Professional Documents
Culture Documents
Bone
Uploaded by
Jesselle LasernaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bone
Uploaded by
Jesselle LasernaCopyright:
Available Formats
Cancer Res Treat.
2007;39(3):104-108
Bone Metastasis from Primary Hepatocellular Carcinoma:
Characteristics of Soft Tissue Formation
Sangwon Kim, M.D.1, Mison Chun, M.D.1, Heejung Wang, M.D.3, Sungwon Cho, M.D.2, Young-Taek
Oh, M.D.1, Seung-Hee Kang, M.D.1 and Juno Yang, O.M.D.1
1
Departments of Radiation Oncology, 2Surgery and 3Internal Medicine, Ajou University School of Medicine, Suwon,
Korea
Purpose: To assess the characteristics of bone meta stasis from hepatocellular carcinoma and the radiation
field arrangement based on imaging studies.
Materials and Methods: Fifty-three patients (84 lesions)
with bone metastasis from a primary hepatocellular carcinoma completed palliative radiation therapy. All patients
underwent one of following imaging studies prior to the initiation of radiation therapy: a bone scan, computed tomography or magnetic resonance imaging. The median
radiation dose was 30 Gy (740 Gy). We evaluated retrospectively the presence of soft tissue formation and the
adjustment of the radiation field based on the imaging
studies.
Results: Soft tissue formation at the site of bony disease
was identified from either a CT/MRI scan (41 lesions) or
from a symptomatic palpable mass (5 lesions). The adjustment of the radiation field size based on a bone scan
was necessary for 31 of 41 soft tissue forming lesions
(75.6%), after a review of the CT/MRI scan. The median
survival from the initial indication of a hepatoma diagnosis
was 8 months (2 to 71 months), with a 2-year survival rate
of 38.6%. The median survival from the detection of a
bone metastasis was 5 months (1 to 38 months) and the
1-year overall survival rate was 8.7%.
Conclusion: It was again identified that bone metastasis
from a primary hepatocellular carcinoma is accompanied
by soft tissue formation. From this finding, an adjustment
of the radiation field size based on imaging studies is
required. It is advisable to obtain a CT or MRI scan of suspected bone metastasis for better tumor volume coverage
prior to the initiation of radiation therapy. (Cancer Res
Treat. 2007; 39:104-108)
Key Words: Bone metastasis, hepatocellular carcinoma, soft tissue formation, radiation
therapy
a higher chance for an extrahepatic metastasis, regardless of
primary site control (3,4). The most favorable sites of
extrahepatic metastasis from an HCC were the lung and central
nervous system (CNS). In contrast to gastric cancer, lung
cancer or breast cancer, the incidence of bone metastasis from
HCC was rare, and the incidence has been reported as ranging
from 3% to 20% (37).
In the cases of an extrahepatic metastasis, anthracycline-based
chemotherapy is effective in a limited role as many patients
have accompanying chronic liver disease or liver cirrhosis. The
reported response rate is about 20%, while the median survival
is approximately 4 months (8).
In general, radiation therapy is a preferred treatment modality
for symptomatic palliation of a bone metastasis from many
carcinomas. However, there have been few published reports
about the role of radiation therapy for a bone metastasis from
a primary HCC (9,10). Some studies with a limited number of
patients have described the characteristics of bone metastasis
from HCC, such as soft tissue formation (7,9,1113).
The purpose of this study is to describe the characteristics
of bone metastasis from HCC and to evaluate the effectiveness
of radiation therapy.
INTRODUCTION
Hepatocellular carcinoma (HCC) ranks third as the most
common carcinoma, constituting approximately 11.3% of all
tumors. Annually, approximately 11,000 new patients are diagnosed with HCC in Korea. In 2004, HCC accounted for 22.6%
of all cancer-related deaths, followed in frequency by lung
cancer and gastric cancer. The overall 5-year survival rate,
according to sex, was 11.8% for men and 13.3% for women
(1).
