Professional Documents
Culture Documents
Preterm Birth and Subsequent Insulin Sensitivity
Uploaded by
angela_karenina_1Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Preterm Birth and Subsequent Insulin Sensitivity
Uploaded by
angela_karenina_1Copyright:
Available Formats
Downloaded from adc.bmj.com on March 4, 2014 - Published by group.bmj.
com
ADC Online First, published on December 20, 2013 as 10.1136/archdischild-2013-304615
Original article
Preterm birth and subsequent insulin sensitivity:
a systematic review
Robert Tinnion,1 Jenna Gillone,1 Timothy Cheetham,2 Nicholas Embleton1
Additional material is
published online only. To view
please visit the journal online
(http://dx.doi.org/10.1136/
archdischild-2013-304615).
1
Department of Neonatal
Medicine, Royal Victoria
Inrmary, Newcastle upon
Tyne, UK
2
Department of Paediatric
Endocrinology, Royal Victoria
Inrmary, Newcastle upon
Tyne, UK
Correspondence to
Dr Nicholas Embleton, Leazes
Wing, Royal Victoria Inrmary,
Queen Victoria Road,
Newcastle upon Tyne NE1 4LP,
UK; nicholas.embleton@ncl.ac.
uk
Received 11 June 2013
Revised 10 November 2013
Accepted 29 November 2013
ABSTRACT
Objective The incidence of preterm birth is increasing
worldwide. Evidence suggests that in later life these
children are at increased risk of metabolic syndrome,
which is itself associated with reduced insulin sensitivity
(IS). We carried out a systematic review to examine
whether preterm birth is associated with later changes in
IS and whether a difference exists between those born
small-for-gestational age (SGA) and appropriate-forgestational age (AGA).
Methods We used the Preferred Reporting Items for
Systematic reviews and Meta-Analyses (PRISMA)
guidance to structure our review with a priori data
extraction criteria to answer the questions posed and
then carried out our literature search. Only papers which
included preterm infants in their study population and
specically assessed IS were included. Findings are
reported by age group to enable change over the life
course to be examined, even though the studies were
mostly cross-sectional, observation studies.
Results We identied and reviewed 26 suitable
publications representing 20 separate cohorts, of which
16 had a term control group. The heterogeneity of the
methods used to measure IS precluded meta-analysis.
In infancy and early childhood there is a measurable
association between IS and preterm birth. In later
childhood and adulthood the strength of this association
reduces, and current body composition becomes the
variable most strongly associated with IS.
Conclusions There is an association between preterm
birth and IS throughout the life course, but the data are
conicting and associations are likely to be affected by
the heterogeneity of each study population and multiple
confounding factors that may change over time. While
the optimal nutritional strategy for preterm infants
remains to be determined, standard public health
guidance to avoid obesogenic lifestyle factors remains
equally important to individuals born preterm.
INTRODUCTION
To cite: Tinnion R,
Gillone J, Cheetham T, et al.
Arch Dis Child Published
Online First: [ please include
Day Month Year]
doi:10.1136/archdischild2013-304615
Approximately 5% to 10% of all births are preterm
(<37 weeks gestation) with long-term survival
rates in developed countries now greater than 50%
for infants born at 24 weeks gestation.1
Neurocognitive impairment is the most important
adverse outcome of preterm birth, but increasing
data show that features of the metabolic syndrome2 3 are also more prevalent (w1, w2).
Reduced insulin sensitivity (IS) is a key component
of the metabolic syndrome2 and is associated with
reduced glucose tolerance,4 hypertension (w3),
hyperlipidaemia and disordered postprandial physiology5. IS is associated with obesity although the
direction of causality is unclear.6
What is already known
Being born small-for-gestational age increases
the risk of later metabolic disease.
Preterm birth may disrupt nutritional
programming windows.
Studies have arrived at different conclusions
regarding the effect of preterm birth on
subsequent sensitivity to insulin in adulthood.
What this study adds
Preterm birth is associated with measurably
reduced insulin sensitivity at various stages of
later life.
With increased maturity the inuence of
environment and diet (manifest as body
composition) becomes more powerful.
The time course of this relationship is unclear
and determination of causality requires further
research.
Low birth weight (<2.5 kg, LBW) is associated
with reduced IS4 (w4, w5) and there are also data to
suggest that early-life growth during sensitive
windows in the prenatal and postnatal period may
programme later metabolic outcomes.7 8 Infants
born preterm will generally be LBW. There are few
data to distinguish between the effects of preterm
birth, compared to LBW at term, on later metabolism, and preterm and term groups may have experienced in utero growth restriction (IUGR). The
majority of published studies are epidemiological
and focus on adults born small-for-gestational age
(SGA, typically birth weight <10th centile) who
were born at term and were also LBW. The objective
of this study was to determine whether preterm
birth was associated with IS in childhood or adulthood, and the effect of being born preterm SGA
compared to appropriate-for-gestational age (AGA).
METHODS
Search strategy
We followed the Centre for Reviews and
Dissemination (University of York, 2009) guidance
for performing systematic reviews and the Preferred
Reporting Items for Systematic reviews and
Meta-Analyses (PRISMA) guidance (2009).9 Eligible
studies were identied by searching electronic bibliographic databases (OVID MEDLINE, EMBASE,
CINAHL, SCOPUS and PUBMED Central) and the
Tinnion R, Article
et al. Arch author
Dis Child 2013;0:17.
1
Copyright
(or theirdoi:10.1136/archdischild-2013-304615
employer) 2013. Produced by BMJ Publishing Group Ltd (& RCPCH) under licence.
