Professional Documents
Culture Documents
Trinh, T. T., Chan,, L. A. Peripheral Venous Catheter-Related Staphylococcus Aureus Bacteremia. Infection Contro
Uploaded by
Rosy SanchezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Trinh, T. T., Chan,, L. A. Peripheral Venous Catheter-Related Staphylococcus Aureus Bacteremia. Infection Contro
Uploaded by
Rosy SanchezCopyright:
Available Formats
See
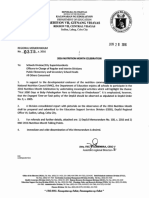
discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/51113862
Peripheral Venous Catheter-Related
Staphylococcus aureus Bacteremia
ARTICLE in INFECTION CONTROL AND HOSPITAL EPIDEMIOLOGY JUNE 2011
Impact Factor: 4.18 DOI: 10.1086/660099 Source: PubMed
CITATIONS
READS
37
233
8 AUTHORS, INCLUDING:
Brian Hollenbeck
Brian L Huang
Lifespan
University of California, Los Angeles
3 PUBLICATIONS 40 CITATIONS
20 PUBLICATIONS 112 CITATIONS
SEE PROFILE
SEE PROFILE
Julie Jefferson
Rhode Island Hospital
10 PUBLICATIONS 97 CITATIONS
SEE PROFILE
Available from: Brian L Huang
Retrieved on: 04 April 2016
infection control and hospital epidemiology
june 2011, vol. 32, no. 6
original article
Peripheral Venous Catheter-Related
Staphylococcus aureus Bacteremia
T. Tony Trinh, MD;1 Philip A. Chan, MD;1,4 Omega Edwards, MD;1,4 Brian Hollenbeck, MD;1 Brian Huang, MD;1
Nancy Burdick, RN;2 Julie A. Jefferson, RN, MPH;3 Leonard A. Mermel, DO, ScM1,3,4
objective. Better understand the incidence, risk factors, and outcomes of peripheral venous catheter (PVC)related Staphylococcus
aureus bacteremia.
design. Retrospective study of PVC-related S. aureus bacteremias in adult patients from July 2005 through March 2008. A pointprevalence survey was performed January 9, 2008, on adult inpatients to determine PVC utilization; patients with a PVC served as a cohort
to assess risk factors for PVC-related S. aureus bacteremia.
setting.
Tertiary care teaching hospital.
results. Twenty-four (18 definite and 6 probable) PVC-related S. aureus bacteremias were identified (estimated incidence density, 0.07
per 1,000 catheter-days), with a median duration of catheterization of 3 days (interquartile range, 26). Patients with PVC-related S. aureus
bacteremia were significantly more likely to have a PVC in the antecubital fossa (odds ratio [OR], 6.5), a PVC placed in the emergency
department (OR, 6.0), or a PVC placed at an outside hospital (P p .005 ), with a longer duration of catheterization (P ! .001 ). These PVCs
were significantly less likely to have been inserted in the hand (OR, 0.23) or placed on an inpatient medical unit (OR, 0.17). Mean duration
of antibiotic treatment was 19 days (95% confidence interval, 1523 days); 42% (10/24) of cases encountered complications. We estimate
that there may be as many as 10,028 PVC-related S. aureus bacteremias yearly in US adult hospitalized inpatients.
conclusion. PVC-related S. aureus bacteremia is an underrecognized complication. PVCs inserted in the emergency department or at
outside institutions, PVCs placed in the antecubital fossa, and those with prolonged dwell times are associated with such infections.
