Professional Documents
Culture Documents
Coccidioidomicosis 1
Uploaded by
Angie TPOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Coccidioidomicosis 1
Uploaded by
Angie TPCopyright:
Available Formats
Disseminated Coccidioidomycosis in Pregnancy
Jody E. Hooper, MD; Qun Lu, MD; Samuel H. Pepkowitz, MD
Coccidioidomycosis is a fungal infection contracted
through the inhalation of airborne spores, which are most
frequently present in desert areas of the southwestern
United States and Mexico. Primary immune response to
infection is by TH1, a subset of helper T cells. Although
pulmonary symptoms are most common, hematogenous
systemic spread can also occur. Pregnancy is a well-noted
risk factor for disseminated Coccidioides infection. The objective of this review is to provide an overview of coccidioidomycosis and to review immunologic and hormonal
factors that increase risk of dissemination in pregnancy.
Dissemination may occur more frequently in pregnant patients than in nonpregnant women because of shifts in
T-cell immunity, changes in cytokine production, and increased hormone levels. There is disagreement regarding
the precise incidence of systemic spread in pregnancy, but
most sources agree that risk is substantially increased and
vigilance must be high in patients with exposures in endemic areas.
(Arch Pathol Lab Med. 2007;131:652655)
DISEASE CHARACTERISTICS AND DIAGNOSIS
Coccidioides immitis is a dimorphic fungus present in the
soil of desert areas of the southwestern United States and
Mexico, as well as parts of Central and South America.
Infection is acquired by inhalation of arthroconidia, or
spores, and exposure to dust in endemic areas produces
a higher incidence of the disease. Person-to-person transmission does not occur.
Coccidioides immitis grows as a septate hyphal form in
soil and creates spores, or arthroconidia, which are shed
easily into the air. When inhaled by animals or humans,
the arthroconidia form thick-walled spherules (parasitic
forms) within airways. Spherule division produces multiple endospores that, on release, will mature in situ into
additional spherules or will be reintroduced into the environment to begin the cycle again. In the human, endospores typically trigger a polymorphonuclear leucocyte response, which converts to a mononuclear cell infiltrate and
granuloma formation as infection becomes more chronic.1
Accepted for publication September 8, 2006.
From the Department of Pathology and Laboratory Medicine, CedarsSinai Medical Center (Drs Hooper and Pepkowitz), and the Department
of Pathology and Laboratory Medicine, UCLA Medical Center (Dr Lu),
Los Angeles, Calif.
The authors have no relevant financial interest in the products or
companies described in this article.
Reprints: Jody E. Hooper, MD, Department of Pathology and Laboratory Medicine, Cedars-Sinai Medical Center, 8700 Beverly Blvd, Los
Angeles, CA 90048 (e-mail: hooperj@cshs.org).
652 Arch Pathol Lab MedVol 131, April 2007
Diagnosis is made principally by serologic testing or by
identification of the organism in tissue. The tube precipitin-reacting antigen test is used to detect immunoglobulin
(Ig) M antibodies earliest in the disease course, and the
complement-fixing antigen test detects IgG antibodies,
which persist in chronic infections.2 Antibodies can be detected by immunodiffusion, enzyme-linked immunosorbent assay, or by complement fixation titers.3 The antibody
titer will fluctuate and can be used to follow the course of
the disease.2 Spherules and endospores may be detected
in tissues on hematoxylin-eosinstained slides and with
Gomori methenamine silver staining, or in cytologic specimens. Coccidioides can be cultured on most media.
DISEASE COURSE
Approximately 60% of patients infected with Cocciodioides will remain asymptomatic. The majority of the remaining patients will show mild-to-moderate flulike
symptoms including fever, cough, night sweats, chest pain,
fatigue, and sometimes arthralgia. Symptoms most frequently appear 1 to 3 weeks after inhalation of spores.
Presentation with pulmonary symptoms is most typical
and is frequently self-limited; however, 5% of patients
without sepsis or other complications will develop pulmonary nodules or cavitary lesions after the acute phase.2
Systemic spread of coccidioidomycosis is usually hematogenous and can involve bones, skin, soft tissues and, less
commonly, other solid organs such as the liver or kidneys.
Spread to the meninges is the most lethal form and carries
the highest risk of relapse. Septic shock can develop even
in immunocompetent patients; 8 patients with this complication who were followed from 1991 to 19934 showed
protracted courses of illness ending in 3 deaths in a 2-year
series from Kern County, California. Estimates of dissemination rates range from 1% to 7% to 22% in one series
from the Naval Medical Center, San Diego.5 Risk factors
for dissemination include African American or Filipino
race and immunocompromise resulting from human immunodeficiency virus, hematologic malignancy, and/or
chemotherapy.6,7 Although men in general are thought to
be at greater risk for disseminated disease, possibly because of more frequent environmental exposures, pregnant women are another well-recognized high-risk group.
