Professional Documents
Culture Documents
6 - Jensen Et Al. - Chemoreflex Control of Breathing During Wakefulness in Healthy Men and Women
Uploaded by
AnaKpotCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
6 - Jensen Et Al. - Chemoreflex Control of Breathing During Wakefulness in Healthy Men and Women
Uploaded by
AnaKpotCopyright:
Available Formats
Chemoreflex control of breathing during wakefulness
in healthy men and women
Dennis Jensen, Larry A. Wolfe, Denis E. O'Donnell and Gregory A. L. Davies
Journal of Applied Physiology 98:822-828, 2005. First published Nov 19, 2004;
doi:10.1152/japplphysiol.01208.2003
You might find this additional information useful...
This article cites 35 articles, 20 of which you can access free at:
http://jap.physiology.org/cgi/content/full/98/3/822#BIBL
Updated information and services including high-resolution figures, can be found at:
http://jap.physiology.org/cgi/content/full/98/3/822
Additional material and information about Journal of Applied Physiology can be found at:
http://www.the-aps.org/publications/jappl
Journal of Applied Physiology publishes original papers that deal with diverse areas of research in applied physiology, especially
those papers emphasizing adaptive and integrative mechanisms. It is published 12 times a year (monthly) by the American
Physiological Society, 9650 Rockville Pike, Bethesda MD 20814-3991. Copyright 2005 by the American Physiological Society.
ISSN: 8750-7587, ESSN: 1522-1601. Visit our website at http://www.the-aps.org/.
Downloaded from jap.physiology.org on February 28, 2005
This information is current as of February 28, 2005 .
J Appl Physiol 98: 822 828, 2005.
First published November 19, 2004; doi:10.1152/japplphysiol.01208.2003.
Chemoreflex control of breathing during wakefulness in healthy men and women
Dennis Jensen,1 Larry A. Wolfe,1,2 Denis E. ODonnell,2,4 and Gregory A. L. Davies3
1
School of Physical and Health Education, Departments of 2Physiology and 3Obstetrics and Gynaecology, and
Division of Respirology and Critical Care, Department of Medicine, Queens University, Kingston, Ontario, Canada
Submitted 11 November 2003; accepted in final form 15 November 2004
hypoxia; chemoreflex sensitivity; ventilatory recruitment threshold;
sleep-disordered breathing
mediated by the peripheral chemoreflex, is greater in men than
women (20, 32, 33), whereas others have reported the opposite
result (1). However, others have found that gender has no
effect on either central (1, 13, 18, 26, 30, 34) or peripheral (13,
26, 27, 32, 34) chemoreflex sensitivity.
Divergent results from previous investigations may be due to
different experimental designs. Some studies did not control
for menstrual cycle status of female subjects (20, 21, 28, 30,
32, 34), whereas others made comparisons between men and
women in the luteal phase (37) and follicular phase (FP) (1, 13,
26, 27) of the menstrual cycle. Also, some studies have not
considered oral contraceptive use among female volunteers
(21, 28, 30) or gender differences in body size and/or lung
functional indexes (20, 26, 28).
Recent epidemiological studies (4, 36) have demonstrated
that the prevalence of sleep-disordered breathing (SDB), a
condition of repeated apneas, hypopneas, and breathing oscillations, is two to three times greater in men than women (4,
36). Differences in the central and/or peripheral chemoreflex
control of breathing during wakefulness may reflect a similar
difference during sleep that could contribute to the high male
prevalence of SDB (12, 37).
This study investigated the effect of gender on the ventilatory recruitment threshold (VRT) for CO2 and the ventilatory
response below (i.e., behavioral drives) and above (i.e., chemoreflex sensitivity) this threshold while maintaining constant
backgrounds of hyperoxia and hypoxia, respectively. We hypothesized that neither the hyperoxic nor hypoxic VRT for
CO2 would differ between men and women. In addition, we
hypothesized that the ventilatory response to CO2 below and
above this threshold would be greater in men than women,
independent of the level of O2.
OVARIAN AND TESTICULAR HORMONES influence the control of
breathing via their effects on both central and peripheral
chemoreflexes (2, 33). Progesterone increases central and peripheral chemosensitivity to hypercapnia and hypoxia (2, 33).
This effect is potentiated by estrogen (2, 33). In addition,
testosterone increases peripheral chemoreflex sensitivity to
hypoxia (2, 17, 33), but its effect on central chemoresponsiveness remains unclear (2, 33). Given the effects of reproductive
hormones on ventilatory control as well as gender differences
in endocrine status, it is reasonable to expect that central and/or
peripheral chemoreflex control characteristics may differ between healthy men and women during wakefulness.
Current evidence suggests that the apneic threshold and
sensitivity of the ventilatory response to CO2, mediated by the
central chemoreflex, is greater in men than women (20, 26, 35,
37), regardless of menstrual cycle status (20, 33, 35). Some
studies have shown that the ventilatory response to hypoxia,
Subjects. Healthy, nonsmoking, normally active men (n 14) and
women (n 14), aged 20 35 yr, were recruited at Queens University
through posted announcements and flyers. Subjects had no history of
cardiorespiratory disease, nor were they born at or recently returned
from high altitude. None was taking medications that affect ventilatory control. Female subjects had regular menstrual cycles, as verified
by questionnaire, and had not used oral contraceptives for 6 mo before
experimental testing.
Before study entry, subjects attended an information session to
familiarize them with the laboratory and study procedures. All subjects completed the revised Physical Activity Readiness Questionnaire
(available online at www.csep.ca/forms.asp) to ensure that there were
no contraindications to participation. Demographic information, including age, occupation, and occupational and recreational physical
activity levels, were assessed by questionnaire. To evaluate menstrual
Address for reprint requests and other correspondence: L. A. Wolfe, School
of Physical and Health Education, Queens Univ., Kingston, Ontario, Canada
K7L 3N6 (E-mail: wolfel@post.queensu.ca).
The costs of publication of this article were defrayed in part by the payment
of page charges. The article must therefore be hereby marked advertisement
in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
822
METHODS
8750-7587/05 $8.00 Copyright 2005 the American Physiological Society
http://www. jap.org
Downloaded from jap.physiology.org on February 28, 2005
Jensen, Dennis, Larry A. Wolfe, Denis E. ODonnell, and
Gregory A. L. Davies. Chemoreflex control of breathing during
wakefulness in healthy men and women. J Appl Physiol 98: 822 828,
2005. First published November 19, 2004; doi:10.1152/japplphysiol.
01208.2003.This study used a modified CO2 rebreathing procedure
to examine the effect of gender on the chemoreflex control of
breathing during wakefulness in healthy men (n 14) and women
(n 14). Women were tested in the follicular phase of the menstrual
cycle. During rebreathing trials, subjects hyperventilated to reduce the
partial pressure of end-tidal CO2 (PETCO2) below 25 Torr and were
then switched to a rebreathing bag containing a normocapnic hypoxic
or hyperoxic gas mixture. During the trial, PETCO2 increased, while O2
was maintained at a constant level. The point at which ventilation
began to rise as PETCO2 increased was identified as the ventilatory
recruitment threshold (VRT). Ventilation below the VRT was measured, and the slope of the ventilatory response above the VRT was
determined. Gender had no effect on the hyperoxic or hypoxic VRT
for CO2. Central chemoreflex sensitivity was significantly greater in
men than women but not after correction for forced vital capacity.
