Professional Documents
Culture Documents
234 Farmer
Uploaded by
Raghavendra NalatawadCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
234 Farmer
Uploaded by
Raghavendra NalatawadCopyright:
Available Formats
See
discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/6584286
Chronic inferior turbinate enlargement and the
implications for surgical intervention
Article in Rhinology January 2007
Impact Factor: 3.76 Source: PubMed
CITATIONS
READS
36
915
2 authors, including:
Ronald Eccles
Cardiff University
227 PUBLICATIONS 5,007 CITATIONS
SEE PROFILE
All in-text references underlined in blue are linked to publications on ResearchGate,
letting you access and read them immediately.
Available from: Ronald Eccles
Retrieved on: 17 July 2016
REVIEW
Rhinology, 44, 234-238, 2006
Chronic inferior turbinate enlargement and the
implications for surgical intervention*
S.E.J. Farmer, R. Eccles
Common Cold Centre, Cardiff School of Biosciences, Cardiff University, Cardiff, United Kingdom
SUMMARY
Nasal obstruction due to chronic enlargement of the inferior turbinate is a common problem for
the ENT surgeon. This review will discuss the pathology of bilateral and unilateral turbinate
enlargement associated with chronic rhinitis and nasal septal deviation, and focus on the structural changes in the turbinates. Cellular hyperplasia, tissue oedema and vascular congestion
all contribute to turbinate enlargement, but there is some evidence that bony enlargement is
associated with unilateral turbinate enlargement. There is no evidence for cellular hypertrophy
despite the common use of the term turbinate hypertrophy and this term should be replaced
with the more correct term of turbinate enlargement. The underlying pathology of turbinate
enlargement has important implications for the surgical management of nasal obstruction.
Key words: turbinate hypertrophy, turbinate enlargement, surgery, mucosa, bone
INTRODUCTION
Chronic nasal obstruction is a common symptom of nasal disease. Enlargement of the inferior turbinates is one of the most
frequent underlying mechanisms (1). Turbinate enlargement
can be bilateral or unilateral. Bilateral turbinate enlargement is
caused by nasal inflammation as a result of allergic and nonallergic rhinitis, other environmental triggers, such as dust and
tobacco and medical causes, including pregnancy (2). Unilateral
turbinate enlargement occurs in association with a congenital,
or acquired anatomical deviation of the nasal septum into the
contralateral nasal passage. It has been proposed that unilateral
turbinate enlargement occurs to protect the more patent nasal
passage from the drying and crusting caused by excess airflow
(3,4)
, but the underlying mechanism for this is unknown.
Turbinate surgery is commonly performed in an attempt to
relieve nasal obstruction, despite a lack of evidence regarding
the underlying pathology of turbinate enlargement. In the literature (3,4) and in rhinology textbooks (1), the mucosal layer of
the inferior turbinate is frequently implicated as the structure
responsible for turbinate enlargement. In particular it is commonly claimed that dilatation of the venous sinuses, due to
engorgement with blood, is the underlying mechanism (1,5).
Pollock (6) suggests that turbinate enlargement is simply due to
mucosal thickening. It has also been suggested that turbinate
enlargement is caused by mucosal oedema with eosinophils
and mast cells present in an inflammatory response (1) .
Saunders (7) describes three ways in which the inferior
turbinate causes nasal obstruction. In addition to mucosal
*Received for publication: September 28, 2006; accepted: October 11, 2006
engorgement he also describes an undue prominence of the
turbinate bone and redundant hyperplastic turbinate mucosa
as potential mechanisms for turbinate enlargement (7) .
Fairbanks and Kaliner (8) claim that turbinate enlargement
involves both bony and mucosal elements.
The term turbinate hypertrophy was first coined in the late
1800s (9,10) to describe enlargement of the inferior turbinate and
it remains in common use today. Hypertrophy is defined as
the enlargement of an organ or tissue resulting from an
increase in size of its cells (11). In contrast, cellular hyperplasia
is enlargement due to an increase in the number of cells.
Hyperplasia and hypertrophy of the mucosal or osseous layers
of the inferior turbinate also provide potential explanations for
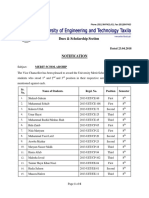
the mechanism of inferior turbinate enlargement (Figure 1).
An understanding of the structural mechanisms of turbinate
enlargement is important to the rhinologist who is frequently
Figure 1. Possible mechanisms of inferior turbinate enlargement.
Dilatation of venous sinuses
Mucosal
Tissue oedema
Cellular hypertrophy
Bilateral or unilateral
inferior turbinate
enlargement
Cellular hyperplasia
Osseous
Cellular hypertrophy
Cellular hyperplasia
Turbinate enlargement
faced with managing this common problem. In particular, it is
helpful to know whether there is mucosal or bony enlargement
as this will impact on the choice of surgery.