COCCIDIOIDOMYCOSIS IN PREGNANCY AND
HOST IMMUNITY
Risk of disseminated disease in infected pregnant women has been cited as 40 to 100 times that of the general
population, or approximately 23% in the first trimester,
59% in the second trimester, and 68% in the third trimester.8 In a 1992 review compiling 90 reported cases from
Disseminated Coccidioidomycosis in PregnancyHooper et al
the literature, 61% of infected pregnant women showed
disseminated disease, with 34 of the 55 cases ending in
death.9 A more recent study in 2000 of 32 infected pregnant patients demonstrated only a 9% (3/32) dissemination rate, although it is important to note that this study
was conducted in an endemic area where diagnosis may
have been at earlier stages of disease than was present in
the previous study.3 However, this was still a substantial
increase compared with dissemination rates among women of reproductive age and in the general population. Amphotericin B was commonly, although not universally, prescribed for the pregnant women in this latter study and
there were no deaths among the cohort.
Host immunity is thought to greatly affect the largely
variable course of coccidioidomycosis, and as our case
study and subsequent discussion will show, this particularly may be true in the case of pregnant women. The
primary immune response to early infection by Coccidioides is cellular, with TH1, a subset of CD4-positive or helper
T cells, provoking release of interferon gamma, interleukin
2, and other proinflammatory cytokines.10 In contrast, another subset of helper T cells, TH2 cells, produce interleukin 4, 5, 9, 10, and other aids to humoral immunity. A
2005 study from Tucson, Ariz, showed CD4 T lymphocytes clustering in the mantle zones of fungal granulomata
with decreased expression of interferon gamma and interleukin 10, suggesting possible down-regulation of the
cellular immune response in coccidioidomycosis.11
Several different mechanisms have been proposed to explain the increased risk of Coccidioides dissemination in
pregnancy. Studies have shown that maternal T-cell responsiveness and patterns of T-cell immunity shift away
from a TH1 response during pregnancy to protect the fetus
and placenta from immunologic attack. Type 1 cytokines
associated with TH1 cells have been shown to inhibit
growth of trophoblast cells and may cause release of factors by macrophages, which could endanger the embryo.12
Increased levels of tumor necrosis factor-alpha (a TH1-associated cytokine) have anecdotally been associated with
pregnancy loss in mice by inducing ovarian hormonal failure.13 As previously explained, the principal response to
Coccidioides in immunocompetent patients utilizes an intact TH1 pathway. A 1991 study of 10 pregnant subjects
showed a decreased response to spherulin antigen in patients who had demonstrated prepartum coccidioidal immunity and little-to-no response in patients with active
infection.14 Elevated estrogen and progesterone levels may
also encourage production of TH2-associated cytokines or
block generalized cytokine production by lymphocytes.12
17--Estradiol has been shown to inhibit growth of myelomonocytic cells in vitro and progesterone to induce apoptosis of HL-60 promyelocytic cells, both possible contributions to changes in cellular immune function during
pregnancy.15 Elevated levels of both hormones have also
been proposed to directly stimulate growth of Coccidioides.6,11
NEONATAL INFECTION
Neonatal coccidioidomycosis rarely occurs. Fifteen cases
have been described in the literature, including the 2 most
recent, published in 1999. These 2 included one environmental exposure in a 23-day-old male infant and one maternal-fetal transmission to a 25-week premature female
infant whose mother developed pulmonary coccidioidomycosis in her 18th week. Her disease included placental
Arch Pathol Lab MedVol 131, April 2007
and cervical involvement and subsequently disseminated.
