Professional Documents
Culture Documents
Love Hormone
Uploaded by
Nanda Nabilah UbayCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Love Hormone
Uploaded by
Nanda Nabilah UbayCopyright:
Available Formats
MINI REVIEW
published: 18 May 2015
doi: 10.3389/fendo.2015.00079
The love hormone oxytocin
regulates the loss and gain of the
fatbone relationship
Graziana Colaianni 1 *, Li Sun 2 , Mone Zaidi 2 and Alberta Zallone 1
1
Department of Basic Medical Science, Neuroscience and Sense Organs, University of Bari, Bari, Italy, 2 Mount Sinai Bone
Program, Mount Sinai School of Medicine, New York, NY, USA
Edited by:
Ez-Zoubir Amri,
University of Nice-Sophia Antipolis,
France
Reviewed by:
Marcel Scheideler,
Helmholtz Zentrum Mnchen,
Germany
Eija Pllnen,
University of Jyvskyl, Finland
Liou Sun,
Southern Illinois University School of
Medicine, USA
*Correspondence:
Graziana Colaianni,
Section of Human Anatomy and
Histology, Department of Basic
Medical Sciences, Neuroscience and
Sense Organs, University of Bari,
Piazza Giulio Cesare 11, Bari 70124,
Italy
graziana.colaianni@libero.it
Specialty section:
This article was submitted to
Endocrinology of Aging, a section of
the journal Frontiers in Endocrinology
Received: 28 February 2015
Paper pending published:
28 March 2015
Accepted: 30 April 2015
Published: 18 May 2015
Citation:
Colaianni G, Sun L, Zaidi M and
Zallone A (2015) The love hormone
oxytocin regulates the loss and gain
of the fatbone relationship.
Front. Endocrinol. 6:79.
doi: 10.3389/fendo.2015.00079
The involvement of oxytocin (OT) in bone metabolism is an interesting area of research
that recently achieved remarkable results. Moreover, several lines of evidence have
largely demonstrated that OT also participates in the regulation of energy metabolism.
Hence, it has recently been determined that the posterior pituitary hormone OT directly
regulates bone mass: mice lacking OT or OT receptor display severe osteopenia,
caused by impaired bone formation. OT administration normalizes ovariectomy-induced
osteopenia, bone marrow adiposity, body weight, and intra-abdominal fat depots in
mice. This effect is mediated through inhibition of adipocyte precursor differentiation and
reduction of adipocyte size. The exquisite role of OT in regulating the bonefat connection
adds another milestone to the biological evidence supporting the existence of a tight
relationship between the adipose tissue and the skeleton.
Keywords: oxytocin, bone, fat, muscle, hormone
Introduction
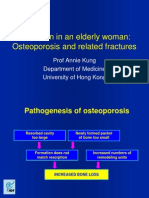
Aging is associated with high incidence to develop both obesity and osteoporosis (1), which are often
simultaneous pathological conditions deriving from an altered balance between fat and bone cells
in bone marrow. During menopause period, the onset or worsening of obesity and osteoporosis
dramatically occurs. Several pharmacologic strategies exert opposite effects on fat versus bone
mass. For instance, the sex hormone replacement treatment has proved to be effective in mitigating
bone loss (2, 3) and reversing menopause-related obesity (4). Likewise, but with opposite effect,
therapy with glucocorticoids could affect bone remodeling (57) and increase obesity (8) or bone
marrow infiltration by adipocytes (1). The ongoing studies on the balance of adipose and bone
cell differentiation in bone marrow have clearly established a negative association between fat and
bone mass. Adipocytes and osteoblasts originate from a common mesenchymal precursor that can
also differentiate into other cell types, but among the various fates, differentiation of adipocyte or
osteoblast becomes of particular relevance because factors that enable osteoblastogenesis inhibit
adipogenesis and vice versa.
Recent studies have grown the interest on pituitary hormones as endocrine skeletal regulators,
demonstrating that their levels correlate with bone microstructure and bone turnover markers
during menopause transition (9). In fact, the pituitarybone axis importance is widely acknowledged, demonstrating that several pituitary hormones, such as growth hormone (GH) (10), follicle
stimulating hormone (FSH) (11), thyroid stimulating hormone (TSH) (12), prolactin (PRL) (13),
oxytocin (OT) (14), and vasopressin (15) regulate skeletal homeostasis. Likewise, haploinsufficient
mice for pituitary hormones or their receptors showed severe skeleton defects while the primary
target organ could remain unaffected, indicating that the skeleton is more responsible to the pituitary
Frontiers in Endocrinology | www.frontiersin.org
May 2015 | Volume 6 | Article 79
Colaianni et al.
Oxytocin controls the bonefatmuscle axis
hormone control (1015). Remarkably, haploinsufficient OT+/
or OTR+/ mice, while lactating normally, exhibit profound
osteopenia (14). In humans, plasma OT levels directly correlate
with the development of osteopenia or osteoporosis in postmenopausal women, as demonstrated by Breuil et al. (16, 17). In
their studies, authors showed that elevated OT levels are associated
with high-bone mineral density (BMD), in particular, at the hip
of women with low estradiol or high-leptin serum levels (16).
Likewise, osteoporotic patients with low OT serum levels display
severe osteoporosis (17), and this association is independent from
other factors regulating OT serum levels, such as estradiol or
leptin (17).
