costs P=0.09 daily checks until surgery type alpha=0.05, the
associated Obesity: discharge followed by Laparoscopic: 12/227 study was
2
with wound BMI, kg/m : meanSD 30 day postop checkup (5.3%) expected to
infections after Intervention: 23.23.6 Control group: n=204 Open: 16/183 (8.7%) have 80% power
colorectal Control: 23.43.8 Wounds closed with P=0.16 to detect a
surgery. P=0.61 conventional polyglactin Laparoscopic surgery: relative risk
Comorbidities: 910 antimicrobial Intervention: 5/119 reduction of 5%;
Diabetes mellitus: sutures (4.2%) a total of 400
Intervention: 41/206 Standard preventive Control: 7/108 (6.5%) patients were
(19.9%) measures: P=0.43 estimated to be
Control: 31/204 Antibiotic prophylaxis: Open Surgery needed.
(15.2%) intravenous Intervention: 4/87 (4.6%) Follow-up: 30
P=0.21 cephalosporin 30 min Control: 12/96 (12.3%) days post
Procedures: colorectal prior to incision; every P=0.061 discharge.
surgeries including 3h of operative time; Funding Source
right, left, and and for 48h postop in Other infections: NR Conflicts:
transverse both groups. Topic-specific Authors: NR
colectomy; Wound protectors: used outcomes: Institution: NR
sigmoidectomy; low during open surgery, Cultured organism (note Study: NR
anterior and and lap protectors used some infections had Supplies: NR
abdominoperineal during delivery of were multi-organism)
resection; total specimens during Enterococcus
colectomy; and laparoscopic surgery. Intervention: 5/9
simple colostomy Closure technique: Control: 6/19
2017 American Medical Association. All rights reserved. 278
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Laparoscopic Surgery interrupted sutures and Enterobacter
Intervention: 119/206 surgical staples for skin Intervention: 0/9
(57.8%) by 7 surgeons. Control: 3/19
Control: 108/204 Bacteroides
(52.9%) Intervention: 3/9
P=0.33 Control: 5/19
Open Surgery MRSA: 0/9 vs. 1/19 (5.3%)
Intervention: 87/206 Missing data: 2/9 (22.2%)
(42.2%) vs. 6/19 (31.6%)
Control: 96/204 Reoperation: NR
(47.1%) Length of stay: (patients
P=0.33 with infected wounds
Indications were discharged and
Setting: 1 hospital wounds were managed
Location: Japan from outpatient clinic)
Dates: April 2009 Postop Hospital Stay,
March 2011 days: median (SD),
Inclusion Criteria: Intervention: 11 (6-79)
Patients undergoing Control: 11.5 (6-93)
elective colorectal P=0.08
surgery during the Postop Hospital Stay,
study dates. days: mean SD
Exclusion Criteria: NR Intervention: 15.211.6
Control: 15.610.4
P=0.71
Mortality: NR
Adverse events: NR
Turtiain- RCT To determine Number of patients: Intervention group: SSI Definitions:
en 1, 2, 3, whether the N=276 n=139 Overall: 22% Surgical wound
68
2012 5, 6, 7, use of Patient Arterial exposure and vein Intervention: 31/139 infection: any
(ES) 8, 9 triclosan- Characteristics harvest incisions closed (22.3%) complication of
coated sutures No significant with triclosan-coated Control: 30/137 (21.9%) surgery was
for wound differences seen polyglactin 910 and designated an
closure would between groups. poliglecaprone 25 Superficial: infection if
reduce the risk Age, y: mean (SD) sutures. Intervention: 24/139 bacteria were
of surgical Intervention: 72 (11) Timing of intervention: (17.3%) isolated from the
wound Control: 72 (11) intraoperative Control: 22/137 (16.2%) wound or if
infection after Gender: m/f Duration of intervention: Deep localized
peripheral Intervention: 87/25 closure until absorption Intervention: 5/139 redness,
2017 American Medical Association. All rights reserved. 279
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
vascular (63%/37%) Device/agent: Triclosan- (3.6%) warmth,
surgery. Control: 86/51 coated or standard Control: 5/137 (3.7%) swelling, and
(63%/37%) polyglactin 910 and Graft Infection pain around the
2
Obesity: BMI (kg/m ) poliglecaprone 25 Intervention: 2/139 wound appeared
mean (SD) sutures. (1.5%) within 30 days
Intervention: 26 (5) Monitoring intervention Control: 3/137 (2.2%) after the
Control: 26 (4) Control group: n=137 operation (CDC
Comorbidities Arterial exposure and vein Other infections: NR definition)
Diabetes harvest incisions closed Topic-specific Superficial: if only
Intervention: 43/139 with standard outcomes: skin and
(31%) polyglactin 910 and Graft Thrombosis: subcutaneous
Control: 44/137 (32%) poliglecaprone 25 Intervention: 7/139 tissue are
COPD sutures. (5.0%) involved
Intervention: 16/139 Control: 6/137 (4.4%) Deep: if wound
(12%) Standard preventive P=0.80 infection
Control: 23/137 (1%) measures: Stroke involves both
Concurrent use of Antibiotic prophylaxis: Intervention: 4/139 fascia and
corticosteroids: At 3 hospitals: 3g (2.9%) muscle layers
Intervention: 19/139 cefuroxime Control: 1/137 (0.7%) Graft/O/S: if an
(14%) administered P=0.18 artery or a graft
Control: 15/137 (11%) intravenously within 1h Cultures taken: no (vein or
prior to incision. resistant bacteria prosthesis)
Procedures: lower limb At 2 hospitals: 1.5g reported. becomes
arterial cefuroxime Reoperations: NR infected.
reconstruction administered Length of stay: days (SD)
Indications: intravenously 1h prior to Intervention: 5.5 (6.5) Perioperative
Claudication incision and then every Control: 5.2 (4.3) care: NR
Intervention: 44/139 8h for the first 24h after P=0.68 Other notes:
(32%) operations. Sample size: for
Control: 27/137 (31%) At 1 hospital: if a Mortality: 10 patients died the study to
Rest pain prosthetic graft was within 30 days of provide an 80%
Intervention: 48/139 used, patients also surgery. (9 had no SSI) power for
(35%) received intravenous 30 day mortality detecting a 50%
Control: 42/137 (31%) vancomycin. Intervention: 6/139 reduction in
Ischemic ulcer (4.3%) infection rate at
Intervention: 34/139 Control: 4/137 (2.9%) =0.05, there
(25%) P=0.55 should be at
Control: 39/137 (29%) Adverse events: least 137
Other Major amputation patients in both
2017 American Medical Association. All rights reserved. 280
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Intervention: 13/139 Intervention: 4/139 groups.
(9%) (2.9%) Follow-up: At least
Control: 29/137 (21%) Control: 5/137 (3.6%) 1 month postop
Setting: 3 tertiary or until the
referral hospitals and wound healed
two secondary Funding Source
referral hospitals. Conflicts:
Location: Finland Authors: NR
Dates: July 2010 Institution: NR
January 2011 Study: NR
Inclusion Criteria: Supplies: NR
adult patients who
underwent
nonemergency lower
limb arterial surgery.
Exclusion Criteria:
Aortoiliac
procedures and the
patients refusal to
participate.
Seim RCT To evaluate Number of patients: Intervention group: SSI Definitions:
69
2012 1, 5, 6, the effects of N-=323 n=163 Overall infection rate: SSI positive
(ES) 7, 8 Triclosan Patient Let wound closure with 33/323 (10.2%) bacterial culture
coated Characteristics: triclosan-coated Intervention: 16/160 and clinical
polyglactin demographic and polyglactin 910 suture (10%) judgment
910 suture on perioperative Timing of intervention: Control: 17/163 (10.4%) Perioperative
standard characteristics Intraoperative care: NR
2
polyglactin between groups are Duration of intervention: BMI and infection (kg/m ) Other notes:
910 suture comparable at Intra and postoperative meanSD: Study power: a-
with regard to baseline except for Device/agent: Standard Infection (n=33): priori, in order to
surgical leg blood glucose (see or triclosan-coated 29.50.8 detect an
wound below). polyglactin 910 sutures No-infection (m=290): estimated 50%
infections Age, y meanSD Monitoring intervention: 27.50.2 reduction in
following Intervention: 63.50.7 by hospital staff in p=0.02 infection rate in
saphenous Control: 63.10.8 hospital, by patient IDDM the triclosan-
vein Gender: female postdischarge. coated suture
harvesting in a Intervention: 17/160 Control group: General Perioperative group and a
prospective (10.6%) Leg wound closure with Data statistical power
randomized Control: 19/163 conventional polyglactin There were no significant level of 0.8, this
2017 American Medical Association. All rights reserved. 281
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
study. (11.7%) 910 suture differences except: study required a
2
Secondly, to Obesity: BMI (kg/m ), Standard preventive Cardiopulmonary bypass minimum sample
examine meanSD measures: time (min) size of 302
patient- and Intervention: 27.70.3 Hair removal: with electric Infection (n=33): patients
operative Control: 27.50.3 razor on the afternoon 86.45.5 Follow-up: 4
characteristics Comorbidities of the day before Control/intervention weeks post
, which are Diabetes mellitus, surgery. (n=17/n=16): discharge (a
assumed to Intervention: 31/160 Pre-Op bathing: in the 81.39.1/92.2.96.0 registration form
predict leg (19.4%) evening before the No-infection (m=290): was returned at
wound Control: 40/163 operation, all patients 77.21.2 4 weeks postop)
infections. (24.5%) took a shower including Control/intervention Funding Source
IDDM washing with soap and (n=146/n=144): Conflicts:
Intervention: 9/160 chlorhexidine gluconate 75.71.7/79.21.9 Authors: None
(5.6%) 40mg/ml. This shower p=0.03 Institution: None
Control: 17/163 repeated on the day of Study: None
(10.4%) surgery. Aortic cross clamping time Supplies: None
Blood Glucose Standard CABG (min)
(mmol/l), meanSD technique: using CPB, Infection (n=33):
Intervention: 6.60.3 moderate hypothermia 48.34.1
o
Control: 8.50.8 (32 C), cold crystalloid Control/intervention
P=0.05 or cold blood (n=17/n=16):
cardioplegia and aortic 44.45.8/53.7.95.8
Procedures: Coronary cross clamping. No-infection (m=290):
Artery Bypass Graft Skin disinfection: with 41.41.1
(CABG) chlorhexidine solution, Control/intervention
Indications: NR 5 mg/ml with 70% (n=146/n=144):
Setting: 1 university ethanol. 40.11.1/43.53.5
hospital Saphenous vein p=0.05
Location: Switzerland harvesting: from the
Dates: September medial malleolus by a Other infections: NR
2009 - September continuous skin Topic-specific
2011 incision, ending either outcomes:
Inclusion Criteria: below or over the knee. Bacterial cultures taken for
patients undergoing Side branches were confirmation results not
CABG at the study ligated or clipped. For reported
center practical reasons, the Reoperations: NR
Exclusion Criteria: left leg was Length of stay: NR
Patients with leg predominantly Mortality: NR
wounds, bilateral preferred. Adverse events: NR
2017 American Medical Association. All rights reserved. 282
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
vein harvesting, Antibiotic prophylaxis:
harvesting of the cefalotine as a single
short saphenous dose of 2g
vein, varicose veins intravenously before
and those skin incision and
undergoing continued with 3-h
emergency CABG intervals to a total of 8g
in both groups.
Drape: wound covered
with drape, compresses
and elastic bandages.
First day postop, the
compresses and elastic
bandages were
removed and third
postop day the drape
removed.
Isik RCT To evaluate Number of patients: Intervention group: SSI Definitions:
79
2012 1, 3, 4, whether the N=510 n=170 Superficial Sternum SSI SSI CDC
(ES) 5, 10 incidence of Patient Wound closure with Total: 16/510 (3.1%) definitions.
sternal and leg Characteristics: triclosan-coated Intervention: 4/170 Perioperative
wound patients were similar polyglactin 910 suture (2.4%) care: NR
infections is in demographic and Timing of intervention: Control: 12/340 (3.5%) Other notes:
reduced when lab characteristics. intraoperative P=0.596 Study power was
coated sutures Age >65 y: Duration of intervention: Mediastinitis: 0 cases calculated on
are used for Intervention: 70 closure until absorption Leg Site SSI the assumption
wound (41.2%) Device/agent: Polyglactin Total: 17/402 (3.7%) that SSI would
closure, Control: 138 (40.6%) 910 suture either Intervention: 5/142 be reduced from
compared with Gender: Male coated or uncoated (3.5%) 6% to 1%, the
non-coated Intervention: 111 Monitoring intervention: Control: 10/260 (3.8%) study group was
sutures (64.7%) Patients inspected daily P=1.000 to be the size
Control: 228 (67.1%) by nurse in hospital. of the control
2
Obesity: BMI>30kg/m Post discharge, patients Gender and SSI group with a
Intervention: 41 were seen every 10 Male total of 510
(24.1%) days in the cardiac No SSI 324/338 (95.9%) patients. Which
Control: 84 (24.7%) rehabilitation center for SSI 14/338 (4.1%) was performed
Comorbidities: 30 days. Female with a risk
Diabetes mellitus Control group: n=340 No SSI 158/172 (91.9%) coefficient () of
Intervention: 57 Standard polyglactin 910 SSI 14/172 (8.1%) 0.05, a
2017 American Medical Association. All rights reserved. 283
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
(33.5%) suture P=0.067 confidence
Control: 120 (35.3%) Standard preventive interval (1-) of
EuroSCORE Risk measures: NR Both sternal and leg 0.95, a risk
Score <5 infections developed in coefficient () of
Intervention: 119 3 patients (not stated 0.20 and a
(70.0%) which group they power (1-) of
Control: 210 (61.8%) belong to) 0.80
EuroSCORE Risk Follow-up: 30
Score >5 SSI in patient with days postop
Intervention: 51 diabetes Funding Source
(30.0%) OR 3.23 (1.45-7.23), Conflicts:
Control: 130 (38.2%) p=0.04 Authors: None
P=0.077 Institution: None
Procedures: SSI in patients with Study: None
Emergency: EuroSCORE > 5 Supplies: None
Intervention: 2 (1.2%) OR 0.98 (0.91-1.05);
Control: 14 (4.1%) P=0.164
P=0.104
Procedures: p=0.78 Other infections: NR
CABG Topic-specific
Intervention: 147 outcomes:
(86.5%) Wound Culture Results
Control: 263(77.4%) S. aureus
Valve repair Intervention Sternum: 0
Intervention: 17 Intervention Leg: 0
(10.0%) Control Sternum: 4
Control: 50 (14.7%) Control Leg: 1
CABG and valve repair S. epidermis
Intervention: 6 (3.5%) Intervention Sternum: 1
Control: 25 (7.4%) Intervention Leg: 0
Other operations Control Sternum: 1
Intervention: 0 Control Leg: 1
Control: 2 (0.6%) Corynebacterium spp.
Indications: NR Intervention Sternum: 0
Setting: Single private Intervention Leg: 0
hospital Control Sternum: 1
Location: Turkey Control Leg: 0
Dates: April 2008 Pseudomonas aeruginosa
September 2009 Intervention Sternum: 1
2017 American Medical Association. All rights reserved. 284
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Inclusion Criteria: Intervention Leg: 0
Patients undergoing Control Sternum: 0
cardiac surgery Control Leg: 0
during the study Klebsiella pneumonaie
period Intervention Sternum: 1
Exclusion Criteria: NR Intervention Leg: 2
Control Sternum: 0
Control Leg: 0
Swabs taken for
suspected wounds.
MRSA was not
recovered from any
wounds in study
Reoperations: NR
Length of stay: NR
Mortality: NR
Adverse events: NR
Williams RCT To assess the Number of patients: Intervention group: n=75 SSI Definitions:
72
2011 1, 2, 4, effect of N=150 Wounds closed with Overall rate SSI all
(ES) 5, 6, 7 triclosan Patient triclosan-coated 2 weeks Postop: 13.7% investigators
coating of Characteristics: subcutaneous (20/146) were conversant
polyglactin Age: media, years polyglactin and Intervention: 9/73 with the CDC
and (Range) triclosan-coated (12.3%) definition of SSI
poliglecaprone Intervention: 61 (32- subcuticular Control: 11/73 (15.1%) and the
sutures for 87) poliglecaprone. P=NS ASEPSIS and
skin closure Control: 59 (30-80) Timing of intervention: 6 weeks postop: 18.9% Southampton
after elective Gender: all female intraoperative (24/127) wound scores.
breast cancer Obesity: NR Duration of intervention: Intervention: 10/66 Perioperative
surgery. Comorbidities: NR closure to absorption (15.2%) care:
Procedures: Breast Device/agent: triclosan- Control: 14/61 (22.9%) Anesthesia:
cancer surgery: coated subcutaneous P=NS general
Wide lump excision, polyglactin and Other infections: NR anesthesia
sentinel node triclosan-coated Topic-specific Other notes:
biopsy, Axillary node subcuticular outcomes: patients given
clearance, poliglecaprone or Patients lost to follow up diaries to record
mastectomy and standard polyglactin Two weeks (n=4) events occurring
localized wire and poliglecaprone Patient request within the 6
excision or some Monitoring intervention: Intervention: 1 weeks postop.
combination of the patients reviewed Control: 1 Significant
2017 American Medical Association. All rights reserved. 285
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
above regularly by nurses and Lost to follow up events were
Indications: NR at two and six weeks Intervention: 0 corroborated by
Setting: Single center postop as outpatients or Control: 1 an attending
Location: United at a home visit. Need for further surgery physician.
Kingdom Control group: n=75 Intervention: 0 Power: estimated
Dates: November 2008 Wounds closed with Control: 1 sample size of
February 2011 subcutaneous Six weeks (n=19) 150 patients (75
Inclusion Criteria: polyglactin and Patient request in each group)
Women >18 years subcuticular Intervention: 1 was considered
undergoing primary poliglecaprone. Control: 0 to have 80%
elective breast Lost to follow up power to show a
surgery under the Standard preventive Intervention: 1 statistically
care of two breast measures: Control: 2 significant
surgeons at the Antibiotic prophylaxis: 8 Need for further surgery difference of
study center patients considered Intervention: 5 p<0.05
Exclusion Criteria: high risk received a Control: 10 Follow-up: 6
Inflammatory breast single intravenous dose weeks postop.
cancer or skin of 1g of amoxicillin Reoperations: Funding Source
ulceration; neo- clavulanate. (high BMI, exclusionary criteria Conflicts:
adjuvant mastectomy or axillary 6/24 SSI needed an Authors: Industry
chemotherapy or clearance_ none of intervention to Institution: NR
radiotherapy; these developed SSI) open/pack or aspirate Study: Industry
surgery for benign or Closure: wounds closed axillary collections. Supplies: NR
reconstructive after surgery using 3/6 required
reasons; known subcutaneous readmission
immune deficiency polyglactin and 1/24 had a delay in
or allergy to subcuticular starting adjuvant
triclosan; and poliglecaprone at the chemotherapy.
inability to give discretion of the Need for further surgery:
consent or suspicion operating consultant Intervention: 5/9 (55.6%)
that the patient was surgeon. Control: 10/14 (71.4%)
unlikely to comply Wound dressing: butterfly Length of stay: NR
with the follow-up. stitches and waterproof, Mortality: NR
transparent dressing or Adverse events: NR
one of two types of
adhesive wound
dressing. OR an
adhesive wound
dressing alone.
2017 American Medical Association. All rights reserved. 286
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
All other interventions
such as pre-medication,
anesthesia, and
phlebothrombosis
prophylaxis were
standard for both
groups.
Baracs RCT To compare Number of patients: Intervention group: SSI Definitions:
71
2011 1, 2, 5, polydioxanone N=385 n=188 Intervention: 23/188 SSI SSI
(ES) 7, 10 suture with Patient Triclosan-coated running (12.2%) described as
and without Characteristics: looped polydioxanone Control: 24/197 (12.2%) divided into
triclosan in groups showed used to close the P=NS superficial
seven high- homogeneity in abdominal fascia. incisional, deep
volume demographic Timing of intervention: Late infection (post incisional,
Hungarian features intraoperative discharge) abdominal
surgical Age, y: mean Duration of intervention: Intervention: 4/188 dehiscence but
institutions Intervention: 62.6 closure and up to 30 (2.1%) these were not
over a one- Control: 63.5 days until absorption Control: 9/197 (4.6%) defined.
year period Gender: m:f Device/agent: Running P=0.41 Perioperative
Intervention: 110:78 looped polydioxanone care: Adjuvant
Control: 111:86 sutures either triclosan- SSI By Operations therapy was not
Obesity: mean BMI of coated or standard Right-sided colon allowed to be
patients with SSI Monitoring intervention: resection started within the
Intervention: 23.14 examination of incision Intervention: 11/46 30-day follow-up
Control: 27.97 site during hospital stay (24%) period
Comorbidities: and telephone call Control: 5/44 (11%) Other notes: Pilot
Type II Diabetes follow up at 30 days P=0.006 study of 50
mellitus post discharge Rectal resection patients showed
Intervention: 27/188 Control group: n=197 Intervention: 6/89 (7%) a 5% SSI rate in
(14.4%) Standard running looped Control: 14/95 (15%) the Triclosan
Control: 26/197 polydioxanone used to P=0.033 coated
(13.4%) close the abdominal Left sided colon and polyglactin 910
Neoadjuvant therapy: fascia. sigmoid resection suture and a
Intervention: 47/188 Intervention: 4/40 (10%) 20% SSI rate in
(25%) Standard preventive Control: 3/45 (7%) the standard 910
Control: 40/197 measures P=NS suture. This
(20.3%) Closure: separate Segmental resection and study showed
2017 American Medical Association. All rights reserved. 287
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
peritoneal closure and colectomy SSI was about
Procedures: subcutaneous sutures Intervention: 2/10 (20%) 10% in each
hemicolectomies, were optional Control: 1/8 (13%) group.
transversectomies, depending on surgeons P=NS Polyglactin is
cecal resection, preference. If Total and subtotal braided and
colostomies, A-P employed, 2-0 suture colectomy polydioxanone is
resections of the utilized. Interrupted 2-0 Intervention: 0/3 monofilament.
rectum, sigmoid poliglecaprone 25 used Control: 1/5 (20%) Follow-up: 30
resections, for the skin closure. days post
abdominal Antibiotic Prophylaxis: a BMI and SSI discharge via
2
resections of the second-generation BMI<20kg/m telephone call.
rectum, subtotal cephalosporin and Intervention: 3/7 (42.8%) Funding Source
colectomies, total metronidazole 30 Control: 3/11 (27.3%) Conflicts:
2
colectomy and minutes before incision) Normal BMI (20-30 kg/m ): Authors: None
abdominal resection Drapes disposable Intervention: 16/147 Institution: None
of the rectum. drapes used. (10.9%) Study: None
Indications: Benign or Incision locations: not Control: 16/139 (11.5%) Supplies: None
2
malignant colon or standardized in either Obese (BMI >30kg/m ):
rectal disease rectal or hemicolectomy Intervention: 3/34
Setting: 7 hospitals (3 surgeries) (11.8%)
university, 4 high- Control: 5/47 (10.6%)
volume hospitals)
Location: Hungary Normal BMI (20-30
2
Dates: December 2009 kg/m ): 11.2% (32/286)
2
November 2010 BMI<20kg/m : 33.3%
Inclusion Criteria: (6/18)
Patients between the P<0.05
ages of 18-80 years Other infections: NR
old with benign or Topic-specific
malignant colon or outcomes:
rectal disease Cultured Organisms
undergoing and Gram Positive:
elective open Pseudomonas
surgical procedure aeruginosa,
involving an Enterococcus faecium,
enterotomy E. coli, Enterococcus
Exclusion Criteria: spp. cultured from
Patients with both groups, numbers
systemic disease not reported.
2017 American Medical Association. All rights reserved. 288
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
influencing local Gram Negative: S.
surgical site healing epidermis:
(e.g. type I diabetes Intervention: 0
mellitus, Child-Pugh Control: 2
class B-C liver
cirrhosis, and Reoperations: NR
chronic kidney Length of stay: NR
disease Mortality: NR
necessitating Adverse events: NR
dialysis) or those
having
immunosuppressive
treatment or
inflammatory bowel
disease. Also, acute
operations with
unprepared bowel (9
cases) & patients
who refused
consent. Some
patients with
intraoperative
findings such as
locally incurable
tumor or sepsis
(abscess, necrotic
tumor), or with
postoperative
findings such as
further surgical
intervention through
the site and patients
who withdrew the
consent later.
Undesirable
complications such
as sterile surgical
site dehiscence and
suture breakage
2017 American Medical Association. All rights reserved. 289
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
during the post-
operative period also
led to exclusion from
the trial.
Galal RCT To assess the Number of patients: Intervention group: SSI: Definitions: CDC
76
2011 1, 2, 3, incidence of N=450 n=230 Total SSI: 50/450 (11%) definitions: an
(ES) 4, 5, 6 surgical site Patient Surgeries where Intervention: 17/230 (7%) infection within
infection using Characteristics: absorbable, braided Control: 33/220 (15%) 30 days of
triclosan- there were no polyglactin 910 triclosan P=0.011 surgery (or
coated significant coated suture used in (please note that the within a year in
polyglactin differences between all steps except in some numbers for clean, case of
910 groups regarding cases polypropylene clean contaminated and prosthetic
antimicrobial age was used for contaminated surgery surgery): (1)
Age: laparotomy closure and do not add up to the n diagnosis
21-30 y vascular suture. for the intervention & consists of
Intervention: 42/230 Poliglecaprone 25 used control group) infection of an
(18.3%) in skin closure. Other infections: NR anatomic plane
Control: 40/220 Timing of intervention: by one of the
(18.2%) intraoperative Topic-specific following
31-40 y Duration of intervention: outcomes: NR manifestations:
Intervention: 75/230 suturing to absorption collection;
(32.6%) Device/agent: Reoperations: NR inflammatory
Control: 85/220 absorbable, braided Length of stay: meanSD signs (pain,
(38.6%) polyglactin 910 suture (range) days tenderness,
41-50 y coated with triclosan. SSI 7.103.92 (3-16) edema,
Intervention: 90/230 Or polyglactin 910 No SSI 3.391.48 (1-13) redness);
(39.1%) suture. P<0.001 dehiscence; or
Control: 75/220 Monitoring intervention: positive culture;
(34.1%) NR Mortality: NR (2) classification
51-60 y Control group: n=230 Adverse events: NR according to
Intervention: 23/230 Surgeries where anatomic plane
(10.0%) conventional as follows:
Control: 20/220 (9.1%) absorbable, braided superficial
2017 American Medical Association. All rights reserved. 290
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
P=0.567 polyglactin 910 suture incisional
Gender male was used in all surgical surgical site
Intervention: 148/230 steps except in some infection:
(64.3%) cases, polypropylene infection of skin
Control: 127/220 was used for and
(57.7%) laparotomy closure and subcutaneous
P=0.1499 vascular suture, and tissue; deep
Obesity: NR Poliglecaprone 25 was incisional
Comorbidities: used in skin closure. surgical site
Diabetes: infection:
Intervention: 32/230 Standard preventive infection of deep
(13.9%) measures: soft tissue
Control: 42/220 Closure: in both groups, (fascia and
(19.1%) monofilament sutures muscles); or
P=0.1386 were the only kind of organ/space
Procedures: suture material used for surgical site
Vascular surgery: n=86 the following infection:
Intervention: 50/230 applications: infection of
(21.7%) polyglecaprone used for organ/space.
Control: 36/220 skin closure in plastic Perioperative care
(16.4%) surgery, hernia, Other notes:
Plastic Surgery: n=82 thyroidectomy, Patients were
Intervention: 40/230 mastectomy, lipoma assessed daily
(17.4%) and hand surgery; in the hospital.
Control: 50/220 polypropylene used for Post discharge
(19.1%) vascular, fascial patients were
Gastrointestinal closure, and skin in requested to
surgery: n=65 surgeries other than return to the
Intervention: 38/230 aforementioned outpatient clinic
(16.5%) surgeries. weekly for 30
Control: 27/220 In this study, they days (then
(12.3%) followed the local monthly until the
Biopsy: n=64 protocol of the end of the first
Intervention: 32/230 infection control unit year in the case
(13.9%) at their institute. This of prosthetic
Control: 3/220 (14.5%) may deviate from surgery)
Hernia: n=63 current modern This was a
Intervention: 30/230 practices. This multicenter
(13.0%) protocol used for both study, however,
2017 American Medical Association. All rights reserved. 291
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Control: 33/220 (15%) groups. (Modern results were only
Thyroidectomy: n=30 protocol is considered reported for 1
Intervention: 9/230 by this study to be: center
(3.9%) clippers rather than Follow-up: 30
Control: 21/220 (9.5%) razors for hair removal; days or 1 year in
Mastectomy: n=15 local skin warming; the case of
Intervention: 10/230 antibiotic prophylaxis orthopedic
(4.3%) given before clean surgery.
Control: 5/220 (2.3%) surgery involving the Funding Source
Lipoma: n=13 placement of a Conflicts:
Intervention: 7/230 prosthesis or implant, Authors: NR
(3.0%) clean contaminated Institution: NR
Control: 6/220 (2.7%) surgery, and Study: NR
General surgical contaminated surgery. Supplies: NR
procedures: n=11 This antibiotic
Intervention: 4/230 prophylaxis is not
(1.7%) routinely used for clean
Control: 7/220 (3.2%) non-prosthetic
Exploration: n=9 uncomplicated
Intervention: 3/230 surgeries and it should
(1.3%) be timely and
Control: 6 /220 (2.7%) appropriate for the
Amputation: n=5 organisms expected.)
Intervention: 3/230
(1.3%)
Control: 2/220 (0.9%)
Also, the following
surgeries had no
SSI:
Hand surgery: n=4
Shoulder Tumor: n=1
Knee tumor: n=1
Orchiectomy: n=1
Indications
Setting: 1 university
hospital
Location: Egypt
Dates: NR
Inclusion Criteria: All
2017 American Medical Association. All rights reserved. 292
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
patients of different
age, sex, and risk
factors who were
candidates for
surgical intervention
during the study
period
Exclusion Criteria:
Patients with an
established
preoperative
infection at the
surgical site
Rasic RCT The aim of this Number of patients: Intervention group: n=93 SSI Definitions: wound
70
2011 1, 2, 4, study was to N=184 Abdominal wall was closed Presence of wound infection not
(ES) 5, 6 compare the Patient with a continuous infection: defined.
effect of Characteristics: single-layer mass Intervention: 4/91 Postoperative data:
triclosan there was no technique (peritoneum, (4.3%) was collected
coated statistical difference muscle, & fascia) with Control: 12/91 (13.2%) from operation
polyglactin in demographic or triclosan coated P=0.035 reports, nurses
910 or preoperative data polyglactin 910 sutures Other infections: NR wound reports,
polyglactin between groups. Timing of intervention: chart review and
910 on Age, years, meanSD intraoperative Topic-specific microbiology
abdominal Intervention: 5814.5 Duration of intervention: outcomes: reports.
wall healing in Control: 5714.7 closure Postop inflammatory Perioperative
patients Gender: male, Device/agent: triclosan reactions to skin care: NR
undergoing Intervention: 49/91 coated or standard sutures: Other notes: None
elective (54%) polyglactin 910 sutures Intervention: 7/91 Follow-up: NR
surgery for Control: 50/91 (54%) Monitoring intervention: (7.5%) Funding Source
colorectal Obesity: BMI>25 biochemical markers of Control: 16/91 (17.5%) Conflicts:
3
carcinoma kg/m , inflammation were P=0.039 Authors: NR
Intervention: 7/91 monitored: white blood Dehiscence Institution: NR
(8%) cell count (WBC); Intervention: 1/91 Study: NR
Control: 9/91 (9%) postoperative (1.1%) Supplies: NR
Comorbidities: NR procalicitonin PCT; Control: 7/91 (7.7%)
Duration of surgery and C-reactive protein P=0.027
Intervention: CRP)
95.517.3 Control group: n=91 Incisional hernia
Control: 91.318.6 Abdominal wall was closed Intervention: 2/91
2017 American Medical Association. All rights reserved. 293
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
P=0.8933 with a continuous (2.2%)
single-layer mass Control: 5/91 (5.5%)
Procedures: surgery technique (peritoneum, P=0.235
for removal of muscle, & fascia) with
colorectal carcinoma polyglactin 910 Reoperations:
Indications: Colorectal Intervention: 1/91
cancer Standard preventive (1.1%)
Setting: 1 university measures: Control: 8/91 (8.8%)
hospital Antibiotic prophylaxis: P=0.015
Location: Croatia Gentamycin 160mg and Intervention Reoperations:
Dates: September metronidazole 500mg, 1/1 = Dehiscence
2008 - September given intravenously Control Reoperations
2009 during induction of 7/8 = dehiscence
Inclusion Criteria: anesthesia. 1/8 = peritonitis
patients diagnosed Operative technique: all Length of stay:
with colorectal operations performed Mean hospitalization
cancer scheduled for through a midline period
elective surgery. incision. Skin was Intervention: 1.21.3
Exclusion Criteria: NR incised (15-18cm days
length) with a scalpel; Control: 21.42.8 days
all other layers P<0.05
transected with Mortality: no deaths in
diathermy. either group
Closure: running sutures Adverse events:
were 1cm apart and Inflammatory reactions to
1.5cm from the wound skin sutures:
edge. Skin closed with Intervention: 7/91
a polyamide. (7.5%)
Control: 16/91 (17.5%)
P=0.039
Mingma- RCT To evaluate Number of patients: Intervention group: n=50 SSI: (follow up 12 Definitions: NR
lairak 1, 2, 3, the efficacy of N=100 Antibacterial-coated months) Perioperative
78
2009 4, 5, 6, triclosan Patient absorbable suture SSI (total) care: NR
(ES) 7, 8, 9, coated Characteristics: No (triclosan) used to close Overall rate: 9/100 9% Other notes: All
10 absorbable statistically the abdominal sheath. Intervention: 5/50 (10%) patients
suture in significant Timing of intervention: Control: 4/50 (8%) completed the
reducing the differences in Intraoperatively P=0.727 study
surgical site demographic Duration of intervention: Superficial Authors set the
2017 American Medical Association. All rights reserved. 294
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
infection rate characteristics, Intraoperatively Intervention: 5/50 (10%) discontinuation
associated preoperative Device/agent: Control: 3/50 (6%) criteria infection
with information and Antibacterial Deep rate >10% in the
appendectomy operative information absorbable suture Intervention: 0/50 intervention
compared with between groups. (triclosan coated) Control: 1/50 (2%) group or >2
traditional, Age, y: mean Monitoring intervention: Organ/Space times in the
non-coated Intervention: 29.1 NR Intervention: 0/50 control group
braided Control: 29.8 Control group: n=50 Control: 0/50 compared with
absorbable Gender: m:f Traditional braided the intervention.
suture. Intervention: 26:24 absorbable suture used Infections were more Or mechanical
Control: 35:15 to close the abdominal common in cases of problems in the
Obesity sheath. ruptured appendicitis intervention
Height: cm ,mean Standard preventive (Infected 5/9 vs. Non- group such as
Intervention: 161.5 measures: infected 11/91 strength, knot
Control: 164.0 AMP: Gentamicin 240mg P=0.007) tight and
P=0.039 and metronidazole The rate of SSI was higher anaphylactic
Weight, kg, mean 500mg given in men than in women. allergy.
Intervention: 59.73 intravenously 30-60 (3:2) Follow-up: At day
Control: 59.53 minutes before the 1, 3, 7, 14, and
Comorbidities: NR operation. Risk factors associated 30, and at 6 and
White Blood Cell count, Surgery: appendectomy with infection 12 months
3
cell/mm , mean: done with standard Infected patients tended to Funding Source
Intervention: 16,564 technique, mainly by a be older, with slightly Conflicts:
Control: 15,062 second year physician. higher temperature, higher Authors: None
P=0.036 white blood cell counts, Institution: None
Operative: and slightly longer Study: None
Preop time, operative operative times, but these Supplies: None
time, type of differences were not
appendicitis and degree statistically significantly
of contamination not different.
statistically significant
Type of appendicitis: Appendicitis case type
Intervention/control Suppurative:
Acute: 24/24 Non- infected: 50/91
Suppurative: 56/48 (54.9%)
Gangrene: 6/10 Infected: 2/9 (22.2%)
Ruptured: 14/18 P=0.050
Degree of Ruptured:
contamination: Non-infected: 11/91
2017 American Medical Association. All rights reserved. 295
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Intervention/Control (12.1%)
Mild: 86/80 Infected: 5/9 (55.6%)
Moderate: 8/12 P=0.007
Severe: 6/8
Procedures: Other infections: NR
Appendectomy Topic-specific
Via grid-iron incision: outcomes:
86% Cultures: No Resistance
Indications: Acute and reported
ruptured Intervention: 1 S. aureus
appendicitis. Control: 1 (deep) P.
Uncomplicated: 76% aeruginosa
Acute Reoperations: NR
Intervention: 24% Length of stay: days
Control: 24% (mean)
Suppurative Intervention: 3.7
Intervention: 56% Control: 3.7
Control: 48% P=0.500
Gangrene Infected vs. uninfected.
Intervention: 6% Uninfected: 3.6 days
Control: 10% Infected: 7.4 days
Ruptured P=0.006
Intervention:14%
Control: 18% Mortality: NR (all
Setting: 1 university available for follow-up)
hospital Adverse events: No
Location: Thailand medical complications
Dates: August 2006 during the present
March 2007 study and no
Inclusion Criteria: complications related to
Patients aged 15-60 suture identified after 1
years, both sexes, year of follow-up.
appendicitis
diagnosed
intraoperatively
through a right lower
quadrant incision
and included both
acute and ruptured
2017 American Medical Association. All rights reserved. 296
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
appendix.
Exclusion Criteria:
Patients with
diabetes,
immunocompromise
d host, HIV, on
immunosuppressive
drug, malignancy,
missed diagnosis
intraoperative,
history of allergy to
the substance, or
pregnancy
Rozzelle RCT To determine Number of patients: N Intervention group: n=46 SSI: (follow up 6 Definitions:
80
2008 1, 2, 3, whether = 61 patients with Antimicrobial (triclosan) months) Shunt infection:
nd
(ES) 4, 5, 6, wound closure 84 shunt coated absorbable SSI at 2 interim period diagnosis
7, 8, 9, with triclosan- procedures sutures were utilized to Overall: 10/84 (11.9%) obtained by
10 coated Patient close the subcutaneous Intervention: 2/46 (4.3%) positive culture
absorbable Characteristics: layer around the CSF Control: 8/38 (21%) from CSF
sutures after Groups differed shunt P= 0.038 sampled through
cerebrospinal slightly but no Timing of intervention: There was no statistically the shunt or from
fluid (CSF) significant difference Intraoperatively significant difference explanted shunt
shunt surgery was found in patient Duration of intervention: between historical rate components.
would reduce characteristics, Intraoperatively and either the Perioperative
the incidence shunt type, Device/agent: intervention or control care: NR
of early shunt indication, or which Antimicrobial (triclosan) group rates. Other notes:
infection (<6 surgeon between coated sutures Intervention was No patients were
months groups. Monitoring intervention: associated with lost to follow up.
postoperativel Age median (range): CSF cultures. Absolute risk reduction Patients requiring a
y) 6.3 y (1 day 48 y) Control group: n= 38 0.167 (95% CI 0.027- new shunt within
Gender: male no (%) Standard (uncoated) 0.235) the 6-month
Intervention: 30/46 absorbable sutures Relative risk reduction surveillance
(65%) were utilized to close 3.84 (95% CI 0.257 window were
Control: 18/38 (47%) the subcutaneous layer 18.78) reenrolled in the
P=0.154 around the CSF shunt Predict intervention suture program using
(Distribution unequal (not the same kind of wound closure would the same suture
between groups with material as the prevent 1 shunt infection assignment as
a weak statistical intervention) for every 6.0 procedures in before. Patients
trend towards the which it is used: receiving new
2017 American Medical Association. All rights reserved. 297
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Intervention group Standard preventive Number to treat=6.0; shunts following
for males.) measures: 95%CI 4.2-36.5) successful
Obesity: NA Surgeon Grade: all shunt 8/10 diagnosed w/in 6 treatment of a
weight <4kg procedures performed weeks shunt infection
Intervention: 7/46 by one of two attending 2/10 diagnosed at 12 and and patients
(15%) pediatric 14 weeks postop. undergoing
Control: 6/38 (16%) neurosurgeons. revision >6
Comorbidities AMP: all participants 8/10 (+) CSF cultures months after
Recent CSF infection received preoperative 1/10 blood and distal randomization
Intervention: 6/46 intravenous catheter cultures grew were re-
(13%) antimicrobials same organism (VA randomized.
Control: 3/38 (8%) (cefazolin, or Shunt) Enrollment ceased
Mean shunt procedure vancomycin if allergic to 1/10 (-) CSF culture, (+) at the second
time was slightly cephalosporins) wound purulence over interim analysis
longer in intervention Skin Prep: all patients distal tubing due to a marked
group but not received preoperative Other infections: NR difference in
statistically chlorhexidine skin Topic-specific infection rates
significant. cleansing, povidone- outcomes: between groups.
Procedures: iodine skin prep. 60 shunts (71.4%) No additional shunt
Implantation or Drapes: all surgeries remained functional and infections
revision of utilized iodine- apparently infection free at diagnosed after
implantation for impregnated adhesive 6 months. enrollment
cerebrospinal fluid drapes Pathogenic isolates n=10 ceased
(CSF) shunting Wound irrigation: all SSIs: Follow-up: 6
devices. patients received Intervention: months
Implants: 40 (47.6%) antibiotic wound 1 MRSA Funding Source
Revisions: 44 (53.4%) irrigation prior to 1 coagulase negative Conflicts:
VP Shunt type: 68 closures. (coag neg) Authors: Industry
operations (81%) Shunt cleaning: Silicone Staphylococcus Institution: None
VPI Shunt type: 9 shunt components were Control: Study: None
operations (10.7%) soaked in bacitracin 1 MRSA Supplies: None
Subdural-peritoneal solution before 3 MSSA
shunt: 6 operations implantation. No 3 coag neg Staph spp.
(7.1%) antibiotic-impregnated 1 P. aeruginosa
VA shunts: 1 operation shunt components used Reoperations:
(1.2%) in this study. 10/84 (11.9%) shunts were
Indications: Closure: skin closures for removed due to
hydrocephalus. all procedures infection prior to 6
Setting: 1 hospital performed with month follow up.
2017 American Medical Association. All rights reserved. 298
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Location: USA poliglecaprone 25 14/ 84 (16.7%) Revision
Dates: April 2005 - sutures. procedures w/in 6 mo
December 2006. where infection was not
Inclusion Criteria: suspected. (Shunt tap
Patients of all ages CSF cultures remained
requiring CSF shunt negative)
implantation or 2/84 (2.4%) revision
revision surgery. procedures >6mo
Exclusion Criteria: postop.
Patients receiving Reasons for revisions NR
ventricular access 7/61 (11.5%) patients
devices or receiving new shunts
ventriculosubgaleal were re-randomized
shunts, patients with after removal of an
active shunt infected shunt that had
infections, and been placed during the
immunocompromise study and appropriate
d patients. antimicrobial therapy
Wounds cultured, MRSA:
1/2 (50%) vs. 1/8
(12.5%) both in revision
surgeries
MSSA: 0/2 vs. 3/8 (37.5%)
all in primary implant
surgeries
Length of stay: NR
Mortality: 2 patients with
shunt infections died
(3.3%). Both were
infants with severe
congenital anomalies
whose parents
ultimately decided to
withdraw care.
Adverse events:
All shunt infections treated
with complete shunt
removal, external
2017 American Medical Association. All rights reserved. 299
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
ventricular drainage,
and appropriate
intravenous
antimicrobial therapy
until daily CSF cultures
remained negative for
5 days, followed by
the replacement of a
new shunt.
Ford RCT To Number of patients: Intervention group: n= SSI: (follow up 80 days) Definitions:
81
2005 1, 4, 5, characterize N=147 98 Infection Day 1-2 Infection: observed
(ES) 7, 8, 9 further the Patient Antimicrobial (triclosan) Intervention: 0% redness >3-5
clinical Characteristics: no coated absorbable Control: 0% mm from the
performance differences in suture was used as Infection Day 14 wound margins,
of baseline suture of various sizes Intervention: 2% edema
antimicrobial characteristics dependent on surgery Control: 0% (characterized
(triclosan) between groups. Timing of intervention: Infection Day 80 by increased
coated Age, y: mean (range): Intraoperatively Intervention: 1% tissue firmness),
absorbable 9.8 y (1-18) Duration of intervention: Control: 0% purulent
suture and Gender: 52% male Intraoperatively Edema, any day 1 discharge, pain,
traditional Obesity: NR Device/agent: Triclosan- Intervention: 10% and increased
non- Mean Height: 137.2 cm coated absorbable Control: 18% skin
antimicrobial (range 67-191 cm) suture. Edema, any Day 14 temperature.
coated Mean Weight: 41.3 kg Monitoring intervention: Intervention: 3% Confirmatory
absorbable (range 8-130 kg) NR Control: 2% culture was not
suture in Comorbidities Control group: n=49 Edema, any Day 14 required.
pediatric Risk factors that could Non-antimicrobial coated Intervention: 0% FLACC behavior
patients affect wound healing absorbable suture was Control: 3% pain assessment
undergoing were present in used as suture of Erythema Day 1 scale was used
various similar proportion: various sizes Intervention: 9% in non-verbal
general individual results by dependent on surgery Control: 7% patients (infants)
surgical risk factor not Erythema Day 14 unable to
procedures. reported Standard preventive Intervention: 9% provide reports
Intervention 29% measures: NR Control: 2% of pain. (face,
Control: 33% Non-Standard Preventive Erythema Day 80 legs, activity,
The most common Measures: Intervention: 1% cry,
risk factors were Perioperative antimicrobial Control: 3% consolability)
obesity and administration: Other infections: 3 Intraoperative
chemotherapy Intervention: 24% infections developed handling:
2017 American Medical Association. All rights reserved. 300
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Actual numbers not Control: 31% and judged not to be overall, ease of
reported related to the suture. passage, first
Received IV 1/3: Day 14 a 13 year old throw, tie-down,
antimicrobials (they male undergoing security, hand,
do not specify if pilonidal cystectomy memory, and
AMP or AMP and developed a new sinus non-fraying.
treatment) tract that was related to Perioperative
Intervention: 65% the location of the cyst care: NR
Control: 82% 1/3: on day 14, a 14-year Other notes:
Taking other old female who had Patient population
medications undergone laparoscopic at each wound
Intervention: 5% cholecystectomy evaluation:
Control: 10% developed a superficial 1-2 days:
Procedures: NR fungal rash around the Intervention: 88
(variable) umbilicus that was Control:45
Indications: NR believed to be due to 14 days:
(variable) body habitus. Intervention: 91
Setting: 1 center 1/3: day 80, a 14 year old Control:44
Location: USA female patient who 80 days
Dates: NR underwent a pilonidal Intervention: 76
Inclusion Criteria: cystectomy developed Control:38
Pediatric patients a new sinus tract distal
aged 1-18 years to the original site of Follow-up: Wound
undergoing clean or excision that was filled healing
clean-contaminated with hair (most likely evaluated at
general surgical represented a new follow-up visits
procedures. lesion) at 1-2 days, 14
Exclusion Criteria: Topic-specific (2) days and 80
Contaminated outcomes: (5) days post-
wound sites; use of Intraoperative handling: implantation.
retention sutures; Overall: Funding Source
inappropriate age; Intervention mean 71% Conflicts:
evidence of Control mean 59% Authors: Industry
malnutrition or Both sutures>94% very Institution: NR
debilitation; good or excellent Study: Industry
coexisting conditions Not statistically significant Supplies: NR
that may impair Specific:
wound healing Excellent
including acquired Intervention mean 75%
2017 American Medical Association. All rights reserved. 301
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
immunodeficiency Control mean 62%
syndrome (AIDS); Both sutures>94% very
incision sites prone good or excellent
to expand, stretch, Not statistically significant
distend, or require Pain Day 1
support; ophthalmic, Intervention: 68%
cardiovascular, or Control: 89%
neurologic surgical P=0.01
sites; a need for Pain Day 14
more than one Intervention: 12%
surgical procedures; Control: 9%
prior participation in Pain Day 80
this study; or allergy Intervention: 3%
to triclosan. Control: 0%
Reoperations:
Adverse events requiring
surgery
Intervention: 17/98 (17%)
Control: 10/49 (20%)
Length of stay: NR
Mortality: NR
Adverse events:
The most common events
consisted of admissions
for chemotherapy.
Any Adverse Events:
Intervention: 17/98
(17%)
Control: 10/49 (20%)
Severe Adverse Events:
Intervention: 1/98 (1%)
Control: 1/49 (2%)
Serious Adverse Events:
Intervention: 13/98
(13%)
Control: 8/49 (16%)
Requiring Surgery: 17/98
(17%) vs. 10/49 (20%)
Device Related: 0/98 vs.
2017 American Medical Association. All rights reserved. 302
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
0/49
Day 1 Antimicrobials
received:
Intervention: 24%
Control: 31%
Day 14 Antimicrobials
received:
Intervention: 13%
Control: 23%
Day 80 Antimicrobials
received:
Intervention: 22%
Control: 29%
Received other
medications that could
impede wound healing:
Day 1
Intervention: 10%
Control: 13% (not
significant)
Day 14
Intervention: 14%
Control: 14%
Day 80
Intervention: 12%
Control: 21%
Suture sinus: none
2017 American Medical Association. All rights reserved. 303
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
eTABLE 34. Evidence Table for Q2D. How safe and effective are antimicrobial dressings applied to surgical incisions
following primary closure in the operating room?
Author
Study
Year
Design Study Population and
(Data Intervention Results Comments
Quality Objective Setting
Extrac-
Score
tor)
Biffi RCT To compare the Number of patients: Intervention group: n=58 SSI (30 days) Definitions:
83
2012 1, 2, 3, efficacy of a N=112 Surgical incision was Overall: 20/112 (17.9%) SSI: CDC
(ES) 4, 5, 6 sterile moisture Patient dressed with a sterile Intervention: 9/58 Definitions
7, 8, 9 retentive Characteristics: moisture retentive (15.5%) Perioperative
dressing with patients were similar dressing with 1.2% Control: 11/54 (20.4%) care: NR
1.2% iconic with regards to their iconic silver covered by P=0.623 Other notes: NR
silver with that demographic a self-adherent Superficial SSI Follow-up: 30
of a common characteristics breathable dressing. Overall: 13/112 (11.6%) days
postoperative between groups. Timing of intervention: Intervention: 5/58 (8.6%) Funding Source
dressing for Age, y: mean SD postoperative Control: 8/54 (14.8%) Conflicts:
preventing Intervention: 63.69.2 Duration of intervention: P=0.802 Authors: None
th
SSIs in elective Control: 62.99.0 removed 7 Deep SSI Institution: NR
colorectal Gender: female postoperative day Overall: 5/112 (4.5%) Study: Industry
cancer surgery. Intervention: 22 Device/agent: sterile Intervention: 3/58 (5.2%) Supplies: NR
(37.9%) moisture retentive Control: 2/54 (3.7%)
Control: 25 (46.3%) dressing with 1.2%
Obesity: BMI iconic silver Organ/space SSI
MeanSD Monitoring intervention: Overall: 2/112 (1.8%)
Intervention: 25.74.3 NR Intervention: 1/58 (1.7%)
Control: 25.44.4 Control group: n=54 Control: 1/54 (1.9%)
Comorbidities Surgical incision was
Procedures: colorectal dressed with a self- Other infections:
cancer surgery adherent breathable Infection within 30 days
rectal: dressing which was Overall: 14/112 (12.5%)
Intervention: 17/58 then covered by Intervention: 6/58
(29.3%) another self-adherent (10.3%)
Control: 18/54 breathable dressing to Control: 8/54 (14.8%)
(33.3%) maintain blinding P=0.802
P=0.687 Standard preventive
measures: Topic-specific
Indications: colorectal AMP: 30 minutes before outcomes: NA
cancer initial incision. Reoperations: NR
Setting: Two Skin prep; preoperative Length of stay: NR
university-affiliated scrub and paint with Mortality: NR
hospitals 10% povidone-iodine; Adverse events: None
Location: Italy Mechanical bowel prep: all related to this study
Dates: June 2008 - patients received it
2017 American Medical Association. All rights reserved. 304
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author
Study
Year
Design Study Population and
(Data Intervention Results Comments
Quality Objective Setting
Extrac-
Score
tor)
September 2010
Inclusion Criteria:
Patients aged 18-75
years old undergoing
elective colorectal
cancer surgery by
laparotomic
approach.
Exclusion Criteria:
History of allergy to
dressing
components,
evidence of active
infection at or
adjacent to the
operative site,
coagulopathy
(defined as platelet
count less than
50,000 cells/ L or a
prothrombin time
>18 seconds),
intestinal
obstruction, active
bowel bleeding, life
expectancy less than
6 months, inability to
give written informed
consent or a
program of minimally
invasive surgery
(laparoscopy or
robot-assisted)
Krieger RCT To conduct a Number of patients: Intervention group: n=55 SSI Definitions:
84
2011 1, 2, 7, prospective, N=109 Silver nylon dressing, Total SSI: CDC
(ES) 8, 9 randomized, Patient hydrated in sterile water Intervention: 7/55 (13%) Definitions.
controlled trial Characteristics before application. Control: 18/54 (33%) Superficial incision
directly Age, y: median Instructions were to P=0.011 definition was
comparing Intervention: 62 rehydrate the dressing Superficial modified to
2017 American Medical Association. All rights reserved. 305
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author
Study
Year
Design Study Population and
(Data Intervention Results Comments
Quality Objective Setting
Extrac-
Score
tor)
silver nylon Control: 58 daily and then replace Intervention: 5/55 (9%) include all
with standard P=0.49 with a new dressing Control: 14/54 (26%) patients who
gauze Gender: female: after 7 days. On P=0.021 were placed on
dressings in Intervention: 27/55 discharge patients had Deep antibiotics
patients (49%) a new dressing applied Intervention: 2/55 (4%) specifically for
undergoing Control: 28/54 (52%) that remained for an Control: 4/54 (7%) these signs or
elective Obesity: NR additional 7 days. P=0.438 symptoms.
colorectal Comorbidities Timing of intervention: Perioperative
operations. Diabetes mellitus: postoperative Other infections: NR care: NR
Intervention: 5/55 Duration of intervention: Topic-specific Other notes: NR
(9%) Device/agent: silver nylon outcomes: NR Follow-up: 30
Control: 4/54 (7%) wound dressing Reoperations days
P=1.00 Monitoring intervention Debridement Funding Source
Transfusion: Control group: n=54 Intervention: 0/55 Conflicts:
Intervention: 7/55 Incisions were dressed Control: 2/54 (4%) Authors: None
(13%) only with sterile gauze P=0.234 Institution:
Control: 0 /54 and paper tape. On Industry
P=0.013 discharge, patients Length of stay: median Study: Industry
instructed to replace (range) Supplies: NR
Procedures: elective their dressings as Intervention: 6 (3-21)
colorectal surgery. needed. days
Indications: Standard preventive Control: 6.5 (2-17) days
Neoplastic, IBD, measures: P=0.210
Other Food restriction: clear Mortality: NR
Setting: One liquid diet 24 hours Adverse events: NR
university-based before surgery.
hospital Mechanical Bowel Prep
Location: USA not used with the
Dates: July 2009 exception of patients
April 2010 undergoing left colon or
Inclusion Criteria: rectal surgery, who
Patients undergoing were given an enema
elective colorectal the morning of their
surgery with operation.
anticipated Antimicrobial prophylaxis:
abdominal incision of 30-60 minutes prior to
at least 3cm. surgery. Standard
Exclusion Criteria: coverage is ertapenem.
Incision <3cm, Patient with penicillin
2017 American Medical Association. All rights reserved. 306
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author
Study
Year
Design Study Population and
(Data Intervention Results Comments
Quality Objective Setting
Extrac-
Score
tor)
known allergy to allergies given
silver, signs of alternative prophylaxis
abdominal wall with ciprofloxacin and
infection, conditions flagyl or gentamicin and
that would prevent clindamycin. All
full closure of the perioperative antibiotics
skin at the primary discontinued within 24
operation, or prior hours.
abdominal mesh that
was not planned to
be fully removed at
the time of
operation. Pregnant
or lactating women
and patients who
had received
antibiotics within 1
week of surgery also
excluded.
2017 American Medical Association. All rights reserved. 307
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.1B3. RISK OF BIAS ASSESSMENTS OF STUDIES: Q2 NON-PARENTERAL AMP
eTABLE 35. Risk of Bias Assessments of Randomized Controlled Trials for Q2 Non-Parenteral AMP
Funding
Randomiza- Outco- Attrition source(s)
Describ- tion Describ- me smaller than Attrition disclosed and
ed as appropriat- ed as asses- Study Investiga- Attrition 10-15% of appropria- no obvious Overa-
Author randomiz ely double- sor participa- tor describ- assigned tely conflict of ll Risk
Year Q ed performed blind blinded nt blinded blinded ed patients analyzed interest of Bias
Question 2: Non-Parenteral Antimicrobial Prophylaxis
Almdahl Mode-
64 2
2011 rate
Al-Sheri Mode-
57 2
1994 rate
Baracs Mode-
71 2
2011 rate
Biffi
83 2 Low
2012
Diener
77 2 Low
2014
Dorge
67 2 High
2013
Ford
81 2 Low
2005
Galal
76 2 Low
2011
Isik Mode-
79 2
2012 rate
Justinger
75 2 Low
2013
Juul Mode-
58 2
1985 rate
Kamath
61 2 Low
2005
Krieger Mode-
84 2
2011 rate
Litmathe Mode-
66 2
2009 rate
Mingmalai-
rak 2 Low
78
2009
Nakamura
74 2 Low
2013
Neri 2 Mode-
2017 American Medical Association. All rights reserved. 308
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Funding
Randomiza- Outco- Attrition source(s)
Describ- tion Describ- me smaller than Attrition disclosed and
ed as appropriat- ed as asses- Study Investiga- Attrition 10-15% of appropria- no obvious Overa-
Author randomiz ely double- sor participa- tor describ- assigned tely conflict of ll Risk
Year Q ed performed blind blinded nt blinded blinded ed patients analyzed interest of Bias
62
2008 rate
Peerboo-
ms 2 Low
65
2009
Raahave Mode-
60 2
1989 rate
Rasic Mode-
70 2
2011 rate
Rozzelle
80 2 Low
2008
Ruiz-
Tovar 2 Low
56
2012
Seco Mode-
59 2
1990 rate
Seim Mode-
69 2
2012 rate
Thimour-
Bergstrom 2 Low
73
2013
Turtiainen
68 2 Low
2012
Vander
Salm 2 High
63
1989
Williams
72 2 Low
2011
2017 American Medical Association. All rights reserved. 309
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.1C. Q3 GLYCEMIC CONTROL
2.1C1. GRADE TABLE: Q3 GLYCEMIC CONTROL
eTABLE 36. GRADE Table for Q3 Glycemic Control
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
Dose-response
Quantity GRADE of Overall
Study Quality
Confounders
Consistency
Directness
Precision
and Type Starting Evidence GRADE of
Comparison Outcome Findings
of GRA-DE for Evidence
Evidence Outcome Base
Q3. How do perioperative blood glucose and hemoglobin A1C levels impact the risk of SSI and what are their optimal perioperative target levels in
diabetic and non-diabetic patients?
Two RCTs in 480 cardiac surgery
predominantly non-diabetic (70%-80%)
populations. Glycemic control protocol
instituted intraoperative and postoperatively in
the SICU for 24-36 hours. Both RCTs report a
primary composite outcome variable that
includes SSI (underpowered to detect
differences in individual outcomes).
1 large (N=371) and one small (N=109)
85 86
RCT, comparing strict (80-100mg/dL) to
standard (<200mg/dL) glycemic control found
Strict no difference in either the composite outcome
glycemic variable which included SSI: RR 1.0 (0.8-1.2);
2 RCT Moderat
control vs. 85,86 p=0.71 (adjusted OR: 0.09 (0.6-1.4); p=0.68; Moderate
SSI* High 0 0 -1 0 0 0 0 0 e
standard or in deep sternal SSIs: RR 0.9 (95%CI, 0.3-
glycemic 2.5); p=0.79. In subanalyses of separate
control diabetic (n=73) and non-diabetic (n=298)
populations, no difference was noted between
groups for either the composite (p=0.40) or
deep sternal SSI (p=0.61) variables. The
study could not examine whether outcomes
differed by diabetes status.
1 small RCT (N=109), comparing strict (80-
86
130mg/dL) to standard (160-200mg/dL)
glycemic control found no difference in either
the composite infection outcome variable:
19.2% vs. 35.3%; p=0.12.and no difference in
SSIs: 11.1% vs. 16.7%; p=0.09.
2017 American Medical Association. All rights reserved. 310
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
Dose-response
Quantity GRADE of Overall
Study Quality
Confounders
Consistency
Directness
Precision
and Type Starting Evidence GRADE of
Comparison Outcome Findings
of GRA-DE for Evidence
Evidence Outcome Base
1 large RCT defined hypoglycemia as
85
<60mg/dL, reported it as number of episodes
in each treatment group. While the study
found no difference between groups for
hypoglycemic episodes in the SICU, it did find
that for both groups a higher proportion of the
episodes occurred in the SICU: 8 (4%) vs. 14
(8%); p=1.00, RR 1.01 (0.06-15.95) as
Hypo- 2 RCT compared to intraoperatively: 1 (1%) vs. 1 High
85,86 High 0 0 0 0 0 0 0 0
glycemia* (1%); p=0.19, RR 1.76 (0.76-4.09).
1 small RCT defined hypoglycemia as
86
<50mg/dL and reported it as the ratio of
hypoglycemic episodes per number of glucose
measurements. It also noted no difference
between groups for hypoglycemic episodes:
2.9% vs. 2.1%, (0.84-1.43); p=0.67.
Neither study reported clinical complications
resulting from hypoglycemia.
Mortality was rare, reported only in the strict
85 glycemic control group, and not associated
Mortality 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
with blood glucose target levels: 4/185 vs.
0/186.
Length of hospital stay (p=0.66) and length of
Length 85
1 RCT SICU stay (p=0.37) were not associated with High 0 0 0 -1 0 0 0 0 Moderate
of stay
blood glucose targets.
*Critical outcome; OR: Odds Ratio; RR: Risk Ratio; CI: Confidence Interval
2017 American Medical Association. All rights reserved. 311
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.1C2. EVIDENCE TABLE: Q3 GLYCEMIC CONTROL
eTABLE 37. Evidence Table for Q3. How do perioperative blood glucose and hemoglobin A1C levels impact the risk of SSI and
what are their optimal perioperative target levels in diabetic and non-diabetic patients?
Study
Author
Design
Year Study Population and Setting
Risk of Intervention Results Comments
(Data Objective (N)
Bias
Extractor)
Score
Chan RCT To Number of patients: Intervention group SSI Definitions:
86
2009 1, 5, 7, 10 investigate N=109 (intensive) n=54 Intervention: 11.1% Hypoglycemia: Defined as
(ES) whether Patient Characteristics: Intervention: 80 -130mg/dL Control: 16.7% <50mg/dL
different the groups were glucose P=0.09
targets of comparable with Timing of intervention: Perioperative care:
intraoperativ respect to age, gender perioperative Other infections: NR parenteral care was not
e and and height. Duration of intervention: Topic-specific outcomes: prescribed for any patients
postoperativ Age: NR from arrival in OR until36h Hypoglycemia in the study.
e glucose Gender: NR postop Reported as: hypoglycemic Other notes: authors
(80-130 Obesity: BMI Device/agent: Glucose episodes per number of indicate that 11 patients
mg/dl, 4.4- Intervention: 24 (3.4) Monitoring intervention: glucose measurements were lost to follow up and
7.2 mEq/l or Control: 26 (4.9) Measurements of whole 2.9% vs. 2.1% P=0.67 (0.84- may have biased the
160-200 Comorbidities: blood glucose in undiluted 1.43) results AND this pilot
mg/dl, 8.8- ASA status P4: arterial blood every 1-4h study sample size was not
11.1 mEq/l) Intervention: 70.2% using a glucose analyzer. Reoperations: NR large enough to allow for
could affect Control: 86.3% Glucose dose was adjusted Length of stay: (days) any definite conclusions or
postoperativ Length of CBP (min) by ICU nurses according to Intervention: 12 (7) recommendations on the
e clinical Intervention: 97.9 a titration algorithm (Leuven Control: 17 (16) effect of strict glucose
outcomes (45.3) modified). algorithm given P= 0.060 (0.24-1.01) control vs. less intensive
after cardiac Control: 116.3 (54) as guidance rather than control
surgery with P=0.060 exact targets Mortality: (%) Follow-up: 30 days
cardiopulmo Procedures: Open-heart Control group: (less Intervention: 6.4% Funding Source Conflicts:
nary bypass. surgery requiring intensive) n=55 Control: 5.9% Authors: None
cardiopulmonary Control: 160-200mg/dL Institution: None
bypass (CBP). glucose Adverse events: Study: None
Indications: NR No clinical complications Supplies: None
Setting: 1 university Standard preventive reported resulting from
hospital measures: hypoglycemia at follow up (30
nd
Location: Brazil AMP: 2 generation days).
Dates: NR (over a period cephalosporin
of 12 months) Transfusion threshold:
Inclusion Criteria: adults hematocrit<30%
from both genders who
were older than 21
years of age and who
2017 American Medical Association. All rights reserved. 312
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and Setting
Risk of Intervention Results Comments
(Data Objective (N)
Bias
Extractor)
Score
were undergoing open-
heart cardiac surgery
requiring CBP.
Exclusion Criteria: (1)
renal failure
(creatinine>1.5g/dl), (2)
neurological dysfunction
(diagnosis from medical
records), (3) chronic
pulmonary obstructive
disease (COPD), (4)
current use of any type
of antimicrobial, (5)
current use of inotropic
support, (6) emergency
and urgent surgeries,
and (7) reoperations.
Ghandi RCT To Number of patients Intervention group: n=185 Definitions:
85
2007 1, 4, 5, 7, determine N=371 Intraoperative glycemic OR: 0.9, 95%CI (0.3-2.5) Primary outcome =
(ES) 8 whether Patient Characteristics: control of 80mg/dL P=0.79 composite of death, sternal
maintenance Baseline characteristics 100mg/dL (4.4mmol/L 5.6 Other infections: NR wound infections,
of near did not differ statistically mmol/L) Topic-specific outcomes: prolonged pulmonary
normoglyce significantly between Hypoglycemia ventilation, cardiac
mia during groups. Timing of intervention: Intraoperative (1 patient in each arrhythmias, stroke, and
cardiac Age: NR intraoperative group) acute renal failure within
surgery by Gender: NR Duration of intervention: RR 1.01 (95%CI 0.06-15.95) 30 days postop.
using Obesity: NR intraoperative only Postoperative (ICU): Hypoglycemia: glucose
intraoperativ Comorbidities: Device/agent: Glucose Intervention: 14 (8%) <60mg/dL;
e 20% had known diabetes Monitoring intervention: Control: 8(4%) Perioperative care : NR
intravenous Arterial blood glucose levels RR 1.76 (95% CI 0.76-4.09) Other notes: this single
insulin Procedures: were measured with a All mild without adverse center study used a
infusion Cardiopulmonary glucometer. consequences composite end point and
reduced bypass surgery Control group: n=186 could not examine whether
perioperative Indications: NR Intraoperative glycemic Reoperations: NR outcomes differed by
death and Setting: 1 tertiary care control target of <200mg/dL Length of stay: diabetes status.
morbidity teaching hospital (11.1mmol/L) if glucose median and mean LOS in Primary outcome variable
when added Location: USA level reached >250mg/dL hospital and ICU P=-.66 and was a composite variable
to rigorous Dates July 2004 April (13.9mmol/L), then p=0.37 because not feasible to
postoperativ 2005 intraoperative bolus was Mortality: power study to detect
2017 American Medical Association. All rights reserved. 313
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and Setting
Risk of Intervention Results Comments
(Data Objective (N)
Bias
Extractor)
Score
e glycemic Inclusion Criteria: Adults given until level was less Overall& In hospital differences in individual
control. undergoing elective than 150mg/dL (8.3mmol/L) 4/185 (2%) vs. 0% components such as
cardiac surgery during Post discharge (up to 30d death, because the rare
study dates Standard preventive postop) occurrences would
Exclusion Criteria: measures: 0% vs. 0%; P=0.061 mandate a very large
Patients who had off- Both groups had strict NOTE: POST DISCHARGE F/U sample size.
pump cardiopulmonary postoperative glycemic in only 4% vs. 5% of patients Follow-up: 30 days
bypass procedures. control of 80mg/dL Funding Source Conflicts:
100mg/dL) Adverse events: None reported Authors: Industry
Institution: NR
Study: NR
Supplies: NR
2.1C3. RISK OF BIAS ASSESSMENTS: Q3 GLYCEMIC CONTROL
eTABLE 38. Risk of Bias Assessments of Randomized Controlled Trials for Q3 Glycemic Control
Funding
Attrition source(s)
Described Randomizati- smaller than disclosed and
as on Described Outcome Study 10-15% of Attrition no obvious Overall
Author randomize- appropriately as double- assessor participant Investigato Attrition assigned appropriate- conflict of Risk of
Year Q ed performed blind blinded blinded blinded described patients ly analyzed interest Bias
Question 3: Glycemic Control
Chan
86 3 High
2009
Gandhi
85 3 High
2007
2017 American Medical Association. All rights reserved. 314
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.1D. Q4-5 NORMOTHERMIA
2.1D1. GRADE TABLE: Q4-5 NORMOTHERMIA
eTABLE 39. GRADE Table for Q4-5 Normothermia
Increase
Decrease GRADE
GRADE
Publication Bias
Dose-response
Quantity GRADE of Overall
Study Quality
Confounders
Consistency
Directness
Magnitude
Precision
and Type Starti-ng Evidence GRADE of
Comparison Outcome Findings
Large
Of GRA-DE for Evidence
Evidence Outcome Base
Q4. How safe and effective is the maintenance of perioperative normothermia in reducing the risk of SSI?
Meta-analysis of 2 RCT (N=616) found
that maintenance of normothermia
associated with reduced risk for SSI (OR:
2
0.29; 95% CI: 0.16 0.53; p<0.0001; I =0)
Mixed surgical populations, multiple
warming techniques
Maintenance of perioperative
normothermia with warming techniques
associated with reduced risk of surgical
2 RCT
SSI* 87,88 site infection High 0 0 0 0 0 0 0 0 High
1 RCT in 416 patients undergoing
87
elective hernia repair, varicose vein and
breast surgery, preoperative systemic
warming only : 13/277 (5%) vs. 19/139
Warming vs. (14%); p<0.01 at 2-6 week follow up High
1 RCT in 200 elective colorectal surgery
88
no warming
patients using intraoperatively only
warming: 6/104 (6%) vs. 18/96 (19%);
p<0.01 at 2 week follow up.
ASEPSIS wound scores were higher in
87 88
control groups (p<0.01 )
In a meta-analysis of the two studies,
ASEPSIS 2 RCT
87, 88 warmed patients were less likely to have High 0 0 0 0 0 0 0 0 High
score
ASEPSIS wound scores >20 (Relative
Risk: 0.19; (95% CI, 0.09 0.39); p<0.01;
2
I =26%
Mortality within 30 days was rare (4
Mortality, 88
1 RCT deaths in 200 patients), with no difference High 0 0 0 -1 0 0 0 0 Moderate
30 days
observed between groups
2017 American Medical Association. All rights reserved. 315
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Publication Bias
Dose-response
Quantity GRADE of Overall
Study Quality
Confounders
Consistency
Directness
Magnitude
Precision
and Type Starti-ng Evidence GRADE of
Comparison Outcome Findings
Large
Of GRA-DE for Evidence
Evidence Outcome Base
Normothermia associated with lower
mean units of blood transfused per
88
Blood Loss 1 RCT patient: 0.41.0 vs. 0.81.2; p=0.01 and High 0 0 0 -1 0 0 0 0 Moderate
fewer patients transfused: 23/104 (22%)
vs. 34/96 (35%)
1 RCT found that core temperature was
87
increased by either local or systemic
warming techniques, delivered pre-
operatively for 30 minutes. The impact of
systemic warming (mean increase: 0.35
C; p<0.01) was greater than local
Core
2 RCT warming (mean increase: 0.13 C;
Temperatu- 87,88 High 0 0 0 0 0 0 0 0 High
p=0.03). The mean core temperature after
re
surgery was within normal limits.
1 RCT found that core temperature at
88
end of surgery was increased with
intraoperative systemic warming (p<0.01),
and remained higher for more than 5
hours following surgery
Normothermia associated with reduced
Length of
88 length of stay (net reduction: 2.6 days;
Hospital 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
p<0.01); difference remained when
Stay
analysis was limited to uninfected patients
Duration of 2 RCT Normothermia not associated with
87,88 High 0 0 0 0 0 0 0 0 High
Surgery increased duration of surgery
Warming: Perioperative warming associated with
perioperative decreased incidence of SSI (12.8% vs.
89
SSI* 1 RCT 26.8%), but this finding was not significant High 0 0 0 -1 0 0 0 0 Moderate
(carbon polymer
mattress [2hours OR 0.4 (0.14-1.13); p=0.08; sample size
based on all complications Moderate
preop, intraop,
and 2 hours
postop], forced 89 3 deaths in 103 patients, with no
Mortality 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
air warming and difference observed between groups
2017 American Medical Association. All rights reserved. 316
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Publication Bias
Dose-response
Quantity GRADE of Overall
Study Quality
Confounders
Consistency
Directness
Magnitude
Precision
and Type Starti-ng Evidence GRADE of
Comparison Outcome Findings
Large
Of GRA-DE for Evidence
Evidence Outcome Base
fluid warmer Perioperative warming associated with
89
intraop) Blood Loss 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
lower blood loss (p<0.01)
vs.
intraoperative Perioperative systemic warming group,
only (carbon higher core temperature achieved
polymer immediately after 2 hours of preoperative
mattress, forced Core warming (p<0.01)
89
air warming and Temperatu- 1 RCT Perioperative systemic warming group High 0 0 0 -1 0 0 0 0 Moderate
fluid warmer) re maintained higher core temperature
during the first 90 minutes of surgery
(median 36.2 vs. 36.1) but not at 2 hours
postoperatively (p=0.47)
Length of
89 Perioperative warming not associated with
Hospital 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
reduced length of hospital stay (p=0.22)
Stay
Perioperative systemic warming was not
Duration of 89
1 RCT associated with increased duration of High 0 0 0 -1 0 0 0 0 Moderate
Surgery
surgery (p=0.15)
Q5. What are the most effective strategies for achieving and maintaining perioperative normothermia? Our search did not identify RCTs or SRs that evaluated
the most effective strategies for achieving and maintaining perioperative normothermia and their impact on the risk of SSI.
*Critical outcome; OR: Odds Ratio; RR: Risk Ratio; CI: Confidence Interval
2017 American Medical Association. All rights reserved. 317
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.1D2. EVIDENCE TABLE: Q4-5 NORMOTHERMIA
eTABLE 40. Evidence Table for Q4. How safe and effective is the maintenance of perioperative normothermia in reducing the
risk of SSI?
Author Study
Year Design Study Population and
(Data Intervention Results Comments
Risk of Objective Setting (N)
Extractor) Bias Score
Wong RCT To examine No. patients: N=103 Intervention: n=47 SSI Definitions:
89
2007 1, 2, 4, 6, the effects of Patient Mattress warmed to Intervention: 6/47(12.8%) SSI- CDC: (1) when pus could
(SIBT) 7, 8, 9 extending Characteristics: 40C 2 hours before Control: 15/56 (26.8%) be expressed from the surgical
systemic (age, sex, ASA surgery, during surgery, Other Infections incision or aspirated from a
warming score, MBI, and for 2 hours after Chest infection loculated mass inside the
duration to POSSUM scores, surgery in addition to Intervention: 2/47 (4.3%) wound (2) if the pus culture was
include pre- baseline standard practice of Control: 6/56 (10.7%) positive for pathogenic bacteria
and temperature, pulse systemic warming with Urinary tract infection: (3) if there was localized
postoperative rate and mean forced air warming Intervention: 3/47 (6.4%) tenderness, localized swelling,
periods and arterial pressure device set at 40C and Control: 2/56 (3.6%) redness or temperature at the
the potential were similar in both with a fluid warmer Topic specific outcomes surgical site, or (4) if the
benefits in groups/not Timing of Intervention: median (range) ; P value treating medical practitioners
reducing statistically pre, intra and post Core Temperature had diagnosed them as infected
postoperative significant except for operatively. Immediately after preoperative and treated them with
complications core temperature Duration of systemic warming: antimicrobials.
in patients before start of intervention : 2h Intervention 36.4 (35.1-37.4) Hypothermia: <36C
undergoing surgery (see results) preoperatively, Control: 36.0 (35.1-36.9) Normothermia: 36C
elective major Age: 18years of intraoperatively and 2 P <0.001 Perioperative care:
abdominal age hours post operatively Intraoperative: 90 minutes Anesthesia: Fentanyl and
surgery.. Median (range) Device: conductive Interventions group vecoronium bromide. Isoflurane
Intervention:62.0 carbon polymer mattress maintained a significantly (in 60% nitrous oxide) titrated to
(24-88) can provide sustained higher temperature during the maintain MAP within 20% of
Control: 60.5 (20-84) heat up to 40C. first 90 minutes of surgery pre-induction values. Additional
Gender: m/f Monitoring: (median 36.2) vs. controls fentanyl at end to improve
Intervention: 24/23 Pre and postoperatively: (36.1). analgesia.
Control: 29/27 before and immediately Core Temperature Postop Other notes: NR
BMI: median (range) after surgery tympanic (2hours): Follow up: every day during
Intervention: thermometer Intervention: 36.3 (34.3-38.1) hospitalization and at 6-8
23.0(15.5-39.2) Intraoperative: Control: 36.2 (34.3-37.9) weeks postoperatively (usually
Control: nasopharyngeal P=0.471 in the home)
25.0 (16.5-36.3) temperature probe Blood loss (ml): Mean (range) Funding Source Conflicts:
ASA score (every 30 minutes) Intervention: 200 (5-1000) Authors: NR
ASA1:29/103 Control: n=56 Control: 400 (50-2300) Institution: NR
(28.2%) Mattress warmed to P=0.011 Study: NR
ASA2: 50/103 40C only during surgery All other outcome variables (IV Supplies: NR
(38.5%) in addition to standard fluids, urine output, blood
2017 American Medical Association. All rights reserved. 318
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
(Data Intervention Results Comments
Risk of Objective Setting (N)
Extractor) Bias Score
ASA3:24/103 practice of systemic transfusion units (none),
(23.3%) warming with forced air duration of antimicrobials,
More than 75% of warming device set at flatus passed, bowels opened,
procedures 40C and with a fluid diet tolerated, duration of
performed by warmer hospital stay and follow up)
consultant (senior) Standard Preventive showed no statistically
surgeon Measures significant difference
Procedure: Elective AMP- not described Reoperations: NR
major abdominal AMP duration: mean Length of Stay: mean
surgery (range) (range); P value
Right Intervention:1 (0-28) Intervention: 11.0 (5-119)
hemicolectomy Control: 2(0-12) Control: 9.0 (5-40)
n=31 P=0.200 P value 0.217
Anterior resection Bowel Prep-not Mortality- 1 (surgical
n=24 described emphysema from intubation
Indications: complication) vs. 2 (renal &
Colorectal cancer respiratory failure) (P=0.566)
n=71 Inflammatory Adverse events:
bowel disease n=15 Total Number of Adverse
Diverticular disease events:
n=7 Gastric Intervention: 15/47 (32%)
carcinoma n=3 Control: 30/56 (54%)
Benign colonic P=0.027
tumor n=2 Others Ileus 7/103 (14.9%)
n=5 Pelvic collection 3/103 (2.9%)
Setting: 1 university Cardiac complications 2/47
hospital (4.3%)
Location: United Renal Failure 2/47(4.3%)
Kingdom Anesthetic complications
Dates: October 1/47(2.1%)
2002 to December Clostridium difficile diarrhea
2003 1/47(2.1%)
Inclusion criteria: Pressure ulcer 1/47(2.1%)
major open For SSI, chest infection and
abdominal surgery urinary tract infection see
requiring bowel Other Infections above
resection, with or
without anastomosis .
Exclusion criteria:
2017 American Medical Association. All rights reserved. 319
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
(Data Intervention Results Comments
Risk of Objective Setting (N)
Extractor) Bias Score
laparoscopic
procedures, use of
corticosteroids or
other
immunosuppressive
drugs (including
cancer
chemotherapy_
during the 4 weeks
before surgery,
recent history of
fever, infection or
both, serious
malnutrition (serum
albumin <3.3g.dl, a
white cell count
<2500 cells per ml
or the loss of more
than 20% of body
weight within 3
months of surgery)
and bowel
obstruction.
Melling RCT To assess the No. patients: N= Intervention1-Systemic SSI (2-6 weeks) Definitions:
87
2001 1, 2, 4, 6, use of a local 416 n=139 group-standard Overall rate of infection 32/416 SSI- purulent discharge or a
(SIBT) 7, 8, 9 warming Patient preoperative care plus (8%) painful erythema that lasted 5
device and a characteristics: minimum 30 minutes SSI: days and was treated with
warm air similar in all groups. preoperative warming to Interventions1&2 13/277 (5%) antimicrobials within 6 weeks of
blanket for the Including age, BMI, the whole body using Control: 19/139(14%) surgery. Wounds swabbed for
reduction of gender, fasting>8h, forced-air, warming P=0.001 culture if purulent discharge
infection after hair removal blanket. ASEPSIS wound scores present at time of review.
clean wound (shaving) >6 h, type Intervention 2- Local significantly higher in control Note: only 14 wound swabs
surgery. of surgery, surgery n=138 standard group vs. combined were obtained because
in last 3 months, preoperative care plus interventions (p=0.007) Postoperative antimicrobials-
cancer diagnosis, minimum 30 minutes ASEPSIS >20 Patients seen at 2 and 6
initial core preoperative warming to Interventions 1&2 10/277 (4%) weeks had often been
temperature, AMP, just the planned wound Control: 17/138 (12%) prescribed antimicrobial
length of surgery, area using a non- treatment by their general
seniority of surgeon. contact, radiant heat Other wound complications practitioner without having
2017 American Medical Association. All rights reserved. 320
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
(Data Intervention Results Comments
Risk of Objective Setting (N)
Extractor) Bias Score
Age, years: 18 dressing. including hematoma, seroma, wound swabbed
years Mean (SD) Timing of intervention: and wound aspiration no Normothermia: NR
Intervention preoperative statistically significant Hypothermia: NR
1:49.7(13.7) Duration of difference between groups. Perioperative care:
Intervention 2: 50 Intervention: for a SSI : Intervention 2 -local vs. Anesthesia- not described
(14.1) minimum of 30 minutes Intervention 1-systemic Follow up: 2-6 weeks
Control: 50.4 (15.3) until just before surgery warming postoperatively in outpatient
Gender m/f: 174/242 Device: No differences in outcomes clinic or home. Direct
Obesity: Systemic-Forced-air between two warming observation, patient diary, if not
2
BMI (mg/kg ): warming blanket methods. available for examination then
Intervention Local- non-contact, Individually both local telephone assessment patient
1:25.7(4.3) radiant heat dressing. (p=0.003) and systemic questionnaire (6/10
Intervention Monitoring (p=0.026) warming had a questionnaires returned)
2:25.8(4.1) intervention: tympanic significant effect on rate of Funding Source Conflicts:
Control:25.6(4.1) thermometers before SSI. Authors: NR
Procedure: Elective any treatment, after any Effect of warming Institution: NR
hernia repair n=155 warming and after interventions compared with Study: Industry
varicose vein surgery control:
Supplies: Industry
surgery n=86 breast Control: - (n=139) Absolute risk reduction (95%
surgery n=175 standard preoperative CI):
Indications: NR care plus no warming Intervention 1 systemic
Setting: 1 district Standard Preventive 10.1% (3.6-16.6)
general hospital Measures: Intervention 2 Local
Location: United Antimicrobial 7.9% (1.0-14.8)
Kingdom prophylaxis- AMP: Relative risk reduction:
Dates: April 1999 to 119/416 (29%) Intervention 1 systemic 73.7%
May 2000 Hair Removal- Shaving Intervention 2 local 57.7%
Inclusion criteria: No shaving Numbers needed to treat:
Elective hernia 110/416(26.4%) Intervention 1 systemic 15
repair, varicose vein Shaving <7h preop: patients.
surgery, or breast 116/416 (27.9%) Intervention 2 local 10
surgery that would Shaving>7h preop: SSI vs. No SSI
result in a scar 183/416 (20%) Mean (SD)
longer than 3 cm in Info missing n = 9 Stepwise logistic regression
length. yielded only body mass index
Exclusion criteria: as significant variable at the
Pregnant, taking 5% level OR 1.12 (95% CI
long-term oral 1.02-1.21)
steroids, had BMI
2017 American Medical Association. All rights reserved. 321
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
(Data Intervention Results Comments
Risk of Objective Setting (N)
Extractor) Bias Score
received SSI: 28.04 (4.44)
radiotherapy ( to the No SSI 25.31(3.98)
incision site) or Breast surgery had higher SSI
chemotherapy in the rate than hernia repair and
last 4 weeks, or had varicose veins
an infection at the Hair Removal:
time of surgery No shaving:
SSI 9/32 (28%)
No SSI 101/384 (27%)
Shaving within 7h of surgery
SSI 6/32 (19%)
No SSI 110/384 (30%)
Shaving >7hrs before surgery
SSI 17/32 (53%)
No SSI 166/384 (44%)
SSI and AMP:
Had AMP
SSI: 6/32 (19%)
No SSI 115/384 (30%)
Topic-specific outcomes
mean (SD); P value
Initial core temperatures were
significantly increased by
intervention 1 and 2 vs. control
Intervention 1Systemic
0.35C(0.58)
P=0.001
Intervention 2 Local: 0.13C(
0.57)
P=0.028 Control initial core
temp: 36.5 (0.55)
Postoperative core
temperatures were within
normal limits: 36.41 (0.59)
Intervention 2-Local received
longer period of warming (min)
as compared to Intervention 1-
systemic (44.94 vs. 38.73,
2017 American Medical Association. All rights reserved. 322
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
(Data Intervention Results Comments
Risk of Objective Setting (N)
Extractor) Bias Score
p=0.005)
Length of stay: NR
Mortality: NR
Adverse events:
Prescribed postop
antimicrobials:
Intervention1&2: 18/277(7%)
Control: 22/139 (16%)
P=0.002
Kurz RCT To test No. patients: Intervention: n=104 SSI: 2 weeks Definitions
88
1996 1, 2, 4, 5, hypothesis N=200 Fluid warmer on. Overall: 24/200 (12%) Wound Infection (Suspected): If
(SIBT) 6, 7, 8, 9 that Patient Forced-air cover 40C Intervention: 6/104 (6%) pus could be expressed from
hypothermia Characteristics: Patient target core Control: 18/96 (19%) the surgical incision or
both characteristics, temp maintain near P=0.009 aspirated from a loculated mass
increases diagnoses, types of 36.5C SSI in smokers(n=62) vs. non- inside the wound
susceptibility surgical procedure, Timing of Intervention: smokers (n=138) Wound Infection (Confirmed) - if
to surgical duration of surgery, intra-operative Smokers: 14/62 (23%) pus culture was positive for
wound hemodynamic Duration of Non-smokers10/138 (7%) pathogenic bacteria.
infection and values, and types of intervention: P=0.004 ASPESIS score >20
lengthens anesthesia were intraoperative ( from SENIC score (1/2/3) Hypothermia 34.5C
hospitalization similar in both induction of anesthesia Intervention:3/95/6 Normothermia 36.5C
groups -no to end of surgery) Control:3/88/5 Perioperative care:
statistically Device: NNISS scores (0/1/2) Anesthesia standardized:
significant difference Fluid warmer and Intervention:32/49/23 thiopental sodium, fentanyl,
Age: 18 to 80 years forced-air cover Control:31/39/26 vecuronium bromide,
meanSD Monitoring: P=0.6 isoflurane, and fentanyl at
Age: Temperature: tympanic ASEPSIS scores: completion for analgesia.
