Professional Documents
Culture Documents
Management of Electrical Burn
Uploaded by
Nurul Dwi UtamiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Management of Electrical Burn
Uploaded by
Nurul Dwi UtamiCopyright:
Available Formats
Indian J Surg (JulyAugust 2013) 75(4):278283
DOI 10.1007/s12262-012-0476-x
ORIGINAL ARTICLE
The Management of Electrical Burn
Ashok Surybhanji Gajbhiye & Mona M. Meshram &
Rekha S. Gajaralwar & Amrish P. Kathod
Received: 8 November 2011 / Accepted: 26 March 2012 / Published online: 22 May 2012
# Association of Surgeons of India 2012
Abstract Aim of treatment is to achieve skin cover to
prevent infection and to allow early mobilization. Electrical
injuries are a relatively uncommon. Adult electrical injuries
usually occur as an occupational hazard, whereas children
are primarily injured accidently. The spectrum of electrical
injury is very broad, ranging from minimal injury to severe
multiorgan involvement, with both occult and delayed complications and death. This is a prospective study from Indira
Gandhi Government Medical College, Nagpur. A total of 98
patients presenting from June 2002 to September 2011 were
included. Patients were treated with surgical excision 31
(31.63 %), fasciotomy 26 (26.53 %), escharotomy 87
(88.78 %), and amputation 12 (12.24 %). In all patients
debridement was performed. After follow-up, there was
8.16 % (8 patients) mortality. Minimal mortality may be due
to less surface area involved or no visceral injury. Patients
survived with morbidity due to amputation. Initial management of electrical burn is imperative to optimize function and
minimize long-term scarring. However, further studies are
required regarding flap repair and microsurgery to minimize
the rate of amputation.
A. S. Gajbhiye (*) : M. M. Meshram : R. S. Gajaralwar :
A. P. Kathod
Department Of General Surgery,
Indira Gandhi Govt. Medical College,
Central Avenue road,
Nagpur -18 Maharashtra, India
e-mail: gsashok72@yahoo.in
A. S. Gajbhiye
e-mail: gsashok1972@gmail.com
Keywords Escharotomy . Debridement . Fasciotomy .
Amputation
Introduction
Approximately 1,000 deaths per year are due to electrical injuries in the United States, with a mortality rate of
35 %. Electrical injuries are estimated to cause approximately 5001000 deaths per year in the United States
[15].
In the laparoscopic and robotic era, different types of
electrical apparatuses are responsible for accidents. Sometimes this is due to the development of a defect in the
insulation and therefore a frayed wire causes a short circuit,
but sometimes it is due to faulty construction of assembly.
Thus, in some instances it is found that the onoff switch
has been incorrectly in the neutral instead of the live wire
and therefore the element remains live even when the switch
is in the off position. Destruction of human tissue by highvoltage electrical burn is very severe. Visceral injury is
possible when the abdominal wall is involved, and early
diagnosis and proper treatment of the injury are then very
important (Figs. 1 and 2).
Pathophysiology and natural history of electrical injury
have been well described. The tissue destruction is often
severe and progressive due to vascular injury and prolonged
production of thromboxanes induced by the electric current.
The involvement of the abdominal wall may result in severe
destruction of the wall itself and even the visceral organs.
The gall bladder, liver, pancreas, intestine, and colon may all
be involved [1, 2, 6].
Indian J Surg (JulyAugust 2013) 75(4):278283
Fig. 1 High-voltage electric
burns al
279
ILLUSTRATIONS:-
a) day-1
c] day-1 entry[l]
b) day-14
d] day-11
e] day-13
h] day-14
g] day-1 abdominal wall
i] day-1,great toe[r]
f] day-14
j] day-13
k] day- exit wound
L] day 13
L] day1 small patches over knee
It is true that high temperature may be produced by the
passage of electric current through the tissues, but the natural history of electric burn differs so clearly from that of
thermal burn that it is impossible to avoid the conclusion
that some specific effect is at least partially responsible for
damage. The skin wound of an electrical burn is clearly
circumscribed to the area of contact and this skin is dead
(Fig. 3). Deep to the skin, the area of injury extends toward
the other point of contact with destruction of deeper tissues.