Furthermore, several reports demonstrated that adipocytes
express OT receptors (OTRs) (18, 19). Elabd et al. (19) identified
OTR as a potential regulator of the osteoblast/adipocyte balance
in human multipotent adipose-derived stem (hMADS) cells. Both
OT and carbetocin (a stable OT analog) negatively modulated
adipogenesis while promoting osteogenesis in both hMADS cells
and human bone marrow mesenchymal stromal cells (19).
Notably, another recent study of Elabd and colleagues (20)
revealed that OT acts directly on muscle stem cells, exerting a promyogenic effects mediated by MAPK/ERK signaling. Additionally, authors reported that plasma OT levels and OTR expression
in muscle stem cells dramatically decline during aging, demonstrating that OT has a pivotal role also in homeostasis of skeletal
muscle tissue (20).
The main goal of researches on OT physiology has been to
gather new insights in the bonefatmuscle connection, in order
to prevent and treat diseases related to the altered communication
among these tissues. For instance, during aging, the lack of mobility due to muscle mass decline could exacerbate obesity and/or
osteoporosis and vice versa. On the other hand, obesity also leads
to metabolic disorders, which in turn stimulates muscle wasting
and bone loss. Although the therapeutic potential of OT to treat
musculoskeletal and metabolic conditions in humans remains
to be determined, data from OT deficient rodent models have
revealed encouraging results (Table 1).
17-estradiolBSA conjugate has shown to be effective in stimulating Erk1/2 phosphorylation within 3 min and OT expression
within 2 h (23). On the contrary, native 17-estradiol, but not
the estradiolBSA conjugate, increased OTR expression at ~6 h,
indicating that OTR induction by estrogen occurs through a traditional genomic mechanism (23). This local circuit of OT produced
in bone, in response to estrogen, acts upon OTR to stimulate
further OT release, which enhances estrogen action (23).
OT Directly Regulates Bone Homeostasis
The maximal fetal and post-natal bone growth occurs during
the last phase of pregnancy and lactation when the mother loses
~120 g of calcium from her skeleton (27). During the intergenerational calcium transfer, the fetal skeleton is mineralized at the
expense of the mother. This bone loss was quantified as 13% per
month, thus much higher than 13% of bone loss per year affecting women with postmenopausal osteoporosis (28). Experimental
evidence, demonstrating a direct action of OT on the skeleton
during pregnancy and lactation, revealed that this hormone plays
an important role in orchestrating the intergenerational calcium
transfer (29). Pups from mothers with genetic OT-deficiency
displayed apparently normal skeletons, without bone/cartilage
defects and any difference in bone volume fraction (BV/TV) of
trabecular bone. Instead, increase in trabecular number, decrease
in trabecular spacing, and no change in trabecular thickness were
found (29). However, consisting with the unchanged BV/TV, even
in the face of greater trabecular number, this result suggested that
in OT/ pups each trabecula was less mineralized than in wild
type (29).
The OT action on the skeleton is mainly mediated not only
through its stimulation of osteoblast differentiation but also
through a modulation of osteoclast formation and function. OT
and OTR knock out mice develop low turnover osteoporosis that
worsens with age in both genders (2). Bone assessment analysis
revealed a pronounced decrease in vertebral and femoral trabecular volume, already evident in the haploinsufficient mice, which
is accompanied by a significant reduction in bone formation rate
(14). Ex vivo osteoblasts from OT/ and OTR/ mice had a
lower expression of all master genes involved in osteoblast differentiation and produced fewer mineralized nodules than osteoblast
from wild-type littermates. Treatment with recombinant OT led
to up-regulation of bone morphogenetic protein 2 (Bmp-2) and
activating transriptor factor 4 (Atf-4), inducing osteoblast development toward a mineralizing phenotype (14). At the same time,
OT stimulated osteoclast differentiation by increasing ratio of
receptor activator of nuclear factor-kappaB ligand (RANK-L) and
osteoprotegerin (OPG), while inhibited bone resorption by triggering cytosolic Ca2+ release and nitric oxide synthesis (14). The
skeletal action of OT is mediated by OTR internalization and
its subsequent translocation to the nucleus through -arrestin
(Arrb). In osteoblasts, OTR interacts with Rab5 and then binds to
the karyopherin transportin-1 (Tnpo1), which facilitates nuclear
transport. OTR intracellular trafficking to the nucleus is abolished
knocking down Arrb or Tnpo1 and, consequently, the action
of OT on osteoblast differentiation genes, namely osterix, Atf-4,
bone sialoprotein, and osteocalcin is dramatically abrogated (30).
Peripheral OT Synthesis in Bone Marrow is
Estrogen Mediated
Estrogen dependence of OT and its receptors synthesis (2123)
further broadened the importance of OT/OTR biological role.
OT is locally synthesized in several organs (2426) and, like in
other tissues, estrogen stimulates OT production in bone (23).
17-estradiol stimulates OT production in osteoblasts through
Erk phosphorylation, following a non-classical, ERE-independent
pathway. The binding of 17-estradiol to cell membrane estrogen receptors (ERs), rather than nuclear ERs, is required to
induce OT synthesis. Thus, the relatively cell-impermeant analog
TABLE 1 | Mice phenotype.
OT/ OTR/ mice (male and female)
Bone tissue phenotype
Adipose tissue phenotype
Muscle tissue phenotype
Osteopenic (at the birth; worsen with age)
Obese (late-onset)
Sarcopenic (early-onset)
Frontiers in Endocrinology | www.frontiersin.org
May 2015 | Volume 6 | Article 79
Colaianni et al.