Gender: m/f 108/92 thermometer Intervention: 710 Follow up: 2 weeks: daily in
Height ,cm: Preop- recorded Control: 1316 hospital and at 2 weeks postop.
Intervention:1709 Intraop- 10 min intervals P=0.002 94% returned for 2 week visit,
Control: 1699 Postop-20 min intervals ASEPSIS scores>20: those who did not were evenly
P=0.43 for 6h Intervention: 6% of patients distributed between the study
Weight, kg Thermal comfort-visual Control: 32% of patients groups and most returned to
Intervention:7314 analog scale (VAS) P<0.001 visit private offices of attending
Control: 7114 Pain- VAS ASEPSIS Score in surgeons. Wound status
P=0.31 Shivering-scale all smokers(n=62) vs. non- determined by calling physician.
Procedure: Elective evaluated at 20min smokers (n=138) No previously unidentified SSIs
colorectal resection intervals for 6 hours Smokers:1518 detected in clinic for the first
Indication: postop. Non-smokers: 810 time
2017 American Medical Association. All rights reserved. 323
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
(Data Intervention Results Comments
Risk of Objective Setting (N)
Extractor) Bias Score
Cancer 182/200 Control: n=96 P<0.001 Funding Source Conflicts:
(91%) Inflammatory Fluid warmer off. SSI Risk Factors, multivariate Authors: None
bowel disease Forced-air cover analysis Institution: NR
18/200 (9%) ambient temperature OR (95%CI) Study: Industry
Setting: 3 hospitals Patient target core Tobacco use (Y/N): 10.5 (3.2- Supplies: NR
1 University n=155 temp: allowed to 34.1)
1 University n=30 decrease to ~34.5C. Group assignment
1 other hospital Standard preventive (Intervention vs. Control)
n=15 measures: 4.9 (1.7-14.5)
Location: Austria Bowel Prep- standard Surgical site (rectum vs. colon)
Dates: July 1993 mechanical bowel prep 2.7 (0.9-7.6)
through March 1995 with an electrolyte NNISS score (per unit
Inclusion criteria: solution. increase)
Abdominal AMP-standardized- IV 2.5 (1.2-5.3)
intraperitoneal pull- cefamandole and Age (per decade) 1.6 (1.0-2.4)
through procedures metronidazole at Other infections:
Exclusion criteria: induction of anesthesia Topic-specific outcomes:
minor colon surgery and maintained for 4 mean SD; P value:
(e.g., polypectomy days postoperatively Intraoperative
or colostomy Fluids: hydrated Transfusions (allogeneic
performed as the aggressively during and blood)
only procedure), use after surgery see Intervention: 0.41.0
of corticosteroids or details Control 0.8 1.2
other Transfusion: Leukocyte P=0.01
immunosuppressive depleted blood at Vasoconstriction
drugs (including surgeons discretion Intervention: 6% of patients
cancer O2- supplemental, nasal Control: 74% of patients
chemotherapy) prongs at 6L/min first P<0.001
during the 4 weeks 3hours postop, gradually Core Temperature at end of
prior to surgery, a eliminated to maintainO2 surgery
recent history of sat >95% Intervention:36.60.5C
fever, infection or Pain- opioids postop Control: 34.70.6C
both, serious (patient controlled) P=<0.001 and remained
malnutrition (serum significantly different for >5
albumin <3.3g/dL, hours postoperatively
white blood cell Postoperative
count <2500 Vasoconstriction
cells/mL, or the loss Intervention: 22% (short-lived)
of more than 20% of Control: 78% (continued
2017 American Medical Association. All rights reserved. 324
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
(Data Intervention Results Comments
Risk of Objective Setting (N)
Extractor) Bias Score
body weight), or throughout 6h recovery)
bowel obstruction. P<0.001
Shivering:
Intervention: a few
Control: 59% of patients
Thermal comfort score- VAS
1h postop:
Intervention: 7314mm
Control: 3517mm
Remained statistically
significant for 3h
Other:
Pain score and amount of
opioid administered virtually
identical in the two groups at
every postop measurement;
hemodynamic values also
similar.
Collagen deposition g/cm
Intervention: 328135
Control: 254114
P=0.04
Days to first solid food:
Intervention: 5.62.5
Control: 6.52.0
P=0.006
Remained statistically
significant even when analysis
was limited to uninfected
patients:
Intervention: 5.21.6
Control: 6.11.6
P<0.001
Days to suture removal
Intervention: 9.82.9
Control: 10.91.9
P=0.002
Remained statistically
significant even when analysis
2017 American Medical Association. All rights reserved. 325
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
(Data Intervention Results Comments
Risk of Objective Setting (N)
Extractor) Bias Score
was limited to uninfected
patients:
Intervention: 9.62.6
Control: 10.61.6
P=0.003
Days to suture removal in
smokers (n=62) vs. non-
smokers (n=138)
Smoker: 10.93.5
Non-smoker10.12.0
P=0.04
Length of stay, days:
Intervention:12.14.4
Control: 14.76.5
P=0.001
Remained statistically
significant even when analysis
was limited to uninfected
patients:
Intervention: 11.84.1
Control:13.54.5
P=0.01
Analysis: smokers(n=62) vs.
nonsmokers (n=138)
Smokers: 14.96.7 days
Non-smokers: 12.95.0
P=0.02
Mortality:30 days
Intervention: 2/104(1.9%)
Control: 2/96 (2.1%)
Adverse events:
ICU Admission- (wound
dehiscence, colon perforation,
peritonitis)
Intervention: 4/104 (3.9%)
Control: 7/96(7.3%)
P=0.47
2017 American Medical Association. All rights reserved. 326
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Q5. What are the most effective strategies for achieving and maintaining perioperative normothermia? Our search did not identify RCTs or SRs that
evaluated the most effective strategies for achieving and maintaining perioperative normothermia and their impact on the risk of SSI.
2.1D3. RISK OF BIAS ASSESSMENTS OF STUDIES: Q4-5 NORMOTHERMIA
eTABLE 41. Risk of Bias Assessments of Randomized Controlled Trials for Q4-5 Normothermia
Funding
Attrition source(s)
Described Randomizati- smaller than 10- disclosed and
as on Described Outcome Study 15% of Attrition no obvious Overall
Author randomize- appropriately as double- assessor participant Investigat- Attrition assigned appropriatelyconflict of Risk of
Year Q ed performed blind blinded blinded or blinded described patients analyzed interest Bias
Question 4: Normothermia
Kurz
88 4 Low
1996
Melling
87 4 Low
2001
Wong
89 4 Low
2007
2017 American Medical Association. All rights reserved. 327
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.1E. Q6-7 OXYGENATION
2.1E1. GRADE TABLE: Q6-7 OXYGENATION
eTABLE 42. GRADE Table for Q6-7 Oxygenation
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
Overall
Dose-response
Quantity GRADE of
Study Quality
Confounders
Consistency
GRADE
Directness
Precision
and Type Starting Evidence
Comparison Outcome Findings of
of GRADE for
Evidence
Evidence Outcome
Base
Q6. In patients with normal pulmonary function, how safe and effective is the perioperative use of increased fraction of inspired oxygen (FiO2) in reducing the
risk of SSI?
General Anesthesia
Intraoperative only (mechanical ventilation)
In one RCT of 434 routine gynecological
and abdominal surgeries, analysis
suggested no difference between groups:
15/226 (6.6%) vs. 15/208 (7.2%); RR: 0.92
(0.46 1.84); p= 0.81. However, this study
did not describe maintenance of
90
SSI, All* 1 RCT normothermia or adequate volume High 0 0 0 -1 0 0 0 0 Moderate
replacement. There were significant
differences in deviation from protocol
between study groups: 3/226 (1.3%) vs.
13/208 (6.3%), p<0.01, with reasons for
80% oxygen deviation in the control group including
vs. 30% desaturation and bradycardia.
oxygen (Both Moderate
groups without Organ/ 90 No difference between groups: 4/226 (1.8%)
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
nitrous oxide) Space vs. 5/208 (2.4%)
Deep 90 No difference between groups: 5/226 (2.2)
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Infection vs. 4/208 (1.9)
Superficial 90 No difference between groups: 6/226 (2.7%)
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Infection vs. 6/208 (2.9%)
No difference between groups in sternal
pain, 5/226 (2.2%) vs. 6/208 (2.9%), p=0.66
Adverse 90
1 RCT No significant difference between groups in High 0 0 0 -1 0 0 0 0 Moderate
Events
nausea and vomiting (17/226 (7.5%) vs.
11/208 (5.3%), p=0.34 or hypotension 3/226
2017 American Medical Association. All rights reserved. 328
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
Overall
Dose-response
Quantity GRADE of
Study Quality
Confounders
Consistency
GRADE
Directness
Precision
and Type Starting Evidence
Comparison Outcome Findings of
of GRADE for
Evidence
Evidence Outcome
Base
(1.3%) vs. 0/208, p=0.10)
Intraoperative mechanical ventilation and postoperative non-rebreathing facemask or nasal cannula for 2-6 hours
All Surgeries
A meta-analysis (N=2622) of 6 RCTs that
included heterogeneous surgeries and
patients, and differences in optimization of
normothermia and adequate tissue
perfusion suggested 80% oxygen was
associated with reduction in SSI: OR: 0.63
2
(0.43 0.92); p=0.02; I =52%
3 high quality RCT
91-93
totaling 1001
colorectal (n=791) and open appendectomy
(n=210) patients, each reported a 40%
reduction in SSI with 80% oxygen. Each
study optimized perioperative tissue oxygen
80% oxygen delivery by standardizing patient core
vs. 30% 91- temperature regulation strategies targeted
6 RCT
oxygen (Both SSI, All* 96 at maintenance of normothermia and fluid High 0 -1 0 0 0 0 0 0 Moderate Moderate
groups without replacement to avoid hypo or hypervolemia
1 high quality RCT of 217 patients
96
nitrous oxide)
undergoing open reduction and internal
fixation of 235 high-energy tibial plateau
(n=78), tibial pilon (n=86) and calcaneus
(n=61) fractures reported a 40% reduction in
SSI with 80% oxygen though this difference
was not significant with a multivariate
adjusted OR: 0.54 (0.22-1.29); p=0.17.
Normothermia and adequate fluid
replacement were not described.
1 high quality RCT in 1386 patients
94
undergoing a variety of general and
gynecologic surgical procedures found no
2017 American Medical Association. All rights reserved. 329
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
Overall
Dose-response
Quantity GRADE of
Study Quality
Confounders
Consistency
GRADE
Directness
Precision
and Type Starting Evidence
Comparison Outcome Findings of
of GRADE for
Evidence
Evidence Outcome
Base
difference between groups. However, this
study did not optimize tissue oxygen
delivery as it failed to maintain perioperative
normothermia and instituted aggressive
perioperative fluid restriction.
Organ/space infections reported in 5% of
Organ/
2 RCT 1386 patients, and comprised 28% of all SSI
Space 94,95 High 0 0 0 -1 0 0 0 0 Moderate
No difference between groups: 36/685 (5%)
Infection
vs. 39/701 (6%)
Deep infections reported in 3% of 1386
Deep 2 RCT patients, and comprised 15% - 18% of all
94,95, High 0 0 0 -1 0 0 0 0 Moderate
Infection SSI; no difference between groups OR: 0.80
(0.42 1.51); p=0.52
Superficial infections reported in 11% of
Superficial 2 RCT 1386 patients, and comprised 54% - 57% of
94,95 High 0 0 0 -1 0 0 0 0 Moderate
Infection all SSI; no difference between groups OR:
1.15 (0.71 1.85); p=0.63
92,93
2 RCTs found that 80% oxygen was
associated with lower ASEPSIS scores
91-
91,94
ASEPSIS 4 RCT 2 RCTs suggested that 80% oxygen
94 High 0 0 0 0 0 0 0 0 High
Scores was associated with fewer patients scoring
>20 on ASEPSIS scale, but this finding was
not significant
1% mortality reported in elective colorectal
91,93
surgery patients at 14days
5% mortality reported in mixed emergency
Mortality,
4 RCT and elective laparotomy patients at 30
14-30 91,93-95 94 High 0 0 0 0 0 0 0 0 High
days
Days
No difference between groups
Mortality unrelated to use of increased
fraction of inspired oxygen
2017 American Medical Association. All rights reserved. 330
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
Overall
Dose-response
Quantity GRADE of
Study Quality
Confounders
Consistency
GRADE
Directness
Precision
and Type Starting Evidence
Comparison Outcome Findings of
of GRADE for
Evidence
Evidence Outcome
Base
Respiratory failure, defined as the need for
Respirato- controlled ventilation or arterial oxygen
2 RCT
ry Failure 94,95 saturation below 90% despite supplemental High 0 0 0 -1 0 0 0 0 Moderate
(14 Days) oxygen was reported in 5% of patients
No difference between groups
Atelectasis diagnosis based on a
Atelectas- radiologists evaluation and description on
2 RCT
is (14 94,95 chest radiograph or computed tomography High 0 0 0 -1 0 0 0 0 Moderate
Days) Reported in 8% of patients
No difference between groups
Subcutaneous tissue oxygen tension was
higher in patients receiving 80% oxygen.
Tissue
93 This was noted both intraoperatively (109
Oxygen 1 RCT High 0 0 0 -1 0 0 0 0 Moderate
mmHg vs. 59mmHg; p<0.01) and
Tension
postoperatively (73 mm Hg vs. 54 mm Hg;
p=0.02)
3 RCTs
91-93
found no statistical difference
between groups
The 2 colorectal surgery studies
91,93
suggested that 80% oxygen was associated
with one day longer duration of hospital stay
but the findings were not significant: 12
93 91
vs.11 days; P=0.26 and p=0.09
respectively
91-
Only the 1 open appendectomy RCT
92
Length of 5 RCT
94,96 High 0 -1 0 0 0 0 0 0 Moderate
Stay reported a significantly longer hospital stay
in the 30% oxygen group (p=0.01).
One RCT (N=235 fractures in 217
96
patients) in fracture fixation surgeries
reported a longer length of hospital stay for
the 80% oxygen group, but this difference
was not significant: 3.5 days (SD 4.1 days)
vs. 2.8 days (SD 2.6 days), p=0.11.
The 1 large, mixed surgical population
2017 American Medical Association. All rights reserved. 331
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
Overall
Dose-response
Quantity GRADE of
Study Quality
Confounders
Consistency
GRADE
Directness
Precision
and Type Starting Evidence
Comparison Outcome Findings of
of GRADE for
Evidence
Evidence Outcome
Base
94
RCT (N=1,386) suggested 80% oxygen
was associated with one day shorter
duration of hospital stay but the findings
were not significant: 6 days (range, 1-34
days) vs. 7 days (range, 2-36 days); p=0.09
Colorectal Surgeries
80% oxygen
vs. 30%
A meta-analysis of 2 RCTs
91,93
oxygen (Both and a
94
groups without subanalysis from a third RCT (N=1424) in
nitrous oxide colorectal surgeries with preoperative oral
3 RCT
and with oral SSI* 91,93,94 bowel prep and maintenance normothermia High 0 0 0 0 0 0 0 0 High High
bowel prep, and adequate tissue perfusion suggested no
maintenance of benefit to 80% oxygen OR: 0.64 (0.40
2
tissue perfusion 1.04); p= 0.07; I =59%
and
normothermia)
Intraoperative mechanical ventilation and postoperative 30 minutes with nitrous oxide
One interim analysis 1 RCT (n=160)
reported 29 (18%) SSIs
97
SSI, All* 1 RCT 80% oxygen was associated with an High 0 0 0 -1 0 0 0 0 Moderate
increased risk of SSI: OR: 2.63; (1.1 6.2);
80% oxygen p=0.02; RR: 2.22 (1.1-4.6)
vs. 35% Deep structures infection reported in 4/160
oxygen (both Deep (3%) of patients an no difference between
97
groups with Structures 1 RCT group: 3/80 (4%) vs. 1/80 (1%); OR 3.08 High 0 0 0 -1 0 0 0 0 Moderate Moderate
nitrous oxide Infection (0.31-30.24); p=0.62
30 minutes Comprised 11% - 15% of all SSI
after incision) Wound infection reported in 18/160 (11%)
patients, comprising 56% - 65% of all SSI
Wound 97
Infection
1 RCT No difference between groups: 13/80 High 0 0 0 -1 0 0 0 0 Moderate
(16.25%) vs. 5/80 (6.25%): OR 2.91 (0.99 -
8.59); p=0.08
2017 American Medical Association. All rights reserved. 332
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
Overall
Dose-response
Quantity GRADE of
Study Quality
Confounders
Consistency
GRADE
Directness
Precision
and Type Starting Evidence
Comparison Outcome Findings of
of GRADE for
Evidence
Evidence Outcome
Base
Both Deep Both deep structures and wound infection
Structures reported in 7/140 (4%) patients, comprising
97
and 1 RCT 20%-33% of all SSIs. High 0 0 0 -1 0 0 0 0 Moderate
Wound No difference between groups: 3/80 (3.75%)
Infection vs. 4/80 (5%) OR: 0.74 (0.16 - 3.42); p=1
97
Mortality 1 RCT 1 death reported, in the control group High 0 0 0 -1 0 0 0 0 Moderate
This study suggested that 80% oxygen was
Length of associated with a longer mean length of
97
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Stay stay (8.3 days vs. 6.4 days), but the finding
was not significant (p=0.07)
NEURAXIAL ANESTHESIA (Intraoperative and postoperative non-rebreathing facemask)
A meta-analysis (N=1559) of 3 RCTs in
heterogeneous patients undergoing
cesarean section surgeries with Neuraxial
anesthesia, and differences in optimization
of normothermia and adequate tissue
perfusion suggested no benefit to 80%
oxygen: OR: 1.31 (0.90 1.90); p=0.16;
2
I =17%
1 large RCT (n=831) in cesarean section
99
98- patients found no difference in SSI
3 RCT
SSI, All* 100 incidence between groups: 8.2% (34/416) High 0 -1 0 0 0 0 0 0 Moderate Moderate
vs. 8.2% (34/415), p=0.89. This study
ensured adequate tissue perfusion, fluid
replacement and normothermia.
Antimicrobial prophylaxis was administered
post cord-clamp
1 large RCT (n=585) and 1 small interim
100
98
analysis (n=143) in cesarean section
patients suggested 80% oxygen delivered
through a non-rebreathing facemask was
associated with non-significant increase in
2017 American Medical Association. All rights reserved. 333
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
Overall
Dose-response
Quantity GRADE of
Study Quality
Confounders
Consistency
GRADE
Directness
Precision
and Type Starting Evidence
Comparison Outcome Findings of
of GRADE for
Evidence
Evidence Outcome
Base
risk of SSI:: 35/288 (12.2%) vs. 26/297
(8.8%), p=0.18 and 25% (95% CI, 15-35%)
vs. 14% (95% CI, 6-22%); p=0.13
respectively . Normothermia and adequate
fluid replacement were not described in
either study.
A meta-analysis (N=1559) of 3 RCTs in
heterogeneous patients undergoing
cesarean section surgeries with Neuraxial
anesthesia, and differences in optimization
of normothermia and adequate tissue
perfusion suggested no benefit to 80%
2
oxygen OR: 1.62 (0.86 3.05); p=0.14; I =0
1 large RCT (n= 585) and 1 small
100 98
80% oxygen
(n=143) interim analysis suggested 80%
vs. 30%
SSI- 98- oxygen was associated with an increase in
oxygen 3 RCT
Endometr- 100 endometritis, , but this was not statistically High 0 -1 0 0 0 0 0 0 Moderate
itis significant in either study 7/288 (2.4%) vs.
2/297 (0.7%), p=0.08, and 9/69 (13%) vs.
5/74 (7%), p=0.26 respectively. Neither
study was adequately powered to detect a
statistical difference in this outcome.
1 large RCT (n=831) suggested no
99
difference in the incidence of endometritis
with 80% oxygenation (2.4% vs. 2.7%,
p=0.66). This study ensured adequate
volume replacement and normothermia.
Length of 98 No difference between groups: median days
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Stay (range): 3 (2-5) vs. 3 (2-6); p=0.92
POSTOPERATIVE ONLY (Facemask and/or nasal cannula)
In1 RCT of 274 lower limb vascular
102
28-30 %
2 RCT
oxygen vs. SSI, All* 101,102 surgeries, multivariate analysis suggested High -1 0 0 0 0 0 0 0 Moderate Moderate
room air no difference between groups: 18% vs.
2017 American Medical Association. All rights reserved. 334
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
Overall
Dose-response
Quantity GRADE of
Study Quality
Confounders
Consistency
GRADE
Directness
Precision
and Type Starting Evidence
Comparison Outcome Findings of
of GRADE for
Evidence
Evidence Outcome
Base
28%; OR: 0.56 (0.30 1.04); p = 0.07.
Isolated groin incision SSIs were
significantly lower in the supplemental
(30%) oxygen group: 5.8% vs. 23.5%;
OR:0.20 (0.04-0.95) ;p=0.04
One lesser quality study of 24 cervical
101
spine surgeries reported no SSIs
Organ/ 102 No infections in the intervention group vs. 2
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Space infections (3%) in the control group
Deep 102
1 RCT No difference : 5.1% in each group High 0 0 0 -1 0 0 0 0 Moderate
Infection
Superficial 102 No difference: 18/137 (13%) vs. 29/137
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Infection (21%); OR 0.56; (0.30-1.07); p=0.11.
ASEPSIS 101 All within satisfactory healing (Score 0-10)
1 RCT High -1 0 0 -1 0 0 0 0 Low
Scores No difference observed between groups
Mortality was rare (4 deaths among 274
Mortality, 102 patients) and did not differ by group: 3/137
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
30 Days (2.2%) vs. 1/137 (0.7%); OR 3.0 (0.31-
28.99); p=0.62.
Adverse events were rare and did not differ
between groups
Adverse 2 RCT Reported adverse events include: wound
101,102 High -1 0 0 -1 0 0 0 0 Low
Events complications, graft thrombosis, cardiac
complications, pneumonia, stroke, renal
insufficiency, major amputation
Tissue Subcutaneous tissue oxygen tension was
101
Oxygen 1 RCT higher in patients receiving supplemental High -1 0 0 -1 0 0 0 0 Low
Tension oxygen (63 mm Hg vs. 48 mm Hg; p<0.01)
2017 American Medical Association. All rights reserved. 335
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
Overall
Dose-response
Quantity GRADE of
Study Quality
Confounders
Consistency
GRADE
Directness
Precision
and Type Starting Evidence
Comparison Outcome Findings of
of GRADE for
Evidence
Evidence Outcome
Base
Length of 102 No difference observed between groups:
1 RCT High 0 0 0 -1 0 0 0 0 Moderate
Stay 6.5d vs. 5.4d; p-=0.13.
Q7. What is the optimal target FIO2 to reduce the risk of SSI; how and when should it be administered? Our search did not identify RCTs or SRs that both
evaluated the optimal fraction of inspired oxygen, how and when it should be administered, and included SSI as an outcome. All studies evaluating the use of
supplemental increased oxygenation both intraoperative and postoperatively used 80% FiO2 as the target level. \
*Critical outcome; OR: Odds Ratio; RR: Risk Ratio; CI: Confidence Interval
2017 American Medical Association. All rights reserved. 336
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.1E2. EVIDENCE TABLE: Q6-7 OXYGENATION
eTABLE 43. Evidence Table for Q6. In patients with normal pulmonary function, how safe and effective is the perioperative
use of increased fraction of inspired oxygen (FiO2) in reducing the risk of SSI?
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Duggal RCT To evaluate Number of patients N=831 Intervention group n=416 SSI Definitions:
99
2013 1, 2, 3, whether Patient Characteristics: the 80% oxygen an aerosol face Composite infection (ITT) (SSI Surgical site infection CDC
(ES) 4, 5, 7, supplemental two groups were well mask delivered oxygen at 80% + Endometritis) % (n Definition: at least 1 of the
9, perioperative matched for age, race, concentration during surgery calculated by extractor) following criteria was
oxygen could parity, BMI number of and for 1h postop. Flow rate Intervention: 8.2% (34/416) required: 1) purulent
reduce the previous cesarean 10L/min. Control: 8.2% (34/415) discharge from incision site;
occurrence of deliveries, elective Timing of intervention: intra- P=0..89 2) organisms isolated from an
surgical site cesarean deliveries, and post-operatively SSI at discharge (usually PO aseptically obtained culture or
infection or history of diabetes, Duration of intervention: day 3) tissue from the superficial
endometritis in cardiac or pulmonary intraoperative and for 1h Intervention: 2.4% (10/416) incision; 3) at least one of the
women disease, anemia, postoperative Control: 2.9% (10/415) following signs or symptoms:
undergoing smoking, or chronic Device/agent: Aerosol face mask P=0.70 pain or tenderness, localized
cesarean steroid use. was used for both intervention SSI assessed by 6wk swelling, redness or heat,
deliver Age: mean SD, y and control Intervention: 3.1% (13/416) and the superficial incision
Intervention: 29.25.6 Monitoring intervention Control: 2.9% (12/415) was opened by the surgeon
Control: 29.55.8 Control group n=415 P=0.72 unless the incision culture
Gender: all female 30% oxygen an aerosol face Total SSI was negative; and 4)
2
Obesity: (kg/m ) mask delivered oxygen at 30% Intervention: 5.5% (23/416) diagnosis of superficial
Total 30 concentration during surgery Control: 5.8% (24/415) incisional surgical site
Intervention: 331/416 and for 1h postop. Flow rate P=0.98 infection by the surgeon.
(79.6) 10L/min. Total Endometritis Endometritis: diagnosed by the
Control: 306/415 (73.7) Standard preventive measures: Intervention: 2.7% (11/416) clinical finding of a temp of
o
BMI 30-34.9 AMP: usually cefazolin (2g) Control: 2.4% (10/415) more than 38 C associated
Intervention: 142/416 intravenously after cord P=0.66 with uterine tenderness
(34.1) clamping. If allergic to without any other source of
Control: 127/415 (30.6) penicillin, patient received Diabetes Subanalysis fever identified.
BMI 35-39.9 clindamycin (900mg). Composite (SSI + Perioperative care: NR
Intervention: 100/416 Closure: if subcutaneous tissue Endometritis) Other notes: Study was
(24.0) was >4cm thick, it was closed % (n/N) powered to demonstrate a
Control: 97/415 (23.4) with 2-0 plain catgut. Method Intervention: 14.4% (13/90) 50% difference in infection
BMI 40 or greater of skin closure was determined Control: 6.9% (6/87) rate with a two-sided of
Intervention: 89/416 (21.4) in operating room. P=0.11 0.05 and a power of 80%.
Control: 82/415 (19.8) Fluid Replacement: care was SSI at discharge, % (n/N) The sample size estimation of
Comorbidities taken to ensure the patients Intervention: 6.7% (6/90) 778 patients was determined
Diabetes received adequate fluid Control: 2.3% (2/87) for the composite outcome of
2017 American Medical Association. All rights reserved. 337
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Intervention: 91/416 (21.9)resuscitation to ensure P=0.17 SSI and Endometritis
Control: 87/415 (20.9) adequate tissue perfusion. SSI at 6week postop (baseline rate 12%)
Normothermia: optimal room Intervention: 3.3% (3/90) Follow-up: 6 weeks
Procedures: Cesarean temperature was maintained to Control: 1.1% (1/87) (postpartum visit)
delivery ensure normothermia. A P=0.34 135 (16.5%) lost to follow up.
Indications: NR warming blanket was used at Total SSI Intervention: 70/416 (16.8%)
Setting: 1 tertiary medical the discretion of the Intervention: 10% (9/90) Control: 65/415 (15.7%)
center anesthesiologist. Control: 3.4% (3/87) P=NS
Location: USA Normoglycemia: a finger-stick P=0.09 Funding Source Conflicts:
Dates: August 2006 blood glucose test was done Total endometritis Authors: NR
August 2010 on day of surgery to ensure Intervention: 4.4% (4/90) Institution: NR
Inclusion Criteria: Women normoglycemia during surgery Control: 3.4% (3/87) Study: NR
undergoing elective or P=0.75 Supplies: NR
emergency cesarean
delivery. Other infections: NR
Exclusion Criteria: Fever Topic-specific outcomes:
(temp 38 C),
o
NR
chorioamnionitis (temp of Diabetic patients were
o
38 C or higher with fetal analyzed separately
or maternal tachycardia), Reoperations: NR
patients who were group Length of stay: NR
B Streptococci-positive Mortality: NR
and had been started on Adverse events: NR
antibiotics,
immunocompromised or
HIV-positive patients,
planned general
anesthesia, age <18
years, and incarcerated
patients.
Stall RCT To assess the Number of patients: N=222 Intervention group: n=119 SSI: Definitions:
96
2013 1, 2, 3, benefits of patients with N=235 After intubation, FiO2 was Overall 33/222 (13%) High Energy Fracture: one
(ES) 4, 5, 6, supplemental fractures adjusted to 80%. After Deep 27/33 (82%) requiring delayed (>5 days
7, 8, 9, perioperative Patient Characteristics: extubation patients were Superficial 6/33 (18%) after injury) definitive fixation
10 oxygen in an demographics and placed on high-flow because of soft tissue
orthopedic perioperative risk factors nonrebreather masks at 15L Overall intervention: 14/119 concerns
patient were similar in the two per minute for 2 hours postop. (12%) Surgical Site infection: based on
population groups overall. Although Timing of intervention: Intra- Overall control: 19/116 (16%) CDC definitions.
undergoing no statistically significant and postop P = 0.31 (40% decrease in Deep infections: involve
2017 American Medical Association. All rights reserved. 338
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
open differences were Duration of intervention: infection rate in the debridement
reduction and observed in the intraoperative and 2 h postop. treatment group) Superficial infections: treated
internal distribution, some Device/agent: Nonrebreather Multivariate OR of all injuries with antibiotics alone.
fixation of imbalances were shown. mask for intervention group, = 0.54 (95%CI: 0.22-1.29), Treatment-Related
high-energy Age: mean (SD) y nasal cannula for control p=0.17 Complications: unexpected
tibial plateau, Intervention: 42.3 (12.1) group. No statistically significant pulmonary complication,
tibial pilon and Control: 42.5 (12.2) Monitoring intervention: pulse difference was seen prolonged intubation, and any
calcaneus Gender: female oximetry between groups in other adverse outcome
fractures. Intervention: 24/119 Adherence to protocol was subanalyses of the three thought to be related to
(20.2%) verified by postanesthesia care types of surgeries oxygen treatment by the
Control: 35/116 (30.2%) unit records. anesthesiologist or primary
Obesity: BMI mean (SD) Control group n= 116 Deep - 27/222 (12.2%) team.
3
kg/m After intubation, FiO2 was Superficial 6/222 (2.7%) Fractures: classified according
Intervention: 28.4 (6.4) adjusted to 30%. After to AO classifications as
Control: 28 (5.9) extubation patients were Other infections: NR determined by one
Comorbidities: placed on nasal cannulae at 4L Topic-specific outcomes: fellowship-trained orthopedic
Diabetes per minute to maintain oxygen NR traumatologist blinded to
Intervention: 7/119 (5.9%) saturation of at least 92% as Reoperations: NR treatment and outcome.
Control: 9/116 (7.8%) determined by pulse oximetry Length of stay:, mean (SD) d Perioperative care: NR
for 2 hours postop Intervention: 3.5 (4.1) Other notes: Study is
Procedures: open reduction Standard preventive measures: Control: 2.8 (2.6) underpowered to detect a
and internal fixation of Multiple operations: P=0.11 statistically significant
high-energy tibial plateau, - Patients with tibial plateau difference in composite SSI.
tibial pilon and calcaneus and tibial pilon fractures were Mortality: NR Trial stopped because funding
fractures. first managed with surgery to Adverse events: NR ran out.
Indications: high tibial place a temporary external Prespecified criteria for early
plateau, tibial pilon or fixator. These patients were termination of the trial were
calcaneus fractures not yet enrolled in the study any adverse event directly
Setting: University Hospital so the oxygenation for the attributable to the treatment
Location: USA initial surgery was standard (hyperoxygenation) and a
Dates: April 2007 practice. A small group of reduction in surgical site
November 2010 patients in the tibial pilon infections of greater than
Inclusion Criteria: all adult group underwent two 50% in the treatment group at
patients (18 years) who definitive operations, typically annual review.
sustained high-energy one approach from the Follow-up: median follow up
tibial plateau, tibial pilon, posterior ankle and another =344 days (range 84-1771
or calcaneus fractures anterior approach separated days; IQR 153-573 days)
undergoing open by a number of days. In Wound monitoring: per routine
reduction and internal these cases, the patients clinical practice, that is, on a
2017 American Medical Association. All rights reserved. 339
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
fixation, received the same treatment daily basis until discharge
Exclusion Criteria: The for both operations. There and at the 2, 6, and 12 week
above surgeries except were also a small number of outpatient follow-up visits. All
those requiring flap patients with more than one wound assessments were
coverage (Gustilo and eligible study fracture, and blinded
Anderson grade IIIB open each fracture was Funding Source Conflicts:
fracture) and those with randomized individually Authors: None
open fractures requiring AMP Standardized for both Institution: None
vascular repair for limb groups. Unless Study: None
salvage (Grade IIIC open contraindicated, patients Supplies: None
fractures). Also, evidence typically received 1 or 2 g
of infection at the fracture of cefazolin administered
site before definitive intravenously
st
fixation. During the 1 preoperatively and every
year of the trial, patients 8 hours for a total of 3
were excluded for any doses, per standard care
diagnosis of infection of the institution. For
requiring antibiotics, even open fractures, surgeons
if it was distant to the site were allowed to continue
of surgical incision. That antibiotics for up to 48h
criterion was removed postop according to their
because it became clinical practice.
apparent that many of the Normothermia: NR
patients received orally Adequate volume replacement::
administered antibiotics at NR
rehabilitation centers
before their definitive
surgery for diagnosis of
pin tract infections or
other infections unrelated
to the study fracture.
Excluding them was
detrimental to study
design because patients
who had recent infection
might have been at
increased risk of surgical
site infection and
therefore benefitted most.
2017 American Medical Association. All rights reserved. 340
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Also, preoperative arterial
hemoglobin saturation
<90% without
supplemental oxygen and
a history of preexisting
pulmonary disease that
can be worsened by high-
dose oxygen such as
COPD and bleomycin
toxicity. Also patients who
were unable to provide
informed consent and
those who were unable to
speak English or Spanish.
Thibon RCT To evaluate Number of patients: N=434 Intervention group: n=226 SSI : Definitions:
90
2012 1, 2, 4, the effects of Patient Characteristics: Pre-oxygenation, induction, Total: 30/434 (6.9%) SSI: CDC definitions were used.
(ES) 5, 6, 7, hyper- The two groups displayed emergence and extubation: Intervention: 15/226 (6.6) An investigator blinded to the
8, 9 oxygenation to no significant differences FIO2 100% Control: 15/208 (7.2) randomization conducted a
80% FiO2 in in baseline After pre-oxygenation, patients P=0.84 systematic review of the
routine characteristics. were ventilated with an RR- 0.92 (95%CI [0.46- patients medical records
abdominal and Age: y, mean (SD) anesthesia respirator. 1.84]) including the documentation
gynecologic Intervention: 52.1 (13.7) Following induction of provided by physicians and
surgery on the Control: 518 (13.3) anesthesia and tracheal Superficial nurses and lab reports.
frequency of Gender: female intubation, patients received Intervention: 6/226 (2.7) Perioperative care: NR
SSI occurring Intervention: 208/226 80% FiO2 Control: 6/208 (2.9) Other notes: Due to intention to
during the 30 (92.0) Timing of intervention: treat analysis, patients
days following Control: 184/208 (88.5) Intraoperative (postoperative at Deep remained in their group even
surgery, and Obesity: BMI>30 physicians discretion) not Intervention: 5/226 (2.2) if the oxygen concentration
to compare Intervention: 29/226 (12.8) intended for postop. Control: 4/208 (1.9) was increased during the
the Control: 27/208 (13.0) Duration of intervention: intervention to maintain
frequencies of Comorbidities: intraoperative Organ/Space saturation
peri- and Diabetes: Device/agent: facemask for both Intervention: 5/226 (2.2%) Follow-up: 30 days (if patients
immediate Intervention: 7/226 (3.1) intervention and control Control: 5/208 (2.4%) did not attend their 30 day
postoperative Control: 12/208 (5.8) Monitoring intervention: NR follow-up visit, their infection
adverse Current Smoker: Protocol not maintained for the Other infections: NR status was assessed by
effects Intervention: 39/226 (17.3) entire duration of the Topic-specific outcomes: calling the patient or their
between a Control: 42/208 (20.2) operation: Oxygen saturation on pulse physician)
group of Procedures: Intervention: 3/226 (1.3) oximetry at closure Loss to follow up: 4 patients
hyper- Gastric/hernia: Control: 13/208 (6.3) (mmHg) mean (SD) were lost to follow up (2 in
2017 American Medical Association. All rights reserved. 341
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
oxygenated Intervention: 13/226 (5.8) P=0.007 Intervention: 98.9 (1.1) each group). They were
patients and a Control:16/208 (7.7) Reasons for deviation - Control: 98.6 (1.3) uninfected when they left the
group of Hepatobiliary Intervention = intraoperative P=0.01 hospital and were considered
patients Intervention: 7/226 (3.1) complications including one Reoperations: NR uninfected in the final
receiving 30% Control: 11/208 (5.3) case of septic shock Length of stay: NR analysis.
oxygen. Colon/Rectum: Control = desaturation and/or Time until diagnosis of SSI Funding Source Conflicts:
Intervention: 19/226 (8.4) bradycardia Overall: 15.4 days8.2 Authors: NR
Control: 11/208 (5.3) Control group n= 208 Intervention: 16.9 days8.0 Institution: NR
Small Bowel Pre-oxygenation, induction, Control: 13.9 days8.4 Study: Industry
Intervention: 4/226 (1.8) emergence and extubation: Mortality: NR Supplies: NR
Control: 5/208 (12.4) FIO2 100% Adverse events:
Gynecologic After pre-oxygenation, patients Nausea and vomiting,
Intervention: 73/226 (32.3) were ventilated with an Intervention: 17/226 (7.5%)
Control: 66/208 (31.8) anesthesia respirator. Control: 11/208 (5.3)%
Breast Following induction of P=0.34
Intervention: 110/226 anesthesia and tracheal Sternal pain,
(48.7) intubation, patients received Intervention: 5/226 (2.2)
Control: 99/208 (47.6) 30% FiO2 Control: 6/208 (2.9)
Indications: NR Standard preventive measures: P=0.66
Setting: Multi-center (1 Pre-Oxygenation: before the Cough:
cancer institute, 1 induction of anesthesia, each Intervention: 1/226 (0.4)
university hospital& 2 patient was pre-oxygenated Control: 0/208 (0)
private hospitals) (100% FiO2) via facemasks for Hypotension:
Location: France at least 3 minutes until the tele- Intervention: 3/226 (1.3)
Dates: June 1, 2003-June expiratory fraction of oxygen Control: 0/208 (0)
30, 2007 was at least 90%. P=0.10
Inclusion Criteria: Patients Normothermia: NR No auditory or visual disorder
>18 years old, and Adequate volume replacement: was noted
scheduled to undergo NR
elective abdominal,
gynecologic, and breast
surgery provided that
anesthesia was provided
Exclusion Criteria: Recent
history of fever and/or
infection, chronic
respiratory failure (oxygen
PaO2 below 60 mmHg,
8.9kPa at rest), and
2017 American Medical Association. All rights reserved. 342
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
bleomycin treatment
(which may induce
sensitivity to oxygen
toxicity).
Scifres RCT To assess the Number of patients: N=585 Intervention group: n=288 SSI: Definitions:
100 o
2011 1, 6, 7, effect of a high Patient Characteristics: Women received oxygen at a flow Endometritis: Endometritis: oral temp of >38 C
(ES) 8, 9, 10 perioperative patient and operative rate of 10 L/min Intervention: 7/288 (2.4%) after the first 24h following
oxygen characteristics were not (corresponding to approx. 80% Control: 2/297 (0.6%) procedure and either (1)
concentration statistically significantly FiO2) by nonrebreather mask RR: 3.6; 95%CI, 0.8-17.2 fundal or lower abdominal
on different unless listed both during surgery and for 2 P=0.08 tenderness greater than
postcesarean below hours after cesarean delivery. Wound infection: expected or (2) foul-smelling
delivery Maternal Age Timing of intervention: Intra and Intervention: 33/288 (11.5%) purulent lochia. Patients were
infectious Intervention: 27.56.4y postoperatively Control: 26/297 (8.8%) diagnosed with endometritis
morbidity in Control: 27.85.9y Duration of intervention: during RR: 1.3; 95%CI, 0.8-2.1 only if other causes for signs
women Gender: all female and for 2 hours after cesarean P=0.28 and symptoms were not
undergoing Obesity BMI at delivery delivery. Composite (wound infection identified. Patients also had
2
cesarean >30kg/m Device/agent: intervention group +endometritis) to be treated with IV
delivery. Intervention: 208/288 used a nonrebreather mask Intervention: 35/288 (12.2%) antibiotics to be diagnosed
(72.22%) and control group used a nasal Control: 26/297 (8.8%) with endometritis.
Control: 230/297 (77.44%) cannula RR: 1.4; 95%CI, 0.9-2.3 Wound infection: only if wound
Comorbidities: Monitoring intervention: P=0.18 opening >1cm or other
Preterm Delivery <32wks: Compliance with the surgical intervention (such as
Intervention: 20/288 (6.9%) supplemental oxygen by face Other infections: laparotomy or debridement of
Control: 9/297 (3.3%) mask (intervention group) was Wound hematoma or seroma: tissue) plus at least 1 of the
P=0.03 assessed by anesthesiologist Intervention: 16/288 (5.4%) following: (1) purulent
Chronic hypertension: intraoperatively and by the Control: 17/297 (5.9%) drainage from the wound, (2)
Intervention: 34/288 postpartum nurse at 30, 60, 90 RR: 1.1; 95%CI, 0.6-2.1 erythema or induration of the
(11.8%) and 120 minutes postop. P=0.79 surrounding tissues, (3)
Control: 21/297 (7.1%) Oxygen saturation was maternal oral temperature
o
P=0.05 assessed both intraoperatively Topic-specific outcomes >38 C, or (4) radiographic
Previous abdominal surgery and postoperatively for both Intravenous antibiotics >24h evidence of infection.
including C-section, groups after delivery
laparoscopy, laparotomy, Compliance with intervention Intervention: 38/288 (13.2%) Perioperative care: NR
Intervention: 181/288 postop: Control: 35/297 (11.8%) Other notes:
(62.9%) Intervention at 30min: 214/288 RR: 1.1; 95%CI, 0.7-1.7 Study utilized infectious
Control: 210/297 (70.7%) (74.3%) P=0.61 morbidity composite
P=0.04 Intervention at 60min: 189/288 Hospital readmission measure. (A combination of
Rupture of membranes (65.6%) Intervention: 15/288 (5.2%) endometritis and wound
before cesarean delivery. Intervention at 90min: 172/288 Control: 10/297 (3.4%) infection). Especially for
2017 American Medical Association. All rights reserved. 343
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Intervention: 84/288 (59.7%) RR: 1.5; 95%CI, 0.7-3.4 subgroup analysis to
(29.2%) Intervention at 120min: 97/288 P=0.27 determine effect of
Control: 59/297 (19.9%) (33.7%) Neonatal outcomes differences between
P<0.01 Control group: n=297 Umbilical artery pO2 (mmHg) populations for causes such
Procedures: Cesarean Women received oxygen at a flow Intervention: 19.49.6 as rupture of membranes,
section rate of 2 L/min (corresponding Control: 17.16.8 labor before cesarean, etc.
Indications: scheduled or to approx. 25-30% FiO2) via P<0.01
intrapartum cesarean nasal cannula during cesarean Umbilical artery CO2 (mmHg) Most non-compliance was
delivery. delivery only. Intervention: 57.011.4 related to discomfort
Setting: One University Standard preventive measures: Control: 58.911.0 associated with wearing the
Hospital Additional supplemental oxygen: P=0.05 non-rebreather mask.
Location: USA with oxygen saturation <95% Antibiotics after birth Particularly in the period of
Dates: February 2008 were supplied supplemental Intervention: 75/288 (26.0%) 60-120min post-op.
March 2010 oxygen as needed to maintain Control: 55/297 (18.5%) Follow-up: 2-4 weeks postop
Inclusion Criteria: Patients appropriate oxygenation P=0.03 during the postop visit.
who underwent scheduled Intervention: 0/288 Anyone who did not return for
or intrapartum cesarean Control: 18/297 (5.9%) Reoperations: NR postop visit within 4 weeks or
delivery with regional Length of stay: NR who had planned follow up
anesthesia Skin Prep: Both groups received Mortality: visit at an outside clinic were
Exclusion Criteria: standard preoperative skin Neonatal mortality contacted by the research
Emergency surgery in prep. Intervention: 8/288 (2.7%) nurse by telephone with the
which participant was AMP: both groups received Control: 1/297 (0.34%) data collection form used as
unable to provide standard AMP (cefazolin was P=0.06 a prompt.
informed consent, human primary antibiotic; clindamycin All deaths were analyzed and Funding Source Conflicts:
immunodeficiency virus was used in the case of none were attributable to Authors: NR
infection, chronic penicillin allergy. supplemental oxygen Institution: NR
corticosteroid therapy or Closure: Subcutaneous sutures Adverse events: NR Study: NR
other immunosuppressive were left to the decision of the Supplies: NR
therapy, general surgical team
anesthesia, and a Adequate fluid replacement: NR
diagnosis of extra-uterine Normothermia: NR
infection (i.e.,
pyelonephritis or
pneumonia) before
cesarean delivery. Acute
chorioamnionitis was not
an exclusion criterion.
2017 American Medical Association. All rights reserved. 344
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Staehr RCT To evaluate Number of patients: N: 213 Intervention: n=102 SSI (Follow up 14 days Definitions:
95
2011 1, 2, 3, the effect of a Patient Characteristics: Intraop: Patients were pre- postop) SSI: CDC definitions (Within 14
(ES) 4, 5, 6, high All demographic and oxygenated with 100% FiO2 Overall: 29% days)
7, 8, 9, inspiratory perioperative until tracheal intubation. Intervention: 32/102 = 31% Pneumonia: CDC (Within 14
10 oxygen characteristics were Patients were given 80% FIO2 Control: 29/111= 26% days)
fraction (80%) similar between groups. from intubation until the end of Univariate OR: Adverse Event: ND
on SSI and Population Characteristics surgery when 100% FIO2 was 1.29 (95% CI, 0.71-2.34) Serious adverse event: Serious
pulmonary Age: 18 years given immediately before P= 0.40 if fatal, life threatening,
complications Gender: m/f: 86/127 extubation. FIO2 was increased Adjusted OR: caused permanent disability,
in obese Morbidly Obese: 73/213 to ensure arterial oxygen 1.22 (95%CI, 0.63-2.39) or required prolonged
patients (32%) above 94%. P=0.57 hospitalization
2
undergoing All characteristics below Postop: The first 2h after surgery Superficial infection Obese: BMI 30-34.9kg/m
Morbidly Obese: BMI 35kg/m
2
laparotomy. are given are for the patients received 80% FIO2 Intervention: 16/32 (50%)
intervention group N=102: from the Nonrebreathing Control: 21/29 (73%) Overweight: BMI= 25.0-
2
Median [5-95% range] or facemask and an oxygen flow Deep Infection 29.9kg/m
Age: 63y [37-81] of 14 l/min and an air flow of 2 Intervention: 8/32 (25%) Normal Weight: BMI= 18.5-
2
Gender: m/f:43/59 l/min. 2 hrs. after surgery, Control: 5/29 (29%) 24.9kg/m
2
Obesity: supplemental O2 was Organ/Space Infection Underweight: BMI<18.5 kg/m
2
Median BMI: 34 kg/m [30- administrated according to Intervention: 8/32 (25%) Perioperative Care:
44] clinical practice Control: 3/29 (10%) Anesthesia-standardized, non-
BMI35kg/m :39 (38%)
2
Timing of Intervention: Intra and Incidence of SSI nitrous oxide
Comorbidity: Postoperatively Obese Patients = 27% Other notes:
Current smoker: 31 (30%) Duration of Treatment: Morbidly Obese Patients This was a planned subgroup
Diabetes mellitus: 16 Intubation to 2 hours after n=73(32%) analysis of the PROXI trial;
(16%) surgery. Sub-analysis of SSI Meyhoff 2009
Pulmonary Disease: 16 Device: Nonrebreathing between Intervention Adjusted OR adjusted for study
(16%) facemask with a reservoir groups distributed by center, diabetes mellitus,
Hypertension: 48 (47%) weight class. (interpreted acute surgery, COPD, current
Other cardiovascular Control: n=111 from graph (%SSI [upper smoker, upper abdominal
disease: 15 (15%) Intraop: Patients were pre- 95% CI]) incision, duration of surgery,
Underweight (BMI<18.5kg/m ) and age (40 years or <40
2
Duration of surgery: 145 [45- oxygenated with 100% FiO2
309] min until tracheal intubation. Intervention: 10% [25%] years) where possible
Epidural analgesia: Patients were given 30% FIO2 Control:19% [37%] Preoperative SSI Risk
thoracic/lumbar/none: from intubation until the end of Normal Weight (BMI 18.5- Stratification:
2
66/4/32 surgery when 100% FIO2 was 24.9 kg/m ) SENIC 1/2/3/4
Type of anesthesia: given immediately before Intervention: 17% [20%] Intervention: 24/32/42/4
Volatile: 25 (25%) extubation. FIO2 was increased Control:18% [21%] Control: 25/35/47/4
Total IV: 77(75%) to ensure arterial oxygen Over Weight (BMI 25.0- NNIS, 0/1/2/3
2
Procedure: Laparotomy above 94%. 29.9kg/m ) Intervention: 20/50/26/6
2017 American Medical Association. All rights reserved. 345
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Colorectal: Postop: The first 2h after surgery Intervention: 19% [24%] Control:28/47/29/7
Intervention: 40/102 (39%) patients received a mixture of Control:22% [28%]
2
Control: 49/111 (44%) O2 (2 l/min) and air (14 l/min) Obese (BMI 30.0-34.9 kg/m ) Pulmonary complications
Primary Anastomic: through above face mask. 2 Intervention: 30% [42%] monitored by clinical exam
Intervention: 31/102 (30%) hrs. after surgery, Control:26% [36%] (attending physician),
Control: 41/111 (37%) supplemental O2 was Morbidly Obese (BMI 35.0 including chest radiographs
2
Other surgeries: administrated according to kg/m ) or computed tomography
Intervention: 62/102 (61%) clinical practice Intervention: 33% [49%] evaluated by radiologist
Control: 41/111 (56%) Control:30% [48%] blinded to allocation
Acute procedures: Monitoring Intervention: Pulse Follow-Up: visit conducted
Intervention: 19/102 (19%) oximetry Per-protocol analysis (N= between postoperative day
Control: 20/111 (18%) Standard Preventative 167) of primary and 13 and 30. Most outcomes
Operation Classification Measures: secondary outcomes measured at 14 days post op
Clean: 36 (35%) Analgesia: epidural showed results similar to except for mortality at
Clean Contaminated: 21 Normothermia: ensured adequate those in the ITT analysis 30days.
(21%) temperature (N=213): Funding Source Conflicts:
Contaminated: 43 (42%) Glycemic: ensured adequate SSI-per protocol analysis Authors: None
Dirty-infected 2 (2%) glucose control Intervention: 31/91 (34%) Institution: None
AMP: appropriate and timely Control: 24/76 (32%) Study: None
Indications: prophylactic antimicrobials P=0.73. Supplies: None
Cancer Diagnosis Received Adequate AMP
Intervention: 56/102 (57%) Intervention n=90(88%) Other infections:
Control: 57/111 (51%) Control n=91 (82%) Pneumonia (Follow up 14
Other: days)
Intervention: 46/102 (45%) Received Timely AMP Intervention:5.9%
Control: 54/111 (49%) Intervention n=64 (63% ) Control: 4.5%
Control n=75 (71%) Obese:6%
Setting: Multi-Center Bowel Prep: absence of Morbidly obese: (3%)
Location: Denmark preoperative oral bowel prep
Dates of Study: October 8, Fluids: Given only once to replace Reoperation: n=43(20%);
2006 - October 6, 2008 measured or calculated deficits Intervention: 22/102 (22%)
Inclusion Criteria: 18 years aiming at body weight increase Control: 21/111 (19%)
or older, BMI 30kg/m ,
2
of less than 1kg. Blood loss Reoperation for SSI n=24
scheduled for acute or was replaced 1:1 with colloids (11%)
elective laparotomy and blood transfusion was Debridement n=5 (2%)
Exclusion Criteria: Inability initiated if blood loss exceeded Length of stay:
to give informed consent, 20ml/kg Intervention: 6 (1-35) days
chemotherapy for Control: 5 (2-45) days
malignancy within 3 30 Day Mortality: Total: 2%
2017 American Medical Association. All rights reserved. 346
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
months, surgery Intervention: 1/102 (1%)
performed under general Control: 3/111 (2.7%)
anesthesia within 30 Adverse Events:
days, preoperative arterial Any adverse event
oxygen saturation less Intervention: 52/102 (51%)
than 90% w/o Control: 58/111 (52%)
supplemental oxygen Wound related:
assessed by pulse Intervention: 18/102
oximetry. (18%)
Control: 20/111 (18%)
Any serious event:
Intervention: 22/102 (22%)
Control: 22/111 (20%)
Sepsis
Intervention: 4/102
(3.9%)
Control: 3/111 (2.7%)
Pulmonary Complications:
Not significantly different
Atelectasis (Follow up 14
days postop)
Intervention: 9/102(8.8%)
Control: 7/111 (6.3%)
Obese:9%
Morbidly Obese:5%
Respiratory Failure(Follow up
14 days postop)
Intervention: 8/102 (7.8%)
Control: 5/111 (4.5%)
Obese: 6%
Morbidly obese:5%
Anastomotic leak
Intervention: 2/31 (6%)
Control: 2/41 (5%)
Rupture of abdominal fascia
15/213 (7%) of patients had
ruptured abdominal fascia
compared with 9/658 (1%) of
normal weight patients in
2017 American Medical Association. All rights reserved. 347
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
PROXY trial
Intervention: 9/102 (9%)
Control: 6/111 (5%)
Admission to ICU (within 14
days if not part of normal
routine care)
Intervention: 11/102 (10%)
Control: 9/111 (8%)
Turtiain- RCT To test the Number of patients: N=274 Intervention: n=137 SSI Definitions:
en 1, 2, 4, hypothesis Patient Characteristics: Postop: 30% FIO2 was delivered Total SSI: 63/ 274 (23%) SSI CDC definition
102
2011 6, 7, that Characteristics were via face mask in the recovery Superficial: 47/63 (74%) Surgical wound infection (SWI)
st
(ES) 8, 9 supplemental analyzed and not found to room and on the 1 Deep: 14/63 (22%) was considered infection if
nd
postoperative be statistically different postoperative day. On the 2 Organ/Space: 2/63 (3%) there were bacteria isolated
oxygen between groups. postoperative day from the wound or if there
decreases the Characteristics reported supplemental oxygen was Intervention vs. Control SSI: were areas of localized
incidence of below are for the delivered via nasal cannula at Intervention: 25/137 patients redness, heat, swelling and
Surgical intervention a constant flow rate of 5l/min. (18.2%) pain around the wound
Wound Age: 18 (Mean: 73.5 [SD Timing of Intervention: Control: 38/137 patients appearing w/in 30 days after
Infection 11]) Postoperatively (27.7%) operative procedure.
(SWI) after Gender (m/f): 78/59 Duration of Treatment: P=0.06 Surgical wounds evaluated by
lower limb Obesity: From the end of surgery until Multivariate vascular surgeon blinded to
2 nd
revascularizati BMI, mean: 26 kg/m (SD 4) 10PM on 2 postoperative day OR 0.56 (95% CI, 0.30-1.04; study arm.
on Co-Morbidities: (at least 48hrs)Device: P=0.07) Pneumonia: clinical diagnosis
st
Coronary artery disease: A face mask for the 1 day to Superficial SSI: and correlative changes in
2
65 (47%) deliver 30% O . Intervention: 18/137 (13%) chest x-ray film
nd 2
Diabetes: 50 (36%) On 2 postop day, FIO delivered Control: 29/137 (21%)
Hypertension: 89 (65%) via nasal cannula. Deep SSI: Perioperative Care:
Rheumatoid arthritis: 7 Monitoring Intervention: Intervention: 7/137 (5.1%) Shaving around intended
(5%) Oxygen level of a toe on operated Control: 7/137 (5.1%) surgical wound site done in
COPD: 13 (9%) limb measured w/ pulse Organ/Space SSI (vascular operating room just before
st
Asthma: 11 (8%) oximeter every 4 hours for 1 2 graft) surgery.
Dialysis: 5 (4%) days. Intervention:0/137 (0% Other notes:
Current smoking: 37 (27%) Control: 2/137 (3%) Primary study design was to
Blood loss (ml [SD]): 341 Control: n=137 deliver supplemental oxygen
(337) Postop: Breathed room air Factors associated w/ SSI via face mask for the first two
(multivariate analysis) postoperative days but
Procedure: N=274 Standard Preventative Prosthetic material use patients found the face
Non-emergency, lower limb Measures: 0.02 (95%CI 0.08-0.50) masks to be uncomfortable
arterial surgery AMP: Antimicrobial prophylaxis p=0.001 so the initial plan was
2017 American Medical Association. All rights reserved. 348
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
(revascularization) was standardized to 3g Asthma changed 2 weeks after data
- 173 bypass procedures cefuroxime via IV w/in 1h 4.83 (95%CI 1.72-13.53) collection had started.
44/173 (25%) prosthetic before incision. If operation > p=0.003
grafts 4h or blood loss>1,500ml then Infrainguinal incision Whether patient received AMP
Femoral endarterectomy another 1.5g Cefuroxime was 2.24 (95%CI 1.07-4.67) per protocol or not, did not
n=84 administered. p=0.03 affect incidence of SWI.
Femoral bypass n=12 AMP per protocol: n=244 (89%) Coronary Artery Disease
Femoropopliteal bypass No AMP n=4 1.94 (95%CI 1.04-3.62) Follow-Up: For 30 days or until
n=92 Received 1.5g cefuroxime n=10 p=0.04 the SWI healed
Crural bypass n=46 Treated for infected ulcer n=11 Supplemental oxygen Funding Source Conflicts:
Pedal bypass n=19 Treated for UTI n=3 0.56 (95%CI 0.30-1.04) Authors: NR
Embolectomy n=3 Treated for sepsis n=2 p=0.07 Institution: NR
Other n=18 Sub-group analysis Study: NR
Operative area 103 patients w/ inguinal Supplies: NR
Inguinal:n-105 (isolated groin) incision
Infrainguinal: n=169 only
Indications: SSI
Claudication: 94/ 274 Total SSI 15/103 (15%)
(34%) Intervention: 3/52 (6%)
Rest pain: 68/ 274 (24.8%) Control: 12/51 (24%)
Ischemic ulcer: 100/274 P=0.01
(36.5%) No differences in secondary
Other: 7//274 (4.4%) outcomes between groups
in the sub-group analysis
2
Setting: 5 Secondary BMI>25kg/m was
referral hospitals & 1 independent risk factor for
tertiary referral hospital SWI
Location: Finland OR 1.22, 95%CI 1.03-
Dates of Study: May 2009- 1.45;P=0.02
February 2010 Supplemental oxygen was
(Varied between 3 and 6 associated with reduced
months between 6 risk
hospitals.) OR, 0.20, 95%CI, 0.04-
Inclusion Criteria: 0.95;P=0.04
Adult patients who Other infections:
underwent non-emergency Pneumonia: p=0.18
lower limb arterial surgery Intervention: 1/137 (0.7%)
Exclusion Criteria Control: 4/137 (2.9%)
Refusal to participate,
2017 American Medical Association. All rights reserved. 349
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
hypercapnic chronic Topic-specific outcomes:
obstructive pulmonary Mean toe tip oxygen
disease (COPD), or oxygen saturation after surgery.
saturation less than 90% Was not significantly
measured by a finger pulse different between 2 groups
oximeter when breathing except at:
room air. 24hrs after surgery
Intervention: 94.4%
Control: 91.9%
P=0.034
28hrs after surgery
Intervention: 95.0%
Control: 92.4%
P=0.025
Reoperation:
58/63 (92%) SSI patients
were cured with
treatment2/63 (3%) SSI
patients required limb
amputation due to SSI (one
study one control group)
Length of Stay:
Postoperative stay
Intervention: 6.5d (SD9.4)
Control: 5.4d (SD4.3)
P=0.13
Mortality: at 30 days
Intervention: 3/137 (2.2%)
Control: 1/137 (0.7%)
Cause of death:
1 aspiration pneumonia
3 myocardial infarction (MI)
including one intervention
patient died from an MI on
POD#30 and SWI had not yet
healed,
3 had no SWI at the time of
death
2017 American Medical Association. All rights reserved. 350
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Of note: 1 control group
patient died of renal failure on
POD#64 and had a SWI not
cured at the time of death
Adverse Events
Graft Thrombosis: p=0.39
Intervention: 5/137 (3.6%)
Control: 8/137 (5.8%)
Cardiac complication: p=0.81
Intervention: 6/137 (4.4%)
Control: 5/137 (3.6%)
Stroke: p=0.08
Intervention: 3/137 (2.2%)
Control: 0/137 (0%)
Renal insufficiency: p=0.31
Intervention: 3/137 (2.2%)
Control: 1/137 (0.7%)
Bickel RCT To assess the Number of patients : Intervention: n= 107 SSI Definitions:
92
2011 1, 2, 3, influence of N=210 Intraop: FIO2 80% combined with Total SSIs: 20/210 (9.5%) SSI: Evaluated clinically
(ES) 4, 5, 6, hyper- Patient Characteristics: No 20% air. Intervention: 6/107 (5.6%) according to obvious signs
7, 8 10 oxygenation statistically significant Postop: In recovery room, flow Control: 14/103 (13.6%) and symptoms such as local
on surgical difference in rate was 10L/min (high-flow) P=0.04 induration & erythema,
site infection characteristics between for 2 hours via non-rebreathing purulent discharge & need to
by using the the 2 groups. (Including mask. SSI by patient subgroup explore the wound.
most smoking history, obesity, Timing of Intervention: Normal appendix (n=9) Supportive results included
homogeneous shaving, and timing of Intra- & post-operatively Intervention: 0/4 increased white blood cell
study antimicrobial Duration of Treatment: Control: 0/4 count, fever, and radiological
population: administration). All From Induction of anesthesia to 2 P >.99 evidence of infectious
single patients categorized as hours post-operatively collections, positive culture
diagnosis having ASA score of 1 or Device: Nasal cannula for control Acute appendicitis (n= 35) findings and resolution of
(acute 2. and nonrebreathing mask with Intervention: 2/18 (11%) mild infectious findings
appendicitis) Age, years: 28.0 (SD 11.5; a reservoir for the intervention Control: 0/17 following antimicrobial
using 1 range 15-71) Monitoring Intervention: P=0.20 treatment.
standard Gender (m/f): 152/57 Pulse oximetry during anesthesia ASEPSIS score taken
surgical Obesity: NR & recovery period. Arterial Phlegmonous appendicitis
approach Co-morbidities (out of blood obtained after (n=123) Perioperative Care:
(open n=210) anesthesia induction & during Intervention: 1/63 Anesthesia introduced with
appendectomy Ischemic heart disease: surgery and 2 hours after Control: 6/60 fentanyl citrate, propfol, or
through a 3.1% recovery from anesthesia. P=0.049 thiopental sodium, and
2017 American Medical Association. All rights reserved. 351
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
McBurney Hypertension: 7.4% Surgical wounds evaluated daily. rocuronium bromide or
incision in the Diabetes: 0.6% After discharge, evaluation Gangrenous appendicitis atracurium besylate following
right lower Pulmonary disease: 1.3% was done at surgical outpatient (n=43) pre-oxygenation via mask.
quadrant of Procedure: Open clinic by senior surgeon w/in 2 Intervention: 3/22 (13.6%) It was maintained with nitrous
the abdomen). appendectomy through a weeks of surgery Control: 8/21 (38.1%) oxide and oxygen,
McBurney incision in the P=0.06 isofluorane, 1% rocronium
right lower quadrant of the Control: n=103 bromide, or atracurium
abdomen Intraop: FIO2 30% O2 combined ASEPSIS Score besylate, and fentanyl citrate.
Indications: acute with 70%N. Satisfactory Healing Other Notes:
appendicitis diagnosed by Postop: In recovery room, flow Intervention: 101 (94.4%) Preoperative SSI Risk
clinical criteria (right lower rate was 4L/min for 2 hours. Control: 89 (86.4%) Stratification:
quadrant pain, local Standard Preventative Disturbance of healing SENIC & NNIS
tenderness, etc.), blood Measures: Intervention: 2 (1.8%)
test results & results of Antimicrobial prophylaxis-: Control: 5 (4.9%) They note that while the rate of
imaging modalities Preoperative antimicrobials: Minor wound infection: SSI reached statistical
(ultrasonography or aminoglycosides (gentamicin Intervention: 2 (1.8%) significance (P=0.04), using
abdominal computed sulfate) and metronidazole. Control: 3 (2.9%) the 2-tailed Fisher exact test
tomography) suggestive When intraoperative findings Moderate wound infection: will lead to a P=0.06
of acute appendicitis indicated gangrenous or Intervention: 2 (1.8%) Follow up: 14 days for SSI,
Setting: Department of perforated appendicitis, Control 5 (4.9%) then length of hospital stay
surgery in a Government antimicrobial treatment lasted Severe wound infection: Funding Source Conflicts:
Hospital 5 days. Intervention: 0 (0%) Authors: None
Location: Israel Fluids: Adequate hydration was Control 1 (1.0%) Institution: None
Dates of Study: November strictly maintained during the ASEPSIS Score: A significant Study: None
1, 2006 May 31, 2009 operation and convalescence difference was recorded Supplies: None
Inclusion Criteria: Ventilation: mechanically between the two study
Adults (>15 years) with controlled at a frequency and populations (P=0.03)
acute appendicitis having tidal volume to maintain Wound problems
open appendectomies normocapnea. Intervention: 6/ 107 (5.6%)
Exclusion Criteria Normothermia: Core temperature Control: 14/ 103 (13.6%)
Chronic obstructive was strictly maintained during Other infections: NR
pulmonary disease, severe the operation and Topic-Specific outcomes:
malnutrition (serum albumin convalescence Partial pressure of oxygen
conc. <3g/dL) or Wound closure: Following (PO2) in arterial blood: mean
immunodeficiency disease resection of inflamed appendix, (SD);P-value
the surgical wound in the lower Before starting surgery:
right quadrant of the abdomen Intervention: 263.30 (87)
was meticulously irrigated and Control: 179.95(78)
sutured with absorbable P=0.001
2017 American Medical Association. All rights reserved. 352
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
sutures. Skin was closed with During surgery before wound
metal clips (including cases of closure
gangrenous appendicitis). Intervention: 275.47 (95)
Control: 149.37 (48)
P=0.001
In recovery room
Intervention 188.6 (73)
Control 142.3 (65)
P=-0.02
Reoperation:
Wound exploration 12/20
SSIs
Intervention: 4/6 (66.7%)
Control: 8/14 (57.1%)
P>0.99
Length of stay: mean (SD)
Total: 2.71 days (1.25)
Intervention: 2.51 days (0.88)
Control: 2.92 days (1.05)
P=0.1
Mortality: NR
Adverse Effects: NR
Meyhoff RCT To assess Number of patients: N = Intervention: n=690 in per SSI: Follow up 14 days Definitions:
94
2009 1, 2, 3, whether use of 1395 in per protocol protocol analysis. 685 in Intervention: 131/685 (19.1%) SSI: CDC definitions
(ES) 4, 5, 6, 80% oxygen analysis. 1386 in intention intention to treat analysis Control: 141/701 (20.1%) Pneumonia- CDC Criteria
7, 8, 9, reduces the to treat analysis Intraop: 100% FIO2 at induction of Univariate OR (NNIS)
10 frequency of Patient characteristics: anesthesia until intubation. 0.94 (95%CI 0.72-1.22) Respiratory failure - the need for
surgical site Pre-operative and Then 80% FIO2 from intubation p=0.64 controlled ventilation or
infection perioperative until the end of surgery. Adjusted OR arterial oxygen saturation
without characteristics compared Postop: The first two hours 0.91 (95%CI 0.69-1.2) p=0.51 below 90% despite
increasing the and no statistically following intubation patients supplemental oxygen
frequency of significant difference received 80% FIO2 via a Infection Location: BMI: <30 or 30 calculated as
pulmonary found between groups. nonrebreathing mask with a Superficial: weight in kg divided by height
2
complications (data below listed for reservoir w/ a flow of 14L O2 & Intervention: 75/131 (57.3%) in m
in patients intervention) 2L air per minute Control: 76/141 (53.9%) Risk of SSI assessed with NNIS
undergoing Age: (median(5-95%)) : 64y Timing of Intervention: Deep and SENIC.
abdominal (27-85) Intra & Postoperatively Intervention: 20/131 (15.3%)
surgery Gender: Duration of Treatment: From Control: 26/141 (18.4%) Perioperative Care:
2017 American Medical Association. All rights reserved. 353
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
(laparotomy). Men (no (%)): 228/690 induction of anesthetic to 2hrs Organ/ Space (Intra- Standardized inhalational or
(41.7%) postop abdominal) intravenous anesthesia
Obesity: Device: High concentration Intervention: 36/131 (27.5%) without nitrous oxide
BMI, median (5-95%): oxygen mask Control: 39/141 (27.7%) depending on attending
2
25kg/m (18-35) Monitoring Intervention: Pulse anesthetist.
BMI30, no (%): 102/690 Oximetry ASEPSIS Score>20: Other notes:
(14.8%) Intervention: 32(4.7) Adjusted OR adjusted for study
Comorbidity: Control: n=705 in per protocol Control: 36 (5.1) center, BMI (<30 or 30),
Current smoker: 207/690 analysis. 701 in intention to Per protocol analysis diabetes mellitus, acute or
(30.0%) treat analysis (N=1081) elective surgery, COPD,
Alcohol consumption Intraop: 100% FIO2 at induction of SSI current smoker, incision
>48g/d: 29/690 (4.2%) anesthesia until intubation. Intervention: 122/555 (22.0%) extending above umbilicus,
Previous abdominal Then 30%FIO2 from intubation Control: 116/526 (22.1%) duration of surgery, and age
surgery: 298/690 (43.2%) until end of surgery. P=0.98 (40 years or <40 years)
Diabetes mellitus 51/690 Postop: During the first two hours Follow-Up: SSI monitoring for
(7.4%) after surgery, patient received Other infections: 14 days, Then postop day
COPD: 35/690 (5.1%) O2 via Nonrebreathing mask w/ Pneumonia: (14 days) 13-30 via telephone if
Other pulmonary disease: a flow of 14L air & 2L O2 per Intervention: 41/685 (6.0%) necessary
45/690 (6.5%) minute. Control: 44/701 (6.3%) Funding Source Conflicts:
Hypertension: 209 (30.3%) Univariate OR Authors: None
Other cardiovascular In both groups FIO2 was 0.95 (95%CI 0.61-1.48) Institution: None
disease: 125/690 (18.1%) increased if hypoxia was p=0.82 Study: None
Current signs of infection: detected or suspected to Adjusted OR Supplies: None
76/690 (11.0%) ensure arterial oxygen 0.95 (95%CI 0.60-1.49)
Immune deficiency: 27/690 saturation >94% and arterial p=0.81
(3.9%) oxygen tension >9kPa.
Other disease209/690 Topic Specific outcomes:
(30.3%) Standard Preventative NR
Procedure: (N=1386) Measures: Reoperations: For all
Colorectal: 633/1386 Analgesia - Epidural reasons- does not specify
(45.7%) Normothermia: control of how many for SSI
Gynecological: 268/1386 temperature Intervention: 104/685 (15.2%)
(19.3%) Glycemic: Control of glucose level Control: 104/701 (14.8%)
Small Bowel surgery: Bowel Prep: absence of pre- Length of stay:
158/1386 (11.4%) operative bowel preparation. Postoperative
Appendectomy: 124/1386 AMP: first and second hospitalization (Mean?
(8.9%) antimicrobial administered w/in (range))
Other: 203/1386 (14.6%) 60 minutes of skin incision. Intervention: 6d (1-34)
Operation Classification: Cefuroxime & metronidazole Control: 7d (2-36)
2017 American Medical Association. All rights reserved. 354
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Clean: 318/1386 (22.9%) given intravenously was OR -0.69 (-2.3-0.93) P=0.09
Clean-contaminated: Mortality: at 30 days
standard choice, but ampicillin
796/1386 (57.4%) or benzylpenicillin in Intervention: 30/685 (4.4%)
Contaminated: 235/1386 combination with gentamicin Control: 20/701 (2.9%)
(17.0%) and metronidazole were also Univariate OR
Dirty-Infected: 37/1386 allowed. 1.56 (95%CI 0.88-2.77)
(2.7%) 1305/1386 (94%) received p=0.13
AMP. Adjusted OR
Indications: (# of Of those that received AMP: 1.55 (95%CI 0.86-2.85)
patients/1386) 1169/1305 (90%) p=0.15
Cancer: 714 (51.5%) Appropriate AMP Adverse Effects: Wound-
Benign neoplasm: 108 880/1305 (67%) Timely related, UTI, Postoperative
(7.8%) AMP nausea or vomiting,
Appendicitis: 121 (8.7%) respiratory, circulatory,
Intestinal obstruction due to Fluids: given only to replace gastrointestinal tract,
benign disease: 124 measured or calculated deficits sepsis, or other recorded
(8.9%) aiming at a post-op weight and not statistically
Inflammatory bowel disease: increase of less than 1kg different between groups.
79 (5.7%) Transfusion: blood replaced 1:1
Diverticulitis: 57 (4.1%) with colloids & transfusion Topic specific outcomes
Other: 183 (13.2%) initiated if blood loss exceeded Hypoxia: NR
Setting:14 Hospitals 20 mL/kg. Atelectasis: (14 days)
Location: Denmark Intervention: 54/685 (7.9%)
Dates of Study: Oct 2006- Control: 50/701 (7.1%)
Oct 2008 Univariate OR 1.11 (95%CI
Inclusion Criteria: Patients 0.75-1.66) p=0.60
18yrs who underwent Adjusted OR
acute or elective 1.13 (95%CI 0.75-1.72)
laparotomy. (When p=0.56
laparotomy was indicated
for gynecological disease, Respiratory Failure (14 days)
only patients with Intervention: 38/685 (5.5%)
suspected malignancy Control: 31/701 (4.4%)
[risk of ovarian OR 1.27 (95% CI, 0.78-2.07)
malignancy index>200 or P=0.34
a specimen showing Adjusted OR 1.22 (95%
atypical or neoplastic CI,0.74-2.03)
cells] were included.) P=0.44
Exclusion Criteria:
2017 American Medical Association. All rights reserved. 355
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Operations performed Admission to ICU (other than
under general anesthesia normal postop-not
w/in 30 days, statistically significant
chemotherapy for
malignancy w/in 3
months, inability to
provide informed consent,
and preoperative arterial
hemoglobin oxygen
saturation below 90%
without supplemental
oxygen assessed by
pulse oximetry
Gardella RCT To test the Number of patients: Intervention: n=69 SSI: Follow up 14 days Definitions:
98
2008 1, 2, 3, hypothesis N=143 80% Oxygen at 15L/min Intervention: 17/69 (25%, 15- SSI: Administration of
(ES) 4, 5, 6, that high- Patient characteristics: Timing of Intervention: 35%) intravenous antimicrobials for
7, 8, 9, concentration, The study groups were Intra and post-operatively Control: 10/74 (14%, 6-22%) postpartum endometritis or
10 inspired similar for a large number Duration of Treatment: Relative risk of outcome oral and intravenous
oxygen of clinical variables, From anesthesia induction to 2hrs associated with High O2 antimicrobial for wound
delivered including body mass post-operatively. 1.8 (95%CI, 0.9-3.8)P=.12 infection during the initial
during index, maternal diabetes, Device: Covered oxygen blender Cellulitis: hospital stay or within 14
cesarean group B streptococcus was set to predetermined Intervention: 10/69 (14%) days of surgery. Included
delivery and colonization, gestational mixture of O2 & air to an adult Control: 7/74 (9%) cellulitis as well as deeper
for 2 hours age at delivery, and nonrebreathing mask RR (95%CI): 1.5 (0.6-3.8) incisional infections that
postoperativel duration of surgery, Monitoring Intervention: p=.44 required wound to be
y decreases surgical blood loss & Venous Blood Gas collection from Postpartum endometritis: opened.
the incidence prophylactic usage of the dorsum of the foot in a Intervention: 9/69 (13%)
Endometritis: Fever 38.5 C
o
of surgical site antimicrobials. subset of the high-oxygen Control: 5/74 (7%)
infection Though not statistically group RR (95%CI): 1.9 (0.67-5.5) within the first 24 hours
o
significant, more patients p=.26 postpartum or>38.0 C for at
with diabetes mellitus were Control: n=74 Wound separation: least 4 hours after the first 24
randomized to the 30% oxygen at 15L/min Intervention: 5/69 (7%) post-partum associated with
intervention group. Control: 2/74 (3%) uterine tenderness greater
Hypertensive disorders Standard Preventative RR (95%CI): 2.7 (0.5-13.4) than expected without other
were more prevalent in Measures: p=.26 identified fever sources
the control group. Skin Prep: Routine surgical (Ernest 2000)
Age: 16-47 y preparation with betadyne Subanalysis of SSI risk Relative Risk Adjustment-
Gender: 100% female scrub. factors: adjusted for gestational or
Obesity: AMP: All but one received Surgical blood loss chronic hypertension
2017 American Medical Association. All rights reserved. 356
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
BMI median (range): 32 prophylactic antimicrobials. 97 Intervention: 900cc (range, Perioperative Care:
2
kg/m (22-51) received it at cord clamp; 45 600-1250) Regional not general anesthetic
Comorbidities: NR received it at case start. Control: 800cc (range, 300- (standard for cesarean
Procedure: Cesarean 1500) section delivery)
section P=0.04 Other notes: The P-value
Indications: Not Recorded All other factors not exceeded the P-value for
Setting:1 University Hospital statistically significant, futility suggesting these
Location: USA including Intraoperative differences were unlikely to
Dates of Study: October partial pressure of venous reach statistical significance
2001 April 2007 oxygen mean and range with continued recruitment.
Inclusion Criteria: Women (P=0.91) and intraoperative The study was ended early
who underwent a clinically partial pressure of venous Eight documented protocol
indicated caesarian oxygen >200mmHg or deviations occurred in each
delivery after the onset of 200mmHg (P=0.76) group, most due to
labor or rupture of Other infections: NR intermittent mask use due to
membranes Topic Specific outcomes: nausea/vomiting during
Exclusion Criteria: Venous Oxygen saturation, surgery or patient request
Cesarean delivery before median % (range) post-partum to facilitate infant
the onset of labor or Intervention: 99 (23-99) bonding.
rupture of membranes, Control: 99 (57-99) Follow-Up: 14 days- All
emergent cesarean P=0.006 participants followed
delivery, general Partial pressure of venous throughout hospitalization; of
endotracheal anesthesia oxygen, median mm Hg those without SSI during
(those who started with (range) initial hospitalization, 7
regional anesthetic and Intervention: 177 (20-449) controls and 2 interventions
converted to general were Control: 122 (20-449) were lost to 2 week
not excluded), clinical P=0.001 postpartum follow up (they
chorioamnionitis, & HIV Surgical Estimated Blood were kept in analysis and
infection Loss: median (range) considered to not have an
Intervention: 900cc (600- SSI)
1,250)
Control: 800cc (300-1,500) Funding Source Conflicts:
p=.04 Authors: None
Reoperation: NR Institution: None
Length of stay: days median Study: None
(range) Supplies: None
Intervention: 3 (2-5)
Control: 3 (2-6)
p=.92
2017 American Medical Association. All rights reserved. 357
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Mortality: NR
Adverse Events:
Readmission:
Intervention: 3/69 (5%)
Control: 2/74 (4%)
RR (95%CI): 1.4 (0.2-8.4)
p=.99
Intravenous antimicrobial
treatment:
Intervention: 10/69 (14%)
Control: 5/74 (7%)
RR (95%CI): 2.1 (0.8-6.0)
p=.17
Belda RCT To test the Number of patients: N= Intervention: n=148 SSI (Follow up 14 days) Definitions:
91
2005 1, 2, 3, hypothesis 291 Intraop: At intubation-Oxygen/ air Total: 57/ 291 (39.3%) SSI
(ES) 4, 5, 6, that Patient Characteristics: mixture with an FIO2 of 80%. Positive cultures for CDC definitions
7, 8, 10 supplemental Morphometric, demographic, Intraop: At extubation increased pathogenic bacteria: 50/57 Surgical wounds assessed daily
oxygen & other preoperative to 100% at extubation. Intervention: 22/ 148 (14.9%) by blinded surgeon. Purulent
reduces characteristics were Postop: First 6hrs non- Control: 35/ 143 (24.4%) exudates were cultured &
infection risk similar in the 2 treatment rebreathing facemask with Analysis for increased risk of when positive for pathogenic
in patients groups. reservoir with oxygen SSI bacteria, appropriate
following Except that intervention was administered at the randomly 80% FIO2 Unadjusted antimicrobial given.
elective shorter in height & had designated concentration univariate Wound Healing
colorectal more women. (80%) at a total flow of 16L/min RR, 0.61; 95%CI 0.38-0.98; Evaluated using ASEPSIS score
surgery Age: Specifics NR = 18-80 Postop after 6 hours-ambient air P=0.04 (>20 =infection)
years with supplemental oxygen 80%FiO2: Adjusted Respiratory Disease- - history of
Gender: m/f provided as necessary to multivariate COPD, asthma requiring routine
Intervention: 71/77 maintain pulse oximetry of at RR 0.46; CI 95%, 0.22-0.95; medication or other clinically
Control: 91/52 least 92% P=0.04 important respiratory
Obesity: Timing of Intervention: Intra and (Risk of SSI reduced 54%) impairment.
BMI: mean (SD): postoperatively Coexisting Respiratory Perioperative Care:
Intervention: 27.1 (4.5) Duration of Treatment: disease: Anesthesia induction &
Control: 26.5 (3.8) From anesthesia induction until 6 Unadjusted univariate treatment were standardized
BMI> 30: hours postoperatively. RR 2.15 (95% CI, 1.03-4.48) across all patients.
Intervention: 26/148 Device: Intraop- intubated; Post- Adjusted multivariate Blinded attending surgeon
(17.5%) op= non-rebreathing face RR 3.23 (95% CI, 1.18-8.86) administered analgesic
Control: 21/143 (14.9%) masks w/ a reservoir. P=0.04 agents, determined initiation
Other than percentage of Monitoring Intervention: ASEPSIS Score >20 on any of feeding, ambulation & the
inspired FIO2 and FIO2, pulse oximetry were postoperative day: duration of hospitalization.
