Professional Documents
Culture Documents
Retinoscopie 1 PDF
Uploaded by
Diana LupoiuOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Retinoscopie 1 PDF
Uploaded by
Diana LupoiuCopyright:
Available Formats
Volume 1, Chapter 37.
Retinoscopy
Page 1 of 33
Chapter 37
Retinoscopy
JONATHAN D. WIRTSCHAFTER and GARY S. SCHWARTZ
Main Menu Table Of Contents
Search
HISTORY OF THE RETINOSCOPE
OPTICS OF THE RETINOSCOPE
OPHTHALMOSCOPIC RETINOSCOPY
NEUTRALIZATION RETINOSCOPY
TECHNIQUES TO EVALUATE ASTIGMATISM
RELIABILITY
REFERENCES
Retinoscopy is the most practical, manual method of objective refraction.
1
Classic textbooks of ophthalmology and visual optics
2,3
have stressed
4,5
that the practice of retinoscopy follows easily from an understanding of
the optics of the retinoscope, whereas monographs on practical
retinoscopy concentrate on the technique in simplified ways that may
offend the textbook authors but still represent a level of sophistication
beyond the observed behavior of most practitioners. Most practitioners
relegate retinoscopy to others, and if asked about it, would merely
restate what they remember about neutralization: With reflex, add plus;
against reflex, add minus. The goal of this chapter is to increase the
usefulness of the retinoscope to the practitioner by encouraging the use
of ophthalmoscopic retinoscopy while reviewing the basis for the more
commonly used neutralization retinoscopy.
The goal of objective refraction is to locate the far point of the spherical
eye or the two far-point planes of an astigmatic one. Although the
retinoscope offers more than two techniques with which to locate the far
point, the most important are ophthalmoscopic retinoscopy and
neutralization retinoscopy. Ophthalmoscopic retinoscopy locates the far
point in space by varying the illumination system and observing the
image of the retinoscope filament on the retina. Neutralization
retinoscopy is a technique that brings the patient's far point to a location
that is a predetermined distance from the patient, the working distance,
usually 66 cm (1.50 diopters [D]) in front of the eye, through the use of
lenses. Neutralization retinoscopy has a well-defined and rather accurate
end point, and, in contrast to ophthalmoscopic retinoscopy, varies the
observation system to observe the image from the illuminated retina.
Although ophthalmoscopic retinoscopy is faster than neutralization
retinoscopy, use of the two techniques in conjunction often requires less
time than neutralization alone, especially in difficult cases. There is
simply no reason to spend more than 5 minutes neutralizing an eye when
ophthalmoscopic retinoscopy can quickly reveal the source of the
difficulty.
Ophthalmoscopic retinoscopy is often referred to as estimation, and, in
fact, works well to estimate a patient's refractive error. However, certain
modifications of the neutralization retinoscopy technique can also enable
the retinoscopist to estimate the patient's refractive error. These
techniques depend primarily on magnification and enhancement of the
observed image, and to a lesser extent on observation of the with and
against or scissors reflexes. Our hope is that in studying this chapter,
the reader will enhance his or her skills in using the retinoscope, thus
increasing both speed and accuracy.
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 2 of 33
We would like this chapter to be read at two levels. First, we hope it will
be useful for the clinician merely hoping to improve his or her clinical
skills in using the retinoscope, and in this regard, this chapter should
serve as a how-to guide. Second, we would like this text to serve as an
initial reference for those wishing to understand the optics and
retinoscope in greater detail. In this respect, we have provided
information on topics that go beyond the minimum information required
for performing ophthalmoscopic and neutralization retinoscopy.
Back to Top
HISTORY OF THE RETINOSCOPE
The observations that led to clinical retinoscopy were made in 1859 with
a plane mirror ophthalmoscope lighted by a candle, when Sir William
Bowman noted a linear shadow seen when examining an astigmatic eye.
By 1875, the optics were explained and the procedure was described as a
shadow test, an allusion to neutralization. H. Parent coined the term
retinoscopy in 1881, but the term is somewhat of a misnomer because
the technique actually provides an ophthalmoscopic view of the light
reflected from a patch of retina. The earliest retinoscopes used a mirror
to reflect a candle, which produced a spot of light. It was soon
discovered that a linear streak of light could be produced with slit-shaped
mirrors. Early electric retinoscopes used spiral filament bulbs and a
rotating slit. Jacob Copeland introduced a linear filament bulb that
4,68
produced a sharp, bright line of light.
The Copeland streak
retinoscope set the standard for future retinoscopic developments.9,10 As
with any instrument, many advances have been incorporated over the
years, and innovations continue to this day, incrementally improving the
viewing system, control of vergence and filament meridians, handle and
sleeve design, and battery power.
Back to Top
OPTICS OF THE RETINOSCOPE
The streak retinoscope has supplanted the spot retinoscope in the
modern eye clinic, and only the streak retinoscope is discussed in this
chapter. Although the various brands of streak retinoscopes differ in
design, they all work similarly. Light is produced by a luminous filament
within the base of the handle and emanates from a mirror in the head as
a linear streak, with both orientation and vergence controlled by the
retinoscopist. The streak of light passes through the patient's tear film,
cornea, anterior chamber, lens, vitreous chamber, and retina. It is then
reflected from the choroid and retinal pigment epithelium as a linear red
reflex that passes back through the sensory retina, vitreous, lens,
aqueous, cornea, and tear film, through the air between the patient and
the examiner, and into the head of the retinoscope, through an aperture
in the mirror, finally exiting through the back of the retinoscope into the
retinoscopist's own eye. By observing qualities of the reflected light (the
reflex) after it leaves the patient's eye, the retinoscopist can make
determinations about the patient's refractive state.
Explaining the optics and proper usage of the retinoscope can be a
confusing business. To help simplify the text, we have chosen to use the
feminine pronouns (e.g., she and her) when referring to the
retinoscopist, and the masculine ones (e.g., he, him, and his) when
referring to the patient.
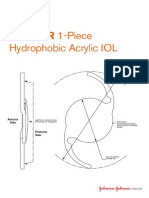
All streak retinoscopes are made of the same fundamental components:
light source, condensing lens, mirror, and sleeve (Fig. 1). The light
source is a light bulb with a fine, linear filament, which projects a fine,
linear streak of light with the passage of an electric current. The filament
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 3 of 33
(which should be considered a linear point source of light), and therefore
the streak, can be rotated 360 degrees by rotating the sleeve of the
retinoscope. Currently, most retinoscopes use a halogen bulb, which
projects a very bright streak. The condensing lens is a plus lens, which
exerts positive vergence on the streak, which is emitted from the pointsource filament in a highly diverging manner. The position of the lens in
relation to the light filament can be altered by raising or lowering the
sleeve. In this way, the vergence of the streak that is emitted from the
retinoscope can be controlled by the retinoscopist, as described
subsequently.
Fig. 1. Diagrammatic cross-section of streak
retinoscope. Light from the filament passes
through the lens to the mirror, where it is
reflected toward the patient. The examiner
views through the aperture behind the mirror.
The arrows represent the two controllable
functions. The curved arrow indicates that the
bulb may be rotated. The straight arrow
indicates that the vergence of the light rays
may be altered by changing the filament to lens
distance. The filament is shown at the focal
length of the lens so that parallel light rays emerge. (Weinstock SM,
Wirtschafter JD: A Decision-Oriented Manual of Retinoscopy. Springfield,
IL: Charles C Thomas, 1976.)
The mirror bends light that originates in the handle and is initially
projected upward toward the ceiling, to instead exit the retinoscope
along an axis parallel to the floor so that it can be projected into the
patient's eye. The mirror should not reflect 100% of visible light; rather,
it must allow some light to pass through it. Only in this way can the
retinoscopist have a view into the patient's pupil that is coaxial to the
path of the streak.
OPTICS OF THE PEEPHOLE
The true peephole of the retinoscope is not the hole on the examiner's
side of the instrument; rather, it is a hole in the reflecting mirror. The
peephole may be manufactured in two basic ways. One is to leave a
round area of the mirror unsilvered, whereas the other is to partially
silver the mirror so that it acts as a beam splitter. The size of the hole is
also a consideration in the design of the instrument. A large hole
decreases the useful light reflected into the subject's eye. At the expense
of internal reflections, the beam-splitter helps provide light needed by
the retinoscopist to find the subject's pupil and to maintain a coaxial
position. To decrease glare and polarization, some retinoscopes introduce
filters between the true peephole and the back of the retinoscope
peephole.
The peephole allows the retinoscopist's view into the patient's eye to be
coaxial to light emitted from the retinoscope. If this coaxial relationship
between the path of the retinoscopist's line of sight and the emitted
streak is not established, or she will not see a red-reflex image of the
streak. Instead, only the patient's black pupil will be seen, and the
retinoscopist cannot obtain any information regarding the patient's
refractive status. Tilting the retinoscope allows some areas of the retinal
reflex to be seen through the peephole while other portions are cut off
and are perceived as a dark shadow in the subject's pupil.
CONTROLLING THE PROPERTIES OF THE RETINOSCOPE
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 4 of 33
The basic idea behind the retinoscope is that the retinoscopist creates a
streak of light, projects it into a patient's eye, bounces it off his retina,
and makes deductions concerning the patient's refractive status based on
what the image of that streak looks like when it reaches the
retinoscopist's eye. To aid her in this task, the retinoscopist has control
over, and can easily vary, certain aspects of the system. Two things she
can control have nothing to do with the intrinsic properties of the
retinoscope she is holdingthe distance between the retinoscopist's eye
and the patient's, and which lenses she may be holding between the
patient's eye and her own; thus, these are not discussed in this section.
However, two properties over which the retinoscopist has total control
are completely intrinsic to the retinoscope she is holding. The first is the
orientation of the streak as it leaves the retinoscope. Because the light
source for the retinoscope is a fine filament, the light emanates from the
retinoscope as a fine streak. By rotating the light source, the
retinoscopist can easily alter the orientation of the streak by more than
360 degrees. Merely by rotating the sleeve on the handle of the
retinoscope, she can project a streak whose orientation is parallel to the
floor, or perpendicular to it, or any meridian in between. This feature of
the retinoscope proves invaluable when examining patients with
astigmatism.
The second property that can be controlled easily by the retinoscopist is
the vergence of the incident streak. With the touch of a finger (or
thumb), the retinoscopist can alter the streak so that it leaves the
retinoscope as converging, diverging, or even parallel light. This feature
gives the retinoscopist an incredible amount of power in evaluating a
patient's refractive state. Unfortunately, it is probably the most
underused feature of the retinoscope. The average retinoscopist uses
only diverging light (plane mirror) when performing an objective
refraction, and therefore limits what she can truly accomplish with the
apparatus.
Changing the distance between the light filament and the condensing
lens alters the vergence of the emitted streak. This can be accomplished
by raising or lowering the sleeve in the handle of the retinoscope. This is
the most fundamental way in which different models of retinoscope will
contrast, and it is obviously important for the retinoscopist to be familiar
with the type of retinoscope with which she is working. In the earliest
models of retinoscopes (e.g., Bausch and Lomb Copeland [1928] and
Copeland-Optec 360 [1958]), the condensing lens is fixed, and the light
source can be raised or lowered by moving the sleeve up or down (Fig.
2). When the sleeve is raised in these retinoscopes, the streak emanates
as a diverging beam; when the sleeve is lowered, the streak emanates in
a converging nature. Most current textbooks on retinoscopy techniques
4,5
use this type of retinoscope in their discussions and therefore use the
term sleeve up when the retinoscope emits diverging light and sleeve
down when it emits converging light.
Fig. 2. Optical effects of moving the
retinoscope bulb to change the
filament to lens distance; this type
of retinoscope emits convergent
light when the sleeve is moved up.
Note the vergences of the emerging
rays: (left) concave mirror effect is
produced when bulb is moved
down; (right) plane mirror effect is
produced when bulb is moved up. (Weinstock SM, Wirtschafter JD: A
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 5 of 33
Decision-Oriented Manual of Retinoscopy. Springfield, IL: Charles C
Thomas, 1976.)
In the U.S. market, retinoscopes that emit a converging beam with the
sleeve down have largely been supplanted with retinoscopes in which the
light source is fixed and the condensing lens can be raised or lowered by
moving the sleeve up or down (Fig. 3). Examples of this type of
retinoscope include those made by Welch Allyn, Heine, Neitz, and Keeler.