Due to developments in surgical techniques and the introduction of effective local therapeutic modalities, such as transarterial chemoembolization (TACE) or radiofrequency ablation,
the overall survival rate of HCC patients has increased, even
in the cases of unresectable disease (2). However, there is also
Correspondence to: Mison Chun, Department of Radiation Oncology,
Ajou University School of Medicine, San-5, Woncheon-dong,
Yeongtong-gu, Suwon, 443-721, Korea. (Tel) 82- 31-219-58845,
(Fax) 82- 31-219-5894, (E-mail) chunm@ajou.ac.kr
Received August 21, 2007, Accepted September 22, 2007
104
Sangwon Kim, et alBone Metastasis from Primary Hepatocellular Carcinoma 105
MATERIALS AND METHODS
1) Patient characteristics
Between October 1994 and December 2004, a total 60
patients were referred for palliative radiation therapy for bone
metastasis from HCC. Fifty-three patients completed planned
radiation therapy for 84 lesions. The remaining seven patients
stopped treatment because of either their own refusal or
deterioration of performance status regardless of treatment. The
median age of all patients was 53 years-old (range 33 to 70
years). With respect to performance status, 13 patients were
scored as ECOG 1, 28 patients were scored as ECOG 2, and
the remaining 12 patients were scored as ECOG 3. Thirty-seven
patients had a single metastatic site, while 16 patients had
multiple lesions. Twenty-three patients presented with synchronous bony metastasis with a diagnosis of primary HCC. The
median interval between the day of the initial HCC diagnosis
and that of the metachronous bone metastasis was 8.5 months,
ranging from 2 months to 70 months (Table 1).
Of the 84 lesions treated, 48 lesions were examined with
CT/MRI. Among them, 41 lesions were also examined with a
bone scan. Thirty-one lesions were examined with a bone scan
only. The remaining 5 lesions, despite of a lack of evaluation
with either a CT/MRI or bone scan, revealed abnormal findings
on a plain x-ray as symptomatic palpable masses.
2) Radiation therapy
Radiation therapy was delivered with a linear accelerator,
utilizing 6 or 15 MV photon beams or electrons, according to
the depth of the lesion. The treatment volume covered the gross
tumor volume (GTV), which was identified with imaging data,
adding a margin of 1.5 to 2 cm in all directions. If vertebral
bodies were targeted for treatment, the treatment volume
included the vertebral bodies, plus one additional segment in
both the cephalad and caudal directions. The median total dose
was 30 Gy, ranging from 7 Gy to 40 Gy. The daily fraction
size was 2.5 or 3 Gy, with the exception of a single fraction
treatment of 7 Gy.
We focused on the comparison of the size of the radiation
field as determined with a bone scan only to the field size
determined by both a bone scan and CT or MRI. We evaluated
the need of adjustment of the radiation field according to the
imaging modality.
After completion of radiation therapy, all patients received
follow-up by either a hospital visit or phone call. The median
period of follow-up was 6 months. Patient data was analyzed
using the Statistical Package for the Social Science (SPSS,
Chicago, IL USA) software package. The Kaplan-Meier method
was also used. The end-point was the day of the patient death,
both from the day of the initial diagnosis of primary disease
and from the day of the initial diagnosis of a bone metastasis.
Table 1. Patient characteristics
Characteristics
Age
Sex ratio (MF)
Performance status
ECOG 1
ECOG 2
Number of bone metastasis
Single
Multiple
Interval of bone metastasis
Synchronous
Metachronous
Total number of patients
Median 53
(range, 3370)
476
13
40
36
17
23
30
53
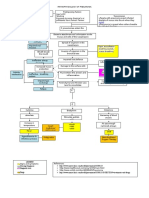
Fig. 1. (A) The pre-treatment CT scan shows osteolysis of the right iliac wing by soft tissue formation. (B) The mass size decreases
2 months after completion of radiation therapy with persistent bony destruction.
106 Cancer Res Treat. 2007;39(3)
2) Adjustment of the radiation field
RESULTS
1) Disease characteristics
Total 84 metastatic sites received radiation treatment. The
C-T-L spines were the most common site (40 lesions), followed
by the pelvic bone, including the hip joints (19 lesions), ribs
(9 lesions), upper and lower extremities (7 lesions), shoulder
joint (4 lesions), skull (3 lesions), and sternum (2 lesions).
