Professional Documents
Culture Documents
Antimalarial Potential of Nosode 30 and 200 Against Plasmodium Berghei Infection in BALB/c Mice
Uploaded by
Dexter BluesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antimalarial Potential of Nosode 30 and 200 Against Plasmodium Berghei Infection in BALB/c Mice
Uploaded by
Dexter BluesCopyright:
Available Formats
J Vector Borne Dis 49, June 2012, pp.
7277
Antimalarial potential of Nosode 30 and 200 against Plasmodium berghei
infection in BALB/c mice
U. Bagai, A. Rajan & S. Kaur
Parasitology Laboratory, Department of Zoology, Panjab University, Chandigarh, India
ABSTRACT
Background & objectives: Homeopathy is considered as an emerging area of alternative medicine which could
be established for the global health care. One of the greatest objections to this science lies in its inability to
explain the mechanism of action of the micro doses based on scientific experiments and proofs. The present
study has been undertaken to screen in vivo antimalarial activity of Malaria Co Nosode 30 and Nosode 200
against Plasmodium berghei infection in BALB/c mice.
Methods: Peters 4-day test was used to evaluate the in vivo schizontocidal effect of Nosode 30 and Nosode 200.
One month follow-up study was done to calculate the mean survival time of mice in each group. Biochemical
analysis was carried out to assess the liver and kidney function tests using diagnostic kits.
Results: Nosode 30 and 200 exhibited 87.02 and 37.97% chemosuppression on Day 7 and mean survival time
(MST) of 18.5 2.16 and 16.5 1.37 days respectively, which were extremely statistically significant when
compared to MST of infected control (8.55 0.83 days). The safety of Nosode 30 was also confirmed by the
comparable levels of ALP, SGOT, SGPT activities, concentration of bilirubin, urea and creatinine to CQ treated
group.
Conclusion: Nosode 30 possesses considerable in vivo antiplasmodial activity against P. berghei infection as
compared to Nosode 200 as evident from the chemosuppression obtained using Peters 4-day test. Further,
studies on the drug can be carried out to establish its antimalarial potential in monotherapy or in combination
with other homeopathic drug formulations.
Key words
Homeopathy; Malaria Co Nosode; parasitaemia; Plasmodium berghei
INTRODUCTION
Antimalarial chemotherapy for decades is cheap, safe
and practicable for outpatient use but resistance to cheap
efficient antimalarial drugs cause a major problem. Homeopathy is a system of curing diseases with very minute
doses of medicine. In homeopathy, crude drug substance
is diluted and triturated or succussed to increase its potency by virtue of which, only the medicinal power of the
substance is retained and drug related side-effects are eliminated. Hahnemann, father of homeopathy believed that
Vital force of a substance was somehow released by the
process of succussion/potentization to the vehicle which
now behaved as the medicine1.
Homeopaths also use treatments called Nosodes made
from diseased or pathological products such as faecal,
urinary or respiratory discharges, blood and tissue. Malaria officinalis/Malaria Co Nosode is not a discharge
but is called vegetable nosode as it is swamp mire that has
been potentised. It was found that the Malaria Nosode is
made out of the rotting vegetation from marsh areas where
the mosquito breeds. The African homeopaths recommended Malaria Co Nosode 30 on a weekly basis for visi-
tors, starting a week before arrival for recurring parasite
which lingers in liver for months. It is one of the most
frequently used antimalarials in homeopathy, but there is
no provings record. A routine of prophylaxis was given in
the form of Abha light complex 30C remedies that contain 5 ingredients, one of them being Malaria Nosode, sold
by Ainsworth Pharmacy, UK which contains four malarial
(Plasmodium falciparum, P. vivax, P. ovale and P.
malariae) and Anopheles mosquitoes. The malaria complex was found very effective in preventing malaria in Kenya.
All recommended prophylaxis for visitors2. Homeopathy is
the second largest system in the world, widely used and
economical but lacks some evidence based research and data
in order to prove its efficacy to the scientific community.
China another homeopathic antimalarial is also reported to
have schizonticidal activity against lethal rodent malaria
parasite. The drug enhanced the mean survival time of the
mice and also found safe on the morphology of red blood
cells of the host as observed in SEM studies3. Present research work is an effort to provide most authentic information about antimalarial Nosode 30 and Nosode 200 to their
in vivo antimalarial activity against P. berghei (NK-65)
infection in BALB/c mice.
73
Bagai et al: Homeopathy against malaria
MATERIAL & METHODS
Mouse and parasite strain
White swiss mice Mus musculus of BALB/c strain
(weighing 2226 g and 4-6 wk old) of either sex, obtained
from the Central Animal House, Panjab University,
Chandigarh were used as experimental model. They were
maintained on a standard pellet diet and water ad libitum.
P. berghei (NK- 65) was maintained by i.p. inoculation
of 1106 parasitized RBCs from infected to nave mice.
Parasitaemia was checked by preparing Giemsa stained
thin blood smears through tail vein incision of infected
mice4. The treatment of mice was according to the guidelines of committee for the purpose of control and supervision on experiments on animals (Reg. No. 45/1999/
CPCSEA), Panjab University, Chandigarh.
Drugs used
The 30 and 200 potency of homeopathic Nosode (Malaria Co Nosode [Nd]) manufactured by M/s. S.B.L. India were used in the present study. These drugs were diluted with distilled water in the ratio 1:2 (v/v) before
administration. Chloroquine (LARIAGO Chloroquine
phosphate suspension containing 50 mg base) manufactured in India, was given to positive control and chloroquine 20 mg/kg was prepared in distilled water.
