Professional Documents
Culture Documents
Csi Group3
Uploaded by
api-299189797Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Csi Group3
Uploaded by
api-299189797Copyright:
Available Formats
1
Group 3
Clinical Practicum III
Craniospinal Irradiation Project
November 9, 2016
Proton Craniospinal Irradiation
Introduction
Compared to x-ray radiation therapy for Craniospinal Irradiation (CSI), proton therapy is
more effective in delivering dose to the target and sparing the normal tissues due to the
characteristics of Bragg-peak and hence the absence of exiting dose from proton beams.1
Because exit dose is absent in proton beam therapy, there is significantly less integral dose
compared with photon therapy techniques. New pencil beam scanning (PBS), also known as spot
scanning, is able to deliver intensity-modulated proton therapy (IMPT), which can further reduce
the dose to normal tissue and minimize secondary neutron contamination and deliver the dose to
the target more precisely at the same time.2 The IMPT is considered a superior technique for
pediatric patients over other proton therapy techniques. In addition, the newly developed robust
optimization method of IMPT allows multi-field optimization for large targets without field
junction shifting, which is an advantage for CSI planning.3 Thus, for this CSI project, the
technique of PBS proton therapy was used to deliver the IMPT plan to the patient.
Target and OR's delineation
The patient was simulated in supine position for comfort and easier access for
anesthesia.4 The clinical target volumes (CTV) contained the entire brain and the spinal canal
including the thecal sac. Optical nerves were included in the CTV as suggested in a recent study
of CSI proton therapy.5 Cribriform plate was also included in the CTV to ensure adequate
coverage, as studies show that underdose of the cribriform plate region caused relapse of
medulloblastoma in the subfrontal brain area.6
In conventional CSI treatment, multiple fields have to be accurately matched by doing
collimator rotation angle and gap calculations. To minimize over and under dose to the spinal
cord, a weekly shift of field junctions has to be performed. To reduce the complexity of manual
feathering and take advantage of inverse planning, IMRT, volumetric modulated arc
radiotherapy (VMAT), and IMPT have been used for CSI. Usually, several small regions are
contoured at the junction area and different dose levels were set for inverse optimization to
simulate a gradient region at the junction. The concept of robust optimization has recently been
implemented in commercial treatment planning software, like RayStation, to take the worst case
scenario into consideration during optimization. Generally CTV is used as the target for
optimization and a robust optimization is performed to account all the uncertainties caused by
proton range, setup, and anatomical motion.2, 7 The idea of this project is to use robust
optimization to optimize the dose in the junction area without creating any extra contours. In a
CSI proton plan, 4 to 5 fields are used. When robust optimization is used for independent beams,
as shown in Figure 1, the total number of scenarios is too much for the optimizer to compute. So
in this IMPT planning, only the superiorinferior direction robust optimization was used to
compensate the over and under dose of the matching fields.7 To compensate the setup errors and
anatomical motions in the other directions, a pencil beam scattering target volume (PBSTV) was
generated by adding a 3 mm margin to the anterior and posterior directions of the brain CTV,
and the left and right directions of spinal CTV, and a 1 mm margin to the left and right directions
of the brain CTV and the anterior and posterior directions of the spinal CTV, which were also the
beam directions. Since robust optimization was used for the superior and inferior directions to
compensate the field misalignment uncertainties at the field junctions, no margin was added in
these two directions. All organs at risk (OR) shown in Table 2 were contoured. The PBSTV and
OR are shown in Figure 2 and 3.
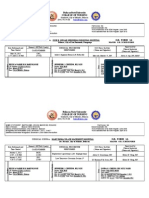
Figure 1. Robust optimization settings for CSI IMPT planning. A 0.3 cm uncertainty in Sup-Inf
direction was used. Independent beams were checked to account all possible combinations of
patient ISO shift uncertainties.
