Professional Documents
Culture Documents
Jurnal 3
Uploaded by
giviOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jurnal 3
Uploaded by
giviCopyright:
Available Formats
Oncology 2013;84(suppl 1):4450 Published online: February 20, 2013
DOI: 10.1159/000345889
Ultrasonography Fusion Imaging System
Increases the Chance of Radiofrequency
Ablation for Hepatocellular Carcinoma with Poor
Conspicuity on Conventional Ultrasonography
Yuki Makino a Yasuharu Imai a Hideko Ohama a Takumi Igura a Sachiyo Kogita a
Yoshiyuki Sawai a Kazuto Fukuda a Manabu Takamura b Hiroshi Ohashi c
Takamichi Murakami d
Departments of a Gastroenterology, b Radiology and c Pathology, Ikeda Municipal Hospital, Ikeda, and
d
Department of Radiology, Kinki University School of Medicine, Osakasayama, Japan
Key Words tem in conjunction with reference images displayed side-by-
Ultrasonography fusion imaging Multimodality fusion side with grayscale US. Conclusion: Since the introduction
imaging Volume Navigation System Hepatocellular of the US fusion imaging system, it has become possible to
carcinoma Radiofrequency ablation perform RFA for HCCs with poor conspicuity on grayscale US.
Copyright 2013 S. Karger AG, Basel
Abstract
Objectives: To investigate the usefulness of the ultrasonog- Introduction
raphy (US) fusion imaging system for radiofrequency abla-
tion (RFA) for hepatocellular carcinoma (HCC). Methods: Hepatocellular carcinoma (HCC), usually developing
Since the US fusion imaging system became available in from chronic liver diseases such as hepatitis B- and C-
2010, we have conducted RFA with this system in all cases. related cirrhosis, is one of the most common cancer types
The characteristics of 75 patients with 120 HCCs and 89 pa- worldwide [1, 2]. The treatments for HCC are usually de-
tients with 123 HCCs who underwent RFA before the intro- termined on the basis of staging and hepatic functional
duction of this system (period A) and after it (period B), re- reserve. Loco-regional treatments such as radiofrequency
spectively, were retrospectively compared. Results: Signifi- ablation (RFA) and percutaneous ethanol injection ther-
cant difference in the characteristics of the patients and apy are indicated, in principal, for HCCs up to 3 nodules
HCCs between the two periods was found only in the pro- and 3 cm in diameter [35]. Although percutaneous eth-
portion of HCCs with poor conspicuity on grayscale US treat- anol injection therapy is preferred in certain situations
ed with RFA (1.7%, 2/120 for period A vs. 15.4%, 19/123 for where it is difficult to perform RFA, such as for tumors
period B, p ! 0.01). Among the 19 HCCs with poor conspicu- surrounded by large vessels [6], RFA is now established as
ity on grayscale US for period B, 5 and 9 HCCs were identified the first-choice loco-regional treatment, since RFA is
on grayscale US and contrast-enhanced US, respectively, by considered superior to percutaneous ethanol injection
the use of the US fusion imaging system, whereas the 5 re- therapy in terms of the local tumor progression and over-
maining undetectable HCCs were treated by using the sys- all survival rates [7].
2013 S. Karger AG, Basel Yasuharu Imai, MD, PhD
00302414/13/08470044$38.00/0 Department of Gastroenterology,
Fax +41 61 306 12 34 Ikeda Municipal Hospital
E-Mail karger@karger.com Accessible online at: 3-1-18, Johnan, Ikeda, Osaka 563-8510 (Japan)
www.karger.com www.karger.com/ocl E-Mail yasuimai@hosp.ikeda.osaka.jp
Since second-generation contrast medium for ultraso- der the US guidance of Aplio XG (Toshiba, Tokyo, Japan) from
nography (US) including Sonazoid (Daiichi-sankyo, To- September 2009 to April 2010 (period A) and LOGIQ E9 (GE
Healthcare Japan, Tokyo, Japan) equipped with the US fusion im-
kyo, Japan) and gadolinium ethoxybenzyl diethylenetri- aging system (Volume Navigation System, GE Healthcare Japan)
amine pentaacetic acid (Gd-EOB-DTPA; Primovist, Bay- from May 2010 to January 2011 (period B). At needle core biopsy,
er Healthcare, Osaka, Japan), a liver-specific magnetic at least 2 samples were taken from each tumor using a 21-gauge
resonance (MR) contrast agent, became available, imag- needle (Majima needle, Top, Tokyo, Japan) to ensure accurate path-
ing diagnosis of HCC has dramatically advanced [814]. ological diagnosis as described previously [19]. We used a 17-gauge
cool-tip single electrode with a 2- or 3-cm exposed tip (Cool-tip RF
As a result, the diagnosis of HCC has come to be made at Ablation System, Covidien, Colo., USA). We used artificial ascites
an earlier stage. If HCCs are diagnosed at an early stage, or pleural effusion for tumors located on the liver surface, in the
RFA is often one of the treatment options. However, since hepatic dome or adjacent to the gastrointestinal tract.
