Professional Documents
Culture Documents
Clinical Pharmacology 9
Uploaded by
ValdilanioCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Pharmacology 9
Uploaded by
ValdilanioCopyright:
Available Formats
CP
Clinical Pharmacology
Andrew Gao and Kapil Goela, chapter editors
Kenneth Lee and Raheem Peerani, associate editors
David Katz, EBM editor
Dr. David Juurlink, staff editor
Acronyms .............................. 2
Therapeutic Drug Monitoring (TOM) ....... 10
General Principles . ...................... 2
Drug Nomenclature
Phases of Clinical Testing
Drug Administration
Overview of Drug Disposition
Adverse Drug Reactions (ADRs) .......... . 10
Type A Drug Reactions
Type B Drug Reactions
Approach to Suspected ADRs
Variability in Drug Response . . ....... .. .. 11
Pharmacokinetics (ADME) ................ 3
Absorption
Mechanisms of Drug Absorption
Factors Affecting the Rate and Extent of
Drug Absorption
Bioavailability
Hepatic First-Pass Effect
Efflux Pump
Distribution
Factors Affecting the Rate and Extent of
Drug Distribution
Volume of Distribution
Plasma Protein Binding
Depots
Barriers
Drug Interactions ....................... 12
Autonomic Pharmacology.... . ........ . .. 13
Parasympathetic Nervous System (PNS)
Sympathetic Nervous System (SNS)
Common Drug Endings ..... . .. . ..... . .. 15
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15
Metabolism (Biotransformation)
Drug Metabolizing Pathways
Factors Affecting Drug Biotransformation
Elimination
Routes of Drug Elimination
Pharmacokinetics Calculations
Time-Course of Drug Action
Half-Life
Steady State
Clearance
Elimination Kinetics
Pharmacodynamics .... . ................. 8
Dose-Response Relationship
Efficacy
Potency
Effects of Drugs on Receptors
Agonists
Antagonists
Effectiveness and Safety
Therapeutic Index (TI)
Toronto Notes 2012
Clinical Pharmacology CPI
CP2 Clinical Pharmacology
Acronyms/General Principles
Toronto Notes 2012
Acronyms
ACh
ADR
888
CL
acetylcholine
adverse drug reaction
blood brain barrier
clearance
GYP
F
GFR
NE
cytochrome P450 protein
bioavailability
glomerularfiltration rate
norepinephrine
Po~w
Pgp
Tl
vd
partition coefficient of a drug
p-glycoprotein
therapeutic index
volume of distribution
General Principles
Drug Nomenclature
chemical name: describes the chemical structure; the same in all countries
e.g. N-(4-hydroxyphenyl)acetamide is acetaminophen
drug company code: a number; usually for drugs that are not yet marketed
non-proprietary (generic) name: shortened form of chemical name; listed in pharmacopoeia
e.g. acetaminophen
proprietary (trade) name: the brand name or registered trademark
e.g. Tylenol
street name: slang term used for a drug of abuse
Phases of Clinical Testing
At the time of drug launch, only data
from phases 1-111 are available; thus true
effectiveness (in contrast to efficacy)
and safety may be unknown because
real-world patients and usage patterns
sometimes differ significantly from
those in premarket phases.
phase 1: first administration to healthy human volunteers, following animal studies; to
determine pharmacokinetics and pharmacodynamics
phase II: first administration to patients, small studies; to determine therapeutic efficacy,
dose range, pharmacokinetics, pharmacodynamics
phase III: large sample, often double-blind RCT; to compare a new drug to placebo or standard
of care, establish safety and efficacy
phase IV: post-marketing surveillance, wide distribution; to determine rare adverse
reactions, effects oflong-term use, determine ideal dosing
Drug Administration
choice of route of administration depends on
properties of the drug
local and systemic effects (limiting action or adverse events)
desired onset and/or duration of action
patient characteristics
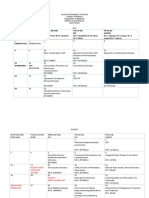
Table 1. Routes of Drug Administration
Common Latin Abbreviations
q
od/bid/tid/qid
hs
ac/pc/cc
prn
gtt
ung
ud
od/os/ou
ad/as/au
each, every
once/twice/three/four
times a day
at bedtime
before/after/with meals
as necessary
drops
ointment
as directed
right/left/each eye
right/left/each ear
Route
Advantage
Disadvantage
Oral IPO)
Convenient, easy to administer
Large surface area for absorption
Inexpensive relative to parenteral administration
Drug metabolism by Gl secretions
Incomplete absorption
Hepatic first-pass effect
Potential Gl irritation
BuccaVSublinguaiiSL)
Rapid onset of action
No hepatic first-pass effect
Must be lipid soluble
Must be non-irritating
Short duration of action
RectaiiPR)
Almost no hepatic first-pass effect
Convenient if patient is NPO,
vomiting or unconscious
Inconvenient
Irritation at site of application
Erratic absorption
Intravenous IIV)
Direct to systemic circulation
No hepatic first-pass effect
Slow infusion or rapid onset of action
Easy to titrate dose
Requires IV access, aseptic technique
Hard to remove once administered
Vascular injury, extravasation
Expensive
Risk of infection, bleeding
Intra-arterial
Direct to specific organs !heart, brain)
No hepatic first-pass effect
Depot storage if oil-based = slow release of drug
Aqueous solution = rapid onset of action
Risk of infection, bleeding, vascular
complications
Pain at site of injection
Subcutaneous ISC)
Non-irritating drugs, small volumes
Constant, even absorption
Alternative to IV
Pain at site of injection
Smaller volumes than IM
May have tissue damage from multiple
injections
Intrathecal
Direct into cerebrospinal fluid ICSF)
Bypass BBB and blood-CSF barrier
Infection
Possibility of brain herniation and coning
Intramuscular liM)
Toronto Notes 2012
General Principles/Pharmacokinetics (ADME)
Clinical Pharmacology CP3
Table 1. Routes of Drug Administration (continued)
Route
Advantage
Disadvantage
Inhalation
Immediate action in lungs
Rapid delivery to blood
Local or systemic action
No hepatic first-pass effect
Must be a gas, vapour or aerosol
Topical
Easy to administer
Localized
Limited systemic absorption
Effects are mainly limited to site of application
Transdermal
Drug absorption through intact skin
Rapid onset of action
No hepatic first-pass effect
Irritation at site of application
Delayed onset of action
Hydrophilic drugs are not easily absorbed
Others: Intraperitoneal,
Intra-articular
Local effect
Risk of infection
Overview of Drug Disposition
Pharmacology = Pharmacokinetics
+ Pharmacodynamics
Pharmacokinetics
the study of "what the body does to a drug;" the fate of a drug in the body
subdivided into ADME: Absorption, Distribution, Metabolism (biotransformation), and
Elimination
Pharmacodynamics
the study of "what a drug does to the body;" the interaction of a drug with its receptor(s) and
the resultant effect(s)
includes dose-response relationship, drug-receptor binding
Pharmacokinetics (ADME}
definition: relationship between drug administration, time-course of distribution, the
concentration achieved in the body (i.e. the manner in which the body handles a drug), and the
drug's removal from the body
examines rate and extent at which drug level concentrations change in the body by observing:
input processes = absorption
output processes responsible for drug delivery and removal from the body = distribution,
metabolism, elimination
Absorption
definition: movement of the drug from the site of administration into plasma
important for the main routes of administration, except IV
Mechanisms of Drug Absorption
most drugs are absorbed into the systemic circulation via passive diffusion
other mechanisms: active transport, facilitated diffusion, pinocytosis/phagocytosis
Factors Affecting the Rate and Extent of Drug Absorption
partition coefficient of a drug (Poil/water), i.e. its relative solubility in oil (lipid) vs. water
