Professional Documents
Culture Documents
Adjuvant Chemotheraphy
Uploaded by
Fatona AgungCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Adjuvant Chemotheraphy
Uploaded by
Fatona AgungCopyright:
Available Formats
Articles
Adjuvant chemotherapy versus observation in patients with
colorectal cancer: a randomised study
QUASAR Collaborative Group*
Summary
Lancet 2007; 370: 202029
See Comment page 1980
*Collaborators listed in the
webappendix
Correspondence to:
QUASAR Study Oce, CRUK
Clinical Trial Unit, Institute for
Cancer Studies,
The Medical School, Birmingham
B15 2TT, UK
QUASAR@trials.bham.ac.uk
Background The aim of the QUASAR trial was to determine the size and duration of any survival benet from adjuvant
chemotherapy for patients with colorectal cancer at low risk of recurrence, for whom the indication for such treatment
is unclear.
Methods After apparently curative resections of colon or rectal cancer, 3239 patients (2963 [91%] with stage II [node
negative] disease, 2291 [71%] with colon cancer, median age 63 [IQR 5668] years) enrolled between May, 1994, and
December, 2003, from 150 centres in 19 countries were randomly assigned to receive chemotherapy with
uorouracil and folinic acid (n=1622) or to observation (with chemotherapy considered on recurrence; n=1617).
Chemotherapy was delivered as six 5-day courses every 4 weeks or as 30 once-weekly courses of intravenous
uorouracil (370 mg/m) with high-dose (175 mg) L-folinic acid or low-dose (25 mg) L-folinic acid. Until 1997,
levamisole (12 courses of 450 mg over 3 days repeated every 2 weeks) or placebo was added. After 1997, patients
who were assigned to receive chemotherapy were given uorouracil and low-dose folinic acid only. The primary
outcome was all-cause mortality. Analyses were done by intention to treat. This trial is registered with the
International Clinical Trial Registry, number ISRCTN82375386.
Findings At the time of analysis, 61 (38%) patients in the chemotherapy group and 50 (31%) in the observation
group had missing follow-up. After a median follow-up of 55 (range 0106) years, there were 311 deaths in the
chemotherapy group and 370 in the observation group; the relative risk of death from any cause with chemotherapy
versus observation alone was 082 (95% CI 070095; p=0008). There were 293 recurrences in the chemotherapy
group and 359 in the observation group; the relative risk of recurrence with chemotherapy versus observation alone
was 078 (067091; p=0001). Treatment ecacy did not dier signicantly by tumour site, stage, sex, age, or
chemotherapy schedule. Eight (05%) patients in the chemotherapy group and four (025%) in the observation
group died from non-colorectal cancer causes within 30 weeks of randomisation; only one of these deaths was
deemed to be possibly chemotherapy related.
Interpretation Chemotherapy with uorouracil and folinic acid could improve survival of patients with stage II colorectal
cancer, although the absolute improvements are small: assuming 5-year mortality without chemotherapy is 20%, the
relative risk of death seen here translates into an absolute improvement in survival of 36% (95% CI 1060).
Introduction
Colorectal cancer is the second most common malignant
disease in developed countries, with 1 million new cases
and 500 000 deaths worldwide every year.1 Cytotoxic
chemotherapy, after apparently complete resection, can
lower the risk of recurrence, but there has been debate
over which patients benet from such adjuvant treatment
and which drug regimens are most eective. A 1-year
course of uorouracil plus levamisole2,3 was widely
recommended as standard treatment for stage III (node
positive) colon cancer in the early 1990s.4,5 However,
subsequent evidence has established that a 6-month
regimen of uorouracil coupled with folinic acid69 is at
least as eective,1012 and that adding levamisole to
uorouracil regimens does not improve outcome.10,13 The
benets from adjuvant uorouracil and folinic acid are
supported by a clear pharmacological rationale14 and by
denite evidence that folinic acid enhances the activity
of uorouracil in advanced disease.15
Chemotherapy with uorouracil and folinic acid has,
therefore, become widely used for stage III (node
2020
positive) colon cancer. However, there remains uncertainty whether stage II (node negative) patients
derive sucient benet from adjuvant chemotherapy to
justify the toxicity, costs, and inconvenience of
treatment.16 Furthermore, although the eect of
adjuvant chemotherapy is assumed to be similar in
rectal and colon cancer, there is little direct randomised
evidence to support this. Giving uorouracil
concurrently with radiotherapy does seem to improve
survival over radiotherapy alone,17 but this could be due
to synergy between radiotherapy and uorouracil. Most
previous trials of uorouracil and folinic acid have
included only patients with colon cancer, and a Dutch
trial of uorouracil and levamisole showed benet in
colon but not rectal cancer.3 Consequently, there has
been doubt among many clinicians whether patients
with rectal cancerwhether node positive or negative
benet from adjuvant chemotherapy. The QUASAR
(QUick And Simple And Reliable) trial was designed to
provide large-scale randomised evidence on the value of
adjuvant chemotherapy with uorouracil and folinic
www.thelancet.com Vol 370 December 15, 2007
Articles
acid in both colon and rectal cancer and, in particular,
in stage II disease.
7559 patients with complete
resection of colon or
rectal cancer
Methods
Patients
Patients were eligible if they were thought to have had a
complete resection of colon or rectal cancer with no
evidence of distant metastases, and if they had no denite
contraindications
to
chemotherapy.
No
prior
chemotherapy was allowable other than a 1 week
post-operative portal vein infusion of uorouracil. Written
consent was sought before randomisation, and after a full
written and verbal explanation of the treatment options
had been given. Ethics approval for the study was given
by the local research ethics committee at each hospital.
Procedures
QUASAR adopted a pragmatic trial design,13 with local
clinical teams categorising patients as having either a clear
or an uncertain indication for adjuvant chemotherapy. The
indication for chemotherapy was decided by each patients
clinicians, after consultation with the patient, rather than
by any per-protocol denition. In practice, lymph node
status was the key discriminant, with 70% of those deemed
to have a clear indication for chemotherapy having stage
III disease, while 91% of those with an uncertain indication
had stage II disease. Data for the patients with a clear
indication for chemotherapy have been reported
elsewhere.13 Patients with an uncertain indication for
chemotherapy were randomly assigned to receive adjuvant
chemotherapy or to observation, but with chemotherapy
considered in the event of recurrence. A minimised
randomisation procedure was used to ensure that
allocations were balanced with respect to age, tumour site,
stage, portal vein infusion or not, pre-operative radiotherapy
or not, planned post-operative radiotherapy or not, and
chemotherapy schedule (weekly or every 4 weeks).
Randomisation was done by telephone call to a central
oce. Until October, 1997, those allocated to receive
chemotherapy were simultaneously randomly allocated to
receive uorouracil plus either high-dose or low-dose
folinic acid, each combined with levamisole or placebo.
Subsequently, all patients allocated to receive chemotherapy
received uorouracil plus low-dose folinic acid.
Chemotherapy consisted of 30 doses of uorouracil
(370 mg/m2 intravenously) combined with either high-dose
(175 mg intravenously) or low-dose (25 mg intravenously)
L-folinic acid. L-folinic acid, the active isomer, is equivalent,
pharmacologically, to double the dose of racemic folinic
acid.18 It was recommended that chemotherapy be given in
six 5-day courses every 4 weeks, but a 30-week schedule of
once weekly administration was also allowable.19 The dose
of uorouracil for subsequent courses was reduced if
substantial toxicity occurred after the previous course.
Levamisole (50 mg or matching placebo) was given three
times daily for 3 days repeated every 2 weeks for 12 courses.