In these retinoscopes, when the sleeve is raised, the streak emanates as
a converging beam, and when the sleeve is lowered, the streak emanates
as a diverging beam. These retinoscopes have a more complex linkage
than the retinoscope described previously because the sleeve has two
different control functions: to raise or lower the lens and to rotate the
bulb filament.
Fig. 3. Optical effects of moving the
lens to change the filament to lens
distance; this type of retinoscope
emits convergent light when the
sleeve is moved up. Note the
vergences of the emerging rays:
(left) plane mirror effect when lens
is moved down; (right) concave
mirror effect when lens is moved
up. (Weinstock SM, Wirtschafter JD: A Decision-Oriented Manual of
Retinoscopy. Springfield, IL: Charles C Thomas, 1976.)
The Copeland streak retinoscope traditionally has been the standard
against which others have been compared. However, our informal survey
of optical instrument distribution reveals that retinoscopes that converge
with the sleeve down are being used in fewer and fewer ophthalmology
offices because more clinicians prefer the Welch Allyn, Heine, Neitz, or
Keeler models. The reasons for this are a mix of technical (i.e.,
compatibility of instrument design with rechargeable battery handles)
and marketing aspects. Regardless, the market currently is dominated by
retinoscopes that converge when the sleeve is up. Therefore, this chapter
takes a departure from prior retinoscopy textbooks and use the
nomenclature sleeve down to mean that the streak is emitted as
diverging light and sleeve up to mean that the streak is emitted as
converging light. The reader must be familiar with her own retinoscope.
When using a Bausch and Lomb Copeland, Copeland-Optec 360, or other
type with a movable light source and fixed condensing lens, she must be
aware that the sleeve position should be in the down position when we
use the term sleeve up and should be in the up position when we use the
term sleeve down.
By altering the vergence of the emitted streak, the retinoscopist is
actually manipulating its focal point, the point where the emitted light
comes to focus in a point in real or virtual space. When in maximum
convergence (sleeve up), that focal point is a real image located 33 cm in
front of the retinoscope. (You can test this by moving the palm of your
hand in front of the retinoscope at a distance of 33 cm, then turning it on
with the sleeve raised all the way up. You should see the image of the
filament in perfect focus on the palm of your hand.) As the sleeve is
lowered, the focal point moves farther from the retinoscope (aim the
retinoscope at a wall and recede) until a point where the sleeve is
roughly two thirds of the way down, when the streak is emitted as
parallel light and the focal point is at infinity. If the retinoscopist
continues to lower the sleeve of the retinoscope, the focal point is
created in virtual space far behind her. As she lowers the sleeve more,
the focal point moves closer to her until the sleeve is lowered all the way,
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 6 of 33
and the focal point is 40 cm behind her. At no time can the focal point of
the streak emanating from the retinoscope be located between 33 cm in
front of and 40 cm behind the retinoscope. In other words, the
retinoscope cannot project the streak to the region in space that the
retinoscope itself occupies. Thus, the retinoscopist must know the
location of the converging and diverging focal points of her retinoscope to
use it to its full potential.
DETERMINING THE VERGENCE OF THE RETINOSCOPE BEAM
To determine the vergence of a retinoscope at any sleeve adjustment, a
simple trick called Foucault's Method (Fig. 4) can be used. The most
instructive part of this exercise is shown in Figure 4A. Note that when a
card is introduced at the edge of a converging beam, an opposite
movement is produced on a screen located beyond the focal point.
Fig. 4. Foucault's method for determining vergence of
rays emerging from a retinoscope. A card or your hand
is introduced close to the retinoscope and moved at
right angles to the emerging rays. Observe the shadow
produced in the unfocused image on a screen or wall in
a darkened room. A. Rays converging at a focal point
before screen cause an against motion. B. Rays
converging beyond screen cause a with motion. C.
Diverging rays cause a with motion. (Weinstock SM,
Wirtschafter JD: A Decision-Oriented Manual of
Retinoscopy. Springfield, IL: Charles C Thomas, 1976.)
CALIBRATING THE RETINOSCOPE SLEEVE
Perform calibration in a semidarkened examining room with a 20-foot
distance from the phoropter to the distant wall. Turn on the retinoscope.
Calibration of the Converging Beam
Bring the sleeve all the way up and place it against a reflecting surface
such as the wall. Move away from the wall and observe from the side
(not through the peephole) until the streak is in sharp focus on the wall.
You should note that when the retinoscope is moved beyond that
distance, the streak will go out of focus because the filament light has
converged and then diverged (see Fig. 4A). Return to the point of sharp
focus and measure to determine the focal point of the retinoscope: it
should be about 33 cm, which corresponds to + 3.00 D.
Calibration of the Parallel Beam
Sit in the patient's examination chair and aim the retinoscope toward the
distant wall while moving the sleeve up and down. Watch where the
finest focused image of the filament is observed. Note the relative
position of the bottom of the sleeve with regard to the range of sleeve
movement. In that position, the retinoscope beam is as parallel as
possible and it has no vergence and thus is focused at infinity. The Heine
retinoscope has a mechanical stop (Para Stop) at the parallel beam
position that can be engaged to prevent the vergence control from being
adjusted to a convergent beam. This position can be used as the plano
calibration.
Calibration of the Diverging Beam
Sit in the patient's examination chair and place the retinoscope
immediately adjacent to the patient's side of the phoropter. Aim the
retinoscope through the phoropter eyehole and onto the distant wall. Do
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 7 of 33
not look through the retinoscope or the phoropter. Move the sleeve all
the way down and select the trial lens that allows for the sharpest focus.
The divergent beam of the retinoscope will be brought to convergence at
infinity when you neutralize it with some lens between + 1.50 to + 2.25
D. Different models of retinoscope vary as to where in space light can be
focused behind them. For example, the Heine retinoscope focuses light to
44 cm behind it (-2.25 D), the Welch Allyn focuses light 50 cm behind it
(-2.00 D), and the Copeland-Optek cannot focus light to any closer than
66 cm behind it (-1.50 D).
Although the retinoscopist should be aware of the convergence and
divergence focal points of the retinoscope that she uses, in truth, very
few retinoscopists actually go through the small amount of trouble to
measure them.
You have now calibrated the sleeve of your retinoscope and determined
that it has an ophthalmoscopic retinoscopy focusing range of 4.00 D of
hyperopia to 2.25 D (or 2.00 D or 1.50 D, depending on the model) of
myopia. You can record these measurements on a label affixed to the
side of the retinoscope (Fig. 5) or simply remember them because you
are using the scale only for the estimate. The most useful aspect of the
label is the position of plano.
Fig. 5. Ophthalmoscopic retinoscopy
scale applied to the sleeve case of a
Heine retinoscope. The scale
corresponds to the approximate
focus of the instrument when used
at 5 cm from the subject's eye. The
reading is taken from the bottom of
the sleeve. In this figure, the sleeve
is adjusted for the plano.
(Reproduced with permission fo the
Regents of the University of
Minnesota. Copyright 2000.)
Back to Top
OPHTHALMOSCOPIC RETINOSCOPY
Copeland taught methods for refracting an individual with a retinoscope
that relied on neither lenses nor verbal responses from the patient. His
technique relied on the recognition of a focused ophthalmoscopic image
of the retinoscope. Although Dr Copeland's skills at ophthalmoscopic
retinoscopy were such that he could write a spectacle prescription based
on information garnered from this technique alone, most of us use it only
as a technique of estimating the refractive error, and few of us feel
comfortable enough with our skills to rely solely on this method.
However, ophthalmoscopic retinoscopy is a valuable technique to use as
a prelude to neutralization, especially in a patient with an unknown
refraction. It is quick, easy, and accurate. It was especially useful when
practitioners refracted with loose lenses, where they could benefit from
any technique that would decrease the number of trips they had to
make to the trial lens case. However, now that most ophthalmic
examination rooms are equipped with phoropters rather than trial lenses,
estimation techniques tend to be underused, and most retinoscopists skip
ophthalmoscopic retinoscopy altogether, and merely dive headlong into
neutralization. We have chosen to replace terms such as estimation
techniques with ophthalmoscopic retinoscopy to indicate a coherent
optical basis rather than describe a collection of estimating tricks.
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 8 of 33
Ophthalmoscopic retinoscopy is quite helpful for the cycloplegic refraction
of uncooperative infants and children, for patients being examined under
anesthesia, or in any circumstance when the first attempt at
neutralization does not yield a useful reflex. Most retinoscopists who only
use the retinoscope for neutralization retinoscopy may be unfamiliar with
the technique of estimation by ophthalmoscopic retinoscopy (Table 1).
TABLE 1. Differences Between Ophthalmoscopic Retinoscopy and
Neutralization Retinoscopy
Ophthalmoscopic
Retinoscopy
Neutralization
Retinoscopy
Refractive
status before
examination
Completely unknown and
uncorrected
Known and almost
perfectly corrected
Refractive
conditions
analyzed
Highly difficult, high
Simple ametropia or
ametropia and astigmatism emmetropia
Refractive
purpose
Estimation
Completion*
Time required
per eye
< 1 min
15 min
Far point
Locates
Confirms desired location
Working range
Sleeve height
Use of trial or phoropter
lenses
End point
566 cm
Spirals from down to up
Never, initially
Sharply focused,
nonmoving image
66 cm
Sleeve always
down
Almost always
Blurred, fast-moving
image; on-off
phenomenon
Optical principle Varying the illuminating
Varying the observation
system vergence to observe system to observe the
image on retina
image from the retina
*Can also be used for estimation of eyes whose net refractive errors are
between 1.50 to 3.00.
For retinoscopes whose beam diverges with sleeve down.
The reader must understand four specific differences between the
performance of ophthalmoscopic retinoscopy and neutralization
retinoscopy. First, during ophthalmoscopic retinoscopy, the working
distance starts at 5 cm from the patient and ends at 66 cm, whereas the
working distance remains at 66 cm for neutralization retinoscopy (Fig. 6).
Second, the sleeve is spiraled up during ophthalmoscopic
retinoscopyit is rotated while it is raised from the sleeve down to the
sleeve up position, whereas for neutralization retinoscopy, it is left in the
sleeve down position and swept from side to side across the pupil. Third,
no lenses are used during initial ophthalmoscopic retinoscopy, but they
are almost always used during neutralization retinoscopy. Fourth, the
end point for ophthalmoscopic retinoscopy is a clear, sharp
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 9 of 33
ophthalmoscopic image of the retinoscope streak, whereas for
neutralization retinoscopy the end point is the neutralization reflex where
the pupil immediately fills with an unfocused image of the streak.
Fig. 6. A. Movement pattern
diagram for ophthalmoscopic
retinoscopy when rays converge
with vergence control up. The
approximate net power scale has
been calibrated using several streak
retinoscopes manufactured by
Heine. B. Movement pattern
diagram for ophthalmoscopic
retinoscopy when rays converge
with vergence control down. The
approximate net power scale has
been calibrated using several
Copeland streak retinoscopes.
The basic idea behind ophthalmoscopic retinoscopy is that the
retinoscopist can determine when the focal point of the retinoscope falls
on the focal point of the patient's eye. When this occurs, the
retinoscopist can see the image of the retinoscope streak as a sharply
focused line in the patient's pupil. By altering both the distance of the
retinoscope to the patient's eye and position of the focal point of the
emitted streak from the retinoscope head (which is another way of
saying the vergence of the emitted streak), the retinoscopist can
superimpose the focal point of the retinoscope onto the focal point of the
patient.
OPHTHALMOSCOPIC RETINOSCOPY OF SPHERICAL EYES
When performing ophthalmoscopic retinoscopy, the retinoscopist begins
with the retinoscope 5 cm (about 2 inches) away from the patient's eye
with the sleeve all the way down (Fig. 7). The streak exits the
retinoscope head as diverging light that comes to focus at a distance 40
cm behind it (behind the retinoscopist's head) in virtual space. If the
patient is a -2.25 D myope, the focal point of the retinoscope lies in the
same point in space as the focal point of the patient, and the
retinoscopist sees a finely focused streak of light in the patient's pupil. It
does not matter that the focal point of the retinoscope is in virtual space;
it only matters that the focal point of the retinoscope is coincident with
the focal point of the patient. At this point, the patient's and
retinoscope's focal points are conjugate. The retinoscopist now rotates
the streak 360 degrees by rotating the sleeve in the retinoscope handle.