Measures of peripheral chemoreflex sensitivity were similar between
genders. However, the slope of the tidal volume (VT) response to
hyperoxic and hypoxic CO2 rebreathing (corrected and uncorrected)
was greater in men than women, respectively. We conclude that
central chemoreflex sensitivity is greater in men compared with
women as reflected by differences in ventilatory (uncorrected) and VT
(corrected and uncorrected) responses to CO2. However, gender has
no significant effect on the central chemoreflex VRT for CO2. The
peripheral chemoreflex control of breathing during wakefulness is
similar between men and women.
EFFECT OF GENDER ON THE VENTILATORY RESPONSE TO CARBON DIOXIDE
J Appl Physiol VOL
A 12-bit analog-to-digital converter (DAQCard-6062E, National
Instruments) digitized the continuous analog output signals from all
monitoring devices for computer analysis using custom-written software (LabVIEW, National Instruments). The data-acquisition soft E, f, VT, PETCO2,
ware calculated breath-by-breath measures of V
PETO2, SaO2, and HR.
Data analyses. Data from rebreathing experiments were imported
to an analysis program (LabVIEW, National Instruments) designed
specifically for this purpose (J. Duffin, personal communication).
Barometric pressure and room temperature were entered, and measured volumes were corrected to body temperature and pressure,
saturated (BTPS). Data from the first equilibration at the start of
rebreathing and any aberrant points detected by the data-acquisition
software during the experiments were excluded from further analysis.
Subsequently, breath-by-breath PETCO2 was plotted against time and
fitted with a least squares regression line, whose slope depends on the
CO2). The equation for this line
metabolic rate of CO2 production (V
provided a predicted value of PETCO2 vs. time, thereby minimizing
E, VT, and f
interbreath variability due to measurement. Thereafter, V
were plotted against the predicted PETCO2.
Each of these plots was fitted with a model made up of the sum of
two segments separated by one breakpoint. All segments were fitted
through an iterative process whereby the breakpoint and other parameters were varied to obtain an optimal fit to the observed data by
minimizing the sum of squares (Levenberg-Marquardt algorithm)
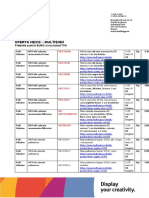
using commercial software (Sigmaplot 7.0, SPSS). Figure 1 is an
E response of a representative
example of the lines fitted to the V
subject during an isooxic hyperoxic CO2 rebreathing procedure. The
first segment of the response was an exponential decline to a final
E, VT, and
value (i.e., basal). This value was taken as a measure of V
f below the VRT for CO2, respectively. Rarely, a short-term potentiation of breathing was observed after hyperventilation, and its waning
was modeled as an exponential decay.
E, VT, and f began to rise in a linear fashion
The point at which V
in conjunction with a rise in PETCO2 was taken as the VRT for CO2
(Fig. 1). On the basis of the modeling of Duffin et al. (9), we assumed
that the VRT measured under hyperoxic conditions originated from
the central chemoreflex alone, because hyperoxia abolishes virtually
Fig. 1. An example of the ventilatory response to progressive hypercapnia
while O2 was maintained at 150 Torr in a representative subject. Note the
measurement of basal ventilation, the ventilatory recruitment threshold, and
chemoreflex sensitivity. PETCO2, end-tidal PCO2. See text for details.
98 MARCH 2005
www.jap.org
Downloaded from jap.physiology.org on February 28, 2005
cycle status, female subjects identified the first day of their last
menstrual cycle and the average length of their cycle. This approach
has been validated in our laboratory by using plasma progesterone
measurements (23). The study protocol and consent form were approved by the Research Ethics Board, Faculty of Health Sciences,
Queens University, and all subjects provided written consent.
Basic physical measurements included height and body mass,
forced vital capacity (FVC), forced expired volume in 1 s (FEV1), and
peak expiratory flow (model S-301, Pneumoscan). Body mass index
(BMI) was calculated as body mass/height2 (kg/m2). Body surface
area (BSA; m2) was calculated from height and body mass measurements. All female subjects were tested in the FP (range: 213 days
from the first day of menstruation) of the menstrual cycle when
circulating estrogen and progesterone levels are low and gender
differences in endocrine status are minimized.
Modified rebreathing protocol. Volunteers abstained from aerobic
and muscular conditioning exercise as well as caffeine and alcohol on
the day of testing. Two rebreathing experiments, each separated by at
least 45 min, were completed in the morning (AM) and evening (PM)
of the same day. AM and PM trials were separated by 12 h.
A modified version of Reads (24) rebreathing procedure that
includes prior hyperventilation and maintenance of a constant (i.e.,
isooxia) end-tidal O2 tension (PETO2) was used to evaluate central and
peripheral chemoreflex control characteristics (9). During each trial,
subjects breathed room air for 5 min, using a slow and deliberate
breathing pattern to avoid the short-term potentiation effect described
by Folgering and Durlinger (10). Prior hyperventilation lowered the
body stores of CO2 below 25 Torr, thereby allowing the VRT to be
identified as the partial pressure of end-tidal CO2 (PETCO2) increased
from hypo- to hypercapnia. Furthermore, prior hyperventilation permits measurement of the ventilatory response below this threshold,
independent of the ventilatory chemoreflexes (i.e., basal), estimating
behavioral drives (29). After hyperventilation, subjects were switched
from room air to a rebreathing bag containing a normocapnic (42
Torr) hypoxic or hyperoxic gas mixture. Rebreathing began with three
deep breaths, producing rapid equilibration of the PCO2 in the bag,
lungs, and arterial blood to that of the mixed venous blood. The
equilibration was verified by a plateau in PETCO2 and was a prerequisite for continuing the test. On equilibration, subjects were asked to
breathe as they felt the need.
