Professional Documents
Culture Documents
CPM 2nd Ed Allergic Rhinitis
Uploaded by
Suresh ShresthaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CPM 2nd Ed Allergic Rhinitis
Uploaded by
Suresh ShresthaCopyright:
Available Formats
Philippine Society of Allergology & Immunology, Inc.
Children's Medical Center & General Hospital, 11 Banawe St., Quezon City
Tel. No.: 712-0845 loc 158 & 197; Telefax No.: 743-1818
Officers and Board Members 1996-1998
President
President Elect
Secretary
Treasurer
P.R.O.
Alendry P. Caviles, Jr., M.D.
Remedios C. Ong, M.D.
Manuel M. Po, M.D.
Madeleine W. Sumpaico, M.D.
Hiyasmin W. Lim, M.D.
Board of Directors
Benigno F. Agbayani,M.D.
Nenita L. Alberto, M.D.
Nanneth T. Tiu, M.D.
Ruby Nagtalon-Foronda, M.D.
Felicidad G. Cua-Lim, M.D.
Manuel F. Ferreria, M.D.
Miguel L. Noche, Jr., M.D.
CPM 2ND EDITION
ALLERGIC RHINITIS
Algorithm for the Treatment of Allergic Rhinitis
1
Rhinitis*
2
History,
Physical
Examination
3
4
Is an
allergy
present?
ALLERGY
(Seasonal,
Perennial or
Occupational)
Refer to
ALLERGY
SPECIALIST
6
Skin test,
RAST*
IgE, Eosinophil
count
9
10
Is an
infection
present?
12
N
Are there
structural
defects?
15
OTHERS
(eg Idiopathic,
NARES**,
Vasomotor,
Hormonal, etc)
Rhinitis
11
Acute or
chronic
infection
Appropriate
antibiotics
14
13
Polyps
Septum,
Turbinates
Positive
laboratory
results?
8
Allergen
avoidance
Antihistamine
Y (topical, oral)
Topical/nasal
steroids
Allergen
immunotherapy
Topical
nasal steroids
17
16
Acute or
chronic
infection
18
Appropriate
antibiotics
REFER to
ENT specialist
if no response
* RAST - radioallergosorbent test
** NARES - non-allergic rhinitis with eosinophile syndrome
+ Rhinitis defined as 2 or more of the following symptoms for
>1 hour on most days; nasal discharge, blockage, sneezing/itch.
267
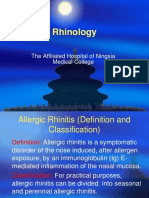
ALLERGIC RHINITIS
CPM 2ND EDITION
Guidelines for the
Treatment of Allergic Rhinitis
Definition
Rhinitis is defined as inflammation of the lining of the
nose, characterized by the following symptoms: nasal
congestion, rhinorrhea, sneezing and itching: occurring
for more than one (1) hour on most days.
Confirmed as allergic rhinitis by skin testing with potent
allergen extracts.
Epidemiology
A. Incidence
In a series of studies, from different countries,
considerable variations occur in the estimate of
prevalence of allergic rhinitis, ranging from 0.5%
(Switzerland) to 28% (Finland).
Allergic rhinitis usually develops in school age or
adolescence.
Incidence (new onset) peaks between ages 10 and
15; declines after age 35.
More frequent in boys than in girls (childhood);
same frequency from adolescence.
B. Risk Factors
1. early allergic rhinitis in persons with a family
history of atopy
2. more common in non-whites than whites, upper
than lower classes (SIBBALD, 1993)
3. birth 1-3 months before the pollen seasons increases risk of allergic rhinitis
4. allergic rhinitis more common in urban than rural
areas.
Diagnosis
Detailed history will usually give the diagnosis of rhinitis.
Important to note: Onset of symptoms, frequency of
symptoms, whether symptoms are daily, episodic, seasonal or perennial; severity and duration of symptoms,
environmental/occupational factors, family history.