Oxytocin controls the bonefatmuscle axis
As other G protein-coupled receptors (GPCRs), OTR internalization can activate signaling pathways quite distinct from those
activated by the same receptors on the cell surface. Notably, effects
of OT on osteoblast differentiation, exerted through its nuclear
translocation, are independent of its effects on activating the
MAPK pathway. In fact, despite knocking down Arrb isoforms,
which abrogate the effects of OTR on gene expression, the pErk
signal remained unaffected (30).
were not affected by the OT treatment. Interestingly, consistent
with the normalization of body fat mass, insulin secretion was
normal, suggesting that OT might protect against ovariectomyinduced insulin resistance. Circulating levels of osteocalcin and its
undercarboxylated form were not altered following OT treatment
after ovariectomy, thus indicating that osteocalcin is not involved
in OT signaling in adipose tissue (37). Finally, the observations
that OT treatment did not significantly reduce adipocyte size, in
ovariectomy-induced hypertrophic fat depots, suggest that OT
led to a reduction of fat mass mainly through a decrease in the
formation of new adipocytes rather than a decrease of adipocyte
hypertrophy (37).
OT Reverses Ovariectomy-Induced Gain of
Fat Mass
Several lines of evidence demonstrated that OT signal and energy
homeostasis are often correlated (31, 32). Following food intake,
a peak of circulating OT levels across a 24-h period was found in
mice (31) and hypothalamic OT mRNA expression was decreased
with fasting and, subsequently, recovered upon refeeding (32).
Noteworthy, the hyperphagic obesity of single-minded 1 (Sim1)
haploinsufficient mice has been explained by reduced OT expression (33), whose obese phenotype can be rescued with OT treatment (33). Human patients suffering hyperphagia and obesity,
such as those affected by SIM1 gene mutation (34) and by
PraderWilli syndrome (35), have reduced number and size of
OT neurons in the paraventricular nucleus of the hypothalamus.
However, OT can also affect body mass independently from
reduction of food intake. Accordingly, OTR null mice develop
late-onset obesity characterized by augmentation of abdominal
fat pads, even in the face of unchanged daily intake of chow
(36). Data from Elabd et al. showed that hypogonadal-induced
bone loss and fat mass increase were both linked to low OT
circulating levels, and that restoring OT levels could therefore
reverse osteopenia and fat mass increase in OVX mice, used as
animal model mimicking the menopause (19).
It is well known that OVX mice gain body weight after surgery
and exhibit increased intra-abdominal fat mass. OVX mice treated
with OT displayed a significantly reduction in body weight compared with mice treated with vehicle. Interestingly, OT did not significantly affect the body weight of Sham operated mice. Of note,
the OT treatment was less effective in decreasing body weight
compared to the quite higher effects on bone parameters (37). Furthermore, plasma and liver triglyceride as well as glucose tolerance
Conclusion
Menopause, characterized by high-skeletal fragility and often
accompanied by increased adiposity, is a worldwide heavy burden
for public health. Osteoblasts and adipocytes, the building cells of
bone and adipose tissue, respectively, share a common origin and,
throughout life, feature an inverse relationship in their differentiation processes. Therefore, the development of new therapeutic
strategies for treating osteoporosis and obesity might require identifying signaling pathways that stimulate mesenchymal stem cells
toward osteogenesis at the expense of adipogenesis. In view of a
potential role of OT to shift the balance in favor of osteogenesis
and against adipogenesis, further investigations will be relevant
to determine if results obtained in rodents can be translated in
human subjects. Considering that OT is an FDA-approved drug,
it would be extremely useful as skeletal anabolic agent to treat
osteoporosis, but might also have potential utility in treating
obesity and adipose tissue-related pathologies. Noteworthy, recent
findings demonstrating that OT is required for muscle tissue
regeneration and homeostasis, suggested a novel potential way to
prevent sarcopenia, which often accompanies osteoporosis and
obesity during aging.
Acknowledgments
The authors are grateful to the MIUR for grant support, namely,
PRIN to AZ and to the NIH for grant support, namely, DK80459
to MZ and SL, AG40132 and AG23176 to MZ.
