Professional Documents
Culture Documents
Trat Empiric Pneumonii
Uploaded by
Elena Traci0 ratings0% found this document useful (0 votes)
11 views4 pagestratamentul empiric in pneumonii
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documenttratamentul empiric in pneumonii
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
11 views4 pagesTrat Empiric Pneumonii
Uploaded by
Elena Tracitratamentul empiric in pneumonii
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
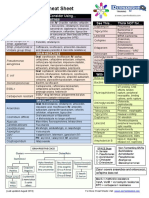
Empiric Therapy Regimens
Community-acquired pneumonia (CAP) is one the most common infectious diseases
addressed by clinicians. It is a major health problem in the United States and is an important
cause of mortality and morbidity worldwide. [1, 2]
CAP is defined as pneumonia acquired outside a hospital or long-term care facility. It occurs
within 48 hours of hospital admission or in a patient presenting with pneumonia who does not
have any of the characteristics of healthcare-associated pneumonia (ie, hospitalized in an
acute care hospital for 2 or more days within 90 days of infection; resided in a nursing home
or long-term care facility; received recent intravenous antibiotic therapy, chemotherapy, or
wound care within the past 30 days of the current infection; or attend a hospital or
hemodialysis clinic). [1, 2]
A number of pathogens can give rise to CAP, generally categorized into typical and atypical
pathogens.
Typical bacterial pathogens that cause CAP include Streptococcus pneumonia(penicillin-
sensitive/resistant strains), Haemophilus influenza (ampicillin-sensitive/resistant strains),
and Moraxella catarrhalis (all strains penicillin-resistant) and account for approximately 85%
of CAP cases. CAP is usually acquired via inhalation or aspiration of a pulmonary pathogen
into a lung segment or lobe. Less commonly, CAP results from secondary bacteremia from a
distant source, such as Escherichiacoli urinary tract infection and/or bacteremia. Aspiration
pneumonia is the only form of CAP caused by multiple pathogens (eg, aerobic/anaerobic oral
organisms). Klebsiella pneumonia CAP occurs primarily in persons with chronic alcoholism
and Staphylococcalaureus may cause CAP in patients with influenza. Pseudomonas
aeruginosa is a cause of CAP in patients with bronchiectasis or cystic fibrosis. [1]
Atypical pathogen CAP manifests a variety of pulmonary and extrapulmonary findings (eg,
CAP plus diarrhea). Atypical CAP can be divided into those caused by either zoonotic or
nonzoonotic atypical pathogens. Zoonotic atypical CAP pathogens
include Chlamydophila (Chlamydia) psittaci (psittacosis), Coxiella burnetii (Q fever),
and Francisella tularensis (tularemia). Nonzoonotic atypical CAP pathogens
include Mycoplasma pneumoniae, Legionella species, andChlamydia pneumoniae. These
organisms account for approximately 15% of all CAP cases. [1]
For all suspected CAP patients, in light of better outcomes with the earliest possible
interventions the Infectious Diseases Society of America (IDSA) recommends initial empiric
antimicrobial therapy until laboratory results can be obtained to guide more specific
therapy. [2]
Empiric therapeutic regimens for CAP are outlined below, including those for outpatients with
or without comorbidities, intensive care unit (ICU) and non-ICU patients, and penicillin-
allergic patients. [2]
Outpatient
No comorbidities/previously healthy; no risk factors for drug-resistant S pneumoniae:
Azithromycin 500 mg PO one dose, then 250 mg PO daily for 4 d or extended-release
2 g PO as a single dose or
Clarithromycin 500 mg PO bid or extended-release 1000 mg PO q24h or
Doxycycline 100 mg PO bid
If received prior antibiotic within 3 months:
Azithromycin or clarithromycin plus amoxicillin 1 g PO q8h or amoxicillin-
clavulanate 2 g PO q12h or
Respiratory fluoroquinolone (eg, levofloxacin 750 mg PO daily ormoxifloxacin 400
mg PO daily)
Comorbidities present (eg, alcoholism, bronchiectasis/cystic fibrosis, COPD, IV drug user,
post influenza, asplenia, diabetes mellitus, lung/liver/renal diseases):
Levofloxacin 750 mg PO q24h or
Moxifloxacin 400 mg PO q24h or
Combination of a beta-lactam ( amoxicillin 1 g PO q8h or amoxicillin-clavulanate 2 g
PO q12h or ceftriaxone 1g IV/IM q24h or cefuroxime 500 mg PO BID) plus a
macrolide (azithromycin or clarithromycin)