In this review the structure of the normal inferior turbinate
and the pathology of turbinate enlargement will be examined.
The review will focus on the evidence for mucosal and bony
changes observed in turbinate enlargement with reference to
bilateral and unilateral disease. The implications of the pathology of turbinate enlargement on the surgical management of
patients with nasal obstruction will be discussed and it is proposed that the term turbinate enlargement is a more accurate
description of the pathology than turbinate hypertrophy.
STRUCTURE OF THE NORMAL INFERIOR TURBINATE
The inferior turbinate is an elongated, scroll-like paired structure of the lateral nasal wall. It consists of a central layer of
bone and a mucosal layer on either side (12). The normal thickness of the mucosal and bony layers has been studied with
computed tomography (CT) (13) and histology (3,12). CT scans
showed the mean anterior dimensions of the medial and lateral mucosa were 3.33 mm and 2.06 mm respectively (13) .
However the patients studied are unlikely to represent normality because all had septal deviations, and the measurements were taken from the nasal passage with the smaller
turbinate. The mean thickness of the medial mucosal and lateral mucosal layers was 1.76 mm and 1.03 mm respectively in a
study examining cadaveric and post-operative inferior
turbinate specimens (3). In a similar study the values were 1.59
mm and 0.94 mm (12). These values seem very thin, and it is
likely that the vascular component of the mucosal width is
underestimated by examining histological specimens because
of collapse of the erectile venous sinuses.
The turbinate is mainly covered with pseudostratified columnar epithelium with smaller islands of squamous epithelium,
basal cells, ciliated and non-ciliated cells and comprises 10%
goblet cells (12). The epithelium is separated from the lamina
propria by a basement layer. The lamina propria is thicker in
the medial layer than the lateral layer and extends to the
periosteum of the bony layer. It consists of connective tissue
containing a few lymphocytes and other immunocompetent
cells, seromucous glands, a rich network of thin walled
venous sinuses and a few arteries. The osseous layer consists
of cancellous bone. The mean thickness of the bone is 1.2
mm (12) in a histological study and 1.6 mm when measured
with CT (13). The mean height of the inferior turbinate is 7.75
mm (3). Age and gender are reported to have no significant
effect on total turbinate thickness or the thickness of individual turbinate layers. However, ageing is associated with a
reduction in the number of submucosal glands and increased
venous sinuses (12).
235
The structure of the inferior turbinate can be studied by several different methods; histology, CT and decongestion.
Histology can provide information on the amounts of soft and
bony tissues and information about the relative amounts of
different tissues such as glands and venous sinuses.
Histological examination can determine whether turbinate
enlargement is due to cellular hypertrophy or hyperplasia. CT
can give measures of soft and bony tissue components in the
turbinates. The relative degree of shrinkage of the turbinate on
application of a topical decongestant can provide information
about the amount of venous sinuses in the turbinates.
1. STRUCTURE OF THE ENLARGED INFERIOR
TURBINATE IN UNILATERAL DISEASE
Histology
Turbinate tissue from patients with septal deviations and compensatory unilateral turbinate enlargement has been examined
in histological studies (3). The proportion of submucosal
glands, connective tissue, epithelium, arteries and venous
sinuses in the inferior turbinates from these patients has not
been shown to be significantly different when compared with
cadaveric controls (3). The width of the medial mucosa and lateral mucosa in both groups were not significantly different
despite the fact that the enlarged inferior turbinates were significantly wider (3). Qualitative assessment of mucosal architecture has shown that 42.1% of turbinates from patients with
compensatory enlargement exhibit pathological changes.
These include dilated, engorged thin-walled venous sinuses,
fibrosis of the lamina propria, subepithelial infiltration of lymphocytes, plasma cells and eosinophils and dilatation of excretory glandular ducts (3).
Histological examination of inferior turbinates from patients
with septal deviations and compensatory enlargement of the
contralateral inferior turbinate has shown significant bone
expansion when compared with cadaveric controls (3). A twofold increase in the thickness of the osseous layer of the inferior turbinate was observed (3). Enlargement of the bony layer
accounted for 3/4 of the entire growth of the inferior turbinate.
The number or size of individual cells was not examined.
Computed tomography
The relative enlargement of bony and soft tissue components
of inferior turbinates in patients with unilateral compensatory
turbinate enlargement associated with nasal septal deviation
has been evaluated by CT in several studies (4,13). These studies
have the advantage of examining the inferior turbinate in life.
The mean width of the anterior medial mucosa in unilateral
turbinate enlargement is significantly wider at 5.33mm,
when compared with the contralateral turbinate as a control. The lateral mucosal layer has also been shown to be
significantly wider in patients with unilateral compensatory
enlargement (13).
236
A study of 99 patients with moderate to severe septal deviation
used CT to calculate intraturbinate ratios at three different levels to assess mucosal contribution to turbinate enlargement (4).
