Professional Documents
Culture Documents
7 Extra Trauma
Uploaded by
Amr SabryCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
7 Extra Trauma
Uploaded by
Amr SabryCopyright:
Available Formats
TRAUMA
37
Golden hour
Role of anesthesiologists in trauma
Permissive hypotension (hypotensive
resuscitation)
Patient trauma severity scores
Management of trauma patient (anesthetic and
intensive care management)
Compartmental syndrome
Airway trauma (compromised airway)
Anesthesia for mass casualty and disaster
situations
Trauma is the leading cause of death in ages from 1 to 35 year old. Trauma is classified into:
a- Penetrating trauma.
b- Blunt trauma, which is associated with more mortality rates due to:
Difficult diagnosis.
Frequent association with more than one organ injury e.g. head injury, chest trauma, and fractures
with abdominal injury.
Golden Hour
Deaths from trauma occur either:
Early (80% of deaths): 50% of deaths occur immediately and
30% of deaths occur within the first few hours of injury.
The causes of death in the early group (during the first hour) are preventable, if proper management is
applied. It is named golden hour i.e. the time elapsing between an injury and definitive surgical care.
Therefore, the first hour of injury decreases the mortality rates from trauma markedly.
Late (20% of deaths).
Role of Anesthesiologists in Trauma
The anesthesiologist is a critical member of the trauma team and must be available 24 hours a day to take
care of severely traumatized patients from the moment that the patient arrives at the emergency
department of the trauma center. Anesthesiologist can provide:
the initial resuscitation.
anesthesia for surgical treatment.
Permissive Hypotension (Hypotensive Resuscitation)
Definition: It is the hypothesis that fluid resuscitation should be delayed until surgical control of
hemorrhage has taken place. This concept is applied in the treatment of hypotensive trauma patients.
Value: The administration of large volumes of intravenous fluids (aggressive fluid treatment) prior to
surgical control of bleeding is felt by some to be potentially deleterious because:
It increases arterial blood pressure (even up to normotensive pressure) and vessel diameter.
It decreases blood viscosity.
It dilutes platelets and clotting factors.
These actually will promote further blood loss increasing the mortality in severe uncontrolled
hemorrhage e.g. ruptured abdominal aortic aneurysm or penetrating truncal injury. Therefore, it is
accepted now to obtain lower than normal mean blood pressure until surgical control of hemorrhage is
achieved within 1 hour. During permissive hypotension, the usual resuscitation is employed e.g. vascular
access...etc. After effective surgical hemorrhage control, rapid warmed fluid loading is established to
restore organ perfusion.
Contraindications: Permissive hypotension is not allowed in shocked multiple trauma patients with
head injuries because the preservation of cerebral perfusion pressure to prevent secondary brain injury
by ischemia is the vital goal. Therefore, early operative intervention to stop hemorrhage and simultaneous
volume replacement to achieve normovolemia and normotension are required.
N.B.: Permissive Managements in Anesthesia: includes
1485
SAFE ANESTHESIA & INTENSIVE CARE
37
1486
Permissive hypotension: as above.
Permissive hypertension, permissive hypervolemia, and permissive hemodilution: are
discussed in HHH therapy in management of subarachnoid hemorrhage in chapter Central
Nervous Diseases.
Permissive hypoxia: is discussed during management of chronic obstructive pulmonary disease.
Permissive hypercarbia: is discussed during management of acute respiratory distress syndrome
(ARDS). Both are discussed in chapter of Respiratory Diseases.
Permissive hypothermia: is discussed in chapter of Cardiac Surgery.
There is no permissive hyperthermia because it is very harmful to the brain.
Patient Trauma Severity Scores
There are three main groups of trauma scores:
1- Anatomical Scores: they includes
a- Abbreviated Injury Scale (AIS).
b- Injury Severity Score (ISS).
c- New Injury Severity Score (NISS).
2- Physiological Scores:
a- Glasgow Coma Score (GCS).
b- Trauma Score (TS).
c- Revised Trauma Score (RTS).
d- Acute Physiology and Chronic Health Evaluation (APACHE).
e- Pediatric Trauma Score (PTS).
f- Glasgow Pediatric Coma Score (GPCS).
3- Combined Scoring System:
Trauma and Injury Severity Score (TRISS).
1- Anatomical Scores
a- Abbreviated Injury Scale (AIS):
The AIS was originally designed to stratify victims of motor vehicle crashes. Only blunt injuries were
included in the first AIS.
Disadvantages: It is unable to predict mortality or outcomes.
It is not a true scale.
1
Minor
2
Moderate
3
Serious
4
Severe
5
Critical
6
Unsurvival
b- Injury Severity Score (ISS):
It is the sum of the squares of the single highest abbreviated injury score (AIS) in each of the three most
severely injured body regions. The body is classified into six regions (head, face, chest, abdomen,
extremities including pelvis, and external structures). ISS ranges from 1 to 75, ISS less than 25 is a minor
risk, 25 to 50 is a moderate risk, 50 to 75 is a high risk.
Disadvantages: It limits total number of contributing injuries to three regions.
It considers at most one injury per body region. Multiple severe injuries in one region
takes no account for physiological variables.
It gives equal weight to each body region.
c- New Injury Severity Score (NISS)
It is a modified ISS. It is defined as the sum of the squares of the abbreviated injury scale. It is
considered the best anatomical scoring system as it considers the severity rather than the site.
For example: a patient has a motor car accident. After history, examination, and investigations, the patient
was complaining of cut wound in the face, small bowel perforation, liver laceration, and bladder
perforation in the abdomen, and fracture femur in the lower limb.
Organ
Score by ISS
Score by NISS
Score by
Lesion
Affected
AIS
Highest score Square
Highest score Square
Face
Cut wound
2
2
4
TRAUMA
37
Abdomen
Lower Limb
Small bowel perforation
Liver laceration
Bladder perforation
Fracture femur
2
3
4
3
Total 4/6
4
16
3
9
Total 29/75
3
4
3
9
16
9
Total 34/75
2- Physiological Scores
a- Glasgow Coma Score (GCS):
It is discussed in more details in chapter Central Nervous Diseases.
b- Trauma Score (TS):
Parameter
Glasgow Coma
Scale
Systemic Blood
Pressure (mmHg)
Respiratory Rate
(Per Minute)
Capillary Refill
Respiratory
Expansion
Degree
14-15
10-13
8-9
5-7
3-4
> 90
70-89
50-69
0-49
No pulse
10-24
25-35
> 36
1-9
None
Normal
Delayed
None
Normal
Restrictive
Total
Score
4
3
2
1
0
4
3
2
1
0
4
3
2
1
0
2
1
0
1
0
0-15
c- Revised Trauma Score (RTS):
It is modified trauma score where it includes only Glasgow coma scale, systolic blood pressure, and
respiratory rate. The range of the score is from 0-12. a score less than 11 is an indication for transfer to a
dedicated trauma center.
Disadvantages: Problems with GCS in intubated patients.
Influence of alcohol and drugs changing physiological parameters with resuscitation.
d- Acute Physiology and Chronic Health Evaluation (APACHE):
It is discussed later in chapter of Intensive Care. It provides guidance about the clinical course of a
patient.
Disadvantage:
APACHE underestimates the likelihood of death in patients who are transferred to intensive care unit
(ICU) after relative stabilization, as it uses intensive care data only and does not account for prior
treatment/resuscitation.
APACHE was developed in mainly non-trauma ICU patients who had different clinical problems.
e- Pediatric Trauma Score (PTS):
It depends on the following variables: weight (kg), systolic blood pressure (mm Hg), mental status,
airway, skeletal affection, and open wounds. Each variable takes a value +2, +1, and -1. The score ranges
from -6 to +12. Above +8 is considered a minor trauma while below 0 is a severe one.
f- Glasgow Pediatric Coma Score:
It is discussed in details in chapter Central Nervous Diseases.
3- Combined Scoring System
Trauma and Injury Severity Score (TRISS):
1487
SAFE ANESTHESIA & INTENSIVE CARE
37
1488
It combines both anatomical and physiological measures of injury severity i.e. it combines both ISS, and
RTS, in addition to patients age. TRISS predicts probability of survival using certain formula.
Disadvantages: It includes the disadvantages of both ISS and RTS.
It takes no account of pre-existing medical conditions.
Management of Trauma Patient
(Anesthetic and Intensive Care Management)
Preoperative Management
A) Primary Survey (Initial Resuscitation):
It includes A, B, C, D, and E sequence of cardiopulmonary resuscitation. These letters indicate Airway,
Breathing, Circulation, Disability, and Exposure. They are not Accuse, Blame, Criticize, or Delay.
1- Airway:
a- Basic Techniques:
Securing airway should be managed as follows:
Chin lift-jaw thrust maneuver.
Neck lift-head tilt maneuver.
Both maneuvers are discussed in chapter of Airway Management.
Sweep out vomitus or foreign bodies visible in the mouth by the index finger in unconscious
patients only (placing a finger in the mouth of a conscious or convulsing patient is not recommended).
Heimlich maneuver:
If the patient is conscious and/or the foreign body cannot be removed by a finger sweep. Removal of
the foreign body can be done while the patient is standing or lying down by a sub-diaphragmatic
abdominal thrust, which elevates the diaphragm expelling a blast of air from the lungs that displaces
the foreign body (figure 37-xxxxxxxxxx).
Complications: Rib fracture.
Trauma to the internal viscera.
Regurgitation.
N.B.: In infants, a combination of back blows and chest thrusts are done.
Figure 37-xxx: Heimlich maneuver can be performed with the victim
Standing (A) or lying down (B)
b- Advanced Techniques:
Suction of blood or secretions from the mouth.
Oropharyngeal or nasopharyngeal airway.
Intubation especially of unconscious patients who are at risk of aspiration.
Combi-tube.
Laryngeal mask airway.
Esophageal obturator or esophageal gastric tube airway.
Tracheostomy with local anesthesia.
Emergency cricothyrotomy for acute obstruction of upper airway.
TRAUMA
37
The above techniques are discussed in details in chapter of Airway Management.
