Professional Documents
Culture Documents
Etiology Ascites
Uploaded by
ponekCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Etiology Ascites
Uploaded by
ponekCopyright:
Available Formats
Turk J Gastroenterol 2005; 16 (3): 171-173
Severe exudative ascites as an initial presentation of
Crohns disease
Crohn hastalnda ilk bavuru yaknmas olarak ciddi eksudatif asid
Fatih TEKN, Sezgin VATANSEVER, mer ZTEMZ, Ahmet MUSOLU, Tankut LTER
Department of Gastroenterology, Ege University Medical School, zmir
Ascites in the course of Crohns diseases is rarely seen and usually is a result of a concomitant malignancy, infection or thrombosis of portal or hepatic veins. In this article, a 55-year-old female patient suffering from severe ascites and finally diagnosed
as Crohns disease is presented. Further investigations revealed
no malignancy, peritoneal infection or vein thrombosis. Treatment of Crohns disease with steroids and 5-aminosalicylic acid
also resulted in the disappearance of the ascites.
Crohn hastal seyrinde asit nadiren grlr ve genellikle elik eden bir maligniteye, enfeksiyona veya portal veya hepatik
ven trombozuna bal geliir. Bu yazda, asit ile prezente olup
Crohn hastal tans alan 55 yanda kadn olgu sunulmaktadr. leri incelemelerde herhangi bir malignite, peritoneal enfeksiyon veya ven trombozu saptanmamtr. Crohn hastalna
ynelik uygulanan steroid ve 5-aminosalisilik asit ile olgunun
asidi de kaybolmutur.
Key words: Ascites, Crohns disease, etiology, malignancy,
thrombosis
Anahtar kelimeler: Asit, Crohn hastal, etyoloji, malignite,
tromboz
INTRODUCTION
Crohns disease is a chronic inflammatory granulomatous disease of the gastrointestinal tract. The
well-known associated hypercoagulability may
contribute to occurrence of portal or hepatic vein
thrombosis which may result in ascites (1, 2). In
addition, chronic inflammation is thought to contribute to the development of malignancy, particularly lymphoma, in patients with Crohns disease.
These patients with malignancy may also present
with ascites (3, 4). Furthermore, infections may also be one of the etiological factors of ascites. However, ascites in the course of Crohns disease without any other cause is rare, and still has unknown
mechanism(s) (5, 6). We present a patient with
Crohns disease with exudative ascites as an initial presentation without any other cause.
CASE REPORT
A 55-year-old female patient was admitted to our
department with a 10-day episode of bloody diarrAddress for correspondence: Fatih TEKN
Ege University Medical School, Department of Gastroenterology,
Bornova 35100, zmir, Turkey
Phone: +90 232 343 43 43/4101 Fax: +90 232 342 77 64
E-mail: drtekinfatih@yahoo.com
hea occurring four to six times per day and associated with abdominal pain. Her history revealed no
recent travel or use of antibiotics. Family history
was negative for inflammatory bowel disease. At
admission, her physical examination was unremarkable except for the presence of ascites. Her
abdomen was distended and tenderness with a fluid wave was detected during percussion. Blood
pressure was 110/60 mmHg, temperature 36.5C,
and pulse rate 82/min. The laboratory findings revealed anemia due to chronic disease (Table 1).
Folate and vitamin B12 levels were normal. Albumin level was in normal ranges. Erythrocyte sedimentation rate was 48 mm/hour and C-reactive
protein was 2.9 mg/dl (normal: <0.5 mg/dl). Liver
and renal function tests, electrolytes, and urinalysis were normal. Tests for antinuclear antibody
and anti-double-stranded DNA were negative.
Stool culture was negative three times. The purified protein derivatives test revealed a negative reaction 3 mm in diameter.
Manuscript received: 28.01.2005 Accepted: 15.03.2005
172
TEKN et al.