If the streak image is in focus in all meridians, the patient has no
astigmatism, and ophthalmoscopic retinoscopy is complete at this stage.
However, if the streak is in sharp focus in one orientation, but out of
focus in another, the patient has astigmatism. Estimation of the
refractive errors of astigmatic individuals is discussed toward the end of
this section. For now, let us concentrate on eyes with spherical refractive
errors.
Fig. 7. At the very bottom of sleeve
adjustment, a bright, thin, focused
image will emerge on the retina if
the far point of the eye is 40 cm in
front of cornea or about 35 cm
behind the retinoscope. Raising the
sleeve from the bottom moves the
virtual focus of the retinoscope
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 10 of 33
closer to the horizon, allowing the
detection of lesser amounts of myopia until the middle the retinoscope,
where plano is detected. The distance that the sleeve is adjusted is a
measure of the refractive distance between plano and -2.25 D.
Emmetropia and Mild Ametropia
If the patient's refractive error is anything other than -2.50 D, the image
of the streak in his pupil as seen by the retinoscopist will be out of
focusthe farther the patient is from -2.50 D, the more out of focus the
image will be. At this point, the retinoscopist slowly raises the
retinoscope sleeve while rotating the streak 360 degrees (a technique
known as spiraling). She keeps the retinoscope head 5 cm from the
patient's eye throughout this step. As the sleeve is raised the first one
third of its range, the focal point of the retinoscope moves farther and
farther from the back of the retinoscopist's head until it lies on the
horizon when the sleeve is approaching one third of the way up. If the
image of the streak is in focus at this point, the patient's focal point must
lie at infinity, and he must therefore be emmetropic (Fig. 8). All patients
with refractive errors between emmetropia and 2.25 D of myopia should
be discovered up to this point with the sleeve between all the way down
and one third of the way up, with the retinoscope positioned 5 cm from
the patient.
Fig. 8. Locating the far point of a plano eye
in ophthalmoscopic retinoscopy when the
retinoscope is 5 cm from the subject's eye.
Move the sleeve toward the middle position
corresponding to the approximate or
calibrated position so that the retinoscopic
rays emerge in a parallel bundle and create
a bright, thin, focused image on the retina. This position can be used to
confirm emmetropia after refractive correction or to confirm the
absence of a significant refractive error in an uncooperative subject. The
far point found corresponds to infinity. In practice, this step is combined
with the steps for estimating any refractive error between -2.25 and +
4.00 D.
The retinoscopist can easily learn to calibrate the sleeve position for the
vergence and refraction at the 5-cm distance and depend on
proprioception and a memorized calibration scale for this information.
The mechanics of most retinoscopes make it difficult to permanently
display this information on the handle. Fortunately, it is possible to place
a written calibration on the handle of the Heine ophthalmoscope so that
the 5-cm ophthalmic retinoscopy can be read with precision (see Fig. 5).
The text in the preceding section explains how to calibrate any
retinoscope, and the exercise can help you understand the optics.
If the retinoscopist gets much above the midsleeve position with the
streak not yet coming into focus, she continues to spiral the sleeve up.
She is now in the area where the image of the streak of patients with low
hyperopic refractive errors will appear in focus. This occurs because the
streak is emitted in a converging nature when the sleeve is raised above
the one-third mark. The focal point of the streak is now located in space
behind the patient's head. When the sleeve is just barely above one third
of the way up, the focal point of the streak is far behind the patient's
head, near the horizon, and will be conjugate with the patient's focal
point only if he is a weak hyperope (Fig. 9). As the sleeve is raised
farther, the focal point of the retinoscope moves closer to the back of the
patient's head. When the sleeve is raised all the way up, the focal point
of the retinoscope lies 33 cm in front of itroughly 25 cm behind the
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 11 of 33
patient's cornea. The focal point of the retinoscope will be conjugate with
the focal point of the patient if he is a + 4 hyperope. All hyperopes with
refractive errors lower than + 4 should be discovered in this way with the
sleeve between one third and all the way up and the retinoscope
positioned 5 cm from the patient. Thus, the retinoscopist can estimate or
confirm the refraction of all patients between -2.25 and + 4 by merely
spiraling the sleeve upward while holding the retinoscope 5 cm from the
patient's eye (Fig. 10).
Fig. 9. Locating the far point of a +
4.00-D eye in ophthalmoscopic
retinoscopy when the retinoscope is
5 cm from the subject's eye. Start
with the sleeve all the way down
and move slowly toward the top. At
or within 1 mm or so of the top, a
bright, thin, focused image will
emerge on the retina if the far point
of the eye is 40 cm behind the cornea. Lowering the sleeve permits you
to detect lesser amounts of hyperopia by moving the virtual focus of the
retinoscope from about 25 cm behind the eye further toward the
horizon, allowing the detection of lesser amounts of hyperopia until
midsleeve, where the retinoscope detects plano. The distance that the
sleeve is lowered is a measure of the refractive distance between +
4.00 D and plano.
Fig. 10. Ophthalmoscopic
retinoscopy: summary of
techniques for locating the far
points of eyes with refractive errors
between -2.25 and + 4.00 D when
the retinoscope is 5 cm from the
subject's eye.
HIGH HYPEROPIA AND HIGH MYOPIA
If the retinoscopist began with the sleeve dropped all the way down and
has raised it all the way up, and still has not seen a clear, sharp image of
the retinoscopy streak in the patient's pupil, she now starts to slowly
move the retinoscope away from the patient. The purpose of this step is
to estimate eyes whose far points are less than 25 cm behind the cornea
(higher hyperopes) or less than 66 cm in front of the cornea (higher
myopes) (Fig. 11). She leaves the retinoscope sleeve all the way up for
this maneuver but continues to rotate the streak 360 degrees.
Remember, with the retinoscope sleeve all the way up and the
retinoscope located 5 cm in front of the patient, the focal point of the
retinoscope is located 25 cm behind the patient's eye. As the
retinoscopist slowly moves away from the patient, the focal point of the
retinoscope moves closer and closer to the patient's eye from behind. It
is in this range that the focal points of higher hyperopes become
conjugate with the focal point of the retinoscope. For example, a 10.00-D
hyperope will have a far point 10 cm behind the patient's eye; to be in
conjugate focus at this point, the retinoscope is located 33 - 10 = 23 cm
in front of the patient's cornea.
Fig. 11. Locating the far point of a
-4.00-D eye using ophthalmoscopic
retinoscopy. The vergence control is
adjusted (all the way up) for the
maximum concave mirror effect,
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 12 of 33
causing the retinoscope filament
image to form about 33 cm in front
of the handle. The retinoscope is
placed so that the examiner sees in the patient's pupil a bright, sharply
focused retinal image through the aperture. This occurs when the far
point of the eye is at the same point as the image of the retinoscope.
The eye shown is 4.00 D myopic and has its far point 25 cm anterior to
the cornea. The far point of the eye is conjugate with the retina.
(Weinstock SM, Wirtschafter JD: A Decision-Oriented Manual of
Retinoscopy. Springfield, IL: Charles C Thomas, 1976.)
When the retinoscope is exactly 33 cm away from the patient's eye and
the sleeve is all the way up, the streak image will be in focus on the
patient's iris and eyelids. We call this point the intercept point, and it
serves as an important landmark. If the image of the streak is in sharp
focus just inside of this landmark, the patient's focal point must lie just
behind the retina, and he must be a high hyperope (Fig. 12). In contrast,
if the image of the streak is in sharp focus just outside of the intercept
point, the patient's focal point must lie just in front of the retina, and he
must be a high myope. Thus, a mere 10 cm (5 cm on either side of the
intercept) separates where the focal points can be found for a -20.00-D
myope and a + 20.00-D hyperope (Fig. 13). Fortunately, the intercept
point is a clear landmark to keep the retinoscopist from losing her way.
Importantly, no patient can have a refractive error such that the streak
image is in focus at the intercept point.
Fig. 12. Locating the far points of
eyes between + 4.00 D and higher
using ophthalmoscopic retinoscopy.
A. The retinoscopist begins at + 4.00
D, with the sleeve all of the way up
and positioned 5 cm from the
subject's eye. If a sharply focused
filament image on the retina is not
seen, the retinoscopist then recedes
until it is seen or until the retinoscope filament is in sharp focus on the
cornea and eyelids. This point is called the intercept. B. If at any point
the retina is in sharp focus, the far point has been located; this point is
behind the cornea and approximately 33 cm in front of the retinoscope,
where the rays converge in virtual space. To determine the approximate
amount of hyperopia, one can estimate the distance from the cornea or
from the intercept (whichever is easier). The intercept occurs at 33 cm
from the cornea. The reciprocal of the distance in meters gives the
power in diopters. For example, if the retinal image is in sharp focus at
28 cm from the eye and 5 cm toward the eye from the intercept, the
reciprocal of 0.05 is + 20.0 D.
Fig. 13. Locating the far points
of eyes between high myopia
and -3.00 D using
ophthalmoscopic retinoscopy.
The retinoscopist begins with
the sleeve all of the way up
and positioned at the intercept
33 cm from the subject's eye.
In practice, this step is done
as a continuation of seeking high hyperopia, as described in Fig. 12. At
the intercept, the retinoscope filament is in sharp focus on the cornea
and eyelids. If a sharply focused filament image on the retina is not
seen, the retinoscopist then recedes until it is seen or until the
retinoscopist has receded to the working distance of 66 cm. If at any
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 13 of 33
point the retina is in sharp focus, the far point has been located; this
point is in front of the cornea and approximately 33 cm in front of the
retinoscope, where the rays converge in real space. To determine the
approximate amount of myopia one, can estimate the distance from the
cornea or from the intercept (whichever is easier). The intercept occurs
at 33 cm from the cornea. The reciprocal of the distance in meters gives
the power in diopters. A. For example, if the retinal image is in sharp
focus with the retinoscope at 33 cm from the eye and 5 cm further from
the eye than the intercept, the reciprocal of 0.05 is -20.00 D. B. Similar
example for -3.00 D. The retinoscope is located at 66 cm.
A sometimes useful and interesting phenomenon occurs when the
converged beam is focused close to the plane of the cornea and lens of
the subject's eye; it is a diffuse red reflex that may retroilluminate
anterior segment opacification. The red reflex when the intercept is
focused on lens of the eye is called the incidence neutral point in
retinoscopy.
11
If the retinoscopist has gone this far in the process of ophthalmoscopic
retinoscopy and the image of the retinoscope streak has not yet come
into focus, she merely continues to move farther from the patient. In this
way, she moves the focal point of the retinoscope through the range
where the focal points of the high and mid-range myopes lie. Eventually,
she will pull the retinoscope back to the point where it is 66 cm away
from the patient's eye. Here, with the retinoscope sleeve all the way up,
the focal point of the retinoscope lies 33 cm in front of it and 33 cm in
front of the patient. Therefore, at arm's length, the focal point of the
retinoscope is conjugate with the focal point of the patient if he is a -3
myope.
Through ophthalmoscopic retinoscopy, all ranges of myopia and
hyperopia can be deduced unless the patient's refractive error lies
between -2.25 and -3.00 D. The focal points of these moderately myopic
patients fall outside of the range accessible to the streak retinoscope
using ophthalmoscopic retinoscopy without a trial lens.
Ophthalmoscopic Retinoscopy of Highly Ametropic Eyes
Ophthalmoscopic retinoscopy reveals a focused streak image very near
the intercept point in all high myopes and high hyperopes. The conjugate
point for high hyperopes lies just inside of the intercept point and for
high myopes lies just beyond it. Certain techniques exist to help finetune the end point.
When the ophthalmoscopic retinoscopy end point lies near the intercept
point, the retinoscopist can return the retinoscope to the point in space
where the intercept point is seen. She can then keep her free hand at
this point in space and move the retinoscope in (for hyperopes) or out
(for myopes) until the end point is seen. She then merely needs to
measure the distance between the retinoscope and her free hand and
convert that distance to diopters. If she had to move the retinoscope
forward 10 cm, she knows that the patient is a + 10.00-D hyperope; if
she had to move the retinoscope backward 5 cm, she knows that the
patient is a -20.00-D myope.
