Professional Documents
Culture Documents
Common Bleeps
Uploaded by
Shannon RamsumairCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Common Bleeps
Uploaded by
Shannon RamsumairCopyright:
Available Formats
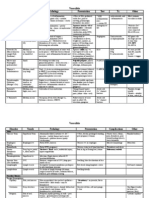
Common Junior Doctor On-call Bleeps
Table 1: Things to consider doing for unwell patients you are bleeped about when on-call (before you escalate to a senior if required)
Fall Tachycardia Hypotension Temperature spike Low urine output Chest pain Shortness of breath Confusion / GCS
Common causes 1. Mechanical 1. Dehydration/ 1. Fluid/blood loss 1. SIRS (sepsis most common 1. Hypovolaemia 1. Musculoskeletal 1. Anxiety 1. Dementia
2. Dehydration hypotension 2. Cardiogenic shock cause) 2. Blocked catheter 2. Arrhythmia 2. COPD/asthma 2. Delirium
3. Postural hypotension 2. Sepsis 3. Sepsis 2. Infections (e.g. chest, UTI) 3. Acute kidney injury 3. PE 3. PE 3. Sepsis
4. Confusion (electrolyte 3. Arrhythmia e.g. AF 4. Anaphylaxis Post-op -Pre: hypotension 4. MI/angina 4. Pneumonia 4. Electrolyte abnormality
abnormality/ dementia/ 4. PE Surgical collections -Renal: acute tubular 5. Oesophagitis/ 5. Pneumothorax 5. Neurological pathology (e.g.
sepsis) 5. Acute pain <2d = atelectasis necrosis, nephrotoxic oesophageal spasm 6. Atelectasis cerebral haemorrhage)
5. Arrhythmia 2-4d = pneumonia medications, GN 7. Arrhythmia
6. Aortic stenosis 4-6d = anastomotic leak -Post: urinary obstruction/ 8. Cardiac failure
6-8d = wound infection retention
8-10d = DVT/ PE
Complications Mechanical injury Reduced myocardial Acute kidney injury Fluid loss Acute tubular necrosis/ acute - Cerebral hypoxia Falls
Cerebral bleed function Reduced GCS Overwhelming sepsis kidney injury Reducing GCS
Arrhythmia End organ failure Airway compromise
Progressive disease
During call Witnessed? Head injury? Background Background Background Background Background Background Background
Background Observations Observations Observations Observations Observations Observations Pre-morbid state
Observations Fluid balance Fluid balance Observations
GCS
Before arrival ECG ECG Fluid challenge (if no Hx Bloods Flush/ change catheter ECG Oxygen Capillary glucose
(if possible) Postural BP of heart failure) Urine dip Bladder scan BP in both arms ECG
Background Read patient notes + latest investigation results
History Usual falls history Determine any symptoms SOCRATES Determine any Determine any symptoms
NS, CVS, RS systems Full systems review RS & CVS system symptoms Full systems review
reviews review RS & CVS system Collateral history
Headache/vomiting/injury Risk factors review
Examination Observations & postural BP Observations Observations Observations Observations Observations Observations Observations & cap glucose
GCS & pupils reactivity to Assess fluid balance Assess fluid balance Sepsis signs (cap refill, skin Assess fluid balance BP in both arms Cardiorespiratory GCS & pupils & orientation
light Look for infection GCS temp, pulse etc) Multi-system exam Cardiorespiratory exam Neurological exam
Neurological exam sources Hydration status exam Look for infection sources: Hydration status exam (esp exam Examine calves Sepsis signs (cap refill, skin
Look for injuries Multi-system exam (inc pulmonary/ multi-system exam, pulmonary/ peripheral Examine calves temp, pulse etc)
Skin: bruising/bleeding Calves (DVT) peripheral oedema) iatrogenic causes (surgical oedema) Look for infection sources:
Bone tenderness/shape Look for infection wounds, drains, lines), Examine/flush catheter multi-system exam + look at
(inc skull) & flex/rotate sources: multi-system exposure (look at skin, surgical wounds, drains,
hips (fractures) exam + look at surgical joints, peri-anal area) chest, etc
wounds, drains, chest