Downloaded from adc.bmj.com on March 4, 2014 - Published by group.bmj.com
Original article
Cochrane Database of Systematic Reviews. Search terms used for
medical subject headings and keywords were: prematurity OR
preterm or neonate OR neonatal OR SGA/small-forgestational age AND Insulin resistance OR IS OR metabolic
syndrome. Results were limited to articles in English and human
studies. Hand searching of review article references and studies
from established preterm cohorts was undertaken. No specied
year limit was applied as a search term. The search was last executed in January 2013.
Article selection
The search yielded 2206 articles including 98 papers from hand
searching (gure 1). Initial screening excluded 2138 articles based
on title, abstract and removal of duplicates and we then reviewed
68 articles in full text. Only studies using a direct measure of IS
and including preterm infants were included in the nal review:
therefore, a further 36 studies and 6 review papers were excluded
to leave a nal total of 26 studies. Studies reporting data from individual cohorts in different publications were included for completeness as they represented longitudinal follow-up or used
different subjects at different times from an original cohort.
Data extraction
Prior to article selection, we determined the key data items for
review: (1) inclusion criteria (gestation or weight); (2) number of
children/adults studied (n); (3) age at measurement; (4) measurement technique; (5) study design and (6) principal study conclusions. Features identied as strengths or weaknesses were recorded
(see online supplementary appendix 1). Gestation and weight at
birth were important considerations for a contemporary neonatal
intensive care unit (NICU) population. The participant numbers
in the studies allowed us to consider the relative weight of study
evidence and age at assessment enabled stratication of our results.
Measurement technique was key to inclusion in the review and
study design helped determine quality of the study.
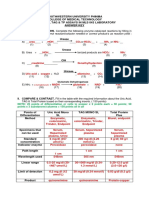
Methodological quality was formally assessed using a modied Newcastle-Ottawa Scale (NOS; table 1). The NOS allows
quantication of the quality of non-randomised and cohort
studies within the elds of population selection (relevance to
preterm infants) and comparability of cohorts studied and the
quality of the methods used to determine the outcome of interest (direct assessment of IS). Unlike use of a single reported
grade of evidence the NOS gives an overall impression of
quality (maximum quality score of 12 stars) as well as an easily
accessible breakdown of strengths and weaknesses in the specic
areas outlined.10 Our NOS weighted the criteria areas as two
stars for optimal practice, with one star for acceptable practice.
Two authors (RT and JG) independently extracted data and
scored the papers for quality. Disagreement was resolved by discussion and review (NE).
We considered whether meta-analysis would be appropriate
for our data set. There was signicant heterogeneity in methodology used to quantify and assess IS in the selected studies.
Combining results would have been inappropriate as there is no
clearly accepted way of standardising between methods and no
universal expression of either absolute IS results or change in IS.
Many of the studies relied on physiological markers to make
estimations of change in IS (eg, split pro-insulin concentrations)
or postmeasurement modelling (eg, homeostasis model assessment (of insulin sensitivity) (HOMA2)) which precludes direct
comparison. In addition, some of the methods used are not well
validated for use in children against gold standards such as
euglycaemic insulin clamp studies. If we had considered only
those studies with the same methodology for meta-analysis, it
would have limited the scope of the study and not reected the
measurement of IS over the life course.
RESULTS
Description of studies included in the systematic review
The selected studies investigated cohorts at different ages, published between 2000 and 2012, with participants from early
infancy through to adulthood, mainly in resource-rich settings.
The studies encompassed 20 unique cohorts. The median NOS
for the selected studies was 8 (range: 6 to 10) from a possible
12 (table 2). Sixteen studies had a term control group4 1125 and
3 studied individuals originally recruited into interventional
trials.13 16 26 One follow-up study was interventional (a
weight-loss programme)20 and one compared cohorts before
and after a change in feeding practice.27
Different methods were used to determine IS. Thirteen used
a variation of a glucose tolerance test (GTT; intravenous
short-sampled
or
frequently
sampled
GTT
(FSGTT)11 14 15 21 25 28 29; oral glucose load4 16 23 24 26 or
milk bolus30) combined with insulin sampling and modelling to
give a measure of IS. Three5 31 32 used hyperinsulinaemic euglycaemic clamp techniques. Others used measures of glucose
metabolism such as fasting insulin and glucose, or 3233 split
pro-insulin, combined with a modelled estimation of IS such as
HOMA. The presence and signicance of altered IS changes
with age,33 so the results are presented by age group: infancy
(<2 years), childhood (210 years), adolescence (1018 years),
early (>18 years) and later adulthood (>35 years). These results
encouraged us to develop a logic model (gure 2) outlining the
changes seen over the life course.
Infant studies
Figure 1 Overview of article selection process for the review.
Three studies investigated early postnatal life.27 29 30 Pittaluga
compared cohorts before and after a change in protocol for
postdischarge feeding27 and showed that altered nutrient
Tinnion R, et al. Arch Dis Child 2013;0:17. doi:10.1136/archdischild-2013-304615
Downloaded from adc.bmj.com on March 4, 2014 - Published by group.bmj.com
Original article
Table 1 Modified Newcastle Ottawa Score
Criteria
Rating
Example
Selection
1. Representativeness of the cohort of
preterm born children
Stars
*****
Truly representative of preterm infants
Tertiary neonatal intensive care unit population;
born <32/40; wt <1500 g
**
Somewhat representative of preterm infants
Single centre; infants <37/40; wt <1800 g
Selected group of patients
Speciality clinic
Not representative
2. Selection of comparison group
(term controls)
Drawn from the same origin as the preterm infants
Hospital or community peer (eg, school) selection
Hospital record
Notes, dating scan
**
Public record
Parents hand-held notes, birth certificates,
gestation estimate after birth
Drawn from a different community
Not reported or no comparison group
3. Ascertainment of prematurity
Not recorded
Comparability
1. Comparability on the basis of design
or analysis
***
The study controls for current body habitus
Mass, body fat (% or index), BMI, height
The study assesses or allows for pubertal stage
Tanner stages used
The study controls for or allows for other concurrent
endocrine pathology (eg, growth hormone deficiency) or
influence
Assessment of Insulin Sensitivity
1. Measurement of Insulin sensitivity
****
Experimental assessment of Insulin sensitivity, assessor
blinded to prematurity or not
For example, glucose disposal during euglycaemic
clamp, fasting insulin and glucose with use of HOMA
Experimental assessment of IS but no report of blinding
**
*
Not reported
2. Adequacy of cohort follow-up
Complete follow-up, that is, all original cohort members
tested at current study
**
Subjects lost to follow-up 20% (ie, unlikely to introduce
bias) OR if description of those lost suggest that they were
not different from those followed
Follow-up rate 80% and no description of those lost OR
description provided indicates substantial difference
Not reported
HOMA, homeostasis model assessment.