early HCCs are sometimes difficult to detect on conven- After applying a local anesthesia, an electrode was inserted
tional US, we are obliged to give up conducting RFA. into the tumor and ablation was initiated. Power output was first
set at 20 or 30 W, respectively, for the 2- or 3-cm active tip of the
The US fusion imaging system, which has recently electrode, and increased by 10 W/min until roll-off. Ablation was
been introduced for the assistance of loco-regional treat- maintained at the energy level just before the first roll-off, until
ment for HCC, can show real-time US images and any the fifth roll-off occurred, or until 12 min had elapsed since the
cross-sectional multiplanar reconstruction images of CT start of ablation. We also ablated the needle track during the with-
or MRI synchronously, side-by-side. The US fusion imag- drawal of the electrode in order to prevent hemorrhage and tumor
dissemination. With the aim of achieving the complete necrosis
ing system has been reported to be useful for the detec- of the tumor, additional ablation was conducted when necessary.
tion of HCC with poor conspicuity on conventional US
[1517]. Therefore, even if a targeted tumor is not con- Follow-Up after RFA
spicuous on conventional US, percutaneous loco-region- Dynamic CT was performed within 7 days after RFA and the
al treatment can be applied by using the US fusion imag- treatment effect was evaluated comparing pre-RFA CT or MRI
and post-RFA CT. If tumor stain was not recognized around the
ing system. coagulated area in the arterial phase and the coagulated area was
The purpose of this study was to retrospectively com- considered to circumferentially extend beyond the pre-RFA tu-
pare the characteristics of the patients and tumors which mor boundary in the portal and equilibrium phases, it was judged
underwent RFA, before and after the introduction of the to be completely ablated. If an obvious residual tumor was ob-
US fusion imaging system, in order to verify the improve- served, additional treatment sessions were carried out until com-
plete ablation was achieved. After complete ablation, a follow-up
ment in the practice of RFA for HCC yielded by this sys- US, dynamic CT or Gd-EOB-DTPA-enhanced MRI and blood
tem. tests including tumor markers were performed every 3 months.
US Fusion Imaging System
Materials and Methods From May 2010 to January 2011 (period B), we used Volume
Navigation System installed in LOGIQ E9 for the assistance of
Patients and HCCs RFA for all cases as described previously [20]. As reference im-
This retrospective study was approved by our institutional re- ages for Volume Navigation System, the imaging modality on
view board and informed consent for this study was waived. Con- which the tumor and landmarks for the positional registration
secutive patients with HCC who underwent RFA from September were most clearly depicted was chosen.
2009 to January 2011 were enrolled in this study. After the volume data of CT or MR images for reference was
The diagnosis of hypervascular HCC was established on the imported as digital imaging and communication in medicine for-
basis of the typical imaging features on dynamic CT, CT angiog- mat, the cross-section of US images approximately parallel to the
raphy or Gd-EOB-DTPA-enhanced MRI [10]. Tumor biopsy was reference was registered. Then, one characteristic corresponding
conducted for the nodules which were more than 10 mm in diam- landmark between US images and reference was marked, respec-
eter and showed hypointensity on the hepatobiliary phase of Gd- tively, and the position was aligned. In order to improve the reg-
EOB-DTPA-enhanced MRI without early enhancement, on at istration accuracy, particularly around the tumor, the positional
least two imaging modalities of contrast-enhanced US (CEUS), registration was repeatedly carried out as close to the tumor as
dynamic CT and Gd-EOB-DTPA-enhanced MRI [9, 18]. Patho- possible. After the positional registration, multiplanar recon-
logical diagnosis of HCC was made according to the histological struction images of CT or MRI were synchronously displayed
criteria of the International Consensus Group for Hepatocellular side-by-side with the real-time US images.
Carcinoma [18].
Image Acquisition
Needle Core Biopsy and RFA Procedures Dynamic CT and CT Angiography
Needle core biopsy and RFA were performed by one of 3 hepa- Dynamic CT and CT angiography were performed with either
tologists with more than 10 years of experience. All needle core the 8-channel multidetector row helical CT (MDCT; LightSpeed
biopsy and RFA procedures were undertaken percutaneously un- Ultra, GE healthcare Japan) from September 2009 to September
Usefulness of the US Fusion Imaging for Oncology 2013;84(suppl 1):4450 45
RFA
2010, or the 64-channel MDCT (Discovery CT 750HD, GE health- System in all cases. Detection of the HCCs by grayscale US and
care Japan) from October 2010 to January 2011, with a slice thick- CEUS was assessed by the consensus of two hepatologists with
ness of 0.675 or 1.25 mm. In the dynamic CT the bolus tracking more than 10 years of experience in abdominal ultrasonography.
method was used for scanning, using 2.0 ml/kg of nonionic con-
trast material with a concentration of 300 gI/ml administered in- Statistical Analysis
travenously for 30 s with an automatic power injector. Images The characteristics of HCCs which underwent RFA before and
were obtained at approximately 3545, 6580 and 190205 s, after after the introduction of Volume Navigation System were com-
starting the injection of the contrast agents for the arterial, portal pared. The 2 statistic was used for the categorical data analysis
and equilibrium phases, respectively [9]. and the Mann-Whitney U test was used for comparing the distri-
For CT angiography, selective catheterization was conducted bution of continuous variables. The data were analyzed using
with two catheters inserted by the Seldinger technique from ei- SPSS version 17.0 software (SPSS, Chicago, Ill., USA) and p value
ther the right or left femoral artery. One was placed in the supe- !0.05 was considered statistically significant.
