Professional Documents
Culture Documents
Nejm 200005043421801
Uploaded by
api-354040213Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nejm 200005043421801
Uploaded by
api-354040213Copyright:
Available Formats
The New England
Journal of Medicine
Co py r ig ht , 2 0 0 0 , by t he Ma s s ac h u s e t t s Me d ic a l S o c ie t y
VOL UME 3 4 2 M A Y 4, 2000 NUM B ER 18
VENTILATION WITH LOWER TIDAL VOLUMES AS COMPARED WITH
TRADITIONAL TIDAL VOLUMES FOR ACUTE LUNG INJURY
AND THE ACUTE RESPIRATORY DISTRESS SYNDROME
THE ACUTE RESPIRATORY DISTRESS SYNDROME NETWORK*
T
ABSTRACT HE mortality rate from acute lung injury
Background Traditional approaches to mechanical and the acute respiratory distress syndrome1
ventilation use tidal volumes of 10 to 15 ml per kilo- is approximately 40 to 50 percent.2-4 Al-
gram of body weight and may cause stretch-induced though substantial progress has been made
lung injury in patients with acute lung injury and the in elucidating the mechanisms of acute lung injury,5
acute respiratory distress syndrome. We therefore there has been little progress in developing effective
conducted a trial to determine whether ventilation treatments.
with lower tidal volumes would improve the clinical Traditional approaches to mechanical ventilation
outcomes in these patients.
use tidal volumes of 10 to 15 ml per kilogram of body
Methods Patients with acute lung injury and the
acute respiratory distress syndrome were enrolled in
weight.6 These volumes are larger than those in nor-
a multicenter, randomized trial. The trial compared mal subjects at rest (range, 7 to 8 ml per kilogram),
traditional ventilation treatment, which involved an but they are frequently necessary to achieve normal
initial tidal volume of 12 ml per kilogram of predicted values for the partial pressure of arterial carbon diox-
body weight and an airway pressure measured after ide and pH. Since atelectasis and edema reduce aer-
a 0.5-second pause at the end of inspiration (plateau ated lung volumes in patients with acute lung injury
pressure) of 50 cm of water or less, with ventilation and the acute respiratory distress syndrome,7,8 inspir-
with a lower tidal volume, which involved an initial atory airway pressures are often high, suggesting the
tidal volume of 6 ml per kilogram of predicted body presence of excessive distention, or stretch, of the
weight and a plateau pressure of 30 cm of water or aerated lung. In animals, ventilation with the use of
less. The first primary outcome was death before a
patient was discharged home and was breathing
large tidal volumes caused the disruption of pulmo-
without assistance. The second primary outcome nary epithelium and endothelium, lung inflammation,
was the number of days without ventilator use from atelectasis, hypoxemia, and the release of inflamma-
day 1 to day 28. tory mediators.9-14 The release of inflammatory me-
Results The trial was stopped after the enrollment diators could increase lung inflammation and cause in-
of 861 patients because mortality was lower in the jury to other organs.10,15 Thus, the traditional approach
group treated with lower tidal volumes than in the to mechanical ventilation may exacerbate or perpet-
group treated with traditional tidal volumes (31.0 per- uate lung injury in patients with acute lung injury and
cent vs. 39.8 percent, P=0.007), and the number of the acute respiratory distress syndrome and increase
days without ventilator use during the first 28 days the risk of nonpulmonary organ or system failure.
after randomization was greater in this group (mean
[SD], 1211 vs. 1011; P=0.007). The mean tidal
volumes on days 1 to 3 were 6.20.8 and 11.80.8 ml
per kilogram of predicted body weight (P<0.001), re-
spectively, and the mean plateau pressures were The writing committee (Roy G. Brower, M.D., Johns Hopkins Univer-
sity, Baltimore; Michael A. Matthay, M.D., University of California, San
256 and 338 cm of water (P<0.001), respectively. Francisco; Alan Morris, M.D., LDS Hospital, Salt Lake City; David
Conclusions In patients with acute lung injury and Schoenfeld, Ph.D., and B. Taylor Thompson, M.D., Massachusetts General
the acute respiratory distress syndrome, mechanical Hospital, Boston; and Arthur Wheeler, M.D., Vanderbilt University, Nash-
ventilation with a lower tidal volume than is tradition- ville) assumes responsibility for the overall content and integrity of the
manuscript. Address reprint requests to Dr. Brower at the Division of
ally used results in decreased mortality and increas- Pulmonary and Critical Care Medicine, Johns Hopkins University, 600
es the number of days without ventilator use. (N Engl N. Wolfe St., Baltimore, MD 21287.
J Med 2000;342:1301-8.) *Members of the Acute Respiratory Distress Syndrome (ARDS) Net-
2000, Massachusetts Medical Society. work are listed in the Appendix.
Vol ume 342 Numb er 18 1301
The New England Journal of Medicine
Downloaded from nejm.org on April 7, 2017. For personal use only. No other uses without permission.
Copyright 2000 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
The use of lower tidal volumes during ventilation Ventilator Procedures
in patients with acute lung injury and the acute res- The volume-assistcontrol mode was used for the ventilator un-
piratory distress syndrome may reduce injurious lung til the patient was weaned from the device or for 28 days after
randomization on day 0. Because normal lung volumes are predict-
stretch and the release of inflammatory mediators.16-18 ed on the basis of sex and height, 26,27 a predicted body weight
However, this approach may cause respiratory aci- was calculated for each patient from these data. 28 The predicted
dosis16,17 and decrease arterial oxygenation19,20 and body weight of male patients was calculated as equal to 50+
may therefore require changes in the priority of some 0.91(centimeters of height152.4); that of female patients was
objectives in the care of these patients. With the tra- calculated as equal to 45.5+0.91(centimeters of height152.4).
In the group treated with traditional tidal volumes, the initial tid-
ditional approach, the attainment of normal partial al volume was 12 ml per kilogram of predicted body weight. This
pressure of arterial carbon dioxide and pH is given was subsequently reduced stepwise by 1 ml per kilogram of pre-
a higher priority than is protection of the lung from dicted body weight if necessary to maintain the airway pressure
excessive stretch. With an approach that involves low- measured after a 0.5-second pause at the end of inspiration (plateau
pressure) at a level of 50 cm of water or less. The minimal tidal vol-
er tidal volumes, the reverse is true. Uncontrolled ume was 4 ml per kilogram of predicted body weight. If the pla-
studies suggested that the use of a lower tidal volume teau pressure dropped below 45 cm of water, the tidal volume was
would reduce mortality in patients with acute lung increased in steps of 1 ml per kilogram of predicted body weight
injury and the acute respiratory distress syndrome,17 until the plateau pressure was at least 45 cm of water or the tidal
but the results of four randomized trials of lung- volume was 12 ml per kilogram of predicted body weight.
In the group treated with lower tidal volumes, the tidal volume
protecting ventilation strategies have been conflict- was reduced to 6 ml per kilogram of predicted body weight within
ing.21-24 The present trial was conducted to deter- four hours after randomization and was subsequently reduced
mine whether the use of a lower tidal volume with stepwise by 1 ml per kilogram of predicted body weight if neces-
mechanical ventilation would improve important clin- sary to maintain plateau pressure at a level of no more than 30 cm
of water. The minimal tidal volume was 4 ml per kilogram of pre-
ical outcomes in such patients. dicted body weight. If plateau pressure dropped below 25 cm of
water, tidal volume was increased in steps of 1 ml per kilogram of
METHODS predicted body weight until the plateau pressure was at least 25 cm
Patients of water or the tidal volume was 6 ml per kilogram of predicted
body weight. For patients with severe dyspnea, the tidal volume
Patients were recruited from March 1996 through March 1999 could be increased to 7 to 8 ml per kilogram of predicted body
at the 10 university centers of the Acute Respiratory Distress Syn- weight if the plateau pressure remained 30 cm of water or less.
drome Network of the National Heart, Lung, and Blood Institute Plateau pressures were measured with a half-second inspiratory
(the centers are listed in the Appendix). The protocol was approved pause at four-hour intervals and after changes in the tidal volume
by the institutional review board at each hospital, and informed or positive end-expiratory pressure. Plateau pressures of more than
consent was obtained from the patients or surrogates at all but 50 cm of water in the patients in the group treated with tradi-
one hospital, where this requirement was waived. A complete de- tional tidal volumes and of more than 30 cm of water in patients
scription of the methods is available on the World Wide Web (at in the group treated with lower tidal volumes were allowed if the
www.ardsnet.org) or from the National Auxiliary Publications tidal volume was 4 ml per kilogram of predicted body weight or
Service (NAPS).* if arterial pH was less than 7.15.