Infect Control Hosp Epidemiol 2011;32(6):579-583
Central venous catheter-associated bloodstream infections affect an estimated 41,000 patients per year in US hospitals.1
Although the risk of bloodstream infection associated with
peripheral venous catheter (PVC) use is lower than that associated with other intravascular devices,2 there is far greater
use of these catheters than of central venous catheters
(CVCs),3-6 leading to the potential for serious infections in
large numbers of patients.6,7
Staphylococcus aureus is the second most common cause
of hospital-acquired bloodstream infection,8 and it is the
pathogen most often associated with serious and costly catheter-related bloodstream infections,9 such as endovascular
and disseminated infections.10,11 Patients with PVC-related S.
aureus bacteremia have a higher risk of complications compared with such infections due to other pathogens.6 Thus, we
set out to determine the incidence, risk factors, treatment,
and outcome of PVC-related S. aureus bacteremia at our
hospital.
methods
We retrospectively reviewed adult patients admitted to our
tertiary care hospital from July 1, 2005, through March 31,
2008, with S. aureus bacteremia. An episode of definite PVCrelated S. aureus bacteremia was defined as a patient with
blood cultures growing S. aureus, a PVC tip culture or PVC
insertion site culture growing S. aureus, no other source of
S. aureus bacteremia identified, and physician or intravenous
(IV) nursing team documentation noting the PVC as the
source of bacteremia. A case of probable PVC-related S. aureus bacteremia was defined as a patient with physical findings
suggesting a PVC infection (erythema, induration, phlebitis,
drainage, or palpable cord related to the PVC insertion site);
no other source of bacteremia based on medical record review
but in whom there was no culture of the PVC tip or drainage
from the insertion site; and no physician, nursing, or IV
nursing team documentation that the PVC was the source of
S. aureus bacteremia. Phlebitis was assessed using the Visual
Affiliations: 1. Department of Medicine, Rhode Island Hospital, and Warren Alpert Medical School of Brown University, Providence, Rhode Island;
2. Department of Nursing, Rhode Island Hospital, Providence, Rhode Island; 3. Department of Epidemiology and Infection Control, Rhode Island Hospital,
Providence, Rhode Island; 4. Division of Infectious Diseases, Rhode Island Hospital, Providence, Rhode Island.
Received September 28, 2010; accepted December 18, 2010; electronically published April 29, 2011.
2011 by The Society for Healthcare Epidemiology of America. All rights reserved. 0899-823X/2011/3206-0007$15.00. DOI: 10.1086/660099
580
infection control and hospital epidemiology
june 2011, vol. 32, no. 6
Infusion Phlebitis score (1, pain and redness around the insertion site; 2, pain, swelling, erythema, and a palpable venous
cord; 3, pain, swelling, erythema, palpable venous cord beyond 3 cm, and the presence of a purulent exudate; 4, all of
the above and evidence of tissue damage). This study was
approved by the Rhode Island Hospital Institutional Review
Board.
Source Identification
Rhode Island Hospital infection control software (Theradoc)
was searched for all microbiologic cultures growing S. aureus
from adult inpatients during the study period. For each patient with S. aureus bacteremia, we reviewed all other cultures
growing S. aureus for 3 months after the S. aureus bacteremia
was documented. Cases of S. aureus bacteremia with a PVC
tip or insertion site wound culture growing S. aureus within
3 days of S. aureus bacteremia were included as cases. Patients
with S. aureus bacteremia without an identified microbiologic
source were further reviewed using electronic patient data. If
there was no identifiable source of bacteremia, we crossreferenced each such case with the IV nursing team records.
Analysis
To estimate total PVC-days during the study period, we used
hospital administrative data to determine the total number
of adult inpatient-days during the study period, and we multiplied that number by the fraction of adult inpatients with
a PVC during a point-prevalence survey we performed on
January 9, 2008, on all adult inpatient units.
Medical record review was performed on all cases of PVCrelated S. aureus bacteremia. Descriptive statistics were generated for demographic and clinical parameters. The MannWhitney U test was used to determine the differences in
duration of catheterization between the patients with PVCrelated S. aureus bacteremia and patients in the PVC pointprevalence survey; otherwise, the Fischer exact test was used.
results
A total of 544 cases of S. aureus bacteremia were identified
(Table 1). Twenty-four (18 definite and 6 probable) PVCrelated S. aureus bacteremias were identified in 24 patients
with a mean age of 63 years (95% confidence interval [CI],
5571 years; Table 2). There were 451,366 adult patient-days
during the study period. In our point-prevalence survey, 298
of 392 of adult inpatients (76%) had a PVC. Thus, during
the study, there were approximately 343,130 PVC-days, leading to an estimated incidence density of PVC-related S. aureus
bacteremia of 0.07 per 1,000 PVC-days.