rior mesenteric artery for CT during arterioportography and the
other in the common hepatic artery for CT during hepatic arteri-
ography. The former images were scanned 3033 s after adminis-
tration of 6680 ml of 150160 mgI/ml nonionic contrast agents Results
at a rate of 2.0 ml/s. The latter images were scanned 58 s after
injection of 2033 ml of 150160 mgI/ml nonionic contrast agents A total of 164 patients with 243 HCCs underwent RFA
at a speed of 1.0 ml/s [19]. between September 2009 and January 2011. Regarding
major complications, intercostal artery hemorrhage was
Gd-EOB-DTPA-Enhanced MRI
Gd-EOB-DTPA-enhanced MR imaging was performed using observed in 2 cases (1.2%). All of the treated tumors were
a 1.5-T system (Signa Excite HD 1.5T, GE Healthcare Japan) with considered to be completely ablated on follow-up dynam-
a slice thickness of 3 or 5 mm. For the contrast enhancement, 25 ic CT at the end, after one or more treatment sessions.
mol/kg body weight (0.1 ml/kg) of Gd-EOB-DTPA (Primovist,
Bayer-Schering Pharma AG, Berlin, Germany) was administered Patient and Tumor Characteristics
intravenously at a rate of 2.0 ml/s. At first, an unenhanced MRI
was obtained using a T1-weighted gradient echo sequence (dual Between September 2009 and April 2010 (period A),
echoes; in-phase and out-of-phase). Then, unenhanced, arterial, 75 patients with 120 HCCs underwent RFA without the
portal, late and hepatobiliary phase images were acquired just be- US fusion imaging system. Eighty-nine patients with 123
fore, 25, 70, 180 s and 20 min, respectively, after injection of the HCCs were treated with RFA with Volume Navigation
contrast agent [9, 10]. System between May 2010 and January 2011 (period B).
Grayscale US and CEUS Clinical characteristics of the subjects are listed in table1.
The ultrasound systems used for the imaging of both grayscale There was no significant difference in the number of
US and CEUS were Aplio XG with a 3.5 MHz curved array convex HCCs treated with RFA per case, the proportion of cases
probe or a 3.5 MHz microconvex probe from September 2009 to using artificial ascites or pleural effusion, and number of
April 2010 (period A) or LOGIQE9 equipped with Volume Navi- treatment sessions between periods A and B. However,
gation System with a 3.5-MHz curved array convex probe or a 1-
to 6-MHz microconvex probe from May 2010 to January 2011 the proportion of tumors with poor conspicuity on gray-
(period B). scale US significantly increased from 1.7 (2/120) to 15.4%
Before RFA, an attempt was made to detect all HCCs on gray- (19/123) after the introduction of Volume Navigation Sys-
scale US at first. The operator sought the tumor, carefully refer- tem.
encing the intrahepatic structures such as blood vessels, cysts or
scars from previous treatments.
If the HCC could not be detected on grayscale US, CEUS using RFA for HCCs with Poor Conspicuity on Grayscale US
Sonazoid was conducted next, with or without the US fusion im- Using the US Fusion Imaging System
aging (periods A and B, respectively), focusing on the site where If a tumor was difficult to visualize on grayscale US,
the target tumor was likely to be depicted. Images of the vascular CEUS was subsequently conducted. Before the introduc-
phase were acquired over a 120-second period with a low me- tion of Volume Navigation System (period A), images of
chanical index of less than 0.3 after injection of 0.0075 ml/kg of
Sonazoid. Images of the postvascular phase were obtained more vascular phase and postvascular phase were obtained by
than 10 min after administration of the contrast agent. If a hy- focusing on the site where the HCC was likely to be visu-
poechoic area suggesting the tumor was observed in the postvas- alized, estimated from axial images of CT or MRI. How-
cular phase, the same dose of Sonazoid was reinjected and the ever, only 2 HCCs could be detected on CEUS and treated
vascularity was evaluated [11]. with RFA in this way. If a tumor could not be detected
Since LOGIQE9 was introduced in May 2010 (period B), gray-
scale US was carried out in order to identify a target tumor with- either on grayscale US or CEUS, we were obliged to give
out Volume Navigation System at first. Subsequently, all proce- up RFA.
dures described above were conducted with Volume Navigation
46 Oncology 2013;84(suppl 1):4450 Makino et al.
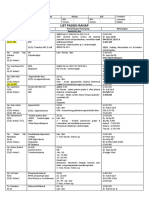
Table 1. Characteristics of the patients and HCCs that underwent RFA with and without the US fusion imaging system
Variables Without US fusion imaging With US fusion imaging p
system (period A) system (period B) value
Patients, n 75 89 n.a.
HCCs, n 120 123 n.a.
HCCs treated with RFA per case, n 1.3980.76 1.3780.66 n.s.a
Mean tumor diameter, mm 15.886.7 14.186.2 n.s.a
HCCs using artificial ascites or pleural effusion, n 77 (64.2%) 90 (73.2%) n.s.b
HCCs with poor conspicuity on grayscale US, n 2 (1.7%) 19 (15.4%) <0.01b
Treatment sessions, n 1.0780.26 1.1180.33 n.s.a
a
Mann-Whitney U test. b 2 statistic.