Patients who were intubated and receiving mechanical ventila- All other objectives and ventilation procedures, including wean-
tion were eligible for the study if they had an acute decrease in ing, were identical in the two study groups (Table 1). If a patient
the ratio of partial pressure of arterial oxygen to fraction of in- became able to breathe without assistance but subsequently re-
spired oxygen to 300 or less (indicating the onset of hypoxemia; quired additional mechanical ventilation within a period of 28 days,
values were adjusted for altitude in Denver and Salt Lake City), the same tidal-volume protocol was resumed.
bilateral pulmonary infiltrates on a chest radiograph consistent with
the presence of edema, and no clinical evidence of left atrial hy- Organ or System Failure
pertension or (if measured) a pulmonary-capillary wedge pressure
Patients were monitored daily for 28 days for signs of the fail-
of 18 mm Hg or less.1 Patients were excluded if 36 hours had
ure of nonpulmonary organs and systems.29 Circulatory failure
elapsed since they met the first three criteria; they were younger
was defined as a systolic blood pressure of 90 mm Hg or less or
than 18 years of age; they had participated in other trials within
the need for treatment with any vasopressor; coagulation failure as
30 days before the first three criteria were met; they were preg-
a platelet count of 80,000 per cubic millimeter or less; hepatic fail-
nant; they had increased intracranial pressure, neuromuscular dis-
ure as a serum bilirubin concentration of at least 2 mg per deciliter
ease that could impair spontaneous breathing, sickle cell disease,
(34 mol per liter); and renal failure as a serum creatinine concen-
or severe chronic respiratory disease; they weighed more than 1 kg
tration of at least 2 mg per deciliter (177 mol per liter). We cal-
per centimeter of height; they had burns over more than 30
culated the number of days without organ or system failure by sub-
percent of their body-surface area; they had other conditions with
tracting the number of days with organ failure from the lesser of 28
an estimated 6-month mortality rate of more than 50 percent; they
days or the number of days to death. Organs and systems were con-
had undergone bone marrow or lung transplantation; they had
sidered failure-free after patients were discharged from the hospital.
chronic liver disease (as defined by ChildPugh class C)25; or their
attending physician refused or was unwilling to agree to the use Plasma Interleukin-6 Concentrations
of full life support.
A centralized interactive voice system was used for randomiza- Blood samples were obtained from 204 of the first 234 patients
tion. Patients were randomly assigned to receive mechanical ven- on day 0 and on day 3 for measurement of plasma interleukin-6
tilation involving either traditional tidal volumes or lower tidal by immunoassay (R & D Systems, Minneapolis).30 Blood samples
volumes. were stored in sterile EDTA-treated glass tubes.
Data Collection
*See NAPS document no. 05542 for 15 pages of supplementary materi-
al. To order, contact NAPS, c/o Microfiche Publications, 248 Hempstead Data on demographic, physiologic, and radiographic character-
Tpk., West Hempstead, NY 11552. istics, coexisting conditions, and medications were recorded with-
1302 May 4 , 2 0 0 0
The New England Journal of Medicine
Downloaded from nejm.org on April 7, 2017. For personal use only. No other uses without permission.
Copyright 2000 Massachusetts Medical Society. All rights reserved.
V E N T I L AT I O N W I T H L OW E R T I DA L VOLU M E S I N PAT I E N T S W I T H T H E AC U T E R E S P I R ATORY D I ST R E S S SY N D R O M E
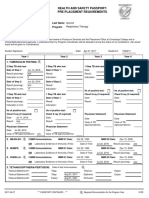
TABLE 1. SUMMARY OF VENTILATOR PROCEDURES.*
GROUP RECEIVING GROUP RECEIVING
TRADITIONAL TIDAL LOWER TIDAL
VARIABLE VOLUMES VOLUMES
Ventilator mode Volume assistcontrol Volume assistcontrol
Initial tidal volume (ml/kg of predicted body 12 6
weight)
Plateau pressure (cm of water) 50 30
Ventilator rate setting needed to achieve a pH 635 635
goal of 7.3 to 7.45 (breaths/min)
Ratio of the duration of inspiration to the 1:11:3 1:11:3
duration of expiration
Oxygenation goal PaO2, 5580 mm Hg, PaO2, 5580 mm Hg,
or SpO2, 8895% or SpO2, 8895%
Allowable combinations of FiO2 and PEEP 0.3 and 5 0.3 and 5
(cm of water) 0.4 and 5 0.4 and 5
0.4 and 8 0.4 and 8
0.5 and 8 0.5 and 8
0.5 and 10 0.5 and 10
0.6 and 10 0.6 and 10
0.7 and 10 0.7 and 10
0.7 and 12 0.7 and 12
0.7 and 14 0.7 and 14
0.8 and 14 0.8 and 14
0.9 and 14 0.9 and 14
0.9 and 16 0.9 and 16
0.9 and 18 0.9 and 18
1.0 and 18 1.0 and 18
1.0 and 20 1.0 and 20
1.0 and 22 1.0 and 22
1.0 and 24 1.0 and 24
Weaning By pressure support; re- By pressure support; re-
quired by protocol quired by protocol
when FiO2 0.4 when FiO2 0.4
*PaO2 denotes partial pressure of arterial oxygen, SpO2 oxyhemoglobin saturation measured by
pulse oximetry, FiO2 fraction of inspired oxygen, and PEEP positive end-expiratory pressure.
Subsequent adjustments in tidal volume were made to maintain a plateau pressure of 50 cm of
water in the group receiving traditional tidal volumes and 30 cm of water in the group receiving
lower tidal volumes.
Further increases in PEEP, to 34 cm of water, were allowed but were not required.
in four hours before the ventilator settings were changed on day 0. ence in ventilator-free days could reflect a difference in mortality,
Physiologic and radiographic data, medication use, and use of oth- ventilator days among survivors, or both. Other outcomes were
er investigational treatments were recorded between 6 and 10 a.m. the number of days without organ or system failure and the oc-
on days 1, 2, 3, 4, 7, 14, 21, and 28. Data were transmitted weekly currence of barotrauma, defined as any new pneumothorax, pneu-
to the network coordinating center. Patients were followed until momediastinum, or subcutaneous emphysema, or a pneumatocele
day 180 or until they were breathing on their own at home. that was more than 2 cm in diameter. Interim analyses were con-
ducted by an independent data and safety monitoring board after
Assessment of Compliance the enrollment of each successive group of approximately 200 pa-
tients. Stopping boundaries (with a two-sided a level of 0.05) were
Randomly selected ventilator and blood gas variables were an-
designed to allow early termination of the study if the use of lower
alyzed for compatibility with the protocol. Quarterly reports of
tidal volumes was found to be either efficacious31 or ineffective.32
these data from each of the 10 centers were used by investigators
The comparison of traditional with lower tidal volumes was
to assess compliance.
one of two trials conducted simultaneously in the same patients
in a factorial experimental design. Ketoconazole was compared with
Statistical Analysis
placebo in the first 234 patients, and lisofylline was compared with
The first primary outcome was death before a patient was dis- placebo in the last 194 patients; no drugs were assessed in the
charged home and was breathing without assistance. Patients who middle 433 patients.
were in other types of health care facilities at 180 days were con- We used Students t-test or Fishers exact test to compare base-
sidered to have been discharged from the hospital and to be breath- line variables. We used analysis of covariance to compare log-trans-
ing without assistance. The second primary outcome was ventila- formed plasma interleukin-6 values. We used Wilcoxons test to
tor-free days, defined as the number of days from day 1 to day 28 compare the day 0 and day 3 plasma interleukin-6 concentrations,
on which a patient breathed without assistance, if the period of ventilator-free days, and organ-failurefree days, which had skewed
unassisted breathing lasted at least 48 consecutive hours. A differ- distributions. We used the 180-day cumulative incidence of mor-
Vol ume 342 Numb er 18 1303
The New England Journal of Medicine
Downloaded from nejm.org on April 7, 2017. For personal use only. No other uses without permission.