Placental involvement is so uncommon that the authors of
this last case theorize that spread might have occurred
through inhalation of amniotic fluid or placental rupture.16
CASE STUDY
A 27-year-old gravida 3, para 2 pregnant woman was
hospitalized at our institution at 26 weeks for disseminated coccidioidomycosis including diffuse pulmonary infiltrates and a lytic bone lesion in her iliac crest. In spite of
treatment with amphotericin B, the patient became ventilator-dependent, developed septic shock from coccidioidomycosis fungemia, and was found to have sustained a
fetal demise. Histologic examination of the placenta revealed coagulative necrosis of chorionic villi and an intense infiltration by neutrophils, lymphocytes, and plasma
cells in the intervillous space (Figure 1). Spherules filled
with round fungal endospores and scattered individual
sporangiospores of coccidioides were identified adjacent
to areas of placental infarction (Figures 2 and 3). Fetal
membranes and umbilical cord were without significant
inflammation. Unfortunately, autopsy of the fetus was declined by the family and thus determination could not be
made whether fungal infection was present. However, a
500-mL retroplacental hemorrhage (abruption) was found
at the time of emergent cesarean section, which could account for the fetal demise without postulating direct fetal
fungal infection. Postoperatively, the patient had an extremely complicated hospital course, with prolonged mechanical ventilation necessitating tracheostomy. Her disseminated spread of coccidioidomycosis necessitated partial internal hemipelvectomy, and irrigation and debridement of the right tibia and knee joint. After more than 7
weeks in the intensive care unit with extended treatment
with vancomycin and voriconazole, she was discharged
home.
The patient returned to our institution 18 months after
discharge complaining of headache. She reported multiple
gaps in her chronic fluconazole therapy and several recent
hospitalizations near her home for presumed Coccidioides
meningitis. Her cerebrospinal fluid Gram stain showed 1
neutrophils and 3 mononuclear cells, with a positive
Coccidioides IgG enzyme immunoassay test. The cerebrospinal fluid IgM enzyme immunoassay and culture were
negative. She was treated with high-dose fluconazole,
which resulted in clinical improvement and discharge
within 5 days, with follow-up lumbar puncture and bone
scan to be done within 2 to 4 months. Although she survived her disseminated infection, this patient will experience ongoing morbidity for many years to come, perhaps
for a lifetime.
CURRENT TREATMENT AND PROGNOSIS
It is possible that our patients survival, despite extensive dissemination and septic shock, was partly the result
of immunologic improvement accompanying the pregnancy loss. One of 3 pregnant patients described with disseminated disease in a 2000 study survived after elective termination.3 A 1996 series examining recovery from the immunosuppression of pregnancy showed that subsets of
CD4 and CD8 lymphocytes increased from 2 to 4 months
postpartum, although values were still lower than those
of comparable healthy women.17 A literature search revealed only one rheumatologic study (with a previous pilot study) examining cytokine markers for TH1 and TH2
Disseminated Coccidioidomycosis in PregnancyHooper et al 653
subsets postpartum, which showed undetectable levels
prepartum and postpartum.18 As unresponsive lymphocytes or inadequate numbers of certain subsets may lead
to disseminated coccidioidomycosis, treatments that stimulate the patients natural cellular immune response may
be particularly helpful in pregnant patients. Dendritic
cells can activate lymphocytes and encourage them to mature toward a TH1 pathway, as well as manufacturing cytokines to advance the immune response to an organism.
A 2002 study pulsed dendritic cells from infected patients and nonimmune individuals with coccidioidal antigen derived from spherules and demonstrated lymphocyte proliferation in response.19 Immune patients naturally
showed the strongest reaction, although anergic or previously nonresponsive patients with disseminated coccidioidomycosis also showed increases in lymphocytes after
exposure to the dendritic cells.
Studies are ongoing to develop a vaccine for Coccidioides
infection. As in the dendritic cell study mentioned previously, immunologic components of the cell wall of the fungus are being evaluated for their stimulatory protective
effects. Mice treated with a recombinant protein homolog
(-1,3-glucanosyltransferase) of Coccidioides posadasii
showed less fungal burden and better survival when exposed to lethal doses of the fungus in a 2003 study.20 As
the genome of C posadasii is sequenced, further epitopes
that will react with T cells may be identified and tested.21
In general, the use of amphotericin B greatly improves
maternal survival, decreasing mortality rates from 81% to
25% as cited in one review of the literature.11 Fluconazole
has also been utilized but its effect on maternal and fetal
mortality is less well documented. Therapeutic abortion is
not recommended in the current literature, even in pregnant patients with disseminated disease unless there is no
response to treatment and the mothers condition deteriorates. Disseminated coccidioidomycosis can have serious
long-term morbidities in the patients who survive initial
infection. Between 6 months and several years of antifungal suppressive therapy is generally recommended after
the initial infection becomes inactive, although some patients with disseminated coccidioidomycosis must continue for a still longer period to avoid recrudescence in the
same or different organ systems. There is disagreement
regarding the precise incidence of dissemination in pregnancy, but most sources agree that the risk is substantially
increased. Clearly, vigilance for the fungal infection must
be high in pregnant patients with environmental exposures and in those who are from endemic areas.