Among the 48 lesions evaluated by either CT or MRI, 41
lesions showed bone destruction combined with soft tissue
formation (Fig. l). There were additional 5 lesions with soft
tissue formation, which were not examined with CT or MRI,
but presented with clinically palpable soft tissue at the site of
bone metastasis as observed on plain x-rays.
Metastatic lesions at the vertebrae were the most frequent
ones with both bone destruction and soft tissue formation
(27/29). Three soft tissue lesions were expressed as a cold spot
(or as a photon defect) rather than with hot uptake as seen on
the bone scan. However, there was no way to detect existing
soft tissue formation around metastatic bone in lesions
evaluated with a bone scan only (Table 2).
Forty-one lesions were examined with both a bone scan and
by CT/MRI. We compared the radiation field size based on a
bone scan image to the field size based on a CT/MRI image.
Thirty-one lesions required an adjustment of the radiation field
size when the radiation field size was determined with CT/MRI
findings rather than with bone scan findings (Fig. 2). These
lesions showed characteristic destruction of the bony framework
and infiltration into the surrounding muscle or fat tissue
extensively. The extent of infiltration into the surrounding
muscle or fat tissue determined the size of modification of the
radiation field. The amount of radiation field adjustment was
an increment of an average 2.5 cm in length (range, 17 cm).
3) Survival
At the time of analysis, we identified 50 patient deaths.
Three patients were lost to follow-up. The median survival
period of all patients from the day of the initial HCC diagnosis
was 8 months (ranging from 2 to 71 months). The survival rate
was 53.9%, 38.6% and 30.1% at 1, 2 and 3 years, respectively.
From the time of the initial diagnosis of bone metastasis, the
overall survival rate was 8.7% at 1 year, with a median survival
Table 2. Location of soft tissue formation
Location
Number of
total lesions
Number of
CT/MRI scanned
Vertebrae (C-T-L spine)
Pelvic bone, sacrum and coccyx
Rib cage
Four extremities
Shoulder joint & clavicle
Skull (including base of skull)
Sternum
40
19
9
7
4
3
2
2
1
4
0
0
2
1
Total number
84
48
Number of soft
tissue formations
27
7
4 (+1)*
0 (+1)*
0 (+1)*
2 (+1)*
1 (+1)*
41 (+5)
*An additional soft tissue lesion that was not evaluated with a CT/MRI scan but presented with a symptomatic palpable mass.
Fig. 2. A bone scan (A) and pelvic MRI (B) of a 46-year-old male patient. Note the osteolytic lesion with expansile soft tissue formation
on the right iliac bone. (C) The difference of radiation field based on the bone scan and MRI of the pelvis.
Sangwon Kim, et alBone Metastasis from Primary Hepatocellular Carcinoma 107
period of 5 months (ranging from 1 to 38 months). Only one
patient survived for more than 2 years. This male patient was
diagnosed with a bone metastasis 6 years after the initial
diagnosis of primary HCC. The median survival period of
patients diagnosed with primary HCC and bone metastasis
synchronously and metachronously were nearly the same-5
months and 4.5 months, respectively (ranging from 2 to 38
months, and 1 to 21 months, respectively). We evaluated the
influence of prognostic factors by use of the log-rank test. By
univariate analysis, the presence of metastasis to other solid
organs was the only significant prognostic factor. The 1-year
survival rate of those patients that had another solid organ
metastasis at the time of the diagnosis of a bone metastasis was
0%, with a median survival period of 3 months, but the 1-year
survival rate of patients that had only a bone metastasis was
14.5% with a median survival period of 8 months (p=0.03).
However, age, sex, performance status, primary disease status
and multiplicity of bony metastasis did not have an impact on
patient prognosis.
DISCUSSION
A bone metastasis from a primary HCC is not common, with
the incidence ranging from 3% to 20% (47). Therefore, there
are few studies concerning the role of radiation therapy for
bone metastasis from HCC.
As mentioned above, the most impressive characteristic of a
bone metastasis from HCC was soft tissue formation that lyses
the bone framework. Many established studies have been
reported with a small number of cases. A retrospective study
like the current study is rare.