2017 American Medical Association. All rights reserved. 358
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
resulting PaO2 there were continuously monitored during Intervention: 25 (16.9%) Other notes:
no significant differences the surgery and in the recovery Control: 37 (25.9%) Preoperative SSI Risk
between the groups for room. P = 0.06 Stratification:
>30 other potential intra Arterial blood sample obtained 1h Other infections: NR SENIC 1/2/3: (%)
or postoperative after anesthesia induction to Topic specific outcomes: Intervention: 19.4/64.2/16.2
confounding factors. evaluate PaO2; another was Partial (arterial) pressure of Control: 15.4/74.1/10.5
Comorbidities: again 2 hours after intubation. oxygen: 1h postinduction in NNIS 0/1/2: (%)
Respiratory disease: Control: n= 143 mm Hg: Intervention: 16.9/58.1/25.0
Intervention: 25/148 Intraop: At intubation Oxygen/ air Intervention: 285.9 (96.6%) Control: 12.6/68.5/18.9
(17.1%) mixture with an FIO2 of 30% Control: 117.5 (40.6%)
Control: 16/143 (11.2%) Intraop: At extubation increased P<0.05 True ITT analysis was not
PaO2 mmHg 1h post- to 100%. Partial (arterial) pressure of possible cause of incomplete
induction Postop: First 6hrs non- oxygen: 2h postinduction: follow up date so they
Intervention: 285.9 (96.6%) rebreathing facemask with Intervention: 233.7 (89.7%) conducted a sensitivity
Control: 117.5(40.6%) reservoir with oxygen Control: 125.4 (49.0%) analysis based on treatment
P<0.05 administered at the randomly P<0.05 group assignment that
PaO2 mmHg 2h post- designated concentration included all patients except 4
induction (30%) at a total flow of 16L/min Reoperations: NR who should have been
Intervention: 233.7 (89.7%) Postop after 6 hours-ambient air Length of stay: excluded because 2 had
Control: 125.4 (49.0%) with supplemental oxygen Intervention: 11.7 days (7.0) laparoscopic surgery and 2
P<0.05 provided as necessary to (SD??) had low preop albumin
Excepting post-op maintain pulse oximetry of at Control: 10.5 days (4.4) Follow-Up: 14 days after
hemoglobin, all other least 92% P=0.09 surgery
physiological variables, Mortality: Funding Source Conflicts:
lab test results dada, Standard Preventative Control: 2 died of multi-organ Authors: None
ASEPSIS index & Measures: failure of septic origin Institution: None
extrinsic infection risk Mechanical Bowel Prep: using an Adverse Events Study: Industry
factors were similar electrolyte solution w/ no ICU Admission (not planned): Supplies: Industry
between groups. antimicrobials or antiseptics Intervention: 4/148 (2.7%)
Postop hemoglobin: mean AMP: w/ metronidazole plus Control: 5/143 (3.5%)
rd
(SD) g/L cefoxitin or a 3 generation P=0.74
Intervention: 11.0 (1.2) cephalosporin was
Control: 11.5 (2.5) administered 60-90 minutes
P< 0.05 before the surgical incision &
continued postoperatively for
Procedure: Colorectal up to 48 hours.
surgery Aminoglycosides used as an
Total or subtotal alternative to -lactam
colectomy: 11/291 (3.8%) antimicrobials in patients who
2017 American Medical Association. All rights reserved. 359
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Hemicolectomy: 89/291 reported cephalosporin allergy
(30.6%) history.
Rectum resection with Type and duration of AMP in first
abdominal-perineal repair: 48hrs similar in the two groups.
29/291 (10.0%) Normothermia: Maintained w/
Sigmoid anterior resection: circulating-water mattresses &
87/291 (29.9%) forced-air heaters.
Rectal anterior resection: Fluids: administered
53/291 18.2%) intraoperatively at 15mL/kg per
Other: 22/291 (7.6%) hour; blood loss restored with
crystalloids or colloids &, when
Indications: necessary, w/ leukocyte-
Cancer filtered allogeneic red blood
Intervention: 126/148 cell concentrate. Fluid
(85.8%) administered at 3mL/kg per
Control: 124/143 (86.7%) hour during first 6
Inflammatory bowel disease postoperative hours then
Intervention: 14/148 (9.4%) reduced to 2mL/kg per hour
Control: 10/143 (7%) after transferred to ward.
Other Wound Closure: They were
Intervention: 7/148 (4.7%) covered with conventional
Control: 9/143 (6.3%) gauze bandages. An antiseptic
Setting: 14 hospitals solution was applied to the
Location: Spain surface of the wound but
Dates of Study: March 1, neither intraperitoneal
2003 October 31, 2004 antimicrobials nor antiseptics
Inclusion Criteria: Patients were used.
undergoing elective Analgesic: Patients who reported
colorectal resection post-op pain score of more
(abdominal-peritoneal than 3cm on a 10-cm visual
reconstructions) analog scale (0=no pain, 10=
Exclusion Criteria: Minor worst pain imaginable), patient
colon surgery, was administered an
(polypectomy, isolated intramuscular or IV morphine &
colostomy), laparoscopic non-steroidal anti-inflammatory
surgery, surgery less than drug.
1 hour, fever, existing
signs of infection,
diabetes mellitus type 1 or
2017 American Medical Association. All rights reserved. 360
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
2, HIV, weight-loss >20%
in the previous 3mos,
serum albumin conc. <
30g/L & a leukocyte count
< 2500 cells/mL
Pryor RCT To determine Number of patients: Intervention: n=80 SSI (Follow up 14 days) No Definitions:
97
2004 1, 2, 3, whether the N=160 Intraop: (%) SSI: SSI was assessed by
(ES) 4, 5, 6, routine use of Patient Characteristics: Pre-oxygenation, induction, Overall: 29/160 (18.1%) investigator blinded to
7, 8, 9, high FIO2 Preoperative patient emergence and extubation: Intervention: 20/80 (25%) randomization via a
10 during the characteristics such as FIO2 100% Control: 9/80 (11.3%) retrospective chart review
perioperative sex, age, etc. were Intraop: 80% Oxygen (FIO2 of P = 0.02 looking for SSI criteria being
period alters recorded and not found to 0.80) OR 2.63 (95%CI, 1.1-6.2) met at one of two phases: (1)
the incidence be statistically significant FIO2 could be increased as RR 2.22(95%CI, 1.1-4.6) during hospitalization and (2)
of SSI in a except for BMI, Obesity & required to maintain arterial Multivariate analysis : FIO2 for those discharged in <14
heterogeneou Pulse though they were oxygen saturation >94%. (P=0.03) and staying days without evidence of SSI,
s general not found to be indicators Postop Transport from OR: 80% intubated at the end of then at first postop visit with
surgical of SSI in multivariate Oxygen 10 L/min via closed surgery remained surgeon, any emergency
population in analysis. reservoir bag-mask predictive of infection department visits, telephone
an academic Age: >18y In recovery extubated: 80% calls or other contacts within
setting. Gender: NR Oxygen via a high-flow non- Superficial (Wound only) first 14 days postop.
BMI mean (SD) rebreathing, humidified, Intervention: 13/20 (65%)
Intervention: 27.1 (6.7) aerosol delivery system for 2 Control: 5/9 (56%) SSI Criteria prospectively
Control: 25.1 (5.0) hours P = 0.84 defined:
P=0.04 In recovery intubated: 80% Deep structures 1.surgical team clearly
Obesity: BMI>30, No (%) Oxygen through ventilator for 2 Intervention: 3/20 (15%) documented clinical
Intervention: 19/80 (23.8%) h, then recovery/ICU team Control: 1/9 (11%) assessment of SSI
Control: 9/80 (11.3%) determined therapy P = 0.84 2.SSI precipitated management
P=0.04 Timing of Intervention: Intra and Wound and Deep structures action (changing
Fifteen obese patients had postoperatively Intervention: 4/20 (20%) antimicrobials, opening
BMI<35. No significant Duration of Treatment: During Control: 3/9 (33%) wound, aspiration, drain
difference between surgery and for the first 2 P = 0.84 placement , further surgery
groups if BMI defined as hours postoperatively Time to first detection of 3.clinical assessment supported
>32 or >35 Device: infection by at least 3 of the following
Pulse, beats/min (SD) During Transport: Mean (SD) 5.6(2.4) days objective criteria
Intervention: 83 (14) Intervention: Closed reservoir Other infections: NR prospectively assigned by the
Control: 79 (14) bag-mask system Topic specific outcomes: study:
P=0.04 Control: Nasal cannula Arterial Oxygen Saturation WBC Count>11000L
Temperature>38.5 C
o
Comorbidities: In recovery: high-flow (recovery)
COPD nonrebreathing, humidified, Intervention vs. control Radiological Evidence
2017 American Medical Association. All rights reserved. 361
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Intervention: 0/80 (0) aerosol delivery system with p=0.005 (rank sum of infection
Control: 5/80 (6.3%) selector to provide stable FIO2 analysis) but values for Extrusion of pus from
P=0.06 to the facemask. both groups well within site
Minimum temp ,mean (SD) Monitoring Intervention: Pulse acceptable range (99% Positive culture from site
C oximetry [1%] vs. 98% [2%]) New erythema and
Intervention: 35.5(0.7) Estimated Blood Loss mL induration that
Control: 35.4(0.6) Control: n=80 mean (SD) responded to treatment
P=0.54 Intraop: Pre-oxygenation, Intervention: 230 (180) of infection
Temp at extubation ,mean induction, emergence and Control: 200 (190)
(SD) C extubation: FIO2 100% P = 0.03 Perioperative Care:
Intervention: 36.2 (0.07) Intraop: 35% Oxygen (FIO2 0.35) Crystalloid L: Anesthesia- general-
Control: 36.1 (0.6) Postop Transport from OR: 35% Intervention: 4.5(2.1) heterogeneity in inhalation
P=0.20 Oxygen at 4 L/min (nasal Control: 3.8(1.9) agents used:
Procedure: Colectomy cannula) P=0.02 Isoflurane
(right, left, hemicolectomy In recovery extubated: 35% Blood loss and Crystalloid not Intervention: 68.8%
& sigmoid), low anterior Oxygen at 4 L/min via a high- significant on multivariate Control: 75%
resection, flow nonrebreathing, analysis Sevoflurane
abdominoperineal humidified, aerosol delivery Nitrous oxide 30 min after Intervention: 21.3%
resection, gastrectomy, system. incision mean (SD), Control: 17.5%
pancreaticoduidenectomy In recovery intubated: 35% %vol/vol Desflurane
, exploratory laparotomy, Oxygen through ventilator for 2 Intervention: 5 (10%) Intervention: 10.0%
and large gynecologic h, then recovery/ICU team Control: 21 (30%) Control: 7.5%
staging/ de-bulking determined therapy P=0.008 Other notes:
procedures in which Standard Preventative Preoperative SSI Risk
bowel or peritoneum was Measures: Reoperations: Stratification: NNIS M/0/1/2/3
involved. Bowel prep: regimen undertaken Intervention: 4/80 (5.0%) Intervention: 7/32/35/5/2
Indications: night before surgery according Control: 0/80 Control:9/31/34/6/0
Cancer to surgeons instructions. AMP P=0.06 P=0.94
Intervention: 36/80 choice and timing recorded. Length of stay: mean days
Control: 30/80 AMP: Intravenous antibiotics (SD) NOTE: Initial power analysis
Non-Cancer either immediately before Intervention: 8.3 (7.5) does not indicate baseline
Intervention: 44/80 arriving or upon arrival to Control: 6.4 (4.7) SSI rate. It determined that
Control: 48/80 operating room according to P= 0.07 300 patients were needed for
Setting: University Hospital surgeons usual practice. SSI: 13.3 (9.9) a detectable treatment effect
Location: NYC, USA Received AMP: No SSI. 6.0 (4.2) of 40%. Interim analysis was
Dates of Study: September Intervention: 80/80 (100%) P<0.001 planned to be performed after
2001-May 2003 Control: 78/80 (97.5%) 160 patients recruited and
Inclusion Criteria: Patients P=.26 Mortality study halted if P0.03. This
>18 y old undergoing POD#16 1 Control patient study represents that interim
2017 American Medical Association. All rights reserved. 362
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
major abdominal surgical Admission to hospital: most who developed an analysis, enrollment stopped
procedures under general admitted on morning of incisional SSI, later a deep after statistically significant
anesthesia. surgery. abscess, had a difference in SSI rates
Laparoscopically assisted postoperative myocardial between groups noted.
procedures were eligible infarction, followed by a Follow-Up:
provided that laparotomy stroke and died 14 days
was performed at some Funding Source Conflicts:
point during the surgery. Adverse Events: Authors: None
Exclusion Criteria: Pulmonary embolus: 1 Institution: None
Exclusively laparoscopic Intervention patient had a Study: None
procedures, patients pulmonary embolus on Supplies: None
whose respiratory status POD#3 but recovered
required an FIO2 in without incident
excess of 0.35, patients
with severe chronic
obstructive pulmonary
disease (COPD) who
were likely to experience
respiratory depression at
FIO2 of 0.80 (minor
COPD acceptable),
patients who were
hemodynamically
unstable prior to surgery
(systolic blood pressure
<90mmHg or use of
vasopressors), patients
who had received
bleomycin at any time &
patients who had an ASA
status class 5 or 5E
indicating patient is not
expected to survive 24
hours regardless of the
surgery. Fully
laparoscopic procedures
were excluded.
2017 American Medical Association. All rights reserved. 363
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Whitney RCT To determine Number of patients: N=24 Intervention: n=13 Wound complications: Definitions:
101
2001 1, 10 the effects of Patient Characteristics: Postop: 28% Oxygen delivered at Clinical healing (assessed SSI: Retrospective medical
(ES) 28% oxygen Subjects compared on rate of 2L/min via nasal through self-report and chart review (documentation
given in the coexisting conditions, cannula medical chart review) of wound complications to
first 36 hours smoking history, Timing of Intervention: showed no significant include presenting
after surgery intraoperative & Postoperative after discharge differences between symptoms, wound
on tissue postoperative variables from recovery and admission groups. appearance, culture results [if
oxygen levels, and there were no to surgical unit Self-report: any] and prescribed
collagen statistically significant Duration of Treatment: Total Wound Problems treatment. Follow up phone
deposition, differences between 36 hours postop Control: 13/ 11 calls with patient questioned
and clinical groups. Device: nasal cannula for Intervention: 9/ 13 about wound healing
healing Age: 18-80 years; Mean delivery of the 28% Self-report included notation problems including wound
outcomes. (SD) supplemental oxygen for of any wound problem, appearance and treatment.
Intervention: 41 (9.9) intervention problems with wound Final wound healing
Control: 42 (11.5) Monitoring Intervention: drainage, concerns about classification:
Gender: m/f Subcutaneous tissue oxygen incision redness, problems Primary: no wound edge
Intervention: 69%/31% (PscO2) measured via silastic with incision swelling, separation or other indication
Control: 85%/15% tonometer inserted incision opening, treatment of wound healing problems.
Obesity: subcutaneously in subjects sought for wound Secondary: only if patient
2
Body surface area m :mean dorsal left upper arm after complications, treatment reported partial or complete
(SD) anesthetic induction. prescribed for problem, separation of the wound
Intervention: 2.00 (0.20) Equilibration and baseline and pain at surgical site edges or other indications of
Control:2.05 (0.30) established while patient on that did not decrease over wound healing problems and
Comorbidities: Cardiac room air. Second equilibration time. I also confirmed by medical
History: Yes (p=0.084) at 30 minutes. PscO2 readings Medical Chart Review (30 record documentation
Intervention: 0% recorded at 1, 2, 18, and 36 days)
Control: 7.1% hours postoperatively Complication necessitated SSI not defined, but wound
Procedure: cervical fusion Wound healing evaluated by clinic visit: complications and infections
and/ or excision of hydroxyproline content in a Intervention: 0/13 (at a left or right neck surgical
cervical intervertebral disk subcutaneous Control: 1/11 wound and in some cases a
(neurosurgery or the polytetrafluoroethylene tube Incision redness thigh skin graft)were
th
orthopedic surgery removed on the 7 post-op day Intervention: 1/12 measured by three
services) Control: n=11 Control: 1/8 individuals using the
Indications: NR Room air Incision drainage ASEPSIS scoring method
Setting: Military regional Standard Preventative Intervention: 0/13 (comparisons of the
medical center Measures: NR Control: 1/8 ASEPSIS method with
Location: Pacific Northwest, Incision swelling standard clinical definitions of
USA Intervention: 0/12 wound infection or
Dates of Study: NR (24 Control: 0/8 complications demonstrated
2017 American Medical Association. All rights reserved. 364
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
month period) Other wound problem: that ASEPSIS was as
Inclusion Criteria: Aged 18- Intervention: 1/12 sensitive as and significantly
80 years, male & female, Control: 0/8 more specific than the other
able to read & speak Wound Healing Assessment indicators of wound problems
English, give informed Histology scores for cellularity Perioperative Care: NR
consent, & discharged and presence of Other notes: NR
from the post-anesthesia connective tissue or mean Follow-Up: for 30 days post-op
care unit without amounts of hydroxyproline via medical record review &
supplemental oxygen in the ePTFE implants- No telephone call to the subject
Exclusion Criteria: NR significant difference Funding Source Conflicts:
between control & Authors: None
intervention groups. Institution: None
However, only subjects in Study: None
intervention group Supplies: None
achieved hydroxyproline
levels >0.40g/mm of
ePFTE tubing.
ASEPSIS Scores- all within
satisfactory healing (0-10
out of 20) without
significant differences
between the mean scores.
Wound healing classification:
all primary healing
Other infections: NR
Topic specific outcomes:
Tissue oxygen mean (SD)
Intervention: 63 mm Hg 14
Control: 48 mm Hg 7
P=0.001
No significant effects for time
or for an interaction
between time and group.
Reoperations: NR
Length of stay: NR
Mortality: NR
Adverse Effects: NR
2017 American Medical Association. All rights reserved. 365
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Greif RCT To test Number of patients: Intervention: n=250 SSI (Follow up 15 days) Definitions:
93
2000 1, 2, 3, hypothesis N=500 Intraop: 80% Oxygen and 20% Note: Follow up evaluations SSI:
(ES) 4, 5, 6, that Patient Characteristics: Nitrogen after induction of not completed in 3 patients Likely infected: when pus could
7, 8, 9, supplemental Patient clinical anesthesia and intubation. who withdrew from the be expressed from the
10 administration characteristics, Increased 10 100% during study-they had no known incision or aspirated from a
of oxygen diagnoses, surgical extubation. infections and in analysis loculated mass within the
during procedures, duration of Postop: 80% Oxygen via were considered wound.
perioperative surgery, hemodynamic nonrebreathing mask for 2 uninfected. Infected: Wounds with culture-
period values and use of hours, then room air unless Overall incidence was 8% positive pus
decreases the anesthetic were recorded additional oxygen required to (6% predicted by NNIS Wound Healing and infection
incidence of & analyzed and not found maintain oxyhemoglobin scores) Scoring: ASEPSIS
wound to be statistically concentrations of >92%. Intervention: 13/250 (5.2%) Perioperative Care:
infections in significant between Timing of Intervention: (95%CI, 2.4-8) Was anesthesia: standardized
patients groups except as noted. Intra and Post-operatively Control: 28/ 250 (11.2%) and induced with IV
undergoing Baseline: Duration of Treatment: (95%CI, 7.3-15.1) thiopental sodium (3-5mg/kg
elective Age (y) (SD) Intraop and 2 hours P=0.01 of bodyweight), fentanyl (1-3
colorectal Intervention: 5715 postoperatively. Absolute difference in SSI g/kg) and vecuronium
resection. Control: 5715 Device: Postop-Nonrebreathing rates: 6% bromide (0.1mg/kg) and
Gender (m/f) 280/220 mask sealed to the patients (95%CI, 1.2-10.8) maintained with isoflurane
Obesity: face and connected to a valved adjusted to keep mean
Weight (kg) Mean SD manifold and oxygen blender. ASEPSIS Scores mean SD arterial blood pressure w/in
Intervention: 7417 Monitoring Intervention: Intervention: 37 20% of pre-induction value.
Control: 7217 Intraop: Concentrations of Control: 59 Additional fentanyl administered
Height (cm) Mean SD inspired oxygen and end-tidal P=0.01 to improve analgesia when
Intervention: 17012 isoflurane and carbon dioxide Mixed Effects model: Only patient emerged from
Control: 16912 were measured use of 30% oxygen anesthesia.
Comorbidities: Intraop and postop: Oxygen (controls) correlated Other notes: NR
Smoker saturation measured with pulse significantly with the risk of Preoperative SSI Risk
Intervention: 24% oximeters infection Stratification: NNIS &
Control: 29% Arterial blood was obtained 1h OR 2.3 (95%CI, 1.2-4.6) SENIC (modified)
Intraop: End-tidal isoflurane after induction of anesthesia SENIC 1/2/3 No. patients
concentration-% and 2h postop to measure Analysis SSI (N=41) vs. No Intervention: 71/158/21
Intervention: 0.9024 partial pressure of oxygen. SSI (N=459) Control: 65/165/20
Control: 0.840.24 Control: n=250 ASEPSIS Scores: P=.86
P=0.005 Intraop: 30% Oxygen and 70% SSI: 2513 NNISS 0/1/2-No.patients
Difference clinically Nitrogen after induction of No SSI: 24 Intervention: 132/100/18
unimportant anesthesia and intubation. P<0.001 Control:127/106/17
Procedure: Elective Increased to 100% during WBC (X10-3/mm) mean SD P=0.86
colorectal resection extubation. Preop- not statistically
2017 American Medical Association. All rights reserved. 366
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Colon: Postop: 30% Oxygen via significant difference Initial plan was to study 1000
Intervention: 71% nonrebreathing mask for 2 between groups. patients evaluate results
Control: 63% hours, then room air unless Postop (POD#1, 3, 6, and 9) after 500750 patients
Rectum: additional oxygen required to patients with SSI had enrolled. A priori criterion of
Intervention: 29% maintain oxyhemoglobin statistically significant ending the study after
Control: 37% concentrations of >92%. higher counts (P value enrollment of 500 patients
Subgroup Analysis#1 N=54 (1 range: <0.001-0.02) was a difference in incidence
Indications: center) Staples removed (days of SSI between groups with
Cancer: Intervention: n=22 postop) one tailed P<0.012.
Intervention: 65% Control: n=32 SSI: 11.12.4
Control: 55% Wound collagen and protein No SSI: 10.31.4 Follow-Up: 15 days postop
Inflammatory Bowel Disease deposition: near end of P<0.001 Wounds evaluated daily until
(IBS) surgery, 7cm expanded Length of stay- see below discharge then at a clinic
Intervention: 20% polytetrafluoroethylene implant visit15 days)
Control: 25% inserted in subcutaneous Other infections: NR Funding Source Conflicts:
Other tissue a few centimeters to one Topic specific outcomes: Authors: None
Intervention: 15% side of and parallel to the Perioperative administration Institution: None
Control:20% surgical incision- removed on of oxygen in concentrations Study: None
Setting: 3 hospitals (2 POD#7 and assayed for that exceeded those Supplies: None
university) hydroxyproline and protein. designated:
Location: Austria (2) and Subcutaneous oxygen tension: Intervention: 1/500
Germany (1) oxygen sensor within Control: 38/500
Dates of Study: July 1996- subcutaneous saline-filled Mean SD
October 1998 tonometer in the lateral upper All patients N=500
Inclusion Criteria: Patients arm. Measurement taken after Arterial oxygen saturation-%
18-80 y undergoing induction of anesthesia and Intraoperative
elective open colorectal continued at designated Intervention: 99.10.6
resection, including those oxygen concentration intraop Control: 98.71.1
undergoing abdominal- and 2 h postop. P=<0.001
peritoneal pull-through Subgroup Analysis#2 N=24 (1 Partial pressure of arterial
procedures center) oxygen-mm Hg
Exclusion Criteria: Patients Intervention: n=12 Intraoperative
undergoing minor colon Control: n=12 Intervention: 34897
surgery (e.g. polypectomy Intraop: muscle oxygen tension: Control: 12134
or isolated colostomy), Oxygen electrode inserted into P<0.001
recent history of fever, quadriceps femoris (0.35mm Postoperative
infection or both, serious diameter needle inserted 1mm Intervention: 20691
malnutrition (serum at a time) Oxygen tension Control: 11435
albumin<3.3g/dl, WBC recorded at each of 200 P<0.001
2017 American Medical Association. All rights reserved. 367
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
<2500 cell/ml3 or loss of measurement points, Oxygen saturation-% (pulse
>20% bodyweight), and histogram constructed for each oximetry)
bowel obstruction. patient. Muscle oxygen tension Postoperative
evaluated 90 minutes after Intervention: 992
induction of anesthesia at the Control: 972
designated FIO2. P=<0.001
Standard Preventative
Measures: Subgroup Analysis #1 N=54
Bowel Prep: Night before, patient Subcutaneous oxygen
underwent standard tension-mm Hg
mechanical bowel prep with an Intraoperative
electrolyte solution but no Intervention: 10943
intraluminal antimicrobials. Control: 5915
AMP: IV for a mean of 2.72.3 P<0.001
days after skin incision. Mostly Postoperative
metronidazole combined with Intervention: 7325
cefazolin, cefamandole, Control: 5425
amoxicillin, clavulanate or P=0.02
mezlocillin. Types and duration Collagen Deposition-ng/mm
of AMP were similar in the two Intervention: 258118
groups. Fluid-Patients Control: 267109
aggressively hydrated. P=0.38
Intraop: Crystalloid 15ml/kg/h IV; Protein Deposition-ng/mm
Blood loss replacement in Intervention 15391
solution to blood ratio 4:1 or Control: 16374
colloid at2:1. P=0.31
Postop: Fluids at 3.5ml/kg/h X Subgroup Analysis#2 N=24
24h then at 2ml/kg/h X24h. Muscle oxygen tension-mm
Leukocyte depleted blood Hg
transfusions as deemed Intervention: 4910
necessary by surgeon. Control: 256
Surgical wound treatment P<0.001
(intraop): There was no
antimicrobial or antiseptic Reoperations: NR
irrigation of the wound or Length of stay:
peritoneal cavity. Intervention: 12.26.1 days
Wound closure: standard all Control: 11.94.0 days
deep layers including P=0.26
peritoneum were closed with Length of stay
2017 American Medical Association. All rights reserved. 368
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
continuous sutures. SSI (N=41) vs. No
Subcutaneous tissues were SSI(N=459)
closed with interrupted sutures SSI: 18.78.3 days
& the skin was stapled No SSI: 11.44.1 days
Normothermia: Intraoperative P<0.001
core temp was maintained at
36C with use of forced air Mortality: Follow up: 15
cover over the patient and days
warming of intravenous fluid. Cause of death in most cases
Intraoperative core temps was sepsis and multi-organ
monitored in the distal failure.
esophagus; Infrared aural- Intervention: 1/250 (0.4%)
canal temps or axillary temps Control: 6/250 (2.4%)
measured throughout p=0.13
hospitalization. Analgesic: Adverse Effects
intravenous & intramuscular Admission to ICU: for surgical
opioids and administered by a complications such as
study blinded nurse blinded to dehiscence, anastomotic
treatment group assignment. leak, * peritonitis.
Restarting feeding, staple Intervention: 5/250 (2%)
removal, patient discharge Control: 12/250 (4.8%)
determined by attending p=0.14
surgeon blinded to treatment
group assignment.
Discharge based on return of
bowel function, control of any
infections and adequate
healing of incision.
Q7. What is the optimal target FIO2 to reduce the risk of SSI; how and when should it be administered? Our search did not identify RCTs or SRs that both
evaluated the optimal fraction of inspired oxygen, how and when it should be administered, and included SSI as an outcome. All studies evaluating the use of
supplemental increased oxygenation both intraoperative and postoperatively used 80% FiO2 as the target level.
2017 American Medical Association. All rights reserved. 369
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.1E3. RISK OF BIAS ASSESSMENTS OF STUDIES: Q6-7 OXYGENATION
eTABLE 44. Risk of Bias Assessments of Randomized Controlled Trials for Q6-7 Oxygenation
Funding
Randomiza- Outco- Attrition source(s)
Describ- tion Describ- me smaller than Attrition disclosed and
ed as appropriate ed as asses- Study Investiga- Attrition 10-15% of appropriat- no obvious Overa-
Author randomiz -ly double- sor participa- tor describ- assigned ely conflict of ll Risk
Year Q ed performed blind blinded nt blinded blinded ed patients analyzed interest of Bias
Question 6: Oxygenation
Belda
91 6 Low
2005
Bickel
92 6 Low
2011
Duggal
99 6 Low
2013
Gardella
98 6 Low
2008
Greif
93 6 Low
2000
Meyhoff
94 6 Low
2009
Pryor
97 6 Low
2004
Scifres
100 6 Low
2011
Staehr
95 6 Low
2011
Stall
96 6 Low
2013
Thibon
90 6 Low
2012
Turtiainen
102 6 Low
2011
Whitney
101 6 High
2001
2017 American Medical Association. All rights reserved. 370
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.1F. Q8-10 ANTISEPTIC PROPHYLAXIS
2.1F1. GRADE TABLE: Q8-10 ANTISEPTIC PROPHYLAXIS
eTABLE 45. GRADE Table for Q8-10 Antiseptic Prophylaxis
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
GRADE Overall
Dose-response
Quantity
Study Quality
Confounders
Consistency
of GRADE
Directness
Precision
and Type Starting
Comparison Outcome Findings Evidence of
of GRADE
for Evidence
Evidence
Outcome Base
Q8. What are the most effective strategies for preparing the patients skin prior to surgery to reduce the risk of SSI?
Q8A. How safe and effective is preoperative antiseptic bathing or showering?
No difference on meta-analysis of 4 RCTs
104-107
(N=7791) in clean, elective and
potentially infected procedures: 356/3906
(9.1%) vs. 389/3885 (10%): RR 0.91 (0.80-
1.04).
No difference on meta-analysis restricted to
104,106
2 higher quality RCTs (N=6302):
293/3167 (9.3%) vs. 305/3135 (9.7%); RR
0.95 (0.82-1.10)
103
Five months into 1 large study
105
SSI* 1 SR the High 0 0 0 0 0 0 0 0 High
placebo was found to have antimicrobial
properties and was changed but results
Chlorhexidine were not stratified nor excluded.
gluconate (CHG)
No difference in each individual trial
solution High
Number preoperative baths, amount of
vs.
antiseptic used per bath, bathing
placebo
instructions to each group, intraoperative
antiseptic skin preparation agent, use of
AMP, and follow up varied between studies.
No difference on meta-analysis of 2 RCTs
104, 107
(N=3589) 9/1804 (0.5%) vs. 10/1785
Product- (0.6%); RR 0.89 (0.36-2.19).
related Every study used 4% CHG
103
Adverse 1 SR Data are driven by the large higher quality High 0 0 0 -1 0 0 0 0 Moderate
104
Reactio- RCT as no allergic reactions were
ns reported in either group in the smaller
107
(N=100), lesser quality RCT .
1 large study (N=1813) not included in the
106
2017 American Medical Association. All rights reserved. 371
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
GRADE Overall
Dose-response
Quantity
Study Quality
Confounders
Consistency
of GRADE
Directness
Precision
and Type Starting
Comparison Outcome Findings Evidence of
of GRADE
for Evidence
Evidence
Outcome Base
meta-analysis also found no difference
reporting 5 patients in each group with
itching or reddening of skin.
No difference on meta-analysis of 3 RCTs
108, 105, 109
(N=1443): 82/752 (10.9%) vs.
94/691 (13.6%); RR 1.02 (0.57-1.84)
Each study used 4% CHG
Heterogeneity for this comparison was high:
2
P=0.08, I =60%.
Only the largest (N=1315) RCT
105
reported
reduction in SSI with 4% CHG: 62/689
(9.0%) vs. 80/626 (12.8%); RR: 0.70 (0.57-
0.96); no special showering/bathing
instructions were given to the un-medicated
CHG solution
bar soap group whereas great care was
vs. 103
SSI* 1 SR taken to ensure that the patients using High 0 0 0 0 0 0 0 0 High High
Un-medicated
[CHG]complied with the instructions.
bar soap
One (N=66) of the two smaller, lesser
108
quality studies suggested higher rate of
SSI with CHG: 8/31 (25.8%) vs. 4/35
(11.4%): RR: 2.26 (0.75-6.77) and the other
109
(N=64) showed no difference: 12/32
(37.5%) vs. 10/30 (33.3%); RR 1.13 (0.57-
2.21)
Number preoperative baths, bathing
instructions, intraoperative antiseptic skin
preparation agent, use of AMP, procedures,
and follow up varied between studies.
No difference on meta-analysis (N=1142) of
CHG solution 107,109,110
103 3 RCTs : 22/623 vs. 29/519; RR
vs. SSI* 1 SR High 0 0 0 -1 0 0 0 0 Moderate Moderate
0.82 (0.26-2.62)
No Wash
Each study used 4% CHG
2017 American Medical Association. All rights reserved. 372
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
GRADE Overall
Dose-response
Quantity
Study Quality
Confounders
Consistency
of GRADE
Directness
Precision
and Type Starting
Comparison Outcome Findings Evidence of
of GRADE
for Evidence
Evidence
Outcome Base
Heterogeneity for this comparison was
2
significantly high: P<0.03, I = 70%.
Studies included outpatient and inpatient
procedures, patients undergoing vasectomy
109 107
, plastic surgery of the trunk and
elective biliary tract, inguinal hernia or
110
breast cancer procedures , plus
differences in SSI definition
Individual study results differed with only the
110
largest (n=978) study favoring 4% CHG:
9/541 (1.7%) vs. 20/437 (4.6%): RR 0.36
(0.17-0.79), the other two suggesting no
difference: 12/32 vs. 9/32; RR: 1.33 (0.65-
109
2.72) and 1/50 vs. 0/50; RR: 3.00 (0.13-
71.92).
Despite instructions to not shower, it is not
clear if the No wash groups did in fact
shower.
Reduced risk of SSI with whole body
110
washing in 1 RCT (N=1093) in elective
CHG solution: biliary tract, inguinal hernia or breast cancer
Whole body 103 procedures: 9/541 (1.7%) vs. 23/552 (4.1%);
SSI* 1 SR High 0 0 0 -1 0 0 0 0 Moderate Moderate
vs. RR: 0.40 (0.19-0.85).
partial body wash Whole body wash = entire body + scalp
Partial body wash = restricted to proposed
surgical site.
1 RCT (N=114) in elective, clean plastic
Aqueous surgical procedures (thorax or abdomen)
iodophor solution reported no infections in either group
111
vs. control (usual SSI* 1 RCT (Follow up NR). The study was designed to High -1 0 -1 -1 0 0 0 0 Very Low Very Low
personal hygiene assess impact of preoperative showering on
routine) skin colonization, not SSI.
Study used 10% povidone iodine solution
2017 American Medical Association. All rights reserved. 373
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
GRADE Overall
Dose-response
Quantity
Study Quality
Confounders
Consistency
of GRADE
Directness
Precision
and Type Starting
Comparison Outcome Findings Evidence of
of GRADE
for Evidence
Evidence
Outcome Base
1 RCT (N=100) in elective shoulder
112
SSI* 1 RCT surgeries reported no infections in either High 0 0 0 -1 0 0 0 0 Moderate
2% chlorhexidine group at a minimum of 2 months postop.
gluconate- In 1 RCT (N=100) in elective shoulder
impregnated surgeries, 12/50 (24%) patients who used Moderate
cloths vs. un- Product-
2% chlorhexidine gluconate-impregnated
medicated bar related 112
1 RCT cloths reported mild itching or a feeling of High 0 0 0 -1 0 0 0 0 Moderate
soap Adverse
dry skin after the application of the cloths.
Events
Adverse events were not reported for the
bar soap group.
Q8B. How safe and effective are antiseptic skin preparation agents individually and in combination?
Iodophors
In a study
113
of 234 oncology surgeries, no
difference was observed in incisional (10%
Aqueous in each group) or intra-abdominal SSI. (2%
2 RCT
Iodophor: SSI* 113,114, vs.3%; p=0.14) infections (30 day follow up) High 0 0 0 0 0 0 0 0 High High
In a study
114
1-step vs. 2-step of 108 CABG patients, no
difference was observed (12% vs. 13%) in
sternal infections (6 week follow up)
Aqueous
Iodophor (1 or 2
step) vs. No difference on a meta-analysis (N=626) of
5 RCT
Iodophor in SSI* 114-118 5 studies: OR: 1.80 (0.50 6.52); p=0.37; High 0 -1 0 -1 0 0 0 0 Low Low
2
Alcohol (1 step, I =67%
with or without
adhesive drape)
CHG-alcohol vs. Aqueous Iodophor
CHG-alcohol (1 In a meta-analysis (N=1976) of 5 RCTs,
or 2 step) vs. 5 RCT CHG-alcohol was associated with reduced
SSI* 116,119-122 High 0 0 0 0 0 0 0 0 High High
Aqueous risk for SSI: OR: 0.59 (0.42 0.83);
2
Iodophor (1 or 2 p=0.003; I =0
2017 American Medical Association. All rights reserved. 374
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
GRADE Overall
Dose-response
Quantity
Study Quality
Confounders
Consistency
of GRADE
Directness
Precision
and Type Starting
Comparison Outcome Findings Evidence of
of GRADE
for Evidence
Evidence
Outcome Base
One study
120
step) (N=849) reported 3 (0.7%)
drug-related adverse events (pruritus,
Product-
erythema or both around the surgical
related 2 RCT
120,121 wound) in each group (P>0.99) High -1 0 0 0 0 0 0 0 Moderate
Adverse
One study
121
(N=500) reported two cases of
Events
skin irritation in aqueous iodophor group,
and no cases in CHG-alcohol group
CHG-alcohol vs. Iodophor-alcohol
CHG-alcohol (1
or 2 step) vs. No difference on meta-analysis of 6 RCTs
6 RCT
Iodophor- SSI* 116,123-127 (N=1323), OR: 0.64 (0.24 1.71); p=0.38; High 0 0 0 0 0 0 0 0 High High
2
alcohol (1 or 2 I =16%
step)
No difference among the 743 patients
available for follow up at 3-4 days in a large
125
(N=866) general surgery study : 27/389
(6.9%) vs. 35/354 (9.9%); p=NS.
Significance varied by procedure: biliary
surgery and other clean operations each
suggested lower incidence of SSI with CGH-
alcohol (p<0.05), in contrast, there was a
lower incidence of SSI (not statistically
CHG-alcohol
significant) with iodophor-alcohol in large
(2 step) vs. 3 RCT
SSI* 123-125 bowel and other laparotomy procedures. High 0 0 0 0 0 0 0 0 High High
Iodophor-
No difference in a study of 250 elective,
124
alcohol (2 step)
clean, plastic surgery breast procedures.
Only 4 superficial SSIs reported at 30 day
follow up, all in the iodophor-alcohol group
(p=0.06)
No infections reported in either group in a
123
small (N=50) study of foot surgeries. The
study was designed to evaluate the
products efficacy in reducing skin
contamination, not SSI (follow up and
2017 American Medical Association. All rights reserved. 375
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
GRADE Overall
Dose-response
Quantity
Study Quality
Confounders
Consistency
of GRADE
Directness
Precision
and Type Starting
Comparison Outcome Findings Evidence of
of GRADE
for Evidence
Evidence
Outcome Base
definition of SSI not reported).
In a study of 80 foot/ankle surgeries , only
126
1 SSI reported (CHG-alcohol group). Follow
up and definition of SSI not reported.
In a study of 100 arthroscopic shoulder
116
CHG-alcohol surgeries, no infections were reported in
(1 step) vs. 3 RCT either group at 10-month follow up.
SSI* 116,126,127 High 0 0 0 0 0 0 0 0 High High
In a study of 100 elective lumbar spinal
127
Iodophor-
alcohol (1 step) surgeries, no infections were reported in
either group at 6 month follow up
All studies were designed to evaluate the
products efficacy in reducing skin
contamination, not SSI
Q8C. How safe and effective is the application of a microbial sealant immediately following skin preparation?
No difference on meta-analysis (N=609) of 4
4 RCT RCTS in cardiac surgery, hernia repair, or
SSI* 128-131 High 0 -2 0 0 0 0 0 0 Low
scoliosis correction: OR: 0.46 (0.08 2.51);
2
p=0.37; I =68%
Cyanoacrylate- In 4 RCTs there were no significant product
based skin related adverse events reported.
Low
In one RCT surgeons reported difficulty
130
sealant vs. Product-
4 RCT
No sealant related 128-131 incising through the clear film in 4/166
High 0 0 0 0 0 0 0 0 High
Adverse patients but no difficulty suturing wounds.
Events- There was one report of visible flaking of
the film at the time of procedure.
Q8D. How safe and effective are plastic adhesive drapes?
Non-Iodophor
No difference on meta-analysis of 4 RCTs
impregnated 4 RCT
SSI* 132-135 (N=1742) (RR: 1.05; 95% CI: 0.81 1.35; High -1 0 0 0 0 0 0 0 Moderate Moderate
adhesive drape 2
p=0.71; I =0
vs. No drape
2017 American Medical Association. All rights reserved. 376
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
GRADE Overall
Dose-response
Quantity
Study Quality
Confounders
Consistency
of GRADE
Directness
Precision
and Type Starting
Comparison Outcome Findings Evidence of
of GRADE
for Evidence
Evidence
Outcome Base
Iodophor-
No difference on meta-analysis of 2 RCTs
impregnated 2 RCT
SSI* 114,136 (N=1113) RR: 1.03 (0.66 1.60); p=0.89; High 0 0 0 0 0 0 0 0 High High
adhesive drape 2
I =0
vs. No drape
*Critical outcome; OR: Odds Ratio; RR: Risk Ratio; CI: Confidence Interval
Increase
Decrease GRADE
GRADE
Publication Bias
GRADE
Dose-response
Quantity Overall
Study Quality
Confounders
Consistency
of
Directness
Magnitude
Precision
and Type Starting GRADE of
Comparison Outcome Findings Evidence
Large
of GRADE Evidence
for
Evidence Base
Outcome
Q9 How safe and effective is antiseptic irrigation prior to closing the surgical incision?
Antiseptic irrigation
In meta-analysis (N=268) of 3 studies in
general surgical contaminated and dirty
abdominal cases no difference noted
between groups with intraperitoneal lavage
using povidone iodine OR: 0.33 (0.08
2
Aqueous 1.34); p=0.12; I =35%. Povidone iodine
Organ/ 137-
iodophor 3RCT concentration and AMP regimens varied
space 139 High 0 -1 0 0 0 0 0 0 Moderate Moderate
irrigation vs. between studies.
Abscess*
In 1 study in 168 patients undergoing
139
Normal saline
laparotomy, peritoneal irrigation with 1 liter
of 1% povidone iodine (0.1% available
iodine) for 60 seconds prior to abdominal
closure reduced the risk of intra-abdominal
abscess formation in dirty procedures: 0/36
2017 American Medical Association. All rights reserved. 377
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Publication Bias
GRADE
Dose-response
Quantity Overall
Study Quality
Confounders
Consistency
of
Directness
Magnitude
Precision
and Type Starting GRADE of
Comparison Outcome Findings Evidence
Large
of GRADE Evidence
for
Evidence Base
Outcome
vs. 6/42; p<0.05 but not in contaminated
procedures: 1/44 vs. 3/46: p=NS
138
A subanalysis of peritoneal lavage with
normal saline then 100ml PI solution prior
to closure in dirty: 4/13 vs. 5/16; p=NS
139
1 study peritoneal lavage with 1L of 10%
PI solution for 60 sec, repeated 3 times
during the procedure, the last time before
closure in contaminated and dirty combined
suggested no difference: 1/37 vs. 4/34;
p=0.12.
In meta-analysis (N=660) of 2 studies of
clean spine surgeries 0.35% povidone
iodine irrigation (volume not reported) and
wound soaking for 3 minutes followed by
irrigation with 2L normal saline was
associated with reduced risk for deep SSI
2
2 RCT OR: 0.08 (0.01 0.58); p=0.01; I =0.
Deep SSI* 140,141 High 0 0 0 0 -1 0 0 0 Moderate
In both studies, irrigation was completed
prior to bone grafting and instrumentation.
It was not repeated prior to wound closure.
Also, AMP was started preoperatively, re-
dosed intraoperatively as appropriate and
continued for 5 days postoperatively.
Of note, 10/12 (83.3%) SSIs were MRSA.
In meta-analysis (N=329) of 2 studies in
general surgical clean-contaminated,
contaminated, and dirty cases
(subpopulations in which both study groups
Superficial 2 RCT were reported to have received parenteral
142,143 High 0 0 0 0 0 0 0 0 High
SSI* AMP), irrigation of the subcutaneous
tissues for 60 seconds with 10% povidone
iodine prior to wound closure was
associated with reduced risk for superficial
2
SSI OR: 0.21 (0.10 0.45); p<0.01; I =0
2017 American Medical Association. All rights reserved. 378
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Publication Bias
GRADE
Dose-response
Quantity Overall
Study Quality
Confounders
Consistency
of
Directness
Magnitude
Precision
and Type Starting GRADE of
Comparison Outcome Findings Evidence
Large
of GRADE Evidence
for
Evidence Base
Outcome
In meta-analysis (N=149) of clean-
contaminated cases, PI associated with
reduced risk OR: 0.15 (0.03 0.72);
2
p=0.02; I =0
In meta-analysis (N=90) of dirty cases, PI
associated with reduced risk OR: 0.26
2
(0.08 0.91); p=0.03; I =0
One study
137
in 168 laparotomy patients
with contaminated peritoneal cavities
reported no complications from the use of
Adverse povidone iodine were noted.
One study
141
Events - 3 RCT in 414 mixed spine surgery
137,141,143 High 0 0 0 0 0 0 0 0 High
Product patients reported no product-related
Related adverse event with 0.35% povidone iodine
followed by normal saline irrigation
One study
143
in 187 general surgical
procedures reported no allergic reactions
One study
140
in posterior spine (no trauma)
reported one incidence of wound
Wound 2 RCT dehiscence event with 0.35% povidone
140,143 High 0 0 0 -1 0 0 0 0 Moderate
Healing iodine followed by normal saline irrigation.
One Study
143
no evidence of delayed
wound healing.
One RCT : no significant change in
142
serum free iodine
137,139
Serum 2 RCT : significant increase in postop
3 RCT 137
Iodine 137,139,142 serum iodine levels at 24h. In 1 RCT the High 0 0 0 0 0 0 0 0 High
139
Level increase resolved by 72h, 1 RCT the
increase resolved by 7 days. Both, no signs
of iodine toxicity.
Q10. How safe and effective is repeat application of an antiseptic skin preparation agent to the surgical site immediately prior to closing the surgical
incision?
Topical antiseptic agents
2017 American Medical Association. All rights reserved. 379
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Publication Bias
GRADE
Dose-response
Quantity Overall
Study Quality
Confounders
Consistency
of
Directness
Magnitude
Precision
and Type Starting GRADE of
Comparison Outcome Findings Evidence
Large
of GRADE Evidence
for
Evidence Base
Outcome
In a lower quality study of 107 gastric or
colorectal procedures, no difference was
observed between povidone iodine and no
topical antiseptic groups for combined or
Aqueous individual incisional or organ/space
iodophor to skin surgical site infections:
144
prior to wound SSI* 1 RCT High -1 0 0 -1 0 0 0 0 Low Low
Combined: 13/54 (24.1%) vs. 12/53
closure vs. no
(22.6%)
topical antiseptic
Gastric Organ/Space: p=0.65
Gastric Incisional: p=0.49
Colorectal Organ/Space: p=0.59
Colorectal Incisional: p=0.61
*Critical outcome; OR: Odds Ratio; RR: Risk Ratio; CI: Confidence Interval
2017 American Medical Association. All rights reserved. 380
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.1F2. EVIDENCE TABLES: Q8-10
Q8. What are the most effective strategies for preparing the patients skin prior to surgery to reduce the risk of SSI?
eTABLE 46. Evidence Table for Q8A. How safe and effective is preoperative antiseptic bathing or showering?
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Webster, SR To review the Study types: RCT Intervention: Any type of All results intervention vs. Definitions: SSI definition used
103
2012 1, 2, 3, 4, evidence for N: 7 RCT, 10,157 participants antiseptic solution (any control RR (95% CI). No by the studies was accepted
(RA) 5, 6, 7, 8, preoperative Inclusion criteria: RCTs strength, any regimen, at significant heterogeneity Perioperative care: NR
10, 11 bathing or comparing any antiseptic any time before the surgery) unless specified Other Notes: None
showering with preparation used for used for preoperative tub- SSI: Follow-up not reported
antiseptics for preoperative full body wash or or bed-bathing or Chlorhexidine 4% vs. Funding Source Conflicts:
preventing showering, with non-antiseptic showering. All studies used placebo all studies (4 Authors: None
nosocomial SSI preparations. 4% chlorhexidine gluconate studies, N=7791): Institution: None
Exclusion criteria: Quasi-RCTs 0.91(0.80-1.04); Fixed Study: None
2
Databases searched: Cochrane Comparison: Non-antiseptic effects model; I =0% Supplies: None
Wounds Group Specialized soap, non-antiseptic soap Chlorhexidine 4% vs.
Register, CENTRAL, solution, no shower or bath placebo high quality
MEDLINE, EMBASE, CINAHL, studies (2 studies,
hand searching, reference lists N=6302): 0.95(0.82-1.10);
2
of retrieved articles (searches Fixed effects model; I =0%
ended October-November Chlorhexidine 4% vs. bar
2010) soap (3 studies, N=1443):
Quality assessment: Using the 1.02(0.57-1.84); Random
2
Cochrane Collaboration Tool effects model; I =60%
for assessing risk of bias, low Chlorhexidine 4% vs. no
risk of bias for: wash (3 studies, N=1142):
Random sequence generation 0.82(0.26-2.62); Random
2
5/7 studies effects model; I =70%
Allocation concealment 3/7 Chlorhexidine full wash vs.
studies partial wash (1 study,
Blinding of investigator and N=1092): 0.40(0.19-0.85)
participant 3/7 studies Allergic reaction:
Blinding of outcome assessor Chlorhexidine 4% vs.
5/7 studies placebo (2 studies,
Incomplete outcome data 6/7 N=3589): 0.89(0.36-2.19);
2
studies Fixed effects model; I =0%
Selective reporting 7/7 studies
Other bias 4/7 studies
Murray RCT To test the Number of patients: N=100 Intervention group: n=50 SSI: Definitions:
112
2011 1, 4, 6, 9 hypothesis that Patient Characteristics Shower with soap and water Total SSI: SSI NR
2017 American Medical Association. All rights reserved. 381
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
(ES) the home use Age, years, meanSD the evening before Intervention: 0/50
of 2% Intervention: 49.016.2 operation and wipe their Control: 0/50 Perioperative care: NR
chlorhexidine Control: 52.016.7 entire operative extremity, Other notes: Positive cultures
gluconate- P=0.14 including the axilla, Other infections: NR were primary outcome of
impregnated Gender: M/F shoulder, and ipsilateral Topic-specific outcomes: interest. Study was powered
cloths would be Intervention: 36/14 (72% male) chest and back with a 2% Compliance with protocol to detect a difference in
more Control: 25/25 (50% male) chlorhexidine gluconate- Intervention: 45/50 (90%) positive cultures. It was
efficacious than P=0.04 impregnated cloth 1h after [4 unable to elevate arm underpowered to detect any
a standard Obesity: NR showering. Then the sufficiently to apply the difference in SSI
soap-and-water Comorbidities: morning of surgery, cloth, 1 patient showered Follow-up: 2 months post op.
shower at Diabetes mellitus: patients were instructed to in between applications of [follow up insufficient for
decreasing the Intervention: 4/50 (8%) avoid showering and apply chlorhexidine- implant SSI]
preoperative Control: 4/50 (8%) a second 2% chlorhexidine impregnated cloth. Funding Source Conflicts:
cutaneous P>0.99 gluconate0-impregnated Control: 50/50 (100%) Authors: NR
levels of Immunosuppressive cloth in the same manner P=0.056 Institution: Industry
pathogenic medications: as the first within 2h of Study: Industry
bacteria on the Intervention: 1/50 (2%) departing for the hospital. Reoperations: NR Supplies: Industry
shoulder Control: 0/50 Timing of intervention: Length of stay: NR
P=0.99 Preoperative Mortality: NR
Shaved axilla Duration of intervention: Adverse events:
Intervention: 8/50 (16%) duration of chlorhexidine- No serious adverse events
Control: 12/50 (24%) impregnated cloth scrub occurred in any patients
P=0.45 Device/agent: 2% Side effects (mild itching or a
Took abx prior to surgery chlorhexidine gluconate- feeling of dry skin):
Intervention: 1/50 (2%) (for impregnated cloth and/or Intervention: 12/50 (24%)
upper respiratory infection) soap Control: 0/50
Control: 0/50 Monitoring intervention: NR P<0.002
P=0.99 Control group: n=50
Patients instructed to shower
Procedures: shoulder surgery with soap and water the
[no acute trauma surgeries] morning of surgery.
Open Standard preventive
Intervention: 6/50 (12%) [6 measures:
primary total shoulder Antimicrobial prophylaxis:
arthroplasties] preop 1g of cefazolin if
Control: 8/50 (16%) [6 primary weight was <90kg and 2g if
total shoulder arthroplasties, 1 weight was >90kg, or
revision total shoulder 900mg clindamycin if
arthroplasty & 1 Weaver- allergic to penicillin, was
2017 American Medical Association. All rights reserved. 382
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Dunn procedure] administered to all patients
P=0.77 within 1h of skin incision.
Arthroscopic Shoulder arthroplasty
Intervention: 44/50 (88%) patients received an
Control: 42/50 (84%) additional 1g vancomycin.
P=0.77 Antimicrobial drape
antibacterial-impregnated
Indications: NR drape used for all cases
Setting: 1 university hospital involving implantation of a
Location: USA prosthesis.
Dates: January 2010 May Intraoperative skin prep: 2%
2010 chlorhexidine gluconate
Inclusion Criteria: Patients and 70% isopropyl alcohol.
scheduled for any type of Hair removal: 6 patients
shoulder surgery. reported shaving their own
Exclusion Criteria: Refusal to hair before surgery but it is
participate had an open not reported which group
wound, a current infection, or they belonged to.
a chronic immunosuppressive
condition.
Veiga RCT To assess the Number of patients: N=114 Intervention group: n=57 SSI (follow up NR) Definitions:
111
2008 1, 4 influence of Patient Characteristics Patients instructed to shower No SSI seen in either group. NR
(ES) povidone- Age: mean 38.3 y (range 18-65) with liquid detergent-based
iodine Gender: m:f: 26:88 povidone-iodine 1-% and Other infections: NR Perioperative care: NR
preoperative Obesity: NR water 2hours before Topic-specific outcomes:
showers on Comorbidities: NR surgery. Patients instructed Patients with no Other notes: NR
skin Procedures: Plastic surgery to rinse thoroughly, lather microorganism growth
colonization in involving the thorax or with detergent, rinse, lather, PVP-I: 33/57 (57.9%) Follow-up: NR
elective plastic abdomen: Breast and rinse again. Control: 0/57 Funding Source Conflicts:
surgery reconstruction, reduction Timing of intervention: Authors: None
procedures mammoplasty, augmentation preop Patients with S. aureus Institution: NR
mammoplasty, liposuction, Duration of intervention: growth (13/114 (11.4%) Study: NR
gynecomasty, scar revision, duration of shower. PVP-I: 1/57 (1.8%) Supplies: NR
supernumerary mammoplasty, Device/agent: Povidone Control: 12/57 (21.1%)
and abdominoplasty. iodine 10% detergent-based P=0.0019
soap
Indications: NR Monitoring intervention:
Setting: 1 school hospital Samples for quantitative Reoperations: NR
Location: Brazil skin sampling obtained in Length of stay: NR
2017 American Medical Association. All rights reserved. 383
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Dates: September 15, 2004 the OR. A 5x10cm area on Mortality: NR
December 1, 2005 the anterior abdominal wall Adverse events: NR
Inclusion Criteria: Patients was swabbed with a sterile
older than 18 years scheduled cotton swab pre-moistened
for elective and clean plastic with sterile saline. Samples
surgery procedures on the were processed within 6h
thorax or abdomen after obtainment and plated
Exclusion Criteria: Patients onto agar plates.
with a history of Control group: n=57
hypersensitivity to povidone- No special instructions for
iodine, presence of rashes, showering implemented
open sores or skin lesions, and before surgery. Patients
antimicrobial use at the time of followed their usual
surgery. personal hygiene routine on
day of surgery
Standard preventive
measures: NR
eTABLE 47. Evidence Table for Q8B. How safe and effective are antiseptic skin preparation agents individually and in
combination?
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Savage RCT To identify Number of patients: N=100 Intervention group: n=50 SSI : Definitions:
127
2012 1 the common Patient Characteristics: No Skin was prepared with 2% Total SSI: 0/100 SSI - NR
(ES) bacterial significant differences chlorhexidine gluconate Superficial SSI Perioperative care: NR
flora on the between groups with and 70% isopropyl Intervention: 0/50 Other notes: study was
skin regards to Age or BMI. alcohol. Spine was Control: 0/50 designed with Colonization
overlying the Age: mean, years prepared according to Deep SSI as primary outcome. SSI
lumbar spine Intervention: 51 the manufacturers Intervention: 0/50 was secondary.
and to Control: 54 instructions. Each Control: 0/50 Power was on the basis of the
evaluate the Gender: NR preparation solution assumption that a 20%
2
efficacy of Obesity: BMI mean (kg/m ) allowed to adequately Other infections: NR difference in positive skin
two readily Intervention: 231 dry for approximately 3-5 Topic-specific culture rates would be
available Control: 175 minutes. outcomes: clinically relevant, the
skin- Comorbidities: NR Timing of intervention: Superficial wound number of patients required
2017 American Medical Association. All rights reserved. 384
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
preparation Diabetes mellitus: Pre-operative dehiscence to achieve 80% power at
solutions in Intervention: 3/50 (6%) Duration of intervention: Intervention: 1/50 (2%) alpha=0.05 was 50/group
the Control: 4/50 (8%) Application + 3-5 min Control: 0/50 Follow-up: minimum of 6
elimination Smoker (>1.5 packs/day): drying time months
of bacterial Intervention: 3/50 (6%) Device/agent: with 2% Reoperations: NR Funding Source Conflicts:
pathogens Control: 3/50 (6%) chlorhexidine gluconate Length of stay: NR Authors: NR
from the Corticosteroid use: and 70% isopropyl Mortality: NR Institution: NR
surgical site Intervention: 3/50 (6%) alcohol, or 0.7% Adverse events: NR Study: NR
following Control: 2/50 (4%) available iodine and 74% Supplies: Industry
skin Immunocompromised: isopropyl alcohol
preparation. Intervention: 2/50 (4%) Monitoring intervention:
Control: 3/50 (6%) NA
Previous Spine Surgery Control group: n=50
Intervention: 10/50 (20%) Skin was prepared with
Control: 9/50 (18%) 0.7% available iodine
History of alcohol abuse: and 74% isopropyl
Intervention: 4/50 (8%) alcohol. Spine was
Control: 2/50 (4%) prepared according to
History of MRSA: the manufacturers
Intervention: 0/50 instructions. Each
Control: 2/50 (4%) preparation solution
Duration of surgery: mean allowed to adequately
(min) dry for approximately 3-5
Intervention: 51 minutes.
Control: 54 Standard preventive
P=0.05 measures: No specific
cleansing or shaving
Estimated Blood Loss: mean protocol prior to the
(mL) surgery. If necessary,
Intervention: 388 hair was removed with
Control: 175 clippers in the operating
P=0.02 room.
Procedures: elective lumbar Antibiotic Prophylaxis: all
spine surgery including received 1 or 2g of
microdisectomy, posterior cefazolin (based on
spinal fusion with or without weight) prior to surgery
an associated interbody except in cases of
fusion, decompression penicillin allergy where
alone, kyphoplasty. they received 900 mg of
2017 American Medical Association. All rights reserved. 385
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Indications: NR clindamycin. Patients
Setting: 1 University Hospital who required spinal
Location: USA instrumentation followed
Dates: February August the same protocol with
2010 the addition of 1g of
Inclusion Criteria: vancomycin.
Consecutive patients Drape same non-
undergoing elective lumbar antimicrobial drape was
spine surgery used in all cases
Exclusion Criteria: If patient
had an open wound at the
incision site, abrasion in the
vicinity of the planned
incision, an active infection
at or near the surgical site,
or an active infection
elsewhere in the body.
Sistla RCT To compare No. Patients: N=400 Intervention: n=200 SSI- (30days) Definitions:
119
2010 1, 4, 5, the efficacy Patient Characteristics: 2.5% chlorhexidine with Overall SSI: 33/400 Infections: CDC criteria
(ES) 6, 7, 9 of povidone Patient characteristics & 70% ethanol applied in (8.3%) Questionnaire: patient self-
iodine and a surgical elements were concentric circles Intervention: 14/200 reported on 1 or more of the
combination similar between groups. No beginning with the site of (7.0%) following conditions: no
of statistically significant incision to the periphery Control: 19/200 (9.5%) problems, redness and pain
chlorhexidin difference. and allowed to dry P=0.364 around the wound which
e-ethanol in All values given for entire before the surgical site Grade of SSI: settled without treatment,
the reduction study group. (N=400) was draped Grade 1: Pus Discharge: redness and pain around the
of skin Age60 years: 306 (76.5%) Timing of Intervention: 12/400 (3%) wound which required
bacterial Age60 years: 94 (23.5%) Preoperative Intervention: 5/200 (2.5%) antimicrobials, discharge of
counts and Gender (m/f): 391/9 Duration of intervention: Control: 7/200 (3.5%) pus from the wound, wound
its effect on Obesity: NR intraoperatively P=0.538 break down, need for
wound Side (bilateral/unilateral): Agents: Sterile cotton Grade 2:Erythema, hospitalization.
infection 38/362 swabs pre-moistened with induration or cellulitis: Note: patients reported to the
rates Comorbidity present: 23 sterile saline, Agent brand 18/400 (4.5%) hospital when they
following (5.8%) name for intervention & Intervention: 8/200 (4%) developed infection for
hernia ASA 3: 9 (2.3%) control NR Control: 10/200 (5%) confirmation and treatment
repair. Preop Stay Monitoring intervention: P=0.605 due to limited free medical
<48 h: 229 (57.3%) N/A Grade 3: Wound facilities.
>48 h: 171 (42.8%) Control: n=200 dehiscence: 3/400 Perioperative care
Duration of Surgery 10% povidone-iodine (0.8%) Shaving of operative site done
2017 American Medical Association. All rights reserved. 386
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
<55 min: 320 (80%) applied in concentric Intervention: 1/200 (0.5%) the night before surgery on
>55 min: 80 (20%) circles beginning with the Control: 2/200 (1%) all patients.
Grade of surgeon site of incision to the P=0.619 Admission preop-patients in
Resident: 378 periphery and allowed to this series were
(94.5%)Procedures: Open dry before the surgical SSI rate in prosthetic predominantly from distant
Hernia repair site was draped repair: 10.6% vs. suture regions, admitted and then
Herniotomy: 18 (4.5%) Standard preventive repair (NR) despite use operated on next available
Herniorrhaphy: 132 (33%) measures of AMP; difference not operating day.
Hernioplasty: 250 (62.5%) AMP: Patients undergoing statistically significant. Type of anesthesia
Indications: prosthetic repair Spinal
Suture repair: 62% (hernioplasty) received a Univariate analysis Risk of Intervention: 172/200 (86%)
Prosthetic repair: 33% single dose of cefazolin SSI Control: 169/200 (84.5%)
Herniotomy: 5% intravenously an hour Operation Side Local
Setting: Academic medical before surgery. Bilateral: 8/38 (21%) Intervention: 28/200 (14%)
institute infected Control: 30/200 (15%)
Location: India Unilateral: 25/362(7%) General
Dates: NR infected Intervention: 0
Inclusion Criteria: Adults RR 3.05 (CI 95%, 1.48- Control: 1/200 (0.5%)
undergoing elective open 6.28) Dressing: Sterile dressings
inguinal hernia repair P= 0.007 applied after surgery &
Exclusion Criteria: Patients Preoperative Stay wounds were left exposed
with recurrent or complicated >48 hrs. : 22/171(13%) after 48 hr.
inguinal hernia and patients infected Other notes:
with a history of allergy to the <48 hrs. : 13/229(6%) NOTE: In Table 1 they indicate
antiseptics infected n=250 (62.5%)
RR 2.27 (95% CI, 1.17- hernioplasties (prosthetic
4.37) repair) BUT in the results
P=0.019 text they state Sixty-two
Duration of surgery percent of patients
> 55min: 11/80 infected underwent suture repair
< 55min: 22/320 [which should be a
RR 2.00 (95%CI, 1.01*- herniorrhaphy]; prosthetic
3.95) repair was performed in 33%
P=0.066 of patient s [which is the
Multivariate analysis found number of herniorrhaphies in
only preoperative stay to table1) unclear which is
be a significant risk correct.
factor
(p<0.001) (not age, They also note that higher
2017 American Medical Association. All rights reserved. 387
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
gender, side of hernia, infection rates in developing
comorbidity, ASA score, countries vs. others is partly
procedure, type of due to certain practices and
anesthesia, grade of special problems in these
surgeon or length of regions: shaving, admission
surgery) prior to surgery, poor
Other infections: NR personal hygiene in some of
Topic Specific the patients in lower
Outcomes: Not relevant socioeconomic strata and
Reoperations: None of not practicing antiseptic
the SSIs with pus or showers preop.
wound dehiscence Follow up: CDC criteria used
necessitated removal of by investigators to record
the prosthetic material infections in the
(mesh) postoperative period.
Length of Stay: NR Patients were given a
Readmission: NR questionnaire to record/
Mortality: NR report wound conditions and
was returned 30 days after
surgery. (72% of 400
completed the questionnaire)
Funding Source Conflicts:
Authors: NR
Institution: NR
Study: NR
Supplies: NR
Darouic- RCT To compare No. Patients: Intervention: SSI within 30 days Definitions:
he 1, 2, 3, the efficacy Intention to treat (ITT) N=849 ITT n=409 ITT N=849 SSI diagnosed on basis of
120
2010 4, 5, 6, of Per protocol N=813 Per protocol: n=391 Any SSI CDC criteria
(ES) 7, 8, 9, chlorhexidin Patient Characteristics: Skin at surgical site was Intervention: 39/409 Malnutrition: Defined as > 10%
10 e-alcohol Patients in the two study scrubbed with an (9.5%) decrease in weight in over 2
with that of groups were similar with applicator that contained Control: 71/440 (16.1%) months
povidone- respect to demographic 2% chlorhexidine RR 0.59 (95% CI, 0.41-
iodine for characteristics, coexisting gluconate & 70% 0.85) p=0.004 Perioperative care
preventing illnesses, risk factors for isopropyl alcohol. More Superficial NR
surgical-site infection, antimicrobial than one chlorhexidine Intervention: 17/409 Other notes
infections exposure, & duration & types alcohol applicator was (4.2%) None
or surgery. used if area exceeded 33 Control: 38/440 (8.6%) Follow up: 30 days; Surgical
2017 American Medical Association. All rights reserved. 388
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
All values given for by 33 cm. RR 0.48 (95% CI, 0.28- site assessed 1x/day during
intervention Timing of Intervention: 0.84) p=0.008 hospitalization, on discharge
Intention to Treat intervention Preoperative Deep Incisional & at time of follow up &
population n=409 Duration of intervention: Intervention: 4/409 (1%) whenever SSI occurred.
Age yr.; mean (range): Intraoperatively Control: 13/440 (3.0%) Investigators called patients
53.314.6 (18-100) Agents: RR 0.33 (95% CI, 0.11- 1x/week during 30 day
Gender: Male Sex (%) 58.9 Intervention: 2% 1.01) p=0.05 follow-up period.
Obesity: NR chlorhexidine gluconate & Organ/space Funding Source Conflicts:
Gastrointestinal Disease: 67% 70% isopropyl alcohol Intervention: 18/409 Authors: Industry
Cardiopulmonary disease: Control: 10% povidone- (4.4%) Institution: NR
33.5% iodine Control: 20/440 (4.5%) Study: NR
Neurologic disease: 12/5% Monitoring intervention: RR 0.97 (95% CI, 0.52- Supplies: NR
Renal disease: 7.3% N/A 1.80)
Immunologic disease: 4.7% P>0.99
Cancer: 58.0% Control: Sepsis from SSI
Diabetes mellitus: 15.4% ITT: n=440 RR -.62; (95% CI, 0.30-
Liver Cirrhosis: 2.2% Per protocol n=422 1.29)
History of Alcohol Abuse: Skin at surgical site was Time to onset of SSI
17.9% scrubbed and painted longer in intervention vs.
History of smoking: 37.2% with an aqueous solution control P=0.004
Procedures of 10% povidone-iodine
ITT population N=849 (Allowed to dry? NR) Per-protocol analysis
Abdominal: yielded similar efficacy
Intervention : 72.6% Standard Preventive results.
Control : 70.0% Measures Other Infections: NR
Colorectal: ITT Population, N=849 Topic Specific
Intervention: 45.5% AMP: All patients received Outcomes:
Control: 43.4% systemic prophylactic ITT population subgroup
Biliary: antimicrobials within 1 analysis
Intervention: 10.8% hour before the initial All Infections by Surgery
Control: 12.3% incision. No significant type
Small Intestine: differences in the type or Abdominal:
Intervention: 10.0% number of antimicrobials Intervention: 37/297
Control: 7.7% given. (12.5%)
Gastroesophageal: AMP postop Control: 63/308 (20.5%)
Intervention: 6.4% Intervention :51.7% 95% CI for absolute
Control: 6.6% Control:48.9$ difference, -13.9to-2.1
Non-Abdominal Surgery P=0.41 percentage points
Intervention: 27.4% Shower: Colorectal
2017 American Medical Association. All rights reserved. 389
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Control: 30.0% Preoperative Shower Intervention: 28/186
Thoracic: Intervention: 26.7% (15.1%)
Intervention:10.8% Control: 27%p=0.94 Control: 42/191 (22.0%)
Control: 13.0% 4% chlorhexidine gluconate Biliary
Gynecologic: P=0.32 Intervention: 2/44 (4.6%)
Intervention:10.3% 10% povidone iodine Control: 5/54 (9.3%)
Control:9.1% P=0.26 Small intestine:
Urologic: 6% triclobarban soap bar Intervention: 4/41 (9.8%)
Intervention: 6.4% P>0.99 Control: 10/34 (29.4%)
Control:8.0% Hair removal- as necessary Gastroesophageal
Indications: NR by hair clipping Intervention: 3/26 (11.5%)
Setting: 6 University-affiliated Control: 6/29 (20.7%)
hospitals Non-Abdominal
Location: USA Intervention: 2/112(1.8%)
Dates: April 2004-May 2008 Control: 8/132 (6.1%)
Inclusion Criteria: Patients 95% CI for absolute
18 years undergoing clean- difference, --7.9 to 2.6
contaminated surgery percentage points
performed under controlled Thoracic:
conditions without Intervention: 2/44 (4.5%)
substantial spillage or Control: 4/57 (7.0%)
unusual contamination. Gynecologic
Exclusion Criteria: A history Intervention: 0/42
of allergy to chlorhexidine, Control: 1/40 (2.5%)
alcohol or iodophors; Urologic
evidence of infection at or Intervention: 0/26
adjacent to the operative Control: 3/35 (8.6%)
site; and the perceived Both the ITT and Per
inability to follow the patients protocol analyses
course for 30 days after showed lower rates of
surgery SSI in the intervention
group for each of the
seven operations
included.
Trial not powered to
compare SSI rates for
subcategories of
patients, however, SSIs
2017 American Medical Association. All rights reserved. 390
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
occurred significantly
less often in intervention
group for small intestinal
(P=0.04), or abdominal
surgery (P=0.009) or
who did not shower
preoperatively (P=0.02)
Factors affecting any
SSIs
Use of Chlorhexidine (vs.
PVP-I)
Univariate: OR: 0.55;
p=0.004
Multivariate: OR: 0.45
p=0.004
Use of Abdominal Surgery
(vs. Non-Abdominal
Surgery)
Univariate: OR: 4.63;
p<0.001
Multivariate: OR: 3.21
p=0.001
Alcohol Abuse
Univariate: OR: 1.11;
p=0.69
Multivariate: OR: 1.12
p<0.001
Liver Cirrhosis
Univariate: OR: 3.28;
p=0.02
Multivariate: OR: 2.14
p=0.02
Immunologic Disease
Univariate: OR: 2.72;
p=0.01
Multivariate: OR: 1.79
p=0.05
Cancer
Univariate: OR: 2.05;
2017 American Medical Association. All rights reserved. 391
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
p=0.002
Multivariate: OR: 1.65
p=0.03
Diabetes Mellitus
Univariate: OR: 1.90;
p=0.01
Multivariate: OR: 1.75
p=0.03
Malnutrition
Univariate: OR: 3.02;
p=0.003
Multivariate: OR: 2.62;
p=0.01
Gastrointestinal Disease
Univariate: OR: 2.96;
p<0.001
Multivariate: OR: 1.27
p=0.05
Days surgical drain in
place
Univariate: OR: 1.03;
p=0.02
Multivariate: OR1.04
p<0.001
Preop shower with
Chlorhexidine (vs. no
shower)
Univariate: OR: 1.56;
p=0.38
Multivariate: OR: 0.95
p=0.19
Preop shower with PVP-I
(vs. no shower)
Univariate: OR: 0.135;
p=0.01
Multivariate: OR; 0.36
p<0.001
Use of Chlorhexidine (vs.
PVP-I)
2017 American Medical Association. All rights reserved. 392
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Univariate: OR: 1.08;
p=0.79
Multivariate: OR: 0.96
p=0.72
Reoperation: NR
Length of Stay: NR
Readmission: NR
Mortality:
Intervention: 4/391 (1%)
None had SSIs
Control: 3/422 (0.7%)
All 3 died from
organ/space SSI related
sepsis
0.3% (95%CI -0.9-1.5); p
=0.72
Adverse events:
Total Serious adverse
events:
Intervention: 72/409
(17.6%)
Control: 70/ 440 (15.9%)
1.7% (95%CI -3.3-6.7); p
=0.52
Bloodstream Infection
Intervention: 11/409
(2.7%)
Control: 23/ 440 (5.2%)
-2.5% (95%CI -5.1-0.1); p
=0.08
Abscess
Intervention: 6/409 (1.5%)
Control: 11/ 440 (2.5%)
-1.0% (95%CI -2.9-0.8); p
=0.33
Pneumonia
Intervention: 6/409 (1.5%)
Control: 9/ 440 (2%)
2017 American Medical Association. All rights reserved. 393
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
-0.6% (95%CI -2.3-1.2); p
=0.61
Antiseptic Agent Related
Adverse Events
Includes pruritus,
erythema, or both
around the surgical
wound. Intervention:
3/409 (0.7%)
Control: 3/ 440 (0.7%)
0.1% (95%CI -1.1-1.2); p
>0.99
No cases of fire or
chemical skin burns in
the operating room
Cheng RCT To compare No. Patients: N=50 Intervention n=25 SSI & Adverse events: Definitions: NR
123
2009 1, 2, 10 the effect of Patient characteristics: No Skin prepared with (Follow up NR) Perioperative care: NR
(ES) povidone- Demonstrable difference in chlorhexidine gluconate None of the 50 patients Other notes: None
iodine and age, sex or site of operation 0.5% in 70% alcohol) developed any post- Follow up: No follow up
chlorhexidin between groups. scrub and paint operative infections or recorded
e gluconate The only demographic Timing of Intervention: wound complications Funding Source Conflicts:
(both with information given were age Preoperative Other Infections: NR Authors: None
isopropyl and gender. Duration of intervention: Topic specific Institution: None
alcohol) on Age y, meanSD intraoperative outcomes: Not relevant Study: None
lowering 51.1 17.4 Agent: Supplies: None
bacterial Gender m/f: 12/38 Intervention: 0.5% Reoperation: None
load and if Obesity: NR Chlorhexidine gluconate Length of Stay: NR
any Procedures: in 70% alcohol Readmission: None
additional Metatarsal osteotomies for Control: 10% Alcoholic Mortality: None
benefits correction of hallux valgus tincture of povidone-
(additional deformity: 23/ 50 (46%) iodine, 1% available
lowering of Removal of osteophytes from iodine
the bacterial the first metatarsal: 15/ 50 Monitoring intervention:
load) were to (30%) NR
be gained by Correction of lesser toe Control: n=25
an additional deformities: 12/ 50 (24%) Skin prepared with
pre-scrub Indications: See Procedures alcoholic tincture,
with a Setting: 1 Hospital povidone-iodine 10%
2017 American Medical Association. All rights reserved. 394
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
bristled Location: United Kingdom (1% available iodine)
surgical Dates: August 2007 January scrub and paint
brush with 2008 Standard Preventive
either of Inclusion Criteria: Measures
these Undergoing foot surgery AMP: All patients were
solutions on Exclusion Criteria: If there given a single dose of a
the non- were current open wounds, prophylactic broad
surgical foot. skin ulcers and/ or sore, a spectrum antimicrobial
history of onychomycosis, prior to their procedure
paronychia or nail deformity, but after skin prep.
poorly controlled diabetes
mellitus or recent
antimicrobial use (w/in one
week of surgery)
Saltzman RCT To examine No. Patients: N=150 Intervention1 n=50 SSI: 10 month minimum Definitions:
116
2009 1, 6, 9 the native Patient Characteristics: 0.7% iodophor and 74% No postoperative infection Not recorded
(ES) bacteria Characteristics given isopropyl alcohol had developed in any of Perioperative care
around the represent the whole study. Intervention2 n=50 the patients in this study Hair removal: 37/ 150 (25%)
shoulder and Age: 17-79 years old 2% chlorhexidine gluconate at a minimum follow-up reported voluntary shaving of
axilla, and to Gender (m/f): 84/66 and 70% isopropyl Other Infections: NR axillary hair prior to
determine Obesity: NRIntervention1: alcohol Topic specific enrollment. All were women.
the efficacy Heavy Smokers (>1.5 pack per Intervention3 n=50 outcomes: Not relevant 12 in control, 9 in
of three day): 1/50 Shoulder prepared with Reoperation: NR intervention1, 16 in
different Diabetes mellitus: 4/50 povidone-iodine scrub & Length of Stay: NR intervention2
surgical Rheumatoid Arthritis: 0/50 paint 0.75% iodine scrub Readmission: NR Other notes: None
skin- History of Alcoholism or and 1.0% iodine paint Mortality: NR Follow up: 10 months
preparation hepatitis: 4/50 Timing of Intervention Adverse events: NR Funding Source Conflicts:
solutions Intervention2: Preoperative Authors: Industry
(2% Heavy Smokers: 0/50 Duration of intervention: Institution: None
chlorhexidin Diabetes mellitus: 6/50 Intraoperative Study: Industry
e gluconate Rheumatoid Arthritis: 2/50 Agent: Supplies: Industry
and 70% History of Alcoholism or Intervention1: 0.7%
isopropyl hepatitis: 2/50 iodophor and 74%
alcohol; Control: isopropyl alcohol
0.7% Heavy Smokers: 3/50 Intervention2: 2%
iodophor Diabetes mellitus: 3/50 chlorhexidine gluconate
and 74% Rheumatoid Arthritis: 0/50 and 70% isopropyl
isopropyl History of Alcoholism or alcohol
alcohol; and hepatitis: 1/50 Control: Povidone-iodine
2017 American Medical Association. All rights reserved. 395
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
0.75% iodine scrub (0.75% iodine scrub
scrub and Procedures and 1.0% iodine paint)
1.0% iodine Arthroscopic Shoulder Prosthetic implant surgeries
paint)on the Surgery= 137/150 (91.3%) utilized antibacterial-
eradication Shoulder Arthroplasties barrier (adherent drape)
of bacteria (primary) = 4 Monitoring intervention:
from the Indications: NR N/A
shoulder by Setting: One hospital Standard Preventive
evaluating Location: USA Measures:
the residual Dates: September 2007 Shower: All patients were
bacteria February 2008 instructed to shower the
present Inclusion Criteria: Patients day before the surgery.
following undergoing shoulder AMP: Preoperative
surgical skin surgery. antimicrobials were
preparation. Exclusion Criteria: If patient administered to all 150
had an open wound or a patients. Arthroscopic or
current infection or were soft tissue surgeries
chronically received cefazolin or
immunosuppressed. clindamycin.
Arthroplasties:
AMP: received the same
AMP as above plus
vancomycin.
Skin Prep: After skin prep
used an antibacterial-
impregnated barriers
(adhesive drapes)
Paochar- RCT To study the No. Patients: N=500 Intervention: n=250 Surgical Wound Definitions:
oen 1 efficacy in Patient characteristics: Age, 4% chlorhexidine in 70% Infection: SSI: if the wound drained
121
2009 the reduction operative time and wound isopropyl alcohol scrub (5 1 month purulent material or if the
(ES) of bacterial class were all analyzed and minutes) followed by 4% Total: (%) surgeon judges it to be
colonization found not to be statistically chlorhexidine in 70% Intervention: 5/250 (2%) infected and opens it. (Dunn
and significant. isopropyl alcohol paint. 2/5 arteriovenous shunt 2005)
postoperativ Characteristics given Timing of Intervention: 2/5 appendectomy
e wound represent the whole study. pre-operatively 1/5 right half colectomy Perioperative care : NR
infection Age 10-60 years old Duration of intervention: Follow up: 1 month. Surgical
among Age y mean (range) intraoperative Control: 8/250 (3.2%) wounds examined twice a
povidone- Intervention: 50.5 (18-79) Agents: 4% chlorhexidine 4/8 arteriovenous shunt week for the first week and
2017 American Medical Association. All rights reserved. 396
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
iodine and Control: 56.2 (20-79) in 70% isopropyl alcohol 1/8 modified radical every week for 1 month.
chlorhexidin Gender (m/f): 297/213 scrub/4% chlorhexidine in mastectomy
e antiseptic Obesity: NR 70% isopropyl alcohol 2/8 appendectomy
skin Operative time hours paint; povidone-iodine 1/8 gastrectomy Other notes
preparations mean (range) scrub solution and paint. Numbers incorrectly reported
in general Intervention: 1.45 (45min- Monitoring intervention: For intervention group (transposed) within results
surgery 3hr) N/A RR 1.61 (CI 95%, 1.40- table 2.
patients Control: 1.43 (40 min-3 h) 1.81) Funding Source Conflicts:
Wound Classification Control: n=250 Authors: NR
Clean (I) Povidone-iodine scrub Other infections: NR Institution: NR
Intervention: 96 (38.4%) solution (5 minutes) Topic Specific Study: NR
Control: 87/250 (34.8%) followed by povidone outcomes: Not relevant Supplies: NR
Clean contaminated (II) iodine paint (Allowed to Reoperation: NR
Intervention: 118/250 (47.2%) dry? NR) Length of Stay: NR
Control: 112/250 (44.8%) Standard Preventive Readmission: NR
Contaminated (III) Measures: The authors Mortality: NR
Intervention: 46/250 (18.4%) allowed other pre- Adverse events: 2 cases
Control: 51/250 (20.4%) operative preparations of skin irritation from
Procedures: All general under the standard povidone-iodine and no
surgery guideline. What these allergies to chlorhexidine
Indications: NR were: NR
Setting: One university
hospital
Location: Thailand
Dates: June 2006 November
2008
Inclusion Criteria: Patients
aged 18-60 years old, with
clean (class 1), clean
contaminated (class 2), and
contaminated wounds (class
3) and ASA class 1 and 2
scores.
Exclusion Criteria: Patient
refusal, dirty wounds,
uncontrolled diabetes,
immunosuppressive drugs,
serum albumin levels less
than 3.0 mg/dl, and a history
2017 American Medical Association. All rights reserved. 397
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
of allergic reaction to either
study agent.
Veiga RCT To compare No. Patients: N=250 Intervention: n=125 SSI: 30 days Definitions:
124
2008 1 povidone- Patient Characteristics: Vigorous scrub with Superficial incisional: SSI: CDC definitions
(ES) iodine and Characteristics given antiseptic soap followed Intervention = 0/125 Perioperative care
chlorhexidin represent the whole study. by absorption with a Control =4/125 (1.6%) NR
e ethanolic Mean operation time: sterile towel. This was P= 0.06 Other notes
solutions for Intervention: 97.9 min followed by skin prep. Not statistically significant This paper is a Viewpoints in
skin Control: 107.9 min Skin was painted with Other infections: NR Plastic & Reconstructive
antisepsis Age: >18 years chlorhexidine 0.5% Topic-specific Surgery
before Gender: NR ethanolic solution and outcomes: Follow up: 30 days
elective, Obesity: NR allowed to dry for 2 Not relevant Funding Source Conflicts:
clean, plastic Procedures: Breast minutes Authors: None
surgery reconstruction, Timing of Intervention: Adverse events: NR Institution: None
procedures. mammoplasty, breast Preoperative Reoperation: NR Study: None
prosthesis, abdominoplasty, Duration of intervention: Length of Stay: NR Supplies: None
scar revision, zetaplasty, Intraoperative Readmission: NR
lipoma exeresis, Agents: Povidone-Iodine Mortality: NR
gynecomasty & 10%, or Chlorhexidine
supernumerary mamma 0.5%
Indications: NR Monitoring intervention:
Setting: 1 hospital Patients were followed up
Location: Brazil to 30 days to determine
Dates: NR postoperative infections
Inclusion Criteria: Patients Control group: n=125
>18 years of age, scheduled Vigorous scrub with
for elective and clean plastic antiseptic soap followed
surgery procedures. by absorption with a
Exclusion Criteria: NR sterile towel. This was
followed by skin prep.
