Professional Documents
Culture Documents
Empirical Prescribing Chart Glasgow
Uploaded by
Hariharan NarendranOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Empirical Prescribing Chart Glasgow
Uploaded by
Hariharan NarendranCopyright:
Available Formats
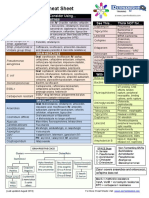
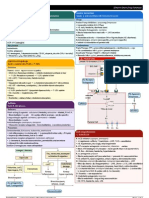
Guidance for initial hospital therapy in adults.
Infection Management Guideline: Empirical Antibiotic Therapy Specialist units may have separate policies.
STOP AND THINK BEFORE YOU GIVE ANTIBIOTIC THERAPY! Antibiotics are overused particulary in the elderly, patients with urinary catheters or suspected UTIs and in patients with viral or non-infective exacerbations of COPD. Always
obtain cultures and consider delay in therapy unless there is a clear anatomical site of infection with high probability of bacterial aetiology, if sepsis syndrome is present or if there is clinical deterioration. Record indication and SIRS score in case notes.
INDICATIONS FOR IV ROUTE (see IVOST guidelines) SIMPLIFY, SWITCH, STOP and STATE Duration! DEFINITION OF SEPSIS (Systemic Inflammatory Response Syndrome (SIRS)) - PLEASE RECORD IN CASE NOTES
IV antibiotic therapy should be commenced within 1 hour of recognition of sepsis or severe Clinical symptoms of infection (sweats, chills, malaise, rigors etc) PLUS 2 or more of the following:
infection in the clinical area where the diagnosis has been made. SIMPLIFY Use narrow spectrum agents whenever possible.
Temp <36C or >38C, HR >90bpm, RR >20/min and WCC <4 or >12 x109/L
1. Sepsis or severe sepsis or deteriorating clinical condition
SWITCH In the absence of +ve microbiology and specific situations (see indications for IV route) Severe sepsis: Sepsis + Organ dysfunction/ hypoperfusion eg. oliguria or urine <40ml/hr, confusion, lactic acidosis or hypotension (eg. systolic BP
2. Febrile with neutropenia/ immunosuppression
switch to oral therapy when signs of sepsis are resolving and oral route is not compromised. <90mmHg or reduction of 40mmHg from baseline)
3. Specific indications: endocarditis, deep abscess, bronchiestasis,
meningitis, CNS infection, bone/joint infection, S.aureus bacteraemia, CF, STOP Observe indicated duration of therapy and stop if alternative non-infectious diagnosis is made. NB. Signs of sepsis may be masked in immunosuppression, the elderly and in the presence of anti-inflammatory drugs or beta-blockers.
intra-abdominal / biliary sepsis infection. RECORD INDICATION, SEPSIS CRITERIA AND DURATION FOR ANTIBIOTIC IN NOTES Culture Blood Collect 2 or more (8-10mls each bottle) and appropriate area ie. Urine, sputum, CSF, wound or venous access site
4. Skin and soft tissue infection: IV therapy if sepsis or 2 of heat, erythema, ORAL DURATION SHOULD ALSO BE RECORDED IN KARDEX
induration/ swelling (usually IV for 48-96 hours)
5. Oral route compromised: nil by mouth, reduced GI absorption, mechanical
NB. Recomended doses are based on normal renal / liver function, Clostridium difficile infection is associated with prescribing of; Cephalosporins, Co-amoxiclav, Clindamycin, Quinolones (Ciprofloxacin,
swallowing disorder, unconscious, no oral formulation, vomiting see BNF for dose adjustments in renal / liver impairment. Levofloxacin, Moxifloxacin, Ofloxacin) and Piperacillin + Tazobactam. These agents must be restricted to reduce selection pressure.
Gastric acid suppression may predispose the patient to Clostridium difficile. Stop gastric acid suppressive therapy if possible.
m Immunocompromised
Lower respiratory tract Skin / soft tissue Gastro-intestinal Urinary tract Bone / joint infection CNS infection Severe systemic infection
patient ? source
Pneumonia EXAC of COPD / LRTI Mild soft tissue Gastroenteritis Lower UTI / cystitis in non Septic arthritis / osteomyelitis
Urgent IV therapy
infection Antibiotic not usually required pregnant women Consider underlying metal work,
CURB 65 score: Antibiotics only if purulent sputum.