Copyright 2000 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
tality to compare the proportion of patients in each group who nificantly lower on days 1, 3, and 7 in the group
died before being discharged home and breathing without assist- treated with lower tidal volumes than in the group
ance,33 after stratification for other experimental interventions:
treatment with ketoconazole, the ketoconazole placebo, lisofylline, treated with traditional tidal volumes (Table 3). The
the lisofylline placebo, or no other agent. We used a chi-square mean (SD) tidal volumes on days 1 to 3 were 6.2
test to determine whether there was an interaction between the 0.8 and 11.80.8 ml per kilogram of predicted body
study group and the other experimental interventions with re- weight (P<0.001), respectively, and the mean pla-
spect to the mean (SE) mortality rates at 180 days. All P values
are two-sided.
teau pressures were 256 and 338 cm of water
(P<0.001), respectively. The partial pressure of ar-
RESULTS terial oxygen was similar in the two groups at all three
The trial was stopped after the fourth interim analy- times, but the positive end-expiratory pressure and
sis because the use of lower tidal volumes was found fraction of inspired oxygen were significantly higher
to be efficacious (P=0.005 for the difference in mor- and the ratio of partial pressure of arterial oxygen to
tality between groups; P value for the stopping bound- fraction of inspired oxygen was significantly lower in
ary, 0.023). The base-line characteristics of the 861 the group treated with lower tidal volumes on days
patients who were enrolled were similar, except that 1 and 3. On day 7, positive end-expiratory pressure
minute ventilation was slightly but significantly high- and the fraction of inspired oxygen were significantly
er (P=0.01) in the group treated with lower tidal higher in the group treated with traditional tidal vol-
volumes (Table 2). umes. The respiratory rate was significantly higher in
The tidal volumes and plateau pressures were sig- the group treated with lower tidal volumes on days
1 and 3, but minute ventilation was similar in the two
groups on these days. The partial pressure of arterial
carbon dioxide was significantly higher on days 1, 3,
and 7 and arterial pH was significantly lower on days
TABLE 2. BASE-LINE CHARACTERISTICS OF THE PATIENTS.*
1 and 3 in the group treated with lower tidal volumes.
The probability of survival and of being discharged
home and breathing without assistance during the
GROUP RECEIVING
LOWER
GROUP RECEIVING
TRADITIONAL
first 180 days after randomization is shown in Figure
TIDAL VOLUMES TIDAL VOLUMES 1. The mortality rate was 39.8 percent in the group
CHARACTERISTIC (N=432) (N=429) treated with traditional tidal volumes and 31.0 per-
Age (yr) 5117 5218 cent in the group treated with lower tidal volumes
Female sex (%) 40 41 (P=0.007; 95 percent confidence interval for the
Race or ethnic group (%) difference between groups, 2.4 to 15.3 percent). The
White 75 71 interaction between the study group and stratifica-
Black 16 19
Hispanic 5 7 tion for other experimental interventions was not sig-
Other or unknown 4 3 nificant (P=0.16).
APACHE III score 8128 8428 Data were available to calculate the static compli-
PaO2:FiO2 13864 13458 ance of the respiratory system at base line in 517 pa-
PaO2:FiO2 200 (%) 82 85
tients (Fig. 2). The interaction between the quartile
Tidal volume (ml) 676119 665125
of static compliance at base line and the study group
Minute ventilation (liters/min) 13.44.3 12.74.3
No. of nonpulmonary organ or 1.81.1 1.81.0
with respect to the risk of death was not significant
system failures (P=0.49).
Lung injury (%) The number of ventilator-free days was significantly
Pneumonia 33 36 higher in the group treated with lower tidal volumes
Sepsis 27 26
Aspiration 15 14 than in the group treated with traditional tidal vol-
Trauma 13 9 umes (Table 4). The median duration of ventilation
Other causes 10 11
Multiple transfusions 2 3
was 8 days among patients in both groups who were
discharged from the hospital after weaning and 10.5
*Plusminus values are means SD. Because of rounding, not all per- and 10 days, respectively, among those who died in
centages total 100. PaO2 denotes partial pressure of arterial oxygen, and
FiO2 fraction of inspired oxygen.
the group treated with lower tidal volumes and the
APACHE III denotes Acute Physiology, Age, and Chronic Health Eval-
group treated with traditional tidal volumes. The num-
uation. Scores can range from 0 to 299, with higher scores indicating more ber of days without nonpulmonary organ or system
severe illness.34 failure was significantly higher in the group treated
Data were missing for one patient. with lower tidal volumes (P=0.006). This group had
Data were available for 300 patients in the group treated with lower tid- more days without circulatory failure (mean [SD],
al volumes and for 290 patients in the group treated with traditional tidal
volumes. 1910 vs. 1711 days; P=0.004), coagulation fail-
P=0.01. ure (2110 vs. 1911 days, P=0.004), and renal
Organ and system failures were defined as described in the Methods failure (2011 vs. 1811 days, P=0.005) than did
section. the group treated with traditional tidal volumes. The
1304 May 4 , 2 0 0 0
The New England Journal of Medicine
Downloaded from nejm.org on April 7, 2017. For personal use only. No other uses without permission.
Copyright 2000 Massachusetts Medical Society. All rights reserved.
V E N T I L AT I O N W I T H L OW E R T I DA L VOLU M E S I N PAT I E N T S W I T H T H E AC U T E R E S P I R ATORY D I ST R E S S SY N D R O M E
TABLE 3. RESPIRATORY VALUES DURING THE FIRST SEVEN DAYS OF TREATMENT IN PATIENTS WITH ACUTE LUNG INJURY
AND THE ACUTE RESPIRATORY DISTRESS SYNDROME.*
VARIABLE DAY 1 DAY 3 DAY 7
GROUP GROUP GROUP
GROUP RECEIVING GROUP RECEIVING GROUP RECEIVING
RECEIVING TRADITIONAL RECEIVING TRADITIONAL RECEIVING TRADITIONAL
LOWER TIDAL TIDAL LOWER TIDAL TIDAL LOWER TIDAL TIDAL
VOLUMES VOLUMES VOLUMES VOLUMES VOLUMES VOLUMES
Tidal volume (ml/kg of predicted 6.20.9 11.80.8 6.21.1 11.80.8 6.51.4 11.41.4
body weight)
No. of patients 387 405 294 307 181 179
Plateau pressure (cm of water) 257 339 267 349 267 379
No. of patients 384 399 294 307 168 173
Peak inspiratory pressure (cm of water) 328 3910 339 4010 339 4410
No. of patients 382 401 295 308 178 177
Mean airway pressure (cm of water) 1713 1712 1714 1917 1714 2010
No. of patients 369 385 288 301 176 173
Respiratory rate (breaths/min) 297 166 307 177 307 207
No. of patients 389 406 296 308 185 181
Minute ventilation (liters/min) 12.93.6 12.64.5 13.43.5 13.44.8 13.73.8 14.95.3
No. of patients 387 401 296 307 182 177
FiO2 0.560.19 0.510.17 0.540.18 0.510.18 0.500.17 0.540.20
No. of patients 390 406 296 308 185 181
PEEP (cm of water) 9.43.6 8.63.6 9.23.6 8.64.2 8.13.4 9.14.2
No. of patients 390 406 296 308 185 181
PaO2:FiO2 15873 17676 16068 17781 16571 16488
No. of patients 350 369 284 297 148 160
PaO2 (mm Hg) 7623 7719 7422 7623 7317 7521
No. of patients 350 369 284 297 148 160
PaCO2 (mm Hg) 4010 358 4312 369 4412 4010
No. of patients 351 369 285 297 147 160
Arterial pH 7.380.08 7.410.07 7.380.08 7.410.07 7.400.07 7.410.08
No. of patients 351 369 285 297 148 160
*Plusminus values are means (SD) of the values recorded between 6 and 10 a.m. on days 1, 3, and 7 after enrollment. The numbers of
patients refers to those who were receiving ventilation and for whom data were available. FiO2 denotes fraction of inspired oxygen, PEEP
positive end-expiratory pressure, PaO2 partial pressure of arterial oxygen, and PaCO2 partial pressure of arterial carbon dioxide. All differences
between study groups were significant on each day (P<0.05) except for mean airway pressure on days 1, 3, and 7; the PaO2:FiO2 on day 7;
minute ventilation on days 1 and 3; pH on day 7; and PaO2 on days 1, 3, and 7.