Chemotherapy and levamisole or placebo treatment
www.thelancet.com Vol 370 December 15, 2007
4320 patients with
clear indication for
chemotherapy
3239 patients with
uncertain indication
for chemotherapy
1617 patients randomly assigned
to observation alone
6 patients received
chemotherapy
1611 did not
47 not agged or
follow-up not received
3 lost to follow-up
1567 patients with recent
follow-up available
for analysis
1622 patients randomly assigned to receive
chemotherapy (607 up to 1997, 1015 after 1997*)
45 did not receive any chemotherapy
1577 start chemotherapy, of whom 13%
receive <80%, 19% receive 8099% and
58% receive 100% of scheduled chemotherapy
54 not agged or
follow-up not received
7 lost to follow-up
1561 patients with recent
follow-up available
for analysis
Figure 1: Trial prole
*Until October, 1997, chemotherapy was delivered as intravenous uorouracil (370 mg/m) with either high-dose
(175 mg) or low-dose (25 mg) L-folinic acid, each combined with levamisole or placebo. After October, 1997, patients
who were assigned to receive chemotherapy were given uorouracil and low-dose folinic acid only.
started in the same week, if possible within 6 weeks of
surgery. Use of radiotherapy for rectal cancers, and all
other aspects of patient management, were left to the
discretion of the responsible physician.13
To facilitate large-scale recruitment, QUASAR adopted a
streamlined trial design13,20 with no extra investigations and
minimal extra workload for participating clinicians.
Important prognostic data were collected at randomisation.
Collaborators were required to notify the trial oce of any
serious unexpected adverse experiences believed to be due
to chemotherapy. But, apart from this, there was just one
yearly follow-up form that requested brief details of serious
toxicity, recurrence, and death. In the UK, this information
was supplemented by use of national mortality records
with extra information sought from clinicians on the
causes of deaths without recorded recurrence. Flagged
patients from England and Wales were assumed to be alive
as of January, 2005, unless notied otherwise. A postal
follow-up of the status of all patients was done in
January, 2004. For analyses of recurrence, and for survival
analyses for patients who had not been successfully
agged, analyses were censored at March, 2004, if a
follow-up reply was received or at last follow-up otherwise.
Dispensing pharmacists were asked to record the doses
and schedule of uorouracil and folinic acid until 1998,
2021
Articles
when central supplies of folinic acid were discontinued.
Health economic data, compliance, treatment toxicity, and
quality of life were measured in a substudy (n=700, from
selected centres in the West Midlands) through patient
questionnaires (European Organisation for Research and
Treatment of Cancer QLQ-3021 with colorectal cancer,22
resource usage modules, and the hospital anxiety and
depression scale23) completed before chemotherapy and
then at 3, 6, 15, and 27 months. Detailed toxicity data were
recorded at the same time points from patient notes.
Pathological reports were requested retrospectively from
all patients. At the time of submission, 650 such reports
Chemotherapy
(n=1622)
Observation
(n=1617)
Stage
I
8 (05%)
8 (05%)
II
1483 (91%)
1480 (92%)
III
131 (8%)
129 (8%)
1148 (71%)
1143 (71%)
474 (29%)
474 (29%)
Site
Colon
Rectum (or both)
Sex
Male
Female
1006 (62%)
973 (60%)
616 (38%)
644 (40%)
Age (years)
<50
185 (11%)
185 (11%)
5059
427 (26%)
428 (26%)
6069
678 (42%)
673 (42%)
70+
331 (20%)
332 (21%)
Range in years
2386
2384
Median age
63 (5668)
63 (5668)
Other adjuvant therapy
Pre-operative radiotherapy
102 (6%)
101 (6%)
Postoperative radiotherapy
133 (8%)
131 (8%)
Portal vein infusion
6 (04%)
5 (03%)
Intended chemotherapy schedule
5-day course every 4 weeks
769 (47%)
765 (47%)
Once weekly
853 (53%)
852 (53%)
Fluorouracil+high-dose folinic acid
+levamisole*
141 (9%)
NA
Fluorouracil+high-dose folinic acid
+placebo*
143 (9%)
NA
Fluorouracil+low-dose folinic acid
+levamisole*
142 (9%)
NA
Fluorouracil+low-dose folinic acid
+placebo*
141 (9%)
NA
Fluorouracil+high-dose folinic acid
20 (1%)
NA
Fluorouracil+low-dose folinic acid
20 (1%)
NA
Fluorouracil+low-dose folinic acid
1015 (63%)
NA
Chemotherapy allocated
No chemotherapy
NA
1617
Data are n (%) or median (IQR). *Randomised between high-dose and low-dose
folinic acid and between levamisole and placebo. Randomised between highdose and low-dose folinic acid.
Table: Baseline characteristics of randomised patients
2022
had been received; these reports were reviewed centrally.
To assess cost-eectiveness as cost per quality-adjusted
life-year (QALY), the average life-years gained through
improved survival with chemotherapy were estimated by
use of UK national mortality statistics and the QALYs lost
during chemotherapy by assigning a utility score to
quantify the reduction in health-related quality of life
while undergoing chemotherapy.
Statistical analysis
Target recruitment was at least 2500 patients, which
would give a more than 80% chance of detecting a
5% improvement in survival (eg, from 75% to 80%)
between chemotherapy (any) and control, at a signicance
level of less than 005. The decision to close recruitment
was made by the trial steering committee without
knowledge of interim results. The primary outcome
measure was all-cause mortality. Secondary outcomes
were death from colorectal cancer, and recurrence.
Analyses were by intention to treat and used standard
log-rank methods. Tests for heterogeneity of treatment
eect between subgroups were as described by the Early
Breast Cancer Trialists Collaborative Group,24 using
recurrence as the most statistically sensitive outcome
measure. Prior hypotheses were that the monthly 5-day
schedule would be more eective than the once-weekly
schedule and that chemotherapy within 6 weeks of
surgery would be more eective than later.
Analyses were done with SAS version 9.1. This trial is
registered with the International Clinical Trial Registry,
number ISRCTN82375386.
Role of the funding source
The general structure of the study was designed by the
UK Coordinating Committee on Cancer Research
(London, UK; now the National Cancer Research
Institute), and managed, analysed, and reported
independently of the funding body or any companies,
who had no representative in its organisation and who,
like the steering committee, remained blind to the results
as they accumulated. All authors had access to all the
data and had nal responsibility for the decision to
submit for publication.
Results
Between May 25, 1994, and Dec 24, 2003, 3239 patients
were entered into the uncertain indication arm of
QUASAR by 332 clinicians from 150 centres in
19 countries. Figure 1 shows the trial prole. Patients
were well balanced with respect to baseline characteristics
(table). The median age of the patients was 63 (IQR 56
68) years; 1979 (61%) were men; 2291 (71%) had colon
cancer; 260 (8%) had stage III, 2963 (91%) stage II, and
16 (05%) stage I disease. Of the 628 patients with data
for vascular invasion and T stage, 81 (13%) had vascular
invasion, 78 (13%) had T4 tumours, and 32 (5%) had
both. If allocated, chemotherapy was scheduled for
www.thelancet.com Vol 370 December 15, 2007
Articles
www.thelancet.com Vol 370 December 15, 2007
group and 132 (127%) of 1040 patients in the observation
group experiencing a recurrence after 2 years (p=094).
The proportional reduction in recurrence with
chemotherapy versus observation alone was much the
same in patients with stage II and in those with stage III
cancer, and in patients with colon and those with rectal
cancer (gure 3). There was also no signicant dierence
in the eect size between men and women, once-weekly
chemotherapy and chemotherapy every 4 weeks, or in
time from surgery to randomisation (gure 3). The
relative risk of recurrence with chemotherapy compared
with observation alone in patients with stage II cancer
was 078 (95% CI 066093; p=0004) and 068 (95% CI
052088; p=0004) in those with rectal cancer (gure 4).
There was no reduction in recurrence for patients aged
over 70 years, but this apparently lesser treatment benet
with increasing age did not reach statistical signicance
A
See Online for webtables 1 and 2
100
90
80
Chemotherapy
Observation
Survival (%)
70
60
50
40
30
20
Deaths OE Var
Chemotherapy 311
345 1702
Observation
370
10
0
Number still at risk
Chemotherapy 1622
Observation 1617
1510
1510
1325
1288
1095
1068
915
890
773
735
627
574
445
412
282
275
129
128
22
19
100
90
80
70
Recurrence (%)
5 days every 4 weeks for 1534 (47%) patients and once a
week for 1705 (53%). Chemotherapy was mainly
uorouracil plus low-dose folinic acid (1318 of
1622 patients, 81%) without levamisole (1337 of
1622 patients, 82%), with 03% also receiving a
postoperative portal vein infusion of uorouracil.