A. Signs and symptoms:
Sneezers and runners
sneezing, especially paroxysmal
watery rhinorrhea
itching nose, nasal blockage (variable)
diurnal rhythm (worse during day and improving
during night)
often associated with conjunctivitis
Blockers
little or no sneezing
268
thick nasal mucus (catarrh) more often, posterior
(postnasal drip)
no itch
nasal blockage often severe
constant day and night but may be worse at
night
B. Classification of Rhinitis:
1. Allergic - main symptoms are itching and
irritation in the nose, sneezing and watery, often
associated with nasal congestion.
a. seasonal
b. perennial
2. Infectious rhinitis
a. acute-usually viral, but may have secondary
bacterial infection with sinus involvement
(Strep pneumonia, H. influenza)
b. chronic maybe caused by specific organisms
e.g. M. tuberculosis, K. rhinoscleromatis
3. Others
a. Idiopathic
b. NARES (non-allergic rhinitis with eosinophile syndrome)
c. Hormonal
d. Occupational
e. Rhinitis medicamentosa
C. Diagnostic Tests:
The tests and procedures listed represent a spectrum of
investigations, only a small number are applicable to
each individual patient.
1. General ENT examination
2. Allergy tests - skin tests (prick, intradermal), total
serum IgE, specific serum IgE
3. Endoscopy rigid, flexible
4. Nasal smear/cytology
5. Nasal swab - bacteriology
6. Radiology - plain sinus radiograph (Water's view),
CT scan, MRI, CXR
7. Mucociliary - nasal mucociliary clearance
(NMCC)
8. Nasal airway assessment
NIPF - nasal inspiratory peak flow
Rhinomanometry (anterior and posterior)
Acoustic rhinometry
9. Olfaction - threshold testing
Scratch and Sniff tests
10. Blood- CBC with differential count
ESR
Thyroid Function tests
(ANCA) - and neutrophil cytoplasmic antibody
Immunoglobulins and IgG subclasses
CPM 2ND EDITION
Treatment & Prevention
A. Environmental Control and Avoidance
In most cases, allergen or irritant avoidance
measures should be advised
When possible, environmental control measures
for indoor allergens should be applied, as they
may generally be inspired by the patient. This may
reduce the need for pharmacologic treatment.
Preventive Measures
1. First remove all rugs, curtains and draperies from
the room except the clothes for daily use. Always
keep closet doors closed.
2. Then clean the woodwork, window sills, screens,
closets and floor of the room. Wax the floor.
3. Change all mattresses and pillows in the bedroom
to solid rubber foam. No cotton, kapok, coconut
coif and feather (down) pillows are allowed.
Remember that spring beds may have kapok
or coconut coir stuffings at the bottom. Change
these beds to plain wooden ones with solid rubber
foam mattresses. Encase pillows and mattresses in
zippered air-tight covers.
4. Prepare the bed using washable sheets and
bedspreads (plain cotton). Do not use fuzzy
bedding such as wool, chenilles, etc. Wash
blankets, bedding and covers in hot water at least
every two weeks
5. Every month, remove all solid rubber foam pillows
and mattresses from their covers and expose both
sides to sunlight for several hours. Change covers
before reusing.
6. Clean wooden and metal chairs may be used. Plain
light curtains may be used only if they are washed
weekly.
7. Books, leather products, stuffed toys, wood
paneling and wall papers should be avoided. Wipe
walls with a mold killing solution.
8. The bedroom may be aired daily (windows open
but doors closed). To avoid dust from adjoining
rooms, the door must be opened only to allow
entrance and exit.
9. The room must be cleaned daily and given a
complete cleaning weekly. The allergic patient
should avoid the room during and up to 3-4
hours after cleaning. If the patient has to do the
housecleaning and making the beds, he should
always wear a face mask.
10. Cleaning should include the use of a damp doth,
mop or oil mop. Brooms and dusters should never
used. Vacuum cleaning is strongly advised.
Environmental Control in Other Parts of the House
1. No smoking rule should be strongly enforced.
2. Do not allow the patient to use a bed other than
his own unless it has been properly prepared.
