Professional Documents
Culture Documents
Nutrition and Fluid Balance Must Be Taken Seriously
Uploaded by
Paola RincónCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nutrition and Fluid Balance Must Be Taken Seriously
Uploaded by
Paola RincónCopyright:
Available Formats
BMJ 2013;346:f801 doi: 10.1136/bmj.
f801 (Published 8 February 2013)
Page 1 of 5
Analysis
ANALYSIS
Nutrition and fluid balance must be taken seriously
Richard Leach and colleagues explain why ensuring adequate nutrition and hydration makes both
clinical and financial sense and requires the attention of everyone involved in healthcare
1
Richard M Leach chair, Royal College of Physicians nutrition committee , Ailsa Brotherton honorary
2
secretary, British Association for Parenteral and Enteral Nutrition , Michael Stroud chair, NICE fluid
3
4
guideline committee , Richard Thompson president
Guys and St Thomas NHS Foundation Trust, London, UK; 2NHS Quest, Salford Royal NHS Foundation Trust, Salford, UK ; 3Gastroenterology
and Nutrition, Southampton University Hospitals NHS Trust, Southampton, UK; 4Royal College of Physicians, London, UK
1
Provision of appropriate nutrition and hydration is a hallmark
of compassionate care but is often neglected in all types of
healthcare.1-5 These problems are not new and have been reported
in the medical literature for nearly four decades.6 7 The
consequences are clinically and financially costly. The estimated
excess UK health related costs of malnutrition are at least 13bn
(15bn; $20bn) annually.1
Patients with malnutrition have a deficit of energy, protein,
vitamins, or minerals, and this has measurable adverse effects
on the body.2 Those at risk include patients with poor intake or
appetite, dysphagia, chronic disease, or poor functional and
social or cognitive ability. Defining adequate hydration is
complex. It is estimated by the synthesis of clinical indicators
(such as confusion, tachycardia, blood pressure, and thirst),
serum biochemistry (such as urea and creatinine), tissue
perfusion markers (such as urine output, lactate levels), and
urine specific gravity. We examine the scale of malnutrition
and poor hydration in our hospitals and communities, explain
why it matters, and put forward proposals for change.
Big problem with bad press
The UK national nutrition surveys estimate that over three
million people are either malnourished or at risk of malnutrition,
of whom more than 90%, or 2.7 million, are cared for in the
community (box 1).1 2 3 5 8 One in three patients admitted to
hospital or a care home, and one in five of those admitted to
mental health facilities were malnourished or at risk of
malnutrition, according to four national surveys (31 646 people
admitted to hospital, 3404 to care homes, and 1206 to mental
health facilities).8 Nutritional status often declines further after
admission to hospital because acute illness or injury can impair
appetite, swallowing, and intestinal absorption. Similar problems
occur in other countries.2 9 10
The health ombudsman for England, Ann Abraham, found a
lack of access to fresh drinking water and inadequate help with
eating in half of cases during her investigations into care of
older people.11 She described this as incomprehensible and said
that everybody working in the NHS, including doctors, nurses,
managers, and chief executives, had a responsibility to deliver
adequate fluid and nutrition. Her findings are not isolated.12 13
The Care Quality Commission (CQC) reported that just 51 of
100 acute NHS hospitals fully complied with their standards
for meeting patients nutritional needs.12 The commissions
dignity and nutrition report on the inspection of 500 care homes
in 2012 is currently awaited.12 Age UKs campaign Hungry to
be heard and the Patients Association report Malnutrition in
the Community and Hospital Setting both indicate inadequate
provision of easily accessible food and hydration in all types of
healthcare facility.5 13
Importance of nutrition and fluid
management
Malnutrition is associated with increased morbidity and
mortality in acute and chronic diseases.1-3 Complications
associated with malnutrition can arise within days in people
with little or no nutritional intake and may precede significant
weight loss.