The intraturbinate ratio is the ratio of overall turbinate cross
sectional area to bony turbinate cross sectional area. In
enlarged turbinates associated with nasal septal deviations, the
intraturbinate ratio was highest in the posterior segment,
implying that the mucosal component is predominantly
responsible for turbinate mass in the posterior segment (4).
The interturbinate ratio is the CT calculated ratio of the cross
sectional area of the inferior turbinate bone on either side of
the septum. The interturbinate ratio for patients with severe
septal deviations has been shown to be significantly higher
compared with patients with normal and mild deviations in the
anterior and middle segments of inferior turbinate bone (4).
This suggests that in compensatory enlargement of the inferior
turbinate associated with severe septal deviation there is
prominent enlargement of the inferior turbinate bone in the
anterior and middle thirds when compared with the contralateral side.
Decongestant studies
Several studies have examined the vascular contribution to
compensatory unilateral turbinate hypertrophy by evaluating
response to decongestants using acoustic rhinometry (14-16).
Hilberg (14) found no significant difference in the effect of
decongestion on minimal cross-sectional area (MCA), crosssectional area at 3.3 cm from the nostril, and cross-sectional
area 4 cm from the nostril, when comparing a group of patients
with turbinate enlargement with normal controls. Grymer (15)
defines mucosal hypertrophy as present if decongestion
increases cross sectional area by more than 100% relative to
the non-decongested value. This is based on the values of a
63% area increase in a normal reference group. In patients with
compensatory unilateral turbinate enlargement due to septal
deviations of varying severity 62% of patients met this criterion
for mucosal hypertrophy (15). This led the authors to conclude
that mucosal hypertrophy is common to patients with nasal
obstruction regardless of the degree of septal deviation.
2. THE STRUCTURE OF THE ENLARGED INFERIOR
TURBINATE IN BILATERAL DISEASE
Histology
Punch biopsies taken from the inferior turbinates of patients
with chronic hypertrophic allergic and non-allergic rhinitis
have shown characteristic features (17). An increase in goblet
cell population with thickening of the basement membrane has
been documented. There is also an increase in the number of
blood vessels observed with associated congestion and dilatation and connective tissue stromal oedema. In addition
patients with allergic rhinitis have increased numbers of
eosinophils and patients with non-allergic rhinitis exhibit a
marked predominance of the mucous acini of the glands (17).
Farmer and Eccles
A scanning electron microscopy study of inferior turbinate
biopsies taken from patients suffering with perennial rhinitis
and normal controls has shown qualitative differences in the
ultrastructure of the mucosa. Patients with perennial rhinitis
have more pseudo-stratified columnar epithelium and more
goblet cells than controls, supporting the idea that cellular
hyperplasia is responsible for turbinate hypertrophy (14).
Berger compared inferior turbinate specimens from patients
with bilateral enlargement with specimens from a control
group undergoing septal surgery (19). Although there are serious issues concerning the nature of the control group, it is the
only study that examines both the mucosal and bony components in bilateral turbinate enlargement. The enlarged
turbinates were significantly wider than the controls and the
medial mucosal layer made the greatest contribution to the
total increase in inferior turbinate width (19). There was no significant difference in the width of the lateral mucosal layer or
the bony layer between groups. Furthermore, the increase in
the width of the medial mucosa was predominantly due to an
increase in the thickness of the lamina propria that houses
subepithelial inflammatory cells, venous sinuses and submucosal glands (19). The relative proportion of venous sinuses in
enlarged turbinates was significantly greater than in controls.
26.8% of the medial mucosal layer of enlarged inferior
turbinates comprised venous sinuses compared to 19.2% of
control inferior turbinates (19). Qualitative assessment of the
enlarged inferior turbinates showed metaplastic squamous
epithelium in 10% of specimens, fibrosis of the lamina propria
in 90% of specimens, dilated and engorged thin-walled venous
sinuses in 15% of specimens and a marked subepithelial
inflammatory cell infiltrate in 65% of specimens. Qualitative
assessment of control inferior turbinates revealed the only
pathology was dilated venous sinuses, which occurred in 5% of
(19)
specimens .
Decongestant studies
Corey used acoustic rhinometry to demonstrate a significant
difference between controls and patients with allergic rhinitis
in their response to a topical decongestant at the minimal
cross-sectional area (MCA) (16). The average total percentage
area change at the MCA for controls was 15.6% compared to
24.6% for patients with allergic rhinitis (16). This infers that
patients with allergic rhinitis have an exaggerated response to
decongestants because there is a greater change in the volume
of the venous sinuses than in controls. However, these patients
were not labelled as having turbinate hypertrophy, although
their symptom scores for nasal congestion were high.
Decongestant studies may underestimate the vascular contribution to mucosal enlargement in some patients with chronic
inflammation where there is mucosal infiltration of fibrous tissue. This can render engorged venous sinuses incapable of
decongestion (21,22).