198 (21%) of the 948 patients with rectal cancer or both
rectal and colon cancer had received pre-operative
radiotherapy, 202 (28%) of these patients were scheduled
for postoperative radiotherapy.
3% (45/1622) of patients allocated chemotherapy did
not start (gure 1). Of those who did, pharmacy record
cards were available for 742 (47%), with 428 (58%)
receiving their full chemotherapy and 558 (77%) at least
80%. In those receiving chemotherapy every 4 weeks,
the cumulative dose of uorouracil was higher for those
aged under 70 years than for older patients
(179 g vs 156 g, p<00001; webtable 1); by contrast, of
the patients receiving once-weekly chemotherapy, there
was no dierence in cumulative dose between those
aged under 70 years and older patients (183 g vs 180 g,
p=009). Radiotherapy use was similar in the
chemotherapy and observation groups.
2793 (86%) patients in QUASAR were entered from the
UK, of whom 2712 (97%) were successfully agged with
the national death registry, and were thus assumed to be
alive as of January, 2005, unless notied otherwise.
Replies to the postal follow-up have been received at the
time of this report for 2306 (90%) of the 2558 patients
still alive. 111 (4%) of the 2558 patients alive had missing
follow-upie, not agged or no recent follow-up received.
The median follow-up of the surviving patients
is 55 (range 0106) years.
Over the whole study period, there were 311 deaths in
the chemotherapy group and 370 in the observation
group. The relative risk of dying from any cause with
chemotherapy versus observation was 082 (95% CI
070095; p=0008; gure 2). The numbers of deaths
from causes other than colorectal cancer were similar in
the chemotherapy and observation groups: 77 (47%) died
in the chemotherapy group versus 86 (53%) in the
observation group (p=03; webtable 2). The relative risk
of dying from colorectal cancer was 081 (95% CI
068096; p=001).
There were 293 recurrences in the chemotherapy group
and 359 in the observation group. The relative risk of
recurrence with chemotherapy versus observation over the
whole study period was 078 (95% CI 067091; p=0001;
gure 2). There was signicant heterogeneity in treatment
eect by period of follow-up, with 149 (92%) recurrences
in the chemotherapy group in the rst 2 years after
randomisation, compared with 227 (140%) in those in the
observation group (p=0004). The relative risk of recurrence
in the rst 2 years with chemotherapy versus observation
was 064 (95% CI 052078; p<00001; gure 3).
Subsequently, there was no benet, or loss of benet,
with 144 (128%) of 1127 patients in the chemotherapy
60
50
40
30
20
Events OE Var
Chemotherapy 293
409 1629
Observation
359
10
0
0
Number still at risk
Chemotherapy 1622
Observation 1617
1420
1390
1175
1088
962
895
4
5
6
Years from randomisation
784
736
645
598
482
435
309
292
159
154
10
41
42
1
..
Figure 2: (A) Risk of all cause mortality and (B) recurrence
2023
Articles
Events/patients
Events in chemotherapy group
Chemotherapy Observation
(OE) Var
Relative risk and CI
Site
199/1148
230/1143
(173%)
(201%)
94/474
129/474
(198%)
(272%)
Interaction between two groups =15; p=021
Colon
196 1072
083 (065107)
Rectum or both
216
068 (048096)
556
Stage
Stage I
Stage II colon
Stage II rectum
Stage III
1/8
(125%)
164/1073
(153%)
70/410
(171%)
58/131
(443%)
2/8
(250%)
194/1073
(181%)
95/407
(233%)
68/129
(527%)
06
07
176
895
082 (063108)
151
412
069 (046104)
100
313
073 (046115)
250
982
078 (060101)
156
647
079 (057108)
36
130
076 (037155)
153
399
068 (045102)
264
740
070 (052094)
45
357
113 (074175)
107
772
087 (065117)
303
856
070 (053093)
275
865
073 (055096)
138
755
083 (062112)
418
940
064 (049084)
Heterogeneity between four groups =12; p=076
Sex
177/1006
(176%)
116/616
(188%)
Men
Women
216/973
(222%)
143/644
(222%)
Interaction between two groups =00; p=093
Age
<50 years
5059 years
6069 years
70+ years
23/185
(124%)
65/428
(152%)
129/678
(190%)
76/331
(230%)
29/185
(157%)
95/427
(222%)
168/673
(250%)
67/332
(202%)
Heterogeneity between four groups =66; p=009
Test for trend over four groups =31; p=008
Schedule
145/853
164/852
(170%)
(192%)
148/769
195/765
Every 4 weeks (intent)
(192%)
(255%)
Interaction between two groups =19; p=017
Once a week (intent)
Time to treatment
200/818
Surgery to randomisation <6 weeks 146/816
(179%)
(244%)
158/788
Surgery to randomisation 6+ weeks 145/799
(181%)
(201%)
Interaction between two groups =07; p=039
Time from randomisation
149/1622
(92%)
127/1127
(113%)
17/564
(30%)
Years 01
Years 24
Years 5+
227/1617
(140%)
107/1040
(103%)
25/511
(49%)
59
584
111 (079155)
49
105
063 (028139)
409 1629
078 (064095)
Heterogeneity between three groups =113; p=0004
Test for trend over three groups =41; p=004
Unstratied
293/1622
(181%)
359/1617
(222%)
Relative risk and 99% CI
Relative risk and 95% CI
0
05
10
15
20
Chemotherapy better
Observation better
Figure 3: Relative risk of recurrence with chemotherapy by site, stage, sex, age, chemotherapy schedule, and timing
See Online for webgure 1
2024
(p=009; gure 3). Comparison of the proportional
reductions in recurrence in the 2 years after
randomisation, where the most extreme eect of
chemotherapy is seen (gure 3), showed a similar,
borderline signicant pattern of decreasing benet with
age (p=005; webgure 1). The relative risk of recurrence
in the 2 years after randomisation was 071 (95% CI
054092; p=001) for patients with stage II colon cancer
www.thelancet.com Vol 370 December 15, 2007
Articles
100
90
Recurrence (%)
80
Chemotherapy
Observation
70
60
50
40
Events OE Var
Chemotherapy 234
325 1307
Observation
289
Events OE Var
Chemotherapy 94
216 556
Observation
129
30
20
10
0
Number still at risk
Chemotherapy 1483 1298 1077 886
Observation 1480 1280 1013 834
721
685
591
554
439
400
280
269
143
142
36
38
1
..
474
474
407
394
339
304
279
248
222
201
185
161
143
119
97
83
52
45
15
14
..
..
100
90
80
Survival (%)
70
60
50
40
30
20
10
Deaths OE Var
Chemotherapy 252
233 1362
Observation
293
Deaths OE Var
Chemotherapy 103
150 580
Observation
129
p=005
p=005
0
0
1
2
3
4
5
6
7
Years from randomisation
Number still at risk
Chemotherapy 1483 1381 1214 1006 841 709 573 405
Observation 1480 1388 1196 989 825 679 533 379
255
252
113
117
10
17
18
474
474
437
433
383
370
316
310
4
5
6
7
Years from randomisation
260
257
216
203
177
159
132
118
10
88
80
41
38
8
5
Figure 4: Eect of chemotherapy on (A) recurrence and (B) survival for stage II patients and on (C) recurrence and (D) survival for patients with rectal cancer
and 057 (95% CI 038089; p=0007) for patients with
stage II rectal cancer (gure 5). For patients aged under
70 years, the relative risk of recurrence in the 2 years after
randomisation was 059 (95% CI 043082; p=00008)
for those with stage II colon cancer and 058 (95%CI
038093; p=001) for those with stage II rectal cancer
(webgure 2).
Subgroup investigations of mortality were less reliable
than for recurrence because of the lesser treatment eect,
but followed a similar pattern (gure 6). The relative risk
of death from any cause in patients with stage II cancer
was 084 (95% CI 068100; p=0046) and 077 (95%CI
054100; p=005) for those with rectal cancer (gure 4).