In wound healing, malnutrition prolongs the inflammatory phase,
decreases fibroblast proliferation, alters collagen synthesis, and
ultimately reduces wound tensile strength.14 Consequently,
malnutrition is associated with increased risk of pressure ulcers,
delayed wound healing, wound infections, and chronic
non-healing wounds. Malnutrition also impairs the immune
system by suppressing cell mediated immunity, complement
systems, phagocyte function, cytokine production and antibody
response and affinity.15 In an observational study, hospital
inpatients identified as high risk by the nutritional risk index
were at three times the risk of nosocomial infection compared
with similar patients who were well nourished.16 Malnutrition
is associated with a twofold to threefold increased risk of
postoperative complications.1 2 8 10
Correspondence to: R M Leach richard.leach@gstt.nhs.uk
For personal use only: See rights and reprints http://www.bmj.com/permissions
Subscribe: http://www.bmj.com/subscribe
BMJ 2013;346:f801 doi: 10.1136/bmj.f801 (Published 8 February 2013)
Page 2 of 5
ANALYSIS
Box 1: Prevalence of malnutrition in UK1-3 5 8
Home
General population (adults):
Body mass index <20=5%
Body mass index <18.5=1.8%
People over 65=14%
Sheltered housing
10-14% of residents
Hospital
25-34% of admissions
Care homes
30-42% of recently admitted residents
Malnutrition also affects patients admitted to hospital with
conditions such as stroke, pressure ulcers, or falls. Increased
morbidity secondary to malnutrition prolongs hospital stay by
an average of three days and increases readmission rates by up
to 50%.1-5 9 10 The effect of poor nutrition is particularly severe
in older people.
Chronic malnutrition is associated with frailty, unintentional
weight loss, weakness, immobility, sarcopenia, and poor
endurance. Those who are malnourished visit their general
practitioner twice as often as the well nourished and are three
times more likely to be admitted to hospital, irrespective of
other conditions.4 They also experience more complications and
higher death rates in all age groups and disease categories.1-5 9 10
People who are risk of malnutrition also seem to experience
adverse outcomes. For example, in a recent, large multicentre
study (n=5051) in 12 countries and 26 hospital departments,
patients at risk of malnutrition had a 12-fold increase in hospital
mortality.10
Dehydration and overhydration are well recognised causes and
consequences of illness and injury. The association between
intravenous fluid overload and subsequent morbidity and
mortality is rarely recognised by regulatory authorities because
of the difficulty in attributing cause and effect. Overhydration
manifested as pulmonary oedema is a common consequence of
excessive intravenous fluids. Pulmonary oedema can be rapidly
corrected with diuretic therapy. However, the pneumonia that
may follow may not be considered a fluid related complication
and is rarely reported. In postoperative patients fluid
mismanagement has been documented in 17-54% of cases and
contributes to about 9000 deaths annually in the United
States.17-19
Improving malnutrition and poor fluid management makes
financial as well as clinical sense.20 The National Institute for
Health and Clinical Excellence has identified improvements in
nutritional care as the fourth largest potential source of NHS
savings.2 A malnourished patient costs the NHS 2000 a year.10
The cost of poor fluid management has not been established.
However, it may be considerable if problems such as acute
kidney injury from avoidable dehydration are added to those
related to excess fluid administration (pulmonary oedema, post
surgical ileus, wound breakdown, etc).17 18
Mismatch between guidance and reality
NICE has issued clear guidance on nutritional screening, dietary
requirements, and care of people identified as at risk (box 22).
However despite the scale and impact of poor nutrition and
hydration these standards are often not met. Many factors may
For personal use only: See rights and reprints http://www.bmj.com/permissions
contribute to poor implementation, such as poor training, lack
of time, competing tasks, and a perception that basic care is less
important than others duties or the responsibility of others (box
3).
Screening
The first job is to identify people who may be malnourished. In
the UK 93% of those who are malnourished, or at risk of
malnutrition, are living in their own homes, and 5% are in care
homes. NICE guidelines state that GPs should screen all
patients nutrition on registration, care homes should screen
people on enrolment, and hospitals at the first outpatient
appointment. However, two thirds of the patients admitted to
hospital who are malnourished or at risk of malnutrition come
directly from their own home, suggesting the need for improved
recognition and management of nutritional problems in the
community.
