Professional Documents
Culture Documents
Antibiotics Dutch Example
Uploaded by
rj99masterCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antibiotics Dutch Example
Uploaded by
rj99masterCopyright:
Available Formats
BMJ 2016;354:i4192 doi: 10.1136/bmj.
i4192 (Published 3 August 2016)
Page 1 of 3
Feature
FEATURE
ANTIMICROBIAL RESISTANCE
Saving antibiotics for when they are really needed: the
Dutch example
Doctors have responded well to the call to reduce unnecessary antibiotic prescriptions. But what
about farming? The Dutch have shown that antibiotic use can be slashed in agriculture too. So why
isnt everybody doing it? Tony Sheldon reports
Tony Sheldon journalist
Netherlands
Dutch healthcare uses the fewest antibiotics in the world, is
the bold and justifiable claim of the Dutch Health Council, the
governments independent scientific advisers. The country has
had low use for decades.1 Yet in veterinary medicine the
Netherlands, the worlds second largest exporter of agri-food
products (after the United States), was, until a few years ago,
among the highest users. This mismatch sparked action that saw
the country cut antibiotic use in farm animals by nearly 60%
from 2007 to 2015.2 3
Today the Netherlands has one of the lowest levels of
antimicrobial resistance in the world, and it believes the only
way to keep resistance levels down is for health and agricultural
sectors everywhere to work together in what it calls a One
Health approach.
If we want to control a problem in healthcare we need to act
everywhere where antibiotics are used. Because of the
continuous evolution of resistance, any reservoir could be a
source of resistant organisms to humans, says Dik Mevius,
head of the National Reference Laboratory on Antimicrobial
Resistance in Animals at the Central Veterinary Institute at
Wageningen University.
In June, after pushing the issue for six months while holding
the rotating EU presidency, the Netherlands convinced the 28
countries of the EU to commit to launching One Health national
antimicrobial resistance action plans by mid-2017.4
Edith Schippers, Dutch health minister, said that even though
countries have different situations and are at different stages in
developing national plans to tackle antimicrobial resistance,
differences between member states cannot be a reason to hinder
progress and avoid taking necessary action.
The new action plans are supposed to include measures to avoid
routine preventive use of antibiotics in agriculture and restrict
animal use of antibiotics that are of critical importance to human
health, such as carbapenems.
They should also include measureable goals adapted to fit each
countrys circumstances. A European One Health network will,
in turn, support the national plans and allow countries to
exchange information on their progress.
Antibiotics are used in huge quantities in farming, and entire
herds are often treated when a single animal falls sick or to
prevent a herd catching a disease. The EU banned the use of
antibiotics to promote animal growth in 2006 and is also now
talking about introducing a ban on preventive use of antibiotics.
Some EU countries are already clamping down as much as the
Netherlands (Denmark, Sweden), and others are taking some
additional measures (Germany, UK). But so far there has been
little transmission of resistant organisms from animals to humans
(apart from people working in close contact with animals), and
many countries, particularly those grappling with high levels
of resistance in humans, such as meticillin resistant
Staphylococcus aureus (MRSA), do not see reducing use in
agriculture as a priority.
How did the Dutch do it?
Use of antibiotics by the intensive poultry, pig, and cattle farms
in the Netherlands more than doubled between 1990 and 2007.
By 2010 the country topped a European league table of the use
of antibacterial agents per weight of slaughtered animal.5
Systematic preventive use of antibiotics was simply cheaper
than stringent hygiene and infection control measures. MRSA,
endemic in the pig population, spread to farmers and vets;
resistant bacteria producing extended spectrum lactamase
(ESBL), endemic in poultry, were linked to a human death.6
There was momentum for change. This was unacceptable, in
a country with 17 million people in a small area with the
production of 450 million broiler chickens a year, who were at
that time all shedding ESBLand in a country where healthcare
was so well controlled, says Mevius.
tonysheldon5@cs.com
For personal use only: See rights and reprints http://www.bmj.com/permissions
Subscribe: http://www.bmj.com/subscribe
BMJ 2016;354:i4192 doi: 10.1136/bmj.i4192 (Published 3 August 2016)
Page 2 of 3
FEATURE
As a result the Dutch Veterinary Medicines Authority was
launched, a trusted public-private partnership of food producers,
vets, and government. Within two years it had data on antibiotic
use from 40 000 farms. Mevius says: We knew which farms
used two or three times as much as others. We also knew the
vets who were prescribing more, and we were then able to start
benchmarking. We created an awareness.
