Professional Documents
Culture Documents
What Is Renal Failure
Uploaded by
Vecky TolentinoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
What Is Renal Failure
Uploaded by
Vecky TolentinoCopyright:
Available Formats
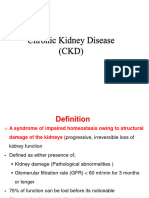
What is renal failure?
Renal failure refers to temporary or permanent damage to the kidneys that results in loss of
normal kidney function. There are two different types of renal failure--acute and chronic. Acute
renal failure has an abrupt onset and is potentially reversible. Chronic renal failure progresses
slowly over at least three months and can lead to permanent renal failure. The causes, symptoms,
treatments, and outcomes of acute and chronic are different.
Diabetic nephropathy
- Diabetes can cause permanent changes, leading to kidney damage.
What is end-stage renal disease (ESRD)?
End-stage renal disease is when the kidneys permanently fail to work.
What are the symptoms of renal failure?
The symptoms for acute and chronic renal failure may be different. The following are the most
common symptoms of acute and chronic renal failure. However, each individual may experience
symptoms differently. Symptoms may include:
Poor appetite
Urinary incontinence
Pale skin
Bad breath
Hearing deficit
Detectable abdominal mass
Tissue swelling
Irritability
Poor muscle tone
Change in mental alertness
Metallic taste in mouth
Vomiting
Bone pain
Headache
Insomnia
Itching
Dry skin
Malaise
Fatigue with light activity
Muscle cramps
High urine output or no urine output
Recurrent urinary tract infections
Pathophysiology
Chronic renal failure often progresses through four stages.
1. reduced renal reserve shows a glomerular filtration rate (gfr) of 35% to 50% of normal;
2. renal insufficiency, a gfr of 20% to 35% of normal;
3. renal failure, a gfr of 20% to 25% of normal;
4. end-stage renal disease, a gfr less than 20% of normal.
"Nephron damage is progressive; damaged nephrons can't function and don't recover. The
kidneys can maintain relatively normal function until about 75% of the nephrons are
nonfunctional. Surviving nephrons hypertrophy and increase their rate of filtration, reabsorption,
and secretion. Compensatory excretion continues as gfr diminishes.
Urine may contain abnormal amounts of protein, red blood cells (rbcs) and white blood cells or
casts. The major end products of excretion remain essentially normal, and nephron loss becomes
significant. As gfr decreases, plasma creatinine levels increase proportionately without regulatory
adjustment. As sodium delivery to the nephron increases, less is reabsorbed, and sodium deficits
and volume depletion follow. The kidney becomes incapable of concentrating and diluting urine.
If tubular interstitial disease is the cause of chronic renal failure, primary damage to the tubules-the medullary portion of the nephron--precedes failure, as do such problems as renal tubular
acidosis, salt wasting, and difficulty diluting and concentrating urine. If vascular or glomerular
damage is the primary cause, proteinuria, hematuria, and nephrotic syndrome are more
prominent.
Changes in acid-base balance affect phosphorus and calcium balance. Renal phosphate excretion
and 1,25(oh)2 vitamin d3 synthesis are diminished. Hypocalcemia results in secondary
hypoparathyroidism, diminished gfr, and progressive hyperphosphatemia, hypocalcemia, and
dissolution of bone. In early renal insufficiency, acid excretion and phosphate reabsorption
increase to maintain normal ph. When gfr decreases by 30% to 40%, progressive metabolic
acidosis ensues and tubular secretion of potassium increases. Total-body potassium levels may
increase to life-threatening levels requiring dialysis.
In glomerulosclerosis, distortion of filtration slits and erosion of the glomerular epithelial cells
lead to increased fluid transport across the glomerular wall. Large proteins traverse the slits but
become trapped in glomerular basement membranes, obstructing the glomerular capillaries.
Epithelial and endothelial injury causes poteinuria. Mesangial-cell proliferation, increased
production of extracellular matrix, and intraglomerular coagulation cause the sclerosis.