Confusion (new onset), recent surgery, risk factors for
Oral therapy usually. Dual therapy Flucloxacillin 1g 6hrly Clostridium difficile Infection (CDI) Antibiotics if; urinary symptoms, IV therapy to be administered Which patient? Review all anatomical systems
Urea >7mmol/L, MRSA
not recommended or if true penicillin allergy Treat before laboratory confirmation frequency, dysuria. Obtain urine URGENTLY on arrival at Chemotherapy within 3 weeks, high dose Hospital vs community-acquired
RR30/min, if suspected CDI (loose stools plus culture. Consider orthopaedic referral steroids (prednisolone>15mg/day for >2
Amoxicillin 500mg 8hrly or Doxycycline 100mg 12hrly or hospital and after blood cultures. infection? E.coli, S. aureus and
BP diast 60 or syst BP<90 mmHg recent antibiotics or hospitalisation). Trimethoprim 200mg 12hrly weeks), other immunosuppressive agents
Age 65 yrs Doxycyline 200mg stat then *Clarithromycin 500mg 12hrly CT scan before LP if age >60, (e.g. anti-TNF, cyclophosphamide), transplant Pneumococcus are commonest
Discontinue if toxin negative. or Nitrofurantoin 50mg 6hrly Diabetic foot sepsis patients ( solid organ or bone marrow) or community blood culture isolates
100mg daily or Duration 7 days seizures, reduced GCS, CNS
Stop / simplify concomitant antibiot- Duration 3 days primary immunodeficiency. Please discuss
*Clarithromycin 500mg 12hrly Assess ulcer, probes to bone, signs or immunosuppression. patients with HIV infection with the ID Brown-
Non-severe community- ics and gastric acid suppressive
Mild human or animal bite Lower UTI in men (without sepsis) neuropathy, peripheral vascular Seek ID / microbiology advice.
lee Centre.
Consider MRSA infection
Duration 5 days therapy if possible. Ensure adequate
acquired pneumonia (CAP) or peri-anal soft tissue hydration Send urine for culture and consider
disease, MRSA risk? healthcare associated sepsis,
Sepsis syndrome
CURB 65 score: 0-1 ? LRTI / UTI infection prostatitis (see therapeutics handbook) For outpatient therapy consult recent hospital discharge, post-
Bacterial Meningitis Neutropenic sepsis : Neutrophil <0.5 or < 1.0
Amoxicillin 500mg 8hrly 1st episode / 1st relapse Trimethoprim 200mg 12hrly diabetic clinic guidelines and falling AND temp > 38C or < 36C on 2 operative wound or line-related
Non severe Co-amoxiclav 625mg 8hrly or Nitrofurantoin 50mg 6hrly Always refer to senior staff occasions 30mins apart. sepsis or sepsis in previous or
or Doxycycline 200mg stat then Severity markers; colonic dilatation
Doxycyline 200mg stat then 100mg daily
100mg daily or if true penicillin allergy >6cm, WCC >15 x109/L, Creatinine Duration 7 days
Obtain synovial fluid / deep tissue IV Ceftriaxone 2g 12hrly + Patients on high dose steroids or severely current MRSA carrier.
or Amoxicillin 500mg 8hrly Doxycycline 100mg 12hrly immunocompromised may not have an in-
or *Clarithromycin 500mg 12hrly >1.5 x baseline, temp > 38.5C or IV Dexamethasone 10mg 6hrly (for
Duration 5 days as appropriate when possible creased temperature but present with low BP,
Consider severe Streptococcal
Duration 7 days + Metronidazole 400mg 8hrly immunosuppression 4 days) hypothermia and / or rigors.
Upper UTI in non pregnant
PLUS Trimethoprim 200mg 12hrly Duration 7 days Severity markers = 0; or if true penicillin allergy sepsis e.g. pharyngitis, erythro-
women and men (without sepsis)
CURB 65 score: 2 (and no sepsis) Duration females 3 days or males 7 days oral Metronidazole 400mg 8hrly Trimethoprim 200mg 12hrly Septic arthritis / osteomyelitis Neutropenic plus sepsis derma, hypotension.
Amoxicillin 500mg 8hrly and either IV Choramphenicol 1g 6hrly +
Severe / sepsis Severity markers 1 or no or if resistant organisims suspected IV Dexamethasone 10mg 6hrly (for
Doxycycline 200mg stat then see Severe systemic infection ? source improvement after 5 days of Co-amoxiclav 625mg 8hrly Native joint IV Piperacillin / Tazobactam 4.5g 6hrly Source unknown
100mg daily 4 days)
metronidazole IV Flucloxacillin 2g 6hrly If SIRS 2 or NEWS 5 IV Benzylpenicillin 1.2g- 2.4g 6hrly + IV
or if true penicillin allergy then seek ID / microbiology advice.