The remaining 2% of those who are malnourished or at risk of
malnutrition are in hospital. Admission to hospital provides a
vital opportunity to identify malnutrition and initiate treatment,
which can then be continued in the community after discharge.
The NICE guidelines suggest that adults nutritional status
should be screened on admission to hospital. Most hospitals
recognise that screening with validated nutritional tools such
as the Malnutrition Universal Screening Tool should be part of
basic clinical care,1-3 21 but many lack robust systems to ensure
it is done or the results acted on.
Recognition
In hospital, poor documentation of fluid balance and nutritional
intake contributes to morbidity and mortality.17 18 22-25 Less than
half of fluid balance sheets are completed adequately, and in
complex cases, electrolyte (biochemical) monitoring is often
poor.17 18 25 One in three nurses does not feel competent to
recognise or treat malnutrition or fluid management.12
Appropriate treatment
Assuming the patient can swallow safely, the first step is to
maximise normal food intake with a balanced mixture of protein,
energy, fibre, electrolytes, vitamins, and minerals. Despite
substantial improvements, some hospitals and care homes
continue to offer unsuitable menus with insufficient provision
for food preferences, ethnic and religious needs, or portion
sizes.2 5 13
A different approach may be needed for patients who have lost
their appetite. Cochrane meta-analysis shows little or no benefit
from dietetic intervention for malnutrition accompanying acute
Subscribe: http://www.bmj.com/subscribe
BMJ 2013;346:f801 doi: 10.1136/bmj.f801 (Published 8 February 2013)
Page 3 of 5
ANALYSIS
Box 2: Key NICE recommendations on nutrition support in adults2
Screening for malnutrition or the risk of malnutrition should be carried out by healthcare professionals with appropriate skills and
training
All hospital inpatients should be screened on admission and all outpatients at their first clinic appointment. Screening should be
repeated weekly for inpatients and, when there is clinical concern, for outpatients. People in care homes should be screened on
admission and when there is clinical concern
Nutrition support should be considered in people who are malnourished, as defined by any of the following:
Body mass index (BMI) <18.5
Unintentional weight loss greater than 10% within past 3-6 months
BMI <20 and unintentional weight loss greater than 5% in the last 36 months.
People who have eaten little or nothing for more than 5 days or are likely to eat little or nothing for the next 5 days or longer
People who have a poor absorptive capacity, high nutrient losses, or increased nutritional needs from causes such as catabolism
Box 3: Barriers to improving nutritional and fluid care
Lack of education for frontline staff on the importance of nutrition and hydration care coupled with poor attitudes and lack of respect
for vulnerable, often elderly patients
Failure of acute trusts to implement 2006 NICE guidance on nutrition steering committees and multidisciplinary nutrition support team
with at least one specialist nutrition support nurse to minimise complications from enteral tube and intravenous nutrition
Reluctance of practitioners, health service managers, and professional groups to accept responsibility for setting polices and standards
at local or national levels
Multiple malnutrition guidelines and initiatives that may add confusion rather than clarity
Some misleading research and public advice causing both professional and public scepticism about nutritional standards
Lack of research on fluid management beyond highly specialised settings and lack of specific guidance on general fluid prescribing
illness. Oral nutritional supplements, often referred to as build
up drinks, may help in the short term.1-3 A Cochrane
meta-analysis of 42 randomised controlled trials of oral
supplements versus standard care in malnourished elderly
hospital patients showed a mean 2.2% increase in weight (95%
confidence interval 1.8 to 2.5) and reductions in a composite
outcome of complications such as infection, deep vein
thrombosis, and pressure sores (relative risk 0.86, 0.75 to 0.99).26
The use and prescription of short term oral nutritional
supplements is variable and controversial in the UK because of
perceived recent rapid increases in their costs and reported
inappropriate use and wastage. Properly planned nutritional care
should reduce inappropriate use and improve individual patient
outcomes. Although demand (and associated expenditure on
supplements ) is likely to increase, the overall treatment costs
should fall significantly.1-3 27
When oral nutrition is not possible or is inadequate, enteral tube
feeding and/or intravenous nutrition are necessary. Both methods
carry risk. In 2009-10, 41 never events were reported to the
National Patient Safety Agency, where a misplaced nasogastric
or orogastric tube was not detected before use.28 The National
Confidential Enquiry into Patient Outcome and Death
(NCEPOD) found that 81% of patients receiving intravenous
nutrition did not receive quality care, characterised by thorough
assessment, appropriate intravenous feed, safe intravenous
access, and electrolyte monitoring, delivered by a trained team.29
There are also problems with prescribing and delivering fluids.4
Volumes and types of fluid prescription are often
inappropriate.17 24 For example, in studies in postoperative
patients there was little correlation between fluid and electrolytes
prescription and preoperative weight, serum electrolyte levels,
or ongoing fluid losses.17 Only 26% of intravenous fluid
prescriptions were administered at the prescribed rate; 67%
were infused too slowly and 8% too fast.24 Lack of routine and
careful fluid assessment during ward rounds led by senior
clinicians and pharmacists is likely to play a part. Decisions
may be left until out of hours periods, when junior doctors must
prescribe fluids for patients they do not know, although formal
evidence for this is lacking.