6. Ventura A, Brunetti G, Colucci S, Oranger A, Ladisa F, Cavallo L, et al.
Glucocorticoid-induced osteoporosis in children with 21-hydroxylase deficiency. Biomed Res Int (2013) 2013:250462. doi:10.1155/2013/250462
7. Faienza MF, Brunetti G, Colucci S, Piacente L, Ciccarelli M, Giordani L,
et al. Osteoclastogenesis in children with 21-hydroxylase deficiency on longterm glucocorticoid therapy: the role of receptor activator of nuclear factorkappaB ligand/osteoprotegerin imbalance. J Clin Endocrinol Metab (2009)
94(7):226976. doi:10.1210/jc.2008-2446
8. de Gregorio LH, Lacativa PG, Melazzi AC, Russo LA. Glucocorticoid-induced
osteoporosis. Arq Bras Endocrinol Metabol (2006) 50:793801. doi:10.1590/
S0004-27302006000400024
9. Sowers M, Jannausch M, McConnell D, Little R, Greendale GA, Finkelstein
JS, et al. Hormone predictors of bone mineral density changes during the
menopausal transition. J Clin Endocrinol Metab (2006) 91:12617. doi:10.1210/
jc.2005-1836
10. Menagh PJ, Turner RT, Jump DB, Wong CP, Lowry MB, Yakar S, et al. Growth
hormone regulates the balance between bone formation and bone marrow
adiposity. J Bone Miner Res (2010) 25:75768. doi:10.1359/jbmr.091015
References
1. Rosen CJ, Bouxsein ML. Mechanisms of disease: is osteoporosis the
obesity of bone? Nat Clin Pract Rheumatol (2006) 2:3543. doi:10.1038/
ncprheum0070
2. Colaianni G, Sun L, Di Benedetto A, Tamma R, Zhu LL, Cao J, et al. Bone
marrow oxytocin mediates the anabolic action of estrogen on the skeleton. J Biol
Chem (2012) 287(34):2915967. doi:10.1074/jbc.M112.365049
3. Manson JE, Martin KA. Postmenopausal hormone-replacement therapy. N Engl
J Med (2001) 345:3440. doi:10.1056/NEJM200107053450106
4. Sorensen MB, Rosenfalck AM, Hojgaard L, Ottesen B. Obesity and sarcopenia
after menopause are reversed by sex hormone replacement therapy. Obes Res
(2001) 9:6226. doi:10.1038/oby.2001.81
5. Brunetti G, Faienza MF, Piacente L, Ventura A, Oranger A, Carbone
C, et al. High dickkopf-1 levels in sera and leukocytes from children
with 21-hydroxylase deficiency on chronic glucocorticoid treatment. Am
J Physiol Endocrinol Metab (2013) 304(5):E54654. doi:10.1152/ajpendo.00535.
2012
Frontiers in Endocrinology | www.frontiersin.org
May 2015 | Volume 6 | Article 79
Colaianni et al.
Oxytocin controls the bonefatmuscle axis
11. Sun L, Peng Y, Sharrow AC, Iqbal J, Zhang Z, Papachristou DJ, et al. FSH
directly regulates bone mass. Cell (2006) 125(2):24760. doi:10.1016/j.cell.2006.
01.051
12. Abe E, Marians RC, Yu W, Wu XB, Ando T, Li Y, et al. TSH is a negative regulator of skeletal remodelling. Cell (2003) 115:15162. doi:10.1016/
S0092-8674(03)00771-2
13. Seriwatanachai D, Thongchote K, Charoenphandhu N, Pandaranandaka J,
Tudpor K, Teerapornpuntakit J, et al. Prolactin directly enhances bone turnover
by raising osteoblast-expressed receptor activator of nuclear factor kappaB
ligand/osteoprotegerin ratio. Bone (2008) 42:53546. doi:10.1016/j.bone.2007.
11.008
14. Tamma R, Colaianni G, Zhu LL, DiBenedetto A, Greco G, Montemurro G,
et al. Oxytocin is an anabolic bone hormone. Proc Natl Acad Sci U S A (2009)
106(17):714954. doi:10.1073/pnas.0901890106
15. Tamma R, Sun L, Cuscito C, Lu P, Corcelli M, Li J, et al. Regulation of bone
remodeling by vasopressin explains the bone loss in hyponatremia. Proc Natl
Acad Sci U S A (2013) 110(46):186449. doi:10.1073/pnas.1318257110
16. Breuil V, Panaia-Ferrari P, Fontas E, Roux C, Kolta S, Eastell R, et al. Oxytocin, a
new determinant of bone mineral density in post-menopausal women: analysis
of the OPUS cohort. J Clin Endocrinol Metab (2014) 99(4):E63441. doi:10.
1210/jc.2013-4126
17. Breuil V, Amri EZ, Panaia-Ferrari P, Testa J, Elabd C, Albert-Sabonnadire C,
et al. Oxytocin and bone remodelling: relationships with neuropituitary hormones, bone status and body composition. Joint Bone Spine (2011) 78(6):6115.
doi:10.1016/j.jbspin.2011.02.002
18. Yi KJ, So KH, Hata Y, Suzuki Y, Kato D, Watanabe K, et al. The regulation
of oxytocin receptor gene expression during adipogenesis. J Neuroendocrinol
(2015) 27(5):33542. doi:10.1111/jne.12268
19. Elabd C, Basillais A, Beaupied H, Breuil V, Wagner N, Scheideler M, et al.
Oxytocin controls differentiation of human mesenchymal stem cells and
reverses osteoporosis. Stem Cells (2008) 26(9):2399407. doi:10.1634/stemcells.
2008-0127
20. Elabd C, Cousin W, Upadhyayula P, Chen RY, Chooljian MS, Li J, et al.
Oxytocin is an age-specific circulating hormone that is necessary for muscle
maintenance and regeneration. Nat Commun (2014) 10(5):4082. doi:10.1038/
ncomms5082
21. Phaneuf S, Carrasco MP, Europe-Finner GN, Hamilton CH, Lpez Bernal A.
Multiple G proteins and phospholipase C isoforms in human myometrial cells:
implication for oxytocin action. J Clin Endocrinol Metab (1996) 81(6):2098103.
doi:10.1210/jcem.81.6.8964834
22. Tahara M, Morishige K, Sawada K, Ikebuchi Y, Kawagishi R, Tasaka K, et al.
RhoA/Rho-kinase cascade is involved in oxytocin-induced rat uterine contraction. Endocrinology (2002) 143(3):9209. doi:10.1210/endo.143.3.8696
23. Colaianni G, Di Benedetto A, Zhu LL, Tamma R, Li J, Greco G, et al. Regulated production of the pituitary hormone oxytocin from human and murine
osteoblasts. Biochem Biophys Res Commun (2011) 411:5125. doi:10.1016/j.