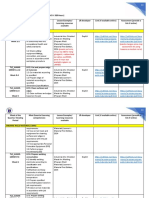
Table 1. Laboratory data of peripheral blood and ascites on admission
Peripheral blood
White blood cell
Hemoglobin
Hematocrit
Platelet count
Total protein (6.5-8.5 g/dl)
Albumin (3.5-5.0 g/dl)
Iron (50-140 g/dl)
Transferrin saturation
Ferritin (13-150 ng/ml)
LDH (230-460 U/l)
7700/mm3
7.8 g/dl
26%
349x103/mm3
6g/dl
3.3g/dl
11g/dl
35%
148ng/ml
280U/L
Ascites
White blood cell
Culture
PCR for tuberculosis
Culture for tuberculosis
Total protein (g/dl)
Albumin (g/dl)
SAAG
Cytology
Glucose
LDH
100/mm3
negative
negative
negative
4 g/dl
2.6 g/dl
0.7
benign
76g/dl
170U/L
PCR: Polymerase chain reaction, SAAG: Serum-ascites albumin gradient, LDH: Lactate dehydrogenase
Abdominal ultrasonography confirmed the ascites
and revealed normal echo and size of the liver, and
no thrombosis of hepatic or portal vein was detected by Doppler ultrasonography. Serum-ascites albumin gradient (SAAG) was 0.7, which strongly
excluded portal hypertension. Analysis of ascitic
fluid showed no bacterial or tuberculous infection
(Table 1). In addition, cytological examination of
the ascitic fluid was repeatedly negative for malignancy. Meanwhile, two units of erythrocyte replacement were performed because of severe anemia.
Upper gastrointestinal system endoscopy was normal. Laparoscopy showed no pathological finding
to identify the etiology of ascites. Colonoscopy revealed normal mucosa of the colon until the cecum. There was severe mucosal inflammation at
the cecum including friability, hyperemia and extensive ulcers. Histopathological examination of
the specimen obtained from the cecum corroborated the inflammation, and polymerase chain reaction (PCR) for tubercle bacilli was negative. The
radiography of the small bowel with air contrast
Figure 1. The radiography of the small bowel with air contrast
barium enema. Note the luminal narrowing and mucosal ulceration at the level of the terminal ileum (small arrow) and cecum
(big arrow)
barium enema showed thickening of the bowel
wall, luminal narrowing, and mucosal ulceration
at the level of the terminal ileum and cecum,
which was consistent with Crohns disease (Figure 1). She was diagnosed as Crohns disease with
these clinical, colonoscopical, histopathological
and radiological features. Treatment with steroid
(40 mg/day), and 5-aminosalicylic acid (2 g/day)
was started. The patient was given no antibiotics,
diuretics or albumin replacement. Her symptoms
began to diminish in the 1st week and disappeared
in the 3rd week of the treatment. In addition, near
disappearance of the ascites was observed in the
3rd week of the treatment. The patient is still free
of symptoms and there has been no recurrence of
ascites after three months of follow-up.
DISCUSSION
Ascites in the course of Crohns disease is an unexpected complication, and few cases are reported in
the literature. Some cases with ascites have also
had hepatic or portal vein thrombosis since hypercoagulability exists in patients with Crohns disease. In a recently published study, 98 cases with
inflammatory bowel disease and confirmed deep
venous thrombosis or pulmonary embolism were
checked for thrombophilic state. The authors reported that thrombophilia was present in 33% of
the 40 patients tested (7). The prevalence of Leiden mutation, the most common inherited thrombophilic state, was reported as 14.28% in Crohn's
disease in another study (8). Magro et al. found
that the frequency of two or more thrombophilic
abnormalities was related to disease activity in
Crohn's disease (9). Thus, when a patient with
Crohns disease suffers from ascites, presence of
portal or hepatic vein thrombosis has to be kept in
mind. Tsujikawa et al. reported a patient with
Crohns disaese and portal vein thrombosis which
was successfully treated with anticoagulant
Exudative ascites in Crohns disease
therapy (2). In our patient, Doppler ultrasonography was performed and revealed no thrombosis
of portal or hepatic veins. In addition, SAAG was
smaller than 1.1, which excluded portal hypertension. Hypoalbuminemia may cause ascites in patients with Crohns disease, but serum albumin level was in normal ranges in our patient. Since SAAG was smaller than 1.1, we especially focused on
malignancy and infections. Another known etiology of ascites in the course of Crohns disease is
malignancy, especially lymphoma (3, 4). It is thought that chronic inflammation contributes to the
development of lymphoma in patients with
Crohns disease. In our patient, repeated cytological examinations of the ascitic fluid revealed no
malignancy, and microbiological investigations
showed no bacterial or tuberculous infection. Furthermore, laparoscopy excluded both peritonitis
carcinomatosis and peritoneal infection. No cause
of the ascites except Crohns disease itself was found. To our knowledge, only two cases with
Crohns diseases and severe exudative ascites ha-
173
ve been reported in the literature previously (5, 6).