Although ophthalmoscopic retinoscopy is typically performed without
lenses, loose lenses can also be used to help refine the estimated end
point of a patient with a high degree of ametropia. For example, take the
situation where the image of the streak is in sharp focus when the
retinoscope is held 36 cm away from the patient's eye. This is the range
at which focal points can be found for high myopes; however, the
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 14 of 33
distance separating the focal points for all those between -8 and -20.00
D is fairly small. In fact, focal points for this range of myopia span an
area only 7.5 cm wide. In this situation, it is helpful to put up a -10.00-D
lens and repeat all the steps of ophthalmoscopic retinoscopy. Now,
suddenly, the -8.00-D patient will behave much differently than a
-14.00-D patient: the -8.00-D patient will appear like a + 2.00-D
hyperope, and the -14.00-D patient will appear like a -4.00-D myope. In
this way, a much truer estimation of the patient's refractive error can be
made. This same technique, of course, works equally well for high
hyperopes and aphakic individuals. The only difference is that the
retinoscopist holds a + 10.00-D lens rather than a -10.00-D lens.
OPHTHALMOSCOPIC RETINOSCOPY OF ASTIGMATIC EYES
Detection
The previous discussion describes the technique for ophthalmoscopic
retinoscopy of patients with spherical refractive errors. When estimating
astigmatic individuals, an extra step must be taken. Unlike someone with
a spherical refractive error who focuses light to a point a single discreet
distance from his pupil, a patient with regular astigmatism focuses light
to two points (actually lines), located two discreet distances from his
pupil. Through this technique of ophthalmoscopic retinoscopy, it is easy
for the retinoscopist to find these two focal distances.
The key to discovering astigmatism by ophthalmoscopic retinoscopy is
that the retinoscopist constantly rotates the streak by rotating the sleeve
in the retinoscope handle. During the first stage of ophthalmoscopic
retinoscopy, while the sleeve is being raised, it is also being rotatedthe
two motions combined result in spiraling. During the later stages of
ophthalmoscopic retinoscopy, while the sleeve is kept in the sleeve up
position, it is rotated while the retinoscopist moves the retinoscope from
5 to 66 cm away from the patient's eye.
For a patient with astigmatism, ophthalmoscopic retinoscopy is begun
just as it is with a patient with a spherical refractive error. The
retinoscope is placed 5 cm in front of the patient's eye with the sleeve all
the way down (Fig. 14). The retinoscopist then rotates the streak without
raising the retinoscope sleeve. Any irregularity in the width of the reflex
indicates regular or irregular astigmatism. This step is referred to as Step
1 of ophthalmoscopic retinoscopy because it is such a helpful first step.
Everything else that had been discussed in the previous section is
referred to as Step 2 and is shown in a flowchart (Fig. 15). The
retinoscopist slowly spirals the sleeve up while evaluating the appearance
of the image of the streak in the patient's pupil. At some point, the image
of the streak should be in sharp focus. Without lowering or raising the
sleeve, the retinoscopist rotates it 360 degrees. If the image of the
streak stays in sharp focus, that patient does not have astigmatism; the
retinoscopist makes note of the sleeve position and distance from the
patient, and ophthalmoscopic retinoscopy is complete. If, however, the
image of the streak goes out of focus while the sleeve height is kept
constant and the streak is rotated, the retinoscopist knows that the
patient has astigmatism. She has estimated the power in one meridian
(where the streak is in focus), and now merely needs to determine the
power in the other.
Fig. 14. Detection of stigmatism,
step 1: how to check for irregular
astigmatism and myopic
astigmatism before beginning the
refraction-estimating step 2 that
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 15 of 33
constitutes the essence of
ophthalmoscopic retinoscopy.
Fig. 15. Ophthalmoscopic
retinoscopy flowchart, step 2: how
to estimate all refractive errors
except those between -2.25 and
-3.00 D using a retinoscope that
converges with vergence control
up. The purpose of this step is to
prepare for neutralization
retinoscopy. (Redrawn from
Weinstock SM, Wirtschafter JD: A Decision-Oriented Manual of
Retinoscopy. Springfield, IL: Charles C Thomas, 1976.)
Quantitative Estimation
At this point, the retinoscopist makes a note of the sleeve position and
retinoscope distance where the first meridian has been found, and
proceeds with ophthalmoscopic retinoscopy by continuing to raise the
sleeve up (if it has not already reached the top) or moving the
retinoscope farther from the patient's eye (if it has). The streak does not
need to be spiraled or rotated at this point because the retinoscopist
knows the axis of the second meridianit must lie 90 degrees from the
first one. At some point, she will come to the position where the second
focal point lies, and the image of the streak will again come into sharp
focus in the patient's pupil.
Occasionally, when performing ophthalmoscopic retinoscopy, the
retinoscopist finds the focal point for one meridian of a patient's
astigmatism, but as she continues on with ophthalmoscopic retinoscopy,
she never finds the second meridian. There are a few reasons why this
might occur. First, the patient may have irregular astigmatism so that
the focal point of a second meridian is difficult to recognize. Second, the
power of the second meridian may lie between -2.00 and -3.00 Dthe
refractive zone where ophthalmoscopic retinoscopy cannot result in a
sharp image. However, the most common reason why the retinoscopist
may find only one meridian of a patient's astigmatism is that she merely
did not recognize the first one when she came upon it. When she comes
upon the second meridian, she mistakes it for the first one, and
continues on. As she continues with ophthalmoscopic retinoscopy, of
course, no second focal point will be found. What she must do once this
error is recognized is go back to the position that she was in when she
discovered the one meridian she did find, and then proceed with
ophthalmoscopic retinoscopy backward until she comes upon the focal
point of the other one (the true first meridian).
Once the focal points are found for the two principal meridians, the
estimation of the patient's refractive state can be calculated. The second
meridian found is the axis of the plus power (assuming the two meridians
were found in the correct order, of course). For example, say we are
examining a patient and find the streak in focus in the vertical meridian
when we are 5 cm from the patient with the sleeve all the way up.
However, the streak goes out of focus when we rotate it to the horizontal
meridian. We know that the power is + 4 with axis 90 degrees. We make
a note of this and continue on. We find the image of the streak in focus
in the horizontal position when the retinoscope is located 15 cm from the
patient, and the sleeve is up. From this, we know that the power is + 6
with axis 180 degrees. We then convert to a plus cylinder formula which
is + 4 + 2 180 or to a minus cylinder formula of + 6 - 2 90 degrees.
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 16 of 33
Ophthalmoscopic retinoscopy allows the instantaneous confirmation of
prescribed spectacles as leaving the patient corrected to emmetropia.
Simply set the sleeve at plano and rotate it while at a distance of 5 cm
from the patient's eyes. If the patient is not accommodating, the
retinoscopist will see a sharply focused image in all meridians.
Back to Top
NEUTRALIZATION RETINOSCOPY
Most clinicians use the retinoscope solely to perform the technique of
neutralization. As discussed previously, it is unfortunate that the
retinoscope is not often used to its fullest potential. However, many
clinicians believe that they get enough information from this one
technique that they do not feel the need to become skilled in the others.
In truth, they cannot be faulted too harshly because neutralization alone
can provide the skilled retinoscopist with a great deal of information
about a patient's refractive status. This is particularly true because most
patients are either near plano or present themselves to the examiner
with an almost correct prescription in their present spectacles.
Neutralization is performed with the retinoscope held at a constant
predetermined distance from the patient with the sleeve all the way
down (light emitted in a diverging manner). The retinoscopist makes
decisions about the patient's refractive error based on the appearance of
the retinoscope reflex after it is reflected off the patient's fundus and
back through the pupil (Fig. 16). What the retinoscopist sees is not the
image on the retina (which is what she sees when performing
ophthalmoscopic retinoscopy), but rather the magnified image of the
retina. Therefore, discussion about neutralization retinoscopy must
begin with discussion about the retinoscopic reflex at neutralization.
Fig. 16. A method of estimating the
magnification of image of the
retina as compared with image on
the retina. Eye has 10.00 D of
myopia. Magnification = Image
of/Image on = 10/2 = 5. (Safir A:
Retinoscopy. In Tasman W, Jaeger
EA [eds]: Duane's Clinical Ophthalmology. Philadelphia: JB Lippincott,
1982.)
THE NEUTRALIZATION REFLEX
When performing neutralization retinoscopy, the retinoscopist shines
diverging light through the patient's pupil from a standard working
distance (usually 66 cm). This light is reflected off the patient's fundus,
and in this way, the fundus acts as a new point source of light. This is
called the illuminating system. The light that originates from the
luminous retina then passes through the patient's vitreous, lens, pupil,
aqueous, and cornea, until it finally exits the patient's eye on its way
back to the retinoscope. This is called the viewing system. The
retinoscopist must be able to differentiate between the illuminating and
viewing systems because different techniques of retinoscopy can depend
on varying the components of one but not the other. For example,
ophthalmoscopic retinoscopy, as described previously, allows the user to
vary different aspects of the illuminating system while keeping the
viewing system constant. Neutralization retinoscopy, conversely, varies
the viewing system while keeping the illumination system constant.
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 17 of 33
When diverging light is shone onto an emmetrope's retina, the retina
becomes luminous and acts as a point source of light. The rays of light
then escape his eye in a parallel fashion. If this concept is not intuitive,
merely follow the standard light ray diagram backward. In similar
fashion, light starting as a point on a myope's luminous retina is emitted
as converging light, where more myopic individuals emit more highly
converging light than less myopic ones. Similarly, light starting as a point
on a hyperope's luminous retina is emitted as diverging light, and
hyperopic patients emit more diverging light than less hyperopic ones.
The vergence of the rays emitted from the eye determines the qualities
of the reflex seen by the retinoscopist. A neutralization reflex occurs
under the circumstance when the far point of the eye correlates with the
location of the peephole of the retinoscope (Fig. 17).
Fig. 17. The optical basis for
neutralization retinoscopy. The
location of far points produces the
with and against motions for a
retinoscope with a divergent beam
when performing neutralization retinoscopy. With motion is seen
under all circumstances except when the far point of the eye-corrective
lens system is situated between the cornea and the peephole of the
retinoscope. The far point of the illustrated eye is at the peephole and is
thus neutralized.
If a retinoscopist were to examine an emmetropic eye at infinity, she
could make assumptions on the diverging, converging, or parallel nature
of the reflected light by sweeping the retinoscope streak back and forth
across the patient's pupil. However, it is not possible to perform
retinoscopy from an infinite distance; it is customary to adapt a working
distance of 66 cm, corresponding to + 1.50 D. By introducing + 1.5 lens
in front of the subject's eye, the far point of a plano prescription is
relocated to 66 cm (correcting the final prescription for the working
distance lens is described subsequently). In this circumstance, what the
retinoscopist is truly evaluating is whether the retinoscope lies between
the patient's eye and far point, lies at the far point, or lies beyond it. If
the patient is an emmetrope, the far point lies on the horizon, and
therefore the retinoscope always must lie between the patient's eye and
far point. If the patient is a hyperope, the far point actually lies beyond
the horizon, and the retinoscope also lies between the patient's eye and
far point. Things are more interesting, however, when evaluating myopes
in this way. Light is emitted from a myope in a converging manner so
that the far point is somewhere in real space in front of the myope's eye.
It is possible for the retinoscope to be placed between the patient and far
point, exactly on the far point, or out beyond the far point. This
relationship depends, of course, on both the location of the retinoscope,
and the level of myopia (which determines the location of the far point).
If the retinoscope is placed between the eye and far point (as it is for all
emmetropes and hyperopes, and some myopes) and turned so that the
emitted streak is swept from side to side across the patient's pupil, the
light reflex seen inside the pupil appears to sweep in the same direction
as the light emitted from the retinoscope (seen on the patient's iris, lids,
brow, and cheek). This motion is called with motion because the light
that is afferent to the retinoscope seems to move with the light that is
efferent from the retinoscope (Fig 18).
Fig. 18. With motion reflex in
hyperopia: a with motion reflex of
light comes into the shadow
projected in the optical system from
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 18 of 33
the aperture of the retinoscope or
the examiner's pupil. The rays from
the filament to the retina are not
shown. They form an unfocused
horizontal filament image on the retina that acts as a new object with
its image behind the retina. When the retinoscope is tilted slightly, the
object moves down and the image moves down and into the shadow.
This is seen as a with motion reflex. Light rays from the image move
up on the examiner's retina. (Weinstock SM, Wirtschafter JD: A
Decision-Oriented Manual of Retinoscopy. Springfield, IL: Charles C.
