Professional Documents
Culture Documents
Klebsiella Panresistente Ytratamiento
Uploaded by
Thelma Cecilia Arce LaurelOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Klebsiella Panresistente Ytratamiento
Uploaded by
Thelma Cecilia Arce LaurelCopyright:
Available Formats
CHALLENGING CLINICAL CASE IN ANTIMICROBIAL RESISTANCE
Successful Treatment of Carbapenemase-Producing Pandrug-Resistant
Klebsiella pneumoniae Bacteremia
Jose F. Camargo,a Jacques Simkins,a Thiago Beduschi,b Akin Tekin,b Laura Aragon,c Armando Prez-Cardona,d Clara E. Prado,e
Michele I. Morris,a Lilian M. Abboa
Rafael Cantn (Commentator)f,g
This Journal section presents a real, challenging case involving a multidrug-resistant organism. The case authors present the rationale for
their therapeutic strategy and discuss the impact of mechanisms of resistance on clinical outcome. An expert clinician then provides a commentary on the case.
New antibiotic options are urgently needed for the treatment of carbapenem-resistant Enterobacteriaceae infections. We report a
64-year-old female with prolonged hospitalization following an intestinal transplant who developed refractory bacteremia due
to a serine carbapenemase-producing pandrug-resistant isolate of Klebsiella pneumoniae. After failing multiple antimicrobial
regimens, the patient was successfully treated.
CASE PRESENTATION
A 64-year-old female with a history of diabetes mellitus developed
Clostridium difficile colitis with toxic megacolon requiring total
colectomy. As a complication of the total colectomy, she had a
volvulus requiring extensive resection of necrotic small bowel
with resultant total parenteral nutrition-dependent short bowel
syndrome (only 15 cm of small bowel left). The patient was referred to our institution for an intestinal transplant. Induction
immunosuppression consisted of antithymocyte globulin at 2
mg/kg of body weight intravenously (i.v.) (5 doses), methylprednisolone at 500 mg i.v. every 24 h (q24h) (4 doses, followed by a
slow taper over the first 2 weeks), and rituximab at 150 mg/m2 i.v.
(1 dose). Maintenance immunosuppression consisted of basiliximab at 40 mg i.v. every 4 weeks for the first 3 months, tacrolimus,
and low-dose prednisone. The antimicrobial prophylaxis regimen
consisted of ganciclovir (5 mg/kg i.v. q12h for 2 weeks, followed by
valganciclovir at 900 mg per os [p.o.] daily) and trimethoprimsulfamethoxazole (80/400 mg p.o. three times a week) for cytomegalovirus and Pneumocystis jirovecii pneumonia prophylaxis,
respectively. No multidrug-resistant organisms were identified by
rectal and nasal surveillance cultures at the time of the transplant.
The early posttransplant course was complicated by an intraabdominal hematoma on postoperative day 1, which required
emergent surgical exploration and evacuation. Abdominal wound
closure was performed on postoperative day 8. On postoperative
day 12, the patient required another surgical exploration with intraoperative findings of pancreatitis with a small peripancreatic
collection. Cultures from this collection obtained in the operating
room yielded a heavy growth of Klebsiella pneumoniae. A Hodge
test was positive, indicating carbapenemase production. The presence of the Klebsiella pneumoniae carbapenemase (KPC) gene was
confirmed using the Verigene (Nanosphere, Inc., Northbrook, IL)
Gram-negative blood culture nucleic acid test. The class B
(IMP-type metallo--lactamase, New Delhi metallo--lacta-
October 2015 Volume 59 Number 10
mase [NDM], and Verona integron-encoded metallo--lactamase [VIM]) and class D (oxacillinase [OXA]-type) carbapenemase genes were not detected. The isolate was resistant to
aminoglycosides but susceptible to tigecycline (MIC, 0.38 g/ml)
and colistin (MIC, 0.19 g/ml). The patient was started on a combination of tigecycline (1 dose of 100 mg i.v., followed by 50 mg
i.v. q12h) and colistin (2.5 mg i.v. q12h) and completed a 14-day
course for complicated intra-abdominal infection (cIAI) due to
carbapenem-resistant Klebsiella pneumoniae (CRKP). The patients subsequent hospital course was complicated by renal failure, requiring hemodialysis and chronic ventilator-dependent respiratory failure. On postoperative day 36, the patient developed
fever and hypotension and was noted to have copious respiratory
secretions. Bronchoalveolar lavage fluid grew CRKP at 104
CFU/ml; the isolate was now resistant to tigecycline (MIC, 256
g/ml) but susceptible to colistin (MIC, 1 g/ml). The patient was
started on a combination of colistin (2.5 mg i.v. q24h) and extended-infusion meropenem (500 mg i.v. q24h), with the dose based
on renal clearance, for ventilator-associated pneumonia due to
CRKP with a good clinical response.
On postoperative day 65, the patient developed recurrent fever
and leukocytosis and was found to have CRKP bacteremia. Since
the bloodstream infection (BSI) was suspected to be catheter re-
Citation Camargo JF, Simkins J, Beduschi T, Tekin A, Aragon L, Prez-Cardona A,
Prado CE, Morris MI, Abbo LM, Cantn R (Commentator). 2015. Successful
treatment of carbapenemase-producing pandrug-resistant Klebsiella pneumoniae
bacteremia. Antimicrob Agents Chemother 59:59035908.
doi:10.1128/AAC.00655-15.
Address correspondence to Jose F. Camargo (case author), jfc31@med.miami.edu,
or Rafael Cantn (Commentator), rafael.canton@salud.madrid.org.