Evaluation of antiplasmodial activity of Nosode (Nd 30
and Nd 200)
Six groups having 6 mice each (same sex and age)
were used for the present study and the groups were designated as G1 to G6 (Table 1). All groups except G-1
(normal control) were injected with 1106 P. berghei parasitized RBCs i.p. on D0 and treated for 4 consecutive days
(D0D3). G1and G2 mice were administered 0.2 ml of
distilled water and were kept as normal control and infected control group respectively. Homeopathic drugs Nd
30 and Nd 200 and CQ (20 mg/kg) as positive control
were evaluated for their schizontocidal effect using Peter
4-day test.
Blood smears were prepared from tail vein incision
on D5 and D7 followed by weekly examination of blood
smears up to 1 month follow up period (i.e. Day 14, 21
and 28). Blood films were stained with Giemsa and examined microscopically. The degree of infection was recorded
as the percentage parasitaemia. Average chemosuppression
for each group and mortality of mice (evaluated as mean
survival time period (MST) in each group were determined
arithmetically.
Biochemical analysis
The therapeutic efficacy of antimalarial drugs was
checked by biochemical analysis (liver and kidney function tests) on Day 7 for G1 and G2 mice and on Day 10
and Day 28 for G3 to G6 mice. The biochemical kits used
for assays were manufactured by M/s. Reckon Diagnostic Pvt. Ltd. and M/s. Span Diagnostic Ltd. Blood was
collected by tail vein incision of mice from each group.
Unhaemolyzed serum was collected and diluted with 0.9%
saline.
Statistical analysis
Data have been presented as mean and standard deviation (SD). Statistical evaluation of differences between
the experimental groups was determined by the Students
t-test with the level of significance of p <0.05.
RESULTS
In vivo antiplasmodial efficacy of Nd 30 and Nd 200
All the mice of infected control (G2) died by Day 9
(Fig. 1a). Mice of G3 negative control also exhibited normal course of infection with 31.623.37% infection on
Day 7 after which all the mice died within Day 10 (Fig.
1b) showing that vehicle (nascent alcohol) itself has no
effect in clearing the rodent malaria parasite (Table 1).
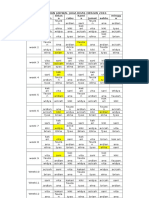
Table 1. Parasitaemia and chemosuppression along with mean survival time period of various experimental groups
Groups
(n=6)
Dosage (0.2 ml OD/Day/mouse)
i.p. infection of 1106 infected RBCs
Parasitaemia
(%) on Day 7
G1
G2
G3
G4
G5
G6
Distilled water (infected D0) at
Distilled water (infected D0)
Nascent alcohol (1:2)
CQ (20 mg/kg), infected on D0
Nd 30 (D0D3), infected on D0
Nd 200 (D0-D3), infected on D0
30.44
31.62
0.6
3.95
18.88
3.40
3.37
0.3*
0.9*
1.31*
Chemosuppression
(Day 7)
96.7
87.02
37.97
Mean survival
time (days)
8.55
8.83
28
18.5
16.5
0.83
1.03
0
2.16
1.37
Note: All the groups except G1 were injected with 1 106 infected RBC on Day 0; Data are given as mean SD. p-value in comparison to
infected control (G2 group) is shown as *extremely statistically significant (p <0.0005).
74
J Vector Borne Dis 49, June 2012
(a)
M1
M3
M2
M6
M5
M4
chemosuppression and MST of 28 days which was maximum among the treated groups.
The infection observed in G5 group (Nd 30) was
1.020.13% on Day 5 which increased to 3.950.9%
(p <0.0005) by Day 7 with 87.02% chemosuppression.
The parasitaemia further increased to 14.690.73% and
only one mouse survived till Day 21 (Fig. 2a) showing
MST of 18.52.16 days. In G6 group (Nd 200),
parasitaemia on Day 5 was 1.470.43% which increased
to 18.181.31% by Day 7, followed by decrease in
parasitaemia to 16.092.41% on Day 14 (Fig. 2b). In this
group also, only one mouse survived till Day 21. Average
chemosuppression was 37.97% and mean survival time
was 16.51.37 (p <0.0005) days which was lowest among
the treated groups but significantly higher than the MST
of infected control.
MEAN+SD
Parasitaemia (%)
55
50
45
40
35
30
25
20
15
10
5
0
Day of infection
(b)
M1
45
M2
M3
M4
M6
M5
MEAN+SD
40
Parasitaemia (%)
35
Biochemical assays
The alkaline phosphatase (ALP) activity of enzyme
in sera of normal mice was recorded to be 7.330.98 KA.
It increased significantly in the infected mice 35.274.69
30
25
20
15
10
(a)
5
3
0
M1
(c)
30
M2
Day of infection
M3
M4
M5
6
M6
MEAN+SD
20
M2
M4
M5
M6
MEAN+SD
14
12
10
8
6
4
2
15
10
(b)
5
M1
M2
Day of infection
M3
M4
M5
14
M6
21
MEAN+SD
30
14
Day of infection
21
28
Fig. 1: Graph showing course of infection in BALB/c mice (G2
group) infected with 1106 P .berghei parasitized red blood
cells : (a) treated with nascent alcohol (G3 group); (b)
chloroquine (G4 group); and (c) Data expressed as
MeanSD of six mice. Parasitaemia (%) of G2 group =
30.443.40, G3 group = 31.62 3.37 on Day 7; and G4 =
0.60.3, 2.31 and 0.240.2 on Days 7, 14 and 28
respectively.