drugs with high lipid solubility can rapidly diffuse across a cell membrane (e.g. anesthetics
are very lipid soluble and thus have a rapid onset of action)
local blood flow at the site of administration (e.g. sublingual vessels provide significant blood
flow and thus rapid absorption)
molecular size (e.g. small molecular weight drugs absorb faster)
pH and drug ionization
drugs are usually weak acids (e.g. acetylsalicylic acid) or weak bases (e.g. ketoconazole) and
thus have both ionized and non-ionized forms
pH and pK. determine the ratio of ionized:non-ionized ratio (using the HendersonHasselbach equation)
non-ionized forms cross cell membranes much faster than ionized (charged) forms
total surface area for absorption
the small intestine has villi, which increase the surface area for absorption, making it the
primary site of absorption for most oral drugs
Partition Coefficient (Potwl
The ratio of a drug's solubility in lipid
as compared to water
More relevant when thought of
in terms of a drug's solubility
in membrane as compared to
extracellular fluid
A large Po1w means that a drug is
highly soluble in lipid and will thus
cross membranes easily
Drug Ionization and the
Henderson-Hasselbach Equation
Ionization reaction for a weak acid:
HA aA- + W ; pKa = pH + log [HA/A- ]
(Henderson-Hasselbach equation)
For a weak acid of pKa = 4.4,
at a gastric pH of 1.4,
non-ionized:ionized = HA:A- = 1: 0.001
Thus, the drug is mainly non-ionized and
diffuses across membrane
Ionization reaction for a weak base:
BW a B + W ; pKa = pH + log [BW/B]
CP4 Clinical Pharmacology
Pharmacokinetics (ADME)
Toronto Notes 2012
The amount of drug that reaches the
systemic circulation (bioavailability) is
highly dependent on absorption and the
first-pass effect. Properties of the drug,
route of administration, and patient
factors should be considered to ensure
clinical effectiveness.
Bioavailability (F)
definition: fraction of dose after administration that reaches systemic circulation in an
unchanged state
factors affecting bioavailability:
drug absorption, metabolism in the gut wall, and hepatic first-pass effect
IV dose has 100% bioavailability (F = 1)
drugs with a low bioavailability may require a much larger oral dose when compared to the IV
dose (e.g. ~-blockers: metoprololS mg IV vs. metoprololSO mg PO)
Examples of Drugs with High First
Pass Effect (Hepatic Extraction)
Levodopa
Morphine
Propranolol
Lidocaine
Organic nitrates
Hepatic First-Pass Effect
definition: drug metabolism by the liver following absorption, but before it reaches systemic
circulation
occurs with PO administration of a drug: GI tract (absorption) ~portal vein in liver (first-pass
metabolism) ~ systemic circulation; significant first-pass effect can drastically reduce a drug's
bioavailability
occurs to much lesser extent with PR administration, because drug absorbed in colon bypasses
the portal system: colon (absorption) ~ internal pudendal veins ~ IVC ~ systemic circulation
Examples of Drugs with Low First
Pass Effect
Diazepam
Digoxin
Phenytoin
Warfarin
Efflux Pump
P-glycoprotein (Pgp) is a protein in the GI tract, renal epithelium, and elsewhere that acts as a
multidrug efflux pump involved in the transport of drugs out of cells
acts to reduce intestinal absorption and enhanced renal elimination of certain drugs
examples of Pgp substrates: digoxin, dabigatran, etexilate, etoposide, paclitaxel, tacrolimus,
cyclopsorine
some drugs (e.g. macrolide antibiotics) inhibit Pgp and can increase absorption ofPgp
substrates and reduce their renal elimination
some tumours overexpress Pgp leading to multi-drug resistance to chemotherapy agents
Distribution
definition: process by which drugs move between different body compartments and to the site
of action
major body fluid compartments: plasma, interstitial fluid, intracellular fluid, transcellular fluid
(e.g. CSF, peritoneal, pleural)
tissue compartments: fat, brain
Factors Affecting the Rate and Extent of Drug Distribution
physicochemical properties of the drug (e.g. partition coefficient)
pH of fluid
plasma protein binding
binding within compartments
cardiac output
regional blood flow
percentage body fat
Total Body Water
60% of body weight
Figure 1. Distribution of Total Body
Water (TBWI
Volume of Distribution (Vdl
maximum actual Vd (anatomic volume accessible to drug) = total body water (40 L for average
adult) (see Figure 1)
Vd: the apparent volume of fluid into which a drug dissolves ( = amount of drug in body/plasma
drug concentration)
a theoretical value that relates amount of drug in the body to the plasma concentration
a calculated value that does not correspond to an anatomical space (when calculated, Vd can
sometimes be hundreds oflitres)
the value takes into account drug distribution into tissues and protein binding
volume of distribution of plasma-protein bound drugs can be altered by liver and kidney disease
example: amiodarone distributes into total body water (TBW = actual Vd = 40 L), but it also
concentrates in fat tissues giving instead an apparent Vd of 400 L; i.e. to achieve a given plasma
concentration of amiodarone, we dose as if the drug distributes into 400 L of body fluid
Plasma Protein Binding
drug molecules in the blood exist in two forms:
1. bound to plasma proteins
+ acidic drugs bind to albumin
+ basic drugs bind to a 1 -acid glycoprotein
2. free or unbound
+ only free drug can leave the circulation to distribute into tissues and exert an effect; free
drug is subject to metabolism and elimination
in plasma, the fractions of free and bound drugs exist in equilibrium, i.e. as free drug leaves the
circulation, more drug unbinds to equilibrate with the portion that is left
Toronto Notes 2012
Pharmacokinetics (ADME)
the fraction of drug that is bound is determined by
drug concentration, drug affinity for protein binding site, and number of binding sites or
protein concentration
saturation of binding sites may result in a large increase in free drug concentration, potentially
leading to toxicity
in hypoalbuminemia (liver failure or nephrotic syndrome), the dose of some highly bound
drugs must be lowered to avoid toxicity
multiple drugs and endogenous substances can compete for the same protein binding sites,
leading to increased free drug concentration but it is rarely of clinical significance
e.g. ASA displaces highly protein bound acidic drugs such as phenytoin, thus possibly
increasing the risk of toxicity; sulfonamide displaces bilirubin from protein binding sites,
which could potentially lead to jaundice and kernicterus in neonates
Depots
a body compartment (i.e. a type of tissue) where drug molecules tend to be stored and released
slowly over a long period of time
fat is a depot for very lipid soluble drugs (e.g. diazepam)
some oil-based medications are injected IM for slow release (e.g. depot medroxyprogesterone
acetate q3mo; depot risperidone q2wks)
Barriers (relative)
body structures that limit or prevent diffusion of drug molecules
e.g. the placenta or blood brain barrier (BBB; a barrier composed of tight junctions between
capillary endothelial cells and astrocytes)
many of these barriers result, in part, from the activity of multidrug efflux pumps (e.g. Pgp)
which serve as a natural defense mechanism against drugs and xenobiotics
need to consider dosing route if drugs are meant to cross these barriers
Clinical Pharmacology CPS
'
Special consideration must be given
in dosing patients in hypoalbuminemic
states to prevent drug toxicity. Highly
proteinbound drugs will exert a greater
effect in these patients than in healthy
individuals because of higher levels of
free drug.