Signs of airway obstruction should be examined (see later). Simply, if a patient can talk the airway is
usually clear.
Additional Care: should be directed to:
Cervical spine fracture (even if there is no known injury). It occurs in 1.5-3% of all major trauma
victims and in 10% of severe head injury. Cervical spine fracture should be suspected by history (as in
alert patient, it often produces neck pain, tenderness, or any neurological symptoms), neck x-ray, or CT
scan. Avoid neck hyperextension and intubation should be with in-line immobilization. Apply neck
stabilization by sandbags, forehead tape, or neck collar. Cervical spine fracture and instability is
discussed in chapters of Airway Management and Central Nervous Diseases.
Other vertebral fractures should be suspected. Care should be taken during patient transportation.
The patient should be transported in one line (figure 37-XXXXXXXXX).
Figure 37-XXXXX: Patient transportation
Mid-face or basilar skull fractures: avoid nasal intubation or nasopharyngeal airways.
2- Breathing:
a- Basic Techniques:
It is assessed by look, listen, and feel approach.
Look for chest wall movement, cyanosis, use of accessory muscles, flail chest, paradoxical abdominal
movement (indicates airway obstruction), and penetrating chest injuries, any bruises, ecchymoses.
Listen for the presence, absence, or diminution of breath sounds.
Feel for airflow, subcutaneous emphysema, tracheal shift, and broken ribs.
Breathing is maintained with oxygenation and cricoid pressure (controversy).
Mouth-to-mouth or mouth-to-mask (mouth-to-barrier device) ventilation may be needed during
cardiopulmonary resuscitation. It is discussed in chapter of Cardio-pulmonary Resuscitation.
Pneumothorax and hemothorax should be suspected in trauma patients.
b- Advanced Techniques:
A self-inflating bag with a non-rebreathing valve connected to a facemask or an endotracheal tube.
Mechanical Ventilators.
Patients with suspected head trauma need hyperventilation to decrease intracranial pressure.
3- Circulation:
Assessment and management of hypovolemic shock is discussed in chapter of Cardiovascular
Diseases.
4- Disability:
Evaluation for disability consists of a rapid neurological assessment such as pupil examination.
Because there is usually no time for a Glasgow coma scale, the AVPU system is used; Awake, Verbal
response, Painful response, and Unresponsive.
5- Exposure:
The patient should be undressed to allow examination for injuries allover the body and should be
covered by a warming blanket.
In-line immobilization should be used if a neck or spinal cord injury is suspected.
B) Secondary Survey (Later Assessment):
In the secondary survey, the patient is evaluated from head to toe and the indicated studies (e.g.
radiographs, laboratory tests, invasive diagnostic procedures) are obtained.
1489
SAFE ANESTHESIA & INTENSIVE CARE
37
1490
1- Assessment of the Injury and Other Associated Injuries:
This is usually done by a specialist by history, examination, and investigations such as:
A general surgery specialist for abdominal injury.
A neurosurgery specialist for head and spinal cord injury.
A cardio-thoracic specialist for chest injury.
An orthopedic specialist for bone fractures.
They determine the surgical diagnosis and the type of the surgery needed. They are essential to be
determined as they dictate the extent of preoperative preparations and methods of anesthesia.
Common Investigations Requested include:
1- X-rays for chest, vertebral column, skull, pelvis, and long bones.
2- Whole body CT scan is recommended in all patients with major chest trauma to detect:
lung contusions, acute respiratory distress syndrome, bronchial rupture.
Blunt aortic injury.
Spinal injury.
Abdominal injury.
3- Peritoneal lavage.
4- A focused assessment with sonography for trauma (FAST) scan is a rapid bedside, ultrasound
examination performed to identify intra-peritoneal hemorrhage or pericardial tamponade. The FAST
scan, which has become an extension of the physical examination of the trauma patient, examines three
areas for free fluids: Peritoneum: perihepatic/hepatorenal space, perisplenic space, and pelvis.
Pericardium.
Pleura.
FAST scan is indicated for all hemodynamically unstable blunt trauma patients.
5- Echocardiography.
6- Transcranial Doppler in head trauma. A cerebral perfusion pressure > 70 mm Hg should be a
resuscitation endpoint in brain-injured patients.
7- ECG (see below).
8- Cardiac enzymes (see below).
2- Assessment of the Past Medical Condition: (by history, examination, and investigations).
It is usually taken from the relatives (if the patient is a child or comatosed).
3- Airway Assessment for Difficult Intubation: Especially in cases of head and face trauma
(airway trauma).
4- Assessment of Aspiration:
All trauma patients must be considered as having a full stomach as gastric emptying stops at the time
of significant trauma due to fear, pain, shock, opioidsetc. Therefore, in all trauma patients, the time
interval between ingestion of food and the accident is a more reliable index of the degree of gastric
emptying than the period of fasting (figure 37-xxxxx).
Precautions against aspiration should be taken such as an oro-gastric tube, antacids, and H2 blockers.
They are discussed in details in chapter of Respiratory Diseases.
Less important
More important
Time
Time of
Time of
Time of
food intake
trauma
surgery
figure 37-xxxxxxxxxxxx: Time interval for food ingestion
5- Premedications:
1- Sedatives are better avoided.
2- Prophylaxis against aspiration.
3- O2 by a facemask.
C) Tertiary Survey:
Definition:
TRAUMA
37
It is a patient evaluation that identifies and catalogues all injuries after initial resuscitation and operative
interventions. It is typically occurs within 24 hours of injuries.
Advantages of Delayed Evaluation:
It avoids missed injuries because between 2% and 50% of traumatic injuries may be missed by primary
and secondary surveys, particularly following blunt multiple traumas (e.g. car accident).
The patient is more awake that allow better communication and expression of all complaints.
More detailed information on the mechanism of injury is obtained.
More detailed examination of the medical record is allowed to determine preexisting co-morbidities.
Method:
Tertiary survey includes another head-to-toe examination and a review of all laboratory and imaging
studies. The usual missed injuries include pelvic fractures, spinal cord injuries, abdominal injuries, and
peripheral nerve injuries.
Intraoperative Management
Try to postpone surgery as much as possible to allow proper preoperative resuscitation before the
induction.
Monitoring:
They should be applied before induction of anesthesia. They include the standard monitors, in addition
to: Urine output by Foleys catheter and urinometer.
Temperature (core and skin).
Central venous pressure, pulmonary artery pressure, and invasive arterial blood pressure monitors
are chosen according to the patients condition and the type of surgery.
Arterial blood gases.
Blood sample is send to the laboratory to monitor hematocrit and coagulation.
Choice of Anesthesia:
A) Regional Anesthesia:
It is usually impractical in hemodynamically unstable patients e.g. brachial plexus block, i.v. regional
anesthesia, subarachnoid or spinal block.
B) General Anesthesia:
Induction:
If the patient is unconscious, intubation should be done by a paralyzing dose of suxamethonium only.
If the patient is conscious,
Rapid sequence induction (with cricoid pressure; a controversy is present about its value). It is
discussed in chapter of The Practice Conduct of Anesthesia.
Inhalational induction, it is used if there is doubt about controlling the airway e.g. maxillofacial
trauma. Guard against aspiration by putting the patient in the lateral or supine position with cricoid
pressure.
Awake Intubation (fiberoptic intubation), it is of choice in patients who are likely to develop unrelievable airway obstruction when loss of consciousness occurs e.g. trismus from dental abscess and
angio-neurotic edema. It is discussed in chapter of Airway Management.
Maintenance:
As usual with the following precautions:
The usual precautions for hypovolemic shocked patients such as opioid-based anesthesia.
Drugs as ketamine and N2O indirectly stimulate cardiac function in normal patients. They can
display cardio-depressant effects in shocked patients who already have maximal sympathetic
stimulation. N2O is avoided by some anesthesiologists for this cause. It is also avoided to increase FiO2
and the possibility of pneumothorax in trauma patients.
The choice of non-depolarizing muscle relaxants depends on the patients condition e.g.
pancuronium increases the heart rate; therefore, it is the best in hypovolemic patients, but not in
ischemic patients.
Recovery:
Awake extubation is indicated in the lateral position.
After airway and maxillo-facial surgeries, the patient is left intubated usually for several days due to
airway edema.
Postoperative Management
1- Postoperative pain relief.
1491
SAFE ANESTHESIA & INTENSIVE CARE
37
1492
2- Postoperative complications e.g. hypothermia, disseminated intravascular coagulopathy (DIC), or
acute respiratory distress syndrome (ARDS).
3- Postoperative prophylactic (elective) ventilation is indicated in:
Prolonged shock (hypoperfusion) state of any cause.
Massive sepsis e.g. focal peritonitis, cholangitis, or septicemia.
Severe ischemic heart disease.
Extreme obesity.
Overt gastric acid aspiration.
Previously severe pulmonary disease.
Special Management in Severely Traumatized Patient
1- Hypovolemic shock
It is one of the major causes of death in trauma. It is discussed in chapter of Cardiovascular Diseases.
2- Head Trauma
It is discussed in chapter of Central Nervous Diseases.
3- Spinal Cord Trauma
It is discussed in chapter of Central Nervous Diseases.
4- Chest Trauma
Thoracic injuries may result from either direct trauma (blunt or crush) or indirect trauma (deceleration or
blast). Thoracic injuries are classified according to the Organ Injury Scaling (OIS)
Degree
Description
A) Chest wall OIS:
III (moderate injury)
Flail sternum or
Unilateral flail segment (< 3 ribs)
IV (severe injury)
Avulsion of chest wall tissues with underlying rib fractures or
Unilateral flail chest (> 3 ribs)
V (massive injury)
Bilateral flail chest (> 3 ribs on both sides)
B) Diaphragm OIS
III (moderate injury)
Laceration 2-10 cm
IV (severe injury)
Laceration > 10 cm with tissue loss < 25 cm2
V (massive injury)
Laceration with tissue loss > 25 cm2
C) Pulmonary (Lung) OIS
III (moderate injury)
Unilateral contusion (one lobe).
Laceration with persistent (72 hours) airleak from distal airway.
Non-expanding intra-parenchymal hematoma.