Because of their fluid content, main vessels form good
280
Indian J Surg (JulyAugust 2013) 75(4):278283
Results
Bar diagram- location of electrical burn
Entry
Exit
After Excetion
Fig. 2 Low-voltage electric burns
conduction and thrombosis of digital or other main vessels
may occur with important consequences.
This article reviews the pathophysiology, clinical features,
and treatment of patients with electrical burns. The clinical
features and management are discussed and the literature is
reviewed.
DOUGHNUT-Surgical treatment of electrical burn
Patients and Methods
This is a prospective study of 98 patients with electrical burn
injuries admitted to Indira Gandhi Government Medical
College, Nagpur. Of 98 patients, 92 patients were admitted
to the burn unit and 6 patients were admitted to the medicine
intensive care unit. Those with an electrical injury were
included in this study, and burns including scald, chemical,
explosive, lightening, and thermal burn were excluded from
this study.
Once the patient is stabilized, the extent and depth of
the burn is assessed. Routine laboratory investigation
urine-myoglobinuria, creatine kinase level, a 12-lead
electrocardiograph, and cardiac enzyme levelswas
done to assess for cardiac arrhythmias and direct cardiac
injury. X-ray abdomen standing was performed to detect
bowel perforation. Color Doppler examination was done
in ischemia.
Discussion
A total of 98 patients of electrical burn were included in this
study which comprised 63 males (64.29 %) and 35 females
(34.3 %). Mean age was 35.5 years in a range of 368 years.
Maximum 17 patients (17.35 %) were presented in the year
2004 and minimum 2 patients (2.04 %) were present in the
year 2002. Electrical injuries exist among the very young
children (<6 years) and among young and working-aged
adults [1, 710]. Patterns of electrical injury vary by age
(e.g., low-voltage household exposures among toddlers and
Fig. 3 Different types of
electrical burns
2] SUPERFICIAL ELECTRICAL BURN
1] CONTACT ELECTRIC BURN
OVER KNEES (FLASH/FERNING)
Indian J Surg (JulyAugust 2013) 75(4):278283
high-voltage exposures among risk-taking adolescents and
via occupational exposure). Rates of childhood electrical
injury are higher in boys than in girls [6]; rates of adult
injury are significantly higher in men than in women, likely
because of occupational predisposition. Most series show
more than 80 % of electrical injuries occur in men. No racial
susceptibility to electrical burns exists [7, 1113].
In more severe burn, the separation of the slough may
result in the exposure of tendon, joints, or bone, and if these
are not protected by viable flap bearing their own blood
supply, sloughing of tendons and sequestration of bone and
cartilage will follow. In domestic supply accident, although
the burn may be deep, the area of deep damage corresponds
in lateral extent approximately with the area of skin damage
and deep prolongation under intact skin is limited. Occasionally main vessels underlying or close to the burn are
seriously damaged and progressive distal thrombosis may
result in gangrene of a digit or rarely the distal part of a limb
not itself actually burned [14].
In the present study of 89 cases (87.22 %) upper limbs
were involved and of 66 cases (66.64 %) lower limbs were
involved. The abdominal wall was involved in 5 (4.9 %)
patients, but there was no evidence of intestinal perforation.
In 67 cases of low-voltage injury, no other part of body was
involved, and in 31 cases of high-voltage injury, other parts
of body were involved. In 1520 % patients, total body surface
area involvement was observed. The majority (93.88 %) were
work-related injuries, most of them (68.37 %) because of lowvoltage (<1,000 V), most frequently electrical flash burns
(64.68 %). Similar types of findings were observed in other
studies [15, 16].
In high-tension injuries, the current may pass through the
skin of the hand and up the centre of the arm as it would up the
core of a conducting cable, and widespread necrosis of forearm muscles, vessels, and nerves may be present under undamaged skin. The current in these instances often finds its
exit through the feet which may suffer comparable damage
[17, 18].