Skin was painted with
10% Povidone-iodine
ethanolic solution and
allowed to dry for 2
minutes
Standard Preventive
Measures: NR
Ellenhorn RCT To prove the No. Patients: N=234 Intervention: n=119 Wound infection-30 days Definitions:
113
2005 1, 2, 10 equivalency Patient Characteristics: Patients underwent only Intervention: 12/ 119 Infection: defined by clinical
2017 American Medical Association. All rights reserved. 398
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
(ES) for two Demographic data (mean painting of the operative (10%) criteria as presence of
commonly age, obesity, diabetes, site with aqueous Control: 12/115 wound erythema or
used preoperative antimicrobial povidone-iodine solution (10%) purulence requiring
techniques administration, and Mean (available iodine 1.0%) P=0.078 therapeutic intervention
of surgical ASA score) were analyzed only. within the first 30 days after
skin site and not found to be Timing of Intervention: Other infections the surgical procedure
preparation. statistically significant Preoperative Intra-abdominal infection
[The between groups (All P10). Duration of intervention- Intervention: 2/ 119 (2%) Perioperative care:
techniques Age (mean) Intraoperative Control: 4/115 (3%) Hair Removal: A razor was
are 1) a Intervention: 57.7 y Agent: Aqueous povidone- P= 0.14 used to remove hair from the
scrub with Control: 60.5 y iodine (1.0%) and operative site. Other notes:
povidone- Gender: NR povidone-iodine detergent Topic-specific None
iodine soap The following (0.75%) outcomes: NR Follow up: 30 days after
followed by characteristics given Monitoring intervention: Reoperation: NR surgery.
paint with represent the whole study. NR Length of Stay: NR Funding Source Conflicts:
aqueous Obese: 43/234 (18.4%) Control: n=115 Readmission: NR Authors: None
povidone- Diabetic: 17/234 (7.3%) Patients underwent a Mortality: NR Institution: None
iodine OR 2) ASA score (mean) vigorous 5-minute scrub Adverse events: NR Study: None
only Intervention: 2.3 using urethane sponges Supplies: None
povidone- Control: 2.4 saturated with povidone-
iodine paint.] Procedures: Comparable iodine detergent
between groups except as (available iodine 0.75%).
noted Detergent was then
Colorectal: 79/234 (33.8%) absorbed with a blotting
Genitourinary: 38/234 (16.2%) towel before painting the
Pancreaticobiliary: 40/234 operative site with
(17.1%) aqueous povidone-iodine
Upper gastrointestinal: 38/234 solution (available iodine
(16.2%) 1.0%) which was allowed
Intervention: 24/20 (20%) to air-dry.
Control: 14/115 (12%) Standard Preventive
Other*: 39/234 (12.3%) Measures:
*Includes retroperitoneal Skin Prep: All patients had
sarcoma, lymph node all gross foreign material
dissection, second-look removed from the skin
ovarian cancer using a dry sponge and
Clean: 70/234 (29.9%) tape remover, if
Clean-contaminated: 164/234 necessary.
(70.1%) Shower: Patients were not
2017 American Medical Association. All rights reserved. 399
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Drain: 67/234 (28.6%) instructed to shower with
Indications: malignancy any antibacterial agent
Setting: cancer center before the operation.
Location: USA Non-Standard
Dates: NR Preventative measures:
Inclusion Criteria: Patients AMP: Use of perioperative
undergoing elective IV antimicrobials left to
abdominal operation the discretion of the
Exclusion Criteria: Active operating surgeon.
infection at the time of AMP given:
operation, neutropenia Total: 229/234 (98%)
defined as a white blood cell Intervention: 98%
count of <2000 or an Control: 97%
absolute neutrophil count of
<500, history of skin reaction
to iodine and anticipated use
of prosthetic material as part
of the surgical procedure.
Bibbo RCT To No. Patients: N=127 Intervention: n=60 SSI (Follow up NR) Definitions: None
122
2005 1, 10 determine Patient characteristics: A 7-minute scrub with No Postoperative wound
(ES) the efficacy Patient characteristics were chlorhexidine gluconate infections developed Perioperative care: NR
of recorded and analyzed and (4%) and isopropyl Other Infections: NR
chlorhexidin they found no differences alcohol (70%) paint. Topic specific Other notes: None
e compared between the two groups Allowed to dry before outcomes: Follow up: NR
with The following draping. Not relevant Funding Source Conflicts:
povidone- characteristics given Timing of Intervention: Reoperation: NR Authors: None
iodine as a represent the whole study. Preoperative Length of Stay: NR Institution: None
preoperative Mean age (Range): 46 y (16- Duration of intervention: Readmission: NR Study: None
skin 85y) intraoperative Reoperation: NR Supplies: None
preparation Gender (m/f): 61/66 Agent: Chlorhexidine Mortality: NR
agent in Obesity: NR gluconate (4%) and Adverse events: NR
reducing Co-morbidities: isopropyl alcohol (70%)
bacterial Compromised hosts: 35% paint; a Povidone-Iodine
skin (includes smokers, diabetics, scrub (7.5%); and a
contaminatio history of steroid use, or povidone-iodine paint
n before history of MRSA (10%)
clean, colonization) Monitoring intervention:
elective foot Procedures: NR Culture swabs taken from
and ankle Indications: NR all the toes, all webs
2017 American Medical Association. All rights reserved. 400
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
surgery. Setting: One Hospital spaces, nail folds, toe
Location: USA surfaces, and from the
Dates: NR site of the proposed
Inclusion Criteria: Patients surgical incision. Patients
with intact, uninfected skin having toe surgery had
having clean, elective foot the dorsal foot swabbed
and ankle surgery as the matching site.
Exclusion Criteria: Patients Swabs were sealed and
with open wounds, skin immediately transported
ulcers and/ or sores, an & processed for aerobic,
active acute or chronic anaerobic, acid fast, and
infection, or who were on fungal cultures
active antimicrobial therapy, Control: n=67
which could alter skin flora. A 7-minute scrub with
povidone-iodine (7.5%)
and painting of the foot
and ankle with a
povidone-iodine (10%)
solution. Allowed to dry
before draping.
Standard Preventive
Measures:
Shower: No special
instructions for bathing or
showering implemented
before surgery. Patients
followed their usual
personal hygiene on the
day of surgery.
AMP: Prophylactic
intravenous antimicrobials
(cefazolin or vancomycin
for patients with
documented penicillin
and/or cephalosporin
allergy) were
administered in the 20
minute window before
incision
2017 American Medical Association. All rights reserved. 401
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Adhesive drapes were not
used.
Ostrander RCT To assess No. Patients: N= 120 Intervention1: n=40 Postoperative infection: Definitions: NR
126
2005 1, 7, 8 the efficacy Patient characteristics: 3% chloroxylenol (Follow up-NR)
(ES) of three The following Intervention2: n=40 Total: 3/120 (2.5%) Perioperative care: All
different characteristics given 2% chlorhexidine gluconate Intervention1 procedures performed by
surgical represent the whole study. and 70% isopropyl Chloroxylenol: 2/40 (5%) one surgeon.
skin- Age y mean (range):48 (19-78) alcohol (1 polymicrobial SSI after Other notes: Power
preparation Gender (m/f): 47/78 Intervention 3 n=40 0.7% open reduction internal calculation not met.
solutions Obesity: NR iodine and 74% isopropyl fixation (ORIF) calcaneal Follow up: NR
(0.7% iodine Comorbidities: alcohol fracture and 1 atypical Funding Source Conflicts:
and 75% Diabetes: Timing of Intervention: mycobacterium SSI after Authors: Industry
isopropyl Intervention 1: 0 Preoperative excision of Morton Institution: None
alcohol; 3% Intervention 2: 0 Duration of intervention: neuroma) Study: None
chloroxyleno Control: 1/ 40 (2.5%) intraoperative Intervention2 Supplies: None
l; & 2% Rheumatoid Arthritis Monitoring intervention: Chlorhexidine gluconate
chlorhexidin Intervention 1: 2/40 (5%) NR and alcohol: 1/40 (2.5%)
e gluconate Intervention 2: 2/40 (5%) Control: Each group (Polymicrobial SSI after
and 70% Control: 4/40 (10%) served as its own control excision of large lipoma
isopropyl Liver disease: for colonies formed (used at lateral heel-portion of
alcohol) in Intervention 1: 2/40(5%) a more proximal tibial large tissue flap
eliminating Intervention 2: 0 site) underwent necrosis with
potential Control: 2/40 (5%) subsequent
bacterial Renal issues Standard Preventive development of SSI)
pathogens Intervention 1: 1/40 (renal Measures: Control Iodine-alcohol:
from the foot insufficiency) Shower: No home cleaning 0/40
by Intervention 2: 1/ 40 (renal or disinfectant protocols P<1.0
evaluating transplant) utilized prior to surgery. Other infections: NR
the residual Intervention 2: 1/40 (end AMP: All patients received Topic Specific
bacterial stage renal disease) intravenously Outcomes: NA
skin Control : 1/40 (renal failure) administered cefazolin) Adverse events: NR
contaminatio Procedures: Foot and ankle within one hour of the Reoperation: NR
n following surgery surgical start time. Length of Stay: NR
surgical skin Indications: NR Readmission: NR
preparation. Setting: One hospital Mortality: NR
Location: USA
Dates: October 2002 May
2003
Inclusion Criteria: Patients
2017 American Medical Association. All rights reserved. 402
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
undergoing foot and ankle
surgery
Exclusion Criteria: If patients
had an open wound,
abrasion, or current infection.
Segal RCT To evaluate No. Patients: N=209 Intervention1: n=52 Sternal wound Definitions
114
2002 1, 2, 5, the effect of Patient characteristics: Povidone-iodine five-minute Infections: 6 weeks Obesity: BMI>120% of ideal
(ES) 9 four different Patient demographics scrub with paint Intervention1: 7/52 weight.
skin compared. Intervention2: n=50 (13.5%) SSI: Clinical exam for signs of
preparations The following One-step iodophor/alcohol Intervention2: 1/50 (2.0%) drainage, redness,
on the characteristics given water insoluble film Intervention 3: 3/51 (5.9%) tenderness, or sternal
incidence of represent the whole study. Intervention3: n=51 Intervention 4: 7/56 instability. Sternal surgical
sternal SSIs All patients had at least one one-step iodophor/alcohol (12.5%) site exhibiting any of these
in patients high-risk factor (the basis of water insoluble film with P=0.117 signs was cultured. Positive
undergoing the study). iodine impregnated Infections per treatment cultures were correlated with
coronary 39% had 2 risk factors surgical adhesive drape Aqueous Iodine ( clinical evidence according
artery 4% had 3 risk factors Intervention 4: n=56 Intervention 1+4) to the CDC guideline to
bypass graft (Percentage numbers appear Povidone-iodine paint 14/108 (13.0%) indicate a sternal SSI
surgery larger in bar graph within Timing of Intervention: Insoluble Iodine
(CABG) paper my copy is difficult to Preoperative (Interventions 2 and 3) Perioperative care
who were read) Duration of intervention: 4/101 (4.0%) NR
identified as Age (y): Mean Intraoperative P=0.02 Other notes
=5.3
2
high risk of 60.9 years (no SD given) Agents: Solutions, Impregnated drapes in
developing Gender: Over 75% male insoluble film & incise Other infections: NR Intervention 3 shown to be
sternal SSI Obesity: NR drapes not specified Topic-specific ineffective as an intervention.
Redo sternotomies: 11.5% Monitoring intervention: outcomes: NR Study deemed underpowered
Procedures performed using Observation by nurses Reoperation: NR Follow up: 6 weeks
the IMA: 88.5 Control: Length of Stay: postoperatively through
Uninfected patients had regularly scheduled clinic
MeanSD Standard Preventive a 5-6 day shorter length visits
Total OR time: 248 min 29 Measures of hospital stay than Funding Source Conflicts:
Cross clamp time: 42 min20 Shower infected patients. Authors: NR
Last OR Glucose: 434210 The nurse instructed Mortality: NR Institution: NR
Procedures: elective CABG patients to take an Adverse events: NR Study: NR
Surgery antimicrobial shower the Supplies: NR
Indications: NR evening before and the
Setting: 1 tertiary/ teaching morning of surgery, or if
hospital they were inpatients, they
Location: USA were given a preoperative
2017 American Medical Association. All rights reserved. 403
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Dates: Oct 1, 1994 April 30- antimicrobial shower in
1997 the hospital.
Inclusion Criteria: Patients Hair removal
undergoing elective CABG If necessary, a qualified
with one or more of the patient care assistant
following conditions: clipped patients hair the
Diabetes morning of surgery in
Obesity patients rooms.
Chronic Obstructive AMP: All patients received
Pulmonary Disease (COPD) a prophylactic
Exclusion Criteria: Patients antimicrobial (i.e.,
with an allergy to topical cefuroxime) or if they had
iodine or with a preexisting a documented allergy to
infection indicated by a white penicillin, they received
blood cell count higher than vancomycin in
10,000 or by a temperature appropriate dosing
o
higher than 100.5 F window to provide
o
(38.06 C) because their adequate coverage at the
procedures were performed time of incision.
emergently.
Hort RCT To No. Patients: N=49 Intervention: n= 25 feet SSI (Follow up NR) Definitions( e.g., SSI)
118
2002 1, 4, 5 investigate Patient Characteristics: Age, (23 patients[2 received NO patient in either group Not defined
(ES) the gender, weight, co- bilateral procedures-]) showed clinical signs of Perioperative care
usefulness morbidities: NR Patient was given two wound infection and all NR
of standard Bilateral Procedures: chlorhexidine gluconate wounds healed Other notes: If a patient
surgical Intervention: 2/23 scrub brushes with uneventfully. underwent a bilateral
preparation Control: 6/26 directions to perform two procedure, both feet
(with separate self-scrubs Other Infections: NR assigned to the same group.
chlorhexidin Procedures: NR several hours apart Topic specific Follow up: NR
e gluconate Indications: NR before retiring to bed the outcomes: NR Funding Source Conflicts:
home scrubs Setting: 1 Hospital night before the Reoperation: NR Authors: NR
and Location: USA operation. In the Length of Stay: NR Institution: NR
preoperative Dates: NR operating room, a 10 Mortality: NR Study: NR
povidone- Inclusion Criteria: Patients minute scrub with Adverse events: NR Supplies: NR
iodine or the undergoing foot or ankle povidone-iodine topical
chlorhexidin surgery solution was followed by
e gluconate Exclusion Criteria: Total painting of the foot with
home scrubs ankle arthroplasties povidone-iodine topical
2017 American Medical Association. All rights reserved. 404
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
plus pre- solution plus the addition
operative of a 3-minute
70% alcohol) preoperative preparation
in prevention of the area with 70%
of surgical alcohol.
site Timing of Intervention:
contaminatio Preoperatively
n. Duration of intervention:
intraoperative Agents:
Povidone-Iodine solution;
Scrub Brushes
Monitoring intervention:
NR
Control: n=32 feet (26
patients;6 had bilateral
procedures)
Patient was given two
chlorhexidine gluconate
scrub brushes with
directions to perform two
separate self-scrubs
several hours apart
before retiring to bed the
night before the
operation. In the
operating room, a 10
minute scrub with
povidone-iodine topical
solution was followed by
painting of the foot with
povidone-iodine topical
solution.
Standard Preventive
Measures
AMP: All patients were
given one dose of broad-
spectrum intravenous
antimicrobial
preoperatively (usually
2017 American Medical Association. All rights reserved. 405
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
cefazolin before
tourniquet)
Operative irrigation:
Wounds were irrigated
frequently during surgery
with an antimicrobial
solution.
Roberts RCT To compare Number of patients: n=200 Intervention group: n=104 SSI (30days) Definitions:
117
1995 1, 2, 7, the efficacy Patient Characteristics: no 1step: patients underwent Overall Infection: Infected Wounds: if purulent
(ES) 8, 9 of 2 significant differences in 1 step iodophor in water 1step: 10/104 (9.6%) material drained from the
commerciall patient characteristics application preop. And 2step: 9/96 (9.4%) incision site. Confirmation of
y available between groups. allowed to air dry NS infection by a positive culture
skin preps: a Age: NR thoroughly for 2-3 min. 1 Chest Infection was not necessary.
relatively Gender: NR unit was used for each 1step: 4/104 (3.8%) Superficial infected surgical
new 1-step, Obesity: NR chest, and each leg. 2step: 6/96 (6.3%) wounds: involved the skin,
iodophor in Comorbidities: NR Timing of intervention: NS subcutaneous tissue or
alcohol, film- Procedures: CABG preop Deep Chest Infection muscle located above the
forming, Indications: NR Duration of intervention: 1step: 0/104 fascial layer.
water- Setting: 1 general hospital NA 2step: 3/96 (3.1%) Deep infected surgical
insoluble Location: USA Device/agent: aqueous wounds: involved tissues or
skin prep, Dates: NR just mentioned a 1 iodophor Leg Infection: spaces at or beneath the
versus the year period Monitoring intervention: 1step: 6/104 (5.8%) fascial layer including
tradition al 5- Inclusion Criteria: consenting NR 2step: 5/96 (5.2%) wounds that spontaneously
10 minute adults undergoing CABG Control group: n=96 NS dehisced or were
aqueous Exclusion Criteria: if patients 2step: patient underwent a deliberately opened for
iodophor were allergic to iodine or its traditional 2step starting Other infections: no drainage.
scrub and compounds with a 5-10min scrub of evidence found for either Elderly: 65yo or older
paint. In both operative sites (chest and group Perioperative care: In both
groups, an legs) with aqueous Topic-specific groups, an iodophor-
iodophor- iodophor solution followed outcomes: NR containing antimicrobial
containing by an application of an Reoperations: incise film was also applied
antimicrobial iodophor solution. The All 3 deep wounds in on the chest. No incise film
incise film sites were then blotted control group required was used on the leg.
was also dry with a sterile towel. surgical intervention. Other notes: Small sample
applied on Standard preventive Length of stay: NR size. Too small to perform
the chest. measures: multivariate analyses.
No incise Showers: patients had Mortality: NR Follow-up: 30 days
film was antimicrobial (iodophor) Adverse events: NR Funding Source Conflicts:
used on the showers on the night prior Authors: NR
2017 American Medical Association. All rights reserved. 406
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
leg. to surgery Institution: NR
AMP: Cefuroxime started in Study: NR
OR approx. 30 min prior Supplies: NR
to incision and continued
every 6h for 36h postop.
Hair removal: with clipper.
Gilliam RCT To compare No. Patients: N=60 Intervention: n=30 SSI (follow up NR) Definitions:
115
1990 1, 8, 9 the efficacy Patient characteristics: Age, Skin was prepared with a None of the patients NR
(ES) of a sex, & duration of operation one-step application of a became infected
traditional were not statistically water-insoluble iodophor- Other Infections: No Perioperative care
skin significantly different in-alcohol solution applied Infections Hair Removal: All hair was
preparation between groups. as paint. Skin was Topic Specific Outcome: removed by dry shave just
of an Age (average), y: allowed to dry before Drape Lift: (yes or no prior to preparing the skin.
aqueous Intervention: 65y covering the surgical area phenomenon) Other notes
iodophor Control: 61y with a sterile, non- Intervention: 0/30 Intervention was found to
consisting of Gender (m:f): antimicrobial plastic Control: 12/30 (40%) increase incise drape
a five-minute Intervention: 11:19 surgical adhesive drapes. P<0.01 adhesion, particularly at the
scrub-and- Control: 8:22 Timing of Intervention: Reoperation: NR wound edges.
paint AND a Obesity: NR Preoperative Length of Stay: NR Follow up: NR
sterile non- Length of Operation (average), Duration of intervention: Readmission: NR Funding Source Conflicts:
antimicrobial Min (range): Intraoperatively Mortality: NR Authors: NR
plastic Intervention: 135 (30-310) Agent Water-insoluble Adverse events: NR Institution: NR
surgical Control: 130 (160-300) iodophor-in-alcohol Study: NR
adhesive solution Supplies: NR
drapes. With Procedures: Primary or Monitoring intervention:
the efficacy revision total hip or total For liquid skin prep NR
of a single knee arthroplasty except for surgical
application Indications: NR adhesive drape, where
of a water- Setting: 1 hospital adhesion to the skin was
insoluble Location: USA evaluated by the
iodophor-in- Dates: NR operating surgeon prior to
alcohol Inclusion Criteria: Patients wound closure
solution undergoing clean total joint Control: n=30
AND a surgery. Skin was prepared with a
sterile non- Exclusion Criteria: NR traditional five-minute
antimicrobial aqueous iodophor scrub
plastic followed by the
surgical application of an aqueous
adhesive iodophor solution as
2017 American Medical Association. All rights reserved. 407
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
drapes. paint. Skin was allowed to
dry before covering the
surgical area with a
sterile, non-antimicrobial
plastic surgical adhesive
drapes.
Standard Preventive
Measures
Preop Shower: All patients
showered the night before
surgery with chlorhexidine
gluconate soap.
Environmental: Surgery
was conducted under a
horizontal unidirectional
laminar air-flow system.
Berry RCT To compare No. Patients: N=866 Intervention: n=453 SSI (Follow up: not Definitions:
125
1982 1, 2, 6, the effect of Patient Characteristics: Two applications of 0.5% clear- wound assessed No definitions, wounds were
(ES) 7, 8, 9 alcoholic Operative & demographic chlorhexidine alcohol. 3-4 days postop and at judged at evaluators
povidone- information was deemed Skin preparation solution discharge) discretion as normal,
iodine and similar between study was applied with sterile More than one type of erythematous, edematous,
alcoholic groups. Details not reported sponges. abnormality reported on discharging or purulent.
chlorhexidin Age: Timing of Intervention: some wounds Moist wounds were swabbed
e (both as <15 years Preoperative Wound abnormality: Any & cultured for both aerobic
skin prep Intervention: 4 (0.9%) Duration of intervention: abnormality agreed by (Cowan 1974) & anaerobic
and surgical Control: 4 (1.0%) Intraoperatively both observers at (biochemical tests)
scrub) on 15-64 years Agent: povidone iodine discharge, all organisms
the Intervention: 338 (74.6%) 10% in alcohol or 0.5% operations Perioperative care : NR
incidence of Control: 309 (74.8%) chlorhexidine in spirit Any wound abnormality
postoperativ 65 years Monitoring intervention: Intervention: 44/453 Other notes: None
e wound Intervention: 112 (24.7%) NA (9.7%) Follow up: Wounds were
infection in a Control: 100 (24.2%) Control: n=413 Control: 61/413 (14.8%) assessed independently by
(1)= 4.7, P=0.03
2
general Gender: NR Two applications of one member of the nursing
surgical unit Obesity: NR povidone-iodine 10% in Biliary tract staff and one member of the
Procedures, No (%): (N=886) alcohol. Skin preparation Intervention: 6/90 (6.7%) medical staff at a standard
Operations on biliary tract: 167 solution was applied with Control: 15/77 (19.5%) period of 3-4 days post-
(1)= 5.1, P<0.05
2
(18.8%) sterile sponges. operatively and then at
Large bowel operations: 61 Other clean operations discharge
(6.9%) Standard Preventive Intervention: 2/105 . If patient was discharged
2017 American Medical Association. All rights reserved. 408
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
rd
Other laparotomy operations: Measures (1.9%) before the 3 day was
96 (10.8%) Surgical hand Scrub: A Control: 13/99 (13.1%) assessed just prior to leaving
(1)= 7.9, P<0.05
2
Hernia/genitals/varicose veins sterile brush was used to the hospital.
338 (38.1%) scrub the hands, paying Differences in procedures Funding Source Conflicts:
Other clean non-abdominal: particular attention to the below, not statistically Authors: NR
204 (23.0%) areas under the nails and significant: Institution: NR
Indications: NR in the nail folds. The Large Bowel Study: NR
Setting: 1 hospital forearms were washed as Intervention: 5/28 Supplies: NR
Location: United Kingdom far as the elbow. Skin (17.9%)
Dates: May 1978 February was scrubbed for 4-5 Control: 3/33 (9.1%)
1980 minutes as Other Laparotomy
Inclusion Criteria: All elective recommended. Intervention: 15/49
surgical cases Control: Scrub solution (30.6%)
Exclusion Criteria: Patients was alcoholic povidone- Control: 9/47 (19.1%)
known to be sensitive to iodine (10% available Hernia, genitalia, veins
either skin preparation iodine) Intervention: 16/181
utilized in this study. Intervention: Scrub (8.8%)
solution was alcoholic Control: 21/157 (13.4%)
chlorhexidine with .5%
available chlorhexidine. Wound abnormalities:
Hair removal: Skin shaving Specific abnormality
was routinely performed agreed by both
on hairy skin 18-24 hours observers at
preoperatively discharge, all
Non-Standard Preventive operations
Measures: Redness of wound:
Antimicrobial Prophylaxis Intervention: 16/453
Only patients undergoing (3.5%)
colonic & rectal surgery Control: 21/413 (5.1%)
received metronidazole 3 Swelling of Wound:
times daily and neomycin Intervention: 12/453
four hourly for 3 days. (2.6%)
Bowel Prep: Routine bowel Control: 12/413 (2.9%)
prep was used only in Discharge from wound:
large bowel surgery. Intervention: 16/453
(3.5%)
Control: 21/413 (5.1%)
Pus from wound:
Intervention: 13/453
2017 American Medical Association. All rights reserved. 409
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
(2.9%)
Control: 22/413 (5.3%)
Any abnormality agreed
by both observers 3-4
days postop (Note: *64
intervention and 59
control patients were
discharged before 3
days, therefore the total
population for results
below is:
Intervention: n=389
Control: n=354Infection
was slightly more common
overall in the control group
but the difference was not
statistically significant:
Total wound abnormalities
Intervention: 27/389
(6.9%)
Control: 35/354 (9.9%)
Biliary tract
Intervention: 2/90 (2.2%)
Control: 8/76 (10.5%)
Large Bowel
Intervention: 3/28
(10.7%)
Control: 0/31
Other Laparotomy
Intervention: 7/49
(14.3%)
Control: 5/47 (10.6%)
Hernia, genitalia, veins
Intervention: 13/157
(8.3%)
Control: 16/150 (10.7%)
Other clean operations
Intervention: 2/65 (3.1%)
Control: 6/50 (12.0%)
2017 American Medical Association. All rights reserved. 410
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Any abnormality
recorded by one or
both observers 3-4 day
postop (i.e.
disagreement between
observers)
Total wound abnormalities
Intervention: 41/389
(10.5%)
Control: 44/354 (12.4%)
Biliary tract
Intervention: 4/90 (4.4%)
Control: 11/76 (14.5%)
(1)= 3.9, P<0.05
2
Overall infection rate for
clean operations
(excluding colonic &
biliary): 11.9%
Infection/ abnormality
rates varied between
surgeries and groups.
NO overall statistically
significant advantage for
either group emerged for
an all-purpose skin prep
solution.
Other Infections: NR
Topic Specific
Outcomes: NA
Reoperation: NR
Length of Stay: NR;
Analysis of the date for
each group showed no
significant difference
between the
preparations in the mean
length of patients stay in
2017 American Medical Association. All rights reserved. 411
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
the hospital
Readmission: NR
Mortality: NR
Adverse events: NR
eTABLE 48. Evidence Table for Q8C. How safe and effective is the application of a microbial sealant immediately following
skin preparation?
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Dromzee RCT To test the Number of patients: Intervention group: n=28 SSI : Definitions:
131
2012 1, 2, 10 hypothesis N=56 Sterile, film-forming cyanoacrylate Total: 6/56 (10.7%) SSI not defined
(ES) that microbial Patient Characteristics liquid application before Intervention: 5/28 Perioperative care:
sealant Age, year: mean (SD) application of the incise drape (18.2%) Anesthesia: general
reduces Intervention: 14.93 (1.7) Timing of intervention: Control: 1/28 (3.6%) anesthesia was used
surgical site Control: 15.21 (1.9) Intraoperative P=0.096 Other notes: 50 patients =
infection in P=0.570 Duration of intervention: NR There were 3 deep and number of cases required to
children and Gender: B NR Device/agent: film forming 3 superficial have an 80% chance of
adolescent Obesity: NR cyanoacrylate liquid infections but it is not detecting an effect of 0.05.
patients with Comorbidities: NR Monitoring intervention: NA report which group Follow-up: NR
scoliosis Number of fused levels, Control group: n=28 they belonged in Funding Source Conflicts:
undergoing mean (SD) Incise drape alone. Authors: None
scoliosis Intervention: 11.93 Standard preventive measures: All infections resolved Institution: None
correction. (2.7) AMP: NR after local wound Study: None
Control: 12.54 (3.09) Pre-op bathing: all patients debridement and Supplies: None
P=0.440 showered with a povidone iodine antibiotics.
Intraoperative blood loss skin antiseptic the day before the
(ml) mean (SD) surgery and early in the morning Age as risk factor for
Intervention: 539.64 of the surgery. early infection
(284.09) Skin prep: in OR using 2 Mean age (SD)
Control: 658.93 consecutive applications of one- Infection (n=6): 17.07
(489.15) step 5% povidone-iodine & (0.47)
P=0.271 alcohol solution. No infection (n=50):
Intraoperative time (min), Drapes: both groups used sterile 14.83 (1.8)
mean (SD) incise drapes P<0.0001
Intervention: 196.61 Drains one to three suction drains
2017 American Medical Association. All rights reserved. 412
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
(62.76) were placed in the wound before Other infections: NR
Control: 234.64 (90.65) closure. Topic-specific
P=0.074 Closure: either skin staples or outcomes: NR
4-6 Week preoperative bioresorbable skin sutures at Reoperations: NR
halo traction: 6/56 surgeons discretion. Length of stay: NR
(10.7%) [which group Mortality: NR
NR] for stiff and Adverse events:
severe deformity No immediate or
Procedures: Scoliosis delayed adverse
correction effects related to the
Indications: 29 had use of sealant were
spinal deformities noted.
from various
neuromuscular
causes. 27 had
adolescent idiopathic
scoliosis.
Setting: 1 university
hospital
Location: France
Dates: June 2010 and
June 2011
Inclusion Criteria: (1)
idiopathic or
neuromuscular
scoliosis, and (2)
indicated for posterior
correction and fusion
Exclusion Criteria: (1)
previous spinal
surgery and (2)
indicated for anterior
or combined
procedures.
2017 American Medical Association. All rights reserved. 413
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
von RCT To determine Number of patients: Intervention group: SSI: (follow up 30 days Definitions:
Eckards- 1, 2, 6, if the use of N=293 Intention to treat (ITT): n= 146 postop) SSI: CDC/ NNIS criteria
tein 7, 8, 9 cyanoacrylate Patient Characteristics: Per protocol: n=131 Patients may have more Adverse events: any
128
2011 -based skin There was no Surgical sites were prepared with than 1 SSI undesirable clinical
(ES) sealant before significant difference commonly used surgical skin For ITT Analysis Below occurrence in a patient that
coronary between groups preparations such as povidone- Intervention: n=146 may be attributed to the
artery bypass except in occurrence iodine or 0.7% available iodine in Control: n=147 study treatment or to SSI.
grafting of obesity (see below) isopropyl alcohol 74%w/w. Total SSIs: Perioperative care: NR
(CABG) could Age, y: mean (SD) Skin sealant was applied on the 23/293 (7.8%) Other notes: None
reduce Intervention: 63.2 surgical sites after surgical skin Intervention: 9/146 Follow-up: For the duration of
surgical (8.53) preparations and just before (6.2%) hospitalization and for 30
wound Control: 62.9 (9.97) making the incision. Surgical Control: 14/147 (9.5%) days postop
contamination Gender (m:f) incise drapes (if used) were p=0.285 Funding Source Conflicts:
by skin Intervention: 120/26 applied after all surgical skin The majority were Authors: None
microflora and Control: 129:18 preparations had dried superficial SSIs: Institution: None
decrease Obesity (BMI>30.0 to completely. Skin sealant was Incision site infection Study: None
37 kg/m )
2
post- considered dry when a film Intervention: 6 (2.7%) Supplies: None
procedure Intervention: 40 formed on the skin. Control: 10 (6.6%)
infections. (27.6%) Timing of intervention:
Control: 20 (13.6%) Intraoperatively Although there
P=0.003 Duration of intervention: frequency of patients
Comorbidities Intraoperatively with SSI was similar
Diabetes Mellitus, Device/agent: Cyanoacrylate- between groups, the
Type I or Type II based skin sealant use of skin sealant
Intervention: 49 Monitoring intervention: NR was associated with a
(33.6%) Control group: 35% relative risk
Control: 49 (33.3%) ITT: n= 147 reduction in the
Tobacco Use, Per Protocol: n=138 occurrence of SSI
Intervention: 84 Surgical sites were prepared with In the subgroup of
(57.5%) commonly used surgical skin obese patients, there
Control: 91 (61.9%) preparations such as povidone- was a relative risk
Alcohol use iodine or 0.7% available iodine in reduction for SSI of
Intervention: 42 isopropyl alcohol 74%w/w. 83.3% associated
(28.8%) with use of skin
Control: 52 (35.4%) Standard preventive measures: sealant. However,
Duration of surgery NR this is based on small
(min): Non-standard preventive patient and event
Intervention: 227.6 (42.4) measures: numbers:
Control: 211.7 (60.6) AMP: administered at the discretion Obesity
2017 American Medical Association. All rights reserved. 414
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
P=0.469 of the surgeon and according to Intervention: 1/40
Intraaortic balloon pump: hospital protocol (2.5%)
Intervention: 9 patients Surgical procedure: dictated by Control: 3/20 (15.0%)
Control: 4 patients current practice and not specified P=0.0.015
Procedures: Elective in the study protocol
Coronary artery Patients with at least
bypass grafting one SSI:
(CABG) Sternal Site Infection
Indications: NR Intervention: 4 (2.7%)
Setting: 5 Centers Control: 7 (4.8%)
Location: USA, Europe, P=0.363
Asia and Latin Graft Site Infection
America Intervention: 7 (4.8%)
Dates: April 2006 - Control: 7 (4.8%)
February 2009 P=0.989
Inclusion Criteria: NOTE:
Patients aged 18 Left saphenous vein
years or older who graft harvest in 74%-
were undergoing 78% of patients
elective CABG Left radial artery or right
surgery with median saphenous vein graft
sternotomy and the harvest in 25-30% of
use of saphenous patients
vein or radial artery as Location and number of
1 of the graft sites. harvest sites did not
Exclusion Criteria: appear to affect risk
Patients undergoing of SSI but does add
additional procedures, further variation to the
known sensitivity or study
allergy to
cyanoacrylate, Sternal and/or Graft
isopropyl alcohol, Site(s)_ Infection
iodine or iodine- Intervention: 9 (6.2%)
containing products or Control: 14 (9.5%)
tape. Also abnormal P=0.285
skin conditions Both Sternal and Graft
around the surgical Site Infection
incision site, Intervention: 2 (1.4%)
antimicrobial- Control: 0
2017 American Medical Association. All rights reserved. 415
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
impregnated incise P=0.247
drapes used during
the operation, Infections for Total
chemotherapy, Population
immunosuppressive Denominators:
therapy or steroid Intervention: n= 146
therapy, use of Control: n= 147
antimicrobials for an Arteriovenous graft site
active infection, HIV infection
infection with CD4 Intervention: 1 (0.7%)
3
count <350mm , Control: 0
therapeutic radiation Incision site infection
or renal dialysis, Intervention: 6 (2.7%)
morbid obesity Control: 10 (6.6%)
2
(BMI>37kg/m ); Mediastinitis
neutropenia, Intervention: 3 (2.1%)
intraaortic balloon Control: 2 (1.4%)
pump or mechanical Osteomyelitis
assist device in place Intervention: 1 (0.7%)
preoperatively, and Control: 1 (0.7%)
hospital stay >14 days Postoperative Wound
Infection
Intervention: 0
Control: 1 (0.7%)
Skin graft Infection
Intervention: 0
Control: 1 (0.7%)
Wound Infection
Intervention: 1 (0.7%)
Control: 0
Other infections: NR
Topic-specific
outcomes:
Frequency of Surgical
Site infection in
patients with Alcohol
use, Tobacco use &
Obesity
2017 American Medical Association. All rights reserved. 416
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Alcohol Use
Intervention: 2/42
(2.7%)
Control: 6/52 (4.8%)
P=0.291
Tobacco Use
Intervention: 3/84
(3.6%)
Control: 11/91 (12.1%)
P=0.050
Obesity
Intervention: 1/40
(2.5%)
Control: 3/20 (15.0%)
P=0.0.015
Skin sealant associated
with a relative risk
reduction of 83% for
obese patients
Alcohol Use or Tobacco
Use or Obesity
Graft Site Infection
Intervention: 2/108
(1.9%)
Control: 6/112 (5.4%)
P=0.037
Sternal Site Infection
Intervention: 4/108
(4.6%)
Control: 5/112 (4.5%)
P=0.546
Graft and/or Sternal Site
Infection
Intervention: 5/108
(4.6%)
Control: 11/112 (9.8%)
P=0.024
Reoperations:
2017 American Medical Association. All rights reserved. 417
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Postoperative re-
exploration of sternal
incision site
Intervention: 5/ 146
(3.4%)
Control: 3/ 147 (2.0%)
Length of stay: NR
Mortality: 4 (1.4%) total
(none considered
related to study
treatment)
Intervention: 1/146
(0.7%)
Sudden death after
spasm of the graft,
myocardial infarction,
pulmonary embolism,
and air embolism
Control: 3/ 147 (2.0%)
1/3 excessive
bleeding, atrial
fibrillation, and global
abdominal ischemia
1/3: ventricular
fibrillation
1/3: hemorrhagic
shock, erosion of the
right atrium and
mediastinitis
P=0.363
Adverse events:
Intervention: n= 146
Control: n= 147
Overall fewer than 10%
of subjects
experienced adverse
events during the
study and most were
related to SSIs
2017 American Medical Association. All rights reserved. 418
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Erythema
Intervention: 1/146
(0.7
Control: 0/ 147
Surgical and medical
procedures:
Hospitalization
Intervention: 0/ 146
Control: 1/ 147 (0.7%)
Iyer RCT To determine Number of patients: Intervention group: n= 47 SSI: (follow up: 1 Definitions:
129
2011 1, 3, 4, the effect of N=47 (94 legs) The long saphenous vein grafts month) Infection: if the wound showed
(ES) 5, 10 pretreatment Patients served as were taken from the below-knee Total saphenous vein signs of infection, it was
with n-butyl their own controls segment in both legs of all harvest site SSI: graded by the Southampton
cyanoacrylate Patient Characteristics: patients. Skin was disinfected 13/94 (13.8%) wound grading system
-based Baseline using alcoholic povidone-iodine Intervention: 1/ 47 (Bailey 1992)
microbial skin characteristics solution & 3 minutes were (2.1%) Grades as follows:
sealant to the between the treated allowed for the disinfecting Control: 12/ 47 (25.5%) 0: Normal healing
saphenous and untreated legs solution to dry. The sealant was P=0.0011; 95% CI for 1: Normal healing with bruising
vein graft were similar because applied to only 1 leg per case difference (-0.374 to - or erythema, subclassified
harvest site in the procedure was after the disinfecting solution was 0.0945) as A, B, or C according to
a population conducted on the allowed to dry. An applicator was the size of bruising
undergoing same individual. used to apply a single even layer Intervention: The leg 2: erythema with other signs of
cardiac Age y, mean (SD): 67.0 of microbial sealant over an area developed a severe inflammation subclassified
surgery and (7.6) overlying the saphenous vein infection and required as A, B, or C according to
discuss its Gender (m:f): 39:8 harvest site. The sealant was incision and drainage. findings at 1 point around
potential use Obesity- NR allowed to dry for 2 minutes. In the same patients, the suture or around the
in decreasing Comorbidities Skin sealant was NOT used at the the untreated leg had whole wound
infections in Arterial hypertension: 31 sternal site. no infection. 3: hemoserous discharge
other kinds of (65.9%) Timing of intervention: Control: These 12 legs (A<2cm, B>2cm, C=large
surgery. Peripheral vascular Intraoperatively showed evidence of volume, d>3 days)
disease: 0 (0%) Duration of intervention: infection that ranged 4: purulent discharge (A<2cm,
Venous disease in the Intraoperatively from oozing of serous B>2cm)
legs: 0 (0%) Device/agent: Cyanoacrylate- fluid which responded 5: deep or severe infection
Diabetes Mellitus: 12 based skin sealant to conservative with or without tissue
(25.5%) Monitoring intervention: NR therapy (n=7) to breakdown.
Hyperlipidemia: 40 Control group: n= 47 severely infected Perioperative care: NR
(85.1%) Skin was disinfected using alcoholic wound requiring Other notes: the study was
Renal Failure: 4 (8.5%) povidone-iodine solution & 3 incision and drainage terminated after ethical
Ejection fraction, mean minutes were allowed for the (n=4) and committee review at the
2017 American Medical Association. All rights reserved. 419
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
(SD): 47.3 (13.3) disinfecting solution to dry. No debridement (n=1) enrollment of 47 patients
Procedures: Coronary skin sealant. Follow-up: 1 month (if the
artery bypass graft Standard preventive measures: There were no other general practitioner involved
(CABG) requiring 3 or Surgical technique: apart from infections observed at with the care after
more lengths of long application of the sealant, the 30 days and discharge detected an
saphenous vein to surgical technique in both legs investigators were not infection before the 4-week
achieve was identical and the vein was aware of any follow-up, an appointment
revascularization. harvested using a single open infections developing was arranged before the
Additional internal incision. Endoscopic techniques after this point. stipulated follow-up and the
thoracic conduit was were not employed and in most findings were recorded.
also routinely used of the patients, the below portion Other infections: NR Funding Source Conflicts:
Indications: NR of the vein was harvested. Topic-specific Authors: None
Setting: 1 hospital Hair removal: performed using an outcomes: Institution: None
Location: Australia electrical clipper the day before Southampton Grade Study: None
Dates: Began August surgery. Intervention: 1/1: Grade Supplies: None
2008 - ???? (NR) Shower: patients washed with soap 4B
Inclusion Criteria: the morning of surgery Control: 3/12: Grade 5
Patients undergoing Drapes: iodine impregnated drapes 2/12: Grade
CABG requiring 3 or were used in all patients. 4B
more lengths of long Closure: Closure of the 2/12: Grade
saphenous vein to subcutaneous layer was with 2-0 3D
achieve absorbable, braided synthetic 4/12: Grade
revascularization sutures, and subcuticular closure 3B
Exclusion Criteria: If of the skin was with 3-0 synthetic 1/12: Grade
the patient required absorbable sutures. A 3A
2 segments of vein hydrocolloid dressing was used
wherein only 1 leg in all patients Reoperations:
was used and any Normothermia: All patients Intervention: The
features that would underwent systemic cooling to infected leg required
o o
cause dissimilarity 32 to 34 C. incision and drainage.
between the legs, Control: 1 severely
which included the infected leg required
vein in either leg not debridement.
being usable, Length of stay: NR
unilateral vascular Mortality: NR
disease, or skin Adverse events:
lesion. Also if there No patients had
was a discrepancy in perioperative
the length of the infarctions and there
2017 American Medical Association. All rights reserved. 420
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
incision between the were no adverse
treated and untreated intraoperative events.
legs.
Towfigh RCT To compare Number of patients: Intervention group: n=83 SSI (2 and 4 weeks): Definitions:
130
2008 1, 2, 3, the safety and N=166 (evaluable for (Per Protocol: 68) Total SSI: 3/148 (2%) Signs of infection: swelling,
(ES) 4, 5, 7, effectiveness effectiveness of Standard surgical skin preparation Intervention: 0 erythema, drainage,
8, 9, 10 of microbial antimicrobial sealant) including a skin prep of 10% Control: 3/80 (3.8%) warmth. And dehiscence.
sealant in Note: 148 (84%) in per povidone-iodine on the operative All 3 SSIs were Perioperative care: NR
reducing the protocol analysis field which was allowed to dry. positive for S. aureus Other notes: A patient was
incidence of Patient Characteristics: This was followed by a single and 1/3 of these was considered lost to follow up
surgical There were no coat application of the a deep infection with after 4 unreturned attempts
incision statistically significant cyanoacrylate-based microbial MRSA at contact.
bacterial differences between sealant. The sealant was allowed Given the low number of Follow-up: at 2 and 4 weeks
contamination the two groups. to dry before the application of events and early postoperatively to access
relative to Age: mean (SD) y surgical drapes. termination of the the incision
surgical skin Intervention: 52.7 study, it is Funding Source Conflicts:
preparation (15.9) Timing of intervention: Pre intra, underpowered to Authors: None
alone in Control: 54.1 (14.9) and postoperatively detect a difference in Institution: None
elective open Values below based on Duration of intervention: Pre intra, SSI. Study: Industry
inguinal Total pop: N=177 and postoperatively Supplies: Industry
hernia repair. Intervention n=88 Device/agent: Cyanoacrylate- Other infections: NR
Control n=89 based microbial sealant Topic-specific
Gender (male) Monitoring intervention: NR outcomes:
Intervention: 84/88 Control group: n=83 Most patients did not
(95.5%) (Per Protocol: 80) maintain a sterile
Control: 86/89 (96.6%) Standard surgical skin preparation wound throughout
2
Obesity: (BMI>30kg/m ) including a skin prep of 10% surgery regardless of
Intervention: 27 povidone-iodine on the operative resultant SSI or not.
(30.7%) field which was allowed to dry. One surgeon reported
Control: 18 (20.2%) Standard preventive measures: visible flaking of the
Comorbidities Instruction: all principal microbial sealant film
Diabetes Mellitus investigators were given hands- during the procedure.
Intervention: 2 (2.3%) on instruction in how to use the One patient in the
Control: 4 (4.5%) applicator prior to enrollment of microbial sealant
7 patients had comorbid subjects. group had skin
clinical characteristics Non-standard preventive irritation (resolved on
that have been measures: its own)
reported to be Surgeons were allowed to perform Surgeons reported 4
associated with the open inguinal hernia repair incidents of difficulty
2017 American Medical Association. All rights reserved. 421
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
wound complications based on their personal incising through the
such as preference with respect to hair clear film.
hyperhidrosis, clipping, perioperative Reoperations:
eczema, psoriasis, or antimicrobials, surgical The deep MRSA
an autoimmune techniques and use of mesh infection from the
disease. One patient Preoperative data: control group required
had a previous history Based on Total population N=176 readmission,
of SSI. because data missing from 1 debridement, mesh
Procedure duration: intervention removal and
(min) Antimicrobial shower: intravenous
Mean (SD) Intervention: 23/87 (26.4%) antimicrobials.
Intervention: 73.7 (28.4) Control: 24/89 (27.0%) Length of stay: NR
Control: 75.6 (31.5) Hair removal: 173/176 (98.3%) Mortality: NR
Procedures: Open Clipping/shaving Adverse events:
inguinal hernia repair. Intervention: 45/35 Serious adverse events
Indications: NR Control:47/36 All serious adverse
Setting: 6 Teaching AMP: administered to 131/176 events occurred in
hospitals (74%) the control group and
Location: USA Intervention: 61/87 (70.1%) resolved at final
Dates: July 2005 - Control: 70 (78.7%) follow up
September 2006 Mesh implanted Admission for SSI due to
(Clinical trial Intervention: 71/88 (81.6%) MRSA:1
discontinued in Control: 72/89 (80.9%) Groin hematoma: 1
September of 2006 Closure using sutures Chest pain: 1
when FDA granted Intervention: 87/88 (98.9%) Dyspnea: 1
regulatory approval Control: 88/89 (98.9%) Scrotal edema: 1
for this product as a Wound covered with a dressing Knee pain: 1
class II medical Intervention 77 (87.5%) Non-serious adverse
device. Control: 80 (89.9%) events
Inclusion Criteria: P=0.62 Scrotal edema,
Scheduled for open, hematoma
class 1 clean inguinal Intervention: 3
hernia repair; aged 18 Control: 2
or older; able to Wound dehiscence
complete mean (SD) Intervention: 1
30 (5) day follow-up.; Control: 0
and able and willing to Incisional pain/ swelling
provide informed Intervention: 1
consent Control: 1
2017 American Medical Association. All rights reserved. 422
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Exclusion Criteria: Skin irritation
Known sensitivity to Intervention: 1
cyanoacrylate Control: 0
formaldehyde or Possibly attributable to
acetone products or investigational device
iodine or iodine Constipation
containing products; Intervention: 1
surgical procedures Control: 0
involving mucous Incisional bleeding
membranes or eyes; Intervention: 1
laparoscopic surgical Control: 0
procedures; evidence Urinary frequency
of coexistent infection Intervention: 0
at a remote body site; Control: 1
skin rashes or Urinary retention
exfoliative condition Intervention: 1
the day of surgery; Control: 1
history of keloid Epigastric hernia
formation; currently drainage
receiving high-dose Intervention: 1
steroid or Control: 0
immunosuppressive Decreased limb
therapy; sensation
chemotherapy Intervention: 0
treatment within 30 Control: 1
days of current
surgery; diagnoses of
diabetes HbA>7.0%
obtained within 90
days; use of oral, IV
or topical (in expected
area of incision)
antimicrobials within
20 days prior to the
day of surgery;
pregnant or nursing;
or participation in any
other study of an
investigational drug or
2017 American Medical Association. All rights reserved. 423
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
device within 2 week
prior to the current
procedure.
eTABLE 49. Evidence Table for Q8D. How safe and effective are plastic adhesive drapes?
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Segal RCT To No. Patients: N=209 Intervention1: n=52 Sternal wound Definitions
114
2002 1, 2, 5, evaluate Patient characteristics: Povidone-iodine five-minute scrub Infections: 6 weeks Obesity: BMI>120% of ideal
(ES) 9 the effect Patient demographics with paint Intervention1: 7/52 weight.
of four were compared. Intervention2: n=50 (13.5%) SSI: Clinical exam for signs of
different The following One-step iodophor/alcohol water Intervention2: 1/50 drainage, redness,
skin characteristics given insoluble film (2.0%) tenderness, or sternal
preparation represent the whole Intervention3: n=51 Intervention 3: 3/51 instability. Sternal surgical
s on the study. one-step iodophor/alcohol water (5.9%) site exhibiting any of these
incidence All patients had at least insoluble film with iodine Intervention 4: 7/56 signs was cultured. Positive
of sternal one high-risk factor (the impregnated surgical adhesive (12.5%) cultures were correlated with
SSIs in basis of the study). drape P=0.117 clinical evidence according
patients 39% had 2 risk factors Intervention 4: n=56 Infections per to the CDC guideline to
undergoing 4% had 3 risk factors Povidone-iodine paint treatment indicate a sternal SSI
coronary (Percentage numbers Timing of Intervention: Aqueous Iodine (
artery appear larger in bar Preoperative Intervention 1+4) Perioperative care
bypass graph within paper my Duration of intervention: 14/108 (13.0%) NR
graft copy is difficult to read) Intraoperative Insoluble Iodine Other notes
surgery Age (y): Mean Agents: Solutions, insoluble film & (Interventions 2 and 3) Impregnated drapes in
(CABG) 60.9 years (no SD given) incise drapes not specified 4/101 (4.0%) Intervention 3 were shown to
who were Gender: Over 75% male Monitoring intervention: P=0.02 be ineffective as an
=5.3
2
identified Obesity: NR Observation by nurses intervention.
as high risk Redo sternotomies: 11.5% Control: Other infections: NR Study deemed underpowered
of Procedures performed Topic-specific Follow up: 6 weeks
developing using the IMA: 88.5 Standard Preventive Measures outcomes: NR postoperatively through
sternal SSI Shower Reoperation: NR regularly scheduled clinic
MeanSD The nurse instructed patients to Length of Stay: visits
Total OR time: 248 min take an antimicrobial shower the Uninfected patients Funding Source Conflicts:
29 evening before and the morning had a 5-6 day shorter Authors: NR
2017 American Medical Association. All rights reserved. 424
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Cross clamp time: 42 of surgery, or if they were length of hospital stay Institution: NR
min20 inpatients, they were given a than infected patients. Study: NR
Last OR Glucose: preoperative antimicrobial Mortality: NR Supplies: NR
434210 shower in the hospital. Adverse events: NR
Procedures: elective Hair removal
CABG Surgery If necessary, a qualified patient
Indications: NR care assistant clipped patients
Setting: 1 tertiary/ hair the morning of surgery in
teaching hospital patients rooms.
Location: USA AMP: All patients received a
Dates: Oct 1, 1994 April prophylactic antimicrobial (i.e.,
30-1997 cefuroxime) or if they had a
Inclusion Criteria: documented allergy to penicillin,
Patients undergoing they received vancomycin in
elective CABG with one appropriate dosing window to
or more of the following provide adequate coverage at
conditions: the time of incision.
Diabetes
Obesity
Chronic Obstructive
Pulmonary Disease
(COPD)
Exclusion Criteria:
Patients with an allergy
to topical iodine or with a
preexisting infection
indicated by a white
blood cell count higher
than 10,000 or by a
temperature higher than
o o
100.5 F (38.06 C)
because their
procedures were
performed emergently.
2017 American Medical Association. All rights reserved. 425
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Ward RCT To Number of patients: Intervention group: n=305 SSI: Definitions:
132
2001 1, 2, 3, evaluate N=605 After drying the cleansed area, a Infection: if two of the 3
(ES) 4, 5, 6, the ability Patient Characteristics: plastic adhesive drape was Drape: 34/305 (11.1%) following features were
7, 8, 9 of the new Characteristics were carefully applied to the skin and No Drape: 30/298 present:
generation similar between groups. toweling and this remained in (10.1%) 1) Erythematous cellulitis
of adhesive situ until the last skin suture or (erythematous induration
surgical Procedures: Caesarean staple had been inserted. The P=0.6933 either side of the incision
drapes to Section drape was then removed and a line
prevent Setting: 1 Regional dressing applied. 2) Seropurulent discharge
Post referral hospital Timing of intervention: from the wound.
Cesarean Location: South Africa Intraoperatively 3) Positive swab culture
Wound Dates: Aug 18, 1992 Duration of intervention: (organisms and
Infection. January 29, 1993 Intraoperatively leucocytes).
Inclusion Criteria: Device/agent: plastic adhesive Perioperative care: NR
Consecutive patients drape Other notes: None
undergoing Caesarean Control group: n=298 Follow-up: 5 days.
Section Same standard preventive Funding Source Conflicts:
Exclusion Criteria: measures but no drape was Authors: NR
Women having applied. Institution: NR
coincidental appendix Standard preventive measures: Study: NR
ruptured or requesting Skin Prep: preoperatively, Supplies: NR
early discharge. abdomen and perineum were
washed with 4% chlorhexidine
soap. On the Operating table,
the abdomen was liberally
swabbed with a solution of 0.5%
chlorhexidine in 80% alcohol for
at least 30s over an area
extending from the
xiphosternum to the flanks,
down as far as the mid-thigh
and across to the perineum in
the midline. The surgeon then
scalpel shaved an area 2cm
either side of the proposed
incision site. Standard sterile
double towel draping followed.
The site was padded dry with a
sterile swab
2017 American Medical Association. All rights reserved. 426
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
AMP: At clamping of umbilical
cord, patient received 1g of
cephazolin intravenously unless
antimicrobials were already
being administered as therapy
or prophylaxis. A 1g
metronidazole suppository was
inserted preoperatively and
repeated after 12h.
Chiu RCT To Number of patients: N= Intervention group: n= 65 SSI: Definitions: NR
133
1993 1 investigate 120 Operation site was covered with a Total: 11/120 (9.2%) Perioperative care: NR
(ES) the Patient Characteristics: plastic adhesive drape. Drape: 6/65 (9.2%) Other notes: None
effectivene The two groups were Timing of intervention: Superficial: 5/65 Follow-up: NR
ss of matched for patient Intraoperatively+ (7.7%) Funding Source Conflicts:
plastic characteristics. Duration of intervention: Deep: 1/65 (1.5%) Authors: NR
adhesive Age: NR Intraoperatively No Drape: 5/55 (9.1%) Institution: NR
skin drapes Gender: NR Device/agent: plastic adhesive Superficial: 4/55 Study: NR
in the Obesity: NR drape (7.3%) Supplies: NR
prevention Comorbidities: NR Control group: n= 55 Deep: 1/55 (1.8%)
of wound Procedures: Acute Hip Operation site was left uncovered.
infection Fracture including Same standard preventive
after acute Internal fixation with measures but no drape was
hip fracture sliding hip-screw done applied.
operations. for trochanteric Standard preventive measures:
fractures; Austin-Moore Ultraclean air: there was no
femoral head laminar flow, ultraclean air, or
replacement inserted exhaust suits in the operating
for displaced subcapital room.
fracture in older AMP: cephalosporin antibiotic was
patients; and for given at induction of anesthesia.
undisplaced fractures or Skin prep: Operation site was
for displaced fractures prepared with povidone solution
in young patients, the then wiped, dried and draped
fracture was fixed with with sterile towels.
three cancellous lag
screws.
Setting: 1 University
Hospital
Location: China
2017 American Medical Association. All rights reserved. 427
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Dates: January
December 1991
Inclusion Criteria:
patients with hip
fracture operations
done by one of two
surgeons done in the
same operating theater.
Exclusion Criteria: NR
Dewan RCT To Number of patients: Intervention group: n=529 SSI: Definitions:
136
1987 1, 2, 4 determine N=1016 Patients with iodophor- Wound infection Infection: present if wound
(ES) 7, 8 if skin Patient Characteristics: impregnated drape applied Intervention: 36/529 discharged pus or if the
organism satisfactory Timing of intervention: (6.8%) discharge of fluid from the
contaminati randomization for the perioperatively. Control: 34/487 (7.0%) wound was as associated
on of the non-parametrically Duration of intervention: surgery Not significantly with appositive bacterial
wound distributed groups was Device/agent: Iodophor- different culture. Infection was also
made confirmed for each of the impregnated drape Other infections: NR diagnosed if the wound
through major wound infection Monitoring intervention: NA Topic-specific showed erythema more than
iodophor risk factors and excluded Control group: n=487 outcomes: NR 1cm lateral to the wound
impregnate a bias from these. Patients where no iodophor- Reoperations: NR margin, and for either one
d incise Age: NR impregnated drape was used. Length of stay: NR third of the length of the
drapes Gender: NR Standard preventive measures: Mortality: NR wound or an 8cm length of it.
should be Obesity: NR Routine skin prep of an iodophor Adverse events: NR Perioperative care: NR
reduced Comorbidities: NR antiseptic followed by alcohol. Other notes: None
and less Procedures: general The operative field was dried Follow-up: 3weeks follow up
than when abdominal operations with a sterile swab. Funding Source Conflicts:
a standard including inguinal hernia Authors: NR
skin repair Institution: NR
preparation Indications: NR Study: NR
is used. Setting: One university Supplies: NR
Thus if hospital
contaminati Location: New Zealand
on is Dates: August 1983 May
significantly 1985
linked to Inclusion Criteria:
infection, a Patients undergoing
reduction in abdominal operation,
the wound including inguinal hernia
infection Exclusion Criteria:
2017 American Medical Association. All rights reserved. 428
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
rate from patients under 10 years
skin of age and patients of
organisms one surgeon when he
should felt the color of the drape
follow. precluded optimal
incision placement. Also,
patients requiring
abdominoplasty and two
patients with a strong
history of previous iodine
allergy.
Psaila RCT To assess Number of patients: Intervention group: N=51 SSI Definitions:
135
1977 1, 8, 9 the role of N=144 (n=98 utilized An adhesive plastic drape was Wound infection: Presence of infection:
(ES) adhesive here) applied over cloth towels at the All: 26/144 (18.0%) 1) Erythema around the
plastic skin Patient Characteristics: abdominal surgery site. Drape: 8/51 (16%) sutures or along the
drapes and Age: NR Timing of intervention No Drape: 10/47 (21%) wound edge with an
plastic ring Gender: NR Duration of intervention Other infections: NR accompanying pyrexia
wound Obesity: NR Device/agent Topic-specific 2) Discharge of exudate
protectors Comorbidities: NR Monitoring intervention outcomes: NR or pus from the wound
in the Procedures: abdominal Control group: n=47 Reoperations: NR 3) Wound breakdown.
prevention surgery. Cloth towels were applied to the Length of stay: NR 4) If infection was
of wound Indications: NR abdominal wound Mortality: NR considered to be
infection Setting: One University Standard preventive measures: Adverse events: NR present, a swab was
following hospital Skin prep: 1 in 30, 0.05% taken and sent.
abdominal Location: United Kingdom chlorhexidine and cetrimide 0.5% Perioperative care: NR
surgery Dates: NR and Chlorhexidine gluconate Other notes: None
rd
Inclusion Criteria: 0.5% in alcohol. Follow-up: daily after the 3
Patients undergoing postoperative day.
abdominal surgery Funding Source Conflicts:
Exclusion Criteria: Authors: NR
Patients receiving Institution: NR
preoperative Study: NR
antimicrobials (with Supplies: NR
exception of non-
absorbable
sulphonamides used for
bowel prep)
2017 American Medical Association. All rights reserved. 429
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author Design
Study
Year Risk of Population and Setting Intervention Results Comments
Objective
(Extractor) Bias
Score
Jackson RCT To conduct Number of patients; Intervention group: n=473 SSI: Definitions :
134
1971 1, 2 a study to n=921 Patients who had a plastic Wound infection Wound infection: defined in
(ES) determine Patient Characteristics: adhesive drape utilized at the Drape: 67/473 (14.2%) terms of the discharge of
the Recorded, not reported site of surgery No Drape: 52/448 pus from the wound.
effectivene by study group. Timing of intervention: (11.6%) Usually a small amount
ss of Age: NR Intraoperative P>0.20 (e.g., the so-called stitch
plastic Gender: NR Duration of intervention: until Other infections: NR abscess), but sometimes a
adhesive Obesity: NR just after incision. Topic-specific wound abscess developed
drapes in Comorbidities: NR Device/agent: Plastic adhesive outcomes: NR which required evacuation
preventing Procedures: NR drape. Reoperations: NR by removal of a suture and
wound Indications: NR Monitoring intervention: NA Length of stay: NR spreading of the wound
infection. Setting: 1 hospital Control group: n=448 Mortality: NR edges. Wherever possible,
Location: England Patients who had no adhesive Adverse events: NR the infecting organism was
Dates: Started December drape utilized. isolated and the cause was
1967 two years later. Standard preventive measures: assessed. If a swab grew a
Inclusion Criteria: All Skin prep: swab soaked in 2.5% microorganism, but no pus
suitable cases operated alcoholic solution of iodine BP was produced, the wound
on by one of the 3 was used to paint the operation was not regarded as
authors or 2 other area. This was wiped dry and infected. The slight
surgeons. ether was painted around the moistness at the site of a
Exclusion Criteria: area of the incision. drainage tube was not
Operations where accepted by itself as an
drapes could not be indication of infection.
used satisfactorily Perioperative care: NR
(mastectomy, perineal Other notes: None
operations, amputation, Follow-up: at least 4 weeks.
limb arterial surgery, Funding Source Conflicts:
etc.); known iodine Authors: NR
sensitivity, cases where Institution: NR
difficulties with Study: NR
adhesiveness of drapes Supplies: NR
were present or where
drapes were
unsatisfactory.
eTABLE 50. Evidence Table for Q9. How safe and effective is antiseptic irrigation prior to closing the surgical incision?
2017 American Medical Association. All rights reserved. 430
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Chang RCT To evaluate Number of patients: Intervention group: n=120 SSI: Definitions:
140
2006 1, 2, 4, the effect of n=244 Wounds were irrigated with Superficial: no infections Superficial infection: above
(ES) 6, 7, 8, wound Patient 0.35%povidone-iodine solution in either group lumbosacral fascia
9, 10 irrigation Characteristics: to soak for 3min, followed by Deep: Deep infections: below
with patient characteristics irrigation with 2000cc of normal Intervention: 0/120 lumbosacral fascia & all
povidone- were not statistically saline to remove povidone- Control: 6/124 (4.8%) deep infections were
iodine on significantly different iodine solution. P=0.29 confirmed by lab
wound between groups Timing of intervention: parameters including the
healing, Age, y: NR intraoperative Other infections: NR erythrocyte sedimentation
infection Gender: NR Duration of intervention: 3min Topic-specific rate (ESR) and level of C-
rate, fusion Obesity: NR Device/agent: 0.53% povidone- outcomes: NR reactive protein (CRP) and
status and Comorbidities: NR iodine solution Reoperations: NR a positive culture of biopsy.
clinical Procedures: primary Monitoring intervention: NA Length of stay: NR Perioperative care: NA
outcome of instrumented Control group: n=124 Mortality: NR Other notes: none
spinal lumbosacral Wound was only irrigated with Adverse events: one Follow-up: every three
surgeries posterolateral fusion 2000cc normal saline incidence of wound months until the end of the
levels for Standard preventive measures: dehiscence event study. Duration was approx.
degenerative spinal Pain control 3 days postop. with 0.35% povidone 19months.
disorder. AMP: preop IV bolus injections of iodine followed by Funding Source Conflicts:
Indications: lumbar or cefazolin and gentamicin, normal saline Authors: None
lumbosacral additional postop cefazolin and irrigation. Institution: None
segmental instability gentamicin injections were Study: None
defined by chronic given for 48h postop followed Supplies: None
back, buttock and/or by oral cefazolin for 3 days
leg pain and postop.
degenerative Custom made orthosis immobilized
spondylolisthesis, patient whenever out of bed for
degenerative 3 months postop.
scoliosis, or isthmic
spondylolisthesis.
Setting: 1 university
hospital
Location: Taiwan
Dates: Jan 2002 Aug
2003
Inclusion Criteria:
patients undergoing
primary instrumented
lumbosacral
2017 American Medical Association. All rights reserved. 431
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
posterolateral fusion
levels for
degenerative spinal
disorder.
Exclusion Criteria:
prior spinal surgery,
spinal trauma,
malignancy
Cheng RCT To evaluate Number of patients: Intervention group: n=208 SSI: Definitions:
141
2005 1, 2, 5, the efficacy N=417 Wound was soaked with povidone Overall Infection: suspected when
(ES) 7, 8, 9 of dilute Patient iodine solution for 3min (5mL of Intervention: 0/208 unusual pain, tenderness,
10 betadine Characteristics: povidone-iodine diluted with Control: 7/206 (3.4%) erythema, induration, fever,
solution in there were no normal saline to achieve 0.35% P=0.0072 or wound drainage was
the statistically significant povidone iodine solution.) The noted. Findings were
prevention of differences between wound was then irrigated with Superficial: investigated with
infection, groups except with copious amounts of normal Intervention: 0/208 measurement of ESR, CRP,
particularly age: saline (2000ml) Control: 1/206 (0.5%) and bacteriological cultures
deep Age (mean) y Timing of intervention: P=0.4976 from the operative site or
infection Intervention: 64 intraoperative Deep: blood. All patients with
following Control: 61 Duration of intervention: 3min Intervention: 0/208 highly suspected wound
spinal P=0.0682 soak Control: 6/206 (2.9%) infection underwent surgical
surgery Gender: NR Device/agent: -.35% povidone- P=0.0146 debridement.
Obesity: NR iodine solution Perioperative care: NR
Comorbidities: NR Monitoring intervention Other infections: NR Other Notes: none
Procedures: spinal Control group: n=206 Topic-specific Follow-up: at 3 month
surgery Patients outcomes: NR intervals until study was
(decompression, Standard preventive measures: Adverse events: no over. (mean length 15.5
pedicle screw fixation, Basic aseptic technique was product-related months)
discectomy, tumor followed. adverse event with Funding Source Conflicts:
excision) Skin prep: with povidone iodine. 0.35% povidone Authors: None
Setting: 1 university AMP: 1 does parenteral cefazolin iodine followed by Institution: None
hospital and gentamicin 1h preop then normal saline Study: None
Location: Taiwan Cefazolin every 6h & irrigation Supplies: None
Dates: January 2002 gentamicin every 12 hours for
May 2003 48h postop. Oral antimicrobial
Inclusion Criteria: doses (cefazolin) were
patients undergoing continued for 3 days.
spinal surgery.
Exclusion Criteria:
2017 American Medical Association. All rights reserved. 432
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Mortality in follow-up
period, also, patients
with overt or
suspected pyogenic
vertebral
osteomyelitis, discitis,
or any form of
preoperative spinal
infection; and patients
with fever or other
suspected sources of
infection.
Sindelar RCT To evaluate Number of patients: Intervention group: n=37 SSI: Definitions: NR
139
1985 1, 2, 7, the efficacy N=75 Irrigation of the intraperitoneal area Total Infections Perioperative care: NR
(ES) 8, 9 and toxicity Patient was performed 3 times during PVP-I LMW: 2/37 (5.4%) Other notes: None
of Characteristics: the operation with 1000ml of a [dirty] Follow-up: 7days
intraperitone The experimental and 10% solution of PVP-I LMW. Saline: 9/38 (26.7%) [7/9 Funding Source Conflicts:
al irrigation control groups did not The Solution was suctioned contaminated; 2/9 Authors: NR
with Low statistically differ with from the peritoneal cavity 30- dirty] Institution: NR
Molecular respect to patient 60s after installation. In patients Study: NR
Weight characteristics. undergoing primary wound Organ/Space Infection Supplies: NR
Povidone Age, y: NR closure, irrigation of the PVP-I LMW: 1/37 (2.7%)
Iodine Gender: NR subcutaneous tissue was [dirty]
Solution Obesity: NR performed prior to skin closure Saline: 6/38 (15.8%) [4/6
(PVP-I Comorbidities: NR with 1000ml of PVP-I LMW contaminated; 2/6
LMW) in Procedures: 10%. dirty
surgical Contaminated or dirty Timing of intervention:
procedures Intra-abdominal intraoperative Deep wound infection
performed in surgical procedures Duration of intervention: duration PVP-I LMW: 0/37
the face of Setting: National of lavage. Saline: 1/38 (2.6%)
bacterial Institute of Health Device/agent: low molecular [Dirty]
contaminatio Location: USA weight povidone iodine solution
n (i.e. intra- Dates: NR (10%) Superficial wound
abdominal Inclusion Criteria: Control group: n=38 infection:
surgical Patients 18yo or Irrigation of the intraperitoneal area PVP-I LMW: 1/37 (2.7%)
procedures older, scheduled for was performed 3 times during [dirty]
where there elective or emergency the operation with 1000ml of Saline: 2/38 (5.3%) [both
was likely to intra-abdominal saline. The Solution was contaminated]
be bacterial surgery involving suctioned from the peritoneal
2017 American Medical Association. All rights reserved. 433
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
contaminatio entry into the cavity 30-60s after installation. CLEAN (No AMP)
n of the peritoneal cavity In patients undergoing primary 0/113 vs.7/121 (6%);
peritoneal where the surgery wound closure, irrigation of the p<0.01
cavity) was classified as subcutaneous tissue was
contaminated or dirty performed prior to skin closure Potentially
(esophageal, gastric, with 1000ml of saline. Contaminated (AMP)
small intestinal, Standard preventive measures: 1/49 vs. 7/49; p<0.05
colonic, hepatic, AMP: patients received peri-
pancreatico-biliary. operative antimicrobials in Contaminated (AMP)
Exclusion Criteria: accordance to the practice of 3/44 vs. 12 /46; p<0.05
Patients undergoing the surgeon responsible.
clean operative Dirty (AMP)
procedures. If there 3/36 vs. 13/42; p<0.001
was a history of
iodine sensitivity, Adverse events:
thyroid disease, renal Significant increase in
insufficiency or postop serum Iodine
surgery involving levels at 24h resolved
ischemic or necrotic by 72h. No clinical
tissues which might signs of iodine toxicity
interfere with wound
healing either in the
presence or absence
of infectious
complications.
Vallance RCT To compare Number of patients: Intervention group: SSI: Definitions: NR
138
1985 1, 7, 8, a Povidone- N=29 PVP-I: n=13 PI: 4/13 (31%) Perioperative care: NR
(ES) 9 Iodine Patient Patients who received a saline Saline: 5/16(31%) Other notes: None
solution Characteristics: lavage until solutions returned p=NS Follow-up: 30 days
against Patient characteristics clear with 100ml PVP-I solution Funding Source Conflicts:
saline alone were not statistically inserted before wound closure Authors: None
for different between the Timing of intervention: Institution: None
peritoneal groups. intraoperatively Study: None
lavage in Age, y: NR Duration of intervention: NR Supplies: None
patients Gender: NR Device/agent: PVP-I or saline
undergoing Obesity: NR Control group:
operations Comorbidities: NR Saline: n=16
for Procedures: dirty Patients who received a saline
generalized laparotomy lavage until solutions returned
2017 American Medical Association. All rights reserved. 434
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
purulent or procedures clear with inserted before
fecal Setting: 1 hospital wound closure
peritonitis Location: UK Standard preventive measures
Dates: NR Fluid maintenance: all patients
Inclusion Criteria: were resuscitated with iv fluids
Patients who were before surgery
confirmed at AMP: all patients were begun on
laparotomy to have broad spectrum antimicrobial
generalized purulent postop prophylaxis which were
or fecal peritonitis. continued for at least 5 days
Exclusion Criteria: postop.
Patients dying within
4 days of the
operation.
Rogers RCT To elucidate Number of patients: Intervention group: n=86 SSI: Definitions:
143
1983 1, 2, 7, further the N=187 After fascial closure, patients Clean (No AMP) Wound infection: any wound in
(ES) 8, 9 potential Patient underwent an approximate one P-I: 2/56 (3.6%) which a purulent discharge
value of Characteristics: minute irrigation of the Saline: 6/68 (8.8%) occurred during a month of
Povidone Age, y: NR subcutaneous tissue with p=?? observation after the
Iodine Gender: NR approximately 60ml of 10% operation.
wound Obesity: NR Povidone Iodine (1% available Clean-contaminated Perioperative care: NR
irrigation as Comorbidities: NR iodine) solution. (AMP) Other notes: None
an adjunct in Procedures: Clean Timing of intervention: P-I: 1/24 (4.2%) Follow-up: 1 month
the (Inguinal hernia intraoperative Saline: 5/27 (18.5%) Funding Source Conflicts:
prevention repair, Duration of intervention: approx. p=? Authors: NR
postoperativ cholecystectomy, 1 minute Institution: NR
ely of wound laparotomy, hiatal Device/agent: PVP-I or saline Dirty (AMP) Study: NR
infections. hernia repair, Control group: n=101 P-I: 1/6 (16.6%) Supplies: NR
proximal gastric After fascial closure, patients Saline: 1/6 (16.6%)
vagotomy, ventral underwent an approximate one p=NS
hernia, and other), minute irrigation of the
clean contaminated subcutaneous tissue with saline
(upper solution.
gastrointestinal,
colorectal, biliary Standard preventive measure:
tract, appendectomy AMP: administered to all patients
and other clean perioperatively in both the
contaminated clean-contaminated and dirty
surgeries), and Dirty categories.
2017 American Medical Association. All rights reserved. 435
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
(perforated viscus, Bowel Prep: mechanical (cleansing
traumatic perforation enema, cathartics & low residue
procedures) liquids) and antimicrobial bowel
procedures. prep (orally administered
Setting: 1 veterans neomycin and erythromycin
hospital base) were used for elective
Location: USA colorectal surgeries.
Dates: July 1, -
December 31, 1979
Inclusion Criteria: All
patients undergoing
operative procedures
Exclusion Criteria:
operations on the
anorectal area; also
patients who died or
who required
reoperation within
three weeks of
primary operation
unless the wounds
were obviously
infected. Vascular
procedures and
operations on the
head and neck
Sindelar RCT To evaluate Number of patients: Intervention group: n=129 SSI: Definitions:
142
1979 1, 7, 8, the efficacy N=266 Patients had subcutaneous tissues Superficial SSI: Infection: if any amount of pus
(ES) 9 of povidone- Patient irrigated for 60 seconds with PI: 7/129 was discharged within 12
iodine Characteristics: 10% povidone-iodine solution Saline: 32/137 weeks of operation. Serous
irrigations of patient groups were Timing of intervention: drainage from questionable
subcutaneou similar in age, sex intraoperative Potentially wounds was cultured and
s tissue distribution and types Duration of intervention: 60 Contaminated was considered infected if
during of surgery. seconds PI: 1/49 any bacterial growth was
wound Age, y: NR Device/agent: 1% available Saline: 7/49 recovered.
closure in Gender: NR iodine, povidone-iodine solution p<0.05 Perioperative care: NR
reducing the Obesity: NR Control group: n=137 Other Notes: None
incidence of Comorbidities: NR Patients had subcutaneous tissues Contaminated Follow-up: up to 12 weeks
superficial Procedures: both irrigated for 60 seconds with PI: 3/44 postop.
2017 American Medical Association. All rights reserved. 436
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
wound elective and saline solution Saline: 12 /46 Funding Source Conflicts:
infections for emergency surgical Standard preventive measures p<0.05 Authors: NR
a variety of procedures including AMP: Parenteral AMP preop and Institution: NR
surgical abdominal & for 48h postop Dirty Study: NR
incisions. gastrointestinal PI: 3/36 Supplies: NR
procedures, oncologic Saline: 13/42
procedures, vascular p<0.001
reconstructions, head
and neck operations, Adverse events: no
thoracic and significant change in
genitourinary free iodine serum
procedures and levels
trauma operations.
Setting: 1 university
hospital
Location: USA
Dates: NR
Inclusion Criteria:
patients undergoing
operative procedures.
Exclusion Criteria:
Amputations for
ischemic disease,
drainage of
subcutaneous
abscesses, skin
grafting and anorectal
procedures. Also,
patients with a history
of iodine sensitivity,
thyroid diseases and
significant renal
impairment
2017 American Medical Association. All rights reserved. 437
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Sindelar RCT To study Number of patients: Intervention group: n=80 SSI: Definitions:
137
1979 1, 5, 7, both the N=168 Prior to closure, the peritoneal Intraabdominal Abscess Intraabdominal abscess: fever,
(ES) 8, 9 possible Patient cavity was irrigated for 60 Overall: 10/168 (5.95%) persistent pain, palpable
toxicity and Characteristics: seconds with 1L of 1% Intervention: 1/80 mass, abnormal
the possible patient groups were povidone-iodine solution, giving (1.3%) roentgenograms, or positive
benefit of similar in age, sex 0.1% available iodine in diluted Control: 9/88 (10.2%) ultrasonographic findings.
povidone- distribution and types form. Following irrigation, the P<0.05 Patients with suspected
iodine of surgery. peritoneum was suctioned and Dirty Procedures: abscesses underwent
peritoneal Age, y: NR the majority (estimated>90%) of Intervention: 0/36 surgical exploration.
irrigations in Gender: NR the irrigant was removed. Control: 6/42 (14.3%) Adverse event: iodine toxicity
reducing the Obesity: NR Timing of intervention: P<0.05 Perioperative care: NR
incidence of Comorbidities: NR intraoperative Contaminated Other notes: None
intra- Procedures: Duration of intervention: 60 Procedures: Follow-up: 3 months or until
abdominal Laparotomy: surgical seconds Intervention: 1/44 death.
abscess explorations in the Device/agent: 1% povidone-iodine (2.3%) Funding Source Conflicts:
formation in presence of solution Control: 3/46 (6.5%) Authors: NR
patients with bacterially Monitoring intervention: NA P=NS Institution: NR
contaminate contaminated Control group: n=88 Other infections: NR Study: NR
d abdomens. peritoneal cavities. Peritoneal cavity was irrigated for Topic-specific Supplies: NR
Indications: 60 seconds with 1L of normal outcomes: NR
contaminated saline solution followed by Reoperations: NR
abdomen suctioning. Length of stay: NR
Setting: 1 university Standard preventive measures Mortality: NR
hospital Amp: all patients received
Location: USA preoperative systemic Adverse events:
Dates: NR antimicrobial prophylaxis which Iodine toxicity:
Inclusion Criteria: were continued for 48h postop Intervention: 5/80
patients undergoing or longer if clinically indicated (6.25%)
laparotomy. by manifestations of sepsis. Control: 0/88
Exclusion Criteria: (Typically clindamycin and
patients with a history gentamicin except in allergy or Serum iodine levels
of iodine sensitivity, possible renal impairment for were elevated 24
thyroid disease, or which doxycycline was hours after
significant renal substituted). intraperitoneal
disease. irrigation with PI
solution and returned
to near normal by 73h
postop and no
complications from
2017 American Medical Association. All rights reserved. 438
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
the use of PI
eTABLE 51. Evidence Table for Q10. How safe and effective is repeat application of an antiseptic skin preparation agent to the
surgical site immediately prior to closing the surgical incision?
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Harihara RCT To investigate Number of patients: Intervention group: n=54 (23 SSI: (Follow up NR) Definitions:
144
2006 1 whether N=107 gastric and 31 colorectal) Gastric Surgery SSI: JNIS system which is a
(ES) incisional (47 Gastric & 60 Before skin closure, skin was Wound Infection: Japanese modification of
topical colorectal) irrigated with 500ml saline Intervention: 1/23 the CDC NNIS System.
application of Patient solution. Povidone-Iodine was (4.3%) Wound infection: infection
Povidone- Characteristics: No applied to the skin around the Control: 0/24 excluding organ/space
iodine (PVP-I) significant difference incision twice using swabs in P=0.4894 infection from SSI.
just before was observed the same manner as the SSI Perioperative care: NR
skin closure between groups. preoperative skin preparation Intervention: 3/23 Other notes: NR
can prevent Age: after irrigation and just before (13.0%) Follow-up: NR
wound Gastric skin closure. Control: 3/24 (12.5%) Funding Source Conflicts:
infection or Intervention: Timing of intervention: P=0.6460 Authors: NR
SSI. 62.111.9y Intraoperatively Colorectal Surgery Institution: NR
Control: 65.011.9 Duration of intervention: Wound Infection: Study: NR
Colorectal Intraoperatively Intervention: 4/31 Supplies: NR
Intervention: Device/agent: Povidone-iodine (12.9%)
62.812.3 (PVP-I) Control: 4/29 (13.7%)
Control: 66.311.5 Monitoring intervention: NR P=0.4894
Gender: m:f Control group: n= 52 (23 gastric SSI
Gastric and 29 colorectal) Intervention: 5/31
2017 American Medical Association. All rights reserved. 439
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Intervention: 18:5 Povidone-Iodine was not applied to (16.1%)
Control: 20:4 the skin around the incision just Control: 5/29 (17.2%)
Colorectal before skin closure. P=0.6460
Intervention: 18:13
Control: 15:14 Standard preventive measures: RISK FACTORS FOR
ASA Physical Status NR INFECTION
(1:2:3:4:5) Gastric Surgery
Gastric No significant risk
Intervention: factors were identified
13:10:0:0:0 affecting either wound
Control: 12:12:0:0:0 infection or SSI rates
Colorectal in the univariate
Intervention: analysis using the
19:10:2:0:0 logistic regression
Control: 10:17:2:0:0 model in gastric
surgery.
Obesity: BMI (only for
colorectal) Colorectal Surgery
Colorectal Univariate Analysis of
Intervention: 23.13.4 Risk Factors
Control: 21.83.2 Wound Infection
Comorbidities: (only for ASA: OR = 3.4232;
colorectal) P=0.0436
Colorectal DM: OR = 5.6400;
Diabetes mellitus (DM) P=0.0573
Intervention: 3/31
(9.7%) SSI
Control: 5/29 (17.2%) ASA: OR = 3.7093;
Smoking >30 years P=0.0206
Intervention: 7/31 DM: OR = 7.6667;
(22.6%) P=0.0162
Control: 9/29 (31.0%) Multivariate Analysis of
Procedures: Gastric Risk Factors
and colorectal Wound Infection: OR
surgery. (95% CI)
Indications: : NR ASA: 2.9039 (0.752-
Setting: 1 medical 11.211)
center DM: 3.8966 (0.637-
Location: Japan 23.834)
2017 American Medical Association. All rights reserved. 440
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Dates: July 2004 P = 0.0452
December 2004.
Inclusion Criteria: SSI: OR (95% CI)
Patients undergoing ASA: 2.6602 (0.6660-
gastric or colorectal 10.725)
surgery between DM: 3.8336 (0.574-
July 2004 and 25.617)
December 2004 Smoking: 2.1090
Exclusion Criteria: NR (0.382-11.644)
Wound Class: 1.7113
(0.153-19.185)
P = 0.0452
Other infections: NR
Topic-specific
outcomes:
Gastric surgery:
No relation was
identified between
wound infection or
SSI rates and skin or
subcutaneous tissue
positive cultures in
gastric surgery.
Colorectal surgery:
Wound infection and
SSI occurred in 2 of 5
skin culture positive
cases.