IV (severe injury)
Segmental or lobar laceration with major airleak.
Expanding intra-parenchymal hematoma.
Primary branch intra-pulmonary vessel disruption
V (massive injury)
Hilar vessel disruption.
VI (lethal injury)
Total uncontained transection of pulmonary hilum.
D) Heart OIS
III (moderate injury)
Blunt cardiac injury with sustained (> 5 beats/min) or multi-focal
ventricular contraction, septal rupture, pulmonary or tricuspid
regurgitation, papillary muscle dysfunction or distal coronary arterial
occlusion without cardiac failure.
Blunt cardiac injury with cardiac failure
Blunt pericardial laceration with cardiac herniation.
IV (severe injury)
Blunt cardiac injury with sustained (> 5 beats/min) or multi-focal
ventricular contraction, septal rupture, pulmonary or tricuspid
regurgitation, papillary muscle dysfunction or distal coronary arterial
occlusion producing cardiac failure.
Blunt cardiac injury with aortic or mitral valve regurgitation.
V (massive injury)
Blunt cardiac injury with proximal coronary arterial occlusion.
VI (lethal injury)
Blunt avulsion of the heart.
TRAUMA
37
F) Thoracic vessel OIS
III (moderate injury)
IV (severe injury)
V (massive injury)
VI (lethal injury)
Carotid, innominate, or subclavian artery,
Thoracic descending aorta, intra-thoracic inferior vena cava, primary intraparenchymal branch of pulmonary artery or vein.
Thoracic ascending aorta or aortic arch, superior vena cava, main trunk of
pulmonary artery or vein.
Uncontained total transection of thoracic aorta or pulmonary hilum.
Specific Conditions in Chest Trauma:
In addition to the above OIS:
1- Rib Fractures and Flail Chest:
Rib fractures occur in 50-70% of patients with blunt chest trauma while flail chest occur in 5-13% of
patients with blunt chest trauma.
Flail chest is defined by the fracture of > 3 adjacent ribs at two or more points, such that the involved
segment can move independently and paradoxically from the remaining chest wall.
2- Lung Contusion:
Definition: a disruption of alveolar capillary integrity resulting in intra-alveolar hemorrhage and edema.
Incidence: 17-26% of patients with blunt chest trauma.
Causes: Post-traumatic atelectasis.
Inhalation of gastric contents or blood.
Lung collapse due to compression by pneumothorax or hemothorax.
Effects: lung contusion causes:
Reduced surfactant production, which decreases lung compliance, leading to ventilation-perfusion
mismatch.
Increased circulating inflammatory mediators, which cause a regional capillary leak, affecting nontraumatized areas of the lung.
Acute lung injury in 30-80% of patients.
3- Acute Respiratory Distress Syndrome (ARDS).
4- Pneumothorax, tension pneumothorax, and hemothorax.
5- Esophageal rupture.
6- Myocardial Contusion (Blunt Cardiac Trauma or Injury):
It is characterized by hemorrhagic infiltrate, coronary artery injury, and tissue edema, usually observed in
the anterior, apical, or basal part of the heart. It includes also intra-atrial or intra-ventricular septal or
valvular rupture. Chest pain is common, which resembles angina pectoris, but is not relieved by
nitroglycerin.
Investigations:
ECG (ST-T wave abnormalities, arrhythmias, and heart block). It should be done at admission and
repeated between 6 and 12 hours after admission and it should be as clinically indicated. It is neither
sensitive nor specific for the diagnosis of blunt cardiac injury, but it is the best screening test available in
the emergency room for cardiac contusion. It correlates with severe cardiovascular complications.
Trans-thoracic or trans-esophageal echocardiography may show impaired ventricular wall motion,
valve regurgitation, and pericardial effusion.
Cardiac enzymes: the creatine kinase (CK) muscle band (MB)-isoform lacks specificity as it increases in
both cardiac and peripheral muscle trauma, in addition to liver, pancreas, lung, and colon trauma (i.e.
poly-traumatized patients). The cardiac isoform of troponin-I is never present in skeletal muscle. It is a
specific test of myocardial injury. A plasma level of cardiac troponin-I > 0.4 g/L corresponds to a
significant myocardial injury. In trauma patients, 3 troponin-I release profiles have been identified:
A very transient (< 12 hours) and limited release (peak < 2 g/L).
A transient (< 36 hours) and significant release (peak > 2 g/L).
A sustained (> 36 hours) and significant release (peak > 2 g/L).
7- Pericardial Trauma:
Severe chest wall trauma may cause pericardial-pleural tears that may result in cardiac herniation and
strangulation. Sometimes, bowel herniates into the pericardial sac or the heart herniates into the abdomen
(if the diaphragm is also injured).
Small herniations may cause impaired cardiac filling, impaired coronary blood flow, idiopathic
pericarditis with/without pericardial tamponade. Large herniations may cause strangulation of the heart
(with impairment of ventricular filling and hemodynamic instability).
Chest x-ray or CT may be needed.
1493
SAFE ANESTHESIA & INTENSIVE CARE
37
1494
Treatment: maintaining of cardiac output with fluids and inotropes.
emergency thoracotomy in large herniations.
Primary, secondary, and tertiary surveys are performed as above.
5- Abdominal Trauma
The following trauma may be present:
Wound of penetrating injury (usually).
Peritoneal irritation causing muscle guarding and tenderness on percussion.
Splenic rupture, liver, or kidney injury causing severe hemorrhage.
Large vessel injury (figure 37-xxxxxxxx).
X-ray abdomen shows free air.
Figure 37-xxxxxxxxxx: Inferior vena cave injury
Peritoneal lavage (Paracentesis): It is a procedure performed in the emergency room to help
determine if a patient has internal bleeding. A mini-laparotomy under local anesthesia is done. A
catheter is then placed into the abdomen and is aspirated for gross blood. If < 20 mL of blood are
aspirated, then 1 liter of lactated ringers solution or normal saline is allowed to drain into the
abdomen. The lavage fluid is then allowed to return by gravity and it is sent to the laboratory for
analysis. Criteria for a positive peritoneal lavage include:
An erythrocyte count of 100 000/mm3.
A white blood cell count of 5000/mm3.
The presence of bile or food particles.
A fluid amylase concentration of 175 u/dL.
If the peritoneal lavage meets one or more of these criteria, then the patient comes to the operating room
for an exploratory laparotomy. The preferred sites are as in the figure (figure 37-xxxxxx) with avoiding
old surgical scars.
TRAUMA
37
Figure 37-xxxxxxx: Preferred sites for abdominal Paracentesis
Search in the net
6- Extremity Traumas
The following trauma may be present:
Vascular injury usually causes massive hemorrhage e.g. femoral fractures may be associated with
1500 mL of occult blood loss.
Dislocations; care is taken during positioning.
Neurovascular bundle injury; care is taken during positioning.
Long bone and pelvis fractures may cause fat embolism leading to respiratory insufficiency.
Microvascular re-implantation surgeries may be needed.
Compartmental syndrome (see later).
7- Burn It is discussed in chapter of Plastic Surgery.
8- Airway Trauma see below.
Compartmental Syndrome
Definition: It is elevated interstitial pressure within a myo-fascial compartment, which compromises
capillary perfusion i.e. impaired tissue perfusion and, hence, neuro-muscular function. It can be chronic
or acute, but only the acute syndrome is limb- and, occasionally, life-threatening.
Normal compartmental pressure is below 30 mm Hg.
Compartmental syndrome pressure is between 30-60 mm Hg.
Complicated compartmental syndrome pressure (associated with neuro-muscular death) is higher
than 60 mm Hg.
Differential pressure = Diastolic pressure- compartment pressure.
When the differential pressure becomes less than 30 surgical fasciotomy is indicated.
Pathophysiology:
The elevated pressure is usually due to either:
Interstitial edema caused by mechanical or ischemic injury.
Bleeding.
It can occur in the buttock, thigh, foot, forearm, and hand. The most common site is the leg because its
muscle bulk is large and its fascial compartments are relatively small and non-compliant.
Causes:
Long bone fractures or crush injuries.
Re-establishment of perfusion after acute ischemia.
Muscle contusion.
Iatrogenic e.g. tightly applied cast.
Predisposing Factors:
Malignant hyperthermia.
Neuroleptic seizures.
Tetany.
Profound shock with massive edema.
Clinical Picture: (for conscious patients)
Pain and tenderness: The pain is severe, progressively increasing, and out of proportion to what is
expected for the condition. Pain is induced or exacerbated by passive stretch of the muscles in that
compartment.
Hypoesthesia and weakness: They are secondary to compression of the sensory nerves in that
compartment.
Finally the compartment is tense and tender on palpation.
Loss of pulse or capillary refill occurs late in the compartmental syndrome and is indicative of
extensive neuro-muscular damage.
N.B.: Epidural analgesia may mask the signs and delay the diagnosis.
Investigations:
1- Nerve conduction studies: they are accurate, but require highly trained individuals, and falsepositive results are seen in those patients with primary nerve injuries.
2- Direct measurement of compartment pressure: It is the most practical and widely used objective test
by using a strain gauge transducer-amplifier attached to a monitor.
All 4 leg compartments should be assessed quickly and repeatedly.
Management:
1495
SAFE ANESTHESIA & INTENSIVE CARE
37
1496
Preoperatively, all constrictive dressings to the leg should be removed. The leg should not be
elevated as elevation can worsen arterial inflow.
Surgical fasciotomy: It should remove all the potentially constricting layers of soft tissue around the
swollen muscle groups to relieve compartmental hypertension, assure that arterial perfusion is
adequate, and debride all obviously necrotic muscle. The fascia is the most constricting layer, and
complete incision of the fascia is the most important step. Complete incision of the skin may also be
necessary, as the skin may be constricting as well.
Technique: A medial calf incision to decompress the superficial and deep posterior compartments.
A lateral incision to decompress the anterior and lateral compartments.
After fasciotomy,
The wound should be left open and covered with moist, sterile dressings.
The leg should be elevated and passive range of motion started.
Wounds usually can be closed in a week, either primarily or with split-thickness skin graft.