composition ( principally extra docosahexaenoic acid (DHA)
and protein) resulted in lower fasting insulin levels at 2 years.
Leipl and Gray investigated preterm SGA status and IS and
are discussed below.
Childhood studies (210 years)
Two studies used frequently sampled intravenous glucose tolerance tests (FSIVGTTs) in children 410 years old.11 15
Preterm children showed reduced IS that correlated with weight
SDS at the time of testing, change in weight from term to 1 year
and change in weight from term to current.11 The other study
showed reduced IS in preterm compared to term controls and
that those born preterm had similar IS to children born SGA at
term.15 Increase in weight and height SDS and a higher
weight-to-height ratio was associated with reduced IS.
One study where just 3.5% of the children were preterm
showed a linear association between birth weight and IS.18 Two
studies using HOMA modelling in 29-year-old children born
preterm showed reduced IS12 17 and that preterm SGA infants
with appropriate catch-up growth had greater IS than term SGA
controls.12 This study also showed that preterm and term AGA
groups had greater IS than the term SGA infants. Gestation and
birth weight were associated with IS even after correction for
body mass index (BMI).
Fewtrell and Singhal13 26 followed up a cohort originally
enrolled into nutritional trials in infancy.34 At 912 years of
age,26 fasting insulin, glucose and pro-insulin were strongly
related to current weight SDS. Regression modelling showed
Tinnion R, et al. Arch Dis Child 2013;0:17. doi:10.1136/archdischild-2013-304615
Adolescent studies (1018 years)
Downloaded from adc.bmj.com on March 4, 2014 - Published by group.bmj.com
Original article
Table 2 Newcastle Ottawa Scores for selected papers (by year then ranking)
Methodological quality
Selection
Author, year,
journal
Kerkhof GF, et al 25
Pittaluga E, et al 27
Rotteveel J, et al 32
Chan PYL, et al 24
Reinehr T, et al 20
De Kort SWK, et al 21
Lemos JO, et al 18
Willemsen RH, et al 14
Darendeliler F, et al 12
Pandolfi C, et al 23
Rotteveel J, et al 31
Rotteveel J, et al 5
Hovi P, et al 4
Dalziel S, et al 16
Regan FM, et al 11
Finken MJ, et al 33
Bo S, et al 37
Toumba M17
Bazaes RA, et al 28
Hofman PL, et al 15
Kistner A, et al 22
Singhal A, et al 13
Leipala JA, et al 29
Gray IP, et al 30
Irving RJ, et al 19
Fewtrell MS, et al 26
Representativeness
*
**
**
**
*
*
**
*
**
**
**
*
**
**
**
*
**
**
**
**
**
*
*
*
Outcome
Selection
of control
*
*
*
*
*
*
*
*
Ascertainment
of prematurity
Comparability
Assessment
**
**
**
**
*
**
**
**
**
**
**
**
**
**
**
**
**
**
**
**
*
**
**
*
**
**
***
**
**
**
***
***
**
***
***
***
**
**
***
***
***
**
***
**
**
***
***
**
**
**
***
**
*
*
*
**
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
**
*
Adequacy of
follow-up
Total Rating
(max 12 stars)
*
*
8
8
7
8
9
8
6
8
10
8
7
7
10
9
9
8
8
7
8
8
8
9
9
7
10
6
**
*
*
**
*
*
*
*
**
**
*
Three studies indicated that current body composition (especially high truncal fat) was the strongest determinant of reduced
IS in adults born preterm.14 32 35 Rotteveel32 demonstrated that
IS was not associated with perinatal factors after correction for
current body composition. In a separate study on the same
cohort they showed that IS was independently associated with
height gain (from 1 to 5 years old) and weight gain (2 to 21
years old).31 Willemsen used FSIVGTT to compare IS and body
composition measured by dual energy X-ray absorptiometry
(DEXA).14 Adjusted IS was signicantly inuenced by height
and weight SDS. Total fat mass and truncal fat mass were the
most signicant variables inuencing IS. Birthweight SDS and
gestation were not signicant determinants after correction for
fat mass. Later analysis of the same cohort suggested that
growth patterns were important determinants of adult outcomes.25 Those with rapid infant catch-up growth had higher
adult body fat percentage and waist circumference, but there
were no signicant associations with IS. When analysed by quartiles of weight SDS gain from birth to term, the highest quartile
weight gain group had higher body fat, waist circumference,
insulin response and disposition index although there were no
associations with IS.
Finken35 showed that rapid weight gain to 3 months was associated with higher fasting insulin and lower IS in preterm born
adults at age 19 years. However, adjustment for current body
composition and other confounders resulted in loss of signicance. There were also strong interactions between birthweight
SDS, current fat mass or body fat percentage and HOMA
index: having a higher fat mass after lower birth weight was
associated with reduction in IS.