Wound infection and SSI
occurred in 4 of 7
subcutaneous culture
positive cases (2
same as in skin
culture) and showed
statistical
significance:
COLORECTAL
SURGERY:
2017 American Medical Association. All rights reserved. 441
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Culture Positive: 7
cases
Culture Negative: 53
cases
Wound Infection
Culture Positive: 4/7
(57.1%)
Culture Negative: 4/53
(7.5%)
P=0.0042
SSI
Culture Positive: 4/7
(57.1%)
Culture Negative: 6/53
(11.3%)
P=0.0115
Reoperations: NR
Length of stay: NR
Mortality: NR
Adverse events: NR
2017 American Medical Association. All rights reserved. 442
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.1F3. RISK OF BIAS ASSESSMENTS OF STUDIES: Q8-10 ANTISEPTIC PROPHYLAXIS
eTABLE 52. Risk of Bias Assessments of Systematic Reviews for Q8-10 Antiseptic Prophylaxis
Databas- Number of Studies
es included/ screened Heterogenei- Characteris- Funding
describe Inclusion excluded by two Data Individ- ty between tics of source(s)
d and two / studies independ- extracted ual study results included disclosed
or more exclusio along with ent by two study assessed studies and no
Search database- n criteria reasons of reviewers independ- quality qualitatively Publicati- reported in obvious Overall
Author terms es describe exclusion for ent assess- and/or on bias evidence conflict Risk of
Year Q describedsearched d described inclusion reviewers ed quantitatively assessed table of interest Bias
Key Question 8-10: Antiseptic Prophylaxis
Webster
103 8 Low
2012
eTABLE 53. Risk of Bias Assessments of Randomized Controlled Trials for Q8-10 Antiseptic Prophylaxis
Funding
Attrition source(s)
Described Randomizati- smaller than disclosed and
as on Described Outcome Study 10-15% of Attrition no obvious Overall
Author randomiz- appropriately as double- assessor participant Investigat- Attrition assigned appropriately conflict of Risk of
Year Q ed performed blind blinded blinded or blinded described patients analyzed interest Bias
Key Question 8-10: Antiseptic Prophylaxis
Berry
125 8 Low
1982
Bibbo
122 8 High
2005
Chang
140 9 Low
2006
Cheng Modera-
123 8
2009 te
Cheng
141 9 Low
2005
Chiu
133 8 High
1993
Darouiche
120 8 Low
2010
Dewan Modera-
136 8
1987 te
Dromzee Modera-
131 8
2012 te
Ellenhorn Modera-
113 8
2005 te
Gilliam 8 Modera-
2017 American Medical Association. All rights reserved. 443
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Funding
Attrition source(s)
Described Randomizati- smaller than disclosed and
as on Described Outcome Study 10-15% of Attrition no obvious Overall
Author randomiz- appropriately as double- assessor participant Investigat- Attrition assigned appropriately conflict of Risk of
Year Q ed performed blind blinded blinded or blinded described patients analyzed interest Bias
115
1990 te
Harihara
144 10 High
2006
Hort Modera-
118 8
2002 te
Iyer Modera-
129 8
2011 te
Jackson
134 8 High
1971
Murray Modera-
112 8
2011 te
Ostrander Modera-
126 8
2005 te
Paochar-
oen 8 High
121
2009
Psaila Modera-
135 8
1977 te
Roberts Modera-
117 8
1995 te
Rogers Modera-
143 9
1983 te
Saltzman Modera-
116 8
2009 te
Savage
127 8 High
2012
Segal Modera-
114 8
2002 te
Sindelar
139 9 Low
1985
Sindelar Modera-
142 9
1979 te
Sindelar Modera-
137 9
1979 te
Sistla
119 8 Low
2010
Towfigh 8 Low
2017 American Medical Association. All rights reserved. 444
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Funding
Attrition source(s)
Described Randomizati- smaller than disclosed and
as on Described Outcome Study 10-15% of Attrition no obvious Overall
Author randomiz- appropriately as double- assessor participant Investigat- Attrition assigned appropriately conflict of Risk of
Year Q ed performed blind blinded blinded or blinded described patients analyzed interest Bias
130
2008
Veiga
124 8 High
2008
Veiga
111 8 High
2008
Vallance Modera-
138 9
1985 te
Von
Eckardstein 8 Low
128
2011
Ward
132 8 Low
2001
2017 American Medical Association. All rights reserved. 445
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.2. Prosthetic Joint Arthroplasty Section GRADE, Evidence, and Risk of Bias Assessment Tables
2.2A. Q11 BLOOD TRANSFUSION
2.2A1. Q11 GRADE TABLE: Q11 BLOOD TRANSFUSION
eTABLE 54. GRADE Table for Q11 Blood Transfusion
Increase
Decrease GRADE
GRADE
Large Magnitude
GRADE Overall
Publication Bias
Dose-response
Quantity of GRADE
Study Quality
Starting
Confounders
Consistency
Comparison Outcome and Type of Findings Evidence of
Directness
GRADE
Evidence for Evidence
Precision
Outcome Base
Q11. How do perioperative blood transfusions impact the risk of SSI in prosthetic joint arthroplasty patients?
Meta-analysis of 6 studies (N=8493) shows
increased risk with transfusion: OR:1.56
2
(1.18 2.06); p<0.01; I =0
Meta-analysis of 4 OBS(N=7484) shows
increased risk with transfusion: OR: 1.59
145,
Transfusion 2 RCT (1.15 2.18); p<0.01
146
vs. Both meta-analyses include a high
SSI* 147- High 0 0 0 0 0 0 0 0 High High
No 4 OBS proportion of infections in patients
150
Transfusion transfused with allogeneic blood only.
Meta-analysis of 2 RCT (N=1009) shows no
increased risk of infection in patients
transfused with autologous or both
autologous plus allogeneic blood
transfusion: OR 1.07 (0.39 2.89); p=0.90.
Q11A. Are specific blood products associated with a risk of SSI?
Allogeneic Blood Transfusion
In meta-analysis of 4 OBS (N=5737),
Allogeneic combing all allogeneic transfusions without
147-
(any) vs. No 4 OBS regard to buffy coat depletion or Low
SSI* 150 Low 0 0 0 0 0 0 0 0 Low
Transfusion leukoreduction, transfusion associated with
increased risk of infection: OR: 1.96 (1.46
2
2.63); p<0.01; I =0
2017 American Medical Association. All rights reserved. 446
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
GRADE Overall
Publication Bias
Dose-response
Quantity of GRADE
Study Quality
Starting
Confounders
Consistency
Comparison Outcome and Type of Findings Evidence of
Directness
GRADE
Evidence for Evidence
Precision
Outcome Base
In a large retrospective OBS (N=28,087) of
primary THA, using a propensity score
Reoperation
151 matched population (N=4508), reoperations
due to 1 OBS
due to infection were rarely reported (only 5 Low 0 0 0 -1 0 0 0 0 Very Low
wound
or 0.2% in each group) and there was no
infection*
difference between groups OR: 0.57 (0.11
2.93)
In a large prospective study (N=3945) of
primary (81%) and revision (19%) hip and
Allogeneic
knee surgeries, subanalysis of 1644
Not WBC
148 patients found allogeneic not- WBC
depleted vs. SSI* 1 OBS Low 0 0 0 -1 0 +1 0 0 Low Low
depleted transfusion was associated with
No
increased risk of wound infection OR: 2.12
Transfusion
(1.13 4.00); p=0.02
Actual WBC content was not reported.
In a large prospective study (N=3945) of
primary (81%) and revision (19%) hip and
Allogeneic
knee surgeries, subanalysis of 1817
WBC
148 patients suggested no difference in risk of
depleted vs. SSI* 1 OBS Low 0 0 0 -1 0 0 0 0 Very Low Very Low
infection with allogeneic WBC depleted
No
blood: 18/637 (3%) vs. 22/1180 (2%);
Transfusion
p=0.19
Actual WBC content was not reported.
In a prospective study of 444 elective
primary total hip replacements, PJIs were
149
Allogeneic PJI* 1 OBS very rare (1% of total population) and no Low 0 0 0 -1 0 0 0 0 Very Low
Buffy Coat difference was observed between groups
Depleted (both groups 1%) Very Low
vs. No Positive wound cultures were identified in
Transfusion SSI*
149 2.3% of population, and no difference was
Incisional 1 OBS Low 0 0 0 -1 0 0 0 0 Very Low
observed between groups (3.3% vs. 2.0 %);
p=0.47
2017 American Medical Association. All rights reserved. 447
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
GRADE Overall
Publication Bias
Dose-response
Quantity of GRADE
Study Quality
Starting
Confounders
Consistency
Comparison Outcome and Type of Findings Evidence of
Directness
GRADE
Evidence for Evidence
Precision
Outcome Base
Allogeneic buffy coat depleted blood
transfusion associated with increased risk of
Wound- wound healing disturbance (31% vs. 18%;
149
healing 1 OBS p<0.05) Low 0 0 0 -1 0 +1 0 0 Low
disturbance On univariate OR 2.1 (1.2-3.5); p=0.03 and
multivariate analyses, transfusion was the
only significant risk factor
In a meta-analysis of 2 OBS (N=1637),
allogeneic WBC filtered was associated with
increased risk OR: 1.92; (1.12 3.29);
2
p=0.02; I =0
147
One study (N=201) in primary unilateral
Allogeneic
hip or knee arthroplasty (N=201) no
WBC
2 OBS difference with allogeneic WBC filtered
Filtered vs. SSI* 147,150 Low 0 0 0 0 0 0 0 0 Low Low
transfusion: 3/100 (3%) vs. 1/101 (1%);
No
p=0.33
Transfusion
150
In a second larger study , subanalysis
(N=1436) in primary and revision TKA
reported increased risk with allogeneic WBC
filtered: 32/637 (5.0%) vs. 22/799 (2.8%);
p=0.03
148
One study (N=1101) comparing
allogeneic WBC depleted and WBC-not
Allogeneic
depleted found no difference between
lower WBC
groups: 18/637 (3%) vs. 18/464 (4%); OR:
content vs. 148,
2 OBS 0.72; 95% CI: 0.37 1.40; p=0.33
Allogeneic SSI* 150 Low 0 0 0 0 0 0 0 0 Low Low
150
One study (N=1243) comparing
higher
allogeneic WBC filtered to WBC-not
WBC
filtered found no difference between
content
groups: No difference: 32/637 (5.0%) vs.
43/606 (7.1%); P=0.30
Autologous Blood Transfusion
2017 American Medical Association. All rights reserved. 448
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
GRADE Overall
Publication Bias
Dose-response
Quantity of GRADE
Study Quality
Starting
Confounders
Consistency
Comparison Outcome and Type of Findings Evidence of
Directness
GRADE
Evidence for Evidence
Precision
Outcome Base
No difference in a meta-analysis of 2 RCTs
(N=970) OR: 1.15 (0.43 3.13); p=0.78
146
In a small RCT of hip arthroplasties
subanalysis (N=58), no infections were
observed in either group: 0/49 vs. 0/9, but
study was designed to evaluate transfusion
induced immunomodulation, not SSI. (7day
follow up)
145
1 larger RCT in hip arthroplasties,
subanalysis (N=912); no difference at 90
2 RCT
Autologous 145,146 day follow up: 9/481 (1.7%) vs. 7/431
(Any) vs. No SSI* (1.6%);p>0.05 High 0 0 0 -1 0 0 0 0 Moderate Moderate
2 OBS
Transfusion 147,148 In a large prospective (N=3945) OBS study
148
of primary and revision hip and knee
surgeries, subanalysis (N=2491) found
autologous transfusion was associated with
a reduction in wound infections: 11/1311
(1%) vs. 22/1180 (2%); OR: 0.45 (0.22
0.92); p=0.03
147
In an OBS study (N=186) of primary hip
or knee arthroplasty patients: 0/85 vs.1/101-
too few events to perform additional
analysis.
No difference in a large RCT (N=1089) in
THA (regardless of WBC filtration status):
Subanalysis of 657 patients reported no
Autologous
difference with autologous no WBC
WBC
145 filtration transfusions: 5/226 (2.2%) vs.
Filtration vs. SSI* 1 RCT High 0 0 0 -1 0 0 0 0 Moderate Moderate
7/431 (1.6%); p=0.59
No
transfusion Subanalysis of 686 patients reported no
difference with autologous WBC filtered
blood transfusions: 3/255 (1.2%) vs. 7/431
(1.6%); p=0.64
146
Autologous SSI* 1 RCT In a small RCT of THA, subanalysis of 34 High 0 0 0 -2 0 0 0 0 Low Low
2017 American Medical Association. All rights reserved. 449
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
GRADE Overall
Publication Bias
Dose-response
Quantity of GRADE
Study Quality
Starting
Confounders
Consistency
Comparison Outcome and Type of Findings Evidence of
Directness
GRADE
Evidence for Evidence
Precision
Outcome Base
Whole patients, no infections in either group at 7
Blood vs. day follow up. Whole blood included
No autologous donated and perioperative
Transfusion salvage blood.
The study was designed to evaluate
transfusion induced immunomodulation, not
SSI.
In a large prospective (N=3945) study of
primary and revision hip and knee
surgeries, subanalysis (N=2491) found
autologous transfusion (including
autologous blood donated whole blood or
packed red blood cells, cell saver, acute
normovolemic hemodilution, and
Autologous
postoperative salvage) was associated with
Not WBC
148 a reduction in wound infections: OR: 0.45
depleted SSI* 1 OBS Low 0 0 0 -1 0 0 0 0 Very Low Very Low
(0.22 0.92); p=0.03, follow up period was
vs. No
limited to the patients stay in the surgical
Transfusion
unit. Transfusion trigger for autologous
blood transfusion is not reported
Autologous donated blood only: 4/610
(0.66%) vs. 22/1180 (1.86%); p=0.05
Autologous postoperative salvage blood
only: 8/191 (4.19%) vs. 22/1180 (1.86%);
p<0.05
146
In a small RCT of hip arthroplasties
(N=33), no infections were observed in
Autologous
either group at 7 day follow up. The study
Buffy Coat 146
1 RCT was designed to evaluate transfusion
Depleted SSI* 147 High 0 0 0 -2 0 0 0 0 Low Low
1 OBS induced immunomodulation, not SSI.
vs. No
147
In 1 OBS (N=186) of primary hip or knee
Transfusion
arthroplasty patients: 0/85 vs.1/101- too few
events to perform additional analysis.
2017 American Medical Association. All rights reserved. 450
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
GRADE Overall
Publication Bias
Dose-response
Quantity of GRADE
Study Quality
Starting
Confounders
Consistency
Comparison Outcome and Type of Findings Evidence of
Directness
GRADE
Evidence for Evidence
Precision
Outcome Base
146
In a small RCT of hip arthroplasties
(N=49), no infections were observed in
Autologous either group at 7 day follow up. The study
lower WBC was designed to evaluate transfusion
content vs. induced immunomodulation, not SSI.
2 RCT
In a large RCT
145
Autologous SSI* 145,146 of total hip arthroplasties High 0 0 0 -1 0 0 0 0 Moderate Moderate
higher (per protocol analysis, (n=481), no
WBC difference was observed between groups:
content OR: 0.53 (0.12 2.23); p=0.30. Only 1 PJI
reported in each group (Intention to treat
analysis n=951)
In one large OBS study of elective primary
and revision hip and knee arthroplasties,
subanalysis in 801 patients showed
Post-
significantly higher infection rates with
operative
postoperative salvage recovery only
salvage
148 autologous blood versus autologous
only vs. SSI* 1 OBS Low 0 0 0 -1 0 +1 0 0 Low Low
donated blood only in both hip: 3/69 (4%)
Autologous
vs. 4/462 (1%); p<0.05 and knee
Donated
arthroplasties: 5/122 (4%) vs. 0/148 (0%);
blood-only
p<0.05. Hip and knee arthroplasties
combined: 8/191 (4.19%) vs. 4/610 (0.66%)
OR: 0.15; (0.04 0.51); p<0.01
Allogeneic vs. Autologous blood transfusion
When combining transfusions without
Allogeneic regard to buffy coat depletion or
(Any) vs. 3 OBS leukoreduction, transfusion with allogeneic
SSI* 147,148,152 Low 0 0 0 0 0 +1 0 0 Moderate Moderate
Autologous blood was associated with increased risk of
(Any) SSI as compared to autologous transfusion
2
OR: 4.53 (2.37 8.65); p<0.01; I =0
Allogeneic Allogeneic NOT WBC Depleted: In a large
148
WBC 2 OBS prospective study of hip and knee
SSI* 148,152 Low 0 0 0 0 0 +1 0 0 Moderate Moderate
depleted vs. surgeries, subanalysis in 1775 patients
Autologous showed increased risk: 18/464 (4%) vs.
2017 American Medical Association. All rights reserved. 451
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
GRADE Overall
Publication Bias
Dose-response
Quantity of GRADE
Study Quality
Starting
Confounders
Consistency
Comparison Outcome and Type of Findings Evidence of
Directness
GRADE
Evidence for Evidence
Precision
Outcome Base
Not WBC 11/1311 (1%); OR: 4.77 (2.24 10.18);
depleted p<0.01
WBC Not Depleted: In one prospective
148
study Allogeneic versus autologous
blood donation only: 18/464 (4%) vs. 4/610
(0.66%); p=0.001
WBC Not Depleted: One prospective study
148
Allogeneic versus postoperative salvage
only: 18/464 (4%) vs. 8/191 (4.19%); p=0.85
148
WBC depleted: One prospective study
Subanalysis in 1948 patients showed
allogeneic WBC depleted transfusion was
associated with increased risk of wound
infection: 18/637 (3%) vs. 11/1311 (1%);
p=0.01
WBC Depleted: In one small observational
152
study in hip arthroplasties, allogeneic
WBC depleted blood transfusion was not
associated with increased risk of infection
as compared to perioperative cell saver
shed washed blood: 2/48 (4.17%) vs. 0/49;
p=0.28
Allogeneic
WBC
Filtered vs. 147
SSI* 1 OBS No difference: 3/100 (3%) vs. 0/85; p=0.23. Low 0 0 0 -1 0 0 0 0 Very Low Very Low
Autologous
Buffy coat
depleted
Both Autologous and Allogeneic Blood Transfusion
145
Both No difference in post-hoc subanalysis
145
Autologous 1 RCT (N=470) : 0 of 39 transfused vs. 1.6% of
and SSI* 2 OBS 431 not transfused (p=0.82) High 0 0 0 -1 0 0 0 0 Moderate Moderate
147,148
148
Allogeneic One study No difference: 8/329 (2%) vs.
(Any) vs. No 22/1180 (2%) OR: 1.31; 95% CI: 0.58
2017 American Medical Association. All rights reserved. 452
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
GRADE Overall
Publication Bias
Dose-response
Quantity of GRADE
Study Quality
Starting
Confounders
Consistency
Comparison Outcome and Type of Findings Evidence of
Directness
GRADE
Evidence for Evidence
Precision
Outcome Base
Transfusion 2.97; p=0.52
147
No difference in subanalysis (n=123):
0/22 vs. 1/101 (1%)
153
In a large OBS study (N=2884) of
primary total hip (n=2016) and knee (n=480)
arthroplasties and hip revisions (n=388),
Both transfusion with both allogeneic (buffy coat
Autologous depleted) and autologous (buffy coat
and depleted and salvaged blood) was
2 OBS
Allogeneic SSI* 148,153 associated with increased risk of wound Low 0 0 0 0 0 0 0 0 Low Low
vs. infection compared with autologous (buffy
Autologous- coat depleted-only) blood alone. Statistical
only testing was not possible (data presented in
graph format).
148
In 1 study SSI= 8/329 (2%) vs. 11/1311
(1%); p=0.02
Q11B. If the risk of SSI is increased, can this effect be isolated from the risk associated with more complex cases?
Increased risk of transfusion among
revisions (THA and TKA combined) in a
Revision vs.
meta-analysis of 2 OBS studies (N=6385):
Primary 2
OR 3.81 (1.61 9.03); p<0.01; I =95%
Arthroplasty
148
2 OBS In one study Increased risk among
(Hip [THA] Transfusion* 148,150 Low 0 -1 0 0 0 +1 0 0 Low Low
revisions: 303/362 (84%) vs. 2112/3118
and knee
(68%); p<0.001
[TKA]
150
combined) In one observational study Increased risk
among revisions: 274/350 (78%) vs.
969/2555 (38%); p<0.01
Revision Higher risk of transfusion among revision
148
THA Transfusion* 1 OBS THA: 252/293 (86%) vs. 51/69 (74%); Low 0 0 0 -1 0 0 0 0 Very Low Very Low
vs. Revision p=0.02
2017 American Medical Association. All rights reserved. 453
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
GRADE Overall
Publication Bias
Dose-response
Quantity of GRADE
Study Quality
Starting
Confounders
Consistency
Comparison Outcome and Type of Findings Evidence of
Directness
GRADE
Evidence for Evidence
Precision
Outcome Base
TKA
Calculated 148 No difference in median calculated blood
1 OBS Low 0 0 0 -1 0 0 0 0 Very Low
blood loss loss: 2875ml vs. 2528ml; p=0.23
148
Any blood transfusion : Higher risk
among revision hip arthroplasties: 252/293
(86%) vs. 1405/2066 (68%); p<0.01
148
Allogeneic only : More allogeneic only
transfusions among transfused revision hips
as compared to primary hip arthroplasties:
115/252 (46%) vs. 503/1405 (36%); p<0.01
148
Autologous only : More autologous only
transfusions among transfused primary hip
as compared to revision hip arthroplasties:
2 OBS
Transfusion* 148,153 83/252 (33%) vs. 737/1405 (52%); p<0.01 Low 0 0 0 0 0 0 0 0 Low
BOTH Autologous and additional allogeneic
blood transfusion; Higher risk among
Revision revision THAs- Meta-analysis (N=4061): OR
2
THA 2.44 (1.77 3.36); p<0.01; I =50%
148
vs. One OBS Higher risk among revision Low
Primary THAs: 54/252 (21%) vs. 165/1405 (12%);
THA p<0.001
153
One OBS Higher risk among revision
THAs: 76/388 (20%) vs. 159/2016 (8%);
p<0.01
Meta-analysis 2 OBS studies: significantly
higher calculated blood loss in revision hips:
mean difference 700 ml (95% CI: 323 ml
2
1076 ml); p=0.0003; I =87%
Calculated 2 OBS
blood loss
148,153 Mean calculated blood loss higher for Low 0 0 0 0 0 0 0 0 Low
148
revision hip: 3060 ml vs. 2143 ml; p<0.01 ;
Mean blood loss significantly higher for
revision hip: 1720460ml vs. 1190480ml;
153
p<0.01
2017 American Medical Association. All rights reserved. 454
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
GRADE Overall
Publication Bias
Dose-response
Quantity of GRADE
Study Quality
Starting
Confounders
Consistency
Comparison Outcome and Type of Findings Evidence of
Directness
GRADE
Evidence for Evidence
Precision
Outcome Base
Significantly longer procedure duration for
Procedure 153 revision hip arthroplasty (mean SD):
1 OBS Low 0 0 0 -1 0 0 0 0 Very Low
duration 18364 minutes vs. 11538 minutes;
p<0.01
Any transfusion no difference for revision
knee as compared to primary knee: 51/69
(74%) vs. 707/1052 (67%); p=0.25 no
difference for revision knee as compared to
primary bilateral knees: 51/69 (74%) vs.
11/13 (85%); p=0.42
Revision 148 Allogeneic only: No difference- 23/51 (45%)
Transfusion* 1 OBS Low 0 0 0 -1 0 0 0 0 Very Low
TKA vs. vs. 245/707 (35%); p=0.13
Autologous only: No difference -17/51 Very low
Primary
TKA (33%) vs. 245/707 (49%); p=0.85
BOTH autologous and additional allogeneic
blood transfusion higher risk of transfusion
for revision knees: 11/51 (21%) vs. 77/707
(11%); p=0.02
Calculated 148 Mean calculated blood loss higher for
1 OBS Low 0 0 0 -1 0 0 0 0 Very Low
blood loss revision knee: 2634 ml vs. 2072 ml; p<0.01
148
Any transfusion : No difference-
1405/2066 (68%) vs. 707/1052 (67%);
p=0.65
148
Allogeneic only : No difference- 503/1405
(36%) vs. 245/707 (35%); p=0.60
Primary
148
148, Autologous only : No difference- 737/1405
THA vs. 2 OBS
Transfusion* 153 (52%) vs. 385/707 (54%); p=0.38 Low 0 0 0 0 0 0 0 0 Low Low
Primary
TKA Both Autologous and additional allogeneic
148
: No difference- 165/1405 (12%) vs.
77/707 (11%); p=0.56
BOTH autologous and additional allogeneic
153
: No difference-159/2016 (8%) vs.
43/480 (9%); p=0.44
2017 American Medical Association. All rights reserved. 455
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
GRADE Overall
Publication Bias
Dose-response
Quantity of GRADE
Study Quality
Starting
Confounders
Consistency
Comparison Outcome and Type of Findings Evidence of
Directness
GRADE
Evidence for Evidence
Precision
Outcome Base
Meta-analysis 2 OBS: No difference- Mean
difference: -19 ml (-176 ml 137 ml);
2
p=0.81; I =84%
Mean calculated blood loss no difference:
148
2143 ml vs. 2072 ml; p=0.24
Mean blood loss higher in primary knee
Calculated 2 OBS arthroplasty 1190480ml vs. 1280403;
148,153 153 Low 0 -1 0 0 0 0 0 0 Very Low
blood loss p<0.01
Median preoperative estimate blood loss
was significantly lower than median
calculated blood loss for both primary total
hip (median 750 vs. 1944ml; p<0.01) and
total knee (median, 800 vs. 1934ml; p<0.01)
148
procedures .
Any transfusion -No difference: 1387/2039
(68%) vs. 18/27 (67%); p=0.88
Allogeneic only: No difference: 496/1387
Primary
(36%) vs. 7/18 (39%); p=0.78
THA: 148
Transfusion* 1OBS Autologous only: No difference 728/1387 Low 0 0 0 -1 0 0 0 0 Very Low Very Low
Unilateral
(53%) vs. 9/18 (50%); p=0.83
vs. Bilateral
BOTH Autologous and additional allogeneic
blood transfusion: No difference: 163/1387
(12%) vs. 2/18 (11%); p=0.93
Any transfusion: No difference: 696/1039
(67%) vs. 11/13 (85%); p=0.20
Allogeneic only: No difference - 242/696
Primary
(35%) vs. 3/11 (27%); p=0.61
TKA: 148
Transfusion* 1OBS Autologous only: No difference 377/696 Low 0 0 0 -1 0 0 0 0 Very Low Very Low
Unilateral
(54%)vs. 8/11 (74%); p=0.23
vs. Bilateral
BOTH Autologous and additional
allogeneic: Only unilateral TKA received
both:- 77/696 (11%) vs. 0/11 (0%); p=0.47
Q11C. How does the volume of transfused blood product impact the risk of SSI? Our search did not identify data that evaluated differences in the volume of
transfused blood product and their impact on the risk of SSI in prosthetic joint arthroplasty patients.
2017 American Medical Association. All rights reserved. 456
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
GRADE Overall
Publication Bias
Dose-response
Quantity of GRADE
Study Quality
Starting
Confounders
Consistency
Comparison Outcome and Type of Findings Evidence of
Directness
GRADE
Evidence for Evidence
Precision
Outcome Base
Q11D. How safe and effective is withholding blood transfusion to reduce the risk of SSI? Our search did not identify data that both evaluated the safety and
effectiveness of withholding blood transfusions and its impact on the risk of SSI in prosthetic joint arthroplasty patients.
*Critical outcome; OR: Odds Ratio; RR: Risk Ratio; CI: Confidence Interval
2017 American Medical Association. All rights reserved. 457
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.2A2. EVIDENCE TABLE: Q11, Q11A, AND Q11B BLOOD TRANSFUSION
Q11. How do perioperative blood transfusions impact the risk of SSI in prosthetic joint arthroplasty patients?
Q11A. Are specific blood products associated with a risk of SSI?
Q11B. If the risk of SSI is increased, can this effect be isolated from the risk associated with more complex cases?
eTABLE 55. Evidence Table for Q11. How do perioperative blood transfusions impact the risk of SSI in prosthetic joint
arthroplasty patients?
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
Frietsch RCT To determine if No. patients: Intervention Group: SSI (3 months) Definitions:
145
2008 1, 2, 3, 4, leukoreduction of ITT: N=951 Leukodepleted AWB ITT Analysis N=951 Wound Infection: Defined either as
(SIBT) 5, 7, 8, 9, autologous whole Per-Protocol=481 (LD-AWB) Wound Infections 1. isolation of bacteria from fluid
10 blood (AWB) ITT n=488 Intervention: 6/488 wound secretions containing pus,
reduces the Patient Per Protocol n=255 (1.2%); 2. abscesses (verified by surgical
. transfusion- Characteristics: (52.3%) Control: 9/463 (1.9%) drainage or aspiration of pus), or
related Baseline Timing of Intervention: OR 0.63 (95% CI, 0.22- 3, arthritis by clinical symptoms
immunomodulatio characteristics of Intra and postoperative 1.78); p=0.27 requiring surgical drainage.
n (TRIM) effect, the patients were Duration of Other infections Respiratory tract infection (RTI): 1)
resulting in similar in the two Intervention: NR Overall, urinary, positive x-ray (chest infiltration)
reduced groups (number, Device/ Agent: respiratory, together with fever, 20 dyspnea or
perioperative sex, age, height, Intervention (LD-AWB): fungal and Other cough or purulent sputum together
infection rate weight, calculated double bag system with (gastrointestinal, with fever, or 3) isolation of bacteria
and/or length of blood volume, inline whole-blood WBC pleuritis, vascular in tracheal secretion (only intubated
hospital stay. overall estimated filter for pre-storage thrombophlebitis, skin patients) together with fever.
perioperative leukoreduction. Blood infection other than ASEPSIS Index: Daily wound
blood loss, was leukoreduced after wound, gynecologic) inspections evaluated for the
donated storage on cooling none with statistically following wound conditions: clear
autologous units plates at 4 to 6C for 1-4 significant difference exudate, erythema, putrid exudate,
per patient, ASA hours. Residual WBC Note: Infections dehiscence of profound tissue layers
score, Anesthesia content was consistently occurred while in with size of relative wound area of
6
type, surgery type below 1 X 10 per unit hospital in 87.5% of the total wound concerned. If more
[cementless, and mean red blood cell cases. than one wound condition was
cemented, hybrid], loss (RBC) was less Per-protocol Analysis existent, only the condition with the
duration of than 10%. N=481 highest rating was scored. Wound
surgery, Control (non-ND Wound Infections inspection scores were added up
anesthesia and AWB): single-bag Intervention: 3/255 (dynamic part). Each of the
hypothermia. system. All units stored (1.2%) additional criteria (antimicrobial
Age years at 4C until transfusion Control: 5/226 (2.2%) treatment, abscess drainage [local
median (range) or expiry 0.53(0.12-2.23);p=0.30 vs. general anesthesia], bacterial
Intervention:63 Both systems contained Other infections growth [positive culture of at least
(28-82) 70ml citrate phosphate Overall, urinary, 100,000 colonies of a single
2017 American Medical Association. All rights reserved. 458
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
Control:63 (26-83) dextrose adenine respiratory, organism], and prolonged hospital
Gender m/f: (CPDA-1) as storage fungal and Other stay (static part) could be added
470/481 medium. (gastrointestinal, once.
meanSD(median/ Monitoring pleuritis, vascular
range) Intervention: thrombophlebitis, skin Perioperative Care
Height (cm) Hemoglobin (Hb) levels. infection other than Preop:
Intervention: Transfusion Trigger: wound, gynecologic) Patients were scheduled to donate 2
1708.9 (170/150- Hemoglobin (Hb) none with statistically or 3 units of AWB (500ml each) in
196) concentration significant difference weekly intervals with surgery
Control: <8.00.5g/L during and planned to take place in weeks 3 to 5
170.39.0(170/14 after surgery In both ITT and Per- after the first donation.
0-197) (irrespective of whether Protocol:
Weight(kg) autologous or allogeneic Overall infection rate, Hb concentration below 110g/L
Intervention: blood was to be ASEPSIS score, during donation period led to
80.1 14.1(80/48- transfused) Length of Stay, postponement of following donation
126) antimicrobial by 1 week.
Control: Control Group- Non- treatment, multidrug
80.414.2(80/50- leukodepleted AWB use, fever>38C after Patients encouraged to take oral iron
2+
136) (non-LD AWB) postop day 3: No (300mgFe orally per day)
ASA1=192/951 ITT n=463 significant difference
(20.2%) Per Protocol n=226 RBC loss was calculated as the
ASA2=628/951(66 (48.8%) SUBGROUP compensated RBC loss
.0%) ANALYSIS 1: (perioperatively transfused RBC
ASA3=125/951(13 Standard preventive Not transfused (NOT-T; volume) plus non-compensated RBC
.1%) measures AMP (second n=431) vs. loss estimated from pre and
Comorbidities: generation Autologous only postoperative (Day 3) hematocrit
NR cephalosporin) , transfused (AUT-T; (Hct) levels correcting large-vessel to
Procedure: normothermia, n=481) total body Hct:
Primary hip normovolemia, adequate vs. RBC loss= (Hctpre-HctPOD3) X Blood
arthroplasty oxygenation Additionally Volume* X 0.86+RBC-Vunits.
(cemented n=30, allogeneically transfused RBC-Vunits=RBC volume of
cementless (ALL-T; n=39) transfused AWB
n=642, hybrid Overall infection rate: *Calculated according to Nadler)
n=274) NOT-T: 14.2% Blood loss=RBC loss/(Hctpre-
Indications: NR AUT-T: 20.6% HctPOD3)/2
Setting: 2 ALL-T: 13.2%
university and 1 p=0.03 Transfusion rates by Center:
urban hospital: Wound infections: No transfusion; autologous only;
Center A n=696 NOT-T: 1.6% autologous and allogeneic
2017 American Medical Association. All rights reserved. 459
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
(73.2%); Center B AUT-T: 1.7% A n=696: 43%;52.7%;4.3%
n=213 (22.4%) ALL-T: 0% B n=213:56.8%;39.4%;3.8%
Center C n=42 p=>0.05 C n=42: 26.2%, 71.4%, 2.4%
(4.4%) Urinary tract Infection: Anesthesia
Location: NOT-T 11.1% Spinal: Intervention: AWB 297/488
Germany AUT-T 16.8% (60.9%)
Dates: NR ALL-T 13.2% Control: Non LD AWB: 312/463
Inclusion criteria: p=0.02 (67.4%)
Patients Other infections: General: Intervention: AWB 187/488
scheduled for Respiratory, fungal, and (38.3%)
primary hip other infections Control: Non LD AWB: 143/463
arthroplasty and (gastrointestinal, (30.9%)
preoperative pleuritis, vascular Epidural: Intervention: AWB 2/488
donation of at thrombophlebitis, skin (0.4%)
least 2 units of infection other than Control: Non LD AWB: 1/463 (0.2%)
AWB wound, gynecologic) all Other Intervention: AWB 2/488
Exclusion p=>0.05 (0.4%)
criteria: Subjects Length of Stay days: Control: Non LD AWB: 3/463 (0.6%)
with meanSD (median)
contraindications NOT-T 13.02.3 (13)
for preoperative AUT-T 13.83.6 (14) Follow up: Phone, letter or an
autologous blood ALL-T 14.34.2 (14) outpatient visit 3 months post op.
donation p=0.01 Wound inspection: daily during the
according to the first 14 postoperative days and
German Note: significant discharge, not on weekends
guidelines, difference in infection Funding Source Conflicts:
immune rate and length of stay Authors: None
deficiency, steroid was paralleled by Institution: None
therapy and significantly longer Study: None
intended use of anesthesia and surgery Supplies: Industry
cell salvage. duration (NR),
suggesting dependency
from the complexity level
of surgery rather than
transfusion.
SUBGROUP
ANALYSIS 2: Micro-
aggregate filtration of
2017 American Medical Association. All rights reserved. 460
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
blood product at bedside
at Centers A and C.
Subgroup analysis to
exclude any influence of
these microfilters on
overall infections rate
showed no statistical
significant difference
(p=0.63, two-sided).
Topic specific
outcomes: N/A
Reoperation:
In both ITT and Per-
Protocol:
antimicrobial treatment,
multidrug use: No
significant difference
In ITT protocol:
Wound infection
requiring revision or
hospitalization:
Intervention: 1/488
(0.2%)
Control: 3/463 (0.6%)
Delayed wound healing
requiring revision or
hospitalization:
Intervention: 7/488
(1.4%)
Control: 7/463 (1.5%)
Surgical wound revision:
Intervention: 3/488
(0.6%)
Control: 8/463 (1.7%)
Prosthesis infection:
Intervention: 1/488
(0.2%)
2017 American Medical Association. All rights reserved. 461
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
Control: 1/463 (0.2%)
Re-surgery - prosthesis
exchange:
Intervention: 1/488
(0.2%)
Control: 1/463 (0.2%)
Length of stay: Median
(range)
ITT
Intervention (LD AWB):
14 days (7-36)
Control (Non-LD
AWB):14 days (8-55)
P=0.17
Per-Protocol
Intervention (LD AWB):
14 days (7-34)
Control (Non-LD
AWB):14 days (9-55)
P=0.71
Mortality: none
Adverse events:
In ITT protocol: not
significantly different
between groups
Total:
Intervention: 1/488
Control: 1/463
Relation to LD:
Possible /unlikely
unrelated
Intervention: 3/7/3
Control: 2/2/8
Myocardial infarction,
bradycardic arrhythmia,
transient cerebral,
ischemic attack,
2017 American Medical Association. All rights reserved. 462
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
respiratory insufficiency
(sleep apnea), deep
venous thrombosis,
dyesthesia foot
Frietsch RCT To address Number of Intervention group: SSI (follow up 7 days) Definitions: NR
146
2001 1, 2, 5, 7, Transfusion- patients N=58 n=2 None of the patients Perioperative care:
(ES) 8, 9, 10 induced Patient Transfused Autologous presented clinical signs Anesthesia: spinal/general
immunomodulatio Characteristics Blood: of infection. Authors WB: 17/8
n (TRIM) caused WB=Whole Blood Blood was donated at indicate This study is RCP: 20/4
by autologous RCP=buffy coat- weekly intervals (450ml not expected to have the NT: 8/1
blood stored poor packed Red each). Surgery was statistical power to
th
either as Whole Cells and fresh- scheduled for the 5 discriminate between the Analytical methodology: Shapiro-
Blood (WB) or as frozen Plasma week after the first two types of storage Wilk test used to probe for normality
buffy coat-poor NT-NO donation. regarding outcome of distribution (P>0.4). For repeated
packed red cells Transfusion RCP: Buffy coat-poor criteria of measurements, baseline corrected
and fresh-frozen Age: meanSD packed red cells (RC) immunomodulation, area under curve (AUC) was
plasma (RCP) WB: 5810 years and fresh-frozen plasma such as wound or calculated. T-test and Wilcoxon rank
in patients RCP: 5910 (FFP): n=24 donated systemic infection rates sum test for independent variables
undergoing hip years blood was separated or LOS, as the infection were used to determine statistical
arthroplasty. NT: 618 years into RC and FFP(80- rate in this type of significance.
Monocyte and Gender: m/f 90% of leukocytes and surgery is generally low Other notes: Small sample size
neutrophil WB: 9/16 >98% platelets were Follow-up: 7 days observation
phagocytic RCP: 10/14 eliminated) period
activities, rate of NT: 7/2 Timing of intervention: Other infections: None Funding Source Conflicts:
systemic and Obesity: intra or postoperatively occurred in either group. Authors: None
wound infection, Weight Duration of Topic-specific Institution: None
se of WB: 7116 kg intervention: Intra outcomes: Study: None
antimicrobials RCP: 7415 kg and/or postoperatively. Supplies: None
and length of NT: 8410 kg Agent: Autologous No allogeneic
hospital stay Height blood. Either Whole transfusions were
(LOS) were WB: 1669 cm blood (WB) or buffy-coat required in any group.
evaluated. RCP: 1687 cm poor packed red cells
NT: 1715 cm (RC) Total Blood loss: median
Comorbidities: - Oldest blood was used (Range)
NR first. WB: 1740 (820-3170)
3Units Monitoring ml
Predeposited intervention: RCP: 1760 (880-3290)
WB: 22/25(88%) hemoglobin count and ml
RCP: 22/24 leucocyte counts were NT: 1530 (1120-2320)
2017 American Medical Association. All rights reserved. 463
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
(91.2%) determined by routine ml
NT: 9/9 (100%) automated laboratory Transfusion of
2 Units methods. Differential predeposited units
Predeposited blood cell count was 3 units
WB: 3/25 (12%) measured by WB: 3/25
RCP: 2/24 depolarized orthogonal RCP[(RC/FFP)/n]:
(8.8%) light scattering (9/7)/24
NT: 0 Control group: n=32 NT: 0
Storage period WB Whole Blood n=25 2 units
(days) donated blood units WB: 8/25
WB: 27.92.9 stored as whole blood RCP[(RC/FFP)/n]:
RCP: 28.42.0 Non-transfused patients (6/6)/24
NT: 28.21.6 (NT) NT: 0
Length of Surgery NT 7 had donated blood 1 unit
WB: 10217 stored as WB vs. 2 as WB: 14/25
minutes RCP. RCP[(RC/FFP)/n]:
RCP: 8921 Standard preventive (9/4)/24
minutes measures NT: 0
NT: 9225 Thromboembolic P0.05 for all transfusion
minutes Prophylaxis: 40mg of unit values (3, 2, 1) for
subcutaneous WB vs. RC
Procedures: Hip enoxaparin administered Volume replacement
arthroplasty 1/day starting 12h prior (ml)
Indications: NR to surgery. Modified Ringers
Setting: 1 AMP: cefuroxime Solution
university hospital administered WB: 4376802
Location: intravenously prior to RCP: 4604642
Germany surgery. NT: 44221190
Dates: NR Cemented, cementless, Colloid Solution
Inclusion and hybrid prostheses WB: 1540628
Criteria: patients were implanted. RCP: 1333602
who had donated Volume replacement: NT: 1417530
autologous blood modified ringers solution
and were and gelatin solution were Patients with Cell
scheduled for hip used. Salvage
arthroplasty Postop_ autologous WB: 12/25 (48%)
Exclusion plasma was re- RCP: 8/24 (33.3%)
Criteria: transfused for volume NT: 1/9 (11.1%)
contraindication replacement primarily in Volume transfused:
2017 American Medical Association. All rights reserved. 464
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
for autologous the RCP group. median(range)
blood donations Analgesic: diclofenac & WB: 510 (240-1200) ml
and diseases prirtarmid. RCP: 610 (4-1600) ml
associated with Cell salvage: performed NT: 360 ml
impaired immune in all groups if a patient
defense. had <3 units and/or Laboratory Analysis:
presented for surgery Regarding hemoglobin
with Hb concentration concentration,
<12g/dl. Blood collected neutrophils, monocytes,
was processed and phagocytic activity, and
retransfused with drain oxidation activity:
blood measured and There were no
sponged blood significant differences in
estimated values between the
Transfusion Triggers: three groups.
Hb, 9g/dl or clinical signs
of myocardial ischemia. Reoperations: NR
Length of stay:
(meanSD)
WB: 15.30.8 days
RCP: 15.30.6 days
NT: 15.01.0 days
Mortality: NR
Adverse events: NR
Pedersen Retrosp- To determine Number of Intervention group: SSI (Follow Up 90 Definitions
151
2009 ective whether patients: Receiving Transfusion Days) Outcomes (within 90 days of index
(ES) concur- allogeneic red N=28,087 Intervention1: n=9063 (Adjusted) procedure):
ent blood cell Matched group (32.3%) Reoperation due to 1. Death,
control transfusion was N=4508 Patients received 1 unit infection 2. Hospitalization with cardiovascular
1, 2, 3, 4, associated with Patient red blood cell (RBC) Intervention2: 5/2254 events including myocardial
5, 6, 7, 8 increased odds of Characteristics: transfusion within 8 days (0.2%) infarction, congestive heart failure,
complications For total group, of surgery Control2: 5/2254 peripheral vascular disease, or
following primary Transfused Intervention2: n=2254 (0.2%) cerebrovascular events,
total hip patients were Patients receiving 1 OR (95%CI): 0.57 (0.11- 3. hospitalization with venous
replacement older & had more unit RBC allogeneic 2.93) thromboembolism, including deep
(THR). comorbid transfusion within 8 days venous thrombosis and/or pulmonary
Complications conditions. They of surgery (matched by Other infections: embolism,
included also were more propensity scoring to the Pneumonia: adjusted 4. hospitalization with pneumonia
2017 American Medical Association. All rights reserved. 465
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
hospitalization likely to be female, control2 group Intervention2: 36/2254 and
with receive a (1.6%) 5. reoperation due to infection.
cardiovascular cemented Timing of intervention: Control2: 17/2254
and/or prosthesis, and to intraoperative &/or (0.8%) Perioperative care:
cerebrovascular have a THR Postoperative OR (95%CI): 2.1 (1.2- Regional Anesthesia:
events, venous procedure of more 3.8) Intervention2: 1753/2254 (77.8%)
thromboembolis than 2 hours. Duration of Control2: 1757/2254 (78.0%)
m, pneumonia, For the intervention: within 8 Topic-specific SMD=0.18378
reoperation due propensity- days of surgery outcomes:
to infection of matched Median (range) number Analytical methodology: To
primary THR, and population, there Agent: Allogeneic red of units transfused: overcome bias due to confounding,
mortality within were no blood cells. Intervention1: 2 (1-20) they matched patients not receiving
90 days of substantial Intervention1: Control: 0 transfusions with patients receiving
primary THR differences for any Median: 2units/patient transfusion with a 1:1 ratio using
of the Range: 1-20 units Duration of operation: propensity score matching. The
characteristics Similar between propensity score for each patient
related to the risk Monitoring matched groups except was calculated using logistic
of transfusion intervention: NA for Longer surgeries: regression. Patients were matched
Standardized >121 minutes: for baseline characteristics.
mean difference Control group: Intervention2: 151 Information on blood lost during
(SMD)>0.1 is No Transfusion (6.7%) surgery was not available for this
indicative of Control1: n=19024 Control2: 157 (7.0%) dataset.
significant Patients who received SMD: 0.20997 They adjusted for hemoglobin
imbalance no transfusion Preoperative concentration 1-7 days postoperative
between groups Control2: n=2254 Hemoglobin as a surrogate measure of blood
Patients who received concentration w/in 3 loss.
Age: Age no transfusion and were months prior to surgery: Information on smoking status,
groupings were matched by propensity <138.5 g/L obesity/BMI, prior history of
similar between scoring to Intervention2 Intervention2: 1410 transfusion, and preoperative history
groups except for (62.6%) of increased perioperative bleeding
80+ years Standard preventive Control2: 1362 (60.4%) and pre-operative history of chronic
Intervention2: measures: NR SMD: 0.25041 anemia was also not available and
404/2254 (17.9%) not included in propensity matching
Control2: Non-standard score.
411/2254 (18.2%) preventive measures:
SMD= 0.18397 Anti-rheumatic drug Length of stay: NR Other notes: Data utilized in this
Prophylaxis for study is from
Gender: female n heterotropic bone Mortality: (within 90 1) The Danish Hip Arthroplasty
(%) formations: days of primary THR) - Registry (DHR). This registry of all
2017 American Medical Association. All rights reserved. 466
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
Intervention2: Intervention2: 195/2254 adjusted primary THR consists of data
1490/2254 (8.7%) Intervention2: 39/2254 recorded prospectively by the
(66.1%) Control2: 208/2254 (1.7%) operating surgeons using
Control2: (9.2%) Control2: 18/2254 standardized forms. (pre-, peri- and
1439/2254 SMD=0.06109 (0.8%) postoperative data). Reoperation
(63.8%) OR (95%CI) 2.17 (1.24- data was also obtained here.
SMD=0.11293 3.80) 2) The Danish Transfusion
Database. Data included all
Obesity: NR Adverse events: allogeneic red blood cell transfusions
Comorbidities: Deep venous administered to included patients
Diabetes thrombosis/ pulmonary within 8 days of primary THR
Intervention2: embolism adjusted surgery. Patients were classified as
134/2254 (5.9%) Intervention2: 28/2254 having received either no or one or
Control2: (1.2%) more units.
115/2254 (5.1%) Control2: 23/2254 3) The Civil Registration System was
SMD=0.05238 (71.0%) utilized for data on mortality.
Preoperative OR (95%CI): 1.17 (0.67- 4) The Danish National Registry of
Hemoglobin 2.06) Patients was used for hospitalization
<138.5g/L within 3 data. Diagnoses were classified
mo. before Cardiovascular or according to the Danish version of
surgery cerebrovascular disease the International Classification of
Intervention2: adjusted Diseases (ICD. The ninth edition
1410/2254 Intervention2: 54/2254 (ICD-8) was used from 1977 to 1993
(62.6%) (2.4%) and the tenth edition (ICD-10) has
Control2: Control2: 39/2254 been used hereafter. The physician
1362/2254 (1.7%) who diagnosed the patient assessed
(60.4%) OR (95%CI): 1.42 (0.93- all discharge codes.
SMD=0.25041 2.15)
Odds estimates may partly reflect
Procedures: Composite outcome unmeasured bias due to blood loss
Primary Total Hip adjusted
Replacement OR (95% CI): 1.67 Limitation: No information on
(THR) (1.23-2.26) intraoperative blood loss which may
Indications: have impacted postop transfusions.
Primary arthrosis Subanalysis of Information on pre/post-operative
Intervention2: composite outcome risk hemoglobin concentration used as a
1647/2254 by Number of surrogate measure of blood loss.
(73.1%) transfusions/ patient:
Control2: Adjusted OR (95%CI) Follow-up: until the occurrence of
2017 American Medical Association. All rights reserved. 467
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
1633/2254 6 transfusions:3.4 (1.3- death, hospitalization for
(72.5%) 9.2) cardiovascular or cerebrovascular
SMD=0.23293 3-4 transfusions: 1.5 events, venous thromboembolism,
Trauma (0.8-2.9) pneumonia, reoperation due to
Intervention2: 2-3 transfusions: 1.2 infection or 90 days after surgery.
323/2254 (14.3%) (0.8-1.9) Funding Source Conflicts:
Control2: 1 transfusion: 2.7 (1.2- Authors: None
319/2254 (14.2%) 5.7) Institution: None
SMD=0.28662 Study: None
Other Subgroup analysis for Supplies: None
Intervention2: history of cardiovascular
284/2254 (12.6%) events
Control2: With History (matched)
302/2254 (13.4%) Intervention2: 407/2254
SMD=0.00682 (18.1%)
Control2: 407/2254
Setting: Multi- (18.1%)
center 20 - Red blood cell
hospitals in North transfusion was
Jutland, Aarhaus, associated with odd of
Funen, and the composite adverse
Copenhagen). outcome within 90 days
These 20 of surgery: 1.2 (0.8-1.9)
orthopaedic
departments serve Without History
~45% of the (matched)
Danish population Intervention2:
(nearly 2.3 million 1834/2254 (81.4%)
people). Control2: 1834/2254
Location: (81.4%)
Denmark In THR patients without
Dates: January 1, cardiovascular events
1999 December prior to surgery, OR of
31, 2007 composite outcome: 1.7
Inclusion (1.1-2.7)
Criteria: Patients
with primary THR Subgroup analysis
procedures postoperative
registered in the hemoglobin (matched)
2017 American Medical Association. All rights reserved. 468
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
Danish Hip Hemoglobin
Arthroplasty concentration <105g/L
Registry (DHR) Intervention2: 729/2254
and performed at (32.3%)
the hospitals Control2: 729/2254
reporting to the (32.3%)
Danish - Adjusted OR: for
Transfusion composite adverse
Database during outcome w/in 90 days of
the study dates. surgery: 1.1 (0.5-2.7) for
This includes transfused vs. non
patients who transfused
sustained right
and left THR Hemoglobin
during the study concentration>105g/L
period as long as Intervention2:
surgery was not 1505/2254 (66.8%)
performed on the Control2: 1505/2254
same day (those (66.8%)
were treated as - Adjusted OR: for
independent composite adverse
operations) outcome w/in 90 days of
Exclusion surgery: 1.6 (1.0-2.5) for
Criteria: Patients transfused vs. non
without possibility transfused
for follow up and
bilateral primary
THR procedures
performed during
the same surgery.
Monte del Prospect- To prospectively Number of Intervention group: SSI (Follow up - NR) Definitions:
Trujillo ive evaluate the patients N=108 n=60 Unadjusted: Postoperative Infectious
152
2008 concurre utility of a new Patient Utilization of the blood Total Infection: Complications (urinary tract,
(ES) nt control device that Characteristics: processing device Intervention: 1 (2%) respiratory tract, and wound
1, 3, 4, 5, automatically There were no designed to wash Control: 5 (10%) infections): CDC definitions.
6, 7, 8 provides washed differences in autologous blood and re- P=0.086 Adverse reactions to WSB
salvaged blood to characteristics infuse the blood. Wound Infection reinfusion: Shivers, fever,
reduce exposure between groups Intervention: 0 (0%) bradycardia, hypotension
2017 American Medical Association. All rights reserved. 469
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
to Allogeneic except age and Timing of intervention: Control: 2 (4%) Estimated blood volume: calculated
Blood Hypertension. intraoperative and/or Infection Rate using gender and body weight
Transfusions Data expressed as postoperative ABT: 12.2% (4/32) [Gross1983]
(ABT) in elective mean SD or n Duration of No ABT: 2.6% (2/76) Total Perioperative Blood Loss (CBL
Total Hip (%) intervention: duration of p=0.046 (ml)) = [Uncompensated RBC loss
Replacement Age (y): transfusion (ml) = Compensated RBC loss
(THR) patients. Intervention: Other infections: (ml)]/0.35
End-points 6214 Agent: Perioperatively Urinary Infection Uncompensated RBC loss (ml)=
include the Control: 679 salvaged WSB. The Intervention: 1 (2%) (preoperative Hct postoperative
impact of P= 0.027 blood was collected with Control: 2 (4%) day 4 Hct) x Estimated Blood
Washed Gender: f/m non-fractionated heparin Volume (EBV)
Salvaged Blood Intervention: and was re-infused Respiratory Infection: Compensated RBC Loss (ml) =
(WSB) return on 27/33 within the first 6h from Intervention: 0 (0%) [Packed allogeneic red cell units x
both the rate of Control: 31/17 the beginning of blood Control: 1 (2%) 165 (ml/unit) = [washed autologous
postoperative Obesity: weight salvage. blood volume x washed autologous
infection and the (kg) Device: A blood Topic-specific blood Hct]
length of hospital Intervention: processing device outcomes: Acute Anemia: hypotension,
stay. 799 designed specifically to Intervention: Enough tachycardia, tachypnea, dizziness,
Control: 8011 adapt to the intermittent WSB blood volume fatigue.
Comorbidities blood loss of orthopedic obtained to be returned:
Diabetes surgical patients. 49/60 (82%) Perioperative care:
Intervention: 7 Mean: 336205 Anesthesia: standard general or
(12%) Monitoring Hct: 635% regional
Control: 12 intervention: NR RBC: 205151ml Cemented THR: Regional/General
(25%) RBC/patient: 1.30.9 Anesthesia
Anemia Control group n=48 Intervention: 6/6
(Hb<130g/l) Patients received normal **Calculated and total Control: 8/9
Intervention: 4 allogeneic blood perioperative blood loss P=0.876
(7%) transfusions (ABT) if was not significantly Uncemented THR: Regional/General
Control: 2 (4%) necessary, one unit of different between groups Anesthesia
Hypertension leukodepleted packed according to age, Intervention: 27/21
Intervention: 16 red blood cell was gender, anesthesia type Control: 13/18
(27%) considered to have a or hypertension. P=0.119
Control: 32 RBC mass of 165ml.
(67%) Calculated Blood Loss Cemented components: 73% of
P=0.001 Standard preventive (ml) patients (79 patients)
measures: Cemented THR:
Patient distribution Surgical Team: All Intervention: 1943906 Oral Iron Supplement
according to patients were operated Control: 2091747 Intervention: 32 (53.3%)
2017 American Medical Association. All rights reserved. 470
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
preoperative Hb on by the same surgical P=0.634 Control: 24 (50%)
levels, team (senior surgeons) Uncemented THR: P=0.338
perioperative Hb and each attending Intervention:
levels, and surgeon performed two 23361015
calculated total operations in each Control: 2347971 Analytical methodology: Chi-
blood loss were no surgical session (1 P=0.966 square or Fishers Exact test for
different in both intervention and 1 qualitative variables. Parametric one-
groups. control) ABT rate, way ANOVA or non-parametric
Preoperative Hb Approach: All patients Total Mann-Whitney for quantitative
(g/dl) were positioned supine Intervention: 15% (n=9) variables.
Cemented THR: and anterolateral Control: 48% (n=23)
Intervention: approach was used to RR:0.31; P=0.001 Other notes: none
14.41.2 the hip. Preoperative Hb13g/dl
Control: 13.61.2 Antimicrobials: surgery RR: 0.32; P=0.003 Follow-up: NR
P=0.067 performed under Preoperative Hb3g/dl Funding Source Conflicts:
Uncemented THR: antimicrobial prophylaxis RR: 1.47; P=0.091 Authors: None
Intervention: Anticoagulant: surgery Age<60yo Institution: None
14.51.6 performed under RR: 0.47; P=0.021 Study: None
Control: 14.61.4 antithrombotic Age60yo Supplies: None
P=0.823 prophylaxis (low RR: 0.17; P=0.027
(note: p<0.05 molecular weight
within control heparin) ABT rate n (%)
group) Analgesia: Postop. Cemented THR:
Procedures: Components: Same Intervention: 1 (8%)
Unilateral Total acetabular and femoral Control: 10 (59%)
Hip Replacement components were used P=0.008
(THR) in all hips. Uncemented THR:
Drains: 2 suction drains Intervention: 8 (17%)
Indications: NR were used in all Control: 13 (42%)
procedures. Removed P=0.013
Setting: 1 Center on POD 2.
Location: Spain Transfusion was Total ABT units
Dates: January indicated when patients Cemented THR:
2005 June 2006 Hb level decreased to Intervention: 2
Inclusion less than 8g/dL or when Control: 20
Criteria: Patients the patient had P=0.017
undergoing THR symptoms of acute Uncemented THR:
anemia (hypotension, Intervention: 13
Exclusion tachycardia, tachypnea, Control: 28
2017 American Medical Association. All rights reserved. 471
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
Criteria: Patients dizziness, fatigue, etc.) P=0.005
with hematological Transfusion Index (ml
diseases or RBC/ transfused patient)
coagulation Allogeneic
disorders, hepatic Overall
or renal diseases, Intervention: 53117
those receiving Control: 371154
anticoagulant P=0.001
therapy or with Cemented THR:
known infection or Intervention: 49129
malignancy. Also, Control: 378142
patients with any P=0.001
other blood-saving Uncemented THR:
strategy (e.g. Intervention: 54118
preoperative Control: 366168
autologous blood P=0.001
donation or Autologous
erythropoietin Cemented THR:
treatment). Intervention: 16377
Control: 0
Uncemented THR:
Intervention: 218153
Control: 0
Overall
Total
Intervention: 263189
Control: 371154
P=0.022
Cemented THR:
Intervention: 212167
Control: 378142
P=0.049
Uncemented THR:
Intervention: 272192
Control: 366168
P=0.001
Reoperations: NR
Length of stay (days):
Intervention: 10.13.1
2017 American Medical Association. All rights reserved. 472
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
Control: 11.67.4
P=0.201
ABT:13.57.9days
No ABT: 9.63.1 days
Difference 3.9 days;
95%CI (1.8-6.0);
P=0.001
Mortality: NR
Adverse events:
DVT
Intervention: 0 (0)
Control: 1 (2%)
Ability to walk (days)
Intervention: 4.61.4
Control: 5.13.4
NoABT:4.41.6 days
ABT: 5.73.5 days
Difference 1.3d; 95%CI
(0.3-2.3) P=0.013
Innerhof- Prospect- To determine that Number of Intervention group: SSI (Follow up- Definitions:
er ive the use of White patients: N=308 Allogeneic (WBC- discharge) Urinary Tract Infection (UTI):
147
2005 concur- Blood Cell (WBC) Preoperative filtered)n=100 Wound infection (total=4 diagnosed by orthopedic surgeon,
(ES) ent filtered blood Autologous Blood (1.2%) established from positive results of
control components Donation (PAD): Allogeneic: 3/100 (3%) microbiologic cultures and clinical
1, 2, 3, 4, should cause n=143 Timing of intervention: No RBC: 1/101 (1.0%) signs of UTI
5, 6, allogeneic No PAD: n=165 Intraoperative and/or Autologous: 0 Pneumonia: when signs of fever,
recipients to No transfusion: postop Both: 0 leukocytosis, and chest infiltrate
exhibit n=101 were observed
postoperative Autologous: n=85 Duration of Wound infection: clinically in the
infection rates Allogeneic, WBC intervention: duration of Other infections: case of purulent secretion and
similar to those of filtered= n=100 transfusion Total infections (UTI, painful erythema.
patients receiving Both, n=22 pneumonia, wound, Purulent Dermatitis (bacterial dermal
autologous blood Patient Agent: all blood purulent dermatitis): infection distinct from operation site):
during elective Characteristics: components produced 22/308 (6.82%) resulting confirmed by positive microbiologic
primary hip or Age: median by hospital in antimicrobial therapy results.
knee arthroplasty (IQR) Autologous or Allogeneic for treatment
using the No RBC: 66y (54- whole blood was Allogeneic: 12/100 Perioperative care: NR
incidence of 73) collected in top and (12%)
postoperative Autologous: 64y bottom bags; citrate No RBC: 7/101 (6.9%) Analytical methodology: Chi-
2017 American Medical Association. All rights reserved. 473
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
infection as an (55-70) phosphate dextrose Autologous: 1/85 (1.2%) square and U test to compare
endpoint Allogeneic: 74y adenine-1 was used as Both: 1/22 (4.6%) baseline data of patients.
(67-78) anticoagulant. WBC P=0.03 Univariate analysis was performed
Both: 72y (65-77) reduction was provided Allogeneic compared for factors associated with
P<0.0001 by pre-storage inline with Autologous postoperative infection and
Gender: f/m WBC filtration of whole transfusions: P=0.0053 transfusion supply.
No RBC: 43/58 blood. Separated RBCs No transfusion Chi-square and Kruskall-Wallis test
Autologous: 44/41 were stored in 100ml of compared with were applied to analyze predictive
Allogeneic: 73/27 saline-ademine-glucose- compared to autologous: factors of infection after allogeneic
Both: 15/7 mannitol additive P=0.06 transfusion.
o
P=0.0001 solution and kept at 4 C Allogeneic + Both: Logistic regression model for
Obesity: BMI and plasma was frozen 10.7% (13/122) evaluating risk factors for
o
No RBC: 28 (25- (to -30 C core temp) Autologous + None: postoperative infection.
31) within 2 hour of 4.3% (8/186)
Autologous: 27 separation. P=0.03 Other notes: As expected, Fresh
(24-30) Autologous blood was Frozen Plasma (FFP) was seldom
Allogeneic: 26 donated by means of **Incidence of infection necessary to correct coagulopathy
(23-29) apheresis, at 400ml of increased significantly (15/308 patients) and
Both: 26 (24-32) RBCs 3-4 weeks before with the number of intraoperatively salvaged blood was
P=0.009 surgery. It was divided transfused allogeneic processed for 44/308 (14%) of
Comorbidities: into 2 units re- WBC-filtered RBCs patients only and therefore was not
Existing Disease suspended in 100ml (p=0.01, data not analyzed further.
(including saline-adenine-glucose- shown)
Coronary artery mannitol each. RBCs Follow-up: Discharge
disease, were not WBC filtered Statistically significant Funding Source Conflicts:
congestive heart and the WBC content Multivariate analysis of Authors: NR
failure, COPD, was 2,000-30,000 variables predicting Institution: NR
Diabetes mellitus, WBCs/L postop infection Study: NR
renal and liver Allogeneic WBC-filtered Supplies: NR
disease, chronic Monitoring RBCs
polyarthritis, intake intervention: NR OR (95%CI): 23.66
of corticosteroids, (1.33-422.06) P=0.02
malignant Control group: n=208
disease) Control1: n=101 Foley catheter (days)
No RBC: 37.6% No RBCs/ no OR (95%CI): 1.23 (1.1-
(n=38) Transfusion 1.4)
Autologous: Control2: n=85 P=0.002
29.4% (n=25) Autologous UTI
Allogeneic: 58% Control 2: n=22 Allogeneic: 7/100
2017 American Medical Association. All rights reserved. 474
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
(n=58) Both Autologous and (7.0%)
Both: 36.4% Allogeneic RBCs No RBC: 5/101 (5.0%)
(n=8) Autologous: 1/85 (1.2%)
P=0.0007 Standard preventive
Hb at admission measures: Both: 0/22
(g/dl): Transfusion trigger: bHb Pneumonia
No RBC: 14.3 levels below 8g/dl and/or Allogeneic: 3/100
(13.7-15.1) physiologic signs of (3.0%)
Autologous: 12.8 anemia No RBC: 0/101
(12.3-13.9) Warming: all patients Autologous: 0/85
Allogeneic: 13.1 were actively warmed
(12.1-13.8) with fluid warmer and a Both: 1/22 (4.5%)
Both: 12.2 (11.4- convective warming Purulent Dermal
12.5) system. infection
P<0.0001 Transfusions: fluid Allogeneic: 0/100
Hb at discharge warmers and 40-m No RBC: 1/101 (1.0%)
(g/dl): blood filters were used Autologous: 0/85
Not significantly AMP: single dose of
different between second-generation Both: 0/22
groups. cephalosporin before
Procedures: incision. Topic-specific
Primary Hip Anticoagulant: outcomes:
Replacement: 189 Enoxaparin administered Total RBCs (units
Primary Knee 12h before operation. transfused):
Replacement: 119 Catheters: all patients Allogeneic: 2 (2-4)
Indications: NR received Foley catheters No RBC: 0
Setting: 1 center on the morning of the Autologous: 2 (1-2)
Location: Austria day of surgery.
Dates: 10 months Non-standard Both: 4 (3-4)
Inclusion preventive measures: P<0.0001
Criteria: Patients Blood Aspiration: blood
undergoing was aspirated into a cell- Shed Blood (ml):
primary hip or saver system and Allogeneic: 500 (300-
knee replacement processed when 700)
surgery appropriate (>1000ml of No RBC: 550 (500-900)
Exclusion blood in the reservoir. Autologous: 500 (450-
Criteria: Any Postoperatively 1000)
infection (including unwashed shed blood
UTI), medical was also re-transfused Both: 500 (300-1000)
2017 American Medical Association. All rights reserved. 475
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
reason for not within 6h P=NS
donating FFP: was only used to Reoperations: NR
autologous blood, treat coagulopathy Length of stay:
surgery for 15/308 (4.9%) With Infection: 16.84.2d
metastatic No Infection: 14.02.1d
process, or P=0.0004
stabilization of Mortality: NR
acute fractures. Adverse events:
Foley Catheter (days)
Allogeneic: 3 (3-4)
No RBC: 3 (2-4)
Autologous: 3 (2-3)
Both: 4 (3-5)
P=0.006
Weber Prospect- To determine the Number of Intervention group: SSI (follow up 6 weeks) Definitions:
149
2005 ive effects of patients: N=444 n=92 Unadjusted results. Wound and urinary tract infections:
(ES) concur- allogeneic blood Received allogeneic Deep Infection defined by the presence of a positive
ent transfusion on Patient blood transfusion. (mean(SEM)) culture. Wounds were examined
control length of hospital Characteristics: Intervention: 1% (10%) daily by orthopedic surgeons who
1, 2, 3, 4 stay in patients mean (SEM) or n Timing of intervention: Control: 1% (8%) were trained to the assessment
undergoing (%) Intraoperative and P=NS protocol but not blinded to
elective total hip Age: years postoperative transfusion.
arthroplasty by Intervention: 64.2 Positive Wound Culture Deep infection: requires joint
examining the (14.5) Duration of (mean(SEM)) involvement
frequency of Control: 63.1 intervention: Intervention: 3.3% Wound-healing disturbance:
allogeneic blood (11.2) Intraoperative with (18%) erythematous inflammation of >1cm,
transfusion, Gender: %male different triggers either Control: 2.0% (14%) wound fluid discharge, purulent
wound-healing Intervention: 13% before or after 4 hours P=NS suture, wound dehiscence, blister, or
disturbances, (34) postop. any degree of wound necrosis.
superficial and Control: 39% (49 Wound Disturbance
deep wound P<0.01 Agent: Packed red (mean(SEM)) Perioperative care: NR
infections, and Obesity blood cells were Intervention: 31% (47%)
length of hospital Height (cm) supplied by local blood Control: 18% (39%) Analytical methodology:
admission. Intervention: 167 bank and consisted of P<0.05 Occurrence of wound disturbance
(8.6) buffy coat-depleted cells, To determine impact of factors in relation to blood
Control: 171 (8.9) mean vol. 320ml, Hb perioperative blood loss, transfusion and other potentially
P<0.05 17.8g/dl, Hct=0.58, and they divided the group related factors were calculated using
9
Weight (kg) Leukocytes 0.4x10 /L into 3 subgroups: logistic regression
2017 American Medical Association. All rights reserved. 476
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
Intervention: 72 Blood loss 1-700mL Risk variables were calculated using
(15.4) Monitoring Blood loss 101-1000mL stepwise conditional backward and
Control: 79 (13.8) intervention: Blood loss >1000mL. forward selection to perform
P<0.001 Info collected For each subgroup they multivariate analysis.
1. At POD 0 - all routine observed essentially the Effect of variables on Length of stay
Comorbidities: clinical postop same proportion in the was calculated with linear regression
Diabetes mellitus assessments, name of incidence of wound analysis. Then log-normalized.
Intervention: 2/92 surgeon, Hb level. disturbances as was
(2.2%) 2. POD1 - blood loss, found for the groups as Other notes: None
Control: 18/352 transfusion data a whole. (Study not
(5.1%)Pulmonary (including units and type powered for this analysis Follow-up: at least 6weeks
disease of blood products given so correlation between postoperatively.
Intervention: 9/92 and Hb before transfusion and wound Funding Source Conflicts:
(9.8%) transfusion) any blood- disturbances did not Authors: NR
Control: 29/352 saving techniques used, reach significance in Institution: NR
(8.2%)Steroids and medications used these subgroups)_ Study: NR
Intervention: 1/92 3. POD4 serum Supplies: NR
(1.1%) prealbumin and pre-
Control: 12/352 transfusion Hb (only if Unadjusted predictors of
(3.4%) transfused) Wound healing
Rheumatoid 4. Discharge blood disturbances: OR
Arthritis loss, transfusion data (95%CI)
Intervention: 6/92 (number of units and Blood Transfusion
(6.5%) type of blood product) OR: 2.1 (1.2-3.5);
Control: 16/352 and length of P=0.03
(4.5%) hospitalization. All other variables not
Procedures: significant
Elective primary Control group: n=352
total hip No transfusion received **Blood transfusion was
arthroplasty also the only significant
Standard preventive variable using
Indications: NR measures: multivariate analysis
All patients received
Setting: 1 hospital standard care acceding Other infections:
to standard protocol by Urinary Tract Infection
Location: The using active body (mean(SEM))
Netherlands warming and so on. Intervention: 3.3%
Therefore, fraction of (18%)
Dates: October inspired oxygen, body Control: 3.7% (19%)
2017 American Medical Association. All rights reserved. 477
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
29, 1998 temperature, and so on P<0.01
October 27, 1999 was comparable
between groups. Topic specific
Inclusion Because of the length of outcomes:
st
Criteria: Patients study period, group of Preop ESR (mm 1 h)
undergoing surgeons was limited Intervention: 18.3 (13.8)
planned elective and their distribution was Control: 14.5 (11.1)
primary total hip comparable between P<0.05
arthroplasty, groups. Preop prealbumin
18yo, living in (mmol/L)
The Netherlands, Non-standard Intervention: 266 (51.4)
or otherwise preventive measures Control: 285 (56.2)
available for follow Transfusion Trigger: P<0.05
up for at least 6 Hb<8.1 g/dl (5.0mmol/l) Preop Hb (mmol/L)
wk. postop during surgery and until Intervention: 8.0 (0.8)
4h postop and Hb<8.9 Control: 8.6 (0.7)
Exclusion g/dl (5.5mmol/l) more P<0.001
Criteria: Any than 4h postop. For Operation time (min)
infection of any patients with Intervention:80 (31.6)
body-system at cardiovascular disease, Control: 71 (19.5)
screening, as all triggers were P<0.05
determined by increased by 0.8g/dl Perioperative blood
symptoms or (0.5mmol/l) loss (mL)
erythrocyte Intervention: 789 (551)
sedimentation rate Gentamycin cement Control: 540 (274)
(ESR)>20mm used (%) (SEM) P<0.001
(unless known to Intervention: 21% (41) Total Blood Loss (mL)
be preexistent); Control: 14% (34) Intervention: 1185 (716)
any blood P=NS Control: 922 (431)
transfusion P<0.001
received within Reoperations: NR
6wk before Length of stay: mean
surgery; and any (SEM) d
other operation Intervention: 12.3 (5.3)
within 6wk preop. Control: 9.8 (3.5)
Also, patients who P<0.001
donated Evaluation to determine
autologous blood if length of stay was
preoperatively. affected by perioperative
2017 American Medical Association. All rights reserved. 478
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
blood loss showed that
duration of
hospitalization was
essentially unaffected by
blood loss and a similar
difference in
hospitalization duration
between transfused and
nontransfused was
maintained among the
subgroups. (Study not
powered to detect
significant differences in
sub-analysis but did
reach significance in
patients who lost more
than 700mL of blood
perioperatively)
Regression model to
predict length of stay
(days) ( (95%CI) (How
much each variable
adds to length of stay)
Age (days per 10yr)
0.9 (0.6-1.2);
P<0.001
Operation time (days per
10 min)
0.2 (0.1-0.4);
P=0.011
Wound disturbance
(days if present)
1.3 (0.4-2.1);
P=0.006
Transfusion (days if
given)
2.2 (1.3-3.1);
P<0.001
Mortality: NR
2017 American Medical Association. All rights reserved. 479
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
Adverse events: NR
Llewelyn Prospect- To conduct a Number of Intervention group: SSI (Follow Up 90 Definitions:
150
2004 ive Pre- two-cohort patients: N=3942 Received Transfusions days) 2 primary outcomes of interest
(ES) Post prospective evaluable n= 2095 Surgical wounds Length of stay and Infections
1, 2, 3, 4, study in patients Total Orthopaedic Length of Stay (LOS): the days
8 undergoing Patient received transfusion: Orthopedic between the operation and discharge
elective coronary Characteristics: 1243 Intervention1: 43/606 form the acute care ward. (Days on
artery bypass using evaluable Intervention1: n=997 (7.1%) intensive care unit and/or high
graft or total hip populations: (Orthopaedic I1 n=606) Intervention2: 32/637 dependency unit plus orthopedic or
and/or knee Transfusions: n= Patients receiving (5.0%) cardiac ward)
replacement Before ULR: n= transfusions before Control1: 31/871 Infections: new suspected and
surgery before 997 mandatory ULR. These (3.6%) proven postop infections for which
and after Ortho before transfusions were Control2: 22/799 antimicrobial s were prescribed
universal n=606 intended to be (2.8%) (excluding topical antimicrobials and
leukoreduction After ULR: unmodified RBC, but antimicrobials given as perioperative
(ULR) to examine n=1098 cohort included patients Proven Infections antimicrobial prophylaxis) plus local
the effects of Ortho after: who received BC-RBC Orthopedic signs and symptoms as follows:
ULR on a large n=637 and/or WBC reduced Intervention1: 50/606 UTI: two or more of following:
group of surgical No Transfusion RBCs ONLY IF they also (8.3%) 1) fever with no other recognized
patients who Before ULR: received at least 2 u Intervention2: 26/637 cause
received n=956 unmodified RBC. (4.1%) 2) urgency
transfusion(s). Ortho before: Intervention2: n=1098 AOR:0.45 (0.28-0.74); 3) frequency
n=871 (Orthopaedic I2 n- p=0.002 4) dysuria
After ULR: n=891 637)Patients receiving Control1: 21/871 Lower Respiratory Tract Infection:
Ortho after: transfusions after (2.4%) LRTI: new or increased production of
o
n=799 mandatory ULR (Full Control2: 29/799 sputum and/or fever (>38 C) with
Age: years cohort2 is WBC reduced (3.6%) appropriate chest signs including
Transfusions: allogeneic RBCs) consolidation and/or chest x-rays
Before Other infections showing new or progressive infiltrate
ULR:68.611.1 Timing of intervention: Wound infections: with purulent
After intraoperative and Lower Respiratory discharge in or exuding from the
ULR:69.210.2 postoperative Infections wound.
No Transfusion Orthopedic Secondary outcomes:
Before ULR: Duration of Intervention1: 21/606 Hospital proven postop infections:
68.010.4 intervention: (3.5%) required clinical symptoms above
After intraoperative and Intervention2: 26/637 leading to antimicrobial prescription
ULR:68.110.3 postoperative (4.1%) PLUS positive microbio culture
Gender: male Control1: 20/871 (except physicians diagnosis of
(%) Agent: (2.3%) pneumonia sufficed as confirmation
2017 American Medical Association. All rights reserved. 480
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
Transfusion: Cohort1: Unmodified Control2: 22/799 of LRTI)
Before ULR: 471 RBCs or unmodified (2.8%) Major non-infectious postop
(47.2%) RBC and RBCs with complications: one or more of the
After ULR: 600 Buffy coat removal (BC- Urinary Tract Infections following: cardiac arrest, infarction,
(54.6%) RBCs), or WBC-reduced Orthopedic renal impairment requiring dialysis,
P = 0.001 RBCs only if they Intervention1: 22/606 confirmed deep vein thrombosis
No Transfusion received at least 2u (3.6%) and/or pulmonary embolism,
Before ULR: 422 unmodified Intervention2: 16/637 respiratory failure, and return to
(44.1%) RBCCohort2: all blood (2.5%) operating room for bleeding from
After ULR: 423 was WBC-reduced Control1: 19/871 surgical wound site.
(47.5%) within 48 hours of (2.0%)
Obesity (weight collection by filtration Control2: 26/799 Perioperative care: NR
(kg)) either of whole blood or (3.3%)
Transfusion: of BC-RBCs. Analytical methodology: 80%
Before ULR: Bacteremia/ Septicemia power and 5% significance, a
75.115.7 Monitoring Orthopedic sample size of 400-500 patients
After ULR: intervention: Intervention1: 3/606 receiving transfusion was adequate
75.714.8 Transfusion recorded. (0.5%) to allow the study to detect an effect
No Transfusion Control group: Intervention2: 1/637 size of 0.125.
Before ULR: No Transfusions n= (0.2%) T-test or chi square.
79.615.6 1847 Control1: 4/871 (0.5%) Binary outcomes required logistic
After ULR: Total Orthopaedic No Control2: 0 regression
80.616.0 Transfusion: n=1670 Time-dependent variables were
Comorbidity (%) Control1: n=956 Other Site Infections analyzed by Cox proportional
Transfusion: Orthopaedic C1 n=871 Orthopedic hazards method
Before ULR: 318 Patients not receiving Intervention1: 17/606
(31.8%) transfusions before (2.8%) Other notes: Data were collected by
After ULR: 341 mandatory ULR Intervention2: 13/637 research nurses or audit staff by
(31.1%) Control2: n=891 (2.0%) review of hospital notes and
No Transfusion Orthopaedic C2:n=799 Control1: 13/871 computer information systems after
Before ULR: 309 Patients not receiving (1.5%) the patients discharge.
(32.3%) transfusions with Control2: 13/799
After ULR: 249 leukocyte reduction (1.6%) Follow-up: 90 days after discharge
(28.0%) (after mandatory ULR) Funding Source Conflicts:
Infection (%) Topic-specific Authors: None
Transfusion: Standard preventive outcomes Institution: None
Before ULR: 65 measures Drain Losses (mL) Study: None
(6.5%) Non-standard Unchanged in Supplies: None
After ULR: 45 preventive measures: orthopaedic patients
2017 American Medical Association. All rights reserved. 481
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
(4.1%) Transfusion Triggers; who received
P=0.013 Each hospital followed transfusions vs. those
No Transfusion its own transfusion who did not
Before ULR: 29 protocols Lowest Hb Level (g/dL)
(3.0%) Data not stratified by
After ULR: 32 procedure type
(3.6%) Discharge Hb level
Hb level (g/dl) (g/dL)
Transfusion: Data not stratified by
Before ULR: procedure type
13.21.4
After ULR: Subgroup analysis: of
13.31.4 storage age and dose of
No Transfusion blood on primary
Before ULR: outcomes before and
13.7151.2 after ULR (including
After ULR: postop infections, and
13.81.2 postop LOS) found no
Procedures: Non- statistically significant
emergent comparisons.
Coronary Artery
Bypass Grafting TRANSFUSION DATA
(CABG) and Number RBC
elective total hip units/patient
replacement and/
or total knee Orthopedic
replacement Before ULR: 2.71.5
(Primary and After ULR: 2.92.0
revisions) P=0.115
Primary Number of patients (%)
Procedure: receiving THIS IS
Orthopedic CABG+ORTHO
Procedures 1 unit of RBCs
Redoes (includes Before ULR: 114/997
bilateral and THR (11.4%)
plus TKR) After ULR: 78/1098
Transfusion: (7.1%)
Before ULR: 145 2-3 units of RBCs
(23.9%) Before ULR: 476/997
2017 American Medical Association. All rights reserved. 482
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
After ULR: 129 (47.7%)
(20.2%) After ULR: 540/1098
P=0.118 (49.2%)
No Transfusion >3 units RBCs
Before ULR: 58 Before ULR: 407/997
(6.7%) (40.8%)
After ULR: 26 After ULR: 480/1098
(3.3%) (43.7%)
P=0.001 P=0.003
TKR (%) FFP/cryoprecipitate
Transfusion: Before ULR: 84/997
Before ULR: 194 (8.4%)
(32.0%) After ULR: 108/1098
After ULR: 242 (12.1%)
(38.0%) P=0.008
P=0.027 PLTs
No Transfusion Before ULR: 75/997
Before ULR: 443 (7.5%)
(50.9%) After ULR: 110/1098
After ULR: 408 (12.3%)
(51.1%) P=0.0004
P=0.934
Indications: Reoperations: NR
variable
Setting: Length of stay: postop
Multicenter (CABG LOS: mean (SD) days
at 4 hospitals and Received Transfusions
Arthroplasty at 7 Orthopedic
hospitals) Before ULR: 2.81.56
Location: After ULR: 3.32.98
England AR 1.16 (1.04-1.30);
Dates: p=0.010
Cohort1 (pre- No Transfusions
ULR): Began Orthopedic
January May Before ULR: 8.33.4
1999 and After ULR: 7.93.8
continued until AR 1.11 (1.00-1.22);
enough patients p=0.042
were recruited
2017 American Medical Association. All rights reserved. 483
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
(approx. 5 Mortality (in hospital
months) and up to 90 days after
Cohort2 (Post discharge home):
ULR): Began
January May Orthopedic
2000 and Intervention1: 7/606
continued until (1.2%)
enough patients Intervention2: 7/637
were recruited (1.1%)
(approx. 5 Control1: 5/871 (0.6%)
months) Control2: 3/799 (0.4%)
Inclusion Adverse events:
Criteria: CABG Major Complications
patients Orthopedic
undergoing Intervention1: 40/606
nonemergency, (6.6%)
whether primary or Intervention2: 39/637
redo procedures, (6.1%)
with or without AOR: 0.85 (0.28-2.61);
aortic or mitral P=0.775
valve replacement Control1: 34/871
or (3.9%)
endarterectomy. Control2: 15/799
Orthopedic (1.9%)
patients AOR: 0.44 (0.24-0.82);
undergoing p=0.010
elective THR or
TKR whether
primary or redo
operations.
Bilateral
procedures were
included if
performed during
the same
operation
Exclusion
Criteria: Patients
receiving
2017 American Medical Association. All rights reserved. 484
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
previously
donated
autologous
transfusions
Cohort1: patients
receiving BR-RBC
& WBC-reduced
transfusions
unless they had
also received at
least 2 units of
unmodified RBCs.
Rosenc- Prospect- To examine Number of Intervention group: SSI (Follow up Definitions:
her ive blood patients: N=3996 Received discharge from Infection: Determination of infection
148
2003 Concurr- management Transfusions: 2762 Surgery Department) was made using physical clinical
(ES) ent practices before, Patient Allogeneic Only Unadjusted: judgment.
Cohort during and after Characteristics (WBC filtration) Overall wound infection Overall Infection Rates: includes
1, 3, 4, 5 elective total Age meanSD =1024/2762 (37%) rate: 81/3996 (2%) wound infections, urinary tract
knee and total hip 6911.2 years Autologous Only Allogeneic-only: 36/999 infection, respiratory tract infection,
arthroplasties in Allogeneic-only: =1393/2762 (50%) (4%) septicemia, and other infections
Europe (including 7110.7 Autologous Blood Autologous-only: Estimated blood Loss: Physicians
revisions and Autologous-only: Donation (ABD) = 11/1311 (1%) estimates of EBL were recorded
(1) = 19.26; p<0.001
2
bilateral 6611.6 1290/1393 (93%) before the surgery.
procedures) and P<0.001 Acute Normovolemic (allogeneic only vs. Baseline Hb level: Hb level collected
to determine Gender: m/f Hemodilution=82/1393 autologous only) during the assessment office visit
factors predictive 1393/2431 (sex (6%) Allogeneic & when the surgery was planned -
of the risk data missing for Cell saver=329 Autologous: 8/329 (2%) 217 days before surgery.
associated with 172 patients) Postop salvage=264 No Transfusion: 22/1180
allogeneic Obesity: NR Allogeneic and (2%) Perioperative care: NR
transfusion. Comorbidities: Autologous: ABD Transfusions only:
Factors Hypertension: n=345/2762 (13%) 4/615 (1%) Analytical methodology: Logistic
examined 1631 (41%) Allogeneic Transfusion regression was used for modeling
included blood Coronary Artery Timing of intervention: WBC-Depleted: the probability of transfusion based
wastage; pre- Disease: 469 Intraoperative/postopera 18/637 (3%) on selected predictor variables.
and (12%) tive Not WBC-Depleted: Otherwise, descriptive statistics or
postoperative Hb Significant 18/464 (4%) Parametric and nonparametric
evolution; differences Duration of No statistically statistical tests after consideration of
transfusion between intervention: significant difference distributional characteristics and
associated transfusion Intraoperative/postopera between WBC depleted statistical test assumptions were
2017 American Medical Association. All rights reserved. 485
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
complications; method groups: tive and non WBC depleted utilized.