Meanwhile, 19 HCCs with poor conspicuity on gray- of the probe [1517, 20]. In this report, we have clearly
scale US could be treated with RFA after the introduction shown that the number of HCCs with poor conspicuity
of Volume Navigation System (period B). Among the 19 on grayscale US and treated with RFA successfully has
HCCs, 5 and 9 HCCs could be identified on grayscale US significantly increased since the introduction of the US
and CEUS, respectively, using Volume Navigation Sys- fusion imaging system.
tem. Nevertheless, the remaining 5 HCCs could not be Gd-EOB-DTPA-enhanced MRI has been reported to
detected either on grayscale US or CEUS with this sys- have significantly higher sensitivity and diagnostic accu-
tem. However, we could carry out RFA on them with the racy for detection of hypervascular HCC compared with
assistance of Volume Navigation System, referencing the multiphasic MDCT, particularly for small HCC, because
intrahepatic structures and hepatic contours on side-by- of the additional effect of hepatobiliary phase images to
side images and aiming at the sites where tumors were dynamic images [10, 22]. It is also reported that Gd-EOB-
expected to be located, or using the global positioning DTPA-enhanced MRI is the most useful imaging tech-
system (GPS) function, as described later. nique for the detection of early HCC [9, 23, 24]. Accord-
Among the HCCs that underwent RFA with Volume ingly, the opportunity to find small HCCs has increased
Navigation System (period B), the diameter of tumors de- since Gd-EOB-DTPA-enhanced MRI became available.
tectable on grayscale US (14.3 8 6.7 mm, n = 104) was As to the local control after RFA, small HCCs are con-
not different from that of HCCs with poor conspicuity on sidered to be a good candidate for RFA, because local tu-
it (15.1 8 6.8 mm, n = 19). In addition, the number of mor progression after RFA is related to the tumor diam-
treatment sessions is also not different between the de- eter [25]. However, RFA is usually conducted under US
tectable HCCs and those with poor conspicuity. Accord- guidance, so it seems difficult to perform RFA in cases
ingly, although the diameter of the HCCs with poor con- where tumor is hardly detectable on conventional US.
spicuity on grayscale US was the same as that of detect- Since the detection of HCC by US is considered to be re-
able HCCs, they could be treated with RFA successfully lated to the tumor size, in addition to the heterogeneous
in a single session in most cases, by virtue of Volume Nav- parenchymal echotexture of cirrhotic liver, it might not
igation System. be easy to identify small HCCs on conventional US and
perform RFA, even if they are diagnosed at an early stage
by other imaging modalities such as Gd-EOB-DTPA-en-
Discussion hanced MRI [2628].
CEUS with Sonazoid is reported to be useful for the
In recent years, the US fusion imaging system for the diagnosis and treatment of HCC [8, 11, 29, 30]. Sonazoid
guidance of RFA has become available [8, 17, 20, 21]. In provides a fine vascular image of hepatic tumors in vas-
the US fusion imaging system, any cross-sectional multi- cular phase, and is very sensitive in detecting an early
planar reconstruction images of the volume data of CT or stain of HCC. Perfusion defect of HCC obtained in the
MRI are synchronously displayed side-by-side with the postvascular phase is also useful for the detection of
real-time US images, in accordance with the movement HCC. However, on the post-vascular phase of CEUS with
Usefulness of the US Fusion Imaging for Oncology 2013;84(suppl 1):4450 47
RFA
a b e
Fig. 1. RFA for HCC undetectable on US with guidance from the
US fusion imaging system in a 63-year-old man. a Arterial phase
of dynamic CT. b Hepatobiliary phase of Gd-EOB-DTPA-en-
hanced MRI. c Fusion images of grayscale US (left side) and hep-
atobiliary phase of Gd-EOB-DTPA-enhanced MRI (right side) us-
ing Volume Navigation System. d Fusion images of grayscale US
just after RFA (left side) and hepatobiliary phase of Gd-EOB-DT-
PA-enhanced MRI (right side) using Volume Navigation System. c
e Portal phase of dynamic CT after RFA. HCC 13 mm in diameter
in segment VIII could be depicted as a hypervascular and hypoin-
tense nodule on dynamic CT (a) and hepatobiliary phase of Gd-
EOB-DTPA-enhanced MRI (b), respectively (arrows). However, it
could not be depicted either on grayscale US or contrast-enhanced
US, even with the assistance of Volume Navigation System. There-
upon, with the GPS function, the location of the targeted tumor
on grayscale US was estimated in reference to the GPS marker,
which indicated the tumor. RFA was then conducted by aiming at
the site. Just after RFA, the tumor was considered to be fully en-
compassed within the high echoic bubbles of the ablation zone
using the GPS function, suggesting complete ablation. Dynamic
CT after RFA also indicated complete ablation, after a single treat-
ment session. d
Sonazoid, some well-differentiated HCCs do not show targeted tumor is not conspicuous or surrounded by con-
hypoechoic appearance and HCCs distant from the body fusing cirrhosis-related nodules, it can be identified with
surface are difficult to detect because of the signal at- confidence by comparing it with intrahepatic structures
tenuation, which is considered to be the limitation of around the tumor on reference images. Kunishi et al. [17]
CEUS with Sonazoid [31, 32]. and Lee et al. [21] also reported that the detection rate of
The noteworthy usefulness of the US fusion imaging HCC on grayscale US had increased by virtue of Volume
system is the detectability of HCCs with poor conspicu- Navigation System, which is consistent with our results.