incidence of barotrauma after randomization was sim- patients in the group treated with traditional tidal
ilar in the two groups. volumes. These included prone positioning in 14 and
There were no significant differences between 9 patients, respectively.
groups in the percentages of days on which neuro- The mean log-transformed plasma interleukin-6
muscular-blocking drugs were used among patients values decreased from 2.50.7 pg per milliliter on
who were discharged home and breathing without day 0 to 2.30.7 pg per milliliter on day 3 in the
assistance (614 percent in the group treated with group treated with traditional tidal volumes and from
lower tidal volumes and 615 percent in the group 2.50.7 pg per milliliter to 2.00.5 pg per milliliter
treated with traditional tidal volumes) or among those in the group treated with lower tidal volumes. The
who died (2032 percent and 1628 percent, respec- decrease was greater in the group treated with lower
tively), or in the percentages of days on which seda- tidal volumes (P<0.001), and the day 3 plasma in-
tives were used among patients who were discharged terleukin-6 concentrations were also lower in this
home and breathing without assistance (6526 per- group (P=0.002).
cent and 6524 percent, respectively) or those who
died (7324 percent and 7128 percent, respec- DISCUSSION
tively). Investigational treatments for acute lung in- In this large study of patients with acute lung in-
jury and the acute respiratory distress syndrome that jury and the acute respiratory distress syndrome, mor-
were not included in the factorial design of the ex- tality was reduced by 22 percent and the number of
perimental interventions were given to 15 patients ventilator-free days was greater in the group treated
in the group treated with lower tidal volumes and 12 with lower tidal volumes than in the group treated
Vol ume 342 Numb er 18 1305
The New England Journal of Medicine
Downloaded from nejm.org on April 7, 2017. For personal use only. No other uses without permission.
Copyright 2000 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
1.0
TABLE 4. MAIN OUTCOME VARIABLES.*
Proportion of Patients
0.9
0.8
0.7 GROUP GROUP
0.6 RECEIVING RECEIVING
LOWER TIDAL TRADITIONAL
0.5 VARIABLE VOLUMES TIDAL VOLUMES P VALUE
Lower tidal volumesI
0.4 mmnSurvivalI Death before discharge home 31.0 39.8 0.007
0.3 mmnDischargeI and breathing without
0.2 Traditional tidal volumesI assistance (%)
mmnSurvivalI
0.1 mmnDischarge Breathing without assistance 65.7 55.0 <0.001
0.0 by day 28 (%)
0 20 40 60 80 100 120 140 160 180 No. of ventilator-free days, 1211 1011 0.007
days 1 to 28
Days after Randomization Barotrauma, days 1 to 28 (%) 10 11 0.43
Figure 1. Probability of Survival and of Being Discharged Home No. of days without failure 1511 1211 0.006
and Breathing without Assistance during the First 180 Days af- of nonpulmonary organs
or systems, days 1 to 28
ter Randomization in Patients with Acute Lung Injury and the
Acute Respiratory Distress Syndrome.
*Plusminus values are means SD. The number of ventilator-free days
The status at 180 days or at the end of the study was known for is the mean number of days from day 1 to day 28 on which the patient had
all but nine patients. Data on these 9 patients and on 22 addi- been breathing without assistance for at least 48 consecutive hours. Baro-
tional patients who were hospitalized at the time of the fourth trauma was defined as any new pneumothorax, pneumomediastinum, or
interim analysis were censored. subcutaneous emphysema, or a pneumatocele that was more than 2 cm in
diameter. Organ and system failures were defined as described in the Meth-
ods section.
0.6
on days 1 and 3. These results, coupled with the great-
Lower tidal volumesI
Traditional tidal volumes
er reductions in plasma interleukin-6 concentrations,
0.5 suggest that the group treated with lower tidal vol-
umes had less lung inflammation.35 The greater re-
0.4 ductions in plasma interleukin-6 concentrations may
Mortality
also reflect a reduced systemic inflammatory response
0.3 to lung injury, which could contribute to the higher
0.2
number of days without organ or system failure and
the lower mortality in the group treated with lower
0.1 tidal volumes.15
Several factors could explain the difference in re-
0.0 sults between our trial and other trials of ventilation
0.150.40 0.410.50 0.510.62 0.631.5
using lower tidal volumes in patients with acute lung
Quartile of Static ComplianceI injury and the acute respiratory distress syndrome.22-24
(ml/cm of water/kg of predicted body weight) First, our study had a greater difference in tidal vol-
Figure 2. Mean (+SE) Mortality Rate among 257 Patients with umes between groups. In one earlier trial, the tradi-
Acute Lung Injury and the Acute Respiratory Distress Syndrome tional tidal volume was equivalent to approximately
Who Were Assigned to Receive Traditional Tidal Volumes and 12.2 ml per kilogram of predicted body weight and
260 Such Patients Who Were Assigned to Receive Lower Tidal the lower tidal volume was equivalent to approximate-
Volumes, According to the Quartile of Static Compliance of the
Respiratory System before Randomization. ly 8.1 ml per kilogram of predicted body weight.23
The interaction between the study group and the quartile of In a second study, the traditional and lower tidal vol-
static compliance at base line was not significant (P=0.49). umes were approximately 10.3 and 7.1 ml per kilo-
gram of dry body weight (calculated as the measured
weight minus the estimated weight gain from fluid
retention), respectively.22 In the present trial, meas-
ured weight exceeded predicted body weight by ap-
with traditional tidal volumes. These results are con- proximately 20 percent. Assuming a similar difference,
sistent with the results of experiments in animals9-14 and assuming that half the difference was dry weight
and observational studies in humans.16,17 in excess of predicted body weight, tidal volumes in
These benefits occurred despite the higher require- the second trial would have been approximately 11.3
ments for positive end-expiratory pressure and frac- and 7.8 ml per kilogram of predicted body weight.
tion of inspired oxygen and the lower ratio of partial Therefore, the traditional tidal volume of 11.8 ml
pressure of arterial oxygen to fraction of inspired ox- per kilogram of predicted body weight in our study
ygen in the group treated with lower tidal volumes was similar to the values in the previous two trials.
1306 May 4 , 2 0 0 0
The New England Journal of Medicine
Downloaded from nejm.org on April 7, 2017. For personal use only. No other uses without permission.
Copyright 2000 Massachusetts Medical Society. All rights reserved.