By contrast, Hovi4 reported a preterm cohort from Helsinki
studied at 1827 years of age and demonstrated reduced IS irrespective of BMI when compared to term controls. While the
effect of prematurity on IS was not affected by adjustment for
BMI, neither fat mass nor fat mass index was included in the
modelling.
Tinnion R, et al. Arch Dis Child 2013;0:17. doi:10.1136/archdischild-2013-304615
that change in weight SDS from 18 months to current age was
positively related to insulin, pro-insulin and split pro-insulin.
Birth weight had a strong negative correlation with 30-min
glucose levels. By 1316 years of age,13 a decrease of 13.4% IS
per unit increase in weight SDS was seen. Adolescents randomised to higher nutrient intakes as neonates had greater split
pro-insulin levels even after adjustment for potential confounders. A stepwise increase in adjusted 3233 split pro-insulin was
found to mirror quartiles of weight gain in the rst two postnatal weeks.
Chan24 investigated 1115-year-old children born term and
preterm and conducted a standard oral glucose tolerance test
(OGTT). They showed lower glucose levels at 2 hours postload
in those born preterm. Reinehr20 studied SGA children 513
years of age (term and preterm) who were obese and assessed
the effects of a weight loss intervention on IS. Birth weight had
a small association with IS. Reduction in obesity was associated
with improved IS.
Early adulthood
Downloaded from adc.bmj.com on March 4, 2014 - Published by group.bmj.com
Original article
Figure 2 Logic model demonstrating the changes in insulin sensitivity in infants born preterm, from birth to childhood.
Pandol23 studied adults born LBW and showed preterm birth
but not adult BMI to be a determinant of IS: they found
reduced IS in LBW and preterm AGA even when corrected for
current BMI, using BMI as a dichotomised variable in their
modelling. Dalziel16 studied adults born preterm at age 30 years
and found that 2-h IS after OGTT was reduced compared to
term born controls. Birth weight adjusted for GA was not associated with reduced IS.
Insulin sensitivity in later adulthood (>35 years)
We did not identify any studies directly measuring IS after early
adulthood. However, Kajante (w1) showed an association
between the risk of developing type 2 diabetes and birth before
35 weeks gestation. A difference was also found between those
born at term who developed type 2 diabetes and those who had
reduced IS alone as measured by OGTT: while both were associated with markers of restricted fetal growth (LBW) and accelerated childhood growth (height), those with reduced IS were
thin during childhood. Those who developed type 2 diabetes
had a high childhood BMI.36
SGA status in adulthood
Rotteveel31 32 showed no effect of SGA status on IS after correction for adult body composition, although there was a difference in IS between SGA and AGA after adjustment for fat mass
measured by bioimpedance. Hovi4 demonstrated that birth
weight <10th centile in preterm infants, who then exhibited
catch-up growth to term, had a 30% decrease in IS per weight
SDS increase.
The gure shows the potential impact of factors over the life
course. Note: arrow thickness varies based on the proportional
inuence of factors relevant to the evidence found in the studies
included in this systematic review. The model should be read
left-to-right. The term metabolic inexibility is used to denote
adverse changes in metabolism that may be developing as precursors to the metabolic syndrome.
DISCUSSION
Leipl29 used FSIVGTT in preterm infants and found no independent effect of SGA status, although postnatal steroid administration was associated with reduced IS in the SGA infants only.
Gray30 used a milk tolerance test in the rst 2 months, showed
that IS was related to weight at the time of test but not to gestation and that SGA preterm infants had higher insulin levels.
Five studies in early childhood showed no clear effect of SGA
status on IS.11 12 15 17 37 Bazaes28 used HOMA modelling with
IVGTT in 57-year-old children and found those born SGA had
reduced IS. While Reinehr20 in a weight loss study in children
516-year-old demonstrated an effect of SGA status on IS, the
study group included those born preterm and term. Chan24
found no difference between SGA/AGA groups in IS in early
adolescence although those born preterm SGA had higher
insulin levels 2 h after OGTT.
Our systematic review aimed to determine evidence outlining
associations between preterm birth and later IS, and the effects
of SGA status. Figure 2 demonstrates this using a logic model
generated from our review. Logic models were originally proposed to examine complex systems where outcomes are not
necessarily quantiable using simple measures. Latterly they
have been adapted as a tool for use in systematic reviews (w8)
to allow either targeting of outcome measures or, as in our
paper, a summary of the ndings of the review in a owchart.
This allows the reader to follow changes through the system (in
our case throughout life) from input to outcome. The logic
model depicts the context we are interested in (ie, preterm
birth), the care that is given (input) and the ways in which the
effects of this input are measured (output). Importantly it also
allows outcomes (ie, the summary evidence presented in the
review) to be displayed at different stages with the magnitude of
inuence of factors associated with IS represented, using linear
arrows, in the direction of inuence.
In childhood, preterm birth is associated with altered IS.11 15
While weight catch up to that expected based on parental size
Tinnion R, et al. Arch Dis Child 2013;0:17. doi:10.1136/archdischild-2013-304615
SGA status in infancy and childhood
Downloaded from adc.bmj.com on March 4, 2014 - Published by group.bmj.com
Original article
is associated with IS similar to those born at term in some
studies,17 26 in others, increasing weight SDS was associated
with decreased IS.13 18 26 By adulthood, the data are conicting,
with some studies demonstrating that fat mass is the major
determinant of IS with no effect of gestation,14 32 35 while
others identify a persisting effect of preterm birth.4 23 A recent
meta-analysis did not conclude there were persisting effects of
preterm birth on IS in adults alone.38
Our secondary outcome was to determine the effect of SGA
status. Changes in the early postnatal period may simply reect
short-term homeostatic effects29 30 but the decreased IS
observed in later childhood may be due to differences in earlylife growth.4 28 31 32 However, other studies found little or no
difference in IS related to SGA status.11 12 15 17 37 There are
likely to be several reasons for the lack of agreement, including
differences in methodology, population and denition of SGA:
not all infants who are SGA will have experienced IUGR; similarly not all growth-restricted term infants will be SGA.