During rebreathing, PETCO2 increased while isooxia was maintained, under computer control, at a constant hyperoxic (150 Torr) or
hypoxic (50 Torr) level. In its hyperoxic form, the modified rebreathing procedure measures central chemoreflex sensitivity equivalent to
that measured using Reads original technique (19). Continuous measures of arterial blood O2 saturation (SaO2) (model OXI, Radiometer,
Copenhagen, Denmark) and heart rate (HR) (Max-1 electrocardiograph, Marquette) were obtained throughout each test. Rebreathing
was terminated if ventilation exceeded 100 l/min, PETCO2 exceeded 60
Torr, SaO2 fell below 70%, and/or subject discomfort.
Rebreathing apparatus. During rebreathing, subjects wore nose
clips and breathed through a mouthpiece connected to one side of a
three-way T-shaped manual directional valve (11.9-ml dead space;
model 2100a, Hans Rudolph) that permitted switching from room air
to the rebreathing bag. Subjects rebreathed from a 10-liter plastic bag
connected to a volume turbine (model VMM-1100, Alpha Technologies). The volume turbine was coupled to the expiratory end of the T
valve and monitored breath-by-breath changes in minute ventilation
E), tidal volume (VT) and respiratory rate (f). A sampling tube
(V
connected to the mouthpiece side of the T valve permitted continuous
analysis of PETCO2 and PETO2 by using a respiratory mass spectrometer
(model MGA 1100, Perkin-Elmer) at a sample flow rate of 64 ml/min.
Isooxia was maintained by a flow of 100% O2 to the bag side of the
T valve. The testing system was calibrated with gases of known
concentrations and a standard 3.004-liter volume syringe (model
1922, CS-3000 AM Systems) before each rebreathing test.
823
824
EFFECT OF GENDER ON THE VENTILATORY RESPONSE TO CARBON DIOXIDE
RESULTS
Physical characteristics. Mean age and BMI were similar
between men and women (Table 1). As expected, body height,
body mass, peak flow, FEV1, FVC, and BSA were significantly
greater in men than women. FEV1/FVC was significantly
greater in women than men. All women were tested within the
FP of the menstrual cycle (8.4 1.0 days from the first day of
menstruation).
Effect of gender on chemoreflex control characteristics.
Significant correlations were observed between body height,
FVC, FEV1, BSA, and both hyperoxic and hypoxic chemoreflex characteristics (Table 2).
J Appl Physiol VOL
Table 1. Physical characteristics of subjects
Variable
Men (n 14)
Women (n 14)
Age, yr
Body height, cm
Body mass, kg
BMI, kg/m2
Peak flow, l/s
FVC, liters
FEV1, liters
FEV1/FVC, %
BSA, m2
25.41.12
1811.8
83.43.29
26.10.9
7.430.18
5.020.14
3.790.12
75.72.26
2.070.05
22.90.66
1641.9*
653.00*
24.10.9
4.980.27*
3.290.14*
2.790.11*
85.52.58*
1.720.04*
Values are means SE; n, no. of subjects. BMI, body mass index; FVC,
forced vital capacity; FEV1, forced expired volume in 1 s; BSA, body surface
area. *Significant between-gender difference; P 0.05.
E and VT were significantly greater in men than
Basal V
women under both hyperoxic and hypoxic conditions (Table
3). However, these differences were abolished after the data
were normalized for FVC (F 0.50, P 0.48). There was no
main effect of gender on the basal f response (F 0.82, P
0.37) during hyperoxic and hypoxic rebreathing.
E (F 2.39, P 0.13)
No main effect of gender on the V
and VT (F 2.58, P 0.11) recruitment threshold for CO2
was observed, independent of the level of isooxia (Table 3). In
contrast, the CO2 recruitment threshold for f was significantly
greater in men than women under both isooxic rebreathing
conditions.
E and VT chemoreflex sensitivities to CO2 were signifiV
cantly greater in men than women under both hyperoxic and
hypoxic rebreathing conditions (Table 3). When comparisons
were made between genders after normalization for FVC,
E chemoreflex sensitivity was not significantly different
mean V
between genders (F 0.10, P 0.76), independent of the
level of O2. In contrast, gender differences in the sensitivity of
the VT response to CO2 during hyperoxic and hypoxic trials
persisted after normalization for FVC. In this regard, elimina E response to CO2 at high
tion of the gender difference in the V
and low levels of O2 could be explained by the effect FVC has
on f because gender differences in the VT response to CO2
remain after correcting for FVC.
Gender had no effect on the peripheral chemoreflex contri E (corrected and uncorrected), VT
bution to the increase in V
(corrected and uncorrected), or f during isooxic hypoxic CO2
rebreathing (Table 4). The observed difference in the uncor E response to hypoxic-hypercapnia may be attributed
rected V
to an effect of gender on central chemoreflex sensitivity.
Effects of isooxic PETO2 (150 vs. 50 Torr) on chemoreflex
control characteristics. There was no main effect of isooxia on
E (F 0.32, P 0.57), VT (F 0.44, P 0.51), or
basal V
f (F 0.01, P 0.93), irrespective of gender (Table 3). The
E and VT was lower, whereas
CO2 recruitment threshold for V
chemoreflex responsiveness was higher, during hypoxic vs.
hyperoxic rebreathing trials, independent of gender. In contrast, the f recruitment threshold for CO2 was significantly
greater, whereas f chemoreflex responsiveness was identical
(F 0.81, P 0.38), during hyperoxic and hypoxic rebreathing trials, independent of gender.
E,
Correlations between chemoreflex characteristics. Basal V
E chemosensitivity estimates obtained from all
VRT, and V
subjects were pooled and grouped according to the isooxic
rebreathing condition (hyperoxic or hypoxic). Correlations
98 MARCH 2005
www.jap.org
Downloaded from jap.physiology.org on February 28, 2005
all peripheral chemoreflex activity (7). Moreover, it was assumed that
the VRT measured under hypoxic conditions derived from the sum of
the central and peripheral chemoreflexes.
E, VT, and f responses above the
The slope of the line fitted to V
VRT was taken as a measure of chemoreflex sensitivity to increases in
E, VT, and f
PETCO2 (Fig. 1). We assumed that the slope of the V
response measured during hyperoxic trials represented central chemoreflex sensitivity, whereas the slope recorded from hypoxic trials
represented the additive effects of central and peripheral chemoreflex
stimulation (9). Thus the slope of the hyperoxic response was subtracted from the slope of the hypoxic response for each subject to
isolate peripheral chemoreflex sensitivity. Because lung volumes vary
in proportion to body size and are usually higher in men than women,
E and VT were corrected for body
basal and sensitivity measures of V
height, body mass, BSA, BMI, FEV1, and FVC, respectively. Comparisons of f responses (i.e., basal, VRT, and sensitivity) were made
between nine women and six men.