or *Clarithromycin 500mg 12hrly
or if true penicillin allergy
ORAL THERAPY USUALLY RECOMMENDED oral Vancomycin 125mg 6 hrly + IV Gentamicin** (max 3-4 days) ADD IV Gentamicin** (review duration) Flucloxacillin 2g 4 - 6hrly
Duration 10 days Ciprofloxacin 500mg 12hrly or if true penicillin allergy If age 50 years, immunosup- If suspected Staphylococcal infection (e.g. + IV Gentamicin** (max 3-4 days)
*Clarithromycin 500mg 12hrly * Clarithromycin is known to have serious drug interactions and may Duration 7 days IV Vancomycin** pressed, pregnant, alcohol excess, line-related sepsis or soft tissue infection)
2nd episode / or subsequent relaps- or if true penicillin allergy or MRSA
(single therapy) prolong the QTc interval. Avoid in patients with other risk factors for QTc + IV Gentamicin** (max 3-4 days) liver disease or if listeria meningitis ADD IV Vancomycin** suspected
Duration 7 days es discuss mith microbiology / ID
prolongation.See BNF (appendix 1) or contact pharmacy for details suspected or If true penicillin allergy (anaphylaxis) IV Vancomycin**
Prosthetic joint ADD IV Amoxicillin 2g 4hrly to above IV Vancomycin** + IV Gentamicin** (max 3-4 days)
Severe CAP Moderate cellulitis Intra abdominal sepsis Pyelonephritis with sepsis IV Vancomycin**
or if true penicillin allergy + IV Gentamicin** (review duration)
Severe / complicated IV Flucloxacillin 1-2g 6hrly
IV Amoxicillin 1g 8hrly or oral route compromised in + IV Gentamicin** (max 3-4 days)
ADD IV Vancomycin** to above + IV Ciprofloxacin 400mg 12hrly if severe Streptococcal infection sus-
CURB 65 score: 3 or or if true penicillin allergy pected ADD IV Clindamycin 600mg 6hrly
CAP PLUS sepsis syndrome:
infective EXAC of COPD + IV Metronidazole 500mg 8hrly non pregnant women and men
or If true penicillin allergy (not anaphylaxis)
(up to 1200mg 6hrly)
IV Vancomycin** Diabetic foot osteomyelitis Duration 7 days (meningococcal), IV Vancomycin**
IV or oral *Clarithromycin 500mg + IV Gentamicin** (max 3-4 days) 14 days (pneumococcal), 21 days Seek ID/ microbiology advice
Use IV therapy if indication for IV Total duration 10 days (IV/oral) IV Amoxicillin 1g 8hrly as above PLUS oral metronidozle + IV Aztreonam 2g 8 hrly
12hrly and either or if true penicillin allergy 400mg 8hrly (listeria).
IV Amoxicillin 1g 8hrly or route (see above) or ventilation + IV Gentamicin** (max 3-4 days)
Severe or rapidly progressing IV Vancomycin** If haematology/oncology patient discuss Possible infective endocarditis
IV Co-amoxiclav 1.2g 8hrly (if previous required or sepsis. IVOST to oral Co- amoxiclav 625mg with appropriate specialist and seek ID /
Cellulitis (non drug user) + IV Metronidazole 500mg 8hrly Duration (IV/oral) dependent on surgi- Possible viral encephalitis microbiology advice. If stem cell / solid organ
treatment in the community) IV Amoxicillin 1g 8hrly or 8 hrly cal intervention. Usually 4 - 6 weeks. Consider if IVDU, line related sepsis, or
IV Flucloxacillin 2g 4 - 6hrly + IV Gentamicin** (max 3-4 days) IV Aciclovir 10mg/kg 8hrly (see therapeu- transplant or acute leukaemia and associ-
or if true penicillin allergy or if true penicillin allergy recent dental extraction. Always seek
IV *Clarithromycin 500mg 12hrly + IV Gentamicin** (max 3-4 days) tics handbook for dosage alteration in
ated severe shock give IV Meropenm + IV
senior specialist advice.