V E N T I L AT I O N W I T H L OW E R T I DA L VOLU M E S I N PAT I E N T S W I T H T H E AC U T E R E S P I R ATORY D I ST R E S S SY N D R O M E
However, the tidal volume of 6.2 ml per kilogram of utes to compliance of the respiratory system and is
predicted body weight in the group receiving lower reduced in many patients with acute lung injury and
tidal volumes was lower than the values in the pre- the acute respiratory distress syndrome,39 may have
vious two trials. obscured a true interaction between tidal volume and
If one assumes that measured weights also exceed- base-line lung compliance.
ed predicted body weights by 20 percent in the ear- Barotrauma occurred with similar frequency in
lier trials, the tidal volumes in the traditional groups the two study groups, a finding consistent with the
were approximately 10.2 and 9.4 ml per kilogram of results of other studies in which the incidence of baro-
measured weight, respectively, as compared with 9.9 trauma was independent of airway pressures.22-24,40,41
ml per kilogram of measured weight in our study. The most common manifestation of barotrauma was
Therefore, the tidal volumes in the traditional groups pneumothorax, which could have been the result of
in each of the three trials were consistent with tradi- invasive procedures. Pneumothorax is not a sensitive
tional recommendations.6,36 or specific marker of stretch-induced injury with the
A second possible explanation for the different re- tidal volumes used in this study.
sults is that the previous trials were designed to detect The similarity in the number of days of ventilator
larger differences in mortality between groups.22-24 use among the survivors in both groups suggests that
Hence, they lacked the statistical power to demon- the higher number of ventilator-free days in the group
strate the moderate effects of lower tidal volumes that treated with lower tidal volumes resulted from re-
we found. duced mortality rather than from a reduced number
A third difference in the trials was in the treat- of days of ventilation among the survivors. However,
ment of acidosis. Increases in the ventilator rate were the comparison of the number of days of ventilator
required and bicarbonate infusions were allowed to use among the survivors could be misleading.42 Some
correct mild-to-moderate acidosis in our study, which patients who would have survived in the group treat-
resulted in smaller differences in the partial pressure ed with traditional tidal volumes might have needed
of arterial carbon dioxide and pH between the study the ventilator on fewer days had they been in the
groups than in the previous trials.22-24 The deleteri- group treated with lower tidal volumes. This bene-
ous effects of acidosis in the previous studies may ficial effect would have been obscured if prolonged
have counteracted a protective effect of the lower ventilation was required before recovery among pa-
tidal volumes. tients who otherwise would have died in the group
In addition to being caused by excessive stretch, treated with traditional tidal volumes. For similar
lung injury may also result from repeated opening reasons, it is also difficult to compare the number of
and closing of small airways or from excessive stress days with organ or system failure among the survi-
at margins between aerated and atelectatic regions of vors in the two study groups.
the lungs.37 These types of lung injury may be pre- We found that treatment with a ventilation ap-
vented by the use of a higher positive end-expiratory proach designed to protect the lungs from excessive
pressure.10,13,37,38 A slightly higher positive end-expir- stretch resulted in improvements in several impor-
atory pressure was necessary in the group treated with tant clinical outcomes in patients with acute lung in-
lower tidal volumes during the first few days to main- jury and the acute respiratory distress syndrome. On
tain arterial oxygenation at a level similar to that in the basis of these results, high priority should be
the group treated with traditional tidal volumes, but given to preventing excessive lung stretch during ad-
positive end-expiratory pressure was not increased as justments to mechanical ventilation, and this lower-
a means of protecting the lungs. tidal-volume protocol should be used in patients with
In a recent trial in 53 patients with acute respira- acute lung injury and the acute respiratory distress
tory distress syndrome, 28-day mortality was signif- syndrome.
icantly lower with a ventilation strategy that used
a higher positive end-expiratory pressure combined Supported by contracts (NO1-HR 46054, 46055, 46056, 46057,
with limited peak inspiratory pressure than with a 46058, 46059, 46060, 46061, 46062, 46063, and 46064) with the Na-
tional Heart, Lung, and Blood Institute.
strategy of traditional ventilation.21 These results sug- Presented in part at the International Conference of the American Lung
gest that both increased positive end-expiratory pres- Association and the American Thoracic Society, San Diego, Calif., April
sure and reduced inspiratory stretch could have ben- 26, 1999.
eficial effects.
We are indebted to the intensive care unit nurses, respiratory ther-
Stretch-induced lung injury may not occur if lung apists, and physicians, as well as our patients and their families, who
compliance is not greatly reduced. However, the ben- supported this trial.
efit of ventilation with a lower tidal volume was in-
dependent of the static compliance of the respiratory APPENDIX
system at base line, suggesting that the lower tidal vol- In addition to the members of the Writing Committee, the members of
the National Heart, Lung, and Blood Institute ARDS Network were as fol-
ume was advantageous regardless of lung compliance. lows: Network Participants: Cleveland Clinic Foundation H.P. Wiede-
Variations in chest-wall compliance, which contrib- mann, A.C. Arroliga, C.J. Fisher, Jr., J.J. Komara, Jr., P. Perez-Trepichio;
Vol ume 342 Numb e r 18 1307
The New England Journal of Medicine
Downloaded from nejm.org on April 7, 2017. For personal use only. No other uses without permission.
Copyright 2000 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
Denver Health Medical Center P.E. Parsons, R. Wolkin; Denver Veterans tilation with permissive hypercapnia: a prospective study. Crit Care Med
Affairs Medical Center C. Welsh; Duke University Medical Center W.J. 1994;22:1568-78.
Fulkerson, Jr., N. MacIntyre, L. Mallatratt, M. Sebastian, R. McConnell, 17. Hickling KG, Henderson SJ, Jackson R. Low mortality associated with
C. Wilcox, J. Govert; Johns Hopkins University D. Thompson; LDS Hos- low volume pressure limited ventilation with permissive hypercapnia in se-
pital T. Clemmer, R. Davis, J. Orme, Jr., L. Weaver, C. Grissom, M. vere adult respiratory distress syndrome. Intensive Care Med 1990;16:372-
Eskelson; McKayDee Hospital M. Young, V. Gooder, K. McBride, C. 7.
Lawton, J. dHulst; MetroHealth Medical Center of Cleveland J.R. Peer- 18. Slutsky AS. Mechanical ventilation: American College of Chest Physi-
less, C. Smith, J. Brownlee; Rose Medical Center W. Pluss; San Francisco cians Consensus Conference. Chest 1993;104:1833-59. [Erratum, Chest
General Hospital Medical Center R. Kallet, J.M. Luce; Jefferson Medical 1994;106:656.]
College J. Gottlieb, M. Elmer, A. Girod, P. Park; University of California, 19. Blanch L, Fernandez R, Valles J, Sole J, Roussos C, Artigas A. Effect
San Francisco B. Daniel, M. Gropper; University of Colorado Health Sci- of two tidal volumes on oxygenation and respiratory system mechanics dur-
ences Center E. Abraham, F. Piedalue, J. Glodowski, J. Lockrem, R. ing the early stage of adult respiratory distress syndrome. J Crit Care 1994;
McIntyre, K. Reid, C. Stevens, D. Kalous; University of Maryland H.J. 9:151-8.
Silverman, C. Shanholtz, W. Corral; University of Michigan G.B. Toews, 20. Hedley-Whyte J, Pontoppidan H, Morris MJ. The response of patients
D. Arnoldi, R.H. Bartlett, R. Dechert, C. Watts; University of Pennsylvania with respiratory failure and cardiopulmonary disease to different levels of
P.N. Lanken, H. Anderson III, B. Finkel, C.W. Hanson; University of constant volume ventilation. J Clin Invest 1966;45:1543-54.
Utah Hospital R. Barton, M. Mone; University of WashingtonHarbor- 21. Amato MBP, Barbas CSV, Medeiros DM, et al. Effect of a protective-
view Medical Center L.D. Hudson, C. Lee, G. Carter, R.V. Maier, K.P. ventilation strategy on mortality in the acute respiratory distress syndrome.