bbrc.2011.06.158
24. Heinrichs M, Baumgartner T, Kirschbaum C, Ehlert U. Social support and
oxytocin interact to suppress cortisol and subjective responses to psychosocial stress. Biol Psychiatry (2003) 54:138998. doi:10.1016/S0006-3223(03)
00465-7
Frontiers in Endocrinology | www.frontiersin.org
25. Jankowski M, Danalache B, Wang D, Bhat P, Hajjar F, Marcinkiewicz M, et al.
Oxytocin in cardiac ontogeny. Proc Natl Acad Sci U S A (2004) 101:130749.
doi:10.1073/pnas.0405324101
26. Thibonnier M, Conarty DM, Preston JA, Plesnicher CL, Dweik RA, Erzurum
SC. Human vascular endothelial cells express oxytocin receptors. Endocrinology
(1999) 140:13019. doi:10.1210/endo.140.3.6546
27. Kovacs CS. Calcium and bone metabolism in pregnancy and lactation. J Clin
Endocrinol Metab (2001) 86:23448. doi:10.1210/jcem.86.6.7575
28. VanHouten JN, Wysolmerski JJ. Low estrogen and high parathyroid hormonerelated peptide levels contribute to accelerated bone resorption and bone loss
in lactating mice. Endocrinology (2003) 144:55219. doi:10.1210/en.2003-0892
29. Liu X, Shimono K, Zhu LL, Li J, Peng Y, Imam A, et al. Oxytocin deficiency
impairs maternal skeletal remodeling. Biochem Biophys Res Commun (2009)
388(1):1616. doi:10.1016/j.bbrc.2009.07.148
30. Di Benedetto A, Sun L, Zambonin CG, Tamma R, Nico B, Calvano CD, et al.
Osteoblast regulation via ligand-activated nuclear trafficking of the oxytocin
receptor. Proc Natl Acad Sci U S A (2014) 111(46):165027. doi:10.1073/pnas.
1419349111
31. Zhang G, Cai D. Circadian intervention of obesity development via restingstage feeding manipulation or oxytocin treatment. Am J Physiol Endocrinol
Metab (2011) 301:E100412. doi:10.1152/ajpendo.00196.2011
32. Kublaoui BM, Gemelli T, Tolson KP, Wang Y, Zinn AR. Oxytocin deficiency
mediates hyperphagic obesity of sim1 haploinsufficient mice. Mol Endocrinol
(2008) 22:172334. doi:10.1210/me.2008-0067
33. Tolson KP, Gemelli T, Gautron L, Elmquist JK, Zinn AR, Kublaoui BM. Postnatal sim1 deficiency causes hyperphagic obesity and reduced mc4r and oxytocin
expression. J Neurosci (2010) 30:380312. doi:10.1523/JNEUROSCI.5444-09.
2010
34. Holder JL Jr, Butte NF, Zinn AR. Profound obesity associated with a balanced
translocation that disrupts the sim1 gene. Hum Mol Genet (2000) 9:1018.
doi:10.1093/hmg/9.1.101
35. Swaab DF, Purba JS, Hofman MA. Alterations in the hypothalamic paraventricular nucleus and its oxytocin neurons (putative satiety cells) in praderwilli syndrome: a study of five cases. J Clin Endocrinol Metab (1995) 80:5739.
doi:10.1210/jcem.80.2.7852523
36. Takayanagi Y, Kasahara Y, Onaka T, Takahashi N, Kawada T, Nishimori K.
Oxytocin receptor-deficient mice developed late-onset obesity. Neuroreport
(2008) 19(9):9515. doi:10.1097/WNR.0b013e3283021ca9
37. Beranger GE, Pisani DF, Castel J, Djedaini M, Battaglia S, Amiaud J, et al. Oxytocin reverses ovariectomy-induced osteopenia and body fat gain. Endocrinology (2014) 155(4):134052. doi:10.1210/en.2013-1688
Conflict of Interest Statement: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be
construed as a potential conflict of interest.
Copyright 2015 Colaianni, Sun, Zaidi and Zallone. This is an open-access article
distributed under the terms of the Creative Commons Attribution License (CC BY).
The use, distribution or reproduction in other forums is permitted, provided the
original author(s) or licensor are credited and that the original publication in this
journal is cited, in accordance with accepted academic practice. No use, distribution
or reproduction is permitted which does not comply with these terms.