For personal use only: See rights and reprints http://www.bmj.com/permissions
Junior clinicians and nursing staff lack basic knowledge about
nutritional care and fluid and electrolyte management. Half of
new foundation doctors lack the basic knowledge to prescribe
perioperative fluid safely.22 25 30 31 Less than half of trainees know
the sodium content of 0.9% saline, suggesting that many do not
know the normal daily fluid and electrolyte maintenance
requirements, or use this knowledge in daily fluid management
practice, a suspicion supported by audit data.25 Although the
curriculums for undergraduate and foundation doctor training
include the essential information for safe fluid prescription, it
is often piecemeal, rarely consolidated to provide practical
guidance, and competency is not robustly monitored.22 This is
because such core general education aligns poorly with specialist
training programmes and is often considered less important.19 22
Way forward
Considerable, but uncoordinated, efforts have been made to
provide high quality guidance on solving these problems, with
over 20 initiatives, guidelines, quality standards, and nutritional
indicators published in service frameworks commissioning
guidelines since 2000.1 5 Yet there has been a failure to translate
this knowledge into high quality care and nutritional and fluid
management standards.
One reason seems to be the haphazard and variable adoption of
the plethora of available and potentially confusing guidelines.
This suggests a need for central responsibility and
coordination of implementation, monitoring, and choice of the
most cost effective services. The second important issue has
been lack of appreciation, engagement, and education of
patients, carers, healthcare professionals, managers,
commissioners, and government executives about the importance
of nutrition and hydration in terms of healthcare outcomes,
service use, and NHS costs.
Delivery of quality, comprehensive, patient focused, nutritional
and fluid care requires a coordinated, uniform and monitored
approach from government, organisations, managers, clinical
staff, and the public (box 4). Communication between these
Subscribe: http://www.bmj.com/subscribe
BMJ 2013;346:f801 doi: 10.1136/bmj.f801 (Published 8 February 2013)
Page 4 of 5
ANALYSIS
groups should be clear and effective. Achieving these goals
requires change.
Central leadership and responsibility
The government must make adequate nutrition a priority for the
National Commissioning Board, as well as public health policies.
European health providers have committed to tackling these
problems, and the malnutrition task force in England is working
to ensure implementation of good nutritional care for all older
people.
Policy change and development
The new Health and Social Care Act is not clear how
cross-cutting clinical themes, like nutrition and fluid
management, should be addressed in national policy. This needs
to be corrected.
Clinical commissioning groups should consider appointing
executive leads responsible for good nutritional care. The British
Association for Parenteral and Enteral Nutrition (BAPEN) has
produced a toolkit for commissioners and providers to help them
deliver high quality nutritional care and fluid management
services.3
Professional bodies and other organisations
A coordinated approach from professional bodies and charities
is needed to implement a uniform, coordinated nutrition strategy.
BAPEN is working to facilitate this.
