Professional Documents
Culture Documents
J. Antimicrob. Chemother. 2013 Nordmann 487 9
Uploaded by
Thelma Cecilia Arce LaurelCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
J. Antimicrob. Chemother. 2013 Nordmann 487 9
Uploaded by
Thelma Cecilia Arce LaurelCopyright:
Available Formats
J Antimicrob Chemother 2013; 68: 487 489
doi:10.1093/jac/dks426 Advance Access publication 26 October 2012
Strategies for identification of carbapenemase-producing
Enterobacteriaceae
Patrice Nordmann* and Laurent Poirel
Service de Bacteriologie-Virologie, INSERM U914 Emerging Resistance to Antibiotics, Hopital de Bicetre, Assistance Publique/Hopitaux
de Paris, Faculte de Medecine et Universite Paris-Sud, K.-Bicetre, France
*Corresponding author. Service de Bacteriologie-Virologie-Hygie`ne, Hopital de Bicetre, 78 rue de General Leclerc, 94275 Le Kremlin-Bicetre Cedex,
France. Tel: +33-1-45-21-36-32; Fax: +33-1-45-21-63-40; E-mail: nordmann.patrice@bct.aphp.fr
Keywords: antibiotics, carbapenems, b-lactams, resistance, Gram-negatives
Introduction
Multidrug resistance is now emerging increasingly in Enterobacteriaceae among nosocomial and community-acquired infections. One of the most important emerging resistance traits
corresponds to the production of the carbapenem-hydrolysing
b-lactamases, which confer resistance to almost all
b-lactams.1 Their current and extensive worldwide spread in
Enterobacteriaceae is an important source of concern since
these carbapenemases are, in most cases, combined with
non-b-lactam resistance mechanisms, therefore leading to
multidrug-resistant isolates.1 The high rate of transmissibility of
the carbapenemase genes, which are mostly located on selfconjugative plasmids carrying other resistance determinants,
explains the need to rapidly identify the carbapenemase producers in order to guide antibiotic therapy but also to prevent the
development of outbreaks.
Categories of carbapenemases and their
properties
Carbapenemases in Enterobacteriaceae are currently mostly of
the KPC, VIM, IMP, NDM and OXA-48 types, and their detailed
properties have been extensively reported.1 KPC enzymes hydrolyse all b-lactams (although they hydrolyse cephamycins at a
low level) and their activity is only inhibited partially in vitro
by clavulanic acid, tazobactam and boronic acid. The
metallo-b-lactamases (MBLs; IMP, VIM and NDM) hydrolyse all
b-lactams except aztreonam and their activity is not affected
by any of the inhibitors that are in clinical use, but they can be
inhibited in vitro with compounds such as zinc chelators (EDTA,
for example). The OXA-48-type enzymes hydrolyse aminopenicillins, ureidopenicillins and carbapenems at low levels, but do not
significantly hydrolyse broad-spectrum cephalosporins.1,2 Their
activity is not affected by the inhibitors in clinical use, but they
are inhibited by NaCl in vitro.2
Susceptibility breakpoints and the debate
around detection
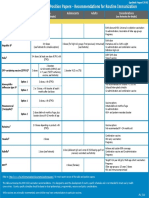
Both the US and European (EUCAST) breakpoints for carbapenems have been lowered recently to permit better recognition
of carbapenem-resistant isolates.3,4 The detection of carbapenemase producers in clinical specimens is based first on the analysis of susceptibility testing. According to the US guidelines
(CLSI) updated in 2012,3 the breakpoints for imipenem and
meropenem are susceptible (S) 1 and resistant (R) 4 mg/L,
and for ertapenem S 0.5 and R 2 mg/L. Ertapenem seems
to be a good candidate for detecting most of the carbapenemase producers since MIC values of ertapenem are usually
higher than those of other carbapenems.2 However, detection
of carbapenemase producers based only on MIC values may
lack sensitivity. According to the CLSI and EUCAST guidelines,
breakpoints have to be considered only when reporting susceptibility or resistance to carbapenems.3,4 Special tests for carbapenemase detection are suggested for epidemiology and infection
control issues only.3,4
# The Author 2012. Published by Oxford University Press on behalf of the British Society for Antimicrobial Chemotherapy. All rights reserved.