Minimum sample size estimate. Sensitivity and VRT measures from
hyperoxic and hypoxic rebreathing conditions were selected as important outcome data for between-gender effects. Minimum sample
size was calculated on the basis of 80% power and a confidence
interval of 0.05 using an unpaired subject formula for the comparison
of means (22). Sample sizes capable of detecting between-gender
differences of 1.5 l min1 Torr1 and 2 Torr were estimated for
sensitivity and VRT parameters, respectively, using standard deviations from Mateika and Ellythy (16). The resulting critical sample
sizes were estimated to be 6 and 9 for hyperoxic and hypoxic
sensitivity parameters and 10 and 9 for hyperoxic and hypoxic VRT
parameters, respectively. Therefore, a sample size of 14 subjects per
group was adequate for this study.
Statistical analyses. Students t-statistics for independent samples
were used for simple between-gender comparisons of physical characteristics. A three-way ANOVA was used to detect main effects for
gender, isooxia, and time of day among the calculated parameters.
Time of day had no effect on the mean data, independent of isooxia.
Furthermore, significant AM-PM correlations (Pearson r) were observed for all hyperoxic (range: r 0.45 0.75; P 0.01) and
hypoxic (range: r 0.67 0.78; P 0.01) rebreathing responses.
Therefore, to reduce random intrasubject variability, data collected
during AM and PM trials were averaged for each subject. A two-way
ANOVA was used to detect differences between genders (men vs.
women) and levels of O2 (hyperoxia vs. hypoxia) on the mean data.
The post hoc test of Tukey (honestly significant difference) was used
to identify between-gender differences under each experimental condition.
Unpaired Students t-statistics were used to identify significant
between-group differences in peripheral chemoreflex sensitivity. Pearson product-moment correlation coefficients (Pearson r) were calculated between hyperoxic and hypoxic chemoreflex parameters and
subject physical characteristics, respectively. Results for all statistical
tests were considered significant if P 0.05. Values are presented as
means SE.
825
EFFECT OF GENDER ON THE VENTILATORY RESPONSE TO CARBON DIOXIDE
Table 2. Correlations between hyperoxic and hypoxic rebreathing responses (all subjects) and
anthropometric and spirometric variables
Basal (subthreshold)
E, l/min
V
VT, ml (BTPS)
Sensitivities to CO2
E, lmin1Torr1
V
1
VT, mlmin
Torr
Condition
Age, yr
Height, cm
Weight, kg
Hyperoxic
Hypoxic
Hyperoxic
Hypoxic
0.32
0.22
0.19
0.02
0.44*
0.36
0.44*
0.41*
0.28
0.34
0.30
0.38*
Hyperoxic
Hypoxic
Hyperoxic
Hypoxic
0.29
0.11
0.15
0.26
0.45*
0.39*
0.74
0.69
0.36
0.20
0.72
0.54
BMI, kg/m2
FVC, liters
FEV1, liters
BSA, m2
0.07
0.22
0.07
0.20
0.50*
0.47*
0.50
0.57
0.44*
0.44*
0.48
0.53
0.34
0.37
0.34
0.40*
0.15
0.01
0.37
0.17
0.44
0.37
0.75
0.64
0.45*
0.45*
0.78
0.72
0.42*
0.27
0.77
0.61
E, minute ventilation; VT, tidal volume. *Significant correlation at the P 0.05 level. Significant correlation at the P 0.01 level.
V
DISCUSSION
The primary findings of this study suggest that central
chemoreflex sensitivity is greater in men than women as
E (uncorrected) and VT (both
reflected by differences in V
corrected and uncorrected) responses to hyperoxic and hypoxic
CO2 rebreathing. However, the central chemoreflex VRT for
CO2 is similar in men compared with women. In addition,
gender has no significant effect on the peripheral chemoreflex
control of breathing during wakefulness when women are
tested in the FP of their menstrual cycle.
Critique of methods. The benefits of the modified rebreathing procedure have been described previously (18, 19). Despite
its advantages, the modified rebreathing technique may initiate
responses, such as induction of short-term potentiation, respi-
ratory muscle fatigue, changes in cerebral blood flow (CBF),
and state of arousal and/or anxiety, that could influence the
ventilatory response after voluntary hyperventilation (14,
16, 18).
Short-term potentiation after hypocapnic hyperventilation is
seldom observed during wakefulness in healthy subjects (14,
15, 19). When it is observed, the time constant is much less
than the time required to reach the VRT for CO2 (14 16, 19).
Furthermore, Morelli et al. (20) recently demonstrated that the
time constant of the poststimulus potentiation induced by
hypocapnic hyperventilation was not significantly different
between men and women. Similarly, Jordan et al. (11) found
no evidence of a gender or menstrual cycle phase effect on the
time constant of the ventilatory decline after hypoxic and
hypercapnic ventilatory stimulation, respectively. These findings suggest that short-term potentiation had no effect on the
VRT calculated from hyperoxic and hypoxic rebreathing trials,
independent of gender within the present study.
It is unlikely that the ventilatory response to hyperoxic and
hypoxic CO2 rebreathing was influenced by respiratory muscle
fatigue because subjects breathed through a low-resistance
apparatus for a shorter period of time than that previously
shown to cause diaphragmatic fatigue under loaded conditions
Table 3. Effects of gender on the ventilation, tidal volume, and breathing frequency response to CO2
under hyperoxic and hypoxic rebreathing conditions
Hyperoxia
Basal (subthreshold)
E, l/min
V
F/FVC, lmin111
V
VT, ml (BTPS)
VT/FVC, ml/l
f, breaths/min
Ventilatory recruitment
threshold for CO2
E, Torr
V
VT, Torr
f, Torr
Sensitivities to CO2
E, lmin1mmHg1
V
E/FVC, lmin1mmHg1l1
V
VT, mlmin1mmHg1
VT/FVC, mlmin1mmHg1l1
f, breathsmin1mmHg1
Hypoxia
Women
Men
Women
Men
9.91.1
3.10.4
73146
22920
14.21.1
16.32.1*
3.30.4
1,070156*
20928
16.11.9
10.51.3
3.20.4
78459
24218
13.91.3
17.72.1*
3.60.5
1,159126*
22922
16.21.9
47.50.6
46.80.8
48.81.0
49.30.5
48.40.6
50.60.5*
43.80.6
43.30.6
46.10.9
43.90.7
43.80.5
48.60.6*
2.830.27
0.900.10
102.588.80
31.562.39
1.500.25
4.350.39*
0.890.08
220.0920.51*
43.713.72*
0.950.15
4.160.50
1.270.14
157.0115.68
47.894.35
1.450.28
5.980.69*
1.220.15
335.7243.30*
66.998.25*
1.500.26
Values are means SE. f, Respiratory rate. *Significant between-gender difference, P 0.05.
