Professional Documents
Culture Documents
Case 2 Almost
Uploaded by
Roberto RamosCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case 2 Almost
Uploaded by
Roberto RamosCopyright:
Available Formats
University of Puerto Rico
Medical Sciences Campus
School of Medicine
Department of Medicine
CASE PRESENTATION
Student's Name:
Raymond Rivera Vergara
Patient's Initials:
DMU
Student Number:
801-07-7280
Date of Encounter:
JAN 3, 2015
_________________________________________________________________________________
Chief Complaint:
" Me senti bien debil, con escalofrios, diarreas y vomitos y mi hijo me llevo al hospital"
History of Present Illness:
DMU is a 85 year old male patient with history of diabetes mellitus type II, chronic pancreatitis, duodenal ulcers
and hypercholesterolemia, that was in his usual state of health and full independence of daily living until the
approximately the beginning of December patient began with nausea, dry cough, watery diarrhea, chills and
change on eyes colors to yellow. Patient said that he had a thermometer and his highest temperature was
98.7F, therefore denning fever. He also denied abdominal pain. He eat a vegetarian diet, with low fat content
motivated by animal well being and personal preference respectively. He refers that during this month, he
developed 4 episodes sporadically with above symptoms and lost around 10 pounds. Patient refers that on
December 30, 2017 he felt worse than ever and his grandson decided to call the ambulance to take patient to
hospital.
He did not come to VA emergency room because ambulance was not allowed to come to VA emergency room
so he was taken to Hospital Buen Samaritano. There he was hospitalized with the diagnosis of obstructive
jaundice, suspected cholangitis, pancreatitis and bronchial pneumonia. Studies done on Buen Samaritano were
abdominal/pelvic CT and abdominal sonogram. Abdominal/pelvic CT shows cystic duct stone, biliary tract and
common bile duct multiple stones resulting in obstructive jaundice with intrahepatic biliary ductal dilatation.
Abdominal sonogram remarkable for compatible with intrahepatic and extrahepatic biliary ductal dilatation likely
from biliary tract obstruction secondary to choledocholitiasis; the common bile duct measures 13mm in diameter
and the pancreas demonstrates slight ill defined echo texture that may represent early pancreatitis. Patient
there was treated with Zosyn and Levaquin. He refers not being evaluated by GI service.
Patient transfered VA hospital for further care and for evaluation by GI service on December 30, 2017.
Magnetic Resonance Cholangiopancreatography (MRCP) done on December 31, 2016 shows extensive
choledocholithiasis and enhancement of the common bile duct walls.
Endoscopic retrograde cholangiopancreatography (ERCP), which will be done tomorrow (January 4, 2015)
Patient now refers feeling marked improvement. He is currently in liquid diet, with some flatulences discomfort.
Case Presentation - Page 2
Allergies:
Aspirin and Penicillin
Childhood illnesses:
None
Adult medical history:
Diabetes mellitus type II, chronic pancreatitis depression, duodenal ulcers, low back pain,
diabetic neuropathy, macular degeneration, lumbar radiculopathy, hypercholesterolemia,
Medications (include doses): Acetaminophen: 650mg. two 325mg tablets po q6h prn
Atorvastatin calcium : 40mg. Give half of 80mg tab po at bedtime
Buspirone hcl 5mg tab 1 tablet po am-pm
Cholecalciferol (vit d3) 1,000unit tab 2000units po daily
Clotrimazole 1% top soln a small amount top bid
Gabapentin 400mg cap 1 capsule po bid and at-bedtime
Insulin glargine,human 100 unt/ml inj 20 units sc at bedtime
Latanoprost 0.005% oph soln 1 drop ou at bedtime
Multivit/ophth areds2/lute/zeax cap/tab 1 capsule po bid
Omeprazole 20mg ec cap 1 capsule po daily
Trazodone hcl 50mg tab 1 tablet po at bedtime
Zolpidem tartrate 5mg tab 1 tablet po at bedtime
Surgical history:
Inpt Meds Only (that are not on Outpt)
March 14, 2015 phacoemulsification and intraocular right eye, September 11, July 16, May 19
and March 14, 2015: Avastin intravitreal injection in left eye.Pancreatitis Surgery(unkn + 10Yrs)
Family history:
Father: Died from a pulmonary embolism
Mother: Died from heart complication
Older Brother: Drug overdose by malpractice hospitalization.