Duration of therapy: minimum of 5 days, should be afebrile for 48-72 hours, or until afebrile
for 3 days; longer duration of therapy may be needed if initial therapy was not active against
the identified pathogen or if it was complicated by extrapulmonary infections
Inpatient, non-ICU
See the list below:
Levofloxacin 750 mg IV or PO q24h or
Moxifloxacin 400 mg IV or PO q24h or
Combination of a beta-lactam (ceftriaxone 1 g IV q24h or cefotaxime 1 g IV
q8h or ertapenem 1 g IV daily or ceftaroline 600 mg IV q12h) plusazithromycin 500
mg IV q24h
Duration of therapy: minimum of 5 days, should be afebrile for 48-72 hours, stable blood
pressure, adequate oral intake, and room air oxygen saturation of greater than 90%; longer
duration may be needed in some cases
Inpatient, ICU:
Severe COPD:
Levofloxacin 750 mg IV or PO q24h or
Moxifloxacin 400 mg IV or PO q24h or
Ceftriaxone 1 g IV q24h or ertapenem 1 g IV q24h plus azithromycin 500 mg IV
q24h
If gram-negative rod pneumonia (Pseudomonas) suspected, due to alcoholism with
necrotizing pneumoniae, chronic bronchiectasis/tracheobronchitis due to cystic fibrosis,
mechanical ventilation, febrile neutropenia with pulmonary infiltrate, septic shock with organ
failure:
Piperacillin-tazobactam 4.5 g IV q6h or 3.375 g IV q4h or 4-h infusion of 3.375 g
q8h or
Cefepime 2 g IV q12h or
Imipenem/cilastatin 500 mg IV q6h or meropenem 1 g IV q8h or
If penicillin allergic, substitute aztreonam 2 g IV q6h plus
Levofloxacin 750 mg IV q24h or
Moxifloxacin 400 mg IV or PO q24h or
Aminoglycoside ( gentamicin 7 mg/kg/day IV or tobramycin 7 mg/kg/day IV )
Add azithromycin 500 mg IV q24h if respiratory fluoroquinolone not used
Duration of therapy: 10-14 days
If concomitant with or post influenza:
Vancomycin 15 mg/kg IV q12h or linezolid 600 mg IV bid plus
Levofloxacin 750 mg IV q24h or
Moxifloxacin 400 mg IV or PO q24h
If received prior antibiotic within 3 months:
High-dose ampicillin 2 g IV q6h (or penicillin G, if not resistant); if penicillin allergic,
substitute with vancomycin 1 g IV q12h plus
Azithromycin 500 mg IV q24h plus
Levofloxacin 750 mg IV q24h or moxifloxacin 400 mg IV/PO q24h
Risk of aspiration pneumonia/anaerobic lung infection/lung abscess:
See the list below:
Clindamycin 300-450 mg PO q8h or
Ampicillin-sulbactam 3 g IV q6h or
Ertapenem 1 g IV q24h or
Ceftriaxone 1 g IV q24h plus metronidazole 500 mg IV q6h or
Moxifloxacin 400 mg IV or PO q24h or
Piperacillin-tazobactam 3.375 g IV q6h or
If methicillin-resistant S aureus (MRSA) is suspected, add vancomycin 15 mg/kg IV
q12h or linezolid 600 mg IV/PO q12h
If influenza is suspected, add oseltamivir 75 mg IV or PO q12h for 5 d
New antimicrobials in CAP
Since the publication of the 2007 IDSA/American Thoracic Society (ATS) guidelines for the
management of CAP in adults, 2 intravenous antimicrobials have been approved by the US
Food and Drug Administration (FDA) for the treatment of CAP: tigecycline and ceftaroline
fosamil.
Use of tigecycline in CAP
Tigecycline was approved by the FDA in 2009 for adults with CAP caused by S
pneumoniae (penicillin-susceptible isolates), including cases with concurrent bacteremia, H
influenza (beta-lactamase-negative isolates), and Legionella pneumophila. In a study
conducted to evaluate the efficacy of tigecycline versus levofloxacin in hospitalized patients
with CAP, tigecycline achieved cure rates similar to those of levofloxacin in hospitalized
patients with CAP. For patients with risk factors, tigecycline provided generally favorable
clinical outcomes. [3]
Data from various sources, including PubMed, the European Medicines Agency (EMEA), and
the FDA were appraised. Tigecycline was found to be noninferior compared with levofloxacin
for the treatment of patients with bacterial CAP requiring hospitalization. [4]
Although tigecycline is indicated for CAP, data from clinical trials suggest a high incidence of
adverse events, particularly gastrointestinal adverse effects, which may limit its use. [5]
Dosing for tigecycline is as follows:
Tigecycline 100 mg IV loading dose, then 50 mg IV q12h for 7-14 d
Use of ceftaroline in CAP
Ceftaroline fosamil is a parenteral cephalosporin antibacterial that was approved by the FDA
in 2010 for the treatment of adults with CAP caused by S pneumoniae, including cases with
concurrent bacteremia; S aureus (methicillin-susceptible isolates only); H influenza; K
pneumonia; Klebsiella oxytoca; and E coli.