Fukutomi et al(7) reported the characteristics of bone
metastasis from HCC. In that study, 24 cases comprising a total
of 29 lesions (83%) examined with MRI showed osteolysis by
expansile soft tissue formation. In another investigation, Sato
et al. (11) found 5 osteolytic lesions by soft tissue formation
on ultrasonography. With a radiation dose of 30 Gy, there was
more than a 50% reduction of gross tumor volume in all cases.
In our study, all 41 lesions evaluated with a CT/MRI scan
revealed expansile soft tissue formation. In addition, another
five lesions presented with a palpable mass at the site of the
metastasis.
Seong et al(9) investigated the effectiveness of palliative
radiation therapy for bone metastasis from HCC. In that study,
51 patients received radiation therapy for 77 bony metastatic
lesions, with a median total dose of 30 Gy. There was pain
relief in 56 lesions (73%). The median survival period from the
occurrence of a bone metastasis was 5 months, with a 1-year
survival rate of 15%.
Kaizu et al(10) reported the influence of the dose-response
relationship on palliation. Patients that received radiation with
time, dose and a fractionation factor (TDF) in excess of 77 (i.e.,
a daily dose of 2 Gy for a total of 48 Gy, or a daily dose of
3 Gy for a total of 39 Gy) showed better palliative responses
than patients that received radiation with a TDF less than 77.
The response rate was 83.8%, and the median survival period
from the time of the initial occurrence of a bone metastasis was
6 months.
In our study, bone destruction with soft tissue formation
presented in 85.4% of all cases that were examined by CT or
MRI. These bone destructive lesions tended to infiltrate the
surrounding muscle or fat lesions. A bone scan, which indicated
abnormal findings within the bony structure, did not reveal the
entire extent of the mass lesion in many cases. Determination
of the radiation field based on a bone scan only could not cover
the entire mass lesion adequately. This study showed that
approximately three-quarters of all cases need an adjustment of
the radiation field based on the findings of a CT/MRI scan as
compared with cases that were based on a bone scan only. The
median survival period from the occurrence of a bone
metastasis in our study was 5 months, which was comparable
with those of published results.
CONCLUSIONS
This study confirmed the characteristic finding of soft tissue
formation at a bone metastasis from a primary heapatocellular
carcinoma. There is a high possibility that a bone metastasis
from a primary hepatocellular carcinoma is expressed as a large
soft tissue mass lesion. The radiation field based on only a bone
scan has a risk of a marginal miss. From this review, we
suggest to obtain a CT scan or MRI scan of a suspected bone
metastasis to define the radiation field adequately.
REFERENCES
1. Park JW, Kim CM. Epidemiology of hepatocellular carcinoma
in Korea. Korean J Hepatol. 2004;11:303-10.
2. Llovet JM, Real MI, Montana X, Planas R, Coll S, Aponte
J, et al. Arterial embolisation or chemoembolisation, versus
symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomized trial. Lancet. 2002;359:
1734-9.
3. Okuda K, Ohtsuki T, Obata H, Tomimatsu M, Okazaki N,
Hasegawa H, et al. Natural history of hepatocellular carcinoma
and prognosis in relation to treatment: study of 850 patients.
Cancer. 1985;56:918-28.
4. Primary liver cancer in Japan: Sixth report. The Liver Cancer
Study Group of Japan. Cancer. 1987;60:1400-11.
5. Okazaki N, Yoshino M, Yoshida T, Hirohashi S, Kishi K,
Shimosato Y. Bone metastasis in hepatocellular carcinoma.
Cancer. 1985;55:1991-4.
6. Lee YT, Geer DA. Primary liver cancer: pattern of metastasis.
J Surg Oncol. 1987;36:26-31.
7. Fukutomi M, Yokota M, Chuman H, Harada H, Zaitsu Y,
Funakoshi A, et al. Increased incidence of bone metastasis in
hepatocellular carcinoma. Eur J Gastroenterol Hepatol.
2001;13:1083-8.
8. Johnson PJ. Is there a role for systemic therapy in hepatocellular carcinoma, and if so, can we assess response? Am Soc
Clin Oncol Ed Book. 2002; 38:310-5.