For Permissions, please e-mail: journals.permissions@oup.com
487
Downloaded from http://jac.oxfordjournals.org/ by guest on January 4, 2017
The spread of carbapenem-hydrolysing b-lactamases in Enterobacteriaceae is becoming a major public health
issue. These b-lactamases hydrolyse almost all b-lactams, are plasmid-encoded and are easily transferable
among enterobacterial species. They are found in multidrug-resistant isolates. Detection of these isolates
from infected specimens first relies on careful recognition of any decreased susceptibility to carbapenems.
After this, rapid biochemical identification of carbapenemase producers using the novel Carba NP test should
be performed. Subsequently, molecular techniques can be used to identify carbapenemase genes if necessary
(epidemiology). Detection of carriers relies on a preliminary screening step, with stools or rectal swabs being
screened on selective culture media such as SUPERCARBA medium, which posseses the broadest spectrum
for detecting any type of carbapenemase producer.
Leading article
We actually disagree with these guidelines, for the following reasons: (i) susceptibility to carbapenems is observed for
several carbapenemase producers; and (ii) there is a paucity of
clinical successes of carbapenem-containing regimens for treating infections due to carbapenemase producers that are susceptible to carbapenems in vitro.1,2 Based on our own experience, we
propose that, as a minimum, detection of carbapenemase activity should be performed on enterobacterial isolates exhibiting
MIC values of ertapenem 0.5 mg/L or of imipenem or meropenem 1 mg/L, and also on any enterobacterial isolate that exhibits even a slight decrease in susceptibility to carbapenems
compared with a wild-type phenotype. This detection will be
useful for treating patients and for preventing nosocomial outbreaks
of carbapenemase producers (and therefore multidrug-resistant
isolates), whatever the carbapenem resistance level is.
A series of non-molecular tests have been proposed for detection of
carbapenemase activity.2 Some have good specificity and sensitivity, but none of them approaches 100%. The modified Hodge test
(MHT), based on in vivo production of a carbapenemase, has been
used for years.3 Addition of zinc to the culture medium has been
shown to improve the sensitivity of this test.5 However, we believe
that this technique is time-consuming and shall be discarded. In
addition, MHT may lack sensitivity for detecting carbapenemase activity in Enterobacter spp. The added value of the inhibition-based
carbapenemase detection tests remains variable.2 These tests
are, for example, based on inhibition by tazobactam, clavulanic
acid or boronic acid for detecting the production of Ambler class A
carbapenemases (KPC), and inhibition by EDTA or dipicolinic acid
for detection of MBL activity. They are time-consuming and have
variable sensitivity and specificity. In addition, they require trained
microbiologists. High-level resistance to temocillin has been suggested to be predictive of production of OXA-48, but the specificity
of this feature remains to be more extensively evaluated.2
Detection of carbapenemase activity can be done using a UV
spectrophotometer, which is available in many microbiology laboratories. It is based on several steps, including: (i) an 18 h
culture (which can be shortened in some cases to 8 h); (ii) a
protein extraction step; and (iii) measurement of imipenem hydrolysis using a UV spectrophotometer.6 We have shown that
this spectrophotometry-based technique has 100% sensitivity
and 98.5% specificity for detecting any kind of carbapenemase activity.6 This cheap technique can accurately differentiate carbapenemase producers from non-carbapenemase producers among
carbapenem-non-susceptible isolates [outer membrane permeability defect, overproduction of cephalosporinases or/and
extended-spectrum b-lactamases (ESBLs)]. It can be implemented in any reference laboratory, but this technique still requires
time. Recently, the use of mass spectrometry for detection of carbapenemase activity has been proposed, based on the analysis of
the degradation of a carbapenem molecule.7,8 Although this technique has to be further evaluated, matrix-assisted laser desorption
ionization time-of-flight mass spectrometry (MALDI-TOF) equipment is increasingly used in the diagnostic bacteriology laboratory.