J Appl Physiol VOL
98 MARCH 2005
www.jap.org
Downloaded from jap.physiology.org on February 28, 2005
among these characteristics were tested by using a Pearson
E and
product-moment correlation analysis. Neither basal V
E chemosensitivity
E and V
VRT (r 0.34, P 0.08) or basal V
(r 0.36, P 0.06) were significantly correlated for hyper E and VRT were not significantly
oxic tests. Similarly, basal V
correlated (r 0.07, P 0.72) for hypoxic tests. However, a
E chemosensi E and V
significant correlation between basal V
tivity (r 0.48, P 0.01) was identified for hypoxic trials.
826
EFFECT OF GENDER ON THE VENTILATORY RESPONSE TO CARBON DIOXIDE
Table 4. Effect of gender on the central and peripheral chemoreflex contribution to the ventilatory,
tidal volume, and breathing frequency response to CO2
Central Chemoreflex
Sensitivities to CO2
Women
Men
E, lmin1mmHg1
V
E/FVC, l/min1mmHg1l1
V
VT, mlmin1mmHg1
VT/FVC, mlmin1mmHg1l1
f, breathsmin1mmHg1
2.830.27
0.900.10
102.588.80
31.562.39
1.500.25
4.350.39*
0.890.08
220.0920.51*
43.713.72*
0.950.15
Peripheral Chemoreflex
P Value
0.48
0.37
Women
Men
P Value
1.320.31
0.380.08
54.4312.06
16.333.61
0.160.24
1.640.57
0.340.12
115.6333.74
23.286.41
0.720.49
0.63
0.77
0.10
0.35
0.28
Values are means SE. *Significant between-gender difference, P 0.05.
J Appl Physiol VOL
have been expected. This was not the case. Furthermore,
environmental factors known to influence the state of arousal
E (29) were controlled and
(i.e., lights, noise) and thus V
maintained for each subject and trial, respectively.
It could be argued that random intrasubject variability due to
testing at different times within the same day may have masked
systematic differences between genders. However, we observed significant AM-PM correlations for all hyperoxic and
hypoxic responses, which demonstrates sufficient reproducibility within the pooled data. In addition, AM and PM responses
were averaged for each subject to further reduce both biological and methodological variability, thereby increasing statistical power and the probability of finding between-gender
differences. Furthermore, minimum sample size calculations
were made before the study by using standard deviations from
a recent report using similar subjects and identical methods
(16) that verified the adequacy of statistical power in the
present study. Therefore, it is unlikely that random intrasubject
variability, subject familiarization, and/or other methodological factors influenced the interpretation of our results.
Ventilatory response to hypocapnia in men and women. To
our knowledge, we are the first to report that the ventilatory
response to hypocapnia (i.e., basal) is greater in men than
women during wakefulness. This effect was attributed to a
E
higher basal VT in male volunteers. However, when basal V
and VT were corrected for FVC, the mean responses were
identical. Therefore, the higher FVCs in men compared with
women accounted for the difference in the uncorrected data.
The ventilatory response to hypoxia in the presence of
hypocapnia has been studied with conflicting results. Findings
from our study and previous investigations (6, 9, 19) have
E is similar between hyperoxic and hypoxic trials
shown that V
when PETCO2 is below the recruitment threshold. Duffin et al.
(9) recently demonstrated that the ventilatory responses to
hypocapnia in the presence of isooxic PETO2 values of 150, 100,
80, 60, and 40 Torr were not significantly different. Thus
current evidence suggests that hypoxia has no independent
E when PETCO2 is below the VRT. These data
effect on V
support the hypothesis that ventilation is influenced by a
wakefulness drive to breathe (29), independent of the ventilatory chemoreflexes.
Effect of gender on the central chemoreflex. The existence of
gender differences in the central chemoreflex control of breathing is controversial. Regensteiner et al. (26) have reported that
gender has no effect on absolute measures of central chemoreflex sensitivity, whereas other studies (1, 21, 28, 30, 34, 35, 37)
have reported that the sensitivity of the central chemoreflex is
greater in men than women, regardless of menstrual cycle
98 MARCH 2005
www.jap.org
Downloaded from jap.physiology.org on February 28, 2005
(3). Subjects also rested for at least 45 min between trials to
avoid respiratory muscle fatigue.
Alterations in CBF due to hypoxia and hypercapnia could
affect the sensitivity and/or VRT for CO2 by modifying the
arteriovenous difference and thus the relationship between
PETCO2 and brain tissue PCO2 (PtiCO2). Although this is a
concern when steady-state methods are used (18), it is of lesser
importance when the modified rebreathing procedure is employed (18, 24). Thus the initial equilibration of CO2 at the
start of rebreathing ensures that changes in CBF do not affect
the arteriovenous difference via washout of PtiCO2 and consequently the slope of the ventilatory response to CO2 (25). In
addition, because the subject and bag are a closed system, both
blood circulation and pulmonary ventilation act as mixing
forces to reduce any differences between PETCO2 and PtiCO2
induced by voluntary hyperventilation (18).
The modified rebreathing procedure permits direct measurement of the VRT for CO2 mediated by the central and peripheral chemoreflex. In contrast, other methods identify the chemoreflex threshold by extrapolation of the linear relation be E and PETCO2 to the x-axis (7). Consequently, the
tween V
threshold is taken as the PETCO2 axis intercept and/or apneic
threshold (7). If the extrapolated threshold were a true estimate
of the apneic threshold, then the VRT for CO2 measured using
E,
the modified rebreathing procedure would depend on basal V
independent of the level of O2. However, a significant correlation was not observed in this study or previous studies (14,
E have
16). In addition, exercise-induced increases in basal V
no effect on the VRT for CO2 mediated by either the central (5)
or peripheral chemoreflex (8).
An additional limitation of the extrapolation method is that
subjects with lower chemoreflex sensitivities will inevitably
have much lower extrapolated thresholds than those with
higher chemoreflex sensitivities. Findings from our study and
past investigations (15, 16) have shown that no significant
correlation exists between threshold and sensitivity parameters.
Therefore, the modified rebreathing procedure provides a more
accurate and representative estimate of the VRT for CO2 than
alternative or traditional methods.