References
Figure 1. Placenta showing area of coagulative necrosis of chorionic
villi and infiltration of inflammatory cells (hematoxylin-eosin, original
magnification 20).
Figure 2. Spherules of coccidioidomycosis filled with round fungal
endospores adjacent to an area of placental infarction (hematoxylineosin, original magnification 400).
Figure 3. Spherules and individual endospores delineated by Gomori
methenamine silver staining (original magnification 400).
654 Arch Pathol Lab MedVol 131, April 2007
1. Pappagianis D, Chandler FW. Coccidioidomycosis. In: Pathology of Infectious Diseases. Stamford, Conn: Appleton & Lange; 1997:977987.
2. Chiller TM, Galgiani JN, Stevens DA. Coccidioidomycosis. Infect Dis Clin
North Am. 2003;17:4157.
3. Caldwell JW, Arsura EL, Kilgore WB, Garcia AL, Reddy V, Johnson R. Coccidioidomycosis in pregnancy during an epidemic in California. Obstet Gynecol.
2000;95:236239.
4. Arsura EL, Bellinghausen PL, Kilgore WB, Abraham J, Johnson RH. Septic
shock in coccidioidomycosis. Crit Care Med. 1998;26:6265.
5. Crum NF, Lederman ER, Stafford CM, Parrish JS, Wallace MR. Coccidiodomycosis: a descriptive survey of a reemerging disease: clinical characteristics and
current controversies. Medicine. 2004;83:149175.
6. Rosenstein NE, Emery KW, Werner B, et al. Risk factors for severe pulmonary and disseminated coccidioidomycosis: Kern County, California, 19951996.
Clin Infect Dis. 2001;32:708715.
7. Blair JE, Smilack JD, Caples SM. Coccidioidomycosis in patients with hematologic malignancies. Arch Intern Med. 2005;165:113117.
8. Busowski JD, Safdar A. Treatment for coccidioidomycosis in pregnancy?
Postgrad Med. 2001;109:7677.
Disseminated Coccidioidomycosis in PregnancyHooper et al
9. Walker MPR, Brody CZ, Resnik R. Reactivation of coccidioidomycosis in
pregnancy. Obstet Gynecol. 1992;79:815817.
10. Berger A. Th1 and Th2 responses: what are they? BMJ. 2000;321(7258):
424.
11. Li L, Dial SM, Schmelz M, Rennels MA, Ampel NM. Cellular immune
suppressor activity resides in lymphocyte cell clusters adjacent to granulomata in
human coccidioidomycosis. Infect Immunol. 2005;73:39233928.
12. Veenstra van Nieuwenhoven AL, Heineman MJ, Faas MM. The immunology of successful pregnancy. Hum Reprod Update. 2003;9:347357.
13. Salmon J. A noninflammatory pathway for pregnancy loss: innate immune
activation? J Clin Invest. 2004;114:1517.
14. Barbee RA, Hicks MJ, Grosso D, Sandel C. The maternal immune response
in coccidioidomycosis: is pregnancy a risk factor for serious infection? Chest.
1991;100:709715.
15. Thongngarm T, Jenkins JK, Ndebele K, McMurray RW. Estrogen and progesterone modulate monocyte cell cycle progression and apoptosis. Am J Reprod
Immunol. 2003;49:129138.
Arch Pathol Lab MedVol 131, April 2007
16. Linsangan LC, Ross LA. Coccidioides immitis infection of the neonate: two
routes of infection. Pediatr Infect Dis J. 1999;18:171173.
17. Gennaro S, Fehder W, Gallagher P, Miller S, Douglas SD, Campbell DE.
Lymphocyte, monocyte, and natural killer cell reference ranges in postpartal
women. Clin Diagn Lab Immunol. 1997;4:195201.
18. Ostenson M, Forger F, Nelson JL, Schuhmacher A, Hebisch G, Villager PM.
Pregnancy in patients with rheumatic disease: anti-inflammatory cytokines increase in pregnancy and decrease post partum. Ann Rheum Dis. 2005;64:839
844.
19. Richards JO, Ampel NM, Lake DF. Reversal of coccidioidal anergy in vivo
by dendritic cells from patients with disseminated coccidioidomycosis. J Immunol. 2002;169:20202025.
20. Delgado N, Xue J, Yu J, Hung CY, Cole G. A recombinant -1,3-glucanosyltranferase homolog of Coccidioides posadasii protects mice against coccidioidomycosis. Infect Immunol. 2003;71:30103019.