Thomas, 1976.)
If the retinoscope is placed beyond the patient's far point and swept from
side to side across the pupil, the light reflex seen inside the pupil appears
to sweep in the opposite direction as the streak emitted from the
retinoscope (Fig. 19). This motion is called against motion because the
light emitted from the eye appears to move against the light that is
emitted directly from the retinoscope.
Fig. 19. Origin of the against
movement. (Safir A: Retinoscopy.
In Tasman W, Jaeger EA [eds]:
Duane's Clinical Ophthalmology.
Philadelphia: JB Lippincott, 1982.)
When the retinoscope is placed exactly on the patient's far point, neither
with nor against motion is seen. At this point, all the light emitted
from the patient's eye enters the retinoscopist's eye simultaneously. At
exact neutrality, in a spherical eye with a small pupil, the retinoscopist
may see no motion at all; rather, the patient's pupil seems to suddenly
fill with light as the streak moves across it. This on-off phenomenon is
important to recognize because it serves as the end point when
performing the technique of neutralization.
In addition to its direction of movement, other qualities of the reflected
retinoscope streak can be evaluated. These qualities all give the
retinoscopist clues as to how close to the far point the retinoscope is
being held. The three most important qualities of the reflex are the speed
at which it moves, its brightness, and its width. If one thinks of the reflex
at the neutralization point as infinitely fast (so fast that it immediately
fills the pupil without apparent motion), infinitely bright, and infinitely
wide, it is easy to understand what the reflex should look like when the
retinoscope is either near to, or far from, the neutralization point (Fig.
20). When the retinoscope is held near the patient's far point, the reflex
should appear fairly fast, bright, and wide. As the retinoscope is moved
farther from the far point, the reflex appears to move slower and is
dimmer and thinner. The retinoscope can eventually be moved so far
from the patient's far point that the reflex is slow, thin, and dim enough
that it is quite difficult to recognize as a reflex at all.
Fig. 20. Neutralization retinoscopy:
diagram of changes in
characteristics of reflex as in the
zone surrounding the point of
neutrality. At neutrality, the reflex
motion may be so fast that it
cannot be detected. The end point or end zone should be approached
from the with reflex side and the judgment of neutrality made erring
toward the with reflex rather than the against reflex. *The point
within the neutralization zone where neutralization is best observed.
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 19 of 33
(After Weinstock SM, Wirtschafter JD: A Decision-Oriented Manual of
Retinoscopy. Springfield, IL: Charles C Thomas, 1976.)
Optics of the Neutralization Reflex
Five features characterize the neutralization end point, the point at which
neither a with nor against reflex can be identified. Three of these are
considered to define the end point, but two others can also be observed.
The three standard characteristics are increases in speed, brightness,
and width of the moving image. To these can be added , the on-off
phenomenon (the intermittent disappearance of the observed reflex)
and the scissors reflex.
1. Speed of the with or against motion: If the retinoscope mirror
is tilted in a highly ametropic eye, the resultant reflex is imaged at
a far point that is much closer to the eye than the reflex of an
almost emmetropic eye, the far point of which is located at a much
greater distance. With regard to the subject's pupil, movement of
the image at the far point of the almost emmetropic eye will seem
to have a greater angular velocity or speed. It should be stressed
that the direction of movement of the fundus image is not
influenced by the patient's ametropia (a downward movement of
the mirror will always produce a downward movement of the light
on the fundus). The with or against movement is a function of
the observation system, thus an against movement occurs only
when the eye and external lens system have a far point between
the patient's eye and the retinoscope peephole.
2. Brightness of the image: As neutrality is approached, all of the rays
emerging from the eye are focused at the peephole, where they
provide the brightest image that the examiner observes.
Illumination increases inversely to the square of image size. At any
other focal distance, some or all of the rays of light will not reach
the peephole and the image becomes duller (Fig. 21).
3. Width: Safir1 has noted that the power of retinoscopy results from
the image of the retina being projected in space with large
magnification. As neutrality is approached, the retinoscopic reflex
appears widest. The apparent width of the moving retinoscopic
image is the most difficult of the concepts to comprehend because
it relates to the concentration of light emerging from the retina
through the patient's pupil and then through the peephole of the
2
retinoscope. Michaels has discussed this subject in detail.
4. The on-off phenomenon: Although the retinoscopic reflex is bright
and wide on either side of neutrality, the reflex may disappear
completely when the retinoscope peephole is exactly conjugate to
the eye-corrective lens system (see Fig. 21). Fortunately, neither
the patient's eye nor the examiner's eye and hand can maintain
this exact position for long, but astute retinoscopist's may notice
the on-off phenomenon at neutrality.
5. The scissors reflex: The refractive elements of the eye are not
perfectly spherical. Thus, the center of the optical path may be
slightly myopic when compared with that of the periphery. The
amount of aberration may be small, but under circumstances of
perfect neutralization and a widely dilated pupil, the center of the
optical path may return a with motion while the periphery returns
an against motion. This pattern of opposing central and
peripheral retinoscopic movements is known as a scissors reflex.
There is only a small dioptric distance over which the scissors reflex
can be detected. The entire reflex returns to all with or all
against motion within about 0.50 D on either side of
neutralization.
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 20 of 33
Fig. 21. The origin of the on-off
phenomenon at neutrality. The far
point of the eye is situated at the
peephole of the retinoscope. Either
all or none of the rays will pass
through the peephole with the
slightest shift in the subject's eye or the retinoscope or the
retinoscopist's eye, causing the retinoscopist to see the contents of the
pupil as either filled with light or black.
Estimating Low Myopes via Neutralization Without Lenses
By now the reader should have determined that it is in fact quite possible
to neutralize low myopes without the use of lenses. The trick is to place
the retinoscope directly on the patient's far point, sweep the retinoscope
streak across the patient's pupil with the sleeve down, recognize the onoff phenomenon of the neutralization reflex, measure the distance from
the patient's eye to the retinoscope in meters, take the reciprocalthus
converting from meters (distance) to diopters (vergence)and voil, the
patient's refractive error has been determined.
For example, neutralization for a -2.00-D myope can be seen by placing
the retinoscope 50 cm from the patient's eye, and for a -4.00-D myope
by placing the retinoscope 25 cm from this patient's eye. Neutralization
for an emmetrope can only be done in this fashion by placing the
retinoscope infinitely far from the patient's eyetheoretically possible,
but not practically feasible. Because the far points of hyperopes do not lie
in real space (they lie beyond infinity), hyperopes cannot be neutralized
in this way.
The patients who are best served by this estimation technique of
neutralization retinoscopy are those whose net refractive errors lie
between -1.50 and -3.00 D, and conveniently this is exactly the group
that lies outside the range of estimation possible with ophthalmoscopic
retinoscopy.
NEUTRALIZATION RETINOSCOPY OF SPHERICAL EYES
The aforementioned technique describes a way to estimate a low
myope's refractive error without the use of lenses. The key to this
method is that the retinoscopist must change the distance that the
retinoscope is held from the patient's eye when trying to find the far
point. When performing neutralization retinoscopy, she does exactly the
oppositeshe holds the retinoscope at a constant specific working
distance and uses lenses to bring the patient's far point to the
retinoscope.
The first thing that a retinoscopist must do is choose a comfortable
working distance. She wants to be as far from her patient as possible
while still being close enough to comfortably manipulate lenses in front of
his eye. Thus, the working distance usually is described as arms length
away from the patient. For the average retinoscopist, this distance works
out to about 66 cm. Taller retinoscopists may prefer 75 cm, whereas
shorter ones may use 50 cm. It is not uncommon for retinoscopists to
work closer than their usual working distance in difficult cases, such as
small children, or adults with cataracts or small pupils. The actual
working distance does not matter as long the retinoscopist is aware of
the distance and adjusts her calculations accordingly.
The retinoscopist should be able to sit at her comfortable working
distance while using lenses to bring the patient's far point to her. The
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 21 of 33
retinoscopist accomplishes this feat by sweeping the retinoscope streak
across the patient's pupil and evaluating the direction, speed, brightness,
and width of the retinoscopy reflex. If she observes against motion, the
retinoscope must lie beyond the patient's far point, and the retinoscopist
can move the far point toward the retinoscope by placing a minus lens in
front of her patient's eye. If the reflex is fast, bright, and wide, the
retinoscope must have been near to the patient's far point, and a weak
minus lens should be chosen. However, if the reflex is slow, dim, and
narrow, the retinoscope probably lies a greater distance from the far
point, and a stronger minus lens should be chosen. If with motion is
observed after a minus lens is placed before the patient's eye, the
patient's far point has been moved beyond the retinoscope because too
strong of a minus lens was chosen. This lens should be removed and
replaced with a weaker minus one.
Similar manipulations are performed if with motion is initially seen
when neutralization is begun. In such cases, the far point must lie
beyond the retinoscopist's comfortable working distance. Again, how far
away the far point lies can be estimated by judging the quality of the
reflex. A plus lens then is chosen to bring the far point forward toward
the retinoscope.
Whenever possible, the retinoscopist should try to manipulate the far
point in such a way that with motion is being observed. A with reflex
typically is sharper and easier to judge than an against reflex. Thus, if
against motion is seen, neutralization will be easier to perform if a
strong enough minus lens is placed to push the far point beyond the
retinoscope, so that the retinoscopist can observe with motion. Care
must always be taken, however, when putting minus lenses in front of
younger patients because they can easily eat up this minus by
accommodating, thus leading the less careful retinoscopist down the
wrong path.
It should also be noted that the neutralization end point is not exactly an
end pointrather it is an end zone that measures about half a diopter in
depth (see Fig. 20). The true size of this zone of doubt varies with pupil
size and working distanceit is narrowest with a small pupil and close
working distance. Best results are achieved when entering the zone of
doubt from the plus side, by watching the with motion reflex get faster,
brighter, and wider until the retinoscopist is convinced the neutralization
reflex has been achieved. If the zone of doubt is entered from the minus
side (through against motion), there is a greater chance for error.
Eventually, after just a few different lenses are placed before the
patient's eye, the retinoscopist can observe the neutralization reflex. At
this point the goal is achieved, and the retinoscopist has managed to
bring the patient's far point to the retinoscope (which is being held at the
working distance). The retinoscopist is now ready to write a spectacle
correction. However, the lenses currently in front of the patient's eye do
not represent the correction needed to see clearly at infinite distance;
rather, the lenses represent the correction needed to see clearly at 66
cm. The patient will be quite dissatisfied if given a prescription for a pair
of glasses that allows for clear vision only 66 cm away or closer.
CORRECTING THE PRESCRIPTION FOR THE WORKING DISTANCE
LENS
The retinoscopist must always remember to modify the prescription for
distance vision, a mathematical manipulation called correcting for the
working distance. The gross power is that which the retinoscopist is
holding when retinoscopy is completed. This corresponds to the power
that brings light from the patient's luminous retina to focus at the
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 22 of 33
working distance. The net power is that which neutralizes the patient's
refractive error for good distance visionthe power that focuses light
from the luminous retina to a point at the horizon. The mathematical
computation is simple. The retinoscopist merely subtracts the working
distance (in diopters) from the gross to get the net. For example, when
the working distance is 66 cm (+ 1.50 D) and the patient is neutralized
with a -2.5 lens, the gross minus the working distance equals the net, or:
-2.5 - (+ 1.5) = -4. The retinoscopist will give a prescription for a -4
lens.
NEUTRALIZATION RETINOSCOPY OF ASTIGMATIC EYES
The previous discussion describes neutralization of spherical patients.
Further steps need to be taken in a patient with astigmatism. In patients
with astigmatism, the retinoscopy reflex seen in the pupil has one more
quality in addition to speed, brightness, and width. The reflex in patients
with astigmatism also appears to break as the light filament is rotated
(Fig. 22). The retinoscope reflex seen in the patient's pupil will not be
continuous with the streak lying on the cornea, lids, forehead, and
cheek; it will appear broken. There will be, however, two meridians
where the retinoscope reflex will be continuous with the streakwhere it
will not appear broken. These meridians correspond to the two axes of
the patient's astigmatism. The retinoscopist merely needs to neutralize
these two meridians separately and combine them to come up with the
desired spectacle correction. This can be done using only spherical lenses
(as is best when neutralizing children with loose lenses), spherical and
plus cylindrical lenses (using a plus cylinder phoropter or loose lenses
and trial frames), or spherical and minus cylindrical lenses (using a
minus cylinder phoropter or loose lenses and trial frames). Let us further
explore the methods of neutralizing astigmatic individuals in whom the
less plus (or more minus) axis is neutralized first and the more plus (or
less minus) axis is neutralized second. When neutralizing the axes in this
order, the retinoscopist can use either only spherical lenses, or spherical
and plus cylindrical lenses.