PBSTV
Optic
nerves
Figure 2. Brain PBSTV (blue) includes the optic nerves (green)
PBSTV
CTV
Figure 3. Spinal PBSTV (blue) and CTV (green)
Treatment planning process
The couch angle was at 0 degree. For the brain PBSTV, two parallel opposed lateral
beams that share the same iso-center were added. Since the maximum field size is 21 cm of our
proton machine, three posterior beams were placed to cover the whole spinal portion of the
PBSTV. The cranial beams overlapped with the superior spinal beams by a few centimeters, and
each two adjacent spinal beams overlapped with each other as well. Each spine field has its own
iso-center. All iso-centers were at the same level and same lateral couch position to minimize
shifts. The beam arrangement and iso-centers are shown in Figure 4.
Figure 4. Beam arrangement and iso-centers
A dose of 36 Gy at 1.8 Gy per day was prescribed to the target volume. A 3mm setup
uncertainty in the superior-inferior direction and 3.5% range uncertainty for the PBSTV were
used for robust optimization (Figure 1). IMPT is delivered by scanning the target volume layerby-layer. By switching energies the proton beams penetrate the target volume at different depths
so that the Bragg peaks stop at different layers. A 1 cm wall with 1 mm gap outside the PBSTV
was generated to keep the dose more conformal. The plan optimization objectives are shown in
Figure 5.
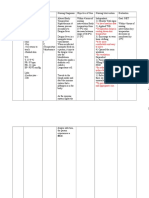
Figure 5. Plan optimization objectives
Plan evaluation and discussions
The coverage of the PBSTV was successfully achieved. 95.1% of the PTV received the
prescribed dose. The maximum dose, defined as the dose to 1% of the PTV6, was 108% of the
prescription dose. Table 1 shows the dosimetry parameters for the target volume. Figure 6 shows
the iso-dose distribution. Figures 7 and 8 show the DVH for the OR and PBSTV. The dose
constraints for all the OR were all met. (Table 2)
Table 1. Dosimetry parameters for the target volume
Target Parameters
Desired Objective
Achieved objective
Maximum Plan Dose (D1):
< 5% of PTV to receive 3960 cGy
3888 cGy
D99:
> 3240 cGy
3359 cGy
V100:
> 95%
95.1%
V95:
> 34.2 Gy (or 95%)
98.9%
Figure 6. Iso-dose distribution
Figure 7. Plan DVH for the OR
Figure 8. Plan DVH for the pencil-beam scatter target volume
Table 2. Desired and achieved objectives for each organ at risk
Organ at risk
Desired
Achieved
Constraints
Objective(s)
Objective(s)
Met/Exceeded
Heart
Mean < 320 cGy
6 cGy
Met
Stomach
V22.5 < 10 cc
0 cc
Met
Lung rt
Mean < 700 cGy
80 cGy
Met
Lung lt
Mean < 700 cGy
107 cGy
Met
Liver
Mean < 1800 cGy
4 cGy
Met
Kidney rt
Mean < 1500 cGy
6 cGy
Met
Kidney lt
Mean < 1500 Gy
7 cGy
Met
Bowel
V24 < 20 cc
0 cc
Met
Rectum
V27.5 < 20 cc
0 cc
Met
Bladder
V16.8 < 15 cc
0 cc
Met
Femur rt
V24 < 10 cc
0 cc
Met
Femur lt
V24 < 10 cc
0 cc
Met
Mandible
DMax < 3600 cGy
800 cGy
Met
Parotids
Mean < 2600 cGy
274 cGy
Met
Submandibular Glands
Mean < 2600 Gy
57 cGy
Met
Glottis
Mean < 2600 Gy
24 cGy
Met
Thyroid
V45 < 100%
0.0
Met
Lens
DMax < 700 cGy
105 cGy
Met
This technique takes into consideration of the field misalignment uncertainties and
optimizes to generate a decreasing dose gradient in the overlapped junction area of one field, and
an increasing dose gradient in the same area of the adjacent field. Figure 9 shows the dose
gradient in the cranial fields and the mid-spinal field when the superior spinal field is removed.