Serious, unexpected adverse events were rare:
eight (05%) patients in the chemotherapy group and
four (025%) of those in the observation group died from
non-colorectal cancer causes within 30 weeks of
randomisation (webtable 2). Only one of these deaths was
deemed to be possibly chemotherapy related.
Quality-of-life measurements directly related to expected
toxicity (diarrhoea, nausea, vomiting, mouth pain, fatigue,
appetite loss, and social functioning) were worse in those
patients in the chemotherapy group than in those in the
observation group (p<0001 for all categories), but only
www.thelancet.com Vol 370 December 15, 2007
during chemotherapy. Chemotherapy patients with
clinician-rated grade 3/4 toxicity reported worse global
quality of life than did those with lesser or no toxicity. The
only material dierence between chemotherapy regimens
was between schedules with more grade 3/4 toxicity with
the four-weekly than the once-weekly schedule. The proportion of patients with grade 3/4 nausea
(6% of 200 patients vs 1% of 227 patients), oral adverse
events (10% vs 0%), diarrhoea (11% vs 5%), neutropenia
(7% vs 1%), and any grade 3/4 toxicity (31% vs 10%]) was
signicantly greater with 4-week courses of chemotherapy
than with once-weekly delivery (p<0001 for all adverse
events; webtable 3).
Resource usage, other than for chemotherapy
administration, did not dier between patients
randomised to chemotherapy and observation. The cost
of delivering QUASAR chemotherapy was estimated to
be between 2000 and 3000 per person. A utility score
for QUASAR chemotherapy was not measured directly,
but in view of the minor eect of chemotherapy on quality
of life, was estimated to be 07 during the 6 months of
chemotherapyie, a loss of about 8 weeks of full health
life. Sensitivity analyses indicate that the two chief
determinants of cost per QALY are the size of survival
See Online for webgure 2
See Online for webtable 3
2025
Articles
Events/patients
Events in chemotherapy group
Chemotherapy Observation
(OE) Var
Colon stage II
86/1073
(80%)
120/1073
(112%)
179
515
Rectum stage II
35/410
(85%)
60/407
(147%)
132
237
Colon stage III
16/70
(229%)
23/67
(343%)
47
97
Rectum stage III
11/61
(180%)
23/62
(371%)
70
85
417
935
Relative risk and CI
071 (049101)
(p=001)
057 (034097)
(p=0007)
062 (027141)
(p=013)
044 (018106)
(p=002)
Heterogeneity between four groups =20; p=057
Unstratied
148/1614
(92%)
226/1609
(140%)
Relative risk and 99% CI
Relative risk and 95% CI
064 (049084)
(p<00001)
05
Chemotherapy better
10
15
20
Observation better
Figure 5: Relative risk of recurrence in rst 2 years after randomisation by stage and site
See Online for webgure 3
benet from chemotherapy and the life expectancy (ie,
age) of the patient (webgure 3). For patients under the
age of 70 years, there was a net gain of a few months of
QALYs even with the lowest estimate of treatment ecacy.
By the age of 80 years, only at the highest estimate of
treatment ecacy was a small net benet seen.
Discussion
The results presented here indicate that, relative to
observation alone, adjuvant chemotherapy with
uorouracil and folinic acid lowers the risk of all-cause
mortality in patients with colorectal cancer who have had
successful resection of the cancer, and who have an
uncertain indication for chemotherapy, by almost a fth.
Of particular interest is the evidence of an improvement
in survival with chemotherapy for patients with stage II
cancer. Although this improvement was of borderline
statistical signicance, the survival benet is supported
by a signicant reduction in recurrence, by evidence that
3-year disease-free survival is a good surrogate for overall
survival,25 by unequivocal evidence from previous trials
of a survival benet for stage III patients,26 by evidence
from pooled analyses of other randomised trials,27,28 and
from individual studies3,29 that suggest that the
proportional reductions in mortality and recurrence from
adjuvant chemotherapy based on uorouracil are much
the same in patients with stage II and III disease. The
data presented here are also consistent with previous trial
evidence, a meta-analysis of which found a mortality risk
ratio of 087 (95% CI 073101; p=007) for patients
with stage II disease.30
There is also evidence that, relative to observation
alone, the risk of death or recurrence in patients with
rectal cancer who received adjuvant chemotherapy was
lowered, indicating that the previously reported lack of
benet in this subgroup3 was probably falsely negative.
In QUASAR, the eect of chemotherapy on recurrence
was larger, albeit not signicantly so, in patients with
2026
stage II rectal cancer than it was in those with stage II
colon cancer. The reduction in stage II colon cancer did
not reach statistical signicance (gure 3), but this could
be explained by the the limited statistical sensitivity of
such subgroup investigations,20 particularly when
subdividing analyses by disease stage and then again by
site. Comparisons of recurrence rates in the rst 2 years
after randomisationthe period when the full eect of
chemotherapy is seenare statistically more reliable
than are comparisons of all events. The relative risks of
recurrence in the rst 2 years were similar in patients
with stage II colon cancer and in those with stage II rectal
cancer (gure 5).
Although probably real, the survival benet from
chemotherapy for a patient with stage II colorectal
cancer is small: if 5-year mortality without chemotherapy
is 20%, a reduction in the relative risk of death of 18%
(95% CI 530) translates into an absolute improvement
in survival of 36% (1060). One encouraging nding
is thatby contrast with a recent trial report31
chemotherapy seems to prevent a proportion of
recurrences and deaths, rather than just delaying them,
which makes the life-years gained more substantial,
especially for younger patients. For example, for a
55-year-old, who would have a life expectancy of 30 more
years if not dying of their cancer, reducing their 5-year
risk of cancer death by 36% (eg, from 20% to 164%)
would increase their life expectancy by about a year. By
contrast, a sustained 36% improvement in survival for
a 75-year-old, with a life expectancy of about 10 years,
would increase their life expectancy by only 4 months.
If a 2-month deduction is made for loss of
quality-adjusted life during chemotherapy, the average
QALYs gained are 10 versus 2 months. Furthermore,
the results presented here suggest that the proportional
reduction in mortality with chemotherapy is less for
older patients. However, this nding could be a false
negative, since other studies have reported benet for
www.thelancet.com Vol 370 December 15, 2007
Articles
patients over the age of 70 years.32,33
Current recommendations are that patients with
stage II disease who have a higher than average risk of
tumour recurrenceeg, those with stage T4 disease or
vascular invasion, about 30% of the QUASAR study
populationshould
be
oered
chemotherapy.16
Pathological data were available for only 20% of the study
population, and so any dierence in ecacy between
those with high-risk stage II disease and those with
low-risk stage II disease could not be investigated.