Ceftaroline, the active form of ceftaroline fosamil, has broad-spectrum in vitro activity against
common causative gram-positive and gram-negative bacteria, including MRSA. However,
there are no clinical data supporting the use of ceftaroline fosamil for MRSA pneumonia. [5]
Ceftaroline fosamil is included in Joint Commission pneumonia core measures as one of the
recommended beta-lactam antibiotics for CAP in immunocompetent, non-ICU patients.
{{Re6}
Dosing for ceftaroline is as follows:
Ceftaroline 600 mg IV q12h
You might also like
- 2015 Sizeguide Rings A4Document1 page2015 Sizeguide Rings A4Ara GrigorasNo ratings yet
- Infectii Cutanate ViraleDocument51 pagesInfectii Cutanate ViraleElena TraciNo ratings yet
- Q FeverDocument2 pagesQ FeverElena TraciNo ratings yet
- Hepatitis TratamientoDocument21 pagesHepatitis TratamientoJamil Saavedra DiazNo ratings yet
- 【医脉通】2016+NICE指南:脓毒症的识别,诊断和早期管理(NG 51)Document49 pages【医脉通】2016+NICE指南:脓毒症的识别,诊断和早期管理(NG 51)afandianddonkey-1No ratings yet
- Defining, Treating and Preventing Hospital Acquired Pneumonia: European PerspectiveDocument21 pagesDefining, Treating and Preventing Hospital Acquired Pneumonia: European PerspectiveElena TraciNo ratings yet
- CA, MG, PDocument18 pagesCA, MG, PElena TraciNo ratings yet
- IntoxicatiiDocument6 pagesIntoxicatiiElena TraciNo ratings yet
- Case Files Internal Medicine PDFDocument578 pagesCase Files Internal Medicine PDFElena TraciNo ratings yet
- Chief ComplinsDocument181 pagesChief ComplinsElena TraciNo ratings yet
- Nejm Hiv KaposiDocument10 pagesNejm Hiv KaposiIlaria IcartNo ratings yet
- ESCMID Guideline For The Management of Acute Sore ThroatDocument28 pagesESCMID Guideline For The Management of Acute Sore ThroatGanang Azhar GuntaraNo ratings yet
- Album de Cusaturi Moldovenesti de Veronica BalanDocument108 pagesAlbum de Cusaturi Moldovenesti de Veronica BalanDrucila100% (16)
- E BM White PaperDocument14 pagesE BM White PaperpongidaeNo ratings yet
- IntoxicatiiDocument6 pagesIntoxicatiiElena TraciNo ratings yet
- Ciuperci NecomestibileDocument4 pagesCiuperci NecomestibileElena TraciNo ratings yet
- Intoxicatie Cu CiuperciDocument6 pagesIntoxicatie Cu CiuperciElena TraciNo ratings yet
- Intoxicatie Cu CiuperciDocument6 pagesIntoxicatie Cu CiuperciElena TraciNo ratings yet
- Mushroom PoisoningDocument6 pagesMushroom PoisoningElena TraciNo ratings yet
- Antibiotic eDocument21 pagesAntibiotic eSinziiana SuhareanuNo ratings yet
- Mushroom PoisoningDocument6 pagesMushroom PoisoningElena TraciNo ratings yet
- Mushroom PoisoningDocument6 pagesMushroom PoisoningElena TraciNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Katzung Pharmacology Semester 5 TablesDocument29 pagesKatzung Pharmacology Semester 5 TablesfatimaNo ratings yet
- AntibiotikDocument10 pagesAntibiotikmayaNo ratings yet
- 26 Tetracyclines Glycylcyc 2015 Mandell Douglas and Bennett S PrincipleDocument24 pages26 Tetracyclines Glycylcyc 2015 Mandell Douglas and Bennett S PrincipleHelen DyNo ratings yet
- Tetracyclines, Macrolides & OthersDocument3 pagesTetracyclines, Macrolides & OthersJaybee SarmientoNo ratings yet
- Sun 2015Document10 pagesSun 2015sarah assegafNo ratings yet
- Drugs of choice for suspected or proved microbial pathogensDocument10 pagesDrugs of choice for suspected or proved microbial pathogensRavi Amin100% (1)