By adding a line dose profile in that area as shown in Figure 10, the dose gradient, as displayed
10
in Figure 11, can be measured. Thus, the proton CSI plan is able to achieve field junction
homogeneity and substantially reduce dose to healthy tissues.
Dose gradient
Dose gradient
Figure 9. Dose gradient in the overlapped field junctions
11
Line dose profile
Figure 10. The line dose profile added to measure the dose gradient (orange)
12
Figure 11. The dose gradient of the overlapped area for the two adjacent fields
13
The hot spots locate at the superior part of the cranial PTV, due to the reduced thickness
of anatomy. The cold spots are at the junction area between fields, which are caused by robust
optimization to prevent hot spots when adjacent fields overlap more than predefined.
For both conventional and IMPT techniques, the higher sensitivity to organ motion was
thought to be the biggest disadvantage to proton therapy, as the beams are not synchronized with
organ motion during beam delivery.8 The newly developed robust optimization method of IMPT
has been demonstrated to account for the range and patient setup uncertainties including tumor
shrinkage, patient weight gain/loss, field misalignment, intrafractional organ motion, etc.2 In
recent published research, the plan robustness was evaluated for robust optimized and
conventional non-robust IMPT plans by shifting the isocenter 3 mm per field.3 Results showed
the deviation for the simulated mismatching error was significantly smaller than that in the
conventional plan, which proved the robust optimization is able to compensate the setup errors
for multi-isocenter fields. This robust optimization method of IMPT allows multi-field
optimization for large targets without field junction shifting, which is an advantage for CSI
planning.
Proton therapy, especially PBS therapy, has been proven to be effective and superior
when treating the craniospinal axis compared to standard photon therapy. The aforementioned
benefits surrounding PBS proton therapy supports the superiority of proton therapy. However,
proton therapy presents with disadvantages of which includes monetary constraints on facilities
to support such equipment and patients to receive treatments of that caliber. Proton therapy
equipment also requires a large operating space within the facility or another spare building. For
the robust optimization, too many scenarios will significantly increase the optimization time. As
a result, more experience is still needed in balancing the number of scenarios and plans adequate
robustness. Lastly, since proton therapy is a newer technique, quality assurance programs are
limited and facilities must implement their own programs until national protocols become
available.8
14
Conclusion
The IMPT using robust optimization is able to account iso shift uncertainties in CSI
treatments. The planning process is much simpler and more robust than other methods. The
doses to the OR and normal tissues are considerably less than photon treatments, which is critical
for young patients.
15
References
1. Liu H, Chang JY. Proton therapy in clinical practice. Chin J Cancer. 2011;30(5):315-326.
http://dx.doi.org/10.5732/cjc.010.10529
2. Liu W, Zhang X, Li Y, Mohan R. Robust optimization of intensity modulated proton therapy.
Med Phys. 2012;39(2):1079-1091. http://dx.doi.org/10.1118/1.3679340
3. Liao L, Lim GJ, Li Y, et al. Robust optimization for intensity modulated proton therapy
plans with multi-Isocenter large fields. Int J Part Ther. September 2016.
http://dx.doi.org/10.14338/IJPT-16-00012.1
4. South, M. Using Composite Planning and Delivery with Feathered Junctions in
Craniospinal, Brain-Spine and Spine-Spine Abutted Fields. [PowerPoint]. Methodist Cancer
Center; 2015.
5. Lin H, Ding X, Kirk M, et al. Supine craniospinal irradiation using a proton pencil beam
scanning technique without match line changes for field junctions. Int J Radiat Oncol Biol
Phys. 2014;90(1):71-78. http://dx.doi.org/10.1016/j.ijrobp.2014.05.029
6. Paulino AC. Radiotherapeutic management of medulloblastoma. Oncology (Williston Park).
1997;11(6):813-823, 827-828, 831.