For 16 of the PVC-related S. aureus bacteremias (67%),
the PVC was placed in our emergency department, 4 (17%)
were placed in an inpatient unit, 2 (8%) were placed by
emergency medical services prior to admission, and 2 (8%)
were placed at outside hospitals. There was no temporal clustering of PVCs inserted in our emergency department that
table 1. Source of Staphylococcus aureus Bacteremia
Source
Soft tissue or bone
CVC or PICCa
Pulmonary
PVC
Endovascular
Urinary tract
Otherb
Unknown
Total
(n p 544)
204
172
88
24
12
12
9
23
(37)
(32)
(16)
(4)
(2)
(2)
(2)
(4)
MSSA
(n p 296)
116
77
43
16
11
8
5
21
(39)
(26)
(15)
(5)
(4)
(3)
(2)
(6)
MRSA
(n p 248)
89
95
45
8
1
4
4
2
(36)
(38)
(18)
(3)
(0.4)
(2)
(2)
(1)
note. Data are no. (%).
a
CVC, central venous catheter; MRSA, methicillin-resistant
Staphylococcus aureus; MSSA, methicillin-susceptible Staphylococcus aureus; PICC, peripherally inserted central catheter;
PVC, peripheral venous catheter.
b
Other includes S. aureus bacteremia associated with injection drug use (6), infected pacemaker (1), traumatic paracentesis (1), or traumatic bladder catheter insertion (1).
led to S. aureus bacteremias. Eleven of the 24 PVCs (46%)
were in the right antecubital fossa, 5 (21%) in the right forearm, 1 (4%) in the right hand, 5 (21%) in the left antecubital
fossa, 1 (4%) in the left forearm, and 1 (4%) in the left hand.
The mean visual phlebitis score was 3 (95% CI, 2.43.4).
Compared with the those in the point-prevalence survey, patients with PVC-related S. aureus bacteremia were more likely
to have the PVC inserted in the emergency department or at
an outside hospital and more likely to have the PVC in the
antecubital fossa (Table 3). The median duration of PVC
dwell time before the blood culture was obtained that grew
S. aureus was 3 days (interquartile range [IQR], 36 days),
compared with a median duration of PVC placement of 1
day (IQR, 12 days) in the point-prevalence survey (P !
.001).
The mean hospital duration for patients with PVC-related
S. aureus bacteremia was 15 days (95% CI, 1019). The mean
prescribed antibiotic course was 19 days (95% CI, 1523).
Eight patients and 1 patient had transthoracic and transesophageal echocardiograms, respectively; none revealed vegetations. Ten (42%) patients encountered complications. Two
patients required incision and drainage of the PVC insertion
site, 3 patients developed complications related to antibiotic
therapy (Clostridium difficile colitis in 2 patients and 1 patient
with upper-extremity deep venous thrombosis related to the
peripherally inserted central catheter for intravenous antibiotics), 2 patients died, and 1 was discharged to hospice
care.