ity on grayscale US. Although RFA is carried out under Moreover, some hypervascular HCCs not detected on
US guidance of intercostal scanning in most cases, it is conventional US have been reported to become detect-
often difficult to guess how a tumor is observed from the able on the post-vascular phase of CEUS with Sonazoid
intercostal view from the axial images of CT or MRI. [11]. Actually, 9 out of 19 tumors which underwent RFA
Hence, it does not seem easy to identify the locus of the with poor conspicuity on grayscale US could be identified
targeted tumor unless it is well defined on grayscale US. combining CEUS and the US fusion imaging system in
However, with the US fusion imaging system, even if the this study (period B), whereas only 2 HCCs with poor
48 Oncology 2013;84(suppl 1):4450 Makino et al.
conspicuity on grayscale US could be detected on CEUS was most frequently used and considered most optimal.
and treated with RFA before the introduction of the sys- One of the reasons is that it has the highest sensitivity for
tem (period A). Another 5 of the 19 HCCs of period B detecting HCC [9, 10, 2224, 33] as described above, and
could be detected on grayscale US, using Volume Naviga- another is the clear depiction of tumors and surrounding
tion System. intrahepatic landmarks [30], which makes the positional
Finally, 5 out of 19 HCCs with poor conspicuity on registration accurate and easy.
grayscale US of period B could not be detected in spite of
the use of the US fusion imaging system. This is consid-
ered to be partly because of the limitation of CEUS, as Conclusion
described above. However, even if a tumor is not detect-
able either on grayscale US or CEUS, there is still the pos- The usefulness of the US fusion imaging system for
sibility of conducting RFA, since we can estimate the ap- RFA of HCC was verified in this study. Although some
proximate location of the tumor using the US fusion im- limitations are still left in terms of the accuracy and the
aging system. In particular, a GPS function installed in long-term prognosis has not been fully investigated yet, it
Volume Navigation System is very helpful in locating has greatly extended the indication of RFA. The US fu-
such HCCs. When GPS markers are indicated on the tar- sion imaging system is certainly a valuable tool which
get on the reference images, corresponding sites are pin- enables us to take advantage of the benefits of early diag-
pointed on real-time US images [20]. Therefore, the site nosis and treatment of HCC.
of the targeted tumor can be easily identified, even if it is
undetectable on US (fig.1). Thus, we could successfully
conduct RFA on 5 HCCs undetectable on grayscale US. Disclosure Statement
In this way, it has become possible to perform RFA for
The authors declare that no financial or other conflict of inter-
HCCs with poor conspicuity on grayscale US since the
est exists in relation to the content of the article.
introduction of the US fusion imaging system.
As for reference images in the US fusion imaging sys-
tem, the hepatobiliary phase of Gd-EOB-enhanced MRI
References
1 Jemal A, Bray F, Center MM, Ferlay J, Ward 5 Bruix J, Sherman M, American Association 10 Onishi H, Kim T, Imai Y, Hori M, Nagano H,
E, Forman D: Global cancer statistics. CA for the Study of Liver Diseases: Management Nakaya Y, Tsuboyama T, Nakamoto A, Tat-
Cancer J Clin 2011;61:6990. of hepatocellular carcinoma: an update. sumi M, Kumano S, Okada M, Takamura M,
2 Imai Y, Kawata S, Tamura S, Yabuuchi I, Hepatology 2011;53:10201022. Wakasa K, Tomiyama N, Murakami T: Hy-
Noda S, Inada M, Maeda Y, Shirai Y, Fuku- 6 Ansari D, Andersson R: Radiofrequency ab- pervascular hepatocellular carcinomas: de-
zaki T, Kaji I, Ishikawa H, Matsuda Y, Nishi- lation or percutaneous ethanol injection for tection with gadoxetate disodium-enhanced
kawa M, Seki K, Matsuzawa Y: Relation of the treatment of liver tumors. World J Gas- MR imaging and multiphasic multidetector
interferon therapy and hepatocellular carci- troenterol 2012;18:10031008. CT. Eur Radiol 2012;22:845854.
noma in patients with chronic hepatitis C. 7 Lencioni R, Crocetti L: Local-regional treat- 11 Kudo M, Hatanaka K, Kumada T, Toyoda H,
Ann Intern Med 1998;129:9499. ment of hepatocellular carcinoma. Radiolo- Tada T: Double-contrast ultrasound: a novel
3 Kudo M, Izumi N, Kokudo N, Matsui O, gy 2012;262:4358. surveillance tool for hepatocellular carcino-
Sakamoto M, Nakashima O, Kojiro M, 8 Murakami T, Imai Y, Okada M, Hyodo T, Lee ma. Am J Gastroenterol 2011; 106:368370.
Makuuchi M, HCC Expert Panel of Japan WJ, Kim MJ, Kim T, Choi BI: Ultrasonogra- 12 Lee JM, Yoon JH, Joo I, Woo HS: Recent ad-
Society of Hepatology: Management of hepa- phy, computed tomography and magnetic vances in CT and MR imaging for evaluation
tocellular carcinoma in Japan: Consensus- resonance imaging of hepatocellular carci- of hepatocellular carcinoma. Liver Cancer
Based Clinical Practice Guidelines proposed noma: toward improved treatment deci- 2012;1:2240.
by the Japan Society of Hepatology (JSH) sions. Oncology 2011;81;8699. 13 Ricke J, Seidensticker M, Mohnike K: Non-
2010 updated version. Dig Dis 2011; 29: 339 9 Kogita S, Imai Y, Okada M, Kim T, Onishi H, invasive diagnosis of hepatocellular carcino-
364. Takamura M, Fukuda K, Igura T, Sawai Y, ma in cirrhotic liver: current guidelines and
4 European Association for the Study of the Morimoto O, Hori M, Nagano H, Wakasa K, future prospects for radiological imaging.