IV or oral Levofloxacin 500mg 12hrly If frail elderly patients or eGFR < 50ml/ IV Gentamicin** monotherapy Amikacin (see Neutropenic Sepsis in poster
NB. oral bioavailability 99-100% Duration 7 days (IV/oral) + IV Clindamycin 600mg 6hrly 2 renal impairment) for details)
or if true penicillin allergy REPLACE min/1.73m prescribe the above but (max 3-4 days)
Discuss management with ID. May require Immunocompromised patients with fever Native Heart valve
Flucloxacillin with IV Vancomycin** REPLACE Gentamicin with Discuss IVOST option with
Duration 7-10 days (IV/oral) or up to 14 NB. Doxycycline not available IV. repeat LP or neuro-imaging to establish and no neutropenia IV Amoxicillin 2g 4hrly
IV Aztreonam 2g 8-12 hrly depending on
days if atypical suspected or bacteraemia Duration 10 days (IV/oral) microbiology / ID diagnosis. If HSV/VSV confirmed continue Manage as per infection management
+ IV Flucloxacillin 2g 4hrly
serverity of infection
Duration 7 days (IV/oral) therapy for 14-21 days IV (no oral switch) guidelines based on anatomical source + IV Gentamicin synergistic dosing
Hospital-acquired pneumonia Severe human or animal Biliary tract infection as above, or if true penicillin allergy / penicillin
Aspiration pneumonia infected bite or peri-anal resistance / MRSA suspected
IV Metronidazole 500mg 8hrly Pancreatitis does not require anti-
Catheter-related UTI Avoid Gentamicin in patients with decompensated liver disease, contact microbiology or ID for advice IV Vancomycin**
4 days of admission infection Remove / replace catheter and culture **Gentamicin/ Vancomycin**
Treat as for CAP (see above)
and either IV Co-amoxiclav 1.2g 8hrly
biotic therapy unless complicated by urine. 7. If Creatinine not available give gentamicin as follows, + IV Gentamicin synergistic dosing
IV Amoxicillin 1g 8hrly or gallstones
Duration 7 days (IV/oral) or if true penicillin allergy 1. To access dose calculator click on the clinical info Actual weight Gentamicin Dose
IV *Clarithromycin 500mg 12hrly Symptomatic bacteriuria without icon on staff intranet page. Prosthetic Heart valve
5 days admission or within 7 days IV Metronidazole 500mg 8hrly Duration up to 7 days (IV/oral), < 40Kg 5mg / kg,
sepsis 2. Check creatinine / renal function daily. IV Vancomycin**
discharge from hospital Duration 7 days (IV/oral) + IV *Clarithromycin 500mg 12hrly but dependent on clinical review 40-49kg 240mg,
Give single dose of IV Gentamicin** 3. Record accurate times of dose administration and + IV Gentamicin synergistic dosing
CURB 65 score: 2 and no sepsis + IV Gentamicin** (max 3-4 days) 50-59kg 280mg,
prior to catheter removal or if IV route concentration measurement. + oral Rifampicin t 70kg 450mg
Oral Co-amoxiclav 625mgs 8 hrly or oral Duration 10 days (IV/oral) Spontaneous bacterial not available give single dose of Oral 60-69kg 320mg, 12hrly, > 70kg 600mg 12 hrly (oral so-
4. Contact pharmacy if advice required.
Doxycycline 200mg stat then 100mg 12 hrly peritonitis Ciprofloxacin 500mg 30 minutes prior to 70-79kg 360mg, dium fusidate if rifampicin not suitable)
Duration 7 days Suspected necrotising fasciitis or any rapidly spreading catheter removal 5. Do not use Gentamicin beyond 3 or 4 days unless on
80kg 400mg.
Chronic liver disease with ascites advice of mircobiology or ID.
5 days admission or within 7 days infection / severe soft tissue infection in IVDU and peritoneal white cell count > 6. Ototoxicity is associated with prolonged use of 8. If CKD5 give 2.5mg/kg (maximum 180mg)
NB discuss synergistic gentamicin dosing
discharge from hospital Symptomatic bacteriuria with sepsis with pharmacy. Duration as per micro/ ID
IV Flucloxacillin 2 g 4 - 6 hrly + IV Benzylpenicillin 2.4g 6 hrly 500/mm3 or >250 neutrophils/mm3 As above and treat as per Pyelonephritis gentamicin. If the patient reports tinnitus, dizziness, poor 9. For gentamicin take a sample 6 -14 hrs after the start of advice. See therapeutics handbook.
CURB 65 score: 3 or sepsis syndrome balance, hearing loss, seeing objects oscillating, STOP the first infusion and review frequency once creatinine and
+ IV Gentamicin** + IV Clindamycin 600mg 6hrly (up to 1200mg 6hrly) / culture results
IV Amoxicillin 1g 8hrly IV Co- amoxiclav 1.2g 8hrly t Rifampicin is known to have serious drug
Gentamicin and contact Micro / ID. concentration are known.