Fig. 22. Break. The line between the streak in the
pupil and outside the pupil is broken when the
streak is off the correct axis. (Corboy JM: Refining
the cylinder. In Corboy JM [ed]: Retinoscopy, p 87.
4th ed. Thorofare, NJ: Slack, 1996.)
Spherical Lens Technique
The first step is for the retinoscopist to find the least plus axis. The
retinoscope streak is swept back and forth across the pupil while it is
rotated 360 degrees by rotating the light filament in the handle. The
retinoscopist then observes at which two meridians the retinoscope reflex
does not appear brokenin cases of regular astigmatism, these two
meridians should be 90 degrees apart. The retinoscopist then compares
the reflex in one meridian to the reflex in the other, noting which
meridian's streak exhibits more against (slower, thinner, dimmer) or
less with (faster, broader, brighter) qualities than the other. This
meridian is neutralized first. If the reflex in one meridian shows with
motion and in the other shows against motion, the meridian with the
reflex that shows against is neutralized first.
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 23 of 33
The more minus meridian of the astigmatic person is then merely
neutralized much as the spherical myope or hyperope described
previously. The axis of the streak is held along the meridian line and
swept in a direction perpendicular to it (i.e., if the 90-degree axis is
being neutralized, the streak is oriented straight up and down and swept
from side to side). At first, it is not intuitive that the streak be held in the
same orientation as the axis meridian because one is searching for the
power of the astigmatism, and the power lies not along the axis, but
perpendicular to it. Here the retinoscopist must remember that the power
is found not by holding the streak still, but rather by sweeping it across
the pupil. Another way of saying this is that for each meridian to be
neutralized, the axis lies in the orientation of the streak, and the power
lies in the direction of the sweep.
Once the proper lens is placed before the patient's eye so that the
neutralization reflex is observed for that meridian, the retinoscopist
merely subtracts the working distance and records the power needed to
correct the patient for that particular axis. She then addresses the other
meridian.
The retinoscope streak is rotated 90 degrees, and the reflex is reexamined. The reflex should not appear broken in the new meridiana
broken reflex signifies that either the retinoscope streak is not exactly
aligned along the patient's second axis or that the patient has irregular
astigmatism. If the reflex is not broken, it is neutralized with lenses. If
spherical lenses are to be used, the second meridian is neutralized in
exactly the same manner as the first. Once the neutralization reflex has
been found, the retinoscopist again subtracts the working distance and
records the lens power needed to correct the patient for that particular
axis. A simple conversion then needs to be performed before presenting
the patient with the proper spectacle prescription, as follows:
Q: A patient is neutralized with the following lenses at a working
distance of 66 cm: [+ 3.50 axis 90] and [+ 4.25 axis 180]. What is the
eyeglasses prescription?
A: Step 1: Subtract the working distance. In this case, the working
distance is 66 cm, which is equal to 1.50 D:
[+ 3.50 axis 90] - 1.50 = + 2.00 axis 90 [+ 4.25 axis 180] - 1.50 = +
2.75 axis 180
Step 2: Transpose from cross-cylinder notation to plus-cylinder
notation:
+ 2.00 sphere + ([+ 2.75 - 2.00] axis 180)
= + 2.00 + 0.75 180
Plus-Cylinder Technique
If the second meridian is to be neutralized with a plus-cylinder lens (as is
done with a plus-cylinder phoropter or loose lenses and trial frames), the
first spherical lens should be left in the phoropter or trial frames. The
axis of the cylindrical lens is oriented in the direction of the axis of the
streak for the second meridian. Because a cylinder lens is being used, no
power is being added along the axis of the second meridian (which, of
course, corresponds to the power of the first meridian). When the
neutralization reflex is found for the second meridian, the streak is
rotated 90 degrees to ensure that the first meridian is still neutralized.
The working distance is then subtracted from the spherical lens, and the
spectacle prescription is easily determined as follows:
Q: A patient is neutralized with the following lenses at a working
distance of 66 cm: [+ 3.50 sphere] and [+ 0.75 axis 180]. What is the
eyeglasses prescription?
A: Step 1: Subtract the working distance from the spherical lens only.
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 24 of 33
In this case, the working distance is 66 cm, which is equal to 1.50 D:
[+ 3.50 sphere] - 1.50 = + 2.00 sphere
Step 2: Add the cylindrical lens to the new power of the spherical lens:
+ 2.00 sphere + [+ 0.75 axis 180]
= + 2.00 + 0.75 180
Minus-Cylinder Technique
Some clinicians prefer to work in minus cylinder. Patients are neutralized
in the same aforementioned manner, except that the more with or less
against meridian is neutralized first with spherical lenses. Then the less
with or more against meridian is neutralized with a minus-cylinder in
much the same way as the previous example used a plus-cylinder lens.
The transposition is done as follows:
Q: A patient is neutralized with the following lenses at a working
distance of 66 cm: [+ 4.25 sphere] and [-0.75 axis 90]. What is the
eyeglasses prescription?
A: Step 1: Subtract the working distance from the spherical lens only.
In this case, the working distance is 66 cm, which is equal to 1.50 D:
+ 4.25 sphere minus 1.50 = + 2.75 sphere
Step 2: Add the minus cylindrical lens to the new power of the spherical
lens:
+ 2.75 sphere + (-0.75 axis 90)
= + 2.75 - 0.75 90
Back to Top
TECHNIQUES TO EVALUATE ASTIGMATISM
It should be intuitive that it is easier for the retinoscopist to evaluate a
bright, thin reflex than a dim, broad one. There are various techniques
that enable one to alter the system so that a brighter reflex is observed.
These techniques include increasing the brightness of the bulb,
increasing the diameter of the peephole, dilating the pupil, and
decreasing the working distance. However, it is even more useful to
make the light reflex not only brighter, but also thinner, especially when
evaluating astigmatism.
At working distance, the pupil is completely or almost completely filled
with light when an emmetropic or mildly hyperopic eye is examined with
the retinoscope sleeve all the way down (Fig. 23). This was noted in the
section on retinoscopic neutralization. The pupil is filled because the
retinal image is magnified to a size at which it is actually larger than the
pupil. Enhancement techniques involve altering the magnification of the
retinoscopy reflex to make it appear as thin as possible. No discussion of
these techniques can be undertaken unless the reader has a solid
understanding of the optics of the magnification properties of the eye in
the context of retinoscopy.
Fig. 23. The relative magnifications
and distances (from the subject's
eye) of images of the retinoscope
filament when observing the image
of the retina in hyperopic eyes.
The eye may be considered the hyperopic version of the schematic eye
shown in Figure 16. The magnification is calculated as the ratio of
distance from the image of the retina to the subject's pupil divided by
distance from the pupil to the retina. A. Cone to which the observer's
view is restricted by the subject's pupil. Its apex is at the observer's
pupil (x) and its angular dimension is determined by the subject's pupil
(y). The lengths of the vertical solid bars traversing the cone represent
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 25 of 33
the widths of the images of the filament at several distances from the
eye. The segment of the bar that lies within the cone is visible to the
observer. B. Proportion of the filament image that can be seen by the
observer represented in another form. The filament image (crosshatched area) rapidly increases as the ametropia decreases. Beyond
approximately 1.00 D, the edges of the filament image cannot lie within
the cone, and enhancement cannot occur. Enhancement can occur in
eyes with 2.00 D or more of hyperopia. The filament image seen
through the subject's pupil is shown as a dark band. The retina is
located 0.02 m from the subject's pupil. Consider the extreme example
of + 50.00 D, in which the image of the retina is on the retina. It
would appear as a very small and bright line that would not fill the
pupil. A 50.00-D refraction at 1/50 of a meter = 2 cm. (Modified from
Safir A: Retinoscopy. In Tasman W, Jaeger EA [eds]: Duane's Clinical
Ophthalmology. Philadelphia: JB Lippincott, 1982.)
The technique of raising the sleeve to thin and brighten the reflex in
evaluating spherical and astigmatic hyperopia is called enhancement
(Fig. 24). A sharply focused filament reflex can be seen in the pupil when
the sleeve is incrementally raised toward the point at which the
emanated beam becomes parallel and enters an eye and working
distance lens that still requires more than 1.50-D hyperopic correction.
This occurs because the focal point of the retinoscope lies near the focal
point of the patient's eye. This makes the width of the focused filament
image on the retina essentially 0 and effectively prevents the appearance
of a magnified image. Rotation of the sleeve will not change the width of
the reflex if the eye has a spherical hyperopic refractive error. Only a thin
reflex is seen in the pupil. Perhaps the most important and practical point
about enhancement is thisif the reflex cannot be enhanced, there
cannot be more than + 1.50 of residual hyperopia.
Fig. 24. Enhancement of hyperopia
by raising the sleeve. Enhancement
is one technique that combines
changing in the illuminating system
with properties of the viewing
system. In hyperopic eyes, it is
possible to narrow the beam on the
retina sufficiently so that its borders
can be seen despite the magnification (cross-hatched) of the viewing
system. The amount that the sleeve is moved and the width of the facial
intercept permit estimation of the amount of hyperopia. Moreover,
meridional comparison is the basis for detection of hyperopic
astigmatism.
Raising the sleeve decreases the divergence of the emitted streak. If this
is done at working distance, the intercept or reflection on the patient's
cornea and lid gets smaller. This appearance phenomenon is called the
intercept. The width of the intercept can be used to estimate the amount
of hyperopia as one learns the apparent ratio of the enhanced reflex to
the width of the enhanced intercept (see Fig. 24).
MAGNIFICATION AND THE PUPIL
In ophthalmoscopic retinoscopy, all methods for detection of astigmatism
depend in some way on the skill of the retinoscopist in creating,
detecting, and maximizing the differential magnification of the
retinoscopic images along the astigmatic axes. As noted in the
introductory section on ophthalmoscopic retinoscopy, the thinnest,
brightest image is seen when the far point of the retinoscope is conjugate
with the far point of the patient's eye. Thus, the focal point of a plano
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 26 of 33
eye will be conjugate with the focal point of a retinoscope held 5 cm from
the patient with the sleeve positioned just above halfway up. At this
point, the retinoscopist will see a thin, bright line while the sleeve is
rotated in all directions, no matter how small the pupil. If the
retinoscopist then recedes from the patient without moving the sleeve,
she will soon note that the observed image widens until it eventually fills
the pupil. At this time, she has left the world of ophthalmoscopic
retinoscopy, where the observations depend on the system that
illuminated the retina, and she has entered the world of neutralization
retinoscopy, where observation depends on the viewing system. She now
makes observations based on the relative magnification at different
meridians of the images that originate from the luminous retina (see Fig.
23). The exact distance at which this happens is controlled by the pupil
size.
The growth of the width of the reflex relative to the pupil has been
compared with the view of a baseball game through a knothole in a
fence. If the observer is placed a great distance from the knothole, the
desired image is too wide for the small hole, and only a small proportion
of the baseball field can be observed. To observe the entire field, the
observer must bring her eye as close to the knothole as possible.
Optics of Magnification
The magnification equation is well known and relatively simple.
Magnification is the ratio of the far point distance of the image to that of
the object. Thus, in the case of an eye with 10.00 D of myopia, the
magnification of the image at the far point is 5 (see Fig. 16). That is,
based on the location of the image at 10 cm and the object at 2 cm, 2
cm is the distance between the dioptrics of the eye and the retina. (The
term dioptrics collapses the combined effect of the cornea and lens and
ignores the effects of refractive index, etc.) Because its image is at
infinity, the magnification of a plano eye will be infinite (see Fig. 16). The
optics of magnification for a hyperopic eye are shown in Figure 23.
If an eye has regular astigmatism with two far-point planes, it will have
two different magnifications, depending on the difference between them.