Immediate amputation is life-saving after fasciotomy, if the patient develops metabolic sequelae of
massive myo-necrosis (metabolic acidosis, hyperkalemia, and myoglobinuria).
Complications: (of neglected cases)
1- Ischemic neuropathy.
2- Rhabdomyolysis: it is characterized by:
Myo-necrosis and fibrosis resulting in contractures.
Permanent loss of function can occur and persistent pain, weakness, and parasthesia can lead to late
amputation.
Hyperkalemia due to release of large amounts of intracellular K+ leading to arrhythmias and cardiac
arrest.
Hyperphosphatemia.
Metabolic acidosis.
Increased creatine kinase levels.
Myoglobinemia occurs with a peak 3 hours after circulation is restored. Myoglobinuria may occur
and causes tea-colored urine.
Treatment of rhabdomyolysis:
Urine output should be 100 mL/min by aggressive i.v. volume resuscitation and mannitol.
Alkalinization of the urine to 6.5 by NaHCO3 to avoid precipitation of myoglobin is beneficial.
Treatment of hyperkalemia is performed by i.v. glucose and insulin, Ca++, NaHCO3, and even
dialysis.
3- Severe shock can occur with the reperfusion of dead or severely compromised muscles as above.
4- Renal failure: due to myoglobinemia and severe shock.
Airway Trauma (Compromised Airway)
Types of Trauma
a- Penetrating Trauma: such as
Shotgun wounds, which cause apparent severe damage of the face.
Bullet wounds, which cause apparent minimal external damage, but with more severe internal
damage e.g. facial fractures or airway edema.
b- Blunt (Crush) Trauma: such as
A blow to the mid-face: it generates an abnormal shearing force leading to fracture of the facial
skeleton and may extend to the base of the skull, but away from the cranial skeleton.
A blow to the mandible: it may cause fracture mandible, but the force of the blow will be
redistributed and the fracture line will not extend into the skull.
Types of Fractures
A) Facial Fractures (Mid-Face):
In 1901, Rene Le Fort studied facial fractures and showed:
There is no relationship between the degree of soft tissue damage of the face and the underlying
facial fractures as an extensive soft tissue trauma may not be accompanied by several facial fracture,
and vice versa, a minor soft tissue trauma may cover severe facial fractures (figure 37-xxxxxx).
TRAUMA
37
1497
Figure 37-xxxx: A patient with facial trauma without any facial fracture
He determined the common lines of fractures of the mid-face as follows (figure 37-xxxxxxxxxxxx):
The Le Fort I Fracture
The Le Fort II Fracture
The Le Fort III Fracture
(Guerin or Transverse
(Pyramidal Fracture of the
(Craniofacial Disjunction)
Maxillary Fracture)
Maxilla)
It is a dental-alveolar fracture
It involves the thick upper part
The line of fracture runs parallel to
of the maxilla passing above
of the nasal bone and the
the base of the skull. The zygomatic
the floor of the nose, involving
thinner portion forming the
arch of the temporal bone is
the lower 1/3 of the nasal
upper margin of the anterior
fractured. The fracture line extends
septum and mobilizing the
nasal aperture. The fracture
through the base of the nose and the
following:
crosses the medial wall of the
ethmoid bone in depth. The
The palate.
orbit, including the lacrimal
cribriform plate of the ethmoid may
Maxillary alveolar process.
bone, runs beneath the
be fractured. Thus disrupting the
The lower 1/3 of pterygoid
zygomatico-maxillary suture,
integrity of the base of the skull and
opening into the subarachnoid
plates.
crossing the lateral wall of the
space.
Part of the palatine bone.
antrum, and then continues
It does not continue up into the
posteriorly through the
medial canthus region.
pterygoid plates.
The mid-face is separated from the
The fracture segment is
The fractured segment is
cranial skeleton, which is usually
displaced posteriorly or
displaced posteriorly or rotated
laterally, rotated about an axis
about an axis or a combination of distracted posteriorly creating the
characteristic dish face deformity.
or any such combination.
both.
Management: little airway
Management: Naso-tracheal
Management: Awake tracheostomy
compromise is seen; therefore,
intubation is relatively
is usually done to secure the airway
the patient may be intubated
contraindicated due to the
thus obviating the risks associated
orally or nasally usually
presence of a fractured nose.
with possible fracture of the base of
without great difficulty.
the skull and leaving the operative
field to the surgeon.
SAFE ANESTHESIA & INTENSIVE CARE
37
1498
Figure 37-xxxxxxxxx: Le Fort Fractures
B) Fractures of the Mandible:
Factors Affecting the Site of the Fractures of the Mandible:
1) The type and shape of the bone of the mandible:
Because the mandible is a tubular bone, it derives its strength from the cortex (figure 37-XXXXXXXX).
At the antero-inferior border: the cortex is thickest; so, it is the strongest and the least vulnerable area
to fracture.
Figure 37-xxxxxxxxx: Common fracture sites of the mandible
At the posterior border near the angle:
The cortex is thinnest; so, it is the weakest and the most vulnerable area to fracture. Because of the
unique horse shoe shape of the mandible, a blow delivered to any part of the mandible may cause
sufficient force to be gathered at the points of vulnerability i.e. the body at the 1st or 2nd molar or the
ramus causing their fractures.
2) The kinetics of the applied force:
With high speed, high impact injuries e.g. automobile crash produces fracture of the ramus, condyle,
and angle of the mandible, which are the most common points of fracture.
With low speed, low impact injuries e.g. the blow from a fist or a fall produces fracture of the body of
the mandible (at the 1st or 2nd molar), symphysis (mentum), and para-symphyseal region, which are the
most common points of fracture (figure 37-xxxxxx and 37-xxxxxx).
Figure 37-xxxx: CT shows fracture mandible
TRAUMA
37
1499
3) The anticipation:
The fact that a low impact blow to the face is usually anticipated allows the victim to turn his/her face
away and take the impact on the lateral side of the body of the mandible.
Therefore, whatever the point of impact and the site of the fracture, one must always consider the
possibility of fractures at the ramus and the body and the possibility of temporo-mandibular joint
dysfunction even though the joint is relatively far away from the point of impact.
Bi-Mandibular Fracture:
It is bilateral fracture at the body of the mandible at the level of the 1st or 2nd molar e.g. a blow from
below usually as the patient falling and striking the face against a counter tip or being thrown forcibly
against the steering wheel of an automobile. This causes distraction of the anterior fracture segment and
postero-inferior displacement of the segment by the muscles of the floor of the mouth taking with it the
tongue and associated para-glottic soft tissues. This causes impaction into the upper airway leading to
partial or complete closure of the airway needing emergency airway management.
This fracture causes a characteristic foreshortening of the mandible (appears as hypoplastic) and is
sometimes called an Andy Gump fracture after a comic strip (cartoon) character popular many years ago.
Factors Limiting Mobility of the Jaw After Trauma: (i.e. the patient cannot open his mouth):
1- Trismus: spasm of the masseter muscle binding the jaw closed.
2- Pain: the most common cause of jaw immobility.
3- Edema.
4- Mechanical disruption of the jaw due to one of the following causes:
Fracture of the condyle.
Dislocation of the tempro-mandibular joint (needing its reduction) (figure 37-xxxxxxxxxx).
Fracture of the zygomatic arch of the temporal bone: It is difficult to fracture the zygomatic arch,
which is protected by the temporal fascia. It splits into lateral and medial sheets enveloping the bone. A
blow from above and from the side may rupture the fascia and break the bone, driving fractured
segment onto the coronoid process of the mandible. The mandible has 2 motions; a hinge-like action on
an axis passing through the condyles and an antero-posterior motion (translation). Translation is limited
by the fracture fragments impinging on the coronoid and the mouth will not open completely. The
anesthesiologist may be deceived when perceiving motion in the jaw, not realizing that further opening
may not occur after the induction of anesthesia and muscle relaxation.
Fracture of the zygoma: may also impinge on the coronoid and limit translation.
SAFE ANESTHESIA & INTENSIVE CARE
37
1500
Figure 37-xxxxxxxxx: Reduction of dislocated tempro-mandibular joint
C) Fracture Base of the Skull:
The craniofacial skeleton is actually two skeletons approximated to each other (i.e. the cranial skeleton
and the facial skeleton). A series of bony buttresses is built into the craniofacial configuration and several
arches serve to disperse applied forces, thus protecting one skeleton against trauma committed on the
other and creating a normal vector of force dispersion and redistribution. Therefore,
A blow to the mandible along the normal vector can fracture the mandible at the point of impact or
elsewhere, but it will not extend into the skull e.g. a blow along the line (A).
A blow to the mid-face however, tends to create an abnormal shearing force, which can tear the facial
skeleton from the cranial skeleton and extend the fracture line into the base of the skull e.g. a blow
along the line (B) (figure 37-XXXXXXXX).
In presence of severe mid-facial trauma, basal skull fractures should always be considered a possibility.
Figure 37-xxxxxxxx: Fracture base of the skull
D) Laryngeal Trauma:
The larynx is relatively superficial and unprotected anteriorly by bone or other firm tissues; therefore, it
is vulnerable to either penetrating or blunt (closed) laryngeal injuries.
Severe injuries cause complete airway obstruction leading to asphyxia, which causes death within 5
min.
Less severe injuries cause partial airway obstruction (with dysphagia, crepitations, poor phonation)
by: Edema and hemorrhage in the airway itself or in the soft tissues of the interior of the larynx.
Edema and hemorrhage in the deep facial planes of the neck, which easily increase in volume and
pressure due to the rich blood supply of the neck and the enveloping layers of cervical fascia.
Both may produce compression on the larynx leading to complete obstruction of the airway at any time
(even within 15 minutes).
Therefore, constant close observation is essential and preparation for immediate intervention should be
always ready.
C) Trauma to the Trachea and Bronchi:
TRAUMA
37
The trachea and bronchi are well protected by the thoracic cage and by the surrounding pulmonary
tissues, which will serve to cushion the effect of blunt trauma and even missile injury.