Deaths/patients
Events in chemotherapy group
Chemotherapy Observation
(OE) Var
Relative risk and CI
Site
Colon
Rectum or both
208/1148
(181%)
103/474
(217%)
241/1143
(211%)
129/474
(272%)
195
1122
084 (066107)
150
580
077 (055108)
10
05
140
927
Interaction between two groups =03; p=060
Stage
Stage I
Stage II colon
Stage II rectum
Stage III
0/8
(00%)
173/1073
(161%)
79/410
(193%)
59/131
(450%)
2/8
(250%)
198/1073
(185%)
95/407
(233%)
75/129
(581%)
086 (066112)
95
435
080 (054119)
125
333
069 (044107)
191 1087
084 (066107)
146
079 (057110)
Heterogeneity between four groups =28; p=042
Sex
201/1006
(200%)
110/616
(179%)
Men
Women
234/973
(240%)
136/644
(211%)
614
Interaction between two groups =02; p=070
Age
<50 years
5059 years
6069 years
70+ years
20/185
(108%)
63/428
(147%)
133/678
(196%)
95/331
(287%)
23/185
(124%)
83/427
(194%)
171/673
(254%)
93/332
(280%)
17
107
085 (039187)
101
364
076 (049116)
232
759
074 (055099)
08
470
102 (070148)
102
820
088 (066117)
245
882
076 (058100)
178
877
082 (062107)
174
815
081 (061107)
160
567
075 (054106)
44
780
095 (071127)
142
355
067 (044103)
345
1702
082 (067099)
Heterogeneity between four groups =33; p=035
Test for trend over four groups =12; p=028
Schedule
Once a week (intent)
Every 4 weeks (intent)
154/853
(181%)
157/769
(204%)
174/852
(204%)
196/765
(256%)
Interaction between two groups =10; p=032
Time to treatment
196/818
Surgery to randomisation <6 weeks 155/816
(190%)
(240%)
173/788
Surgery to randomisation 6+ weeks 154/799
(193%)
(220%)
Interaction between two groups =00; p=095
Time from randomisation
Years 01
Years 24
Years 5+
98/1622
(60%)
154/1227
(126%)
59/668
(88%)
129/1617
(80%)
158/1182
(134%)
83/629
(132%)
Heterogeneity between three groups =34; p=018
Test for trend over three groups =01; p=079
Unstratied
311/1622
(192%)
Relative risk and 99% CI
Relative risk and 95% CI
370/1617
(229%)
05
10
15
20
Chemotherapy better
Observation better
Figure 6: Relative risk of death with chemotherapy by site, stage, sex, age, chemotherapy schedule, and timing
www.thelancet.com Vol 370 December 15, 2007
2027
Articles
See Online for webappendix
2028
However, the similar proportional reductions with
chemotherapy in the risk of recurrence in patients with
stage II disease and those with stage III disease suggest
that the proportional reductions in the risk of recurrence
in high-risk and in low-risk stage II disease will also be
similar. Thus, because pathological variables are only
moderately prognostic of outcome in stage II disease,
they are only moderately useful as discriminants of
treatment benet. For example, preliminary analyses of
pathological data from QUASAR suggest that the 5-year
risks of death for an untreated patient with stage II
disease with and without high-risk features are about 30%
and 20%, respectively (data not shown). The absolute
benet from an 18% reduction in mortality would
be 54% in those with high-risk features and 36% in
those without, which might both be considered sucient
to justify well-tolerated QUASAR-type chemotherapy,34 at
least for younger patients. Reliable predictors of
sensitivity to chemotherapy would constitute a more
useful means to help individualise adjuvant therapy.
QUASAR includes a substudy of stored cancer tissue
that will help clarify the role of high-risk factors in stage II
disease and, hopefully, identify tumour markers that will
enable targeting of treatment at the most responsive
patients.
The optimum chemotherapy regimen for stage II
disease is unclear. 20% of patients in QUASAR received
levamisole or high-dose folinic acid, or both, but this has
no relevant eect on interpretation of the study ndings
because neither the addition of levamisole nor use of a
higher dose of folinic acid had any eect on the ecacy of
the combination of uorouracil and folinic acid.10,12,13
Treatment every 4 weeks had a larger eect on recurrence
than did the once-weekly regimen; however, the
once-weekly regimen was less toxic. Furthermore, the two
schedules seemed to have similar ecacy in patients in
QUASAR who had a clear indication for treatment.19 If
treatment every 4 weeks is more eective than the
once-weekly schedule then the benets from an optimum
chemotherapy regimen will be larger than reported here.
Similarly, enhanced survival benets might be achieved
with newer chemotherapy regimens that are more
ecacious at preventing recurrence than is the
combination of uorouracil and folinic acid.3537 However,
whether these newer regimens produce a worthwhile
extra survival benet has yet to be established. Furthermore,
safety is a major consideration in choosing adjuvant
chemotherapy, in particular for patients at low risk of
recurrence. There have been ve toxicity-related deaths
all receiving treatment every 4 weeks13in almost
6000 patients treated with chemotherapy in QUASAR,
considerably fewer than reported with newer chemotherapy
regimens.3539
The small but denite benet from well-tolerated
chemotherapy found here should provide helpful new
information for discussions between patients and
physicians on the potential benets of chemotherapy,
and allow the patient to make a better informed decision
to proceed with, or refuse, the oer of chemotherapy.
Longer follow-up of QUASAR, and meta-analysis with
other studies, is needed to resolve whether chemotherapy
produces worthwhile benets for those aged over
70 years, and further trials are needed to dene the
optimum chemotherapy regimen.
Contributors
The writing committee consisted of Richard Gray (Birmingham
Clinical Trials Unit, University of Birmingham, Birmingham, UK),
Jennifer Barnwell (CRUK Trials Unit, University of Birmingham,
Birmingham, UK), Christopher McConkey (Warwick Medical School
Clinical Trials Unit, University of Warwick, Coventry, UK),
Robert K Hills (Welsh School of Medicine, Cardi University, Cardi,
UK), Norman S Williams (Royal London Hospital, London, UK), and
David J Kerr (Department of Clinical Pharmacology, University of
Oxford, Oxford, UK). A full list of contributors can be found in the
webappendix.
Conict of interest statement
None of the writing committee members have any conict of interest to
declare.
Acknowledgments
We thank the patients who participated in QUASAR, without whose help
this study would not have been possible. QUASAR was funded
principally by the UK Medical Research Council, the Imperial Cancer
Research Fund, the Cancer Research Campaign (now merged as CRUK),
and the Department of Health. Randomisation and other support was
provided by the BHF/CR UK/MRC Clinical Trial Service Unit, Oxford.
Additional sponsorship (for meeting costs) was provided by Lederle (now
Wyeth-Ayerst), who also donated L-folinic acid, and by the Mark Hardy
Research Fund. Levamisole was donated by Janssen Pharmaceuticals.
References
1
Ferlay J, Bray E, Pisani P, Parkin DM. GLOBOCAN 2002: cancer
incidence, mortality and prevalence worldwide. IARC CancerBase
number 5, version 2.0. Lyon, France: IARC Press, 2004.
2
Moertel CG, Fleming TR, Macdonald JS, et al. Levamisole and
uorouracil as adjuvant therapy of resected colon carcinoma.
N Engl J Med 1990; 322: 35258.
3
Taal BG, van Tinteren H, Zoetmulder FA, et al. Adjuvant 5FU plus
levamisole in colonic or rectal cancer: improved survival in stage II
and III. Br J Cancer 2001; 85: 143743.
4
Seventh Kings Fund Forum. Cancer of the colon and rectum
consensus statement. Brit J Surg 1990; 77: 106365.
5
Anon. NIH Consensus Conference: adjuvant cancer therapy. JAMA
1990; 264: 144450.
6
Francini G, Petrioli R, Lorenzini L, et al. Folinic acid and
5-uorouracil as adjuvant chemotherapy in colon cancer.
Gastroenterology 1994; 106: 899906.
7
International Multicentre Pooled Analysis of Colorectal Cancer
Trials (IMPACT) Investigators. Ecacy of adjuvant uorouracil and
folinic acid in colon cancer. Lancet 1995; 345: 93944.
8
OConnell M, Mailliard J, Kahn MJ, et al. Controlled trial of
uorouracil and low-dose leucovorin given for 6 months as
post-operative adjuvant therapy for colon cancer. J Clin Oncol 1997;
15: 24650.
9
Wolmark N, Rockette H, Fisher B, et al. The benet of leucovorin
modulated uorouracil as postoperative adjuvant therapy for primary
colon cancer: results from National Surgical Adjuvant Breast and
Bowel Project protocol C-03. J Clin Oncol 1993; 11: 187987.
10 Wolmark N, Rockette H, Mamounas E, et al. Clinical trial to assess
the relative ecacy of uorouracil and leucovorin, uorouracil and
levamisole and uorouracil, leucovorin, and levamisole in patients
with Dukes B and C carcinoma of the colon: results from National
Surgical Adjuvant Breast and Bowel Project C-04. J Clin Oncol 1999;
17: 355359.
11 OConnell MJ, Laurie JA, Kahn M, et al. Prospectively randomized
trial of postoperative adjuvant chemotherapy in patients with
high-risk colon cancer. J Clin Oncol 1998; 16: 295300.
12 Haller DG, Catalano PJ, MacDonald JS, et al. Phase III study of
uorouracil, leucovorin, and levamisole (LEV) in high-risk stage II
www.thelancet.com Vol 370 December 15, 2007
Articles
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
and III colon cancer: nal report of Intergroup 0089. J Clin Oncol
2005; 23: 867178.