May 2015 | Volume 6 | Article 79
You might also like
- Bone Aging: Anatomy and Physiology of BoneDocument7 pagesBone Aging: Anatomy and Physiology of BoneHarun NasutionNo ratings yet
- The Endocrine Role of The Skeleton: Background and Clinical EvidenceDocument9 pagesThe Endocrine Role of The Skeleton: Background and Clinical EvidenceRuth BritoNo ratings yet
- Does Obesity Protect Postmenopausal Women Against Osteoporosis?Document10 pagesDoes Obesity Protect Postmenopausal Women Against Osteoporosis?Indah MaulidawatiNo ratings yet
- Articular Cartilage and Changes in Arthritis An Introduction: Cell Biology of OsteoarthritisDocument7 pagesArticular Cartilage and Changes in Arthritis An Introduction: Cell Biology of OsteoarthritisBasheer HamidNo ratings yet
- Primary Osteoporosis in Postmenopausal WomenDocument5 pagesPrimary Osteoporosis in Postmenopausal WomenAzmi FarhadiNo ratings yet
- ArtikelDocument13 pagesArtikelAulia Rahma AgustianNo ratings yet
- Normal Bone Formation and RemodelingDocument4 pagesNormal Bone Formation and RemodelingFernando AnibanNo ratings yet
- Nutritional Zinc Plays A Pivotal Role in Bone Health and Osteoporosis PreventionDocument14 pagesNutritional Zinc Plays A Pivotal Role in Bone Health and Osteoporosis PreventionDewi HenssaNo ratings yet
- Effect of Estrogen Deficiency on Postmenopausal Bone HealthDocument10 pagesEffect of Estrogen Deficiency on Postmenopausal Bone HealthAyu Wulandari TrianggoNo ratings yet
- OsteoartritisDocument11 pagesOsteoartritisSavira Rizka MeidySNo ratings yet
- J of Bone Mineral Res - 2009 - Hamrick - Leptin Treatment Induces Loss of Bone Marrow Adipocytes and Increases BoneDocument8 pagesJ of Bone Mineral Res - 2009 - Hamrick - Leptin Treatment Induces Loss of Bone Marrow Adipocytes and Increases BoneTemtem HmNo ratings yet
- Physiologic Processes in The Skeletal SystemDocument6 pagesPhysiologic Processes in The Skeletal SystemAry Romeo ShakespeareNo ratings yet
- Review Role of Oestrogen in The Regulation of Bone Turnover at The MenarcheDocument12 pagesReview Role of Oestrogen in The Regulation of Bone Turnover at The MenarcheSherly LudjiNo ratings yet
- Pathophysiology AssignmentDocument12 pagesPathophysiology AssignmentBalqis HyoleeNo ratings yet
- Cell Lines and Primary Cell Cultures in The Study of Bone Cell Biology PDFDocument24 pagesCell Lines and Primary Cell Cultures in The Study of Bone Cell Biology PDFFilipa PereiraNo ratings yet
- Ar 3148Document12 pagesAr 3148kakashiryuNo ratings yet
- Herbal Treatment For Osteoporosis: A Current Review: Ping Chung Leung, Wing Sum SiuDocument6 pagesHerbal Treatment For Osteoporosis: A Current Review: Ping Chung Leung, Wing Sum Siusiska khairNo ratings yet
- Treatment of Postmenopausal OsteoporosisDocument8 pagesTreatment of Postmenopausal OsteoporosisLaura_Puspita__9294No ratings yet
- NejmDocument12 pagesNejmIbna Ibni IbnuNo ratings yet
- Update Osteoporosis Management (Listo)Document18 pagesUpdate Osteoporosis Management (Listo)Jossie AcuñaNo ratings yet
- Asms 07 1504Document2 pagesAsms 07 1504bushra.khairNo ratings yet
- ProjectDocument11 pagesProjectChristian AndersonNo ratings yet
- JCM 11 04676 v2Document14 pagesJCM 11 04676 v2DeepaNo ratings yet
- Osteoporosis For BonesDocument24 pagesOsteoporosis For BonesRoking KumarNo ratings yet
- Chapter 23: Osteoporosis of The SpineDocument15 pagesChapter 23: Osteoporosis of The SpineTraian UrsuNo ratings yet
- Obsop Journal 1Document14 pagesObsop Journal 1Radditt GoberNo ratings yet
- Patogenesis of Bone MetastaseDocument7 pagesPatogenesis of Bone MetastasekhairachungNo ratings yet
- Osteoporosis Associated With PregnancyDocument9 pagesOsteoporosis Associated With Pregnancysnakemamba00No ratings yet
- OsteoporosisDocument16 pagesOsteoporosisDe Sesto Rhys CarloNo ratings yet
- MT16 QSU60104 M221 | MUSCLE AND BONE PROBLEMSDocument6 pagesMT16 QSU60104 M221 | MUSCLE AND BONE PROBLEMSFOONG YI KUAN MoeNo ratings yet
- Agm2 2 147 PDFDocument10 pagesAgm2 2 147 PDFAntonioNo ratings yet
- Tea and Bone Health Steps Forward in Translational NutritionDocument6 pagesTea and Bone Health Steps Forward in Translational NutritionLandroNo ratings yet
- 1042 FullDocument9 pages1042 Fulloki harisandiNo ratings yet
- Bone Metabolism and Fracture Risk in Type 2 Diabetes MellitusDocument12 pagesBone Metabolism and Fracture Risk in Type 2 Diabetes MellituslusianapsNo ratings yet
- Stini-1990-American Journal of Physical AnthropologyDocument44 pagesStini-1990-American Journal of Physical AnthropologyIsolda Alanna RlNo ratings yet
- Osteoporosis Literature ReviewDocument5 pagesOsteoporosis Literature Reviewafmzinuvouzeny100% (1)