(3)=13.82;
2
and predictors of allogeneic transfusions
allogeneic P<0.001 Device/agent: Other notes: The tables and data
transfusion. Diabetes: 382 Transfused blood Knee Patients only were not uniformly presented.
(10%) ABD only: 0/148 Numbers & % were frequently
COPD: 317 (8%) Monitoring Postop salvage only: mislabeled leading to problems
Rheumatic: 149 intervention: 5/122 (4%) interpreting the data. Missing data
(1) = 5.97; p<0.05
2
(4%) CRF=case report forms from every table resulted in
Significant were utilized to report, (Knee ABD vs. Postop apparent discrepancies in the
differences scan then analyze the Salvage) counts adding to the problem of
between perioperative data Hip Patients Only interpretation.
transfusion including transfusion ABD only: 4/462 (1%)
method groups: type and amount. Postop salvage only: Follow-up: Until discharge from
(3)=13.29;
2
3/69 (4%) Surgery Department
(1) = 5.60; p<0.05
2
P<0.001 Control group: n=1234 Funding Source Conflicts:
Hematologic: 106 No transfusions (Hip ABD vs. Postop Authors: NR
(3%) Salvage) Institution: NR
Standard preventive Study: NR
Procedures: measures: NR Overall Infection Rates: Supplies: NR
Elective total hip Allogeneic-only: 110/999
and total knee (11%)
arthroplasties. Autologous-only:
Primary unilateral 93/1311 (7%)
hip: 2027 (51%) Allogeneic &
Primary bilateral Autologous: 30/329 (9%)
hip: 27 (1%) No Transfusion: 94/1180
Primary unilateral (8%)
knee: 1036 (26%) ABD transfusion only:
Primary bilateral 25/615 (4%)
knee: 13 (0%) Allogeneic Transfusion
Hip revision: 292 WBC-Depleted:
(7%) 82/637 (13%)
Knee revision: 69 Not WBC-Depleted:
(2%) 42/464 (9%)
Knee Patients only
Indications: ABD only: 6/148(4%)
Variable Postop salvage only:
13/122 (11%)
Setting: 225 Hip Patients Only
2017 American Medical Association. All rights reserved. 486
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
Centers ABD only: 19/462 (4%)
Postop salvage only:
Location: Europe 12/69 (17%)
--France,
Germany, Greece, Other infections: SEE
Italy, the ABOVE
Netherlands, and Topic-specific
Spain outcomes:
Donated Blood: n=
Dates: NR Baseline Hb Level was
linearly regressed with
Inclusion the probability of
Criteria: All allogeneic transfusion:
patients WOMEN:
undergoing total Base Hb level of 8.0 =
hip or total knee 75% prob of transfusion
replacement. Base Hb level of
Enrollment of 16.0=12% prob of
consecutive transfusion
patients was MEN:
requested with a Base Hb level of 8.0 =
limit of 20 patients 70% prob of transfusion
per center. Base Hb level of
16.0=8% prob of
Exclusion transfusion
Criteria: NR
Reoperations: NR
Length of stay: days
Allogeneic: 13.08.1
Autologous: 12.310.5
Autologous-only
collected via ABD
method: 11.97.7
and No transfusion:
10.712.3
vs. Allogeneic
(allogeneic only or
allogeneic and
2017 American Medical Association. All rights reserved. 487
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
autologous): 13.510.2
P<0.001
Mortality: NR
Adverse events:
Fluid volume overload:
Ranged from 3-4%
across transfusion
methods: NS
Suspected Clinical DVT:
Ranged from 2-3%
across transfusion
methods including no
transfusion. NS
Transfusion Reactions:
Recorded not reported
Borghi Prospect- To evaluate the Number of Intervention group: n= SSI (follow up: Definitions
153
2000 ive incidence and patients N=2884 278 discharge from Perioperative care:
(ES) concur- risk factors for Patient Patients receiving orthopedic ward) MSBOS: the actual number of blood
ent allogeneic blood Characteristics allogeneic concentrated All infection data was units transfused in 90% of patients
control transfusion (after Age: (meanSD) red blood cell (ARBC) presented in bar graph receiving one individual surgical
1, 2, 3, 4, autologous blood years transfusions after all form. The below procedure.
5, 8 transfusion) in THA: 6112 autologous blood (both numbers are Anesthesia: either balanced general,
patients TKA: 688 pre-donations and blood percentages inferred. regional or integrated
scheduled for HR: 6411 recovered intra and epidural/general anesthesia. The
primary hip, Gender m/f postoperatively. Statistical Significance type was freely decided by the
primary knee or THA: 726/1290 Timing of intervention of difference between attending anesthesiologist with no
revision hip TKA: 125/355 Duration of ARBC PLUS randomization.
arthroplasties HR: 124/264 intervention Autologous and No Analytical methodology:
and receiving an Obesity Agent: ARBC across each Continuous variables: Analysis of
aggressive Weight (kg) Autologous Blood group is as follows variance
autotransfusion THA: 6811 Collected: According to GROUP THA: p=0.0005 Post hoc comparisons: Tukeys test
regimen TKA: 7010 the Maximum surgery GROUP TKA: p=0.008 and students t-test with Bonferronis
HR: 6810 blood order on GROUP HR: p=0.005 correction.
Categorical variables: -square or
2
Height (cm) Schedule, 2 units of pre- Infection:
THA: 1629 donated blood were THA: Fishers exact test. Multivariate
TKA: 1608 collected for THA and ARBC plus autologous: analysis of variance for repeated
HR: 1618 TKA and 3 units for 1% measures with Wilks -test for
2017 American Medical Association. All rights reserved. 488
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
Comorbidities: Revision of Hip No ARBC: 0.5% changes over time
NR Arthroplasty. Autologous TKA: After univariate analysis, partial risk
Duration of blood was separated ARBC plus autologous: factors associated with the response
Surgery (min) into RBC and FFP. FFP 2% were further evaluated by multiple
THA: 11538 re-infused at end of No ARBC: 0.5% logistic regression analyses.
TKA: 11744 surgery or within 24h; HR: Other notes: None
HR: 18364 pre-donated RBCs ARBC plus autologous: Follow-up: Discharge from
P (THA vs. transfused during 3d 1% orthopedic ward
HR)=0.0005 postop. No ARBC: 0.5% Funding Source Conflicts:
P (TKA vs. Monitoring Authors: None
HR)=0.0005 intervention: NR Wound Hematoma Institution: None
Control group: n=2606 THA: Study: None
Procedures: Patients receiving ARBC plus autologous: Supplies: None
Total hip autologous blood 11%
arthroplasty: transfusion (pre- No ARBC: 2%
2016/2884 donation separated into TKA:
(69.9%) RBC and FFP) plus ARBC plus autologous:
Total knee intraoperative re-infused 11%
arthroplasty: cell-salvage and No ARBC: 5%
480/2884 (16.6%) postoperative closed HR:
Hip revision of system drain(see details ARBC plus autologous:
arthroplasty: below) 8%
388/2884 (13.5%) Standard preventive No ARBC: 2%
Indications: measures
variable Iron Supplement: during Other infections: NR
Setting: 1 each pre-donation of Topic-specific
orthopedic autologous blood and outcomes:
institute the first 4 POD, all Perioperative Blood
Location: Italy patients received Losses (ml)
Dates: NR (5 year intravenous iron THA: 1190480
period) (200mg/day) TKA: 1280403
Inclusion Perioperative Blood HR: 1720460
Criteria: Patients Return: P (THA vs. HR)=0.0005
undergoing Total Intraoperatively, P (TKA vs. HR)=0.0005
Hip Arthroplasty uncoagulated blood was
(THA) Total Knee collected from wound Intraoperative Blood
Arthroplasty (TKA) into a reservoir using an recovery (ml)
or Hip Revision of aspirator and collection THA: 267168
Arthroplasty (HR) bag connected to the TKA: 16292
2017 American Medical Association. All rights reserved. 489
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
Exclusion inferior edge of the HR: 524387
Criteria: NR surgical wound in order P (THA vs. TKA)=0.0005
to concentrate, wash P (THA vs. HR)=0.0005
and infuse red cells. P (TKA vs. HR)=0.0005
These were immediately
returned to the patient. Postoperative Blood
Postoperatively, recovery (ml)
uncoagulated blood lost THA: 387237
from the surgical wound TKA: 541294
was monitored and HR: 465287
collected using a closed P (THA vs. TKA)=0.0005
recovery system P (THA vs. HR)=0.0005
connected to the P (TKA vs. HR)=0.0005
surgical drains. If blood
losses exceeded 200ml Patients receiving ABRC
st
during 1 8h postop, the plus autologous
units of fresh frozen Transfusion
plasma were re-infused THA: 159 (8%)
at the end or within the TKA: 43 (9%)
first 24h of surgery. HR: 76 (20%)
Autologous P (THA vs. HR)=0.0005
Transfusion Trigger: if P (TKA vs. HR)=0.0005
Hb <11g/dl (number of patients
Allogeneic receiving ABRC
concentrated Red transfusions was not
Blood cells significantly different
Transfusion Trigger: across anesthesia types
presence of for each surgery type)
asymptomatic anemia
(vertigo, dizziness, Hb concentration:
postural hypotension, Baseline Hb
headache, insomnia, concentration was
confusion, tachycardia, significantly lower for HR
angina, dyspnea) or than for THR and TKR at
st rd
when Hb<6g/dl (10g/dl 1 and 3
in patients with POD(p<0.0005 vs. THA
cerebrovascular or & P<0.001 vs. TKA)
coronary artery disease)
Main Risk factors
2017 American Medical Association. All rights reserved. 490
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
associated with An
increased incidence of
Perioperative transfusion
of Allogeneic blood:
Preoperative Hb<10g/dl:
OR: 8.8 (6.5-16.8);
p=0.004
Hip Revision
Arthroplasty
OR: 5.8 (3.9-8.5);
p=0.0001
No MSBOS pre-
donation:
OR: 3.4 (2.7-4.1); p-
0.0001
Reoperations: NR
Length of stay:
Patient Discharge (days
after Surgery)
THA: 125
TKA: 166
HR: 157
P (THA vs. TKA)=0.0005
P (THA vs.
THR)=0.0005
Patients not receiving
ARBCs log-rank curve
showed significantly
shorter durations of stay
than the log-rank curve
for patients receiving
ARBC plus autologous
transfusion (p=0.0005)
Mortality: NR
Adverse events:
No severe adverse
2017 American Medical Association. All rights reserved. 491
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
effects were reported
during either
preoperative collection
of autologous blood or iv
iron administration
Statistical Significance
of difference between
ARBC plus autologous
blood and No ARBC
across each group is
as follows
GROUP THA: p=0.0005
GROUP TKA: p=0.008
GROUP HR: p=0.005
Dysrhythmia
THA:
ARBC plus autologous:
3%
No ARBC: 0.5%
TKA:
ARBC plus
autologous:9%
No ARBC: 1%
HR:
ARBC plus autologous:
7%
No ARBC: 1.5%
Respiratory Failure
THA:
ARBC plus autologous:
2%
No ARBC: 0.5%
TKA:
ARBC plus autologous:
0
No ARBC: 1%
2017 American Medical Association. All rights reserved. 492
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
HR:
ARBC plus autologous:
4%
No ARBC: 1%
Myocardial Ischemia
THA:
ARBC plus autologous:
6%
No ARBC: 0.5%
TKA:
ARBC plus autologous:
0
No ARBC: 0.5%
HR:
ARBC plus autologous:
4%
No ARBC: 0.5%
Pulmonary Embolism
THA:
ARBC plus autologous:
1%
No ARBC: 0.5%
TKA:
ARBC plus autologous:
2%
No ARBC: 0
HR:
ARBC plus autologous:
5%
No ARBC: 0.5%
Deep Vein Thrombosis
THA:
ARBC plus autologous:
0.4%
No ARBC: 0.5%
TKA:
2017 American Medical Association. All rights reserved. 493
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Population and
Risk of Study Objective Intervention Results Comments
(Data Setting (N)
Bias
Extractor)
Score
ARBC: 2%
No ARBC: 1.5%
HR:
ARBC plus autologous:
0%
No ARBC: 0.5%
Q11C. How does the volume of transfused blood product impact the risk of SSI? Our search did not identify data that evaluated differences in the
volume of transfused blood product and their impact on the risk of SSI in prosthetic joint arthroplasty patients.
Q11D. How safe and effective is withholding blood transfusion to reduce the risk of SSI? Our search did not identify data that both evaluated the
safety and effectiveness of withholding blood transfusions and its impact on the risk of SSI in prosthetic joint arthroplasty patients.
2017 American Medical Association. All rights reserved. 494
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.2A3. RISK OF BIAS ASSESSMENTS OF STUDIES: Q 11 BLOOD TRANSFUSION
eTABLE 56. Risk of Bias Assessments of Randomized Controlled Trials for Q11 Blood Transfusion
Funding
Attrition source(s)
Described Randomizati- Describe- smaller than disclosed and
as on d as Outcome Study 10-15% of Attrition no obvious Overall
Author randomiz- appropriately double- assessor participant Investiga- Attrition assigned appropriate- conflict of Risk of
Year Q ed performed blind blinded blinded tor blinded described patients ly analyzed interest Bias
Question 11: Blood Transfusion
Frietsch
145 11 Low
2008
Frietsch
146 11 Low
2001
eTABLE 57. Risk of Bias Assessments of Other Controlled Studies for Q11 Blood Transfusion
Attrition not Statistical Funding
All study groups significantly Investigator Potential adjustment for source(s)
derived from similar different Measure of Measure of blinded to confounde- potential disclosed and no Overall
Author source/reference across study exposure is outcome is endpoint rs confounders obvious conflict Risk of
Year Q populations groups valid valid assessment identified done of interest Bias
Question 11: Blood Transfusion
Borghi
153 11 Low
2000
Del Trujillo
152 11 Low
2008
Innerhofer
147 11 Low
2005
Llewelyn
150 11 Low
2004
Pedersen
151 11 Low
2009
Rosencher Moder-
148 11
2003 ate
Weber Moder-
149 11
2005 ate
2017 American Medical Association. All rights reserved. 495
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.2B. Q12-16 SYSTEMIC IMMUNOSUPPRESSIVE THERAPY
2.2B.1 GRADE TABLE: Q12-16 SYSTEMIC IMMUNOSUPPRESSIVE THERAPY
eTABLE 58. GRADE Table for Q12-16 Systemic Immunosuppressive Therapy
Increase
Decrease GRADE
GRADE
Large Magnitude
Overall
Publication Bias
Quantity GRADE of
Dose-response
GRADE
Study Quality
and Type Starting Evidence
Confounders
Consistency
Comparison Outcome Findings of
Directness
of GRADE for
Evidence
Precision
Evidence Outcome
Base
Systemic Immunosuppressive Therapy: Biologic Agents (Non-Tumor Necrosis Factors [TNF] and Anti-TNFs) and Disease Modifying Antirheumatic Drugs-
(DMARD)
Q12. How does systemic corticosteroid or other immunosuppressive therapy impact the risk of SSI in prosthetic joint arthroplasty patients?
Q12A. Does the type of agent impact the risk of SSI?
In meta-analysis of 2 OBS studies (N=528) ,
biologic agents were associated with a
higher risk for SSI: OR: 5.90 (2.68 12.99);
2 OBS 2
SSI* 154,155 p<0.01; I =0 Low 0 0 0 0 0 0 +1 0 Moderate
In each of these studies
154,155
multivariate
logistic regression analysis identified biologic
agents as a significant risk factor SSI.
In a meta-analysis of 2 OBS (N=528),
biologic agents were not associated with a
higher risk for PJI: OR: 3.59 (0.52 24.88);
Biologic- 2
p=0.20; I =0
agents
In one study , 3 (0.7%) total organ/space
154
2 OBS
(non-TNF PJI* 154,155 Low 0 0 0 -1 0 0 0 0 Very Low
SSIs among 420 RA patients undergoing Very
and anti-
THA or TKA: 1/48 (2.08%) vs. 2/372 (0.54%); Low
TNF)
p=0.27
vs.
In the other study , 1/54 (1.85%) vs. 0/54
155
DMARDs
(0%); p=0.50
In a meta-analysis of 2OBS (N=528), biologic
agents associated with increased risk for
superficial SSI OR: 5.80 (2.55 13.18);
2
p<0.01; I =0
Superfic- 2 OBS
1 OBS study = 24 (5.7%) total superficial
154
154,155 Low 0 0 0 0 0 +1 0 0 Moderate
ial SSI*
SSIs among 420 RA patients undergoing
THA or TKA: 9/48 (18.75%) vs. 15/372
(4.03%); p<0.01
1 OBS Study = 7/54 (12.96%) vs. 1/54
155
2017 American Medical Association. All rights reserved. 496
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Overall
Publication Bias
Quantity GRADE of
Dose-response
GRADE
Study Quality
and Type Starting Evidence
Confounders
Consistency
Comparison Outcome Findings of
Directness
of GRADE for
Evidence
Precision
Evidence Outcome
Base
(1.85%); p=0.06
1 small study (N= 113): 2/39 (5.1%) vs. 5/74
(6.8%); OR 0.7459 (0.14-4.03); p=1.00
(results include 4 ankle fusions)
Adverse
No difference on subanalysis (30 THAs and
events of 156
1 OBS 65 TKAs- THA: none in either group; TKA: Low 0 0 0 -1 0 0 0 0 Very Low
surgical
4/51 (7.8%) vs. 1/14 (7.1%); OR 0.90 (0.09-
wounds
8.80). 92.3% of all patients on biologic
agents (infliximab and etanercept) were also
on methotrexate (DMARD).
1 small (N=90) retrospective 1:1 pair-
matched case-control study of deep venous
thrombosis (DVT) in joint arthroplasty (96%)
Adverse
and other joint procedures (4%): increased
events- 155
1 OBS incidence of DVT with biologic agents 23/45 Low 0 0 0 -1 0 0 0 0 Very Low
drug
(51%) vs. 12/45 (26%); p=0.02.
related
On multivariate logistic regression analysis
biologic agents (anti-TNF) were the only risk
factor for DVT: OR 2.83 (1.10-7.25); p=0.03
No difference in 1 study (N=202) total joint
replacements in RA patients: 3/92 (3.26%)
157 vs. 2/110 (1.81%); p=0.66 at 6m follow-up
PJI* 1 OBS Low 0 0 0 -1 0 0 0 0 Very Low
Revision total joint replacements: 1/9
DMARD: (11.1%) vs. 0/16; p=0.26
methotrex- Bilateral TKA: 0/3 vs. 1/11 (9.09%); p=1.00
ate vs. Very
Deep
No 157 No difference: 0/92 vs. 1/110 (0.91%); Low
DMARD wound 1 OBS Low 0 0 0 -1 0 0 0 0 Very Low
p=0.57
therapy abscess*
Infected No difference: 2/92 (2.2%) vs. 1/110 (0.9%);
157
Hemat- 1 OBS p=0.47 Low 0 0 0 -1 0 0 0 0 Very Low
oma* Bilateral TKA 1/3 (33%) vs. 0/11; p=0.14
2017 American Medical Association. All rights reserved. 497
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Overall
Publication Bias
Quantity GRADE of
Dose-response
GRADE
Study Quality
and Type Starting Evidence
Confounders
Consistency
Comparison Outcome Findings of
Directness
of GRADE for
Evidence
Precision
Evidence Outcome
Base
Necrotic 157 No difference: 2/92 (2.17%) vs. 0/110;
1 OBS Low 0 0 0 -1 0 0 0 0 Very Low
eschar p=0.24
Serous 157 No difference: 1/92 (1.09%) vs. 1/110
1 OBS Low 0 0 0 -1 0 0 0 0 Very Low
drainage (0.91%)
Q12B. Does the preoperative duration of the therapy impact the risk of SSI?
154
In a study comparing RA patients on
biologics (anti-TNF) and DMARDs
undergoing arthroplasty surgery, multivariate
logistic regression analysis comparing
infected to non-infected patients showed
years of disease duration was a risk factors
for SSI: OR 1.09 (1.04-1.14); p<0.01.
154
Disease duration for the cohort was a
Disease 2 OBS
SSI* 154,155 median of 14.5 years (interquartile range 8.9- Low 0 0 0 0 0 0 0 0 Low Low
duration
21) but these results were not stratified by
biologic agents vs. DMARDs.
155
In a study comparing RA patients on
biologic (anti-TNF) and DMARDs undergoing
arthroplasty surgery multivariate logistic
regression analysis also suggested disease
duration as a risk factor for SSI: OR 1.17
(1.03-1.33); p=0.02.
Q12C. Does the agent dose impact the risk of SSI?
In a retrospective 1:1 matched pair case
Biologic- 155
control study 64 rheumatoid arthritis
agents
patients on biologic agents (anti-TNF) were
(anti-Tumor 2 OBS Very
155,154 matched to 64 patients on DMARDs. 0 -1 0 0 0 0 0 0 Very Low
necrosis SSI* Low Low
Patients in the biologic agent (anti-TNF)
factors) vs.
group were on significantly higher daily
DMARDs
doses of prednisone (5mg/day; range 2-7)
2017 American Medical Association. All rights reserved. 498
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Overall
Publication Bias
Quantity GRADE of
Dose-response
GRADE
Study Quality
and Type Starting Evidence
Confounders
Consistency
Comparison Outcome Findings of
Directness
of GRADE for
Evidence
Precision
Evidence Outcome
Base
than the DMARD patients (3mg/day, range 0-
5); p<0.01. Multivariate logistic regression
analysis showed that prednisone dose OR
1.43 (1.01-2.04); p=0.05 was a risk factor for
SSI.
In a retrospective study of 420 THAs and
154
TKAs in RA patients, multivariate logistic
regression analysis comparing infected to
non-infected patients did not show
prednisone dose to be a risk factor for SSI.
Both patients with SSI (n=27) and those
without SSI (n=393) were on prednisone
doses of 3mg/day, (range 0-5); p=0.27.
Results were not stratified by biologic agents
vs. DMARDs.
Q13. What are the most effective strategies in managing systemic corticosteroids or other immunosuppressive therapy perioperatively to reduce the risk of
SSI in prosthetic joint arthroplasty patients?
Q13A. How safe and effective is the discontinuation of these agents preoperatively and when should they be resumed?
In a meta-analysis (N=180) of 3 small
observational studies, the data suggests that
stopping methotrexate is associated with
lower risk for PJI, but the result is not
DMARD: significant (OR: 0.20 (0.04 1.03); p=0.05;
2
Methotrex- I =0
1 small OBS study , overall SSI: 3/41
159
ate
4 OBS
stopped vs. 157-160 (7.3%)
PJI* Low 0 0 0 0 0 0 0 0 Low Low
1 OBS study , no difference: 0/26 y
159
continued
perioperat- vs.3/15; p=0.08. 1y follow up. Methotrexate 2
ively weeks perioperatively
In each of these studies - No difference:
157
1/47 (2.1%) vs. 2/45 (4.44%); p=0.54; 6m
follow up. Methotrexate stopped indefinitely
No difference in one small (N=47) study :
158
0/32 vs.1 /15 (6.67%); p=0.25. No PJIs
2017 American Medical Association. All rights reserved. 499
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Overall
Publication Bias
Quantity GRADE of
Dose-response
GRADE
Study Quality
and Type Starting Evidence
Confounders
Consistency
Comparison Outcome Findings of
Directness
of GRADE for
Evidence
Precision
Evidence Outcome
Base
reported among 32 patients who stopped
methotrexate therapy 4 or more weeks
preoperatively as compared to 1 among the
15 patients who were one methotrexate
within 4 weeks of surgery:
160
In 1 OBS study (N=462) in RA patients
undergoing 657 THAs and TKAs, patients
were receiving at least 1 DMARD within 3
months of surgery in 336 of those 657
procedures. DMARD therapy was withheld in
192/336 (57%) of these procedures.
Stopping DMARD therapy at the time of
surgery lowered the risk of subsequent PJI:
OR 0.65 (0.09-4.95) but this was not
statistically significant.
No patient in either group experienced a
159
RA Flare 1 OBS postoperative flare of their rheumatoid Low 0 0 0 -1 0 0 0 0 Very Low
arthritis
Infected
157
Hemato- 1 OBS No difference: 2/47 (4.25%) vs. 0/45; p=0.30 Low 0 0 0 -1 0 0 0 0 Very Low
ma
Necrotic 157
1 OBS No difference: 2/47 (4.25%) vs. 0/45; p=0.30 Low 0 0 0 -1 0 0 0 0 Very Low
eschar
Non-
commun-
157
icating 1 OBS No difference: 0/47 vs. 1/45 (2.22%);p=0.48 Low 0 0 0 -1 0 0 0 0 Very Low
serous
drainage
Biologic Subanalysis of 50/462 RA patients on
160 Very
agent: Anti- PJI* 1 OBS biologic agent (anti-TNF) therapy Low 0 0 0 -1 0 0 0 0 Very Low
Low
tumor (etanercept, adalimumab, infliximab, or
2017 American Medical Association. All rights reserved. 500
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Overall
Publication Bias
Quantity GRADE of
Dose-response
GRADE
Study Quality
and Type Starting Evidence
Confounders
Consistency
Comparison Outcome Findings of
Directness
of GRADE for
Evidence
Precision
Evidence Outcome
Base
necrosis anakinra) who underwent hip or knee
factor (anti- arthroplasties, suggested an increase in
TNF): incidence of PJIs among those in whom anti-
Stopped TNF therapy was continued perioperatively,
vs. but the findings were not statistically
continued significant: 0/12 (0%) vs. 3/38 (7.9%).
perioperat-
ively
Q13B. Should the agent dose be adjusted, and if so, for how long? Our search did not identify data that evaluated perioperative immunosuppressive therapy dose
adjustment and its impact on the risk of SSI in prosthetic joint arthroplasty patients.
Q14. What is the optimal duration of postoperative AMP to reduce the risk of SSI in prosthetic joint arthroplasty patients who are on systemic corticosteroid
or other immunosuppressive therapy? Our search did not identify data that specifically evaluated differences in duration of postoperative AMP in prosthetic joint
arthroplasty patients who were on systemic corticosteroids or other immunosuppressive agents and its impact on the risk of SSI. However, multiple procedures examined
in the Core section, Q1.E: Postoperative AMP duration that included patients on immunosuppressive therapy showed no benefit of continuing AMP after closing the
surgical incision in the operating room. Therefore, the broader recommendation for duration of postoperative AMP should be applied to prosthetic joint arthroplasty
procedures irrespective of use if systemic corticosteroid or other immunosuppressive therapy.
Intra-articular Corticosteroid Injections
Q15. How do preoperative intra-articular corticosteroid injections impact the risk of SSI in prosthetic joint arthroplasty patients?
History of
corticoster-
161- Meta-analysis (N=1146) 5 OBS studies; OR:
oid 5 OBS 2
SSI* 165 1.91 (1.01 3.61); p=0.05; I =13% Low 0 0 0 0 0 0 0 0 Low Low
Injection
35/476 (7.4%) vs. 26/670 (3.9%)
vs.
no injection
In a meta-analysis of 2 studies (N=414), no
2 OBS
SSI* 161,162 difference between groups OR: 1.89 (0.53 Low 0 0 0 -1 0 0 0 0 Very Low
2
6.76); p=0.33; I =50%
TKA:
Injection In a meta-analysis of 2 studies (N=414), no Very
vs. No difference between groups OR: 12.30 (0.62 Low
Injection 2 OBS 242.88); p=0.10
PJI* 161,162 Low 0 -1 0 -1 0 0 0 0 Very Low
161
1 study (N=144) reported significant risk of
PJI for TKA patients injected prior to surgery:
3/54 (5.6%) vs. 0/90 (0%); p<0.03 at 1yr
2017 American Medical Association. All rights reserved. 501
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Overall
Publication Bias
Quantity GRADE of
Dose-response
GRADE
Study Quality
and Type Starting Evidence
Confounders
Consistency
Comparison Outcome Findings of
Directness
of GRADE for
Evidence
Precision
Evidence Outcome
Base
follow up. All 3 had received a steroid
injection within 11mo of surgery; mean
(range): 9.6mo (8-11)
162
One study (N=270) matched 90 injected
patients to 180 patients not injected prior to
TKA and reported no infections in either
group at 1 year follow up: 0/90 vs. 0/180.
Half were injected within 1yr prior to surgery.
In a meta-analysis of 2 studies (N=414): no
difference between groups OR: 1.71 (0.68
2
4.31); p=0.26; I =16%
161
One study (N=144) reported 22 (15.3%)
total superficial SSIs and no difference at 30
Superfic- 2 OBS
161,162 day follow up: 12/54 (22.2%) vs. 10/90 Low 0 0 0 0 0 0 0 0 Low
ial SSI*
(11.1%); p=0.1
162
One study (N=270) reported 7(2.6%) total
superficial SSIs and no difference at 30 day
follow up: 2/90(2.2%) vs. 5/180 (2.7%); RR
0.80 (0.16-4.03); p=1.0
In a meta-analysis of 3 studies (N=732), no
difference between groups: 18/332 vs.
163- 11/400; p=0.07; OR: 1.70 (0.58 4.96);
3 OBS 2
SSI* 165 p=0.34; I =13% Low 0 0 0 -1 0 0 0 0 Very Low
163
1 OBS Study , SSI= 0/68 vs. 2/136
164
1 OBS Study , SSI= 14/224 vs. 9/224
THA:
165
1 OBS Study , SSI= 4/40 vs. 0/40
Injection Very
vs. No In a meta-analysis of 3 studies (N=732), no Low
Injection difference between groups7/332 (2.1%) vs.
2/400 (0.5%); OR: 2.95 (0.61 14.18);
163- 2
3 OBS p=0.18; I =0%
PJI* 165 Low 0 0 0 -1 0 0 0 0 Very Low
163
One study (n=202) found 66 injected
patients (68 THAs) to 136 not-injected
patients (136 THAs): no difference: 0/68
(0%) vs. 1/136 (0.73%); p=0.80.
2017 American Medical Association. All rights reserved. 502
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Overall
Publication Bias
Quantity GRADE of
Dose-response
GRADE
Study Quality
and Type Starting Evidence
Confounders
Consistency
Comparison Outcome Findings of
Directness
of GRADE for
Evidence
Precision
Evidence Outcome
Base
Methylprednisolone 40mg/dL injections were
administered an average of 14 months
before surgery (median, 11months)
164
One retrospective matched cohort study
(N=4448) in THA reported no difference:
3/224 (1.33%) vs. 1/224 (0.44%) at 2y follow
up. Hazard ratio: 3 (0.3-29.8). Cumulative
risk of deep infection at 5yr was 3% (95% CI,
0-7%) for the injection group and 0.6%
(95%CI, 0-1.7%) for the no-injection group.
Steroid dose average 20.47mg (range, 6-40)
165
1 small (N=80) study in joint infections
requiring revision THA reported no
difference: 4/80 (5%); 4/40 (10%) vs. 0/40
(0%); p=0.13 at 1y follow up (used
methylprednisolone 80mg/dL)
In a meta-analysis of 3 studies (N=732), no
difference between groups OR: 1.32 (0.54
2
3.22); p=0.55; I =0
163
One study found no difference: 0/68 (0%)
vs. 1/136 (0.73%); p=0.80. (30 day follow up)
164
One study found no difference: 11/224
163-
Superfic- 3 OBS (4.9%) vs. 8/224 (3.6%) 2 year follow up;
165 Low 0 0 0 0 0 0 0 0 Low
ial SSI* Hazard ratio 1.5 (95% CI, 0.6-3.6);
Cumulative risk of superficial SSI at 5 years:
4.5% (95% CI, 2.4-8.4) vs. 3.7% (95% CI,
1.1-6.1)
165
One study found no infections: 0/40 vs.
0/40 (1 year follow up).
Q16 What are the most effective strategies for managing the preoperative use of intra-articular corticosteroid injections to reduce the risk of SSI in prosthetic
joint arthroplasty patients?
Q16A. Does the length of time between intra-articular corticosteroid injection and prosthetic joint arthroplasty impact the risk of SSI?
2017 American Medical Association. All rights reserved. 503
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Overall
Publication Bias
Quantity GRADE of
Dose-response
GRADE
Study Quality
and Type Starting Evidence
Confounders
Consistency
Comparison Outcome Findings of
Directness
of GRADE for
Evidence
Precision
Evidence Outcome
Base
THA:
In a small (N=80) matched, cohort (injected:
not injected) study: neither the total number
of injections (p=0.89) before THA nor the
time interval between the injection and the
operation (p=0.88) differed. For this
Length of
particular measure, the study was
time
underpowered (0.052 and 0.053,
between
respectively)
most
No association between the average time
recent SSI* 2 OBS
164,165 from intra-articular corticosteroid injection to Low 0 0 0 0 0 0 0 0 Low Low
injection
primary THA and the development of
and
superficial SSI or PJI
surgery
Mean time between injection and THA: 112
days (SD=81days).
Mean time between injection and THA for 3
patients who developed PJI was less than
half the length of time for those who
developed superficial SSI (n=11): 44 days
(SD=23) vs. 112days (SD=94d).
Q16. What are the most effective strategies for managing the preoperative use of intra-articular corticosteroid injections to reduce the risk of SSI in prosthetic
joint arthroplasty patients?
Our search did not identify data that evaluated preoperative strategies for managing the use of intra-articular corticosteroid injections in prosthetic joint arthroplasty
patients and their impact on risk of SSI.
Q16A. Does the length of time between intra-articular corticosteroid injection and prosthetic joint arthroplasty impact the risk of SSI? Our search did not
identify data that evaluated different lengths of time between preoperative intra-articular corticosteroid injection administration and its impact on the risk of TKA.
Q16B. Does the corticosteroid injection dose impact the risk of SSI? Our search did not identify data that evaluated different doses of preoperative intra-articular
corticosteroid injections and their impact on the risk of SSI.
*Critical outcome; OR: Odds Ratio; RR: Risk Ratio; CI: Confidence Interval
2017 American Medical Association. All rights reserved. 504
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.2B.2: EVIDENCE TABLES: Q12-16 SYSTEMIC IMMUNOSUPPRESSIVE THERAPY
Q12. How does systemic corticosteroid or other immunosuppressive therapy impact the risk of SSI in prosthetic joint arthroplasty patients?
Q12A. Does the type of agent impact the risk of SSI?
Q12B. Does the preoperative duration of the therapy impact the risk of SSI?
Q12C. Does the agent dose impact the risk of SSI?
Q13. What are the most effective strategies in managing systemic corticosteroids or other immunosuppressive therapy perioperatively to reduce the
risk of SSI in prosthetic joint arthroplasty patients?
Q13A. How safe and effective is the discontinuation of these agents preoperatively and when should they be resumed?
eTABLE 59. Evidence Table for Q12-13 Systemic Immunosuppressive Therapy
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
Bridges Retrospe- To compare the Number of patients: N=38 Intervention group: n=19 SSI (6 weeks) Definitions:
158
1991 ctive surgical patients (6 patients in (6 patients in both groups) PJI Complications:
(ES) concurre- outcomes of both groups) and 47 [19 procedures] MTX-on: 1/15 procedures prosthetic joint infection
nt control patients with procedures MTX-On - Patients who (6.7%) or would dehiscence or
1, 2, 3, 4, Rheumatoid Patient Characteristics: received MTX within 4 MTX-off: 0/32 infection documented in
6, 7, 8 Arthritis (RA) in no statistically significant weeks of surgery P=0.25 the medical record within
whom differences between the Timing of intervention: NA 6 weeks after surgery
methotrexate patients in control and Duration of intervention: Other infections: NR Perioperative care: NR
(MTX) was intervention groups with NA Topic-specific outcomes: Analytical
stopped more regard to any of the Device/agent: NA Flares NR methodology: students
than 4 weeks characteristics examined. Monitoring intervention: Reoperations: NR t test, chi-square test, or
preoperatively Age: NA Length of stay: NR Fishers exact, 2-tailed
with those in Gender: Control group: n=25 (6 Mortality: as appropriate.
whom MTX Obesity: patients in both groups) MTX-on: 6/19 (31.6%) Other notes: none
was stopped Comorbidities: [34 procedures] MTX-off: 4/25 (16.7%) Follow-up: 6 weeks
less than 4 Procedures: n/N MTX-Off patients in whom One (1) patient death postop
weeks procedures MTX was discontinued 4 or overlapped both groups. Funding Source
preoperatively. TJA of hip or knee (n) more weeks before the Conflicts:
All orthopedic MTX-on: 12/19 (63.2%) surgery, and those in whom Adverse events: NR Authors: NR
surgeries were MTX-off: 32/34 (94.1%) surgery was performed Institution: NR
included. MCP arthroplasty before or after the MTX Study: NR
MTX-on: 2/19 (10.5%) treatment period and who Supplies: NR
MTX-off: 0/34 were taking no disease
Metatarsal head resection modifying anti rheumatic
MTX-on: 1/19 (5.3%) drugs (DMARDs) for at least
MTX-off: 1/34 (2.9%) 3 months prior to surgery.
Shoulder arthroplasty Standard preventive
MTX-on: 1/19 (5.3%) measures: NR
MTX-off: 0/34
2017 American Medical Association. All rights reserved. 505
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
Other
MTX-on: 3/19 (15.8%)
MTX-off: 1/34 (2.9%)
Indications: Rheumatoid
Arthritis (RA)
Setting: 1 University
hospital
Location: USA
Dates: 1981-1989
Inclusion Criteria: Patients
with RA who began MTX
therapy and who underwent
elective primary orthopedic
surgery before January
1990.
Exclusion Criteria:
Patients undergoing
revision Total Joint
Arthroplasty.
Carpen- Prospecti- To Number of patients: N=32 Intervention group: n=19 SSI (1 year) Definitions: none
ter ve prospectively patients (41 procedures) (26 procedures) PJI Perioperative care: NR
159
1996 Concurre- follow all Patient Characteristics: Patients assigned to MTX-on: .3/15 procedures Analytical
(ES) nt control rheumatoid no significant differences in discontinue MTX the week (20%) methodology: two-
1, 2, 3, 4, arthritis (RA) patient characteristics prior and during the week of MTX-off: 0/26 procedures sample t test. Bonferroni
6, 7 patients between groups surgery (total of 2 weeks) p=0.08 correction was used for
receiving Procedures: Timing of intervention: NA Other infections: NR multiple comparisons.
Methotrexate THA: Duration of intervention: Topic-specific outcomes: Fishers exact test.
(MTX) who MTXon 8/26 (30.8%) NA Flares: no flares reported in Other notes: none
underwent total MTXoff 4/16 (25%) Device/agent: Methotrexate either group Follow-up: at least 1
joint TKA: Monitoring intervention: Reoperations: NR year postop
arthroplasty to MTXon 7/26 (26.9%) NA Length of stay: NR Funding Source
determine if MTXoff 3/16 (18.8%) Control group: n=13 (15 Mortality: NR Conflicts:
continuing or TWA: procedures) Adverse events: NR Authors: NR
stopping MTX MTXon 3/26 (11.5%) Patients assigned to Institution: NR
during the MTXoff 3/16 (18.8%) continue MTX through the Study: NR
perioperative TMCPA: perioperative period. Supplies: NR
period MTXon 7/26 (26.9%) Standard preventive
influenced the MTXoff 4/16 (25%) measures: NR
rate of TEA
postoperative MTXon 0/26
2017 American Medical Association. All rights reserved. 506
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
infections. MTXoff 1/16 (6.25%)
Indications: Rheumatoid
Arthritis
Setting: 1 army medical
center
Location: USA
Dates: January 1982
December 1991
Inclusion Criteria: All RA
patients receiving MTX at
the time they were to
undergo total joint
arthroplasty or joint fusion
during study dates.
Exclusion Criteria:
patients on azathioprine
concurrently
Perhala Retrospe- To assess Number of patients: Intervention Group: n=60 SSI (6 months) Definitions: NR
157
1991 ctitve whether the N=121 patients (202 patients (92 procedures) PJI Perioperative care: NR
(ES) concurre- risk of local procedures) Patients who had taken MTX vs. NO MTX Analytical
nt control infectious Patient Characteristics: MTX: All Total Joint methodology: Students
1, 2, 3, 4, complications unless listed below, no Intervention group1: Replacements t test, Chi square
6, 7 or poor wound statistically significant MTXoff: Patients who had MTX: 3/92 (3.26%) analysis.
healing is differences in taken MTX but stopped NoMTX: 2/110 (1.81%) Other notes: None
increased characteristics existed more than 4 weeks prior to p=0.66 Follow-up: 6 months
during the between groups. the surgery Revision total joint Funding Source
postoperative Age: mean (Y) Intervention group2: replacements: MTX: 1/9 Conflicts:
course in MTX: 54.6 MTXon: patients who had (11.1%) Authors: None
Rheumatoid NoMTX: 59.0 taken MTX but who took NoMTX 0/16 Institution: None
arthritis (RA) P=0.03 MTX within 4 weeks of p=0.26 Study: None
patients treated Gender: surgery Bilateral TKA Supplies: None
with Obesity: Timing of intervention: NA MTXon 0/3
Methotrexate Comorbidities: Duration of intervention: NoMTX: 1/11 (9.09%)
(MTX) Daily prednisone dose: NA p=1.00
mean(mg) Device/agent: Methotrexate Continuous MTX vs.
MTX: 4.87 Monitoring intervention: Pausing MTX
NoMTX: 3.69 NA PJI
P=0.08 Control group: n=61 MTXon: 2/45 (4.44%)
Procedures: THA And TKA Patients who had never MTXoff: 1/47 (2.12%)
Indications: Rheumatoid taken MTX p=0.54
2017 American Medical Association. All rights reserved. 507
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
Arthritis Standard preventive
Setting: 1 hospital measures: All patients Other infections:
Location: USA received antimicrobial s MTX vs. No MTX
Dates: January 1, 1978 perioperatively (Cefazolin or Deep Wound Abscess
December 31, 1987 vancomycin) MTX: 0/92
Inclusion Criteria: Patients NoMTX: 1/110 (0.91%)
who underwent Total hip or p=0.57
total knee replacement at Infected Hematoma
the center during the study MTX: 2/92 (2.17%)
dates. And who were NoMTX: 1/110 (0.91%)
classified by the American p=0.47
Rheumatism Association Bilateral TKA
criteria as having classic or MTX: 1/3 (33%)
definite RA (30). NoMTX 0/11
Exclusion Criteria: p=0.14
Patients who had Necrotic eschar
undergone apheresis or MTX: 2/92 (2.17%)
total lymphoid irradiation or noMTX: 0/110
had been treated with p=0.24
azathioprine, Serous Drainage
cyclophosphamide, or MTX: 1/92 (1.09%)
chlorambucil concurrently NoMTX: 1/110 (0.91%)
Continuous MTX vs.
Paused MTX
Infected Hematoma
MTXoff: 2/47 (4.25%)
MTXon: 0/45;
p=0.30
Necrotic eschar
MTXoff: 2/47 (4.25%)
MTXon: 0/45
p=0.30
Serous Drainage
MTXoff: 0/47
MTXon: 1/45 (2.22%)
p=0.48
Topic-specific outcomes:
NR
Reoperations: NR
Length of stay: NR
2017 American Medical Association. All rights reserved. 508
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
Mortality: NR
Adverse events: NR
Momoh- Retrospe- To analyze the Number of patients: Intervention group: n= 48 SSI (Follow Up NR) Definitions:
ara ctive risk ratios of N=420 Biologic DMARDS TOTAL INFECTIONS SSI: diagnosed by
154
2011 concurre- SSI after total THA = 81 (19.3%) THA = 11 27 total Postop surgeon according to
(ES) nt control hip arthroplasty TKA = 339 (80.7%) TKA= 37 Complications (6.4%) CDC SSI Guideline
1, 2, 3, 4, (THA) or total Patient Characteristics: IFX: 19 (4.5%) Superficial incisional SSI: 1999.
5, 6, 7, knee given for total population ETN: 23 (5.5%) 24 (5.7%) [treated with
arthroplasty given as n (%) or median ADA: 2 (0.5%) antimicrobials] Perioperative care:
(TKA) in (IQR) TCZ: 4 (1.0%) Organ/Space SSI: 3 (0.7%) General, lumbar and/or
Rheumatoid Age: 61 (54.8-68) y [required surgical epidural anesthesia
Arthritis (RA) Gender % female: 382 Timing of intervention: For treatment to remove the were all utilized
patients treated (91.0%) TNF-blockers was artificial joint prosthesis]
with biologic Obesity: 21.4 (19.4-23.8) performed in accordance Non-biologic DMARDs: Analytical
DMARDs BMI with British Society for 2/3 (66.7%) methodology:
(mainly TNF Comorbidities: Rheumatology and Japan IFX: 1/3 (33.3%) Multivariate logistic
blockers) Diabetes: 34 (8.1%) College of Rheumatology regression to test the
compared with Smoking (ever): 67 (16.0%) Guidelines.: That TNF- Statistically significant risk association of SSI with
RA patients Surgical history: 193 blocker treatment should be factors putative risk factors and
treated with (46.0%) withheld 2-4 weeks prior to Disease Duration (years) with the use of non-
non-biologic Disease Duration: 14.5 major surgical procedures: SSI: 23.3 (17.6-26.4) biologic DMARDs and
DMARDs. (8.9-21.0)y specifically No-SSI: 14.1 (8.1-19.6) biologic DMARDs.
Also to Preop CRP: 0.98 (0.25- ETN & ADA: 2-4 weeks OR: 1.09 (1.04-1.14);
determine 2.19) IFX & TCZ: 4 weeks (TCZ p=0.003 Other notes: NR
whether Preop Hb: 10.9 (10.2-11.8) was restarted 4 weeks after Biologic DMARDs Follow-up: NR
perioperative Preop WBC: 7.25 (6.1-9.0) surgery) SSI: 10/27 (37.0%) Funding Source
interruption of Revision: 16 (3.8%) Duration of intervention: No-SSI: 38/393 (9.7%) Conflicts:
TNF blockers variable OR: 5.69 (2.07-15.61); Authors: Industry
decreases SSI. Procedures: Total Hip Agent: biologic Disease p=0.0007 Institution: NR
Arthroplasty (THA) or Total Modifying Antirheumatic Prednisone dose not a Study: NR
FROM Knee Arthroplasty (TKA) Drugs (bDMARDS) statistically significant risk Supplies: NR
DISCUSSION Indications: Rheumatoid Monitoring intervention: factor
2017 American Medical Association. All rights reserved. 509
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
The aims of Arthritis (RA) NR SSI: 3 (0-5
this study were Setting: 1 Medical Control group: n=372 No-SSI: 3 (0-5
to assess the University Institute of THA=70 OR: 1.09 (0.93-1.28);
influence of Rheumatology TKA=302 p=0.27
non-biologic Location: Japan
DMARDs and Dates: January 2005 and Non-biologic DMARDs. As a
biologic December 2009 rule were continued
DMARDs, as Inclusion Criteria: Patients perioperatively but were Statistically significant
well as the who full the 1987 revised administered cautiously in Medications as SSI risk
withholding of American College of individual patients if there factors (where n>10
TNF-blocker Rheumatology (ACR) were comorbidities or were administered patients)
therapy on the criteria for RA who elderly. IFX
incidence of underwent THA or TKA Patients in this group SSI: 4/27 (14.8%)
SSI. between January 2005 and received one or more No-SSI: 15/393 (3.8%)
December 2009 and were immunosuppressive and/or OR: 9.8 (2.41-39.82);
treated with biologic or non- immunomodulatory Non- p=0.001
biologic DMARDs biologic medication ETN
Exclusion Criteria: NR IMMUNOSUPPRESIVE SSI: 6/27 (22.2%)
AGENTS No-SSI: 17/393 (4.3%)
MTX: 279 (66.4%) OR: 9.16 (2.77-30.25);
Leflunomide: 4 (1%) p=0.0003
Tacrolimus: 31 (7.4%)
Mizoribine: 15 (3.6%) Other infections: NR
Cyclophosphamide: 3 (0.7%) Topic-specific outcomes:
IMMUNOMODULATORY NR
AGENTS Reoperations:
Salazosulfapyridine: 93 3 Organ/Space SSI (0.7%)
(22.1%) required removal of artificial
Bucillamine: 52 (12.4%) joint prosthesis
Minocycline: 7 (1.7%) Length of stay: NR
Actarit: 9 (2.1%) Mortality: NR
Auranofin: 4 (1.0%) Adverse events: No cases
Gold Sodium Thiomalate: 1 of sever delayed wound
(0.2%) healing requiring additional
-penicillamine: 16 (3.8%) sutures were observed.
Glucocorticoids: 296 (70.4%)
at average dose of
3.0mg/day
Standard preventive
2017 American Medical Association. All rights reserved. 510
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
measures:
All surgeries were performed
with protective clothing
against infection, in a
bioclean room.
AMP: cefazolin or
ampicillin/cloxacillin were
given intravenously twice
before surgery and 2h after
the start of surgery. AMP
was not administered
regularly after the day of
surgery.
Hirano Retrospe- To investigate Number of patients: Intervention group: n=39 SSI (follow-up NR) Definitions:
156
2010 ctive the influences N=113 INF: 24/39 (61.5%) Infection Adverse events (AEs) of
(ES) Concurre- of anti-Tumor Patient Characteristics: ETA: 15/39 (38.5%) TNF: 1 (2.6%) TKA surgical wounds
nt Cohort Necrosis Factor mean SD (Range) or n Tumor Necrosis Factor Agents administered included wound
2, 3, 4, 5, 8 (TNF) agents (%) (TNF) group: patients INF, MTX and oral dehiscence and
on the Age: year (range) treated with anti-TNF agents prednisone continuation of
postoperative TNF: 58.99.0 (31-73) from both centers Non-TNF: 5 (6.8%) discharge that were
recovery in Non-TNF: 62.69.1 (30- Administration of agents OR: 0.7459 (0.138-4.0336) healed by conservative
patients with 77) were stopped prior to P=0.7459 treatment
Rheumatoid P=0.0308 surgery and restarted after Wound dehiscence:
Arthritis (RA) Gender: Female (%) complete wound healing: Other infections: NR wound which is not
and the effects TNF: 32 (82.1%) Timing of intervention: Pre Topic-specific outcomes: completely healed in 14
of biologics on Non-TNF: 65 (87.8%) and postoperatively Subanalysis: influence of POD or which requires
wound healing. Obesity: NR anti-TNF on wound secondary suture.
Comorbidities: Duration of intervention: healing Infection: positive culture
RA Duration: years variable THA N=30 total results
(Range): INF: agent stopped 3-4 TKA N= 65 total Time for complete
TNF: 13.57.8 (4-32) weeks prior to surgery. TNF n=13 wound healing: the
Non-TNF: 16.511.7 (1- (mean 29.8 days preop) TNF n=14 period from the date of
51) ETA: agent stopped 1-2 Non-TNF n=17 operation to the removal
Steinbrocker Stage III vs. IV weeks prior to the surgery. Non-TNF=51 of surgical staples.
TNF: 18.8% vs. 81.2% (mean 9.6 days preop) Postop Febrile periods:
body temp37.5 C
o
Non-TNF: 52.7% vs. AE Occurrence rate for
47.3% Agents: Anti-TNF surgical wounds: % recovery of
P=0.0249 Infliximab (INF) or THA = 0 .0% in both TNF hemoglobin (%Hb), %
%MTX use etanercept (ETA) and non-TNF groups. recovery of total protein
2017 American Medical Association. All rights reserved. 511
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
TNF: 92.3% (%TP), and % recovery
Non-TNF: 50.0% Monitoring intervention: TKA of serum albumin
P=0.001 NR TNF: 1 (7.1%) (%Alb):
Control group: n=74 Non-TNF: 4 (7.8%) Perioperative care: NR
Procedures: Ankle Non-TNF Group (traditional OR= 0.9038 (0.0928-
arthrodesis and total DMARDs) consisting of 8.7992) p=NS Analytical
arthroplasty of the hip, patients only from the methodology:
knee, elbow, shoulder and University Hospital. Febrile Period Continuous variables
ankle. Only the first THA evaluated with Mann
operation for each patient Standard preventive TNF: 3.52.0 days Whitney U Test. Or
was included. measures: NR Non-TNF: 3.11.9days Fishers exact test to
TKA OR= 0.9038 (0.0928- evaluate the difference
TNF: 14 (35.9%) 8.7992) p=NS in Proportions.
Non-TNF: 51 (68.9%) TKA Other notes: Data was
THA TNF: 2.62.5 days collected from medical
TNF: 13 (38.2%) Non-TNF: 2.91.7 days records.
Non-TNF: 17 (23.0%) Follow-up: NR
TEA %Hb, %TP, %Alb: The only Funding Source
TNF: 8 (20.5%) statistically significant Conflicts:
Non-TNF: 4 (5.4%) difference between TNF Authors: None
AD and non-TNF groups Institution: None
TNF: 3 (7.7%) occurred in the THA Study: None
Non-TNF: 1 (1.4%) subgroup for %Hb Supplies: None
TSA TNF: 101.014.4%
TNF: 1 (2.6%) Non-TNF: 83.810.0%
Non-TNF: 0 P=0.0016
TAA Reoperations:
TNF: 0 TNF infection was treated
Non-TNF: 1 (1.4%) with surgical debridement
without implant removal;
Indications: Rheumatoid antimicrobials were
Arthritis (RA) administered for 4 weeks.
Setting: 1 University Length of stay: NR
Hospital and 1 medical Mortality: NR
center Adverse events:
Location: Japan Adverse Events (AEs) of
Dates: April 2004 July surgical wounds
2007 TNF: 2 (5.1%)
Inclusion Criteria: Patients Non-TNF: 5 (6.8%)
with RA undergoing Ankle OR: 0.7459 (0.138-4.0336)
2017 American Medical Association. All rights reserved. 512
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
arthrodesis and total P=0.7459
arthroplasty of the hip, Time to Complete Wound
knee, elbow, shoulder and Healing
ankle TNF: 10.91.2 days
Exclusion Criteria: Non-TNF: 10.81.3 days
revision surgery and other Postop Febrile Periods:
minor operations such as TNF: 2.62.2 days
foot operations and wrist Non-TNF: 2.91.7 days
operations %Hb
TNF: 96.314.3%
Non-TNF: 90.111.5%
P=0.0156
%TP
TNF: 100.89.5%
Non-TNF: 100.89.2%
%Alb
TNF: 98.913.5%
Non-TNF: 98.011.3%
Kawak- Retrospe- To validate that Number of patients: Intervention group: n=64 SSI (follow up If using Definitions:
ami ctive perioperative N=128 surgeries (112 surgeries (49 patients) CDC criteria then all SSI: CDC SSI Guideline
155
2010 Concurre- interruption of patients) Anti-TNF group superficial 30d and criteria (1999)
(ES) nt control Tumor Patient Characteristics: IFX = 35 anything with an implant Flare-ups: Arthralgia
1, 2, 3, 4, Necrosis Factor Patients were matched for ETN = 29 wound be 1yr for deep was evaluated using
5, 6, 7 (TNF) blocker type of surgery and gender NOTE: 56 (87.5%) of TNF and organ/space) subjective patient
therapy between groups. group was also on MTX and Superficial SSI assessments.
decreases Age: years 53 (82.8%) were on TNF: 7/64 (10.9%) Serological markers like
complications TNF: 57.0 (51.8-64.0) prednisone 5mg/day (range requiring the use of CRP and ESR have not
utilizing the DMARDs: 57.0 (47.0-64.0) 2-7) (see patient antimicrobials been deemed suitable
British Society Gender: male/female characteristics) DMARDs: 1/64 (1.6%) for measuring the
for TNF: 13/51 Timing of intervention: P=0.016 disease activity during
Rheumatology DMARDs: 13/51 ETN was withheld 2-4 weeks the perioperative period.
guidelines and Obesity (BMI) before surgery infliximab Deep SSI: Recurrences of
the Japanese TNF: 21.2 (20.3-22.7) (IFX) was withheld 4 weeks TNF 1/64 (1.6%) IFX Arthralgia were
College of DMARDs: 21.2 (20.1-23.9) before surgery. and required prosthesis considered Flare-ups.
Rheumatology Comorbidities Both were restarted after removal Venous
recommendatio Disease Duration (y) there was no evidence of DMARD: 0 thromboembolism of
ns for TNF: 10.6 (8.0-19.8) infection and once wound lower extremities:
withholding DMARDs: 13.4 (8.9-19.1) healing was satisfactory. Multivariate analysis of diagnosed by 3
infliximab (IFX) Methotrexate (MTX) Duration of intervention: putative risk factors for SSI: experienced medical
and etanercept TNF: 56 (87.5%) Pre and postoperative OR (90%CI) technologists using
2017 American Medical Association. All rights reserved. 513
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
(ETN) for 2-4 DMARDs: 48 (75%) Agent: Disease duration (y): 1.169 ultrasonography
week prior to P=0.06 Anti-Tumor Necrosis Factor (1.030-1.326); P=0.015 Perioperative care:
major surgical DMARDs (TNF) agents: Infliximab TNF-blocker: 21.8 (1.231- All surgery was
procedures TNF: 8 (12.5%) (INF) or etanercept (ETN) 386.1) p=0.036 performed under general
then restarting DMARDs: 31 (48.4%) Monitoring intervention: PSL dosage: 1.433 (1.007- or epidural anesthesia
treatment once P=7.99E-06 NR 2.040) p=0.046 Analytical
there is no Prednisone (PSL) Control group: n=64 methodology
evidence of TNF: 53 (82.8%) surgeries (63 patients) Other infections: Multivariate logistic
infection and DMARDs: 40 (62.5%) Patients treated with non- Urinary Tract Infection: regression was
once wound P=0.008 biologic DMARDs. Some TNF: 1/64 (1.6%) performed to test the
healing is PLS, dose, mg/day patients took more than 1 DMARD: 0 association of SSI &
satisfactory. TNF: 5 (2-7) DMARD Respiratory Inflammation DVT with putative risk
Wound DMARDs: 3 (0-5) Methotrexate (MTX): n=48 TNF: 0 factors
complications, P=0.006 Salazosulphapyridine: n=18 DMARD: 1/64 (1.6%) Baseline characteristics
Deep Venous Bycillamine: n=6 were compared using
Thrombosis Baseline characteristics for =penicillamine: n=4 Topic-specific outcomes: Mann-Whitney U-test or
and flare-ups DVT Subanalysis (Listed NOTE: 40 (62.5%) of Flare-ups due to Fishers exact test.
following joint below are only those DMARD patients were on interruption of anti-TNF: Other notes
surgery were factors that demonstrated prednisone 3mg/day (range Arthralgia (+): Follow-up: If using CDC
assessed. statistically significant 0-5) (see patient IFX: 2/35 (5.7%) criteria then all
differences between groups characteristics) ETN: 9/29 (31.0%) superficial 30d and
Methotrexate (MTX) Standard preventive P=0.009 anything with an implant
TNF: 39 (86.7%) measures: None The ETN patients wound be 1yr for deep
DMARDs: 32 (71.1%) experienced difficulty for a and organ/space
P=0.06 while during post-op rehab, Funding Source
DMARDs but recovered after Conflicts:
TNF: 7 (15.6%) resumption of ETN Authors: Industry
DMARDs: 24 (53.3%) Treatment. Institution: None
P=1.54E-04 Majority of IFX patients Study: None
Prednisone (PSL) underwent surgery in the Supplies: None
TNF: 38 (84.4%) middle of an 8-week
DMARDs: 29 (64.4%) infusion treatment.
P=0.026 Reoperations:
PLS, dose, mg/day 1 deep SSI (TNF group
TNF: 5 (2-7) (IFX)) required removal of
DMARDs: 3 (0-5) artificial joint prosthesis.
P=0.041 Length of stay NR
Procedures: Mortality NR
1:1 pair-matched case Adverse events:
control study so numbers Postoperative complication
2017 American Medical Association. All rights reserved. 514
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
below are number of of delayed wound healing
procedure PER STUDY was absent in both groups.
GROUP DVT Subgroup analysis
Arthroplasty procedures: DVT Positive
n=54 (84%) TNF: 23/45 (51%)
Shoulder Arthroplasty (SA): DMARDs: 12/45 (26%)
1 P=0.015
Unilateral, elective elbow Multivariate logistic
arthroplasty: 2 regression showed that
Implant replacement TNF blockers were the only
arthroplasty of the MCP statistically significant risk
joints: 2 factor for DVT.
Wrist arthroplasty:6 OR= 2.83 (1.10-7.25)
Unilateral, Elective THA: 8 p=0.03
Unilateral, elective TKA: 33
Total ankle arthroplasty
(TAA): 1
Bipolar hip
hemiarthroplasty: 1 Non
Arthroplasty procedures:
n=10 (16%)
Arthroscopic synovectomy
of the knee: 3
Foot surgery: 5
Ankle arthrodesis:1
Open reduction and internal
fixation (ORIF): 1
Indications: Rheumatoid
Arthritis
Setting: 1 medical
university
Location: Japan
Dates: May 2004 March
2009.
Inclusion Criteria: Patients
in matched pairs either
treated with anti-TNF
agents or conventional
DMARDS and who
underwent joint surgery for
2017 American Medical Association. All rights reserved. 515
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
RA. All patients fulfilled the
1987 revised ACR Criteria
for RA
Exclusion Criteria:
Surgery in which TNF agent
adalimumab (ADA) was
used
Bongar- Retrospe- To determine Number of patients: Intervention group: n=462 SSI (mean follow up 4.3 Definitions
tz ctive the cumulative N=924 patients with 657 years) RA Diagnosis: verified
160
2008 concurre- and 1-year Patient Characteristics surgeries. PJI in matched cohorts at 5 by using validated RA
(ES) nt cohort incidence of Age: meanSD y Patients with RA undergoing years classification criteria.
1, 2, 3, 4, prosthetic joint RA: 63.613.3 either THA or TKA. RA: 15/462 (4.2%) According to the
5, 6, 7 infection (PJI) OA: 67.210.8 Timing of intervention: Pre OA: 4/ 462 (1.4%) American College of
in total hip P<0.001 or post operatively Log rank p=0.005 Rheumatology
arthroplasty Gender: n% female Duration of intervention: If HR: 4.08 (1.35-12.33) classification criteria.
(THA) and total RA: 363 (78.6%) DMARD therapy was After adjusting for previous OA Diagnosis: verified
knee OA: 338 (73.2%) withheld around the time of infection in the index joint: during chart review
arthroplasty P=0.06 surgery, the stop and start HR: 3.74 (1.23-11.33) using physicians
(TKA) in a Obesity: NR dates were abstracted based [age, sex, functional class, diagnosis of hip and/or
modern cohort Comorbidities: on pharmacokinetic half-life and comorbidity were not knee OA and absence of
of patients with At least 1 comorbidity and/or data on the biologic significant predictors of RA
RA and to RA: 337 (73.0%) activity of each DMARD. infection) PJI: diagnosed when at
further explore OA: 383 (83.0%) According to the information PJI in matched cohorts at 1 least 1 of the following
potential risk P<0.0001 below, the DMARD use was year were present:
factors for Mean disease Duration: judged as either withheld or RA: 10/462 (2.3%) 1. Isolation of the same
these 21.1 years maintained. OA: 1/ 462 (1.4%) organism from 2
infections. Previous PJI in index joint Duration of days medication p=deemed statistically cultures of joint aspirates
Additionally, RA: 43 (9.3%) was withheld: significant, but P=NR or intraoperative tissue
the frequency OA: 24 (5.2%) Methotrexate:8 OR: 10.30 (1.31-80.26) specimens.
of this Steinbrocker functional Leflunomide: 85 days or 14 2. Acute inflammation
complication of classification at time of days with cholestyramine PJI in RA population consistent with infection
patients with surgery (p<0.0001) wash-out RA: 23/657 (3.7%) on histopathologic
RA as Class1 (patient normally Oral gold: 8 (14[2.2%] infected w/in first examination (as
compared with active): Intramuscular gold: 29 year) determined by the
patients with RA: 4 (0.9%) Sulfasalazine: 8 Revision: 15/255 (5.9%) pathologist).
OA who OA: 6 (1.3%) Hydroxychloroquine: 85 Primary: 8/402 (2.0%) 3. Cutaneous sinus tract
undergo the Class2 (patient able to Azathioprine: 8 THA: 12/328 (3.7%) communicating with the
2017 American Medical Association. All rights reserved. 516
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
same type of maintain occupation but Cyclosporine: 8 TKA: 11/329 (3.3%) joint prosthesis
surgery was less active): Cyclophosphamide: 8 Previous PJI: 7/67 (10.4%) 4. Purulence in the joint
assessed. RA: 183 (39.6%) -penicillamine: 15 space (as determined by
OA: 338 (73.2%) Etanercept: 8 Statistically significant risk the surgeon).
Class3 (unable to maintain Adalimumab: 15 factors for SSI (univariate) Perioperative care
occupation): Infliximab: 57 HR (95%CI) [p=NR]
RA: 184 (39.6%) Anakinra:8 Revision arthroplasty: 2.99 Analytical
OA: 108 (23.4.2%) (1.02-8.75) methodology:
Class4 (largely or wholly Agent: See above Previous infection of index Proportion of surgeries
incapacitated): joint: 5.49 (1.87-16.14) complicated by a PJI
RA: 86 (18.6%) Monitoring intervention: Operation Time: 1.36 per was estimated by
OA: 8 (1.7%) NR 60-min increase (1.02-1.81 Kaplan-Meier
Unknown: Techniques.
RA: 6 (1.3%) Control group: n=462 ** NOTE** - Patients in this Cox proportional
OA: 2 (0.4%) patients study who had a previous hazards models were
Matched cohort of patients PJI had a risk of another used to examine the
Procedures: Total knee with OA instead of RA. infection of only 3.5% as association between the
arthroplasty (TKR) or total Patients were listed in the compared with 29.2% after risk of prosthetic joint
hip arthroplasty (THA) registry as having a revision of the previously inspection for
Primary THA: 164 (25.0%) diagnosis of OA and no infected joint. explanatory variables.
Revision THA: 164 (25.0%) diagnosis of RA. Matching Also used to compare
Primary TKA: 238 (36.2%) was performed according to DMARD the risk of infection
Revision TKA: 91 (13.8%) age (5 years), site (hip or Stopping DMARD therapy between the RA and OA
Indications: Rheumatoid knee), type (revision or at the time of surgery cohorts.
Arthritis (RA) or primary arthroplasty), and lowered the Risk of
Osteoarthritis (OA) time point of first surgery. subsequent PJI: HR 0.65 Other notes: None
(0.09-4.95) but not
Setting: 1 hospital Standard preventive statistically significant. Follow-up:
measures: Patients who did not stop Length of FU. meanSD
Location: USA AMP: Preop AMP: 656 anti-TNF therapy before (years)
(99.9%) surgery:3/38 (7.9%) RA: 3.12.4
Dates January 1, 1996 infections OA: 3.82.6
June 30, 2004 Nonstandard preventive Patients who stopped
measures: Anti-TNF therapy before All patients were
Inclusion Criteria: All Antimicrobial impregnated surgery: 0/12 infections. followed up by surgeon
patients with a diagnosis of cement: 209 (31.8%) P=NS examination at least
RA or OA who underwent surgeries were performed twice in the first
THA or TKA during the with antimicrobial Perioperative cortisone was postsurgical year and
study dates. impregnated cement not associated with then at least every 5
increased risk of prosthesis years thereafter. If in-
2017 American Medical Association. All rights reserved. 517
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
Exclusion Criteria: NR infections person follow up was not
Other infections: NR possible, patients were
Topic-specific outcomes: contacted by letter
NR and/or phone and asked
Reoperation : to complete a
16/23 (69.6%)infections standardized form
were treated with For outstanding or
prosthesis removal. 6/16 unclear issues as well as
had subsequent for a follow-up <1 year,
reimplantation primary physicians were
7/23 (30.4%) were treated contacted.
with debridement and long- Funding Source
term antimicrobial Conflicts:
suppression therapy. Authors: Industry
Length of stay: NR Institution: None
Mortality: NR Study: None
Adverse events: NR Supplies: None
Q13B. Should the agent dose be adjusted, and if so, for how long? Our search did not identify data that evaluated perioperative immunosuppressive therapy
dose adjustment and its impact on the risk of SSI in prosthetic joint arthroplasty patients.
Q14. What is the optimal duration of postoperative AMP to reduce the risk of SSI in prosthetic joint arthroplasty patients who are on systemic
corticosteroid or other immunosuppressive therapy? Our search did not identify data that specifically evaluated differences in duration of postoperative AMP
in prosthetic joint arthroplasty patients who were on systemic corticosteroids or other immunosuppressive agents and its impact on the risk of SSI. However,
multiple procedures examined in the Core section, Q1.E: Postoperative AMP duration that included patients on immunosuppressive therapy showed no benefit of
continuing AMP after closing the surgical incision in the operating room. Therefore, the broader recommendation for duration of postoperative AMP should be
applied to prosthetic joint arthroplasty procedures irrespective of use if systemic corticosteroid or other immunosuppressive therapy.
2017 American Medical Association. All rights reserved. 518
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
eTABLE 60.Evidence Table for Q15. How does preoperative intra-articular corticosteroid injection impact the risk of SSI in
prosthetic joint arthroplasty patients?
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Desai Retrospe- To compare the Number of patients: Intervention group: n=90 SSI (Follow up at least 1 Definitions:
162
2009 ctive incidence of N=360 knees (250 knees (80 patients) year) Superficial Infections:
(ES) Concurr- infection in patients) Patients who had an Unadjusted Results cases which had
ent patients who injection prior to undergoing Superficial Infection (All discharge from
Control had an intra- Patient Characteristics knee replacement surgery. treated with antimicrobials superficial layers within
1, 2, 3, 4, articular steroid Age: mean (Range) years 45/80 (56.3%) patients had a & no further complications) one moth of surgery;
5 infiltration prior Injection: 68 (49-87) TKR within 12 months after Injection: 2/90 (2.2%) patients who received
to a knee No Injection: 72 (51-88) the injection [both patients received antimicrobial cover for
replacement, Gender: m/f Timing of intervention: injections 18 months prior more than 1 week
with those who Injection: 26/54 preoperative to surgery as an outpatient delayed wound healing
hadnt. SSI and No Injection: 74/96 Duration of intervention: procedure] and cases which had
Knee of TKR: right/left Variable No Injection: 5/180 (2.7%) positive cultures form
Injection: 42/48 Agent: (40mg/dL RR 0.80 (0.16-4.03) P=1.0 superficial layers which
No Injection: 82/98 methylprednisolone and settled and did not
Obesity: NR 5mg/mL levobupivacaine) 6/7 Infections occurred in require further surgery
Comorbidities: NR intra-articular steroids. patients with Osteoarthritis. for the knee
Infiltration was conducted in Deep Infection: cases
Procedures: Total Knee the operating theater as a Deep Infection: No Cases with positive swab
Arthroplasty (TKR) day-case procedure in either group cultures or tissue biopsy
(patients were discharged from the deep tissues,
Indications: later the same day). Injection Other infections: NR patients who under-went
Osteoarthritis was conducted under strict Topic-specific outcomes: exploration and wash
Injection: 58/80 (72.5%) aseptic precautions. None out of the wound with
No Injection: 133/170 30 knees (the earlier Reoperations: None positive culture report
(78.2%) surgeries) were performed Length of stay: NR and cases which
Rheumatoid arthritis as out-patient procedures Mortality: NR underwent revision
Injection: 22/80 (27.5%) with strict aseptic Adverse events: NR surgery for infection.
No Injection: 37/170 precautions. Perioperative care: NR
(21.7%) Monitoring intervention: Analytical
Setting: 1 hospital NR methodology: Normal
Location: England Control group: n=180 approximation method
Dates: 1997 - 2005 knees (170 patients) was utilized to assess
Inclusion Criteria: Patients Knees undergoing TKR that non-inferiority of
who had total knee had no injection prior to TKR injection on risk of
replacement within the surgery. Knees were infection.
study dates with a minimum matched two control knees Other notes: Patients
1-year follow-up including to one Intervention knee. were retrospectively
2017 American Medical Association. All rights reserved. 519
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
patients with diabetes Matching was done on the identified by analysis of
mellitus and a history of basis of age, sex and year of the notes in a
smoking. operation. Age selection was prospective database of
Exclusion Criteria: A done by 10 yearly intervals TKRs performed by the
history of malignancy, and year of operation was primary author.
immune-suppressive drugs, done by 3-yearly intervals Cohort matching was
sero-negative inflammatory Standard preventive done prior to any
arthropathy or a previous measures: evaluation of patient
infection in the ipsolateral Prosthesis: All TKR were notes with respect to
knee. cemented, fixed bearing infection rates.
knee systems. Authors estimate that
Approach: midvastus given low infection rate,
approach under tourniquet sample size of ~2000
Suction: usage was kept to a patients per group
minimum and only used needed to rule out (with
during pulsed lavage 95% CI) a 50% increase
irrigation prior to in infection rate among
cementation. those injected.
Irrigation: prior to wound Follow-up: At least 1
closure and with 0.05 year follow up. Mean
chlorhexidine. follow-up was 48
Hemostatis: meticulously months. Range 1-
achieved before closure over 6years)
drains Funding Source
Tourniquet was released Conflicts:
after wound closure Authors: NR
AMP: 3 doses of Cefuroxime Institution: NR
postoperatively in addition to Study: NR
the loading dose to ensure Supplies: NR
cover for 24 hours Postop
2017 American Medical Association. All rights reserved. 520
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Sreeku- Retrosp- To determine if Number of patients: Intervention group: n=66 SSI (F-U at least 1 year) Definitions: None
mar ective intra-articular N=202 patients (68 hips) Infection at most recent
163
2007 Concurr- steroid injection Patient Characteristics Injection Cohort: received follow up Perioperative care: NR
(ES) ent prior to joint Age: avg. (range) median, intra-articular injection of Total Infections:
Control (hip) y steroids prior to hip Injection: 0 Analytical
1, 2, 3, 4, replacement Injection: 62.2 (32-89) replacement surgery No Injection: 2/136 (1.4%) methodology:
5 increases the 62.62 Timing of intervention: Difference in incidence: Statistical analysis was
risk of injection No-injection: NR (39-89) Pre-operatively 1.4% (-0.5%-3.3%) performed using Stata.
in replaced 64.09 Duration of intervention: 95%CI was obtained by
joints relative to Gender: m/f variable Superficial: the normal
patients who Injection: 15/51 Agent: 40mg/dL Injection: 0 approximation method
had no intra- No-injection: 32/104 methylprednisolone and No Injection: 1/136 (0.7%)
articular Obesity: Any patient 5mg/mL levobupivacaine noticed at 4 weeks postop Other notes: All
injection prior considered overweight were injected. Patients were and responded to procedures performed
to the same (BMI>35) was advised to discharged the same day. antimicrobials. by single surgeon
surgery. lose weight prior to surgery. Monitoring intervention: Deep Infection
The operation was deferred NR Injection: 0 Follow-up: at least 1
until the patient achieved Control group: n=136 No Injection: 1/136 (0.7%) year
target weight. patients (136 hips) who presented 2 months postop Average Follow Up:
Comorbidities received no intra-articular with pyrexia and severe Injection: 25.33 months
Infections: patients were injection prior to surgery pain. Patient was 75yo. Hip No Injection: 22.28
critically assessed for any Each hip in the intervention was aspirated and months
focus of sepsis, including was matched to two hips in antimicrobials were started. Funding Source
form the bladder, skin and the control (non-injection) Other infections: NR Conflicts:
lungs. group Topic-specific outcomes: Authors: NR
Time between injection and Matching was done on the NR Institution: NR
operation for Injection basis of age (10-year Reoperations: Study: NR
Cohort: Mean 14 months intervals), gender, and year Reattachment of trochanter Supplies: NR
(median 11 months) of operation (3-year Injection: 1/66 (1.5%)
Procedures: Hip intervals). When exact occurred at 2 years Postop
replacement matches were unavailable, due to persisting pain
Right/left the next closest match was No Injection: 0
Injection: 41/27 chosen. Length of stay: NR
Bilateral Procedure: Standard preventive Mortality:
Injection: 2/66 measures: Injection: 0
Indications: NR Surgeon: all surgeries were No Injection: 1/136 (0.7%)
Setting: 1 Tertiary Referral performed by the senior Patient with joint infection
Hospital author presented at 2 months
Location: England Approach: by the trans- postop developed acute
2017 American Medical Association. All rights reserved. 521
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Dates: 1997 - 2004 trochanteric. Trochanteric renal shutdown and died of
Inclusion Criteria: Patients osteotomy was done and the multi-organ system failure
who underwent hip hip was exposed. at 3 months.
replacement surgery after Suction: kept to a minimum Adverse events:
steroid filtration. A matched used only during pulsed Aching hip postop
cohort of patients was lavage to reduce the suction Injection: 3/66 (4.5%)
created of patients who catheter sucking air towards [had absence of infection
underwent hip replacement the patient. confirmed by ESR, CRP
without steroid infiltration Irrigation: regular washing of Levels & isotope scans]
prior to surgery. the wound was done with
Exclusion Criteria: chlorhexidine 0.05%.
Patients who had previous Hemostatis: meticulous
operations on the same hip hemostasis was achieved
and patients who had before closure of the drains
malignancy or were on AMP: 3 doses of cefuroxime,
immune-suppressive drugs. postoperatively, in addition
Patients with a previous to the loading dose to
infection in the same hip ensure coverage for 24h
were excluded. postop.
McIntosh Retrosp- To determine if Number of patients: Intervention group: n=224 SSI (follow-up minimum 2 Definitions:
164
2006 ective the N=448 Patients who received intra- years) Superficial Infection: any
(ES) Concurr- administration Patient Characteristics articular steroid injection Superficial Infections wound infection that did
ent of an intra- Age: mean (SD) years within 1 year prior to total hip Injection: 11 (4.9%) not penetrate the deep
Control articular steroid Injection: 70 (9.8) arthroplasty No Injection: 8 (3.6%) fascia and included any
1, 2, 3, 4, injection into an No Injection: 69 (9.6) Timing of intervention: Hazard Ratio: 1.5 (0.6-3.6) patients with persistent
5, 8 osteoarthritic Gender m/f Preoperative Cumulative Risk of postoperative wound
hip within 1 Injection: 93/131 Duration of intervention: superficial infection at 5 drainage, superficial
year of No Injection: 92/132 Variable years: wound dehiscence, or
subsequent Obesity: Calculated from Agent: (Agent-Not Injection 4.5% (2.4-8.4) suture abscess
primary THA mean height/weight standardized) Steroids No Injection: 3.7% (1.1- formation.
would increase reported: delivered via intra-articular 6.1) Perioperative care: NR
the rate of Injection: 30.1 injection. All injections were 15/19 superficial infections
superficial and No injection: 29.8 performed by members of were treated with local Analytical
deep Height: mean (SD) cm the radiology department wound care and 7/15 were methodology:
periprosthetic Injection: 167 (24) within 1 year prior to the also treated with a course Kaplan-Meier method
infection when No Injection: 168 (9.7) THA using standard aseptic of oral antimicrobial was used to estimate the
compared with Weight: mean (SD) kg protocols. Hip penetration prophylaxis cumulative risk of
a matched Injection: 84 (19.9) was confirmed Deep infections (developed infections.
2017 American Medical Association. All rights reserved. 522
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
control group No Injection: 84 (19.9) fluoroscopically by the at a mean of 1.69 years) Cox proportional hazard
who did not Comorbidities: NR installation of radiopaque Injection: 3 (1.3%) model was used to
receive a Time from injection to THA: dye before steroid No Injection: 1 (0.4%) assess the difference in
preoperative mean (SD) days administration. Type and Hazard Ratio: 3 (0.3-29.8) survivals between
intra-articular Injection: 112 (81) amount of steroid dispensed Cumulative Risk of deep groups. Taking into
steroid No Injection: NA was left to the discretion of infection at 5 years: account the timing of
injection. Operative Time: mean (SD) the performing radiologist. Injection: 3% (0-7%) injection and the length
minutes: Monitoring intervention: No Injection: 0.6% (0- of follow-up.
Injection: 182 (47) NR 1.7%) Other notes:
No Injection: 182 (48.1)
Control group: n=224 None of the superficial Follow-up: at 3 months,
Procedures: Total Hip Patients who did not receive infections had deep 1 year, 2 years, and 5
Arthroplasty intra-articular steroid infections develop. years. Or until THA
Indications: Osteoarthritis injections prior to Total Hip 2/4 deep infections were revision for instability,
Setting: I Research Arthroplasty. Patients were preceded by multiple loosening, implant
Hospital matched to the Injection recurrent dislocations (both resection for deep
Location: USA Group (intervention) in injection group) infection, or death.
Dates: January 1998 May Standard preventive 2/4 deep infections also Minimum 2 years
2002 measures: NR had a chronic medical Average follow up
Inclusion Criteria: Patients condition (years)
with OA of the hip during 1/2 had a tracheostomy Injection: 2.7 (1.4)
the study dates. for sever obstructive sleep No Injection: 2.6 (1.6)
Exclusion Criteria: apnea and was on chronic Funding Source
Diagnosis of inflammatory anticoagulation for atrial Conflicts:
arthritis, connective tissue fibrillation & DVT and/or Authors: None
disorders, any history of pulmonary embolism. Institution: None
acetabular or femoral 1/2 had type II diabetes Study: None
fracture, any previous mellitus Supplies: None
surgery on the index hip, or
tumor of the acetabulum or No association was found
femur. between the average time
from intraarticular injection
to primary THA and the
development of Superficial
or Deep Infections
Overall average time
between steroid injection
and THA for injection
group: 112 (SD 81) days
2017 American Medical Association. All rights reserved. 523
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Superficial: 112 (SD 94)
days
Deep: 44 (SD 23) days
Probability value could not
be calculated because of
limited number of patients
with deep infections
Other infections: NR
Topic-specific outcomes:
NR
Reoperations:
Superficial infections
2/15 had surgical removal
of retained drains
2/15 had wounds incised
followed by irrigation and
debridement with
documentation of fascial
integrity
Deep Infections
3/3 treated with two-stage
exchange
1/3 treated by debridement
with prosthesis retention
and chronic suppression
with oral antimicrobial
therapy
Length of stay: NR
Mortality:
Unrelated to THA:
Injection: 12 (5.4%)
No Injection: 13 (5.8%)
Adverse events:
Revision for aseptic
loosening:
Injection: 5 (2.2%)
No Injection: 4 (1.8%)
Dislocations
2017 American Medical Association. All rights reserved. 524
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Injection: 6 (2.7%)
No Injection: 5 (2.2%)
Mean time to dislocation:
(yr.)
Injection: 1.41 (0.02-3.13)
No Injection: 1.54 (0.02-5)
4/11: demonstrated hip
stability with conservative
treatment
7/11: reoperations
Injection: 4 (1.8%)
No Injection: 3 (1.3%)
Papavas- Retrosp- To determine Number of patients: Intervention group: n=54 SSI Definitions:
iliou ective the rate of N=144 Patients who had received Superficial: 30 days Superficial incisional
161
2006 Concurr- infection in Patient Characteristics: one or more intra-articular Superficial wound infection: infection: an SSI which
(ES) ent patients who Age: NR injection of steroid in their Injection: 12/54 (22.2%) occurred within 30 days
Control had undergone Gender: NR operated knee No injection: 10/90 of surgery and involved
1, 2, 3, 4, TKR and to Obesity: NR (11.1%) only the skin or
5, 8 correlate this Comorbidities: NR Timing of intervention: P=0.1 subcutaneous tissue
rate with the Procedures: Total knee variable preoperatively around the incision.
pre-operative replacement Deep wound infection: 1 One of the following
use of intra- Indications: See exclusion Duration of intervention: year criteria had to be met:
articular criteria variable Injection: 3/54 (5.6%) 1) purulent drainage
steroids. Setting: 1 hospital No injection: 0 from the incision
Location: England Agent: Methylprednisolone- P<0.025 2) cultured organisms
Dates: February 2002 Steroid delivered via intra- from a swab or tissue
October 2004 articular injection in an All 3 deep infections were biopsy from the
orthopedic clinic, treated with long-term superficial wound layers.
Inclusion Criteria: All rheumatology clinic, or antimicrobial therapy and Deep Incisional
patients who underwent general practice setting revision surgery. infection: an SSI which
TKR during the study dates before surgery. All 3 deep infections had occurred within 30 days
Monitoring intervention: injections within 12 months. of surgery and involved
Exclusion Criteria: If NA only the skin or
records were incomplete, No relationship was found subcutaneous tissue
patients who had previous Control group: n=90 between the number or around the incision.
surgery on the affected Patients with no record of timing of injections and the One of the following
knee (other than having received an intra- risk of postoperative criteria had to be met:
arthroscopy), a diagnosis of articular injection of steroid infection 1) purulent drainage
inflammatory arthritis, before surgery. from the depths of the
2017 American Medical Association. All rights reserved. 525
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
immunosuppression, and a Other infections: NR incision
previous history of infection Standard preventive Topic-specific outcomes: 2) microbiological culture
around the knee, smoking measures: Recorded but NR from aseptically-
and diabetes. not reported. Reoperations: aspirated fluid, a swab
Revision surgery for deep or a tissue biopsy from
infection the deep-tissue layers or
Injection: 3/54 (5.6%) pus cells present on
No injection: 0 microscopy
P<0.025 3) a deep incision which
Length of stay: NR spontaneously dehisced
Mortality: NR or was deliberately
Adverse events: opened by a surgeon
Postoperative when the patient had a
o
investigations for deep temperature >38 C,
infection due to symptoms localized pain, or
of persistent pain or tenderness
swelling. 4) an abscess or other
Injection: 5/54 (9.3%) evidence of infection
No injection: 0 involving the deep
incision which was found
by direct examination,
during re-operation, or
by histopathological or
radiological examination
5) Diagnosis of a deep
incisional SSI by an
attending physician
Perioperative care: NR
Analytical
methodology: Chi-
squared test
Other notes:
A pilot study of 420
patients who had
received a TKR was
performed by reviewing
the records looking for
incidences of deep
2017 American Medical Association. All rights reserved. 526
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
infection: 6/420 (1.4%)
deep infections
occurred. 5/6 infections
had received an intra-
articular injection of
steroid prior to surgery.