Liver, European Organisation for Research Hayashi N, Murakami T: Gd-EOB-DTPA- Liver Cancer 2012;1:5158.
and Treatment of Cancer: EASL-EORTC enhanced magnetic resonance images of he- 14 Bota S, Piscaglia F, Marinelli S, Pecorelli A,
clinical practice guidelines: management of patocellular carcinoma: correlation with his- Terzi E, Bolondi L: Comparison of interna-
hepatocellular carcinoma. J Hepatol 2012;56: tological grading and portal blood flow. Eur tional guidelines for non-invasive diagnosis
908943. Radiol 2010;20:24052413. of hepatocellular carcinoma. Liver Cancer,
in press.
Usefulness of the US Fusion Imaging for Oncology 2013;84(suppl 1):4450 49
RFA
15 Kim YJ, Lee MW, Park HS: Small hepatocel- 21 Lee MW, Rhim H, Cha DI, Kim YJ, Choi D, 27 Kim PN, Choi D, Rhim H, Rha SE, Hong HP,
lular carcinomas: ultrasonography guided Kim YS, Lim HK: Percutaneous radiofre- Lee J, Choi JI, Kim JW, Seo JW, Lee EJ, Lim
percutaneous radiofrequency ablation. Ab- quency ablation of hepatocellular carcino- HK: Planning ultrasound for percutaneous
dom Imaging 2012, E-pub ahead of print. ma: fusion imaging guidance for manage- radiofrequency ablation to treat small (^3
16 Nakai M, Sato M, Sahara S, Takasaka I, ment of lesions with poor conspicuity at con- cm) hepatocellular carcinomas detected on
Kawai N, Minamiguchi H, Tanihata H, ventional sonography. AJR Am J Roentgenol computed tomography or magnetic reso-
Kimura M, Takeuchi N: Radiofrequency ab- 2012;198:14381444. nance imaging: a multicenter prospective
lation assisted by real-time virtual sonogra- 22 Di Martino M, Marin D, Guerrisi A, Baski study to assess factors affecting ultrasound
phy and CT for hepatocellular carcinoma M, Galati F, Rossi M, Brozzetti S, Mascian- visibility. J Vasc Interv Radiol 2012; 23: 627
undetectable by conventional sonography. gelo R, Passariello R, Catalano C: Intraindi- 634.
Cardiovasc Intervent Radiol 2009;32:6269. vidual comparison of gadoxetate disodium- 28 Mita K, Kim SR, Kudo M, Imoto S, Nakajima
17 Kunishi Y, Numata K, Morimoto M, Okada enhanced MR imaging and 64-section T, Ando K, Fukuda K, Matsuoka T, Maekawa
M, Kaneko T, Maeda S, Tanaka K: Efficacy of multidetector CT in the detection of hepato- Y, Hayashi Y: Diagnostic sensitivity of imag-
fusion imaging combining sonography and cellular carcinoma in patients with cirrhosis. ing modalities for hepatocellular carcinoma
hepatobiliary phase MRI with Gd-EOB- Radiology 2010;256:806816. smaller than 2 cm. World J Gastroenterol
DTPA to detect small hepatocellular carci- 23 Sano K, Ichikawa T, Motosugi U, Sou H, 2010;16:41874192.
noma. AJR Am J Roentgenol 2012; 198: 106 Muhi AM, Matsuda M, Nakano M, Sakamo- 29 Minami Y, Kudo M: Review of dynamic con-
114. to M, Nakazawa T, Asakawa M, Fujii H, Kita- trast-enhanced ultrasound guidance in abla-
18 International Consensus Group for Hepato- mura T, Enomoto N, Araki T: Imaging study tion therapy for hepatocellular carcinoma.
cellular Neoplasia: Pathologic diagnosis of of early hepatocellular carcinoma: useful- World J Gastroenterol 2011; 17:49524259.
early hepatocellular carcinoma: a report of ness of gadoxetic acid-enhanced MR Imag- 30 Numata K, Luo W, Morimoto M, Kondo M,
the international consensus group for hepa- ing. Radiology 2011;261:834844. Kunishi Y, Sasaki T, Nozaki A, Tanaka K:
tocellular neoplasia. Hepatology 2009; 49: 24 Inoue T, Kudo M, Komuta M, Hayaishi S, Contrast enhanced ultrasound of hepatocel-
658664. Ueda T, Takita M, Kitai S, Hatanaka K, Yada lular carcinoma. World J Radiol 2010; 2: 68
19 Imai Y, Murakami T, Yoshida S, Nishikawa N, Hagiwara S, Chung H, Sakurai T, Ueshi- 82.
M, Ohsawa M, Tokunaga K, Murata M, Shi- ma K, Sakamoto M, Maenishi O, Hyodo T, 31 Wong GL, Xu HX, Xie XY: Detection of focal
bata K, Zushi S, Kurokawa M, Yonezawa T, Okada M, Kumano S, Murakami T: Assess- liver lesions in cirrhotic liver using contrast-
Kawata S, Takamura M, Nagano H, Sakon M, ment of Gd-EOB-DTPA-enhanced MRI for enhanced ultrasound. World J Radiol 2009;
Monden M, Wakasa K, Nakamura H: Super- HCC and dysplastic nodules and compari- 1:2536.