Steinberg; Vanderbilt University G. Bernard, M. Stroud, B. Swindell, L. N Engl J Med 1998;338:347-54.
Stone, L. Collins, S. Mogan; Clinical Coordinating Center: Massachusetts 22. Brochard L, Roudot-Thoraval F, Roupie E, et al. Tidal volume reduc-
General Hospital and Harvard Medical School M. Ancukiewicz, D. Hay- tion for prevention of ventilator-induced lung injury in acute respiratory
den, F. Molay, N. Ringwood, G. Wenzlow, A.S. Kazeroonian; National distress syndrome. Am J Respir Crit Care Med 1998;158:1831-8.
Heart, Lung, and Blood Institute Staff: D.B. Gail, C.H. Bosken, P. 23. Stewart TE, Meade MO, Cook DJ, et al. Evaluation of a ventilation
Randall, M. Waclawiw; Data and Safety Monitoring Board: R.G. strategy to prevent barotrauma in patients at high risk for acute respiratory
Spragg, J. Boyett, J. Kelley, K. Leeper, M. Gray Secundy, A. Slutsky; Pro- distress syndrome. N Engl J Med 1998;338:355-61.
tocol Review Committee: T.M. Hyers, S.S. Emerson, J.G.N. Garcia, J.J. 24. Brower RG, Shanholtz CB, Fessler HE, et al. Prospective, random-
Marini, S.K. Pingleton, M.D. Shasby, W.J. Sibbald. ized, controlled clinical trial comparing traditional versus reduced tidal vol-
ume ventilation in acute respiratory distress syndrome patients. Crit Care
REFERENCES Med 1999;27:1492-8.
25. Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R.
1. Bernard GR, Artigas A, Brigham KL, et al. The American-European Transection of the oesophagus for bleeding oesophageal varices. Br J Surg
Consensus Conference on ARDS: definitions, mechanism, relevant out- 1973;60:646-9.
comes, and clinical trial coordination. Am J Respir Crit Care Med 1994; 26. Crapo RO, Morris AH, Gardner RM. Reference spirometric values us-
149:818-24. ing techniques and equipment that meet ATS recommendations. Am Rev
2. Sloane PJ, Gee MH, Gottlieb JE, et al. A multicenter registry of pa- Respir Dis 1981;123:659-64.
tients with acute respiratory distress syndrome: physiology and outcome. 27. Crapo RO, Morris AH, Clayton PD, Nixon CR. Lung volumes in
Am Rev Respir Dis 1992;146:419-26. healthy nonsmoking adults. Bull Eur Physiopathol Respir 1982;18:419-25.
3. Doyle RL, Szaflarski N, Modin GW, Wiener-Kronish JP, Matthay MA. 28. Knoben JE, Anderson PO, eds. Handbook of clinical drug data. 7th
Identification of patients with acute lung injury: predictors of mortality. ed. Hamilton, Ill.: Drug Intelligence, 1993.
Am J Respir Crit Care Med 1995;152:1818-24. 29. Bernard GR, Wheeler AP, Arons MM, et al. A trial of antioxidants
4. Zilberberg MD, Epstein SK. Acute lung injury in the medical ICU: co- N-acetylcysteine and procysteine in ARDS. Chest 1997;112:164-72.
morbid conditions, age, etiology, and hospital outcome. Am J Respir Crit 30. Arons MM, Wheeler AP, Bernard GR, et al. Effects of ibuprofen on
Care Med 1998;157:1159-64. the physiology and survival of hypothermic sepsis. Crit Care Med 1999;27:
5. Pittet JF, Mackersie RC, Martin TR, Matthay MA. Biological markers 699-707.
of acute lung injury: prognostic and pathogenic significance. Am J Respir 31. OBrien PC, Fleming TR. A multiple testing procedure for clinical tri-
Crit Care Med 1997;155:1187-205. als. Biometrics 1979;35:549-56.
6. Marini JJ. Evolving concepts in the ventilatory management of acute 32. DeMets DL, Ware JH. Group sequential methods for clinical trials
respiratory distress syndrome. Clin Chest Med 1996;17:555-75. with a one-sided hypothesis. Biometrika 1980;67:651-60.
7. Gattinoni L, Presenti A, Torresin A, et al. Adult respiratory distress 33. Kalbfleisch JD, Prentice RL. The statistical analysis of failure time
syndrome profiles by computed tomography. J Thorac Imaging 1986; data. New York: Wiley, 1980.
1:25-30. 34. Knaus WA, Wagner DP, Draper EA, et al. The APACHE III prognos-
8. Maunder RJ, Shuman WP, McHugh JW, Marglin SI, Butler J. Preser- tic system: risk prediction of hospital mortality for critically ill hospitalized
vation of normal lung regions in the adult respiratory distress syndrome: adults. Chest 1991;100:1619-36.
analysis by computed tomography. JAMA 1986;255:2463-5. 35. Ranieri VM, Suter PM, Tortorella C, et al. Effect of mechanical ven-
9. Tsuno K, Miura K, Takeya M, Kolobow T, Morioka T. Histopathologic tilation on inflammatory mediators in patients with acute respiratory dis-
pulmonary changes from mechanical ventilation at high peak airway pres- tress syndrome: a randomized controlled trial. JAMA 1999;282:54-61.
sures. Am Rev Respir Dis 1991;143:1115-20. 36. Carmichael LC, Dorinsky PM, Higgins SB, et al. Diagnosis and ther-
10. Tremblay L, Valenza F, Ribeiro SP, Li J, Slutsky AS. Injurious ventila- apy of acute respiratory distress syndrome in adults: an international survey.
tory strategies increase cytokines and c-fos m-RNA expression in an isolat- J Crit Care 1996;11:9-18.
ed rat lung model. J Clin Invest 1997;99:944-52. 37. Muscedere JG, Mullen JB, Gan K, Slutsky AS. Tidal ventilation at low
11. Parker JC, Hernandez LA, Peevy KJ. Mechanisms of ventilator-induced airway pressures can augment lung injury. Am J Respir Crit Care Med
lung injury. Crit Care Med 1993;21:131-43. 1994;149:1327-34.
12. Dreyfuss D, Basset G, Soler P, Saumon G. Intermittent positive-pres- 38. Corbridge TC, Wood LD, Crawford GP, Chudoba MJ, Yanos J, Sznaj-
sure hyperventilation with high inflation pressures produces pulmonary mi- der JI. Adverse effects of large tidal volume and low PEEP in canine acid
crovascular injury in rats. Am Rev Respir Dis 1985;132:880-4. aspiration. Am Rev Respir Dis 1990;142:311-5.
13. Webb HH, Tierney DF. Experimental pulmonary edema due to inter- 39. Mergoni M, Martelli A, Volpi A, Primavera S, Zuccoli P, Rossi A. Im-
mittent positive pressure ventilation with high inflation pressures: protec- pact of positive end-expiratory pressure on chest wall and lung pressure-
tion by positive end-expiratory pressure. Am Rev Respir Dis 1974;110: volume curve in acute respiratory failure. Am J Respir Crit Care Med 1997;
556-65. 156:846-54.
14. Kolobow T, Moretti MP, Fumagalli R, et al. Severe impairment in lung 40. Schnapp LM, Chin DP, Szaflarski N, Matthay MA. Frequency and im-
function induced by high peak airway pressure during mechanical ventila- portance of barotrauma in 100 patients with acute lung injury. Crit Care
tion: an experimental study. Am Rev Respir Dis 1987;135:312-5. Med 1995;23:272-8.
15. Slutsky AS, Tremblay LN. Multiple system organ failure: is mechanical 41. Weg JG, Anzueto A, Balk RA, et al. The relation of pneumothorax
ventilation a contributing factor? Am J Respir Crit Care Med 1998;157: and other air leaks to mortality in the acute respiratory distress syndrome.
1721-5. N Engl J Med 1998;338:341-6.