Follow-up: NR
Funding Source
Conflicts:
Authors: None
Institution: None
Study: None
Supplies: None
Kaspar Retrosp- To determine Number of patients: N=80 Intervention group: n=40 SSI (mean follow up 29.8 Definitions
165
2005 ective the influence of (entire database 979) Received intra-articular months) Perioperative care
(ES) Concurr- intra-articular Patient Characteristics steroids prior to THA. Details Deep Infection Analytical
ent steroid injection Age mean SEM (Range) of injections were found from Injection: 4/40 (10%) methodology:
Control on the rate of y an examination of patients No Injection: 0 Descriptive statistics,
1, 2, 3, 4, surgical site Injection: 71.031.53 (45- receiving injections in the P=0.01 unpaired t-test, Fishers
5, 8 infection in 87) fluoroscopy suite. exact test for categorical
patients with No Injection: 70.551.50 Timing of intervention: Overall rate of established data, Kaplan-Meier
osteoarthritis (46-87) Preoperatively infections and possible survival analysis, and
undergoing Gender: m/f infections comparison of survival
subsequent Injection: 25/15 Duration of intervention: Injection: 12/40 (30%) plots by Mantel-Cox type
THA Obesity: BMI variable No Injection: 3/40 (7.5%) log-rank testing.
Injection: 28.580.72 (17- Other infections: NR Power analysis
39) Agent: Methylprednisolone Topic-specific outcomes: performed by univariate
No Injection: 29.940.77 80mg with 1-5ml of Time between most recent modeling.
(21-43) bupivacaine. Steroids injection and THA: mean Other notes: Study was
Comorbidities: Mean ASA delivered via intra-articular SEM (95%CI) underpowered
score for both groups was injection. Injections were Infection and/or infection
2.2 indicating most patients performed in a fluoroscopy test: 11.383.03 (5.6-17.2) Follow-up:
had few comorbidities suite under aseptic No Infection/ no infection Mean length of follow
Problems with the spine technique Test: 10.861.74 (7.2-14.5) up: 29.80.4 months
were present in P=0.878 Injection: 33.22.1
approximately half of the Monitoring intervention: Power: 0.053 months
population evenly NR No Injection: 30.21.6
distributed across groups. Total number of injections months
Control group: n=40 before THA mean SEM Funding Source
2017 American Medical Association. All rights reserved. 527
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study
Risk of Population and Setting Intervention Results Comments
(Data Objective
Bias
Extractor)
Score
Procedures: Total hip Did not receive intra-articular Infection and/or infection Conflicts:
arthroplasty steroid injections prior to test: 1.430.25 Authors: None
Cemented: 19 in each THA. Matched cohort. No Infection/ no infection Institution: None
group Patients were matched in Test: 1.460.11 Study: None
Non-Cemented: 21 in each descending order of priority P=0.891 Supplies: None
group by gender, cemented or Power: 0.052
cementless THA, age, BMI,
Indications: ASA pre-op score, year of Reoperations:
Osteoarthritis operation, and surgeon. Overall rate of revision
Injection: 1/40 (2.5%) Injection: 5/40 (12.5%)
No Injection: 1/40 (2.5%) Standard preventive No Injection: 1/40 (2.5%)
Inflammatory Arthritis measures: Recorded but Note: Authors report
Injection: 39/40 (97.5%) not reported revision rate of 1.02%
No Injection: 39/40 (10/979) for all unmatched
(97.5%) controls/primary THAs
performed at their hospital
Setting: 1 hospital over the study time period
Location: USA (excludes those with
Dates:1995 - 1998 primary THA performed
Inclusion Criteria: Patients elsewhere or before the
undergoing THA during the database was established).
study dates. Length of stay:
Exclusion Criteria: Injection: 6.580.49 (2-18)
prostatic malignancy, No Injection: 7.260.96 (4-
previous ipsilateral fracture 36)
of the hip or earlier surgery Mortality: NR
on the affected side. Also Adverse events: NR
patients who were
immunocompromised,
previously or presently
infected, affected with
cancer in the hip or
suspected tumors around
the hip or who had been
given an initial diagnosis of
osteoarthritis.
Q16. What are the most effective strategies for managing the preoperative use of intra-articular corticosteroid injections to reduce the risk of SSI in
prosthetic joint arthroplasty patients?
2017 American Medical Association. All rights reserved. 528
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Our search did not identify data that evaluated preoperative strategies for managing the use of intra-articular corticosteroid injections in prosthetic joint arthroplasty
patients and their impact on risk of SSI.
A. Does the length of time between intra-articular corticosteroid injection and prosthetic joint arthroplasty impact the risk of SSI? Our search did
not identify data that evaluated different lengths of time between preoperative intra-articular corticosteroid injection administration and its impact on the risk
of TKA.
B. Does the corticosteroid injection dose impact the risk of SSI? Our search did not identify data that evaluated different doses of preoperative intra-
articular corticosteroid injections and their impact on the risk of SSI.
2017 American Medical Association. All rights reserved. 529
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.2B.3 RISK OF BIAS ASSESSMENTS: Q12-16 SYSTEMIC IMMUNOSUPPRESSIVE THERAPY
eTABLE 61. Risk of Bias Assessments of Other Controlled Studies for Q12-16 Systemic Immunosuppressive Therapy
Attrition not Funding
All study groups significantly Statistical source(s)
derived from different Measure Investigator Potential adjustment for disclosed and
similar across of Measure of blinded to confounde- potential no obvious Overall
Author source/reference study exposure outcome is endpoint rs confounders conflict of Risk of
Year Q populations groups is valid valid assessment identified done interest Bias
Questions 12 16: Immunosuppressive Therapy
Bongartz
160 13 Low
2008
Bridges
158 13 Low
1991
Carpenter
159 13 Low
1996
Desai
162 15 Low
2009
Hirano
156 12 Low
2010
Kaspar
165 15 Low
2005
Kawakami
155 12 Low
2010
McIntosh
164 15 Low
2006
Momohara
154 12 Low
2011
Papavasil-
iou 15 Low
161
2006
Perhala
157 12 Low
1991
Sreekum-
ar 15 Low
163
2007
2017 American Medical Association. All rights reserved. 530
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.2C. Q17 ANTICOAGULATION
2.2C.1 GRADE TABLE: Q17 ANTICOAGULATION
eTABLE 62. GRADE Table for Q17 Anticoagulation
Increase
Decrease GRADE
GRADE
Large Magnitude
Overall
Publication Bias
Quantity GRADE of
Dose-response
GRADE
Study Quality
and Type Starting Evidence
Confounders
Consistency
Comparison Outcome Findings of
Directness
of GRADE for
Evidence
Precision
Evidence Outcome
Base
Q17. What are the most effective strategies for managing perioperative venous thromboembolism (VTE) prophylaxis to reduce the risk of SSI?
Q17A. Does the risk of SSI differ by individual VTE prophylaxis agent?
No difference in a meta-analysis of 4 RCTs
167-170
166 (N=7237) in primary or revision THA,
SSI* 1 SR High -1 0 -1 0 0 0 0 0 Low
Enoxaparin TKA, or hip fracture surgery: group: 29/3621
vs. (0.8%) vs. 37/3616 (1.0%). (11 day follow up)
Low
Fondapari-
nux Drug
related 166 No episode of decreased platelet count was
1 SR High -1 0 -1 0 0 0 0 0 Low
adverse reported in either group
events
No difference in a meta-analysis of 4 RCTs
(N=12,383): 28/6200 (0.5%) vs. 27/6183
2
(0.4%); OR: 1.03 (0.60 1.76); p=0.92; I =0;
30-35 day follow up
171-
171,172
4 RCT Two studies found no difference in THA
SSI* 174 High 0 0 0 0 0 0 0 0 High
(n=6890): 14/3453 (0.41%) vs. 16/3437
(0.47%). SSIs were rare (30 or 0.40%)
173,174
Two studies found no difference in TKA
Enoxaparin
(n=5493): 14/2747 (0.51%) vs. 11/2746
vs. High
(0.40%). Infections were rare (25 or 0.46%)
Rivaroxaban
No difference in 4 RCTs (THA and TKA
combined data) composite of excessive
Hemor-
wound hematoma and reported surgical site
rhagic 171-
4 RCT bleeding: 105/6200 (1.7%) vs. 100/6183
wound 174 High 0 0 0 0 0 0 0 0 High
(1.6%); p=NS
complic
171,172
Two studies found no difference in
ations
THA: 59/3453 (1.7%) vs. 54/3437 (1.6%); p
=NS
2017 American Medical Association. All rights reserved. 531
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Overall
Publication Bias
Quantity GRADE of
Dose-response
GRADE
Study Quality
and Type Starting Evidence
Confounders
Consistency
Comparison Outcome Findings of
Directness
of GRADE for
Evidence
Precision
Evidence Outcome
Base
173,174
Two studies found no difference in
TKA: 46/2747 (1.7%) vs. 46/2746 (1.7%);
p=NS
No difference in 4 RCTS modified intention to
treat analysis: 970/6200 (15.6%) vs.
Drug
171- 971/6183 (15.7%)
related 4 RCT
171,172
174 Two studies found no difference in High 0 0 0 0 0 0 0 0 High
adverse
THA: 15% both 514/3453 vs. 515/3437
events
173,174
Two studies found no difference in
TKA: (17% both) 456/2747 vs. 456/2746
1 large OBS study (N=2437) Logistic
regression analysis showed that enoxaparin
(started 12-24 hours postoperatively) was not
175
SSI* 1 OBS associated with increased risk of SSI in Low 0 0 0 -1 0 0 0 0 Very Low
primary THA; OR 2.11 (0.24-18.5); p=0.499;
or primary TKA: OR 1.07 (0.23-4.95);
p=0.932.
Enoxaparin
Logistic regression analysis showed that
vs. ASA and Very
enoxaparin (started 12-24 hours
mechanical Low
postoperatively) was associated with longer
prophylaxis
Time time until wound was dry for primary THA
until 175 (p<0.01) but not for primary TKA (p=0.62)
1 OBS Low 0 0 0 -1 0 0 0 0 Very Low
wound Patients on enoxaparin had longer time until
was dry wound was dry as compared to those on
ASA or those on warfarin; this difference was
th
significant on the 5 (p<0.01) but not by the
th
8 postoperative day.
Enoxaparin In a nested case-control study of TKA
vs. patients (n=36 infections, 106 controls)
Bemiparin specific anticoagulation agents were not
176 Very
vs. Fraxiparin PJI* 1 OBS associated with increased risk of SSI: p=0.97 Low 0 0 0 -1 0 0 0 0 Very Low
Low
vs. Only 50 of 5496 (0.91%) patients developed
Fondaparin- an SSI; (95% CI, 0.68%-1.20%).
ux Hematoma identified as an independent risk
2017 American Medical Association. All rights reserved. 532
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Overall
Publication Bias
Quantity GRADE of
Dose-response
GRADE
Study Quality
and Type Starting Evidence
Confounders
Consistency
Comparison Outcome Findings of
Directness
of GRADE for
Evidence
Precision
Evidence Outcome
Base
factor for PJI. Adjusted OR 4.2 (1.1-16.6)
No difference in retrospective study
Enoxaparin, (N=41,917) using administrative data from a
dalterparin, national sample of primary TKAs:
tinzaparin or 4366/37,198 (12%) vs. 559/4719 (12%);
177 Very
fondaparinux SSI* 1 OBS adjusted OR 1.08 (0.95-1.24). Low 0 0 0 -1 0 0 0 0 Very Low
Low
vs. ASA Authors indicated that subtherapeutic dosing
mechanical and/or inappropriate timing of the LMWHs or
prophylaxis synthetic Factor Xa inhibitor may have
impacted the results.
In a large (n=1742) study in primary
unilateral TKA, infections were rare 14/1742
(0.8%) and did not differ between groups:
9/957 (0.9%) vs. 5/785 (0.6%)
178
SSI* 1 OBS Goal INR: 1.6-2.2 for 6 weeks. Follow up was Low 0 0 0 -1 0 0 0 0 Very Low
Warfarin vs. 3 months.
No Study excluded patients already on
pharmacolo- preoperative anticoagulation therapy for Very
gic or other conditions. Low
mechanical Deep Deep SSIs were rare 8/1742 (0.5%) and did
178
prophylaxis Incision 1 OBS not differ between groups: 6/957 (0.6%) vs. Low 0 0 0 -1 0 0 0 0 Very Low
al SSI 2/785 (0.3%)
Superfic
Superficial SSIs were rare 7/1742 (0.4%) and
ial 178
1 OBS did not differ between groups: 3 (0.3%) vs. 3 Low 0 0 0 -1 0 0 0 0 Very Low
Incision
(0.4%)
al SSI
175
In a large OBS study (n=2437) of primary
Warfarin vs.
THA (n=1211) and TKA (n=1226), logistic
ASA 2 OBS
SSI* 175,177 regression analysis among THAs showed Low 0 0 0 0 0 0 0 0 Low Low
mechanical
that warfarin with a target INR of 2.0, started
prophylaxis
on the day of surgery, was not associated
2017 American Medical Association. All rights reserved. 533
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Overall
Publication Bias
Quantity GRADE of
Dose-response
GRADE
Study Quality
and Type Starting Evidence
Confounders
Consistency
Comparison Outcome Findings of
Directness
of GRADE for
Evidence
Precision
Evidence Outcome
Base
with an increased risk of wound infection OR
7.47 (0.62-89.3); p=0.112. On logistic
regression analysis, warfarin does not
appear as one of the variables influencing
wound infection after TKA. Follow up was not
reported
177
In a large OBS study (N=93, 840) of
administrative data on primary TKA,
subanalysis (n=56,642), showed no
difference; 6349/51923 (12%) vs. 559/4719
(12%); adjusted OR: 1.10 (0.96-1.26). Target
INR not reported. SSIs were detected at the
time of admission or on readmission within
30 days of index procedure.
Warfarin was not associated with longer time
with wound drainage after neither THA
Time (p=0.834) nor TKA (p=0.197)
until 175 Patients on enoxaparin had longer time until
1 OBS Low 0 0 0 -1 0 0 0 0 Very Low
wound wound was dry as compared to those on
was dry SAS or those on warfarin; this difference was
th
significant on the 5 (p<0.01) but not by the
th
8 postoperative day.
In a 2:1 case control study (N=154) of 78
cases who underwent revision THA or TKJA
for septic failure compared to 156 non-
infected controls who underwent the same
procedure, all on postoperative warfarin
Higher vs.
179 (target INR=1.5) found that while the mean Very
Lower Mean 1 OBS Low 0 0 0 -1 0 0 0 0 Very Low
PJI* INR at all time-points was higher in the Low
INR
infected group, it was not statistically
significant (p=0.06).
INR level was significantly higher in patients
with wound-related problems who later
developed infection (p=0.03)
2017 American Medical Association. All rights reserved. 534
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Overall
Publication Bias
Quantity GRADE of
Dose-response
GRADE
Study Quality
and Type Starting Evidence
Confounders
Consistency
Comparison Outcome Findings of
Directness
of GRADE for
Evidence
Precision
Evidence Outcome
Base
Twice as many infected patients with mean
INR >1.5 as compared to controls: 22% vs.
11%; p=0.05
Infected patients were more likely to have
INR>1.5 at time of hospital discharge; 17%
vs. 8%; p=0.04
INR>1.5 at time of hospital discharge was
more prevalent in group with wound
complications vs. those with uncomplicated
postoperative wound healing; 22% vs. 8%;
p=0.005
Multivariate logistic regression analysis
showed the following were significant risk
factors for PJI:
Wound complications including development
of hematoma: OR 27.02 (11.04-91.59); <0.01
Persistent wound drainage: OR 32.20 (8.7-
119.17); p<0.01
ASA comorbidities: OR 2.07 (1.08-0.97);
p=0.03
Postoperative transfusion: PR 1.63; (1.14-
2.33); p<0.01
13/78 (17%) of patients in the PJI cohort
were on anticoagulation therapy
preoperatively for another condition. These
patients were heparinized postoperatively
until fully coagulated with warfarin (target
INR = 2-3). 9/13 (69%) developed wound
complications including hematoma (n=3),
persistent wound drainage (n=5) and
delayed wound healing (n=1)
Wound Infected patients had a higher incidence of
179
hemato 1 OBS wound hematomas: 11 (14%) vs. 2 (1%); Low 0 0 0 -1 0 0 0 0 Very Low
ma p=0.0001.
2017 American Medical Association. All rights reserved. 535
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Overall
Publication Bias
Quantity GRADE of
Dose-response
GRADE
Study Quality
and Type Starting Evidence
Confounders
Consistency
Comparison Outcome Findings of
Directness
of GRADE for
Evidence
Precision
Evidence Outcome
Base
Wound
draina- Infected patients had a higher incidence of
179
ge- 1 OBS wound drainage: 24 (31%) vs. 4 (3%); Low 0 0 0 -1 0 0 0 0 Very Low
persist- p<0.01
ent
Q17B. What is the optimal timing and duration of perioperative VTE prophylaxis that also reduces the risk of SSI?
In a nested case-control study of TKA
patients (n=36 infections, 106 controls),
infected patients received the first dose of
anticoagulant within 12 hours (before or
Prophylaxis
after) of surgery more frequently than those
started
not infected: OR 1.5 (0.73-3.0).
preoperative- 176 Very
PJI* 1 OBS After adjusting by main risk factors, no Low 0 0 0 -1 0 0 0 0 Very Low
ly vs. Low
statistical association was found between
Postoperati-
close perioperative timing of the first dose of
vely
anticoagulant and risk of PJI.
Hematoma formation identified as an
independent risk factor for PJI. Adjusted OR
4.2 (1.1-16.6)
Q17C. How safe and effective is modifying the dose of the perioperative VTE prophylaxis agent to reduce the risk of SSI? Our search did not identify data that
evaluated the safety and effectiveness of modifying perioperative VTE prophylaxis and its impact on the risk of SSI.
*Critical outcome; OR: Odds Ratio; RR: Risk Ratio; CI: Confidence Interval
2.2C.2 EVIDENCE TABLE: Q17 ANTICOAGULATION
Q17. What are the most effective strategies for managing perioperative venous thromboembolism (VTE) prophylaxis to reduce the risk of SSI?
Q17A. Does the risk of SSI differ by individual VTE prophylaxis agent?
Q17B. What is the optimal timing and duration of perioperative VTE prophylaxis that also reduces the risk of SSI?
eTABLE 63. Evidence Table for Q17. What are the most effective strategies for managing perioperative venous
thromboembolism (VTE) prophylaxis to reduce the risk of SSI?
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
2017 American Medical Association. All rights reserved. 536
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
Turpie RCT To assess the Number of patients: Intervention group: SSI (follow up 41-50 days) Definitions
174
2009 1, 2, 3, 4, 5, efficacy and N=3034 n=1584 Postoperative wound SSI-NR
(ES) 7, 8, 9 safety of oral Patient Characteristics Rivarox: Patients assigned infection: Perioperative care: NR
rivaroxaban Age: mean (SD) y to receive 10 mg 1x/day Rivarox: 4/1526 (0.3%) Other notes: None
(Rivarox) 10mg Rivarox: 64.4 (9.7) rivaroxaban PO.in the Enox: 3/1508 (0.2%) Follow-up: for 30-35
RECORD once daily Enox: 64.7 (9.7) evening beginning 6-8h days after last dose of
4 compared with Gender: Female n (%) after wound closure or Other infections: NR anticoagulant. (41-50
30mg Rivarox: after adequate hemostasis Topic-specific outcomes days postop)
enoxaparin 1007/1526(66.0%) was achieved. Plus Hemorrhagic wound Funding Source
(Enox) given Enox: 1508/1508 (64.1%) placebo injection complications: Conflicts:
2
subcutaneously Obesity: mean (SD) kg/m Timing of intervention: Rivarox: 21/1526(1.4%) Authors: NR
every 12h for Rivarox: 30.9 (6.2) Preop Enox: 22/1508 (1.5%) Institution: NR
the prevention Enox: 30.7 (6.0) Duration of intervention: Study: Industry
of venous Comorbidities Postop until the evening Reoperations: NR Supplies: NR
thromboemboli History of VTE: before venography on Length of stay: days mean
sm after Rivarox: 38/1526(2.5%) POD 11-15 (SD)
elective total Enox: 28/1508 (1.9%) Device/agent: Rivarox: 8.0 (6.1)
knee Rivaroxaban Enox: 7.9 (6.3)
arthroplasty. Procedures: Total Knee Monitoring intervention:
Arthroplasty: n (%) NA Mortality:
Primary: Control group: n=1564 Rivarox: 6/1526 (0.4%)
Rivarox: 1488/1526 Enox: patients assigned to Enox: 6/1508 (0.4%)
(97.5%) receive 30mg
Enox: 1479/1508 (98.1%) subcutaneously every 12h Adverse events:
Revision: beginning 12-24h post Drug related Adverse
Rivarox: 37/1526 (2.4%) wound closure. Plus Events:
Enox: 28/1508 (1.9%) placebo tablet Rivarox: 310/1526
None or missing data Standard preventive (20.3%)
Rivarox: 1/1526 (0.1%) measures: NR Enox: 295/1508 (19.6%)
Enox: 1/1508 (0.1%)
Indications: NR
Setting: Multi-Center
Location: Bulgaria,
Canada, Denmark, India,
Israel, Lithuania, Pakistan,
Poland, Sri Lanka, Sweden,
USA,
Dates: June 2006
October 2007
Inclusion Criteria: Patients
2017 American Medical Association. All rights reserved. 537
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
18 and older scheduled for
total knee arthroplasty
Exclusion Criteria:
Patients with active
bleeding or a high risk of
bleeding, or any disorder
contraindicating the use of
enoxaparin or that might
necessitate enoxaparin
dose adjustment. Also
disorders preventing
bilateral venography,
clinically significant liver
disease, severe renal
impairment (creatinine
clearance <30ml/min),
concomitant use of drugs
that strongly inhibit
cytochrome P450 such as
protease inhibitors or
ketoconazole, pregnancy or
breastfeeding, planned
intermittent pneumatic
compression or the
requirement for ongoing
anticoagulant therapy.
Eriksson RCT To assess the Number of patients: Intervention group: SSI (follow up 66-77 days) Definitions:
171
2008 1, 2, 3, 4, 5, efficacy and N=4433 n=2266 Postoperative wound SSI - none
(ES) 7, 8, 9 safety of a Patient Characteristics Patients who received infection Perioperative care: NR
postoperative Age: mean (range) y 10mg oral rivaroxaban Rivarox: 8/2209 (0.4%) Other notes: None
RECORD 10-mg dose of Rivarox: 63.1 (18-91) 1x/day. Rivaroxaban was Enox: 8/2224 (0.4%) Follow-up: 30-35 days
1 rivaroxaban Enox: 63.3 (18-93) started 6-8h after wound after the last dose of the
(Rivarox) given Gender: female n (%) closure and administered Other infections: NR study drug. (60-77 days)
once daily as Rivarox: 1220/2209 every 22-26h in the Funding Source
compared with (55.2%) evening. Plus placebo Topic-specific outcomes: Conflicts:
a 40mg Enox: 1242/2224 (55.8%) injection Hemorrhagic wound Authors: Industry
subcutaneous Obesity: BMI mean (range) Timing of intervention: complications: Institution: NR
dose of Rivarox: 27.8 (16.2-53.4) Postop for Rivaroxaban & Rivarox: 34/2209 (1.5%) Study: Industry
enoxaparin (a Enox: 27.9 (15.2-50.2) pre and postop for Enox: 38/2224 (1.7%) Supplies: NR
low-molecular Comorbidities Enoxaparin
2017 American Medical Association. All rights reserved. 538
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
weight History of VTE Duration of intervention: Reoperations: NR
heparin), with Rivarox: 47/2209 (2.1%) 36 days postop (range 30-
the first Enox: 55/2224 (2.5%) 42) until patient had a Length of stay
[Enox]dose Procedures: Total Hip mandatory bilateral Mortality:
given the Arthroplasty venography. Although Death possibly related to
evening before Primary further thromboprophylaxis study drug
surgery and Rivarox: 2127/2209 was continued at the Rivarox: 3/2209 (0.01%)
subsequent (96.3%) investigators discretion. Enox: 1/2224 (0.04%)
doses given Enox: 2118/2224 (95.2%) Device/agent: 10mg oral
once daily, for Revision rivaroxaban or 40mg Adverse events:
extended Rivarox: 66/2209 (3.0%) subcutaneous injections of Drug related adverse
thromboprophyl Enox: 86/2224 (3.9%) enoxaparin. events
axis after Total Missing Data Monitoring intervention: Rivarox: 270/2209
Hip Rivarox: 16/2209 (0.7%) NA (12.2%)
Arthroplasty Enox: 20/2224 (0.9%) Control group: n=2224 Enox: 265/2224 (11.9%)
Patients who received
Indications: NR 40mg subcutaneous
Setting: Multi center injections of enoxaparin
Location: International: administered 1x/day. It
Argentina, Australia, was initiated 12h before
Austria, Belgium, Brazil, surgery and restarted 6-8h
Canada, Chile, Colombia, after wound closure then
Czech Republic, Denmark, administered every 22-26h
France, Finland, Germany in the evening. Plus
Greece, Hungary, Israel, placebo tablet
Italy, Lithuania, the Standard preventive
Netherlands, Norway, measures: NR
Poland, Slovakia, South
Africa, Spain, Sweden,
Turkey, United States.
Dates: February 2006
March 2007
Inclusion Criteria: men
and women at least 18
years of age who were
scheduled to undergo
elective total hip
arthroplasty.
Exclusion Criteria: Those
scheduled to undergo
2017 American Medical Association. All rights reserved. 539
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
staged bilateral THA, were
pregnant or breast-feeding,
had active bleeding or a
high risk of bleeding, or had
a contraindication for
prophylaxis with enoxaparin
or a condition that might
require an adjusted dose of
enoxaparin. Also conditions
preventing bilateral
venography, substantial
liver disease, severe renal
impairment (creatinine
clearance <30ml/min),
concomitant use of
protease inhibitors for the
treatment of human
immunodeficiency virus
infection, planned
intermittent pneumatic
compression, or a
requirement for
anticoagulant therapy that
could not be stopped.
Lassen RCT To conduct a Number of patients: Intervention group: SSI (follow up 40-49 Definitions:
173
2008 1, 2, 3, 4, 5, multicenter, N=1459 n=1220 days): SSI postoperative
(ES) 7, 8, 9 randomized, Patient Characteristics Rivarox: Patients who Postoperative infection of infection of wound was
double-blind Age: mean (Range) y received once daily oral wound classified according to
trial that Rivarox: 67.6 (28-91) rivaroxaban in a 10-mg Rivarox: 7/1220 (0.6%) the Medical dictionary
RECORD compares the Enox: 67.6 (30-90) tablet. Treatment was Enox: 11/1239 (0.9%) for Regulatory Activities
3 efficacy and Gender: female n (%) initiated 6-8h after wound (MEdDRA a registered
safety of oral Rivarox: 857/1220 closure. Then Other infections: NR trademark of the
rivaroxaban (70.2%) administered every 24h Topic-specific outcomes: International Federation
(Rivarox) 10mg Enox: 821/1239 (66.3%) until POD10-14. Further Hemorrhagic Wound of Pharmaceutical
once daily Obesity: BMI Mean thromboprophylaxis was Complications Manufacturers and
administered (RANGE) given at investigators Rivarox: 25/1220 (2.0%) Associations)
postoperatively, Rivarox: 29.5 (16.3-51.1) discretion according to Enox: 24/1239 (1.9%) Hemorrhagic wound
with those of Enox: 29.8 (16.0-54.3) local practice. complication: excessive
enoxaparin Comorbidities Timing of intervention: Reoperations: NR wound hematoma or
2017 American Medical Association. All rights reserved. 540
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
(Enox), 40mg History of VTE Postop Length of stay: bleeding at the surgical
given Rivarox: 48/1220 (3.9%) Duration of intervention: Rivarox: 48/1220 (3.9%) site.
subcutaneously Enox: 42/1239 (3.4%) from 6-8h after wound Enox: 42/1239 (3.4%) Perioperative care: NR
once daily closure until POD10-14 Other notes: None
administered Procedures: Elective total Device/agent: Mortality: Follow-up. 30-35 days
preoperatively, knee arthroplasty Rivaroxaban 10mg tablets Death after the last dose of
for the Primary: Monitoring intervention: Rivarox: 0/1201 (3.9%) medication. (POD 40-
prevention of Rivarox: 1176/1220 NA Enox: 6/1217 (3.4%) 49?)
venous (96.4%) Control group: n=1239 Funding Source
thromboemboli Enox: 1186/1239 (95.7%) Enox: Patients who Adverse events: Conflicts:
sm after Revision received a once-daily Drug related adverse Authors: Industry
elective total Rivarox: 24/1220 (2.0%) subcutaneous injection of events: Institution: NR
knee Enox: 30/1239 (2.4%) 40mg enoxaparin sodium. Rivarox: 146/1220 Study: Industry
arthroplasty None/Missing data This was initiated 12h (12.0%) Supplies: NR
Rivarox: 20/1220 (1.6%) before surgery and was Enox: 161/1239 (13.0%)
Enox: 23/1239 (1.9%) given again 6-8h after
Indications: NR wound closure, then
Setting: Multi-center administered every 24h.
Location: Austria, Belgium, Study medications were
Canada, China, Colombia, continued until at least
Czech Republic, Denmark, POD 10 and up to POD
France, Germany, Israel, 14. Further
Italy, Mexico, the thromboprophylaxis was
Netherlands, Poland, Peru, given at investigators
South Africa, Spain, discretion according to
Sweden. local practice.
Dates: February 2006 Standard preventive
November 2006 measures: NR
Inclusion Criteria: Patients
who were 18 years of age
or older and scheduled for
Total knee arthroplasty.
Exclusion Criteria:
Patients with active
bleeding or a high risk of
bleeding that
contraindicated the use of
low-molecular-weight-
heparin and patients with
any contraindication
2017 American Medical Association. All rights reserved. 541
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
necessitating adjustment of
its dose. Also, conditions
preventing bilateral
venography, clinically
significant liver disease,
concomitant use of
protease inhibitors of the
human immunodeficiency
virus or fibrinolytic agents,
planned intermittent
pneumatic compression,
requirement of ongoing
anticoagulation therapy,
and pregnancy or
breastfeeding.
Kakkar RCT To assess the Number of patients: Intervention group: SSI (follow-up 30-35 days) Definitions:
172
2008 1, 2, 3, 4, 5, efficacy of N=2457 (Safety n=1228; Postoperative wound Deep vein thrombosis
(ES) 6, 7, 8, 9 extended population) VTE= 961; Primary infections was assessed and
thromboprophyl N=1923 population for Efficacy=864 RivaRox: 8/1228 (0.7%) confirmed by ascending
axis with an major VTE RivaRox: Patients Enox: 6/1229 (0.5%) bilateral venography.
RECORD oral factor Xa N=1733 ITT population receiving extended In cases of suspected
2 inhibitor, for Primary Efficacy duration rivaroxaban as Other infections: pulmonary embolism,
rivaroxaban Patient Characteristics: thromboprophylaxis for 5 Infections and infestations: pulmonary angiography,
(RivaRox), for this information is for the weeks. Starting 6-8 hours RivaRox: 88/1228 (7.2%) perfusion/ventilation lung
31-39 days, safety population: after wound closure and Enox: 87/1229 (7.1%) scintigraphy with chest
compared with RivaRox: n=1228 continued for 31-39 days. radiography or spiral
a short-term Enox: n=1229 In addition, they received Topic-specific outcomes: computed tomography
LMWH Age: mean (SD, IQR) placebo injections for 10- Non-Fatal Pulmonary was done.
enoxaparin years 14 days starting 12h Embolism n (95%CI) Major bleeding: bleeding
(Enox) regimen RivaRox: 61.4 (13.2, 53- before surgery. RivaRox: 1/864 (0.1%, that was fatal, into a
for 10-14 days 71) Timing of intervention: <0.1-0.6) critical organ (e.g.
followed by Enox: 61.6 (13.7, 54-72) pre and postoperative Enox: 4/869 (0.5%, 0.1- retroperitoneal,
placebo in Gender: female (%) Duration of intervention: 1.2) intracranial, intraocular,
patients RivaRox: 667 (54.3%) begun 6-8 hours after Absolute Risk Reduction: intra-spinal), required re-
undergoing Enox: 651 (53.0%) wound closure and (95%CI) operation, or clinically
total hip Obesity: BMI mean (SD, continued for 31-39 days. 0.3% (-0.2-1.1), p=0.37 overt extra-surgical-site
arthroplasty IQR) Agent: Oral rivaroxaban bleeding associated with
(THA) RivaRox: 26.8 (4.8, 23.5- (10mg) once daily Deep vein thrombosis in a fall in hemoglobin of
This is known 29.4) Monitoring intervention: Safety Population 20g/L or more,
2017 American Medical Association. All rights reserved. 542
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
as the Enox: 27.1 (5.2, 23.6- Liver biochemistry and RivaRox: 37/1228 (3.0%) calculated from the
RECORD 2 30.0) cardiovascular adverse Enox: 86/1229 (7.0%) POD1 baseline value or
study Comorbidities: events were monitored requiring infusion of two
Regulation of Previous history of VTE throughout the treatment Deep-vein Thrombosis in or more units of whole
Coagulation in RivaRox: 10 (0.8%) and follow-up periods. ITT population: n (95%CI) blood or packed cells.
Orthopaedic Enox: 20 (1.6%) Mandatory bilateral RivaRox: 14/864 (1.6%, On-treatment non-major
surgery to Duration of surgery: median venography the day after 0.9-2.7) bleeding any on-
prevent Deep- (IQR) (min) the last dose of the study Enox: 71/869 (8.2%, 6.4- treatment bleeding event
vein thrombosis RivaRox: 95.0 (72-125) mediation (day 32-40) 10.2) not adjudicated as major
and pulmonary Enox: 93.0(73-126) Control group: n=1229; Absolute Risk Reduction: bleeding
embolism) VTE: 962; Primary (95%CI) Hemorrhagic wound
Procedures: Elective Hip Efficacy=869 6.5% (4.3-8.5), p<0.0001 complications:
Arthroplasty (THA) Enox: Patients receiving composite of excessive
Previous Orthopedic the heparin-based Proximal DVT: n (95%CI) wound hematoma and
Surgery thromboprophylaxis RivaRox: 5/864 (0.6%, surgical-site bleeding
RivaRox: 225 (18.3%) Enoxaparin for 2 weeks. It 0.2-1.3) Any post-operative
Enox: 232 (18.9%) was initiated 12h before Enox: 44/869 (5.1%, 3.7- bleeding: bleeding
Primary surgery and restarted 6-8 6.7) starting after the first
RivaRox: 1160 (94.5%) hours after wound closure. Absolute Risk Reduction: tablet intake and ending
Enox: 1157 (94.1%) And continued for 10-14 (95%CI) up to 2 days after the
Revision POD. Patients also 4.5% (2.9-6.0), p<0.0001 last intake of study
RivaRox: 52 (4.2%) received placebo tablets Distal DVT: n (95%CI) medication.
Enox: 50 (4.1%) for 31-39 days starting 6- RivaRox: 9/864 (1.0%, Safety Analysis: patients
Missing/no surgery 8h after surgery. 0.5-2.0) who received at least 1
RivaRox: 16 (1.3%) Standard preventive Enox: 27/869 (3.1%, 2.1- dose of medication
Enox: 22 (1.8%) measures: NR 4.5) Modified ITT population:
Nonstandard preventive Absolute Risk Reduction: patients who were valid
Indications: NR measures: (95%CI) for safety analysis, had
Setting: Multicenter (123 Use of cement 2.0% (0.7-3.3), p=0.0025 undergone planned
centers) RivaRox: 621 (50.6%) surgery, and had
Location: Multinational (21 Enox: 608 (49.8%) Major venous adequate assessment of
countries worldwide) thromboembolism: n thromboembolism.
Dates: February 2006 (95%CI) Patients valid for
April 2007 RivaRox: 6/961 (0.6%, assessment of major
Inclusion Criteria: Patients 0.2-1.4) venous
enrolled during the study Enox: 49/962 (5.1%, 3.8- thromboembolism
dates aged 18 years or 6.7) those valid for safety
older, scheduled to undergo Absolute Risk Reduction: analysis and in whom
elective THA. (95%CI) the venograms were
Exclusion Criteria: Those 4.5% (3.0-6.0), p<0.0001 evaluable for the
2017 American Medical Association. All rights reserved. 543
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
scheduled to undergo proximal veins,
staged bilateral hip Symptomatic venous irrespective of whether
arthroplasty, who had thromboembolism: n they were valid for distal
active bleeding or a high (95%CI) veins
risk of bleeding, or had any RivaRox: 3/1212 (0.2%, Perioperative care: NR
condition contraindicating <0.1-0.7) Analytical
the use of enoxaparin, or Enox: 15/1207 (1.2%, 0.7- methodology:
that might require 2.0) Mantel-Haenszel
enoxaparin dose Absolute Risk Reduction: weighting stratified by
adjustment, including (95%CI) country with
severe renal impairment. 1.0% (0.3 -1.8), p=0.0040 corresponding
Also including significant asymptotic two-sided
liver disease, pregnancy or Symptomatic venous 95%CI and two-sided p
breastfeeding, concomitant thromboembolism in follow- value. Unweighted RR
use of HIV protease up period: n (95%CI) reduction calculated with
inhibitors, use of fibrinolytic RivaRox: 1/1212 (0.1%, an asymptotic method.
therapy or planned <0.1-0.5) Sensitivity analysis: 1)
intermittent pneumatic Enox: 2/1207 (0.2%, <0.1- included all randomized
compression during the 0.6) patients with evaluable
study period, conditions Absolute Risk Reduction: bilateral venography
preventing bilateral (95%CI) (irrespective of whether
venography, or the 0.1% (-0.2-0.4), p=0.62 it was in the time
requirement for an window) or a confirmed
anticoagulant that could not Major on-treatment symptomatic/asymptoma
be discontinued. bleeding tic event/death
RivaRox: 1/1228 (<0.1%) irrespective of the time
[hemorrhagic diarrhea and window. 2) All
hematemesis and resulted randomized participants
in discontinuation of included in Sensitivity
rivaroxaban; patient analysis 1. Plus those
received acetylsalicylic acid who had evaluable
w/o gastric protection bilateral venography/
before surgery] ultrasonography as done
Enox: 1/1229 (<0.1%) by the investigator,
[Blood in cerebrospinal irrespective of the time
fluid. Deemed not related to window, or a
study drug but enoxaparin symptomatic/
was discontinued] asymptomatic event/
Non-Major on-treatment death, irrespective of the
bleeding: time window, provided
2017 American Medical Association. All rights reserved. 544
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
RivaRox: 80/1228 (6.5%) the symptomatic event
Enox: 67/1229 (5.5%) was not adjudicated. To
Clinically relevant non- be a non-event by the
major bleeding committee.
RivaRox: 40/1228 (3.3%) Other notes: Sample
Enox: 33/1229 (2.7%) size based on event rate
Any bleeding after initiation of 11% in Enoxaparin
of placebo or Rivaroxaban: group. And a RR of 40%
RivaRox: 56/1197 (4.7%) in rivaroxaban. Thus 914
Enox: 49/1193 (4.1%) patients per group would
be enough to
Patients receiving blood demonstrate a
transfusion: Reduction in RR with a
RivaRox: 485/1228 power of 90%
(39.5%)
Enox: 514/1229 (41.8%) Follow-up: 30-35 days
after the last dose of
medication
Reoperations: No major Funding Source
bleeding events leading to Conflicts:
reoperation in either group Authors: Industry
Length of stay: NR Institution: NR
Mortality up to day 30-42: Study: Industry
Death: n (95%CI) Supplies: NR
RivaRox: 2/864 (0.2%,
<0.1-0.8) (both of
cardiovascular cause)
Enox: 6/869 (0.7%, 0.3-
1.5) (one of pulmonary
embolism, 4 unrelated to
venous thromboembolism,
one unexplained)
Absolute Risk Reduction:
(95%CI)
0.5% (-0.2-1.1), p=0.29
Death in follow-up period: n
(95%CI)
RivaRox: 0/1228 (0.0%,
0.0-0.3)
Enox: 2/1229 (0.2%, <0.1-
2017 American Medical Association. All rights reserved. 545
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
0.6)[one to pulmonary
embolism, one
unexplained]
Absolute Risk Reduction:
(95%CI)
0.2% (-0.1-0.6), p=0.50
Adverse events
Any on treatment adverse
event:
RivaRox: 768/1228
(62.5%)
Enox: 807/1229 (65.7%)
Drug related adverse
events:
RivaRox: 245/1228
(20.0%)
Enox: 249/1229 (20.3%)
Drug related serious on-
treatment adverse events
RivaRox: 13/1228 (1.1%)
Enox: 17 (1.4%)
Serious on-treatment
adverse events:
RivaRox: 90/1228 (7.3%)
Enox: 131/1229 (10.7%)
Adverse events leading to
discontinuations:
RivaRox: 46/1228 (3.8%)
Enox: 64/1229 (5.2%)
Edema peripheral
RivaRox: 55/1228 (4.5%)
Enox: 48/1229 (3.9%)
2017 American Medical Association. All rights reserved. 546
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
Turpie Meta- To perform a Study types and number: Intervention group: SSI: Definitions
166
2002 Analysis meta-analysis N=4 n=3668 Wound infection (by day VTE: deep vein
(ES) 3, 4 of 4 Phase III clinical trials: 4/5 Efficacy population: = 11) thrombosis, pulmonary
randomized, 2682 Fond: 37/3616 (1.0%) embolism or both up to
double-blind Number of total patients Fond: Patients Enox: 29/3621 (0.8%) day 11.
trials using the in the review: N=7344 administered Bleeding index: the sum
same Efficacy Population: Fondaparinux as an Complications at surgical of the number of units of
comparative N=5385 anticoagulant site leading to prolonged packed red blood cells
drug 4/4 studies: fondaparinux hospitalization or re- or whole blood
(Enoxaparin Inclusion criteria: 4 was administered at2.5mg hospitalization: transfused and the
[Enox] and multicenter, randomized, qd with the time of first Fond: 52/3616 (1.4%) difference of the
Fondaparinux double blind studies. injection 6h2h postop and Enox: 52/3621 (1.4%) hemoglobin values
[Fond]), end Exclusion criteria: NR the time to second (g/dL) before and after
points (venous Databases searched: NA injection 12h after first the bleeding occurrence
thromboemboli Studies were all dose. Other infections: NR (i.e. bleeding
sm, and conducted as a part of the Timing of intervention: Topic-specific outcomes: index=units of
proximal deep Phase 3 studies in a clinical Postoperatively Patients treated for VTE by transfusion +
vein trial program. Eriksson: 2001 if surgery day 11: hemoglobin before
thrombosis), Aggregate summary was delayed 24-48h after Fond: 199/3616 (5.5%) bleeding hemoglobin
and score: NR admission, fondaparinux Enox: 351/3621 (9.7%) after bleeding)
adjudication was initiated 122h P<0.001 Fatal bleeding: bleeding
committee and Eriksson 2001 Hip preoperatively (68/626 Venous thromboembolism: that was retroperitoneal,
to report the Fracture (19.9%)). Omission of Fond: 182/2682 (6.8%) intracranial, intraspinal
results of the Lassen 2002 Hip preop injections was Enox: 371/2703 (13.7%) or involved any other
meta-analysis. Replacement recommended in both Any deep vein thrombosis critical organ,
Turpie 2002 Hip cohorts if a spinal or Fond: 174/2677 (6.5%) Perioperative care: NR
Replacement epidural anesthesia, or Enox: 363/2698 (13.5%)
Bauer 2001 Major Knee catheterization was Any Proximal Deep Vein Other notes: None
Surgery planned. Thrombosis
Eriksson 2003 Hip Lassen: Fondaparinux was Fond: 35/2756 (1.3%) Follow up:
Fracture initiated a mean of 6.25h Enox: 81/2775 (2.9%) wound infection: 11 days
after surgery in 86% of Distal Deep Vein (wound infection and
patients Thrombosis VTE)
Turpie: Fondaparinux was Fond: 141/2704 (5.2%) entire study: 49 days
initiated a mean of 6.5h Enox: 293/2709 (10.8%) (PE)
after surgery in 92% of
patients. All odds ratios favor Funding Source
Bauer: Fondaparinux was Fondaparinux regarding Conflicts:
initiated a mean of 6.25h Surgery type, Obesity, age, Authors: Industry
in 94% of patients gender, type of anesthesia, Institution: NR
2017 American Medical Association. All rights reserved. 547
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
Duration of intervention: use of cement or duration Study: NR
for 5-9 days of surgery with no Supplies: NR
postoperatively or until a significant difference seen
mandatory bilateral in odds ratios for variations
venography was in these factors.
performed to assess for a Common Odds Ratio
new VTE after a minimum between studies favors
5-day hospital stay Fondaparinux with regards
Agent: Fondaparinux to VTE:
-55.2 (-63.1 to -45.8);
Monitoring intervention: p<0.001
NR
Control group: n=3676 Post-hoc analysis of
Efficacy population = timing of Fondaparinux
2703 injection:
Enox: Patients A statistically significant
administered enoxaparin relationship was shown
as an anticoagulant. between the timing
2/4 Studies: enoxaparin in (between 3-9 hours postop)
st
40mg qd with time of 1 of the first fondaparinux
injection 12h2h injection and major
preoperatively bleeding (p=0.008)
2/4 studies: enoxaparin in A statistically significant
st
30mg qd with time of 1 relationship also existed
injection 12-24h between the incidence of
postoperatively overt bleeding associated
1/4 studies: Time to with a bleeding index 2
second injection 12-2h and the timing of the first
postop fondaparinux injection
3/4 studies: time to second (p=0.008)
injection NR Efficacy was not affected by
Standard preventive this timing: p=0.67
measures:
Other thromboembolic Re-operations: See
prophylaxes: Intermittent Infections
pneumatic compression, Length of stay: See
dextran and thrombolytic infections
or anticoagulant agents Mortality
were prohibited; centers Fatal bleeding
2017 American Medical Association. All rights reserved. 548
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
were instructed to avoid Fond: 0/3616
the use of aspirin or Enox: 1/3621 (0.0%)
nonsteroidal anti- Death from any cause
inflammatory drugs when Fond: 15/3616 (0.4%)
possible; other antiplatelet Enox: 21/3621 (0.6%)
agents were prohibited Death from any cause up to
Graduated compression 49 days
stockings: use was Fond: 48/3616 (1.3%)
allowed and physiotherapy Enox: 52/3621 (1.4%)
was recommended
Length of administration: Adverse events:
investigators could extend Adjudicated bleeding
prophylaxis during follow- events up to day 11:
up with any currently Fond: 96/3616 (2.7%)
available therapy, but only Enox: 63/3621 (1.7%)
after a venography was P=0.008
performed.
VTE: after occurrence, Bleeding into critical organ
treatment was left to the Fond: 0/3616
surgeons discretion. Enox: 1/3621 (0.0%)
Bleeding leading to another
operation
Fond: 12/3616 (0.3%)
Enox: 8/3621 (0.2%)
Bleeding with a bleeding
index2
Fond: 84/3616 (2.3%)
Enox: 53/3621 (1.5%)
Any Transfusions
Fond: 1950/3616 (53.9%)
Enox: 1864/3621 (51.5%)
P=0.04
2017 American Medical Association. All rights reserved. 549
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
Asenio Prospective To investigate Number of patients: Intervention group: n=36 SSI (Follow up 6 months Definitions:
176
2010 concurrent the N=5496 Patients who underwent postop) Prosthesis infection:
(ES) control with independent Nested Case Control: TKA and developed a For total population of CDC definitions an
a nested effect of Low N=142 prosthetic joint infection. 5496: infection involving the
case Molecular Patient Characteristics: Timing of intervention Prosthetic infection periprosthetic tissues
control Weight Heparin for case control patients First Dose of LMWH incidence rate: 0.91 and
1, 2, 3, 4, 5, (LMWH) timing Age: meanSD y Preoperatively cases/100 patients Infection: Occurring
6, 7, 8 for Deep Intervention: 71.36.1 48h operated (95%CI 0.68-1.2) within the first 6 months
Venous Control: 71.48.5 Intervention: 0 Infection rate ranged from postop and meeting at
Thrombosis Gender male n (%) Control: 2 (1.9%) 0.25%-2.34% by center least 1 of the following
(DVT) Intervention: 13 (36.1%) 24-48h (p=0.14) criteria:
prophylaxis Control: 30 (28.3%) Intervention: 0 1. an organism was
related to the Obesity Control: 1 (1%) 68% of infections were isolated from a culture of
start of surgery Intervention: 23 (63.9%) 13-24h identified post-discharge. fluid or tissue aseptically
on the risk of Control: 66 (62.3%) Intervention: 12 (33.3%) Time from procedures to obtained from an
prosthesis Comorbidities Control: 31 (29.8%) infection median: 37 days incision deliberately
infection Diabetes mellitus 7-12h (IQR: 16-63) opened by the surgeon
among patients Intervention: 10 (27.8%) Intervention: 3 (8.3%) Early Postoperative 2. an abscess or other
undergoing Control: 13 (12.3%) Control: 6 (5.8%) Infection: 46% evidence of infection
Total Knee OR:2.83 (1.08-7.38) 6h was detected on direct
Arthroplasty p=0.03 Intervention: 0 Adjusted OR for examination, either
(TKA). Other Hypertension: Control: 1 (1%) independent risk factors for during reoperation or by
objectives were Intervention: 27 (75%) POSTOPERTIVELY infection: histopathological or
to establish the Control: 64 (60.4%) 6h Diabetes: 3.2 (95%CI:1.2- radiographic
risk of OR: 2.07 (0.86-5.0); Intervention: 3 (8.3%) 8.8) examination,
prosthesis p=0.10 Control: 6 (5.8%) Hematoma formation: 4.2 3. prosthesis infection
infection and 7-12h 95%CI (1.1-16.5) was diagnosed by a
their Procedures: Total knee Intervention: 10 (27.8%) surgeon or attending
microbiological arthroplasty (TKA) Control: 29 (27.9%) Other infections: NR physician.
characteristics Non-Primary Arthroplasty 13-24h Topic-specific outcomes: Early prosthesis
and to evaluate Intervention: 2 (5.7%) Intervention: 4 (11.1%) Bleeding infection: an
the relative Control: 4 (4.0%) Control: 17 (16.4%) Intervention: 12 (33.3%) organ/space wound
effect of other Surgery duration 24-48h Control: 32 (30.2%) infection that developed
potential risk Intervention: 112.834.2 Intervention: 4 (11.1%) within 1 month
factors. Control: 121.443.1 Control: 11 (10.6%) Wound Hematoma postoperatively.
Timing of any dose of Intervention: 19 (52.8%) Late Prosthesis
Indications: NR LMWH Control: 50 (47.6%) infection: a prosthesis
Within 24h preop OR:3.58 (0.96-13.40) infection that developed
Setting: Multicenter (13 Intervention: 15(41.7%) p=0.06 between 1-6 months
Spanish hospitals) Control: 41 (38.7%) postop.
2017 American Medical Association. All rights reserved. 550
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
Within 24h postop Reoperations: NR Perioperative care: NR
Location: Spain Intervention: 31 (86.1%) Length of stay: NR Analytical
Control: 89 (84.0%) Mortality: NR methodology Univariate
Dates: January 1, 2005 Adverse events: NR logistic regression,
December 31, 2006 Duration of intervention: paired t-test, multiple
variable conditional logistic
Inclusion Criteria: All Agent: Low Molecular regression modal was
patients undergoing primary Weight Heparin (LMWH). developed from a
TKA or total knee Doses received were saturated model
replacement in 13 Spanish stratified related to the containing all non-
traumatology surgical units time of surgery, and the correlated risk factors
during the study dates. time interval relative to that were significant at
Exclusion Criteria: surgical time. the .1 level. Only cases
Patients with infected Enoxaparin that could be matched to
prostheses. Intervention: 19 (52.8%) controls were included in
Control: 50 (47.6%) the risk factor analysis.
Bemiparin Other notes: None
Intervention: 8 (22.2%) Follow-up: Active
Control: 26 (24.8%) surveillance by surgeons
Fraxiparin and/or hospital
Intervention: 7 (19.4%) epidemiologists during
Control: 23 (21.9%) the 6 months post-op
When clinical records
Fondaparinux- NOT a did not provide enough
LMWH; synthetic information to rule out
pentasaccharide factor Xa infection during the first
inhibitor 6 months, patients were
Intervention: 2 (5.6%) interviewed by
Control: 6 (5.7%) telephone. Investigators
P=0.97 extracted all information
Monitoring intervention: from medical records
NA Funding Source
Control group: n=106 Conflicts:
For every intervention Authors: None
patient who developed an Institution: None
infection, 3 control patients Study: None
were chosen who did not Supplies: None
develop an infection within
the first 6 postoperative
months. Patients were
2017 American Medical Association. All rights reserved. 551
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
matched by medical center
and date of index case
procedures 2 weeks.
Standard preventive
measures:
AMP: AMP were given
across patients, however,
timing was not standard
and breaks down as
follows:
>2h preop
Intervention: 2 (5.6%)
Control: 12 (11.3%)
2h preop
Intervention: 29 (80.6%)
Control: 84 (79.2%)
Postop
Intervention: 5 (3.9%)
Control: 10 (9.4%)
Non-Standard preventive
measures:
Hair Removal P=0.07
between groups
Shaving not done
Intervention: 6 (22.2%)
Control: 25 (28.7%)
Blade Razor
Intervention: 8 (29.6%)
Control: 12 (13.8%)
OR:3.3 (0.26-42.1)
Electrical Clipper
Intervention: 13 (48.1%)
Control: 50 (57.5%)
OR: 0.18 (0.02-2.24)
Normothermic Blanket
Intervention: 8 (22.2%)
Control: 38 (35.8%)
OR: 0.30 (0.09-1.01)
p=0.05
2017 American Medical Association. All rights reserved. 552
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
Bozic Retrospect- To utilize Number of patients: Intervention group: SSI (30 days) Definitions:
177
2010 ive administrative N=93,840 Aspirin (n=4719): Patients Wound infection TKA ICD-9-CM
(ES) concurrent data from a Patient Characteristics who received aspirin Aspirin: 559/4719 (12%) procedure code 81.45
cohort large national Age: mean (SD) y mechanical prophylaxis Injectable: 4366/37.198 Postoperative
1, 2, 3, 4, 5, sample of Aspirin: 66.4 (10.7) and no other (12%) complications, including
6, 7, 8 patients Injectable: 66.5 (10.5) pharmacologic VTEP Warfarin: 6349/51,923 venous
undergoing Warfarin: 67.3 (10.4) agent (12%) thromboembolism (any
primary total P<0.001 Timing of intervention: thromboembolic event
knee Gender: male n (%) NR SSI population: n=1037 including proximal or
arthroplasty Aspirin: 1679 (36%) Duration of intervention: Adjusted ORs (95%CI) distal DVT as well as
(TKA) to Injectable: 12,505 (34%) NR Aspirin as referent PE), proximal DVT and
compare the Warfarin: 18,085 (35%) Agent: Aspirin, Warfarin, Injectable: 1.08 (0.95- PE only; surgical site
risk of venous Obesity: or Injectable VTEPs 1.24) bleeding; and surgical
thromboemboli Aspirin: 833 (18%) (LMWH Enoxaparin] or Warfarin: 1.10 (0.96-1.26) site infection were
sm (VTE), Injectable: 5105 (14%) fondaparinux [Factor Xa defined using ICD-9-CM
surgical site Warfarin: 6454 (12%) inhibitor] Other infections: NR diagnosis codes recoded
bleeding, Comorbidities Monitoring intervention: Topic-specific outcomes: during the index
surgical site Diabetes: NA Any thromboembolism admission as well as
infection (SSI), Aspirin: 754 (16%) Control group: Aspirin: 110 (2.3%) principal diagnosis
and mortality Injectable: 6561 (18%) Warfarin (n=51,923): Injectable: 1152 (3.1%) associated with any
between Warfarin: 8839 (17%) patients who received Warfarin: 2009 (4%) readmissions occurring
patients who Deficiency anemia Warfarin as the VTEP P<0.01 for all w/in 30 days of
received Aspirin: 456 (10%) Injectable (n=37,198): comparisons discharge.
aspirin, Injectable: 5056 (14%) Patients who received Adjusted ORs (95%CI) Perioperative care: NR
warfarin, or Warfarin: 5824 (11%) VTEP with injectable n=3271
injectable Aspirin patients had lower agents (e.g. LMWHs or Aspirin as referent Analytical
(LMWH and baseline VTE risk score fondaparinux) Injectable: 1.03 (0.76- methodology
fondaparinux) than warfarin or Standard preventive 1.39) Alternating logistic
VET LMWH/fondaparinux measures: NR Warfarin: 1.36 (1.02 -1.82) regression models were
Prophylaxis patients (p<0.001) P<0.01 for all used to assess the
(VETP) Aspirin Patients had fewer comparisons independent association
medical comorbidities than between the 3 VTEP
Injectable (p<0.001) but Proximal DVT or PE strategies and the risk of
similar to Warfarin Patients Aspirin: 77 (1.6%) complications or death.
(p=0.69) Injectable: 901 (2.4%) A Propensity score was
Aspirin patients less likely Warfarin: 1632 (3%) used in all models due to
to have a charge for P<0.01 for all the threat of bias from
sequential compression comparisons group allocation. The
devices in perioperative Adjusted ORs (95%CI) resultant c-statistic was
period: n=2610 0.725 which was
2017 American Medical Association. All rights reserved. 553
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
Aspirin 38% Aspirin as referent included in all core
LMWH/fondaparinux 48% Injectable: 0.99(0.76-1.28) multivariable models as
Warfarin 55% Warfarin: 1.34 (1.05 -1.70) a covariate intended to
(p<0.001) P<0.01 for all adjust for allocation bias.
Procedures: Total knee comparisons In a secondary analysis,
arthroplasty (TKA) 3 propensity scores,
Indications: NR Bleeding related to wound including assignment to
Setting: Multicenter (307 site injectable VTEP vs.
Hospitals participating in a Aspirin: 30 (0.6%) other VETP, etc. These
proprietary database Injectable: 459 (1%) scores did not
developed for measuring Warfarin: 548 (1%) substantially nor
quality and healthcare use P<0.01 for all directionally alter the
in hospitalized patients) comparisons results, thus the first
The centers are Adjusted ORs (95%CI) propensity score was
predominantly small to n=1037 used.
midsize nonteaching Aspirin as referent Other notes: None
facilities serving a largely Injectable: 1.11 (0.77- Follow-up: 30 days
urban patient population. 1.60) Funding Source
Location: USA Warfarin: 0.97 (0.65 -1.47) Conflicts:
Dates: October 2003 - Authors: None
September 2005 Ultrasound or venogram Institution: None
Inclusion Criteria: Patients any time after operative day Study: None
admitted during the study (n, %) Supplies: None
dates, were 18 years old, Aspirin: 1 (0.02%)
and had primary TKA as Injectable: 73 (0.20%)
their principal procedure Warfarin: 28 (0.05%)
during their hospitalization
Exclusion Criteria: Use of pneumatic
Patients with no charges for compression
any VTEP treatments, and devices
those who had charges for Aspirin: 1795 (38%)
VTEP treatments in Injectable: 17,756 (48%)
formulations representing Warfarin: 28,757 (55%)
therapeutic rather than
prophylactic Reoperations: NR
anticoagulation. Length of stay: median
(IQR)
Aspirin: 1 (3-4)
Injectable: 4 (3-4)
Warfarin: 3 (3-4)
2017 American Medical Association. All rights reserved. 554
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
P<0.001
Patients on Aspirin also
more likely to be
discharged home (vs. an
extended care facility)
Aspirin 30%
LMWH/fondaparinux 23%
Warfarin: 21%
P<0.001
Mortality:
Aspirin: 9 (0.2%)
Injectable: 45 (0.1%)
Warfarin: 54 (0.1%)
Adjusted ORs (95%CI)
n=109
Aspirin as referent
Injectable: 0.63 (0.30-
1.34)
Warfarin: 0.54 (0.25-1.15)
Adverse events: NR
Parvizi Retrospect- To determine Number of patients: Intervention group: n=78 SSI (adjusted results Definitions:
179
2007 ive Case whether N=234 Cases: Patients who when possible; Periprosthetic infection:
(ES) Control patients Patient Characteristics developed periprosthetic unadjusted otherwise) patient has at least 3 of
1, 2, 3, 5, 6, receiving Age: meanSD (years) infection Mean duration between 5 of the following criteria:
7, 8 excessive Cases: 6610 index joint arthroplasty and 1) abnormal serology
anticoagulation Controls: 6610 Timing of intervention: development of infection (erythrocyte
(an Gender: female (%) pre-and postoperatively was 256 days (range 4- sedimentation rate of
international Cases: 36 (46%) 1890 days) >30mm/h; C-reactive
normalized Control: NR Duration of intervention: protein level of >1mg/dL)
ratio [INR] of Obesity: BMI >30 kg/m2 given on the day of Multivariate analysis: 2) Strong clinical and
greater than Cases: 44 (56%) surgery and continued for Risk factors for radiographic suspicion
clinically Control: 80 (51%) a period of 6 weeks. periprosthetic infection for periprosthetic
2
intended level) BMI 9kg/m (meanSD) If patient a) was on (OR (95%CI) infection
were at risk for Cases: 329 anticoagulation before ASA score 3) positive joint
developing Controls: 327 surgery for other 2.07 (1.08-0.97); p=0.03 aspiration culture for
wound-related Comorbidities: conditions b) had known Postoperative Transfusions: infection
problems, ASA Score (meanSD) allergy to warfarin, or c) 1.63 (1.14-2.33); P=0.007 4) evidence of purulence
which in turn, Cases: 2.60.57 developed Postoperative wound during the subsequent
predisposes Controls: 2.40.56 thromboembolism in the complications including surgical intervention
them to P=0.01 postoperative period; the development of hematoma: 5) Positive intraoperative
2017 American Medical Association. All rights reserved. 555
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
periprosthetic Diabetes mellitus patient was given either 27.02 (11.04-91.59); culture.
infection. Cases: 14 (18%) subcutaneous and/or p=0.0002 Wound discharge
Ultimately, this Control: 22 (14%) intravenous heparin as the Wound Drainage: beyond POD 7 was
study is to Steroid Therapy sole or the bridging agent 32.20 (8.7-119.17); deemed clinically
examine the Cases: 8 (10%) until adequate and full p<0.0001 significant and
correlation Control: 5 (3%) anticoagulation (goal INR- abnormal.
between P=0.03 2-3) with oral agent could Other infections: NR Perioperative care: NR
anticoagulation NNIS1 be established Topic-specific outcomes:
and Cases: 50 (64%) Wound Hematoma Analytical
periprosthetic Control: 73 (47%) Agent: All patients in both Cases: 11 (14%) methodology:
infection. P=0.01 groups were given low- Control: 2 (1%) Wilcoxon procedure: to
SURGICAL DATA dose warfarin (goal P=0.0001 perform unadjusted
Total Transfusion: INR=1.5) unless indicated Wound Drainage analysis to compare
meanSD otherwise Cases: 24 (31%) means across
Cases: 0.781.15 Control: 4 (3%) continuous variables.
Controls: 0.390.79 Monitoring intervention: P=0.0001 Fisher exact test:
P=0.002 INR Other Complications compare proportions
Allogeneic Transfusion (including PE, DVT & UTI) across categorical
Cases: 10 (13%) Control group: n=156 Cases: 18 (23%) variables.
Control: 3 (2%) Controls: Patients Control: 18 (12%) T-statistics for
P=0.0006 undergoing TKA or THA P=0.02 continuous variables
for categorical
2
Autologous Transfusion who underwent same Received injectable
Cases: 47 (60%) index procedure but did anticoagulant in addition to variables
Control: 111 (71%) not develop a subsequent oral Multivariate stepwise
P=0.09 infection. Cases: 13/78 (16.7%) logistic regression was
(including 1 LMWH) used to perform adjusted
Procedures: Standard preventive Received intravenous analysis
Primary TKA: measures heparin: Other notes: None
Cases: 33/78 (%) AMP: Cephalosporin or an Cases: 13/74 (16.7%) Follow-up: NR
Controls: NR alternative for patients with 9/13 heparinized resulted in Funding Source
Revision TKA: penicillin allergies was would complications Conflicts:
Cases: 10/78 (%) administered within 60 Hematoma: 3/9 Authors: None
Controls: NR minutes of arthroplasty Persistent wound Institution: None
Primary THA: procedure and continued drainage: 5/9 Study: None
Cases: 12/78 (%) for 24h postop. Delayed wound healing: Supplies: None
Controls: NR Antimicrobial was 1/9
Revision THA administered at a mean of
Cases: 23/78 (%) 39 min pre-incision. INR
Controls: NR Mean INR>1.5
Cases: 16 (21%)
2017 American Medical Association. All rights reserved. 556
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
Indications: Degenerative Control: 17 (11%)
P=0.05; =3.97
2
joint arthritis was the most
common diagnosis in both INR at day of
groups. Discharge>1.5
Posttraumatic arthritis: Cases: 13 (17%)
4/234 (1.7%) Control: 12 (8%)
P=0.04; =4.39
2
Inflammatory arthropathy:
2/234 (0.9%) INR>1.5 on day of
Setting: 1University discharge
Hospital Wound complications:22%
Location: USA No Wound Complications:
8%
Dates: 2000 - 2005 P=0.005
Inclusion Criteria: All INR level was statistically
patients undergoing primary higher in patients with
or revision total knee (TKA) wound-related problems
or total hip arthroplasty who later developed
(THA) for an aseptic infection compared with
diagnosis. patients who did not
Exclusion Criteria: NR develop infection (p=0.03)
Reoperations:
Cases: 14 (18%)
Control: 3 (2%)
OR: 11.2; p<0.0001
Indications for reoperations
included:
CASES:
Evacuation of hematoma:
9/14 (64.3%)
Debridement and wash out
of draining wound: 3/14
(21.4%)
Debridement and closure
for wound dehiscence: 2/14
(14.3%)
CONTROLS
Evacuation of hematoma:
2/3 (66.7%)
Delayed wound healing:
1/3: (1%)
2017 American Medical Association. All rights reserved. 557
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
Length of stay:
Cases: 6 (Range 1-11)
days
Controls: 4 (range 2-6)
days
P=0.006
Mortality: NR
Adverse events
Wound dehiscence
developed in 2 patients
both of whom later
developed infection
Patel Retrospect- The purpose of Number of patients: Intervention group: n=25 SSI (unadjusted Follow Definitions:
175
2007 ive this study is to N=2437 Patients undergoing Up NR) Normal Weight: BMI
24.9 kg/m
2
(ES) concurrent identify Patient Characteristics THR(n=15) or TKR (n=10) Overall: 25/2412 (1.0%)
control pharmacologic Age: mean (years) assigned to receive THA: 15/1211 (1.2%) Overweight: BMI 25-29.9
2
1, 2, 3, 5, 6, factors Infected THA: 59.1 Warfarin, LMWH or aspirin [5/15 had cellulitis which kg/m
7, 8 (prophylaxis Uninfected THA: 60.1 at the surgeons resolved with Obese: BMI 30.0-39.9
2
against deep Infected TKA: 63.1 preference who developed antimicrobials. 10/15 had kg/m
venous Uninfected TKA: 66.5 a postoperative wound persistent drainage despite Morbidly Obese: BMI
40 kg/m
2
thrombosis), Gender: m/f infection 3 days IV antimicrobials
surgical factors Infected THA: 0.6%/1.2% and underwent operative Length of stay: time/date
(estimated Infected TKA: 0.3%/1.0% Timing of intervention: irrigation and debridement] of admission to
blood loss and Obesity: NR postoperative TKA: 10/1226 (0.8%) time/date of discharge
surgical time), Comorbidities: NR [7/10 had cellulitis which (as determined by the
and patient Duration of intervention: resolved with surgeon) either to home
specific factors Procedures: variable antimicrobials; 2/10 or to a rehabilitation
(BMI and drain Total Hip Arthroplasty required component setting.
output) that are (THA):1211 Agent: removal due to persistent The surgical wound was
associated with Total knee arthroplasty Warfarin: target infection; 1/10 underwent inspected daily with
the time until (TKA): 1226 international normalized operative irrigation and notation made of when
postoperative ratio (INR)= 2.0 debridement due to infected the wound appeared dry
wound is dry Indications: NR Low-Molecular-Weight- hematoma but joint according to the
following Heparin(LMWH): started components were retained] definition of Weiss and
primary total Setting: 1 tertiary care between 12-24 hours Logistic regression analysis Krackow. Wound was
joint teaching hospital. postop of variables influencing considered actively
arthroplasty, Aspirin (ASA): 325mg in wound infection after THA: draining if a 2x2-cm
and to Location: USA conjunction with OR(95%CI) area of gauze covering
determine pneumatic compression Time until wound dry: the wound was wet or if
whether Dates: January 1997 July devices started the 1.42 (1.18-1.71); p<0.001 fluid was noted to be
2017 American Medical Association. All rights reserved. 558
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
prolonged 2004 morning after surgery. Coumadin vs. aspirin and originating from the site.
wound pneumatic compression (spotting on gauze was
drainage Inclusion Criteria: Primary Monitoring intervention: devices: not considered to be
results in a unilateral total hip and total NA 7.47 (0.62-89.3); p=0.112 actively draining)
longer hospital knee arthroplasties in who LMWH vs. aspirin and Perioperative care: NR
stay or closed suction drains had Control group: n=2412 pneumatic compression Analytical
increases the been utilized and who had Patients undergoing THR devices: methodology: Multiple
risk of early a normal coagulation (n=1196) or TKR (n=1216) 2.11 (0.24-18.5); p=0.499 linear regression
postoperative profile. assigned to receive analysis was used to
wound Exclusion Criteria: NR Warfarin, LMWH or aspirin Logistic regression analysis model the effects of
infection. at the surgeons of variables influencing prophylaxis against deep
preference who developed wound infection after TKA: venous thrombosis
a postoperative infection OR(95%CI) (DVT), BMI, age, & type
BMI: 1.08 (1.01-1.16); of anesthesia on time to
Standard preventive p=0.018 a dry wound.
measures: LMWH vs. aspirin and Multiple logistic
Drains: were removed at pneumatic compression regression analysis was
36 hours postop or devices: used to calculate the OR
whenever drain output 1.07 (0.23-4.95); p=0.932 between postop infection
during any 8-h shift fell Other infections: NR and the time to a dry
below 25mL. Topic-specific outcomes: wound while controlling
AMP: routine preoperative Regression Analysis of for DVT prophylaxis,
and postoperative variables influencing Time BMI, surgical time, EBL
prophylactic antimicrobials until wound was dry after 7 Drain output.
(cefazolin if patient was THA: Other notes: None
not allergic to penicillin, LMWH: Coefficient = 0.318 Follow-up: NR
otherwise, clindamycin) P=0.027 (compared with Funding Source
including at least 30min aspirin group) Conflicts:
prior to initial incision. Morbidly Obese: Coefficient Authors: None
= 0.667; P=0.001 Institution: None
Drain Output: Coefficient Study: None
0.002; P=<0.001 Supplies: None
Statistically Significant
variables influencing Time
until wound was dry after
TKA:
Drain Output: coefficient =
0.0003; P=0.023
Drain output:
THA group: every additional
2017 American Medical Association. All rights reserved. 559
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
100-mL increase in postop
drain output resulted in an
additional 0.20 day of
wound drainage time.
TKA group: every additional
100-mL increase in postop
drain output resulted in an
additional 0.03 day of
wound drainage time.
Reoperations:
THA: 10/1211 (0.8%)
10/15 underwent
operative irrigation and
debridement
TKA: 3/1226 (0.2%)
2/3 required component
removal due to persistent
infection; 1/3 underwent
operative irrigation and
debridement due to infected
hematoma but joint
components were retained
Length of stay:
There was a strong positive
correlation between the
length of hospital stay and
the number of days until
surgical wound was dry:
r=0.29; p<0.001
THA: r=0.34; p<0.001
TKA: r=0.26; p<0.001
Mortality: NR
Adverse events: NR
2017 American Medical Association. All rights reserved. 560
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
Sachs Retrospect- To determine Number of patients: Intervention group: SSI (follow-up 3 months) Definitions: NR
178
2003 ive the safety and N=1742 n=957 Overall:
(ES) concurrent efficacy of 6 Patient Characteristics Received low-dose Warfarin: 9/957 (0.94%) Perioperative care:
control weeks of low- Age: Median Age for both warfarin as No Prophylaxis: 5/785 Patients were
1, 2, 3, 4, 5, dose warfarin groups was 70 years. thromboprophylaxis (0.64%) encouraged to undergo
6 when Gender: both groups Superficial infection spinal anesthesia
compared with included approximately Timing of intervention: Warfarin: 3 (0.4%) [two
no 44% men and 56% women Postoperative required readmission and Analytical
thromboprophyl Obesity: NR IV antimicrobial therapy; methodology: Chi-
axis in total Comorbidities: NR Duration of intervention: one treated with an oral square analysis, Mann-
knee 6 weeks antimicrobial and Whitney test
arthroplasty Procedures: Unilateral, developed wound necrosis
using infection Primary Total Knee Agent: low-dose warfarin and required readmission Other notes: None
and Arthroplasty (TKA) maintained at an and plastic surgery]
complication international normalized No Prophylaxis: 3 (0.3%) Follow-up: 3 months
rates as the Indications: NR ration (INR) from 1.6-2.2 [two required readmission postop
primary for 6 weeks and IV antimicrobials]
outcome Setting: Multicenter Deep Wound Infection Funding Source
measures Monitoring intervention: Warfarin: 6 (0.6%) [6 Conflicts:
Location: USA NR required surgery, 5 with Authors: None
Dates: 1995 - 2000 successful resolution; 1 Institution: None
Control group: n=785 required 5 subsequent Study: None
Inclusion Criteria: Patients Patients received no surgeries without Supplies: None
who were treated with thromboprophylaxis. While resolution; 1 developed
postoperative warfarin as in the hospital, this group necrosis requiring
recorded in the records of did not receive any aspirin readmission and surgery for
the warfarin clinic during or NSAIDs and were not wound coverage and
the study dates. Patients placed on any type of closure]
underwent total knee venous compression No Prophylaxis: 2 (0.3%)
arthroplasty and were device. [both required readmission
operated on by one of 4 and surgery]
surgeons who were using Standard preventive Wound Necrosis(described
warfarin on an unselected measures: above)
basis for several years. Postoperative protocol: Warfarin: 2 (0.2%)
Controls were identified Continuous passive No Prophylaxis: 0 (0%)
who were treated without motion (CPM), physical
any chemical or mechanical therapy, and weight Total Complication Rate
thromboprophylaxis and bearing, as well as most (including infections)
were operated on by 1 of 3 orders for pain control and Warfarin: 17 (2.2%)
surgeons whose routine nausea were essentially No Prophylaxis: 45 (4.7%)
2017 American Medical Association. All rights reserved. 561
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
was to avoid the same for all patients. P<0.01
thromboprophylaxis during Both groups received One or more complication
TKA initial wound care from a Warfarin: 5%
Exclusion Criteria: small group of orthopedic No Prophylaxis: 2%
Patients undergoing special care nurses who Other infections:
bilateral or revision TKA, performed dressing Pneumonia
patients on warfarin changes, suture removal Warfarin: 5 (0.5%)
prophylaxis for previous and wound observations No Prophylaxis: 1 (0.1%)
chronic arterial fibrillation or for the first month after Topic-specific outcomes:
thromboembolic events surgery. DVT
Warfarin: 2 (0.2%) [two
calf vein DVTs]
No Prophylaxis: 0 (0%)
PE
Warfarin: 1 (0.1%)
[required readmission]
No Prophylaxis: 2 (0.3%) [
these two events were non-
fatal occurring within initial
hospitalization and resolved
with treatment
Reoperations:
Subsequent surgeries
Warfarin: 11 (1.1%)
No Prophylaxis: 2 (0.3%)
=4.66; P<0.01
2
Length of stay- NR
Mortality:
Deaths (within 90 days)
Warfarin: 1 (0.1%); patient
admitted 1w postop with GI
bleed, unsuccessful
attempts to control resulted
in myocardial infarction and
death
No Prophylaxis: 2 (0.3%);
1 in 91yo patient who
sustained a fata myocardial
infarction 5w postop; 1 in a
73yo patient without prior
2017 American Medical Association. All rights reserved. 562
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study
Population and Setting Intervention Results Comments
(Data Risk of Objective
Extractor) Bias Score
history of cardiac disease
readmitted in congestive
heart failure 11 days
postoperatively, contracted
pneumonia and expired
None due to
thromboembolic disease
Adverse events:
New Arrhythmia
Warfarin: 6 (0.6%)
No Prophylaxis: 1 (0.1%)
All recovered
Angina
Warfarin: 5 (0.5%)
No Prophylaxis: 0 (0%)
MI
Warfarin: 3 (0.3%)
No Prophylaxis: 2 (0.3%)
TIA
Warfarin: 1 (0.1%)
No Prophylaxis: 1 (0.1%)
CVA
Warfarin: 2 (0.2%)
No Prophylaxis: 1 (0.1%)
GI Bleeding
Warfarin: 3 (0.3%)
No Prophylaxis: 0 (0%)
Other
Warfarin: 7 (0.7%)
No Prophylaxis: 4 (0.5%)
Q17C. How safe and effective is modifying the dose of the perioperative VTE prophylaxis agent to reduce the risk of SSI? Our search did not identify data
that evaluated the safety and effectiveness of modifying perioperative VTE prophylaxis and its impact on the risk of SSI.
2017 American Medical Association. All rights reserved. 563
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.2C.3. RISK OF BIAS ASSESSMENTS OF STUDIES: Q17 ANTICOAGULATION
eTABLE 64. Risk of Bias Assessment of Systematic Reviews for Q17 Anticoagulation
Database Number of Studies Funding
s included/ screened Heterogenei- Characterist- source(s)
described excluded by two Data Individ- ty between ics of disclosed
and two studies independe- extracted ual study results included and no
Search or more Inclusion/ along with nt by two study assessed studies obvious
terms database- exclusion reasons of reviewers independe- quality qualitatively Publicati- reported in conflict Overall
Author describe es criteria exclusion for nt assess- and/or on bias evidence of Risk of
Year Q -ed searched described described inclusion reviewers ed quantitatively assessed table interest Bias
Question 17: Anticoagulation
Turpie
166 17 High
2002
eTABLE 65. Risk of Bias Assessments of Randomized Controlled Trials for Q17 Anticoagulation
Funding
Outco- Attrition source(s)
Described Randomizat- Describ- me smaller than disclosed and
as ion ed as assess- Study 10-15% of Attrition no obvious Overall
Author randomiz- appropriately double- or participant Investiga- Attrition assigned appropriate- conflict of Risk of
Year Q ed performed blind blinded blinded tor blinded described patients ly analyzed interest Bias
Question 17: Anticoagulation
Eriksson
171 17 Low
2008
Kakkar
172 17 Low
2008
Lassen
173 17 Low
2008
Turpie
174 17 Low
2009
eTABLE 66. Risk of Bias Assessments of Other Controlled Studies for Q17 Anticoagulation
Attrition not Funding
All study groups significantly Investigator Statistical source(s)
derived from different Measure blinded to Potential adjustment for disclosed and
similar across of Measure of endpoint confoun- potential no obvious Overall
Author source/reference study exposure outcome is assessme- ders confounders conflict of Risk of
Year Q populations groups is valid valid nt identified done interest Bias
Question 17: Anticoagulation
Asensio
176 17 Low
2010
Bozic 17 Low
2017 American Medical Association. All rights reserved. 564
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Attrition not Funding
All study groups significantly Investigator Statistical source(s)
derived from different Measure blinded to Potential adjustment for disclosed and
similar across of Measure of endpoint confoun- potential no obvious Overall
Author source/reference study exposure outcome is assessme- ders confounders conflict of Risk of
Year Q populations groups is valid valid nt identified done interest Bias
177
2010
Parvizi
179 17 Low
2007
Patel
175 17 Low
2007
Sachs
178 17 Low
2003
2017 American Medical Association. All rights reserved. 565
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.2D. Q18 ORTHOPAEDIC SPACE SUIT
2.2D.1. GRADE TABLE: Q18 ORTHOPAEDIC SPACE SUIT
eTABLE 67. GRADE Table for Q18 Orthopaedic Space Suit
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
Quantity GRADE of Overall
Dose-response
Study Quality
and Type Starting Evidence GRADE of
Confounders
Consistency
Comparison Outcome Findings
Directness
of GRADE for Evidence
Precision
Evidence Outcome Base
Q18. How safe and effective are orthopaedic space suits in reducing the risk of SSI in prosthetic joint arthroplasty patients and then which healthcare
personnel should wear them?
One retrospective study (N=8288) in TKA
using Medicare claims data, found no
difference in risk of deep SSI requiring
reoperation within 90 days of surgery:
Deep 0.28% (0.11-0.46) vs. 0.38% (0.20-0.55);
SSI RR 0.75 (0.34-1.62)
require- 180 Deep Infections identified through ICD9-
1 OBS Low 0 0 0 -1 0 0 0 0 Very Low
ng CM diagnosis codes for multiple joint/bone
reopera- infection, debridement, and implant
tion* removal codes (not revision total joint
arthroplasty codes). In this study deep
infection might be referring to PJI.
Use of laminar flow varied between
Space Suit groups.
Very Low
vs. No suit One study large joint registry study
(N=88,311) with multiple subgroup
analyses, found use of space suits was
associated with an increased number of
deep SSIs requiring revision surgery within
Deep
6 months of THA or TKA (P<0.01) but this
SSI
181 evidence is limited in size (only 96 events
require- 1 OBS Low 0 0 0 -1 0 0 0 0 Very Low
or 0.109%):
ng
The results did not differ in the presence
revision*
or absence of laminar flow
Deep SSI in this study might be referring
to PJI.
60% of primary procedures used
antimicrobial impregnated cement.
2017 American Medical Association. All rights reserved. 566
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
Quantity GRADE of Overall
Dose-response
Study Quality
and Type Starting Evidence GRADE of
Confounders
Consistency
Comparison Outcome Findings
Directness
of GRADE for Evidence
Precision
Evidence Outcome Base
One small study (N=62) evaluating
contamination using space suit or
conventional gowns with single hood plus
surgical mask, during THA or hip
hemiarthroplasty reported only 1 deep SSI
in the exhaust suit group (11 days postop)
but this evidence is limited in size: 1/31
Deep 182
(3.2%) vs. 0/31. (24 month follow up).
1 OBS Low 0 0 0 -1 0 0 0 0 Very Low
SSI*
Statistical significance was not reported.
HEPA filtration was present in both study
groups.
Deep SSI was not defined-in this study
might be referring to incisional SSI
Study was designed to evaluate
contamination
One study (14,484) found no difference in
risk of superficial SSI for patients
undergoing THA or hip hemiarthroplasty: 1
(3.2%) superficial SSI in each group at 16
Superfi- 182
1 OBS and 15 days postoperatively, respectively. Low 0 0 0 -1 0 0 0 0 Very Low
cial SSI
Follow up 24 months.
Statistical significance was not reported.
HEPA filtration was present in both study
groups.
*Critical outcome; OR: Odds Ratio; RR: Risk Ratio; CI: Confidence Interval
2017 American Medical Association. All rights reserved. 567
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.2D.2. EVIDENCE TABLE: Q18 ORTHOPAEDIC SPACE SUIT
eTABLE 68. Evidence Table for Q18. How safe and effective are orthopaedic space suits in reducing the risk of SSI in
prosthetic joint arthroplasty patients and then which healthcare personnel should wear them?