- Study of The Role of Leukotriene B in Abnormal Function of Human Subchondral Osteoarthritis OsteoblastsDocument9 pagesStudy of The Role of Leukotriene B in Abnormal Function of Human Subchondral Osteoarthritis OsteoblastsRifki MaulanaNo ratings yet
- Fimmu 13 1005665Document14 pagesFimmu 13 1005665sopha seyhaNo ratings yet
- OsteoblastDocument9 pagesOsteoblastPRATIK GANGULYNo ratings yet
- L36 - Back Pain in An Elderly Woman - 2012Document46 pagesL36 - Back Pain in An Elderly Woman - 2012edwinfy123No ratings yet
- Type 1 Diabetes and Osteoporosis A Review of LiteratureDocument8 pagesType 1 Diabetes and Osteoporosis A Review of LiteraturebqvlqjugfNo ratings yet
- Osteoporosis Review of EtiologyDocument17 pagesOsteoporosis Review of EtiologyClaudiaGuerreroNo ratings yet
- Streptozotocin - Type 1 Diabetes - Severity An BoneDocument20 pagesStreptozotocin - Type 1 Diabetes - Severity An BoneJonathan Santos MuñozNo ratings yet
- Relationship Between Knee and Ankle Degeneration in A Population of Organ DonorsDocument11 pagesRelationship Between Knee and Ankle Degeneration in A Population of Organ DonorsNguyễn HùngNo ratings yet
- Cellular and Molecular Mechanisms of Bone RemodelingDocument9 pagesCellular and Molecular Mechanisms of Bone RemodelingDwi Rizky LestariNo ratings yet
- tmp8ECD TMPDocument11 pagestmp8ECD TMPFrontiersNo ratings yet
- Nutrition and BoneDocument6 pagesNutrition and BonedionyessNo ratings yet
- Correlacion Osteoporosis y Enfermedad CardiovascularDocument3 pagesCorrelacion Osteoporosis y Enfermedad CardiovascularCorin Boice TelloNo ratings yet
- Duque2021 Article OsteosarcopeniaAGeriatricGiantDocument4 pagesDuque2021 Article OsteosarcopeniaAGeriatricGiantVERONICA BARRERANo ratings yet
- A Review On The Diseases and Treatments That Affect The Bone Physiology and StrengthDocument17 pagesA Review On The Diseases and Treatments That Affect The Bone Physiology and StrengthErnest Gabriel Cruz AdvinculaNo ratings yet
- Use of Non-Collagen Markers in Osteoporosis Studies: Calcified Tissue InternationalDocument5 pagesUse of Non-Collagen Markers in Osteoporosis Studies: Calcified Tissue InternationalDaniel SilvaNo ratings yet
- Osteoporosis Bone Remodeling and Risk FactorsDocument2 pagesOsteoporosis Bone Remodeling and Risk Factorsbiologoroger3637No ratings yet
- Role of Exercise in Post-Menopausal WomenDocument15 pagesRole of Exercise in Post-Menopausal Womenapi-304463583No ratings yet
- Antioxidants ARANDANO PDFDocument20 pagesAntioxidants ARANDANO PDFjairo perdomoNo ratings yet
- Short Communication: Dietary Bovine Milk-Derived Exosomes: Improve Bone Health in An Osteoporosis-Induced Mouse ModelDocument9 pagesShort Communication: Dietary Bovine Milk-Derived Exosomes: Improve Bone Health in An Osteoporosis-Induced Mouse ModelIneke NabilahNo ratings yet
- Pathogenesis of Osteoporosis 2: Cli Ord J. RosenDocument13 pagesPathogenesis of Osteoporosis 2: Cli Ord J. RosenRonald TejoprayitnoNo ratings yet
- (1479683X - European Journal of Endocrinology) FSHR Gene Polymorphisms Influence Bone Mineral Density and Bone Turnover in Postmenopausal WomenDocument8 pages(1479683X - European Journal of Endocrinology) FSHR Gene Polymorphisms Influence Bone Mineral Density and Bone Turnover in Postmenopausal WomenPoldo ReinaldoNo ratings yet
- Obesity and Osteoarthritis: More Complex Than Predicted!Document3 pagesObesity and Osteoarthritis: More Complex Than Predicted!Linda FatrisiaNo ratings yet
- Nutrients 10 01103 v2Document21 pagesNutrients 10 01103 v2Ida Ayu LitaNo ratings yet
- Free Certificate Templates from HloomDocument1 pageFree Certificate Templates from HloomNanda Nabilah UbayNo ratings yet
- Workshop Participation CertificateDocument1 pageWorkshop Participation CertificateNanda Nabilah UbayNo ratings yet
- Scholarship Award CertificateDocument1 pageScholarship Award CertificateNanda Nabilah UbayNo ratings yet
- Sample of Certificates of Appreciation TemplateDocument1 pageSample of Certificates of Appreciation TemplateNanda Nabilah UbayNo ratings yet
- Certificate of Appreciation For DonationDocument2 pagesCertificate of Appreciation For DonationNanda Nabilah UbayNo ratings yet
- Printable Certificate of ParticipationDocument1 pagePrintable Certificate of ParticipationNanda Nabilah UbayNo ratings yet
- Graduation Certificate TemplateDocument1 pageGraduation Certificate TemplateNanda Nabilah UbayNo ratings yet
- FlowchartDocument1 pageFlowchartNanda Nabilah UbayNo ratings yet
- Application Form Unilever General 2013 - tcm108-348092Document8 pagesApplication Form Unilever General 2013 - tcm108-348092Nanda Nabilah UbayNo ratings yet
- Nomer TogelDocument2 pagesNomer TogelNanda Nabilah UbayNo ratings yet
- CobasDocument8 pagesCobasNanda Nabilah UbayNo ratings yet
- Direct LDL-C Assay KitDocument2 pagesDirect LDL-C Assay KitNanda Nabilah UbayNo ratings yet