ALLERGIC RHINITIS
3. Use only washable toys. Avoid wall pennants,
macrame hangings and other dust collectors.
4. No animal (dog, cat, bird) should be in contact
with the patient either in or out of the house unless
your doctor derides otherwise.
5. If possible, upholstered furniture should be covered with airtight plastic or vacuumed daily.
6. Dust and molds often contaminate air conditioners.
It is essential that the filter and fan can be cleaned
once a week. An electric fan may be used but must
be cleaned weekly.
7. Limit the numbers of house plants. Pollens and
mold spores become airborne when plants are
watered or disturbed.
8. Do not use insect sprays or powders. Children
should not play with cosmetics. Avoid substances
with strong odors, such as paint, moth balls and
air fresheners.
9. Blankets and clothings that have been stored
should be thoroughly cleaned and ironed before
use.
10. Bathroom and kitchen walls, floors and sinks
should be cleaned frequently with a mold killing
solution of equal parts of water and household
bleach.
11. Plumbing leaks and roof leaks indicated by water
stains or peeling paint should be repaired as soon
as possible.
12. Correct drainage problems near the house. Prune
trees shading the house, compost collection of
leaves are potential mold sources.
Other instructions:
1. Reasonable exercise and outdoor exposure are
encouraged for allergic people. Unless a definite
pollen allergy is known, the person with allergic
symptoms should not limit his outdoor activities
during any season.
2. Although the patient should not help with the
house cleaning, he should be expected to help with
the other work in the house which do not involve
dust exposure.
B. Phannacologic Treatment
1. Antihistamines - bind to histamine receptor
a. sedating - e.g. (Diphenhydramine,
Clemastine, Tydroxyzine)
b. non-sedating - e.g. (Cetirizine, Loratadine,
Acrivastine, Terfenadine, Astemizole)
- Oral
- Topical antihistamines Azelastine
2. Corticosteroids (topical nasal)
reduces inflammatory cell infiltration; decreases
the number of mast cells, eosinophils in the superficial layers of the nasal mucosa, diminishes
hypersensitivity and vascular permeability
3. Sodium cromoglycate
269
ALLERGIC RHINITIS
4. Decongestants
5. Anticholinergics
C. Immunotherapy
Is a method employing subcutaneous injections of
gradually increasing doses of antigenic (allergenic
materials) for the purpose of altering the immunologic response of atopic agents. Many studies show
that immunotherapy, especially benefits patients
with allergic rhinitis and bronchial asthma.
It should be considered if: pharmacotherapy
insufficiently controls symptoms or produces
undesirable side effects.
Appropriate avoidance measures of indoor
allergens fail to control symptoms.
There are positive skin tests or serum specific IgE
which correlates with rhinitis symptoms.
270
CPM 2ND EDITION
CPM 2ND EDITION
ALLERGIC RHINITIS
Drugs Mentioned in the Treatment Guideline
The following index lists therapeutic classifications as recommended by the treatment guideline. For the prescriber's
reference, available drugs are listed under each therapeutic class.