Author Study
Year Design Study Population and
Intervention Results Comments
(Data Risk of Objective Setting
Extractor) Bias Score
Hooper Retrospe- To review Number of Intervention group: SSI (Follow up: 6 Definitions:
181
2011 ctive the New patients: N=88,311 Intervention1: Space Suit months) SSI- deep (joint
(ES) concurre- Zealand Primary THR: n=20,385 Unadjusted results: space)
nt control Joint 51,485 THR: 21% (n=10,811) THR Revision due to
1, 2, 3, 4, Registry to Primary TKR: TKR: 26% (n=9,574) Early revision for deep early infection: any
5, 6, 8 determine if 36,826 Intervention2: Laminar infection: such procedure
the use of Patient Flow Theater: n=30,983 46/51485 (0.089%) performed within
laminar flow Characteristics: THR: 33% (n=16,990) Intervention1- Space 6months of the
and recorded, not TKR: 38% (n=13,993) Suit: 0.186% initial operation
protective reported but Note: Authors only Control1-No Space Suit: Perioperative
suits with narrative details that provide percentages; n 0.064% care: NR
hoods and there were no was calculated. P<0.0001 Analytical
self- significant Intervention3: Both Space Intervention2- Laminar methodology:
contained differences in clinical Suit and Laminar Flow- Flow theater: 0.148% Percentages with
exhaust details between the Numbers not reported Control2-conventional revision for deep
systems groups and there (See Other Notes) theater: 0.061% infection were
(space suits) was similar duration Timing of intervention: P<0.003 compared between
would of operations intraoperative Intervention3-BothSpace groups using the
reduce the Age: NR Duration of suit + laminar flow: Chi-squared test or
rate of early Gender: NR intervention: 0.198% Fishers exact test
deep Obesity: NR intraoperative Control3 -Neither No when expected
infection Comorbidities: NR Device: either laminar air Space suit in a frequencies were
requiring a Procedures: Total flow or protective suits conventional OR: 0.053% low. A p-value of
revision Hip replacement with hoods and self- P<0.001 <0.05 was
procedure (THR) and total contained exhaust From Figure 1c (Bar considered
following knee replacement systems (space suits) or Graph- details not reported significant
total hip (TKR) and revisions both. in text) Other notes:
(THR) and due to early Laminar Flow: All Conventional OR: There was a steady
knee (TKR) infections. hospitals confirmed that Suit: ~0.15% increase in the use
replacement Indications: they had a regular No Suit: 0.053% of intervention
s at 10 Osteoarthritis: 94% maintenance program for Laminar Flow OR: procedures and In
years for both THR and filters. There were no Suit: 0.198% 2008 almost half of
TKR hospitals which used No Suit:~ 0.10% all procedures were
Inflammatory laminar flow combined P values for above NR performed in
Arthritis: with a complete surgical SURGEON SPECIFIC laminar-flow
THR: 3% enclosure. SURGICAL PRACTICE theaters with space
TKR: 4% Space Suits: All the suits INFECTION RATES suits
2017 American Medical Association. All rights reserved. 568
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
Intervention Results Comments
(Data Risk of Objective Setting
Extractor) Bias Score
Setting: Multi-center were contemporary in 33 surgeons did or did not The registry
(64 hospitals) design and no surgeon wear space suits captures 98% of
Location: New worked in a fully-enclosed Intervention1 (with space both primary and
Zealand space. No surgeon suit): 0.082% revision
Dates: 1999-2008 worked with all staff in the Control1 (without space arthroplasties
Inclusion Criteria: theater. suit) :0.057% performed in New
All primary THR & Monitoring intervention: P=0.755 Zealand and
TKR and revisions NR 43 surgeons performed records revision
due to early Control group: n=NR more than 50 operations in procedures
infections with full Control1: (n=67,926) both operating secondary to deep
information on THR or TKR performed environments infection.
theater environment without Space Suit Intervention2(Laminar
and a minimum THR: 79% (n=40,674) Flow): 0.110% Surgeon
follow up of 6 TKR: 74% (n=27,252) Control2 (Conventional Questionnaire:
months. Control2: (n=57,328)THR OR): 0.028% They compared
Specifically or TKR performed In P<0.03 rates for surgeons
surgeons who had Conventional theater 30 surgeons used both who used space
experience in both THR: 67% (n=34,495) space suit AND laminar suits in both
conventional and THR:62% (n=22,833) flow or neither operating room
laminar-flow Control3: in conventional Intervention3 (space suit settings (laminar
operating theaters theater with no space suit AND laminar flow): flow and
and who had Standard preventive 0.1035% conventional) and
performed at least measures: Control3 (NO space suit completed at least
50 procedures in Non-standard AND conventional OR): 50procedures in
both. Also surgeons preventive measures: 0/3598 procedures each (similar
who had used AMP: in New Zealand, P=0.09 surgical practices).
space-suits in both prophylactic TKR Questionnaire
settings and who antimicrobials are given Early revision for deep requested
had completed at for most THR and TKR infection: information on
least 50 procedures procedures. (Registry 50/36826 (0.136%) frequency of suit
in each shows 96%) Intervention1- Space use, members of
Exclusion Criteria: Antimicrobial agent in Suit: 0.243% the team who wore
NR cement: Registry data Control1-No Space Suit: them, whether
shows 60% utilization 0.098% practice changed
rate P<0.001 depending on OR
Intervention2- Laminar team and whether
Flow theater: 0.193% they wore full suits
Control2-conventional or just
theater: 0.100% hood/exhaust
P<0.019 system.
2017 American Medical Association. All rights reserved. 569
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
Intervention Results Comments
(Data Risk of Objective Setting
Extractor) Bias Score
Intervention3-Both Space
suit AND Laminar Flow: Discussion
0.25% comments
Control3-Neither (No regarding potential
Space suit AND reasons for
Conventional OR): 0.087% increased rate of
P<0.001 infection with use of
From Figure 2c (Bar space suit include:
Graph- details not reported Observers in OR
in text) have noted
Conventional OR: surgeons often
Suit: ~0.25% adjust suit or hood
No Suit:0.087 % during procedure
Laminar Flow OR: and subsequently
Suit: 0.25% unknowingly
No Suit:~0.12 % contaminate their
P values for above NR gloves.
SURGEON RELATED Exhaust system
INFECTION RATES there is no
23 surgeons space suits: information as to
Intervention1 (Space the flow of the
suit): 0.251% expelled air from
Control1 (No Space exhaust systems
suit):0.028% and whether air is
P=0.016 concentrated with
32 surgeons performed debris and
more than 50 operations in significant numbers
both operating of colony forming
environments units close to the
Intervention2 (Laminar surgical site.
Flow): 0.147%
Control2 (Conventional Follow-up:
OR): 0.189% Minimum 6 months
P=0.597 Funding Source
Conflicts:
NOTE: One hospital of 64 Authors: None
was identified as having a Institution: None
significantly increased rate Study: None
of revision for early deep Supplies: None
infection when the use of a
2017 American Medical Association. All rights reserved. 570
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
Intervention Results Comments
(Data Risk of Objective Setting
Extractor) Bias Score
conventional theater and
no space suit was
compared with laminar
flow with a space suit. The
hospital contributed only a
small number to the
database and when these
were removed from the
analysis, there was no
change in the significance
of the results.
Other infections: NR
Topic-specific
outcomes:
Surgeon Questionnaire
35/60 (58.3%) response
rate
Space suit used in all
replacement procedures:
35/35
Surgical technique the
same regardless of
laminar flow vs.
conventional OR: 35/35
Full space suit: 28/31
OR team members
wearing full suit: surgeon,
assistant and scrub nurse.
OR team members NOT
wearing space suit:
anesthetist or technician
Reoperations: All
infections were
reoperations
Length of stay: NR
Mortality: NR
Adverse events:
Surgeon Questionnaire:
Spatial awareness limited
by hood (space suit)
2017 American Medical Association. All rights reserved. 571
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
Intervention Results Comments
(Data Risk of Objective Setting
Extractor) Bias Score
Easier to contaminate
themselves while wearing
space suit since there was
an apparent false sense of
security within it
Miner Retrospe- To assess Number of Intervention group: SSI (follow up 90 days) Definitions:
180
2007 ctive the current patients: N=8288 Intervention1: n=3538 Unadjusted results SSI-deep prosthetic
(ES) concurre- effects of procedures Patients in Hospitals Overall 90-day cumulative joint infection
nt control laminar which used exhaust suits incidence of deep infection Infection:
1, 2, 3, 5, 8 airflow Patient in more than 75% of requiring reoperation: International
systems and Characteristics: procedures 28/8288 TKR Classification of
body NR Intervention2: n=3513 (0.34%)BODY EXHAUST Diseases, Ninth
exhaust Ag: NR Patients in Hospitals SUIT revision (ICD-9)
suits on the Gender: NR which used laminar air Intervention1: 10/3538 diagnosis and
risk of Obesity: NR flow in more than 75% of (0.28% (95%CI: 0.11- procedures codes
postoperativ Comorbidities: NR procedures 0.46)) for evidence of
e infections Control1: 18/4750 (0.38 postoperative deep
via a Procedures: Timing of intervention: (95%CI: 0.20-0.55)) infection that
secondary Unilateral primary Intraoperative required additional
analysis of total knee Risk Ratio (95%CI) for operation.
data replacement (TKR) Duration of Body Exhaust Suit: 0.75 Reoperations within
collected for intervention: (0.34-1.62) 90 days
a larger Indications: NR Intraoperative Perioperative
study of LAMINAR AIR FLOW care: NR
hospital Setting: 256 centers Device: Laminar air flow Intervention2: 15/3513 Analytical
characteristi in Illinois, Ohio, or Exhaust suits. (0.43% (95%CI: 0.21- methodology:
c and North Carolina and Laminar air flow: 0.64)) None
patient Tennessee that horizontal and vertical Control2: 13/4750 (0.27 Did not adjust for
outcomes submitted a claim for laminar airflow systems (95%CI: 0.12-0.42)) clustering of events
after total TKR during 2000 were combined into a within hospitals
knee single group that 28 TKR were performed in bb/c 22/25
replacement Location: USA represented regular use 25 hospitals. hospitals with
(TKR) of laminar air flow. infections reported
Dates: January 1 Exhaust Suit: Not Other infections: NR only a single
August 30, 2000 indicated: who wore Topic-specific infection and
2017 American Medical Association. All rights reserved. 572
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
Intervention Results Comments
(Data Risk of Objective Setting
Extractor) Bias Score
exhaust suits, specifics of outcomes: because no
Inclusion Criteria: design. OR Flow or traffic 30% of hospitals in hospital reported
Data from Medicare Monitoring intervention: analysis reported regular more than 2
claims parts A and B NR use of laminar airflow infections.
to identify unilateral systems Other notes:
primary TKRs. For Control group: 41% of hospitals in this UV Light use-
patients with a Control1: n=4750 analysis reported regular collected data on
second TKR during Patients in Hospitals use of body exhaust suits. use of UV lights but
a separate which used exhaust suits Reoperations: All this was used only
hospitalization, only at frequencies of not at incidences of infection at 13/256 hospitals
the first procedure all, used in less than were reoperations within and did not allow
was considered. 26% of procedures, 90 days. analysis of effect
used in 26%-75% of Length of stay: NR on infectious
proceduresControl2: Mortality: NR outcomes.
Hospitals had to n=4775 Adverse events: NR Low number of
meet the following Patients in Hospitals events (n=28)
criteria: 1. The which used Laminar Air yielded low power
orthopedic Flow at frequencies of to exclude potential
administrator not at all, used in less benefits. Also
returned the survey than 26% of procedures, precluded analysis
on use of laminar used in 26%-75% of of subgroups and
airflow systems procedures interactions
(horizontal or between infection
vertical) and body Standard preventive control techniques.
exhaust suits during measures: Also potential for
TKR in year 2000, 2. Use of laminar air flow misclassification of
The survey and exhaust suit was individual
contained distributed roughly procedures (focus
information independently among on hospital
regarding use of hospitals. Most hospitals standard practice)-
laminar airflow reported that these infections
systems and body methods were either part associated with
exhaust suits as of their standard infection hospitals classified
infection control control practices as using
measures, and 3. (used>75% of time) or intervention
There was evidence not at all. technique most of
of at least 1 the time, could
Medicare claim for a have occurred in
TKR performed patients for whom
during January 1 the technique was
2017 American Medical Association. All rights reserved. 573
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
Intervention Results Comments
(Data Risk of Objective Setting
Extractor) Bias Score
and August 1, 2000 not use.
Follow-up: 90
Exclusion Criteria: days
Bilateral TKR during Funding Source
the same Conflicts:
hospitalization. Authors: None
Institution: None
Study: None
Supplies: None
Pasquar- Prospecti- To evaluate Number of Intervention group: SSI (follow up 24 Definitions:
ella ve the effect on patients: N=62 n=31 months) Deep and
182
2003 Concurre- aerobic operations Body exhaust suits were Unadjusted: superficial wound
(ES) nt control bacterial Patient worn by one surgeon, the Total: 3/61 (4.8%) infections not
1, 2, 3, 4, sedimentatio Characteristics first assistant and the Deep: 1/61 (1.6%) defined but
5, n of a mixed Age: mean 70.80 scrub nurse who Superficial: 2/61 (3.2%) recorded.
operating years range= 30-95 remained seated Perioperative
theater years SD=12.39 throughout the whole Intervention (Exhaust suit): care:
ventilation Gender: m/f: 33/29 operation. The circulating Deep: 1/31 (3.2%) Anesthesia: either
with Obesity: NR nurse wore a postop day 11 general or spinal.
separate Comorbidities: NR conventional gown. Superficial: 1/31 (3.2%) Analytical
operating Procedures: Total Operation was conducted postop day 16 methodology:
and hip replacements in a diluted airflow system Control (conventional Settle plate results
anesthetic (THR) or with separation zones. gown): were compared
areas and to hemiarthroplasties Timing of intervention: Deep: 0/31 between patient
compare the Indications: Intraoperative Superficial: 1/31 (3.2%) and anesthetist
contaminatio Hemiarthroplasties: Duration of postop day 15 areas and between
n using either coxoarthrosis intervention: conventional gowns
body or fracture (trauma) Intraoperatively Other infections: NR and body exhaust
exhaust THR: NR Device: Topic-specific suits using Mann-
gowns or Setting: Orthopedic Diluted airflow system outcomes: NA Whitney U tests
conventional department in 1 with separation zones: after normality
clothing hospital Unidirectional airflow Reoperations: NR checking to
during hip Location: system where the air is Length of stay: NR establish significant
joint Switzerland forced through a 0.3m Mortality: NR differences
Arthroplasty Dates: December H14 99.995% HEPA Adverse events: NR between variables.
(THR and 1997-January 1998 (high efficiency Other notes: None
hemiarthropl Inclusion Criteria: particulate air) filter and Follow-up: 24
asty) Patients scheduled supplied through eight air months
for THR or ceiling diffusers located Funding Source
hemiarthroplasties over the operating table Conflicts:
2017 American Medical Association. All rights reserved. 574
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
Intervention Results Comments
(Data Risk of Objective Setting
Extractor) Bias Score
for either and the instrument table. Authors: NR
coxoarthrosis or The air is extracted by Institution: NR
fracture between the means of two floor-level Study: NR
study dates return air grilles in the Supplies: Industry
Exclusion Criteria: walls of the anesthetic
NR area. Air turnover rate
24 air changes /h with a
positive pressure of 2 Pa.
A plexiglass barrier
separates the OR into the
patient area and the
anesthetic area. The
Patients head and the
anesthesiologist remain
outside the patient area
during the operation.
Body exhaust suit:
Manufacturer named but
suit not described.
Conventional Gowns:
65% polyester 35%
cotton with the head
cover consisting of a
single hood plus surgical
mask and the neck
remaining partially
exposed.
Monitoring intervention:
NA
Control group: n=31
Conventional gowns worn
by all surgical staff during
operation in diluted
airflow system with
separation zones
Standard preventive
measures:
AMP: IV injection of
cefamandole 30min
before anesthesia
2017 American Medical Association. All rights reserved. 575
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Author Study
Year Design Study Population and
Intervention Results Comments
(Data Risk of Objective Setting
Extractor) Bias Score
followed by a second
dose of cefamandole in
operations lasting longer
than 2h.
Operating Room Traffic:
Operating Team (1
surgeon, 2 assistants, 2
nurses) same for all
procedures. Surgeon first
assistant and scrub nurse
remained seated entire
operation (second
assistant stood at
opposite end of room and
circulating nurse moved
around).
Extraneous personnel
were excluded from the
OR. Swing doors were
closed to all personnel
after the final preparation
of the patient on the
operating table.
2017 American Medical Association. All rights reserved. 576
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.2D.3. RISK OF BIAS ASSESSMENTS: Q18 ORTHOPAEDIC SPACE SUIT
eTABLE 69. Risk of Bias Assessments of Other Controlled Studies for Q18 Orthopaedic Space Suit
Attrition not Funding
All study groups significantly Investigator Statistical source(s)
derived from different Measure blinded to Potential adjustment for disclosed and
similar across of Measure of endpoint confound potential no obvious Overall
Author source/reference study exposure outcome is assessme- -ders confounders conflict of Risk of
Year Q populations groups is valid valid nt identified done interest Bias
Question 18: Surgical Attire
Hooper
181 18 Low
2011
Miner
180 18 Low
2007
Pasquarel-
la 18 Low
182
2003
2017 American Medical Association. All rights reserved. 577
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.2E. Q20 BIOFILM
2.2E.1. GRADE TABLE: Q20 BIOFILM
eTABLE 70. GRADE Table for Q20 Biofilm
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
Quantity GRADE of Overall
Dose-response
Study Quality
and Type Starting Evidence GRADE of
Confounders
Consistency
Comparison Outcome Findings
Directness
of GRADE for Evidence
Precision
Evidence Outcome Base
Q20. What are the most effective strategies to reduce the risk of biofilm formation and SSI in prosthetic joint arthroplasty patients?
Q20A. How effective are cement modifications (i.e., antimicrobial and nanoparticle loading)?
Meta-analysis 2 RCTs (N=418), reduced
risk for deep SSI in primary hybrid TKA
(cemented tibial and patellar components)
with cefuroxime 2g in 40g
polymethylmethacrylate loaded cement:
2
OR: 0.08 (0.01 0.59); p=0.01; I =0
1 study in 350 TKAs, non-diabetics:
183
0/178 vs. 5/162 (3.1%); p=0.02
1 study in 78 TKAs, all diabetics: 0/41
184
Deep 2 RCT
Cefuroxime SSI* 183,184 vs. 5/37 (13.5%); p=0.02 High 0 0 0 0 -1 0 0 0 Moderate
loaded Based on definition deep SSI included PJI
cement vs. All TKAs performed by same surgeon, in
plain operating rooms without ultraviolet light,
cement; laminar flow, or orthopaedic space suit Moderate
both AMP included parenteral cefazolin and
groups with gentamycin preoperatively then every 6
perioperat- and 12 hours, respectively postop for 36
ive AMP hours followed by cefazolin orally for 7
more days.
Meta-analysis 2 RCT (N=418), no
difference OR: 0.91 (0.18 4.55); p=0.90;
2
I =0
In one study of 350 TKAs for
183
Superfi- 2 RCT
183,184 High 0 0 0 -1 -1 0 0 0 Low
cial SSI osteoarthritis with no diabetes mellitus:
2/178 vs. 2/162; p=1.00
In one study of 78 TKAs all with
184
diabetes mellitus: 1/41 vs. 1/37; p=0.84
2017 American Medical Association. All rights reserved. 578
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Increase
Decrease GRADE
GRADE
Large Magnitude
Publication Bias
Quantity GRADE of Overall
Dose-response
Study Quality
and Type Starting Evidence GRADE of
Confounders
Consistency
Comparison Outcome Findings
Directness
of GRADE for Evidence
Precision
Evidence Outcome Base
Q20B. How effective are prosthesis surface modifications (i.e., antimicrobial coating, galvanic couples, printing technologies, and nanotechnology)? Our
search did not identify in vivo studies that evaluated the safety and effectiveness of prosthesis modifications and their impact on biofilm formation and the risk of SSI.
Q20C. How effective are vaccines? Our search did not identify in vivo studies that evaluated the safety and effectiveness of vaccines and their impact on biofilm
formation and the risk of SSI.
Q20D. How effective are other biofilm control agents (e.g., biofilm dispersants, quorum-sensing inhibitors, novel antimicrobial agents)? Our search did not
identify in vivo studies that evaluated the safety and effectiveness of biofilm control agents and their impact on biofilm formation and the risk of SSI
*Critical outcome; OR: Odds Ratio; RR: Risk Ratio; CI: Confidence Interval
2017 American Medical Association. All rights reserved. 579
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.2E.2. EVIDENCE TABLE: Q20 BIOFILM
Q20. What are the most effective strategies to reduce the risk of biofilm formation and SSI in prosthetic joint arthroplasty patients?
eTABLE 71. Evidence Table for Q20A. How effective are cement modifications (i.e., antimicrobial and nanoparticle loading)?
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
Chiu RCT To Number of patients: Intervention group: SSI: (range 26-80 months) Definitions: (McQueen
183
2002 1, 5, 10 evaluate N=285 patients n=178 knees Early Superficial Infections: 1990)
(ES) the efficacy (340 knees) Cefuroxime-impregnated Intervention: 2/178 (1.1%) Superficial Infection
of Patient cement ( 2g of cefuroxime Control: 2/162 (1.2%) infection superficial to
cefuroxime Characteristics: Age, in 40 g cement) was P=1 the deep fascia with
- tourniquet time, utilized for fixation of the Early or Intermediate Deep positive or negative
impregnate operative time, amount tibial an patellar Infections: cultures and no delays in
d cement in of blood transfusion, components only Intervention: 0/178 wound healing.
the The Hospital for Special Timing of intervention: Control: 5/162 (3.1%) Deep Infection
prevention Surgery Knee Score Intra and postoperatively Early: 3/5 (60%) Infection extending deep
of deep (pre & post operatively), Duration of intervention: Intermediate: 2/5 (40%) to the deep fascia, with
infection sex, side of operation, The duration of P=0.0238 persistent wound
after and preoperative implantation (indefinitely). No deep infections in bilateral discharge or joint pain,
primary diagnosis were all Device: Cefuroxime- procedures positive or negative
total knee analyzed and were impregnated cement; pure cultures from deep
arthroplasti found to be similar cement without Other infections: NR tissues and delays in
es between groups. cefuroxime; prosthetic Topic-specific outcomes: NR wound healing.
performed Age: Mean SD knee Re-operations attributable to SSI: Deep Infections also
without Intervention :707.4yr Monitoring intervention: All four early superficial wound confirmed by laboratory
clean-air Control:686.9yr Radio graphic evaluation infections were treated with wound parameters (the
measures Gender: (m/f) at every visit & functional debridement & intravenous erythrocyte
such as Intervention evaluation (Hospital for antimicrobials for 1 week then oral sedimentation rate &
laminar :69%/31% Special Surgery score) antimicrobials for another week. level C-reactive protein)
flow and Control:70%/30% performed at every visit & positive culture of joint
rd
body- Obesity: NR starting with the 3 postop Length of stay: Mean Stay, days fluid.
exhaust Comorbidities: NR visit. (range): Early Infections:
suits. Operation Side: Control group: n= 162 8 days (5-15 days) Developing <2 months
(left/right) knees Mortality: NR after operation
Intervention Cement did not contain Adverse events: Intermediate Infections:
:51%/49% cefuroxime. Only tibial and Loose femoral component at 2 Developing 2-24 months
Control:55%/45% patellar components were years: after operation
Procedures: Primary fixed with cement. Intervention: 1/178 (0.6%) Late Infections:
total knee arthroplasties Bilateral TKAs: n=55 underwent revision of the femoral Developing >24 months
with cementless fixation patients ; one knee treated component after operation.
of the femoral with intervention, the other Not significant statistically with (Rand 1993)
2017 American Medical Association. All rights reserved. 580
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
component and cement with controls available numbers Follow-up: at 3 weeks,
fixation (mixing method Standard preventive 8 weeks, and 6 months
of cement NR) of the measures: Patellar fracture after traumatic then every 6 months
patellar and tibial Environmental: No episode: thereafter. Average was
components. ultraviolet light for Control: 1/162 (0.6%) treated with 49 months (Range 26-80
Indications: disinfection; no laminar ORIF with tension band wiring months)
Osteoarthritis: flow nor body-exhaust Perioperative care: NR
Control: 146/162 suits were used. Other notes:
(90.1%) AMP Preop: intravenous All surgeries performed
Intervention: 154/178 bolus injections of by 1 surgeon
(86.5%) cefazolin & gentamicin. The authors report the
Rheumatoid Arthritis AMP Postop: Intravenous operating room was not
Control: 6/162 (3.7%) injections of cefazolin modern like more
Intervention: 10/178 every 6hrs for 36 hours; developed countries with
(5.6%) Intravenous injections of better facilities. This
Posttraumatic arthritis: gentamicin every 12hrs for study was an effort to
Control: 6/162 (3.7%) 36 hours; and oral show that antimicrobial
Intervention: 10/178 cefazolin every 6hrs for 7 impregnated cement
(5.6%) days. could be utilized as part
Gouty arthritis Drain: Used routinely and of a bundle to reduce
nd
Control: 2/162 (1.2%) removed on the 2 day. SSI without clean air
Intervention: 1/178 Continuous passive facilities.
(0.6%) motion: used every day Funding Source
Osteonecrosis: until discharge Conflicts:
Control: 1/162 (0.6%) Weight bearing: on the Authors: None
Intervention: 3/178 involved knee was allowed Institution: None
(1.7%) form the second Study: None
Setting: 1 Hospital postoperative day and Supplies: None
Location: Taiwan, crutches were used as
China needed
Dates: 1994-1998
Inclusion Criteria:
Patients undergoing
primary total knee
arthroplasty
Exclusion Criteria:
Patients with diabetes
mellitus, peripheral
arterial occlusive
2017 American Medical Association. All rights reserved. 581
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
disease, psoriasis, prior
knee surgery, any kind
of lower-extremity
infection, osteomyelitis,
or a malignant tumor
who were being treated
with
immunosuppressive
agents.
Chiu RCT To Number of patients: Intervention group: n=41 SSI: (range 26-88 months) Definitions:
184
2001 1, 5, 10 evaluate N=78 knees (35 patients-6 Early superficial wound infection: SSI
(ES) the effect Patient Bilateral TKA) Intervention: 1/ 41 (2.4%) Classified according to
of Characteristics: Age; Cefuroxime-impregnated Control: 1/37 (2.7%) (McQueen et al 1990)
antimicrobi sex; side of operation; cement (2g of cefuroxime P= 0.835 and confirmed by
al type of diabetes; type of in 40 g cement) was Deep infection measurement of the
(cefuroxim diabetic treatment; utilized for fixation of the Intervention: 0/41 ESR & level of C-
e) duration of diabetes tibial and patellar Control: 5/37 (13.5%) reactive protein and
impregnate mellitus; tourniquet components only. P=0.021 culture of joint fluid.
d cement time; operation time, Timing of intervention: Relative probability of not developing Perioperative care:
on the volume of blood Intra and post-operatively a deep infection in intervention group Authors report patients
prevention transfusion; Duration of intervention: 0.865 (95%CI 0.769-0.973) had poor control of blood
of deep preoperative fasting The duration of All deep infections were in unilateral glucose and the
infection blood sugar; implantation (indefinitely). TKAs operating room was not
after preoperative 2 hours Device: Cefuroxime- All deep infections were considered modern. Also used 7
primary post meal blood sugar; impregnated cement; pure late (1-6mo postop) and were day course of a systemic
total knee postoperative fasting cement without deemed healing satisfactorily until antimicrobial because
arthroplast blood sugar, cefuroxime; prosthetic after the first follow-up visit. operating environment
y (TKA) in postoperative 2 hours knee No deep infections occurred in was poor and patients
patients post meal blood sugar; Monitoring intervention: bilateral surgeries. were in poor state of
with preoperative knee Patients were examined at hygiene. They report
diabetes score; and 3 weeks, 8 weeks & 6 Other infections: NR trying to shorten regimen
mellitus postoperative knee months post-operatively. Topic-specific outcomes: by using antimicrobial
(DM). score were all analyzed Then every 6 months Deep infections impregnated cement
and found to be similar there-after. Radio graphic Type 1 Diabetes: Other notes: All
between groups except evaluation at every visit & 1/5 6mo postop 70yoMale surgeries performed by
postoperative knee functional evaluation 1 surgeon
score (HHS-functional) (Hospital for Special Type 2 Diabetes: Follow-up: Patients
Age: mean (range) Surgery score) performed 4/5 (1,2,3 and 6 mo. postop in 67- were examined at 3
Intervention: 72y (56- at every visit starting with 73yo Males) weeks, 8 weeks & 6
2017 American Medical Association. All rights reserved. 582
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
rd
90) the 3 postop visit. months post-operatively.
Control: 69y (54-81) Control group: n= 37 Infecting organism in deep Then every 6 months
Gender: m/f (%) knees (32 patients-5 infections: there-after Mean follow
Intervention: 80/20 Bilateral TKA) Staphylococcus aureus: 3/5 up was 50 months
Control: 67/33 Cement did not contain Staphylococcus epidermis: 2/5 (Range 26-88 months)
Obesity: NR cefuroxime. Only the tibial
Comorbidities: and patellar components Postoperative knee score (HHS- Funding Source
NIDDM/IDDM: were fixed with cement. functional) Conflicts:
Intervention: 32/3 Bilateral TKAs: Intervention: 91 (SD 2.8) Authors: None
Control: 28/4 cefuroxime-impregnated Control: 86 (SD 9.2) Institution: None
Duration of Diabetes: y cement used on one side P= 0.0093 Study: None
(SD) (Intervention n=6) and not Caused by five cases of deep Supplies: None
Intervention: 12y (8.7) the other (Control n=5). All infection in control group
Control: 10y (7.8) undertaken in sequence
Left/right: (%) under difference Re-operations: Both early
Intervention: 80/20 anesthetics superficial wound infections were
Control: 52/48 Standard preventive successfully treated with
Procedures: Total measures: debridement and intravenous
knee arthroplasty with Environmental: No antimicrobials administered for 1
cementless fixation of ultraviolet light for week and orally for another week.
the femoral component disinfection; no laminar Deep Infections
and cement fixation flow nor body-exhaust 3/5 radical debridement was
(mixing method of suits were used. followed by four weeks of
cement NR) of the AMP Preop: intravenous intravenous antimicrobials and then
patellar and tibial bolus injections of two months of oral antimicrobials
components. cefazolin & gentamicin. 2/5 deep SSIs underwent two stage
Indications: AMP Postop: Intravenous re-implantation procedures.
Osteoarthritis injections of cefazolin Length of stay: Mean lengths was 8
Setting: 1 hospital every 6hrs for 36 hours; days (Range 5-14 days)
Location: Taiwan, Intravenous injections of Mortality: NR
China gentamicin every 12hrs for Adverse events: NR
Dates: 1993-1998 36 hours; and oral
Inclusion Criteria: cefazolin every 6hrs for 7
Patients with diabetes days.
mellitus undergoing Drain: (not vacuum) Were
total knee arthroplasty used for 36 hours
Exclusion Criteria: Continuous passive
Patients with motion: Prescribed
rheumatoid arthritis, immediately and used
2017 American Medical Association. All rights reserved. 583
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
Study
Author
Design
Year Study Population and
Risk of Intervention Results Comments
(Data Objective Setting
Bias
Extractor)
Score
psoriasis, previous every day until discharge
knee surgery, any type Weight bearing: on the
of infection of the lower operated knee was
limb, osteomyelitis, allowed immediately &
malignant tumor or crutches used as needed.
those who were
undergoing
immunosuppressive
therapy.
Q20B. How effective are prosthesis surface modifications (i.e., antimicrobial coating, galvanic couples, printing technologies, and
nanotechnology)? Our search did not identify in vivo studies that evaluated the safety and effectiveness of prosthesis modifications and their impact on
biofilm formation and the risk of SSI.
Q20C. How effective are vaccines? Our search did not identify in vivo studies that evaluated the safety and effectiveness of vaccines and their impact on
biofilm formation and the risk of SSI.
Q20D. How effective are other biofilm control agents (e.g., biofilm dispersants, quorum-sensing inhibitors, novel antimicrobial agents)? Our
search did not identify in vivo studies that evaluated the safety and effectiveness of biofilm control agents and their impact on biofilm formation and the risk
of SSI.
2017 American Medical Association. All rights reserved. 584
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
2.2E.3. RISK OF BIAS ASSESSMENTS: Q20 BIOFILM
eTABLE 72. Risk of Bias Assessments of Randomized Controlled Trials for Q20 Biofilm
Funding
Outco- Attrition source(s)
Described Randomizat- Describ- me smaller than Attrition disclosed and
as ion ed as assess- Study 10-15% of appropria- no obvious Overall
Author randomiz- appropriately double- or participant Investiga- Attrition assigned tely conflict of Risk of
Year Q ed performed blind blinded blinded tor blinded described patients analyzed interest Bias
Question 20 Biofilm
Chiu Mode-
183 20
2002 rate
Chiu Mode-
184 20
2001 rate
2017 American Medical Association. All rights reserved. 585
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
3. EVALUATION OF THE RISK OF BIAS OF AN INDIVIDUAL STUDY
3.1. Instructions
Check off each item in the appropriate checklist if it is present in the study
Divide the total number of checked items by the total number of questions on the checklist
Rate the risk of bias as follows:
If < 25% of checklist items were present in study, the Risk of Bias was rated as High
If > 25% and 50% of checklist items were present in study, the Risk of Bias was rated as Moderate
If >50% of checklist items were present in study, the Risk of Bias was rated as Low
3.2. Checklist for Systematic Reviews
1) Search terms described
2) Databases searched described and two or more databases searched
3) Inclusion/exclusion criteria described
4) Number of included/excluded studies along with reasons of exclusion described
5) Studies screened by two independent reviewers for inclusion
6) Data extracted by two independent reviewers
7) Individual study quality assessed
8) Heterogeneity between study results assessed qualitatively and/or quantitatively
9) Publication bias assessed
10) Characteristics of included studies reported in evidence table
11) Funding source(s) disclosed and no obvious conflict of interest
3.3. Checklist for Randomized Controlled Trials
1) Described as randomized
2) Randomization appropriately performed (e.g. random number table, computerized scheme)
3) Described as double-blind
4) Outcome assessor blinded
5) Study participant blinded (e.g. interventions identical in appearance)
6) Investigator blinded (e.g. opaque sealed envelopes)
7) Attrition described
8) Attrition smaller than 10-15% of assigned patients
9) Attrition appropriately analyzed (e.g. intention to treat analysis)
10) Funding source(s) disclosed and no obvious conflict of interest
3.4. Checklist for Observational Studies
1) All study groups derived from similar source/reference populations
2) Attrition not significantly different across study groups
3) The measure of exposure is valid
4) The measure of outcome is valid
5) Investigators blinded to endpoint assessment
6) Potential confounders identified
2017 American Medical Association. All rights reserved. 586
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
7) Statistical adjustment for potential confounders done
8) Funding source(s) disclosed and no obvious conflict of interest
3.5. Translating Risk of Bias into GRADE Tables
When the risk of bias was rated as High for >50% of studies making up the evidence base for a given outcome, one point was deducted for Study Quality in the GRADE table.
2017 American Medical Association. All rights reserved. 587
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
4. EVIDENCE TABLE EXTRACTION TEMPLATES
eTABLE 73. Systematic Review (SR) Extraction Template
Author
Study
Year
Design Study Population and
(Data Intervention(s) Results (by intervention) Comments
Quality Objective Setting
Extrac-
Score
tor)
SR Narrative Study types and Intervention group: SSI: Definitions:
Quality number: Timing of intervention: Other infections: Perioperative
Score Number of total Duration of intervention: Topic-specific care:
patients in the Device: outcomes: Other notes:
review: Monitoring intervention: Re-operations: Follow up:
Inclusion criteria: Control group: Length of stay: Funding source
Exclusion criteria: Standard preventive Mortality: conflicts:
Databases searched: measures: Adverse events:
Aggregate summary
score:
eTABLE 74. Randomized Controlled Trial (RCT) Extraction Template
Author
Study
Year
Design Study Population and
(Data Intervention Results Comments
Quality Objective Setting
Extrac-
Score
tor)
RCT Narrative Number of patients: Intervention group: SSI: Definitions:
Quality Patient Timing of intervention: Other infections: Perioperative
Score Characteristics: Duration of intervention: Topic-specific care:
Age: Device/agent: outcomes: Other notes:
Gender: Monitoring intervention: Reoperations: Follow-up:
Obesity: Control group: Length of stay: Funding source
Comorbidities: Standard preventive Mortality: conflicts:
Procedures: measures: Adverse events:
Indications:
Setting:
Location:
Dates:
Inclusion Criteria:
Exclusion Criteria:
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
eTABLE 75. Other Observational Studies (OBS) Extraction Template
Author
Study
Year
Design Study Population and
(Data Intervention Results Comments
Quality Objective Setting
Extract-
Score
or)
Study Narrative Number of patients: Intervention group: SSI: Definitions:
Design Patient Timing of intervention: Other infections: Perioperative
Quality Characteristics: Duration of intervention: Topic-specific care:
Score Age: Device/agent: outcomes: Analytical
Gender: Monitoring intervention: Reoperations: methodology:
Obesity: Control group: Length of stay: Other notes:
Comorbidities: Standard preventive Mortality: Follow-up:
Procedures: measures: Adverse events: Funding source
Indications: conflicts:
Setting:
Location:
Dates:
Inclusion Criteria:
Exclusion Criteria:
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
5. STUDY TYPE DETERMINATION
eFIGURE A. STUDY TYPE DETERMINATION ALGORITHM (Adapted from: Hartling et. al. 2010185)
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
6. REFERENCES
1. Akinyoola AL, Adegbehingbe OO, Odunsi A. Timing of antibiotic prophylaxis in tourniquet surgery. J Foot Ankle Surg. 2011;50(4):374-376.
2. Soriano A, Bori G, Garcia-Ramiro S, et al. Timing of antibiotic prophylaxis for primary total knee arthroplasty performed during ischemia. Clin Infect Dis.
2008;46(7):1009-1014.
3. Osman B, Abbas A, Ahmed MA, Abubaker MS, Adam I. Prophylactic ceftizoxime for elective cesarean delivery at Soba Hospital, Sudan. BMC Res Notes. 2013;6:57.
4. Macones GA, Cleary KL, Parry S, et al. The timing of antibiotics at cesarean: a randomized controlled trial. Am J Perinatol. 2012;29(4):273-276.
5. Witt A, Doner M, Petricevic L, et al. Antibiotic prophylaxis before surgery vs after cord clamping in elective cesarean delivery: a double-blind, prospective, randomized,
placebo-controlled trial. Arch Surg. 2011;146(12):1404-1409.
6. Yildirim G, Gungorduk K, Guven HZ, et al. When should we perform prophylactic antibiotics in elective cesarean cases? Arch Gynecol Obstet. 2009;280(1):13-18.
7. Thigpen BD, Hood WA, Chauhan S, et al. Timing of prophylactic antibiotic administration in the uninfected laboring gravida: a randomized clinical trial. Am J Obstet
Gynecol. 2005;192(6):1864-1868; discussion 1868-1871.
8. Sullivan SA, Smith T, Chang E, Hulsey T, Vandorsten JP, Soper D. Administration of cefazolin prior to skin incision is superior to cefazolin at cord clamping in
preventing postcesarean infectious morbidity: a randomized, controlled trial. Am J Obstet Gynecol. 2007;196(5):455 e451-455.
9. Wax JR, Hersey K, Philput C, et al. Single dose cefazolin prophylaxis for postcesarean infections: before vs. after cord clamping. J Matern Fetal Med. 1997;6(1):61-65.
10. Cuthbertson AM, McLeish AR, Penfold JC, Ross H. A comparison between single and double dose intravenous timentin for the prophylaxis of wound infection in
elective colorectal surgery. Dis Colon Rectum. 1991;34(2):151-155.
11. Mui LM, Ng CS, Wong SK, et al. Optimum duration of prophylactic antibiotics in acute non-perforated appendicitis. ANZ Journal of Surg. 2005;75(6):425-428.
12. Tamayo E, Gualis J, Florez S, Castrodeza J, Eiros Bouza JM, Alvarez FJ. Comparative study of single-dose and 24-hour multiple-dose antibiotic prophylaxis for cardiac
surgery. J Thorac Cardiovasc Surg. 2008;136(6):1522-1527.
13. Su HY, Ding DC, Chen DC, Lu MF, Liu JY, Chang FY. Prospective randomized comparison of single-dose versus 1-day cefazolin for prophylaxis in gynecologic
surgery. Acta Obstet Gynecol Scand. 2005;84(4):384-389.
14. Buckley R, Hughes GNF, Snodgrass T, Huchcroft SA. Perioperative cefazolin prophylaxis in hip fracture surgery. Can J Surg. 1990;33(2):122-127.
15. Fujita S, Saito N, Yamada T, et al. Randomized, multicenter trial of antibiotic prophylaxis in elective colorectal surgery: single dose vs 3 doses of a second-generation
cephalosporin without metronidazole and oral antibiotics. Arch Surg. 2007;142(7):657-661.
16. Oostvogel HJ, van Vroonhoven TJ, van der Werken C, Lenderink AW. Single-dose vs. short-term antibiotic therapy for prevention of wound infection in general surgery.
A prospective, randomized double-blind trial. Acta Chir Scand. 1987;153(10):571-575.
17. Ali M, Raza A. Role of single dose antibiotic prophylaxis in clean orthopedic surgery. J Coll Physicians Surg Pak. 2006;16(1):45-48.
18. Gatell JM, Garcia S, Lozano L, Soriano E, Ramon R, SanMiguel JG. Perioperative cefamandole prophylaxis against infections. J Bone Joint Surg Am. 1987;69(8):1189-
1193.
19. Garotta F, Pamparana F. Antimicrobial prophylaxis with ceftizoxime versus cefuroxime in orthopedic surgery. Ceftizoxime Orthopedic Surgery Italian Study Group. J
Chemother. 1991;3 Suppl 2:34-35.
20. Wymenga AB, Hekster YA, Theeuwes A, Muytjens HL, van Horn JR, Slooff TJ. Antibiotic use after cefuroxime prophylaxis in hip and knee joint replacement. Clin
Pharmacol Ther. 1991;50(2):215-220.
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
21. Ritter MA, Campbell E, Keating EM, Faris PM. Comparison of intraoperative versus 24 hour antibiotic prophylaxis in total joint replacement. A controlled prospective
study. Orthop Rev. 1989;18(6):694-696.
22. Kow L, Toouli J, Brookman J, McDonald PJ. Comparison of cefotaxime plus metronidazole versus cefoxitin for prevention of wound infection after abdominal surgery.
World J Surg. 1995;19(5):680-686; discussion 686.
23. Carr ND, Hobbiss J, Cade D, Schofield PF. Metronidazole in the prevention of wound sepsis after elective colorectal surgery. J R Coll Surg Edinb. 1984;29(3):139-142.
24. Grundmann R, Burkardt F, Scholl H, Koelschbach D. One versus three doses of metronidazole/mezlocillin for antibiotic prophylaxis in colon surgery. Chemioterapia.
1987;6(2 Suppl):604-605.
25. Bates T, Roberts JV, Smith K, German KA. A randomized trial of one versus three doses of augmentin as wound prophylaxis in at-risk abdominal surgery. Postgrad Med
J. 1992;68(804):811-816.
26. Aberg C, Thore M. Single versus triple dose antimicrobial prophylaxis in elective abdominal surgery and the impact on bacterial ecology. J Hosp Infect. 1991;18(2):149-
154.
27. Mayer HO, Petru E, Haas J, Heydarfadai M. Perioperative antibiotic prophylaxis in patients undergoing radical surgery for gynecologic cancer: single dose versus
multiple dose administration. Eur J Gynaecol Oncol. 1993;14(3):177-181.
28. Hemsell DL, Heard ML, Nobles BJ, Hemsell PG. Single-dose cefoxitin prophylaxis for premenopausal women undergoing vaginal hysterectomy. Obstet Gynecol.
1984;63(3):285-290.
29. Turano A. New clinical data on the prophylaxis of infections in abdominal, gynecologic, and urologic surgery. Multicenter Study Group. Am J Surg. 1992;164(4A
Suppl):16S-20S.
30. Lyimo FM, Massinde AN, Kidenya BR, Konje ET, Mshana SE. Single dose of gentamicin in combination with metronidazole versus multiple doses for prevention of
post-caesarean infection at Bugando Medical Centre in Mwanza, Tanzania: a randomized, equivalence, controlled trial. BMC Pregnancy Childbirth. 2013;13:123.
31. Hussain MI, Alam MK, Al-Qahatani HH, Al-Akeely MH. Role of postoperative antibiotics after appendectomy in non-perforated appendicitis. J Coll Physicians Surg
Pak. 2012;22(12):756-759.
32. Conte JE, Jr., Cohen SN, Roe BB, Elashoff RM. Antibiotic prophylaxis and cardiac surgery. A prospective double-blind comparison of single-dose versus multiple-dose
regimens. Ann Intern Med. 1972;76(6):943-949.
33. Nooyen SM, Overbeek BP, Brutel de la Riviere A, Storm AJ, Langemeyer JJ. Prospective randomised comparison of single-dose versus multiple-dose cefuroxime for
prophylaxis in coronary artery bypass grafting. Eur J Clin Microbiol Infect Dis. 1994;13(12):1033-1037.
34. Austin TW, Coles JC, Burnett R, Goldbach M. Aortocoronary bypass procedures and sternotomy infections: a study of antistaphylococcal prophylaxis. Can J Surg.
1980;23(5):483-485.
35. Lin MH, Pan SC, Wang JL, et al. Prospective randomized study of efficacy of 1-day versus 3-day antibiotic prophylaxis for preventing surgical site infection after
coronary artery bypass graft. J Formos Med Assoc. 2011;110(10):619-626.
36. Bernard A, Pillet M, Goudet P, Viard H. Antibiotic-prophylaxis in pulmonary surgery - a prospective randomized double-blind trial of flash cefuroxime versus 48-hour
cefuroxime. J Thorac Cardiovasc Surg. 1994;107(3):896-900.
37. Hasselgren PO, Ivarsson L, Risberg B, Seeman T. Effects of prophylactic antibiotics in vascular surgery. A prospective, randomized, double-blind study. Ann Surg.
1984;200(1):86-92.
38. Hall JC, Christiansen KJ, Goodman M, et al. Duration of antimicrobial prophylaxis in vascular surgery. Am J Surg. 1998;175(2):87-90.
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
39. Liu SA, Tung KC, Shiao JY, Chiu YT. Preliminary report of associated factors in wound infection after major head and neck neoplasm operations--does the duration of
prophylactic antibiotic matter? J Laryngol Otol. 2008;122(4):403-408.
40. Carroll WR, Rosenstiel D, Fix JR, et al. Three-dose vs extended-course clindamycin prophylaxis for free-flap reconstruction of the head and neck. Arch Otolaryngol Head
Neck Surg. 2003;129(7):771-774.
41. Chang WC, Hung YC, Li TC, Yang TC, Chen HY, Lin CC. Short course of prophylactic antibiotics in laparoscopically assisted vaginal hysterectomy. J Reprod Med.
2005;50(7):524-528.
42. Suzuki T, Sadahiro S, Maeda Y, Tanaka A, Okada K, Kamijo A. Optimal duration of prophylactic antibiotic administration for elective colon cancer surgery: A
randomized, clinical trial. Surgery. 2011;149(2):171-178.
43. Becker JM, Alexander DP. Colectomy, mucosal proctectomy, and ileal pouch-anal anastomosis. A prospective trial of optimal antibiotic management. Ann Surg.
1991;213(3):242-247.
44. Hall JC, Watts JM, Press L, O'Brien P, Turnidge J, McDonald P. Single-dose antibiotic prophylaxis in contaminated abdominal surgery. Arch Surg. 1989;124(2):244-247.
45. Juul P, Klaaborg KE, Kronborg O. Single or multiple doses of metronidazole and ampicillin in elective colorectal surgery. A randomized trial. Dis Colon Rectum.
1987;30(7):526-528.
46. Mendel V, Jung D, Heymann H. Single-shot antibiotic prophylaxis in colon surgery. Chemioterapia. 1987;6(2 Suppl):597-600.
47. McArdle CS, Morran CG, Pettit L, Gemmell CG, Sleigh JD, Tillotson GS. Value of oral antibiotic prophylaxis in colorectal surgery. Br J Surg. 1995;82(8):1046-1048.
48. Moesgaard F, Lykkegaard-Nielsen M. Preoperative cell-mediated immunity and duration of antibiotic prophylaxis in relation to postopertive infectious complications. A
controlled trial in biliary, gastroduodenal and colorectal surgery. Acta Chir Scand. 1989;155(4-5):281-286.
49. Wenzel M, Heinrich M, Schmidt C. Peri-operative infection prophylaxis with ornidazole and gentamicin in elective colonic surgery. Pharmatherapeutica. 1985;4(6):351-
355.
50. Karran SJ, Sutton G, Gartell P, Karran SE, Finnis D, Blenkinsop J. Imipenem prophylaxis in elective colorectal surgery. Br J Surg. 1993;80(9):1196-1198.
51. Imamura H, Kurokawa Y, Tsujinaka T, et al. Intraoperative versus extended antimicrobial prophylaxis after gastric cancer surgery: a phase 3, open-label, randomised
controlled, non-inferiority trial. Lancet Infect Dis. 2012;12(5):381-387.
52. Haga N, Ishida H, Ishiguro T, et al. A prospective randomized study to assess the optimal duration of intravenous antimicrobial prophylaxis in elective gastric cancer
surgery. Int Surg. 2012;97(2):169-176.
53. Mohri Y, Tonouchi H, Kobayashi M, Nakai K, Kusunoki M, Group MSIR. Randomized clinical trial of single- versus multiple-dose antimicrobial prophylaxis in gastric
cancer surgery. Br J Surg. 2007;94(6):683-688.
54. Hirokawa F, Hayashi M, Miyamoto Y, et al. Evaluation of postoperative antibiotic prophylaxis after liver resection: a randomized controlled trial. Am J Surg.
2013;206(1):8-15.
55. Togo S, Tanaka K, Matsuo K, et al. Duration of antimicrobial prophylaxis in patients undergoing hepatectomy: a prospective randomized controlled trial using flomoxef.
J Antimicrob Chemother. 2007;59(5):964-970.
56. Ruiz-Tovar J, Santos J, Arroyo A, et al. Effect of peritoneal lavage with clindamycin-gentamicin solution on infections after elective colorectal cancer surgery. J Am Coll
Surg. 2012;214(2):202-207.
57. Al-Shehri MY, Saif S, Ibrahim A, et al. Topical ampicillin for prophylaxis against wound infection in acute appendicitis. Ann Saudi Med. 1994;14(3):233-236.
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
58. Juul P, Merrild U, Kronborg O. Topical ampicillin in addition to a systemic antibiotic prophylaxis in elective colorectal surgery. A prospective randomized study. Dis
Colon Rectum. 1985;28(11):804-806.
59. Seco JL, Ojeda E, Reguilon C, et al. Combined topical and systemic antibiotic prophylaxis in acute appendicitis. Am J Surg. 1990;159(2):226-230.
60. Raahave D, Hesselfeldt P, Pedersen T, Zachariassen A, Kann D, Hansen OH. No effect of topical ampicillin prophylaxis in elective operations of the colon or rectum.
Surg Gynecol Obstet. 1989;168(2):112-114.
61. Kamath S, Sinha S, Shaari E, Young D, Campbell AC. Role of topical antibiotics in hip surgeries - A prospective randomised study. Injury. 2005;36(6):783-787.
62. Neri V, Fersini A, Ambrosi A, Tartaglia N, Valentino TP. Umbilical port-site complications in laparoscopic cholecystectomy: role of topical antibiotic therapy. JSLS.
2008;12(2):126-132.
63. Vander Salm TJ, Okike ON, Pasque MK, et al. Reduction of sternal infection by application of topical vancomycin. J Thorac Cardiovasc Surg. 1989;98(4):618-622.
64. Almdahl SM, Veel T, Halvorsen P, Vold MB, Molstad P. Randomized prospective trial of saphenous vein harvest site infection after wound closure with and without
topical application of autologous platelet-rich plasma. Eur J Cardiothorac Surg. 2011;39(1):44-48.
65. Peerbooms JC, de Wolf GS, Colaris JW, Bruijn DJ, Verhaar JAN. No positive effect of autologous platelet gel after total knee arthroplasty A double-blind randomized
controlled trial: 102 patients with a 3-month follow-up. Acta Orthop. 2009;80(5):557-562.
66. Litmathe J, Philipp C, Kurt M, Boeken U, Gams E, Feindt P. The use of autologous platelet gel (APG) for high-risk patients in cardiac surgery - is it beneficial?
Perfusion. 2009;24(6):381-387.
67. Dorge H, Sellin C, Bury MC, et al. Incidence of deep sternal wound infection is not reduced with autologous platelet rich plasma in high-risk cardiac surgery patients.
Thorac Cardiovasc Surg. 2013;61(3):180-184.
68. Turtiainen J, Saimanen EI, Makinen KT, et al. Effect of triclosan-coated sutures on the incidence of surgical wound infection after lower limb revascularization surgery: a
randomized controlled trial. World J Surg. 2012;36(10):2528-2534.
69. Seim BE, Tonnessen T, Woldbaek PR. Triclosan-coated sutures do not reduce leg wound infections after coronary artery bypass grafting. Interact Cardiovasc Thorac
Surg. 2012;15(3):411-415.
70. Rasic Z, Schwarz D, Adam VN, et al. Efficacy of antimicrobial triclosan-coated polyglactin 910 (Vicryl* Plus) suture for closure of the abdominal wall after colorectal
surgery. Coll Antropol. 2011;35(2):439-443.
71. Baracs J, Huszar O, Sajjadi SG, Horvath OP. Surgical site infections after abdominal closure in colorectal surgery using triclosan-coated absorbable suture (PDS Plus) vs.
uncoated sutures (PDS II): a randomized multicenter study. Surg Infect (Larchmt). 2011;12(6):483-489.
72. Williams N, Sweetland H, Goyal S, Ivins N, Leaper DJ. Randomized trial of antimicrobial-coated sutures to prevent surgical site infection after breast cancer surgery.
Surg Infect (Larchmt). 2011;12(6):469-474.
73. Thimour-Bergstrom L, Roman-Emanuel C, Schersten H, Friberg O, Gudbjartsson T, Jeppsson A. Triclosan-coated sutures reduce surgical site infection after open vein
harvesting in coronary artery bypass grafting patients: a randomized controlled trial. Eur J Cardiothorac Surg. 2013;44(5):931-938.
74. Nakamura T, Kashimura N, Noji T, et al. Triclosan-coated sutures reduce the incidence of wound infections and the costs after colorectal surgery: a randomized
controlled trial. Surgery. 2013;153(4):576-583.
75. Justinger C, Slotta JE, Ningel S, Graber S, Kollmar O, Schilling MK. Surgical-site infection after abdominal wall closure with triclosan-impregnated polydioxanone
sutures: results of a randomized clinical pathway facilitated trial (NCT00998907). Surgery. 2013;154(3):589-595.
76. Galal I, El-Hindawy K. Impact of using triclosan-antibacterial sutures on incidence of surgical site infection. Am J Surg. 2011;202(2):133-138.
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
77. Diener MK, Knebel P, Kieser M, et al. Effectiveness of triclosan-coated PDS Plus versus uncoated PDS II sutures for prevention of surgical site infection after abdominal
wall closure: the randomised controlled PROUD trial. Lancet. 2014;384(9938):142-152.
78. Mingmalairak C, Ungbhakorn P, Paocharoen V. Efficacy of antimicrobial coating suture coated polyglactin 910 with tricosan (Vicryl plus) compared with polyglactin 910
(Vicryl) in reduced surgical site infection of appendicitis, double blind randomized control trial, preliminary safety report. J Med Assoc Thai. 2009;92(6):770-775.
79. Isik I, Selimen D, Senay S, Alhan C. Efficiency of antibacterial suture material in cardiac surgery: a double-blind randomized prospective study. Heart Surg Forum.
2012;15(1):E40-45.
80. Rozzelle CJ, Leonardo J, Li V. Antimicrobial suture wound closure for cerebrospinal fluid shunt surgery: a prospective, double-blinded, randomized controlled trial. J
Neurosurg. 2008;2(2):111-117.
81. Ford HR, Jones P, Gaines B, Reblock K, Simpkins DL. Intraoperative handling and wound healing: controlled clinical trial comparing coated VICRYL plus antibacterial
suture (coated polyglactin 910 suture with triclosan) with coated VICRYL suture (coated polyglactin 910 suture). Surg Infect (Larchmt). 2005;6(3):313-321.
82. Diener MK, Knebel P, Kieser M, Probst P, Buchler MW. Antibiotic sutures against surgical site infections--Authors' reply. Lancet. 2014;384(9952):1425-1426.
83. Biffi R, Fattori L, Bertani E, et al. Surgical site infections following colorectal cancer surgery: a randomized prospective trial comparing common and advanced
antimicrobial dressing containing ionic silver. World J Surg Oncol. 2012;10:94.
84. Krieger BR, Davis DM, Sanchez JE, et al. The use of silver nylon in preventing surgical site infections following colon and rectal surgery. Dis Colon Rectum.
2011;54(8):1014-1019.
85. Gandhi GY, Nuttall GA, Abel MD, et al. Intensive intraoperative insulin therapy versus conventional glucose management during cardiac surgery: a randomized trial. Ann
Intern Med. 2007;146(4):233-243.
86. Chan RP, Galas FR, Hajjar LA, Bello CN, Piccioni MA, Auler JO, Jr. Intensive perioperative glucose control does not improve outcomes of patients submitted to open-
heart surgery: a randomized controlled trial. Clinics. 2009;64(1):51-60.
87. Melling AC, Ali B, Scott EM, Leaper DJ. Effects of preoperative warming on the incidence of wound infection after clean surgery: a randomised controlled trial. Lancet.
2001;358(9285):876-880.
88. Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection
and Temperature Group. N Engl J Med. 1996;334(19):1209-1215.
89. Wong PF, Kumar S, Bohra A, Whetter D, Leaper DJ. Randomized clinical trial of perioperative systemic warming in major elective abdominal surgery. Br J Surg.
2007;94(4):421-426.
90. Thibon P, Borgey F, Boutreux S, Hanouz JL, Le Coutour X, Parienti JJ. Effect of perioperative oxygen supplementation on 30-day surgical site infection rate in
abdominal, gynecologic, and breast surgery: the ISO2 randomized controlled trial. Anesthesiology. 2012;117(3):504-511.
91. Belda FJ, Aguilera L, Garcia de la Asuncion J, et al. Supplemental perioperative oxygen and the risk of surgical wound infection: a randomized controlled trial. JAMA.
2005;294(16):2035-2042.
92. Bickel A, Gurevits M, Vamos R, Ivry S, Eitan A. Perioperative hyperoxygenation and wound site infection following surgery for acute appendicitis: a randomized,
prospective, controlled trial. Arch Surg. 2011;146(4):464-470.
93. Greif R, Akca O, Horn EP, Kurz A, Sessler DI, Group OR. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. N Engl J Med.
2000;342(3):161-167.
94. Meyhoff CS, Wetterslev J, Jorgensen LN, et al. Effect of high perioperative oxygen fraction on surgical site infection and pulmonary complications after abdominal
surgery The PROXI randomized clinical trial. JAMA. 2009;302(14):1543-1550.
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
95. Staehr AK, Meyhoff CS, Rasmussen LS, Group PT. Inspiratory oxygen fraction and postoperative complications in obese patients: a subgroup analysis of the PROXI
trial. Anesthesiology. 2011;114(6):1313-1319.
96. Stall A, Paryavi E, Gupta R, Zadnik M, Hui E, O'Toole RV. Perioperative supplemental oxygen to reduce surgical site infection after open fixation of high-risk fractures:
a randomized controlled pilot trial. J Trauma Acute Care Surg. 2013;75(4):657-663.
97. Pryor KO, Fahey TJ, 3rd, Lien CA, Goldstein PA. Surgical site infection and the routine use of perioperative hyperoxia in a general surgical population: a randomized
controlled trial. J Am Med Assoc. 2004;291(1):79-87.
98. Gardella C, Goltra LB, Laschansky E, et al. High-concentration supplemental perioperative oxygen to reduce the incidence of postcesarean surgical site infection: a
randomized controlled trial. Obstet Gynecol. 2008;112(3):545-552.
99. Duggal N, Poddatoori V, Noroozkhani S, Siddik-Ahmad RI, Caughey AB. Perioperative oxygen supplementation and surgical site infection after cesarean delivery: a
randomized trial. Obstet Gynecol. 2013;122(1):79-84.
100. Scifres CM, Leighton BL, Fogertey PJ, Macones GA, Stamilio DM. Supplemental oxygen for the prevention of postcesarean infectious morbidity: a randomized
controlled trial. Am J Obstet Gynecol. 2011;205(3):267 e261-269.
101. Whitney JD, Heiner S, Mygrant BI, Wood C. Tissue and wound healing effects of short duration postoperative oxygen therapy. Biol Res Nurs. 2001;2(3):206-215.
102. Turtiainen J, Saimanen EI, Partio TJ, et al. Supplemental postoperative oxygen in the prevention of surgical wound infection after lower limb vascular surgery: a
randomized controlled trial. World J Surg. 2011;35(6):1387-1395.
103. Webster J, Osborne S. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev. 2012;9(9):CD004985.
104. Byrne DJ, Napier A, Cuschieri A. The value of whole body disinfection in the prevention of postoperative wound infection in clean and potentially contaminated surgery.
A prospective, randomised, double-blind placebo-controlled clinical trial. Surg Res Commun. 1992;12(1):43-52.
105. Hayek LJ, Emerson JM, Gardner AM. A placebo-controlled trial of the effect of two preoperative baths or showers with chlorhexidine detergent on postoperative wound
infection rates. J Hosp Infect. 1987;10(2):165-172.
106. Rotter ML, Larsen SO, Cooke EM, et al. A comparison of the effects of preoperative whole-body bathing with detergent alone and with detergent containing
chlorhexidine gluconate on the frequency of wound infections after clean surgery. J Hosp Infect. 1988;11(4):310-320.
107. Veiga DF, Damasceno CA, Veiga-Filho J, et al. Randomized controlled trial of the effectiveness of chlorhexidine showers before elective plastic surgical procedures.
Infect Control Hosp Epidemiol. 2009;30(1):77-79.
108. Earnshaw JJ, Berridge DC, Slack RC, Makin GS, Hopkinson BR. Do preoperative chlorhexidine baths reduce the risk of infection after vascular reconstruction? Eur J
Vasc Surg. 1989;3(4):323-326.
109. Randall PE, Ganguli L, Marcuson RW. Wound infection following vasectomy. Br J Urol. 1983;55(5):564-567.
110. Wihlborg O. The effect of washing with chlorhexidine soap on wound infection rate in general surgery. A controlled clinical study. Ann Chir Gynaecol. 1987;76(5):263-
265.
111. Veiga DF, Damasceno CA, Veiga Filho J, et al. Influence of povidone-iodine preoperative showers on skin colonization in elective plastic surgery procedures. Plast
Reconstr Surg. 2008;121(1):115-118; discussion 119-120.
112. Murray MR, Saltzman MD, Gryzlo SM, Terry MA, Woodward CC, Nuber GW. Efficacy of preoperative home use of 2% chlorhexidine gluconate cloth before shoulder
surgery. J Shoulder Elbow Surg. 2011;20(6):928-933.
113. Ellenhorn JD, Smith DD, Schwarz RE, et al. Paint-only is equivalent to scrub-and-paint in preoperative preparation of abdominal surgery sites. J Am Coll Surg.
2005;201(5):737-741.
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
114. Segal CG, Anderson JJ. Preoperative skin preparation of cardiac patients. AORN J. 2002;76(5):821-828.
115. Gilliam DL, Nelson CL. Comparison of a one-step iodophor skin preparation versus traditional preparation in total joint surgery. Clin Orthop Relat Res. 1990(250):258-
260.
116. Saltzman MD, Nuber GW, Gryzlo SM, Marecek GS, Koh JL. Efficacy of surgical preparation solutions in shoulder surgery. J Bone Joint Surg Am. 2009;91(8):1949-
1953.
117. Roberts A, Wilcox K, Devineni R, Harris R, Osevala M. Skin preparation in CABG surgery: a prospective randomized trial. Complication Surg. 1995;14(6):724, 741-724,
747.
118. Hort KR, DeOrio JK. Residual bacterial contamination after surgical preparation of the foot or ankle with or without alcohol. Foot Ankle Int. 2002;23(10):946-948.
119. Sistla SC, Prabhu G, Sistla S, Sadasivan J. Minimizing wound contamination in a 'clean' surgery: comparison of chlorhexidine-ethanol and povidone-iodine.
Chemotherapy. 2010;56(4):261-267.
120. Darouiche RO, Wall MJ, Jr., Itani KM, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010;362(1):18-26.
121. Paocharoen V, Mingmalairak C, Apisarnthanarak A. Comparison of surgical wound infection after preoperative skin preparation with 4% chlorhexidine [correction of
chlohexidine] and povidone iodine: a prospective randomized trial. J Med Assoc Thai. 2009;92(7):898-902.
122. Bibbo C, Patel DV, Gehrmann RM, Lin SS. Chlorhexidine provides superior skin decontamination in foot and ankle surgery: a prospective randomized study. Clin
Orthop Relat Res. 2005;438:204-208.
123. Cheng K, Robertson H, St Mart JP, Leanord A, McLeod I. Quantitative analysis of bacteria in forefoot surgery: a comparison of skin preparation techniques. Foot Ankle
Int. 2009;30(10):992-997.
124. Veiga DF, Damasceno CAV, Veiga J, et al. Povidone iodine versus chlorhexidine in skin antisepsis before elective plastic surgery procedures: a randomized controlled
trial. Plast Reconstr Surg. 2008;122(5):170e-171e.
125. Berry AR, Watt B, Goldacre MJ, Thomson JW, McNair TJ. A comparison of the use of povidone-iodine and chlorhexidine in the prophylaxis of postoperative wound
infection. J Hosp Infect. 1982;3(1):55-63.
126. Ostrander RV, Botte MJ, Brage ME. Efficacy of surgical preparation solutions in foot and ankle surgery. J Bone Joint Surg Am. 2005;87(5):980-985.
127. Savage JW, Weatherford BM, Sugrue PA, et al. Efficacy of surgical preparation solutions in lumbar spine surgery. J Bone Joint Surg Am. 2012;94(6):490-494.
128. von Eckardstein AS, Lim CH, Dohmen PM, et al. A randomized trial of a skin sealant to reduce the risk of incision contamination in cardiac surgery. Ann Thorac Surg.
2011;92(2):632-637.
129. Iyer A, Gilfillan I, Thakur S, Sharma S. Reduction of surgical site infection using a microbial sealant: a randomized trial. J Thorac Cardiovasc Surg. 2011;142(2):438-
442.
130. Towfigh S, Cheadle WG, Lowry SF, Malangoni MA, Wilson SE. Significant reduction in incidence of wound contamination by skin flora through use of microbial
sealant. Arch Surg. 2008;143(9):885-891; discussion 891.
131. Dromzee E, Tribot-Laspiere Q, Bachy M, Zakine S, Mary P, Vialle R. Efficacy of integuseal for surgical skin preparation in children and adolescents undergoing scoliosis
correction. Spine (Phila Pa 1976). 2012;37(21):E1331-1335.
132. Ward HRG, Jennings OGN, Potgieter P, Lombard CJ. Do plastic adhesive drapes prevent post caesarean wound infection? J Hosp Infect. 2001;47(3):230-234.
133. Chiu KY, Lau SK, Fung B, Ng KH, Chow SP. Plastic adhesive drapes and wound infection after hip fracture surgery. Aust N Z J Surg. 1993;63(10):798-801.
134. Jackson DW, Pollock AV, Tindal DS. The value of a plastic adhesive drape in the prevention of wound infection. A controlled trial. Br J Surg. 1971;58(5):340-342.
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
135. Psaila JV, Wheeler MH, Crosby DL. The role of plastic wound drapes in the prevention of wound infection following abdominal surgery. Br J Surg. 1977;64(10):729-
732.
136. Dewan PA, Van Rij AM, Robinson RG, Skeggs GB, Fergus M. The use of an iodophor-impregnated plastic incise drape in abdominal surgery--a controlled clinical trial.
Aust N Z J Surg. 1987;57(11):859-863.
137. Sindelar WF, Mason GR. Intraperitoneal irrigation with povidone-iodine solution for the prevention of intra-abdominal abscesses in the bacterially contaminated
abdomen. Surg Gynecol Obstet. 1979;148(3):409-411.
138. Vallance S, Waldron R. Antiseptic vs. saline lavage in purulent and faecal peritonitis. J Hosp Infect. 1985;6 Suppl A:87-91.
139. Sindelar WF, Brower ST, Merkel AB, Takesue EI. Randomised trial of intraperitoneal irrigation with low molecular weight povidone-iodine solution to reduce intra-
abdominal infectious complications. J Hosp Infect. 1985;6 Suppl A:103-114.
140. Chang FY, Chang MC, Wang ST, Yu WK, Liu CL, Chen TH. Can povidone-iodine solution be used safely in a spinal surgery? Eur Spine J. 2006;15(6):1005-1014.
141. Cheng MT, Chang MC, Wang ST, Yu WK, Liu CL, Chen TH. Efficacy of dilute betadine solution irrigation in the prevention of postoperative infection of spinal surgery.
Spine (Phila Pa 1976). 2005;30(15):1689-1693.
142. Sindelar WF, Mason GR. Irrigation of subcutaneous tissue with povidone-iodine solution for prevention of surgical wound infections. Surg Gynecol Obstet.
1979;148(2):227-231.
143. Rogers DM, Blouin GS, O'Leary JP. Povidone-iodine wound irrigation and wound sepsis. Surg Gynecol Obstet. 1983;157(5):426-430.
144. Harihara Y, Konishi T, Kobayashi H, et al. Effects of applying povidone-iodine just before skin closure. Dermatology. 2006;212:53-57.
145. Frietsch T, Karger R, Scholer M, et al. Leukodepletion of autologous whole blood has no impact on perioperative infection rate and length of hospital stay. Transfusion.
2008;48(10):2133-2142.
146. Frietsch T, Krombholz K, Tolksdorf B, Nebe T, Segiet W, Lorentz A. Cellular immune response to autologous blood transfusion in hip arthroplasty: whole blood versus
buffy coat-poor packed red cells and fresh-frozen plasma. Vox Sang. 2001;81(3):187-193.
147. Innerhofer P, Klingler A, Klimmer C, Fries D, Nussbaumer W. Risk for postoperative infection after transfusion of white blood cell-filtered allogeneic or autologous
blood components in orthopedic patients undergoing primary arthroplasty. Transfusion. 2005;45(1):103-110.
148. Rosencher N, Kerkkamp HEM, Macheras G, et al. Orthopedic Surgery Transfusion Hemoglobin European Overview (OSTHEO) study: blood management in elective
knee and hip arthroplasty in Europe. Transfusion. 2003;43(4):459-469.
149. Weber EW, Slappendel R, Prins MH, van der Schaaf DB, Durieux ME, Strumper D. Perioperative blood transfusions and delayed wound healing after hip replacement
surgery: effects on duration of hospitalization. Anesth Analg. 2005;100(5):1416-1421, table of contents.
150. Llewelyn CA, Taylor RS, Todd AAM, et al. The effect of universal leukoreduction on postoperative infections and length of hospital stay in elective orthopedic and
cardiac surgery. Transfusion. 2004;44(4):489-500.
151. Pedersen AB, Mehnert F, Overgaard S, Johnsen SP. Allogeneic blood transfusion and prognosis following total hip replacement: a population-based follow up study.
BMC Musculoskelet Disord. 2009;10:167.
152. del Trujillo MM, Carrero A, Munoz M. The utility of the perioperative autologous transfusion system OrthoPAT (R) in total hip replacement surgery: a prospective study.
Arch Orthop Trauma Surg. 2008;128(10):1031-1038.
153. Borghi B, Casati A, Rizzoli Study Group on Orthopaedic Anaesthesia. Incidence and risk factors for allogenic blood transfusion during major joint replacement using an
integrated autotransfusion regimen. Eur J Anaesthesiol. 2000;17(7):411-417.
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
154. Momohara S, Kawakami K, Iwamoto T, et al. Prosthetic joint infection after total hip or knee arthroplasty in rheumatoid arthritis patients treated with nonbiologic and
biologic disease-modifying antirheumatic drugs. Mod Rheumatol. 2011;21(5):469-475.
155. Kawakami K, Ikari K, Kawamura K, et al. Complications and features after joint surgery in rheumatoid arthritis patients treated with tumour necrosis factor-alpha
blockers: perioperative interruption of tumour necrosis factor-alpha blockers decreases complications? Rheumatology (Oxford). 2010;49(2):341-347.
156. Hirano Y, Kojima T, Kanayama Y, et al. Influences of anti-tumour necrosis factor agents on postoperative recovery in patients with rheumatoid arthritis. Clin Rheumatol.
2010;29(5):495-500.
157. Perhala RS, Wilke WS, Clough JD, Segal AM. Local infectious complications following large joint replacement in rheumatoid arthritis patients treated with methotrexate
versus those not treated with methotrexate. Arthritis Rheum. 1991;34(2):146-152.
158. Bridges SL, Jr., Lopez-Mendez A, Han KH, Tracy IC, Alarcon GS. Should methotrexate be discontinued before elective orthopedic surgery in patients with rheumatoid
arthritis? J Rheumatol. 1991;18(7):984-988.
159. Carpenter MT, West SG, Vogelgesang SA, Casey Jones DE. Postoperative joint infections in rheumatoid arthritis patients on methotrexate therapy. Orthopedics.
1996;19(3):207-210.
160. Bongartz T, Halligan CS, Osmon DR, et al. Incidence and risk factors of prosthetic joint infection after total hip or knee replacement in patients with rheumatoid arthritis.
Arthritis Rheum. 2008;59(12):1713-1720.
161. Papavasiliou AV, Isaac DL, Marimuthu R, Skyrme A, Armitage A. Infection in knee replacements after previous injection of intra-articular steroid. J Bone Joint Surg Br.
2006;88B(3):321-323.
162. Desai A, Ramankutty S, Board T, Raut V. Does intraarticular steroid infiltration increase the rate of infection in subsequent total knee replacements? Knee.
2009;16(4):262-264.
163. Sreekumar R, Venkiteswaran R, Raut V. Infection in primary hip arthroplasty after previous steroid infiltration. Int Orthop. 2007;31(1):125-128.
164. McIntosh AL, Hanssen AD, Wenger DE, Osmon DR. Recent intraarticular steroid injection may increase infection rates in primary THA. Clin Orthop Relat Res.
2006;451:50-54.
165. Kaspar S, de Beer JD. Infection in hip arthroplasty after previous injection of steroid. J Bone Joint Surg Br. 2005;87B(4):454-457.
166. Turpie AGG, Bauer KA, Eriksson BL, Lassen MR, Steering Committees of the Pentasaccharide Orthopedic Prophylaxis Studies. Fondaparinux vs enoxaparin for the
prevention of venous thromboembolism in major orthopedic surgery - A meta-analysis of 4 randomized double-blind studies. Arch Intern Med. 2002;162(16):1833-1840.
167. Bauer KA, Eriksson BI, Lassen MR, Turpie AG, Steering Committee of the Pentasaccharide in Major Knee Surgery Study. Fondaparinux compared with enoxaparin for
the prevention of venous thromboembolism after elective major knee surgery. N Engl J Med. 2001;345(18):1305-1310.
168. Eriksson BI, Bauer KA, Lassen MR, Turpie AG, Steering Committee of the Pentasaccharide in Hip-Fracture Surgery Study. Fondaparinux compared with enoxaparin for
the prevention of venous thromboembolism after hip-fracture surgery. N Engl J Med. 2001;345(18):1298-1304.
169. Lassen MR, Bauer KA, Eriksson BI, Turpie AG, European Pentasaccharide Elective Surgery Study Steering Committee. Postoperative fondaparinux versus preoperative
enoxaparin for prevention of venous thromboembolism in elective hip-replacement surgery: a randomised double-blind comparison. Lancet. 2002;359(9319):1715-1720.
170. Turpie AG, Bauer KA, Eriksson BI, Lassen MR, Pentathalon Study Steering Committee. Postoperative fondaparinux versus postoperative enoxaparin for prevention of
venous thromboembolism after elective hip-replacement surgery: a randomised double-blind trial. Lancet. 2002;359(9319):1721-1726.
171. Eriksson BI, Borris LC, Friedman RJ, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N Engl J Med. 2008;358(26):2765-2775.
172. Kakkar AK, Brenner B, Dahl OE, et al. Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip
arthroplasty: a double-blind, randomised controlled trial. Lancet. 2008;372(9632):31-39.
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
173. Lassen MR, Ageno W, Borris LC, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty. N Engl J Med. 2008;358(26):2776-2786.
174. Turpie AG, Lassen MR, Davidson BL, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty (RECORD4): a randomised trial. Lancet.
2009;373(9676):1673-1680.
175. Patel VP, Walsh M, Sehgal B, Preston C, Dewal H, Di Cesare PE. Factors associated with prolonged wound drainage after primary total hip and knee arthroplasty. J Bone
Joint Surg Am. 2007;89A(1):33-38.
176. Asensio A, Antolin FJ, Sanchez-Garcia JM, et al. Timing of DVT prophylaxis and risk of postoperative knee prosthesis infection. Orthopedics. 2010;33(11):800.
177. Bozic KJ, Vail TP, Pekow PS, Maselli JH, Lindenauer PK, Auerbach AD. Does aspirin have a role in venous thromboembolism prophylaxis in total knee arthroplasty
patients? J Arthroplasty. 2010;25(7):1053-1060.
178. Sachs RA, Smith JH, Kuney M, Paxton L. Does anticoagulation do more harm than good? A comparison of patients treated without prophylaxis and patients treated with
low-dose warfarin after total knee arthroplasty. J Arthroplasty. 2003;18(4):389-395.
179. Parvizi J, Ghanem E, Joshi A, Sharkey PF, Hozack WJ, Rothman RH. Does "excessive" anticoagulation predispose to periprosthetic infection? J Arthroplasty.
2007;22(6):24-28.
180. Miner AL, Losina E, Katz JN, Fossel AH, Platt R. Deep infection after total knee replacement: impact of laminar airflow systems and body exhaust suits in the modern
operating room. Infect Control Hosp Epidemiol. 2007;28(2):222-226.
181. Hooper GJ, Rothwell AG, Frampton C, Wyatt MC. Does the use of laminar flow and space suits reduce early deep infection after total hip and knee replacement? The ten-
year results of the New Zealand Joint Registry. J Bone Joint Surg Br. 2011;93B(1):85-90.
182. Pasquarella C, Pitzurra O, Herren T, Poletti L, Savino A. Lack of influence of body exhaust gowns on aerobic bacterial surface counts in a mixed-ventilation operating
theatre. A study of 62 hip arthroplasties. J Hosp Infect. 2003;54(1):2-9.
183. Chiu FY, Chen CM, Lin CF, Lo WH. Cefuroxime-impregnated cement in primary total knee arthroplasty: a prospective, randomized study of three hundred and forty
knees. J Bone Joint Surg Am. 2002;84-A(5):759-762.
184. Chiu FY, Lin CF, Chen CM, Lo WH, Chaung TY. Cefuroxime-impregnated cement at primary total knee arthroplasty in diabetes mellitus. A prospective, randomised
study. J Bone Joint Surg Br. 2001;83(5):691-695.
185. Agency for Healthcare Research and Quality, Hartling L, Bond K, et al. Developing and Testing a Tool for the Classification of Study Designs in Systematic Reviews of
Interventions and Exposures. Developing and Testing a Tool for the Classification of Study Designs in Systematic Reviews of Interventions and Exposures 2010; AHRQ
Publication No. 11-EHC-007. :https://www.ncbi.nlm.nih.gov/books/NBK52670/pdf/Bookshelf_NBK52670.pdf. Accessed January 25, 2017.
2017 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/surg/0/ on 05/21/2017
You might also like
- Certificate (Yohanes)Document1 pageCertificate (Yohanes)Yohanes BongNo ratings yet
- Kmspico Install EditionDocument2 pagesKmspico Install EditionYohanes BongNo ratings yet
- Difference of Episleritis and ScleritisDocument8 pagesDifference of Episleritis and ScleritisYohanes BongNo ratings yet
- INAYAH I11111027 TuberkulosisDocument23 pagesINAYAH I11111027 TuberkulosisYohanes BongNo ratings yet
- Journal Reading YohanesDocument2 pagesJournal Reading YohanesYohanes BongNo ratings yet
- CatatanDocument2 pagesCatatanYohanes BongNo ratings yet
- Is There A Role of Intracellular Magnesium in Prevention of Heart Failure 2329 9495 1000148Document5 pagesIs There A Role of Intracellular Magnesium in Prevention of Heart Failure 2329 9495 1000148Yohanes BongNo ratings yet
- Hepatic Syndromes in RCCDocument5 pagesHepatic Syndromes in RCCYohanes BongNo ratings yet
- Scholastyka Febrylla I11111012 FASTDocument19 pagesScholastyka Febrylla I11111012 FASTYohanes BongNo ratings yet
- Right Ventricular Dysfunction in Myocardial Infarction A New Risk Factor For Clopidogrel Resistance 2155 9880 1000401Document5 pagesRight Ventricular Dysfunction in Myocardial Infarction A New Risk Factor For Clopidogrel Resistance 2155 9880 1000401Yohanes BongNo ratings yet
- Indonesia "The Islands Country"Document44 pagesIndonesia "The Islands Country"Yohanes BongNo ratings yet
- Acls Aha 2010Document67 pagesAcls Aha 2010heraaaaNo ratings yet
- Jadwal Jaga Emergency RSAADocument3 pagesJadwal Jaga Emergency RSAAYohanes BongNo ratings yet
- CV OliviaDocument2 pagesCV OliviaYohanes BongNo ratings yet
- CPR (The Simple One)Document22 pagesCPR (The Simple One)Yohanes BongNo ratings yet
- CPR (The Simple One)Document22 pagesCPR (The Simple One)Yohanes BongNo ratings yet
- National Project Dare To Dream in China Join Us If You Like Children EducationDocument3 pagesNational Project Dare To Dream in China Join Us If You Like Children EducationYohanes BongNo ratings yet
- CPR (The Simple One)Document22 pagesCPR (The Simple One)Yohanes BongNo ratings yet
- Pelargonium GuideDocument73 pagesPelargonium GuideYohanes BongNo ratings yet
- Konservasi - Sangon, YogyakartaDocument17 pagesKonservasi - Sangon, YogyakartaYohanes BongNo ratings yet
- Glandula SuprarenalisDocument6 pagesGlandula SuprarenalisYohanes BongNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Bartók On Folk Song and Art MusicDocument4 pagesBartók On Folk Song and Art MusiceanicolasNo ratings yet
- Unit 6 ListeningDocument27 pagesUnit 6 ListeningRagini Sanjay GhoshNo ratings yet
- Terpenoid and PerfumeDocument5 pagesTerpenoid and PerfumeJillian Mae DacerNo ratings yet
- ACC - COM220 Paper 2 Cultural Book Analysis (The House On Mango Street)Document10 pagesACC - COM220 Paper 2 Cultural Book Analysis (The House On Mango Street)chiquitagirlNo ratings yet
- Quiz Template: © WWW - Teachitscience.co - Uk 2017 28644 1Document49 pagesQuiz Template: © WWW - Teachitscience.co - Uk 2017 28644 1Paul MurrayNo ratings yet
- Language Assistant in ColombiaDocument2 pagesLanguage Assistant in ColombiaAndres CastañedaNo ratings yet
- TEST Lop 5Document3 pagesTEST Lop 5tan nguyen vanNo ratings yet
- Emcee RubricDocument1 pageEmcee RubricAdi Ruzaini Di EddyNo ratings yet
- 320 Lecture 26Document8 pages320 Lecture 26marcelofilgueirasNo ratings yet
- Data Rs910Document36 pagesData Rs910Cusco PardoNo ratings yet
- Circuit Theory NOV-DeC 2014Document12 pagesCircuit Theory NOV-DeC 2014sunil1237No ratings yet
- Seminar Assignments Ticket Vending MachineDocument13 pagesSeminar Assignments Ticket Vending MachineCandy SomarNo ratings yet
- NafsDocument3 pagesNafsMabub_sddqNo ratings yet
- PepsiDocument101 pagesPepsiashu548836No ratings yet
- Week 5 AssignmentDocument2 pagesWeek 5 AssignmentNGUYEN HAINo ratings yet
- Earnings Price Anomaly (Ray Ball, 1992)Document27 pagesEarnings Price Anomaly (Ray Ball, 1992)jeetNo ratings yet
- Module 6 - El FilibusterismoDocument4 pagesModule 6 - El FilibusterismoSilver GoldNo ratings yet
- ScienceDocument112 pagesScienceAnkit JainNo ratings yet
- Understanding First Language AcquisitionDocument4 pagesUnderstanding First Language AcquisitionShiela Mae Saladaga TanNo ratings yet
- Workshop 3-6: RCS of A Cube: Introduction To ANSYS HFSSDocument11 pagesWorkshop 3-6: RCS of A Cube: Introduction To ANSYS HFSSRicardo MichelinNo ratings yet
- Final InternshipDocument64 pagesFinal Internshippradeep100% (2)
- Principles-Versus Rules-Based Accounting Standards: The FASB's Standard Setting StrategyDocument24 pagesPrinciples-Versus Rules-Based Accounting Standards: The FASB's Standard Setting StrategyEhab AgwaNo ratings yet
- Turney-High - Primitive WarDocument280 pagesTurney-High - Primitive Warpeterakiss100% (1)
- Rifts - Novel - Path of The StormDocument104 pagesRifts - Novel - Path of The StormHoward Howen100% (1)
- Police Planning 2ndDocument8 pagesPolice Planning 2ndLester BalagotNo ratings yet
- Skripsi Tanpa Bab Pembahasan PDFDocument117 pagesSkripsi Tanpa Bab Pembahasan PDFArdi Dwi PutraNo ratings yet
- 2014 JC2 H2 Econs Prelim Paper 2Document3 pages2014 JC2 H2 Econs Prelim Paper 2Ezra Notsosure WongNo ratings yet
- FREE Soroban Abacus Mental Math Learning - BasicDocument74 pagesFREE Soroban Abacus Mental Math Learning - BasicTatyana Sukhomlinova100% (3)
- MEASURING HORIZONTAL DISTANCESDocument11 pagesMEASURING HORIZONTAL DISTANCESJosiah M. TubagaNo ratings yet
- Collage of Business and Economics Department of Management (MSC in Management Extension Program)Document4 pagesCollage of Business and Economics Department of Management (MSC in Management Extension Program)MikealayNo ratings yet