9. Seong J, Koom WS, Park HC. Radiotherapy for painful bone
metastasis from hepatocellular carcinoma. Liver Int. 2005;
25:261-5.
10. Kaizu YT, Karasawa K, Tanaka Y, Matuda T, Kurosaki H,
Tanaka S, et al. Radiotherapy for osseous metastasis from
hepatocellular carcinoma: a retrospective study of 57 patients.
Am J Gastroenterol. 1998;93:2167-71.
108 Cancer Res Treat. 2007;39(3)
11. Sato M, Ishida H, Konno K, Hamashima Y, Naganuma H,
Komatsuda T, et al. Peripheral bone metastasis from hepatocellular carcinoma: sonographic findings. Abdom Imaging.
2001;26:524-8.
12. Goilimbu C, Firooznia H, Rafii M. Hepatocellular carcinoma
with skeletal metastasis. Radiology. 1985;154:617-8.
13. Kuhlman JE, Fishman EK, Leichner PK, Magid D, Order SE,
Siegelman SS. Skeletal metastasis from hepatoma: frequency,
distribution and radiographic features. Radiology. 1986;160:
175-8.
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Efficiency of Care and Satisfaction For Head Injury Patients at Emergency Department in Mansoura Emergency HospitalDocument11 pagesEfficiency of Care and Satisfaction For Head Injury Patients at Emergency Department in Mansoura Emergency HospitalJesselle LasernaNo ratings yet
- CE Mild Traumatic Brain Injury.24Document7 pagesCE Mild Traumatic Brain Injury.24Jesselle LasernaNo ratings yet
- European Down Syndrome Association: February 2016Document7 pagesEuropean Down Syndrome Association: February 2016Jesselle LasernaNo ratings yet
- Pathophysiology of PneumoniaDocument2 pagesPathophysiology of PneumoniaJesselle LasernaNo ratings yet
- NCSBN's Reviews For The NCLEX-RN & Nclex-PN: Weekly Study PlanDocument3 pagesNCSBN's Reviews For The NCLEX-RN & Nclex-PN: Weekly Study PlanJesselle LasernaNo ratings yet
- 857 1857 1 PBDocument4 pages857 1857 1 PBJesselle LasernaNo ratings yet
- Basic Concepts On Communityacquired Bacterial Pneumonia in PediatricsDocument6 pagesBasic Concepts On Communityacquired Bacterial Pneumonia in PediatricsJesselle LasernaNo ratings yet
- Metronidazole Ds Case Pre 4th YrDocument2 pagesMetronidazole Ds Case Pre 4th YrJesselle LasernaNo ratings yet
- 188-Knowledge, Attitude and Practice On Antenatal CareDocument9 pages188-Knowledge, Attitude and Practice On Antenatal CareJesselle LasernaNo ratings yet
- Wvsu Scholarship f09Document2 pagesWvsu Scholarship f09Jesselle LasernaNo ratings yet
- Problem ListDocument1 pageProblem ListJesselle LasernaNo ratings yet
- SultamicillinDocument2 pagesSultamicillinJesselle LasernaNo ratings yet
- 222 765 1 PBDocument8 pages222 765 1 PBJesselle LasernaNo ratings yet
- Down Syndrome (DS) and Hirschsprung's Disease (HSCR)Document3 pagesDown Syndrome (DS) and Hirschsprung's Disease (HSCR)Jesselle LasernaNo ratings yet
- ReadmeDocument2 pagesReadmeJesselle LasernaNo ratings yet
- PathoPhysiology of Hypertension DiagramDocument4 pagesPathoPhysiology of Hypertension DiagramKat Taasin100% (1)
- Care of Patient With Copd: Chronic Obstructive Pulmonary DiseaseDocument32 pagesCare of Patient With Copd: Chronic Obstructive Pulmonary DiseaseJesselle LasernaNo ratings yet
- NCP CVA Activity IntoleranceDocument2 pagesNCP CVA Activity IntoleranceJesselle LasernaNo ratings yet
- Schematic Diagram of Pleural EffusionDocument2 pagesSchematic Diagram of Pleural EffusionJesselle Laserna0% (1)