Performing a novel task (i.e., voluntary hyperventilation,
breathing through a mouthpiece) without familiarization may
have increased our subjects state of arousal and/or anxiety and
consequently the ventilatory response to CO2. Although basal,
VRT, and sensitivity responses were higher than those reported
by Duffin et al. (9), they are consistent with ongoing studies in
Duffins laboratory (J. Duffin, personal communication) as
well as our own (D. Jensen and L. A. Wolfe, unpublished
observations). If a lack of subject familiarity had had an effect
on our results, differences between AM and PM trials would
EFFECT OF GENDER ON THE VENTILATORY RESPONSE TO CARBON DIOXIDE
J Appl Physiol VOL
Effect of gender on the ventilatory patterning response to
CO2. Inconsistencies in the literature regarding the effect of
gender on the chemoreflex control of breathing may exist
because VT and f were not considered. As previously discussed, the slope of the VT response to CO2 (both corrected and
uncorrected) at high and low levels of O2 were significantly
greater in men than women. In addition, the f recruitment
threshold for CO2 was significantly lower in women, independent of the level of O2, even though the slope of the f response
was similar. However, gender had no effect on the peripheral
E (corrected and uncorchemoreflex contribution to the V
rected), VT (corrected and uncorrected), and f response during
hypoxic CO2 rebreathing. These findings are consistent with
Sajkov et al. (27) and suggest that the ventilatory response to
CO2, mediated by the central chemoreflex, is more critically
dependent on an increase in f than VT in women than men. This
may be due, at least in part, to an effect of gender and/or sex
hormones on central neuromodulatory mechanisms that influence the regulation of respiratory rhythm (2). Future studies are
needed to confirm this hypothesis.
Implications for SDB. Recent epidemiological studies (4, 36)
have identified male gender as a predisposing risk factor for the
development of SDB. Differences in airway morphology, fat
distribution, endocrine status, and/or the chemoreflex control
of breathing may explain the greater incidence of SDB in men
compared with women (12).
Chemoreflex drives are the sole support of rhythmic breathing during sleep, as behavioral drives present during wakefulness are withdrawn (31). Zhou et al. (37) recently demonstrated
that both chemosensitivity and the apneic threshold for CO2 are
greater in men than women. These differences, in combination
with the observation that men require a significantly smaller
reduction in PETCO2 to induce central apnea and/or hypopnea
than women (37), may explain the high male prevalence of
SDB.
However, we have shown, in accordance with previous
investigations (15, 16, 20), that behavioral drives to breathe
have no effect on either the central or peripheral VRT for CO2.
Thus our data suggest that gender has no effect on the central
and peripheral VRT for CO2, proceeding withdrawal of behavioral stimuli during sleep. Therefore, gender-related differences in the central and peripheral VRT for CO2 may not
contribute to the greater incidence of SDB in men relative to
women.
We have demonstrated that central chemoreflex sensitivity is
greater in men than women during wakefulness. Therefore,
men may be more susceptible to ventilatory overshoot and a
more pronounced hypocapnia (i.e., decrease in central respiratory drive, initiation and prolongation of recurrent apneic
events) on apnea termination than women, despite similar
central and peripheral VRTs for CO2. However, body size and
CO2 were significantly greater in men compared
therefore V
with women. Thus the degree of ventilatory overshoot required
to reduce PETCO2 below the central and peripheral VRT for CO2
during sleep is also greater in men than women because of the
increasing hyperbolic relation between alveolar CO2 and alve CO2 (7). Taken together, genderolar ventilation at a higher V
related differences in the central and peripheral chemoreflex
control of breathing may not solely explain the pathogenesis
and high male prevalence of SDB (12, 36).
98 MARCH 2005
www.jap.org
Downloaded from jap.physiology.org on February 28, 2005
status (20, 35, 37). In keeping with these latter results, we have
E (uncorrected) and VT (corrected and
shown that both V
uncorrected) responses to isooxic hyperoxic CO2 rebreathing
are greater in men than women. Thus our data support an effect
of gender on central chemoreflex sensitivity that may be
attributed to increased levels of circulating testosterone in men
relative to women. In this regard, laboratory animals treated
with testosterone demonstrate significant increases in central
chemoreflex responsiveness (33).
Only a few studies have examined the effect of gender on the
central chemoreflex threshold for CO2. Most studies have
shown that chemoresponsiveness, and consequently the apneic
threshold for CO2, is greater in men than women (21, 35, 37),
whereas Regensteiner et al. (26) reported that no gender
difference exists. Furthermore, Morelli and coworkers (20)
recently showed that gender has no effect on the VRT for CO2
estimated from isooxic hyperoxic CO2 rebreathing trials. Our
data confirm these latter results as estimates of the central
chemoreflex VRT for CO2 did not differ between genders.
Effect of gender on the peripheral chemoreflex. Several
studies have used the progressive isocapnic hypoxia procedure
to examine the effect of gender on peripheral chemoreflex
sensitivity (1, 13, 26, 34, 35). However, this procedure is
problematic because neither the sensitivity nor threshold of the
interaction between hypoxia and CO2 is apparent from the
E and PETO2. Moreover, the
curvilinear relation between V
PETCO2 chosen to represent isocapnia may be above or below
the VRT for CO2, resulting in an over- or underestimation of
peripheral chemoreflex sensitivity, respectively. For these reasons, we employed the modified rebreathing procedure that, in
its hypoxic form, permits measurement of the threshold and
sensitivity of the ventilatory response to CO2, mediated by the
sum of both central and peripheral chemoreflexes.
E response to CO2 during hypoxic
The sensitivity of the V
trials was significantly greater in men than women but not after
correction for FVC. However, gender differences in the slope
of the VT response persisted even after correction for FVC.
E
Because the peripheral chemoreflex contribution to the V
(corrected and uncorrected), VT (corrected and uncorrected),
and f responses were not significantly different between genders, we concluded that only central chemoreflex sensitivity is
different between men and women. White et al. (35) reported
that peripheral chemoreflex sensitivity (even after correction
for BSA) was significantly greater in men compared with
women. Similarly, Morelli et al. (20) recently demonstrated
that the ventilatory response to isooxic hypoxic CO2 rebreathing is significantly greater in men than women. However, it is
unclear whether gender had an effect on peripheral chemoreflex sensitivity, as Morelli et al. failed to determine the peripheral chemoreflex contribution to the hypoxic-hypercapnic ventilatory response. Nevertheless, our findings are consistent with
the majority of previous investigations showing that gender has
no significant effect on peripheral chemoreflex sensitivity (1,
13, 26, 27, 32, 34). Moreover, findings from our study and a
past investigation (20) demonstrate that the peripheral chemoreflex VRT for CO2 is not significantly different between
genders. Taken together, we conclude that gender has no
significant effect on the peripheral chemoreflex control of
breathing.
827
828
EFFECT OF GENDER ON THE VENTILATORY RESPONSE TO CARBON DIOXIDE
Summary. The present study supports the hypothesis that
central chemoreflex sensitivity is greater in men than women.
However, gender has no effect on the central chemoreflex VRT
for CO2. There is no significant effect of gender on the
peripheral chemoreflex control of breathing during wakefulness when women are tested in the FP of the menstrual cycle.
Further study is recommended to confirm and clarify the effect
of gender and sex hormones on the chemoreflex and neural
control of breathing during wakefulness and sleep.