Injuries of the trachea and bronchi (if they occur) are usually associated with serious fatal injuries of the
heart, and great blood vessels (due to close proximity).
Anesthetic Management
Preoperative Management
1- Primary Survey (Initial Assessment): as before in management of the trauma.
2- Assessment of the Airway Obstruction: Airway obstruction is either partial or complete
Partial obstruction is characterized by noisy breathing with active accessory muscles of respiration and
paradoxical respiration.
Complete obstruction is characterized by silent breath sounds and paradoxical respiration. Patients will
struggle against their closed airway. Death occurs by asphyxia within 3-5 minutes.
Airway obstruction is discussed in chapter of Airway Management.
3- Assessment of the Extent of Airway Trauma:
Head and neck: Assess the degree of extension, rotation, and flexion. Avoid forced movement due to
the possibility of cervical spine injury.
With extension of the head, the distance between the hyoid bone and the mentum
should accommodate at least 3 finger breadth otherwise difficult intubation should be
suspected.
Mouth: The degree of mouth (jaw) opening and cause of immobility.
The tongue for cutting, edema, ability to be protruded beyond the incisors.
Loose teeth.
Mallampati classification for difficult intubation.
Nasal Passage: Fracture.
Patency, by closing each nostril serially using the force of expiration through each
nostril to indicate the patency.
Larynx: Auscultated for stridor
Face and mandible: Fractures.
Airway Penetration: is indicated by presence of hemoptysis, stridor, hoarseness, subcutaneous or/and
mediastinal emphysema.
4- Assessment for Other Associated Injuries or Medical Illness.
5- Preoperative Investigations:
For bleeding: Hemoglobin and hematocrit are rough indices of acute blood loss.
Blood sample for typing and screening.
Plain x-ray for facial bones, cervical spine, and chest.
CT scan for skull (especially at the base), cervical spine (as x-ray of cervical spine may not reveal
damage to C1 to C2 or C7).
Other investigations for the associated injuries or medical illness.
6- Premedications:
Sedatives: are better avoided, but if awake intubation is planned and the patient is hemodynamically
stable, small incremental doses of midazolam 0.25 mg (up to 4-5 mg) may be used to sedate the patient
with close monitoring because midazolam (even in small dose) may:
unmask hypotension and
lead to loss of consciousness with respiratory impairment.
N.B.: Avoid naso-gastric tube to empty the stomach in presence of compromised airway because:
1- Passage of nasogastric tube is hazardous if fracture base of skull is present.
2- It increases the risk of vomiting and aspiration.
3- It does not guarantee an empty stomach because the tube cannot remove large solid particles.
4- It acts as a wick facilitating aspiration.
Intraoperative Management
Monitoring: as in management of trauma patient.
Airway Management: (securing the airway)
Difficult airway management and management of airway obstruction is discussed in chapter Airway
Management.
The choice between these different methods is according to the type of injury:
1501
SAFE ANESTHESIA & INTENSIVE CARE
37
1502
1- If there is a possibility of cervical spine injury:
Intubation is done by in-line immobilization (without much extension of the neck) better with awake
intubation (fiberoptic or blind).
If it fails, tracheostomy is done.
2- If there is a possibility of fracture base of skull:
Avoid manual ventilation by bag and mask.
Avoid nasopharyngeal airway.
Avoid naso-tracheal intubation.
As they may introduce air, foreign material (even the airway or the tube itself) into the skull causing
damage to intracranial contents, increased intracranial pressure and meningitis.
3- If there is immobility of the jaw: (i.e. the patient cannot open his mouth)
a- If due to trismus or pain:
Intubation can be done by the usual i.v. induction and muscle relaxants because anesthetics and
muscle relaxants relieve pain and trismus.
But if the trismus lasts 2 weeks, fibrosis will invade the masseters. Trismus will respond poorly or
not respond at all to the anesthetics or muscle relaxants; so, awake intubation would be needed.
b- If due to mechanical dysfunction of the temporo-mandibular joint:
Awake intubation either fiberoptic or blind.
Fiberoptic intubation may be of little value in the presence of anatomic distortion, hemorrhage, or
edema.
N.B.: If immobility of the jaw is due to edema, it usually does not affect intubation a lot.
4- If there is a bi-mandibular fracture:
If the airway is stable and the patient has no respiratory distress, it may be possible to intubate the
patient by i.v. induction and muscle relaxant or awake intubation.
If there is soft tissue impaction into the upper airway with edema, blood and secretion causing
partial or near complete obstruction, emergency tracheostomy, or cricothyrotomy are needed.
N.B.: In a truly emergent situation (i.e. near complete obstruction), the anesthesiologist should grasp the
mandible in the midline and gently, but forcefully draw it forward, reducing the fracture and disimpacting the soft tissues lodged in the oropharynx.
5- If there is penetrating airway injury (in the larynx or trachea):
A long uncut endotracheal tube is positioned; so that, the tube cuff is below the penetration site to
protect the airway and allow the surgeon to repair the disruption without interfering with ventilation.
Endotracheal tube without a Murphy eye is used.
Tracheostomy can be done as an alternative.
6- If there is trauma to the larynx:
Fiberoptic intubation.
Tracheostomy can be done as an alternative.
7- If there is complete airway obstruction: Immediate intervention is required by:
Emergency tracheostomy: It is very difficult in a struggling patient.
Operative cricothyrotomy.
Needle cricothyrotomy (trans-laryngeal ventilation).
8- If there is lung injury:
A double lumen tube is used to isolate the injured lung or the more injured lung (if bilateral lung
injury) allowing ventilation to the more healthy lung.
It is not suitable for nasal intubation due to its large size.
General Rules:
1- If there is no risk of airway obstruction, i.v. induction and suxamethonium should be used.
2- If there is a little risk of airway obstruction, inhalational induction should be used.
3- If there is a true risk of airway obstruction, awake induction should be used.
4- If there are emergency or severe conditions, tracheostomy or cricothyrotomy should be used.
N.B.: The role of the laryngeal mask airway in patients with upper airway trauma:
The laryngeal mask has a little role in the management of the traumatized airway because:
It does not protect against aspiration of vomitus.
It does not offer complete security of the airway (as a tube does).
However, if the upper airway is severely compromised and endotracheal intubation is impossible and
ventilation is inadequate, the laryngeal mask may be used as a life-saving technique as a last resort.
Induction of Anesthesia:
TRAUMA
37
It is usually done after securing the airway as in anesthesia for trauma patients
Ketamine should be avoided due to:
the associated increased intracranial tension in head trauma.
No guarantee airway protection (if airway is not yet secured).
Maintenance and Recovery:
As that in management of trauma patients.
Postoperative Management
1- Extubation:
Time of Extubation: It is done after:
The patient fulfills the criteria of extubation such as alertness, complete reversal of muscle relaxants,
hemodynamically stable, acceptable blood gases, and acceptable respiratory mechanics.
Subsiding of the edema: It is impossible to visualize the interior of the airway; so, edema of the airway
can be suspected by:
Presence of external edema on the neck may indicate internal edema.
Presence of an edematous tongue that extends beyond the incisors may indicate internal edema.
Technique of Extubation:
After airway surgery, edema can occur in the airway immediately after extubation; therefore,
1- Blunt the airway reflexes: by 3-4 mL of 2% lidocaine directly injected into the endotracheal tube before
its removal to produce partial anesthesia of the airway (avoid opioids to blunt airway reflexes at time of
extubation due to their respiratory depressant effect). The patient should be fasting to avoid the risk of
aspiration.
2- Place a ventilating tube exchanger through the endotracheal tube then withdraw the endotracheal tube
slowly to the outside (or place a fiberoptic bronchoscope through the endotracheal tube) then after
withdrawal of the endotracheal tube, observe for signs of airway obstruction. If they occur, intubate again
using the ventilating tube exchanger or bronchoscope.
3- After extubation, close observation of the patient and auscultation of the larynx frequently searching
for stridor and other signs of airway obstruction should be done for at least one hour after extubation,
with complete availability for immediate intervention if needed.
2- Postoperative Analgesia:
If the patient is still intubated and ventilated, opioids can be used.
If the patient is extubated, usually the pain is moderate; so, ketorolac is used (has no respiratory
depressant effect).
Anesthesia for Mass Casualty and Disaster Situations
Definitions
Mass casualty and disasters are events that occur when destructive effects (the number of casualties)
overwhelm the ability of a given community, state, or even country to meet the medical needs of its
victims.
Types of Mass Casualty and Disaster Situations
1- Cataclysmic Events:
They are either: natural e.g. earthquake, tsunami, or tornado, or
man-made e.g. nuclear reactor meltdown, or chemical spill.
2- War: (either full scale or small as guerrilla warfare)
It is characterized by:
Big numbers of victims with casualties may present continuously over days or weeks.
The health care infra-structure may be severely damaged or destroyed.
The health care providers may themselves be in danger or under direct attack.
Treatment of victims may have to be delayed until their transfer to more safe areas.
Tactical commanders have top priority in supply, communications, and manpower. At these times,
severe shortage in all 3 areas may be present.
Information can be scarce or false in a phenomenon known as the fog of war.
The physician may be expected to treat enemy soldiers, which may carry a risk to physicians from their
attack.
Fear, fatigue, and confusion among care providers create additional levels of stress.
1503
SAFE ANESTHESIA & INTENSIVE CARE
37
1504
Military health care facilities and equipment designed for use in forward locations are generally
simple, easy to maintain, mobile, and lightweight.
N.B.: Weapons of mass destruction (WAD) and Hazardous Materials (HAZMAT) can be used.
3- Terrorism:
It can range from the conventional e.g. small arms and bombs to unconventional e.g. biological,
chemical, and even nuclear attacks.
Because there is generally little advance warning of a terrorist attack, facilities, systems, and providers
are unprepared.
Some times the anesthesiologist provides care with equipment and monitoring which are not standard
and can provide care to more than one victim simultaneously.
Emergency Medical Service Providers
1. The Tactical Emergency Medical Services (TEMS):
It developed mainly to deal with high-risk warrant services and other dangerous activities. TEMS is
either: TACMED: those are military personnel who receive medical training to enable them to provide
emergency care to the wounded.