discussion
In our study, 12% of S. aureus catheter-related bacteremias
were due to PVCs, similar to 11% reported by others12 but
in contrast to another study that found an equal number of
S. aureus bacteremias due to PVCs and CVCs.13 Our study
reaffirms the substantial medical burden that arises from these
staphylococcus aureus bacteremia
581
table 2. Characteristics of Peripheral Venous Catheter (PVC)Related Staphylococcus aureus
Bacteremia Cases
Patient characteristics
Mean age, years (95% CI)
Female
Male
Clinical setting of PVC insertion
Emergency department
Inpatient medical unit
Rescue
Outside hospital
Anatomical site of PVC insertion
Right hand
Right antecubital area
Right forearm
Left hand
Left antecubital area
Left forearm
Clinical and microbiological characteristics
Mean duration of PVC insertion prior to PVCrelated S. aureus bacteremia, days (95% CI)
Mean visual infusion phlebitis score (95% CI)a
Yes
No
Definite
(n p 18)
Probable
(n p 6)
Total
(n p 24)
63 (5570)
5 (28)
13 (72)
65 (3595)
1 (17)
5 (83)
63 (5571)
6 (25)
18 (75)
13 (72)
4 (22)
1 (6)
0
3 (50)
0
1 (17)
2 (33)
16
4
2
2
(67)
(17)
(8)
(8)
1
10
3
0
3
1
(17)
(6)
0
1
2
1
2
0
(17)
(33)
(17)
(33)
1
11
5
1
5
1
(4)
(46)
(21)
(4)
(21)
(4)
3.8 (35)
3 (23)
7 (39)
11 (61)
4
3
1
5
(27)
(24)
(17)
(83)
4
3
8
16
(36)
(34)
(33)
(67)
(6)
(56)
(17)
note. Data are no. (%) unless otherwise indicated. CI, confidence interval.
a
Visual infusion phlebitis score: 1 pain or redness around insertion site; 2 pain, swelling,
redness, palpable venous cord; 3 pain, swelling, induration, redness, palpable venous cord beyond
3 cm, presence of pus; 4 all of the above and presence of tissue damage.
infections, as 42% of our patients with PVC-related S. aureus
bacteremia encountered complications.
More PVCs causing S. aureus bacteremia were placed in
the emergency department than PVCs in our point-prevalence survey, consistent with findings of emergent catheter
insertion increasing the risk of phlebitis14 and independently
increasing the risk of catheter colonization or local infection.15
A greater than expected number of PVC-related S. aureus
bacteremias involved catheters in the antecubital fossa, possibly related to an increased risk of phlebitis at this site16 and
cannulation of veins in areas of joint flexion.17 It is unknown
whether the antecubital fossa has a greater density of S. aureus
colonization than do other upper-extremity sites or whether
it is more difficult to maintain dressing placement at this site.
The median duration of time between PVC placement and
the first positive blood culture growing S. aureus was 3 days
(IQR, 36 days); however, 46% of patients with PVC-related
S. aureus bacteremia had a PVC duration greater than 3 days.
A meta-analysis suggests that changing PVCs every 3 days
does not reduce infection risk.18 However, in a national survey, in more than 90% of PVC-associated sepsis cases, the
PVC was in situ for 3 or more days,3 and there is an independent linear relationship between PVC infectious complications and dwell time.19 Thus, the meta-analysis may have
been underpowered to address the issue as a result of a small
number of catheters in place beyond 3 days and the low risk
of bloodstream infection.
We found 0.06 PVC-related S. aureus bacteremias per 1,000
catheter-days. The true incidence may have been underestimated because of our retrospective study design and the tendency for clinicians to overlook a PVC as a source for bacteremia. Another limitation of our study was the comparison
group, which was based on a 1-day point-prevalence survey;
as such, this may not have been a representative sample of
patients with uninfected PVCs.
Various hospital PVC care campaigns have reduced risk of
PVC infections. Intravenous nursing teams reduce the risk
of PVC infections,20-22 and this may relate to better compliance with relocating PVCs within 72 hours or within 24 hours
for emergently inserted PVCs.23 Insertion of a PVC after hand
hygiene with an alcohol waterless antiseptic or after donning
gloves is independently associated with lower risk of infectious complications.19 PVCs are often in situ, despite being
unused for 2 or more days,23,24 and quality improvement efforts can eliminate such idle catheters.24 Other interventions
can reduce the risk of such infections.25,26
PVC infections have been deemphasized, as most of our
national and local preventative efforts have focused on CVCs.