Social history:
Alcohol: Drank for many years, quit 22 years ago, Tobacco: smoked 1ppd for 30 years, quit 18
years ago. Married: More than 40 years, work on plummer and electronics.
Review of systems:
Yes
No
SYSTEM
General:
Recent weight loss
Recent weight gain
Weakness
Fatigue
Fever
Chills
Skin:
Rashes
Lumps
Sores
Itching
Dryness
Yes
No
SYSTEM
Changes in skin color
Changes in hair
Changes in nails
Changes in size or color of moles
Head, Eyes, Ears, Nose & Throat
Headache
Dizziness
Lightheadedness
Loss of vision
Wears glasses or contact lenses
Eye pain
Redness of the eyes
Excessive tearing
Case Presentation - Page 3
Yes
No
SYSTEM
Yes
No
SYSTEM
Head, Eyes, Ears, Nose & Throat
Cardiovascular
Blurred vision
Paroxysmal nocturnal dyspnea
Double vision
Edema
Spots, flecks, flashing lights
Gastrointestinal
Loss of hearing
Trouble swallowing
Tinnitus
Heartburn
Vertigo
Loss of appetite
Earache
Nausea and/or vomiting
Ear discharge
Change in bowel habits
Frequent ear infections
Change in stool color
Frequent colds
Change in stool consistency
Nasal stuffiness
Pain with defecation
Nasal discharge
Rectal bleeding
Nosebleeds
Tarry black stools
Sinus pain
Hemorrhoids
Neck
Constipation
Swollen glands or lumps
Diarrhea
Goiter
Abdominal pain
Pain
Excessive belching
Stiffness
Excessive flatulence
Breasts
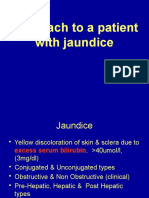
Jaundice
Lumps
Peripheral Vacular
Pain
Intermittent claudication
Discomfort
Leg cramps
Nipple discharge
Varicose veins
Respiratory
Ulcers
Cough
Past clots in veins
Sputum
Swelling of calves, legs or feet
Hemoptysis
Color change in fingertips or toes when cold
Dyspnea
Urinary
Wheezing
Increased frequency
Pleurisy
Nocturia
Cardiovascular
Urgency
History of heart murmurs
Burning or pain during urination
Chest pain or discomfort
Frequent urinary infections
Palpitations
Flank pain
Dyspnea on exertion
History of kidney stones
Orthopnea
Hematuria
Case Presentation - Page 4
Yes
No
SYSTEM
Yes
No
SYSTEM
Urinary (Male)
Neurologic
Reduced caliber or force of urinary stream
Changes in speech
Hesitancy
Changes in orientation
Dribbling
Frequent headaches
Genital (Male)
Dizziness
Hernias
Fainting or blackouts
Discharge from penis
Weakness
Sores or ulcers
Paralysis
Testicular pain
Numbness or loss of sensation
Testicular masses
Tingling sensation
Scrotal swelling
Tremors
History of sexually transmitted disease
Involuntary movements
Genital (Female)
Seizures
Irregular menses
Hematologic
Prolonged menses
History of anemia
Excessive bleeding
Easy bruising
Bleeding between periods
Excessive bleeding
Dysmenorrhea
Past transfusions
Menopause
Endocrine
Menopausal symptoms ("hot flushes")
Heat or cold intolerance
Postmenopausal bleeding
Excessive sweating
Vaginal discharge
Excessive sweat or hunger
Vaginal itching
Polyuria
Sores, ulcers or lumps
Changes in shoe or glove size
History of sexually transmitted diseases
Musculoskeletal
Muscle pain
Joint pain
Backache
Swelling of the joints
Stiffness of the joints
Muscular weakness
Limitation of motion
History of fractures or trauma
Psychiatric
Nervousness
Anxiety
Depressed mood
Health Maintenance:
Vaccinations
Hepatitis B
Last Dose
unknown
Influenza
10/14/2009
Measles-Mumps-Rubella
unknown
Pneumococcal
09/19/2003
Tetanus toxoid
07/18/2006
Varicella
not done
Case Presentation - Page 5
Health Maintenance:
Screening
Last Performed
Bone densitometry
Screening
Last Performed
Lipid profile
Not done
Colonoscopy
10-20 years ago.