Antihistamines
Hydroxyzine
Cibacen
Captopril
Capoten
Primace
Vasogard
Captopril/Hydrochlorothiazide
Capozide
Cetirizine
Virlix.................................... 31
Zyrtec................................... 31
Chlorpheniramine
Chlor-Trimeton..................... 31
Clormetamine....................... 31
Cohistan .............................. 31
Pharex-Chlorpheniramine.. . 31
UL-Chlorphenamine ........... 31
USA-Chlorphenamine.......... 32
Clemastine
Tavegyl................................. 32
Dimenthindene
Fenistil.................................. 32
Diphenhydramine
Alertuss................................ 32
Benadryl............................... 32
Diphenhydarmine Hizon................................. 32
Nebrecon.............................. 33
USALab
Diphenhydramine.............. 33
Loratadine
Claritin ..................................33
Mebhydrolin
Fabahistin............................. 33
Terfenadine
Terfar.....................................33
Bethamethasone/
Chlorphenamine
Betneton ...............................34
Bethamethasone/
Dexchlorphenamine
Celestamine ..........................34
Chlorphenamine/Prednisolone
Clormetalone........................ 34
Dexamethasone/
Chlorphenamine
Decilamine........................... 34
Disodium cromoglycate
benzalkonium
Vividrin Nasal Spray............ 33
Nasal Steroids
Beclomethasone
Bedomethasone Pharbita............................ 356
Beconase............................ 240
Becotide/Becloforte............ 356
Respocort ............................356
Budesonide
Budecort Nasal............ 240,356
Fluticasone
Flixotide Aqueous
Nasal Spray .................240,356
Fusafungine
Locabiotal ...........................240
Pheniramine/Mepyramine
Triaminic ............................344
Sodium cromoglycate
Intal.................................... 357
Others (Decongestants)
Phenylpropanolamme
Disudrin
Reformulated................... 342
Phamaco Phenylpropanolamine...... 342
Brompheniramine/
Phenylephrine/
Phenylpropanolamme
Dimetapp ............................342
Carbinoxime/Phenylephrine
Rhinopront......................... 343
Carbinoxime/Pseudoephedrine
Rondec-D/
Rondec-S......................... 343
Clemastine/
Phenylpropanolamine
Tavegyl-D........................... 343
Loratadine/Pseudoephedrine
Clarinase .............................342
Phenylpropanolamine/
Chlorphenamine
Nafarin ................................343
Phenylpropanolamine/
Paracetamol
Coldenal Pediatric
Suspension .......................342
Nasathera . ..........................343
Omex.................................. 343
Phenylpropanolamine/
Chlorphenamine/Paracetamol
Alledec .............................. 342
Coldrex............................... 342
Nafarin-A........................... 343
Phenylpropanolaminel
271
You might also like
- Facial Diagnosis Cell Salt IntroductionDocument15 pagesFacial Diagnosis Cell Salt IntroductionRalucaFlorentina100% (3)
- Parkland Trauma HandbookDocument540 pagesParkland Trauma HandbookSuresh Shrestha100% (1)
- Rodent ChecklistDocument5 pagesRodent ChecklistAnonymous zKUNzIjNo ratings yet
- How To Solve A 4x4 Cube - The Rubik's RevengeDocument15 pagesHow To Solve A 4x4 Cube - The Rubik's RevengeSuresh ShresthaNo ratings yet
- Acute Stroke Treatment - CPM 8th EdDocument22 pagesAcute Stroke Treatment - CPM 8th EdSuresh ShresthaNo ratings yet
- How To Solve A 3x3x3 Rubik's Cube For BEGINNERSDocument12 pagesHow To Solve A 3x3x3 Rubik's Cube For BEGINNERSSuresh ShresthaNo ratings yet