Neurological (81.6 %) and psychological (71 %) symptoms were the most common sequelae. The most frequent
neurological symptoms were numbness (42 %), weakness
(32 %), memory problems (32 %), paraesthesia (24 %), and
chronic pain (24 %). The most common psychological symptoms were anxiety (50 %), nightmares (45 %), insomnia
(37 %), and flashbacks (37 %) of the event. These findings
are comparable with those reported by different authors [3, 6,
16, 19].
In this study, immediate management is directed toward
the preservation of life.
(1) Treatment of unconsciousness: In 8 (8.16 %) cases
immediate endotracheal intubation with oxygenation was
given at once and continued until recovery occurred or
unequivocal signs of death were present.
281
(2) Shock: Surgical shock occurs only in high-tension
injuries with extensive tissue damage. In these cases, red
cell as well as plasma loss occurs and whole blood transfusion rather than plasma is indicated.
(3) Hot element burn: In this study, 5 (5.10 %) children
were suffered from electrical appliance contact burn. They
were treated by the conservative method till the slough had
separated when thin split-skin graft was applied. In another
3 (3.06 %) cases, when the area of full-thickness loss was
circumscribed, the burn was treated by early excision and
application of thick split-skin graft or Wolfe graft. And
under favorable circumstances, this primary operation may
provide a satisfactory definitive repair. Debridement was
done in the entire patients. Escharotomy was done in 87
(88.78 %) patients, and early surgical excision was performed in 23 (23.47.%) patients of low-voltage electric burn
with split-skin grafting and out of which in 6 (6.12 %)
patients, the graft failed to take due to infection. The most
common causative organism was pseudomonas. The late
surgical excision with grafting was done after 10 days in
8 (8.16 %) patients of high-voltage electrical burn. Amputation was done in 12 (12.24 %) patients of gangrene after
development of line of demarcation. Fasciotomy and subsequently secondary suturing due to fasciotomy incision were
performed in 26 (26.53 %) patients each.
Muir has suggested that treatment of more extensive
burns is often difficult and there is no general agreement
as to the best method to adopt. A brief review of the
possibilities and arguments is therefore given.
(A) Early excision and grafting: The burn is excised
down to bleeding and apparently healthy tissue and a free
graft is applied. In some instances good results are obtained,
but in others the graft fails to take, often tissue thought to be
healthy becomes necrotic and not infrequently joints and
tendon become exposed.
(B) Late excision and grafting: This is advised on the
grounds that after 1014 days it is easier to differentiate
between viable and nonviable tissues, that further necrosis
will not occur, and that grafts will take more readily. Examination of the records, however, has given no support to this
hypothesis, for loss of graft, and further necrosis has occurred even excision has been delayed as long as 21 days.
(C) Allowing spontaneous separation: This exceptionally
takes 46 weeks or more, and during the whole time the
danger of infection is present. Even when spontaneous
separation has occurred, the granulation is so unhealthy that
free grafts will often not take, exposure of tendons or joints
still occurs, and repair by flap is often necessary even after
the long delay.
(D) Excision and repair by flap: Results show that this is
a very satisfactory method with few failures and the flaps
have taken well and given good cover when used at all
periods after burning from the day of injury to the 21st
282
day. This method owes its success to the fact that a flap of
skin and fat bearing its own blood supply can resist infection
and can protect viable but damage tissue from baneful effect
of infection.
Repair by flap has a number of practical disadvantages if
distant flaps (e.g., cross arm or abdominal) have to be used.
The necessary positioning and immobilization of the hand
may interfere with active movements and may take limitation
of edema by elevation impossible. Furthermore, the patient
will usually have to remain in hospital until the flap is divided.