Mammography
N/A
Diabetes screening
already +
Pap smear
N/A
Physical Exam:
Vital signs:
Temperature
Weight
Normal
Abnormal
98F
135.2lb
Heart rate
Height
74
5.6 ft
Respirations
BMI
SYSTEM
19
Blood pressure
Pain
Skin: Moist skin. No ulcers, rashes, or lumps. Normal hair
and nails. No jaundice.
Neck: No palpable masses or lumps. No goiter. Neck supple.
No palpable lymph nodes. No jugular venous distention. No
carotid bruits.
Thorax and Lungs: No tenderness to palpation of spinal
processes. Normal lung expansion. Normal tactile fremitus
No egophony or whispered pectoriloquy. Lungs clear to
auscultation with no ronchi, crackles or wheezing.
Breasts and Axillae: No lumps or masses. No discharge.
Heart: Non-displaced apex. Regular rhythm. Normal S1
and S2. No S3 or S4. No audible murmurs. No clicks, rubs
or other sounds.
Abdomen: Normal bowel sounds. No abdominal bruits
No tenderness to palpation. No masses. Normal liver span.
No splenomegaly. No ascites.
Extremities: No ulcers or discoloration. No edema.
Peripheral pulses +2 throughout. No deformities of the
joints. Normal range of motion. Normal muscle bulk and
tone.
ABNORMAL FINDINGS
General: Alert, awake, and oriented. Appropriate grooming
and hygiene. No acute distress.
HEENT: Normocephalic. Sclearea white. Normal visual
acuity. Pupils equally reactive to light. Normal eye fundi.
Normal ear canal. Weber midlince. Rinne AC>BC.
Normal nasal mucosa. No sinus tenderness. Moist oral
muscosa. Good dentition. No erythema or exudates.
157/76
Poor visual acuity.
Case Presentation - Page 6
Normal
Abnormal
SYSTEM
ABNORMAL FINDINGS
Neurologic:
Mental status: Alert, awake, and oriented. Appropriate
speech. Normal mentation, insight, judgement, and memory.
Cranial nerves: Normal sense of smell. Normal visual
acuity, visual fields, and ocular fundi. Normal pupillary
reaction. Normal extraocular movements. Normal corneal
reflex, facial sensation, and jaw movements. Normal facial
movements. Normal hearing. Weber midline. Rinne AC>
BC. Normal swallowing and rise of the palate. Intact gag
reflex. Normal voice and speech. Normal shoulder and
neck movements. Normal tongue symmetry and position
Motor system: Normal muscle tone and bulk. Strength 5/5 in
all muscle groups. Point-to-point movements and rapid
alternating movements intact. Normal gait.
Sensory system: Normal sensation to pain, temperature,
light touch, vibration,and point discrimination.
Reflexes: Normal biceps, triceps, brachioradialis, patellar,
and Achilles deep tendon reflexes.
Motor evaluation for lower limb was
ommitted due to chronic back pain.
Patient refuses motor system
examination.
Laboratory Findings:
12.7
10.1
139
99
14.9
254
38.6
202
4.6
27
0.9
Segmented neutrophils
62.1%
Aspartate dehydrogenase (AST)
24
Lymphocytes
21.4%
Alanine dehydrogenase (ALT)
38
Eosinophils
6.1%
Alkaline phosphatase
266
Monocytes
9.9%
Bilirubin, total
1.4
Mean corpuscular volume
86.7fL
Bilirubin, direct
0.8 (ind=0.6)
Mean corpuscular hemoglobin
32.9pg
Magnesium
1.6
Other relevant laboratories:
Imaging studies:
Amylase:.69, lipase, 33
MRCP December 31, 2015:
Extensive choledocholithiasis accounting for biliary obstruction. Enhancement of the
common bile duct walls may represent cholangitis in the proper clinical scenario.
Electrocardiogram:
- Normal Sinus Rhythm
- Vent Rate: 66bpm
-Chest
QTc: AP
423ms
portable view December 31, 2015:
Imaging Studies
MRCP December 31, 2015:
Extensive choledocholithiasis accounting for biliary obstruction. Enhancement of the
common bile duct walls may represent cholangitis in the proper clinical scenario.
Chest AP portable view December 31, 2015:
Mild hyperexpansion and increased pulmonary markings suggesting obstructive and
interstitial lung disease. Compare with prior, no significant acute radiographic changes are
noted.
