Professional Documents
Culture Documents
English
Uploaded by
Puteri hirika reptes0 ratings0% found this document useful (0 votes)
14 views5 pagesEnglish
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentEnglish
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
14 views5 pagesEnglish
Uploaded by
Puteri hirika reptesEnglish
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 5
Members of Group 1
1. Nur Khriesna Habita
2. Rachma Anisa Ulya
3. Agnes Ose Tokan
4. Tri Sulistyawati
5. Puteri Hirika Reptes
6. Nora Dwi Purwanti
7. Dwi Retna Heruningtyas
8. Ninik Dwi Purweni
Our group 1 would like to report the results of our discussions regarding the
gastrointestinal system diseases are diarrhea
Definition
Diarrhea is a condition where an increase in the frequency of defecation unusual
(more than three times a day), changes in the number and consistency (liquid
faeces).
Etiology
1. The specific treatment
2. Feeding through a tube
3. The metabolic and endocrine disorders
4. viral infection / bacteria
5. Other causes of nutritional disorders and malabsorption, defisist anal
sphincter, and intestinal obstruction.
Clinical Manifestation
1. Increased frequency and content of fluid in the stool.
2. Abdominal cramping, distention, bowel sounds (borborigmus), anorexia
and thirst the nature and can eksplosis onset and gradual.
3. Dehydration and weakness
4. Stool soft because many contain water
5. Mucus and pus in the stool
Management
1. Medical management of primary for mild diarrhea, increase fluid intake by
mouth; Oral glucose and electrolyte solution to moderate diarrhea, nonspecific drugs, diphenoxylate (Lomotif) and Ioperamid (Imodium) to
decrease the motility of non-infectious source
2. Prescribed antimicrobial preparations if the identified infectious or
diarrhea worsens
3. Intravenous therapy for dehydration quickly, especially for patients who
are very young and elderly
Assesment
1. Complete medical history to identify the onset and pattern of diarrhea, and
the presence of the following signs and symptoms associated with drug
therapy last, input the daily diet, past medical history related, and trips
abroad who had just performed
2. Observe and do a complete physical examination with special attention to
the characteristics of the bowel, stool inspection, and blood pressure
3. Mucous membranes and skin inspection to determine hydration status,
inspection of the perianal skin irritation, consider the input and output and
weight
4. Ask patient or family members history of diarrhea
5. Ask Patient or family members about frequently, color, consistency of
stools
6. Assesment about vital sign
7. Assesment about intake and output
8. Observasion about sign and symptomp of dehydrasion
9. Assesment about nutritional status
Nursing Diagnosis for Diarrhea
1. Diarrhea related to presence of toxins
2. Fluid and Electrolyte Imbalances related to fluid loss secondary to diarrhea
3. Risk for Impaired Skin Integrity related to an increase in the frequency of
diarrhea.
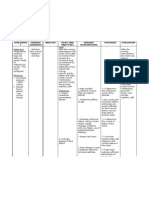
Nursing Care Plan for Diarrhea
1. Diarrhea related to presence of toxins
Goal : After 4 hours of nursing interventions, the patient will report
reduction in frequency of stools
Intervention and Rational
1) Assess pattern of defecation or have client keep a diary that includes
the following: time of day defecation occurs; usual stimulus for
defecation; consistency, amount, and frequency of stool; type of,
amount of, and time food consumed; fluid intake; history of bowel
habits
and
laxative
use;
diet;
exercise
patterns;
2)
3)
4)
5)
6)
7)
obstetrical/gynecological, medical, and surgical histories; medications;
alterations in perianal sensations; and present bowel regimen.
R/ Assessment of defecation pattern will help direct treatment.
Use Standard Precautions when caring for clients with diarrhea to
prevent spread of infectious diarrhea; use gloves and handwashing.
Clostridium difficile has been shown to be contagious and at times
epidemic.
R/ One study of medical patients demonstrated that more than 30%
developed nosocomial diarrhea after admission to a nursing unit, and
the majority of cases were caused by Clostridium
difficile.
Clostridium difficile is spread by direct or indirect contact, placing
other clients at risk for infection.
Identify cause of diarrhea if possible (e.g., viral, rotavirus, human
immunodeficiency virus/HIV), food, medication effect, radiation
therapy, protein malnutrition, laxative abuse, stress).
R/ Identification of the underlying cause is imperative because the
treatment and expected outcome depend on it. If the onset of diarrhea
is sudden with no obvious cause, a colonoscopy is recommended to
rule out colon cancer. When reviewing medication, assess for
medications that increase peristalsis, such as metoclopramide. HIV
infection is also commonly associated with diarrhea.