paramagnetic iron oxide-enhanced magnet- son of detection sensitivity versus MDCT. J 32 Arita J, Hasegawa K, Takahashi M, Hata S,
ic resonance images of hepatocellular carci- Gastroenterol 2012; 47:10361047. Shindoh J, Sugawara Y, Kokudo N: Correla-
noma: correlation with histological grading. 25 Komorizono Y, Oketani M, Sako K, Yama- tion between contrast-enhanced intraopera-
Hepatology 2000;32:205212. saki N, Shibatou T, Maeda M, Kohara K, tive ultrasound using Sonazoid and histo-
20 Makino Y, Imai Y, Igura T, Ohama H, Kogita Shigenobu S, Ishibashi K, Arima T: Risk fac- logic grade of resected hepatocellular car-
S, Sawai Y, Fukuda K, Ohashi H, Murakami tors for local recurrence of small hepatocel- cinoma. AJR Am J Roentgenol 2011; 196:
T: Usefulness of the multimodality fusion lular carcinoma tumors after a single ses- 13141321.
imaging for the diagnosis and treatment of sion, single application of percutaneous 33 Golfieri R, Renzulli M, Lucidi V, Corcioni B,
hepatocellular carcinoma. Dig Dis, in press. radiofrequency ablation. Cancer 2003; 97: Trevisani F, Bolondi L: Contribution of the
12531262. hepatobiliary phase of Gd-EOB-DTPA-en-
26 Lee MW, Kim YJ, Park HS, Yu NC, Jung SI, hanced MRI to Dynamic MRI in the detec-
Ko SY, Jeon HJ: Targeted sonography for tion of hypovascular small (^2 cm) HCC in
small hepatocellular carcinoma discovered cirrhosis. Eur Radiol 2011;21:12331242.
by CT or MRI: factors affecting sonographic
detection. AJR 2010;194:396400.
50 Oncology 2013;84(suppl 1):4450 Makino et al.
Reproduced with permission of the copyright owner. Further reproduction prohibited without
permission.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- EOs PDFDocument91 pagesEOs PDFArushee BhatnagarNo ratings yet
- 2017 Book BiomarkersInLiverDiseaseDocument1,012 pages2017 Book BiomarkersInLiverDiseaserifdahNo ratings yet
- Data by Name Lansia Desa TambakDocument41 pagesData by Name Lansia Desa TambakgiviNo ratings yet
- Particular Cancer Power PointDocument101 pagesParticular Cancer Power PointKoRnflakesNo ratings yet
- Ijerph 19 09026Document36 pagesIjerph 19 09026giviNo ratings yet
- MSL 2019 68Document10 pagesMSL 2019 68giviNo ratings yet
- 496 1971 1 PBDocument16 pages496 1971 1 PBaliNo ratings yet
- Ijerph 19 09026Document36 pagesIjerph 19 09026giviNo ratings yet
- Asamrew (2020) Level of Patient Satisfaction With Inpatient Services and Its Determinants A Study of A Specialized Hospital in EthiopiaDocument12 pagesAsamrew (2020) Level of Patient Satisfaction With Inpatient Services and Its Determinants A Study of A Specialized Hospital in EthiopiaDiego RiveraNo ratings yet
- MSL 2019 68Document10 pagesMSL 2019 68giviNo ratings yet
- Jadwal QR Bulan AprilDocument12 pagesJadwal QR Bulan AprilgiviNo ratings yet
- Data Desbin ExcelDocument125 pagesData Desbin ExcelGindy AuliaNo ratings yet
- Jurnal 3Document7 pagesJurnal 3giviNo ratings yet
- Tanggal: Nama KaryawanDocument1 pageTanggal: Nama KaryawangiviNo ratings yet
- List Pasien Ranap: Tanggal: 24 November 2021 Dokter: GiviDocument18 pagesList Pasien Ranap: Tanggal: 24 November 2021 Dokter: GivigiviNo ratings yet
- Hasil Nilai Pre Post TestDocument1 pageHasil Nilai Pre Post TestgiviNo ratings yet
- International Journal of Surgery: Emma J. Noble, Ros Harris, Ken B. Hosie, Steve Thomas, Stephen J. LewisDocument6 pagesInternational Journal of Surgery: Emma J. Noble, Ros Harris, Ken B. Hosie, Steve Thomas, Stephen J. LewisChristopher AdhisasmitaNo ratings yet
- Morikawa2016Document6 pagesMorikawa2016giviNo ratings yet
- Cutaneous Larva MigranDocument3 pagesCutaneous Larva MigrangiviNo ratings yet
- Refleksi Kasus VesicolitiasisDocument14 pagesRefleksi Kasus VesicolitiasisgiviNo ratings yet
- Jurnal 3Document7 pagesJurnal 3giviNo ratings yet
- 2 PDFDocument7 pages2 PDFgiviNo ratings yet
- Jurnal Obgyn 1 PDFDocument8 pagesJurnal Obgyn 1 PDFgiviNo ratings yet