Interestingly, glucose levels in AGA/SGA preterm groups were
often similar.27 29 30
There are likely to be multiple mechanisms explaining associations between preterm birth and later IS. Preterm birth may be
spontaneous or the result of a compromised pregnancy. Neonatal
care in the rst few weeks is complex, and recommended nutrient intakes are difcult to meet39 meaning many experience ex
utero growth restriction, compounding pre-existing IUGR decits. Early nutrition is primarily parenteral, using imperfect
amino acid and lipid solutions and most receive a greater proportion of their calories from lipid, and lower intakes of protein,
compared to the in utero fetus. Growth failure in early life may
set the scene for later catch-up growth but a lack of controlled
trials means that determining causality is difcult.
The physiological alterations determining the relationships
between early-life events and subsequent IS are complex and
may involve structural change within organ systems, alterations
to endocrine feedback mechanisms (w2), cellular ageing and/or
epigenetic mechanisms (w6, w7). Few of the studies reviewed
adjusted for early-life factors such as nutrition and many did
not adjust for childhood growth, obesity or lifestyle factors.
Only one controlled trial identied an association between
more rapid weight gain in the rst two postnatal weeks and
decreased IS in adolescence. While current data suggest the possibility of associations with later epochs of growth, the data are
conicting and are open to bias, confounding and the possibility
of reverse causation. Decreased IS may lead to increased obesity:
equally, high body fat content may result in decreased IS. There
is insufcient evidence to determine optimal nutritional regimens
and whether these may differ for those born SGA.
Importantly, later lifestyle effects appear to be of greater signicance than early-life exposures and continued efforts should
focus on modiable behaviours through childhood20 and into
adulthood. However, lifestyle behaviours may be programmed
by early-life events: preterm birth itself may alter later appetite
or encourage more sedentary behaviour.40
This review is limited due to the heterogeneity in populations,
early-life exposures, methodology of IS assessment, adjustment
for confounders and the robustness with which current-life
parameters have been assessed. Follow-up studies reporting outcomes in adults reect neonatal care practices of 2030 years
ago, predating the widespread use of antenatal steroids, surfactant and parenteral nutrition, all of which have effects on survival and outcome. We endeavoured to provide a life course
approach to IS, summarised in a simple model, while accepting
that a review of cross-sectional studies at differing time points
6
will not provide the same data as longitudinal studies, even after
adjustment for any bias introduced by attritional losses over
time.
CONCLUSIONS
There are associations between preterm birth and IS throughout
the life course, but this is affected by multiple, confounding
factors that change over time. Contemporary lifestyle factors
confound this association and may be of greater magnitude.
While the optimal nutritional strategy for preterm infants in
early life remains to be determined, standard public-health guidance to avoid an obesogenic lifestyle is equally applicable to
individuals born preterm. Future research must include prospective controlled trials with detailed measures of early exposures and longitudinal follow-up.
Contributors All four authors are responsible for the reported research and have
participated in the concept and design, analysis and interpretation of data, drafting
or revising, and have approved this manuscript as submitted. RT conceptualised and
designed the study, carried out the literature search, data extraction and quality
scoring, drafted the rst draft of the manuscript and edited the nal manuscript for
submission. JG carried out in parallel data extraction and quality scoring, and
reviewed and revised the manuscript. TC reviewed and edited the manuscript,
supervised the parallel data extraction process and contributed to the nal submitted
manuscript. NM had the original idea, provided third-person arbitration during data
extraction and quality scoring, and contributed to the nal submitted manuscript.
Dr Embleton is corresponding author. All authors have approved the submission of
this version of the manuscript and takes full responsibility for it.
Competing interests None.
Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
Moore T, Hennessy EM, Myles J, et al. Neurological and developmental outcome in
extremely preterm children born in England in 1995 and 2006: the EPICure studies.
BMJ 2012;345:e7961.
Samuel VT, Petersen KF, Shulman GI. Lipid-induced insulin resistance: unravelling
the mechanism. Lancet 2010;375:226777.
Bremer AA, Mietus-Snyder M, Lustig RH. Toward a unifying hypothesis of metabolic
syndrome. Pediatrics 2012;129:55770.
Hovi P, Andersson S, Eriksson JG, et al. Glucose regulation in young adults with
very low birth weight. N Engl J Med 2007;356:205363.
Rotteveel J, van Weissenbruch MM, Twisk JW, et al. Abnormal lipid prole and
hyperinsulinaemia after a mixed meal: additional cardiovascular risk factors in young
adults born preterm. Diabetologia 2008;51:126975.
Sinaiko AR, Caprio S. Insulin resistance. J Pediatr 2012;161:1115.
Lucas A. Role of nutritional programming in determining adult morbidity. Arch Dis
Child 1994;71:28890.
Burdge GC, Lillycrop KA. Nutrition, epigenetics, and developmental plasticity:
implications for understanding human disease. Annu Review Nutr 2010;30:31539.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting
systematic reviews and meta-analyses of studies that evaluate healthcare
interventions: explanation and elaboration. BMJ 2009;339:b2700.
Deeks JJ, Dinnes J, DAmico R, et al. Evaluating non-randomised intervention
studies. Health Technol Assess 2003;7:1173, iiix.