7. Liu W, Frank SJ, Li X, et al. PTV-based IMPT optimization incorporating planning risk
volumes vs robust optimization. Med Phys. 2013;40(2):021709-1-8.
http://dx.doi.org/10.1118/1.4774363
8. Khan FM, Gibbons JP. The Physics of Radiation Therapy. 5th ed. Philadelphia, PA:
Lippincott Williams & Wilkins; 2014.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- BrachyevaluationDocument2 pagesBrachyevaluationapi-299189797No ratings yet
- 12 11 FinalDocument11 pages12 11 Finalapi-299189797No ratings yet
- ElectronevaluationDocument2 pagesElectronevaluationapi-299189797No ratings yet
- ElectronpdfDocument2 pagesElectronpdfapi-265264098No ratings yet
- Public Version CV Yinan Wang 2016Document3 pagesPublic Version CV Yinan Wang 2016api-299189797No ratings yet
- Tangents Photon EvaluationDocument2 pagesTangents Photon Evaluationapi-299189797No ratings yet
- Oct EvaluationDocument3 pagesOct Evaluationapi-299189797No ratings yet
- Monthly Evaluation12-15Document3 pagesMonthly Evaluation12-15api-299189797No ratings yet
- Nov EvaluationDocument3 pagesNov Evaluationapi-299189797No ratings yet
- Photon Summary EvaluationDocument3 pagesPhoton Summary Evaluationapi-299189797No ratings yet
- CW Photon EvaluationDocument2 pagesCW Photon Evaluationapi-299189797No ratings yet
- Budget ActivityDocument2 pagesBudget Activityapi-247490129No ratings yet
- Fall Case Log TotalsDocument2 pagesFall Case Log TotalsBen LemieuxNo ratings yet
- Tangents Photon EvaluationDocument2 pagesTangents Photon Evaluationapi-299189797No ratings yet
- Avoid Imrt EvaluationDocument2 pagesAvoid Imrt Evaluationapi-299189797No ratings yet
- Summary Imrt EvaluationDocument3 pagesSummary Imrt Evaluationapi-299189797No ratings yet
- Case StudyDocument1 pageCase Studyapi-299189797No ratings yet
- Yinanwang Service No PicDocument3 pagesYinanwang Service No Picapi-299189797No ratings yet
- Case StudyDocument1 pageCase Studyapi-299189797No ratings yet
- Yinanwang Service No PicDocument3 pagesYinanwang Service No Picapi-299189797No ratings yet
- Qa Tables YinanwangDocument12 pagesQa Tables Yinanwangapi-299189797No ratings yet
- Mentoring Paper YwDocument5 pagesMentoring Paper Ywapi-299189797No ratings yet
- Cns Assignment2016Document2 pagesCns Assignment2016api-299189797No ratings yet
- Craniospinal Irradiation YinanwangDocument7 pagesCraniospinal Irradiation Yinanwangapi-299189797No ratings yet
- Fall Case Log TotalsDocument2 pagesFall Case Log TotalsBen LemieuxNo ratings yet
- April EvaluationDocument3 pagesApril Evaluationapi-299189797No ratings yet
- Prostate Imrt EvaluationDocument2 pagesProstate Imrt Evaluationapi-299189797No ratings yet
- Prostate With Nodes Imrt EvaluationDocument2 pagesProstate With Nodes Imrt Evaluationapi-299189797No ratings yet
- Para-Aortic or Nodal Irradiation EvaluationDocument2 pagesPara-Aortic or Nodal Irradiation Evaluationapi-299189797No ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Rehabilitation of Muscle Dysfunction in HemophiliaDocument14 pagesRehabilitation of Muscle Dysfunction in HemophiliadavidcorzoNo ratings yet
- Formulari Ubat KKM Bil.2 2013Document170 pagesFormulari Ubat KKM Bil.2 2013zilott90No ratings yet