Copyright 2015, American Society for Microbiology. All Rights Reserved.
doi:10.1128/AAC.00655-15
Antimicrobial Agents and Chemotherapy
aac.asm.org
5903
Downloaded from http://aac.asm.org/ on November 11, 2015 by guest
Department of Medicine, Division of Infectious Diseases, University of Miami Miller School of Medicine, Miami, Florida, USAa; Miami Transplant Institute and Department
of Surgery, University of Miami Miller School of Medicine, Miami, Florida, USAb; Department of Pharmacy, Jackson Memorial Hospital, Miami, Florida, USAc; Department of
Microbiology, Jackson Memorial Hospital, Miami, Florida, USAd; Department of Microbiology, University of Miami, Miami, Florida, USAe; Servicio de Microbiologa, Hospital
Universitario Ramn y Cajal and Instituto Ramn y Cajal de Investigacin Sanitaria (IRYCIS), Madrid, Spainf; Red Espaola de Investigacin en Patologa Infecciosa (REIPI),
Madrid, Spaing
Challenging Clinical Case
lated, all of the patients central venous catheters were changed in
a timely fashion. CRKP was also isolated from the urine at 105
CFU/ml as well as from the central venous catheter tip (102
CFU/ml). Despite previous courses of colistin, the CRKP isolate
remained susceptible (MIC, 0.5 g/ml). The patient was started
on a renal clearance-based dose of colistin (1.25 mg/kg i.v. q12h),
tigecycline (50 mg i.v. q12h), and extended-infusion meropenem
(1 g i.v. q12h). Although she was hemodynamically stable, her
blood cultures remained positive for more than 6 days despite this
combination of antibiotics.
CHALLENGE QUESTION
TREATMENT AND OUTCOME
Mortality rates for cases of CRKP bacteremia exceed 50% (1, 2).
Combination antimicrobial therapy yields the best outcomes (3),
but treatment options are limited. The two main antibiotic options available for CRKP infection are colistin and tigecycline,
both of which have suboptimal efficacy and toxicity profiles.
Colistin remains the most active agent against CRKP, but its tolerability is limited due to common and serious nephrotoxicity and
neurotoxicity. Tigecycline is usually not recommended for the
treatment of BSI in critically ill patients because it does not achieve
adequate serum levels (4) and higher mortality rates associated
with the use of tigecycline have been reported (5). In addition, the
emergence of CRKP strains resistant to colistin and tigecycline is
increasingly reported (1). Intravenous fosfomycin has been used
in Europe for the treatment of CRKP infections with promising
results and a low incidence of adverse events (2, 6). Unfortunately,
intravenous fosfomycin is not currently available in the United
States. In addition, the relatively quick emergence of resistance
during therapy, particularly among immunocompromised hosts,
is a major limitation of fosfomycin (6).
Ceftazidime-avibactam (CAZ-AVI; AstraZeneca/Forest Laboratories) was until recently an investigational antimicrobial but
has now been approved by the U.S. Food and Drug Administration
(FDA) for the treatment of adult patients with cIAI (in combination
with metronidazole) and complicated urinary tract infections (cUTI)
(http://www.fda.gov/newsevents/newsroom/pressannouncements
/ucm435629.htm). CAZ-AVI consists of a combination of ceftazidime and the novel non--lactam -lactamase inhibitor avibactam. The addition of avibactam greatly improves the activity
of ceftazidime against most species of Enterobacteriaceae (4- to
1,024-fold reduction in MIC) (7), including ceftazidime-nonsusceptible pathogens. CAZ-AVI demonstrates in vitro activity
against extended-spectrum -lactamase (ESBL) and KPC but not
metallo--lactamase (e.g., VIM, NDM, IMP) producers. In an in
vitro study of 1,466 Gram-negative bacterial isolates collected
from hospitalized patients in the United States during 2012, a total
of 99.8% of Enterobacteriaceae isolates from patients with BSI,
99.4% from pneumonia patients, and 100% from patients with
IAI and UTI exhibited a CAZ-AVI MIC of 4 g/ml, which is the
Clinical and Laboratory Standards Institute (CLSI) susceptible
5904
aac.asm.org
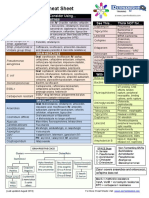
FIG 1 Ceftazidime-avibactam (CAZ-AVI) and carbapenem disc diffusion
susceptibility testing of the pandrug-resistant isolate of CRKP in a MuellerHinton agar. On the left side of the plate are the discs of ertapenem, meropenem, and imipenem (top to bottom) with no zones of inhibition. On the
right side of the plate is the CAZ-AVI disc alone with a zone of 26 mm. In the
center are three sets of discs of ertapenem, meropenem, and imipenem (top to
bottom) alongside CAZ-AVI. Note that there is an enhancement in the zone of
inhibition in each set of discs compared to that of CAZ-AVI alone, indicating
a possible synergistic effect of these drug combinations.
breakpoint for ceftazidime when tested alone against Enterobacteriaceae (8). In phase 2 clinical trials, CAZ-AVI has been proved to
be safe and effective in the treatment of cUTI as well cIAI (in
combination with metronidazole) (9, 10). Phase 3 clinical trials of
CAZ-AVI in patients with cUTI (NCT01595438) and cIAI
(NCT01499290, NCT01726023, and NCT01500239) were recently
completed, and phase 3 studies in patients with nosocomial pneumonia (NCT01808092) are ongoing (https://clinicaltrials.gov). The efficacy of CAZ-AVI in the treatment of BSI has not been established.