Examples of highly protein-binding
drugs: warfarin, digoxin, diazepam,
furosemide, amitriptyline.
Main Factors Governing Penetration
of Blood Brain Barrier (BBB)
1. Small molecular size ( < 500 Daltons)
2. High lipid solubility
3. Active transport mechanisms
(e.g. Pgp multidrug efflux pump)
Many Drugs Cross BBB:
General anesthetics
Alcohol
Nicotine
Caffeine
L-dopa
Opioids
Psychotropic medications
Metabolism (Biotransformation)
definition: chemical transformation of a drug in vivo
sites of biotransformation: liver (main), GI tract, lung, plasma, kidney
goal is to make compounds more hydrophilic to enhance renal elimination
as a result of the process of biotransformation:
a pro-drug may be activated to an active drug (e.g. tamoxifen to endoxifen; codeine to
morphine)
a drug may be changed to another active metabolite (e.g. diazepam to oxazepam)
a drug may be changed to a toxic metabolite (e.g. meperidine to normeperidine)
a drug may be inactivated (e.g. procaine to PABA)
Drug Metabolizing Pathways
phase I (P450) reactions
small molecular changes introduce or unmask polar chemical groups on a parent compound
to increase its water solubility (e.g. oxidation-reduction, hydrolysis, hydroxylation); the
change in the partition coefficient is typically minimal (demethylation, deamination,
hydroxylation) compared to phase II, and often phase I places a polar 'handle' on a lipophilic
drug to allow for phase II
mediated by cytochrome P450 enzymes found in the endoplasmic reticulum
product of the reaction can be excreted or undergo further phase II reactions
phase II (conjugation) reactions
conjugation with large polar endogenous substrates (e.g. glucuronidation, glutathione
conjugation, sulfation)
dramatically increases water solubility and renal elimination
can occur independently of phase I reactions
Factors Affecting Drug Biotransformation
genetic polymorphism of metabolizing enzymes
individuals may metabolize drugs faster or slower depending on their genotype, resulting in
poor, intermediate, extensive or ultrarapid metabolizers
may lead to toxicity or ineffectiveness of a drug at a normal dose (e.g. tamoxifen and codeine
are prodrugs activated by 2D6, nonfunctional alleles reduce effectiveness whereas overactive
alleles or allelic duplication impart "ultrarapid metabolizer" phenotype), while warfarin
metabolized by 2C9 (nonfunctional alleles lead to lower dose requirements)
enzyme inhibition may sometimes be due to other drugs
e.g. CYP3A4 inhibition leads to an increased concentration of the substrate drug
erythromycin, ketoconazole and indinavir inhibit CYP3A4 and predispose a patient to drug
toxicity from other drugs metabolized by it
grapefruit juice inhibits gut CYP3A4 and effectively increases a substrate's bioavailability
Cytochrome P450 System
The P450 enzymes are a superfamily
of heme proteins that are grouped into
families and subfamilies according
to their amino acid sequence. These
proteins are responsible for the
metabolism of drugs, chemicals and
other substances.
Nomenclature: CYP3A4
"CYP" = cytochrome P450 protein
1st number = family
letter = subfamily
2nd number = isoform
The CYP1 , CYP2, and CYP3 families
metabolize most drugs in humans. The
most important isoforms are CYP3A4
and CYP2D6; therefore, anticipate drug
interactions if prescribing drugs using
these enzymes.
CP6 Clinical Pharmacology
Some Common Examples of P450
Inhibitors and Inducers
P450 inhibitors "MINCE"
Metronidazole (GYP 2G9)
Isoniazid (GYP 2G9), lndinavir (GYP 3A4)
Naringin or bergamottin (bioflavenoid in
grapefruit) (GYP 3A4)
Ciprofloxacin (GYP 3A4, 1A2)
Cimetidine (GYP 2G19, 206)
Erythromycin (macrolides) (GYP 3A4)
P450 inducers
Phenytoin (GYP 3A4)
Phenobarbital (GYP 3A4)
Rifampin (GYP 206, 3A4)
Smoking (GYP 1A2)
Note: The above list is not exhaustive.
The very young and the very old are
very sensitive to the actions of drugs.
Pharmacokinetics (ADME)
Toronto Notes 2012
enzyme induction
certain medications enhance gene transcription leading to an increase in the activity of a
metabolizing enzyme
a single drug may stimulate multiple P450 isoenzymes simultaneously
a drug may induce its own metabolism (e.g. carbamazepine) or that of other drugs
(e.g. phenobarbital can induce the metabolism of OCP and bilirubin) by inducing the P450
enzyme system
other potent enzyme inducers: phenytoin, dexamethasone
liver dysfunction caused by disease (such as hepatitis, alcoholic liver, biliary cirrhosis, or
hepatocellular carcinoma) may decrease drug metabolism, but this may not be clinically
significant due to the liver's reserve capacity
renal disease often results in decreased drug clearance if it is cleared by the kidneys
extremes of age (neonates or elderly) have reduced biotransformation capacity, and doses
should be adjusted accordingly
nutrition
insufficient protein and fatty acid intake decrease P450 biotransformation
vitamin and mineral deficiencies may also impact metabolizing enzymes
alcohol: while acute alcohol ingestion inhibits 21, chronic consumption can induce this
same enzyme and increase the risk of hepatocellular damage from acetaminophen by
increasing the generation of acetaminophen's toxic metabolite
smoking can induce 1A2, thus increasing the metabolism of some drugs (e.g. smokers
may require higher doses of theophylline, which is metabolized by 1A2)
Elimination
definition: removal of drug from the body
rn
Avoid toxicity from drug or metabolite
accumulation by adjusting a drug's
dosage according to the elimination
characteristics of the patient (e.g. in
renal impairment).