Tubulointerstitial injury occurs from toxic or ischemic tubular damage, as with acute tubular
necrosis. Debris and calcium deposits obstruct the tubules. The resulting defective tubular
transport is associated with interstitial edema, leukocyte infiltration, and tubular necrosis.
Vascular injury causes diffuse or focal ischemia of renal parenchyma, associated with thickening,
fibrosis, or focal lesions of renal blood vessels. Decreased blood flow then leads to tubular
atrophy, interstitial fibrosis, and functional disruption of glomerular filtration, medullary
gradients, and concentration.
The structural changes trigger an inflammatory response. Fibrin deposits begin to form around
the interstitium. Microaneurysms result from vascular wall damage and increased pressure
secondary to obstruction or hypertension. Eventual loss of the nephron triggers compensatory
hyperfunction of uninjured nephrons, which initiates a positive-feedback loop of increasing
vulnerability.
Eventually, the healthy glomeruli are so overburdened that they become sclerotic, stiff, and
necrotic. Toxins accumulate and potentially fatal changes ensure in all major organ systems.
You might also like
- Chronic Renal FailureDocument13 pagesChronic Renal FailureAnusha VergheseNo ratings yet
- Pathofishiologis Chronic Kidney DiseaseDocument4 pagesPathofishiologis Chronic Kidney DiseaseNisaNo ratings yet
- Presented By: Sonia Dagar: Renal FailureDocument40 pagesPresented By: Sonia Dagar: Renal FailureRavanshi ThakurNo ratings yet
- Renal FailureDocument33 pagesRenal FailureDeniela Jamaicy Herbert100% (6)
- Renal FailureDocument3 pagesRenal Failurerjones53No ratings yet
- Renal Failure: Prepare by Mohammed Sahman Basees Alsharari - 391110030Document33 pagesRenal Failure: Prepare by Mohammed Sahman Basees Alsharari - 391110030jsksNo ratings yet
- Renal SystemDocument20 pagesRenal SystemRahul DasNo ratings yet
- Kidney Function and Chronic Renal FailureDocument50 pagesKidney Function and Chronic Renal FailureKevin MontoyaNo ratings yet
- Renal FailureDocument4 pagesRenal FailureMunish DograNo ratings yet
- CKD NotesDocument11 pagesCKD NotesMaria WibawaNo ratings yet
- CaseStudy ChronicRenalFailureDocument29 pagesCaseStudy ChronicRenalFailureCarlcedrick ManlapusNo ratings yet
- Renal Failure: Prepare by Mohammed Sahman Basees Alsharari - 391110030Document31 pagesRenal Failure: Prepare by Mohammed Sahman Basees Alsharari - 391110030jsksNo ratings yet
- Pathophysiology ESRDDocument9 pagesPathophysiology ESRDJaye DangoNo ratings yet
- Acute Renal Failure TeoriDocument24 pagesAcute Renal Failure TeoriVera Andri YaniNo ratings yet
- Pathophysiology CKDDocument3 pagesPathophysiology CKDCyndi Jane Bandin CruzataNo ratings yet
- crf03 1Document16 pagescrf03 1Aswin DamodaranNo ratings yet
- FLG 332 Renal Physiology-3 (2019)Document29 pagesFLG 332 Renal Physiology-3 (2019)Huzaifa KhanNo ratings yet
- Renal Failure Renal Failure Renal Failure: Causes and ManagementDocument13 pagesRenal Failure Renal Failure Renal Failure: Causes and Managementjaycey24RM,RNNo ratings yet
- Kidney FailureDocument2 pagesKidney Failuredanee しNo ratings yet