The most important and recent development for the accurate
identification of carbapenemase-producing Enterobacteriaceae
488
Molecular tests for carbapenemase genes
Molecular techniques remain the gold standard for the precise
identification of carbapenemase genes.2 Most of these techniques
are based on PCR and may be followed by a sequencing step if a
precise identification of the carbapenemase gene is needed (e.g.
VIM type, KPC type, NDM type or OXA-48 type).10,11 They are
either single or multiplex PCR techniques. A PCR technique performed directly on colonies can give results within 4 6 h (or less
when using real-time PCR technology) with excellent sensitivity
and specificity. Similarly, other molecular techniques are useful
for this purpose.12 The main disadvantages of the molecularbased technologies are their cost, the requirement for trained
microbiologists and the inability to detect novel unidentified
genes. Sequencing of the genes is interesting mostly for research
and epidemiological purposes. Precise identification of the type
of carbapenemase is not actually needed for treating patients or
for preventing outbreaks. We believe these molecular techniques
may be mostly used in reference laboratories.
Screening of colonized patients
Preventing the spread of carbapenemase producers relies on the
accurate detection of colonized patients at an early stage of hospitalization or on admission/discharge either to the hospital or to a
specific unit. Screening should include as a minimum at-risk
patients, such as those in intensive care units, transplant recipients
and the immunocompromised, and those transferred from any
foreign hospital (unknown prevalence of carbapenemase producer carriage) or from non-foreign hospitals but known to face a
high risk of carriage of carbapenemase producers.1 Geographical
regions with high prevalence of carbapenemase producers are increasingly known.1 Since the reservoir of Enterobacteriaceae is
mostly the intestinal flora, stools and rectal swabs are the most suitable specimens for performing such screening. Three screening
media are currently known, but mostly for carbapenem-resistant
rather than carbapenemase-producing organisms.
The first marketed screening medium was the CHROMagar KPC
medium, which contains a carbapenem (CHROMagar, Paris,
France).13 It detects carbapenem-resistant bacteria only if they
exhibit high-level resistance to carbapenems. Its main disadvantage therefore remains its lack of sensitivity since it does not
detect carbapenemase producers exhibiting a low level of
Downloaded from http://jac.oxfordjournals.org/ by guest on January 4, 2017
Non-molecular tests for carbapenemase
production
is the Carba NP test.9 This biochemical test, applicable to isolated
bacterial colonies, is based on in vitro hydrolysis of the carbapenem
imipenem.9 Hydrolysis of imipenem is detected by a change in the
pH value of the indicator (red to yellow/orange). This test is 100%
sensitive and specific, as are molecular techniques.9 It detects not
only all known carbapenemases (belonging to Ambler A, B and D
classes) in Enterobacteriaceae but should also identify virtually
any new emerging carbapenemase, in contrast to molecular techniques. This rapid (,2 h), user-friendly and inexpensive technique
can be implemented in any laboratory worldwide. In addition, it
does not require any specific equipment. We believe this technique
will soon become a reference technique since it fulfils the clinical
requirement of a rapid and low-cost identification method for
carbapenemase-producing Enterobacteriaceae.
JAC
Leading article
carbapenem resistance, as observed for several MBL or OXA-48 producers.1 The second screening medium also contains a carbapenem
(CRE Brilliance, Thermo Fisher Scientific, UK).14 It detects KPC and MBL
producers well, and most but not all OXA-48 producers.14,15 Finally,
one of the most recently developed screening media (SUPERCARBA)
contains cloxacillin, zinc and ertapenem.16 It shows excellent sensitivity and specificity for detection of any kind of carbapenemase producer (not only high-level carbapenem-resistant isolates).16 Compared
with the two other media, it also shows improved sensitivity and specificity for detecting all types of carbapenemase producers (including
the OXA-48 producers) when present in low amounts in stools. Once
carbapenem-resistant isolates are selected on SUPERCARBA
medium, we recommend use of the Carba NP test for detecting
carbapenemase activity. Then, if needed, molecular identification of
the carbapenemase genes may be performed.