Thus, if one meridian were plano and the other either -2 or + 2, either of
these meridians will have far points at 50 cm from the eye. The
approximate magnification of the astigmatic meridian will be 50 2, or
25. The astigmatic meridian will appear smaller than the infinite
magnification of the plano meridian. The observer will detect astigmatism
as the sleeve is rotated at the optimal height. Identification of plus or
minus astigmatism depends on other techniques described elsewhere.
The detection of astigmatism usually depends on meridian differences in
image size (Fig. 25).
Fig. 25. Optics of meridional comparison
for astigmatism Astigmatism is detected
by observing meridional differences in
the sizes of virtual retinal images
projected into the far-point plane of a
hyperopic eye. The diagram (not to
scale) shows differences in the far point
image sizes for an eye with compound
hyperopic astigmatism requiring a net
correction of + 2.00 D, + 2.00 D 180 degrees. The unfocused
filament image of the retinoscope is shown projected onto the retina in
the vertical meridian only. The retina serves as an object for the images
focused in the far-point plane of each meridian. Note that the largest
image results from magnification because of its being focused at twice
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 27 of 33
the distance from the nodal point of the eye as the smaller image. The
scale measures distance (cm) posterior to the cornea. On the right are
shown the retinal images as viewed by the examiner when the filament
is alternately positioned on the principal meridians. The black ring
represents the patient's pupil. When the filament is vertical, the pupil is
almost flooded out. When the filament is horizontal, a much thinner line
is observed. Moving the retinoscope further from the eye would cause
both meridians to flood out the patient's pupil. (Weinstock SM,
Wirtschafter JD: A Decision-Oriented Manual of Retinoscopy. Springfield,
IL: Charles C Thomas, 1976.)
Magnification at Working Distance
In clinical neutralization retinoscopy, magnification is observed at 66 cm
from the eye through the peephole of the retinoscope and the pupil of
the examiner. In the condition of neutralization (e.g., an emmetropic eye
examined with a + 1.50-D working distance lens) the eye is illuminated
by a -2 divergent beam emitted from the retinoscope and converged by
the + 1.50 lens to a wide beam on the retina. Ignore the illuminating
system (it is irrelevant) and consider the observation system. The
observation system consists of an eye with an object distance (from the
dioptrics to the retina) of 2 cm and an image distance (from the dioptrics
to the far point) of 66 cm. The magnification will be 66 cm 2 cm, or
about 3.3X. This image will fill the pupil. Similar calculations of
magnification can be performed to show that the image of mildly
hyperopic eyes also is large enough to more than fill the pupil.
ENHANCEMENT TO DETECT ASTIGMATISM AND IDENTIFY PLUSCYLINDER AXIS
Rotation of the sleeve does not change the width of the reflex if the eye
has only a spherical hyperopic refractive error. However, if the eye is
astigmatic, a sharp image can be seen along only one axis unless the eye
is both hyperopic and astigmatic. The sharpest, brightest image is the
least magnified whereas the widest, dullest image is the most magnified.
The sharpest, brightest image is seen along the plus-cylinder axis so that
an eye with the rule astigmatism will have a plus cylinder axis at 90
degrees and a vertical, thin, bright filament image will be seen if there is
more than 1.50 D of hyperopia as the sleeve is raised. If raising the
sleeve detects two bright lines at right angles at two different heights,
the eye has both hyperopia and astigmatism (see Fig. 25). Assuming this
finding occurs during neutralization at standard working distance, the
retinoscopist should increase the amount of plus so that she is closer to
the spherical end point. The amount of plus lens to add should be
sufficient to eliminate enhancement in one meridian.
STRADDLING
Once astigmatism is detected, it is almost second nature to tune the
sleeve to the axis at which the reflex is the thinnest and brightest and
then to adjust the sleeve height and rotation to maximize the
observation (Fig. 26). The reflex becomes thicker if the retinoscopist
rotates the sleeve about 15 degrees to either side of the presumed
cylinder axis. This technique is called straddling because the retinoscope
beam is alternately rotated an equal angle on either side of the presumed
cylinder axis. When the cylinder power is weak, straddling reveals an
initial incorrect estimate of the axis location. The thinner image is called
the guide because it guides us to adjust the plus-cylinder axis toward
the thinner image. This step provides the initial detection of astigmatism,
and the phoropter axis can be adjusted so that plus lenses can be dialed
into place along the enhanced meridian.
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 28 of 33
Fig. 26. Straddling. The straddling
meridians are 45 degrees off the glass
axis, at roughly 35 and 125 degrees. As
you move back from the eye while
comparing meridians, the reflex at 125
degrees remains narrow (A) at the
same distance that the reflex at 35
degrees has become wide (B). This
dissimilarity indicates axis error; the
narrow reflex (A) is the guide toward which we must turn the glass axis.
(Corboy JM: Refining the cylinder. In Corboy JM [ed]: Retinoscopy, p
91. 4th ed. Thorofare, NJ: Slack, 1996.)
BREAK PHENOMENON
Astigmatism can also be detected by observation of the break
phenomenon. The break phenomenon is similar to straddling with the
enhanced beam. It is useful in refining the axis of large astigmatic
cylinders because one can observe a discontinuity, or break, between
the enhanced intercept axis and that of the retinal reflex when the
retinoscope filament beam is rotated somewhat away from the correct
cylinder axis (see Fig. 22). Both the guide and the break phenomenon
during straddling serve to identify the astigmatic axis.
ENHANCEMENT TO ESTIMATE PLUS-CYLINDER POWER
It is useful to observe the intercept reflection of the retinoscope beam
from the surface of the phoropter as the sleeve is raised. The intercept
narrows as the sleeve is raised and can be used to light the number axis
numbers and markings (see Fig. 24). The decreasing width of the
intercept can be observed as the sleeve is raised to the point of best
enhancement. The retinoscopist can use the observed width of the
intercept and the height of the sleeve to provide a rough estimate of
cylinder power with the best enhancement is seen. Using this technique,
the retinoscopist can detect any amount of hyperopia from + 1.50 D to +
infinity. For practical purposes, the sleeve should not be raised beyond
the plano (parallel beam) position or you will be in myopic territory with
a convergent beam. As you adjust astigmatic power and axis, you can
alternately repeat enhancement until cylinder axis and power are no
longer detectable. The retinoscopist then proceeds to refinement.
REFINEMENT OF NEUTRALIZATION RESULTS
The retinoscopist may choose to refine by neutralization at all meridians,
as described previously in the neutralization section of this chapter, or
she may choose to use some or all of the following special techniques:
1. Observe the intensity of the unenhanced band to refine cylinder
power. Rotate the sleeve when it is in the completely down
position. If the two astigmatic meridians are not equally bright (or
dull), make them even by adding + 0.25 D to the bright one or
subtracting + 0.25 D from the dull one. This technique may be
performed first by moving forward from the working distance to a
point about 20 cm closer to the patient's eye. At this distance, a
reflex will not fill the pupil. As you recede, the reflex will flood out
beyond the pupil; it is at this point that it is best to observe for any
differences in intensity. Repeat the step to confirm that equal
intensity is observed along all meridians.
2. Observe the intensity of the unenhanced band to refine cylinder
axis. If the previous step did not resolve the detected asymmetry,
recheck the axis. Simply move in again and locate the optimum
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 29 of 33
distance that maximizes the asymmetry. Straddle the presumed
plus-cylinder axis and note the thinnest or brightest meridian and
turn the plus-cylinder axis in that direction. Then repeat the power
refinement described in the previous step.
3. Observe the skew phenomenon of the unenhanced band to refine
cylinder axis (see Fig. 27). This is the only test of cylinder axis
location that does not involve straddling or rotation of the streak
from the presumed cylinder axis. The test is basically more useful
to confirm cylinder axis than to determine it. It consists of
sweeping the streak (without rotation) to either side of the
presumed axis. If the axis is correct, the reflex and the intercept
move parallel with each other; but if the axis is not correct, the
reflex deviates from the intercept and appears to be skewed. The
skew phenomenon detects far smaller abnormalities of cylinder axis
than the break phenomenon. The two differ in that skew is
performed without rotation of the filament axis and cannot be
observed except when the retinoscope is moving.
Fig. 27. Skew (oblique motion). The arrows indicate
that movement of the reflex and intercept are not
parallel. The reflex and intercept do not move in the
same direction but are skewed when the streak is off
axis. (Corboy JM: Refining the cylinder. In Corboy JM
[ed]: Retinoscopy, p 89. 4th ed. Thorofare, NJ: Slack,
1996.)
The Skew Phenomenon: An Optical Illusion
2
Michaels has explained as an optical illusion the oblique motion seen in
astigmatism that prompted the development of retinoscopy. Try the
experiment he proposed. Observe a pencil held at 45 degrees through a
2.5-cm hole in a piece of paper held 25 cm from your eye. Sweep the
pencil horizontally behind the hole and observe that the pencil seems to
move obliquely. The oblique reflex motions and the break phenomenon
observed in astigmatism as a consequence of the conoid of Sturm. The
magnification of the retinal reflex varies in each meridian. Only when the
retinal reflex and the intercept are aligned do they form an unbroken
line. Movement of the streak along any other meridian produces an
oblique reflex motion.
Back to Top
RELIABILITY
In a previous edition, Safir noted that retinoscopy is the best method for
1
objectively evaluating the dioptric state of the eye. Much of what follows
is quoted verbatim. Retinoscopy, however, measures only one aspect of
refractionthe optics that are necessary to place images of distant
objects in sharp focus on the retina. It does not measure the rest of the
subjective visual experience. Retinoscopy should, therefore, be combined
with subjective refraction whenever possible.
STATISTICAL CONSIDERATIONS
The less cooperative the patient, the greater the reliance on objective
observations. In the extreme case of poor cooperationfor example, the
young child or mentally challenged patientsedation or even general
anesthesia may be necessary. In cases that are not quite so difficult, the
practitioner who is very skillful with a retinoscope has a great advantage
over the practitioner who is not. This situation is the one that truly
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 30 of 33
rewards the retinoscopist who can quickly and accurately determine a
patient's refractive error through the techniques of ophthalmoscopic
retinoscopy and neutralization retinoscopy.
Because important therapeutic judgments may depend on the
retinoscopic measurements, it is necessary to know how reliable these
measurements are.12 Reliability and precision are terms that describe the
degree to which repeated measurements resemble one another. For
example, five repeated measurements for one patient might yield the
following five spherical results: + 2.25, + 2.75, + 2.50, + 2.75, + 2.25.
With another examiner, the following values might be found: + 1.75, +
2.50, + 3.25, + 2.75, + 2.25. The first examiner displays a higher
degree of reliability or precision than the second one. Nevertheless, the
average value is the same for both: + 2.50. If any single measurements
had been accepted as the patient's true refractive error, the patient
might have been misjudged by only D by the first examiner, but by as
much as D by the second.
How is it possible, then, to judge the reliability of any measurement? The
answer is straightforward: There must be repeated measurements so
that the variability of the measurements can be assessed. The repeated
measurements should be independent of one another, each derived
without the measurer having knowledge of what the preceding ones
were. These are usually called replicate measurements, and there is no
way to judge reliability without them. In clinical practice, we often do
these replicate measurements informally and almost intuitively.
Fluctuations in the measurement process are unavoidable; statisticians
call them error. The second examiner in the previous example is less
precise than the first. She showed greater variability and larger error.
Reliability and error for retinoscopy have been evaluated. One study by
Safir and coworkers entailed five clinicians performing retinoscopy on ten
healthy young subjects on two separate occasions separated by one to
13,14
Results showed a 50% probability that the two
three weeks.
measurements of spherical power would differ by 0.40 D. The Safir study
also showed a threefold difference in reliability among retinoscopists.
Accuracy is another concept that is important in the understanding of
measurement. Accuracy is the physical scientist's term for the quality
that psychologists call validity. Accurate measurements are those that
are close to the true value being measured. Accuracy is a relative
concept; one procedure may be more or less accurate than another.
Suppose, for example, that a subject's true spherical refractive error
were 2.00 D, and that ophthalmologist A measured it five times as 2.25,
2.25, 2.00, 2.00, 1.75, whereas ophthalmologist B got values of 2.5, 2.5,
2.75, 2.75, and 3. It is apparent that the method of ophthalmologist A is
more accurate than that of ophthalmologist B. The typical measurement
for ophthalmologist A is closer to the quantity sought than that of
ophthalmologist B, even though the precision of the two refractionists is
about the same. This example shows that there is no predefined
relationship between precision and accuracy.