In group G4 (CQ 20 mg/kg), the parasitaemia was
0.340.1% on Day 5 which continuously increased up to
2.31% by Day 14 after which the parasitaemia declined
to 0.24 0.2% on Day 28 (Fig. 1c). CQ exhibited 96.7%
Parasitaemia (%)
M3
16
25
Parasitaemia (%)
M1
18
Parasitaemia (%)
25
20
15
10
5
0
Day of infection
14
21
Fig. 2: Graph showing course of infection in BALB/c mice treated
with Nosode 30 (G5 group): (a) Nosode 200 (G6 group);
and (b) Data expressed as MeanSD of six mice.
Parasitaemia (%) of G5 group = 3.950.9, 14.69; G6 group =
18.181.31, 16.092.41 on Days 7 and 14, respectively.
75
Bagai et al: Homeopathy against malaria
Table 2. Alterations in ALP activity, bilirubin concentration, SGOT activity, SGPT activity, concentration of urea and creatinine in
various experimental groups on Day 7 and Day 10
Group
G1 (D 7)
G2 (D 7)
G3 (D 7)
G4 (D 10)
(D 28)
G5 (D 10)
G6 (D 10)
ALP
(KA units)
7.33
35.27
34.34
12.3
6.6
12
28.84
0.98
4.69
5.41
1.3***
2.5***
4.45***
3.21*
Bilirubin
(mg/dl)
0.65
2.31
1.87
1.78
1.5
1.10
2.29
0.27
0.31
0.12
0.2**
0.11***
0.21***
0.23#
SGOT
activity (U/l)
13.68
76.46
80
44
23
47.05
56.46
0.55
0.82
12.24
5.02***
4.3***
4.06***
9.54***
SGPT
activity (U/l)
29
133.19
131.05
60
58
87.23
128.63
Urea
(KA units)
0.2
3.09
6.12
3.8***
6.2***
8.82***
1.2*
32.0
62.6
74.05
59.3
52
73.33
106.66
1.05
2.25
10.47
3.3#
6.2**
5.22***
9.81***
Creatinine (mg/dl)
1.04
4.57
4.49
5.5
4.1
2.04
2.34
0.18
0.18
0.08
1.02#
0.3*
0.30***
0.16***
Note: Data are given as meanSD; p-value in comparison to infected control (G2) is shown as ***extremely statistically significant
(p<0.0005), **very statistically significant (p <0.005), *statistically significant (p <0.05), #not statistically significant (p >0.05) .
KA which was five times the normal value. Similar activity was found in G3 group (34.345.41 KA). A significant decrease in ALP activity was observed in G4 group
by the Day 28 (6.62.5 KA) as compared to Day 10
(12.31.3 KA). In G6 group, ALP activity was maximum,
i.e. 28.843.21 KA followed by G5 group (124.45 KA)
on Day 10. Serum bilirubin level was also found to be
increased in G2 group (2.310.31mg/dl) and G3 group
(1.870.12 mg/dl) as compared to G1 group (0.650.27
mg/dl). The concentration of bilirubin was maximum in
G6 group (2.290.23 mg/dl) followed by G4 and G5
groups. In G4 group, the bilirubin concentration decreased
from 1.780.2 mg/dl on Day 10 to 1.50.11 mg/dl on
Day 28 (Table 2).
Serum glutamate oxaloacetate transaminase (SGOT)
activity was found to be 13.680.55 U/l in G1 group while
in G2 and G3 groups it was increased more than six times,
i.e. 76.46 0.82 U/l and 8012.24 U/l respectively. In
G4 group, SGOT activity was 445.02 U/l on Day 10
and 234.3 U/l on Day 28. SGOT activity was observed
maximum in G6 group (56.469.54 U/l), followed by G5
group (47.054.06 U/l). Serum glutamate pyruvate transaminase (SGPT) activity was also found five times more
in G2 (133.193.09 U/l) and G3 (131.056.12 U/l) than
G1 (29.00.20 U/l). SGPT activity was found maximum
in G6 group (128.631.2 U/l), followed by G5 group
(87.238.82 U/l), G4 group (603.8 U/l on Day 10 and
586.2 U/l on Day 28).
In G1 group the level of serum urea was determined
to be 32.01.05 mg/dl which increased two fold to 62.6
2.25 mg/dl in G2 group than normal value. In positive
control, there was decrease in concentration of urea on
Day 10 from 59.33.3 mg/dl to 526.2 mg/dl on Day 28.
Serum urea was found maximum in G6 group (106.66
9.81 mg/dl) followed by G5 group (73.335.22 mg/dl).
Increased creatinine concentration is an indicative of re-
nal diseases which was evident in G2 group (4.570.18
mg/dl) and G3 group (4.49 0.08 mg/dl) as compared to
normal mice (1.04 0.18 mg/dl). Concentration of creatinine in G4 group was 5.5 1.02 mg/dl on Day 10 which
decreased to 4.1 0.3 mg/dl on Day 28. Its concentration
was 2.34 0.16 mg/dl in G6 group and 2.04 0.30 mg/dl
in G5 group.
DISCUSSION
The antimalarial chemotherapy is the keystone of
malaria control efforts. But the major problem to the use
of antimalarial drugs is resistance developed by the parasite5. Homeopathy offers more affordable and safer approach to disease management. In the present study,
antiplasmodial efficacy of homeopathic drugs Nd 30 and
Nd 200 has been evaluated in vivo.