The addition of fosfomycin was considered for our patient, but
her isolate was resistant (MIC, 64 g/ml). Based on previous reports suggesting the efficacy of double-carbapenem regimens for
carbapenemase-producing multidrug-resistant Klebsiella pneumoniae (11, 12), the patient was switched to a combination of
colistin (1.25 mg/kg i.v. q12h), meropenem (1 g i.v. q12h), and
ertapenem (1 g i.v. q24h), adjusted to renal function. She initially
responded to this regimen but developed breakthrough bacteremia 12 days later. The isolate had now become resistant to colistin
(MIC, 12 g/ml). At this point, an emergency investigational new
drug application (EIND no. 125649) was obtained from the FDA
to administer CAZ-AVI to our patient with refractory CRKP bacteremia. The medication was kindly provided by AstraZeneca/
Forest Laboratories after a compassionate use request. This singlepatient protocol was also approved by our local institutional
review board, and the patient provided written informed consent.
Antimicrobial Agents and Chemotherapy
October 2015 Volume 59 Number 10
Downloaded from http://aac.asm.org/ on November 11, 2015 by guest
Assuming that adequate source control has been achieved, the
addition of which of the following therapeutic options is more
appropriate for this patient?
A. Intravenous fosfomycin
B. Dual-carbapenem therapy
C. Ceftazidime-avibactam
D. Other
Challenging Clinical Case
COMMENTARY
Carbapenemases are increasingly recognized worldwide. They are
particularly prevalent in Klebsiella pneumoniae from several geographic areas, including the Indian subcontinent and the Mediterranean countries (13). In addition, the Centers for Disease
Control and Prevention (CDC) noted their increase in the United
States and advised on potential measures to avoid their spread
(14). What is worrying is that these enzymes are being increasingly
detected in Escherichia coli, which indicates an efficient transference of carbapenemase genes among Enterobacteriaceae (13). As
previously seen with extended-spectrum -lactamases, patients
colonized with carbapenemase-producing Enterobacteriaceae
(CPE) are at risk of infection due to these organisms (15). Treatment of infected patients with CPE is always problematic due to
their multidrug and pan-drug resistance phenotype, and several
therapeutic options have been considered. The best alternative is
always a combined therapy in which, surprisingly, one of the drugs
is always a carbapenem (16, 17). The most appropriate is meropenem, which should be administered at high doses (2 g/8 h) with
an extended infusion (up to 3 h) to enhance its pharmacokinetic
and pharmacodynamic properties (18). With this approach and
despite hydrolysis of carbapenems by the carbapenemase enzyme,
these compounds maintain their bactericidal effect. This has been
demonstrated both in in vitro and in animal models (17, 19, 20).
Bactericidal activity decreases with the increase of the MIC and is
observed only in isolates for which the MICs are up to 8 to 16
g/ml. These data reinforce carbapenem-resistance clinical
breakpoints established by CLSI and EUCAST (7, 21). The agents
that are combined with meropenem must be active in vitro and
include colistin, tigecycline, fosfomycin, aminoglycosides, fluoroquinolones, and even nitrofurantoin in urinary tract infections, all
of them with variable results (16, 17). High carbapenem MICs
(e.g., meropenem MIC of 8 g/ml) and resistance to the other
compounds have made some of these combinations ineffective
(16, 17). With this scenario, new antimicrobial agents that are
active against CPE are urgently needed.
Ceftazidime-avibactam (CAZ-AVI) has been recently approved by the U.S. Food and Drug Administration (FDA) to treat
adults with complicated intra-abdominal infections, in combina-
October 2015 Volume 59 Number 10
tion with metronidazole, and complicated urinary tract infections, including pyelonephritis, who have limited or no treatment
options (7). Avibactam is a synthetic non--lactam -lactamase
inhibitor that inhibits the activities of Ambler class A and C -lactamases and some Ambler class D enzymes, including KPC carbapenemases, AmpC, and OXA-48-like carbapenemases, respectively. However, it does not inhibit metallo--lactamases, such us
VIM or NDM variants.
In the case presentation above, Camargo et al. have described
the treatment of a patient with a bacteremia due to a KPC-producing K. pneumoniae isolate that was susceptible only to colistin
and tigecycline. Different antibiotic combination regimens were
subsequently administered, including double or triple therapy
with tigecycline (1 dose of 100 mg i.v. followed by 50 mg i.v. q12h),
colistin (2.5 mg i.v. q24h), and extended-infusion of meropenem
(0.5 to 1 g i.v. q24h), all adjusted for impaired renal function. Due
to refractory bacteremia and previous reports suggesting efficacy
of a double-carbapenem regimen for carbapenemase-producing
K. pneumoniae infections, the patient was treated with colistin
(1.25 mg i.v. q24h), meropenem (1 g i.v. q24h), and ertapenem (1
g i.v. q24h). The emergence of colistin resistance, a situation not
infrequently observed in KPC-producing K. pneumoniae isolates,
was noted, and the patient was switched to a combination of CAZAVI (1 g/250 mg i.v. q8h) and ertapenem (1 g i.v. q24). The use of
CAZ-AVI in a patient with bacteremia, an indication that is not
included in the FDA prescribing information for this product, has
not been previously reported, unlike the association of different
carbapenems (Table 2).
Double-carbapenem therapy was initially explored in animal
models and later used in patients infected with CPE (Table 2).
Although the rationale for this combination has not been extensively explored, it is hypothesized that one of the carbapenem
compounds distracts the carbapenemase enzyme acting as a suicide inhibitor, thus allowing and preserving the other carbapenems activity. This could be a situation similar to the classical treatment with an amoxicillin-clavulanate combination. Clavulanate
preserves the activity of amoxicillin, as the inhibited -lactamase
has higher affinity for the clavulanate than for the amoxicillin; the
clavulanate is hydrolyzed (suicide inhibitor), and the amoxicillin
is able to act (22). An alternate hypothesis is that there is an initial
reduction in bacterial density by one of the compounds, thus facilitating the activity of the other carbapenem against a reduced
inoculum (23).