For these reasons, local flaps should be used whenever possible as these will permit immobilization in the position of
choice and elevation. Cross-finger flaps are very suitable for
burns of the palmer aspect of fingers and thenar flaps may be
used for burns of finger pulp. On the dorsum of the hand,
rotation or transposed flaps are of value although the limits
between safety and necrosis are narrow and the surgeon
should not be too ambitious. The palm of the hand presents
greater difficulty. The inelasticity of the skin makes true
rotation flaps unsuitable and transposed flap should be used
with the greatest discretion. For extensive lesions, direct flaps
from a distance become necessary. The opposite arm is usually a better site than the abdomen because it frequently allows
better positioning of the fingers which very easily become stiff
in extension if the hand is fixed to the abdomen.
As a rule every attempt should be made to preserve and
repair fingers which promise to retain or regain good function, but if tendon or joints are obviously seriously damaged
then early rather than late amputation should be considered.
In this connection it should be remembered that it is frequently possible to retain a useful amount of skin of an
otherwise useless finger and that this may make an excellent
flap for repairs of the palm or adjacent finger. If tendon or
joints become exposed during the course of surgical excision or following the failure of a free graft, then repair by
flap becomes urgent if these structures are to be saved [14].
Wang has stated that in high-tension injuries destruction
of tissues is so extensive that it is often impossible to
employ the most desirable methods of local treatment and
less reliable methods have to be used. The assessment of the
depth and extent of electrical burns may be difficult initially
because previously healthy muscles may necrose later on if
the nutrient vessel thromboses due to thermal effect induced
by the electrical energy. Sometimes visceral injuries are
obvious, but often the initial signs and symptoms are very
slight due to delayed perforation and the masking effect of
the abdominal burn wound.
Initially, to obtain maximal penetration of the burn eschar, the hand is dressed with mafenide cream (Sulfamylon
cream) until surgical debridement can be performed. Fasciotomies and escharotomies should be performed within 6
8 h of injury if compartment syndrome is suspected. Clinical
signs such as edema, pain with passive motion, and subjective
Indian J Surg (JulyAugust 2013) 75(4):278283
firmness of the compartments are adequate indicators of the
need for compartment release. It is essential that all compartments of the hand and potentially the forearm, both dorsal and
volar, as well as all digits, Guyons canal, and the carpal
tunnels are released. Serial debridements should then be performed in preparation for definitive reconstruction [14].
This study shows the incidence of complication of hypertropic scar seen in 6.12 % cases, which was managed conservatively. Keloid was seen in 2 (2.04 %) patients, which was
managed by steroid (local injection), and contracture was seen
in 2 patients, which was released with skin grafting. These
findings are comparable with those reported by different
authors [16, 19].
Due to the nature of occupational hazards with electricity,
electrical injuries represent the fourth leading cause of workrelated traumatic death (56 % of all workers deaths) [17].
Morbidity and mortality are largely affected by the particular type of electrical contact involved in each exposure.
Overall mortality is estimated to be 315 % [1, 11]. There
were 8 (8.16 %) cases of mortality. Minimal mortality may
be due to less surface area involved or without visceral
involvement. Patients survived with morbidity (10.20 %)
due to amputation in the present study. This is compared and
correlated well with those of different series [1, 11, 16, 17, 19].
Thus, it is concluded that initial management of electrical
burn is imperative to optimize function and minimize longterm scarring. However, further studies are required regarding flap repair and microsurgery to minimize the rate of
amputation.
Acknowledgement Dr.B.S.Gedam, MBBS, MS.GEN.Surgery,
M.S.ortho, Professor in surgery,are heartily thanked for his technical
assistance in the preparation of the manuscript.