+ IV Aztreonam 2g 8hrly + IV Metronidazole 500mg 8hrly AND CONSIDER EARLY DEBRIDEMENT/ interactions. See BNF (appendix1)
or if true penicillin allergy or contact pharmacy for details.
or if true penicillin allergy EXPLORATION / SURGICAL REFERAL
If MRSA suspected or if true penicillin allergy REPLACE Flucloxacillin IV or Oral Ciprofloxacin 12hrly
IV or oral Levofloxacin 500mg 12hrly
NB. oral bioavailability 99-100% + Benzylpenicillin with IV Vancomycin** + IV Vancomycin** SEVERE INFECTIONS or INFECTIONS WHERE IV THERAPY IS USUALLY RECOMMENDED
Duration 7 -10 days (IV/oral) or up to 14 Duration 7 -10 days (IV/oral),
Review Antibiotic therapy DAILY: Stop? Simplify? Switch?
At 48 hours discuss with microbiology / ID before changing to oral
days if atypical suspected or bacteraemia
Duration as per microbiology / ID advice but dependent on clinical review
RATIONALISE ANTIBIOTIC THERAPY when microbiology results become available or clinical condition changes. FURTHER ADVICE Can be obtained from the Duty Microbiologist or Clinical Pharmacist or the ID Unit (Brownlee Centre), Gartnavel General Hospital,
Review IV therapy daily and remember IV-ORAL SWITCH or your local Respiratory Unit (for pneumonia) or Therapeutics handbook. Infection Control advice may be given by the duty microbiologist.
CRP- does not reflect the severity of infection and may remain elevated when the infection is resolving.
Greater Glasgow & Cyde Antimicrobial Utilisation Committee, ADTC. August 2014 expires Aug 2017. Review updates on .www.ggcformulary.scot.nhs.uk/Guidelines MIS 165760/a.
It cannot be used, in isolation, to assess the severity of infection and hence the need for IV therapy.
You might also like
- Clin Pharm Lile Antibacterial Classes and ExamplesDocument4 pagesClin Pharm Lile Antibacterial Classes and ExamplesNicole BerryNo ratings yet
- Antibiotics Summary - Flattened PDFDocument3 pagesAntibiotics Summary - Flattened PDFmicheal1960100% (5)
- Antibiotic Study Cheat Sheet October 2018Document1 pageAntibiotic Study Cheat Sheet October 2018Nourhan100% (3)
- A.1. Community-Acquired: Use Antibiotics JudiciouslyDocument33 pagesA.1. Community-Acquired: Use Antibiotics JudiciouslymaxgroovesNo ratings yet
- Wellington ICU Antibiotic SummaryDocument1 pageWellington ICU Antibiotic SummaryDesi Hutapea100% (4)
- Antibiotics ChartDocument10 pagesAntibiotics ChartTrina Si100% (6)
- Diabetes Mellitus Drug ChartDocument3 pagesDiabetes Mellitus Drug Chartlui.stephanie1751100% (1)
- Common infections and recommended antibioticsDocument3 pagesCommon infections and recommended antibioticsNicole BerryNo ratings yet
- The Principles of Antibiotic Therapy: S. Aureus Streptococcus PneumoniaeDocument16 pagesThe Principles of Antibiotic Therapy: S. Aureus Streptococcus PneumoniaeDianne Chua100% (7)
- Antibiotics Quick ReviewDocument5 pagesAntibiotics Quick Reviewpranjl100% (5)
- AntibioticsDocument6 pagesAntibioticsOccamsRazor100% (1)
- Drug Interactions 2 Paper PDFDocument2 pagesDrug Interactions 2 Paper PDFAzima AbdelrhamanNo ratings yet
- AB ClassesDocument4 pagesAB Classesrayooona88100% (2)
- Antibiotics Handout ReferenceDocument3 pagesAntibiotics Handout Referencebl9nkverseNo ratings yet
- Cardiac Meds CompleteDocument3 pagesCardiac Meds CompleteDanielle100% (2)
- Antibiotics 101Document49 pagesAntibiotics 101Tony VoNo ratings yet
- Antibiotic Cheat SheetDocument1 pageAntibiotic Cheat SheetCarla M. BeauchampNo ratings yet
- Antibiotic Study Cheat Sheet August 2019Document1 pageAntibiotic Study Cheat Sheet August 2019Ryan TurnerNo ratings yet
- Antibacterial Drugs SummaryDocument13 pagesAntibacterial Drugs SummaryNeo Ramagaga100% (1)
- Introduction to commonly used antibioticsDocument2 pagesIntroduction to commonly used antibioticsAmir AmirulNo ratings yet