It can be speculated that the inflammatory nature
of Crohns disease may be the reason for the associated ascites via transmural inflammation and/or
lymphatic stasis. If so, ascites would usually be seen in patients with Crohns disease when it is more severe or exacerbated. However, to our observation, ascites does not appear in most of the patients at the exacerbation time of Crohns disease.
Thus, it is difficult to explain the occurrence mechanism(s) of ascites by only severity of the disease.
On the other hand, treatment of Crohns disease
with anti-inflammatory drugs without any antibiotics, diuretics or albumin replacement resulted in
the disappearance of ascites in our patient.
In conclusion, occurrence mechanism(s) of ascites
in the course of Crohns disease remains unknown.
Treatment of Crohns disease with anti-inflammatory drugs may result in dramatic disappearance
of ascites; however, further investigations with
large series are needed.
REFERENCES
1. Witteman BJ, Weterman IT, Griffioen G, et al. Intestinal
obstruction caused by non-absorbable tablets and BuddChiari syndrome in a patient with Crohn's disease. Ned
Tijdschr Geneeskd 1991; 135(17): 766-9.
2. Tsujikawa T, Ihara T, Sasaki M, et al. Effectiveness of combined anticoagulant therapy for extending portal vein
thrombosis in Crohn's disease. Report of a case. Dis Colon
Rectum 1996; 39(7): 823-5.
3. Perosio PM, Brooks JJ, Saul SH, et al. Primary intestinal
lymphoma in Crohn's disease: minute tumor with a fatal
outcome. Am J Gastroenterol 1992; 87(7): 894-8.
4. Hara T, Ozaki S, Kosaka M, et al. Biclonal lymphoplasmacytic immunocytoma associated with Crohn's disease.
Intern Med 1999; 38(6): 500-3.
5. Aparicio Tormo JR, Laveda R, Gomez Andres A. Crohn's disease and ascites. Gastroenterol Hepatol 2000; 23(8): 384-8.
6. Paspatis GA, Kissamitaki V, Kyriakakis E, et al. Ascites
associated with the initial presentation of Crohn's disease.
Am J Gastroenterol 1999; 94(7): 1974-6.
7. Solem CA, Loftus EV, Tremaine WJ, et al. Venous thromboembolism in inflammatory bowel disease. Am J Gastroenterol 2004; 99(1): 97-101.
8. Mozsik G, Figler M, Gasztonyi B, et al. Prevalence of Leiden mutation in various gastrointestinal disorders. Orv
Hetil 2002; 143(9): 447-50.