Regan FM, Cuteld WS, Jefferies C, et al. The impact of early nutrition in premature
infants on later childhood insulin sensitivity and growth. Pediatrics
2006;118:19439.
Darendeliler F, Bas F, Bundak R, et al. Insulin resistance and body composition in
preterm born children during prepubertal ages. Clin Endocrinol 2008;68:7739.
Singhal A, Fewtrell M, Cole TJ, et al. Low nutrient intake and early growth for later
insulin resistance in adolescents born preterm. Lancet 2003;361:108997.
Willemsen RH, Leunissen RW, Stijnen T, et al. Prematurity is not associated with
reduced insulin sensitivity in adulthood. J Clin Endocrinol Metab 2009;94:1695700.
Hofman PL, Regan F, Jackson WE, et al. Premature birth and later insulin resistance.
N Engl J Med 2004;351:217986.
Dalziel SR, Parag V, Rodgers A, et al. Cardiovascular risk factors at age 30
following pre-term birth. Int J Epidemiol 2007;36:90715.
Toumba M, Hadjidemetriou A, Topouzi M, et al. Evaluation of the auxological and
metabolic status in prepubertal children born small for gestational age. J Pediatr
Endocrinol Metab 2005;18:67788.
Lemos JO, Rondo PH, Pereira JA, et al. The relationship between birth weight and
insulin resistance in childhood. Br J Nutr 2010;103:38692.
Tinnion R, et al. Arch Dis Child 2013;0:17. doi:10.1136/archdischild-2013-304615
Downloaded from adc.bmj.com on March 4, 2014 - Published by group.bmj.com
Original article
19
20
21
22
23
24
25
26
27
28
Irving RJ, Belton NR, Elton RA, et al. Adult cardiovascular risk factors in premature
babies. Lancet 2000;355:21356.
Reinehr T, Kleber M, Toschke AM. Former small for gestational age (SGA) status is
associated to changes of insulin resistance in obese children during weight loss.
Pediatr Diabetes 2010;11:4317.
de Kort SW, van Doorn J, van de Sande AG, et al. Serum insulin-like growth
factor-binding protein-2 levels and metabolic and cardiovascular risk factors in
young adults and children born small for gestational age. J Clin Endocrinol Metab
2010;95:86471.
Kistner A, Jacobson SH, Celsi G, et al. IGFBP-1 levels in adult women born small
for gestational age suggest insulin resistance in spite of normal BMI. J Intern Med
2004;255:828.
Pandol C, Zugaro A, Lattanzio F, et al. Low birth weight and later development of
insulin resistance and biochemical/clinical features of polycystic ovary syndrome.
Metabolism 2008;57:9991004.
Chan PY, Morris JM, Leslie GI, et al. The long-term effects of prematurity and
intrauterine growth restriction on cardiovascular, renal, and metabolic function.
Int J Pediatr 2010;2010:280402.
Kerkhof GF, Willemsen RH, Leunissen RW, et al. Health prole of young adults born
preterm: negative effects of rapid weight gain in early life. J Clin Endocrinol Metab
2012;97:4498506.
Fewtrell MS, Doherty C, Cole TJ, et al. Effects of size at birth, gestational age and
early growth in preterm infants on glucose and insulin concentrations at
912 years. Diabetologia 2000;43:71417.
Pittaluga E, Vernal P, Llanos A, et al. Benets of supplemented preterm formulas on
insulin sensitivity and body composition after discharge from the neonatal intensive
care unit. J Pediatr 2011;159:92632, e2.
Bazaes RA, Alegria A, Pittaluga E, et al. Determinants of insulin sensitivity and
secretion in very-low-birth-weight children. J Clin Endocrinol Metab
2004;89:126772.
Tinnion R, et al. Arch Dis Child 2013;0:17. doi:10.1136/archdischild-2013-304615
29
30
31
32
33
34
35
36
37
38
39
40
Leipala JA, Raivio KO, Sarnesto A, et al. Intrauterine growth restriction and postnatal steroid
treatment effects on insulin sensitivity in preterm neonates. J Pediatr 2002;141:4726.
Gray IP, Cooper PA, Cory BJ, et al. The intrauterine environment is a strong
determinant of glucose tolerance during the neonatal period, even in prematurity.
J Clin Endocrinol Metab 2002;87:42526.
Rotteveel J, van Weissenbruch MM, Twisk JW, et al. Infant and childhood growth
patterns, insulin sensitivity, and blood pressure in prematurely born young adults.
Pediatrics 2008;122:31321.
Rotteveel J, van Weissenbruch MM, Twisk JW, et al. Insulin sensitivity in prematurely
born adults: relation to preterm growth restraint. Horm Res Pediatr 2011;75:2527.
Kurtoglu S, Hatipoglu N, Mazicioglu M, et al. Insulin resistance in obese children
and adolescents: HOMA-IR cut-off levels in the prepubertal and pubertal periods.
J Clinical Res Pediatr Endocrinol 2010;2:1006.
Lucas A, Gore SM, Cole TJ, et al. Multicentre trial on feeding low birthweight
infants: effects of diet on early growth. Arch Dis Child 1984;59:72230.
Finken MJ, Keijzer-Veen MG, Dekker FW, et al. Preterm birth and later insulin
resistance: effects of birth weight and postnatal growth in a population based
longitudinal study from birth into adult life. Diabetologia 2006;49:47885.
Eriksson JG, Forsen T, Tuomilehto J, et al. Effects of size at birth and childhood
growth on the insulin resistance syndrome in elderly individuals. Diabetologia
2002;45:3428.
Bo S, Bertino E, Bagna R, et al. Insulin resistance in pre-school very-low-birth
weight pre-term children. Diabetes Metab 2006;32:1518.