- ECG ReadingDocument11 pagesECG ReadingSuresh Shrestha100% (1)
- 09.Project-Hospital Management SystemDocument37 pages09.Project-Hospital Management Systemzahidrafique0% (1)
- Allergy Investigatory Project Biology Class 12Document15 pagesAllergy Investigatory Project Biology Class 12Arijit Bose88% (8)
- Respiratory System Upper Respiratory DiseasesDocument32 pagesRespiratory System Upper Respiratory DiseasesPrince Rener Velasco Pera100% (1)
- Allergic RhinitisDocument27 pagesAllergic RhinitisArvindhanNo ratings yet
- Allergy Bio Investig Probe 2Document17 pagesAllergy Bio Investig Probe 2PRAVIN SNo ratings yet
- AlergiDocument9 pagesAlergiAnggit MargaNo ratings yet
- Allergic Rhinitis PDFDocument3 pagesAllergic Rhinitis PDFdrbilalmunirNo ratings yet
- Reducing Your Child's Asthma Using Integrated Pest ManagementDocument5 pagesReducing Your Child's Asthma Using Integrated Pest ManagementCarol WestinghouseNo ratings yet
- Canine Atopic Dermatitis - A Practical ApproachDocument15 pagesCanine Atopic Dermatitis - A Practical ApproachlirmvetNo ratings yet
- Allergic: Care of Patient WithDocument23 pagesAllergic: Care of Patient WithEzshkha OngueNo ratings yet
- Asthma: A. What Is Asthma?Document15 pagesAsthma: A. What Is Asthma?Farel McCartneyNo ratings yet
- Indoor Air Pollution 2Document30 pagesIndoor Air Pollution 2Dalia Talaat WehediNo ratings yet
- Wood Smoke: Controlling Asthma and Allergy Triggers in The HomeDocument3 pagesWood Smoke: Controlling Asthma and Allergy Triggers in The HomeAbdelkader HociniNo ratings yet
- Nursing Management of Patients With Cancer of The Larynx Cancer of The LarynxDocument6 pagesNursing Management of Patients With Cancer of The Larynx Cancer of The Larynxمحمد سعد طه احمدNo ratings yet
- PracticalmanualAgEnto1 1Document44 pagesPracticalmanualAgEnto1 1Idris IbrahimNo ratings yet
- Prepared By: Ulfat Amin MSC Pediatric NursingDocument25 pagesPrepared By: Ulfat Amin MSC Pediatric NursingAngelic khanNo ratings yet
- Environmental AlterationsDocument4 pagesEnvironmental AlterationsSiti lestarinurhamidahNo ratings yet
- Emergency Poisoning FinalDocument81 pagesEmergency Poisoning FinalMohammed Gazo100% (2)
- Allergic Rhinitis in Children: Jomary Torres Mercado Medico Interno Manati Medical CenterDocument38 pagesAllergic Rhinitis in Children: Jomary Torres Mercado Medico Interno Manati Medical CenterJomary Torres MercadoNo ratings yet
- Allergy AND Asthma: What Can Be Done About Allergies and Asthma?Document2 pagesAllergy AND Asthma: What Can Be Done About Allergies and Asthma?Anny AunNo ratings yet
- Shree Krishna Public SchoolDocument21 pagesShree Krishna Public Schoolharishparsai35No ratings yet
- Carlsbad Mold.20130126.050044Document2 pagesCarlsbad Mold.20130126.050044metalanger6No ratings yet
- Skin Physical ExamDocument10 pagesSkin Physical ExamVenkatesan VidhyaNo ratings yet
- ImmunedisorderDocument3 pagesImmunedisorderDyan LazoNo ratings yet
- Biology Investigatory ProjectDocument19 pagesBiology Investigatory ProjectDebkanti Gupta BhayaNo ratings yet
- MastoiditisDocument37 pagesMastoiditisAkanksha EkkaNo ratings yet
- The Definitive Guide To Cleaning Your Kitchen.20121110.092839Document2 pagesThe Definitive Guide To Cleaning Your Kitchen.20121110.092839anon_280995323No ratings yet
- Managing OtitisDocument9 pagesManaging OtitisdanielguerinNo ratings yet
- Material To Read AlergologyDocument6 pagesMaterial To Read AlergologyLeo PaulNo ratings yet