Implement current guidelines
Many guidelines exist to improve the quality of nutritional
care.1-3 5 Implementation of NICE nutrition guidance would save
clinical commissioning groups about 28 500/100 000
population every year.21 Various monitoring and audits systems
are available to enable organisations to document achievement
of key targets and key performance indicatorsfor example,
nutrition dashboards and the patient environment action teams
annual assessments.32
Senior clinicians and managers must take
responsibility
Perceived lack of interest of senior clinicians to engage with
nutritional issues often has a detrimental effect on the views of
the wider medical team. Nutrition and hydration should not be
delegated to junior clinicians. Teams must develop an approach
to dealing routinely with fluid management and nutritional care
on ward rounds despite competing demands. Simple measures
such as ward round checklists may improve fluid management
and nutrition.33
Identifying who is responsible and accountable for nutrition
and hydration at an organisational level is necessary but
challenging. It will involve coordination of different professional
groups, departments, and organisations. Many organisations do
not have senior clinicians or executives with responsibility for
nutrition and hydration. The emphasis on nutrition and hydration
must extend from board rooms and into the wards, clinics, and
community services.
Every trust should have reliable systems within its management
and governance frameworks to ensure delivery of high quality
nutrition and fluid management targets. This should include a
multidisciplinary nutrition support team that reports to a nutrition
steering committee. An identified senior clinician should act as
the trusts nutrition champion. The NICE quality standards
released in 2012 should facilitate delivery of better nutritional
For personal use only: See rights and reprints http://www.bmj.com/permissions
care, including the required nutrition screening and care planning
standards.34 NICE guidance and quality standards on intravenous
fluid prescribing are also due in 2013. Future development of
realistic and achievable key performance indicators may be
needed.
Education for staff, patients, and carers
Medical and nursing graduates need minimum levels of
competence in nutrition and fluid management, such as those
developed by the Academy of Medical Royal Colleges
Intercollegiate Group on Nutrition.34 Basic principles of
nutritional care and intravenous fluid prescription must be
embedded in general and specialty training programmes. Some
e-learning materials are already available. The Royal College
of Physicians has raised the importance of improving general
medical training on vital core medical competencies (including
fluid management and nutrition) that are often neglected in
current specialty training programmes.
In a busy ward environment it is easy to overlook the basic
requirements of humane, compassionate care. Staff should
ensure food and fresh drink are within easy reach and that
mealtimes are protected. Red trays can act as a visible indicator
to all staff of vulnerable or malnourished patients who need
additional support with eating and careful monitoring of food
intake. Relatives should be allowed access to the wards to help
at mealtimes when feeding is a problem.
The importance of educating patients and carers in optimal
nutrition is often overlooked and can be addressed at the bedside,
in consulting rooms, and through educational material such as
leaflets. Relatives often appreciate the opportunity to help with
this vital and intimate aspect of care.
Time to act
Now is the time to take fluid and nutrition seriously, not only
within hospitals but also in care homes and the community.
Failure to address these essential but often complex issues has
profound, often avoidable effects on morbidity and mortality
and results in unnecessary costs.
Contributors and sources: RML is a consultant physician and intensivist
and is a previous member and current chair of the RCP nutrition
committee. AB was a clinical dietitian and senior research fellow before
developing an interest in improvement science. MS is a senior lecturer
and consultant gastroenterologist and previous chair of BAPEN. He has
extensive experience in clinical nutrition, research, and guideline
development and has reported widely on implementation of good
nutritional care. RT is a professor and consultant gastroenterologist,
now president of the RCP. This article arose from discussions arising
at the RCP nutrition committee following high profile media reports of
failure to deliver appropriate standards of fluid management and
nutritional care in hospitals.
Competing interests: We have read and understood the BMJ Group
policy on declaration of interests and have no relevant interests to
declare.
Provenance and peer review: Not commissioned; externally peer
reviewed.
1
2
3
Elia M, Russell CA. Combating malnutrition; recommendations for action. A report from
the advisory group on malnutrition. BAPEN, 2009.