At the same time parliament rapidly agreed an ambitious, if
unscientific, target of 50% reduction. A massive 58.1% in six
years followed. Today, patterns of use still vary, and a further
30% fall is still thought possible.
Mevius was surprised: We thought that in a country which has
very industrialised animal production it would be difficult to
change habits. It was in fact very easy. This shows there was
a huge overuse of antibiotics in livestock.
And crucial to the success was that it was carried out privately
by all the parties involved in animal production while the
government just imposed the targets. It was a top-down
decision to do something and a bottom-up implementation that
was the success, says Mevius.
Different medical culture
The story is different in humans. Dutch doctors dont
overprescribe antibiotics and Dutch patients dont demand them.
Studies over decades have consistently shown the Netherlands
to be among the European leaders for prudent antimicrobial use
in human health.1 Public health experts estimate 15% of the
population are prescribed antibiotics by their primary care doctor
in any one year, half or a third of the proportion in southern
European countries. The latest 2013 figures show the
Netherlands with 11 daily doses of antibiotics per 1000
population, half of the UKs rates.7 Equally, rates of MRSA
infection are among the lowest, at about 0.5% among the general
population.
In the Netherlands antibiotics must be supplied on prescription,
with primary care, which has a strong gatekeeper function in
Dutch healthcare, accounting for 80%. A culture of cautious
prescribing has been built up over decades through general
practitioners acceptance of strict professional guidance.
Indications for use, type, and dosage are issued by the College
of General Practitioners (NHG). Recent statistics show use is
continuing to decline, with a 6% fall recorded between 2011
and 2014 in daily doses of antibiotics dispensed by pharmacies.8
Jaap van Dissel, director of the Centre for Infectious Disease
Control at the National Institute for Public Health and the
Environment, says: GPs are convinced that many indications
should not be treated with an antibiotic, even though they are
in other countries. He cites the example of acute otitis media
in children.
We know from studies that the positive benefits of antibiotics
are limited. The infection causes a couple of hours pain, which
could be treated by paracetamol,9 he says.
Roger Damoiseaux, professor of general practice at Utrecht
University Medical Centre, helped draw up the NHG guidelines
advising against using antibiotics in children aged over 2 years
for common problems, including tonsillitis and sinusitis. He
has seen rates of antibiotic use fall for these conditions since
1990. Younger GPs, in particular, prescribe less. The guidelines
are really working. Training, since [the guidelines] came out,
has played a major part in bringing down the rates of
unnecessary prescribing.
Yet the Netherlands continues to push for a further 50%
reduction in both incorrect prescribing and avoidable healthcare
For personal use only: See rights and reprints http://www.bmj.com/permissions
related infection from 2015 to 2020. It has recently launched a
publicity campaign to increase national awareness of the need
to avoid using antibiotics whenever possible.
Can other countries follow the Dutch
example?
The Dutch are fortunate. Their country and population are
relatively small, perhaps making it easier to bring all the
necessary players on board to cooperate in a One Health
approach. Dutch hospital architecture allows for the option of
single rooms, so patients can be easily isolated to control
outbreaks of infection such as Clostridium difficile. Dutch
farmers all have computerised systems, unlike in many countries,
which allow monitoring and comparisons of antibiotic use.
The Dutch also consciously decided to make antimicrobial
resistance a priority sooner than most countries. Decades of
work on hospital infection through the Prevention Working
Group and promoting prudent antimicrobial use through the
Working Party on Antibiotic Policy (http://www.swab.nl/
english) means that these issues are foremost in the minds of
the professionals, says van Dissel.