Lethality of P. berghei to mice has been reported by
many workers6. P. berghei preferentially invades reticulocytes79 and its infection is associated with mortality rates
which are confirmed in the present study too. When vehicle (nascent alcohol) was administered to BALB/c mice
the parasitaemia on Day 7 was comparable to infected
control group, indicating that vehicle does not provide any
protection and have no placebo effect. The homeopathic
medicines have been shown effective than placebo controls in 60 (43.5%) findings of 138 randomized controlled
trials till 2008. In drug treated groups, the chemosuppression of Nd 30 was 87.02% on Day 7 which was
higher than Nd 200 treated group. The mean survival time
period was also more in Nd 30 (18.52.16 days).
This observation is in accordance with the earlier studies where 30 potency of homeopathic drugs China, Chelidonium and Artemisia vulgaris were found to be very
effective against rodent malaria parasite exhibiting maximum chemosuppression and enhancement of mean sur-
76
J Vector Borne Dis 49, June 2012
vival time of mice1013. According to the Hahnemann, any
disease may remain unaffected by the lowest potency,
whereas, higher potency probably is too powerful which
may cause adverse effect, so use of correctly selected
medium potency may prove more effective14. It has been
reported that Cinchona officinalis (China) can be taken
as prophylactic drug in a 30 C dose weekly prior to entering a malarial zone15. All these findings establish that the
30 potency of homeopathic drug formulations is most
effective against the malaria parasite as compared to lower/
higher potencies which is observed in the present study
too.
In positive control (CQ 20 mg/kg) on Day 7, chemosuppression was 96.7% and mean survival time was 28
days which was again in accordance with the earlier studies in which mice inoculated with 1105, 1106, 1107
pRBC and then treated with chloroquine (20 mg/kg)
showed a marked effect with the mean survival more than
28 days16 .
The functioning of liver and kidney was also checked
by measuring the levels of serum alkaline phosphatase
activity, concentration of bilirubin, SGOT activity, SGPT
activity, urea and creatinine concentration. The increased
serum ALP activity among patients indicate that the liver
stage of malaria infection accompanied by perturbation
of the host hepatocytes membrane leading to leakage of
this enzyme out of liver cells17. In the present study also,
the activity of serum alkaline phosphatase in G2 (35.27
4.69 KA) and G3 (34.345.41 KA) groups was increased
twice in comparison to normal mice (7.330.98 KA). In
positive control, it was 12.31.3 KA on Day 10 which
decreased to 6.62.5 KA on Day 28. Studies have shown
that chloroquine affects a wide range of biochemical processes including inhibition of key metabolic enzymes such
as alcohol dehydrogenase, succinate dehydrogenase and
glucose-6-phosphate dehydrogenase18,19. ALP activity was
maximum in G6 (28.843.21 KA) group, followed by G5
group (124.45 KA) almost comparable amount of ALP
activity to normal mice prompting the safety of homeopathic formulation for liver of host.
Serum bilirubin concentration (>3 mg/dl) is a common feature attributed in part to liver damage and
haemolysis of parasitized and non-parasitized cells20. In
infected control, bilirubin concentration was observed to
rise four times as compared to normal. While in chloroquine treated group bilirubin concentration was 1.780.2
mg/dl. The serum bilirubin levels were observed to increase in all treated groups indicating jaundice like symptoms.
The ratio of AST to ALT is useful in differentiating
between causes of liver damage21,22. SGOT activity in-
creased six times in infected control and vehicle treated
group than the normal control. In G4 group, SGOT activity was decreased by Day 28 which was comparable to
normal value. The results of the present study revealed a
significant increase of serum transaminases. The elevation during acute infection results in necrosis of hepatic
cells. These enzymes are released into the circulation with
consequent rise in the serum levels2325. SGPT activity
was observed to rise in all treated groups. In chloroquine
treated (G4) group also, considerable increase in SGPT
activity was recorded.
Serum urea and creatinine concentration are used for
the assessment of renal sufficiency26. There was significant increase in serum urea and creatinine in infected control as compared to normal. Higher levels of serum urea
and creatinine are indications of deficiency in renal function2729. All the treated groups recorded increase in serum urea levels. Chloroquine administration is also reported to impair kidney function, resulting inappropriate
Na+ and Cl retention30. In the present study also, the creatinine levels were also considerably elevated in CQ treated
group indicating impairment of kidney function. In treated
groups, the increase in creatinine concentration was less
as compared to P. berghei infected mice.
CONCLUSION
These findings suggest that chemosuppression observed in Nd 30 treated group is considerable. Further
studies are needed to establish Malaria Co Nosode 30 (Nd
30) as potent antimalarial in monotherapy or in combination therapy with other homeopathic formulations.
ACKNOWLEDGMENTS
The authors are grateful to the UGC-CAS programme
of the Department of Zoology, Panjab University,
Chandigarh for the financial assistance.
REFERENCES
1.
2.
3.
4.
Khuda-Bukhsh AR. Towards understanding molecular mechanisms of action of homeopathic drugs: an overview. Mol Cell
Biochem 2003; 253: 33945.
Birch K. Vaccine free prevention and treatment of infectious
contagious disease with homeopathy. USA: Trafford Publishing 2007; p. 3619.
Rajan A, Bagai U. SEM studies on blood cells of Plasmodium
berghei infected Balb/c mice treated with artesunate and homeopathic medicine China. J Parasit Dis 2011; 35(2): 1349.
Santiyanont R. Parasite identification, counting and staining,
application of genetic engineering techniques in tropical diseases pathogen, with special reference to Plasmodia. A laboratory manual of selected techniques. Bangkok, Thailand : UNDP/
Bagai et al: Homeopathy against malaria
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
World Bank/WHO special programme for research and training
in tropical disease 1985; 87(7): 4138.
Warhurst D. New developments: Chloroquine resistance in Plasmodium falciparum. Drug Resist Update 2001; 4: 141.