Assess for dehydration by observing skin turgor over sternum and
inspecting for longitudinal furrows of the tongue. Watch for excessive
thirst, fever, dizziness, lightheadedness, palpitations, excessive
cramping, bloody stools, hypotension, and symptoms of shock.
R/ Severe diarrhea can cause deficient fluid volume with extreme
weakness and cause death in the very young, the chronically ill, and
the elderly.
Observe and record stool frequency, characteristics, amount and
precipitating factors
R/ Helps differentiate individual disease and assesses severity of
episode
Observe for symptoms of sodium and potassium loss (e.g., weakness,
abdominal or leg cramping, dysrhythmia). Note results of electrolyte
laboratory studies.
R/ Stool contains electrolytes; excessive diarrhea causes electrolyte
abnormalities that can be especially harmful to clients with existing
medical conditions.
Promote bed rest
R/ Rest decreases intestinal motility and reduces metabolic rate
8) Provide bedside commode
R/ Urge to defecate may occur without warning and uncontrollable,
increasing risk of incontinence or falls if facilities are not close at
hand
9) Identify foods and fluids that precipitate diarrhea
R/ Avoiding intestinal irritans promotes intestinal rest
10) Restart oral fluid intake gradually. Offer clear liquids hourly and avoid
cold fluids
R/ Provides colon rest by ommiting or decreasing stimulus of foods or
fluids. Gradual consumption of liquids may prevent cramping and
recurrence of diarrhea. Cold fluids can increase intestinal motility.
11) Encourage to eat foods like banana and apple
R/ Fruits that are stool former
12) Avoid foods that are oily, spicy and caffein
R/ Foods that may precipitate gastric cramping
13) Administer anti-diarrheals as prescribled b the physician
R/ Decreases GI motility or peristalsis and diminishes digestive
secretions to relieve cramping and diarrhea
2. Fluid and Electrolyte Imbalances related to fluid loss secondary to diarrhea
Goal : fluid and electrolyte balance is maintained to the fullest
Expected outcomes:
a. Vital signs within normal limits
b. Elastic turgor, mucous membranes moist lips
c. Consistency soft bowel movements, frequency of 1 time per day.
Interventions and Rational:
1) Monitor signs and symptoms of fluid and electrolytes:
R/Decrease in circulating fluid volume causes mucosal dryness and
urinary concentration. Early detection enables immediate fluid
replacement therapy to correct the deficit
2) Monitor intake and output
R/Dehydration may increase the glomerular filtration rate, making the
output is not adequate to clear metabolic waste.
3) Measure your weight every day
R/Detecting fluid loss, a decrease of 1 kg equal to 1 ltr of fluid loss
4) Encourage the family to give the drink a lot on the client, 2-3 lt / day
R/Replace lost fluids and electrolytes orally.
3. Risk for Impaired Skin Integrity related to an increase in the frequency of
diarrhea.
Goal: no impaired skin integrity.
Expected outcomes:
a. Avoid irritation: redness, blisters, cleanliness maintained,
b. Families are able to demonstrate perianal care properly.
Intervention and Rational:
1) Discuss and explain the importance of keeping the bed:
R/Hygiene prevent the proliferation of germs.
2) Demonstrate and involve families in the treatment of perianal (when
wet and dressed down as well as the base):
R/Prevent skin irritation is not expected because of the humidity and
the stool acidity.
3) Adjust the position of sleeping or sitting with an interval of 2-3 hours:
R/Smooth vascularization, reducing the emphasis on time so did not
happen ischemia and irritation.
Evaluation
1) Evaluate medications client is taking. Recognize that many medications
can result in diarrhea, including digitalis, propranolol, ACE inhibitors, Hxreceptor antagonists, NSAIDS, anticholinergic agents, oral hypoglycemia
agents, antibiotics, and others. A drug-associated cause should always be
considered when treating diarrhea in the older person; many drugs can
result in diarrhea.
2) Monitor client closely to detect whether an impaction is causing diarrhea;
remove impaction as ordered. Impactions are more common in the elderly
than in younger clients. It is very important that the client be checked for
impaction before being given any antidiarrheal medication.
3) Seek medical attention if diarrhea is severe or persists for more than 24
hours, or if client has symptoms of dehydration or electrolyte disturbances
such as lassitude, weakness, or prostration. Elderly clients can dehydrate
rapidly. The greatest concern for elderly clients with severe diarrhea is
hypokalemia. Hypokalemia is treatable but when missed can be fatal.