Proposed algorithm for carbapenemase detection
We propose the following scheme for detection of carbapenemase producers in Enterobacteriaceae.
(i) Infecting strains: Carba NP test on isolated colonies with
decreased susceptibility to carbapenems. If positive, molecular
identification of the genes, mainly for epidemiological reasons.
(ii) Screening of carriers: screening of carbapenem-resistant
isolates using e.g. SUPERCARBA medium, followed by the Carba
NP test to be performed on selected colonies. If the latter test
is positive, molecular identification of the genes, mainly for
epidemiological reasons.
The proposed scheme for detection of carbapenemase producers presents several advantages. It will lead to rapid identification of carbapenemase producers, allowing adequate antibiotic
stewardship. This is of the utmost importance due to the
current shortage of novel antibiotics. It will prevent the development of nosocomial outbreaks due to the multidrug-resistant
bacteria that represent one of the most worrisome medical
threats. The Israeli experience with containment of the KPC outbreaks has demonstrated the possibility of obtaining frank
success by acting rapidly, and on a large scale.17 This strategy,
based on broad and rapid detection of carbapenemase producers, may also have a significant impact in preventing their
spread in the community. Finally, the first proposed steps
(screening, susceptibility testing and Carba NP test), excluding
the molecular techniques (needed for epidemiological purposes),
can be implemented immediately in any laboratory worldwide,
since they are based on inexpensive and affordable techniques.
References
1 Nordmann P, Naas T, Poirel L. Global spread of carbapenemase-producing
Enterobacteriaceae. Emerg Infect Dis 2011; 17: 17918.
2 Nordmann P, Gniadkowski M, Giske CG et al. Identification and
screening of carbapenemase-producing Enterobacteriacae. Clin
Microbiol Infect 2012; 18: 432 8.
3 Clinical and Laboratory Standards Institute. Performance Standards for
Antimicrobial Susceptibility Testing: Twenty-first Informational Supplement
M100-S21. CLSI, Wayne, PA, USA, 2012.
4 Leclercq R, Canton R, Brown DF et al. EUCAST expert rules in
antimicrobial susceptibility testing. Clin Microbiol Infect 2011;
doi:10.1111/j.1469-0691.2011.03703.x
5 Girlich D, Poirel L, Nordmann P. Value of the modified Hodge test for
detection of emerging carbapenemases in Enterobacteriacae. J Clin
Microbiol 2012; 50: 477 9.
6 Bernabeu S, Poirel L, Nordmann P. Spectrophotometry-based detection
of carbapenemase producers in Enterobacteriaceae. Diagn Microbiol
Infect Dis 2012; 74: 88 90.
7 Burckhardt I, Zimmermann S. Using matrix-assisted laser desorption
ionization-time of flight mass spectrometry to detect carbapenem
resistance within 1 to 2.5 hours. J Clin Microbiol 2011; 49: 3321 4.
8 Hrabak J, Walkova R, Studentova V et al. Carbapenemase activity
detection by matrix-assisted laser desorption ionization-time of flight
mass spectrometry. J Clin Microbiol 2011; 49: 3327 32.
9 Nordmann P, Poirel L, Dortet L. Rapid detection of carbapenemaseproducing Enterobacteriaceae. Emerg Infect Dis 2012; 18: 15037.
10 Poirel L, Walsh TR, Cuvillier V et al. Multiplex PCR for detection of acquired
carbapenemase genes. Diagn Microbiol Infect Dis 2011; 70: 11925.
11 Avlami A, Bekris S, Ganteris G et al. Detection of metallo-b-lactamase
genes in clinical specimens by a commercial multiplex PCR system.
J Microbiol Methods 2010; 83: 185 7.
12 Cuzon G, Naas T, Bogaerts P et al. Evaluation of a DNA microarray for
the rapid detection of extended-spectrum b-lactamases (TEM, SHV and
CTX-M), plasmid-mediated cephalosporinases (CMY-2-like, DHA, FOX,
ACC-1, ACT/MIR and CMY-1-like/MOX) and carbapenemases (KPC,
OXA-48, VIM, IMP and NDM). J Antimicrob Chemother 2012; 67: 1865 9.