- SCR 200 Nursing Care Plan TWDocument6 pagesSCR 200 Nursing Care Plan TWJesselle LasernaNo ratings yet
- Review of Systems Cheat SheetDocument2 pagesReview of Systems Cheat Sheetarmymedic7No ratings yet
- Barthel Index (0-20)Document2 pagesBarthel Index (0-20)Yessika Adelwin Natalia95% (19)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Occipitocervical Instability & DislocationDocument205 pagesOccipitocervical Instability & DislocationM Ivan Pratama ZebuaNo ratings yet
- Vitamin K PDocument2 pagesVitamin K Papi-435620975No ratings yet
- PDRI TablesDocument7 pagesPDRI TablesCamille Chen100% (1)
- Kantar Article (2012) PsychopathologyDocument3 pagesKantar Article (2012) PsychopathologyShelby Jones-StachnikNo ratings yet
- Benefit 1Document10 pagesBenefit 1HL LauNo ratings yet
- The Curious Case of Postprandial Glucose Less Than Fasting Glucose Little Things That Matter MuchDocument3 pagesThe Curious Case of Postprandial Glucose Less Than Fasting Glucose Little Things That Matter MuchTony Miguel Saba SabaNo ratings yet
- Flow Trac SystemDocument4 pagesFlow Trac Systempolar571No ratings yet
- Jurnal Reading PanumDocument28 pagesJurnal Reading PanumIdris MohammadNo ratings yet
- Acrylic Removable Partial Denture & Impression Techniques in Complete DentureDocument9 pagesAcrylic Removable Partial Denture & Impression Techniques in Complete DentureMohammed ZiaNo ratings yet
- Nclex PNDocument416 pagesNclex PNSandhu Sdhu100% (9)
- Tumors of Salivary GlandDocument28 pagesTumors of Salivary Glandrameshparajuli14100% (1)
- Evaluation of Intraoral Verticosagittal Hashemi2008Document4 pagesEvaluation of Intraoral Verticosagittal Hashemi2008carolina vega hernandezNo ratings yet
- Saylani ReportDocument4 pagesSaylani ReportAsif Muhammad100% (1)
- AssertivenessDocument4 pagesAssertivenessDamir MujagicNo ratings yet
- Discover Your Subpersonalities PDFDocument20 pagesDiscover Your Subpersonalities PDFjayadush67% (3)
- Generic Name Drug ListingDocument17 pagesGeneric Name Drug ListingPradeep PaudelNo ratings yet
- NCP HPNDocument5 pagesNCP HPNGwyneth SantiagoNo ratings yet
- Lupus NephritisDocument15 pagesLupus NephritisVilza maharaniNo ratings yet
- Referat ObesitasDocument20 pagesReferat ObesitasfaisalNo ratings yet
- R115Patients PDFDocument14 pagesR115Patients PDFcarneoliaNo ratings yet
- Renal Diseases " Review "Document22 pagesRenal Diseases " Review "api-3827876No ratings yet
- Counselling-GATHER ApproachDocument23 pagesCounselling-GATHER ApproachAnilkumar JaraliNo ratings yet
- NutritionDocument22 pagesNutritionAsrar ZakNo ratings yet
- 02 NST Icu Intake 0007Document8 pages02 NST Icu Intake 0007anariela kityNo ratings yet
- Tools For Family AssessmentDocument44 pagesTools For Family AssessmentBayna LestariNo ratings yet
- Personality Stability, Development, and ChangeDocument24 pagesPersonality Stability, Development, and ChangeLouNo ratings yet
- Artificial LiverDocument1 pageArtificial LiverPradeep MahalikNo ratings yet
- Case Study Systemic Lupus ErythematosusDocument54 pagesCase Study Systemic Lupus ErythematosusCharmaine Paran100% (3)
- Myocardial Infarction "Heart Attacks"Document16 pagesMyocardial Infarction "Heart Attacks"Camzii Borland100% (1)
- Hispanic ObesityDocument25 pagesHispanic Obesityapi-253509573No ratings yet