9. Magro F, Dinis-Ribeiro M, Araujo FM, et al. High prevalence of combined thrombophilic abnormalities in patients
with inflammatory bowel disease. Eur J Gastroenterol Hepatol 2003; 15(11): 1157-63.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Strategies Hospitalists Can Take To Prevent Antibiotic ResistanceDocument10 pagesStrategies Hospitalists Can Take To Prevent Antibiotic ResistanceponekNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Fetal Monitor WirelessDocument1 pageFetal Monitor WirelessponekNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Resource Job Aid Excluding PregnancyDocument2 pagesResource Job Aid Excluding PregnancyponekNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Checklist Dmpa EnglishDocument3 pagesChecklist Dmpa EnglishponekNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Kanker ServiksDocument308 pagesKanker ServiksponekNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Sadiq KhanDocument5 pagesSadiq KhanponekNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Kanker ServiksDocument308 pagesKanker ServiksponekNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Lesi Pra Kanker Serviks LeafletDocument1 pageLesi Pra Kanker Serviks LeafletponekNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Amniotic Laser PhotocoagulationDocument18 pagesAmniotic Laser PhotocoagulationponekNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Sadiq KhanDocument5 pagesSadiq KhanponekNo ratings yet
- Resource Checklists Screening Clients Who Want Initiate Use LNG Ius English 2017Document3 pagesResource Checklists Screening Clients Who Want Initiate Use LNG Ius English 2017ponekNo ratings yet
- Checklist Iud EnglishDocument3 pagesChecklist Iud EnglishponekNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Conization of The CervixDocument5 pagesConization of The CervixponekNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Checklist Iud EnglishDocument3 pagesChecklist Iud EnglishponekNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Caesarean SectionDocument51 pagesCaesarean SectionFebrinata MahadikaNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Skripsi Tanpa Bab PembahasanDocument84 pagesSkripsi Tanpa Bab PembahasanponekNo ratings yet
- Scientific Schedule: Alarm Course Day 1Document11 pagesScientific Schedule: Alarm Course Day 1ponekNo ratings yet
- Skripsi Tanpa Bab PembahasanDocument84 pagesSkripsi Tanpa Bab PembahasanponekNo ratings yet
- Scientific Schedule: Alarm Course Day 1Document11 pagesScientific Schedule: Alarm Course Day 1ponekNo ratings yet
- BF and Early Nutrition Mother DMDocument44 pagesBF and Early Nutrition Mother DMponekNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- NCDsDocument40 pagesNCDsponekNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Pharmacology Cardiovascular1Document33 pagesPharmacology Cardiovascular1ponekNo ratings yet
- REFERAT - Neonatal HSV InfectionDocument5 pagesREFERAT - Neonatal HSV InfectionponekNo ratings yet
- Preclinical Condition MagementDocument27 pagesPreclinical Condition MagementponekNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Resus - Makrosomia (Ardicho) - REFERAT Macrosomia Prediction Using USGDocument4 pagesResus - Makrosomia (Ardicho) - REFERAT Macrosomia Prediction Using USGponekNo ratings yet
- Guidline TetanusDocument363 pagesGuidline TetanusferianaNo ratings yet
- BF and Early Nutrition Mother DMDocument44 pagesBF and Early Nutrition Mother DMponekNo ratings yet
- REFERAT - Check List VBAC Antenatal Periode PDFDocument2 pagesREFERAT - Check List VBAC Antenatal Periode PDFponekNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- REFERAT - Neonatal HSV InfectionDocument5 pagesREFERAT - Neonatal HSV InfectionponekNo ratings yet
- Pengendalian Pengadaan Alat Kesehatan Habis Pakai di RSBTDocument12 pagesPengendalian Pengadaan Alat Kesehatan Habis Pakai di RSBTponekNo ratings yet
- Management of Infant with GastroschisisDocument2 pagesManagement of Infant with GastroschisisAnonymous 9wHscMNo ratings yet