Miller LH, Carter R. Innate resistance in malaria. Exp Parasitol
1976; 40: 13246.
Janse CJ, Boorsma EG, Ramesar J, Grobbe MJ, Mas B. Host
cell specificity and schizogony of P. berghei under different in
vitro conditions. Int J Parasitol 1989; 19: 50914.
Galinski MR, Medina CC, Ingranallo P, Barnwell JW. A reticulocyte binding protein complex of P. vivax merozoites. Cell 1992;
69(7): 121326.
Martinelli A, Rodrigues LA, Cravo P. Plasmodium chabaudi:
Efficacy of artemisinin + curcumin combination treatment on a
clone selected for artemisinin resistance in mice. Exp Parasitol
2008; 119(2): 3037.
Bagai U, Rajan A. Efficacy of artesunate and homeopathic drug
China alone and in combination against Plasmodium berghei
infection in mice. XII International conference on parasitology, August 1520, 2010, Melbourne, Australia, 2001; ABSSMC8F46-KTMHS-CM88N.
Rajan A, Bagai U. Evaluation of antiplasmodial efficacy and
safety of Cinchona officinalis (China) against lethal murine
malaria parasite. Am J Homeo Med 2012; [In press].
Rajan A, Bagai U. Effect of homeopathic medicine Chelidonium against blood stage infection of rodent malaria parasite.
Advances in parasitology: A novel approach towards a disease
free world. Proceedings of 22nd National Congress of Parasitology, October 30 November 1, 2010. Kalayani: University of
Kalyani, West Bengal, India 2011; p. 2331.
Bagai U, Kalia S, Sharma I, Walter NS. Antimalarial efficacy
of homeopathic drugs Artemisia vulgaris and Curcuma longa
against Plasmodium berghei infection in Balb/C mice. Panjab
Univ Res J (Sci) 2012; 61 [Accepted].
Wijk MV. Importance of the right potency: Role of potency selection in homeopathy. Homeopathy Everyone 2012; 9(5): 234.
Shah H. Malaria and homeopathy. India : Mayur Jain, Indian
Book and Periodical Publisher 1999; p. 1233, ISBN 81-74670572.
Ishih A, Suzuki T, Muregi FW, Matsuki K, Terada M. Chloroquine efficacy in Plasmodium berghei NK-65 infected ICR mice
with reference to the influence of initial parasite load and start-
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
ing day of drug administration on the outcome of treatment.
South East Asian J Trop Med Public Health 2006; 37(1): 137.
Garba IH, Ubom G. Serum alkaline phosphatase activity as a
potential biomarker for the integrity of the hepatic drainage system in acute falciparum malaria infection. Int J Infect Dis 2005;
4(2). DOI: 10.5580/b42.
Emerole Go, Thabrew MI. Changes in some rat hepatic microsomal components induced by prolonged administration of chloroquine. Biochem Pharmacol 1983; 32: 30059.
Dass EE, Shah KK. Paracetamol and conventional antimalarial
drugs induced hepatotoxicity and its protection by methionine
in rats. Int J Exp Biol 2000; 38: 113842.
Wilairatana P, Looareesuwan S, Charoenlarp P. Liver profile
changes and complications in jaundiced patients with falciparum
malaria. Trop Med Parasitol 1994; 45: 298302.
Nyblom H, Berggren U, Balldin J, Olsson R. High AST/ALT
ratio may indicate advanced alcoholic liver disease rather than
heavy drinking. Alcohol 2004; 39(4): 3369.
Nyblom H, Bjornson E, Simren M, Aldenborg F, Almer S. The
AST/ALT ratio as an indicator of cirrhosis in patients with PBC.
Liver Int 2006; 26(7): 8405.
Wroblewski F, La Due JS. Serum glutamic oxaloacetic transaminase activity as an index of liver cell injury from cancer. A
prelim report. Cancer 1955; 8: 115563.
Molander DW, Sheppard E, Payne MA. Serum transaminase in
liver disease. J Am Med Assoc 1957; 163: 14615.
Zelman S, Wang CC, Appelhanz I. Transaminases in needle
aspiration biopsies. Am J Med Sci 1959; 237: 32333.
Smith GL, Shlipak MG, Havranek EP, Foody JM, Masoudi FA.
Serum urea, nitrogen, creatinine and estimators of renal function. Arch Int Med 2006; 166(10): 113442.
Narayanan S, Appleton HD. Creatinine: A review. Clin Chem
1980; 26(8): 111926.
Mouton R, Holder K. Laboratory tests of renal function. Anaes
Int Care Med 2006; 7(7): 2403.
Whelton A, Watson AJ, Rock RC. Nitrogen metabolites and
renal function. In: Teitz textbook of clinical chemistry. Burtis
CA, Ashwood ER, editors. London: WB Saunders Company
1994; p. 1528.
Musabayane CT, Nidhlovu CE, Balmet RJ. The effects of oral
chloroquine administration on kidney function. Renal failure
1994; 16(2): 2218.
Correspondence to: Dr Upma Bagai, Associate Professor, Department of Zoology, Panjab University, Chandigarh160 014, India.