13 Moran-Gilad J, Carmeli Y, Schwartz D et al. Laboratory evaluation of
the CHROMagar KPC medium for identification of carbapenem-nonsusceptible Enterobacteriaceae. Diagn Microbiol Infect Dis 2011; 70: 5657.
14 Withey S, Scopes E. A new screening medium for detection of
carbapenem-resistant Enterobacteriaceae. In: Abstracts of the
Twenty-first European Congress for Clinical Microbiology and Infectious
Diseases, Milan, 2011. Abstract P862. European Society for Clinical
Microbiology and Infectious Diseases, Basel, Switzerland.
This work was partially funded by grants from the INSERM (UMR914) and
the University Paris Sud, France.
15 Girlich D, Poirel L, Nordmann P. Strategy of detection of
carbapenemase-producing Enterobacteriaceae. In: Abstracts of the
Twenty-second European Congress for Clinical Microbiology and Infectious
Diseases, London, 2012. Abstract P2315. European Society for Clinical
Microbiology and Infectious Diseases, Basel, Switzerland.
Transparency declarations
16 Nordmann P, Girlich D, Poirel L. Detection of carbapenemase
producers in Enterobacteriaceae by use of a novel screening medium.
J Clin Microbiol 2012; 50: 2761 6.
Funding
This work was partially funded by grants from the Institut National de la
Sante et de la Recherche Medicale (INSERM) (UMR914). An international
patent form for the Carba NP test has been filed on behalf of INSERM
Transfert (Paris, France). P. N. and L. P. are employed by and receive
17 Schwaber MJ, Lev B, Israeli A et al. Containment of country-wide
outbreaks of carbapenem-resistant Klebsiella pneumoniae in Israeli hospitals
via a nationally implemented intervention. Clin Infect Dis 2011; 52: 84855.
489
Downloaded from http://jac.oxfordjournals.org/ by guest on January 4, 2017
Conclusion
funding from INSERM. P. N. is a director of the INSERM U914 Emerging
Resistance to Antibiotics.
You might also like
- Predictores de KPC OutcomesDocument6 pagesPredictores de KPC OutcomesThelma Cecilia Arce LaurelNo ratings yet
- In Vivo Development of Ertapenem Resistance in A Patient WitDocument4 pagesIn Vivo Development of Ertapenem Resistance in A Patient WitThelma Cecilia Arce LaurelNo ratings yet
- Carbapenemasas de LombardiDocument8 pagesCarbapenemasas de LombardiThelma Cecilia Arce LaurelNo ratings yet
- In Vivo Development of Ertapenem Resistance in A Patient WitDocument4 pagesIn Vivo Development of Ertapenem Resistance in A Patient WitThelma Cecilia Arce LaurelNo ratings yet
- Carbapenemasas de LombardiDocument8 pagesCarbapenemasas de LombardiThelma Cecilia Arce LaurelNo ratings yet
- In Vivo Development of Ertapenem Resistance in A Patient WitDocument4 pagesIn Vivo Development of Ertapenem Resistance in A Patient WitThelma Cecilia Arce LaurelNo ratings yet
- Klebsiella Panresistente YtratamientoDocument6 pagesKlebsiella Panresistente YtratamientoThelma Cecilia Arce LaurelNo ratings yet
- ARBOVIRUSDocument21 pagesARBOVIRUSThelma Cecilia Arce LaurelNo ratings yet
- F 1982 MBI Amino Acids Enhance Adaptive Behaviour of Pseudomonas Aeruginosa in TH - PDF 2737Document10 pagesF 1982 MBI Amino Acids Enhance Adaptive Behaviour of Pseudomonas Aeruginosa in TH - PDF 2737Thelma Cecilia Arce LaurelNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Church Supper Outbreak Case StudyDocument13 pagesChurch Supper Outbreak Case StudyJoseDavidSierraLugoNo ratings yet