- KidneyDocument18 pagesKidneyRacha MougharbelNo ratings yet
- Chronic Kidney DiseaseDocument17 pagesChronic Kidney Diseaseniken_rizkiNo ratings yet
- Renal Failur E: Mamta Kumari Asst - Prof. Igims-ConDocument51 pagesRenal Failur E: Mamta Kumari Asst - Prof. Igims-ConMamta KumariNo ratings yet
- Chronic Kidney DiseaseDocument41 pagesChronic Kidney DiseaseveraveroNo ratings yet
- NephritisDocument16 pagesNephritisyikesNo ratings yet
- Acute Renal FailureDocument4 pagesAcute Renal FailurePerrilyn PereyNo ratings yet
- Laporan Pendahuluan Gagal Ginjal KronikDocument26 pagesLaporan Pendahuluan Gagal Ginjal Kronikarief rafsanjaniNo ratings yet
- Acute Kidney Failure OverviewDocument13 pagesAcute Kidney Failure Overviewsingireddi1revathiNo ratings yet
- Acute-Renal-Failure Lecture OnlyDocument17 pagesAcute-Renal-Failure Lecture OnlyeyesontheskyNo ratings yet
- BubreDocument10 pagesBubreharryNo ratings yet
- Heart Failure Is Common and Is Due To Sodium and Water Retention, Acid-BaseDocument3 pagesHeart Failure Is Common and Is Due To Sodium and Water Retention, Acid-BaseLuna AstanehNo ratings yet
- Acute Renal Failure Nursing CareDocument85 pagesAcute Renal Failure Nursing Careellise abundoNo ratings yet
- Acute and Chronic Renal FailureDocument21 pagesAcute and Chronic Renal FailureStephina ImmaculateNo ratings yet
- Chronic Renal FailureDocument28 pagesChronic Renal FailuremarshmalouNo ratings yet
- Acute Renal Failur E: By: Miss Santoshi Naik Assistant Professor Yenepoya Pharmacy College & Research CentreDocument15 pagesAcute Renal Failur E: By: Miss Santoshi Naik Assistant Professor Yenepoya Pharmacy College & Research CentreAnusikta PandaNo ratings yet
- AlaaDocument7 pagesAlaaduskblade502No ratings yet
- Your Kidneys: Anatomy, Function and Common ConditionsDocument2 pagesYour Kidneys: Anatomy, Function and Common ConditionsEarl Jay UayanNo ratings yet
- Askep Gagal Ginjal - Ns. FitrioDocument32 pagesAskep Gagal Ginjal - Ns. FitriodesyNo ratings yet
- Renal Failure Cronic Group 6Document18 pagesRenal Failure Cronic Group 6Wiwi Hardiyanti100% (1)
- Acute Renal FailureDocument9 pagesAcute Renal FailureNipul MondolNo ratings yet
- Chronic Kidney Disease OverviewDocument28 pagesChronic Kidney Disease Overviewomie22100% (9)
- Chronic Kidney DiseaseDocument8 pagesChronic Kidney DiseaseAyiessa_AJNo ratings yet
- Case Analysis FinDocument64 pagesCase Analysis Finlhiamdm1208No ratings yet
- Lecture 3 CKDDocument53 pagesLecture 3 CKDPharmswipe KenyaNo ratings yet
- Renal Physiology StagesDocument22 pagesRenal Physiology Stagesسمية صالحNo ratings yet
- Acute Renal Failure & Chronic Renal FailureDocument38 pagesAcute Renal Failure & Chronic Renal FailureArti GondNo ratings yet
- Renal FailuireDocument39 pagesRenal FailuireAmbroseNo ratings yet
- Renal Diseaseppt2789Document112 pagesRenal Diseaseppt2789Sundeep SharmaNo ratings yet
- Chronic Renal FailureDocument4 pagesChronic Renal FailureHercy Emarie AnabeNo ratings yet
- Etiology: I. Predisposing FactorDocument12 pagesEtiology: I. Predisposing FactorIbcp SalvacionNo ratings yet
- HTTPDocument10 pagesHTTPkasmiatiNo ratings yet