- Treatment of Otomycosis Due To Aspergillus Niger With Tolnaftate PDFDocument3 pagesTreatment of Otomycosis Due To Aspergillus Niger With Tolnaftate PDFMei Risanti SiraitNo ratings yet
- 113 Latex Allergy Asthma or Eczema.: FitkitDocument33 pages113 Latex Allergy Asthma or Eczema.: FitkitNeela MukthaNo ratings yet
- AnaplasmosisDocument4 pagesAnaplasmosisBasit AliNo ratings yet
- Allergic RhinitisDocument21 pagesAllergic RhinitisRahmadona NandaNo ratings yet
- Allergic RhinitisDocument2 pagesAllergic RhinitisJamie IcabandiNo ratings yet
- Reading - 94-262Document169 pagesReading - 94-262jijo kurian mathewNo ratings yet
- Rhinitis: by KhairunnisaDocument40 pagesRhinitis: by KhairunnisaayuniNo ratings yet
- Important Topics in OtologyDocument94 pagesImportant Topics in OtologyDr. T. Balasubramanian100% (1)
- All About Asthma Triggers singlesFinal2ADocument45 pagesAll About Asthma Triggers singlesFinal2AJanelleNo ratings yet
- Allergic Rhinitis 1Document5 pagesAllergic Rhinitis 1Ace FabrigasNo ratings yet
- Bites & StingsDocument78 pagesBites & StingsleemurrieNo ratings yet
- Auburn - Feline Board Review 1Document19 pagesAuburn - Feline Board Review 1Fateh Batth100% (2)
- Lo 3 Clean Premises: Information Sheet No.6 - LO3 - Sanitation in HousekepingDocument10 pagesLo 3 Clean Premises: Information Sheet No.6 - LO3 - Sanitation in HousekepingJohn Paul MartinNo ratings yet
- Doctor Franke OtitisDocument6 pagesDoctor Franke OtitisMelanie McguireNo ratings yet
- Mission - Dust Control - HypothesisDocument5 pagesMission - Dust Control - HypothesisjoshuaNo ratings yet
- Presentation On HousingDocument25 pagesPresentation On HousingPawan Barai100% (2)
- BDS Practical Notebook.Document77 pagesBDS Practical Notebook.Hamda AnjumNo ratings yet
- DengueDocument6 pagesDengueteabagmanNo ratings yet
- Unit 4Document4 pagesUnit 4qweyo yhuNo ratings yet
- House Dust MiteDocument17 pagesHouse Dust MiteThaddeus Lewis0% (1)
- Health6 - Q3 - Module 7 Ways To Prevent and Control Pests and RodentsDocument19 pagesHealth6 - Q3 - Module 7 Ways To Prevent and Control Pests and RodentsALMA MALLONGANo ratings yet
- Biology Year OneDocument16 pagesBiology Year Onewuraola oladipoNo ratings yet
- Env 8Document44 pagesEnv 8Kamal Kant GuptaNo ratings yet
- Bio InvestigatoryDocument22 pagesBio InvestigatoryTEJAS JAINNo ratings yet
- Classification of Guest Room According To PrizeDocument9 pagesClassification of Guest Room According To PrizeAurora Babon-CompetenteNo ratings yet
- FleasDocument27 pagesFleasapi-301746262100% (6)
- Name: Bhanderi Akashkumar H. Clinical Clerk BCCM. ROTATION: OCT. 11-20, 2020Document7 pagesName: Bhanderi Akashkumar H. Clinical Clerk BCCM. ROTATION: OCT. 11-20, 2020Venkatesh GarikapatiNo ratings yet
- Sterilization IN Orthodontics: G.Shekar Subramanian Ist Yr PGDocument79 pagesSterilization IN Orthodontics: G.Shekar Subramanian Ist Yr PGShekar SubramanianNo ratings yet
- Concept Map Indelicato Peds 2014Document2 pagesConcept Map Indelicato Peds 2014api-277318016No ratings yet
- Pedia Module Preschooler PDFDocument11 pagesPedia Module Preschooler PDFRegine CuntapayNo ratings yet
- Rabies Reduced Dose ScheduleDocument1 pageRabies Reduced Dose ScheduleSuresh ShresthaNo ratings yet
- CPM 1st Ed HypertensionDocument26 pagesCPM 1st Ed HypertensionSuresh ShresthaNo ratings yet
- Understanding CBC Histogram PDFDocument17 pagesUnderstanding CBC Histogram PDFSuresh ShresthaNo ratings yet
- Signs and HallmarksDocument15 pagesSigns and HallmarksSuresh ShresthaNo ratings yet