MEDTAC: those are primarily personnel with a medical background who receive training in the
tactical activities.
2. Emergency Medical Services (EMS):
It includes EMS helicopters, on land ambulances, and mobile intensive. In the USA, the personnel are
physicians, but in Europe, they are mainly anesthesiologists. They provide pre-hospital medical care.
Pre-Hospital Planning and Response
All hospitals must have a disaster plan and test this plan twice a year. There are 2 levels of these plan and
tests: a) 1st level: is by using computer software for disaster modeling. It is the most simple and
inexpensive.
b) 2nd level: is full-scale or real life systems that involve life-size modeling including victims, actual
response and transport units as ambulances, fire trucks, and helicopters. This simulation is expensive
and requires a great deal of coordination. Drills are mock alarms designed to test the readiness of a
system usually without advance warning.
Phases of Any Disaster Response
Three phases: 1- Activation.
2- Implementation.
3- Recovery.
1) Activation:
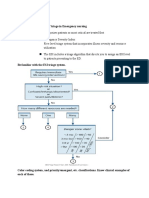
It is the initial response followed by notification and establishment of an incident command post (figure
37-xxxxxxxxxxxxx). The reports include:
The nature of the incident.
The number and types of injuries.
The potential hazards for victims and rescuers.
The extent of damage to the area.
The possible access routes to and away from the scene.
The incident commander has overall authority on the scene (either, the fire chief or the chief of police).
After disaster, the area is divided to many zones.
Inner (hot) zone: only fire and rescue personnel are permitted to enter it.
Decontamination (warm) zone: victims are brought from the hot zone to the decontamination area
where the decontamination process occurs.
Support (cold) zone: victims are taken to the casualty collection point (CCP) for triage and
stabilization. Also in this zone, transport crews, ambulances, and resources are readily available as
needed to avoid congestion at the scene. A command post is present and a helicopter-landing zone is
identified.
TRAUMA
37
1505
Figure 37-xxxxxxxxx: Activation of the disaster response
2) Implementation: It involves:
a- Search and Rescue (SAR):
SAR is done by specially trained personnel. Rescuers must be adapted to conducting large-scale searches
over vast (big) areas in short time. Medical personnel not trained in SAR should wait at the CCP to avoid
becoming victims themselves.
b- Triage:
It means (to sort) from French word. It is a method of sorting large numbers of patients according to the
priority with which they should be treated and transported. This allows good use of the resources. It is
done by anesthesiologists.
The concept of reverse triage is the exclusion of the patients with lethal injuries, thereby focusing
available resource allocation on those with the greatest chance of survival. Triage applies to both
treatment and transport of patients. Triage is done 1st by rescuers at the scene, followed by EMS personnel
at the CCP then during transport and finally by medical staff at the hospital where definitive care is given.
Casualties are classified into 4 categories during triage:
Class
Injury Description
Action Taken
Priority
1- Minimal
Minor injuries not needing prompt medical care Treated and transported
3rd
(i.e. walking wounded patients).
after immediate and delayed
patients.
2- Delayed
Serious injuries needing treatment, but not
Treated and transported
2nd
immediate life threatening.
after immediate patients.
3- Immediate Injuries needing immediate treatment to save a
Treated and transported
1st
life or a limb.
first.
4- Expectant Severe injuries making survival unlikely.
Comfort and analgesic
4th
measures only (opioids and
benzodiazepines).
3) Recovery:
It consists of 3 steps:
1st step: It is the systematic withdrawal of all personnel and equipment from the scene.
2nd step: It is the return of all parties to normal operations.
3rd step: Where debriefing occurs, which is the analysis of all events in an attempt to improve future
responses. The emotional and psychological effects of the disaster on the rescue and medical personnel
is discussed and treated as it ranges from mild effects to post-traumatic stress disorders.
Role of Anesthesiologists in Managing Mass Casualties
Decontamination of victims (if needed).
SAFE ANESTHESIA & INTENSIVE CARE
37
1506
Management of victims of mass casualties.
Triage of the patients.
Management in emergency department.
Anesthesia in operating rooms.
Management in intensive care units.
Mechanisms of Trauma
There are many types of trauma, but the major categories during mass casualty include blast injuries, toxic
trauma (chemical or biological weapons), burns, and inhalational injuries.
1) Blast (Bombing) Injuries
Blast injuries result from explosions, are one of the following effects:
at atmospheric pressure in the air.
above atmospheric pressure under water (sea).
below atmospheric pressure in space.
Injuries result from:
1- A sudden release of energy that produces a localized increase in pressure and temperature.
2- Mechanical injuries e.g. explosive devices with sharp objects.
3- Electrical injuries.
4- Chemical injuries e.g. explosive devices with toxic chemicals (figure 37-xxxxxxxxxxxx).
When explosion occurs in the air, transformation of substance into gas results, which rapidly expands a
sphere of high-pressure, high-temperature and positive pressure blast wave (over-pressure waves). These
waves radiate from the source at nearly the speed of sound; therefore,
they reach trenches through air.
they are transmitted through the ground leading to ground shock.
they are reflected, increasing and aggravating the original trauma.
Figure 37-xxxxxxxx: Blast injury
The longer the over-pressure waves and the longer the duration of exposure of body in its path, the
greater the potential for injury. Positive pressure waves are followed by a negative pressure component
(under-pressure) resulting in pressure changes. This causes mass movement of air leading to high velocity
blasts that are directed toward or away from the source in an alternating fashion. The same damage
occurs as the initial over-pressure waves do.
Relative effects of various over-pressures (lasting 4 msec).
Over-Pressure (psi)
Effects
1
Damage to ordinary structures e.g. flying glass and debris.
2
Slight chance of perforation of tympanic membrane.
15
50% chance of perforation of tympanic membrane.
40
Serious damage to reinforced concrete structure.
TRAUMA
37
70
130
50% chance of severe pulmonary damage.
50% chance of mortality.
Patterns of Blast Injuries:
1. Primary blast injuries: arise from direct exposure to blast over-pressure.
2. Secondary blast injuries: arise from blunt, penetrating or impalement from flying materials
energized by the blast, arising either from the explosive device itself or from victims thrown a distance
away from the device.
3. Tertiary blast injuries: arise from blast-induced whole or partial body displacement caused by the
blast winds as high-energy explosions when people fly through the air and strike other objects.
4. Quaternary injuries: include crush injuries, burns and inhalational injuries from hot gases, dust, or
other debris or from fires resulting from the explosions.
2) Toxic Trauma (Chemical or Biological Weapons)
Hazardous Materials (HAZMAT)
Special equipment and protective clothing may be needed, as the medical responders may be at risk
themselves. They include 4 levels:
Level
Protective Clothing
Level A
It is the most protective and consists of self-containing breathing apparatus (SCBA), fully
encapsulating, vapor tight, chemical resistant suits, with a hard hat, a cooling vest and 2 way
radio communications.
Level B
It is worn when the highest respiratory protection is needed with less eye, skin, and mucous
membrane protection.
It is the same equipment as level A except that the protective suit is not vapor-tight.
Level C
As level B except for respiratory equipment.
Air-purifying respirators are used in place of SCBA. It filters the air and it is used with
atmospheric O2.
Level D It is simply a work uniform with no special protective properties.
Hospitals willing to accept victims of chemical agent attacks should have:
A decontamination room.
Filtration systems to provide decontaminated air into the interior.
Personnel trained in decontamination processes.
At first, isolation and confining the hazmat is done. This is followed by evacuation of people at risk,
decontamination (removal of all clothing and washing the victims with warm water care is taken to avoid
hypothermia) and stabilization of victims and transporting them for definitive care e.g. airway control,
isolation of spontaneously breathing patients with escape mask or SCBA, spine immobilization,
hemorrhage control.
A- Chemical Weapons:
Most casualties of chemical agent incidents require supportive care only. No specific treatment is present
except nerve agents and blood agents. Most chemical agents are liquid at room temperature, and when
vaporized, all are heavier than air (hydrogen cyanide is an exception) and concentrate in low areas
(trenches, basements). If exposed, individuals should ascend to higher levels, and even standing provides
some protection as opposed to lying down.
1- Nerve Agents (Organophosphorus Compounds):
They include di-isopropyl fluorophosphate (DFP), tetra-ethyl pyrophosphate (TEPP), sarin, soman, and
tuban. The mechanism of action, clinical picture, and management of organophosphorus compounds are
discussed in chapter of Pharmacology of Anesthesia & Intensive Care.
2- Blood Agents (Cyanide Agents):
They include hydrogen cyanide, cyanogen chloride, and arsine.
Route of toxicity: Inhalation of great amounts of cyanide.
Ingestion of cyanide (mostly with suicidal intent).
It poisons the cytochrome a 3 in the mitochondria inhibiting cellular respiration especially in the
neurological cells. Therefore, these cells cannot use O2.
Clinical Picture: loss of consciousness, seizures, apnea, and death within 8-10 min.
Treatment: is discussed in chapter Pharmacological Adjuncts to Anesthesia & Intensive Care.
3- Pulmonary Agents (Pulmonary Intoxicants):
1507
SAFE ANESTHESIA & INTENSIVE CARE
37
1508
These are substances, which damage the airway and the parenchyma of the lung.
For example, Sulfur mustard.
Phosgene (carbonyl chloride).
Chlorine.
Clinical Picture:
Mild cough, chest discomfort, and dyspnea.
Pulmonary edema (acute respiratory distress syndrome) within 2-6 hours after exposure (i.e. severe
injury). It may be delayed up to 72 hours (i.e. mild injury).
Treatment: There is no antidote. Only supportive treatments are administered such as ventilation, O2, and
fluids for hypovolemia. Steroids may be useful.
4- Skin Agents (Skin Vesicants):
They are substances that cause vesicles or blisters.
For example, Sulfur mustard.
Nitrogen mustard.
Lewsite (an arsenical agent).
Phosgene oxime.
Clinical Picture: They affect DNA causing damage of cells. After a brief period or mild exposure, the
following manifestations occur in order:
Erythema, pruritis, burning, tingling then blisters, and necrosis that occur within 2-24 hours.
