Professional Documents
Culture Documents
Wse Week 1 2
Uploaded by
api-302138606Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Wse Week 1 2
Uploaded by
api-302138606Copyright:
Available Formats
Weekly Self Evaluation
Week 1 & 2
Manaia Genovia
SLO: Practice as a member of a multi-disciplinary health care team
This week in clinical, I actually felt like a member of health care team for my patient
instead of just an observer or helper. I completed my head-toe physical assessment with the
primary nurse who did a focus assessment instead of a thorough assessment. I read in the notes
that my patient had a heart murmur but when I listened to his heart sounds I wasnt sure on
what I should be hearing. I should have asked the primary nurse while we were doing the
assessment together. Later, I asked my clinical instructor to help me listen to his heart murmur
and now I know what to listen for in the future. I did not find any abnormal findings therefore I
reported to my CI and primary nurse that everything was within normal limits. When my
patient had a fever of 100.5F, I immediately told the primary nurse, who then instructed me
administer p.o. Tylenol and she would call the doctor to find out what they would like us to do.
My patient has a PICC and is on antibiotics so any sign of infection (fever, increased pain,
elevated labs) should be reported as soon as possible.
SLO: Demonstrate therapeutic communication skills in interactions and relationships
with families, individuals, and other members of the health care team with attention to the
identification and correction of non-therapeutic communication techniques.
This week in clinical, I had a thirteen-year-old male patient who has been in the
hospital for the past 3 weeks. Immediately, I asked him what his daily routine was so I could plan
around his day. I told him that my I would come around every hour to check him and at 0800 /
1200 I would take his VS and complete a head-toe physical assessment. He has a lot of people
coming in and out of the room, so I thought it would be important to let him know my objectives
for the day and want I needed to do with him. He was slightly irritable when I did my 1200
assessment and was saying no when I asked him if I could check his eyes with a penlight. He
asked me if he could do it to my eyes. I was hesitant at first, but I realized if he understood the
rationale he wouldnt be as resistant, so I allowed him to check my pupil reflex, which he got
very excited about it. I then explained the rationale behind checking his pulse, listening to his
lung/heart sounds, and capillary refill and he seemed very engaged. I learned that adolescents
like to know what to expect, so I kept that in mind during my time with my patient.
You might also like
- Careplan Week2Document2 pagesCareplan Week2api-302138606No ratings yet
- Makaha ClubhouseDocument1 pageMakaha Clubhouseapi-302138606No ratings yet
- Wse Week 4Document2 pagesWse Week 4api-302138606No ratings yet
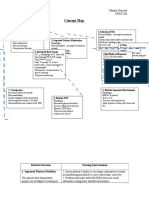
- Concept Map MgenoviaDocument5 pagesConcept Map Mgenoviaapi-302138606No ratings yet
- Sbar CommunicationDocument4 pagesSbar Communicationapi-302138606No ratings yet
- QUESTION: Does A Minor Have The Right To Request Contraception From A Doctor Without Parental Consent?Document5 pagesQUESTION: Does A Minor Have The Right To Request Contraception From A Doctor Without Parental Consent?api-302138606No ratings yet
- Wse Week 1 MgenoviaDocument2 pagesWse Week 1 Mgenoviaapi-302138606No ratings yet
- Wse Week 6 EportfolioDocument2 pagesWse Week 6 Eportfolioapi-302138606No ratings yet
- Emotion Color WheelDocument1 pageEmotion Color Wheelapi-302138606No ratings yet
- Health Policy Memo MgenoviaDocument5 pagesHealth Policy Memo Mgenoviaapi-302138606No ratings yet
- Uk Cultural PaperDocument6 pagesUk Cultural Paperapi-302138606No ratings yet
- Ethics Paper Final DraftDocument5 pagesEthics Paper Final Draftapi-302138606No ratings yet
- Mobility ReflectionDocument1 pageMobility Reflectionapi-302138606No ratings yet