QUASAR Collaborative Group. Comparison of uorouracil with
additional levamisole, higher-dose folinic acid, or both, as adjuvant
chemotherapy for colorectal cancer: a randomised trial. Lancet 2000;
355: 158896.
Kerr DJ. 5-uorouracil and folinic acid: interesting biochemistry or
eective treatment? Br J Cancer 1989; 60: 80708.
Meta-Analysis Group in Cancer. Modulation of uorouracil by
leucovorin in patients with advanced colorectal cancer: an updated
meta-analysis. J Clin Oncol 2004; 22: 376675.
Benson AB, Schrag D, Somereld MR, et al. American Society of
Clinical Oncology recommendations on adjuvant chemotherapy for
stage II colon cancer. J Clin Oncol 2004; 22: 340819.
Krook JE, Moertel CG, Gunderson LL, et al. Eective surgical
adjuvant therapy for high-risk rectal carcinoma. N Engl J Med 1991;
324: 70915.
Zittoun J, Marquet J, Pilkorger JJ, et al. Comparative eect of 6S,6R
and 6RS leucovorin on methotrexate rescue and modulation of
5-uorouracil. Br J Cancer 1991; 63: 88588.
Kerr DJ, Gray R, McConkey C, et al. Adjuvant chemotherapy with
5-uorouracil, L-folinic acid and levamisole for patients with
colorectal cancer: non-randomised comparison of weekly versus
four-weekly schedulesless pain, same gain. Ann Oncol 2000;
11: 94755.
Collins R, Peto R, Gray R, Parish S. Large-scale randomized
evidence: trials and overviews. In: Weatherall D, Ledingham JGG,
Warrell DA, eds. Oxford textbook of medicine, volume 1. Oxford,
UK: Oxford University Press, 1996: 2132.
Aaronson NK, Ahmedzai S, Bergman B, et al. The European
Organisation for Research and Treatment of Cancer QLQ-C30: a
quality-of-life instrument for use in international clinical trials in
oncology. J Natl Cancer Inst 1993; 85: 36576.
Davidson-Homewood J, Norman A, Kchler T, Cunningham D,
Watson M. Development of a disease specic questionnaire to
supplement a generic tool for QoL in colorectal cancer.
Psychooncology 2003; 12: 67585.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale.
Acta Psychiatr Scand 1983; 67: 36170.
Early Breast Cancer Trialists Collaborative Group. Treatment of
early breast cancer, volume 1, worldwide evidence 19851990.
Oxford, UK: Oxford University Press, 1990. http://www.ctsu.ox.ac.
uk/reports/ebctg-1990.html (accessed Dec 3, 2007).
Sargent DJ, Wieand HS, Haller DG, et al. Disease-free survival
versus overall survival as a primary end point for adjuvant colon
cancer studies: individual patient data from 20,898 patients on
18 randomized trials. J Clin Oncol 2005; 23: 866470.
Melville A, Sheldon TA, Gray R, Sowden A. Management of
colorectal cancer. Qual Health Care 1998; 7: 10308.
Mamounas C, Wieand S, Wolmark N, et al. Comparative ecacy of
adjuvant chemotherapy in patients with Dukes B versus Dukes C
www.thelancet.com Vol 370 December 15, 2007
28
29
30
31
32
33
34
35
36
37
38
39
colon cancer: results from four national surgical adjuvant breast
and bowel project adjuvant studies (C-01, C-02, C-03, and C-04).
J Clin Oncol 1999; 17: 134955.
Gill S, Loprinzi CL, Sargent D, et al. Pooled analysis of
uorouracil-based adjuvant therapy for stage II and III colon
cancer: what benets and by how much? J Clin Oncol 2004;
22: 1797806.
Glimelius B, Dahl O, Cedermark B, et al. Adjuvant chemotherapy
in colorectal cancer: A joint analysis of randomised trials by the
Nordic Gastrointestinal Tumour Adjuvant Therapy Group.
Acta Oncologica 2005; 44: 90412.
Figueredo A, Charette ML, Maroun J, Brouwers MC, Zuraw L.
Adjuvant therapy for stage II colon cancer: a systematic review from
the cancer care on Ontario program in evidence-based cares
gastrointestinal cancer disease site group. J Clin Oncol 2004;
22: 3395407.
Smith RE, Colangelo L, Wieand HS, Begovic M, Wolmark N.
Randomized trial of adjuvant therapy in colon carcinoma: 10-year
results of NSABP Protocol C-01. J Natl Cancer Inst 2004; 96:
112832.
Sargent DJ, Goldberg RM, Jacobson SD, et al. A pooled analysis of
adjuvant chemotherapy for resected colorectal cancer in elderly
patients. N Engl J Med 2001; 345: 109197.
Goldberg RM, Tabah-Fisch I, Bleiberg H, et al. Pooled analysis of
safety and ecacy of oxaliplatin plus uorouracil/leucovorin
administered bimonthly in elderly patients with colorectal cancer.
J Clin Oncol 2006; 24: 408591.
Jansen SJ, Otten W, Stiggelbout AM. Review of determinants of
patients preferences for adjuvant therapy in cancer. J Clin Oncol
2004; 22: 318190.
Twelves C, Wong A, Nowacki MP, et al. Capecitabine as adjuvant
treatment for stage III colon cancer. N Engl J Med 2005; 352:
2696704.
Andr T, Boni C, Mounedji-Boudiaf L, et al. Oxaliplatin,
uorouracil, and leucovorin as adjuvant treatment for colon cancer.
N Engl J Med 2004; 350: 234351.
Wolmark N, Wieand HS, Kuebler L, et al. A phase III trial
comparing FULV to FULV + oxaliplatin in stage II or II carcinoma
of the colon: results of NSABP protocol C-07. Proc Am Soc Clin Oncol
2005; 23: 16S.
Schmoll HJ, Cartwright T, Tabernero J, et al. Phase II trial of
capecitabine plus oxaliplatin as adjuvant therapy for stage III colon
cancer: a planned safety analysis in 1,864 patients. J Clin Oncol 2007;
25: 10209.
Smith RE, Colangelo L, Wieand HS, et al. The occurrence of severe
enteropathy among patients with stage II/III resected colon cancer
(CC) treated with 5-FU/leucovorin (FL) plus oxaliplatin (FLOX).
Proc Am Soc Clin Oncol 2003; 22: 294.