References
1. Lee RC (1997) Injury by electrical forces: pathophysiology, manifestations, and therapy. Curr Probl Surg 34(9):677764
2. Spies C, Trohman RG (2006) Narrative review: Electrocution and
life-threatening electrical injuries. Ann Intern Med 145(7):531537
3. Koumbourlis AC (2002) Electrical injuries. Crit Care Med 30(11
Suppl):S424S430
4. Dawes DM, Ho JD, Reardon RF, Miner JR (2010) Echocardiographic evaluation of TASER X26 probe deployment into the
chests of human volunteers. Am J Emerg Med 28(1):4955
5. Strote J, Walsh M, Angelidis M, Basta A, Hutson HR (2009)
Conducted electrical weapon use by law enforcement: an evaluation of safety and injury. J Trauma 68:12391246
6. Rai J, Jeschke MG, Barrow RE, Herndon DN (1999) Electrical
injuries: A 30-year review. J Trauma 46(5):933936
7. Kopp J, Loos B, Spilker G, Horch RE (2004) Correlation between
serum creatinine kinase levels and extent of muscle damage in
electrical burns. Burns 30(7):680683
8. Thomas SS (1996) Electrical burns of the mouth: still searching for
an answer. Burns 22(2):137140
Indian J Surg (JulyAugust 2013) 75(4):278283
9. Palmieri TL (2009) Initial management of acute pediatric hand
burns. Hand Clin 25(4):461467
10. Choi M, Armstrong MB, Panthaki Z (2009) Pediatric hand burn:
thermal, electrical, and chemical. J Craniofac Surge 20(4):10451048
11. Luz DP, Millan LS, Alessi MS et al (2009) Electrical burns: a
retrospective analysis across a 5-year period. Burns 35(7):10151019
12. Ferreiro I, Melendez J, Regalado J, Bejar FJ, Gabilondo FJ (1998)
Factors influencing the sequelae of high tension electrical injuries.
Burns 24(7):649653
13. Hussmann J, Kucan JO, Russell RC, Bradley T, Zamboni WA
(1995) Electrical injuriesmorbidity, outcome and treatment rationale. Burns 21(7):530535
14. Knox KR, Mortin RJ, Fleegler EJ (2009) Electrical burn of the
upper extremity: interesting case series. Division of Plastic Surgery, New Jersey Medical School, Newark
283
15. Claudet I, Marechal C, Debuisson C, Salanne S (2010) Risk of
arrhythmia and domestic low-voltage electrical injury. Arch
Pediatr 17(4):343349
16. Singerman J, Gomez M, Fish JS (2008) Long-term sequelae
of low-voltage electrical injury. J Burn Care Res 29(5):773
777
17. Casini V (1998) Worker deaths by electrocution: A summary of
NIOSH Surveillance and Investigative Findings. Department of
Health and Human Services, Washington DC, pp 58
18. Rabban J, Adler J, Rosen C, Blair J, Sheridan R (1997) Electrical
injury from subway third rails: serious injury associated with
intermediate voltage contact. Burns 23(6):515518
19. Price T, Cooper MA (2002) Electrical and lighting injuries. In:
Marx J, Hockberger R, Walls R. Rosens Emergency Medicine. Vol
3, 5th ed. Mosby, 20102020
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Case DiscussionDocument8 pagesCase DiscussionAishwarya BharathNo ratings yet
- Conflict Resolution Lesson Plan PDFDocument2 pagesConflict Resolution Lesson Plan PDFapi-448873912No ratings yet
- Blood CollectionDocument25 pagesBlood Collectionطاهرة حربية AlcaldeNo ratings yet
- Self Help For PanicDocument10 pagesSelf Help For PanicIqbal Baryar100% (1)