National Institute for Health and Clinical Excellence. Nutrition support in adults. Clinical
Guideline 32. 2006. http://guidance.nice.org.uk/CG32.
Brotherton A, Simmonds N, Stroud M, BAPEN Quality Group. Malnutrition matters. Meeting
quality standards in nutritional care. A toolkit for commissioners and providers in England.
2010. www.bapen.org.uk/pdfs/toolkit-for-commissioners.pdf.
Subscribe: http://www.bmj.com/subscribe
BMJ 2013;346:f801 doi: 10.1136/bmj.f801 (Published 8 February 2013)
Page 5 of 5
ANALYSIS
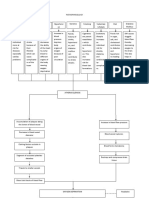
Box 4: How to improve nutritional and fluid management
Government
Include nutritional care in its mandate to the National Commissioning Board
Appoint a senior leader with overall responsibility for nutrition
Department of Health
Embed nutritional care into policy
Appoint a national clinical director for nutrition and hydration
Use the appropriate system levers to incentivise providerseg, national commissioning for quality and innovation targets
Regions and clinical commissioning groups
Appoint executive leads for nutrition
Take responsibility for commissioning nutritional care
Include in contracts and national targets
Acute trust and providers
Reliable systems, with nutrition steering committees and nutrition support teams
Education for all frontline staff
Ensure nutrition screening and planned care
Patients and public
Increased awareness of malnutrition
Self management
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
Guest JF, Panca M, Baeyens JP, de Man F, Ljungqvist O, Pichard C, et al. Health
economic impact of managing patients following a community-based diagnosis of
malnutrition in the UK. Clin Nutr 2011;30:422-9.
Patients Association. Malnutrition in the community and hospital setting. PA, 2011.
Bistrian BR, Blackburn GL, Vitale J, Cochran D, Naylor J. Prevalence of malnutrition in
general medical patients. JAMA 1976;235:1567-70.
McWhirter JP, Pennington CR. Incidence and recognition of malnutrition in hospital. BMJ
1994;308:945.
Russell CA, Elia M. Nutritional screening survey in the UK and Republic of Ireland 2011.
www.bapen.org.uk/pdfs/nsw/nsw-2011-report.pdf.
Stratton RJ, Green CJ, Elia M. Disease-related malnutrition: an evidence based approach
to treatment. CABI, 2003.
Sorensen J, Kondrup J, Prokopowicz J, Schiesser M, Krahenbuhl L, Meier R et al.
EuroOOPS: an international, multicentre study to implement nutritional risk screening and
evaluate clinical outcome. Clin Nutr 2008;27:340-9.
Parliamentary and Health Service Ombudsman. Care and compassion? Report of the
health service ombudsman on ten investigations into NHS care of older people. 2011.
www.ombudsman.org.uk/care-and-compassion.
Care Quality Commission. National report on dignity and nutrition. CQC, 2011. www.cqc.
org.uk/public/reports-surveys-and-reviews/themes-inspections/dignity-and-nutrition-olderpeople.
Age UK. Still hungry to be heard. The scandal of people in later life becoming malnourished
in hospital. Age UK, 2010.
Stechmiller JK. Understanding the role of nutrition and wound healing . Nutr Clin Pract
2010;25:61-8.
Marcos A, Nova E, Montero A. Changes in the immune system are conditioned by nutrition.
Eur J Clin Nutr 2003;57(suppl 1):S669.
Schneider SM, Veyres P, Pivot X, Soummer AM, Jambou P, Filippi J, et al. Malnutrition
is an independent factor associated with nosocomial infections. Br J Nutr 2004;92:105-11.
Walsh SR, Walch CJ. Intravenous fluid associated morbidity in postoperative patients.
Ann R Coll Surg Engl 2005;87:126-30.
Walsh SR, Cook EJ, Bentley R, Farooq N, Gardner-Thorpe J, Tang T, et al. Peri-operative
fluid management: prospective audit. Int J Clin Pract 2008;62:492-7.
Arieff AI. Fatal postoperative pulmonary edema: pathogenesis and literature review. Chest
1999;115:1371-7.