- Aerobic vs Anaerobic Bacteria: Understanding Their DifferencesDocument2 pagesAerobic vs Anaerobic Bacteria: Understanding Their DifferenceschandramohanvinNo ratings yet
- Intrinsic Resistance and Unusual Phenotypes Tables v3.2 20200225Document12 pagesIntrinsic Resistance and Unusual Phenotypes Tables v3.2 20200225Roy MontoyaNo ratings yet
- 1 s2.0 S0196655316001693 MainDocument3 pages1 s2.0 S0196655316001693 MainSandu AlexandraNo ratings yet
- Antibiotice in Terapie IntensivaDocument9 pagesAntibiotice in Terapie IntensivaLiliana NăstaseNo ratings yet
- Artigo Produtos NaturaisDocument39 pagesArtigo Produtos NaturaisMillygoNo ratings yet
- Antimicrobial Stewardship HandbookDocument65 pagesAntimicrobial Stewardship HandbookHhaNo ratings yet
- Guoying Wang, Guo ZhaoDocument17 pagesGuoying Wang, Guo ZhaoHQ HQNo ratings yet
- Diabetic Foot Infections: by Scott Bergman, Pharm.D., BCPS-AQ ID and Punit J. Shah, Pharm.D., BCPSDocument20 pagesDiabetic Foot Infections: by Scott Bergman, Pharm.D., BCPS-AQ ID and Punit J. Shah, Pharm.D., BCPSPrashant LokhandeNo ratings yet
- Antimicrobial Agents and Chemotherapy-2016-Oshima-e02056-16.fullDocument9 pagesAntimicrobial Agents and Chemotherapy-2016-Oshima-e02056-16.fullI Made AryanaNo ratings yet
- Tetracycline's: Jagir R. Patel Asst Prof Dept. Pharmacology Anand Pharmacy CollegeDocument21 pagesTetracycline's: Jagir R. Patel Asst Prof Dept. Pharmacology Anand Pharmacy CollegeJagirNo ratings yet
- Antibiotik StewardshipDocument13 pagesAntibiotik StewardshipSeptiandry Ade PutraNo ratings yet
- Antifungal Agents: LipopeptidesDocument8 pagesAntifungal Agents: LipopeptidesCristian QuitoNo ratings yet
- Newer Antibiotics: Guide: DR Saroja A ODocument51 pagesNewer Antibiotics: Guide: DR Saroja A OparahulNo ratings yet
- Chapter 043Document6 pagesChapter 043borisdevic223No ratings yet
- Antibiotic Study Cheat Sheet August 2019Document1 pageAntibiotic Study Cheat Sheet August 2019Ryan TurnerNo ratings yet
- Drug Bug TableDocument1 pageDrug Bug TableLes SangaNo ratings yet
- Yovita - The Role of Clinical Pharmacist On Safe Administration AntibioticDocument48 pagesYovita - The Role of Clinical Pharmacist On Safe Administration AntibioticRois HasyimNo ratings yet
- Tigecycline Antibacterial Activity, Clinical Effectiveness, and Mechanisms and Epidemiology of ResistanceDocument20 pagesTigecycline Antibacterial Activity, Clinical Effectiveness, and Mechanisms and Epidemiology of ResistanceDanielle pfizerNo ratings yet
- Gram-Negative Bacteria: Antibiogram of Bacteria - Year 2020 (Icu at Kfafh)Document2 pagesGram-Negative Bacteria: Antibiogram of Bacteria - Year 2020 (Icu at Kfafh)jen nalusNo ratings yet
- Journal of Infection and Public HealthDocument3 pagesJournal of Infection and Public Healthtasneem abdallahNo ratings yet
- PKLI Microbiology Lab Report Shows Acinetobacter baumannii IsolatedDocument1 pagePKLI Microbiology Lab Report Shows Acinetobacter baumannii IsolatedWaqas SaleemNo ratings yet
- IDSA Guideline PDFDocument80 pagesIDSA Guideline PDFArifHidayatNo ratings yet
- Basic Clinical Pharmacology 14th Edition McGraw Hill Education Bertram G. Katzung 2017 829 847Document19 pagesBasic Clinical Pharmacology 14th Edition McGraw Hill Education Bertram G. Katzung 2017 829 847Faye Kashmier Embestro NamoroNo ratings yet
- Discromii 1Document4 pagesDiscromii 1defineyoung5No ratings yet