Double-carbapenem therapy was tested in chemostat experiments and in an immunocompetent-mouse thigh infection with a
TABLE 1 Recommended doses of ceftazidime and avibactam
Estimated CLCR
(ml/min/1.73 m)a
Ceftazidime and avibactam doses and intervalc
50
5031
3016
156
6b
2,000 mg ceftazidime and 500 mg avibactam q8h
1,000 mg ceftazidime and 250 mg avibactam q8h
750 mg ceftazidime and 187.5 mg avibactam q12h
750 mg ceftazidime and 187.5 mg avibactam q24h
750 mg ceftazidime and 187.5 mg avibactam q48h
Estimated creatinine clearance (CLCR) as determined by using the most recent serum
creatinine value, the patients most recent actual (not ideal) body weight, and the
Cockcroft-Gault formula (30).
b
Both ceftazidime and avibactam are hemodialyzable; thus, ceftazidime-avibactam
should be administered after hemodialysis on hemodialysis days.
c
Given over 120 min at a constant rate of infusion.
Antimicrobial Agents and Chemotherapy
aac.asm.org
5905
Downloaded from http://aac.asm.org/ on November 11, 2015 by guest
Disc diffusion susceptibility testing revealed in vitro susceptibility
of the tigecycline-colistin-fosfomycin-resistant isolate of CRKP to
CAZ-AVI (zone diameter, 26 mm) and a possible synergistic effect
of CAZ-AVI with all the carbapenems tested (Fig. 1). Treatment
with a combination of intravenous CAZ-AVI (1,000 mg/250 mg
i.v. q8h based on the recommended dose determined by creatinine
clearance [Table 1]) and ertapenem (1 g i.v. q24h) was then
started. The patient responded well, with sterilization of her blood
cultures within 24 h of this regimen. She completed a course of 2
weeks and by the end of therapy, for the first time since her admission, was transferred out of the intensive care unit. No adverse
events developed during therapy.
To the best of our knowledge, this is the first report of successful treatment of pandrug-resistant CRKP bacteremia with a CAZAVI-containing regimen. Although larger studies are needed to
establish the role of CAZ-AVI in the treatment of BSI due to
CRKP, this report suggests that the combination of CAZ-AVI with
ertapenem is a novel, safe, and effective antibiotic option for the
treatment of serious infections with CRKP in critically ill patients
who have limited or no alternative treatment options.
aac.asm.org
Antimicrobial Agents and Chemotherapy
October 2015 Volume 59 Number 10
Urine
Spinal cord injury
Blood, sputum,
abdominal wound
Abdominal wound,
blood, urine, CVC
Intestinal transplant
Blood, CVC
Hip joint
replacement
Adenocarcinoma and
hepatocarcinoma
Blood
Renal hematoma
Sputum
Blood
Left lower limb
revascularization
Necrotizing
pancreatitis
Blood
Aortic prosthesis
replacement
Blood, endotracheal
aspirate
Blood, urine
Subarachnoid
hemorrhage
Cerebral hemorrhage
Blood, urine, CVC
Spinal cord injury
Clinical sample(s)
KPC-producing
K. pneumoniae
KPC-producing
K. pneumoniae
KPC-producing
K. pneumoniae
Carbapenemaseproducing K.
pneumoniae
Carbapenemaseproducing K.
pneumoniae
Carbapenemaseproducing K.
pneumoniae
Pan-drugresistant K.
pneumoniae
KPC-3-producing
K. pneumoniae
KPC-2-producing
K. pneumoniae
KPC-2-producing
K. pneumoniae
KPC-2-producing
K. pneumoniae
Microorganism
12-day treatment. Microbiological eradication
after 1-day treatment. Clinical recovery but
death due to heart failure 1 mo after end of
treatment.
ERT (1 g q24h i.v.) MER (2 g
q8h i.v.)
ERT (0.5 g q24h i.v.) MER (1
g q12h i.v.)
ERT (1 g q24h i.v.) MER (2 g
q8h i.v.)
ERT (1 g q24h i.v.) MER (2 g
q8h i.v., 4-h infusion) CST
(6 MU loading dose, 4.5 MU
q12h)
ERT (1 g q24h i.v.) DOR (1 g
q8h i.v., 4-h infusion, 2 h
after ERT) POL-B
(750,000 U q12h i.v.) CST
(inhaled 2 MU q8h)
ERT (0.5 g q24h i.v.) DOR
(0.5 g q8h i.v., 2 h after ERT)
POL-B (750,000 U q12h
i.v.)
ERT, 128; MER, 256; CST, 16
ERT, 256; MER, 256; CST, 16
ERT, 256; MER, 128; CST, 16
ERT, 128; MER, 256; CST, 32
ERT R, MER R, IMI R; CST,
0.191; CAZ-AVI, 4
ERT, 32; MER, 32; IMI,
32; CST (not determined)
ERT (1 g q24h i.v.) MER (1 g
q12h, 2 h after ERT) CST
(750,000 U q12h)
21-day treatment (7 days with CST). Sterile
blood and urine cultures after 4 days of
treatment.
ERT (0.51 g q24h i.v.) DOR
(0.251 g q8h i.v., 4-h
infusion)
ERT, 256512; MER, 64; DOR,
3264; CST, 1631
ERT, 4; MER, 16; DOR, 8; POLB, 1
MER adjusted to renal function. Microbiological
eradication after 48 h of treatment. Death due
to heart failure after 4 days of treatment.
24-day treatment. Clinical recovery.
ERT (1 g q24h i.v.) MER (2 g
q8h i.v., 3-h infusion, 1 h
after ERT)
ERT, 8; MER, 32; DOR, 8;
CST, 16
12-day treatment (adjusted to renal function).