ACKNOWLEDGMENTS
We acknowledge the technical support of Dr. James Duffin, Safraaz
Mahamed (Respiratory Research Group, University of Toronto), and Ken Hall
(Queens University). We thank Lindsay A. Nettlefold for contribution to data
collection.
GRANTS
REFERENCES
1. Aitken ML, Franklin JL, Pierson DJ, and Schoene RB. Influence of
body size and gender on control of ventilation. J Appl Physiol 60:
1894 1899, 1986.
2. Behan M, Zabka AG, Thomas CF, and Mitchell GS. Sex steroid
hormones and the neural control of breathing. Respir Physiol Neurobiol
136: 249 263, 2003.
3. Bellemare F and Grassino A. Effect of pressure and timing of contraction on human diaphragm fatigue. J Appl Physiol 53: 1190 1195, 1982.
4. Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, Vela-Bueno A,
and Kales A. Prevalence of sleep-disordered breathing in women: effects
of gender. Am J Respir Crit Care Med 163: 608 613, 2001.
5. Casey K, Duffin J, and McEvoy GV. The effect of exercise on centralchemoreceptor threshold in man. J Physiol 383: 9 18, 1987.
6. Corne S, Webster K, and Younes M. Hypoxic respiratory response
during acute stable hypocapnia. Am J Respir Crit Care Med 167: 1193
1199, 2003.
7. Cunningham DJC, Robbins PA, and Wolff CB. Integration of respiratory responses to changes in alveolar partial pressures of CO2 and O2 and
in arterial pH. In: Handbook of Physiology. The Respiratory System.
Control of Breathing. Bethesda, MD: Am. Physiol. Soc., 1986, sect. 3, vol.
II, pt. 2, chapt. 15, p. 475528.
8. Duffin J and McEvoy GV. The peripheral-chemoreceptor threshold to
carbon dioxide in man. J Physiol 406: 1526, 1988.
9. Duffin J, Mohan RV, Vasilou P, Stephenson R, and Mahamed S. A
model of the chemoreflex control of breathing in humans: model parameters measurement. Respir Physiol 120: 1326, 2000.
10. Folgering H and Durlinger M. Time course of posthyperventilation
breathing in humans depends on alveolar CO2 tension. J Appl Physiol 54:
809 813, 1983.
11. Jordan AS, Catcheside PG, Orr RS, ODonoghue FJ, Saunders NA,
and McEvoy RD. Ventilatory decline after hypoxia and hypercapnia is
not different between healthy young men and women. J Appl Physiol 88:
39, 2000.
12. Kapsimalis F and Kryger MH. Gender and obstructive sleep apnea
syndrome, part 2: mechanisms. Sleep 25: 499 506, 2002.
13. Kunitomo F, Kimura H, Tatsumi K, Kuriyama T, Watanabe S, and
Honda Y. Sex differences in awake ventilatory drive and abnormal
breathing during sleep in eucapnic obesity. Chest 93: 968 976, 1988.
14. Mahamed S, Cunningham DA, and Duffin J. Changes in respiratory
control after three hours of isocapnic hypoxia in humans. J Physiol 547:
271281, 2003.
J Appl Physiol VOL
98 MARCH 2005
www.jap.org
Downloaded from jap.physiology.org on February 28, 2005
This work was supported by grants from the Ontario Thoracic Society and
the William M. Spear Respiratory Research Endowment Fund (Queens
University). D. Jensen was supported by an R. S. McLaughlin fellowship
(Queens University), Queens Graduate Award, Ontario Thoracic Society
Research Training Fellowship, and an Ontario Graduate Scholarship for
Science and Technology.
15. Mahamed S and Duffin J. Repeated hypoxic exposures change respiratory chemoreflex control in humans. J Physiol 534: 595 603, 2001.
16. Mateika JH and Ellythy M. Chemoreflex control of ventilation is altered
during wakefulness in humans with OSA. Respir Physiol Neurobiol 138:
4557, 2003.
17. Mateika JH, Omran Q, Rowley JA, Zhou XS, Diamond MP, and Badr
MS. Treatment with leuprolide acetate decreases the threshold of the
ventilatory response to carbon dioxide in healthy males. J Physiol 501:
637 646, 2004.
18. Mohan RM, Amara CE, Cunningham DA, and Duffin J. Measuring
central-chemoreflex sensitivity in man: rebreathing and steady-state methods compared. Respir Physiol 69: 227235, 1999.
19. Mohan R and Duffin J. The effect of hypoxia on the ventilatory response
to carbon dioxide in man. Respir Physiol 108: 101115, 1997.
20. Morelli C, Badr MS, and Mateika JH. Ventilatory responses to carbon
dioxide at low and high levels of oxygen are elevated after episodic
hypoxia in men compared with women. J Appl Physiol 97: 16731680,
2004.
21. Patrick JM and Howard A. The influence of age, sex, body size and lung
size on the control and pattern of breathing during CO2 inhalation in
caucasians. Respir Physiol 16: 337350, 1972.
22. Press WH, Flannery BP, Teukolsky SA, and Vetterling WT. Numerical
Recipes: The Art of Scientific Computing (2nd ed.). London: Cambridge
University Press, 1992.
23. Preston RJ, Heenan AP, and Wolfe LA. Physicochemical analysis of
phasic menstrual cycle effects on acid-base balance. Am J Regul Integr
Comp Physiol 280: R481R487, 2001.
24. Read DJC. A clinical method for assessing the ventilatory response to
CO2. Australas Ann Med 16: 20 32, 1967.
25. Read DJ and Leigh J. Blood-brain tissue PCO2 relationships and ventilation during rebreathing. J Appl Physiol 23: 5370, 1967.
26. Regensteiner JG, Pickett CK, McCullough RE, Weil JV, and Moore
LG. Possible gender differences in the effect of exercise on hypoxic
ventilatory response. Respiration 53: 158 165, 1988.
27. Sajkov D, Neill A, Saunders NA, and McEvoy RD. Comparison of
effects of sustained isocapnic hypoxia on ventilation in men and women.
J Appl Physiol 83: 599 607, 1997.
28. Sebert P, Barthelemy L, and Mialon P. CO2 chemoreflex drive of
ventilation in man: effects of hyperoxia and sex differences. Respiration
57: 264 267, 1990.
29. Shea SA. Behavioural and arousal-related influences on breathing in
humans. Exp Physiol 81: 126, 1996.
30. Sin DD, Jones RL, and Man GC. Hypercapnic ventilatory response in
patients with and without obstructive sleep apnea. Chest 117: 454 459,
2000.
31. Skatrud JB and Dempsey JA. Interaction of sleep state and chemical
stimuli in sustaining rhythmic ventilation. J Appl Physiol 55: 812 822,
1983.