The Cockcroft-Gault Equation can
estimate creatinine clearance (CrCI)
in adults 20 yrs of age and older:
For males
GrGI (mLJmin) =
[(140- age in yrsl x Weight !kg)] x 1.2
serum Gr ().lmoVL)
For females, multiply above equation
X 0.85
Only applies when renal function is at
steady state
Routes of Drug Elimination
kidney (main organ of elimination)
two mechanisms for renal elimination
1. glomerular filtration
- a passive process, so that only the free drug fraction can be filtered
- drug filtration rate depends on GFR, degree of protein binding of drug, and size of
drug
2. tubular secretion
- an active process that is saturable, allowing both protein-bound and free drug
fractions to be excreted
-two distinct transport mechanisms for weak acids (e.g. penicillin, salicylic acid,
probenecid, chlorothiazide) and weak bases (e.g. quinine, quaternary ammonium
compounds such as choline)
- drugs may competitively block mutual secretion if both use the same secretion system
(e.g. probenecid can be used to reduce the excretion of penicillin, thereby prolonging
the half-life and thus the effect of the antibiotic)
tubular reabsorption: drugs can be passively reabsorbed back to the systemic circulation,
countering elimination mechanisms
elimination rate depends on renal function, which decreases with age and is affected by
many disease states; renal function is assessed clinically using serum creatinine (Cr) levels
thus, in those with renal impairment, dosage adjustments may be required for medications
affected by renal elimination
stool
some drugs and metabolites are actively excreted in the bile (e.g. corticosteroids) or directly
into the intestinal tract from systemic circulation
enterohepatic circulation counteracts stool elimination, and thus can substantially prolong
the drug's duration in the body
some glucuronic acid conjugates that are excreted in the bile will be hydrolyzed in the
intestines by bacteria; this results in the drug being converted back to its original form
and allows for systemic reabsorption
lungs
elimination of anesthetic gases and vapours by exhalation
saliva
saliva concentrations of some drugs parallel their plasma levels (e.g. rifampin)
Pharmacokinetics (ADME)
Toronto Notes 2012
Clinical Pharmacology CP7
Pharmacokinetics Calculations
definition: the quantitative description of the rates of the various steps of drug disposition, i.e.
how drugs move through the body
the pharmacokinetic principles of ADME (absorption, distribution, metabolism, and
elimination) can be graphically represented on the concentration vs. time graph (see Figure 2)
Time-Course of Drug Action
many kinetic parameters are measured using IV dosing, such that absorption is immediate and
distribution for most drugs is rapid; thus elimination is the main process being measured
the concentration axis is converted to a log10 concentration to allow for easier mathematical
calculations (see Figure 3)
Half-Life (t112)
definition: time taken for the serum drug level to fall to 50% during elimination
for drugs with first order kinetics, takes five half-lives to reach steady state with repeated dosing,
or for drug elimination once dosing is stopped
see sidebar for calculation
# of Half Lives
Concentration
2
50%
75%
87.5%
3.3
90%
93.8%
Principles of Pharmacokinetics
Vd = amount of drug in the body/
plasma drug concentration
CL = rate of elimination of drug/plasma
drug concentration
Half-life (t112) = 0.7xVJCL
For most drugs, it takes 5 half-lives to
reach steady state with repeated dosing
or to eliminate a drug once dosing is
stopped.
1. Absorption Phase
2. Peak Absorption
3. Post-Absorption
Distribution Phase
4. Elimination Phase
(half-life based on
this)
96.9%
Steady State
the concentration at which the same amount of drug entering the system is eliminated
from the system
time is important for therapeutic monitoring since drug levels are reliable only when the
drug has reached steady state (see Figure 4)
special situations
use a loading dose for drugs with a long half-life and when there is clinical need to rapidly
achieve therapeutic levels (e.g. amiodarone, digoxin, phenytoin)
use continuous infusion for drugs with a very short half-life and when there is need for a
long-term effect and multiple or frequently repeated doses are too inconvenient
(e.g. nitroprusside, insulin, unfractionated heparin)
Clearance (CL)
a quantitative measurement of the rate of removal of a substance from the body
relates the rate of elimination to the plasma concentration
clearance = body fluid volume from which a substance is removed per unit time
consider: clearance from a specific part of the body and total body clearance
CL = rate of elimination of drug/plasma drug concentration
Time to Peak Absorption
Figure 2. Time Course of Drug
Action
/
C, = concentration at time 0
.,"
.0
/K=slope
t:
"'g
0
'-'
_g
"'
Time (hrs)
Figure 3. Log Concentration vs.
Time Graph (IV bolus dose)
Steady state of adrugwith t1a of 3 hrs. It takes
about 15 hrs (5xt1nl to reachsteady state.
Elimination Kinetics (see Figure 5)
first-order kinetics (most common type)
predictable relationship that leads to a constant fraction of drug eliminated per unit time
the amount of drug eliminated is based on the concentration of drug present
zero-order kinetics (less common, associated with toxicities, e.g. alcohol)
a constant rate of drug eliminated regardless of concentration
clearance slows as drug concentration rises
some drugs can follow first-order kinetics until elimination is saturated (usually at large
doses) at which point the clearance decreases
Table 2. Loading vs. Maintenance Dosing
12
Time (hrs)
Loading Dose
Maintenance Dose
Use when you need an IMMEDIATE effect
Consider either: after a loading dose OR beginning with maintenance doses
Often parenteral medication
Steady-state levels achieved after -5 half lives
Rationale: give large dose of medication to "fill up" Can be given as either a continuous infusion (relatively rare, short half-life drug)
the volume of distribution
OR much more commonly as intermittent doses
Figure 4. Steady State of a Drug
"
0
100
-~
t:
"'" 50
"
"'
C1
0
'-'
2
25
8
Time (hrs)
Figure 5. First and Zero Order
Kinetics. In first order kinetics (solid line), a
constant fraction of thedrugis eliminated per unit time;
in zero order kinetics (dashed line), aconstant amount of
the drugis eliminated per unit time.
CPS Clinical Pharmacology
Pharmacodynamics
Toronto Notes 2012
Pharmacodynamics
For unit conversion factors, please see
Appendix: Common Unit Conversions.
Dose-Response Relationship
efficacy and potency are two important pharmacodynamic characteristics of a drug that can be
quantified using dose-response curves
with gradual dose-response relationships, the response of the drug reflects the number of
receptors that are effectively occupied
Efficacy versus Potency
Efficacy measures a drug's maximal
effect and is independent of
concentration.
Potency measures a drug's
concentration needed to produce a
certain effect.