Initial response but breakthrough bacteremia
after 12 days of treatment. CST resistance
development (MIC, 12 g/ml).
10-day treatment. Microbiological eradication in
sputum and abdominal wound after 5 days of
treatment. Relapse 10 days after end of
treatment in blood cultures but not in sputum
sample
21-day treatment. Recovered after treatment.
21-day treatment. Bacteremia cleared after 8-day
of treatment. ERT and DOR doses were
adjusted during treatment to renal clearance.
No relapse 1 mo after end of treatment.
ERT (1 g q24h i.v.) MER (1 g
q8h i.v., 3-h infusion, 1 h
after ERT)
ERT, 8; MER, 32; DOR, 8;
CST, 16
Treatment duration, comments, and outcome
20-day treatment. Patient became afebrile on day
4 with negative blood and cultures after 2 days
of treatment. No relapse after 10 mos of
follow-up.
14-day treatment. MER dose reduced due to
renal function. Patient became afebrile on day
3, and blood and urine cultures were sterile
during therapy and after 3-wk follow-up.
10-day treatment. Sterile urine cultures after 2
days of treatment. No relapse after 6 mos of
follow-up
ERT (1 g q24h i.v.) DOR (2 g
q8h i.v., 4-h infusion, 1 h
after ERT)
ERT, 8; MER, 32; DOR, 8;
CST, 16
Drugs and MICs (g/ml)b
Abbreviations: CVC, central venous catheter; ERT, ertapenem; MER, meropenem; DOR, doripenem; CST, colistin; POL-B, polymyxin B; CAZ-AVI, ceftazidime-avibactam.
Ranges are presented when different isolates were isolated and different susceptibility testing MICs were obtained. R, resistant by disc diffusion.
Camargo et al.
(present case
article), United
States
Chua et al. (27),
Singapore
Oliva et al. (25),
Italy
Ceccarelli et al.
(12), Italy
Giamarellou et al.
(11), Greece
Underlying disease(s)
Dual-carbapenem therapy (dose
and infusion conditions when
included)
Downloaded from http://aac.asm.org/ on November 11, 2015 by guest
5906
Reference or source
and country
TABLE 2 Reported clinical cases of double-carbapenem therapy in patients infected with multidrug-resistant and pan-drug resistant K. pneumoniae, including carbapenemase producersa
Challenging Clinical Case
Challenging Clinical Case
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
REFERENCES
1. Neuner EA, Yeh JY, Hall GS, Sekeres J, Endimiani A, Bonomo RA,
Shrestha NK, Fraser TG, van Duin D. 2011. Treatment and outcomes
in carbapenem-resistant Klebsiella pneumoniae bloodstream infections.
Diagn Microbiol Infect Dis 69:357362. http://dx.doi.org/10.1016/j
.diagmicrobio.2010.10.013.
2. Navarro-San Francisco C, Mora-Rillo M, Romero-Gmez MP,
Moreno-Ramos F, Rico-Nieto A, Ruiz-Carrascoso G, Gmez-Gil R,
Arribas-Lpez JR, Mingorance J, Pao-Pardo JR. 2013. Bacteraemia due
to OXA-48-carbapenemase-producing Enterobacteriaceae: a major clinical challenge. Clin Microbiol Infect 19:E72E79. http://dx.doi.org/10
.1111/1469-0691.12091.
3. Tumbarello M, Viale P, Viscoli C, Trecarichi EM, Tumietto F, Marchese A, Spanu T, Ambretti S, Ginocchio F, Cristini F, Losito AR,
Tedeschi S, Cauda R, Bassetti M. 2012. Predictors of mortality in bloodstream infections caused by Klebsiella pneumoniae carbapenemase-
October 2015 Volume 59 Number 10
4.
16.
17.
18.
19.
producing K. pneumoniae: importance of combination therapy. Clin Infect Dis 55:943950. http://dx.doi.org/10.1093/cid/cis588.
Meagher AK, Ambrose PG, Grasela TH, Ellis-Grosse EJ. 2005. The
pharmacokinetic and pharmacodynamic profile of tigecycline. Clin Infect
Dis 41:S333S340. http://dx.doi.org/10.1086/431674.
Prasad P, Sun J, Danner RL, Natanson C. 2012. Excess deaths associated
with tigecycline after approval based on noninferiority trials. Clin Infect
Dis 54:1699 1709. http://dx.doi.org/10.1093/cid/cis270.
Pontikis K, Karaiskos I, Bastani S, Dimopoulos G, Kalogirou M, Katsiari M, Oikonomou A, Poulakou G, Roilides E, Giamarellou H. 2014.
Outcomes of critically ill intensive care unit patients treated with fosfomycin for infections due to pandrug-resistant and extensively drugresistant carbapenemase-producing Gram-negative bacteria. Int J Antimicrob Agents 43:5259. http://dx.doi.org/10.1016/j.ijantimicag.2013.09
.010.
Zhanel GG, Lawson CD, Adam H, Schweizer F, Zelenitsky S, LagacWiens PR, Denisuik A, Rubinstein E, Gin AS, Hoban DJ, Lynch JP, III,
Karlowsky JA. 2013. Ceftazidime-avibactam: a novel cephalosporin/lactamase inhibitor combination. Drugs 73:159 177. http://dx.doi.org/10
.1007/s40265-013-0013-7.
Flamm RK, Farrell DJ, Sader HS, Jones RN. 2014. Ceftazidime/
avibactam activity tested against Gram-negative bacteria isolated from
bloodstream, pneumonia, intra-abdominal and urinary tract infections in
US medical centres (2012). J Antimicrob Chemother 69:1589 1598. http:
//dx.doi.org/10.1093/jac/dku025.