Abdominal CT and sonogram on December 30, 2015
Abdominal/pelvic CT shows cystic duct stone, biliary tract and common bile duct multiple
stones resulting in obstructive jaundice with intrahepatic biliary ductal dilatation. Abdominal
sonogram remarkable for compatible with intrahepatic and extrahepatic biliary ductal
dilatation likely from biliary tract obstruction secondary to choledocholitiasis; the common
bile duct measures 13mm in diameter and the pancreas demonstrates slight ill defined
echo texture that may represent early pancreatitis.
Case Presentation - Page 7
Assessment:
DMU is a 85 year old male patient with history of diabetes mellitus type II, chronic pancreatitis, duodenal
ulcers and hypercholesterolemia, twas in his usual state of care until December, 2015 were he experience
around 4 episodes of nausea, dry cough, watery diarrhea, chills and change on eyes colors to yellow. On
December 30,2015 patient was hospitalized in Hospital Buen Samaritano for obstructive jaundice, suspected
cholangitis, pancreatitis and broncopulmonea. He was then transfered to VA for further care and for GI
evaluation. MRCP results showes extensive choledocholithiasis accounting for biliary obstruction.
Enhancement of the common bile duct walls may represent cholangitis in the proper clinical scenario.
Patient was evaluated at bedside upon arrival at IM ward. He was alert, awake, and oriented in all spheres.
Currently patient afebrile, normotensive, hemodynamically stable, with adequate vital signs. Physical exam
findings remarkable for the above mentioned findings. Lungs essentially clear. Normal heart sounds. Benign
abdominal exam. No focal neurological deficits. No jaundiced present at time of examination but there was
elevated alkaline phosphatase and Indirect bilirubin on laboratories done on January 3,2016. Normal
Amylase and lipase levels. alkaline phospatase levels in person more than 60 y/o tend to be 1 o 1.5 more
than normal values. therefore, alkaine phospatase should be tested together with GGC an 5' glucosidase.
In view of above mentioned history and physical exam findings, most likely diagnosis is choledocholelithiasis.
Patient with CT and sonogram from Buen Samaritano shows cystic duct stone, billiary and common bile duct
stone with intrahepatic ductal dilation. Another possible diagnosis would be pancreatitis. Patient had CT and
sonogram finding suggestive of pancreatitis. He also developed the following clinical symptoms consistent
with possible diagnosis: nausea, vomiting and diarrhea. Negative findings for diagnostic were abdominal pain,
and normal amylase (60U/L) and lipase (33 U/L) levels. It is important to mention that normal amylase and
lipase level are not sensitive for chronic pancreatitis. BISAP score value were 1 base on this laboratory
values: BUN: 14.9 (less than 25) (0), cognitive competent(0), did not met SIRS criteria(0), did not present with
pleural effusion (0) at time of osculation and on A/P CT scan and patient age is more than 60 y/o (85 y/o)
(1). This give a mortality probability of 0.4%. Nevertheless, patient has improved clinically and abdominal
exam is completely benign.
Patient was started on Zosyn and Levaquin to cover pneumonic process and abdomen flora, treating or
preventing possible cholangitis. Patient was transferred for GI evaluation and the will perform an ERCP
tomorrow for evaluation and removal of choledocholithiasis in case they are present and accessible to study.
Plan:
Will hydrate patient with Ringer's lactate, vitals will be measured every 8 hours, patient activity is limited to
bed rest and will follow a liquid diet. Patient will be evaluated on January 4, 2016 with ERCP for examination
and possible removal of choledolitiasis. Patient will be treated with Heparin for BVT prophylaxis.