- Good Laboratory Practice Bahasa IndonesiaDocument3 pagesGood Laboratory Practice Bahasa IndonesiaMuhammad Thoriqur Rohman Al-KhotamiNo ratings yet
- Lesson 74Document12 pagesLesson 74Nanda Nabilah UbayNo ratings yet
- Measuring small, dense LDL cholesterolDocument2 pagesMeasuring small, dense LDL cholesterolNanda Nabilah UbayNo ratings yet
- MltiruleDocument15 pagesMltiruleNanda Nabilah UbayNo ratings yet
- API 20 E Part IDocument5 pagesAPI 20 E Part IÖzgür ÇanakNo ratings yet
- Spider-80 API Product BrochureDocument5 pagesSpider-80 API Product BrochureNanda Nabilah UbayNo ratings yet
- A Sty Is An Acute Infection of The Secretory Glands of The EyelidsDocument1 pageA Sty Is An Acute Infection of The Secretory Glands of The EyelidsNanda Nabilah UbayNo ratings yet
- Gravimetric Analysis Lab ReportDocument5 pagesGravimetric Analysis Lab Reportclaire_miller_16100% (1)
- Features General Description: 3A 24V 340Khz Synchronous Buck ConverterDocument18 pagesFeatures General Description: 3A 24V 340Khz Synchronous Buck ConverterAntonioNobregaNo ratings yet
- Orrick PostedbyrequestDocument4 pagesOrrick PostedbyrequestmungagungadinNo ratings yet
- Pick The Gender of Your Baby - Free EditionDocument26 pagesPick The Gender of Your Baby - Free EditionAlicia Adrianti0% (1)
- Dental Radiographs and Photographs in Human Forensic IdentificationDocument8 pagesDental Radiographs and Photographs in Human Forensic IdentificationBudi PurnomoNo ratings yet
- Hydraulic Power Steering System Design PDFDocument16 pagesHydraulic Power Steering System Design PDFAdrianBirsan100% (1)
- Finite Element Simplified Fatigue AnalysisDocument4 pagesFinite Element Simplified Fatigue AnalysisJin Hwan KimNo ratings yet
- ASIAN LIVESTOCK PERSPECTIVESDocument18 pagesASIAN LIVESTOCK PERSPECTIVESMuadz AbdurrahmanNo ratings yet
- 1.1 Hardware and SoftwareDocument13 pages1.1 Hardware and SoftwareNurhanis SyazwaniNo ratings yet
- Fundamentals of VolleyballDocument2 pagesFundamentals of VolleyballLawrence CezarNo ratings yet
- Civil Engineering Subjects (1st - 5th Year) - 1Document5 pagesCivil Engineering Subjects (1st - 5th Year) - 1Vincent TayagNo ratings yet
- Ped 201 Toddler Observation LabDocument6 pagesPed 201 Toddler Observation Labapi-477856901No ratings yet
- Shakes Beer: Specialty CocktailsDocument2 pagesShakes Beer: Specialty CocktailsGilberto Luiz MeleiroNo ratings yet
- Operating and Installation Guide For The Digital Instrument: Motoscope Tiny / Speedster / VintageDocument12 pagesOperating and Installation Guide For The Digital Instrument: Motoscope Tiny / Speedster / Vintagepeter timmermansNo ratings yet
- General Psychology - Unit 2Document23 pagesGeneral Psychology - Unit 2shivapriya ananthanarayananNo ratings yet
- ETHICS NOTES PART 1 - IAS PCS PathshalaDocument15 pagesETHICS NOTES PART 1 - IAS PCS PathshalaATULNo ratings yet
- Dimensions and Relations of The Dentogingival Junction in Humans. Gargiulo 1961Document7 pagesDimensions and Relations of The Dentogingival Junction in Humans. Gargiulo 1961Linda Garcia PNo ratings yet
- English Qualification TestDocument5 pagesEnglish Qualification TestMoh FaisolNo ratings yet
- Rapid Communication: Spontaneous Abortions and Policies On COVID-19 mRNA Vaccine Use During PregnancyDocument14 pagesRapid Communication: Spontaneous Abortions and Policies On COVID-19 mRNA Vaccine Use During PregnancyStéphane BoucherNo ratings yet
- Secretary Birds: Fascinating Hunters of the African SavannahDocument32 pagesSecretary Birds: Fascinating Hunters of the African Savannahpwint phyu kyawNo ratings yet
- The LM393Document2 pagesThe LM393mayron vasquezNo ratings yet
- Manoeuvrability Final EditedDocument12 pagesManoeuvrability Final EditedSaptarshi BasuNo ratings yet
- GSM Based Power Grid Monitoring SystemDocument41 pagesGSM Based Power Grid Monitoring SystemPreetham SurepallyNo ratings yet
- HHG4M - Lifespan Development Textbook Lesson 4Document88 pagesHHG4M - Lifespan Development Textbook Lesson 4Lubomira SucheckiNo ratings yet
- Manual of Curatorship: A Guide To Museum PracticeDocument7 pagesManual of Curatorship: A Guide To Museum PracticeLuísa MenezesNo ratings yet
- Makalah Bahasa Inggris - Narrative TextDocument21 pagesMakalah Bahasa Inggris - Narrative TextFenny KartikaNo ratings yet
- Reference Design Hardware Guide for EVM CE-2Document7 pagesReference Design Hardware Guide for EVM CE-2Angie FoleyNo ratings yet
- Infinera Product BrochureDocument4 pagesInfinera Product Brochurebarry_fieldNo ratings yet
- Chemistry How To Make Stuff PDFDocument184 pagesChemistry How To Make Stuff PDF2967449CEENo ratings yet
- MATERIAL SAFETY DATA SHEET FOR PREVENTOL-D6 PRESERVATIVEDocument3 pagesMATERIAL SAFETY DATA SHEET FOR PREVENTOL-D6 PRESERVATIVEAkshay PushpanNo ratings yet