237
Turbinate enlargement
DISCUSSION
This is the first review to examine the evidence for the mechanism of turbinate enlargement. Despite the common occurrence of turbinate enlargement there is little evidence to
explain which turbinate structures are responsible for the
enlargement. The limited evidence available appears to suggest
that there may be two types of turbinate enlargement with
underlying differences in the pathology.
In unilateral turbinate enlargement associated with nasal septal
deviation of the contralateral turbinate there is limited evidence for bony expansion as a major contributing factor. There
is evidence from CT studies to suggest that an element of
mucosal enlargement is also important. Although there is
some evidence for an increase in size of the bony component
of the turbinate it is not clear if this is merely due to an
increase in the overall size of the turbinate. It is generally
assumed that the unilateral turbinate enlargement associated
with septal deviation occurs to protect the more patent side
from the drying and crusting caused by excess airflow (3,4). A
deviated nasal septum may be congenital, the product of
growth asymmetry, or the result of trauma. However, it is
unclear whether cellular hyperplasia or hypertrophy is the
underlying mechanism for bone expansion. The underlying
cause of unilateral turbinate enlargement is also unknown.
The turbinate enlarges to occupy the increased volume of the
nasal passage, but factors that trigger and control the increase
in the size of the turbinate are unknown.
In bilateral turbinate enlargement there is evidence for a
mucosal contribution to enlargement. Histological studies suggest that a combination of mechanisms may be responsible for
mucosal enlargement, including cellular hyperplasia, tissue
oedema and vascular congestion. There is no evidence for cellular hypertrophy. Therefore there is no evidence to substantiate use of the term turbinate hypertrophy and it is proposed
that the term turbinate enlargement is a more accurate
description of the condition. There is no evidence to support
bony enlargement in bilateral disease. With cases of acute
rhinitis it appears that the main cause of turbinate enlargement
is filling of venous sinuses since the size of the turbinate can
be reduced by application of a topical decongestant (22). In
cases of chronic rhinitis there may be some tissue fibrosis due
to a chronic inflammatory response and this may make it difficult to reverse the increase in turbinate size by medical intervention, such as treatment with topical corticosteroids. In
these cases surgery to reduce the size of the turbinate may be
the only option for treatment of nasal obstruction.
Many surgical techniques have been described to reduce the
size of enlarged turbinates. Today, these can be broadly divided into two main categories: turbinate electrosurgery or soft
tissue reduction (including submucosal diathermy and surface
diathermy) and turbinate bone resection/reduction (including
crushing and trimming of the inferior turbinate bone and total
turbinectomy). An appreciation of the relative enlargement of
the bony and soft tissue constituents of the inferior turbinate is
important when deciding on which type of surgical intervention is most appropriate.
Electrosurgical techniques result in heating of intracellular
contents and vaporization of cells. Heat causes coagulation and
obliteration of the venous sinuses leading to submucosal fibrosis and scarring (23) which is thought to anchor the mucosa to
the periosteum. Therefore electrosurgery would be most suited for the treatment of mucosal turbinate enlargement due to
vascular congestion and oedema, and avoids the additional
risks associated with surgery involving the inferior turbinate
bone. Inferior turbinate enlargement due to predominantly
bony changes, as occurs in unilateral compensatory enlargement associated with a septal deviation, would be best treated
by reduction or resection of the inferior turbinate bone.
REFERENCES
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
Jones AS. Intrinsic Rhinitis. In: Kerr AG, ed. Scott-Brown's
Otolaryngology. Oxford: Butterworth Heinemann, 1997; 4/9/14/9/17.
Rohrich RJ, Krueger JK, Adams WP, Marple, BF. Rationale for
submucous resection of hypertrophied inferior turbinates in rhinoplasty: an evolution. Plastic and Reconstructive Surgery 2001; 108:
536-544.
Berger G, Hammel I, Berger R, Avraham S, Ophir D.
Histopathology of the inferior turbinate with compensatory hypertrophy in patients with deviated nasal septum. Laryngoscope 2000;
110: 2100-2105.
Uzun L, Savranlar A, Beder LB et al. Enlargement of the bone
component in different parts of compensatorily hypertrophied
inferior turbinate. Am J Rhinol 2004; 18: 405-410.
Cauna N, Cauna D. The fine structure and innervation of the
cushion veins of the human nasal respiratory mucosa. Anat Rec.
1975; 181: 1-16.
Pollock RA, Rohrich RJ. Inferior turbinate surgery: an adjunct to
successful treatment of nasal obstruction in 408 patients. Plastic
and Reconstructive Surgery 1984; 74: 227-236.
Saunders WH. Surgery of the inferior nasal turbinates. Ann Otol
Rhinol Laryngol 1982; 91; 445-447.
Fairbanks DNF, Kaliner M. Nonallergic rhinitis and infection. In:
Cummings CW, Fredrickson JM, Harker AL, Krause CJ,
Richardson MA, eds. Otolaryngology Head and Neck Surgery. 3rd
ed. St. Louis: Mosby, 1998; 910-920.