E-mail: upmabagai@yahoo.co.in
Received: 19 October 2011
77
Accepted in revised form: 28 May 2012
You might also like
- Evaluation of The Antimalarial Activity of The Aqueous Leaf Extract of Gossypium Barbadense (Malvaeceae) in MiceDocument3 pagesEvaluation of The Antimalarial Activity of The Aqueous Leaf Extract of Gossypium Barbadense (Malvaeceae) in MiceDrugs & Therapy StudiesNo ratings yet
- Antibact AssayDocument7 pagesAntibact Assaymakerk82No ratings yet
- Article1401275147 - Shah Et AlDocument6 pagesArticle1401275147 - Shah Et AlGustavo Gutiérrez GómezNo ratings yet
- Tmp5a61 TMPDocument8 pagesTmp5a61 TMPFrontiersNo ratings yet
- Ding Et AlDocument4 pagesDing Et AlNguyễn Quang HiếuNo ratings yet
- Bacteraemia Endocarditis PDFDocument13 pagesBacteraemia Endocarditis PDFnirmacandradewiNo ratings yet
- Immunomodulatory and in Vivo Antiplasmodial Activities of Propolis ExtractsDocument4 pagesImmunomodulatory and in Vivo Antiplasmodial Activities of Propolis ExtractsPanggih SaputroNo ratings yet
- Aps 200752Document6 pagesAps 200752Recky PatalaNo ratings yet
- Immunocytotoxic Effect of Aqueous Leaf Extract of Cassia Occidentalis On Human Peripheral Blood Mononuclear Cells and NeutrophilsDocument7 pagesImmunocytotoxic Effect of Aqueous Leaf Extract of Cassia Occidentalis On Human Peripheral Blood Mononuclear Cells and NeutrophilsUMYU Journal of Microbiology Research (UJMR)No ratings yet
- Brown 2012Document9 pagesBrown 2012mcs.vet8473No ratings yet
- A. Crassicauda, M. Eupeus and H. Lepturus Scorpion Venoms Initiate A Strong in Vivo Anticancer Immune Response in CT26-tumor Mice ModelDocument8 pagesA. Crassicauda, M. Eupeus and H. Lepturus Scorpion Venoms Initiate A Strong in Vivo Anticancer Immune Response in CT26-tumor Mice ModelJuan Nicolas Perez GarzonNo ratings yet
- Jiw 632Document10 pagesJiw 632Robert StryjakNo ratings yet
- Longevity Effect of Liuwei Dihuang in Both: Caenorhabditis Elegans and Aged MiceDocument14 pagesLongevity Effect of Liuwei Dihuang in Both: Caenorhabditis Elegans and Aged Micemeltwithsnow163.comNo ratings yet
- Vitellaroside A New Cerebroside From Vitellaria Paradoxa Sapotaceae and Its Bioactivities 2475 7675 1000306Document9 pagesVitellaroside A New Cerebroside From Vitellaria Paradoxa Sapotaceae and Its Bioactivities 2475 7675 1000306p6trqpc4qkNo ratings yet
- tmpFB45 TMPDocument6 pagestmpFB45 TMPFrontiersNo ratings yet
- The Effect of Standarized Extract Pegagan Embun (Hydrocotyle Sibthorpioides Lam.) On Total Leukocyte and Percentage Leukocytes in Male White Mice Exposed To H5N1 Virus AntigenDocument5 pagesThe Effect of Standarized Extract Pegagan Embun (Hydrocotyle Sibthorpioides Lam.) On Total Leukocyte and Percentage Leukocytes in Male White Mice Exposed To H5N1 Virus AntigenInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Proposal RawDocument12 pagesProposal RawSedem StanisloveNo ratings yet
- Penyebab Baru OsteomyelitisDocument3 pagesPenyebab Baru OsteomyelitisIka Benny Kartika SariNo ratings yet
- A Dried Yeast Fermentate Prevents and Reduces InflammationDocument8 pagesA Dried Yeast Fermentate Prevents and Reduces InflammationsteeljackNo ratings yet
- International Journal For Parasitology: Drugs and Drug ResistanceDocument11 pagesInternational Journal For Parasitology: Drugs and Drug Resistancemohammad khazarNo ratings yet
- S U R J S S: Indh Niversity Esearch Ournal (Cience Eries)Document8 pagesS U R J S S: Indh Niversity Esearch Ournal (Cience Eries)Imam HasanNo ratings yet
- IMM 265 - Galley Proof - 5may21 - VelikkakamDocument13 pagesIMM 265 - Galley Proof - 5may21 - VelikkakamSoraya Torres GazeNo ratings yet
- Desmodium Adscen (Manayupa)Document8 pagesDesmodium Adscen (Manayupa)Anonymous NEJodF0HXqNo ratings yet
- New Horizons in Pharmaceutical & Biomedical SciencesDocument360 pagesNew Horizons in Pharmaceutical & Biomedical SciencesPrema PérezNo ratings yet
- Safety and Activity of The Immune Modulator HE2000 On The Incidence of Tuberculosis and Other Opportunistic Infections in AIDS PatientsDocument3 pagesSafety and Activity of The Immune Modulator HE2000 On The Incidence of Tuberculosis and Other Opportunistic Infections in AIDS PatientsJosueNo ratings yet
- Tiostop Et Al. 2023-InvestChemPharmaDocument10 pagesTiostop Et Al. 2023-InvestChemPharmaArmel J. SeukepNo ratings yet
- 10126-Article Text-75914-1-10-20181208Document5 pages10126-Article Text-75914-1-10-20181208Odessa EnriquezNo ratings yet