References:
STUDENT SIGNATURE:
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Case 3Document8 pagesCase 3Roberto RamosNo ratings yet
- History: Chief Complaint: History of Present Illness: Patient Is A 59 Year Old G6 P1051 Woman Who Is An Inmate That WasDocument9 pagesHistory: Chief Complaint: History of Present Illness: Patient Is A 59 Year Old G6 P1051 Woman Who Is An Inmate That WasRoberto RamosNo ratings yet
- Soap RoutineDocument3 pagesSoap RoutineRoberto Ramos100% (1)
- Universidad Puerto Rico Manual 1415Document161 pagesUniversidad Puerto Rico Manual 1415Roberto RamosNo ratings yet
- Paciente 3Document80 pagesPaciente 3Roberto RamosNo ratings yet
- DR - Umpierrere2012 2013 4Document70 pagesDR - Umpierrere2012 2013 4Roberto RamosNo ratings yet
- Ob-Gyn Clerkship Daily Schedule (Aug-Sep 2015)Document3 pagesOb-Gyn Clerkship Daily Schedule (Aug-Sep 2015)Roberto RamosNo ratings yet
- HTTPDocument1 pageHTTPRoberto RamosNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Liver Abscess ThesisDocument7 pagesLiver Abscess Thesisjenniferalexanderfortlauderdale100% (1)
- Antibiotics in ICUDocument63 pagesAntibiotics in ICUsayantanNo ratings yet
- Cholestasis: Dr. Darmadi SPPD, FinasimDocument20 pagesCholestasis: Dr. Darmadi SPPD, FinasimTiens MonisaNo ratings yet
- IcdDocument30 pagesIcdSuryaAtmajayaNo ratings yet
- Management of Postcholecystectomy Biliary Complications: A Narrative ReviewDocument8 pagesManagement of Postcholecystectomy Biliary Complications: A Narrative ReviewHassanNo ratings yet
- Acute PancreatitisDocument10 pagesAcute PancreatitisAndrés Menéndez RojasNo ratings yet
- Jaundice: M.Prasad Naidu MSC Medical Biochemistry, Ph.D.Research ScholarDocument22 pagesJaundice: M.Prasad Naidu MSC Medical Biochemistry, Ph.D.Research ScholarDr. M. Prasad NaiduNo ratings yet
- Gallstone Disease: Tad Kim, M.D. Connie Lee, M.DDocument35 pagesGallstone Disease: Tad Kim, M.D. Connie Lee, M.DWorapat ChNo ratings yet
- General Surgery OME PDFDocument25 pagesGeneral Surgery OME PDFNathan Korean KimNo ratings yet
- TG 13 Updated Tokyo GuidelinesDocument8 pagesTG 13 Updated Tokyo GuidelinessamuelionardiNo ratings yet
- Benign Condition of Biliary ApparatusDocument19 pagesBenign Condition of Biliary ApparatusRiya ShindeNo ratings yet
- JAUNDICE and CHOLECYSTITISDocument109 pagesJAUNDICE and CHOLECYSTITISSarah Racheal AkelloNo ratings yet
- Theme 5. Gallstone Disease-1Document18 pagesTheme 5. Gallstone Disease-1HashmithaNo ratings yet
- Choledocholithiasis FinalDocument65 pagesCholedocholithiasis FinalClark Llamera100% (1)
- Biliary Tree LectureDocument58 pagesBiliary Tree Lecturesgod34No ratings yet
- Billiary SystemDocument60 pagesBilliary SystemDONALD UNASHENo ratings yet
- Acute CholangitisDocument12 pagesAcute CholangitisWira LinNo ratings yet
- List of Autoimmune DiseasesDocument11 pagesList of Autoimmune DiseasesDuwa AhmadNo ratings yet
- Surgery Sep+Oct+NovDocument122 pagesSurgery Sep+Oct+Novﻋﻤﻴﺪ ﺍﻟﺸﻤﻴﺮﻱNo ratings yet
- JaundiceDocument36 pagesJaundiceNasser SalahNo ratings yet
- Absite CH 32 BilliaryDocument14 pagesAbsite CH 32 BilliaryJames JosephNo ratings yet
- Autoimmune HepatitisDocument41 pagesAutoimmune HepatitisMigi Pradysta100% (1)
- Case Study SurgW FinalDocument59 pagesCase Study SurgW FinalLovely CacapitNo ratings yet
- Overview of Autoimmune Hepatitis - UpToDateDocument33 pagesOverview of Autoimmune Hepatitis - UpToDatebagir_dm10No ratings yet
- List of Medical Triads and Pentads - WikipediaDocument3 pagesList of Medical Triads and Pentads - WikipediaSubhajitPaul100% (1)
- Medical ClassificationsDocument28 pagesMedical ClassificationsluffysamaNo ratings yet
- EJMCM Volume 7 Issue 10 Pages 413-418Document6 pagesEJMCM Volume 7 Issue 10 Pages 413-418rifa iNo ratings yet
- Batu EmpeduDocument140 pagesBatu Empeduyanuar h wijayaNo ratings yet
- 1 LiverDocument10 pages1 LiverAlbino Fulgencio Santos III100% (1)
- Cholelytiasis 2013 2015Document37 pagesCholelytiasis 2013 2015Nurul RamadhantyNo ratings yet