Mackenzie M. Hypertrophy of the mucosal membrane of the
nose. In: Mackenzie M. A manual of diseases of the throat and
nose, including the pharynx, larynx, trachea, oesophagus, nose,
and naso-pharynx. London: Churchill, 1884; 317-323.
Jones M. Turbinal hypertrophy. Lancet 1895; 2: 879.
th
Pearsall J, ed. The Concise Oxford Dictionary. 10 ed. Oxford:
Oxford University Press, 2001.
Berger G, Balum-Azim M, Ophir D. The normal inferior
turbinate: histomorphometric analysis and clinical implications.
Laryngoscope 2003; 113: 1192-1198.
Egeli E, Demirci L, Yazycy B, Harputluoglu U. Evaluation of the
inferior turbinate in patients with deviated nasal septum by using
computed tomography. Laryngoscope 2004; 114: 113-117.
Hilberg O, Grymer LF, Pederson OF, Elbrond O. Turbinate
hypertrophy. Evaluation of the nasal cavity by acoustic rhinometry. Arch Otolaryngol Head Neck Surg 1990; 116: 283-289.
Grymer LF, Illum P, Hilberg O. Septoplasty and compensatory
inferior turbinate hypertrophy: a randomized study evaluated by
acoustic rhinometry. J Laryngol Otol 1993; 107: 413-417.
Corey JP, Kemker BJ, Nelson R, Gungor A. Evaluation of the
238
17.
18.
19.
20.
21.
22.
Farmer and Eccles
nasal cavity by acoustic rhinometry in normal and allergic subjects.
Otolaryngol Head Neck Surg 1997; 117: 22-28.
Talaat M, El-Sabawy E, Baky FA, Raheem AA. Submucous
diathermy of the inferior turbinates in chronic hypertrophic rhinitis. J Laryngol Otol 1987; 101: 452-460.
Mygind N. Scanning electron microscopy of the human nasal
mucosa. Rhinology 1975; 13: 57-75.
Berger G, Gass S, Ophir D. The histopathology of the hypertrophic inferior turbinate. Arch Otolaryngol Head Neck Surg 2006;
132: 588-594.
Jones AS, Lancer JM, Moir AA, Stevens JC. The effect of submucosal diathermy to the inferior turbinates on nasal resistance to
airflow in allergic and vasomotor rhinitis. Clin Otolaryngol 1985;
10: 249-252.
Cook PR. Sinusitis and allergy. Current Opinion in
Otolaryngology & Head and Neck Surgery 1997; 5: 35-39.
Eccles R. Nasal airflow in health and disease. Act Otolaryngol
2000; 120; 580-595.
23. Jones AS, Lancer JM, Moir AA, Stevens JC. The effect of submucosal diathermy to the inferior turbinates on nasal resistance to
airflow in allergic and vasomotor rhinitis. Clinical Otolaryngology
1985; 10: 249-252.
Miss SEJ Farmer
Common Cold Centre
Cardiff School of Biosciences
Cardiff University
Park Place
Cardiff CF10 3US
United Kingdom
Tel: +44-292-087-4099
Fax: +44-292-087-4093
Email: farmers@cardiff.ac.uk
You might also like
- Clin Physio Funct Imaging - 2013 - Munkholm - Mucociliary Clearance Pathophysiological AspectsDocument7 pagesClin Physio Funct Imaging - 2013 - Munkholm - Mucociliary Clearance Pathophysiological AspectsIkon ikonicNo ratings yet
- Eustachian TubeDocument6 pagesEustachian TubeMusyfiqoh TusholehahNo ratings yet
- JurnalDocument7 pagesJurnalandiniNo ratings yet
- 216851-Article Text-533920-1-10-20211102Document5 pages216851-Article Text-533920-1-10-20211102Vaino MungobaNo ratings yet
- New Horizons Symposium Papers: Anatomy and Physiology of TracheostomyDocument7 pagesNew Horizons Symposium Papers: Anatomy and Physiology of TracheostomySteven WilsonNo ratings yet
- Laryngeal Split & Rib Cartilage Interpositional GraftingDocument9 pagesLaryngeal Split & Rib Cartilage Interpositional GraftingAlexi Chávez EchevarríaNo ratings yet
- Bilateral Nasolabial Cyst MarcoviceanuDocument4 pagesBilateral Nasolabial Cyst MarcoviceanubamsusiloNo ratings yet
- JurnalDocument6 pagesJurnalYazid Eriansyah PradantaNo ratings yet
- Pi Is 1043181014000153Document11 pagesPi Is 1043181014000153diana mistraNo ratings yet
- Airway Management in The Adult - Miller's Anesthesia 2009Document38 pagesAirway Management in The Adult - Miller's Anesthesia 2009UrgenciasCol FoamNo ratings yet