In some countries the agricultural sector may be a reluctant to
act if it is more cost effective to use preventive antibiotics at
moments of risk, such as when weaning piglets, than to take
measures to improve hygiene. Meanwhile Meviuss plea to act
everywhere is easier to ignore if multidrug resistant Klebsiella
or MRSA is already endemic in hospitals.
Although actions have to fit the cultural context of each
country, Van Dissel fears that in some it is a less important
topic than others. We are now at a point where we need to
convince policy makers, including on a European level, that
these are important issues. It is a matter of the priorities of the
politicians.
In the UK, the Department for Environment, Food and Rural
Affairs is leading a five year antimicrobial resistance strategy
in animals for 2013-18.10 This encourages good farm
management, biosecurity, and animal husbandry to reduce the
risk of disease and minimise the need for antibiotic use in
animals. In May, a review of antimicrobial resistance by
economist Jim ONeill commissioned by the UK government
and the Wellcome Trust, highlighted reducing the extensive
and unnecessary use of antibiotics in agriculture as one of four
main interventions.11
Whether the EU health ministers agreement under the Dutch
presidency will give the One Health approach a further boost
in the post-Brexit UK remains to be seen. But it has been largely
welcomed elsewhere.
Sascha Marschang, policy manager of the Brussels based
network of not-for-profit health organisations, the European
Public Health Alliance, told The BMJ that while the agreement
the Dutch achieved during their EU presidency was progress,
she feared the plans risk not being concrete enough for the
scale and urgency of the threat. Crucially, she urged that
stronger legislation is needed to remove any financial incentives
to individuals and institutions to use antimicrobials gratuitously.
Instead, across Europe, vets and farmers should rather be
incentivised to reduce prophylactic use and improve animal
welfare to reduce the need for antimicrobials.
The Dutch believe that the US and Canada are also following
their achievements with interest. Any solution would need to
be global. The ONeill report pointed out that in the US, 70%
(by weight) of antibiotics defined as medically important for
Subscribe: http://www.bmj.com/subscribe
BMJ 2016;354:i4192 doi: 10.1136/bmj.i4192 (Published 3 August 2016)
Page 3 of 3
FEATURE
humans by the Food and Drug Administration, were sold for
use in animals.
Dutch health minister Schippers highlighted the importance of
international action to her EU colleagues at the June meeting.
She stressed that antibiotic resistance would be on the agenda
for the United Nations General Assembly in New York this
September. She and other Dutch representatives will be there.
Competing interests: I have read and understood BMJ policy on
declaration of interests and have no relevant interests to declare.
Provenance and peer review: Commissioned; not externally peer
reviewed.
1
European Centre for Disease Prevention and Control, European Food Safety Authority,
European Medicines Agency. ECDC/EFSA/EMA first joint report on the integrated analysis
of the consumption of antimicrobial agents and occurrence of antimicrobial resistance in
bacteria from humans and food-producing animals. EFSA J 2015;13:4006doi:10.2903/j.
efsa.2015.4006.
Mevius D, Heerderik D. Reduction of antibiotic use in animals lets go Dutch.J Verbr
Lebensm 2014;9:177. doi:10.1007/s00003-014-0874-z.
For personal use only: See rights and reprints http://www.bmj.com/permissions
3
4
5
6
7
8
9
10
11
Speksnijder DC, Mevius DJ, Bruschke CJ, Wagenaar JA. Reduction of veterinary
antimicrobial use in the Netherlands. The Dutch success model. Zoonoses Public Health
2015;62(Suppl 1):79-87. doi:10.1111/zph.12167. pmid:25421382.
European Council. Council conclusions on the next steps under a One Health approach
to combat antimicrobial resistance. Press release, 17 Jun 2016. www.consilium.europa.
eu/en/press/press-releases/2016/06/17-epsco-conclusions-antimicrobial-resistance.