- (FC) Ayesha Dhanani A19091Document10 pages(FC) Ayesha Dhanani A19091Iqbal PatelNo ratings yet
- Grade 9 12 SMAWDocument10 pagesGrade 9 12 SMAWFlor Gagasa100% (4)
- Efects of Family Demographics and The Passage of Time On Parents' Difficulty With Their Lesbian, Gay or Bisexua Youth's Sexual OrientationDocument8 pagesEfects of Family Demographics and The Passage of Time On Parents' Difficulty With Their Lesbian, Gay or Bisexua Youth's Sexual OrientationGamer BoyNo ratings yet
- Unidade 1 Texto: Know Your Brain: Mirror Neurons - SIMULADODocument2 pagesUnidade 1 Texto: Know Your Brain: Mirror Neurons - SIMULADOJoseano SouzaNo ratings yet
- Chapter - 036 Urinay DisordersDocument8 pagesChapter - 036 Urinay DisordersClaudina CariasoNo ratings yet
- ISEF GuidelinesDocument26 pagesISEF GuidelinesShinjiro OdaNo ratings yet
- Apgvb Insurance Consent LetterDocument1 pageApgvb Insurance Consent LetterMahesh PasupuletiNo ratings yet
- Fundamental of Nursing 1st Semester BSN Notes, Educational PlatformDocument526 pagesFundamental of Nursing 1st Semester BSN Notes, Educational PlatformFatima FaisalNo ratings yet
- Gravida para WorksheetDocument1 pageGravida para WorksheetJulie RobertsonNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Effect of Therapeutic Exercises On Pregnancy-Related Low Back Pain and Pelvic Girdle Pain: Secondary Analysis of A Randomized Controlled TrialDocument7 pagesEffect of Therapeutic Exercises On Pregnancy-Related Low Back Pain and Pelvic Girdle Pain: Secondary Analysis of A Randomized Controlled TrialSUCIUNo ratings yet
- November Pulse 2021Document4 pagesNovember Pulse 2021api-303444111No ratings yet
- Zomeo Mobile AppDocument23 pagesZomeo Mobile AppDr. KaarthikaNo ratings yet
- TONG HOP TOT NGHIEP 9 TestsDocument28 pagesTONG HOP TOT NGHIEP 9 TestsPhuong Mai TranNo ratings yet
- GAD7Document2 pagesGAD7Alice Bonnie CaulfieldNo ratings yet
- Medical Economics Magazine PDFDocument41 pagesMedical Economics Magazine PDFxtineNo ratings yet
- Q1-Lesson 2 Module 5-Prepare Client For Hair BleachingDocument23 pagesQ1-Lesson 2 Module 5-Prepare Client For Hair Bleachingveniflor gerardoNo ratings yet
- SEO-Optimized title for mercury-sulfur system Pourbaix diagram dataDocument18 pagesSEO-Optimized title for mercury-sulfur system Pourbaix diagram dataFiorelaRosarioJimenezLopezNo ratings yet
- Quantitative Risk Assessment of Incident ScenariosDocument34 pagesQuantitative Risk Assessment of Incident ScenariosAmol LakareNo ratings yet
- Suicide Awareness and PreventionDocument4 pagesSuicide Awareness and PreventionKeerthi RajpurohitNo ratings yet
- PE.4 - BPEd2NUÑEZ, MYRADocument25 pagesPE.4 - BPEd2NUÑEZ, MYRANuñez MyraNo ratings yet
- Pediatrics Nursing UnitDocument43 pagesPediatrics Nursing UnitShweta SainiNo ratings yet
- Viktor Frankl: Dr. C. George Boeree DR C. George Boeree Shippensburg University Universitas ShippensburgDocument20 pagesViktor Frankl: Dr. C. George Boeree DR C. George Boeree Shippensburg University Universitas Shippensburgs4f11snNo ratings yet
- Arcadis Orbic Arcadis Orbic 3D: Designed For Enhanced Surgical PrecisionDocument24 pagesArcadis Orbic Arcadis Orbic 3D: Designed For Enhanced Surgical PrecisionHeidi BlueNo ratings yet
- Premium Metal-Guard® 65, 75, 100, 150 MSDSDocument2 pagesPremium Metal-Guard® 65, 75, 100, 150 MSDSrahul chandranNo ratings yet
- Evolve 5 - Mid Term Test ReviewDocument9 pagesEvolve 5 - Mid Term Test ReviewLaiza Godoy100% (3)
- Jeltrate Dustless: Dustless Alginate Impression Material Regular Set and Fast SetDocument10 pagesJeltrate Dustless: Dustless Alginate Impression Material Regular Set and Fast SetGuillermo Delgadillo RochaNo ratings yet
- Manage Pneumonia through Appropriate Nursing InterventionsDocument1 pageManage Pneumonia through Appropriate Nursing InterventionsNora BacolNo ratings yet
- Mizo Hmeichhe Tangrual PawlDocument42 pagesMizo Hmeichhe Tangrual PawlLalliantluanga HauhnarNo ratings yet
- What Is A Lobotomy, History, Uses and SummaryDocument8 pagesWhat Is A Lobotomy, History, Uses and SummaryHussain AfzalNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)