NHS Institute for Innovation and Improvement. High impact actions for nursing and
midwifery. 2009. www.institute.nhs.uk/images//stories/Building_Capability/HIA/NHSI%
20High%20Impact%20Actions.pdf.
21
22
23
24
25
26
27
28
29
30
31
32
33
34
NICE. Cost saving guidance. 2009. www.nice.org.uk/usingguidance/
benefitsofimplementation/costsavingguidance.jspwww.nice.org.uk/usingguidance/
benefitsofimplementation/costsavingguidance.jsp.
Powell AGMT, Paterson-Brown S. FY1 doctors still poor in prescribing intravenous fluids.
BMJ 2011;342:d2741.
Callum KG, Carr NJ, Gray AJG, Hargreaves CMJ, Hoile RW, Ingram GS, et al. The 2002
report of the national confidential enquiry into perioperative deaths. www.ncepod.org.uk/
pdf/2002/02full.pdf.
Rooker JC, Gorard DA. Errors of intravenous fluid infusion rates in medical inpatients.
Clin Med 2007;7:482-5.
Powell-Tuck Jeremy, Gosling P, Lobo DN, Allison SP, Carlson GL, Gore M, et al. British
consensus guidelines on intravenous fluid therapy for adult surgical patients. 2011. www.
bapen.org.uk/pdfs/bapen_pubs/giftasup.pdf.
Milne AC, Potter J, Vivanti A, Avenell A. Protein and energy supplementation in elderly
people at risk from malnutrition. Cochrane Database Syst Rev 2009;2:CD003288.
Elia M, Startton R, Russell C, Green C, Pang F. The cost of disease-related malnutrition
in the UK and economic considerations for the use of oral nutritional supplements. BAPEN,
2005.
National Patient Safety Agency. Reducing harm caused by the misplacement of nasogastric
feeding tubes. www.nrls.npsa.nhs.uk/resources/?entryid45=59794www.nrls.npsa.nhs.uk/
resources/?entryid45=59794
NCEPOD. Artificial nutrition enquiry report: a mixed bag. 2010.
www.ncepod.org.uk/2010pn.htm.
Tang VCY, Lee EWY, Fluid balance chart: do we understand it? Clin Risk 2010;16:10-3.
National Patient Safety Agency patient environment action teams (PEAT). 2010. http://
www.nrls.npsa.nhs.uk/patient-safety-data/peat/.
Royal College of Physicians, Royal College of Nursing. Ward rounds in medicine. 2012.
www.rcplondon.ac.uk/sites/default/files/documents/ward-rounds-in-medicine-web.pdf.
Soong J, Bravis V, Smith D, LeBall K, Levy J. Improving ward round processes: a pilot
medical checklist improves performance. Paris: International Forum on Quality and Safety
in Healthcare, 2012.
Academy of Medical Royal Colleges. UNEIG undergraduate curriculum . www.aomrc.org.
uk/committees/item/curricula.html.