- Treatment guidelines for common infectionsDocument1 pageTreatment guidelines for common infectionsJoseph De JoyaNo ratings yet
- Drug Mechanism Clincal Use Side Effects Antifungal: Amphote Ricin BDocument30 pagesDrug Mechanism Clincal Use Side Effects Antifungal: Amphote Ricin BCess Lagera Ybanez0% (1)
- AntibioticsDocument6 pagesAntibioticsyezan27100% (8)
- Clinical Medicine Cheat Sheet Ebook PDFDocument18 pagesClinical Medicine Cheat Sheet Ebook PDFMokaNo ratings yet
- Antibiotics Cheat SheetDocument2 pagesAntibiotics Cheat SheetAlejandro Rodas Salinas100% (1)
- Anti Infective Drug ChartDocument1 pageAnti Infective Drug ChartJessica100% (1)
- 1000 Drug CardsDocument33 pages1000 Drug CardsJelly BeanNo ratings yet
- AntibioticGuidelines PrimaryDocument12 pagesAntibioticGuidelines PrimaryHandriyato SukmaNo ratings yet
- Antibiotic SheetDocument4 pagesAntibiotic SheetAngelo Ostrea100% (1)
- SuperDrugs! Simon's Short Drug SummaryDocument5 pagesSuperDrugs! Simon's Short Drug Summarybriancripe100% (2)
- Pharm MnemonicsDocument33 pagesPharm MnemonicsThomson George75% (4)
- Pharmacology Chart 3Document2 pagesPharmacology Chart 3Omar ClorNo ratings yet
- Gram Positive Cocci (GPC) Gram Neg (Rods GNR) Anaerobes Atypicals Classification AntibioticDocument2 pagesGram Positive Cocci (GPC) Gram Neg (Rods GNR) Anaerobes Atypicals Classification AntibioticRami RaedNo ratings yet
- Pharmacology Complete Drug TableDocument6 pagesPharmacology Complete Drug Tableninja-2001100% (4)
- Git Drugs TablesDocument3 pagesGit Drugs TablesSulochan Ssplendid Splinterr Lohani100% (1)
- Bumetanide Torsemide: Desmopressin - V2Document1 pageBumetanide Torsemide: Desmopressin - V2med testNo ratings yet
- Pharmacology SummaryDocument16 pagesPharmacology Summarysechzhen96% (46)
- Classification of major antibiotic classes and examplesDocument1 pageClassification of major antibiotic classes and examplesSY WongNo ratings yet
- TLDR Anticoag Cheat Sheet v1.1Document3 pagesTLDR Anticoag Cheat Sheet v1.1nitishavenkat100% (9)
- Drugs PharmacologyDocument87 pagesDrugs PharmacologyVarun MehrotraNo ratings yet
- Drug Charts: Pharmacology OverviewDocument39 pagesDrug Charts: Pharmacology OverviewAsim Ishaq100% (5)
- Lab Normal Value S&Sof S&Sof : Loma Linda University School of Nursing Accepted Lab Values Adapted From KaplanDocument3 pagesLab Normal Value S&Sof S&Sof : Loma Linda University School of Nursing Accepted Lab Values Adapted From KaplanGiacen100% (3)
- 17 Cardiac DrugsDocument6 pages17 Cardiac DrugshiwaralelataNo ratings yet
- Pharmacology Charts PDFDocument88 pagesPharmacology Charts PDFMohamad Samir90% (10)
- Drug of Choice in Various DiseasesDocument5 pagesDrug of Choice in Various DiseasesRitesh Singh100% (5)
- Top 300 Drugs Pocket Reference Guide (2021 Edition)From EverandTop 300 Drugs Pocket Reference Guide (2021 Edition)Rating: 5 out of 5 stars5/5 (1)
- Mnemonics for Medicine: Differential Diagnoses and Other PearlsFrom EverandMnemonics for Medicine: Differential Diagnoses and Other PearlsRating: 5 out of 5 stars5/5 (3)
- Transport of Critically Ill Adults 2011Document1 pageTransport of Critically Ill Adults 2011velocity25No ratings yet
- IMG EmpAposterDocument1 pageIMG EmpAposterChiu LeoNo ratings yet
- Tetanus toxoid side effects and nursing responsibilitiesDocument10 pagesTetanus toxoid side effects and nursing responsibilitiesElle RosalesNo ratings yet
- Empirical Antimicrobial Therapy Prescribing Guidance For AdultsDocument1 pageEmpirical Antimicrobial Therapy Prescribing Guidance For AdultsPsychology TodayNo ratings yet
- Sepsis GuidelinesDocument1 pageSepsis GuidelinesYezenashNo ratings yet
- Clindamycin and Balsalazide Drug SheetDocument5 pagesClindamycin and Balsalazide Drug SheetLouwella RamosNo ratings yet
- PENYAKIT HATI DAN EMPEDUDocument46 pagesPENYAKIT HATI DAN EMPEDUfannyNo ratings yet