16. Hickling KG, Walsh J, Henderson S, Jackson R. Low mortality rate in 42. Heitjan DF. Causal inference in a clinical trial: a comparative example.
adult respiratory distress syndrome using low-volume, pressure-limited ven- Control Clin Trials 1999;20:309-18.
1308 May 4 , 2 0 0 0
The New England Journal of Medicine
Downloaded from nejm.org on April 7, 2017. For personal use only. No other uses without permission.
Copyright 2000 Massachusetts Medical Society. All rights reserved.
You might also like
- Low-Tidal-Volume Ventilation in The Acute Respiratory Distress SyndromeDocument8 pagesLow-Tidal-Volume Ventilation in The Acute Respiratory Distress SyndromeJimmy Christianto SuryoNo ratings yet
- Gattinoni2006 Reclutamiento Pulmonar en Pacientes Con SdraDocument12 pagesGattinoni2006 Reclutamiento Pulmonar en Pacientes Con SdraRenatoNo ratings yet
- ARDS Berlin Definition UpdateDocument43 pagesARDS Berlin Definition UpdateAgnes Pritama Fahmi100% (1)
- Ventilation During Lung Resection and Critical Care ComparativeDocument11 pagesVentilation During Lung Resection and Critical Care Comparativeema moralesNo ratings yet
- Ventilatorymanagement Ofthenoninjuredlung: David L. Bowton,, Louis Keith ScottDocument10 pagesVentilatorymanagement Ofthenoninjuredlung: David L. Bowton,, Louis Keith ScottGhost11mNo ratings yet
- Low-Tidal-Volume Ventilation in The Acute Respiratory DistressDocument12 pagesLow-Tidal-Volume Ventilation in The Acute Respiratory DistressJesus FrancoNo ratings yet
- 2006 Comparison of Two Fluid-Management Strategies in Acute Lung InjuryDocument12 pages2006 Comparison of Two Fluid-Management Strategies in Acute Lung InjuryyaritzaalviarezNo ratings yet
- 40Document9 pages40Eduardo SoaresNo ratings yet
- CcventilacioninicialbuenoDocument3 pagesCcventilacioninicialbuenoARELHI ROSARIO GARCIA MONROYNo ratings yet
- Ajustesiniciales VNIDocument3 pagesAjustesiniciales VNIDamian Torres SperanzaNo ratings yet
- Newer Modes of Ventilation2Document9 pagesNewer Modes of Ventilation2Saradha PellatiNo ratings yet
- Invasive Mechanical Ventilation PDFDocument4 pagesInvasive Mechanical Ventilation PDFRaquel AguilarNo ratings yet
- RCT of Aprv Vs LPV in Ards PtsDocument11 pagesRCT of Aprv Vs LPV in Ards PtsOldriana Prawiro HapsariNo ratings yet
- Azitromicyn COPDDocument10 pagesAzitromicyn COPDLucrécia BórgiaNo ratings yet
- JAMA 2008 OLV (May-20-2010)Document9 pagesJAMA 2008 OLV (May-20-2010)V ANo ratings yet
- Azithromycin For Prevention of Exacerbations of COPDDocument10 pagesAzithromycin For Prevention of Exacerbations of COPDAJNo ratings yet
- Effect of A Protective-Ventilation Strategy On Mortality in The Acute Respiratory Distress SyndromeDocument8 pagesEffect of A Protective-Ventilation Strategy On Mortality in The Acute Respiratory Distress Syndromeiturraspe12No ratings yet
- Original ContributionsDocument9 pagesOriginal ContributionsEduardo SoaresNo ratings yet
- Manajemen VentiDocument2 pagesManajemen VentiBos AseNo ratings yet
- Effect of Lowering VT On Mortality in Acute Respiratory DistressDocument8 pagesEffect of Lowering VT On Mortality in Acute Respiratory DistressFabio RepettoNo ratings yet
- Overventilation and Lung DamageDocument8 pagesOverventilation and Lung DamageDaniel MoralesNo ratings yet
- Advances in Mechanical Ventilation 4AH PDFDocument11 pagesAdvances in Mechanical Ventilation 4AH PDFsérgio_nakano_2No ratings yet
- High-Frequency Oscillation For Acute Respiratory Distress SyndromeDocument8 pagesHigh-Frequency Oscillation For Acute Respiratory Distress SyndromeLintang SuroyaNo ratings yet
- Wiedeman Comparison of Two Fluid-Management Strategies in Acute Lung Injury NEJM 2006Document12 pagesWiedeman Comparison of Two Fluid-Management Strategies in Acute Lung Injury NEJM 2006Della Puspita SariNo ratings yet
- Evidence-Based Management of Acute Lung Injury and Acute Respiratory Distress SyndromeDocument17 pagesEvidence-Based Management of Acute Lung Injury and Acute Respiratory Distress SyndromeretNo ratings yet
- Lung Insufflation Capacity in Neuromuscular Disease: Original Research ArticleDocument6 pagesLung Insufflation Capacity in Neuromuscular Disease: Original Research ArticleEzeBorjesNo ratings yet
- Acute Respiratory Distress SyndromeDocument6 pagesAcute Respiratory Distress SyndromeNove Mae EscabarteNo ratings yet
- CF Ventilation ManagementDocument10 pagesCF Ventilation ManagementSherry SaidNo ratings yet
- Inflamt VMDocument6 pagesInflamt VMDiana Reaño RuizNo ratings yet
- Treatment of ARDS: Ventilation, Fluids, NutritionDocument15 pagesTreatment of ARDS: Ventilation, Fluids, Nutritionf3wlNo ratings yet
- Ventilation in Acute Lung Injury and ARDS Clinicians' Approaches To MechanicalDocument8 pagesVentilation in Acute Lung Injury and ARDS Clinicians' Approaches To MechanicalEduardo SoaresNo ratings yet
- Pharmacologictreatments Foracuterespiratory DistresssyndromeDocument17 pagesPharmacologictreatments Foracuterespiratory DistresssyndromeLuis HernándezNo ratings yet
- ARTventilacion Mecanica en EMDocument3 pagesARTventilacion Mecanica en EMNicole Ivette Arias RizikNo ratings yet
- BMJ Open 2015 ZhangDocument10 pagesBMJ Open 2015 ZhangLuis CordovaNo ratings yet
- The Open Anesthesia JournalDocument11 pagesThe Open Anesthesia JournalmikoNo ratings yet
- Roberts 2019 Year in Review Adult Invasive MechDocument6 pagesRoberts 2019 Year in Review Adult Invasive MechJose Luis Escobar zabaleguiNo ratings yet
- Ventilación Del Pulmón Sano CC Current 20Document5 pagesVentilación Del Pulmón Sano CC Current 20Silvia Lorena Mireles GonzálezNo ratings yet
- Intraoperative Protective Mechanical Ventilation For Prevention of Postoperative Pulmonary ComplicationsDocument22 pagesIntraoperative Protective Mechanical Ventilation For Prevention of Postoperative Pulmonary ComplicationsPatricia Aguirre ChevezNo ratings yet
- Acute Respiratory Distress Syndrome GuideDocument6 pagesAcute Respiratory Distress Syndrome GuideVijeyachandhar DorairajNo ratings yet
- Ajrccm 158 6 9801044Document8 pagesAjrccm 158 6 9801044Guillermo MartínezNo ratings yet
- Bedside Selection of Positive End-Expiratory Pressure in Mild, Moderate, and Severe Acute Respiratory Distress SyndromeDocument13 pagesBedside Selection of Positive End-Expiratory Pressure in Mild, Moderate, and Severe Acute Respiratory Distress SyndromeSüleyman YıldırımNo ratings yet
- Slut Sky 2013Document11 pagesSlut Sky 2013GuadalupeNo ratings yet
- Angiotensin IIDocument12 pagesAngiotensin IIFelicia HoseaNo ratings yet