32. Tarbichi AGS, Rowley JA, Shkoukani MA, Mahadevan K, and Badr
MS. Lack of gender difference in ventilatory chemoresponsiveness and
post-hypoxic ventilatory decline. Respir Physiol Neurobiol 137: 4150,
2003.
33. Tatsumi K, Moore LG, and Hannhart B. Influences of sex hormones on
ventilation and ventilatory control. In: Lung Biology in Health and
Disease. Regulation of Breathing, edited by Dempsey JA, and Pack AI.
New York: Dekker, 1995, p. 829 864.
34. Van Klaveren RJ and Demedts M. Determinants of the hypercapnic and
hypoxic response in normal man. Respir Physiol 113: 157165, 1998.
35. White DP, Douglas NJ, Pickett CK, Weil JV, and Zwillich CW. Sexual
influence on the control of breathing. J Appl Physiol 54: 874 879, 1983.
36. Young T, Palta M, Dempsey J, Skatrud J, Weber S, and Badr S. The
occurrence of sleep-disordered breathing among middle-aged adults.
N Engl J Med 328: 1230 1235, 1993.
37. Zhou XS, Shahabuddin S, Zahn BK, Babcock MA, and Badr MS.
Effect of gender on the development of hypocapnic apnea/hypopnea
during NREM sleep. J Appl Physiol 89: 192199, 2000.
You might also like
- Integration of Cerebrovascular CO2 Reactivity and Chemoreflex Control of Breathing - Mechanisms of Regulation, Measurement, and InterpretationDocument23 pagesIntegration of Cerebrovascular CO2 Reactivity and Chemoreflex Control of Breathing - Mechanisms of Regulation, Measurement, and InterpretationAnaKpot100% (1)
- Integration of Cerebrovascular CO2 Reactivity and Chemoreflex Control of Breathing - Mechanisms of Regulation, Measurement, and InterpretationDocument23 pagesIntegration of Cerebrovascular CO2 Reactivity and Chemoreflex Control of Breathing - Mechanisms of Regulation, Measurement, and InterpretationAnaKpot100% (1)
- Integration of Cerebrovascular CO2 Reactivity and Chemoreflex Control of Breathing - Mechanisms of Regulation, Measurement, and InterpretationDocument23 pagesIntegration of Cerebrovascular CO2 Reactivity and Chemoreflex Control of Breathing - Mechanisms of Regulation, Measurement, and InterpretationAnaKpot100% (1)
- Chemoreflex Control PDFDocument49 pagesChemoreflex Control PDFAnaKpotNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Newborn Care Volume 1 2020-1Document192 pagesNewborn Care Volume 1 2020-1Shyvonne PeirisNo ratings yet
- Stetler Model EBP PosterDocument1 pageStetler Model EBP PosterEmily MNo ratings yet
- Alfa ArbutinDocument49 pagesAlfa ArbutinReno Vier100% (1)
- TIVA Part I - Pharmacokinetic Principles and Methods of Delivery PDFDocument56 pagesTIVA Part I - Pharmacokinetic Principles and Methods of Delivery PDFMaria José RecheNo ratings yet
- Oferta Hexis - Multisign: Preturile Sunt in EURO Si Nu Includ TVADocument9 pagesOferta Hexis - Multisign: Preturile Sunt in EURO Si Nu Includ TVAPoschina CiprianNo ratings yet
- Snap Glass CleanerDocument7 pagesSnap Glass Cleanerlovenan02No ratings yet
- Michael DeLong V Oklahoma Mental Health: PetitionDocument30 pagesMichael DeLong V Oklahoma Mental Health: PetitionTony OrtegaNo ratings yet
- Package List Swasthysathi 2018-Grade BDocument150 pagesPackage List Swasthysathi 2018-Grade BKuntal GuptaNo ratings yet
- Tushar FinalDocument29 pagesTushar FinalRaj Prixit RathoreNo ratings yet
- 11 - Comfort, Rest and Sleep Copy 6Document28 pages11 - Comfort, Rest and Sleep Copy 6Abdallah AlasalNo ratings yet
- Boy Scouts Lipa City Investiture CampDocument1 pageBoy Scouts Lipa City Investiture CampAndro Brendo VillapandoNo ratings yet
- Class 7 PolityDocument10 pagesClass 7 PolityNakka nikithaNo ratings yet
- Crodua Prioritization TableDocument10 pagesCrodua Prioritization TableThea DuoNo ratings yet
- 31congenital GlaucomasDocument12 pages31congenital GlaucomasShari' Si WahyuNo ratings yet
- UNIT-I (A) - Hospital and It's OrganizationDocument25 pagesUNIT-I (A) - Hospital and It's Organizationrajeshwari ninaweNo ratings yet
- Benign Breast DiseaseDocument26 pagesBenign Breast DiseaseMedicine 0786No ratings yet
- The Differential Diagnosis of Fluoride and Non-Fluoride OpacitiesDocument4 pagesThe Differential Diagnosis of Fluoride and Non-Fluoride OpacitiesRajshekhar BanerjeeNo ratings yet
- Pricelist Aleena Skin Clinic KendariDocument2 pagesPricelist Aleena Skin Clinic Kendariwildan acalipha wilkensiaNo ratings yet
- Reiki Tummo Brochure 2013Document2 pagesReiki Tummo Brochure 2013Alicia TerryNo ratings yet
- Legal Medicine 2020 2021Document4 pagesLegal Medicine 2020 2021Zie DammiNo ratings yet
- Assessed Conference Presentations ScheduleDocument2 pagesAssessed Conference Presentations ScheduleAna Maria Uribe AguirreNo ratings yet
- Artikel 3Document23 pagesArtikel 3Hadian UwuoNo ratings yet
- Lester Desjarlais Inquest Parts I and IIDocument108 pagesLester Desjarlais Inquest Parts I and IIJames Turner100% (1)
- Full Plate Diet BookDocument164 pagesFull Plate Diet BookScarlettNyx100% (4)
- Jacked at Home - Bodyweight Muscle-Building WorkoutsDocument6 pagesJacked at Home - Bodyweight Muscle-Building Workoutsmohamed aliNo ratings yet
- PIDSR Other DiseasesDocument45 pagesPIDSR Other DiseasesMichelle TuraNo ratings yet
- BAH Press Release (Feb. 20, 2023)Document1 pageBAH Press Release (Feb. 20, 2023)Sinclair Broadcast Group - EugeneNo ratings yet
- Table : Number of Population, Hospitals and Beds in All Over JordanDocument8 pagesTable : Number of Population, Hospitals and Beds in All Over JordanjNo ratings yet
- K55 MSDSDocument7 pagesK55 MSDSalocNo ratings yet
- Lesson 1 Local Government's Historical BackgroundDocument16 pagesLesson 1 Local Government's Historical BackgroundLorienelNo ratings yet