Efficacy
a measure of a drug's ability to elicit a concentration-independent effect at its receptor
measured as Emax =the maximal response that a drug can elicit (see Figure 6)
e.g. if Drug A causes a greater maximum intensity of response than Drug B regardless of dose,
then Drug A is more efficacious than Drug B
Potency
a measure of the effect produced by a certain drug concentration
measured as EC50 = the effective concentration of a drug needed to produce 50% of the
maximal possible effect (see Figure 6)
can compare the EC50 of two or more drugs that have parallel log dose-response curves
the drug that reaches its EC50 at the lower dose is the more potent
if the potency of a drug is low, this may be overcome by increasing the dose of the drug
(e.g. 30 mg vs. 15 mg); this is not problematic provided that the higher dose not cause adverse
effects
100
Em~
of A and C
c
Potency:
A> B>C
~ 60
ill
"~
(both Band C
are less potent
than A)
50
Q)
0::
30
Efficacy:
A= C> B
Log of dose
Jason Raine
Figure 6. Log Dose-Response Curve Illustrating Efficacy and Potency
Effects of Drugs on Receptors
drugs that act on specific receptors can be broadly classified as agonists or antagonists
(see Figure 7)
Agonists
drugs that mimic endogenous ligands and exert an effect
have two main properties
affinity: the ability of the agonist to bind to the receptor (e.g. the ~2 -agonist salbutamol has
greater affinity for ~2 - receptors than ~ 1 -receptors)
efficacy: the ability to cause a response via the receptor interaction (e.g. binding of
salbutamol to ~2 -receptors results in smooth muscle relaxation)
full agonists: can elicit a maximal effect at a receptor
partial agonists: can only elicit a partial effect, no matter how high the concentration
e.g. reduced efficacy compared to full agonists
Antagonists
drugs that have affinity (can bind to a receptor), but no efficacy
these are drugs that block the action of an agonist or of an endogenous ligand
chemical antagonism: direct chemical interaction between agonist and antagonist that prevents
agonist binding to receptor
e.g. chelating agents for removal of heavy metals
Toronto Notes 2012
Pharmacodynamics
functional antagonism: interaction of two agonists that act independently at different receptors
but have opposite physiological effects
e.g. acetylcholine at the muscarinic receptor decreases HR, constricts pupils, and stimulates
intestinal motility; whereas epinephrine at the adrenergic receptor increases HR, dilates
pupils, and decreases intestinal motility
reversible competitive antagonism (most common in clinical practice, see Figure 8)
antagonist reversibly binds to the same receptor as the agonist, thus displacing it
(e.g. naloxone is an antagonist to morphine or heroin)
irreversible competitive antagonism (see Figure 9)
antagonist irreversibly binds to the same receptor as the agonist, blocking it from binding
(e.g. acetylsalicylic acid irreversibly binds cyclo-oxygenase in platelets)
non-competitive antagonism (see Figure 9)
antagonist binds to an alternate site separate but near the agonist site, producing allosteric
effects that change the ability of the agonist to bind (e.g. organophosphates irreversibly bind
acetylcholinesterase)
AGONIST BINDING
.,;.. 0
D c[]
c::::>
Receptor
Clinical Pharmacology CP9
Dose of Agonist
A -> C increasing dose of competitive
antagonist
At each dose of antagonist, increasing the
concentration of agonist can overcome
the inhibition.
Figure 8. The Log Dose-Response
Curve for Competitive Reversible
Antagonism
c::::> '"; """
A
BINDING
B
ANTAGONIST BINDING
1) Competitive reversible binding
,.:::::~
D tJ
c::::> 0
Receptor
~~c[] c::::>
c::::>
Antagonist
binding
REVERSIBLE
BINDING
Increased
concentration
of agonist
overcomes
antagonist
binding
competition
2) Competitive irreversible binding
Agonist
Antagon
0
c:::::> o~jt:
c:::::> 00 (]=11t~:
c:::::>
:::
:::
Receptor
oo
Antagonist
binding
IRREVERSIBLE
BINDING
D 0
Agonist
cannot bind
receptor which
is irreversibly
blocked by
antagonist
0
Dose of Agonist
A -> D increasing dose of irreversible
antagonist
With one dose of antagonist, increasing
dose of agonist does not completely
overcome antagonism, as seen in B.
Eventually with high enough antagonist
concentrations, no amount of agonist can
elicit a response, as seen in D.
Figure 9. The Log Dose-Response
Curve for Irreversible Antagonism
3) Non-competitive irreversible binding
Agonist
Antagonist @
c:::::>
Receptor
c:::::>
Antagonist
binding
Mc:::::>
oc;J
ALLOSTERIC
CHANGE
Antagonist
bound to
alternative
site prevents
agonist from
binding to
receptor
Figure 7. Mechanism of Agonists and Antagonists
Effectiveness and Safety
---------------------------------"
Effectiveness
ED 50 (Effective Dose- 50%): the dose of a drug needed to cause a therapeutic effect in 50% of a
test population of subjects
Safety
LD 50 (Lethal Dose- 50%): the dose of a drug needed to cause death in 50% of a test population
of subjects (usually rodents)
TD 50 (Toxic Dose - 50%): the dose needed to cause a harmful effect in 50% of a test population
of subjects
The two most clinically relevant
properties of any drug are effectiveness
and safety.
CPIO Clinical Pharmacology
Pharmacodynamics/Drug Monitoring!Adverse Drug Reactions
Toronto Notes 2012
Therapeutic Index (TI)
Drugs with a narrow Tl have a high
likelihood of causing toxicity and need
close therapeutic monitoring.
defined as TD 50/ED50 (see Figure 10)
reflects the "margin of safety" for a drug - the likelihood of a high dose causing serious toxicity
or death
the larger the TI, the safer a drug (e.g. amoxicillin has a wide TI, thus therapeutic monitoring is
not needed, whereas warfarin has a narrow TI and must have accurate therapeutic monitoring)
factors that can change the ED50 , LD50 or TD 50
presence of interacting drugs
changes in drug absorption, distribution, metabolism, elimination
100%
Efficacy
Toxicity
100%
Toxicity
a>
~ 50%
50%
5r
a>
a>
a:;:
a:;:
Log Dose
Log Dose
The therapeutic index (TD5,/ED50 ) is a measure
of the margin of safety of a given drug.
Drug A has a much narrower therapeutic index than Drug B. The
dose of Drug A required to achieve a 100% therapeutic response
will be toxic in 50% of patients. For Drug 8, this is only 10%.