- Adverse Effects of Incorporating Ketoprofen Into Established Rodent StudiesDocument11 pagesAdverse Effects of Incorporating Ketoprofen Into Established Rodent StudiesVivi FatimatuzzuhroNo ratings yet
- Sambiloto 4Document8 pagesSambiloto 4Radiksa AzryNo ratings yet
- Evaluation of Antihyperlipidemic, Anti-Inflammatory, and Analgesic Activities of Eurycoma Longifolia in Animal ModelsDocument4 pagesEvaluation of Antihyperlipidemic, Anti-Inflammatory, and Analgesic Activities of Eurycoma Longifolia in Animal Modelsmendal sciNo ratings yet
- Assessment of Selected Yemeni Medicinal Plants For Their in Vitro Antimicrobial, Anticancer and Antioxidant ActivitiesDocument11 pagesAssessment of Selected Yemeni Medicinal Plants For Their in Vitro Antimicrobial, Anticancer and Antioxidant ActivitiesvalvemayamNo ratings yet
- Antioksidan Ic50Document13 pagesAntioksidan Ic50Prapti ChantiqueNo ratings yet
- Jurnal PendukungDocument5 pagesJurnal PendukungAulia SabriaNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- ManuscriptDocument7 pagesManuscriptndumanyachisom23No ratings yet
- Abstract 1-DubaiDocument1 pageAbstract 1-DubaipelinNo ratings yet
- Clinical Trial: Effectiveness of Lactobacillus Rhamnosus (Strains E N, Oxy and Pen) in The Prevention of Antibiotic-Associated Diarrhoea in ChildrenDocument8 pagesClinical Trial: Effectiveness of Lactobacillus Rhamnosus (Strains E N, Oxy and Pen) in The Prevention of Antibiotic-Associated Diarrhoea in ChildrenBryan Paul RamirezNo ratings yet
- Safdar Et Al 2004 in Vivo Pharmacodynamic Activity of DaptomycinDocument6 pagesSafdar Et Al 2004 in Vivo Pharmacodynamic Activity of DaptomycinduongnguyenNo ratings yet
- Investigation of Immunomodulatory Potential of Methanolic and Hexane Extract of Musa Acuminate Peel (Plantain) ExtractsDocument6 pagesInvestigation of Immunomodulatory Potential of Methanolic and Hexane Extract of Musa Acuminate Peel (Plantain) ExtractsDelyana Fitria DewiNo ratings yet
- Κινέζικο ματζούνιDocument4 pagesΚινέζικο ματζούνιAndreas TassopoulosNo ratings yet
- 1 12Document5 pages1 12Eriques Goncalves SilvaNo ratings yet
- Pelagia Research Library: Evaluation of Ulcer Protective Effects of Ocimum Sanctum and ZingiberDocument8 pagesPelagia Research Library: Evaluation of Ulcer Protective Effects of Ocimum Sanctum and ZingiberYaseen GiganiNo ratings yet
- Acute and Sub-Chronic (28-Day) Oral Toxicity Studies of Hydroalcohol Leaf Extract of Ageratum Conyzoides L (Asteraceae)Document5 pagesAcute and Sub-Chronic (28-Day) Oral Toxicity Studies of Hydroalcohol Leaf Extract of Ageratum Conyzoides L (Asteraceae)Hendry RaoNo ratings yet
- Fungi: Initial Results of The International Efforts in Screening New Agents Against Candida AurisDocument7 pagesFungi: Initial Results of The International Efforts in Screening New Agents Against Candida AurisYY CheungNo ratings yet
- AHPND PhagePublication2 2017Document5 pagesAHPND PhagePublication2 2017jtosuna01No ratings yet
- Ahmed 2013Document5 pagesAhmed 2013sii nuriantiNo ratings yet
- GJHS 5 150Document5 pagesGJHS 5 150Wisnu Aditya WardanaNo ratings yet
- 2016 Is Hyperbaric Oxygen or Ozone Effective in Experimental Endocarditis?Document5 pages2016 Is Hyperbaric Oxygen or Ozone Effective in Experimental Endocarditis?Acupuntura de EquinosNo ratings yet
- Volume Probiotic Adjuvant Therapy Chronic Urticaria 4842allasp1Document8 pagesVolume Probiotic Adjuvant Therapy Chronic Urticaria 4842allasp1fatima amaliaNo ratings yet
- Speman 056Document3 pagesSpeman 056mohd_ikrayemNo ratings yet
- Evaluation of Vaccine Immunogenic Activity Against ClostridiosisDocument3 pagesEvaluation of Vaccine Immunogenic Activity Against ClostridiosisAcademic JournalNo ratings yet
- Ganoderma Lucidum Extract Inhibit Proliferation of SW480 Human Colorectal Cancer CellsDocument5 pagesGanoderma Lucidum Extract Inhibit Proliferation of SW480 Human Colorectal Cancer CellsGandalfNo ratings yet
- 10 5798-Dicletip 1086124-2303017Document9 pages10 5798-Dicletip 1086124-2303017Rawaz Mahammad RasulNo ratings yet
- Antigen Op 29Document13 pagesAntigen Op 29Gabriel AvilaNo ratings yet
- Antibiotic Resistance Pattern in Pseudomonas Aeruginosa Species Isolated at A Tertiary Care Hospital, AhmadabadDocument4 pagesAntibiotic Resistance Pattern in Pseudomonas Aeruginosa Species Isolated at A Tertiary Care Hospital, AhmadabadDrashua AshuaNo ratings yet
- The Scientific World Journal, 2020 - ER - CompressedDocument14 pagesThe Scientific World Journal, 2020 - ER - CompressederlidawatiNo ratings yet