Investigations ECG ECG Image possible sources Full septic screen: B: U&Es + VBG (acidosis/low B: bloods, D-dimer if B: bloods, D-dimer if Bloods (inc calcium) + VBG
Bloods CT if: 2 or more vomits, U&Es + VBG of fluid loss B: bloods (WCC, Hb, plt bicarb/hyperkalaemia) low wells score, low wells score, (lactate)
Orifice tests pupils problem, severe Sepsis Ix if CXR if pulmonary (DIC)), blood cultures, VBG O: urine dip cardiac enzymes cardiac enzymes, Urine dip
X-rays/imaging headache, GCS decreased differential (see oedema (lactate) X: bladder scan (to (now and at 12 ABG if low sats Sepsis Ix if differential (see
ECG by 1 or more temperature spike) Sepsis Ix if differential O: urine dip, culture any determine if its urinary hours) O: sputum culture temperature spike)
Special tests Sepsis Ix if differential (see (see temperature spike) other fluids retention i.e. >500ml or true O: - X: CXR CT head if neurological
temperature spike) X: CXR, CT abdo if may low UO), consider renal USS X: CXR E: ECG pathology
have surgical collection E: - E: ECG S: -
E: - S: - S: -
S: -
ABCDE See OSCEstop ABCDE notes
management
Specific Treat cause Treat cause Fluid challenges Sepsis six Fluid bolus and reassess Treatment-dose Treat cause Treat cause (e.g. antibiotics
management Neurological observations Analgesia Treat cause of fluid loss Empirical antibiotics as per (repeat bladder scan if no clexane if PE likely Sit up if infection)
as per protocol if hit head Correct electrolytes hospital protocol UO) MONAC + Cardiology Oxygen/ saline nebs/ Airway placement if GCS <8
Empirical antibiotics Crystalloids (20-30ml/kg) Stop renal excreted drugs referral if MI salbutamol nebs/
if required Oxygen/saline nebs/ Catheterise (relieve retention Analgesia chest physio
Fluids salbutamol nebs/physio / accurately monitor fluid Oxygen Treatment-dose
If AF, consider rate Catheterise balance) or flush catheter clexane if PE likely
limiting medication Surgery may be needed Treat cause e.g. fluids for
(joint/ abdo/ necrosis pre-renal, relieve obstruction
sepsis) for post-renal
Other common bleeps include: Assess critically unwell patients (see OSCEstop ABCDE notes); Review blood results or chest x-rays (see OSCEstop interpretation notes); Clerking a new admission (see OSCEstop admission clerking notes); Clerk a patient for operation the following day (see OSCEstop pre-op
assessment notes); Post-operative complications (see OSCEstop post-op complications notes); Fluid prescriptions (see OSCEstop fluids notes); Narrow therapeutic range drug prescriptions (see OSCEstop monitoring narrow therapeutic range drugs notes)
2013 Dr Christopher Mansbridge at www.OSCEstop.com, a source of free OSCE exam notes for medical students finals OSCE revision
You might also like
- Differentials For Finals: - Pleuritic Chest Pain - Pulmonary Embolism - Pneumothorax PneumoniaDocument9 pagesDifferentials For Finals: - Pleuritic Chest Pain - Pulmonary Embolism - Pneumothorax PneumoniaOlivia MoranNo ratings yet
- ECG ReviewDocument146 pagesECG ReviewThea DinoNo ratings yet
- Hematology & Oncology - Passmedicine 2012Document64 pagesHematology & Oncology - Passmedicine 2012dheajst100% (1)
- SABER IM PrometricDocument71 pagesSABER IM Prometricisra zaidNo ratings yet
- Cardiovascular History: Chest PainDocument5 pagesCardiovascular History: Chest PainTom MallinsonNo ratings yet
- Endocarditis: (Post Strep Infection)Document8 pagesEndocarditis: (Post Strep Infection)Eben Ezar Dela CruzNo ratings yet
- Physical Diagnosis Overview Guide ScribdDocument117 pagesPhysical Diagnosis Overview Guide ScribdTrisNo ratings yet
- ECG Interpretations GoodDocument104 pagesECG Interpretations GoodaymenNo ratings yet
- Vasculitis: Disorder Vessels Pathology Presentation Test TX OtherDocument3 pagesVasculitis: Disorder Vessels Pathology Presentation Test TX OthermcwnotesNo ratings yet