Figure 10. ED 50 , TD 50, and the Therapeutic Index (TI)
Therapeutic Drug Monitoring (TOM)
Examples of drugs whose levels need to
be monitored: warfarin (via INR levels),
digoxin, lithium, anti-epileptics (e.g.
phenytoin, carbamazepine), and many
others.
definition: using serum drug concentration data to optimize drug therapy (e.g. dose adjustment,
monitor compliance)
serum drug samples are usually taken when the drug has reached steady state (e.g. trough
level- the lowest level before the next dose), and thus, before the next dose
TDM can serve to monitor for side effects (e.g. vancomycin trough levels) and for desired effect
(e.g. INR when on warfarin therapy)
TDM is often used for drugs that have:
narrow therapeutic index (TI)
unpredictable dose-response relationship
significant consequences associated with therapeutic failure or toxicity
wide inter-patient pharmacokinetic variability
Adverse Drug Reactions (ADRs)
In Canada, an estimated 1.6% of
patients admitted to hospitals
experience a serious adverse drug
reaction. Furthermore, up to 24% of
hospitalizations are drug related, of
which 35.5% are adverse drug reactions.
classification of adverse drug reactions
type A: undesirable normal/augmented responses to the drug (>80% of all ADRs)
type B: reaction unrelated to the known pharmacological actions of the drug
additional adverse drug reaction categories
type C (chronic effects), typeD (delayed effects), type E (end-of-treatment effects), and
type F (failure of therapy)
Table 3. Comparison of Characteristics of Type A and Type B Reactions
~A
~8
Predictable extension of drug's pharmacologic effect
Unpredictable
Usually dose dependent
Rarely dose dependent
low mortality (some exceptions)
High mortality (some exceptions)
Responds to dose reduction
Responds to drug withdrawal
Toronto Notes 2012
Adverse Drug Reactions/Variability in Drug Response
Clinical Pharmacology CPII
Type A Drug Reactions
extension of a drug's pharmacological effects: excessive but characteristic pharmacological
effect from usual dose of a drug (e.g. ~-blockers causing bradycardia; acetaminophen causing
hepatitis)
overdose/toxicity: exaggerated but characteristic pharmacological effect from supra-therapeutic
dose
teratogen: drug may produce developmental defects in fetus (not always in a dose-related
manner)
Type B Drug Reactions
idiosyncratic: uncharacteristic response to drug, unrelated to pharmacology (e.g. sulfacontaining medications causing toxic epidermal necrolysis)
pseudoallergenic: mimics immune-mediated reaction
allergic/immune-mediated: does not occur on first exposure (up to 7 d), immediate with
subsequent exposure, may occur with low doses, often resolves within 3-4 d of discontinuation
Approach to Suspected ADRs
history and physical examination: signs and symptoms of the reaction (e.g. rash, fever, hepatitis,
anaphylaxis, etc.), timing, risk factors, detailed medication history including all drugs and
timing, dechallenge (response when drug is removed) and rechallenge (response when drug is
given again)
check with literature, Health Canada and FDA; contact the pharmaceutical company
differentiate between drug therapy vs. disease pathophysiology
treatment: stop the drug, supportive care, symptomatic relief
Canadian Adverse Drug Reaction Monitoring Program online
report all suspected ADRs that are: 1) unexpected, 2) serious, or 3) reactions to recently
marketed drugs (on the market <5 yrs) regardless of nature or severity
Table 4. Sample of Clinically Relevant Adverse Drug Reactions
Classification
Drug(sl
Adverse Drug Reaction
Comments
~-blockers
Bradycardia
Dose dependent
ACEI
Cough
Switch AGEl to ARB
Vancomycin
Red Man Syndrome
Pruritic erythematous rash on upper body related to rapid
infusion; histamine release
Not considered an allergy
SuHa Drugs
Stevens-Johnson Syndrome
Toxic Epidermal Necrolysis
Life threatening; do not rechallenge under any
circumstance
Penicillins
Rash
Many children with EBV infection will develop a rash when
given amoxicillin; this is NOT a true penicillin allergy
Aminoglycosides
Ototoxicity and nephrotoxicity Dose dependent
Acetaminophen,
valproic acid,
Chinese herbs
Hepatotoxicity
Many other drugs are hepatotoxic (e.g. statins, OCPs,
isoniazid!
Variability in Drug Response
recommended patient dosing is based on clinical research and represents mean values for a
select population, but each person may be unique in their dosing requirements
the majority (but not all) of the patients will experience the desired therapeutic effect of a
drug with minimal ADRs on the recommended dose
may need to adjust dosing or alter medication altogether
there may be multiple causes of individual variability in drug response at a given dose, and they
should be considered when prescribing and dosing medications
Sulfa-Containing Medications
Sulfamethoxazole
Sulfasalazine
Dapsone
CP12 Clinical Pharmacology
Variability in Drug Response/Drug Interactions
Toronto Notes 2012
possible causes of variable drug responses include problems with:
intake
patient adherence, e.g. hard to follow dosing schedule, non-palatable drug, costly drug
pharmacokinetics (review pages CP3-CP7)
absorption
- decreased by vomiting, diarrhea or steatorrhea
- hepatic first pass effect too high due to enzyme induction, or too low due to liver disease
- absorption change due to drug interactions (e.g. calcium carbonate chelates iron)
distribution
- very high or low percentage body fat, intact or disrupted BBB
- patient is elderly or a neonate, or has liver dysfunction
biotransformation and elimination
- certain genetic polymorphisms or lack of enzymes to metabolize drugs
(e.g. acetylcholinesterase deficiency, CYP polymorphism)
- kidney or liver dysfunction, or obstruction of bile elimination pathway
pharmacodynamics
genetic variability in drug response (e.g. malignant hyperthermia due to specific
anesthetic agents)
disease process that affects drug pharmacodynamics
drug tolerance or cross-tolerance
Drug Interactions
concomitant prescription of multiple drugs may lead to a situation where one drug alters the
effect of another by changing its pharmacokinetic fate and/or pharmacodynamic action
pharmacokinetic interactions involve altered absorption, distribution, metabolism, excretion
absorption: alterations in gastrointestinal pH, gastric emptying, intestinal motility, gut
mucosal function
distribution: alterations in blood flow, plasma protein binding, tissue stores
biotransformation: alterations in drug metabolizing enzymes can increase or decrease drug
concentration, duration of action, clearance
excretion: alterations in renal elimination (glomerular filtration, tubular reabsorption and
secretion)
pharmacodynamic interactions are drug-induced alterations in the effects of other drugs due to
exertion of similar changes to the body's physiology (additive) or opposing changes (subtractive)
Table 5. Sample of Clinically Relevant Drug Interactions
Interaction
Potential Effect