- Espondilodiscitis Infecciosa Por Patógenos Poco ComunesDocument5 pagesEspondilodiscitis Infecciosa Por Patógenos Poco ComunesOthoniel RamirezNo ratings yet
- AACR 2022 Proceedings: Part A Online-Only and April 10From EverandAACR 2022 Proceedings: Part A Online-Only and April 10No ratings yet
- Potential Antiviral Agents for Coronaviruses: Compounds, Herbal Products, and Drug TargetsFrom EverandPotential Antiviral Agents for Coronaviruses: Compounds, Herbal Products, and Drug TargetsNo ratings yet
- Garlic (Allium sativum): Monograph on a herb reputed to be medicinalFrom EverandGarlic (Allium sativum): Monograph on a herb reputed to be medicinalNo ratings yet
- Jurnal Anak RirinDocument10 pagesJurnal Anak RirinDexter BluesNo ratings yet
- Fix ObgynDocument17 pagesFix ObgynDexter BluesNo ratings yet
- The Seven Cardinal MovementsDocument4 pagesThe Seven Cardinal MovementsDexter BluesNo ratings yet
- Referat Obgyn FixDocument29 pagesReferat Obgyn FixDexter BluesNo ratings yet
- Rincian Jadwal Jaga Koas Obsgin 2016 Senin Selas A Rabu Kami S Jumat Sabtu Mingg UDocument1 pageRincian Jadwal Jaga Koas Obsgin 2016 Senin Selas A Rabu Kami S Jumat Sabtu Mingg UDexter BluesNo ratings yet
- 1830 PDF PDFDocument5 pages1830 PDF PDFDexter BluesNo ratings yet
- UlnarClubHandweb PDFDocument2 pagesUlnarClubHandweb PDFDexter BluesNo ratings yet
- Ngeo2472 s1 PDFDocument4 pagesNgeo2472 s1 PDFDexter BluesNo ratings yet
- Aerobic and Anaerobic ExercisesDocument3 pagesAerobic and Anaerobic ExercisesBonak na BataNo ratings yet
- ROJoson PEP Talk: RUQ Abdominal Pain and Gallbladder DisordersDocument80 pagesROJoson PEP Talk: RUQ Abdominal Pain and Gallbladder DisordersrojosonNo ratings yet
- Indices MeasuringDocument27 pagesIndices Measuringdinesh11rNo ratings yet
- Clinical Evaluation FormDocument1 pageClinical Evaluation FormAndalNo ratings yet
- Employee HealthDocument3 pagesEmployee HealthkrishkeshwalaNo ratings yet
- Summary and Conclusions: Urinary Biomarkers in Experimental DiabetesDocument1 pageSummary and Conclusions: Urinary Biomarkers in Experimental DiabetesNikesh DoshiNo ratings yet
- Final Osce Care PlanDocument8 pagesFinal Osce Care Planapi-526590140100% (1)
- Physical Education SBA G.GajieDocument29 pagesPhysical Education SBA G.Gajieselina fraser83% (6)
- Jurnal Plasenta PreviaDocument10 pagesJurnal Plasenta Previadiah_201192No ratings yet
- The Benefits of Immunotherapy CombinationsDocument1 pageThe Benefits of Immunotherapy CombinationsMicheleFontanaNo ratings yet
- CHEDDA's Textbook of PaediatricsDocument546 pagesCHEDDA's Textbook of Paediatricsbrij bhushan kumarNo ratings yet
- Pathophysiology On Liver CirrhosisDocument38 pagesPathophysiology On Liver CirrhosisYogi AnjasmaraNo ratings yet
- Gabapentin FDADocument37 pagesGabapentin FDAAnish NairNo ratings yet
- Virani Et Al 2021 Heart Disease and Stroke Statistics 2021 UpdateDocument490 pagesVirani Et Al 2021 Heart Disease and Stroke Statistics 2021 UpdatehendridunantikoNo ratings yet
- 03 NCP 5 Pulmonary Tuberculosis LalitDocument17 pages03 NCP 5 Pulmonary Tuberculosis Lalitamit100% (2)
- Marc A. Levitt: AuthorDocument16 pagesMarc A. Levitt: AuthorAlonso Rodriguez EscobedoNo ratings yet
- A Silent KillerDocument3 pagesA Silent KillerLinhNguyeNo ratings yet
- Janet RowleyDocument1 pageJanet RowleyANA GABRIELA PEREZ VIDALNo ratings yet
- ProQuestDocuments 2023 04 26Document3 pagesProQuestDocuments 2023 04 26Adriana Salazar MonjaNo ratings yet
- Alcoholism and Native AmericansDocument3 pagesAlcoholism and Native AmericansGary DeMonteNo ratings yet
- Iowa Neonatology HandbookDocument11 pagesIowa Neonatology HandbookLowelly napitupuluNo ratings yet
- Social Change Campaign in IndiaDocument7 pagesSocial Change Campaign in IndiaGauri GargNo ratings yet
- Heart DiseaseDocument40 pagesHeart DiseaseAhmer TahirNo ratings yet
- D Dimer Test in VTEDocument35 pagesD Dimer Test in VTEscribmedNo ratings yet
- Electrocardiogram: What Is An ECG?Document8 pagesElectrocardiogram: What Is An ECG?Ali dhyaa100% (1)
- Reviewer RenalDocument13 pagesReviewer Renalsean blaze100% (1)
- Normal Spontaneous DeliveryDocument4 pagesNormal Spontaneous Deliveryvivian magnoNo ratings yet
- 2014 09 - LOINC Tutorial - ImagingDocument34 pages2014 09 - LOINC Tutorial - ImagingDaniel VreemanNo ratings yet
- Assignment 10 χ²-test (B. V. Sc. & A.H. 2017 batch) Type A: χ² - Test of goodness of fitDocument7 pagesAssignment 10 χ²-test (B. V. Sc. & A.H. 2017 batch) Type A: χ² - Test of goodness of fitK0% (1)
- Rosh Review 11Document6 pagesRosh Review 11Sarwar BaigNo ratings yet