Accepted: 1 December 2012
Cite this as: BMJ 2013;346:f801
BMJ Publishing Group Ltd 2013
For personal use only: See rights and reprints http://www.bmj.com/permissions
Subscribe: http://www.bmj.com/subscribe
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Barack Huessein Obama Is The Most Dangerous Man To Ever LiveDocument3 pagesBarack Huessein Obama Is The Most Dangerous Man To Ever LivetravisdannNo ratings yet
- Drugs & Cosmetics ActDocument70 pagesDrugs & Cosmetics ActAnonymous ibmeej9No ratings yet
- Failures in Periodontal Therapy: Review ArticleDocument6 pagesFailures in Periodontal Therapy: Review ArticlezinniaNo ratings yet
- Pharmacy Math CalculationsDocument8 pagesPharmacy Math CalculationsRahmawati KuswandiNo ratings yet
- Recurrent Gingival Cyst of Adult: A Rare Case Report With Review of LiteratureDocument5 pagesRecurrent Gingival Cyst of Adult: A Rare Case Report With Review of Literaturesayantan karmakarNo ratings yet
- Drug Hypersensitivity & Drug Induced DiseasesDocument23 pagesDrug Hypersensitivity & Drug Induced DiseasesBella100% (1)
- Hospital ICU Organization and TypesDocument82 pagesHospital ICU Organization and TypesPaul Shan GoNo ratings yet
- Mu 089Document4 pagesMu 089Rahul RaiNo ratings yet
- Blessing IwezueDocument3 pagesBlessing Iwezueanon-792990100% (2)
- Antibacterial and Antifungal Activities ofDocument6 pagesAntibacterial and Antifungal Activities ofSamiantara DotsNo ratings yet
- Pathophysiology Tia VS CvaDocument6 pagesPathophysiology Tia VS CvaRobby Nur Zam ZamNo ratings yet
- A Study of Demographic Variables of Violent Asphyxial Death: JPAFMAT, 2003, Vol.: 3 ISSN - 0972 - 5687Document4 pagesA Study of Demographic Variables of Violent Asphyxial Death: JPAFMAT, 2003, Vol.: 3 ISSN - 0972 - 5687Reza ArgoNo ratings yet
- Kayachikitsa Paper 1 PDFDocument24 pagesKayachikitsa Paper 1 PDFMayura JainNo ratings yet
- Anggi Retno Wardani - 40121064Document91 pagesAnggi Retno Wardani - 40121064febyNo ratings yet
- Reversal of Fortune: The True Story of Claus von Bülow's Conviction and Alan Dershowitz's Innovative DefenseDocument9 pagesReversal of Fortune: The True Story of Claus von Bülow's Conviction and Alan Dershowitz's Innovative Defensetamakiusui18No ratings yet
- Bioactive Compounds in Phytomedicine BookDocument228 pagesBioactive Compounds in Phytomedicine BookAnil KumarNo ratings yet
- Hospital List 06052016Document5 pagesHospital List 06052016Azhar ThireiNo ratings yet
- SOCA Blok 12Document21 pagesSOCA Blok 12safiraNo ratings yet
- Guppy Brain Atlas SmallerDocument4 pagesGuppy Brain Atlas Smallerapi-394354061No ratings yet
- Minha Biblioteca Catalogo Julho 2022 Novos TitulosDocument110 pagesMinha Biblioteca Catalogo Julho 2022 Novos TitulosMarcelo SpritzerNo ratings yet
- Klinefelter SyndromeDocument6 pagesKlinefelter Syndromemeeeenon100% (1)
- Gold Foil: Safety Data SheetDocument4 pagesGold Foil: Safety Data SheetSyawatulshuhada SyawalNo ratings yet
- The Herbal Market of Thessaloniki N GreeDocument19 pagesThe Herbal Market of Thessaloniki N GreeDanaNo ratings yet
- VMC Customer Service Complaint and Letter of DemandDocument3 pagesVMC Customer Service Complaint and Letter of DemandJames Alan BushNo ratings yet
- Siddha Therapeutic Index - 18-Article Text-133-1-10-20210308Document7 pagesSiddha Therapeutic Index - 18-Article Text-133-1-10-20210308Dr.kali.vijay kumkarNo ratings yet
- Datex-Ohmeda Aespire 7900 - Maintenance and Troubleshooting PDFDocument118 pagesDatex-Ohmeda Aespire 7900 - Maintenance and Troubleshooting PDFJosé Morales Echenique100% (1)
- Anaesthesia - 2020 - Griffiths - Guideline For The Management of Hip Fractures 2020Document13 pagesAnaesthesia - 2020 - Griffiths - Guideline For The Management of Hip Fractures 2020BBD BBDNo ratings yet
- Pharmacology For Nurses by Diane Pacitti Blaine T. SmithDocument570 pagesPharmacology For Nurses by Diane Pacitti Blaine T. SmithJessica Anis0% (1)
- Medic Alert Short BrochureDocument2 pagesMedic Alert Short BrochureDerek DickersonNo ratings yet
- Breast Assessment Learning ObjectivesDocument6 pagesBreast Assessment Learning Objectivesalphabennydelta4468No ratings yet