Comments
Warfarin plus ciprofloxacin, clarithromycin,
erythromycin, metronidazole, or trimethoprim-
Increased effect of warfarin
Use alternative antibiotic
Antibiotics inhibit intestinal production of
vitamin K
Inhibition of hepatic metabolism of warfarin
Oral contraceptive pills plus rifampin,
antibiotics, or troglitazone
Decreased effectiveness of oral
contraception
Avoid if possible
Increased metabolism of exogenous estrogen
Sildenafil plus nitrates
Hypotension
Absolute contraindication
Vasodilatation
SSRI plus St. John's wort, naratriptan,
rizatriptan, sumatriptan, zolmitriptan
Serotonin syndrome
Avoid if possible
Monitor for signs and symptoms of serotonin
syndrome
SSRI plus selegiline or non-selective MAO-I
Hypertensive crisis
Avoid
Additive serotonergic effects
HMG-CoA reductase inhibitor plus niacin,
gemfibrozil, erythromycin, or itraconazole
Possible rhabdomyolysis
Avoid if possible
su~amethoxazole
Toronto Notes 2012
Autonomic Pharmacology
Clinical Pharmacology CP13
Autonomic Pharmacology
Peripheral Nervous System
I
Somatic
Autonomic (ANS)
Sympathetic (SNS)
Fight or Flight
Parasympathetic (PNS)
Rest and Digest
Preganglionic
Neuron
Figure 11. Subdivisions of the Peripheral Nervous System
most organs are innervated by both sympathetic and parasympathetic nerves; these have
opposing effects (see Figure 13)
almost all ANS efferent tracts are divided into preganglionic and postganglionic nerves, which
synapse in the autonomic ganglion (see Figure 12)
sympathetic preganglionic fibers originate in the spinal cord at spinal levels Tl-L3, and
terminate in one of two ganglia
1. paravertebral ganglia (i.e. the sympathetic trunk) that lie in a chain close to the vertebral
column
2. pre-vertebral ganglia (i.e. celiac and mesenteric ganglia) that lie within the abdomen
parasympathetic preganglionic fibers originate in the lower brainstem from cranial nerves III,
VII, IX, X, and in the sacral spinal cord at levels S2-S4; they terminate in the ganglionic cells
located near or within the target organ
both sympathetic and parasympathetic pre-ganglionic nerves release acetylcholine (ACh) which
acts on a nicotinic receptor
post-ganglionic sympathetic nerves release norepinephrine (NE), which acts on a and~
receptors, while post-ganglionic parasympathetic nerves release ACh which acts on muscarinic
receptors
the exceptions are post-ganglionic sympathetic nerves to blood vessels, sweat glands, spleen
capsule, adrenals, which do NOT have parasympathetic innervation
PARASYMPATHETIC
A
B
C
D
E
Constricts pupil
Stimulates salivation
Slows heart rate
Constricts bronchi
Stimulates peristalsis
F Stimulates bile
G Stimulates intestinal
mobility
H Relaxes rectum
I Contracts bladder
Figure 13. Autonomic Nervous System
SYMPATHETIC
1 Dilates pupil
2 Inhibits salivation
3 Accelerates heart rate and
improves contractility
4 Dilates bronchi
5 Stimulates secretion of
adrenaline and noradrenaline
Stimulates metabolism
and glucose release
7 Inhibits peristalsis
8 Inhibits intestinal mobility
9 Contracts rectum
10 Relaxes bladder
~
]1
o;
"'
~
~
~
@
''
1
1
1
1
Autonomic
Ganglion
ACh
AChor NE
Target
Organ
Figure 12. Autonomic Nervous
System (ANS) Efferent Tracts
CP14 Clinical Pharmacology
Autonomic Pharmacology
Toronto Notes 2012
Parasympathetic Nervous System (PNS)
ACh is the main neurotransmitter of the parasympathetic nervous system
ACh receptors include
nicotinic (pre-ganglionic) receptors located in the autonomic ganglia and nicotinic
(post-ganglionic) receptors in the adrenal medulla
muscarinic (only post-ganglionic) receptors
M 1 located in the CNS
M 2 receptors located on smooth muscle, cardiac muscle, and glandular epithelium
ACh action is terminated by metabolism in the synaptic cleft by acetylcholinesterase and in the
plasma by pseudocholinesterase
e.g. acetylcholinesterase inhibitors (donepezil, galantamine, rivastigmine) are used to
increase ACh levels in conditions such as myasthenia gravis and Alzheimer's disease
Sympathetic Nervous System (SNS)
NE is the major neurotransmitter of the SNS
receptors include
~ 1 : predominately in cardiac tissue
~ 2 : predominately in smooth muscle and glands
a 1: predominately on post-synaptic receptors in smooth muscles and glands
a 2: predominately on pre-synaptic terminals, where they feed back to inhibit further NE
release; also exist as post-synaptic terminals in the brain, uterus, and vascular smooth muscle
NE action is terminated by reuptake by the presynaptic membrane, diffusion from the synaptic
cleft and degradation by monoamine oxidase (MAO) and catechol-0-methyl transferase
(COMT)
Table 6. Direct Effects of Autonomic Innervation on the Cardiorespiratory System
Organ
Heart
1. Sinoatrial
2. Atrioventricular node
3. Atria
4. Ventricles
Blood Vessels
1. Skin, splanchnic
2. Skeletal muscle
Sympathetic Nervous System
Receptor
Action
Receptor
Action
~I
~I
~I
~I
Increased HR
Increased conduction
Increased contractility
Increased contractility
M
M
M
M
Decreased HR
Decreased conduction
Decreased conduction
Decreased conduction
a,, a,
Constriction
Constriction
Dilatation
Constriction
Dilatation
M
M
M
M
M
Dilatation
Dilatation
Dilatation
Dilatation
Dilatation
Relaxation
Increased secretion
M
M
Constriction
Stimulation
a.
~2 -large muscles
3. Coronary
a., a,
~2
Lungs
1. Bronchiolar smooth muscle
2. Bronchiolar glands
Parasympathetic Nervous System
j3,
a,, ~2
Toronto Notes 2012
Common Drug Endings/References
Clinical Pharmacology CPIS
Common Drug Endings
Table 7. Common Drug Endings
Ending
Category
Example
-alii
5-PDE inhibitor
sildenafil
-ane
Inhaled general anesthetic
halothane
-azepam
Benzodiazepine
lorazepam
-azole
Antifungal
ketoconazole
-caine
Local anesthetic
lidocaine
-olol
~-blocker
propranolol
-prazole
Proton pump inhibitor
omeprazole
-pril
ACE inhibitor
captopril
-sartan
ARB
candesartan
-stalin
HMG-CoA inhibitor
atorvastatin
-terol
~' agonist
albuterol
-tidine
H, antagonist
cimetidine
-tropin
Pituitary hormone
somatotropin
-vir
Antiviral
acyclovir
-zosin
a, antagonist
prazosin
Note: Some medications are exceptions to the rule, e.g. methimazole (antithyroid)
References
Ament PW, Bertolino JG, Liszewski Jl. Clinically Significant Drug Interactions. Am Fam Physician. 2000; 61:1745-54.
Baker GR, Norton PG, Flintoft V. Blais R, Brown A. Cox J, et al. The Canadian Adverse Events Study: the incidence of adverse events among hosprral patients in Canada. CMAJ. 2004; 170:1678-86.
Hardman JG and limbird LR, edrrors. Goodman and Gilman's the Phannacological Basis of Therapeutics. 9th ed. New Yoric McGraw-Hill; 1996.
Hardy Band Bedard M. Serum Drug Concentration Monitoring. In: Compendium of Phannaceuticals and Speciatties. Ottawa: CanadianPhannacists Association; 2002.
Indiana University Division of Clinical Phannacology P450 Drug Interaction Table httpJ/medicine.iupui.edulclinpharnvllDis/table.aspx
Kalant H, Grant DM, Mitchell J, editors. Principles of Medical Phannacology. 7th ed.Toronto: Elsevier Canada; 2007.