- Valvular Heart DseDocument8 pagesValvular Heart DseJane Pineda CuraNo ratings yet
- IVMS Classic Cause-Findings Flash FactsDocument1,214 pagesIVMS Classic Cause-Findings Flash FactsMarc Imhotep Cray, M.D.No ratings yet
- Skin and MSK EverythingDocument31 pagesSkin and MSK EverythingBernard HernandezNo ratings yet
- IM Part 1 and 2 CombinedDocument100 pagesIM Part 1 and 2 CombinedsasghfdgNo ratings yet
- Recognize Valvular Heart Diseases and Their Clinical FeaturesDocument8 pagesRecognize Valvular Heart Diseases and Their Clinical FeaturesRobert So JrNo ratings yet
- ECG Interpretation DR - Rawan AlshreemDocument25 pagesECG Interpretation DR - Rawan AlshreemMarymii Al-sahlawiiNo ratings yet
- Amboss Hemolytic AnemiaDocument16 pagesAmboss Hemolytic AnemiaAhmed Ali100% (2)
- OPTOMED-HW2-Diabetic Retinopathy PDFDocument3 pagesOPTOMED-HW2-Diabetic Retinopathy PDFDanalie SalvadorNo ratings yet
- Medscape NeurologyDocument54 pagesMedscape NeurologyShannon RamsumairNo ratings yet
- (Warding) Guideline 1 - QCGH-HISTORY - PE - GUIDELINEDocument4 pages(Warding) Guideline 1 - QCGH-HISTORY - PE - GUIDELINEHynne Jhea Echavez100% (1)
- Treatment and Classification of Heart FailureDocument2 pagesTreatment and Classification of Heart FailureShannon RamsumairNo ratings yet
- Quizlet (4) MMMMMMDocument30 pagesQuizlet (4) MMMMMMnaimNo ratings yet
- Accordion Sign-Appearance (C. Difficile)Document41 pagesAccordion Sign-Appearance (C. Difficile)Andra HijratulNo ratings yet
- Growth Adaptations to Skin Pathology in PathomaDocument5 pagesGrowth Adaptations to Skin Pathology in PathomaKing John PascualNo ratings yet
- Internal Medicine Table SummaryDocument31 pagesInternal Medicine Table SummaryShazaan Nadeem100% (1)
- Respiratory Tract InfectionsDocument1 pageRespiratory Tract InfectionsShannon RamsumairNo ratings yet
- Acute AbdomenDocument47 pagesAcute AbdomenDani LeeNo ratings yet
- Discharge Summary Format Guide - How to Write a Discharge SummaryDocument1 pageDischarge Summary Format Guide - How to Write a Discharge SummaryeresdNo ratings yet
- Pathology Pneumonics For BegginersDocument38 pagesPathology Pneumonics For BegginersAnandNo ratings yet
- ENT Differential Diagnosis and History Taking NotesDocument12 pagesENT Differential Diagnosis and History Taking NotesStanley ShanNo ratings yet
- Heart Failure - Notes From "Cardiology" (Timmis Et Al) : Main CausesDocument3 pagesHeart Failure - Notes From "Cardiology" (Timmis Et Al) : Main CausesPrarthana Thiagarajan100% (3)
- Hematology Oncology - Anemia ApproachDocument1 pageHematology Oncology - Anemia ApproachEugen MNo ratings yet
- AA Vision and MissionDocument8 pagesAA Vision and MissionAkshata BansodeNo ratings yet
- Symptoms and Signs of Respiratory Disease Lecture 2: DyspnoeaDocument9 pagesSymptoms and Signs of Respiratory Disease Lecture 2: DyspnoeaShannon RamsumairNo ratings yet
- IMDocument128 pagesIMShaz ChindhyNo ratings yet
- Concise SEO-Optimized Title for Clotting DocumentDocument3 pagesConcise SEO-Optimized Title for Clotting DocumentRyan TurnerNo ratings yet
- ADHD: Clinical Practice Guideline For The Diagnosis, Evaluation, and TreatmentDocument18 pagesADHD: Clinical Practice Guideline For The Diagnosis, Evaluation, and TreatmentBen CulpepperNo ratings yet
- Two Ethics Case ScenariosDocument3 pagesTwo Ethics Case ScenariosEguia NielNo ratings yet
- Nursing Care PlanDocument7 pagesNursing Care Planmcd7r883% (6)
- Basic AudiologyDocument42 pagesBasic Audiologyapi-3743483100% (2)
- Scenar CourseDocument29 pagesScenar Courseretoxproductions100% (7)
- Detailed Lesson Plan in Mapeh 8 JoanneDocument9 pagesDetailed Lesson Plan in Mapeh 8 JoanneLANI JOY TABAMONo ratings yet