- International Review of Experimental Pathology: Kidney DiseaseFrom EverandInternational Review of Experimental Pathology: Kidney DiseaseG. W. RichterRating: 5 out of 5 stars5/5 (1)
- Surgery For Pharyngeal Pouch or Zekers DivertulaDocument19 pagesSurgery For Pharyngeal Pouch or Zekers DivertulaKumaran Bagavathi RagavanNo ratings yet
- Turbinate Dysfunction March 2003Document11 pagesTurbinate Dysfunction March 2003putriNo ratings yet
- Nasopalatine Duct CystDocument4 pagesNasopalatine Duct CystVikneswaran Vîçký100% (1)
- Eosinophilic Angiocentric Fibrosis of The Nasal Septum: Case ReportDocument15 pagesEosinophilic Angiocentric Fibrosis of The Nasal Septum: Case ReportPriskila Marlen YoltuwuNo ratings yet
- MainDocument6 pagesMainDhio ArieyonaNo ratings yet
- Pediatric Laryngotracheal Stenosis and Airway Reconstruction: A Review of Voice Outcomes, Assessment, and Treatment IssuesDocument11 pagesPediatric Laryngotracheal Stenosis and Airway Reconstruction: A Review of Voice Outcomes, Assessment, and Treatment Issuescanndy202No ratings yet
- KumarasingheDocument4 pagesKumarasingheVitta Kusma WijayaNo ratings yet
- Sinusliftprocedures: Anoverviewof Currenttechniques: Avichai Stern,, James GreenDocument1 pageSinusliftprocedures: Anoverviewof Currenttechniques: Avichai Stern,, James Greenأسامه ممتاز مرادNo ratings yet
- Anal Abscess and FistulaDocument12 pagesAnal Abscess and FistulaGustavoZapataNo ratings yet
- Tonsillectomy TechniquesDocument11 pagesTonsillectomy TechniquesBrigita De VegaNo ratings yet
- Chondro-Osseous Respiratory Epithelial Adenomatoid Hamartomas in 3 DogsDocument4 pagesChondro-Osseous Respiratory Epithelial Adenomatoid Hamartomas in 3 DogsfisheirNo ratings yet
- Fundamental Considerations of The Design and Function of Intranasal AntrostomiesDocument4 pagesFundamental Considerations of The Design and Function of Intranasal AntrostomiessevattapillaiNo ratings yet
- Trans-Septal Suture Method Versus Intranasal Silicone Splint in SeptoplastyDocument7 pagesTrans-Septal Suture Method Versus Intranasal Silicone Splint in SeptoplastyInternational Jpurnal Of Technical Research And ApplicationsNo ratings yet
- Surgical Management of Parapharyngeal AbscessDocument3 pagesSurgical Management of Parapharyngeal AbscessmeyNo ratings yet
- Peritonsillar Abscess in Emergency MedicineDocument14 pagesPeritonsillar Abscess in Emergency Medicinerissa neNo ratings yet
- Hobai 2012Document22 pagesHobai 2012CristianpalmarNo ratings yet
- Cleft Lip and Palate Management: A Comprehensive AtlasFrom EverandCleft Lip and Palate Management: A Comprehensive AtlasRicardo D. BennunNo ratings yet
- 14 PDFDocument12 pages14 PDFeliasNo ratings yet
- Achalasia With Megaesophagus and Tracheal Compr - 2015 - International Journal oDocument3 pagesAchalasia With Megaesophagus and Tracheal Compr - 2015 - International Journal ooomculunNo ratings yet
- Hemorrhoids: From Basic Pathophysiology To Clinical ManagementDocument16 pagesHemorrhoids: From Basic Pathophysiology To Clinical ManagementSASNo ratings yet
- Recurent EpistaxisDocument3 pagesRecurent EpistaxisFongmeicha Elizabeth MargarethaNo ratings yet
- OJOLNS-10 - II - Invited Editorial PDFDocument5 pagesOJOLNS-10 - II - Invited Editorial PDFDR K C MALLIKNo ratings yet
- Pharynx Lecture 2Document4 pagesPharynx Lecture 2Amy KochNo ratings yet
- Internet Scientific PublicationsDocument12 pagesInternet Scientific PublicationsAnonymous h0DxuJTNo ratings yet
- The Anatomy and Pathology of The Lesser Sac Implications For...Document7 pagesThe Anatomy and Pathology of The Lesser Sac Implications For...Medical StudentNo ratings yet
- Laser Tonsil Cryptolysis: In-Office 500 Cases Review: Yosef P. Krespi, MD, Victor Kizhner, MDDocument5 pagesLaser Tonsil Cryptolysis: In-Office 500 Cases Review: Yosef P. Krespi, MD, Victor Kizhner, MDerdikasatriaNo ratings yet
- Bases Anatomicas PerforantesDocument12 pagesBases Anatomicas PerforantesAngela GarciaNo ratings yet