2029
You might also like
- Cancer Regional Therapy: HAI, HIPEC, HILP, ILI, PIPAC and BeyondFrom EverandCancer Regional Therapy: HAI, HIPEC, HILP, ILI, PIPAC and BeyondNo ratings yet
- Rectal Cancer: International Perspectives on Multimodality ManagementFrom EverandRectal Cancer: International Perspectives on Multimodality ManagementBrian G. CzitoNo ratings yet
- CA ServiksDocument10 pagesCA ServiksAndi Farid ANo ratings yet
- NPCDocument8 pagesNPCArsy Mira PertiwiNo ratings yet
- Neoadjuvant chemoradiotherapy followed by surgery standard for esophageal cancerDocument14 pagesNeoadjuvant chemoradiotherapy followed by surgery standard for esophageal cancerkrsna2studyNo ratings yet
- MeduloblastomaDocument7 pagesMeduloblastomasilvia erfanNo ratings yet
- 2021 Consolidation Theraphy in Esophageal CancerDocument6 pages2021 Consolidation Theraphy in Esophageal CancerykommNo ratings yet
- Nej Me 068121Document2 pagesNej Me 068121anissakikinNo ratings yet
- Carboplatin-Paclitaxel vs Carboplatin-Pegylated Liposomal Doxorubicin for Platinum-Sensitive Ovarian CancerDocument6 pagesCarboplatin-Paclitaxel vs Carboplatin-Pegylated Liposomal Doxorubicin for Platinum-Sensitive Ovarian Cancerbettzy21No ratings yet
- Referatneoadjuvan EnggrisDocument22 pagesReferatneoadjuvan EnggrisPonco RossoNo ratings yet
- Adjuvant Systemic Therapies in Breast CancerDocument19 pagesAdjuvant Systemic Therapies in Breast CancerSapp ChaamaraNo ratings yet
- Allen2021 Article ChemotherapyVersusChemotherapyDocument8 pagesAllen2021 Article ChemotherapyVersusChemotherapyXavier QuinteroNo ratings yet
- Magic TrailDocument10 pagesMagic Trailchootu509No ratings yet
- Glockzin - 2012 - Surgical Oncology Clinics of North AmericaDocument9 pagesGlockzin - 2012 - Surgical Oncology Clinics of North AmericaPraveen RavishankaranNo ratings yet
- Breast-Cancer Adjuvant Therapy With Zoledronic Acid: Methods Study PatientsDocument11 pagesBreast-Cancer Adjuvant Therapy With Zoledronic Acid: Methods Study PatientsAn'umillah Arini ZidnaNo ratings yet
- CDDP Gemzar BilcanDocument9 pagesCDDP Gemzar BilcanhodimirekNo ratings yet
- Analysis of Compliance, Toxicity and Survival WeeklyDocument11 pagesAnalysis of Compliance, Toxicity and Survival Weeklydanu20No ratings yet
- Curran 2011Document9 pagesCurran 2011Nguyễn Hoàng PhúcNo ratings yet
- Cancer Colo-Rectal StudiuDocument3 pagesCancer Colo-Rectal StudiuEghet SilviuNo ratings yet
- 013 - Surgeon-Led-Clinical-Trials-in-Pancrea - 2023 - Surgical-Oncology-Clinics-of-NorDocument9 pages013 - Surgeon-Led-Clinical-Trials-in-Pancrea - 2023 - Surgical-Oncology-Clinics-of-NorDr-Mohammad Ali-Fayiz Al TamimiNo ratings yet
- Capecitabine Monotherapy For Recurrent and Metastatic Nasopharyngeal CancerDocument6 pagesCapecitabine Monotherapy For Recurrent and Metastatic Nasopharyngeal Cancertrifamonika23No ratings yet
- Standard surgical procedures and adjuvant therapies for colon cancerDocument46 pagesStandard surgical procedures and adjuvant therapies for colon cancerNadia Iriana DewiNo ratings yet
- Intergroup 0123Document8 pagesIntergroup 0123radonc17No ratings yet
- Resection of The Primary Colorectal CancDocument7 pagesResection of The Primary Colorectal CancjorgehogNo ratings yet
- Bristow 2002Document12 pagesBristow 2002Lưu Chính HữuNo ratings yet
- 1 4918218693336367165 PDFDocument14 pages1 4918218693336367165 PDFjorgeaznarNo ratings yet
- The OncologistDocument7 pagesThe OncologistManunart FeungpeanNo ratings yet
- Preoperative and Adjuvant Therapies For Upper Gastrointestinal CancersDocument7 pagesPreoperative and Adjuvant Therapies For Upper Gastrointestinal Cancersajaymanvikar007No ratings yet
- Clinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypeDocument12 pagesClinical Impact of External Radiotherapy in Non-Metastatic Esophageal Cancer According To Histopathological SubtypesilviailieNo ratings yet
- TraztuzumabDocument8 pagesTraztuzumabArlina Wiyata GamaNo ratings yet
- Updates in Management of Ampullary Carcinomas: Highlight ArticleDocument4 pagesUpdates in Management of Ampullary Carcinomas: Highlight Articlecorinna291No ratings yet
- Brief CommunicationDocument13 pagesBrief CommunicationsantovazNo ratings yet
- JCOG9912Document7 pagesJCOG9912BobQuNo ratings yet
- P ('t':'3', 'I':'176969959') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document8 pagesP ('t':'3', 'I':'176969959') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Cecep Saeful HudaNo ratings yet
- The Comparison of Surgery and Chemo-Radio Therapy in Locally Recurrent Colorectal CancerDocument4 pagesThe Comparison of Surgery and Chemo-Radio Therapy in Locally Recurrent Colorectal CancerInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- AsdasdDocument10 pagesAsdasdAdhi PratamaNo ratings yet
- Short-Term Metronidazole Not Linked To CancerDocument1 pageShort-Term Metronidazole Not Linked To CancerTika Ayu andaniNo ratings yet
- Pancreatic Cancer Literature ReviewDocument10 pagesPancreatic Cancer Literature Reviewea813c29No ratings yet
- HCC 5Document7 pagesHCC 5TeodoraNo ratings yet
- 1475 2891 12 118Document8 pages1475 2891 12 118SunardiasihNo ratings yet
- Bladder Cancer LancetDocument11 pagesBladder Cancer LancetYesenia HuertaNo ratings yet
- Adjuvant Versus Salvage Radiotherapy Following Radical Prostatectomy: Do The AUA/ASTRO Guidelines Have All The Answers?Document6 pagesAdjuvant Versus Salvage Radiotherapy Following Radical Prostatectomy: Do The AUA/ASTRO Guidelines Have All The Answers?Anonymous jBoDXi3sNo ratings yet
- Axtner Et Al. - 2016 - Health Services Research of Integrative Oncology in Palliative Care of Patients With Advanced Pancreatic CancerDocument10 pagesAxtner Et Al. - 2016 - Health Services Research of Integrative Oncology in Palliative Care of Patients With Advanced Pancreatic CancerMaría Reynel TarazonaNo ratings yet
- 009 - The-Perioperative-and-Operative-Management-of - 2023 - Surgical-Oncology-ClinicsDocument17 pages009 - The-Perioperative-and-Operative-Management-of - 2023 - Surgical-Oncology-ClinicsDr-Mohammad Ali-Fayiz Al TamimiNo ratings yet
- The Optimal Neoadjuvant Treatment of Locally Advanced Esophageal CancerDocument11 pagesThe Optimal Neoadjuvant Treatment of Locally Advanced Esophageal CancerdjonesthoracicNo ratings yet
- Effect of More Vs Less Frequent Follow-Up Testing On Overall and Colorectal Cancer-Specific Mortality in Patients With Stage II or III Colorectal CancerDocument9 pagesEffect of More Vs Less Frequent Follow-Up Testing On Overall and Colorectal Cancer-Specific Mortality in Patients With Stage II or III Colorectal CancerMr. LNo ratings yet
- Evidence-Based Guidance For Breast Cancer SurvivorshipDocument19 pagesEvidence-Based Guidance For Breast Cancer SurvivorshipZuriNo ratings yet
- 211 FullDocument17 pages211 Fullalfarisi_auliaNo ratings yet
- Eficacia de Azul de Metileno VO en ColonoDocument11 pagesEficacia de Azul de Metileno VO en ColonoMarielaDiazNo ratings yet
- Treatment of Metastatic Endometrial CancerDocument24 pagesTreatment of Metastatic Endometrial CancerKaroline Pascoal Ilidio PeruchiNo ratings yet
- Ournal of Linical Ncology: OriginalDocument10 pagesOurnal of Linical Ncology: OriginalMaulida Nurazmi OctaviaNo ratings yet