Vazquez JA, Gonzlez Patzn LD, Stricklin D, Duttaroy DD, Kreidly Z,
Lipka J, Sable C. 2012. Efficacy and safety of ceftazidime-avibactam
versus imipenem-cilastatin in the treatment of complicated urinary tract
infections, including acute pyelonephritis, in hospitalized adults: results of
a prospective, investigator-blinded, randomized study. Curr Med Res
Opin 28:19211931. http://dx.doi.org/10.1185/03007995.2012.748653.
Lucasti C, Popescu I, Ramesh MK, Lipka J, Sable C. 2013. Comparative
study of the efficacy and safety of ceftazidime/avibactam plus metronidazole versus meropenem in the treatment of complicated intra-abdominal
infections in hospitalized adults: results of a randomized, double-blind,
phase II trial. J Antimicrob Chemother 68:11831192. http://dx.doi.org
/10.1093/jac/dks523.
Giamarellou H, Galani L, Baziaka F, Karaiskos I. 2013. Effectiveness
of a double-carbapenem regimen for infections in humans due to carbapenemase-producing pandrug-resistant Klebsiella pneumoniae. Antimicrob Agents Chemother 57:2388 2390. http://dx.doi.org/10.1128
/AAC.02399-12.
Ceccarelli G, Falcone M, Giordano A, Mezzatesta ML, Caio C, Stefani
S, Venditti M. 2013. Successful ertapenem-doripenem combination
treatment of bacteremic ventilator-associated pneumonia due to colistinresistant KPC-producing Klebsiella pneumoniae. Antimicrob Agents Chemother 57:2900 2901. http://dx.doi.org/10.1128/AAC.00188-13.
Nordmann P, Poirel L. 2014. The difficult-to-control spread of carbapenemase producers among Enterobacteriaceae worldwide. Clin Microbiol
Infect 20:821 830. http://dx.doi.org/10.1111/1469-0691.12719.
Centers for Disease Control and Prevention, National Center for
Emerging and Zoonotic Infectious Diseases, Division of Healthcare
Quality Promotion. 2 June 2015, last update. 2012 Toolkit guidance for
control of carbapenem-resistant Enterobacteriaceae (CRE). Centers for
Disease Control and Prevention, Atlanta, GA. http://www.cdc.gov/hai
/organisms/cre/cre-toolkit/index.html.
Pao Pardo JR, Serrano Villar S, Ramos Ramos JC, Pintado V. 2014.
Infections caused by carbapenemase-producing Enterobacteriaceae: risk
factors, clinical features and prognosis. Enferm Infecc Microbiol Clin
32(Suppl 4):41 48. http://dx.doi.org/10.1016/S0213-005X(14)70173-9.
Daikos GL, Markogiannakis A, Souli M, Tzouvelekis LS. 2012. Bloodstream infections caused by carbapenemase-producing Klebsiella pneumoniae: a clinical perspective. Expert Rev Anti Infect Ther 10:13931404.
http://dx.doi.org/10.1586/eri.12.138.
Tzouvelekis LS, Markogiannakis A, Piperaki E, Souli M, Daikos GL.
2014. Treating infections caused by carbapenemase-producing Enterobacteriaceae. Clin Microbiol Infect 20:862 872. http://dx.doi.org/10.1111
/1469-0691.12697.
Roberts JA, Kirkpatrick CM, Lipman J. 2011. Monte Carlo simulations:
maximizing antibiotic pharmacokinetic data to optimize clinical practice
for critically ill patients. J Antimicrob Chemother 66:227231. http://dx
.doi.org/10.1093/jac/dkq449.
Daikos GL, Panagiotakopoulou A, Tzelepi E, Loli A, Tzouvelekis LS,
Antimicrobial Agents and Chemotherapy
aac.asm.org
5907
Downloaded from http://aac.asm.org/ on November 11, 2015 by guest
KPC-3-producing K. pneumoniae isolate using ertapenem and
doripenem (24). This combination rapidly reduced bacterial
counts compared with carbapenems alone. Ertapenem was the
suicide inhibitor, as this compound has a higher affinity than
doripenem for the carbapenemase. In fact, in the murine
model, ertapenem was administered an hour before doripenem
to ensure enzyme inactivation when doripenem was acting. A
recent report, also using the murine model, confirmed this
approach, which can even be enhanced with prolonged exposure and higher doses (20). The efficacy under these conditions
was maintained in isolates for which doripenem MICs were 8 to
16 g/ml in immunocompetent infected mice and to a lesser
degree in neutropenic mice.
These findings were translated into the clinical setting (11,
12, 22, 2527). At least 10 other patients with dual-carbapenem
therapy have been reported, all of them treated with ertapenem
plus doripenem or meropenem (Table 2). Occasionally, as
done by Camargo et al. in the case described above, colistin was
added to the double-carbapenem regimen. Clinical and/or microbiological efficacy was observed, except for one patient and
that described in this report, who presented a microbiology
failure (breakthrough bacteremia). In addition, the patient in
this report developed colistin resistance.
Finally, CAZ-AVI (0.25 g/1 g i.v. q8h based on the recommended dose by creatinine clearance) and ertapenem (1 g i.v.
q24h) were used in combination, with a rapid clinical response.
Although the case authors do not explain the justification for this
new combination and do not provide information about carbapenem MICs, we can hypothesize that on this occasion, avibactam
inhibits the KPC enzyme, ensuring not only the activity of ceftazidime but also that of ertapenem. Moreover, a potential synergistic (or eventually additive) effect of a combination with these
-lactams might be expected, as ceftazidime binds preferentially
to penicillin-binding protein 3 (PBP 3) and ertapenem to PBP 2
and PBP 3 (28, 29).