- Tuberculosis. (Gram Positive, Rod-Shaped, Acid-Fast and Aerobic) - PasteurizationDocument5 pagesTuberculosis. (Gram Positive, Rod-Shaped, Acid-Fast and Aerobic) - PasteurizationraphaelNo ratings yet
- OB Drug StudyDocument5 pagesOB Drug Studyvanni213No ratings yet
- Guidelines Emporical Antibiotic Therapy in AdultDocument2 pagesGuidelines Emporical Antibiotic Therapy in Adultgulf jobsNo ratings yet
- Adverse Effects and Nursing Responsibilities for Ceftriaxone and FurosemideDocument3 pagesAdverse Effects and Nursing Responsibilities for Ceftriaxone and FurosemideThyataira chuaNo ratings yet
- Question GlaucomaDocument1 pageQuestion GlaucomaHariharan NarendranNo ratings yet
- Applicant Handbook 2018Document58 pagesApplicant Handbook 2018Hariharan NarendranNo ratings yet
- SoudhgDocument1 pageSoudhgHariharan NarendranNo ratings yet
- 2017 Part 1 FRCOphth Information Pack 1Document24 pages2017 Part 1 FRCOphth Information Pack 1Hariharan NarendranNo ratings yet
- History PerformaDocument5 pagesHistory PerformaHariharan NarendranNo ratings yet
- History PerformaDocument5 pagesHistory PerformaHariharan NarendranNo ratings yet
- Guidelines For Insulin Initiation 2010-01 NHSDocument37 pagesGuidelines For Insulin Initiation 2010-01 NHSLalalala Gabriella KristianiNo ratings yet
- Self-Assessment in Optic and Refraction by Prof Chua, Dr. Chieng, DR - Ngo and Dr. AlhadyDocument107 pagesSelf-Assessment in Optic and Refraction by Prof Chua, Dr. Chieng, DR - Ngo and Dr. AlhadyKelvin TeoNo ratings yet
- DiabetesDocument28 pagesDiabetesHariharan NarendranNo ratings yet
- Writing Task 1 Band DescriptorsDocument1 pageWriting Task 1 Band DescriptorsIbrahim Babatunde OladapoNo ratings yet
- Developing World-Class CoachesDocument48 pagesDeveloping World-Class CoachesJordan Tant86% (7)
- Recruitment Applicant Handbook 2017Document58 pagesRecruitment Applicant Handbook 2017Hariharan NarendranNo ratings yet
- Safe HandoverDocument38 pagesSafe HandoverMatt Turner100% (1)
- Re Audit EndartectomyDocument16 pagesRe Audit EndartectomyHariharan NarendranNo ratings yet
- History PerformaDocument5 pagesHistory PerformaHariharan NarendranNo ratings yet
- All Wards Handover PDFDocument4 pagesAll Wards Handover PDFHariharan NarendranNo ratings yet
- Recruitment Applicant Handbook 2017Document58 pagesRecruitment Applicant Handbook 2017Hariharan NarendranNo ratings yet
- Oxygen AdministrationDocument29 pagesOxygen AdministrationKemal TaufikNo ratings yet
- DiabetesDocument28 pagesDiabetesHariharan NarendranNo ratings yet
- Archer C8 V1 UG PDFDocument143 pagesArcher C8 V1 UG PDFHariharan NarendranNo ratings yet
- Dermatology Handbook For Medical Students 2nd Edition 2014 Final2Document76 pagesDermatology Handbook For Medical Students 2nd Edition 2014 Final2Nogra CarlNo ratings yet
- A4 Boys 0-4YRS (4th Jan 2013)Document2 pagesA4 Boys 0-4YRS (4th Jan 2013)Mutiara SazkiaNo ratings yet
- DiabetesDocument28 pagesDiabetesHariharan NarendranNo ratings yet
- DiabetesDocument28 pagesDiabetesHariharan NarendranNo ratings yet
- DiabetesDocument28 pagesDiabetesHariharan NarendranNo ratings yet
- MBChB Year 4 & 5 Past Papers + Answers for Respiratory, Gastrointestinal, Neurology and MoreDocument172 pagesMBChB Year 4 & 5 Past Papers + Answers for Respiratory, Gastrointestinal, Neurology and MoreHariharan NarendranNo ratings yet
- DiabetesDocument28 pagesDiabetesHariharan NarendranNo ratings yet
- MBChB Year 4 & 5 Past Papers + AnswersDocument170 pagesMBChB Year 4 & 5 Past Papers + AnswersHariharan NarendranNo ratings yet
- Adie SyndromeDocument1 pageAdie SyndromeHariharan NarendranNo ratings yet
- Soap Making: Borax (NaDocument15 pagesSoap Making: Borax (Naa aNo ratings yet
- Chemical Equation CalculationsDocument6 pagesChemical Equation CalculationsHera RiegoNo ratings yet