- Annals of Surgery Volume 257 Issue 6 2013 (Doi 10.1097/sla.0b013e31826eda3b) Iida, Tomohiko Nomori, Hiroaki Shiba, Mitsutoshi Nakajima, Ju - Prognostic Factors After Pulmonary Metastasectomy ForDocument6 pagesAnnals of Surgery Volume 257 Issue 6 2013 (Doi 10.1097/sla.0b013e31826eda3b) Iida, Tomohiko Nomori, Hiroaki Shiba, Mitsutoshi Nakajima, Ju - Prognostic Factors After Pulmonary Metastasectomy ForNurul Dwi UtamiNo ratings yet
- CA Recti Pulmonal MetastasisDocument7 pagesCA Recti Pulmonal MetastasisNurul Dwi UtamiNo ratings yet
- Suicide Risk of Depressed PatientDocument6 pagesSuicide Risk of Depressed PatientNurul Dwi UtamiNo ratings yet
- International Journal of Clinical Oncology Volume 17 Issue 1 2012 (Doi 10.1007/s10147-011-0315-2) Toshiaki Watanabe Michio Itabashi Yasuhiro Shimada Shinji Tan - Japanese Society For Cancer of T PDFDocument29 pagesInternational Journal of Clinical Oncology Volume 17 Issue 1 2012 (Doi 10.1007/s10147-011-0315-2) Toshiaki Watanabe Michio Itabashi Yasuhiro Shimada Shinji Tan - Japanese Society For Cancer of T PDFNurul Dwi UtamiNo ratings yet
- Metastatic Pattern of Colorectal CarcinomaDocument7 pagesMetastatic Pattern of Colorectal CarcinomaNurul Dwi UtamiNo ratings yet
- Metastatic Colorectal CancerDocument9 pagesMetastatic Colorectal CancerNurul Dwi UtamiNo ratings yet
- Survival After Lung Metastasectomy in Colorectal Cancer Patients With Previously Resected Liver MetastasesDocument6 pagesSurvival After Lung Metastasectomy in Colorectal Cancer Patients With Previously Resected Liver MetastasesNurul Dwi UtamiNo ratings yet
- International Journal of Clinical Oncology Volume 17 Issue 1 2012 (Doi 10.1007/s10147-011-0315-2) Toshiaki Watanabe Michio Itabashi Yasuhiro Shimada Shinji Tan - Japanese Society For Cancer of T PDFDocument29 pagesInternational Journal of Clinical Oncology Volume 17 Issue 1 2012 (Doi 10.1007/s10147-011-0315-2) Toshiaki Watanabe Michio Itabashi Yasuhiro Shimada Shinji Tan - Japanese Society For Cancer of T PDFNurul Dwi UtamiNo ratings yet
- Lung CancerDocument11 pagesLung CancerNurul Dwi UtamiNo ratings yet
- Lung CancerDocument11 pagesLung CancerNurul Dwi UtamiNo ratings yet
- Effect of Environment To Colorectal CarcinomaDocument14 pagesEffect of Environment To Colorectal CarcinomaNurul Dwi UtamiNo ratings yet
- Fasting Enhances Cancer TherapyDocument9 pagesFasting Enhances Cancer TherapyNurul Dwi Utami100% (1)
- Radiofrequency TreatmentDocument5 pagesRadiofrequency TreatmentNurul Dwi UtamiNo ratings yet
- Neuroblastoma PDFDocument5 pagesNeuroblastoma PDFHanna G. FauziaNo ratings yet
- Neuroblastoma PDFDocument5 pagesNeuroblastoma PDFHanna G. FauziaNo ratings yet
- DX N Manage Lower Limb CellulitisDocument4 pagesDX N Manage Lower Limb CellulitisNurul Dwi UtamiNo ratings yet
- GC Damage HC PDFDocument5 pagesGC Damage HC PDFNurul Dwi UtamiNo ratings yet
- Guidelines IDSA STI 2014Document43 pagesGuidelines IDSA STI 2014Nurul Dwi UtamiNo ratings yet
- A 16 Suppl1 029Document11 pagesA 16 Suppl1 029Nurul Dwi UtamiNo ratings yet
- Brain Mapping On EA St36 by FmriDocument4 pagesBrain Mapping On EA St36 by FmriNurul Dwi Utami100% (1)
- Ea Prvents Cognitive Deficit in Pilocarpine Induced RatDocument5 pagesEa Prvents Cognitive Deficit in Pilocarpine Induced RatNurul Dwi UtamiNo ratings yet
- Community Building ProcessDocument17 pagesCommunity Building ProcessKarolina HutagalungNo ratings yet