- High Myopia JournalDocument7 pagesHigh Myopia JournalindahpratiwiindraNo ratings yet
- Jurnal 3Document13 pagesJurnal 3giviNo ratings yet
- Jurnal 2Document9 pagesJurnal 2giviNo ratings yet
- Jurnal GynDocument6 pagesJurnal GyngiviNo ratings yet
- Jurnal GynDocument6 pagesJurnal GyngiviNo ratings yet
- Jurnal GynDocument6 pagesJurnal GyngiviNo ratings yet
- 89 1473095747Document6 pages89 1473095747giviNo ratings yet
- Jurnal Obgyn 1 PDFDocument8 pagesJurnal Obgyn 1 PDFgiviNo ratings yet
- Handbook of RadioembolizationDocument349 pagesHandbook of RadioembolizationEdu MassanaNo ratings yet
- CPG Hepatitis BDocument17 pagesCPG Hepatitis BBianca Watanabe - RatillaNo ratings yet
- Student SYB: Chet Cunha MS IV January 22, 2009Document15 pagesStudent SYB: Chet Cunha MS IV January 22, 2009okarasemNo ratings yet
- 2.3 - LIVER Patho - ARBDocument73 pages2.3 - LIVER Patho - ARBCRUZ Jill EraNo ratings yet
- Chalasani Et Al 2018 HepatologyDocument30 pagesChalasani Et Al 2018 HepatologyAlex DcostaNo ratings yet
- Chronic Liver DiseaseDocument3 pagesChronic Liver DiseaseNikey LimNo ratings yet
- Medical Tribune January 2012 HKDocument72 pagesMedical Tribune January 2012 HKKarena SabadoNo ratings yet
- MEDICAL TERMINOLOGY PRAKTIKUM.2020docxDocument17 pagesMEDICAL TERMINOLOGY PRAKTIKUM.2020docxEvangeline EngieNo ratings yet
- MASLD - A Systemic Metabolic Disorder With Cardiovascular and Malignant Complications 2024Document12 pagesMASLD - A Systemic Metabolic Disorder With Cardiovascular and Malignant Complications 2024draanalordonezv1991No ratings yet
- C-Reactive Protein: Key FactsDocument12 pagesC-Reactive Protein: Key FactsAngel CañaresNo ratings yet
- Liver FactsDocument26 pagesLiver FactsLiezl SabadoNo ratings yet
- Liver Fibrosis Causes and Methods of Assessment ADocument11 pagesLiver Fibrosis Causes and Methods of Assessment AmichaelNo ratings yet
- Git & Hepatobiliary-Ii 4 Year MBBS: KMU (IHPER) - Central Curriculum CommitteeDocument50 pagesGit & Hepatobiliary-Ii 4 Year MBBS: KMU (IHPER) - Central Curriculum CommitteeF ParikhNo ratings yet
- Gastroenterology PT MRCP I 2019 2nd Edition PDF HXP DR NotesDocument1,142 pagesGastroenterology PT MRCP I 2019 2nd Edition PDF HXP DR NotesRami NaousNo ratings yet
- AB-M02-CH2.3-LIVER PATH-Focal Abnormalities PDFDocument40 pagesAB-M02-CH2.3-LIVER PATH-Focal Abnormalities PDFThomas AndersonNo ratings yet
- Adherence and Perceived Barriers To Oral Antiviral Therapy For Chronic Hepatitis BDocument11 pagesAdherence and Perceived Barriers To Oral Antiviral Therapy For Chronic Hepatitis BLuciano DelphinoNo ratings yet
- Viral Hepatitis TableDocument2 pagesViral Hepatitis TableJohnNo ratings yet
- 61Document205 pages61Carlos HernándezNo ratings yet
- NEJM Treatment of Patients With Cirrohsis Aug 2016Document11 pagesNEJM Treatment of Patients With Cirrohsis Aug 2016risewfNo ratings yet
- Hepatobiliary Tract and Pancreatic Pathology Assignment - PAYSONDocument22 pagesHepatobiliary Tract and Pancreatic Pathology Assignment - PAYSONRodrigo Joseph PaysonNo ratings yet
- Jeevandan: Donor Organ Sharing SchemeDocument15 pagesJeevandan: Donor Organ Sharing SchemesumanNo ratings yet
- DUMMYZ005 : LPL - Production Test Collection Centre Sector - 18, Block-E Rohini DELHI 110085Document2 pagesDUMMYZ005 : LPL - Production Test Collection Centre Sector - 18, Block-E Rohini DELHI 110085Yatin VermaNo ratings yet
- Apasl MafldDocument31 pagesApasl MafldAtmaningtyas RahayuNo ratings yet
- FIRST ANN - Booklet ROICAM 10Document22 pagesFIRST ANN - Booklet ROICAM 10ssjjhrftbgNo ratings yet
- LiverCirr 2011Document303 pagesLiverCirr 2011EnderNo ratings yet
- HCV Persistence: Cure Is Still A Four Letter Word: See Article On Page 106Document3 pagesHCV Persistence: Cure Is Still A Four Letter Word: See Article On Page 106bmnlthyukNo ratings yet
- ENDOPHTHALMITISDocument1 pageENDOPHTHALMITISb99401114No ratings yet