We documented 24 PVC-related S. aureus bacteremias involving 77,852 adult hospital discharges. There was a mean
582
infection control and hospital epidemiology
june 2011, vol. 32, no. 6
table 3. Comparison of Peripheral Venous Catheters (PVCs) Associated with Documented Staphylococcus aureus Bacteremia and
PVCs without Associated Documented S. aureus Bacteremia
Anatomical site of PVC insertion
No. of PVCs
Hand
Antecubital area
Forearm
Location of PVC insertion
No. of patients with a PVC
Emergency department
Inpatient medical unit
Rescue
Outside hospital
Operating room or radiology
Unknown
Duration of PVC insertion
Median, days (IQR)
PVC-related S. aureus
bacteremia
PVC without S. aureus
bacteremiaa
24
2 (8)
16 (67)
6 (25)
317b
91 (29)
75 (24)
151 (48)
1.00
0.23
6.45
0.37
24
16
4
2
2
0
0
298
79
170
7
0
18
24
1.00
6.03
0.17
4.03
(67)
(17)
(8)
(8)
3 (36)
Exact odds ratio
(95% CI)
(reference)
(0.20.95)
(2.4718.02)
(0.121.00)
(6)
(8)
(reference)
(2.310.76)
(0.040.53)
(0.3822.76)
...
0 (03.06)
0 (02.19)
1 (12)
...
(27)
(57)
(2)
P valueb
.03
!.001
.03
!.001
!.001
.7
.005
.3
.4
!.001
note. Data are no. (%) unless otherwise indicated. CI, confidence interval; IQR, interquartile range.
a
PVCs identified in a point-prevalence survey; some patients had more than 1 PVC.
b
Fischers exact test
of 32,529,144 adult patient discharges from US hospitals from
2005 through 2007.27 Thus, we estimate that there may be as
many as 10,028 PVC-related S. aureus bacteremias each year
in adults hospitalized in the United States. One study found
that having a PVC was independently associated with a lower
risk of S. aureus bacteremia.28 However, the risk posed by
PVCs must be viewed on a national scale since many patients
have a PVC during their hospital stay. Our study suggests
that hospitals should assess their risk of PVC-related infections and initiate interventions to mitigate risk if such infections are found. Minimizing PVC placement in the antecubital fossa, consideration for removing catheters within
24 hours if they were placed under emergent conditions, and
strong consideration for replacing PVCs after a 72-hour dwell
time will reduce risk of infection in adult patients.
acknowledgments
We appreciate the secretarial support of Nicole Lundstrom; the statistical
assistance of Jason Machan, PhD (Rhode Island Hospital and Warren Alpert
Medical School of Brown University); and the nurses who kindly carried out
the point-prevalence survey.
Financial support. This study had no external funding.
Potential conflicts of interest. L.A.M. has received research support from
Theravance and Pfizer and has served as a consultant for CorMedix, Ash
Access, Semprus, CareFusion, Bard, and Catheter Connections. None of these
activities involved peripheral intravenous catheters. All other authors report
no conflicts of interest relevant to this article.
Address correspondence to Leonard Mermel, DO, ScM, Division of Infectious Diseases, Rhode Island Hospital, 593 Eddy Street, Providence, RI
02903 (lmermel@lifespan.org).
references
1. Centers for Disease Control and Prevention. Vital signs: central
lineassociated blood stream infectionsUnited States, 2001,
2008, and 2009. MMWR Morb Mortal Wkly Rep 2011;60:243
248.
2. Maki DG, Kluger DM, Crnich CJ. The risk of bloodstream infection in adults with different intravascular devices: a systematic
review of 200 published prospective studies. Mayo Clinic Proc
2006;81:11591171.
3. Collignon PJ. Intravascular catheter associated sepsis, a common
problem: the Australian study on intravascular catheter-associated sepsis. Med J Aust 1994;161:374378.
4. Voges KA, Webb D, Fish LL, Kressel AB. One-day point-prevalence survey of central, arterial, and peripheral line use in adult
inpatients. Infect Control Hosp Epidemiol 2009;30:606608.
5. Ritchie S, Jowitt D, Roberts S; and the Auckland District Health
Board Infection Control Service. The Auckland City Hospital
Device Point Prevalence Survey 2005: utilisation and infectious
complications of intravascular and urinary devices. N Z Med J
2007;120:U2683.
6. Pujol M, Hornero A, Saballs M, et al. Clinical epidemiology and
outcomes of peripheral venous catheter-related bloodstream infections at a university-affiliated hospital. J Hosp Infect 2007;67:
2229.