4) Provide emotional support for clients who are having trouble controlling
unpredictable episodes of diarrhea. Diarrhea can be a great source of
embarrassment to the elderly and can lead to social isolation and a feeling
of powerlessness.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Contoh Leaflet Pra NikahDocument2 pagesContoh Leaflet Pra NikahPuteri hirika reptesNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Tugas KKDocument6 pagesTugas KKPuteri hirika reptesNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Contoh Leaflet Pra NikahDocument2 pagesContoh Leaflet Pra NikahPuteri hirika reptesNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- EnglishDocument5 pagesEnglishPuteri hirika reptesNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Argumentative Essay - Docx Air ConditionDocument3 pagesArgumentative Essay - Docx Air ConditionKUGESELVINACHAPPANNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Heat Exhaustion DehydrationDocument3 pagesHeat Exhaustion Dehydrationnoor amirullahNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Physical Education 3Document10 pagesPhysical Education 3joyce dionglayNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Why CowayDocument21 pagesWhy CowayNur AdlinaNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Subjective: Sto: DX: Fully Met: TheDocument2 pagesSubjective: Sto: DX: Fully Met: TheSoniaMarieBalanayNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Acute Viral Gastroenteritis in Children in Resource-Rich Countries - Clinical Features and DiagnosisDocument19 pagesAcute Viral Gastroenteritis in Children in Resource-Rich Countries - Clinical Features and DiagnosisNuno AlmeidaNo ratings yet
- Fluid & Electrolyte ImbalanceDocument37 pagesFluid & Electrolyte ImbalanceoutkastedNo ratings yet
- Acute Viral Gastroenteritis in Adults UpToDateDocument12 pagesAcute Viral Gastroenteritis in Adults UpToDateItzrael DíazNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Seizure NCPDocument2 pagesSeizure NCPFlashbomb Paras92% (12)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- IV Therapy History and StandardsDocument31 pagesIV Therapy History and Standardsrommelrn100% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Peh 4 12 3QDocument37 pagesPeh 4 12 3QChid CabanesasNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- DehydrationDocument14 pagesDehydrationChelly JimenoNo ratings yet
- Practice Listening & Grammar TestDocument10 pagesPractice Listening & Grammar TestLê TùngNo ratings yet
- Peer NCPDocument10 pagesPeer NCPDANA JANE SORILLANo ratings yet
- Pediatrics NCLEX Review Pointers: Signs of Increased Intracranial PressureDocument14 pagesPediatrics NCLEX Review Pointers: Signs of Increased Intracranial PressureCathryn Dominique Tan100% (1)
- Approach To The Underperforming AthleteDocument6 pagesApproach To The Underperforming AthleteGiovanni AgudeloNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Introduction To Structured Water With Clayton NolteDocument133 pagesIntroduction To Structured Water With Clayton NolteCharles Betterton, MSCED100% (7)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Department of Health, PhilippinesDocument38 pagesDepartment of Health, PhilippinesClaribel Domingo BayaniNo ratings yet
- Intake and Output MonitoringDocument9 pagesIntake and Output MonitoringlovlyNo ratings yet
- Risk for Infection r/t Knowledge DeficitDocument3 pagesRisk for Infection r/t Knowledge DeficitcattleyaNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- XcaretDocument9 pagesXcaretmubarek abdurohemanNo ratings yet
- Cholera Outbreak AssessmentDocument26 pagesCholera Outbreak AssessmentRahmiati LaoNo ratings yet
- Dehydration - PedsCase - v9Document1 pageDehydration - PedsCase - v9Chinenye ModestaNo ratings yet
- KALIBANGADocument3 pagesKALIBANGAPhil Edward Marcaida VillanuevaNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Pocket Card - IV Fluids - September 2021Document6 pagesPocket Card - IV Fluids - September 2021NeweeJoonYowNo ratings yet
- NutritionDocument14 pagesNutritionعبدالسلام الأسمرNo ratings yet
- FM 90-3 Desert OperationsDocument168 pagesFM 90-3 Desert Operationsone2much100% (2)
- Ineffective Airway Clearance R/T Tracheobronchial ObstructionDocument23 pagesIneffective Airway Clearance R/T Tracheobronchial ObstructionGuia Rose SibayanNo ratings yet
- Homeostatis F & EDocument11 pagesHomeostatis F & EYa Mei LiNo ratings yet
- NCP-Deficient Fluid VolumeDocument1 pageNCP-Deficient Fluid Volumejanmichael8No ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)