Retinoscopy is better at measuring cylinder than sphere. It is most
sensitive for cylinder axis, next for cylinder power, and poorest for
sphere power. It is sobering to realize that our ability to judge spherical
power may be rather limited. If the patient is uncooperative (e.g., a
restless child) and the examiner must work quickly, the error is likely be
even higher. Young retinoscopists must also resist the temptation to
accommodate through the retinoscope when evaluating a difficult patient
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 31 of 33
because this further decreases both reliability and accuracy. We can only
guess, but errors of 1.00 D or more must be commonplace.
THE ROLE OF THE RETINOSCOPE IN A MODERN EYE CLINIC
In the 21st century, we are faced with an ever-more automated world,
and the ophthalmic practice has paralleled this move toward automation.
The retinoscope, really little more than a light filament, lens, and mirror,
is now joined by many more sophisticated (and certainly more
expensive) devices developed to help us obtain information regarding the
refractive state of our patients. One family of such instruments consists
of the automated refractorstabletop or hand-held devices that perform
an objective refraction in a matter of seconds at the touch of a button.
The largest advantage of the automated refractor is that clinic personnel
who have almost no knowledge in the art of refraction can use it. For the
average patient, automated refractors are reasonably accurate when
compared with the retinoscope and generally agree within D.15,16 If
automated refractors err, they tend to overestimate minus sphere by a
fraction of a diopter. This discrepancy probably stems from the fact that
patients accommodate in response to their sense that the automated
refractor is at a closer distance to the patient than is the 6 meter far
point used in retinoscopy. This is true even though the devices are
designed to relax accommodation while fixing on an artificial distant
target.
Where the automated refractor is at an undeniable disadvantage to the
retinoscope is in evaluating patients with irregular astigmatism, either
from pathology (e.g., keratoconus, pellucid marginal degeneration) or
postsurgically (e.g., corneal transplant, laser in situ keratomileusis
[LASIK]). All the automated refractor operator can do is press a button
while having the patient fixate on the target. The automated refractor
then either calculates a best fit refraction or flashes an error message
that there too much irregular astigmatism exists to make a reading. The
retinoscopist, however, can gain much more information about the
refractive state of the patient by judging the quality of the light reflex
observed in the patient's pupil. A skilled retinoscopist usually can deduce
quantities and qualities of astigmatism in patients for whom the
automated refractor fails. This is especially true in patients with poor
best-corrected visual acuity.
Other instruments that must be compared with the retinoscope are the
17
keratoscope and the automated corneal modeling systems. Although it
is tempting to compare these instruments with the retinoscope because
they each provide important information regarding astigmatism, it must
be remembered that these instruments serve different purposes within
the ophthalmic practice. The keratoscope and corneal topographers are
used to evaluate corneal astigmatism only. The retinoscope, however, is
used to determine the entire refractive state of the eye. These
instruments all have their place and can complement each other well.
A final issue, one that is becoming more important with every passing
year, is the role of the retinoscope in managing the refractive surgery
patient. Few studies address this problem. Retinoscopy has been shown
18
to be accurate in evaluating the postoperative patient. Anecdotally, we
agree with these results. In our practice, we rely heavily on retinoscopy
in evaluating pre- and postoperative refractive surgery patients. We
believe that automated refractors cannot accurately evaluate the
refractive state of someone with a surgically altered cornea and therefore
believe that they have no role in providing data on these patients. Other
studies have shown that corneal topography alone is not adequate in
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 32 of 33
19
evaluating patient satisfaction after laser refractive surgery.
Remembering that the critical zone of the retinoscopy reflex is the central
3 mm, and that the average excimer laser ablation diameter is 6 mm,
one can see that the retinoscope is well suited to evaluate these patients.
When patients who had previously had corneal refractive surgery
subsequently undergo cataract extraction with intraocular lens (IOL)
implantation, there is more variability in the postoperative refractions
than for typical cataract patients. The IOL calculations rely not on
retinoscopy (objective refraction), but instead on keratometry (corneal
curvature) and a-scan ultrasonography (axial length). One can only
wonder if the diagnostic procedure of choice for these patients might
someday be for the surgeon to remove the cataract, perform
intraoperative retinoscopy of the aphakic eye, calculate the necessary
lens power, then place the desired IOL implant. In that way, the IOL
would depend on the patient's refractive state rather than on artificial
calculations based on the patient's altered ocular anatomy.
Back to Top
REFERENCES
1. Safir A: Retinoscopy. In Tasman W, Jaeger EA, eds: Duane's Clinical
Ophthalmology. Philadelphia: JB Lippincott, 1982
2. Michaels DD: Visual Optics and Refraction: A Clinical Approach, pp 357
376. 2nd ed. St Louis: CV Mosby, 1980
3. Rubin ML: Optics for Clinicians. 2nd ed. Gainesville, FL: Triad Science
Publishers, 1974
4. Corboy JM: The Retinoscopy Book, pp 16. 4th ed. Thorofare, NJ:
Slack, 1996
5. Weinstock SM, Wirtschafter JD: A Decision-Oriented Manual of
Retinoscopy. Springfield, IL: Charles C Thomas, 1976
6. Kettesy A: Uber die theorein der skiaskopic anlasslich ihres 100
jahrigen bestehens. Klinisch Monatsblauer fur Augenheilkunde 162:26
33, 1973
7. Millodot M: A centenary of retinoscopy. J Am Optom Assoc 44:1057
1059, 1973
8. Safir A: Some retinoscope reflections: The instruments. Surv
Ophthalmol 18:6270, 1973
9. Copeland JC: Streak retinoscopy. In Sloane AE (ed): Manual of
Refraction. 2nd ed. Boston: Little, Brown, 1970.
10. Copeland JC: The refraction of children with special reference to
retinoscopy. Int Ophthalmol Clin 3:959970, 1963
11. Pascal JI: The incidence neutral point in retinoscopy. Arch
Ophthalmol 39:550551, 1948
12. Hyams L, Safir A: Statistical concepts in refraction. Int Ophthalmol
Clin 11:103114, 1971
13. Safir A, Hyams L, Philpot J et al: Studies in refraction: I. The
precision of retinoscopy. Arch Ophthalmol 84:4961, 1970
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
Volume 1, Chapter 37. Retinoscopy
Page 33 of 33
14. Hyams L, Safir A, Philpot J: Studies in refraction: II. Bias and
accuracy of retinoscopy.Arch Ophthalmol 85:3341, 1971
15. Salvesen S, Kohler M: Automated refraction: A comparative study of
automated refraction with the Nidek AR-1000 autorefractor and
retinoscopy. Acta Ophthalmologica 69:342346, 1991
16. Grosvenor T, Perrigin DM, Perrigin J: Three-way comparison of
retinoscopy, subjective, and Dioptron Nova refractive findings. Am J
Optom Physiol Opt 62:6365, 1985
17. Rowsey JJ, Fowler WC, Terry MA et al: Use of keratoscopy, slit-lamp
biomicroscopy, and retinoscopy in the management of astigmatism after
penetrating keratoplasty. Refract Corneal Surg 7:3341, 1991
18. Nagy ZZ, Suveges I, Senyi K et al: Retinoscopy after excimer laser
photorefractive treatments. Acta Chir Hung 35:307313, 1995-6
19. Kampmeier J, Tanzer DJ, Er H et al: Significance of corneal
topography in predicting patient complaints after photorefractive
keratectomy. J Cataract Refract Surg 25:492499, 1999
Back to Top
http://80.36.73.149/almacen/medicina/oftalmologia/enciclopedias/duane... 08.04.2016
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- How To PornograpgyDocument31 pagesHow To Pornograpgyfriends.sanjauli0% (1)
- Performing Physical Assessment of The EyeDocument14 pagesPerforming Physical Assessment of The Eyezyrine jhen100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Corrie White - The Ultimate Guide To Water Drop PhotographyDocument111 pagesCorrie White - The Ultimate Guide To Water Drop PhotographyBrent100% (1)
- Voigtlaender PDFDocument22 pagesVoigtlaender PDFkjfotoNo ratings yet
- Soal Bahasa Inggris Kelas 9Document4 pagesSoal Bahasa Inggris Kelas 9Doel Maleeq Terra80% (10)
- Science Summative AssessmentDocument3 pagesScience Summative AssessmentRamir BecoyNo ratings yet
- Milky Way Photography: The Definitive Guide (2021)Document124 pagesMilky Way Photography: The Definitive Guide (2021)Steven PollardNo ratings yet
- Retinoscopie 1 PDFDocument33 pagesRetinoscopie 1 PDFDiana LupoiuNo ratings yet
- 2013 Tiffany & Co. Sunglass CollectionDocument60 pages2013 Tiffany & Co. Sunglass CollectionDiana LupoiuNo ratings yet
- File ListDocument5 pagesFile ListDiego BrandaoNo ratings yet
- TradussDocument2 pagesTradussDiana LupoiuNo ratings yet
- Caiet Materiale enDocument30 pagesCaiet Materiale enDiana LupoiuNo ratings yet
- Takumar Lenses SpecificationsDocument15 pagesTakumar Lenses SpecificationsazamamaNo ratings yet
- FUJIFILM Superia X-TRA 400 color negative film guideDocument6 pagesFUJIFILM Superia X-TRA 400 color negative film guideFelipe EduardoNo ratings yet
- Easy WorkDocument9 pagesEasy WorkGtgt68No ratings yet
- RAK Security LawsDocument11 pagesRAK Security LawsyasirNo ratings yet
- TANDBERG TRC-4 Remote Control User GuideDocument2 pagesTANDBERG TRC-4 Remote Control User GuideJean RibeiroNo ratings yet
- Simplified Guide to Operating a System Controller MatrixDocument20 pagesSimplified Guide to Operating a System Controller MatrixHamzagNo ratings yet
- Generic ConventionsDocument5 pagesGeneric Conventionsapi-388565090No ratings yet
- Geometric Optics - Mirrors and LensesDocument74 pagesGeometric Optics - Mirrors and Lenses11-CG14 Jao, Kathleen Maye E.No ratings yet
- Test Bank For Abnormal Child Psychology 7th Edition MashDocument36 pagesTest Bank For Abnormal Child Psychology 7th Edition Mashpoleytallierbuj0cfNo ratings yet
- JVC Camcorder Detailed Manual GZ-HM30Document99 pagesJVC Camcorder Detailed Manual GZ-HM30arfynessNo ratings yet
- Gcse-Photoshoot-Planner 14Document1 pageGcse-Photoshoot-Planner 14api-265587792No ratings yet
- ScriptDocument7 pagesScriptapi-477398671No ratings yet
- NAEST 2022 Prelims EXPERIMENT-3Document3 pagesNAEST 2022 Prelims EXPERIMENT-3Prapanj KtNo ratings yet
- Overview of Alignment Procedures CM12/120 Microscopes: LegendDocument49 pagesOverview of Alignment Procedures CM12/120 Microscopes: LegendManuel CasanovaNo ratings yet
- DH-HAC-B4A21-VF: 2MP HDCVI IR Bullet CameraDocument3 pagesDH-HAC-B4A21-VF: 2MP HDCVI IR Bullet CameraChristopher NolanNo ratings yet
- BX3 Unit Guide ENDocument20 pagesBX3 Unit Guide ENqanunjiNo ratings yet
- Metals 09 00749Document11 pagesMetals 09 00749rockon12No ratings yet
- Sensar 1 Piece - AAB00Document2 pagesSensar 1 Piece - AAB00rhymenNo ratings yet
- IPC Products PromotionDocument118 pagesIPC Products PromotionLucia Fernanda RUBINA CHUMPITAZNo ratings yet
- C8W Pro 2K - DatasheetDocument11 pagesC8W Pro 2K - DatasheetOLX LMNo ratings yet
- Cycloplegic Effect of 0.5%tropicamide and 0.5%phenylephrine Mixed Eye Drops - Objective Assessment in Japanese Schoolchildren With MyopiaDocument5 pagesCycloplegic Effect of 0.5%tropicamide and 0.5%phenylephrine Mixed Eye Drops - Objective Assessment in Japanese Schoolchildren With Myopiaal_dhi_01No ratings yet
- Joseph Jackson ListerDocument4 pagesJoseph Jackson Listerjovmac2uNo ratings yet
- Beginner Unit 3bDocument2 pagesBeginner Unit 3bgrover0% (1)