- Diabetes HDL ArticleDocument3 pagesDiabetes HDL Articleapi-302138606No ratings yet
- Cover LetterDocument1 pageCover Letterapi-302138606No ratings yet
- MgenoviaresumeDocument1 pageMgenoviaresumeapi-302138606No ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Essentials For Nursing Practice 8th Edition Potter Test BankDocument25 pagesEssentials For Nursing Practice 8th Edition Potter Test BankMatthewCurryeaqy100% (55)
- Medical List For Regular28 09 2018Document97 pagesMedical List For Regular28 09 2018RahulPrakash0% (1)
- Impact of Nursing Diagnoses On Patient and Organisational Outcomes: A Systematic Literature ReviewDocument43 pagesImpact of Nursing Diagnoses On Patient and Organisational Outcomes: A Systematic Literature ReviewLucas Teles IanniNo ratings yet
- Social and Public HealthDocument54 pagesSocial and Public HealthMekuriya BeregaNo ratings yet
- Health Programme (Ayurveda Library - Dr. Vivek Tiwari) 2Document24 pagesHealth Programme (Ayurveda Library - Dr. Vivek Tiwari) 2NinnnNo ratings yet
- Windshield Survey: Elements & Descriptions Community ObservationsDocument6 pagesWindshield Survey: Elements & Descriptions Community Observationslesliecurtis79100% (12)
- TP Leads - GurgaonDocument32 pagesTP Leads - GurgaonDeepika Aggarwal0% (1)
- 506371Document256 pages506371Dandhi Firmansyah100% (1)
- National Hospital StandardsDocument267 pagesNational Hospital Standardsقمةالثقه100% (1)
- Simon.-Ideas For IELTS Topics (Updated)Document47 pagesSimon.-Ideas For IELTS Topics (Updated)Phuong DinhNo ratings yet
- Temporary Anchorage Devices in OrthodonticsDocument435 pagesTemporary Anchorage Devices in OrthodonticsAmrita Shrestha100% (5)
- Peran IPCNDocument38 pagesPeran IPCNSANITASI LINGKUNGAN RSPBGNo ratings yet
- Disaster Management in NursingDocument12 pagesDisaster Management in NursingSameeksha SinghNo ratings yet
- Resume2 DraftDocument3 pagesResume2 Draftapi-527335577No ratings yet
- Hemophilia Burden of Disease: A Systematic Review of The Cost-Utility Literature For HemophiliaDocument11 pagesHemophilia Burden of Disease: A Systematic Review of The Cost-Utility Literature For HemophiliaRiszyu Almas SuriszNo ratings yet
- Origins of Writing Ancient Civilizations Attributed The Origins of Writing To The GodsDocument8 pagesOrigins of Writing Ancient Civilizations Attributed The Origins of Writing To The GodsPeHmyang Pineda DielNo ratings yet
- Apmc National Internship Program PrimerDocument10 pagesApmc National Internship Program PrimerSMR100% (1)
- Community-Based Immunization RecordDocument3 pagesCommunity-Based Immunization RecordEngelynAbuzoTambis-AndajaoNo ratings yet
- Facts and Figures: Geographical and Demographic ProfileDocument4 pagesFacts and Figures: Geographical and Demographic ProfileJulius MarcelinoNo ratings yet
- Hofstede's Dimensions Milestone 2Document14 pagesHofstede's Dimensions Milestone 2Wambui WangechiNo ratings yet
- Genicular Nerve Ablation Zeitlinger2019Document7 pagesGenicular Nerve Ablation Zeitlinger2019drjorgewtorresNo ratings yet
- Healing The Incest WoundDocument1 pageHealing The Incest WoundLaura Paola GarciaNo ratings yet
- Dying To Get High Marijuana As MedicineDocument2 pagesDying To Get High Marijuana As MedicineEmil PyykönenNo ratings yet
- Clinical Lab TechnqDocument67 pagesClinical Lab TechnqRatnamala SarmaNo ratings yet
- Memisovski V Maram PowerpointDocument29 pagesMemisovski V Maram Powerpointgummybear917100% (1)
- The Somatic Movement Coach ProgrammesDocument24 pagesThe Somatic Movement Coach ProgrammesIrina Moldoveanu100% (2)
- 1169 2589 1 PBDocument6 pages1169 2589 1 PBnurul khaeriaNo ratings yet
- Medicare Correct Coding GD PDFDocument58 pagesMedicare Correct Coding GD PDFvrushgangNo ratings yet
- Bhaisajya Kalpana Vijnanam PDFDocument610 pagesBhaisajya Kalpana Vijnanam PDFVedant Agrawal86% (14)
- Lakhmir Singh Solutions Class 9 Biology Chapter 5 Why Do We Fall IllDocument4 pagesLakhmir Singh Solutions Class 9 Biology Chapter 5 Why Do We Fall IllPremshankar RajbharNo ratings yet