Katzung BG, edrror. Basic and Clinical Phannacology. 8th ed. New York: McGraw-Hill Companies; 2001.
lewis T. Using the NO TEARS tool for medication review. BMJ. 2004; 329(7463):434.
MedEffect Canada. Canada Vigilance Adverse Reaction Online Database [Internet]. Ottawa (ON): Heatth Canada. c1964 [last updated 2011 Mar 31; cited 2011 Aug 20]. Available from:
httpJ/www.hc-sc.gc.ca/dhp-mps/medeff/ databasdorVindex_e.html.
P450 Drug Interaction Table [Internet]. India: Division of Clinical Phannacology, Indiana University; c2009 [updated 18 Aug 2011; cited 20Aug 2011]. Available from: httpJ/medicine.iupui.edwclinpharnvUDis/table.aspx
Rang H, DaleM, Ritter J, editors. Phannacology. 4th ed. Edinburgh: Churchill Livingstone; 1999
Samoy LJ, Zed PJ, Wilbur K, BalenRM, Abu-laban RB, Roberts M. Drug-Related Hospitalizations inaTertiary Care Internal Medicine Service of aCanadian Hosprral: AProspective Study. Phannacotherapy. 2006; 26(11):1578-86.
CP16 Clinical Pharmacology
u\foteg_ _ _ _ _ _ _ _ _ __
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Ingredients and Foods Associated With Adverse Reactions in Dogs and CatsDocument2 pagesIngredients and Foods Associated With Adverse Reactions in Dogs and CatsWilliam Chandler100% (1)
- Somalia Standard Treatment Guidelines and Training ManualDocument154 pagesSomalia Standard Treatment Guidelines and Training ManualAhmed Reda DoniaNo ratings yet
- The Relationship Between Lithium and Cancer Proliferation: A Case-Based Review of The LiteratureDocument10 pagesThe Relationship Between Lithium and Cancer Proliferation: A Case-Based Review of The LiteratureValdilanioNo ratings yet
- Pahwa 2021Document9 pagesPahwa 2021ValdilanioNo ratings yet
- Office 2016 Preview: Don't Have Office 365?Document3 pagesOffice 2016 Preview: Don't Have Office 365?ValdilanioNo ratings yet
- ArtigoDocument13 pagesArtigoValdilanioNo ratings yet
- Artigo HematomaDocument6 pagesArtigo HematomaValdilanioNo ratings yet
- Cardiovascular Risk Factors of Taxi DriversDocument18 pagesCardiovascular Risk Factors of Taxi DriversValdilanioNo ratings yet
- (SpringerBriefs in Economics) Noriatsu Matsui, Yukio Ikemoto (Eds.) - Solidarity Economy and Social Business - New Models For A New Society-Springer Japan (2015)Document113 pages(SpringerBriefs in Economics) Noriatsu Matsui, Yukio Ikemoto (Eds.) - Solidarity Economy and Social Business - New Models For A New Society-Springer Japan (2015)ValdilanioNo ratings yet
- Epilepsy Guideline ST Epilepticus Children N Adult 2016Document14 pagesEpilepsy Guideline ST Epilepticus Children N Adult 2016Desi ChiloupChaNo ratings yet
- Assignment 1Document13 pagesAssignment 1林佑邦No ratings yet
- Diabetic RetinopathyDocument18 pagesDiabetic Retinopathymohelshiekh100% (3)
- Prosedur Manual PlasentahjhjjhkjkjDocument15 pagesProsedur Manual PlasentahjhjjhkjkjMif Al-HudaNo ratings yet
- Spleen Diseases DiagnosisDocument2 pagesSpleen Diseases DiagnosisPraveen VontiNo ratings yet
- Pharmacology of Oleanolic Acid and Ursolic Acid: Review ArticleDocument12 pagesPharmacology of Oleanolic Acid and Ursolic Acid: Review ArticlepunitNo ratings yet
- Components of General Anesthesia: UnconsciousnessDocument17 pagesComponents of General Anesthesia: UnconsciousnessDanieleNo ratings yet
- Medication BookDocument448 pagesMedication BookAlbert ChuwaNo ratings yet
- Test 9 - UpDocument18 pagesTest 9 - UpSon NguyenNo ratings yet
- CNA Practice TestDocument12 pagesCNA Practice TestJoe Prempeh50% (4)
- Section A Schedule - Didactic 2Document5 pagesSection A Schedule - Didactic 2AdityaTiwariNo ratings yet
- Handouts Lymphatic System F11Document7 pagesHandouts Lymphatic System F11Kelly TrainorNo ratings yet
- Ayuvediya Approch Toward Iron Deficiency Anaemia - A Case StudyDocument4 pagesAyuvediya Approch Toward Iron Deficiency Anaemia - A Case StudyIJAR JOURNALNo ratings yet
- AnemiaDocument40 pagesAnemiaRajaNo ratings yet
- Bodytalk:: Exploring The 3 BrainsDocument31 pagesBodytalk:: Exploring The 3 BrainsPenelopeReyesNo ratings yet
- Prepared by Muhammad Salman: This Brand Plan Has Been Designed For The ProductDocument90 pagesPrepared by Muhammad Salman: This Brand Plan Has Been Designed For The ProductMuhammad SalmanNo ratings yet
- Occupational Therapy - Kids Health Information: Scar ManagementDocument4 pagesOccupational Therapy - Kids Health Information: Scar Managementmuambany1No ratings yet
- 2006 TOUCH FOR HEALTH Annual Meeting ReporDocument80 pages2006 TOUCH FOR HEALTH Annual Meeting Reporlectavares100% (2)
- Alatrol: Cetirizine Hydrochloride BPDocument1 pageAlatrol: Cetirizine Hydrochloride BPAfsana AfrinNo ratings yet
- Msds Nano PolishDocument5 pagesMsds Nano PolishGan LordNo ratings yet
- Music Therapy Improves Sleep Quality in Acute and ChronicDocument12 pagesMusic Therapy Improves Sleep Quality in Acute and ChronicLaras Ciingu SyahrezaNo ratings yet
- Cervical Cancer and Human Papillomavirus: HearingDocument596 pagesCervical Cancer and Human Papillomavirus: HearingScribd Government DocsNo ratings yet
- Template HalodocDocument104 pagesTemplate HalodocSonia WulandariNo ratings yet
- Prob PDFDocument12 pagesProb PDFwallace120No ratings yet
- CV Stoskopf 12 06Document52 pagesCV Stoskopf 12 06shinevoiceNo ratings yet
- Arq AmberDocument4 pagesArq AmberMaqsood AnsariNo ratings yet
- Bio Mechanics of The Normal andDocument5 pagesBio Mechanics of The Normal andJuanolo Oo100% (1)
- ES V 0281 001 FinalSPCDocument4 pagesES V 0281 001 FinalSPCPankaj BeniwalNo ratings yet