- Pathological complete response in recurrent colon cancer following neoadjuvant radiotherapy and intraperitoneal chemotherapyDocument4 pagesPathological complete response in recurrent colon cancer following neoadjuvant radiotherapy and intraperitoneal chemotherapyAlice AugustinNo ratings yet
- JCO 2003 Lin 631 7Document7 pagesJCO 2003 Lin 631 7Adhika Manggala DharmaNo ratings yet
- Research Article: Prevalence of Cachexia in Cancer PatientsDocument9 pagesResearch Article: Prevalence of Cachexia in Cancer Patientsadri20121989No ratings yet
- Neoadjuvant Paclitaxel For Operable Breast Cancer: Multicenter Phase II Trial With Clinical OutcomesDocument6 pagesNeoadjuvant Paclitaxel For Operable Breast Cancer: Multicenter Phase II Trial With Clinical OutcomesSubhash SugathanNo ratings yet
- Jurnal DMDocument10 pagesJurnal DMMalisa LukmanNo ratings yet
- Esofago Carvical Valmasoni 2018Document9 pagesEsofago Carvical Valmasoni 2018Carlos N. Rojas PuyolNo ratings yet
- Prognostic Factors in Nasopharyngeal Carcinoma With Synchronous Liver Metastasis: A Retrospective Study For The Management of TreatmentDocument7 pagesPrognostic Factors in Nasopharyngeal Carcinoma With Synchronous Liver Metastasis: A Retrospective Study For The Management of TreatmentChairul Nurdin AzaliNo ratings yet
- Sequential Chemoradiotherapy With Gemcitabine and Cisplatin For Locoregionally Advanced Nasopharyngeal CarcinomaDocument9 pagesSequential Chemoradiotherapy With Gemcitabine and Cisplatin For Locoregionally Advanced Nasopharyngeal CarcinomadheaonyonNo ratings yet
- Cytotoxic Treatment of Metastatic Breast Cancer Which Drugs and Drug Combinations To UseDocument7 pagesCytotoxic Treatment of Metastatic Breast Cancer Which Drugs and Drug Combinations To UseGamer MadaNo ratings yet
- A Population-Based Cohort Study On Adherence To Practice Guidelines For Adjuvant Chemotherapy in Colorectal CancerDocument9 pagesA Population-Based Cohort Study On Adherence To Practice Guidelines For Adjuvant Chemotherapy in Colorectal CancerFatona AgungNo ratings yet
- Soal Penilaian Tengah Semester XIDocument1 pageSoal Penilaian Tengah Semester XIFatona AgungNo ratings yet
- Puskesmas Solo Free Health Care Clinic Patient Visit Recap February 2019Document294 pagesPuskesmas Solo Free Health Care Clinic Patient Visit Recap February 2019Fatona AgungNo ratings yet
- Clinico-Pathological Correlation of SerialDocument5 pagesClinico-Pathological Correlation of SerialFatona AgungNo ratings yet
- Glioblastoma5 PDFDocument10 pagesGlioblastoma5 PDFFatona AgungNo ratings yet
- Glioblastoma3 PDFDocument29 pagesGlioblastoma3 PDFFatona AgungNo ratings yet
- Glioblastoma4 PDFDocument29 pagesGlioblastoma4 PDFFatona AgungNo ratings yet
- GlioblastomaDocument11 pagesGlioblastomaFatona AgungNo ratings yet
- Lampiran PetaDocument4 pagesLampiran PetaFatona AgungNo ratings yet
- Little Child Dry Your Crying EyesDocument1 pageLittle Child Dry Your Crying EyesFatona AgungNo ratings yet
- SxceoeoeoDocument6 pagesSxceoeoeolionfairwayNo ratings yet
- Almost EasyDocument1 pageAlmost EasyFatona AgungNo ratings yet
- Little Child Dry Your Crying EyesDocument1 pageLittle Child Dry Your Crying EyesFatona AgungNo ratings yet
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Review More Than BlueDocument1 pageReview More Than BlueB2 - Dimatulac, Jessieryl A.No ratings yet
- GlutathioneDocument21 pagesGlutathioneGB R100% (1)
- ISSA Senior Fitness Certification Chapter PreviewDocument21 pagesISSA Senior Fitness Certification Chapter Previewscorpion9990% (1)
- Kuretase Case Report 2Document3 pagesKuretase Case Report 2Lydia AmaliaNo ratings yet
- 2.High-Resolution CT of The Lung EDITIA A-3-A.Document736 pages2.High-Resolution CT of The Lung EDITIA A-3-A.RamonataleNo ratings yet
- OSU Orthopaedics Accomplishments Report 2010Document32 pagesOSU Orthopaedics Accomplishments Report 2010osuorthopaedicsNo ratings yet
- Angela Tang-Tan ResumeDocument2 pagesAngela Tang-Tan Resumeapi-459113948No ratings yet
- Intravenous PyelogramDocument23 pagesIntravenous Pyelogramrachael100% (1)
- Gastrointestinal Bleeding Guide: Causes, Symptoms, Diagnosis & TreatmentDocument46 pagesGastrointestinal Bleeding Guide: Causes, Symptoms, Diagnosis & TreatmentSyarifah FauziahNo ratings yet
- Food Adultration ObjectiveDocument11 pagesFood Adultration ObjectiveGourav Som0% (1)
- 2015 PM Lecture 4 Barium EnemaDocument62 pages2015 PM Lecture 4 Barium EnemaObrian ReidNo ratings yet
- Preventing Breast Cancer Through Lifestyle and ScreeningDocument5 pagesPreventing Breast Cancer Through Lifestyle and ScreeningDana LebadaNo ratings yet
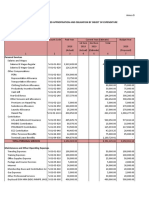
- Programmed Appropriation and Obligation by Object of ExpenditureDocument7 pagesProgrammed Appropriation and Obligation by Object of ExpenditureKristin Villaseñor-MercadoNo ratings yet
- Akupuntur InfertilityDocument7 pagesAkupuntur Infertilitybustanul aswatNo ratings yet
- Tobacco Smoking-Associated Alterations in The Immune Microenvironment of Squamous Cell CarcinomasDocument7 pagesTobacco Smoking-Associated Alterations in The Immune Microenvironment of Squamous Cell CarcinomasKamado NezukoNo ratings yet
- Gestational Trophoblastic DiseaseDocument40 pagesGestational Trophoblastic DiseaseAayupta Mohanty100% (2)
- Autoimmune EncephalitisDocument9 pagesAutoimmune EncephalitisDini Fajriah OmariNo ratings yet
- Genetic Attribution For Schizophrenia, Depression, and Skin Cancer: Impact On Social DistanceDocument7 pagesGenetic Attribution For Schizophrenia, Depression, and Skin Cancer: Impact On Social DistancenigoNo ratings yet
- Pre TestDocument6 pagesPre TestPRINTDESK by DanNo ratings yet
- Gastrointestinal Endoscopy Volume 71 Issue 7 2010 (Doi 10.1016/j.gie.2009.12.029) Lisette G. Capelle Annemarie C. de Vries Jelle Haringsma Fran - The Staging of Gastritis With The OLGA System by PDFDocument9 pagesGastrointestinal Endoscopy Volume 71 Issue 7 2010 (Doi 10.1016/j.gie.2009.12.029) Lisette G. Capelle Annemarie C. de Vries Jelle Haringsma Fran - The Staging of Gastritis With The OLGA System by PDFAleida VivalloNo ratings yet
- Annals of Medicine - HPV VaccineDocument12 pagesAnnals of Medicine - HPV VaccineJudicial Watch, Inc.100% (3)
- 006 Pathology MCQ ACEM Primary CellularDocument5 pages006 Pathology MCQ ACEM Primary CellularIrum RafeeqNo ratings yet
- GI Disorders NursingDocument93 pagesGI Disorders NursingAmy100% (4)
- Guide: DR Srinath Rao Presenter:Dr SR Soumya (Materia Medica MD Part-1) 15/12/14Document50 pagesGuide: DR Srinath Rao Presenter:Dr SR Soumya (Materia Medica MD Part-1) 15/12/14Krishna Veni100% (2)
- Colour BlindnessDocument4 pagesColour BlindnessDanial HazimNo ratings yet
- Kerala Uiversity Bhms PapersDocument31 pagesKerala Uiversity Bhms PapersKarthikNo ratings yet
- Ayva Içerik Cydonia Oblonga PDFDocument20 pagesAyva Içerik Cydonia Oblonga PDFZeynep Emirhan ŞenyüzNo ratings yet
- Follicular Cholecystitis With Cholelithiasis A Rare Case ReportDocument3 pagesFollicular Cholecystitis With Cholelithiasis A Rare Case ReportSSR-IIJLS JournalNo ratings yet
- Clinical Summary Guide 05Document2 pagesClinical Summary Guide 05Diarti_PMIKNo ratings yet
- CeramFab Inc. & WYG Refractories SuitDocument27 pagesCeramFab Inc. & WYG Refractories SuitBenjamin DuerNo ratings yet