7. Zingg W, Imhof A, Maggiorini M, Stocker R, Keller E, Ruef C.
Impact of a prevention strategy targeting hand hygiene and
catheter care on the incidence of catheter-related bloodstream
infections. Crit Care Med 2009;37:21672173.
8. Hidron AI, Edwards JR, Patel J, et al, for the National Healthcare
Safety Network Team and Participating National Healthcare
Safety Network Facilities. NHSN annual update: antimicrobialresistant pathogens associated with healthcare-associated infections: annual summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and
staphylococcus aureus bacteremia
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
Prevention, 20062007. Infect Control Hosp Epidemiol 2008;29:
9961011.
Arnow PM, Quimosing EM, Beach M. Consequences of intravascular catheter sepsis. Clin Infect Dis 1993;16:778784.
Lowy FD. Staphylococcus aureus infections. N Engl J Med 1998;
339:520532.
Fowler VG Jr, Justice A, Moore C, et al. Risk factors for hematogenous complications of intravascular catheter-associated
Staphylococcus aureus bacteremia. Clin Infect Dis 2005;40:695
703.
Malanoski GJ, Samore MH, Pefanis A, Karchmer AW. Staphylococcus aureus catheter-associated bacteremia: minimal effective
therapy and unusual infectious complications associated with
arterial sheath catheters. Arch Intern Med 1995;155:11611166.
Thomas MG, Morris AJ. Cannula-associated Staphylococcus aureus bacteraemia: outcome in relation to treatment. Intern Med
J 2005;35:319330.
Larson E, Hargiss C. A decentralized approach to maintenance
of intravenous therapy. Am J Infect Control 1984;12:177186.
Goetz AM, Wagener MM, Miller JM, Muder RR. Risk of infection due to central venous catheters: effect of site of placement
and catheter type. Infect Control Hosp Epidemiol 1998;19:842
845.
Adams SD, Killien M, Larson E. In-line filtration and infusion
phlebitis. Heart Lung 1986;15:134140.
Lavery I, Ingram P. Prevention of infection in peripheral intravenous devices. Nurs Stand 2006;20:4956.
Webster J, Osborne S, Rickard C, Hall J. Clinically indicated
replacement versus routine replacement of peripheral venous
catheters. Cochrane Database Syst Rev 2010;3:CD007798.
Hirshmann H, Fux L, Podusel J, et al; and the European In-
20.
21.
22.
23.
24.
25.
26.
27.
28.
583
terdisciplinary Committee for Infection Prophylaxis. The influence of hand hygiene prior to insertion of peripheral venous
catheters on the frequency of complications. J Hosp Infect 2001;
49:199203.
Tomford JW, Hershey CO, McLaren CE, Porter DK, Cohen DI.
Intravenous therapy team and peripheral venous catheterassociated complications: a prospective controlled study. Arch
Intern Med 1984;144:11911194.
Meier PA, Fredrickson M, Catney M, Nettleman MD. Impact
of a dedicated intravenous therapy team on nosocomial bloodstream infection rates. Am J Infect Control 1998;26:388392.
Soifer NE, Borzak S, Edlin BR, Weinstein RA. Prevention of
peripheral venous catheter complications with an intravenous
therapy team: a randomized controlled trial. Arch Intern Med
1998;158:473477.
Lederle FA, Parenti CM, Berskow LC, Ellingson KJ. The idle
intravenous catheter. Ann Intern Med 1992;116:737738.
Parenti CM, Lederle FA, Impola CL, Peterson LR. Reduction of
unnecessary intravenous catheter use: internal medicine house
staff participate in a successful quality improvement project.
Arch Intern Med 1994;154:18291832.
Aziz AM. Improving peripheral IV cannula care: implementing
high-impact interventions. Br J Nurs 2009;18:12421246.
OGrady NP, Alexander M, Burns LA, et al. Guidelines for the
prevention of intravascular catheter-related infection. Clin Infect
Dis 2011;52:e162e193.