Grave K, Torren-Edo J, Mackay D. Comparison of the sales of veterinary antibacterial
agents between 10 European countries. J Antimicrob Chemother 2010;65:2037-40. doi:
10.1093/jac/dkq247 pmid:20587611.
Sheldon T. Dutch doctors warn of dangers of overuse of antibiotics in farming. BMJ
2010;341:c5677. doi:10.1136/bmj.c5677.
CBS. Within Europe, antibiotics use lowest in the Netherlands. https://www.cbs.nl/en-gb/
news/2016/06/within-europe-antibiotics-use-lowest-in-the-netherlands.
ZonMw. Antibiotic resistance programme. 2015. http://www.zonmw.nl/uploads/tx_
vipublicaties/Prorammatekst_Antibiotica_Resistentie.pdf).
Van Buchem FL, Dunk JH, vant Hof MA. Therapy of acute otitis media: myringotomy,
antibiotics, or neither? A double-blind study in children. Lancet 1981;318:883-7.http://
www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=6117681&
dopt=Abstractdoi:10.1016/S0140-6736(81)91388-X.
Department of Health. Department of Food Agriculture and Rural Affairs, UK five year
antimicrobial resistance strategy 2013 to 2018. www.gov.uk/government/uploads/system/
uploads/attachment_data/file/244058/20130902_UK_5_year_AMR_strategy.pdf.
Review on microbial resistance. Tackling drug-resistant infections globally: final report
and recommendations. May 2016. http://amr-review.org/.
Published by the BMJ Publishing Group Limited. For permission to use (where not already
granted under a licence) please go to http://group.bmj.com/group/rights-licensing/
permissions
Subscribe: http://www.bmj.com/subscribe
You might also like
- A Study of AntsDocument2 pagesA Study of Antsrj99masterNo ratings yet
- Armoury of The ExoditesDocument1 pageArmoury of The Exoditesrj99masterNo ratings yet
- 5IT01 01 Que 20110110Document24 pages5IT01 01 Que 20110110rj99masterNo ratings yet
- 5IT01 01 Que 20110110Document24 pages5IT01 01 Que 20110110rj99masterNo ratings yet
- 2.2.3 Amylase PH ProcedureDocument15 pages2.2.3 Amylase PH Procedurerj99masterNo ratings yet
- Siri Guru Granth Sahib, RomanizedDocument1,432 pagesSiri Guru Granth Sahib, Romanizedrj99masterNo ratings yet
- 40k Army List Eldar1000Document2 pages40k Army List Eldar1000rj99masterNo ratings yet
- EldarDocument2 pagesEldarrj99masterNo ratings yet
- Change LogDocument2 pagesChange Logrj99masterNo ratings yet
- EldarDocument2 pagesEldarrj99masterNo ratings yet
- EldarDocument2 pagesEldarrj99masterNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Behavioral Pain Scale (BPS) For Pain Assessment in Intubated Patients - MDCalcDocument2 pagesBehavioral Pain Scale (BPS) For Pain Assessment in Intubated Patients - MDCalcJeane SuyantoNo ratings yet
- Very Early Signs and SymptomsDocument3 pagesVery Early Signs and SymptomsMichelle TeodoroNo ratings yet
- Urinalysis in Children and Adolescents, (2014)Document11 pagesUrinalysis in Children and Adolescents, (2014)Enrique MANo ratings yet
- Safety Culture AHRQDocument8 pagesSafety Culture AHRQangga rizkiNo ratings yet
- 2014 Final With Answers: 10000 SeriesDocument36 pages2014 Final With Answers: 10000 SeriesMareeswaranNo ratings yet
- Raynaud'S Phenomenon: Dr. Ajay Panwar Japi (May 2010)Document23 pagesRaynaud'S Phenomenon: Dr. Ajay Panwar Japi (May 2010)Ajay PanwarNo ratings yet