- Protective Ventilation of Patients With Acute Respiratory Distress Syndrome Review ArticleDocument10 pagesProtective Ventilation of Patients With Acute Respiratory Distress Syndrome Review ArticleshackeristNo ratings yet
- Mechanical Ventilation - Lessons From The ARDSNet TrialDocument5 pagesMechanical Ventilation - Lessons From The ARDSNet TrialRDG20202No ratings yet
- Effects of Thoraco-Pelvic Supports During Prone PositionDocument9 pagesEffects of Thoraco-Pelvic Supports During Prone PositionAdam KurniaNo ratings yet
- Esteban 2004Document9 pagesEsteban 2004Fermin LombardiaNo ratings yet
- The Effect of The Duration of Pre-Oxygenation Before Endotracheal Suction On Hemodynamic SymptomsDocument7 pagesThe Effect of The Duration of Pre-Oxygenation Before Endotracheal Suction On Hemodynamic SymptomsnurharyantidarmaningtyasNo ratings yet
- 8. Negative-_versus_positive-pressure_ventilation_in_Document11 pages8. Negative-_versus_positive-pressure_ventilation_in_Dwi Putri SekariniNo ratings yet
- 2022-10# (PEERJ) RR in ECMODocument17 pages2022-10# (PEERJ) RR in ECMOjycntuNo ratings yet
- Hfo 2Document9 pagesHfo 2markus_danusantosoNo ratings yet
- Acute Respiratory Distress SyndromeDocument77 pagesAcute Respiratory Distress SyndromeAnnisa Dyah ChairiniNo ratings yet
- Respiratory - ARDS Vent Revised - QuestionsDocument6 pagesRespiratory - ARDS Vent Revised - QuestionsRyan ReNo ratings yet
- Coastal Life Publication (Project)Document9 pagesCoastal Life Publication (Project)mohamedsalahudeen193No ratings yet
- Ecmo Clase 2 - 4Document11 pagesEcmo Clase 2 - 4Johanna GiraldoNo ratings yet
- Arti Revi 11Document8 pagesArti Revi 11LuLu NikhlaturNo ratings yet
- AnastesiDocument22 pagesAnastesidhitadwynNo ratings yet
- Chatham 2004Document5 pagesChatham 2004raul huertaNo ratings yet
- Use of Early Extra-Corporeal Membrane Oxygenation (ECMO) For Severe Refractory Status AsthmaticusDocument3 pagesUse of Early Extra-Corporeal Membrane Oxygenation (ECMO) For Severe Refractory Status Asthmaticusintanlidyawati26gmaiNo ratings yet
- Field STD - Hospal Visit Assignment PDFDocument1 pageField STD - Hospal Visit Assignment PDFapi-354040213No ratings yet
- Field Studies 2 - Ass 2 PDFDocument1 pageField Studies 2 - Ass 2 PDFapi-354040213No ratings yet
- NEJMoa 1000678Document10 pagesNEJMoa 1000678FernandoFelixHernandezNo ratings yet
- Field Studies Assignment 1Document1 pageField Studies Assignment 1api-354040213No ratings yet
- Field STD WordDocument4 pagesField STD Wordapi-354040213No ratings yet
- Ass 4Document2 pagesAss 4api-354040213No ratings yet
- CJRT 51 69Document3 pagesCJRT 51 69api-354040213No ratings yet
- Deepa Govind - Worker Health and Safety Awareness in 4 Steps Certificate 1Document1 pageDeepa Govind - Worker Health and Safety Awareness in 4 Steps Certificate 1api-354040213No ratings yet
- Assignment 1 - Article Summary WordDocument3 pagesAssignment 1 - Article Summary Wordapi-354040213No ratings yet
- Health 1Document3 pagesHealth 1api-354040213No ratings yet
- CJRT 51 69Document3 pagesCJRT 51 69api-354040213No ratings yet
- Performance-Based Reward System Performance and Development Plan and Review DocumentDocument8 pagesPerformance-Based Reward System Performance and Development Plan and Review DocumentMusyimi TitusNo ratings yet
- CS Form No. 212 Revised Personal Data SheetDocument5 pagesCS Form No. 212 Revised Personal Data SheetKim Rose Sabuclalao85% (13)
- Riggenbach - CBT ToolboxDocument366 pagesRiggenbach - CBT ToolboxRam V100% (5)
- Concept Paper SampleDocument8 pagesConcept Paper Samplejv syNo ratings yet
- Acrylic Partial DenturesDocument6 pagesAcrylic Partial Denturesruth graceNo ratings yet
- 38-Year-Old P4 With Heavy Menstrual BleedingDocument36 pages38-Year-Old P4 With Heavy Menstrual BleedingCodillia CheongNo ratings yet
- Gestational Diabetes MellitusDocument7 pagesGestational Diabetes MellitusYujen0% (1)
- Drug Tariff Workshop 13-14 - StudentDocument10 pagesDrug Tariff Workshop 13-14 - StudentCrystal Sia Yiik SwanNo ratings yet
- Compounding and DispensingDocument9 pagesCompounding and DispensingElida Rizki MhNo ratings yet
- Psychological Disorders GuideDocument4 pagesPsychological Disorders GuideCarlyn HarfordNo ratings yet
- Leadership Program BrochureDocument2 pagesLeadership Program BrochureGeorge VascanNo ratings yet
- Syl 1415 Psychodynamic PsychotherapyDocument3 pagesSyl 1415 Psychodynamic PsychotherapyMaBinNo ratings yet
- Retinoblastoma - EyeWikiDocument11 pagesRetinoblastoma - EyeWikimay171989No ratings yet
- Overview On Peripheral Artery Disease - FinalDocument78 pagesOverview On Peripheral Artery Disease - FinalMITHANo ratings yet
- Impetigo and CHMDocument2 pagesImpetigo and CHMcbrammah9357No ratings yet
- EMCC Block One Nursing - Exam 1 Study GuideDocument2 pagesEMCC Block One Nursing - Exam 1 Study GuidedavidvpnNo ratings yet
- Renal ExamDocument12 pagesRenal ExamCamille Espinosa100% (6)
- 1-2-5 - Assignment - UPLOADDocument6 pages1-2-5 - Assignment - UPLOADmdzvi86% (14)
- Nursing Care PlanDocument6 pagesNursing Care PlanNeza AgdalesNo ratings yet
- NeurotransmittersDocument5 pagesNeurotransmittersJoezerk Jhon Biel100% (1)
- Lecture 5 Health Care OrganizationsDocument24 pagesLecture 5 Health Care OrganizationsSajida Bibi NoonariNo ratings yet
- GR Corplus Manual PDFDocument346 pagesGR Corplus Manual PDFAni Maulidia0% (1)
- Helping Amy: A Social Worker's Treatment PlanDocument6 pagesHelping Amy: A Social Worker's Treatment PlanAngy ShoogzNo ratings yet
- Epilepsy Emergencies - Status Epilepticus, Acute Repetitite Seizures, and Autoimmune EncephalitisDocument23 pagesEpilepsy Emergencies - Status Epilepticus, Acute Repetitite Seizures, and Autoimmune Encephalitisnight.shadowNo ratings yet
- Obsessive-Compulsive Disorder in Children and Adolescents: Georgina Krebs, Isobel HeymanDocument5 pagesObsessive-Compulsive Disorder in Children and Adolescents: Georgina Krebs, Isobel HeymanRidwan AdiansyahNo ratings yet
- Prep SheetDocument3 pagesPrep Sheetdlh1129No ratings yet
- Fundamental Facts About Mental Health 2016Document112 pagesFundamental Facts About Mental Health 2016Jac1999No ratings yet
- A Fear of PainDocument2 pagesA Fear of PainBabac Compass PashazadehNo ratings yet
- ADR Reporting, Medication Error Reporting SystemDocument100 pagesADR Reporting, Medication Error Reporting Systemfarmasi_hm100% (1)
- Learn Facial AcupunctureDocument216 pagesLearn Facial Acupuncturebintanglima95% (19)