Eye redness then damage.
Airway mucosa is damaged from the upper to the lower airway according to the dose.
Bone marrow damage decreasing the resistance to infections.
Gastrointestinal mucosal damage resulting in hemorrhage.
Treatment: There is no antidote. Only supportive treatment is present.
B- Biological Weapons (Bioterrorism):
For example,
Disease
Anthrax
Botulism
Plague
Brucellosis
Cholera
Typhoid
Smallpox
Agent
Bacillus anthracis
Clostridium botulinum toxins
Yersinia pestis
Brucella
Vibreo cholerae
Salmonella typhi
Variola major
Route of Transmission
Aerosol
Ingestion
Aerosol
Ingestion or aerosol
Ingestion or aerosol
Ingestion or aerosol
Ingestion or aerosol
Management of Suspected Victims of Chemical or Biological Warfare:
1- High index of suspicion based on features suggesting exposure or infection with chemical or biological
weapons such as:
Unusually high incidence or mortality from a diseases cluster.
Single case of an unusual pathogen (inhaled anthrax, smallpox).
Cluster of patients with a suspicious clinical illness such as:
Flu-like illness leading to acute respiratory distress syndrome, shock, or meningitis (anthrax).
Acute febrile illness with pustular lesions (smallpox).
Occurrence of a disease outside its natural geographic boundaries (hemorrhagic fever, plague).
Cluster of patients with acute flaccid paralysis (botulism).
Clustering of diseases that affect animals as well as humans.
2- Protection of health care workers (gowns, gloves, masks) as above.
3- Notify hospital, public health, and governmental officials.
4- Decontamination of exposed individuals:
Hospitals should have decontamination facilities as part of their disaster preparedness plan.
Contaminated clothing is removed and the skin decontaminated at the scene before transportation.
Soap and water are effective decontaminants, and if available, a dilute solution (0.5%-2%) of hypochlorite (household bleach) can be used to decontaminate the skin.
5- Triage (some require isolation).
Designate a hospital ward and selected health care workers to care for patients with suspected
infectious diseases or contaminated chemicals.
TRAUMA
37
Stable and noninfectious patients should be discharged to reduce the risk of exposure to contagious
diseases.
6- Label all materials from affected patients with bioterrorist/biohazard tags.
7- Active immunization or prophylactic antibiotics may prevent or attenuate the disease e.g.
immunization and ciprofloxacin as a prophylaxis for smallpox.
8- ABCDE management should be applied as soon as possible to victims (as above).
N.B.: Toxic Advanced Life Support (TOXALS):
The conventional advanced life support is usually delayed to be applied to contaminated patients until
decontamination occurs, by new devices and recent technologies field care providers by using especially
protective suits that allow them to perform life-saving procedures and assessing basic physiologic
parameters e.g. respiratory rate, heart rate, blood pressure. Therefore, patients in hot and warm zones
do not need to wait until being removed from the decontamination area before being intubated and
receiving drugs and fluid resuscitation. Performing intubation during wearing protective gear is
possible, but needs a longer time. The main problem is fixation of the tube. Now laryngeal masks and
combi-tubes can be used.
9- Anesthetic management and equipment for mass casualty (if needed) is discussed later.
3) Nuclear Accidents
Nuclear accidents can occur such as nuclear power plants, reactor accidents, terrorist action, theater
nuclear war (detonation of nuclear bombs).
Effects of Nuclear Accidents:
Tissues with the most frequent turnover rate (lymphoid tissues, bone marrow, skin, joints, gonadal cells,
gastrointestinal mucosa) are most susceptible to radiation injury.
Managements:
1- Decontamination:
If possible, patients should be decontaminated at the site of exposure rather than risk bringing material
emitting ionizing radiation to the hospital.
Removal of clothing is important to eliminate any residual beta and gamma rays and neutrons.
The patients skin should be rinsed with warm soapy water.
Biological materials (saliva, blood, urine, stool) must be isolated because they may be contaminated
with radioisotopes.
2- Assessment of the Degree of Exposure of Individuals to Radiations:
It is very difficult to assess the degree of exposure of individuals to radiations. Generally:
Individuals who have no symptoms after 6 hours of suspected exposure are unlikely to have
received a dose of radiation that requires hospitalization.
Individuals, who are symptomatic, are suspected to have radiation exposure. They should be
hospitalized.
1- Serial complete blood counts should be obtained at least on initial contact and after 24 hours to
determine the absolute lymphocyte count.
At 24 hours, an absolute lymphocyte count less than 1000 cells/mm3 suggests moderate exposure
and less than 500 cells/mm3 suggests severe exposure.
If white blood cell counts remain stable for 48 hours, the patient may be not exposed and can be
dismissed.
2- All body orifices (nostrils, ears, mouth, rectum) should be swabbed.
3- A 24-hour stool and urine collection performed if internal contamination is considered.
3- Radiation Syndrome (or Sickness):
The symptoms and signs of radiation syndrome should be assessed and managed.
Acute:
Bone marrow depression leading to granulocytopenia and thrombocytopenia with increased
incidence of infection and coagulopathy.
Gastrointestinal injury leading to bleeding (secondary to mucosal injury and thrombocytopenia),
nausea, vomiting, diarrhea, and fever (in severe cases).
Hypothyroidism.
Later on:
Hypotension.
Central nervous system dysfunction.
1509
SAFE ANESTHESIA & INTENSIVE CARE
37
1510
Hematopoietic syndrome from lymphoid and bone marrow suppression may lead to death in 8 to 50
days.
4- Preventive Measures:
Potassium iodide tablets or solution (Lugols solution) should be distributed to the susceptible
individuals within 24 hours to be effective in prevention of radiation-induced thyroid effects.
Oral and gastrointestinal decontamination via nasopharyngeal lavage, early stomach lavage, or the
administration of emetics and osmotic laxatives should be performed to avoid gastrointestinal
affection.
Ammonium chloride, calcium gluconate, and diuretics may be administered to facilitate renal
excretion.
Measures to decrease infection, including food with a low microbial content, clean water supplies,
frequent hand washing, and air filtration especially during the neutropenic phase of acute radiation
syndrome.
Empirical antibiotics.
Hematopoietic growth factors (granulocyte colony stimulating factor G-CSF) may shorten the
duration of neutropenia.
Oral feeding is preferred over i.v. feeding to maintain the immunological and physiological integrity
of the gastrointestinal tract and decrease bacterial translocation.
Administered blood products should be irradiated and cytomegalovirus negative.
5- Surgical Treatment:
Surgical treatment of life-threatening injuries must precede any treatment of associated radiation injury
because the skin is impermeable to most radionuclides, but particles can be absorbed through open
wounds. Contaminated wounds should be decontaminated with copious irrigation.
4) Burns and Inhalational Injuries
Field care providers must be able to quickly assess the extent and severity of burns and provide initial
triage. The anesthetic and perioperative management of burned patients is discussed before in chapter
of Plastic Surgery. Burn patients require critical care resources e.g. i.v. fluids, airway management,
mechanical ventilations. The number of intensive care unit burn beds is usually limited; so, triage is
important.
Anesthesia Equipment for Austere Conditions
Hospital facilities are often damaged or destroyed in affected areas. When hospitals are compromised, the
government may need to establish field hospitals (figure 37-xxxxxxxxx).
Figure 37-xxxxx: An example of a field hospital
Anesthesia Devices, in these field hospitals with austere unfavorable conditions, should be
characterized by the following features:
TRAUMA
37
An extended battery life.
Increased durability.
Low cost.
Ease of operation and repair.
Portable.
Ability to conserve O2 supply and anesthetic agents.
Electrical requirements and fresh gas needs should be minimal.
Multi-task equipment i.e. many functions in one condensed package.
A draw-over anesthetic system is better used because its vaporizer can use ambient air as a carrier gas
(O2 can be added when available) such as tri-service anesthesia apparatus. These devices are discussed
in chapter of Anesthetic Apparatus & Equipment.
Monitoring Equipment:
During disaster conditions, sometimes the monitoring equipment is deficient. Although all the usual
monitors are important, a successful anesthesiologist in a disaster situation should be able to provide safe
anesthesia by using the available monitors.
Pulse oximeter is the most important and it can be the only monitor due to its small size, low cost, and it
gives many data as pulse, hemoglobin saturation, and peripheral perfusion.
O2 Supply:
O2 is the most essential drug administered to trauma patients. It can be supplied by many methods such
as pipe systems, O2 tanks, liquid O2, but the most suitable method in austere conditions is the O2
concentrators as they can supply oxygen from room air.
Anesthetic Management of Mass Casualty
Anesthetic Management of Poly-Traumatized Patient:
Primary, secondary, and tertiary surveys are discussed above.
The choice of anesthetic techniques and anesthetic drugs should depend on the availability and that with
the least side effects and complications, which necessitates less monitoring and close observations.
For example:
a- Regional and local blocks such as subarachnoid, epidural, axillary, i.v. Bier block are sometimes
preferred because they do not need one-on-one monitoring after the initial block is established, which
save anesthesiologists for other victims. Patients can be monitored with less trained personnel. They
conserve also O2 supply and anesthetic agents.
b- Analgesic agents used in field conditions:
1- Non-steroidal anti-inflammatory drugs (NSAIDs) are preferred because they do not cause
respiratory depression. This decreases the need for close observation and monitoring and decreases the
need for respiratory support and mechanical ventilation, which is always required during mass
casualty.
2- Opioid agonist/antagonist such as buprenorphine and nalbuphine are preferred because they have
a ceiling effect on respiratory depression and relative cardiovascular stability; therefore, they also do not
need the close observation and monitoring.
Short acting opioids such as fentanyl are preferred due to its rapid onset and short duration.
3- Ketamine is the agent of choice in austere conditions due to its relative portability, extended shelf
life, high relative potency versus dose given, and the ability to preserve the respiratory drive. It does not
need close monitoring and respiratory support. It can be taken by i.v., intramuscular, subcutaneous, or
even oral route.