- Syndrome Differentiation According To The Eight Principles - TCM Basic Principles ShennongDocument5 pagesSyndrome Differentiation According To The Eight Principles - TCM Basic Principles ShennongYi-Ying LuNo ratings yet
- Recommended Procedures For Doctors and Nurse in The Management of Kawasaki DiseaseDocument34 pagesRecommended Procedures For Doctors and Nurse in The Management of Kawasaki DiseaseJOSHUA DICHOSONo ratings yet
- Chest Physiotherapy For Pneumonia in ChildrenDocument30 pagesChest Physiotherapy For Pneumonia in ChildrenristaseptiawatiningsihNo ratings yet
- 2018 HIV GuidelinesDocument125 pages2018 HIV GuidelinesAndrew KaumbaNo ratings yet
- 7 Stars Doctors Required by WHO and FKUIDocument2 pages7 Stars Doctors Required by WHO and FKUIWidya Ayu92% (12)
- Essay About Why We Need Physiology in Our LifeDocument8 pagesEssay About Why We Need Physiology in Our LifeWendelieDescartinNo ratings yet
- Different Therepeutic Category of Drugs and Its Example Drug ProductsDocument8 pagesDifferent Therepeutic Category of Drugs and Its Example Drug ProductsGermie PosionNo ratings yet
- PR Truenat WHO Endorsement 02072020Document4 pagesPR Truenat WHO Endorsement 02072020KantiNareshNo ratings yet
- Pfeiffer 5 Ppts Chapter05 - The Psychology of Injury (Student Copy)Document13 pagesPfeiffer 5 Ppts Chapter05 - The Psychology of Injury (Student Copy)api-287615830No ratings yet
- Pulmonary FibrosisDocument4 pagesPulmonary FibrosisDimpal Choudhary100% (2)
- DesenteryDocument3 pagesDesenteryAby Gift AnnNo ratings yet
- Heparin and WarfarinDocument2 pagesHeparin and WarfarinBaeyer100% (1)
- Immune Thrombocytopenia: Causes of Secondary ITPDocument3 pagesImmune Thrombocytopenia: Causes of Secondary ITPkrataiwanNo ratings yet
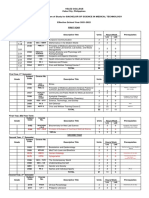
- Velez College Cebu City, Philippines: GEC - PC GEC - MMW Pmls 1Document3 pagesVelez College Cebu City, Philippines: GEC - PC GEC - MMW Pmls 1Armyl Raul CanadaNo ratings yet
- CA A Cancer J Clinicians - 2018 - Bray - Global Cancer Statistics 2018 GLOBOCAN Estimates of Incidence and MortalityDocument31 pagesCA A Cancer J Clinicians - 2018 - Bray - Global Cancer Statistics 2018 GLOBOCAN Estimates of Incidence and MortalityAngelia Adinda AnggonoNo ratings yet
- Covid-19 Pandamic by PriyanshDocument5 pagesCovid-19 Pandamic by PriyanshShri ram PujariNo ratings yet
- RPT - 54 - Stereotactic Radiosurgery PDFDocument50 pagesRPT - 54 - Stereotactic Radiosurgery PDFMaría José Sánchez LovellNo ratings yet
- Discharge PlanDocument1 pageDischarge PlanGail GenturalezNo ratings yet
- Community Health Nursing Vs Public Health NursingDocument1 pageCommunity Health Nursing Vs Public Health NursingAnnalisa Telles100% (2)
- Thesis SumaryDocument7 pagesThesis SumaryAnonymous hnIkb5No ratings yet
- BSC Nursing: Medical Surgical Nursing - I Unit V - Disorders of The Cardio Vascular SystemDocument36 pagesBSC Nursing: Medical Surgical Nursing - I Unit V - Disorders of The Cardio Vascular SystemPoova RagavanNo ratings yet
- Example - Pharmacist Care PlanDocument10 pagesExample - Pharmacist Care PlanHOD ODNo ratings yet
- 1cardiovascular and Pulmonary Physical TherapyDocument347 pages1cardiovascular and Pulmonary Physical TherapyLiviu CuvoiNo ratings yet
- Felix Widal TestDocument9 pagesFelix Widal TestGaluhAlvianaNo ratings yet