- RanulaDocument3 pagesRanulaRyo RaolikaNo ratings yet
- Understanding The Nasal AirwayDocument21 pagesUnderstanding The Nasal AirwayGera AguilarNo ratings yet
- Management of Anal FistulaDocument5 pagesManagement of Anal Fistulailham adhaniNo ratings yet
- Pleural DiseaseDocument12 pagesPleural DiseaseEdgar Romero RamirezNo ratings yet
- Accessory Spleen: V. Durgesh, CH. Roja RaniDocument3 pagesAccessory Spleen: V. Durgesh, CH. Roja RaniIOSRjournalNo ratings yet
- Perianal AbscessFistula DiseaseDocument9 pagesPerianal AbscessFistula Diseasetri jayaningratNo ratings yet
- Peritonsillar Abscess DrainageDocument4 pagesPeritonsillar Abscess Drainagesyibz100% (1)
- E17 FullDocument5 pagesE17 FullSajit RawatNo ratings yet
- Pleural Disease NEJM 2018 PDFDocument12 pagesPleural Disease NEJM 2018 PDFPanayiotis StavroulakisNo ratings yet
- Nasopalatine Duct Cyst-Manuscript Case Report Haji - MIODocument6 pagesNasopalatine Duct Cyst-Manuscript Case Report Haji - MIOdrg.montessoNo ratings yet
- Enfermedades Pleurales NEJM 2018Document12 pagesEnfermedades Pleurales NEJM 2018rene.javier.96No ratings yet
- Superficial Thrombophlebitis Follow-Up Study: Legs: Randomized, ControlledDocument7 pagesSuperficial Thrombophlebitis Follow-Up Study: Legs: Randomized, ControlledFlorin BzoviiNo ratings yet
- Thyroglossal Duct Cysts: Anatomy, Embryology and TreatmentDocument7 pagesThyroglossal Duct Cysts: Anatomy, Embryology and TreatmentTasia RozakiahNo ratings yet
- CDH Modern MX PDFDocument12 pagesCDH Modern MX PDFThia SanjayaNo ratings yet
- Jcedv 10 I 5 P 495Document4 pagesJcedv 10 I 5 P 495Yohana SimanjuntakNo ratings yet
- A Case Report On - A Rare Case of Laryngocele in A Young Male MenDocument4 pagesA Case Report On - A Rare Case of Laryngocele in A Young Male MenIOSRjournalNo ratings yet
- Paper Alumnos 6Document12 pagesPaper Alumnos 6Victor Martinez HagenNo ratings yet
- Cyto Lungtumorbook1Document104 pagesCyto Lungtumorbook1ixNo ratings yet
- Tuberculosis of The Chest Wall With Massive Tuberculous Pleural EffusionDocument3 pagesTuberculosis of The Chest Wall With Massive Tuberculous Pleural EffusionwulanNo ratings yet
- Acalasia Articulo EspaniolDocument4 pagesAcalasia Articulo Espaniolmanuel jimenezNo ratings yet
- Miller Airway ManagementDocument65 pagesMiller Airway ManagementBenediktus BayuNo ratings yet
- PDFDocument4 pagesPDFBhavesh MevadaNo ratings yet
- Endoscopy ReportDocument1 pageEndoscopy ReportRaghavendra NalatawadNo ratings yet
- R6230280 Nalatawad 191119052334Document4 pagesR6230280 Nalatawad 191119052334Raghavendra NalatawadNo ratings yet
- Pavan Biodata PDFDocument1 pagePavan Biodata PDFRaghavendra NalatawadNo ratings yet
- Management of Inferior Turbinate Hypertrophy: A Comparative Study Between Partial Turbinectomy and Submucous Diathermy Mohammad Hassan Al-BaldawiDocument4 pagesManagement of Inferior Turbinate Hypertrophy: A Comparative Study Between Partial Turbinectomy and Submucous Diathermy Mohammad Hassan Al-BaldawiRaghavendra NalatawadNo ratings yet
- Thyroplasty Hands On WorkshopDocument1 pageThyroplasty Hands On WorkshopRaghavendra NalatawadNo ratings yet
- 209th LLE Project - Dhalai - Ambassa Project ScheduleDocument1 page209th LLE Project - Dhalai - Ambassa Project ScheduleRaghavendra NalatawadNo ratings yet
- Bio Medical Waste Bags Sizes & ColorsDocument1 pageBio Medical Waste Bags Sizes & ColorsRaghavendra NalatawadNo ratings yet
- Seat Prefernce List - UpdatedDocument1 pageSeat Prefernce List - UpdatedRaghavendra NalatawadNo ratings yet
- DNBDocument20 pagesDNBRaghavendra NalatawadNo ratings yet
- Endoscopic Management of CSF RhinorrheaDocument16 pagesEndoscopic Management of CSF RhinorrheaRaghavendra NalatawadNo ratings yet
- Research Proposal Topics for MD AnaesthesiologyDocument37 pagesResearch Proposal Topics for MD AnaesthesiologyRaghavendra NalatawadNo ratings yet