Parkinson JR, Hyde MJ, Gale C, et al. Preterm birth and the metabolic syndrome in
adult life: a systematic review and meta-analysis. Pediatrics 2013;131:e124063.
Embleton NE, Pang N, Cooke RJ. Postnatal malnutrition and growth retardation: an
inevitable consequence of current recommendations in preterm infants? Pediatrics
2001;107:2703.
Kajantie E, Strang-Karlsson S, Hovi P, et al. Adults born at very low birth weight
exercise less than their peers born at term. J Pediatr 2010;157:61016.
Downloaded from adc.bmj.com on March 4, 2014 - Published by group.bmj.com
Preterm birth and subsequent insulin
sensitivity: a systematic review
Robert Tinnion, Jenna Gillone, Timothy Cheetham, et al.
Arch Dis Child published online December 20, 2013
doi: 10.1136/archdischild-2013-304615
Updated information and services can be found at:
http://adc.bmj.com/content/early/2013/12/20/archdischild-2013-304615.full.html
These include:
Data Supplement
"Supplementary Data"
http://adc.bmj.com/content/suppl/2013/12/20/archdischild-2013-304615.DC1.html
References
This article cites 40 articles, 10 of which can be accessed free at:
http://adc.bmj.com/content/early/2013/12/20/archdischild-2013-304615.full.html#ref-list-1
P<P
Email alerting
service
Topic
Collections
Published online December 20, 2013 in advance of the print journal.
Receive free email alerts when new articles cite this article. Sign up in
the box at the top right corner of the online article.
Articles on similar topics can be found in the following collections
Pregnancy (254 articles)
Notes
Advance online articles have been peer reviewed, accepted for publication, edited and
typeset, but have not not yet appeared in the paper journal. Advance online articles are
citable and establish publication priority; they are indexed by PubMed from initial
publication. Citations to Advance online articles must include the digital object identifier
(DOIs) and date of initial publication.
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
All in-text references underlined in blue are linked to publications on ResearchGate, letting you access and read them immediately.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Gestational Diabetes Diagnosis & CareDocument100 pagesGestational Diabetes Diagnosis & CareAahr JjhayNo ratings yet
- DM Case StudyDocument4 pagesDM Case Studyapi-273276737100% (3)
- Research ProposalDocument36 pagesResearch ProposalShakilaNo ratings yet
- Southwest University Phinma MLS Quiz on UA, TAG & TP Assays Answer KeyDocument61 pagesSouthwest University Phinma MLS Quiz on UA, TAG & TP Assays Answer KeyZylith NanaseNo ratings yet
- Diabetes MellitusDocument85 pagesDiabetes MellitusPriyanka Hr GowdaNo ratings yet
- FFD Intensive Reversal ProgramDocument69 pagesFFD Intensive Reversal ProgramCh RambabuNo ratings yet
- Urine Specimen Collection Types & ProceduresDocument27 pagesUrine Specimen Collection Types & ProceduresMikeyla Moral100% (1)
- ASCP Recalls 2017-2018 Flashcards - Quizlet - AmgadDocument80 pagesASCP Recalls 2017-2018 Flashcards - Quizlet - AmgadShiv Prajapati100% (16)
- Chemical Pathology For TH BeginnersDocument455 pagesChemical Pathology For TH BeginnersMikael Akif100% (1)
- Diabetes Care Nov 2003Document8 pagesDiabetes Care Nov 2003Priscilla ArtesNo ratings yet
- Kapoor 2018Document8 pagesKapoor 2018angela_karenina_1No ratings yet
- UMEM Educational Pearls - University of Maryland School of Medicine, Department of Emergency MedicineDocument2 pagesUMEM Educational Pearls - University of Maryland School of Medicine, Department of Emergency Medicineangela_karenina_1No ratings yet
- Tide Man 2016Document9 pagesTide Man 2016angela_karenina_1No ratings yet
- Translational Research in Anatomy: James P. Nott, Elizabeth A. Bonney, James D. Pickering, Nigel A.B. SimpsonDocument7 pagesTranslational Research in Anatomy: James P. Nott, Elizabeth A. Bonney, James D. Pickering, Nigel A.B. Simpsonangela_karenina_1No ratings yet
- Ditorial What's in A Word?: Stewart. Michael@mayo - EduDocument2 pagesDitorial What's in A Word?: Stewart. Michael@mayo - Eduangela_karenina_1No ratings yet
- Traumasystems: Origins, Evolution, and Current ChallengesDocument13 pagesTraumasystems: Origins, Evolution, and Current Challengesangela_karenina_1No ratings yet
- S - An Outcome Audit of Three Day Antimicrobial Prescribing For The Acute Dentoalveolar AbscessDocument4 pagesS - An Outcome Audit of Three Day Antimicrobial Prescribing For The Acute Dentoalveolar Abscessangela_karenina_1No ratings yet
- Park 2015Document7 pagesPark 2015angela_karenina_1No ratings yet
- Peran GNRHDocument7 pagesPeran GNRHMerliana DebyantiNo ratings yet
- Morgan 2016Document3 pagesMorgan 2016angela_karenina_1No ratings yet
- Ong 2017Document5 pagesOng 2017angela_karenina_1No ratings yet
- S - Histology of Ancient Soft Tissue Tumors A ReviewDocument13 pagesS - Histology of Ancient Soft Tissue Tumors A Reviewangela_karenina_1No ratings yet