As occurred with dual-carbapenem therapy (20), in order to
understand the dynamics of the carbapenemase inhibition by
avibactam and the activity of ertapenem in the presence of
ceftazidime, further research is required in in vitro and animal
models. It should be stressed that this combination might be
effective only in infections due to KPC- or OXA-48-like-producing CPE but not with metallo--lactamase-producing CPE.
Moreover, the specific selection of carbapenem should be
driven by carbapenemase hydrolysis and the patients renal
function.
Challenging Clinical Case
20.
21.
22.
23.
25.
5908
aac.asm.org
26.
27.
28.
29.
30.
siella pneumoniae bloodstream infections. J Antimicrob Chemother 69:
1718 1720. http://dx.doi.org/10.1093/jac/dku027.
Oliva A, Mascellino MT, Cipolla A, DAbramo A, De Rosa A, Savinelli
S, Ciardi MR, Mastroianni CM, Vullo V. 2015. Therapeutic strategy for
pandrug-resistant Klebsiella pneumoniae severe infections: short-course
treatment with colistin increases the in vivo and in vitro activity of double
carbapenem regimen. Int J Infect Dis 33:132134. http://dx.doi.org/10
.1016/j.ijid.2015.01.011.
Chua NG, Zhou YP, Tan TT, Lingegowda PB, Lee W, Lim TP, Teo J,
Cai Y, Kwa AL. 2015. Polymyxin B with dual carbapenem combination
therapy against carbapenemase-producing Klebsiella pneumoniae. J Infect
70:309 311. http://dx.doi.org/10.1016/j.jinf.2014.10.001.
Hayes MV, Orr DC. 1983. Mode of action of ceftazidime: affinity for the
penicillin-binding proteins of Escherichia coli K12, Pseudomonas aeruginosa and Staphylococcus aureus. J Antimicrob Chemother 12:119 126.
http://dx.doi.org/10.1093/jac/12.2.119.
Kohler J, Dorso KL, Young K, Hammond GG, Rosen H, Kropp H,
Silver LL. 1999. In vitro activities of the potent, broad-spectrum carbapenem MK-0826 (L-749,345) against broad-spectrum beta-lactamase-and
extended-spectrum beta-lactamase-producing Klebsiella pneumoniae and
Escherichia coli clinical isolates. Antimicrob Agents Chemother 43:1170
1176.
Cockcroft DW, Gault MH. 1976. Prediction of creatinine clearance from
serum creatinine. Nephron 16:31 41.
Antimicrobial Agents and Chemotherapy
October 2015 Volume 59 Number 10
Downloaded from http://aac.asm.org/ on November 11, 2015 by guest
24.
Miriagou V. 2007. Activity of imipenem against VIM-1 metallo-betalactamase-producing Klebsiella pneumoniae in the murine thigh infection
model. Clin Microbiol Infect 13:202205. http://dx.doi.org/10.1111/j
.1469-0691.2006.01590.x.
Wiskirchen DE, Nordmann P, Crandon JL, Nicolau DP. 2013. Efficacy
of humanized carbapenem exposures against New Delhi metallo-lactamase (NDM-1)-producing Enterobacteriaceae in a murine infection
model. Antimicrob Agents Chemother 57:3936 3940. http://dx.doi.org
/10.1128/AAC.00708-13.
Cantn R, Canut A, Morosini MI, Oliver A. 2014. Breakpoints for
carbapenemase-producing Enterobacteriaceae: is the problem solved? Enferm Infecc Microbiol Clin 32(Suppl 4):S33S40. http://dx.doi.org/10
.1016/S0213-005X(14)70172-7.
Bush K. 1988. Beta-lactamase inhibitors from laboratory to clinic. Clin
Microbiol Rev 1:109 123.
Thomson KS. 2012. Double-carbapenem therapy not proven to be more
active than carbapenem monotherapy against KPC-positive Klebsiella
pneumoniae. Antimicrob Agents Chemother 56:4037. http://dx.doi.org
/10.1128/AAC.06409-11.
Bulik CC, Nicolau DP. 2011. Double-carbapenem therapy for carbapenemase-producing Klebsiella pneumoniae. Antimicrob Agents Chemother
55:30023004. http://dx.doi.org/10.1128/AAC.01420-10.