Conversely, some believe that ketamine is not suitable in conditions as military or mass casualties due
to its involuntary muscle movement, vivid hallucinations, hypertension, and increased intracranial
tension in head injuries.
4- Nitrous oxide is used in pre-hospital and emergency departments, but It needs a special portable
apparatus e.g. Entonox device (with 50% in O2).
c- Anesthetic agents used in field conditions:
1- Barbiturates:
Advantage: it is of low cost and has favorable effects on intracranial tension.
Disadvantage: It is a poor analgesic and cannot be used for prolonged infusion.
2- Diazepam:
Advantage: it is administered i.v or intramuscular and with long t1/2; and so, administered less
frequently.
Disadvantage: it may cause respiratory depression but it is reversed by flumazenil.
3- Midazolam:
1511
SAFE ANESTHESIA & INTENSIVE CARE
37
1512
Advantages: Good cardiovascular stability, decreased perioperative awareness especially in trauma
patients.
Disadvantages: short t1/2 so, it needs frequent dosing.
4- Etomidate:
Advantages: good cardiovascular stability; so, it is the best in shocked patient.
5- Propofol:
Advantages: sedation and total intravenous anesthesia (TIVA), and high clearance rate.
Disadvantages: cardiovascular inhibition (especially in shocked patient). Respiratory depression
(especially in head trauma).
6- Inhalational agents: are mainly used for maintenance of anesthesia. They are not used for induction
(even with the single-breath technique of sevoflurane) due to the risk of full stomach. Isoflurane and
sevoflurane are the drugs of choice.
d- Blood Transfusion:
In mass causality, blood conservation is very important, as blood is usually not available.
Auto transfusion techniques can be used due to their low technique and low cost. As long as sterility is
maintained, it can be done in the pre-hospital or inside hospitals, operating rooms, or intensive care units.
Homologous blood transfusion after typing, screening, and testing donors for diseases is also used.
Psychologic Impact of Trauma
Anesthetic Implications
Mass casualty and disaster situations produce psychological and emotional effects on:
The patients: they are usually treated with care should be paid for perioperative awareness during
anesthesia.
The care providers: they are usually neglected.
The anesthesiologists themselves: they are usually neglected.
Therefore, anesthesiologists should be aware of these psychological effects. Life-threatening posttraumatic stress disorders may occur to the care providers. Many strategies are done to decrease this
post-traumatic stress disorder. The most popular is the critical incident stress debriefing system, which
is based on group discussions and talking out emotionally charged issues.
Further Readings:
Brooks AJ, Rowlands BJ: Blunt abdominal injuries. Br Med Bull 1999;55:844.
Dutton RP: Airway Trauma. In Anesthesiology problem-oriented patient management, Yao FF, Fontes ML, Malhotra V (eds), 6th edn., Lippincott
Williams and Wilkins 2008;Vol 3,46;993-1006.
Dutton RP, Sharrar SR: Trauma. Int Anesth Clin 2002:40:1.
Little WC, Freeman GL: Pericardial disease. Circulation 2006;113:1622-1632.
Spodick DH: Acute pericarditis: Current concepts and practice. JAMA 2003;289:1150-1153.
Stoelting RK, Miller RD (eds): Bioterrorism and natural disasters. In Basics of anesthesia, 5th edn. Churchil Livingstone,2007;616-629
Sybrandy KC, Cramer MJ, Burgersdijk C: Diagnosing cardiac contusion: Old wisdom and new insights. Heart 2003;89:485-489.
Trunkey DD, Lewis FR: Current therapy of Trauma, 4th ed. Mosby-yearbook, 1999.
Wall MJ Jr, Mattox KL, Wolf DA: The cardiac pendulum: Blunt rupture of the pericardium with strangulation of the heart J Trauma 2005;59:136-141.
Web Sites:
http://www.trauma.org/
You might also like
- EyeDocument8 pagesEyeAmr SabryNo ratings yet
- دكتور تفريغDocument52 pagesدكتور تفريغGalalMohammedNo ratings yet
- Oxford Handbook of Pain ManagementDocument385 pagesOxford Handbook of Pain ManagementSalma Cortez100% (8)
- TRG Ip Mti FlowDocument1 pageTRG Ip Mti FlowAmr SabryNo ratings yet
- FRCA Primary Onexamination 7Document79 pagesFRCA Primary Onexamination 7Amr SabryNo ratings yet
- List of Approved Tests and Providers - From 13 November 2017Document14 pagesList of Approved Tests and Providers - From 13 November 2017Florin ChituNo ratings yet
- Urinary SystemDocument10 pagesUrinary SystemAmr SabryNo ratings yet
- 2 IntroductionDocument14 pages2 IntroductionAmr SabryNo ratings yet
- 1tnna.::.ru: MiddleDocument4 pages1tnna.::.ru: MiddleAmr SabryNo ratings yet
- 2 RespiratoryDocument8 pages2 RespiratoryAmr SabryNo ratings yet
- - ـلا cell نع ةرابع 3 تاجاح: لاؤس ةمهم MCQ ىجيب ىللا لاؤسلا ع ملعو كاعم رمحا ملق ىلخ MCQ .)Document21 pages- ـلا cell نع ةرابع 3 تاجاح: لاؤس ةمهم MCQ ىجيب ىللا لاؤسلا ع ملعو كاعم رمحا ملق ىلخ MCQ .)Amr SabryNo ratings yet
- 10 1164@rccm 201703-0548ST-1Document11 pages10 1164@rccm 201703-0548ST-1dogui0071No ratings yet
- 1 SkinDocument9 pages1 SkinAmr SabryNo ratings yet
- Uro DynamicsDocument5 pagesUro DynamicsAmr SabryNo ratings yet
- File To Download From ScribdDocument4 pagesFile To Download From ScribdAmr SabryNo ratings yet
- English Today 04Document26 pagesEnglish Today 04tomy85No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- HypokalemiaDocument17 pagesHypokalemiaZero_Sugar100% (1)
- DR Arzoo Nephrology ThesesDocument35 pagesDR Arzoo Nephrology ThesesAzam ArzooNo ratings yet
- Compartment Syndrome: - DiscussionDocument11 pagesCompartment Syndrome: - DiscussionatrisniaNo ratings yet
- HyperphosphatemiaDocument18 pagesHyperphosphatemiaS.R.Cogo100% (1)
- MRCS Osce Sample-2 PDFDocument25 pagesMRCS Osce Sample-2 PDFAmmarNo ratings yet
- NCMB 316Document36 pagesNCMB 316Venansius GanggusNo ratings yet
- Rhabdomyolysis: - Striated - Muscle - BreakdownDocument45 pagesRhabdomyolysis: - Striated - Muscle - BreakdownHelmi Ismunandar100% (1)
- Nsg241 Study Guide Exam 5Document76 pagesNsg241 Study Guide Exam 5NatalieAndersonNo ratings yet
- Diseases and Disorders of The Skeletal SystemDocument11 pagesDiseases and Disorders of The Skeletal SystemJames Roy100% (1)
- GHGHDocument16 pagesGHGHAltair LopesNo ratings yet
- Hyperthermia Case StudyDocument28 pagesHyperthermia Case StudyJanelle GimenezNo ratings yet
- Alcohol Abuse-Related Severe Acute Pancreatitis With Rhabdomyolysis ComplicationsDocument4 pagesAlcohol Abuse-Related Severe Acute Pancreatitis With Rhabdomyolysis ComplicationsMihai SebastianNo ratings yet
- Statins Side Effects - Pain, Inflammation, and MoreDocument6 pagesStatins Side Effects - Pain, Inflammation, and MoreJeff TeeNo ratings yet
- Crush Syndrome & Compartment Syndrome 2020Document45 pagesCrush Syndrome & Compartment Syndrome 2020Icha Marissa SofyanNo ratings yet
- Snake BiteDocument104 pagesSnake Bitenehanirmal0% (1)
- Heat StrokeDocument15 pagesHeat Strokevague_darklordNo ratings yet
- Electrolyte Repletion GuidelineDocument6 pagesElectrolyte Repletion GuidelineIla MahiraNo ratings yet
- Causes of Muscle Breakdown: RhabdomyolysisDocument3 pagesCauses of Muscle Breakdown: RhabdomyolysisemirkurtalicNo ratings yet
- Golpe de Calor NEJMDocument11 pagesGolpe de Calor NEJMJair Alexander Quintero PanucoNo ratings yet
- Acute Kidney Injury in Crush Syndrome and Renal Disaster-Experience in Bangladesh After Garment Factory CollapseDocument6 pagesAcute Kidney Injury in Crush Syndrome and Renal Disaster-Experience in Bangladesh After Garment Factory CollapseMinerva Medical Treatment Pvt LtdNo ratings yet
- Rhabdomyolysis In-Service WuDocument24 pagesRhabdomyolysis In-Service Wuapi-323356666No ratings yet
- Baycol Recall FDA AnnouncementDocument4 pagesBaycol Recall FDA AnnouncementZainab WowoussNo ratings yet
- UrinalysisDocument2 pagesUrinalysisKiersten Karen Policarpio VerinaNo ratings yet
- Plabable-Gems-30. Nephrology Plabable GemsDocument34 pagesPlabable-Gems-30. Nephrology Plabable GemsHabo HaboNo ratings yet
- Propofol Infusion Syndrome PDFDocument3 pagesPropofol Infusion Syndrome PDFPGI AnaesthesiaNo ratings yet
- Muscular Development - February 2009 (US)Document199 pagesMuscular Development - February 2009 (US)S Lucian Stefan100% (3)
- Internal Medicine 1 Conrad FischerDocument35 pagesInternal Medicine 1 Conrad Fischerjaber fathiNo ratings yet
- Diseases of Muscular SystemDocument2 pagesDiseases of Muscular SystemChari Mae Tamayo PanganibanNo ratings yet
- How To Reduce The Size of My Buccinator Muscles With Mewing - QuoraDocument1 pageHow To Reduce The Size of My Buccinator Muscles With Mewing - QuoraJan DušekNo ratings yet
- Creatinine KinaseDocument1 pageCreatinine KinaseUria Prasetya Tidar SiagianNo ratings yet