- Post Test 19Document4 pagesPost Test 19Naomi VirtudazoNo ratings yet
- Drugs Affecting The G.I.T.Document11 pagesDrugs Affecting The G.I.T.Mona MahfouzNo ratings yet
- DR Anuj Raj BijukchheDocument60 pagesDR Anuj Raj BijukchheMUHAMMAD JAWAD HASSANNo ratings yet
- Nursing Management A. Nursing Care PlanDocument12 pagesNursing Management A. Nursing Care Planmabzbutterfly69% (13)
- Brain Tumor Segmentation and Detection Using Nueral NetworksDocument9 pagesBrain Tumor Segmentation and Detection Using Nueral Networksjoshi manoharNo ratings yet
- Physical Exam of the Eye: Structures, Findings, DiagnosesDocument16 pagesPhysical Exam of the Eye: Structures, Findings, DiagnosesriveliNo ratings yet
- Chest PainDocument13 pagesChest Paing3murtulu100% (1)
- New PRC Form SampleDocument8 pagesNew PRC Form SampleLanie Esteban EspejoNo ratings yet
- Schizophrenia Presentation by Dr. MORAHDocument39 pagesSchizophrenia Presentation by Dr. MORAHChikezie OnwukweNo ratings yet
- What is cephalexin antibiotic used forDocument9 pagesWhat is cephalexin antibiotic used forYaleswari Hayu PertiwiNo ratings yet
- DENGUE CS NCP 1Document8 pagesDENGUE CS NCP 1Karyl SaavedraNo ratings yet
- OASIS Patient History GuidanceDocument20 pagesOASIS Patient History GuidancebiskwetNo ratings yet
- Prometric Exam Ophthalmology 28-3-2013Document10 pagesPrometric Exam Ophthalmology 28-3-2013Hasan Dahamsheh100% (4)
- Nursing Care Plan For "Herniated Nucleus Pulposus Ruptured Inter Vertebral Disc"Document9 pagesNursing Care Plan For "Herniated Nucleus Pulposus Ruptured Inter Vertebral Disc"jhonroks100% (7)
- Caroline Stone. Osteopathic ApproachDocument54 pagesCaroline Stone. Osteopathic ApproachIoan Andra100% (5)
- WLP Health Makatao Q1 W5Document13 pagesWLP Health Makatao Q1 W5Rosemarie Mañabo RamirezNo ratings yet
- Rife Frequenciesfor CancerDocument9 pagesRife Frequenciesfor CancerFranquicio Perez JavierNo ratings yet
- Referensi Nomor 5Document4 pagesReferensi Nomor 5audreynatalia777No ratings yet
- Triage Process Prioritizes PatientsDocument5 pagesTriage Process Prioritizes PatientsWyen Cabatbat50% (2)
- Amniotic Fluid Embolism: Principles of Early Clinical ManagementDocument5 pagesAmniotic Fluid Embolism: Principles of Early Clinical Management16.11Hz MusicNo ratings yet
- 1st Bio CH 5 McqsDocument4 pages1st Bio CH 5 Mcqsanon_768348720No ratings yet
- Vascular Diseases: Idar Mappangara Department of Cardiology Hasanuddin UniversityDocument31 pagesVascular Diseases: Idar Mappangara Department of Cardiology Hasanuddin UniversityriniNo ratings yet
- Autopsy PDFDocument3 pagesAutopsy PDFstprepsNo ratings yet
- 2020 Collet-Sicard Syndrome After Jefferson FractureDocument3 pages2020 Collet-Sicard Syndrome After Jefferson FractureJose ColinaNo ratings yet
- OmronDocument19 pagesOmrondekifps9893No ratings yet
- Ds Pedia WardDocument2 pagesDs Pedia WardRhea Mae Valles - ReyesNo ratings yet
- Current Liberty Healthcare ContractDocument46 pagesCurrent Liberty Healthcare ContractABC10No ratings yet
- Case Study CKD DM Type 2Document7 pagesCase Study CKD DM Type 2Brian Cornel0% (3)