- Isospora 1 PDFDocument9 pagesIsospora 1 PDFAdriana Horna BazánNo ratings yet
- Immunology Uworld Notes (Step 1)Document12 pagesImmunology Uworld Notes (Step 1)Burkitt's LymphomaNo ratings yet
- Quarterly Exam in MAPEH and Health for Los Baños Integrated SchoolDocument3 pagesQuarterly Exam in MAPEH and Health for Los Baños Integrated SchoolRaquel S. De CastroNo ratings yet
- Travel Medicine: Health Quarantine 2021 Dr. Esther Meylina SipahutarDocument35 pagesTravel Medicine: Health Quarantine 2021 Dr. Esther Meylina SipahutarEsther Meyline XhypaNo ratings yet
- Immunization Routine Table1Document11 pagesImmunization Routine Table1Fred C. MirandaNo ratings yet
- Nepal National Hiv Testing and Treatment Guidelines 2022Document158 pagesNepal National Hiv Testing and Treatment Guidelines 2022medical ChyNo ratings yet
- What Vaccines Do BC Adults NeedDocument2 pagesWhat Vaccines Do BC Adults NeedCatalina VisanNo ratings yet
- E Coli-PowerpointDocument29 pagesE Coli-PowerpointThrina Gynae CondezNo ratings yet
- Introduction To FungiDocument4 pagesIntroduction To Fungikep1313No ratings yet
- Glanders in HorseDocument43 pagesGlanders in HorseWerner AlbuquerqueNo ratings yet
- Mnemonic SDocument20 pagesMnemonic SViral ParekhNo ratings yet
- Powerpoint TaeniasisDocument23 pagesPowerpoint TaeniasisAyshaShariff0% (1)
- A Concept Paper: HIV: By: Nichol Niño H. BanaagDocument2 pagesA Concept Paper: HIV: By: Nichol Niño H. Banaaglhuk banaagNo ratings yet
- The Complete Guide to Colloidal SilverDocument20 pagesThe Complete Guide to Colloidal Silveracuario33100% (7)
- Textbook of Surgery For Dental Students-smile4DrDocument400 pagesTextbook of Surgery For Dental Students-smile4DrRotariu Ana Maria100% (8)
- Gram Stains and Characteristics of Major Anaerobic BacteriaDocument73 pagesGram Stains and Characteristics of Major Anaerobic BacteriaMaria ClaraNo ratings yet
- IHD stone treatmentDocument49 pagesIHD stone treatmentFitriardi SejatiNo ratings yet
- General Parasitology L2Document27 pagesGeneral Parasitology L2kayse abtidoonNo ratings yet
- Prep 2018Document970 pagesPrep 2018Dr. Faten AlKatebNo ratings yet
- Control of Communicable Diseases ManualDocument715 pagesControl of Communicable Diseases ManualChris Mahfood100% (3)
- European Patent Application of EntecavirDocument10 pagesEuropean Patent Application of Entecavirmike116No ratings yet
- Septic Shock in Children - Rapid Recognition and Initial Resuscitation (First Hour) PDFDocument18 pagesSeptic Shock in Children - Rapid Recognition and Initial Resuscitation (First Hour) PDFLilik NatasubrataNo ratings yet
- Antibiotic TableDocument5 pagesAntibiotic TableLiana Et Murat KalabalikNo ratings yet
- Food Borne DiseasesDocument12 pagesFood Borne DiseasesEngr AliNo ratings yet
- gtbr14 Main Text PDFDocument134 pagesgtbr14 Main Text PDFAnonymous fqa7PO8oNo ratings yet
- Critical Review SampleDocument3 pagesCritical Review SampleAhmad Muammar100% (1)
- Quiz 3 - ProtistaDocument3 pagesQuiz 3 - ProtistaDon King Evangelista0% (1)
- New AntibioticsDocument219 pagesNew Antibioticslilian_armstrong8401No ratings yet
- Book 1Document166 pagesBook 1Puput HepitasariNo ratings yet