- Presentation مسنين عمليDocument19 pagesPresentation مسنين عمليzoubia209No ratings yet
- Chronic Kidney Disease - Genitourinary Disorders - MSD Manual Professional EditionDocument11 pagesChronic Kidney Disease - Genitourinary Disorders - MSD Manual Professional EditionAdi PomeranzNo ratings yet
- Chronic Kidney DiseaseDocument11 pagesChronic Kidney DiseaseMah AlfaroNo ratings yet
- Manage Renal Failure Through Prevention, Treatment and Self-CareDocument13 pagesManage Renal Failure Through Prevention, Treatment and Self-CaretrrdsNo ratings yet
- LP CKD AnemiaDocument12 pagesLP CKD AnemiaNanan SaputraNo ratings yet
- Chronic Kidney Failure Transplant 2Document22 pagesChronic Kidney Failure Transplant 2Gail Leslie HernandezNo ratings yet
- Acute Kidney InjuryDocument6 pagesAcute Kidney Injurytherese BNo ratings yet
- The Renal Diet Kitchen: 60+ Quick and Delicious Renal Diet Recipes to Improve Kidney FunctionFrom EverandThe Renal Diet Kitchen: 60+ Quick and Delicious Renal Diet Recipes to Improve Kidney FunctionNo ratings yet
- Summary of GradesDocument1 pageSummary of GradesVecky TolentinoNo ratings yet
- What Is End-Stage Renal Disease (ESRD) ?Document2 pagesWhat Is End-Stage Renal Disease (ESRD) ?Vecky TolentinoNo ratings yet
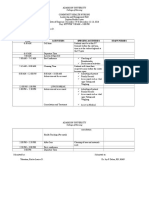
- Day 5 Time Activities Specific Activities Staff Nurses: College of NursingDocument2 pagesDay 5 Time Activities Specific Activities Staff Nurses: College of NursingVecky TolentinoNo ratings yet
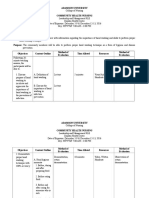
- Management Plan: Head Nurse: Tolentino, Ericka Louise Area: FEU-NRMFDocument2 pagesManagement Plan: Head Nurse: Tolentino, Ericka Louise Area: FEU-NRMFVecky TolentinoNo ratings yet
- ESRD Lab Test, Drug Study and NCPDocument3 pagesESRD Lab Test, Drug Study and NCPVecky TolentinoNo ratings yet
- ESRDDocument37 pagesESRDVecky TolentinoNo ratings yet
- ESRDDocument37 pagesESRDVecky TolentinoNo ratings yet
- Pathophy EsrdDocument4 pagesPathophy EsrdVecky TolentinoNo ratings yet
- ESRD Lab Test, Drug Study and NCPDocument3 pagesESRD Lab Test, Drug Study and NCPVecky TolentinoNo ratings yet
- Teaching Plan Hand WashingDocument4 pagesTeaching Plan Hand WashingVecky Tolentino50% (2)
- FliersDocument2 pagesFliersVecky TolentinoNo ratings yet
- Nursing Care for FatigueDocument2 pagesNursing Care for FatigueVecky TolentinoNo ratings yet
- Discharge Plan Post SeizureDocument2 pagesDischarge Plan Post SeizureVecky TolentinoNo ratings yet
- Case Study Colon CancerDocument8 pagesCase Study Colon CancerVecky Tolentino100% (4)
- Nursing Care for FatigueDocument2 pagesNursing Care for FatigueVecky TolentinoNo ratings yet
- FliersDocument2 pagesFliersVecky TolentinoNo ratings yet
- Drug StudyDocument41 pagesDrug StudyVecky TolentinoNo ratings yet
- Viii. Nursing Care Plan Assessment Nursing Diagnosis Planning Interventions Rationale EvaluationDocument6 pagesViii. Nursing Care Plan Assessment Nursing Diagnosis Planning Interventions Rationale EvaluationVecky TolentinoNo ratings yet
- Case Study Post Stroke SeizuresDocument12 pagesCase Study Post Stroke SeizuresVecky TolentinoNo ratings yet