- Study Suggestions RevisedDocument11 pagesStudy Suggestions RevisedSuresh Shrestha100% (1)
- TB Burden and Treatment Guidelines: DR Malgosia Grzemska Global TB Programme, WHO/HQDocument25 pagesTB Burden and Treatment Guidelines: DR Malgosia Grzemska Global TB Programme, WHO/HQSuresh ShresthaNo ratings yet
- 03 Cutaneous MycosesDocument30 pages03 Cutaneous MycosesFelix AyornuNo ratings yet
- Ajnr Benign Enhancing Lesion of Foramen MagnumDocument5 pagesAjnr Benign Enhancing Lesion of Foramen Magnumapi-288086961No ratings yet
- Abdominal Swelling and Ascites: Global ConsiderationsDocument5 pagesAbdominal Swelling and Ascites: Global ConsiderationsJacob BorongNo ratings yet
- Inspection Observations FY22Document358 pagesInspection Observations FY22dsevolveNo ratings yet
- Y10 Chapter+13 ExcretionDocument67 pagesY10 Chapter+13 ExcretionLOW YUEBEI RIJNo ratings yet
- Assessment of ADHD and ComorbidityDocument3 pagesAssessment of ADHD and ComorbidityFelipe CafureNo ratings yet
- NCP BaiaeDocument7 pagesNCP BaiaeJonathan Delos ReyesNo ratings yet
- Case ReportDocument9 pagesCase ReportAlmah Mae Duro-onNo ratings yet
- Grade 9 Biology - Lesson Note April 8,2020Document10 pagesGrade 9 Biology - Lesson Note April 8,2020micahxNo ratings yet
- HbA1c OdtDocument2 pagesHbA1c OdtAhmed AssafNo ratings yet
- Microbiology PneumoniaDocument31 pagesMicrobiology PneumoniaKartika Rezky100% (1)
- Dysbiosis of The Human Oral Microbiome During The Menstrual Cycle and Vulnerability To The External Exposures of Smoking and Dietary SugarDocument14 pagesDysbiosis of The Human Oral Microbiome During The Menstrual Cycle and Vulnerability To The External Exposures of Smoking and Dietary SugarPaloma C. PeñaNo ratings yet
- 10 Commandments of ConsultationDocument4 pages10 Commandments of ConsultationZlatan KurjakovicNo ratings yet
- Fecal Elimination and Urinary EliminationDocument6 pagesFecal Elimination and Urinary Eliminationincent100% (1)
- Healing Following Implant Surgery: Osseous Healing-Early PhaseDocument2 pagesHealing Following Implant Surgery: Osseous Healing-Early PhaseUrjita PatilNo ratings yet
- NCP - Activity IntoleranceDocument5 pagesNCP - Activity IntolerancePrincess Alane MorenoNo ratings yet
- Compendium of Instructions - Covid19Document472 pagesCompendium of Instructions - Covid19Ramesh Babu TatapudiNo ratings yet
- Kurva LubchencoDocument3 pagesKurva LubchencoDanil Armand67% (3)
- Cervical Spine Injury: Julie C. LeonardDocument15 pagesCervical Spine Injury: Julie C. LeonardCamilla CristinaNo ratings yet
- E Stimation of HemoglobinDocument13 pagesE Stimation of HemoglobinSANANo ratings yet
- Basic First Aid (Bfa)Document118 pagesBasic First Aid (Bfa)Hamza Moussa100% (1)
- Psychiatry 101Document17 pagesPsychiatry 101Vaso Talakvadze0% (1)
- Ataxia 10Document19 pagesAtaxia 10Cristina GhizdavetNo ratings yet
- Print - Chapter 14. Ammonia and UreaDocument9 pagesPrint - Chapter 14. Ammonia and UreabelaginaNo ratings yet
- A Huge Completely Isolated Duplication CystDocument6 pagesA Huge Completely Isolated Duplication CystNurlyanti RustamNo ratings yet
- The Control and Prevention of MRSA in Hospitals and in The CommunityDocument41 pagesThe Control and Prevention of MRSA in Hospitals and in The CommunityDimas RfNo ratings yet
- Zygomatic Arch and Orbital FracturesDocument6 pagesZygomatic Arch and Orbital FractureszacrouchyNo ratings yet
- Jurnal BTKV Herman 1Document11 pagesJurnal BTKV Herman 1Elyas MuhammadNo ratings yet