Oliva A, DAbramo A, DAgostino C, Iannetta M, Mascellino MT,
Gallinelli C, Mastroianni CM, Vullo V. 2014. Synergistic activity and
effectiveness of a double-carbapenem regimen in pandrug-resistant Kleb-
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Diagnosis Cure Treatment, Disease Prevention: Sources of Drug InformationDocument11 pagesDiagnosis Cure Treatment, Disease Prevention: Sources of Drug InformationShyen100% (11)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Antibiotic Study Cheat Sheet August 2019Document1 pageAntibiotic Study Cheat Sheet August 2019Ryan TurnerNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Wellington ICU Antibiotic SummaryDocument1 pageWellington ICU Antibiotic SummaryDesi Hutapea100% (4)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Infections in DialysisDocument20 pagesInfections in DialysisZiad LalmiNo ratings yet
- Pharmacology Review: Characteristics of DrugsDocument11 pagesPharmacology Review: Characteristics of DrugsPaige Heath ButlerNo ratings yet
- Antibacterial Cell Wall and Membrane InhibitorsDocument28 pagesAntibacterial Cell Wall and Membrane Inhibitorscbac1990100% (5)
- Mnemonics For AntibioticsDocument1 pageMnemonics For AntibioticsshirleyNo ratings yet
- List of Antibiotics: Bactericidal vs BacteriostaticDocument4 pagesList of Antibiotics: Bactericidal vs BacteriostaticMuthu Kumar100% (2)
- Ertapenem Nursing ResponsibilitiesDocument3 pagesErtapenem Nursing ResponsibilitiesBea Dela CenaNo ratings yet
- Print Antibiotics ReviewDocument6 pagesPrint Antibiotics ReviewtiuwangNo ratings yet
- Antibiotics PDFDocument8 pagesAntibiotics PDFSarah JaneNo ratings yet
- Predictores de KPC OutcomesDocument6 pagesPredictores de KPC OutcomesThelma Cecilia Arce LaurelNo ratings yet
- In Vivo Development of Ertapenem Resistance in A Patient WitDocument4 pagesIn Vivo Development of Ertapenem Resistance in A Patient WitThelma Cecilia Arce LaurelNo ratings yet
- In Vivo Development of Ertapenem Resistance in A Patient WitDocument4 pagesIn Vivo Development of Ertapenem Resistance in A Patient WitThelma Cecilia Arce LaurelNo ratings yet
- Carbapenemasas de LombardiDocument8 pagesCarbapenemasas de LombardiThelma Cecilia Arce LaurelNo ratings yet
- J. Antimicrob. Chemother. 2013 Nordmann 487 9Document3 pagesJ. Antimicrob. Chemother. 2013 Nordmann 487 9Thelma Cecilia Arce LaurelNo ratings yet
- Carbapenemasas de LombardiDocument8 pagesCarbapenemasas de LombardiThelma Cecilia Arce LaurelNo ratings yet
- In Vivo Development of Ertapenem Resistance in A Patient WitDocument4 pagesIn Vivo Development of Ertapenem Resistance in A Patient WitThelma Cecilia Arce LaurelNo ratings yet
- ARBOVIRUSDocument21 pagesARBOVIRUSThelma Cecilia Arce LaurelNo ratings yet
- F 1982 MBI Amino Acids Enhance Adaptive Behaviour of Pseudomonas Aeruginosa in TH - PDF 2737Document10 pagesF 1982 MBI Amino Acids Enhance Adaptive Behaviour of Pseudomonas Aeruginosa in TH - PDF 2737Thelma Cecilia Arce LaurelNo ratings yet
- 2015 Nelson's Pedi Antimicrobial TX PDFDocument263 pages2015 Nelson's Pedi Antimicrobial TX PDFMarcel PopaNo ratings yet
- Ertapenem Review of New CarbapenemDocument17 pagesErtapenem Review of New CarbapenemFra1312No ratings yet
- Antibiotic Resistance in Diabetic Foot Soft Tissue Infections: A Series From GreeceDocument5 pagesAntibiotic Resistance in Diabetic Foot Soft Tissue Infections: A Series From GreeceBelinda AngelNo ratings yet
- Beta-lactam antibiotics cell wall synthesis inhibitorsDocument29 pagesBeta-lactam antibiotics cell wall synthesis inhibitorsRen PastelNo ratings yet
- MonobactamDocument18 pagesMonobactamVALENTINA ZAMBRANO ROMERONo ratings yet
- Dr. Ronald Irwanto Natadidjaja, SPPD - Kpti, Finasim: PendidikanDocument28 pagesDr. Ronald Irwanto Natadidjaja, SPPD - Kpti, Finasim: PendidikanayuNo ratings yet
- Ertapenem Package Insert PDFDocument2 pagesErtapenem Package Insert PDFDavidNo ratings yet
- Anti InfectivesDocument4 pagesAnti InfectivesAlecxir PharmacyNo ratings yet
- Microbiology Newlab سالى ابو السعود 0864986Document1 pageMicrobiology Newlab سالى ابو السعود 0864986Mohammed TahounNo ratings yet
- Antibacterial and Anti Viral AgentsDocument51 pagesAntibacterial and Anti Viral AgentsabdeljelileNo ratings yet
- Health PEI: Provincial Antibiotic Advisory Team Empiric Antibiotic Treatment Guidelines For Sepsis Syndromes in AdultsDocument10 pagesHealth PEI: Provincial Antibiotic Advisory Team Empiric Antibiotic Treatment Guidelines For Sepsis Syndromes in AdultsFarmasi RSUD Kramat JatiNo ratings yet
- The Antibiotics: Understanding Their Mechanisms and Appropriate UseDocument56 pagesThe Antibiotics: Understanding Their Mechanisms and Appropriate UseCabdi IshakNo ratings yet
- Top 10 List of Antibiotic ClassesDocument10 pagesTop 10 List of Antibiotic ClassesZubair khanNo ratings yet
- Ampi+Salbactum Amo+ Clavulanate Piper+Tazobactam: ST ST ND ND ND ND TH ST ND TH TH TH RD RD RD TH THDocument1 pageAmpi+Salbactum Amo+ Clavulanate Piper+Tazobactam: ST ST ND ND ND ND TH ST ND TH TH TH RD RD RD TH THAnnieNo ratings yet
- AMR Guideline7001495889Document64 pagesAMR Guideline7001495889Drkrantianand Anand100% (1)
- Allergy Evaluation For Immediate Penicillin Allergy: Skin Test-Based Diagnostic Strategies and Cross-Reactivity With Other Beta-Lactam AntibioticsDocument29 pagesAllergy Evaluation For Immediate Penicillin Allergy: Skin Test-Based Diagnostic Strategies and Cross-Reactivity With Other Beta-Lactam Antibioticsthao hoangNo ratings yet
- MID 3 PHARMA Chemotherapeutic AgentsDocument85 pagesMID 3 PHARMA Chemotherapeutic AgentsMariah Angela PinedaNo ratings yet
- Newer Antibiotics: Guide: DR Saroja A ODocument51 pagesNewer Antibiotics: Guide: DR Saroja A OparahulNo ratings yet
- Allergy Evaluation For Immediate Penicillin AllergyDocument13 pagesAllergy Evaluation For Immediate Penicillin AllergyAnonymous ZUaUz1wwNo ratings yet