- Self-motivation quiz tipsDocument1 pageSelf-motivation quiz tipsRose D GuzmanNo ratings yet
- Model of Decision MakingDocument34 pagesModel of Decision MakingPalalikesjujubesNo ratings yet
- Complete Guide To Communication Problems After StrokeDocument22 pagesComplete Guide To Communication Problems After Strokeapi-215453798100% (1)
- Treatment of Child Victims of Abuse and NeglectDocument18 pagesTreatment of Child Victims of Abuse and NeglectSri Harsha KothapalliNo ratings yet
- Randomized trial therapy worksheetDocument2 pagesRandomized trial therapy worksheetmermerytaNo ratings yet
- AnemiaDocument40 pagesAnemiaRajaNo ratings yet
- Job Shadowing PresentationDocument8 pagesJob Shadowing Presentationapi-360560383No ratings yet
- ent-CLINICAL CASE REPORTDocument23 pagesent-CLINICAL CASE REPORTAlexandra DukeNo ratings yet
- The Contribution of Carl Rogers and Humanistic Theory To The Understanding of Personality DevelopmentDocument13 pagesThe Contribution of Carl Rogers and Humanistic Theory To The Understanding of Personality DevelopmentOtto_CondliffeNo ratings yet
- Cognitive Behavioral Model of Clinical Perfectionism Shafran Cooper Fairburn 2002 En-UsDocument1 pageCognitive Behavioral Model of Clinical Perfectionism Shafran Cooper Fairburn 2002 En-UsPavlov PicassoNo ratings yet
- Cheat Sheet (AutoRecovered)Document2 pagesCheat Sheet (AutoRecovered)Garry LeeNo ratings yet
- Healthy Hair Guide Magazine PDFDocument15 pagesHealthy Hair Guide Magazine PDFjagan100% (1)
- JVPDocument5 pagesJVPYhr YhNo ratings yet
- KlsjlkdajslkdajslkDocument4 pagesKlsjlkdajslkdajslkRejed VillanuevaNo ratings yet
- YOGA THERAPY for Digestive HealthDocument3 pagesYOGA THERAPY for Digestive Healthrabirm77No ratings yet
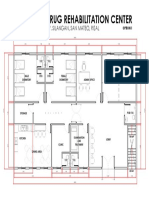
- Proposed Drug Rehabilitation Center: Monterey Sudb., Brgy. Silangan, San Mateo, RizalDocument1 pageProposed Drug Rehabilitation Center: Monterey Sudb., Brgy. Silangan, San Mateo, RizalJonathan MazonNo ratings yet
- Mobility: How To Fix The 3 Most Common Mobility IssuesDocument32 pagesMobility: How To Fix The 3 Most Common Mobility Issuespablo ito100% (4)
- Psychoanalytic EssayDocument7 pagesPsychoanalytic Essayapi-462360394No ratings yet
- Spiramycin Drug Information for Toxoplasmosis TreatmentDocument14 pagesSpiramycin Drug Information for Toxoplasmosis TreatmentRevina AmaliaNo ratings yet
- NeuroblastomaDocument10 pagesNeuroblastomadita100% (1)
- Revised Case Report - HemorrhoidsDocument47 pagesRevised Case Report - Hemorrhoidschristina_love08100% (2)
- SWOT Analysis of The Emergency ServiceDocument20 pagesSWOT Analysis of The Emergency ServiceScribdTranslationsNo ratings yet
- Nursing Care Plan - Acute Pain Assessment Diagnosis Scientific Rationale Planning Intervention Rationale EvaluationDocument3 pagesNursing Care Plan - Acute Pain Assessment Diagnosis Scientific Rationale Planning Intervention Rationale EvaluationNicole cuencosNo ratings yet
- Poisoning and Environmental Exposure PDFDocument148 pagesPoisoning and Environmental Exposure PDFAbdullahNo ratings yet
- Caries Predication, Risk Assessment and Treatment PlanningDocument74 pagesCaries Predication, Risk Assessment and Treatment PlanningmohammadNo ratings yet