AHRQ. National Inpatient Sample. http://hcupnet.ahrq.gov. Accessed April 12, 2010.
Stryjewski ME, Kanafani ZA, Chu VH, et al. Staphylococcus aureus bacteremia among patients with health care-associated fever.
Am J Med 2009;122:281289.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Matchstick MenDocument9 pagesMatchstick Menmichael_arnesonNo ratings yet
- Cancer of Oral CavityDocument27 pagesCancer of Oral CavityMihai AlexandruNo ratings yet
- The Tuskegee Syphilis StudyDocument11 pagesThe Tuskegee Syphilis Studyapi-285171544No ratings yet
- Aesthetic Jurnal PDFDocument20 pagesAesthetic Jurnal PDFTarrayuanaNo ratings yet
- 1000 Days Ni Baby PDFDocument31 pages1000 Days Ni Baby PDFppantollanaNo ratings yet
- Sfbtnarr 2Document19 pagesSfbtnarr 2api-267074391No ratings yet
- Congenital Syphilis Causes and TreatmentDocument4 pagesCongenital Syphilis Causes and TreatmentAlya Putri Khairani100% (1)
- Practicing The A, B, C'S: Albert Ellis and REBTDocument24 pagesPracticing The A, B, C'S: Albert Ellis and REBTShareenjitKaurNo ratings yet
- MNA EnglishDocument1 pageMNA Englishdidik hariyadiNo ratings yet
- Registered Dietitians in Primary CareDocument36 pagesRegistered Dietitians in Primary CareAlegria03No ratings yet
- NM ObtDocument22 pagesNM ObtIlyan NastiNo ratings yet
- Huckstep Nail For Periimplant FractureDocument3 pagesHuckstep Nail For Periimplant FracturePurushothama Rao NalamatiNo ratings yet
- Brand Name Generic Name Disease Group Consumer Medicine Information More InfoDocument9 pagesBrand Name Generic Name Disease Group Consumer Medicine Information More InfoBairavi RathakrishnanNo ratings yet
- M5W Wang FeedbackDocument21 pagesM5W Wang FeedbackIsaac HassanNo ratings yet
- Magnetic StimulationDocument5 pagesMagnetic StimulationMikaelNJonssonNo ratings yet
- Twins Bootcamp StudyDocument5 pagesTwins Bootcamp Studyandi dirhanNo ratings yet
- علاجDocument5 pagesعلاجabramNo ratings yet
- Lymphatic Drainage 101Document6 pagesLymphatic Drainage 101Vy HoangNo ratings yet
- Country Presentation: CambodiaDocument11 pagesCountry Presentation: CambodiaADBI Events100% (1)
- Drugs in PregnancyDocument14 pagesDrugs in Pregnancyhenry_poirotNo ratings yet
- Case Report in Psychiatry051.03Document4 pagesCase Report in Psychiatry051.03Christian Tan Getana100% (1)
- Puyer Asthma and Diare Medication DosagesDocument1 pagePuyer Asthma and Diare Medication DosagesAlbert SudharsonoNo ratings yet
- Aromatherapy PRDocument1 pageAromatherapy PRNilamdeen Mohamed ZamilNo ratings yet
- Types of PsychologyDocument62 pagesTypes of PsychologyParamjit SharmaNo ratings yet
- Safety Data Sheet for Masterseal 345Document7 pagesSafety Data Sheet for Masterseal 345mkashkooli_scribdNo ratings yet
- Ethical PrinciplesDocument2 pagesEthical PrinciplesyoonjessNo ratings yet
- Wound AssessmentDocument19 pagesWound Assessmentdrsonuchawla100% (1)
- Gestalt PsychotherapyDocument2 pagesGestalt PsychotherapyAnson AtilanoNo ratings yet
- Psychotherapeutic Traditions HandoutDocument5 pagesPsychotherapeutic Traditions HandoutTina Malabanan CobarrubiasNo ratings yet
- A Case Study For Electrical StimulationDocument3 pagesA Case Study For Electrical StimulationFaisal QureshiNo ratings yet