- DLL - Science 6 - Q2 - W1Document6 pagesDLL - Science 6 - Q2 - W1AnatasukiNo ratings yet
- Corrosion and Its Objective QuestionsDocument2 pagesCorrosion and Its Objective QuestionsSrinivasan Alagappan100% (4)
- The Positive and Negative Syndrome Scale PANSS ForDocument5 pagesThe Positive and Negative Syndrome Scale PANSS ForditeABCNo ratings yet
- Energy Certification of Buildings and Nearly Zero-Energy BuildingsDocument70 pagesEnergy Certification of Buildings and Nearly Zero-Energy BuildingsOgnjen BobicicNo ratings yet
- The Problem of Drop Outs and School Building ConstructionDocument26 pagesThe Problem of Drop Outs and School Building ConstructionSweetaddy castilloNo ratings yet
- Fault Location of Overhead Transmission Line With Noncontact Magnetic Field MeasurementDocument10 pagesFault Location of Overhead Transmission Line With Noncontact Magnetic Field MeasurementJkNo ratings yet
- Transactional Analysis (TA)Document21 pagesTransactional Analysis (TA)Rohan TandonNo ratings yet
- Quartz Textures in Epithermal VeinsDocument16 pagesQuartz Textures in Epithermal VeinsAlvaro MadridNo ratings yet
- Numerical Modelling of Drying Kinetics of Banana Flower Using Natural and Forced Convection DryersDocument5 pagesNumerical Modelling of Drying Kinetics of Banana Flower Using Natural and Forced Convection DryersMuthu KumarNo ratings yet
- Kawasaki Ultra 250x Manual de Taller PDFDocument477 pagesKawasaki Ultra 250x Manual de Taller PDFAntonio Jose Planells100% (3)
- ITC's diverse businesses: cigarettes, packaging, hotels, paperboards, stationery, matches, incense sticks, retail, food, exportsDocument1 pageITC's diverse businesses: cigarettes, packaging, hotels, paperboards, stationery, matches, incense sticks, retail, food, exportsShashank JainNo ratings yet
- Evonik Copi BrochureDocument5 pagesEvonik Copi BrochureRovshan HasanzadeNo ratings yet
- Norris Claire White Paper Liftware PDFDocument14 pagesNorris Claire White Paper Liftware PDFmeysam NaaNo ratings yet
- Integrated Management of Childhood IllnessDocument8 pagesIntegrated Management of Childhood IllnessSehar162No ratings yet
- TST-13 Aircraft Manual With 503 Engine LSA Rev.1Document52 pagesTST-13 Aircraft Manual With 503 Engine LSA Rev.1smeassick100% (1)
- 02-Plant Morphology (Exercise)Document5 pages02-Plant Morphology (Exercise)varshavishuNo ratings yet
- Frenny PDFDocument651 pagesFrenny PDFIftisam AjrekarNo ratings yet
- Kovach 1987Document10 pagesKovach 1987Quyen ta thi nhaNo ratings yet
- E IA Diagnostic Atmos Cube 2012-07-04Document32 pagesE IA Diagnostic Atmos Cube 2012-07-04RogerNo ratings yet
- Precision Forging Processes GuideDocument35 pagesPrecision Forging Processes GuideRiski RamadhanNo ratings yet
- Reliance Tabletop SonicDocument20 pagesReliance Tabletop SonicbrisaNo ratings yet
- DIAGEO2Document12 pagesDIAGEO2Tatiana Zuleta RojasNo ratings yet
- Trilead bis(carbonate) dihydroxide identified as SVHC due to reproductive toxicityDocument7 pagesTrilead bis(carbonate) dihydroxide identified as SVHC due to reproductive toxicityCekinNo ratings yet
- Making your own Agar PlateDocument8 pagesMaking your own Agar PlateCheska EngadaNo ratings yet
- HVAC Report FINALDocument65 pagesHVAC Report FINALIanNo ratings yet
- Chapter Test A: Teacher Notes and Answers 17Document5 pagesChapter Test A: Teacher Notes and Answers 17Mmf 123 JanNo ratings yet
- Business Plan: in Partial Fulfillment For The Requirements in Entrepreneurship 2 Semester, S.Y. 2019-2020Document48 pagesBusiness Plan: in Partial Fulfillment For The Requirements in Entrepreneurship 2 Semester, S.Y. 2019-2020John Guden100% (1)
- ICH Topic Q 3 B (R2) Impurities in New Drug Products: European Medicines AgencyDocument14 pagesICH Topic Q 3 B (R2) Impurities in New Drug Products: European Medicines AgencyJesus Barcenas HernandezNo ratings yet