- QuizletDocument33 pagesQuizletnaimNo ratings yet
- CARAS SCUTSHEET 2nd EditDocument2 pagesCARAS SCUTSHEET 2nd EditFrances Katrina Siruno100% (1)
- Me 1Document74 pagesMe 1Shaz ChindhyNo ratings yet
- The Craming MDDocument132 pagesThe Craming MDRosalie Catalan EslabraNo ratings yet
- Step 2 CS - Headache DDX, Physical Exam, Work-UpDocument118 pagesStep 2 CS - Headache DDX, Physical Exam, Work-UpnaimNo ratings yet
- Urological History TakingDocument6 pagesUrological History TakingayuniNo ratings yet
- Dr. Ali’s Uworld Notes For Step 2 CK Infectious DiseasesDocument40 pagesDr. Ali’s Uworld Notes For Step 2 CK Infectious Diseasesmarina shawkyNo ratings yet
- Examination of The Central Nervous SystemDocument3 pagesExamination of The Central Nervous Systemkenners100% (13)
- Arteriolar Dilator Decreases After Load Ejection FractionDocument1 pageArteriolar Dilator Decreases After Load Ejection FractionJack GuccioneNo ratings yet
- Anti FungalsDocument5 pagesAnti FungalskakuNo ratings yet
- QuizletDocument37 pagesQuizletnaimNo ratings yet
- SketchyPath ChecklistDocument1 pageSketchyPath ChecklistFajar Raza100% (1)
- Post-Strep Infxn Ddressler's Sydrome: Endocarditis Valvular Dse Pericarditis Cardiac TamponadeDocument5 pagesPost-Strep Infxn Ddressler's Sydrome: Endocarditis Valvular Dse Pericarditis Cardiac TamponadeEben Ezar Dela CruzNo ratings yet
- Cardiac Murmurs and Maneuvers GuideDocument1 pageCardiac Murmurs and Maneuvers GuidePkernNo ratings yet
- Pulmonology Exam: Comprehensive Chest AssessmentDocument33 pagesPulmonology Exam: Comprehensive Chest AssessmentSagit Nauman81No ratings yet
- Quizlet (22) QQQQQDocument5 pagesQuizlet (22) QQQQQnaimNo ratings yet
- Approximate Equivalents:: 0.100 Gmn. 1.00 GMDocument8 pagesApproximate Equivalents:: 0.100 Gmn. 1.00 GMakane ryuNo ratings yet
- Henoch-Schonlein Purpura, Atopic Dermatitis, Seborrheic Dermatitis & Oral Isotretinoin TherapyDocument5 pagesHenoch-Schonlein Purpura, Atopic Dermatitis, Seborrheic Dermatitis & Oral Isotretinoin TherapyJoan ChoiNo ratings yet
- Internal Medicine NotesDocument271 pagesInternal Medicine NotesMUNNA shaik100% (1)
- Arterial DiseaseDocument57 pagesArterial DiseaseYil MosNo ratings yet
- Tiki Taka EndocrinoloyDocument17 pagesTiki Taka EndocrinoloykakuNo ratings yet
- Interpreting the Biochemisty PanelDocument4 pagesInterpreting the Biochemisty PanelNatalie KingNo ratings yet
- Breast Mass GuideDocument20 pagesBreast Mass GuideFabian Ramirez HincapiéNo ratings yet
- OME StudyGuide 3monthDocument6 pagesOME StudyGuide 3monthanaNo ratings yet
- NBME Neuro 2Document2 pagesNBME Neuro 2naimNo ratings yet
- EKG On June 13Document19 pagesEKG On June 13Shannon RamsumairNo ratings yet
- Effective listening skills for OET and IELTS examsDocument3 pagesEffective listening skills for OET and IELTS examsShannon RamsumairNo ratings yet
- IELTS Guidance by Rabia TM..docx - 1488817854459-1Document7 pagesIELTS Guidance by Rabia TM..docx - 1488817854459-1Shannon RamsumairNo ratings yet
- Asthma Lecture: Chronic Airway Inflammation, Triggers, and TreatmentDocument23 pagesAsthma Lecture: Chronic Airway Inflammation, Triggers, and TreatmentShannon RamsumairNo ratings yet
- Post Operative ComplicationsDocument2 pagesPost Operative ComplicationsShannon RamsumairNo ratings yet
- Streptococcus Australis MeningitisDocument4 pagesStreptococcus Australis MeningitisShannon RamsumairNo ratings yet
- Cervical SmearDocument1 pageCervical SmearShannon RamsumairNo ratings yet
- BronchiectasisDocument17 pagesBronchiectasisShannon RamsumairNo ratings yet
- BTL CounselingDocument9 pagesBTL CounselingShannon RamsumairNo ratings yet
- Guidelines For Common Medical EmergenciesDocument101 pagesGuidelines For Common Medical EmergenciesShannon RamsumairNo ratings yet