- Atlas Anatomy of The Nose and Paranasal SinusesDocument43 pagesAtlas Anatomy of The Nose and Paranasal SinusesRaghavendra NalatawadNo ratings yet
- Aerospace Medicine Spine Injuries ScintigraphyDocument359 pagesAerospace Medicine Spine Injuries ScintigraphySaurabh Max54% (13)
- Anatomyofthyroidgland 2 140129144245 Phpapp02Document25 pagesAnatomyofthyroidgland 2 140129144245 Phpapp02Raghavendra NalatawadNo ratings yet
- Cert DegDocument3 pagesCert DegRaghavendra NalatawadNo ratings yet
- Unit 9 What Does APES Say?Document17 pagesUnit 9 What Does APES Say?johnosborneNo ratings yet
- English: Quarter 1 - Module 1Document16 pagesEnglish: Quarter 1 - Module 1Ryze100% (1)
- American Wire & Cable Daily Rated Employees Union v. American Wire & Cable Co and Court of AppealsDocument2 pagesAmerican Wire & Cable Daily Rated Employees Union v. American Wire & Cable Co and Court of AppealsFoxtrot Alpha100% (1)
- 2nd YearDocument5 pages2nd YearAnbalagan GNo ratings yet
- Friday August 6, 2010 LeaderDocument40 pagesFriday August 6, 2010 LeaderSurrey/North Delta LeaderNo ratings yet
- Zsoka PDFDocument13 pagesZsoka PDFMasliana SahadNo ratings yet
- Year 11 Physics HY 2011Document20 pagesYear 11 Physics HY 2011Larry MaiNo ratings yet
- THE LEGEND OF SITU BAGENDIT by AIN 9CDocument2 pagesTHE LEGEND OF SITU BAGENDIT by AIN 9CwahyubudionoNo ratings yet
- Fill in The BlanksDocument38 pagesFill in The Blanksamit48897No ratings yet
- Elliptic FunctionsDocument66 pagesElliptic FunctionsNshuti Rene FabriceNo ratings yet
- Towards Emotion Independent Languageidentification System: by Priyam Jain, Krishna Gurugubelli, Anil Kumar VuppalaDocument6 pagesTowards Emotion Independent Languageidentification System: by Priyam Jain, Krishna Gurugubelli, Anil Kumar VuppalaSamay PatelNo ratings yet
- Batman Vs Riddler RiddlesDocument3 pagesBatman Vs Riddler RiddlesRoy Lustre AgbonNo ratings yet
- Arcmap and PythonDocument29 pagesArcmap and PythonMiguel AngelNo ratings yet
- Walter Horatio Pater (4 August 1839 - 30 July 1894) Was An English EssayistDocument4 pagesWalter Horatio Pater (4 August 1839 - 30 July 1894) Was An English EssayistwiweksharmaNo ratings yet
- Term2 WS7 Revision2 PDFDocument5 pagesTerm2 WS7 Revision2 PDFrekhaNo ratings yet
- Zeng 2020Document11 pagesZeng 2020Inácio RibeiroNo ratings yet
- Sterilization and DisinfectionDocument100 pagesSterilization and DisinfectionReenaChauhanNo ratings yet
- M Information Systems 6Th Edition Full ChapterDocument41 pagesM Information Systems 6Th Edition Full Chapterkathy.morrow289100% (24)
- IOT Liquid Level Monitoring SystemDocument5 pagesIOT Liquid Level Monitoring SystemNegmNo ratings yet
- 2-Library - IJLSR - Information - SumanDocument10 pages2-Library - IJLSR - Information - SumanTJPRC PublicationsNo ratings yet
- Group Assignment Topics - BEO6500 Economics For ManagementDocument3 pagesGroup Assignment Topics - BEO6500 Economics For ManagementnoylupNo ratings yet
- Branch ListDocument65 pagesBranch Listannamichelle1001No ratings yet
- FS2 Learning Experience 1Document11 pagesFS2 Learning Experience 1Jona May BastidaNo ratings yet
- Career Guidance Program Modules MonitoringDocument7 pagesCareer Guidance Program Modules MonitoringJevin GonzalesNo ratings yet
- Dues & Scholarship Section: NotificationDocument6 pagesDues & Scholarship Section: NotificationMUNEEB WAHEEDNo ratings yet
- Puberty and The Tanner StagesDocument2 pagesPuberty and The Tanner StagesPramedicaPerdanaPutraNo ratings yet
- Coursebook 1Document84 pagesCoursebook 1houetofirmin2021No ratings yet
- Bioethics: Bachelor of Science in NursingDocument6 pagesBioethics: Bachelor of Science in NursingSherinne Jane Cariazo0% (1)
- Kristine Karen DavilaDocument3 pagesKristine Karen DavilaMark anthony GironellaNo ratings yet
- Lesson 12 Elements of A Concept PaperDocument4 pagesLesson 12 Elements of A Concept PaperTrending Now100% (2)