21. Cox RA, Magee DM. Coccidioidomycosis: host response and vaccine development. Clin Microbiol Rev. 2004;17:804839.
Disseminated Coccidioidomycosis in PregnancyHooper et al 655
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Introduction To BioethicsDocument15 pagesIntroduction To BioethicsMaureen A. Bawang100% (3)
- Gastrointestinal MCQDocument25 pagesGastrointestinal MCQLương Thế Đoàn100% (2)
- Chapter 19Document16 pagesChapter 19missy23pap100% (1)
- Lecture 1 Introduction To The Course and History of PharmacyDocument19 pagesLecture 1 Introduction To The Course and History of Pharmacyahusain100% (1)
- Iliotibial Band Syndrome - FannyDocument13 pagesIliotibial Band Syndrome - FannyAlfiani Rosyida Arisanti Syafi'iNo ratings yet
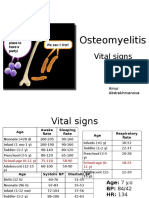
- PBL 2 - OsteomyelitisDocument10 pagesPBL 2 - OsteomyelitisAinur AbdrakhmanovaNo ratings yet
- RNTCPDocument30 pagesRNTCPDeepa SharmaNo ratings yet
- Revised Instrument Packet 2Document44 pagesRevised Instrument Packet 2Abdiaziz Walhad0% (1)
- What Is Pityriasis Rosea?Document1 pageWhat Is Pityriasis Rosea?andinaNo ratings yet
- Med Surg Test AnswersDocument9 pagesMed Surg Test AnswersAshley Rose100% (3)
- Fire Drill Senarios ToolDocument5 pagesFire Drill Senarios ToolAzmatRaoNo ratings yet
- What Is Medical Marijuana?Document8 pagesWhat Is Medical Marijuana?Dragoș TiculaNo ratings yet
- Bipolar DisorderDocument65 pagesBipolar DisorderEffectively Creative GroupNo ratings yet
- Admission and DischargeDocument61 pagesAdmission and DischargeRafia Khalil100% (2)
- Ewout JasperDocument400 pagesEwout JasperJohnny AtmanNo ratings yet
- Analysis of The Socket Bone Wall Dimensions in The Upper Maxilla in Relation To Immediate Implant PlacementDocument6 pagesAnalysis of The Socket Bone Wall Dimensions in The Upper Maxilla in Relation To Immediate Implant PlacementLeonardo PolitoNo ratings yet
- Acr Mri BiradsDocument3 pagesAcr Mri BiradsFilipe BarraNo ratings yet
- Communicable Disease Nursing Clinical FocusDocument2 pagesCommunicable Disease Nursing Clinical Focusrceponelas1127No ratings yet
- Issues Around Vaginal Vault Closure: ReviewDocument6 pagesIssues Around Vaginal Vault Closure: ReviewKeeranmayeeishraNo ratings yet
- First Aid Pharmacology AntimicrobialsDocument23 pagesFirst Aid Pharmacology AntimicrobialsLaura Lopez RocaNo ratings yet
- College Essay Example #3: This Is A College Essay That Worked ForDocument2 pagesCollege Essay Example #3: This Is A College Essay That Worked For4- Desiree FuaNo ratings yet
- Pathology Mcqs 2Document6 pagesPathology Mcqs 2Numan Rox100% (5)
- Prenatal Care: Ocampo, Joan Oh, Howard Panganiban, JamesDocument21 pagesPrenatal Care: Ocampo, Joan Oh, Howard Panganiban, JamesHoward Vince OhNo ratings yet
- Paper 5 Review The Literature of Balanced Scorecard and Performance Measurement 1Document15 pagesPaper 5 Review The Literature of Balanced Scorecard and Performance Measurement 1Kepher OnukoNo ratings yet
- DR Mohd Suhaimi Tajudin Overview TriageDocument39 pagesDR Mohd Suhaimi Tajudin Overview Triageshinichi kudoNo ratings yet
- Gender Differences in Human Brain A Review PDFDocument20 pagesGender Differences in Human Brain A Review PDFSwami GurunandNo ratings yet
- Inno-Lia HCV ScoreDocument14 pagesInno-Lia HCV ScoreMaria CorreiaNo ratings yet
- Surgery Department: Emergency Case ReportsDocument46 pagesSurgery Department: Emergency Case ReportsMohamad ZulfikarNo ratings yet
- RMFADocument86 pagesRMFASELVA GANESH100% (1)
- Quality Improvement Priorities 2016-17 Consultation Draft v0.4 - QGCDocument26 pagesQuality Improvement Priorities 2016-17 Consultation Draft v0.4 - QGCZack AdamsNo ratings yet