- Patofisiologi Preeklamsi1Document4 pagesPatofisiologi Preeklamsi1Andini RizkyNo ratings yet
- Clin Infect Dis.-2011-Lawn-1384-7 PDFDocument4 pagesClin Infect Dis.-2011-Lawn-1384-7 PDFangela_karenina_1No ratings yet
- Vaughan and Asbury's General Ophthalmology, 17th Edition: System For Ophthalmic Dispensing WasDocument2 pagesVaughan and Asbury's General Ophthalmology, 17th Edition: System For Ophthalmic Dispensing Wasangela_karenina_1No ratings yet
- Distance Visual Acuity Measurement StudyDocument1 pageDistance Visual Acuity Measurement Studyangela_karenina_1No ratings yet
- Autophagy and Autophagy-Related Proteins in The Immune SystemDocument12 pagesAutophagy and Autophagy-Related Proteins in The Immune Systemangela_karenina_1No ratings yet
- Neonatal Side Effects of Maternal Labetalol Treatment in Severe PreeclampsiDocument5 pagesNeonatal Side Effects of Maternal Labetalol Treatment in Severe Preeclampsiangela_karenina_1No ratings yet
- Asymptomatic Bacteriuria During Pregnancy: Eyal Sheiner, Efrat Mazor-Drey, & Amalia LevyDocument5 pagesAsymptomatic Bacteriuria During Pregnancy: Eyal Sheiner, Efrat Mazor-Drey, & Amalia Levyangela_karenina_1No ratings yet
- Jia 2016Document12 pagesJia 2016angela_karenina_1No ratings yet
- Prognostic Impact of HIF-1α Expression in PatientsDocument6 pagesPrognostic Impact of HIF-1α Expression in Patientsangela_karenina_1No ratings yet
- Bacterial VaginosisDocument9 pagesBacterial Vaginosisangela_karenina_1100% (1)
- Padegimas2015 PDFDocument12 pagesPadegimas2015 PDFangela_karenina_1No ratings yet
- Carica papaya seed extract reduces steroidogenesis and spermatogenesis in ratsDocument5 pagesCarica papaya seed extract reduces steroidogenesis and spermatogenesis in ratsangela_karenina_1No ratings yet
- Maconochie2015 PDFDocument22 pagesMaconochie2015 PDFangela_karenina_1No ratings yet
- HIV in ChildrenDocument28 pagesHIV in Childrenangela_karenina_1No ratings yet
- Morley 2004Document6 pagesMorley 2004angela_karenina_1No ratings yet
- S - Factors That Affect The Decision To Undergo Amniocentesis in Women With Normal Down Syndrome Screening Results It Is All About The Age PDFDocument12 pagesS - Factors That Affect The Decision To Undergo Amniocentesis in Women With Normal Down Syndrome Screening Results It Is All About The Age PDFangela_karenina_1No ratings yet
- Obermair 2003Document7 pagesObermair 2003angela_karenina_1No ratings yet
- Who Should We Cool After Perinatal AsphyxiaDocument6 pagesWho Should We Cool After Perinatal Asphyxiaangela_karenina_1No ratings yet
- Diabetes Mellitus in PregnancyDocument5 pagesDiabetes Mellitus in PregnancyRockyNo ratings yet
- Villamar, Rolando PMLS-2Document29 pagesVillamar, Rolando PMLS-2VILLAMAR, Rolando Jr. V.No ratings yet
- RSSDI - Practice GuidelinesDocument303 pagesRSSDI - Practice Guidelineschinnu prakashNo ratings yet
- 11 - Manoj Kumar MinjDocument8 pages11 - Manoj Kumar MinjIndah SarihandayaniNo ratings yet
- A Dissertation OnDocument102 pagesA Dissertation OnSaliha KabeerNo ratings yet
- Livro Robbins PathologyDocument18 pagesLivro Robbins Pathologyernestooliveira50% (2)
- Quiz 2 Gestational Diabetes MellitusDocument10 pagesQuiz 2 Gestational Diabetes MellitusShirley L. CarumbaNo ratings yet
- Clinical Biochemistry AssaysDocument29 pagesClinical Biochemistry AssaysBobskinnyNo ratings yet
- Endocrinology Module Study Guide 2023 FinalDocument24 pagesEndocrinology Module Study Guide 2023 Finaldomitam105No ratings yet
- IDF Diabetes Atlas: Global Estimates of Undiagnosed Diabetes in Adults For 2021Document9 pagesIDF Diabetes Atlas: Global Estimates of Undiagnosed Diabetes in Adults For 2021Usee TvNo ratings yet
- Diabetes, Often Referred To by Doctors As Diabetes Mellitus, Describes A Group of MetabolicDocument4 pagesDiabetes, Often Referred To by Doctors As Diabetes Mellitus, Describes A Group of MetabolicLheiDanielMariellMonteroNo ratings yet
- CDocument31 pagesCHambrian Wijaya100% (1)
- Modeling Glucose-Insulin Metabolism with Coupled ModelsDocument124 pagesModeling Glucose-Insulin Metabolism with Coupled ModelsBrasoveanu GheorghitaNo ratings yet
- 10 1097@aog 0000000000002159 PDFDocument15 pages10 1097@aog 0000000000002159 PDFHerry SasukeNo ratings yet
- Diagnosis of Diabetes MellitusDocument23 pagesDiagnosis of Diabetes MellitusNkosinathi ShongweNo ratings yet
- Diabetes MellitusDocument17 pagesDiabetes MellitusRuqayya KobatteNo ratings yet
- 1 DMDocument49 pages1 DMDrMohammad KhadrawyNo ratings yet
- Ispad 2014Document290 pagesIspad 2014Sheyla Alegre Pariona100% (1)
- Special Collections and Point of Care TestingDocument42 pagesSpecial Collections and Point of Care Testingmicah cajandabNo ratings yet
- Special Collections and Point-of-Care Testing GuideDocument12 pagesSpecial Collections and Point-of-Care Testing GuideMark GuinobanNo ratings yet