- The PartogramDocument6 pagesThe PartogramCamille AliNo ratings yet
- Skin Physical ExamDocument10 pagesSkin Physical ExamVenkatesan VidhyaNo ratings yet
- Pe CranialexamDocument35 pagesPe CranialexamJunaidahMubarakAliNo ratings yet
- Stillbirth CounselingDocument13 pagesStillbirth CounselingShannon RamsumairNo ratings yet
- Varicose VeinsDocument7 pagesVaricose VeinsTarran PhagooNo ratings yet
- Comm Health Communication Skills GuideDocument26 pagesComm Health Communication Skills GuideShannon RamsumairNo ratings yet
- Psychiatry AlcoholDocument1 pagePsychiatry AlcoholShannon RamsumairNo ratings yet
- An Introduction To Urinary Stone DiseaseDocument10 pagesAn Introduction To Urinary Stone DiseaseShannon RamsumairNo ratings yet
- Ospe Station 14 CaseDocument2 pagesOspe Station 14 CaseShannon RamsumairNo ratings yet
- Managing Asthma in The CaribbeanDocument73 pagesManaging Asthma in The CaribbeanShannon RamsumairNo ratings yet
- Practice Osce Scenarios PDFDocument20 pagesPractice Osce Scenarios PDFa1docNo ratings yet
- An Introduction To Prostatic DiseasesDocument18 pagesAn Introduction To Prostatic DiseasesShannon RamsumairNo ratings yet
- Acute AbdomenDocument2 pagesAcute AbdomenShannon RamsumairNo ratings yet
- Theme 4 - HTN in The OSCEDocument1 pageTheme 4 - HTN in The OSCEShannon RamsumairNo ratings yet
- Herpes Simplex Oral: EpidemiologyDocument5 pagesHerpes Simplex Oral: EpidemiologyFariz RamadhanNo ratings yet
- 4.3.1 Triage in Light of Four Hour TargetDocument16 pages4.3.1 Triage in Light of Four Hour TargetWilliam Wagner Müller XavierNo ratings yet
- Liver Exam Findings for DiseasesDocument2 pagesLiver Exam Findings for DiseasesSatrio WicaksonoNo ratings yet
- Introduction RHDDocument5 pagesIntroduction RHDapriellejoyjovenaNo ratings yet
- Ds OresolDocument2 pagesDs OresolShannie PadillaNo ratings yet
- Case 3Document18 pagesCase 3alwaysbeclosing52No ratings yet
- Uri Flush 3 Liquid Stones ProblemDocument4 pagesUri Flush 3 Liquid Stones ProblemSourabh KoshtaNo ratings yet
- Secondary Prevention Stroke AHA ChecklistDocument1 pageSecondary Prevention Stroke AHA ChecklistGyörgy HalászNo ratings yet
- Surgical Versus Medical Treatment of Drug-Resistant Epilepsy: A Systematic Review and Meta-AnalysisDocument10 pagesSurgical Versus Medical Treatment of Drug-Resistant Epilepsy: A Systematic Review and Meta-AnalysisSebastianNo ratings yet
- Rabie CateiDocument3 pagesRabie CateiC LNo ratings yet
- Journal ReadingDocument21 pagesJournal ReadingMelvita KurniawanNo ratings yet
- Crown 1Document1 pageCrown 1محمدعبده راشد الشاهريNo ratings yet
- Symptoms of A Stomach Ulcer - Ulcers of The StomachDocument3 pagesSymptoms of A Stomach Ulcer - Ulcers of The StomachmeoluoinhacNo ratings yet
- FINAL People BrochureDocument19 pagesFINAL People BrochureWilliam PerkinsNo ratings yet
- Population Dynamics and Control of ContraceptionDocument16 pagesPopulation Dynamics and Control of Contraceptionjaish8904No ratings yet
- S.S. Hospital OPD ScheduleDocument4 pagesS.S. Hospital OPD Schedulegaurav SinghNo ratings yet
- Phlebotomy TechniqueDocument87 pagesPhlebotomy TechniqueJigs YumangNo ratings yet
- Principles of Bag TechniqueDocument3 pagesPrinciples of Bag TechniqueClare AlcoberNo ratings yet
- Hospital PharmacyDocument19 pagesHospital PharmacySUMIT MASKENo ratings yet
- Case Report:: Microbrush Stamp TechniqueDocument2 pagesCase Report:: Microbrush Stamp TechniqueAlex LxNo ratings yet
- 21 CFR 1271 Human Cells Tissues and Cellular and Tissue-Based Products PDFDocument27 pages21 CFR 1271 Human Cells Tissues and Cellular and Tissue-Based Products PDFjgregors8683No ratings yet
- Dafpus IskDocument4 pagesDafpus IskmarsyaNo ratings yet
- Safety Regulations in CSSDocument4 pagesSafety Regulations in CSSMM Ayehsa Allian SchückNo ratings yet